Abstract
Objective:
The association of Fe metabolism with obesity in children remains unclear. The present study aimed to assess the status of Fe metabolism parameters, the prevalence of anaemia, Fe deficiency (ID) and Fe-deficiency anaemia (IDA), and the associations of these variables with obesity in Chinese schoolchildren.
Design:
A cross-sectional study conducted in 5295 schoolchildren aged 7–11 years in Guangzhou, China, 2014–2015. Full data of anthropometric and Fe metabolic parameters were collected to assess obesity, anaemia, ID and IDA. Logistic regression models were established to determine the possible associations of anaemia, ID and IDA with obesity. Two-tailed P values of <0·05 was considered statistically significant.
Setting:
Guangzhou City, China.
Participants:
Schoolchildren aged 7–11 years (n 5295).
Results:
In this sample, mean Hb concentration was 128·1 g/l and the prevalence of anaemia, ID and IDA was 6·6, 6·2 and 0·6 %, respectively. Of the participants, 14·0 % were overweight and 8·8 % were obese. Importantly, obesity was associated with lower anaemia risk (adjusted OR = 0·553; 95 % CI 0·316, 0·968) but higher ID risk (adjusted OR = 1·808; 95 % CI 1·146, 2·853) after adjustment for confounders. No significant relationship was found between obesity and IDA.
Conclusions:
Our results confirmed that anaemia and ID remain public health concerns among schoolchildren in Guangzhou, while IDA is remarkably less prevalent. Furthermore, obesity was associated with lower anaemia risk, but higher ID risk. More efforts should be made to prevent the onset of ID and obesity in the same individual, thus improving the health and fitness of children.
Keywords: Anaemia, Iron deficiency, Iron-deficiency anaemia, Obesity, Schoolchildren
Anaemia, Fe deficiency (ID) and Fe-deficiency anaemia (IDA) in children have long been public health concerns worldwide. ID is generally recognized as the most common micronutrient deficiency and its long-term outcome, IDA, accounts for 50 % of all anaemia(1). Prevalence of anaemia, ID and IDA varies across countries, usually being higher in low- and middle-income countries(2–4). In China, prior studies have focused mainly on pre-school children (younger than 5 years), while few studies have assessed anaemia/ID/IDA in schoolchildren (older than 5 years). Besides, with the rapidly developing economy and increasing living standard, China has become a prime example of a middle-income country in transition, with the changes in family income, food availability, nutritional status and lifestyle contributing to the ever-increasing obesity prevalence in Chinese young populations. It is time to reassess anaemia/ID/IDA status in China, especially in schoolchildren (older than 5 years). In addition, few researchers in China have tried to assess the exact levels of the Fe metabolism parameters which are usually adopted to define anaemia/ID/IDA, including Hb, serum ferritin (SF), serum Fe (SI), total Fe-binding capacity (TIBC) and transferrin saturation (TS). Considering the facts mentioned above, it is necessary to re-evaluate the status of anaemia, ID and IDA, as well as the exact levels of Fe metabolism parameters, in Chinese schoolchildren.
It is generally believed that obese children are less likely to be anaemic, since they are prone to consume more animal-based foods relatively rich in Fe, folic acid, vitamin B12 and other micronutrients that are critical to Hb formation(5–7). However, in recent years, some studies have indicated that children with obesity are more likely to develop ID and IDA than their normal-weight counterparts(8–10). In fact, research did observe decreased serum Fe level in obese individuals as early as the 1960s(11). Furthermore, a study in Iran reported that ID was three times more prevalent in children with obesity compared with those of normal weight(12). A similar association was found in the Third National Health and Nutritional Survey (NHANES) in the USA, as well as in a study including 321 Israeli children(8,13,14). Based on prior studies, researchers hypothesized that inflammation-induced hepcidin in obese individuals was likely causing decreased dietary Fe absorption, thus impairing dietary repletion efforts(15). However, no internationally recognized conclusion on the positive association between obesity and IDA has been made yet due to unclear mechanisms and the lack of longitudinal data.
China has the largest population of children and adolescents in the world, while few studies have updated the weight status of the same population in recent years. On the other hand, most of the previous studies focused on children under 5 years of age, while the situation in children older than 5 years remains uncertain and needs more investigation. That is one of the reasons why we did this research.
Given the above-mentioned facts, we assumed that the prevalence of anaemia, ID and IDA in Chinese schoolchildren is higher than that in children from most high-income countries, and that children with obesity are at increased risk for ID and IDA, but at decreased risk for anaemia, compared with those of normal weight. The current study aimed to determine the status of Fe metabolism parameters; to assess the prevalence of anaemia, ID and IDA; and to investigate the associations between anaemia/ID/IDA and obesity in schoolchildren aged 7–11 years from Guangzhou, China.
Methods
Study population
A cross-sectional study was conducted among students from fourteen primary schools in Guangzhou City, China, 2014–2015, involving standardized physical examinations, laboratory investigations and questionnaires. Children aged 7–11 years who had complete data on five Fe metabolism parameters (Hb, SF, SI, TIBC and TS) and BMI were included in our analysis (n 5295; 2866 boys and 2429 girls).
Ethics statement
The Sun Yat-sen University Institutional Review Board approved the study protocol and this study was conducted according to the guidelines laid down in the Declaration of Helsinki. Written informed consent was provided by parents or other legal guardians of the participants.
Sample size
The anaemia prevalence (7·1 %) based on our annual surveillance data in Guangzhou (2013) was adopted to calculate the sample size. The calculation result was 1564, increased to 3476 after taking account of the cluster sampling method and 90 % power.
A total of 6146 children and adolescents aged 7–11 years were initially selected via a multistage cluster sampling method. After excluding those without full blood sample and questionnaire data (13·8 %), the sample size fell to 5295, which is greater than the original calculated sample size, adequate enough to detect the statistical differences in anaemia.
Anthropometry
The anthropometric data in our study were collected by trained physicians according to standardized methods, with the participant wearing light clothing. Height was measured to the nearest 0·1 cm with a stadiometer (Yilian TZG, Jiangsu, China). Body weight was measured to the nearest 0·1 kg using a self-zeroing scale (Hengxing TGT-140, Jiangsu, China), with the participant shoeless, pockets empty and at a standing position. BMI was calculated as weight in kilograms divided by the square of height in metres.
All measurements were performed by the same group of experienced clinicians and nurses from the Health Promotion Center for Primary and Middle School Children in Guangzhou. Medical cards for participants were used to record the data standardly and accurately.
Laboratory measurements
Participants were reminded to fast for 12 h on the night before the test. Any participant who did not meet the requirement was excluded from the blood sampling. Venous blood samples were obtained from the antecubital vein before breakfast and collected into EDTA vacuum tubes, by standardly trained phlebotomists. Samples were centrifuged at 3000 rpm for 10 min at 4°C within 2 h, then stored at –80°C until analysis. Fe metabolism parameters including Hb, SF, SI, TIBC and TS were determined at a specialty laboratory accredited by Sun Yat-sen University. Hb levels were quantified on an automated haematological analyser (TC Hemaxa 1000; Teco Diagnostic, Anaheim, CA, USA), using a hemiglobincyanide method. SF concentrations were determined by the enzyme immunoassay method, using commercial kits (FERRITIN ELISA; Diametra, Boldon, UK). SI levels were determined by a commercial test using a colorimetric method (Ferentest; bioMérieux® SA, France). Quantitative determination of TIBC was assessed by colorimetric methods using commercial kits (TOTAL IRON BINDING CAPACITY ELISA Kit; Beckman Coulter, France). TS was calculated as SI value divided by TIBC value. For these parameters, the intra-assay and inter-assay CV were below 5·7 and 6·7 %, respectively.
Questionnaire
To obtain information about demographic characteristics (including age and gender), food intake, physical activity and birth weight, standardized questionnaires were provided for both children and parents, respectively. Food intake, physical activity and birth weight were assessed as follows.
Food intake
For the reason that it is relatively difficult to conduct an FFQ or 3 d dietary recall survey among such a large number of participants, a simplified self-report dietary questionnaire was adopted instead. Data on the intake of seven types of food were recorded via seven questions in the questionnaire, including the intake amount and consumption frequency of fruit, vegetables, meat, sugar-sweetened beverages, milk products, high-energy foods and fried foods. Since only fruit and meat intakes were found to be significantly associated with one of our main outcomes (anaemia) in the bivariate analysis, only data on fruit/meat were included in the final multivariate logistic regression model and presented in the results. The intakes of fruit and meat were assessed by two successive questions: ‘(i) How many days did you eat fruit/meat in the past seven days? (ii) How many servings of fruit/meat did you eat per day during the days you ate them? Fruits are the fleshy seed-associated structures of a plant that are sweet or sour and edible in the raw state, including apples, pears, bananas, oranges and so on. Meat here includes the flesh of mammalian species (e.g. pigs, cattle, lambs) and meat products (e.g. bacon and sausages). One serving of fruit equals the size of an adult’s fist, while one serving of meat equals the size of an adult’s palm’ (pictures displaying the exact size of a fist/palm were provided as references, beside the questions).
Two repeated assessments with the same self-report dietary questionnaire and a 3 d dietary record were used to evaluate the reliability and validity of the present dietary questionnaire before the study commenced. The variables of the dietary questionnaire were used to calculate intraclass correlation coefficients for reliability and Spearman’s correlation coefficients for validity. According to a sample size calculation, 298 pupils (aged 6–12 years) were recruited from a primary school to complete the evaluation. Two repeated measurements with the same dietary questionnaire were conducted with a 7 d interval and the intraclass correlation coefficient was calculated to evaluate reliability, which was from 0·443 to 0·589 (P < 0·05). The dietary questionnaire was also compared with the 3 d dietary record and the Spearman’s correlation coefficient was calculated to evaluate validity, which was from 0·344 to 0·485 (P < 0·05).
Physical activity
Data on physical activity, including vigorous-intensity activities, moderate-intensity activities, walking and sedentary behaviours, were collected by giving examples. For the reason that only moderate-intensity activity was significantly associated with one of our main outcomes (ID) in the bivariate analysis, only data on moderate-intensity activity were included in the final multivariate logistic regression model and presented in the results. Moderate-intensity activity was assessed by the question, ‘How many days and how many hours did you perform moderate-intensity activity in the past seven days? Moderate-intensity activity, including bicycling, playing table tennis, moving something light, dancing and so on, causes people to mildly perspire and experience slight exhaustion (requiring 3–6 metabolic equivalents)’.
Validity and reliability of the physical activity questionnaire were evaluated before the study commenced. The variables of the physical activity questionnaire were used to calculate intraclass correlation coefficients for reliability and Spearman’s correlation coefficients for validity. The intraclass correlation coefficient between two repeated measurements with the same questionnaire was from 0·344 to 0·485 (P < 0·05). The Spearman’s correlation coefficient for the physical activity questionnaires and a 3 d physical activity log was from 0·341 to 0·545 (P < 0·05).
Birth weight
Parents or other legal guardians were required to write down the exact birth weight of the participants (in grams) on the self-report questionnaire. Questionnaires without the record of birth weight were returned to the children and their guardians to refill.
Definitions
Anaemia/iron deficiency/iron-deficiency anaemia
Anaemia was defined as Hb < 115 g/l (for children aged 5–11 years), according to the definition proposed by WHO in 2001(1). In order to make comparisons with other studies in China, ID was defined following a multiple-index model, proposed by the Chinese Medical Association in 2010(16), as the presence of two or more of the following four abnormal values: (i) SF < 15 ng/ml; (ii) SI < 10·7 μmol/l; (iii) TIBC > 62·7 μmol/l; and (iv) TS < 15 %. Additionally, IDA was defined as the presence of both anaemia and ID in the same individual, as suggested by WHO in 2001(1).
BMI status
To investigate the associations between anaemia/ID/IDA and obesity, measured BMI was used to categorize participants into obesity (>+2), overweight (>+1 and <+2), normal weight (>–2 and <+1) and thinness (<–2), following the BMI Z-scores proposed by WHO in 2007(17).
Birth weight
According to the International Classification of Diseases, 11th Revision (ICD-11), proposed by WHO in 2018, birth weight was categorized into high birth weight (≥4000 g), normal birth weight (≥2500 g but <4000 g) and low birth weight (<2499 g, including extremely low birth weight and other low birth weight)(18).
Statistical analysis
All data were entered via EpiData3.0 software (The EpiData Association, Odense, Denmark) by double entry and validation. The collected data were analysed via the statistical software package IBM SPSS Statistics version 21.0. Group differences were analysed by one-way ANOVA for continuous variables and the χ 2 test for categorical values. Pearson correlation analysis was adopted to determine the linear correlations between Fe parameters and age.
Logistic regression models were established to assess the possible associations between anaemia/ID/IDA and different weight status (including obesity), respectively. Since food intake basically decides the intake of various nutrients (including Fe), it plays an important role in the development of anaemia/ID/IDA. Besides, physical activity as well as birth weight have already been revealed to be significantly associated with BMI and obesity. To minimize the bias in the logistic regression, we tried to put age, gender, physical activity and food intake data into a cross-tabulation or bivariate analysis model at first. Then we found that age and gender were significantly associated with all three main outcomes (anaemia/ID/IDA). However, only birth weight and fruit/meat intake were associated with anaemia, and only moderate-intensity activity was associated with ID. In this way, these factors mentioned above were included in the final three multivariate logistic regression models for anaemia, ID and IDA, respectively. Results of logistic regression were presented as adjusted odds ratios and 95 % confidence intervals, with P values. Two-tailed P values of <0·05 were considered statistically significant.
Results
Basic characteristics and iron metabolism parameters
Basic information about age, gender, anthropometry, Fe metabolism parameters, food intake, physical activity and birth weight is presented in Table 1. Overall, 5295 children (2866 boys and 2429 girls) aged 7–11 years were included in the present study, with a mean age of 8·8 years. Among the anthropometric parameters, girls had higher values in height, while boys had higher values in weight and BMI.
Table 1.
Basic characteristics of participants: schoolchildren aged 7–11 years from Guangzhou, China, 2014–2015 (n 5295)
| Overall (n 5295) | Boys (n 2866) | Girls (n 2429) | |||||
|---|---|---|---|---|---|---|---|
| Variable | Mean or /% | sd | Mean or % | sd | Mean or % | sd | P value |
| Age (years) | 8·8 | 1·4 | 8·8 | 1·4 | 8·8 | 1·4 | 0·992 |
| Anthropometry | |||||||
| Weight (kg) | 31·6 | 9·3 | 32·4 | 9·4 | 30·7 | 9·1 | <0·001* |
| Height (cm) | 136·4 | 10·3 | 136·2 | 9·8 | 136·6 | 10·8 | 0·002* |
| BMI (kg/m2) | 16·7 | 3·1 | 17·2 | 3·2 | 16·1 | 2·9 | <0·001* |
| BMI category | |||||||
| Normal | 70·0 | – | 64·8 | – | 76·2 | – | <0·001* |
| Overweight | 14·0 | – | 16·9 | – | 10·6 | – | <0·001* |
| Obesity | 8·8 | – | 12·7 | – | 4·1 | – | <0·001* |
| Thinness | 7·2 | – | 5·6 | – | 9·1 | – | <0·001* |
| Questionnaire | |||||||
| Fruit intake (servings/week) | 9·1 | 8·3 | 8·7 | 8·1 | 9·6 | 8·4 | 0·001* |
| Meat intake (servings/week) | 12·2 | 10·9 | 13·1 | 11·4 | 11·2 | 10·1 | <0·001* |
| Moderate-intensity PA (h/week) | 3·8 | 4·4 | 3·8 | 4·5 | 3·8 | 4·3 | 0·845 |
| Birth weight | |||||||
| Normal birth weight | 90·2 | – | 89·1 | – | 91·3 | – | <0·001* |
| Low birth weight | 5·4 | – | 4·8 | – | 6·0 | – | 0·026* |
| High birth weight | 4·4 | – | 6·1 | – | 2·7 | – | <0·001* |
| Fe metabolism parameters | |||||||
| Hb (g/l) | 128·1 | 8·5 | 128·4 | 8·5 | 127·7 | 8·5 | 0·005* |
| SF (ng/ml) | 72·6 | 32·1 | 73·2 | 34·2 | 71·8 | 29·3 | 0·110 |
| SI (μmol/l) | 16·7 | 5·3 | 16·3 | 5·3 | 17·1 | 5·2 | <0·001* |
| TIBC (μmol/l) | 60·0 | 6·7 | 60·4 | 6·6 | 59·7 | 6·9 | <0·001* |
| TS (%) | 28·0 | 9·2 | 27·1 | 9·1 | 29·0 | 9·2 | <0·001* |
PA, physical activity; SF, serum ferritin; SI, serum Fe; TIBC, total Fe-binding capacity; TS, transferrin saturation.
Data are presented as mean and standard deviation or as percentage.
BMI categories were defined by BMI Z-scores as proposed by WHO in 2007(17).
Fruit intake and meat intake were described by the number of servings in the past 7 d. Moderate-intensity PA was described by the time spent on moderate-intensity PA in the past 7 d.
Birth weight was categorized into low birth weight, normal birth weight and high birth weight according to the International Classification of Diseases, 11th Revision (ICD-11), proposed by WHO in 2018(18).
P < 0·05, boys v. girls, assessed by one-way ANOVA.
From the information collected by questionnaires, we found girls ate more fruits than boys, while boys ate more meat. For birth weight, more boys were born with a high birth weight (6·1 v. 2·7 %), while more girls were born with a normal (91·3 v. 89·1 %) or low birth weight (6·0 v. 4·8 %).
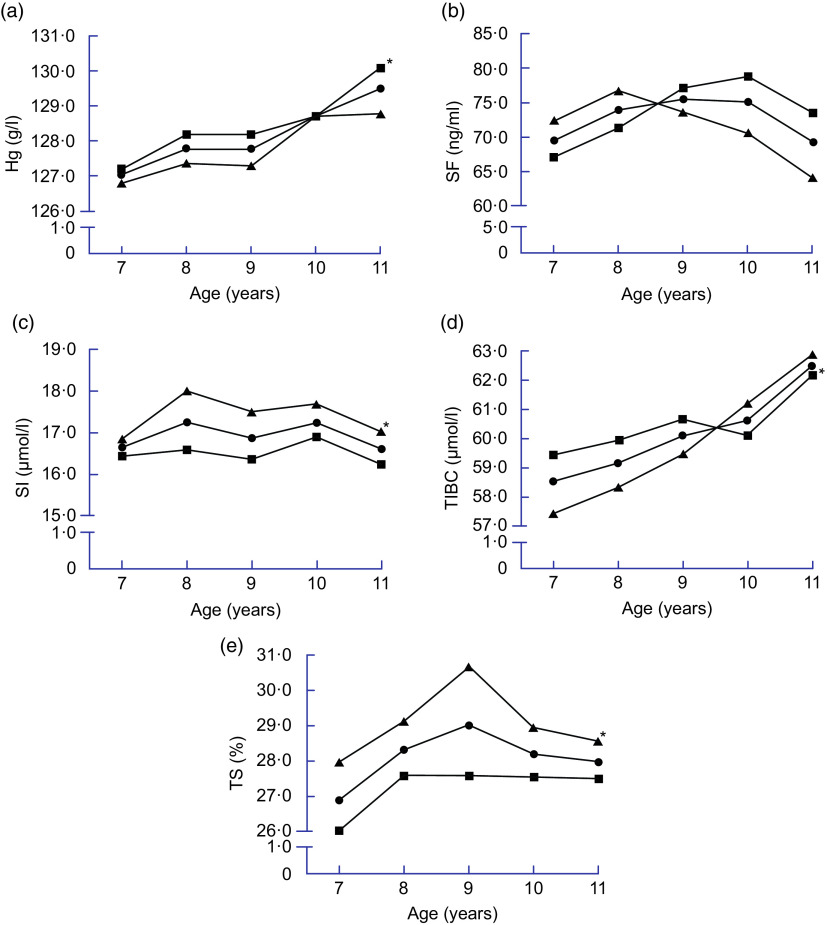
For the five Fe metabolism parameters, mean levels of Hb, SF, SI, TIBC and TS were 128·1 g/l, 72·6 ng/ml, 16·7 μmol/l, 60·0 μmol/l and 28·0 %, respectively. Distribution of individual Fe metabolism parameters by age and gender is presented in Fig. 1. Higher levels of Hb and TIBC were found in boys, while higher values of SI and TS were found in girls. There was no significant difference by gender for SF level. Besides, weak linear correlations were found between Hb/SI/TIBC levels and age by Pearson correlation analysis (Hb v. age, r = 0·09; SI v. age, r = 0·10; TIBC v. age, r = 0·19; all P < 0·05).
Fig. 1.
Distribution of individual iron metabolism parameters among schoolchildren aged 7–11 years ( , overall;
, overall;  , boys;
, boys;  , girls) from Guangzhou, China, 2014–2015 (n 5295): (a) Hb; (b) serum ferritin (SF); (c) serum iron (SI); (d) total iron-binding capacity (TIBC); (e) transferrin saturation (TS). Positive but weak linear correlations between Hb/SI/TIBC levels and age were found by Pearson correlation analysis (Hb v. age, r = 0·09; SI v. age, r = 0·10; TIBC v. age, r = 0·19; all P < 0·05). *P < 0·05, boys v. girls, assessed by one-way ANOVA
, girls) from Guangzhou, China, 2014–2015 (n 5295): (a) Hb; (b) serum ferritin (SF); (c) serum iron (SI); (d) total iron-binding capacity (TIBC); (e) transferrin saturation (TS). Positive but weak linear correlations between Hb/SI/TIBC levels and age were found by Pearson correlation analysis (Hb v. age, r = 0·09; SI v. age, r = 0·10; TIBC v. age, r = 0·19; all P < 0·05). *P < 0·05, boys v. girls, assessed by one-way ANOVA
Prevalence of anaemia, iron deficiency and iron-deficiency anaemia
Anaemia was found in 6·6 % of the 5295 participants (6·2 % of boys, 7·0 % of girls; Table 2). At the age of 7 years, girls had significantly higher anaemia prevalence than did boys, while no gender differences were found in other age groups.
Table 2.
Prevalence of anaemia, iron deficiency (ID) and iron-deficiency anaemia (IDA) among schoolchildren aged 7–11 years from Guangzhou, China, 2014–2015
| Age (years) | n | Overall (n 5295) |
Boys (n 2866) |
Girls (n 2429) |
P value |
|---|---|---|---|---|---|
| Anaemia (%) | |||||
| 7 | 1273 | 7·1 | 5·8 | 8·7 | 0·048* |
| 8 | 1099 | 6·7 | 7·2 | 6·3 | 0·549 |
| 9 | 1005 | 6·7 | 6·5 | 6·9 | 0·800 |
| 10 | 1027 | 5·4 | 5·2 | 5·6 | 0·783 |
| 11 | 891 | 7·1 | 6·8 | 7·4 | 0·707 |
| 7–8 | 2372 | 6·9 | 6·4 | 7·5 | 0·296 |
| 9–11† | 2923 | 6·3 | 6·1 | 6·6 | 0·600 |
| Total | 5295 | 6·6 | 6·2 | 7·0 | 0·271 |
| ID (%) | |||||
| 7 | 1273 | 8·0 | 9·5 | 6·2 | 0·032* |
| 8 | 1099 | 6·4 | 7·9 | 4·7 | 0·034* |
| 9 | 1005 | 5·2 | 6·7 | 3·4 | 0·021* |
| 10 | 1027 | 4·8 | 5·4 | 4·1 | 0·335 |
| 11 | 891 | 6·3 | 5·1 | 7·7 | 0·120 |
| 7–8 | 2372 | 7·3 | 8·8 | 5·5 | 0·002* |
| 9–11† | 2923 | 5·4† | 5·7† | 4·9 | 0·343 |
| Total | 5295 | 6·2 | 7·1 | 5·2 | 0·004* |
| IDA (%) | |||||
| 7 | 1273 | 0·9 | 1·0 | 0·7 | 0·587 |
| 8 | 1099 | 0·9 | 1·0 | 0·8 | 0·613 |
| 9 | 1005 | 0·3 | 0·4 | 0·2 | 0·653 |
| 10 | 1027 | 0·2 | 0·2 | 0·2 | 0·898 |
| 11 | 891 | 0·6 | 0·2 | 1·0 | 0·119 |
| 7–8 | 2372 | 0·9 | 1·0 | 0·7 | 0·461 |
| 9–11† | 2923 | 0·3† | 0·3† | 0·4 | 0·363 |
| Total | 5295 | 0·6 | 0·6 | 0·6 | 0·936 |
Data are presented as number or percentage.
Anaemia was defined as Hb concentration <115 g/l, as proposed by WHO in 2001(1).
ID was defined by a multiple-index model, as proposed by the Chinese Medical Association in 2010(16).
IDA was defined as the presence of both anaemia and ID(1).
P < 0·05, boys v. girls, assessed by the χ 2 test for categorical variables.
P < 0·05, age 7–8 years v. 9–11 years, assessed by the χ 2 test for categorical variables.
The prevalence of ID and IDA was 6·2 and 0·6 % overall, respectively, both being higher in 7–8-year-olds than in 9–11-year-olds (7·3 v. 5·4 % for ID; 0·9 v. 0·3 % for IDA). ID was found to be more prevalent in boys than in girls (7·1 v. 5·2 %), while no gender difference was found in IDA. The prevalence of ID was highest at the age of 7 years (8·0 %) and decreased to its minimum at the age of 10 years (4·8 %). Comparing IDA prevalence with anaemia prevalence in the current study, we found that IDA accounted for 8·9 % (n 31) of total anaemia (n 349).
Distribution of children with different weight status
Prevalence rates of different weight status (categorized by BMI Z-score) are presented in Table 1. Most children had a BMI within the normal range (70·0 %). Of the participants, 14·0 % were overweight and 8·8 % were obese, only 7·2 % of them were thin. Rates of overweight and obesity were higher in boys than in girls, while the rate of thinness was higher in girls.
Prevalence of anaemia, iron deficiency and iron-deficiency anaemia in children with different weight status
Prevalence of anaemia/ID/IDA among participants with different weight status is presented in Table 3. Prevalence of anaemia was progressively lower with increasing BMI (from thinness to obesity), being lowest in children with obesity (4·1 %). On the contrary, prevalence of ID was progressively higher with increasing BMI, being highest in children with obesity (8·4 %). However, due to the relatively low IDA prevalence in the present study (0·6 % on average), no significant increasing or decreasing trend in IDA prevalence was observed with participants’ BMI.
Table 3.
Prevalence of anaemia, iron deficiency (ID) and iron-deficiency anaemia (IDA), according to different weight status, among schoolchildren aged 7–11 years from Guangzhou, China, 2014–2015 (n 5295)
| Age (years) | Anaemia (n 5295) | ID (n 5295) | IDA (n 5295) | |||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Thinness (n 382) |
Normal (n 3707) |
Overweight (n 741) |
Obesity (n 465) |
Thinness (n 382) |
Normal (n 3707) |
Overweight (n 741) |
Obesity (n 465) |
Thinness (n 382) |
Normal (n 3707) |
Overweight (n 741) |
Obesity (n 465) |
|||||||||||||
| n | % | n | % | n | % | n | % | n | % | n | % | n | % | n | % | n | % | n | % | n | % | n | % | |
| 7 | 6 | 6·8 | 76 | 7·9 | 5 | 3·8 | 3 | 3·4 | 7 | 8·0 | 79 | 8·2 | 7 | 5·3 | 9 | 10·2 | 0 | 0·0 | 9 | 0·9 | 1 | 0·8 | 1 | 1·1 |
| 8 | 6 | 7·7 | 57 | 7·2 | 5 | 3·6 | 6 | 6·4 | 1 | 1·3 | 52 | 6·6 | 10 | 7·2 | 7 | 7·4 | 1 | 1·3 | 7 | 0·9 | 1 | 0·7 | 1 | 1·1 |
| 9 | 7 | 9·0 | 46 | 6·8 | 10 | 6·5 | 4 | 4·2 | 5 | 6·4 | 31 | 4·6 | 8 | 5·2 | 8 | 8·3 | 0 | 0·0 | 3 | 0·4 | 0 | 0·0 | 0 | 0·0 |
| 10 | 6 | 9·7 | 41 | 5·9 | 6 | 3·6 | 2 | 1·9 | 4 | 6·5 | 32 | 4·6 | 4 | 2·4 | 9 | 8·3 | 1 | 1·6 | 1 | 0·1 | 0 | 0·0 | 0 | 0·0 |
| 11 | 4 | 5·3 | 46 | 7·8 | 9 | 6·0 | 4 | 5·1 | 1 | 1·3 | 32 | 5·5 | 17 | 11·4 | 6 | 7·6 | 0 | 0·0 | 2 | 0·3 | 2 | 1·3 | 1 | 1·3 |
| Total | 29 | 7·6 | 266 | 7·2 | 35 | 4·7 | 19 | 4·1 | 18 | 4·7 | 226 | 6·1 | 46 | 6·2 | 39 | 8·4 | 2 | 0·5 | 22 | 0·6 | 4 | 0·5 | 3 | 0·6 |
Associations between anaemia/iron deficiency/iron-deficiency anaemia and obesity
In Table 4, multivariate logistic regression models show that obesity was negatively associated with anaemia (adjusted OR = 0·553; 95 % CI 0·316, 0·968) while positively associated with ID (adjusted OR = 1·808; 95 % CI 1·146, 2·853). For IDA, no significant association was found between IDA and obesity. The logistic regression model for anaemia was adjusted for age, gender, birth weight and fruit/meat intake. The model for ID was adjusted for age, gender and moderate-intensity activity, and the model for IDA was adjusted for only for age and gender.
Table 4.
Logistic regression analysis of anaemia, iron deficiency (ID) and iron-deficiency anaemia (IDA) v. weight status among schoolchildren aged 7–11 years form Guangzhou, China (n 5295)
| Anaemia‡ | ID§ | IDA|| | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Weight status | AOR | 95 % CI | P value | AOR | 95 % CI | P value | AOR | 95 % CI | P value |
| Normal | 1·000 | Ref. | – | 1·000 | Ref. | – | 1·000 | Ref. | – |
| Overweight | 0·768 | 0·516, 1·143 | 0·193 | 1·044 | 0·656, 1·659 | 0·857 | 0·984 | 0·335, 2·889 | 0·976 |
| Obesity | 0·553 | 0·316, 0·968 | 0·038* | 1·808 | 1·146, 2·853 | 0·011* | 1·151 | 0·337, 3·394 | 0·823 |
| Thinness | 1·074 | 0·679, 1·699 | 0·761 | 0·443 | 0·179, 1·099 | 0·079 | 0·909 | 0·213, 3·891 | 0·898 |
AOR, adjusted odds ratio; ref., reference category.
Anaemia was defined as Hb concentration <115 g/l, as proposed by WHO in 2001(1).
ID was defined by a multiple-index model, as proposed by the Chinese Medical Association in 2010(16).
IDA was defined as the presence of both anaemia and ID(1).
P < 0·05, assessed by multivariate logistic regression.
The regression model was adjusted for age, gender, birth weight and food intake.
The regression model was adjusted for age, gender and moderate-intensity physical activity.
The regression model was adjusted for age and gender.
Discussion
In recent decades, a number of studies observed lower serum Fe or higher ID prevalence in children with obesity, while no conclusion has been made yet and the mechanism remains unclear. The present study evaluated Fe metabolism parameters, namely anaemia/ID/IDA, and their associations with obesity in schoolchildren from Guangzhou, China. We found a mean Hb level of 128·1 g/l; also, the prevalence of anaemia, ID and IDA was 6·6, 6·2 and 0·6 %, respectively. Importantly, increased ID prevalence and decreased anaemia prevalence were observed in children with obesity.
Status of iron metabolism parameters
The present study observed a similar Hb level as prior studies but a relatively higher SF level than previous studies. The Hb level in the present study is in line with a meta-analysis in China (2017)(19), but higher than that in some low-income areas, such as South Africa and Cambodia(20,21). The poor medical condition and standard of living in low-income areas might partly explain this difference in Hb concentration. On the other hand, we observed a relatively higher SF value (72·6 ng/ml on average) in the present study than most prior studies. Studies in South Africa and Colombia reported lower results than the current study (25·0 and 41·4 ng/ml, respectively)(22,23),while the NHANES (2006) reported a significantly higher SF level (82·5 ng/ml on average)(24). Increased standard of living and health awareness might contribute to the higher SF status in China and the USA.
Prevalence of anaemia/iron deficiency/iron-deficiency anaemia
The prevalence of anaemia in the current study is generally consistent with most prior studies in China, while lower than that in some low-income countries. Studies in Nepal and Kazakhstan reported significantly higher anaemia prevalence than did the present study (40 and 27 %, respectively)(25,26), while studies in the USA and Colombia found results similar to the present study(27,28).
The present study found a mild prevalence of ID (6·2 %), but a significantly low prevalence of IDA (0·6 %), which is consistent with US studies(27). Higher prevalence of both ID and IDA has been found in some low-income countries, including Brazil (45·4 and 10·3 %, respectively)(29). As is known to us, IDA can be diagnosed only when the exhausted Fe store has reduced Hb to a certain level. With increased health awareness and improved medical care, a large number of ID children could be identified and medical practices taken, preventing ID from progressing into IDA. Besides, ample food supply is usually available in high- and middle-income countries. Few children are sorely lacking in Fe intake, leading to fewer children progressing into IDA. Therefore, ID was found to be far more prevalent than IDA in the present study.
Interestingly, in the present study IDA accounts for only about 9 % of total anaemia (0·6 % out of 6·6 %), which is inconsistent with the WHO’s suggestion that ID is responsible for about 50 % of total anaemia. Low IDA prevalence in children similar to the present study has been reported in several middle- to high-income countries, including the USA (1·1 and 2·0 %), Italy (1·92 %) and Belgium (1·53 %)(2,27,30). Studies from Ethiopia and Rwanda also claimed that IDA accounts for less than 25 % of all causes of anaemia(30,31). These results suggest that, in certain populations, ID might not be the main reason for anaemia; instead, vitamin B12 or folate deficiency, chronic diseases, sickle cell disease, bone marrow disorders, thalassaemia and acquired haemolysis might contribute a larger proportion of the total anaemia(33).
According to the WHO guideline for IDA in 2001, infants and younger children are more likely to suffer from ID and IDA, compared with their older counterparts (anaemia was used as an indirect indicator for IDA)(1). This might partly explain the higher prevalence in 7–8-year-olds. Another important finding is the significantly higher ID prevalence in boys than in girls (7·1 v. 5·2 %, respectively). The extremely higher obesity rate in boys (12·7 v. 4·1 %) might be the main reason for the ID difference between genders, as suggested by some prior studies(1,5,34). Besides, menstruation was also taken into consideration when assessing anaemia in the present study, to account for the effects of menstrual blood loss on anaemia in females. However, we did not observe higher IDA prevalence in girls than in boys, probably due to the reason that only 5 % of the female participants had started menstruating.
Distribution of children with different weight status
The present study found 22·8 % of the participants were overweight (14·0 %) or obese (8·8 %), similar to the result of another study conducted in 9–12-year-old students in Guangzhou (20·5 %, 2014) and consistent with other studies in China(35–37). Looking back on relevant data in China during the last two decades, a significant upward trend in overweight/obesity could be observed(38,39) and researchers suggest that increased fast-food consumption, poor sleep habits, inadequate physical activity, and other factors stimulated by increased income, urbanization, busier lifestyle and ample food availability, are responsible for most part of the ever-increasing overweight/obesity burden in children and adolescents(36,40). The present study again confirmed this disturbing concern and indicates that government regulation on related fast-food industries as well as public health education for both children and parents are urgently needed to control the rising trend, thus preventing CVD and other relevant health problems that might come along in later life.
Associations of anaemia/iron deficiency/iron-deficiency anaemia with obesity
The present study demonstrated that children with obesity had a lower likelihood of being anaemic but a higher likelihood of having ID compared with those of normal weight, which seems paradoxical but actually is reasonable in this population. Similar to our study, decreased anaemia prevalence in obese children has been reported in Colombia and Peru(6,7) and evidence did show the association between obesity and higher Hb concentration(5). Although specific mechanisms remain poorly understood as yet, a high-energy diet, adequate intake of animal-based foods and adequate food supply in obese children might ensure that they consume in more Fe, folate, vitamin B12 and other micronutrients that are critical to Hb formation and might lead to anaemia if not ingested in sufficient quantity. As a consequence, children with obesity are less likely to be anaemic.
However, adequate intake of micronutrients does not always guarantee adequate absorption in the body, and Fe is the exception when it comes to obese children. Although more Fe might be consumed by obese individuals among the dietary factors, decreased Fe level and increased ID prevalence have been found in the present study as well as a number of prior studies. Studies from the USA, Iran and Israel demonstrated that obese children were two to three more likely to have ID than those of normal weight(8,12–14). In studies conducted to reveal the potential mechanism of Fe absorption inhibition in obese individuals, Bekri et al. found increased hepcidin (a hepatic-derived peptide) mRNA expression in adipose tissue from obese females(41) and several other researchers in recent years did observe increased hepcidin in obese women and children(42–44). Although studies did show decreased Fe level and increased hepcidin level in obese individuals as mentioned above, the exact mechanism of how obesity affects Fe status still remains unclear. On the basis of the existing associations, researchers hypothesized that inflammation-induced hepcidin in obese individuals was likely causing decreased dietary Fe absorption by diminishing the expression of ferroportin-1 located on the basolateral membrane of intestinal enterocytes, thus impairing dietary repletion efforts, although few studies have measured hepcidin concentrations yet(15).
No significant results were found between IDA and obesity in the present study. Different from our results, a positive association between IDA and obesity was found in Taiwan(45). This inconsistency might be partly due to the significantly low IDA prevalence in the present study, which is inadequate to detect its potential associations with other factors.
As mentioned above, hepcidin might be the key mediator in the process of weight gain affecting Fe status. In future study, it would be helpful to assess the hepcidin concentration of participants to further investigate the potential mechanisms.
Participants in the present study were selected randomly from all districts of Guangzhou, therefore the sample could be highly representative of urban children in Guangzhou. Our results confirm that anaemia and ID still remain a public health concern among schoolchildren in Guangzhou, China. Although the IDA prevalence is relatively low (0·6 %), it still remains a concern, with a large number of children suffering from ID which might progress to IDA in future. These results suggest that the present government policies aiming at anaemia/ID/IDA elimination, including Fe-fortified salt, other Fe-fortified foods and health education programmes, might have helped improved the Fe status of Chinese children in the past few years. However, more efforts are needed in this field, considering the situation in anaemia and ID. Specific strategies aimed at children with obesity might be a more efficient way to eliminate ID and IDA.
Limitations
Despite including a large sample in the present study, there are still some limitations. First, we did not assess hepcidin, transferrin receptor, erythrocyte protoporphyrin or serum transferrin receptor, hampering us from assessing ID using different methods and making comparisons with some prior studies. Second, we did not take inflammation into consideration when assessing ID and IDA. Since inflammation could affect the level Fe metabolism parameters(46), it would be more accurate to take inflammation into consideration when assessing ID and IDA. Third, the food intake data in the current study were collected via a simplified self-report questionnaire, which might not be accurate enough to reflect the real food intake status of the participants owing to the crude nature of the data and the existence of recall bias.
Conclusions
In the present study, anaemia and ID were prevalent (6·6 and 6·2 %, respectively) among schoolchildren in Guangzhou, China, while IDA was notably less prevalent (0·6 %) in the same population. Overweight or obesity was present in 22·8 % of the participants, and importantly obesity was found to be associated with lower anaemia risk while higher ID risk. The present study provides evidence for the higher ID risk in children with obesity and helps ascertain the association between under- and overnutrition. More attention should be paid to both over- and undernutrition, especially the micronutrient deficiencies in children with obesity, in order to improve the health and fitness of children.
Acknowledgements
Acknowledgements: The authors gratefully acknowledge the participants for their continuous and enthusiastic participation in the investigation. Also, they appreciate the doctors and nurses involved in this study for their clinical technical support. Financial support: This work was supported by the Guangdong Provincial Natural Science Foundation (grant numbers 2015A030313175 and 2017A030313844); the Fundamental Research Funds for the Central Universities in SYSU (grant number 15ykpy09); and the Sanming Project of Medicine in Shenzhen (grant number SZSM201803061). The funders had no role in the study design, data collection and analysis, decision to publish, or manuscript preparation. Conflict of interest: The authors have no conflicts to disclose. Authorship: Y.Z. designed the research study. W.L., M.C. and W.T. carried out the experiments and collected the data. H.Z. analysed the data. All authors were involved in writing the paper and had final approval of the submitted and published versions. Ethics of human subject participation: This study was conducted according to the guidelines laid down in the Declaration of Helsinki and all procedures involving human subjects were approved by the Sun Yat-sen University Institutional Review Board. Written informed consent was obtained from the parents or other legal guardians of all participants.
References
- 1. World Health Organization (2001) Iron deficiency anaemia: assessment, prevention, and control. A guide for programme managers. http://www.who.int/nutrition/publications/micronutrients/anaemia_iron_deficiency/WHO_NHD_01.3/en/ (accessed April 2018).
- 2. Gupta PM, Perrine CG, Mei Z et al. (2016) Iron, anemia, and iron deficiency anemia among young children in the United States. Nutrients 8, 330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Desalegn A, Mossie A & Gedefaw L (2014) Nutritional iron deficiency anemia: magnitude and its predictors among school age children, southwest Ethiopia: a community based cross-sectional study. PLoS One 9, e114059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Foote EM, Sullivan KM, Ruth LJ et al. (2013) Determinants of anemia among preschool children in rural, western Kenya. Am J Trop Med Hyg 88, 757–764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Qin Y, Melse-Boonstra A, Pan X et al. (2013) Anemia in relation to body mass index and waist circumference among Chinese women. Nutr J 12, 10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Kordas K, Fonseca Centeno ZY, Pachon H et al. (2013) Being overweight or obese is associated with lower prevalence of anemia among Colombian women of reproductive age. J Nutr 143, 175–181. [DOI] [PubMed] [Google Scholar]
- 7. Rodriguez-Zuniga MJ (2015) Obesity, overweight and anemia in children from a rural area of Lima, Peru. Medicina (B Aires) 75, 379–383. [PubMed] [Google Scholar]
- 8. Nead KG, Halterman JS, Kaczorowski JM et al. (2004) Overweight children and adolescents: a risk group for iron deficiency. Pediatrics 114, 104–108. [DOI] [PubMed] [Google Scholar]
- 9. Zhao L, Zhang X, Shen Y et al. (2015) Obesity and iron deficiency: a quantitative meta-analysis. Obes Rev 16, 1081–1093. [DOI] [PubMed] [Google Scholar]
- 10. Cepeda-Lopez AC, Aeberli I & Zimmermann MB (2010) Does obesity increase risk for iron deficiency? A review of the literature and the potential mechanisms. Int J Vitam Nutr Res 80, 263–270. [DOI] [PubMed] [Google Scholar]
- 11. Seltzer CC & Mayer J (1963) Serum iron and iron-binding capacity in adolescents. II Comparison of obese and non-obese subjects. Am J Clin Nutr 13, 354–361. [DOI] [PubMed] [Google Scholar]
- 12. Moayeri H, Bidad K, Zadhoush S et al. (2006) Increasing prevalence of iron deficiency in overweight and obese children and adolescents (Tehran Adolescent Obesity Study). Eur J Pediatr 165, 813–814. [DOI] [PubMed] [Google Scholar]
- 13. Pinhas-Hamiel O, Newfield RS, Koren I et al. (2003) Greater prevalence of iron deficiency in overweight and obese children and adolescents. Int J Obes Relat Metab Disord 27, 416–418. [DOI] [PubMed] [Google Scholar]
- 14. Tussing-Humphreys LM, Liang H, Nemeth E et al. (2009) Excess adiposity, inflammation, and iron-deficiency in female adolescents. J Am Diet Assoc 109, 297–302. [DOI] [PubMed] [Google Scholar]
- 15. Tussing-Humphreys L, Pusatcioglu C, Nemeth E et al. (2012) Rethinking iron regulation and assessment in iron deficiency, anemia of chronic disease, and obesity: introducing hepcidin. J Acad Nutr Diet 112, 391–400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Subspecialty Groups of Hematology and Child Health Care, Society of Pediatrics, Chinese Medical Association (2010) Recommendations for prevention and treatment of iron deficiency and iron deficiency anemia in children. Chin J Pediatr 18, 724–726 (in Chinese). [PubMed] [Google Scholar]
- 17. World Health Organization (2007) WHO growth reference for children aged between 5–19 years. http://www.who.int/growthref/who2007_bmi_for_age/en/ (accessed April 2018).
- 18. World Health Organization (2018) International Classification of Diseases, 11th revision. https://icd.who.int/browse11/l-m/en (accessed May 2019).
- 19. Song Y, Wang HJ, Dong B et al. (2017) National trends in hemoglobin concentration and prevalence of anemia among Chinese school-aged children, 1995–2010. J Pediatr 183, 164–169.e2. [DOI] [PubMed] [Google Scholar]
- 20. Gwetu TP, Chhagan MK, Taylor M et al. (2017) Anaemia control and the interpretation of biochemical tests for iron status in children. BMC Res Notes 10, 163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Perignon M, Fiorentino M, Kuong K et al. (2014) Stunting, poor iron status and parasite infection are significant risk factors for lower cognitive performance in Cambodian school-aged children. PLoS One 9, e112605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Motadi SA, Mbhenyane XG, Mbhatsani HV et al. (2015) Prevalence of iron and zinc deficiencies among preschool children ages 3 to 5 y in Vhembe district, Limpopo province, South Africa. Nutrition 31, 452–458. [DOI] [PubMed] [Google Scholar]
- 23. Perng W, Mora-Plazas M, Marin C et al. (2013) Iron status and linear growth: a prospective study in school-age children. Eur J Clin Nutr 67, 646–651. [DOI] [PubMed] [Google Scholar]
- 24. Gottfried RJ, Gerring JP, Machell K et al. (2013) The iron status of children and youth in a community mental health clinic is lower than that of a national sample. J Child Adolesc Psychopharmacol 23, 91–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Chandyo RK, Ulak M, Adhikari RK et al. (2015) Prevalence of iron deficiency and anemia among young children with acute diarrhea in Bhaktapur, Nepal. Healthcare (Basel) 3, 593–606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Hashizume M, Chiba M, Shinohara A et al. (2005) Anaemia, iron deficiency and vitamin A status among school-aged children in rural Kazakhstan. Public Health Nutr 8, 564–571. [DOI] [PubMed] [Google Scholar]
- 27. Kemmer TM, Novotny R & Ah Ping I (2008) Iron deficiency and anemia: disparity exists between children in American Samoa and children living within the US. Eur J Clin Nutr 62, 754–760. [DOI] [PubMed] [Google Scholar]
- 28. Agudelo GM, Cardona OL, Posada M et al. (2003) Prevalence of iron-deficiency anemia in schoolchildren and adolescents, Medellin, Colombia, 1999. Rev Panam Salud Publica 13, 376–386. [DOI] [PubMed] [Google Scholar]
- 29. Cardoso MA, Scopel KK, Muniz PT et al. (2012) Underlying factors associated with anemia in Amazonian children: a population-based, cross-sectional study. PLoS One 7, e36341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Levi M, Rosselli M, Simonetti M et al. (2016) Epidemiology of iron deficiency anaemia in four European countries: a population-based study in primary care. Eur J Haematol 97, 583–593. [DOI] [PubMed] [Google Scholar]
- 31. Gebreegziabher T & Stoecker BJ (2017) Iron deficiency was not the major cause of anemia in rural women of reproductive age in Sidama zone, southern Ethiopia: a cross-sectional study. PLoS One 12, e0184742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Donahue Angel M, Berti P, Siekmans K et al. (2017) Prevalence of iron deficiency and iron deficiency anemia in the northern and southern provinces of Rwanda. Food Nutr Bull 38, 554–563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Wang M (2016) Iron deficiency and other types of anemia in infants and children. Am Fam Physician 93, 270–278. [PubMed] [Google Scholar]
- 34. Huang YF, Tok TS, Lu CL et al. (2015) Relationship between being overweight and iron deficiency in adolescents. Pediatr Neonatol 56, 386–392. [DOI] [PubMed] [Google Scholar]
- 35. Wang J, Adab P, Liu W et al. (2017) Prevalence of adiposity and its association with sleep duration, quality, and timing among 9–12-year-old children in Guangzhou, China. J Epidemiol 27, 531–537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Ji M, Tang A, Zhang Y et al. (2018) The relationship between obesity, sleep and physical activity in Chinese preschool children. Int J Environ Res Public Health 15, 527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Zhou Y, Zhang Q, Wang T et al. (2017) Prevalence of overweight and obesity in Chinese children and adolescents from 2015. Ann Hum Biol 44, 642–643. [DOI] [PubMed] [Google Scholar]
- 38. Wang Y, Mi J, Shan XY et al. (2007) Is China facing an obesity epidemic and the consequences? The trends in obesity and chronic disease in China. Int J Obes (Lond) 31, 177–188. [DOI] [PubMed] [Google Scholar]
- 39. Ng M, Fleming T, Robinson M et al. (2014) Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 384, 766–781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Wang Y, Wang L, Xue H et al. (2016) A review of the growth of the fast food industry in China and its potential impact on obesity. Int J Environ Res Public Health 13, 1112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Bekri S, Gual P, Anty R et al. (2006) Increased adipose tissue expression of hepcidin in severe obesity is independent from diabetes and NASH. Gastroenterology 131, 788–796. [DOI] [PubMed] [Google Scholar]
- 42. Aeberli I, Hurrell RF & Zimmermann MB (2009) Overweight children have higher circulating hepcidin concentrations and lower iron status but have dietary iron intakes and bioavailability comparable with normal weight children. Int J Obes (Lond) 33, 1111–1117. [DOI] [PubMed] [Google Scholar]
- 43. del Giudice EM, Santoro N, Amato A et al. (2009) Hepcidin in obese children as a potential mediator of the association between obesity and iron deficiency. J Clin Endocrinol Metab 94, 5102–5107. [DOI] [PubMed] [Google Scholar]
- 44. Tussing-Humphreys LM, Nemeth E, Fantuzzi G et al. (2010) Elevated systemic hepcidin and iron depletion in obese premenopausal females. Obesity (Silver Spring) 18, 1449–1456. [DOI] [PubMed] [Google Scholar]
- 45. Chang JS, Chen YC, Owaga E et al. (2014) Interactive effects of dietary fat/carbohydrate ratio and body mass index on iron deficiency anemia among Taiwanese women. Nutrients 6, 3929–3941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Verma S & Cherayil BJ (2017) Iron and inflammation – the gut reaction. Metallomics 9, 101–111. [DOI] [PMC free article] [PubMed] [Google Scholar]