Abstract
We sought proof of principle that one of the safest human vaccines, measles virus Edmonston B (MV-Edm), can be genetically modified to allow entry via cell surface molecules other than its receptor CD46. Hybrid proteins consisting of the epidermal growth factor (EGF) or the insulin-like growth factor 1 (IGF1) linked to the extracellular (carboxyl) terminus of the MV-Edm attachment protein hemagglutinin (H) were produced. The standard H protein gene was replaced by one coding for H/EGF or H/IGF1 in cDNA copies of the MV genome. Recombinant viruses were rescued and replicated to titers approaching those of the parental strain. MV displaying EGF or IGF1 efficiently entered CD46-negative rodent cells expressing the human EGF or the IGF1 receptor, respectively, and the EGF virus caused extensive syncytium formation and cell death. Taking advantage of a factor Xa protease recognition site engineered in the hybrid H proteins, the displayed domain was cleaved off from virus particles, and specific entry in rodent cells was abrogated. These studies prove that MV can be engineered to selectively eliminate cells expressing a targeted receptor and provide insights into the mechanism of MV entry.
Measles virus (MV) is a nonsegmented negative-strand RNA virus of the family Paramyxoviridae, genus Morbillivirus. It remains one of the leading causes of infant death in developing countries, but live attenuated vaccines derived from the MV strain Edmonston B (MV-Edm) have almost completely eliminated measles-related fatalities in countries that have adopted compulsory vaccination (13). We aim to transform MV-Edm, an extremely cost-effective public health tool, into a replicating vector for cytoreductive therapy. Restriction of cell entry through the use of receptor-specific virus attachment is the approach that we are developing to achieve selective MV replication in target cells. To this end, we describe here the production of dual tropic MV-Edm derivatives that specifically enter rodent cells through a targeted receptor.
The MV envelope is composed of two glycoproteins: the hemagglutinin (H) and the fusion (F) protein. The H protein binds directly to the cellular receptor (17), and the F protein, containing a putative hydrophobic fusion peptide, executes fusion between the viral and the cell membrane at a neutral pH (50). A cellular receptor for MV-Edm is the type I glycoprotein CD46 (18, 34), a ubiquitous regulator of complement activation expressed in humans and Old World monkeys. CD46 is a major determinant of virus tropism, and its expression allows MV binding, entry, and replication in normally nonsusceptible rodent cells (6, 18, 33). The CD46 extracellular part consists of four complement control protein domains (CCP) and other small repeats (30). The viral H protein binds initially the two most distal domains, CCP 1 and 2 (6, 32), followed by secondary contacts with CCP 4 (12, 16). Several CCP 1 and 2 amino acids important for virus binding have been identified (5, 22), and the crystal structure of these domains (8) reveals an extended binding surface.
It is well established that the MV H protein is the major determinant of MV entry and cell tropism (47), but limited information is available on the residues of the H protein making CD46 contacts. A recent study identified amino acids 473 to 477 as a site involved in H-CD46 interaction (37). Furthermore, two amino acids, at positions 451 and 481, are critical for determining the ability of MV strains to cause hemabsorption, cell fusion, and CD46 downregulation (2, 29). In particular, tyrosine 481 found in MV-Edm appears to strongly influence the efficiency of CD46 binding in a baculovirus-based cell-binding assay (23). Nevertheless, a recombinant virus with a wild-type H protein (including asparagine 481) does propagate in Vero cells, though not as efficiently as MV-Edm (24). Furthermore, certain clinical MV isolates are able to infect mouse lymphocytes expressing CD46, but infection of human peripheral blood monocytic cells is not inhibited by the presence of anti-CD46 antibodies (31). We also note that in the attenuation process, MV-Edm was passaged in chicken embryo fibroblasts, which do not express a molecule antigenically related to human CD46 (20). Therefore, different MV strains, with slightly different attachment proteins, may recruit alternative cell surface proteins to support entry.
The possibility of producing viruses selectively entering a cell type of choice after binding to a specific receptor has generated much interest because of its application for the delivery of therapeutic genes and for the elimination of deleterious cells. Adenoviruses and retroviruses have been the first virus families explored for retargeting at the entry level, because they have distinctive advantages as vectors for the delivery of therapeutic genes. However, so far these efforts have met only limited success (39). One of the major obstacles in the development of retargeted viruses is the necessity of preserving accurate and efficient virus assembly and subsequent cell entry, while displaying a specificity determinant on the virus coat. The cell attachment and fusion functions being separated on two proteins in MV, we reasoned that this virus might be more easily amenable to retargeting at the level of entry.
On the basis of the observation that certain wild-type MV have the 35 carboxyl-terminal H amino acids deleted (36), we tested the possibility of retargeting MV by adding large specificity domains to the extracellular (carboxyl) H-protein terminus. Indeed, hybrid H proteins retained the fusion help function in a transient expression assay. Thus we attempted to produce recombinant viruses incorporating these proteins instead of H. These viruses were rescued and replicated to titers approaching those of the parental strain in certain primate cells. Most importantly, these viruses acquired the capacity of entering nonprimate cells expressing the cognate protein of the displayed specificity domain.
MATERIALS AND METHODS
Plasmids.
The parental plasmids pCG-F and pCG-H code for the F and H proteins of MV-Edmonston (9). Plasmids pCG-H/SfiI/NotI and pCG-H/XSfiI/NotI, the second including a factor Xa (FXa) protease cleavage signal before the SfiI/NotI cloning sites, were constructed and digested with SfiI and NotI to provide the backbone in which the coding regions for the displayed domains were inserted. The constructs pCG-H/hEGF, pCG-H/XhEGF, pCG-H/hIGF1, and pCG-H/XhIGF1 were made by transferring the SfiI/NotI human epidermal growth factor (hEGF) and human insulin-like growth factor 1 (hIGF1) fragments from pEGF-GS1A1 (38) and pIGFNA1 (11), respectively, into SfiI/NotI-digested pCG-H/SfiI/NotI and pCG-H/XSfiI/NotI. The coding sequence of the linker region (IEGRAAQPAMA, one-letter code) is 5′-ATCGAGGGAAGGGCGGCCCAGCCGGCCATGGCC-3′. The four constructs were tested to verify their functionality in cell fusion assays.
The PacI-SpeI fragments containing the hybrid H genes were corrected to comply with the rule of six (7) by a PCR deleting one nucleotide between the stop codon (underlined) and the SpeI site (italics), the final sequence being 5′-TAGTAACTAGT. The fragments were then inserted into PacI-SpeI-digested p(+)MV-NSe (44) encoding the MV Edmonston antigenome, yielding plasmids p(+)MV-H/hEGF, p(+)MV-H/XhEGF, p(+)MV-H/hIGF1, and p(+)MV-H/XhIGF1.
Plasmids p(+)MVgreen-H/XhEGF and p(+)MVgreen-H/XhIGF1 encoding the enhanced green fluorescent protein as an additional transcription unit upstream of the N gene (21) were constructed using a unique SacII restriction site located within the P gene and the SpeI site found downstream of the H coding region. The SacII/SpeI fragments from p(+)MV-H/XhEGF and p(+)MV-H/XhIGF1 containing the hybrid H genes were inserted into the SacII/SpeI opened backbone of p(+)MVgreen (19).
Cells, viruses, and infections.
Cells were grown in Dulbecco's modified Eagle's medium supplemented with 5% fetal calf serum (DMEM-5) for Vero (African green monkey kidney) and A431 (human carcinoma) cells or with 10% fetal calf serum (DMEM-10) for CHO (Chinese hamster ovary) cells or in DMEM-10 containing 1 mg of G418/ml for the rescue helper cell line 293-3-46 (human embryonic kidney), CHO-hEGFr, CHO-hEGF.tr, and 3T3-hIGF1r (mouse fibroblast) cells. The Edmonston B-based parental MV strain and all its recombinant derivatives were rescued, propagated, and purified basically as described previously (41). Viral titers were determined by 50% end-point dilution assays (10).
Infections were generally performed in Opti-MEM I reduced serum medium (O-MEM; Gibco). One day prior to infection, 4 × 105 cells were seeded into a 35-mm well. Before infection, cells were washed with 2 ml of O-MEM, and the infection was performed in 1 ml of O-MEM for 1 to 2 h at 37°C. The cells were washed again in 2 ml of O-MEM and overlaid with 2 ml of DMEM-5 or DMEM-10, depending on the cell line infected.
One-step growth analysis.
Vero cells (5 × 105) were infected with parental and recombinant MV at a multiplicity of infection (MOI) of 3 for 2 h. After infection, the cells were overlaid with 1 ml of DMEM-10, and incubation was continued at 32°C. Released and cell-associated virus samples were collected at different times postinfection. Cell-associated virus was subjected to one cycle of freezing-thawing, and then the samples were stored at −80°C for at least 4 h prior to titration. Before titration, the samples were centrifuged in a table-top centrifuge (Spectrafuge 16M; Labnet) for 2 min at 8,000 rpm to remove cell debris.
Purification of viral particles.
For each virus, two T175 bottles (Falcon) with Vero cells of 80% confluency (2 × 107) were infected at a MOI of 0.1 for 2 h at 37°C. The infection solution was replaced by 20 ml of DMEM-5, and cells were incubated at 32°C until 80 to 100% of all nuclei were found in syncytia. Supernatants were collected in 36-ml polypropylene tubes (Sorvall) and were clarified by 30 min of centrifugation at 8,000 rpm in a Surespin 630 rotor (Sorvall). Clarified supernatants were transferred into new 36-ml tubes and were pelleted by velocity centrifugation (2 h at 28,000 rpm in a Surespin 630 rotor) through 20% sucrose onto a 60%-sucrose cushion prepared in TNE buffer (10 mM Tris-HCl [pH 7.5], 100 mM NaCl, 1 mM EDTA [pH 7.5]). The fraction containing the virus was harvested, diluted by the addition of TNE, and pelleted at the bottom of the tube by 2 h of centrifugation at 28,000 rpm. After careful removal of all liquid, viruses were dissolved in 200 μl of phosphate-buffered saline (PBS; Gibco) and stored at −80°C.
Receptor saturation assays.
Vero, CHO-hEGFr, and 3T3-hIGF1r cells (5 × 105) were incubated in 0.5 ml of O-MEM containing either hEGF or hIGF1 (R&D Systems, no. 236-EG and 291-G1) for 30 min at 37°C. For infection, another 0.5 ml of O-MEM containing the virus was added to each well, yielding final hEGF and hIGF1 concentrations of 0.25 and 1 μM or 0.05 and 0.2 μM, respectively, in 1 ml of O-MEM. Infection was allowed to continue for 3 h at 37°C. The cells were washed with 2 ml of O-MEM and were overlaid with DMEM-10 without hEGF or hIGF1.
FXa protease pretreatment of viral particles.
Virus stocks were diluted in O-MEM to a concentration of 104 PFU in 20 μl. Forty microliters of diluted virus was incubated with either 0.2 or 2 μg of FXa protease, yielding a concentration of 5 or 50 μg of FXa/ml, respectively. After 1 h of incubation at 37°C, 2 ml of O-MEM was added to each virus sample. Cells were infected with 1 ml of virus sample per 35-mm well, as described above.
Immunoblotting.
Approximately 5,000 PFU of purified virus in 10 μl of PBS was lysed by the addition of 9 μl of lysis buffer (50 mM Tris [pH 8.0], 62.5 mM EDTA, 1% IGEPAL CA-630 (former NP-40), 0.4% deoxycholate). Lysed virus samples were adjusted to a volume of 20 μl with either 1 μl of PBS or with 1 μl of a solution containing 1 μg of FXa protease (New England Biolabs)/μl, incubated for 1 h at room temperature, and subjected to sodium dodecyl sulfate-polyacrylamide gel electrophoresis (SDS-PAGE). The gels were blotted onto polyvinylidene difluoride membranes (Millipore). The membranes were blocked with 5% bovine serum albumin–5% skim milk powder in TBST (10 mM Tris [pH 8.0], 150 mM NaCl, 0.05% Tween 20) for 1.5 h at room temperature. They were then incubated with either goat anti-MV antiserum diluted 1:1,000 (courtesy of S. Udem) or rabbit anti-H cytoplasmic tail antiserum diluted 1:2,500 (10). After intense washing, the proteins were visualized by incubation with peroxidase-conjugated goat anti-rabbit immunoglobulin G (IgG; Jackson Immuno Research, no. 111-035-003) or peroxidase-conjugated rabbit anti-goat IgG (Calbiochem, no. 401504) for 1 h at room temperature and by subsequent treatment with chemiluminescent substrate (Pierce, no. 34080ZZ).
ELISA.
Enzyme-linked immunosorbent assay (ELISA) plates were coated with 100 μl of 1-μg/ml dilutions of monoclonal anti-hEGF and anti-hIGF1 antibodies (R&D Systems, no. MAB236 and MAB291) for 2 h at 37°C and were blocked by incubation with 200 μl of 1% blocking reagent (Boehringer Mannheim, no. 1 096 176) in Tris-buffered saline (TBS) (10 mM Tris [pH 8.0], 150 mM NaCl). The plates were incubated with 100 μl of recombinant MV diluted in 1% blocking solution overnight at 4°C. Plates were washed three times with 200 μl of TBS, and bound virus was detected by incubation with 100 μl of a rabbit anti-Hcterm specific antiserum diluted 1:100 in 1% blocking solution for 2 h at 4°C. The Hcterm antiserum was raised in rabbits against a peptide corresponding to the 12 H-protein carboxy-terminal amino acids (NH2-CTVTREDGTNRR) linked to keyhole limpet hemocyanin through the naturally occurring cysteine (C). For detection, peroxidase-conjugated goat anti-rabbit IgG (Jackson Immuno Research, no. 111-035-003) diluted 1:5,000 in 1% blocking solution was added for 1 h at 4°C, and after intense washing the color reaction was performed using the POD substrate from Boehringer Mannheim (no. 1 363 727).
FACScan analysis.
Expression levels of CD46, hEGFr, and hIGF1r were determined by inoculating 5 × 105 cells in 50 μl of PBS with 1:100 dilutions of monoclonal anti-CD46 clone 11/88 (courtesy of J. Schneider-Schaulies), monoclonal anti-hEGFr clone 528 (Santa Cruz, no. sc-120), and monoclonal anti-hIGF1r clone 33255.111 (R&D Systems, no. MAB391) for 1 h on ice. After washing, the cells were incubated with a 1:50 dilution of a fluorescein-conjugated donkey anti-mouse IgG (Jackson Immuno Research, no. 715-095-151) for 30 min on ice and were washed again, fixed in PBS containing 1% paraformaldehyde, and analyzed.
To analyze virus binding, 105 CHO-hEGFr and 3T3-hIGF1r cells in a total volume of 50 μl of PBS were incubated with 104 PFU of purified Edmonston or recombinant MV for 2 h on ice. The samples were washed once in 3.5 ml of PBS with 2% fetal calf serum (FCS) and incubated in 50 μl of PBS containing a 1:100 dilution of the monoclonal anti-H antibody I41 (43) for 1.5 h on ice. Subsequent incubations were performed as described above.
RESULTS
H proteins displaying a specificity domain functionally replace standard H protein.
As the first step towards the production of retargeted MV, we investigated if a domain could be appended to the extracellular terminus of this protein without interfering with its fusion support function. The hEGF (53 amino acids) and the hIGF1 (70 amino acids) were selected as prototype ligands because their interactions with the respective receptors have been extensively characterized biochemically and they have been functionally displayed on other viruses. A hybrid protein was constructed in which the hEGF coding region was fused in frame with the H coding region but with the last two arginine residues eliminated to avoid the possibility of introducing an undesired furin cleavage site (H/hEGF; Fig. 1A, second line from bottom). A flexible linker region (AAQPAMA, one-letter code) was added between the domains to increase the probability of independent folding function. In another hybrid protein, an FXa protease cleavage site (IEGR) was added before the linker region (H/XhEGF; Fig. 1A, second line from bottom). Analogously hybrid H/hIGF1 and H/XhIGF1 proteins were constructed (Fig. 1A, bottom line). When the hybrid proteins were coexpressed with a MV F protein, H/hEGF and H/XhEGF retained the same level of fusion help as parental H, whereas the fusion help efficiency of H/hIGF1 and H/XhIGF1 was reduced but remained clearly over background (data not shown).
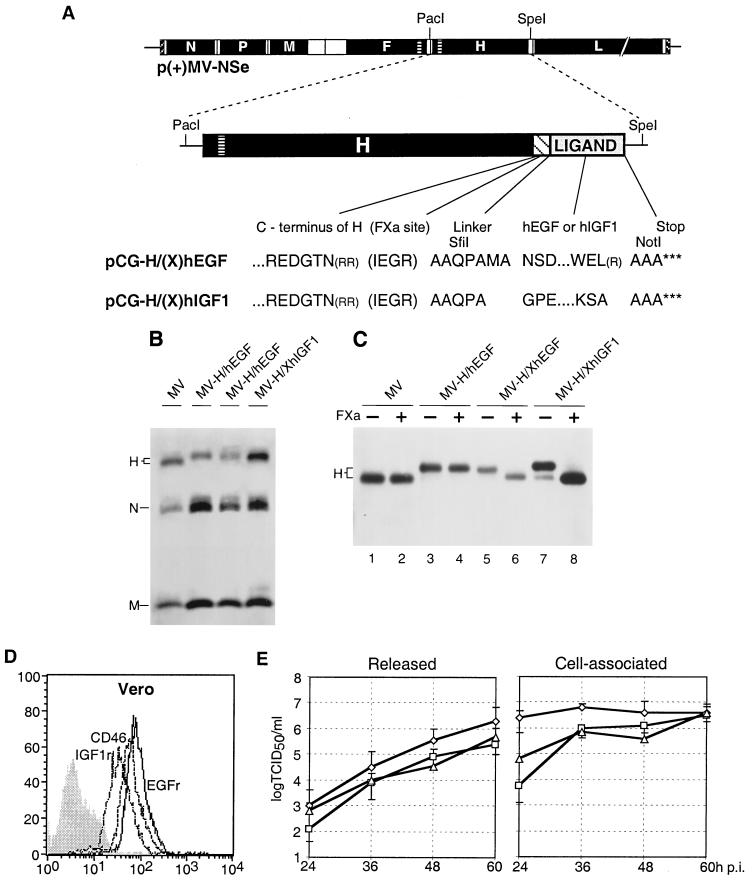
FIG. 1.
Genomic structure, protein composition, and replication of recombinant MV. (A) Plasmid p(+)MV-NSe coding for the MV antigenome (top), PacI-SpeI fragments used for subcloning (center), and amino acid sequences (one-letter code) of the junctions between the H protein ectodomain and the specificity domains (bottom). Coding regions of the six MV cistrons are represented by solid black boxes, the transmembrane segment of the F and H proteins by a horizontally lined box, the FXa cleavage site and the flexible linker by a hatched box, and the ligand by a gray box. Arginine residues in parentheses have been deleted. For details see text. (B) Protein composition of recombinant viruses. Viral particles were purified by centrifugation through a 20% sucrose layer onto a 60% sucrose cushion and subsequent pelleting. The viruses were titrated, 5,000 PFU was subjected to lysis, and proteins were separated by SDS-PAGE. For immunodetection, a MV-specific antiserum was used. (C) FXa protease sensitivity of hybrid H proteins. Purified viral particles (5,000 PFU) were lysed and incubated for 1 h without (−) or with (+) FXa protease at room temperature. Proteins were separated by SDS-PAGE and detected with an H-specific antiserum. (D) FACS analysis of CD46 (interrupted line), IGF1r (dotted line), and EGFr (continuous line) expression on Vero cells. Vertical axis, cell number; horizontal axis, fluorescence intensity. The greyed profile represents incubation of the cells without the primary antibody. (E) Time course of released (left panel) and cell-associated (right panel) virus production in Vero cells infected with parental MV (diamonds), MV-H/XhEGF (squares), and MV-H/XhIGF1 (triangles). Cells were infected at a MOI of 3 and were incubated at 32°C for the times indicated. Viral titers were determined by 50% end-point dilution. Indicated values are averages of three experiments.
Based on these positive findings, we asked whether the hybrid H proteins could functionally replace H in viral particles. For this we exchanged the H gene of an infectious MV cDNA cloned in p(+)MV-NSe (44) with genes coding for the hybrid proteins. Helper cells (41) were transfected with those plasmids. Three to 4 days after transfection with p(+)MV-NSe, p(+)MV-H/hEGF, and p(+)MV-H/XhEGF, and 5 to 7 days after transfection with p(+)MV-H/hIGF and p(+)MV-H/XhIGF, syncytia were detected, suggesting virus rescue. Infectivity could be passaged in Vero cells, the African green monkey cell line routinely used to grow and titrate MV, and the recombinant viruses reached titers in a range similar to that of the parental virus (see below).
To test whether the specificity domains had effects on H protein incorporation into particles, we analyzed the protein composition of a standardized amount of each virus (5,000 PFU, as determined on Vero cells). As shown in Fig. 1B, purified particles from the MV-H/hEGF, MV-H/XhEGF, and MV-H/XhIGF1 viruses contained an amount of H protein similar to that of parental MV but with more N and M proteins. These results suggest that the hybrid H proteins are incorporated slightly less efficiently than H in particles and that the particle-to-infectivity ratio of the recombinant MV is slightly higher than that of the parental strain.
We then verified that specific proteolytic cleavage of the displayed domain from purified virus particles occurred. In Fig. 1C it is shown that FXa protease indeed specifically cleaves off the displayed domain from the H protein of MV-H/XhEGF (lane 6) and MV-H/XhIGF1 (lane 8) but not from the control viruses MV (lane 2) and MV-H/hEGF (lane 4).
We then verified by fluorescence-activated cell sorter (FACS) analysis the levels of expression of CD46 and of the targeted receptors in Vero cells (Fig. 1D). The EGF receptor (hEGFr, continuous line), IGF receptor (hIGF1r, dotted line), and CD46 (interrupted line) were all expressed. For one-step growth analysis, Vero cells were infected in parallel with a MOI of 3 of either MV-H/XhEGF, MV-H/XhIGF1, or the parental MV strain. Released and cell-associated virus were harvested at 12-h intervals and were titrated on Vero cells. Results spanning the times from 24 to 60 h postinfection (p.i.) are shown in Fig. 1E. Cell-associated titers of MV-H/XhEGF (squares) rose more slowly than those of the parental strain (diamonds), whereas those of MV-H/XhIGF1 (triangles) were intermediate, but all viruses reached similar maximum titers of about 5 × 106/ml (Fig. 1E, right panel). Release of infectious virus in the supernatant followed slower kinetics, as expected, and peaked at 1.7 × 106 for the parental strain and at 3.5 and 6.3 times lower levels (Fig. 1E, left panel) for MV-H/XhIGF1 and MV-H/XhEGF, respectively. These results indicate that in Vero cells replication and intracellular assembly of the two recombinant viruses are slower than in the parental strain. Nevertheless, the maximum titers of cell-associated virus are similar for all three strains. Release of the two recombinant viruses is slightly less efficient than that of parental MV.
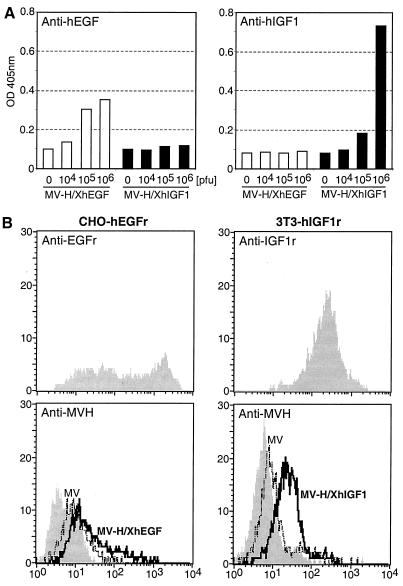
The next question related to the accessibility of the displayed domains. We tested whether recombinant viruses could bind to monoclonal antibodies recognizing the displayed domains in an enzyme-linked immunoassay. Figure 2A shows that plates coated with an anti-hEGF monoclonal antibody incubated with increasing amounts of MV-H/XhEGF retained increasing amounts of virus (left panel, white columns), whereas on plates coated with anti-hIGF1, only background retention levels were detected (right panel, white columns). The opposite was the case for the MV-H/XhEGF1 virus, which was selectively retained by the anti-hIGF1 monoclonal antibody (black columns in right panel). Thus the displayed domains are accessible for binding by certain antibodies.
FIG. 2.
Binding of recombinant viral particles to immobilized hEGF- and hIGF1-specific antibodies (A) and to rodent cells expressing a target receptor (B). (A) ELISA plates were coated with either anti-hEGF or anti-hIGF1 monoclonal antibodies. After blocking, the plates were incubated with different dilutions of MV-H/XhEGF and MV-H/XhIGF1. Bound virus was detected using an H-specific antiserum. (B) Expression levels of hEGFr in CHO-hEGFr cells (top left) and of hIGF1r in 3T3-hIGF1 cells (top right). Cells incubated only with the secondary antibody showed a background level of fluorescence (mean 3.9 versus 466.5 for CHO-hEGFr cells and 5.7 versus 250.8 for 3T3-hIGF1 cells [data not shown]). Binding of MV-H/XhEGF to CHO-hEGFr cells (bottom left) and of MV-H/XhIGF1 to 3T3-hIGF1r cells (bottom right) are shown. Thick lines, incubations with the recombinant viruses; thin lines, incubation with MV; grey areas, control incubations without virus; vertical axis, cells counted; horizontal axis, fluorescence intensity.
MV displaying a specificity domain bind to, infect, and fuse rodent cells expressing the cognate receptor.
Next we investigated whether MV particles displaying a specificity domain bind to cells expressing the cognate receptor. Edmonston MV-derived strains are expected to bind CD46, which is expressed on the surface of all nucleated cell types from most primates. To verify if the displayed hEGF and hIGF1 domains did confer attachment to their cognate receptors, we relied on CD46-negative rodent cells: Chinese hamster ovary cells stably expressing the hEGF receptor (CHO-hEGFr; X.-Y. Wang, A. Blahnik, and C. D. James, unpublished data) and mouse NIH-3T3 cells stably expressing the hIGF1 receptor (3T3-hIGF1r) (28).
Figure 2B presents a FACS analysis confirming that CHO-hEGFr cells (upper left panel) and 3T3-hIGF1r (upper right panel) express the corresponding human protein on their surface. When these cells were incubated with MV-H/XhEGF (lower left panel) or MV-H/XhIGF1 (lower right panel), respectively, and virus binding was detected with an anti-H monoclonal antibody (thick line), a shift in the number of strongly fluorescent cells from background antibody binding (gray area) and from binding of control MV (thin lines) was shown in both cell lines.
We then asked if the MV particles displaying the specificity domains could productively enter, and replicate in, rodent cells expressing the cognate receptor. To detect viral gene expression early after entry, we constructed viruses expressing high levels of the enhanced green fluorescent protein (eGFP) (52). For this, a MV genomic plasmid containing an eGFP transcription unit (19) was combined with p(+)MV-H/XhEGF and p(+)MV-H/XhIGF1. The new viruses were rescued and named MVgreen-H/XhEGF and MVgreen-H/XhIGF1.
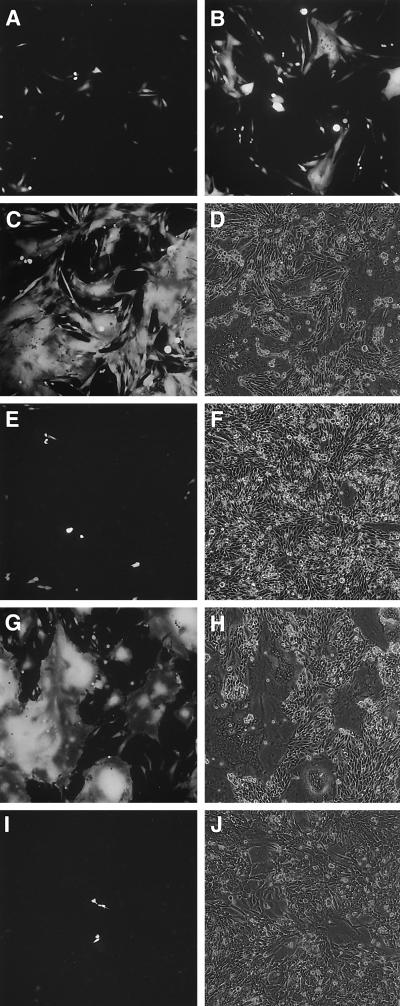
Figure 3 presents three time points (24, 48, and 72 h p.i.) of an infection of CHO-hEGFr cells with MVgreen-H/XhEGF at a MOI of 1. At 24 h p.i. (Fig. 3A), fluorescence was detected in single cells; at 48 h p.i. (Fig. 3B), a large fraction of the cells showed a strong signal, and remarkably, several fused cells were registered; at 72 h p.i., the majority of the cells had fused in large syncytia (Fig. 3D), which were fluorescent (Fig. 3C). In control CHO-hEGFr cells infected with MVgreen, no fluorescence was detected 24 h p.i., and few positive cells were detected 72 h p.i. (Fig. 3E). The same was true for another negative control, CHO cells infected with MVgreen-H/XhEGF (Fig. 3I, shown 72 h p.i.). The few small syncytia detected in MVgreen-infected CHO-hEGFr cells and MVgreen-H/XhEGF-infected CHO cells (Fig. 3F and J) were not fluorescent (Fig. 3E and I, respectively) and thus were due to spontaneous fusion at high cell density. On the other hand, CHO-hEGFr.tr cells, expressing a hEGF receptor with a truncated cytoplasmic tail and thus inefficiently internalized upon ligand binding (W.-Y. Wang, A. Blahnik, and C. D. James, unpublished data), supported efficient MVgreen-H/XhEGF infection, which resulted in cell fusion (Fig. 3G and H, shown 72 h p.i.). Thus CHO cells expressing the human EGF receptor or a mutant receptor without the cytoplasmic tail support efficient, CD46-independent cell entry of MVgreen-H/XhEGF, indicating that internalization or intracellular signaling does not affect MV entry. Strikingly, in these cells the MV infection results in extensive syncytium formation.
FIG. 3.
Infection of CHO-hEGFr cells (A to F), CHO-hEGFr.tr cells (G and H), and CHO cells (I and J) with MVgreen-H/XhEGF (A to D and G to J) or MV (E and F). Cells were infected at a MOI of 1 and were monitored by fluorescent or phase-contrast microscopy 24 (A), 48 (B), or 72 (C to J) h after infection.
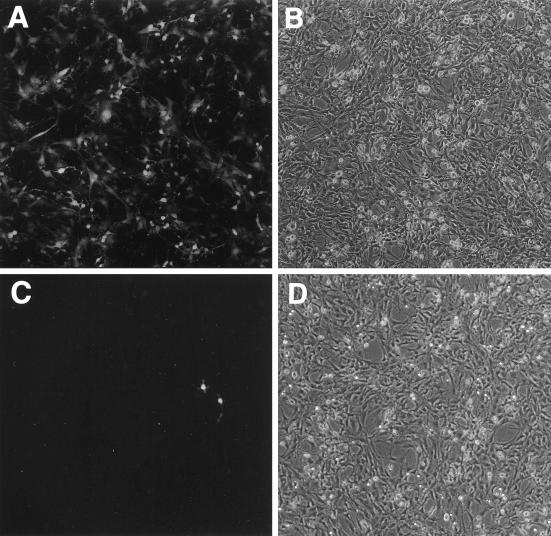
Figure 4 presents 3T3-hIGFr cells 24 h after infection with a MOI of 3 of MVgreen-H/XhIGF1 (Fig. 4A and B) and MVgreen (Fig. 4C and D), respectively. Many cells infected with MVgreen-H/XhIGF1 were strongly fluorescent (Fig. 4A), whereas only rare fluorescent cells were detected after MVgreen infection (Fig. 4C). To gain some information on the relative efficiency of entry of MVgreen-H/XhIGF1 and MVgreen in 3T3-hIGF1r cells, these cells were infected with either one of the viruses at a MOI of 3, 0.3, or 0.03. In a 35-mm dish, 735 positive cells infected with MVgreen-H/XhIGF1 at a MOI of 0.03 were counted, and 87 positive cells infected with MVgreen at an MOI of 3 were counted. Thus, about 1,000 times more infectious particles of MVgreen than of MVgreen-H/XhIGF1 were needed to elicit detectable eGFP expression in the same number of 3T3-hIGF1r cells. Even late in infection of 3T3-hIGF1r cells with MVgreen-H/XhIGF1, fusion was limited, in line with the limited fusion of primate Vero cells (data not shown).
FIG. 4.
Infection of 3T3-hIGF1r cells with MVgreen-H/XhIGF1 (A and B) or MVgreen (C and D). Cells were infected at a MOI of 3, and infection was monitored by fluorescent (A and C) or phase-contrast (B and D) microscopy 24 h after infection.
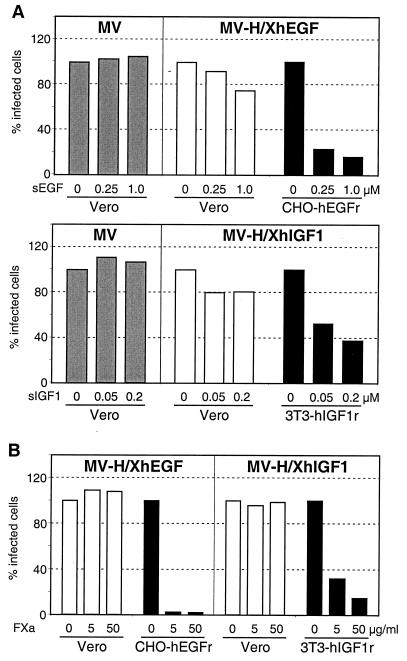
We then sought confirmation that the interaction of the displayed domains with their receptor mediates virus entry. First, we assayed if entry of MVgreen-H/XhEGF or MVgreen-H/XhIGF1 could be competed by the addition to the medium of a soluble form of hEGF or hIGF1, respectively. As shown in Fig. 5A (top panel, black columns), the addition of 0.25 or 1 μM soluble human EGF to the medium of CHO-hEGFr cells reduced the number of cells infected with MVgreen-H/XhEGF approximately 5 to 6 times. There was no inhibition of the MVgreen infection of Vero cells by 1 μM soluble EGF (Fig. 5A, top panel, gray columns), but interestingly there was a small but reproducible effect of soluble EGF in inhibiting the MVgreen-H/XhEGF infection of those cells (Fig. 5A, top panel, white columns). Analogously, soluble human IGF interfered selectively with the infection of MVgreen-H/XhIGF1, more strongly on 3T3-hIGF1r cells than on Vero cells (Fig. 5A, lower panel).
FIG. 5.
Competition of viral entry by soluble receptors (A) and the effect of proteolytic cleavage of the specificity domain on entry (B). (A) Competition of viral infections by soluble EGF (sEGF; top panel) or soluble IGF1 (sIGF1; bottom panel). CHO-hEGFr and Vero cells pretreated or not with sEGF were infected with MVgreen or MVgreen-H/XhEGF at a MOI of 0.3. 3T3-hIGF1r and Vero cells pretreated or not with sIGF1 were infected with MVgreen and MVgreen-H/XhIGF1 at a MOI of 0.1. The number of infected cells was determined at 24 h p.i. by counting GFP-expressing cells in a standard area. Percentages are relative to the number of GFP-expressing cells in infections without added soluble receptor. Results obtained with MV Edmonston on Vero cells are indicated by gray columns. Results obtained with recombinant MV on Vero cells are indicated by white columns and on rodent cells by black columns. (B) Effects of the treatment of recombinant viruses with FXa protease prior to infection. Vero and CHO-hEGFr or Vero and 3T3-hIGF1r cells were infected with MVgreen-H/XhEGF or MVgreen-H/XhIGF1 (104 PFU/well), respectively, and were pretreated with 0, 5, or 50 μg of FXa protease/ml. The number of GFP-expressing cells was determined 42 h p.i. Percentages refer to the number of cells infected with untreated virus. For details, see text.
Next we took advantage of the FXa protease cleavage site present in the H/XhEGF and H/XhIGF1 proteins to verify whether the elimination of the displayed specificity domain from recombinant virus particles did influence entry. When MV-H/XhEGF particles were treated with 5 or 50 μg of FXa protease/ml for 1 h, the number of green fluorescent CHO-hEGFr cells diminished by almost two orders of magnitude (Fig. 5B, left panel, black column), whereas FXa treatment did not significantly change the infectivity of these particles on Vero cells (Fig. 5B, left panel, white columns). Analogously, proteolytic cleavage of MV-H/XhIGF1 virus particles with FXa protease resulted in the loss of more than 80% of the infectivity selectively in 3T3-hIGF1r cells (Fig. 5B, right panel, compare black and white columns). Thus, by two different approaches, competition with a soluble form of the displayed domain and proteolytic cleavage of that domain from viral particles, it was confirmed that entry of recombinant MV in rodent cells depends on the interaction of the specificity domain with the cognate receptor.
DISCUSSION
We sought proof of principle that the human vaccine strain MV-Edm can be retargeted. Indeed, we showed that MV-Edm can display large specificity domains, namely hEGF or hIGF1, on the extracellular terminus of its attachment protein without losing its replication competence on primate cell lines. The displayed growth factors were accessible at the viral surface, as shown by capture of viral particles onto a solid support coated with anti-EGF or anti-IGF1 antibodies, and conferred specific binding of virus particles to cells expressing the targeted receptor. Furthermore, the recombinant viruses gained the ability to efficiently infect rodent cells expressing the targeted receptor.
To confirm that entry into rodent cells depends on the displayed domain, high concentrations of EGF or IGF1 were used to saturate the respective tyrosine kinase receptors before and during infection. Inhibition of virus entry was clearly demonstrated but was incomplete. This suggests that multivalent virus attachment cannot be efficiently inhibited by monomeric ligands. On the other hand, the number of hEGFr-positive hamster cells infected with the hEGF-displaying MV was reduced by almost two orders of magnitude when the displayed hEGF domain was proteolytically cleaved from the virus. For the hIGF1-displaying virus, a sixfold inhibition of entry into hIGF1r-positive 3T3 cells was observed after protease treatment. Thus, we conclude that the displayed domains do retarget MV entry on rodent cells. On Vero cells, protease pretreatment of viral particles or receptor saturation with soluble growth factors had no or only a weak inhibitory effect on entry efficiency, indicating that the recombinant viruses are dualtropic: they maintained CD46-dependent entry and gained entry via the targeted tyrosine kinase receptor.
Mechanism of MV cell entry.
That the MV-Edm vaccine strain can enter cells by a CD46-independent pathway may not be unexpected, since indications of the existence of alternative receptors for wild-type MV exist (2, 20, 23). However, the observation that MV attachment through the displayed growth factors to receptors structurally unrelated to CD46 leads to virus entry as efficiently as attachment to the natural receptor is surprising and has consequences for our understanding of receptor function in MV entry. According to one hypothesis, binding of MV and other paramyxoviruses to their receptors triggers a conformational change in the H protein that is transmitted to the F protein. In turn, the F protein undergoes a radical conformational change culminating in the insertion of the hydrophobic fusion peptide into the target cell membrane, thereby initiating the process of membrane fusion (27). Even if we cannot exclude that completely different binding events trigger a stereotypical alteration of the H oligomer, this appears unlikely considering that H and the displayed domains are joined by a flexible linker. An alternative hypothesis predicts that receptor binding serves merely to anchor the virus particle in close proximity to the target cell membrane, increasing the efficiency with which secondary interactions between the viral glycoproteins and components of the cell membrane leading to the induction of the fusion process can occur (27). Our data are consistent with this hypothesis; binding of the recombinant MV to the tyrosine kinase receptors may simply increase the efficiency of secondary interactions with another, yet unidentified cell membrane component.
MV entry can be dissociated from cell-to-cell fusion.
MVgreen-H/XEGF not only entered CHO-hEGFr cells but also fused them with high efficiency. On the other hand, MVgreen-H/XIGF1 almost completely failed to induce syncytium formation on 3T3 cells, despite efficient entry. To elucidate whether the differences in inducing cell fusion are due to the displayed domain or to the cells, we produced a 3T3 cell line expressing hEGFr. Infection of these cells with the EGF virus revealed low to undetectable fusion, as for the IGF virus (data not shown). This demonstrates a strong influence of the host cell on the fusion potential of recombinant MV. Indeed, MV-Edm fuses different primate cell lines with variable efficiency.
In addition, domain specific differences in the ability to induce cell-to-cell fusion were observed. Both recombinant MVs efficiently entered Vero cells and reached similar titers; nevertheless, their competence to induce cell-to-cell fusion was different. Whereas the size and growth rate of the syncytia elicited by MVgreen-H/XEGF were similar to those of MV-Edm, MVgreen-H/XIGF1 had a clearly reduced cell fusion capacity (data not shown). This suggests that structural differences of the displayed domains, and possibly the interaction with the target receptors, influence the cell-to-cell fusion potential. Nevertheless, entry efficiency and virus production are similar for both viruses. Thus, different requirements for these processes do exist.
Reengineering viral entry.
This is the first demonstration that large specificity domains covalently linked to a viral glycoprotein support not only binding to a new receptor class but also efficient cell entry through the targeted receptor. This demonstration is remarkable because it was obtained with a replication-competent virus rather than with viral vectors. The display of EGF or IGF1, attached to the extracellular terminus of a retroviral envelope glycoprotein, supported efficient receptor binding but interfered with virus entry (11, 35). Even if recent studies identified a region of the retroviral glycoprotein that tolerates the insertion of specificity domains without compromising entry function (25), engineering of the retroviral envelope remains challenging (51), to the point that bifunctional noncovalent cross-linkers bridging the virus coat to a receptor have been considered to retarget entry of these vectors (4, 45). However, cross-linkers may be inappropriate for virus-mediated gene delivery in an organism because of problems with stability.
Similarly, in adenoviruses (49), an elegant combination of structural analysis and mutagenesis has been used to ablate the original receptor specificity and display a short peptide which redirected entry to an antibody expressed on the surface of host cells (42). With MV it is shown here that 53 and 70 amino acid domains on the viral surface can retarget virus entry, and we have recently used a single-chain antibody against carcinogenic embryonic antigen (CEA) to retarget a replicating MV to mouse cells expressing human CEA (A. L. Hammond et al., unpublished data). Thus the MV envelope is easily amenable to retargeting.
MV and cytoreductive therapy.
Members of the paramyxovirus family have shown therapeutic effects in a number of malignancies. Mumps virus was administered to 90 patients with advanced or terminal cancer. In almost half of the patients, the virus caused significant tumor regression in the treated region, displaying minimal toxicity (1). There are several reported cases of regression of Hodgkin and of non-Hodgkin lymphoma after natural MV infection (3, 46), and recently it was shown that intraneoplastic inoculation with MV-Edm led to complete regression of lymphoma and myeloma tumor xenografts in severe combined immunodeficiency mice (Grote and Fielding, personal communication; Peng and Russell, personal communication). Thus, MV-Edm has potential for tumor therapy, and the use of retargeted virus should increase the efficacy of therapy and reduce the likelihood of toxicity.
One concern in the development of replicating MV-Edm for oncolytic therapy is that the high prevalence of MV antibody seropositivity in the human population might compromise its therapeutic value. There is evidence to suggest that this may not be the case, since examination of the immune response of convalescent children suggested that MV infection can occur after vaccination without resulting in disease (15). Moreover, it was recently shown that macaques vaccinated with live attenuated virus or DNA can experience a subclinical infection at challenge (40). Finally, recent evidence from phase II human trials of replicating adenovirus suggests that the impact of circulating antibodies after intratumoral virus injection may be minimal (26), and it is encouraging that the efficacy of conditionally replicating herpesviruses (48) and reoviruses (14) was not abolished by preexisting viral antibodies. Nevertheless, to evaluate the effect of antibodies on virus clearance, we are currently developing a model using genetically modified mice (33) in whom preexisting MV immunity can be established (44). On the other hand, it is conceivable that tumor treatment might benefit from the immune stimulatory potential of MV-Edm by induction of an antitumoral immune response.
ACKNOWLEDGMENTS
We thank Martin A. Billeter and Charles Weissmann for helpful discussions during the early stages of this work, Veronika von Messling for advice, and David James and Mark Chadwick for cell lines.
This work was supported by grants 31-45900.95 and 31-29343.90 (START) from the Swiss National Science Foundation, by the Kanton Zurich, by the British Medical Research Council (S.J.R. and F.B.), and by the Siebens Foundation.
REFERENCES
- 1.Asada T. Treatment of human cancer with mumps virus. Cancer. 1974;34:1907–1928. doi: 10.1002/1097-0142(197412)34:6<1907::aid-cncr2820340609>3.0.co;2-4. [DOI] [PubMed] [Google Scholar]
- 2.Bartz R, Firsching R, Rima B, ter Meulen V, Schneider-Schaulies J. Differential receptor usage by measles virus strains. J Gen Virol. 1998;79:1015–1025. doi: 10.1099/0022-1317-79-5-1015. [DOI] [PubMed] [Google Scholar]
- 3.Bluming A Z, Ziegler J L. Regression of Burkitt's lymphoma in association with measles infection. Lancet. 1971;ii:105–106. doi: 10.1016/s0140-6736(71)92086-1. [DOI] [PubMed] [Google Scholar]
- 4.Boerger A L, Snitkovsky S, Young J A. Retroviral vectors preloaded with a viral receptor-ligand bridge protein are targeted to specific cell types. Proc Natl Acad Sci USA. 1999;96:9867–9872. doi: 10.1073/pnas.96.17.9867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Buchholz C J, Koller D, Devaux P, Mumenthaler C, Schneider-Schaulies J, Braun W, Gerlier D, Cattaneo R. Mapping of the primary binding site of measles virus to its receptor CD46. J Biol Chem. 1997;272:22072–22079. doi: 10.1074/jbc.272.35.22072. [DOI] [PubMed] [Google Scholar]
- 6.Buchholz C J, Schneider U, Devaux P, Gerlier D, Cattaneo R. Cell entry by measles virus: long hybrid receptors uncouple binding from membrane fusion. J Virol. 1996;70:3716–3723. doi: 10.1128/jvi.70.6.3716-3723.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Calain P, Roux L. The rule of six, a basic feature for efficient replication of Sendai virus defective interfering RNA. J Virol. 1993;67:4822–4830. doi: 10.1128/jvi.67.8.4822-4830.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Casasnovas J M, Larvie M, Stehle T. Crystal structure of two CD46 domains reveals an extended measles virus-binding surface. EMBO J. 1999;18:2911–2922. doi: 10.1093/emboj/18.11.2911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cathomen T, Buchholz C J, Spielhofer P, Cattaneo R. Preferential initiation at the second AUG of the measles virus F mRNA: a role for the long untranslated region. Virology. 1995;214:628–632. doi: 10.1006/viro.1995.0075. [DOI] [PubMed] [Google Scholar]
- 10.Cathomen T, Naim H Y, Cattaneo R. Measles viruses with altered envelope protein cytoplasmic tails gain cell fusion competence. J Virol. 1998;72:1224–1234. doi: 10.1128/jvi.72.2.1224-1234.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chadwick M P, Morling F J, Cosset F L, Russell S J. Modification of retroviral tropism by display of IGF-I. J Mol Biol. 1999;285:485–494. doi: 10.1006/jmbi.1998.2350. [DOI] [PubMed] [Google Scholar]
- 12.Christiansen D, Loveland B, Kyriakou P, Lanteri M, Escoffier C, Gerlier D. Interaction of CD46 with measles virus: accessory role of CD46 short consensus repeat IV. J Gen Virol. 2000;81:911–917. doi: 10.1099/0022-1317-81-4-911. [DOI] [PubMed] [Google Scholar]
- 13.Clements C J, Cutts F T. The epidemiology of measles: thirty years of vaccination. In: ter Meulen V, Billeter M A, editors. Measles virus. Berlin, Germany: Springer-Verlag; 1995. pp. 13–33. [DOI] [PubMed] [Google Scholar]
- 14.Coffey M C, Strong J E, Forsyth P A, Lee P W. Reovirus therapy of tumors with activated Ras pathway. Science. 1998;282:1332–1334. doi: 10.1126/science.282.5392.1332. [DOI] [PubMed] [Google Scholar]
- 15.Damien B, Huiss S, Schneider F, Muller C P. Estimated susceptibility to asymptomatic secondary immune response against measles in late convalescent and vaccinated persons. J Med Virol. 1998;56:85–90. doi: 10.1002/(sici)1096-9071(199809)56:1<85::aid-jmv14>3.0.co;2-v. [DOI] [PubMed] [Google Scholar]
- 16.Devaux P, Buchholz C J, Schneider U, Escoffier C, Cattaneo R, Gerlier D. CD46 short consensus repeats III and IV enhance measles virus binding but impair soluble hemagglutinin binding. J Virol. 1997;71:4157–4160. doi: 10.1128/jvi.71.5.4157-4160.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Devaux P, Loveland B, Christiansen D, Milland J, Gerlier D. Interactions between the ectodomains of haemagglutinin and CD46 as a primary step in measles virus entry. J Gen Virol. 1996;77:1477–1481. doi: 10.1099/0022-1317-77-7-1477. [DOI] [PubMed] [Google Scholar]
- 18.Dorig R E, Marcil A, Chopra A, Richardson C D. The human CD46 molecule is a receptor for measles virus (Edmonston strain) Cell. 1993;75:295–305. doi: 10.1016/0092-8674(93)80071-l. [DOI] [PubMed] [Google Scholar]
- 19.Duprex W P, McQuaid S, Hangartner L, Billeter M A, Rima B K. Observation of measles virus cell-to-cell spread in astrocytoma cells by using a green fluorescent protein-expressing recombinant virus. J Virol. 1999;73:9568–9575. doi: 10.1128/jvi.73.11.9568-9575.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Escoffier C, Gerlier D. Infection of chicken embryonic fibroblasts by measles virus: adaptation at the virus entry level. J Virol. 1999;73:5220–5224. doi: 10.1128/jvi.73.6.5220-5224.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hangartner L. M.Sc. thesis. Zurich, Switzerland: University of Zurich; 1997. [Google Scholar]
- 22.Hsu E C, Dorig R E, Sarangi F, Marcil A, Iorio C, Richardson C D. Artificial mutations and natural variations in the CD46 molecules from human and monkey cells define regions important for measles virus binding. J Virol. 1997;71:6144–6154. doi: 10.1128/jvi.71.8.6144-6154.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hsu E C, Sarangi F, Iorio C, Sidhu M S, Udem S A, Dillehay D L, Xu W, Rota P A, Bellini W J, Richardson C D. A single amino acid change in the hemagglutinin protein of measles virus determines its ability to bind CD46 and reveals another receptor on marmoset B cells. J Virol. 1998;72:2905–2916. doi: 10.1128/jvi.72.4.2905-2916.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Johnston I C, ter Meulen V, Schneider-Schaulies J, Schneider-Schaulies S. A recombinant measles vaccine virus expressing wild-type glycoproteins: consequences for viral spread and cell tropism. J Virol. 1999;73:6903–6915. doi: 10.1128/jvi.73.8.6903-6915.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kayman S C, Park H, Saxon M, Pinter A. The hypervariable domain of the murine leukemia virus surface protein tolerates large insertions and deletions, enabling development of a retroviral particle display system. J Virol. 1999;73:1802–1808. doi: 10.1128/jvi.73.3.1802-1808.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Khuri F R, Nemunaitis J, Ganly I, Arseneau J, Tannock I F, Romel L, Gore M, Ironside J, MacDougall R H, Heise C, Randlev B, Gillenwater A M, Bruso P, Kaye S B, Hong W K, Kirn D H. A controlled trial of intratumoral ONYX-015, a selectively-replicating adenovirus, in combination with cisplatin and 5-fluorouracil in patients with recurrent head and neck cancer. Nat Med. 2000;6:879–885. doi: 10.1038/78638. [DOI] [PubMed] [Google Scholar]
- 27.Lamb R A. Paramyxovirus fusion: a hypothesis for changes. Virology. 1993;197:1–11. doi: 10.1006/viro.1993.1561. [DOI] [PubMed] [Google Scholar]
- 28.Lammers R, Gray A, Schlessinger J, Ullrich A. Differential signalling potential of insulin- and IGF-1-receptor cytoplasmic domains. EMBO J. 1989;8:1369–1375. doi: 10.1002/j.1460-2075.1989.tb03517.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lecouturier V, Fayolle J, Caballero M, Carabana J, Celma M L, Fernandez-Munoz R, Wild T F, Buckland R. Identification of two amino acids in the hemagglutinin glycoprotein of measles virus (MV) that govern hemadsorption, HeLa cell fusion, and CD46 downregulation: phenotypic markers that differentiate vaccine and wild-type MV strains. J Virol. 1996;70:4200–4204. doi: 10.1128/jvi.70.7.4200-4204.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Liszewski M K, Post T W, Atkinson J P. Membrane cofactor protein (MCP or CD46): newest member of the regulators of complement activation gene cluster. Annu Rev Immunol. 1991;9:431–455. doi: 10.1146/annurev.iy.09.040191.002243. [DOI] [PubMed] [Google Scholar]
- 31.Manchester M, Eto D S, Valsamakis A, Liton P B, Fernandez-Munoz R, Rota P A, Bellini W J, Forthal D N, Oldstone M B. Clinical isolates of measles virus use CD46 as a cellular receptor. J Virol. 2000;74:3967–3974. doi: 10.1128/jvi.74.9.3967-3974.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Manchester M, Valsamakis A, Kaufman R, Liszewski M K, Alvarez J, Atkinson J P, Lublin D M, Oldstone M B. Measles virus and C3 binding sites are distinct on membrane cofactor protein (CD46) Proc Natl Acad Sci USA. 1995;92:2303–2307. doi: 10.1073/pnas.92.6.2303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mrkic B, Pavlovic J, Rulicke T, Volpe P, Buchholz C J, Hourcade D, Atkinson J P, Aguzzi A, Cattaneo R. Measles virus spread and pathogenesis in genetically modified mice. J Virol. 1998;72:7420–7427. doi: 10.1128/jvi.72.9.7420-7427.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Naniche D, Varior-Krishnan G, Cervoni F, Wild T F, Rossi B, Rabourdin-Combe C, Gerlier D. Human membrane cofactor protein (CD46) acts as a cellular receptor for measles virus. J Virol. 1993;67:6025–6032. doi: 10.1128/jvi.67.10.6025-6032.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Nilson B H, Morling F J, Cosset F L, Russell S J. Targeting of retroviral vectors through protease-substrate interactions. Gene Ther. 1996;3:280–286. [PubMed] [Google Scholar]
- 36.Outlaw M C, Pringle C R. Sequence variation within an outbreak of measles virus in the Coventry area during spring/summer 1993. Virus Res. 1995;39:3–11. doi: 10.1016/s0168-1702(95)00060-7. [DOI] [PubMed] [Google Scholar]
- 37.Patterson J B, Scheiflinger F, Manchester M, Yilma T, Oldstone M B. Structural and functional studies of the measles virus hemagglutinin: identification of a novel site required for CD46 interaction. Virology. 1999;256:142–151. doi: 10.1006/viro.1999.9644. [DOI] [PubMed] [Google Scholar]
- 38.Peng K W. Ph.D. thesis. Cambridge, United Kingdom: University of Cambridge; 1997. [Google Scholar]
- 39.Peng K W, Russell S J. Viral vector targeting. Curr Opin Biotechnol. 1999;10:454–457. doi: 10.1016/s0958-1669(99)00009-9. [DOI] [PubMed] [Google Scholar]
- 40.Polack F P, Lee S H, Permar S, Manyara E, Nousari H G, Jeng Y, Mustafa F, Valsamakis A, Adams R J, Robinson H L, Griffin D E. Successful DNA immunization against measles: neutralizing antibody against either the hemagglutinin or fusion glycoprotein protects rhesus macaques without evidence of atypical measles. Nat Med. 2000;6:776–781. doi: 10.1038/77506. [DOI] [PubMed] [Google Scholar]
- 41.Radecke F, Spielhofer P, Schneider H, Kaelin K, Huber M, Dotsch C, Christiansen G, Billeter M A. Rescue of measles viruses from cloned DNA. EMBO J. 1995;14:5773–5784. doi: 10.1002/j.1460-2075.1995.tb00266.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Roelvink P W, Mi Lee G, Einfeld D A, Kovesdi I, Wickham T J. Identification of a conserved receptor-binding site on the fiber proteins of CAR-recognizing adenoviridae. Science. 1999;286:1568–1571. doi: 10.1126/science.286.5444.1568. [DOI] [PubMed] [Google Scholar]
- 43.Sheshberadaran H, Chen S N, Norrby E. Monoclonal antibodies against five structural components of measles virus. I. Characterization of antigenic determinants on nine strains of measles virus. Virology. 1983;128:341–353. doi: 10.1016/0042-6822(83)90261-1. [DOI] [PubMed] [Google Scholar]
- 44.Singh M, Cattaneo R, Billeter M. A recombinant measles virus expressing hepatitis B virus surface antigen induces humoral immune responses in genetically modified mice. J Virol. 1999;73:4823–4828. doi: 10.1128/jvi.73.6.4823-4828.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Snitkovsky S, Young J A. Cell-specific viral targeting mediated by a soluble retroviral receptor-ligand fusion protein. Proc Natl Acad Sci USA. 1998;95:7063–7068. doi: 10.1073/pnas.95.12.7063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Taqi A M, Abdurrahman M B, Yakubu A M, Fleming A F. Regression of Hodgkin's disease after measles. Lancet. 1981;i:1112. doi: 10.1016/s0140-6736(81)92286-8. [DOI] [PubMed] [Google Scholar]
- 47.Tatsuo H, Okuma K, Tanaka K, Ono N, Minagawa H, Takade A, Matsuura Y, Yanagi Y. Virus entry is a major determinant of cell tropism of Edmonston and wild-type strains of measles virus as revealed by vesicular stomatitis virus pseudotypes bearing their envelope proteins. J Virol. 2000;74:4139–4145. doi: 10.1128/jvi.74.9.4139-4145.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Todo T, Rabkin S D, Sundaresan P, Wu A, Meehan K R, Herscowitz H B, Martuza R L. Systemic antitumor immunity in experimental brain tumor therapy using a multimutated, replication-competent herpes simplex virus. Hum Gene Ther. 1999;10:2741–2755. doi: 10.1089/10430349950016483. [DOI] [PubMed] [Google Scholar]
- 49.Wickham T J. Targeting adenovirus. Gene Ther. 2000;7:110–114. doi: 10.1038/sj.gt.3301115. [DOI] [PubMed] [Google Scholar]
- 50.Wild T F, Malvoisin E, Buckland R. Measles virus: both the haemagglutinin and fusion glycoproteins are required for fusion. J Gen Virol. 1991;72:439–442. doi: 10.1099/0022-1317-72-2-439. [DOI] [PubMed] [Google Scholar]
- 51.Wu B W, Lu J, Gallaher T K, Anderson W F, Cannon P M. Identification of regions in the Moloney murine leukemia virus SU protein that tolerate the insertion of an integrin-binding peptide. Virology. 2000;269:7–17. doi: 10.1006/viro.2000.0201. [DOI] [PubMed] [Google Scholar]
- 52.Yang T T, Cheng L, Kain S R. Optimized codon usage and chromophore mutations provide enhanced sensitivity with the green fluorescent protein. Nucleic Acids Res. 1996;24:4592–4593. doi: 10.1093/nar/24.22.4592. [DOI] [PMC free article] [PubMed] [Google Scholar]