Abstract
Posttraumatic stress disorder (PTSD) is more prevalent among sexual minority women (SMW) than among heterosexual women. PTSD risk varies among SMW, but no meta-analysis has clarified sexual identity-related disparities in probable PTSD among women or SMW’s heterogeneity in PTSD risk. SMW are also at pronounced risk of comorbid PTSD and hazardous drinking (HD). However, the difference in comorbid PTSD/HD between SMW and heterosexual women is understudied. This meta-analysis aimed to provide a comprehensive understanding of differences between SMW and heterosexual women and among SMW across demographic characteristics. Peer-reviewed publications that were written in English and reported quantitative data on PTSD specific to SMW were included. Eligible publications (n = 45) were identified through a systematic search of 11 electronic databases, supplemented by a search of reference lists of relevant papers. We found that probable PTSD, PTSD symptom severity, and probable comorbid PTSD/HD are highly prevalent among SMW, with SMW of color, transgender and gender diverse people, and bi+ women (e.g., bisexual, pansexual, queer) being at greatest risk. These results emphasize the need to improve accurate assessment of trauma-related sequelae among SMW and to develop, disseminate, and implement culturally sensitive treatments to reduce PTSD and comorbid PTSD/HD among at-risk SMW.
Keywords: Sexual minority women, posttraumatic stress disorder, trauma exposure, comorbid posttraumatic stress disorder and hazardous drinking, meta-analysis
Introduction
Posttraumatic stress disorder (PTSD) can occur in individuals following direct or indirect exposure to actual or threatened death, serious injury, or sexual violation (American Psychiatric Association; APA, 2013). PTSD is characterized by intrusive thoughts, persistent avoidance, negative alteration in cognition and mood, and marked alteration in arousal and reactivity (APA, 2013) and contributes to substantial morbidity and mortality (Possemato et al., 2015; Sullivan et al., 2020). PTSD is highly comorbid with hazardous drinking (HD; i.e., high-risk drinking patterns that increase the likelihood of developing alcohol use disorders), especially among women (Castillo-Carniglia et al., 2019; Smith & Cottler, 2018). Women also vary in risk of PTSD and comorbid HD, with findings showing a higher prevalence of PTSD and comorbid PTSD/HD among sexual minority women (SMW; e.g., lesbian, bisexual, queer) than heterosexual women (Evans-Polce & McCabe, 2020). Yet, current literature lacks a comprehensive understanding of these disparities. Identifying marginalized groups, including SMW, at greatest risk of PTSD, severe PTSD symptoms, and comorbid PTSD/HD could help to develop and enhance targeted prevention and intervention efforts.
Gender Disparities in Lifetime, Past-Year, and Past-Month Rates of PTSD
Most psychobiological studies have found higher rates of PTSD in women than men, partly due to lower levels of social support, younger age at the time of trauma, and greater exposure to traumatic events which are strongly predictive of PTSD, including interpersonal violence (vs. war-related trauma or other adversities) (Blanco et al., 2018; Goldstein et al., 2016; Lehavot et al., 2018; Olff et al., 2007). For example, studies among the general U.S. population demonstrate that lifetime prevalence of PTSD is 8.0%–9.5% among women and 3.4%–5.6% among men (Blanco et al., 2018; Lehavot et al., 2018); past-year prevalence of PTSD is 6.0%–6.1% for women and 2.6%–3.2% for men (Goldstein et al., 2016; Lehavot et al., 2018). A recent systematic review found that among studies using large, nationally representative samples, lifetime prevalence of PTSD among women is 8.0%, compared to 4.1% of men; past-year estimates for women are 6.0% and 2.6% for men (Schein et al., 2021). Among a college sample, 32.6% of women met criteria for lifetime probable PTSD vs. 11.4% of men (Cusack et al., 2019). In addition, one study using a nationally representative survey of Black Americans found that 8.7%–14.0% of women vs. 4.6%–6.3% of men met criteria for lifetime PTSD; past-year PTSD estimates for women are 2.9%–6.4% and 2.2%–3.4% for men (Jones et al., 2022). Another study using a nationally representative sample of veterans indicated that past-month PTSD prevalence estimates among women are 11.2% (vs. 4.3% among men; Wisco et al., 2022). Findings are mixed on the presence of gender differences in PTSD symptom severity among those who meet subthreshold PTSD (but not full PTSD; Lehavot, Stappenbeck, et al., 2014; Olff et al., 2007).
SMW’s Heightened Risk of PTSD Relative to Heterosexual Women
Comparative studies have shown that SMW are at least twice as likely as heterosexual women to meet PTSD criteria (20.2%–35.3%; Dworkin et al., 2020; Helminen et al., 2021; Kerridge et al., 2017; Roberts et al., 2010). Other research has demonstrated that SMW have greater PTSD symptom severity than heterosexual women (Lehavot et al., 2019; López & Yeater, 2021). Nonetheless, no study has meta-analyzed sexual identity disparities in probable diagnosis of PTSD (i.e., likelihood of meeting diagnostic criteria for PTSD based on valid cut-off scores using self-report checklists vs. structured clinical interviews; hereafter “probable PTSD”; Steel et al., 2009) and PTSD symptom severity among women. This gap in existing literature can lead to potentially inaccurate estimates and impede work toward mental health equity among marginalized populations exposed to trauma. Indeed, accurately estimating sexual identity disparities in PTSD among women could substantiate the need for clinical research to improve prediction and assessment of PTSD, identify etiologic and maintenance mechanisms of PTSD, and define clinical subtypes of PTSD (e.g., low threshold for activating the adrenergic hyperarousal response, deficits in fear regulation, trauma-related cognitive intrusions) among SMW (Ressler, 2018). Such findings could also inform flexibly applied modular approaches to treating PTSD according to SMW’s concerns (e.g., behavioral health comorbidities, stigma-related stress reactivity; Juster et al., 2019; Karatzias & Cloitre, 2019; Ressler, 2018).
Extensive sexual identity disparities in PTSD diagnosis and severity among women are likely due to SMW’s increased vulnerability to experiencing adverse events that are strongly predictive of PTSD, including dating and sexual violence (McCabe et al., 2022; Porsch et al., 2022). Sexual minority individuals, including SMW, also face stigma-related stressors (i.e., minority stress; Brooks, 1981; Meyer, 2003), including distal stigma-related experiences, such as discrimination, stemming from SMW’s marginalized social statuses (Brooks, 1981; Meyer, 2003; Pachankis et al., 2017; Page, Cerezo et al., 2021). Distal minority stressors can lead to negative psychological processes and compensatory behaviors, such as anticipated rejection, internalized stigma, and identity concealment, in an effort to prevent future stigma (Dyar et al., 2018; Meyer, 2003; Pachankis et al., 2020). Sexual minority people also engage in chronic threat vigilance due to inadequate social safety (e.g., unreliable social inclusion; Diamond & Alley, 2022). This chronic threat vigilance overlaps with complex posttraumatic outcomes common in individuals with early onset, multiple, and extended adverse experiences (Briere & Spinazzola, 2005). Sensitization to early and repeated trauma, chronic minority stress, and inadequate social safety may lower SMW’s threshold for tolerating future distress, contributing to lasting effects on stress reactivity and conferring risk for PTSD and comorbid behavioral health issues, including HD (Diamond & Alley, 2022; Helminen et al., 2021; Juster et al., 2019).
Vulnerable Subgroups of SMW at Increased Risk of PTSD
Differential vulnerability models suggest that some SMW, for example, those with “multi-minoritized identities” (Estrada et al., 2021) are more susceptible to stress sensitization (Hatzenbuehler et al., 2014). Nevertheless, research applying differential vulnerability models to examine potential subgroup differences in PTSD among SMW is sparse as studies tend to aggregate data across SMW subgroups (Hughes et al., 2020). Moreover, results from the few existing studies examining whether PTSD risk varies across SMW subgroups, for example, by race/ethnicity and sexual identity, are inconsistent (Krueger & Upchurch, 2019; McCabe et al., 2020; Ovrebo et al., 2018; Sigurvinsdottir & Ullman, 2016; Veldhuis et al., 2022). Some evidence indicates higher rates of PTSD among SMW of color relative to White SMW (Balsam et al., 2015; Sigurvinsdottir & Ullman, 2016) while others show a significantly higher prevalence of probable PTSD among White than Black and Latinx SMW (Veldhuis et al., 2022). Several studies have found similar rates of PTSD symptom severity between lesbian and bisexual women (Ovrebo et al., 2018; Sigurvinsdottir & Ulman, 2015); other findings suggest that past-year and lifetime prevalence of PTSD are higher among bisexual women (Evans-Polce & McCabe, 2020; Veldhuis et al., 2022). However, no meta-analysis has clarified SMW’s heterogeneity in probable PTSD risk and PTSD symptom severity levels, hindering the development and refinement of interventions that aim to reduce those disparities (Estrada et al., 2021).
SMW’s gender identities and presentations often transcend cisheteronormative gender roles (Halberstam, 2012; Levitt et al., 2012); many SMW identify as gender diverse (e.g., nonbinary; Dworkin et al., 2018; Page et al., 2021). In fact, mental and behavioral health risks associated with societal stress (e.g., heterosexism, sexism, cissexism) differ for SMW based on gender identity and expression (Batchelder et al., 2022; Puckett et al., 2016; Scheer et al., 2021). These intragroup disparities in mental health burdens facing SMW may be explained by higher rates of victimization and intersectional minority stressors (Bostwick et al., 2019; Cerezo & Ramirez, 2020; Dworkin et al., 2018; Sarno et al., 2021; Scheer, Clark, et al., 2022). No studies have reported PTSD diagnosis or symptom severity rates among SMW based on gender identity, limiting our understanding of potential within-group health disparities (Lehavot et al., 2012; Puckett et al., 2016). We aim to address this gap by contacting authors with requests for data on SMW’s risk of probable PTSD and PTSD symptom severity across gender identity.
Prevalence and Etiology of Comorbid PTSD and HD
Knowledge is also limited regarding the relationship between PTSD and co-occurring externalizing behaviors, including HD. While studies with the general U.S. population consistently find that PTSD and HD frequently co-occur, estimates vary widely (e.g., 9.8% to 61.3%, depending on trauma timing and type and cutoff scores used to denote PTSD and harmful drinking; Debell et al., 2014). Other findings suggest that PTSD and alcohol use disorders co-occur in 28% to 85% of treatment-seeking people (Ralevski et al., 2014; Wisco et al., 2016). Comorbid PTSD/HD estimates also vary among women, with some research suggesting that SMW are at heightened risk of comorbid PTSD/HD. For example, one study found that 60.5% of bisexual women in the sample met criteria for past-year alcohol use disorder and had a psychiatric comorbidity, including PTSD, relative to 44.6% of heterosexual women (Evans-Polce & McCabe, 2020). Other research suggests that 8.5%−17.6% of SMW report probable comorbid PTSD/HD (Helminen et al., 2021). PTSD also partly explains SMW’s (but not heterosexual women’s) increased risk of HD (Lehavot, Browne, et al., 2014). While longitudinal research is needed to determine whether PTSD is a proximal antecedent of SMW’s HD (Dworkin et al., 2020), SMW’s heightened risk of comorbid PTSD/HD highlights the need for integrated interventions (Flanagan et al., 2016) that attend to PTSD and HD in this population.
Several etiologic models (e.g., self-medication, mutual maintenance, PTSD susceptibility, negative reinforcement, shared vulnerability) have been tested to explain comorbid PTSD/HD in the general population and among SMW (Dworkin et al., 2020; Hawn, Cusack, et al., 2020; Kelley et al., 2018). Notably, the self-medication hypothesis (Khantzian, 1985), which suggests that alcohol may be used to seek momentary relief from distressing affective states and negative internal experiences, including PTSD symptoms, is the most widely accepted and rigorously tested (Hawn, Cusack, et al., 2020). The “drinking-to-cope” self-medication model postulates that individuals with PTSD may be more prone to developing problematic drinking behaviors, including HD, due to short-term negative reinforcement effects of alcohol (Hawn, Bountress, et al., 2020; Khantzian, 1985). Compared to PTSD and HD alone, comorbid PTSD/HD is associated with worse PTSD and alcohol treatment prognosis, increased alcohol craving, and greater functional impairment (Ralevski et al., 2014). Yet, a precise and systematic evaluation of SMW’s disproportionate risk of comorbid PTSD/HD has not been documented. Such findings are imperative for monitoring equity in service delivery and improving outcomes among SMW.
The Present Study
In this meta-analysis we aimed to examine (1) the proportion of SMW who meet criteria for probable PTSD; (2) mean PTSD symptom severity levels among SMW; (3) whether SMW are more likely than heterosexual women to meet criteria for probable PTSD; (4) whether SMW report greater mean PTSD symptom severity levels than heterosexual women; (5) whether SMW’s likelihood of meeting criteria for probable PTSD varies by race/ethnicity, sexual identity, and gender identity; (6) whether SMW’s mean PTSD symptom severity levels vary by race/ethnicity, sexual identity, and gender identity; (7) the proportion of SMW who meet criteria for probable comorbid PTSD/HD; and, (8) whether SMW are more likely than heterosexual women to meet criteria for probable comorbid PTSD/HD. These findings could yield important clinical insights into risk stratification across treatment settings and improve the lives of SMW, a recognized public health research priority group (National Institutes of Health Sexual and Gender Minority Research Coordinating Committee, 2015; Pérez-Stable, 2016).
Individuals who present with significant, clinical levels of distress but who do not meet full criteria for PTSD (i.e., subthreshold PTSD) report similar impairment as full PTSD (Morgan-López et al., 2020). Thus, we treated PTSD as a categorical diagnostic and a continuous symptom severity variable, aligned with clinical recommendations (Christ et al., 2021).
Methods
This meta-analysis followed guidelines for Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA; Page et al., 2021) and was preregistered with PROSPERO (CRD42021233281).
Inclusion Criteria
Inclusion criteria for studies were: (1) reported in English, (2) published in a peer-reviewed journal, (3) presented empirical data on probable PTSD and/or PTSD symptom severity, and (4) presented findings specific to SMW. Furthermore, studies were required to include a search term for: (1) sexual identity, (2) gender, and (3) PTSD.
Within this study, SMW included individuals who identified as cisgender women, transgender men and women, nonbinary, and other diverse gender labels (e.g., genderqueer, agender), consistent with SMW-focused literature (Drabble et al., 2020; Page et al., 2021; Scheer, Clark, et al., 2022). Further, bisexual plus (bi+) included SMW who identified as bisexual, pansexual, queer, and those with attractions to more than one gender regardless of gender identity (Jhe et al., 2021; Mereish et al., 2017).
Search Strategy
We searched 11 electronic databases using search terms related to women, sexual identity, and PTSD. No publication date limit was imposed. Databases included Anthropology Plus, APA PsycArticles, APA PsycInfo, APA PsycTests, Applied Science & Technology, Health and Psychosocial Instruments, Humanities International Index, LGBTQ+ Source, PubMed, Social Work Abstracts, and Women’s Studies International. See the Supplemental Material for a full list of search terms and an example search in PubMed. Papers from databases were gathered until December 2022, and reference lists of relevant papers were searched to include additional papers. For studies that (1) gathered data on gender identity, sexual identity, and PTSD but did not report PTSD data for SMW separately in published articles and (2) gathered data on comorbid PTSD/HD but did not report this data for SMW separately in published articles, authors were contacted with requests for information and given a specific window to respond.
Study Selection and Data Extraction
All papers were gathered using search terms and databases specified previously, and duplicates were removed. Titles and abstracts were screened by independent coders (second, third, fifth, and sixth authors) to remove non-pertinent articles. A third coder (first author) rescreened titles and abstracts for which there were disagreements between the first two coders. Full texts of the remaining articles were reviewed by independent coders (second, fourth, fifth, and sixth authors) and inclusion and exclusion criteria were applied to exclude articles that did not meet criteria. Disagreements between coders for the full-text screening process were re-examined by the meta-analysis team to determine whether to keep the text.
Data for each study, including SMW sample size (and heterosexual women sample size, if applicable), sexual identity, and measures of probable PTSD and PTSD symptom severity, were extracted and are summarized in Appendix B. Empirical data were also extracted, including the proportion of samples that met criteria for probable PTSD, PTSD symptom severity scores, and the proportion of samples that met criteria for probable comorbid PTSD/HD. Data were extracted by independent coders (second, fourth, fifth, and sixth authors), and data were checked for accuracy by an independent coder (third author).
Data Analysis
Meta-analyses, moderation analyses, and publication bias analyses were conducted in R version 4.1.2 using the packages metafor (Viechtbauer, 2010) and meta (Balduzzi et al., 2019). To meta-analyze probable PTSD diagnosis and mean levels of PTSD symptom severity among SMW and between SMW and heterosexual women, when applicable, we used several different types of meta-analytic effect sizes (described below). All individual study effect sizes were inverse-variance weighted to account for sample size of each study, such that studies with larger samples were more heavily weighted in the meta-analyses (Lipsey & Wilson, 2001). An inclusion criterion (sample size ≥30) was added during the search process to reduce threats to internal validity and risks of sampling error (Lin, 2018). For each meta-analysis, only one effect size per population was used to meet the assumption of independence for meta-analysis data.
Probable PTSD and Mean Levels of PTSD Symptom Severity among SMW
Proportions of SMW meeting criteria for probable PTSD were extracted from each study. These proportions were then logit transformed prior to meta-analysis. Logit-transformed proportion effect sizes are recommended when between-study heterogeneity is important (Lipsey & Wilson, 2001). The logit-transformed proportion was used given that this study aimed to examine how methodological and population characteristics influenced overall effect sizes. Once logit-transformed proportions were combined, the aggregate effect size was then transformed back into a proportion for interpretation. Probable PTSD rates were interpreted based on standards for the measure(s) used (e.g., ≥33 on the PCL-5; Bovin et al., 2016). For studies that reported PTSD symptom severity using the same measure (e.g., PCL-5), mean symptom severity levels were calculated across these samples and used as an effect size (Lipsey & Wilson, 2001).
Potential Disparities in Probable PTSD and Mean Levels of PTSD Symptom Severity between SMW and Heterosexual Women
When studies included a heterosexual-women comparison group, separate proportions for SMW and heterosexual women who met criteria for probable PTSD were extracted. Odds ratios were calculated for each study from extracted proportions and log transformed before meta-analysis to center effect sizes around zero and make calculating standard errors easier (Lipsey & Wilson, 2001). Once logit-transformed odds ratios were combined, the aggregate effect size was then transformed back into an odds ratio for interpretation. For studies that reported PTSD symptom severity using a continuous measure, the standardized mean difference (SMD) was used to compare mean levels of PTSD symptom severity.
Probable PTSD and Mean Levels of PTSD Symptom Severity among SMW across Race/Ethnicity, Sexual Identity, and Gender Identity
We examined race/ethnicity, sexual identity, and gender identity as moderators of the proportion of SMW meeting criteria for probable PTSD. Proportions of probable PTSD among different SMW subgroups (i.e., racial/ethnic minority vs. White; bi+ vs. gay/lesbian; transgender or gender diverse vs. cisgender) were separated; odds ratios were calculated for each comparison and logit-transformed before being meta-analyzed. Once logit-transformed odds ratios were combined, the aggregate effect size was then transformed back into an odds ratio.
We also examined race/ethnicity, sexual identity, and gender identity as moderators of PTSD symptom severity among SMW. SMD was calculated for each subgroup comparison and meta-analyzed to report an overall SMD. The SMD was then used to compare PTSD symptom severity among SMW subgroups as it allowed us to analyze PTSD symptom severity across all relevant studies, regardless of the PTSD measure used (Lipsey & Wilson, 2001). We used small, medium, and large effect size designations from Cohen (1988) when interpreting the SMD.
Proportion of SMW with Probable Comorbid PTSD/HD and Disparities in Probable Comorbid PTSD/HD between SMW and Heterosexual Women
For studies that included measures of both PTSD and HD, proportions of SMW reporting comorbid PTSD/HD were extracted, if reported in the paper or provided by study authors separately. Proportions were then logit-transformed and meta-analyzed, and the aggregate effect size was transformed back into a proportion for interpretation. For studies that included proportions of both SMW and heterosexual women with comorbid PTSD/HD, we extracted proportions or requested proportions from authors. We then computed odds ratios for individual studies, logit transformed individual-study odds ratios, meta-analyzed logit-transformed odds ratios, and transformed the aggregate effect size back into an odds ratio for interpretation. HD rates were interpreted based on standards for the measure(s) used (i.e., ≥8 on the AUDIT, ≥3 on the AUDIT-C; and ≥2 on the AUDADIS-5; Babor et al., 2001; Bush, 1998; Grant et al., 2015).
Study Quality Assessment
Study quality was assessed by the fourth and seventh authors with the National Institutes of Health (NIH) Quality Assessment Tool for Observational Cohort and Cross-Sectional studies (National Heart, Lung, and Blood Institute, 2014), which examines study quality based on 14 criteria related to study planning, recruitment, measures used, and data analysis plan.
Publication Bias Assessment
We assessed publication bias by computing the Egger’s test for each meta-analysis with at least ten effect sizes (Egger et al., 1997). If the Egger’s test was significant, we used the trim- and-fill method (Duval & Tweedie, 2000) to examine the effect of publication bias on our meta-analytic results. Individual study effect sizes and standard errors were plotted to see if the plot forms a funnel shape around the aggregate effect size. After conducting a trim-and-fill analysis, a new overall mean effect size was calculated to determine the extent to which potentially missing studies influenced the original aggregate effect size.
Results
A total of 385 papers were identified during the search process (see Figure 1). Duplicates were removed (n = 185), and remaining titles and abstracts were screened. Next, 79 papers were removed and 132 papers remained for full-text analysis. After applying inclusion and exclusion criteria during full-text review, 45 papers remained and were included in the meta-analysis.
Figure 1.
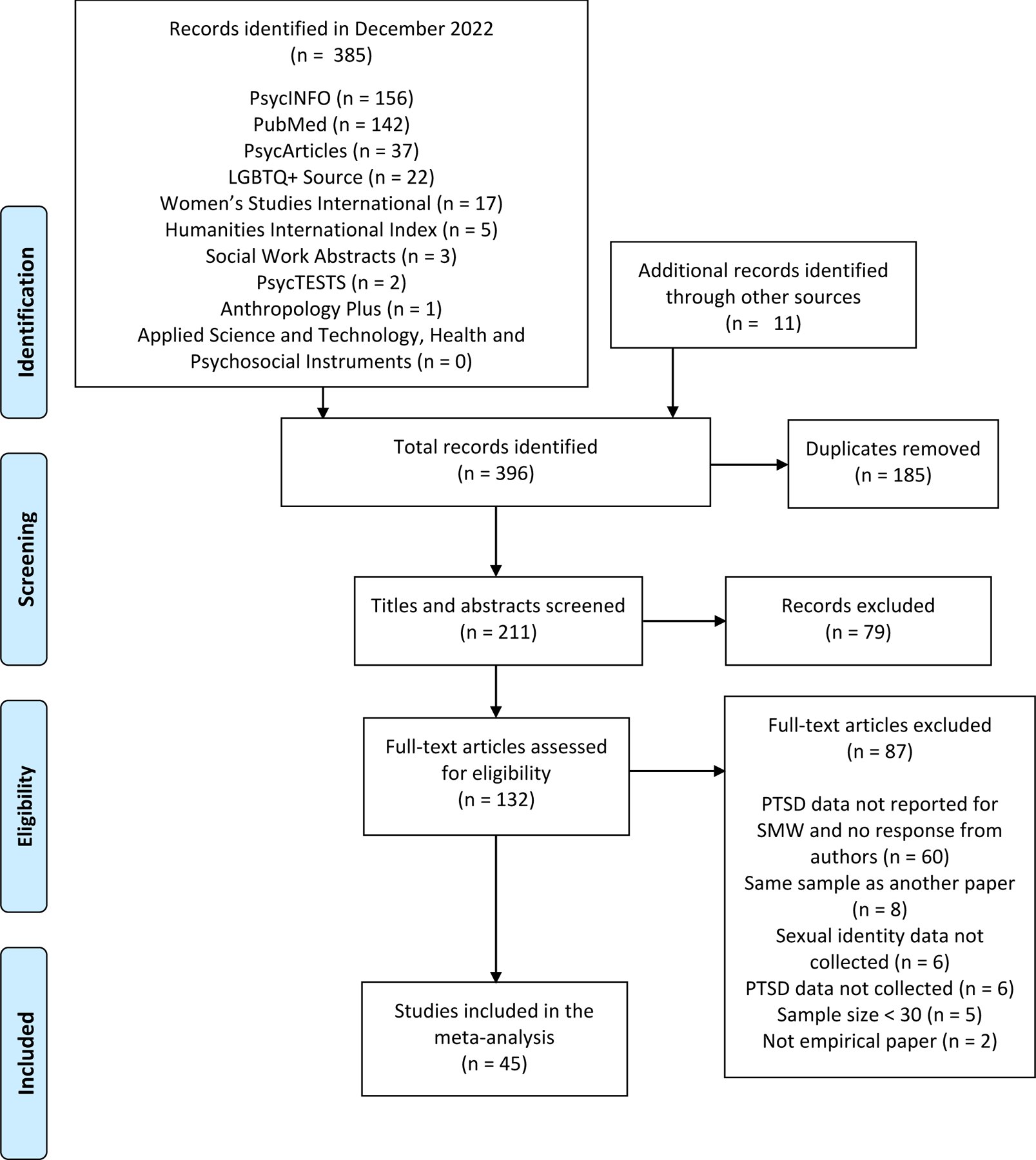
Flow Diagram for Including Studies in this Meta-Analysis
Meta-Analyses
SMW with Probable PTSD
Overall, a total of 43 studies reported probable PTSD rates among SMW (N = 17,395). Probable PTSD rates ranged from 7% to 87% across studies. After individual probability estimates were logit-transformed and meta-analyzed, the aggregate proportion of SMW meeting criteria for PTSD was 35% (95% CI = 29–42; p < .001; see Figure 2). The funnel plot for this meta-analysis did not demonstrate significant asymmetry with the Egger’s test (t(41) = 1.54, p = 0.13 (see Supplemental Material)).
Figure 2.
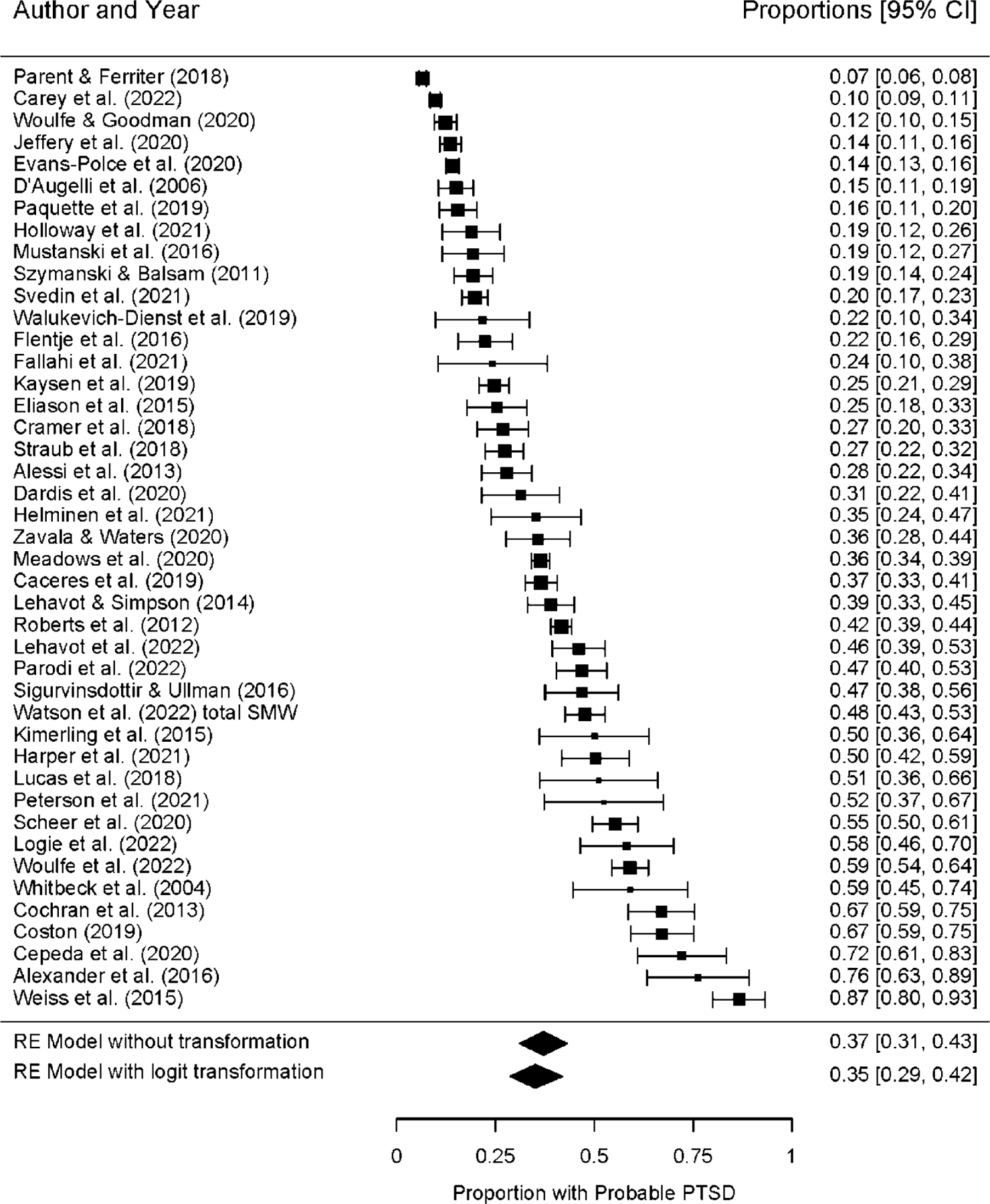
Proportion of SMW with Probable PTSD
Note. SMW = sexual minority women; RE = random effects; CI = confidence interval; PTSD = posttraumatic stress disorder.
Mean Levels of PTSD Symptom Severity among SMW
Overall, there were enough measurements to meta-analyze symptom severity for two sets of measures (i.e., PCL-C/PCL-S and PCL-5; see Table S.1 in the Supplemental Material). Nine papers reported symptom severity using the PCL-C or the PCL-S, and the meta-analysis demonstrated an overall moderate symptom severity score of 35.08 (Range = 17–85; SD = 15.62). Ten papers reported symptom severity using the PCL-5, and the meta-analysis demonstrated an overall symptom severity score of 24.51, which is below the diagnostic cutoff of 33 (Range = 0–80; SD = 20.45).
Probable PTSD Rates between SMW and Heterosexual Women
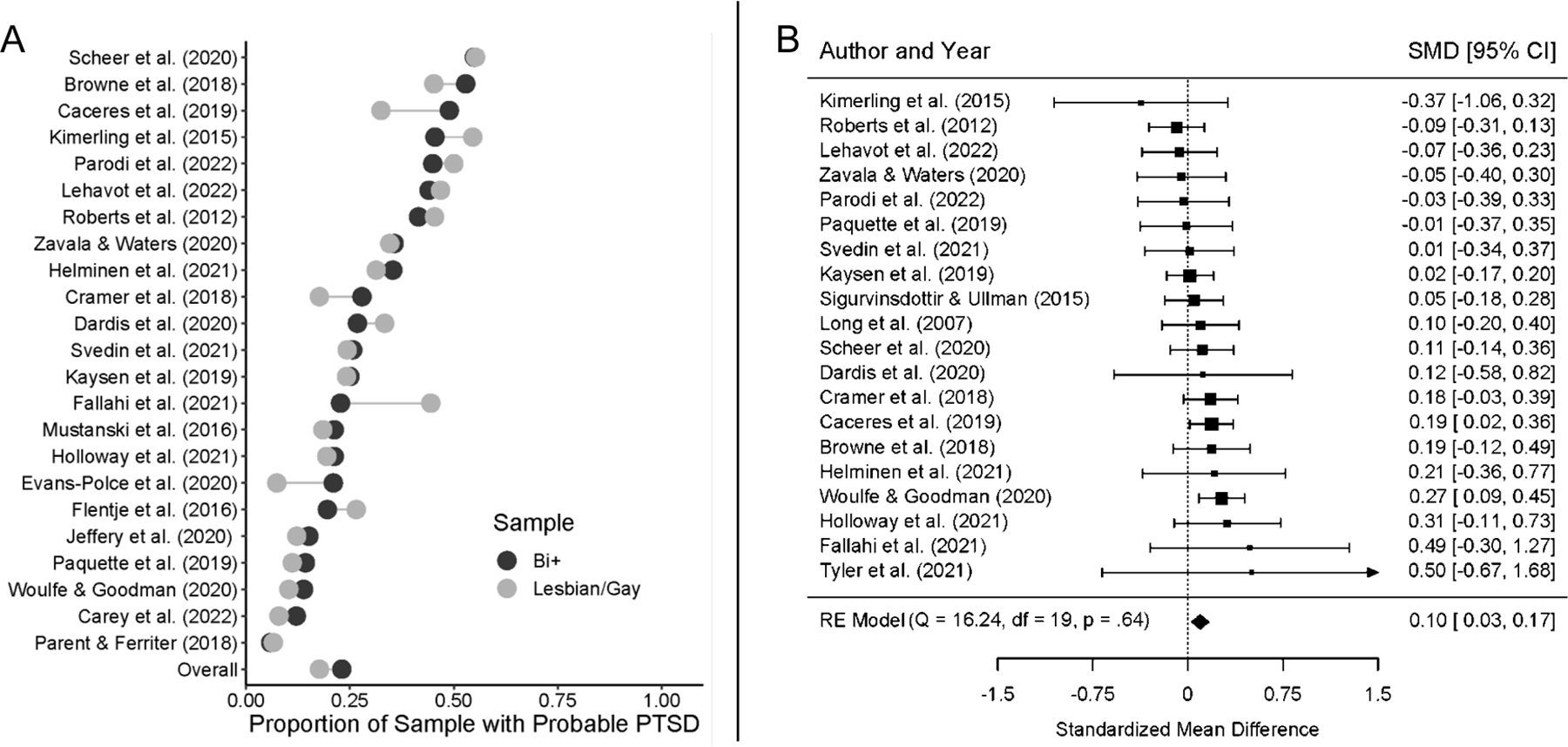
SMW were more likely than heterosexual women to meet criteria for probable PTSD (OR = 2.15; 95% CI = 1.70–2.73; p < .001; Figure 3, panel A). The funnel plot for this meta-analysis did not demonstrate significant asymmetry with the Egger’s test (t(26) = −0.26, p = 0.80 (see Supplemental Material)).
Figure 3.
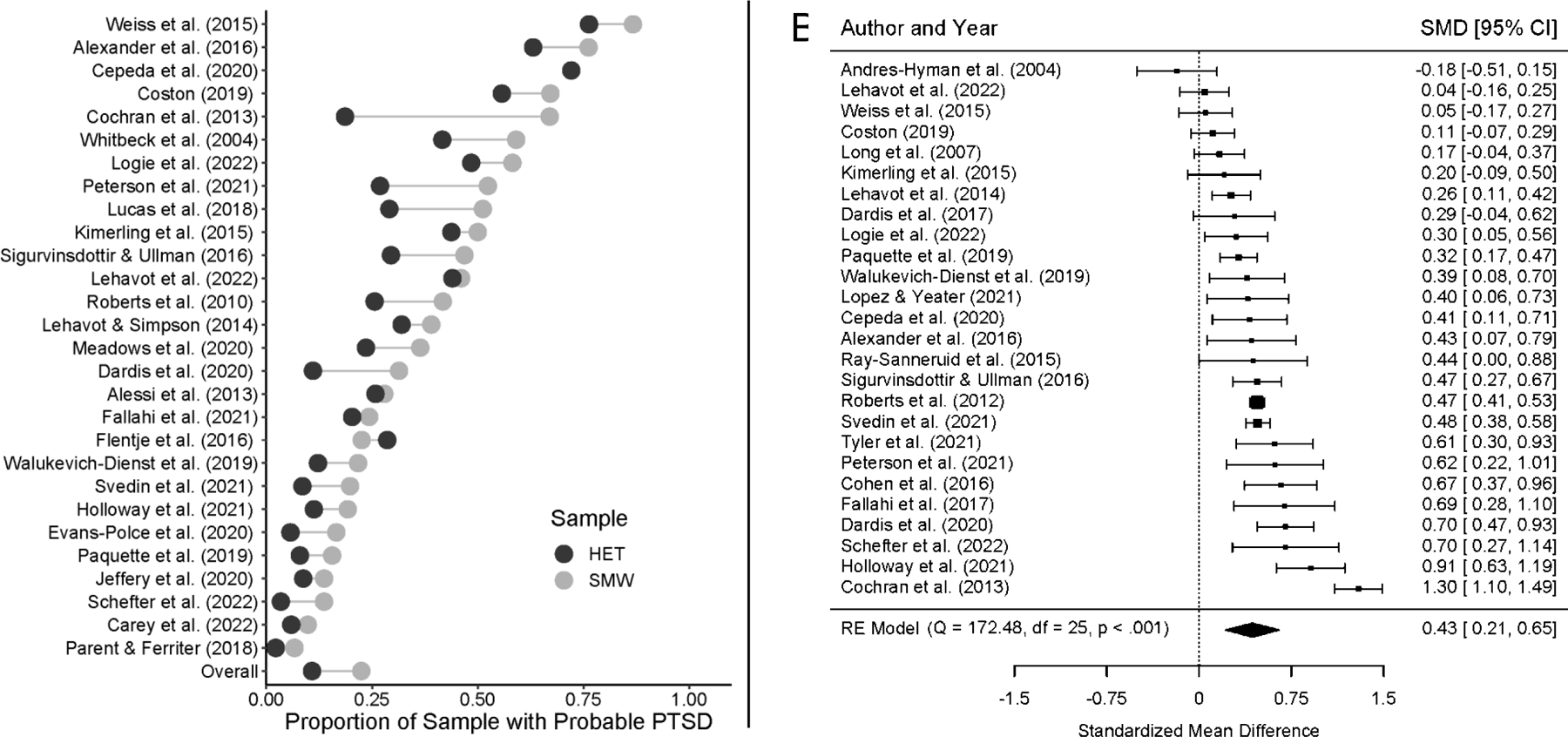
Comparisons between SMW and Heterosexual Women for Proportion with Probable PTSD (A) and PTSD Symptom Severity (B)
Note. SMW = sexual minority women; HET = heterosexual women; SMD = standardized mean difference; RE = random effects; CI = confidence interval; PTSD = posttraumatic stress disorder. Positive SMD values in Panel B indicate higher symptom severity for SMW compared to heterosexual women.
Mean Levels of PTSD Symptom Severity between SMW and Heterosexual Women
SMW also reported greater mean levels of PTSD symptom severity than heterosexual women, with a medium effect size (SMD = 0.43; 95% CI = 0.21–0.65; p < .001; Figure 3, panel B). The funnel plot for this meta-analysis did not demonstrate significant asymmetry with the Egger’s test (t(24) = −0.22, p = 0.82 (see Supplemental Material)).
Demographic Moderators of Probable PTSD among SMW
SMW of color were more likely than White SMW to meet criteria for probable PTSD (OR = 1.19; 95% CI = 1.01–1.39; p = .03; Figure 4, panel A). Probable PTSD rates did not differ between bi+ and gay/lesbian participants (OR = 1.21; 95% CI = 0.997–1.48; p = .053; Figure 5, panel A). Transgender and gender diverse people were more likely than cisgender SMW to meet criteria for probable PTSD (OR = 1.75; 95% CI = 1.22–2.50; p = .002; Figure 6, panel A).
Figure 4.
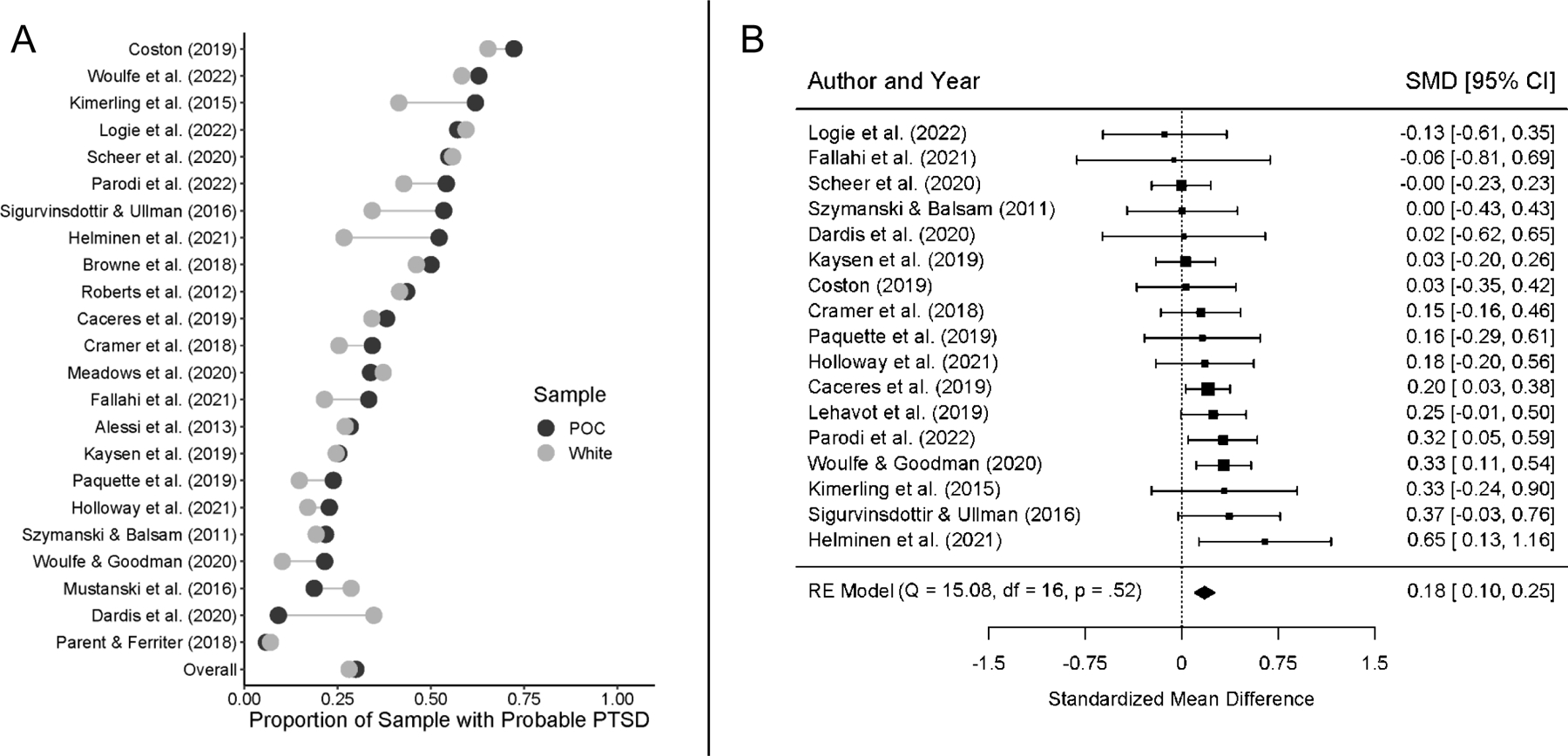
Comparisons between SMW of Color and White SMW for Proportion with Probable PTSD (A) and PTSD Symptom Severity (B)
Note. SMW = sexual minority women; POC = sexual minority women of color; SMD = standardized mean difference; RE = random effects; CI = confidence interval; PTSD = posttraumatic stress disorder. Positive SMD values in Panel B indicate higher symptom severity for SMW of color compared to White SMW.
Figure 5.
Comparisons between Bi+ SMW and Gay/Lesbian SMW for Proportion with Probable PTSD (A) and PTSD Symptom Severity (B)
Note. SMW = sexual minority women; SMD = standardized mean difference; RE = random effects; CI = confidence interval; PTSD = posttraumatic stress disorder. Positive SMD values in Panel B indicate higher symptom severity for bi+ SMW compared to gay/lesbian SMW.
Figure 6.
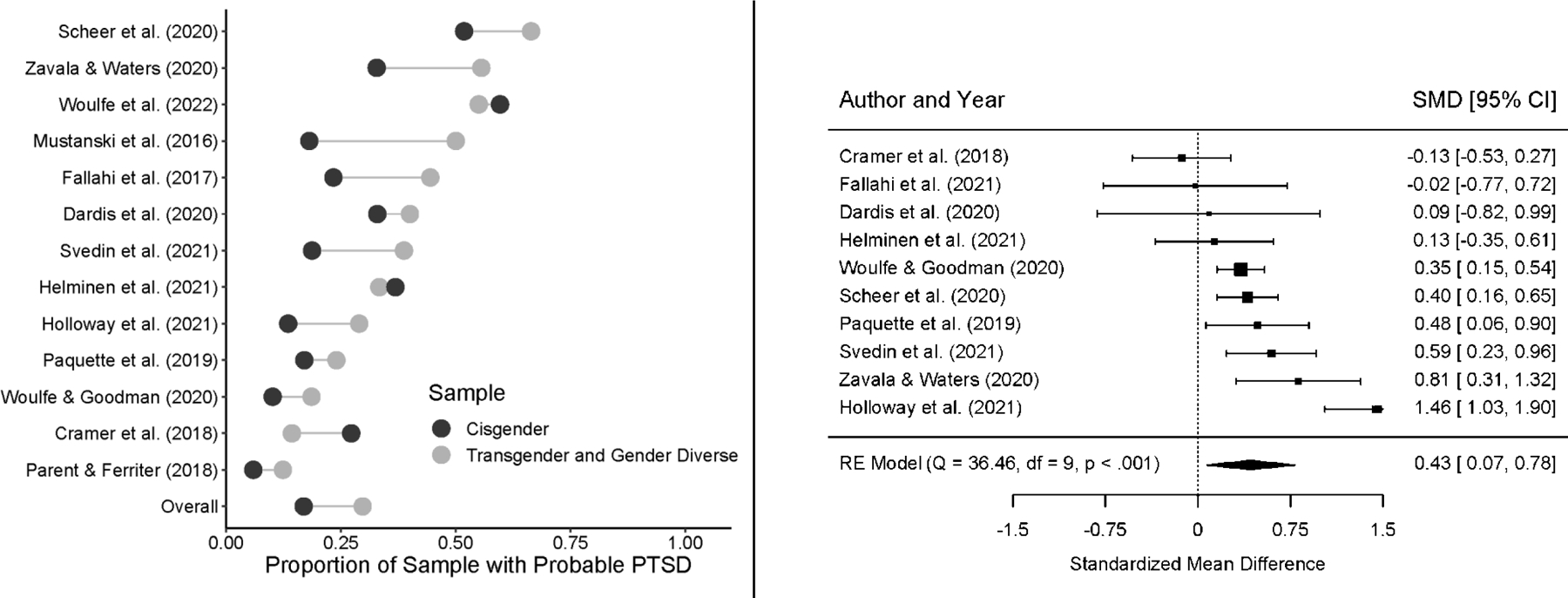
Comparisons between Transgender and Gender Diverse People and Cisgender SMW for Proportion with Probable PTSD (A) and PTSD Symptom Severity (B)
Note. SMW = sexual minority women; SMD = standardized mean difference; RE = random effects; CI = confidence interval; PTSD = posttraumatic stress disorder. Positive SMD values in Panel B indicate higher symptom severity for transgender and gender diverse people compared to cisgender SMW.
The funnel plot for the meta-analysis examining differences across race/ethnicity (t(21) = 2.31, p = .03) and sexual identity (t(21) = −3.21, p = .004) (i.e., race/ethnicity and sexual identity as demographic moderators of probable PTSD among SMW) demonstrated significant asymmetry with Egger’s tests (see Figure S.2 in the Supplemental Material). Using the trim-and- fill method to correct for publication bias, the aggregate effect size comparing probable PTSD between SMW of color and White SMW became non-significant (OR = 1.06; 95% CI = 0.88–1.27), and the aggregate effect size comparing probable PTSD between bi+ and gay/lesbian SMW became significant (OR = 1.44; 95% CI = 1.20–1.72), with bi+ SMW being more likely to report probable PTSD. The funnel plot for the meta-analysis examining differences in probable PTSD across gender identity did not demonstrate significant asymmetry with the Egger’s test (t(11) = 0.13, p = .90).
Demographic Moderators of Mean Levels of PTSD Symptom Severity among SMW
SMW of color reported greater mean levels of PTSD symptom severity than White SMW with a small effect size (SMD = 0.18, 95% CI = 0.10–0.25; p < .001; Figure 4, panel B). Bi+ women reported greater mean levels of PTSD symptom severity than gay/lesbian SMW with a small effect size (SMD = 0.10, 95% CI = 0.03–0.17; p = .004; Figure 5, panel B). Transgender and gender diverse people reported greater levels of PTSD symptom severity than cisgender SMW with a medium effect size (SMD = 0.43, 95% CI = 0.07–0.78; p = .02; Figure 6, panel B).
The funnel plot for the meta-analysis examining differences across race/ethnicity, t(15) = −0.32, p = .76; sexual identity, t(18) = −0.32, p = .75; and gender identity, t(8) = 0.16, p = .87 (i.e., race/ethnicity, sexual identity, and gender identity as demographic moderators of mean levels of PTSD symptom severity among SMW), did not demonstrate significant asymmetry with Egger’s tests (see Supplemental Material).
Probable Comorbid PTSD/HD among SMW
Overall, six studies reported probable PTSD/HD comorbidity among SMW. After individual proportions were logit-transformed and meta-analyzed, the aggregate proportion of SMW who met criteria for probable comorbid PTSD/HD was 17% (95% CI = 10–28; p < .001) (see Figure S.1 in the Supplemental Material).
Probable Comorbid PTSD/HD between SMW and Heterosexual Women
Five studies included a heterosexual comparison group. In these, SMW were more likely than heterosexual women to meet criteria for probable comorbid PTSD/HD (OR = 4.51; 95% CI = 1.49–13.62; p = .008; see Figure 7).
Figure 7.
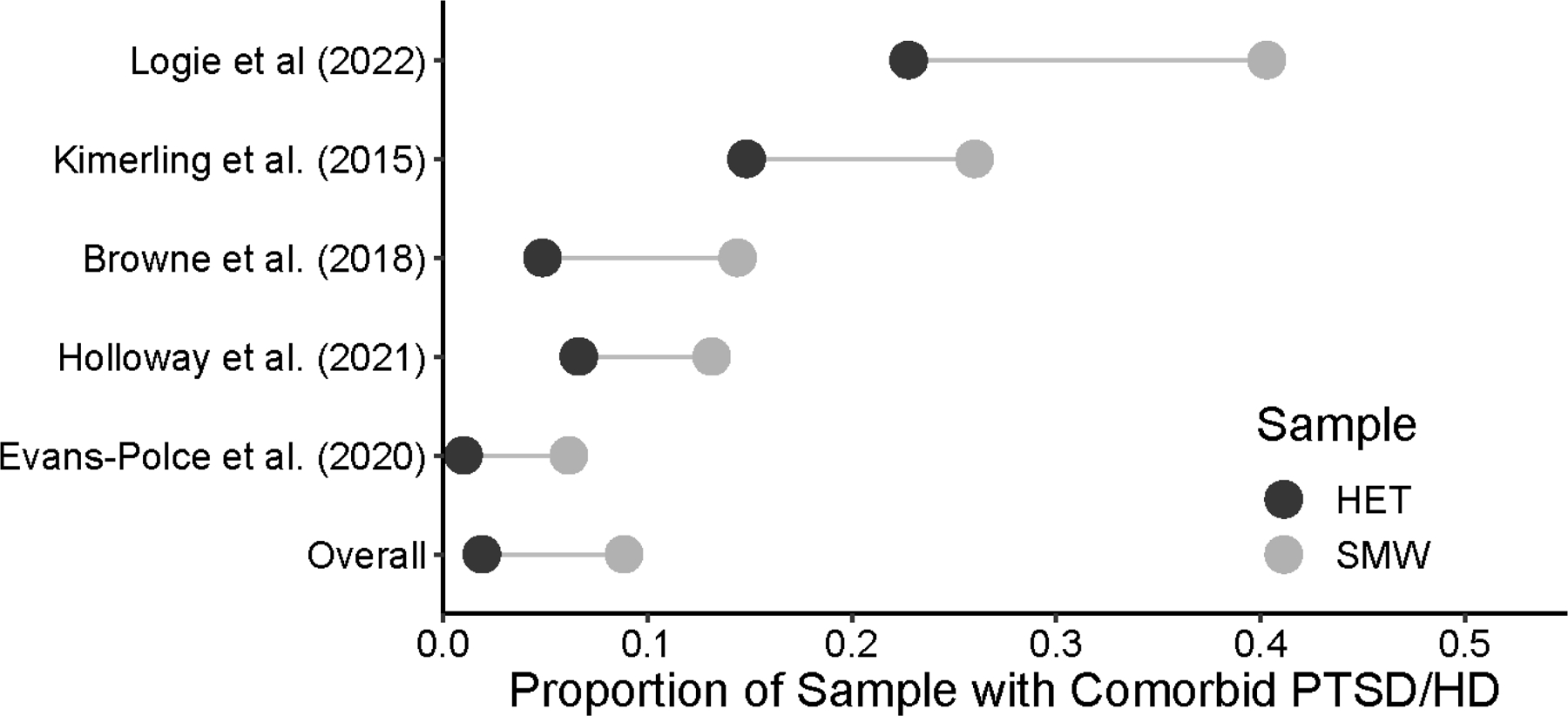
Comparisons between SMW and Heterosexual Women for Proportion with Probable PTSD/HD
Note. SMW = sexual minority women; HET = heterosexual women; PTSD = posttraumatic stress disorder; HD = hazardous drinking.
Study Quality Results
The study quality assessment is detailed in the Supplemental Material. The primary study quality concerns identified in this body of literature were related to the use of cross-sectional designs and lack of justification for sample size with a power analysis.
Discussion
Responding to calls for research to identify individuals at greatest risk of developing PTSD (Christ et al., 2021), this meta-analysis yielded the most current and robust estimates of SMW’s disproportionate risk of probable PTSD and PTSD symptom severity compared to heterosexual women. Specifically, SMW were more than twice as likely as heterosexual women to meet criteria for probable PTSD. SMW also reported greater mean levels of PTSD symptom severity. Results further clarified SMW’s distinct risk of probable PTSD and PTSD symptom severity, particularly among SMW of color, transgender and gender diverse people, and bi+ SMW. We also derived estimates of SMW’s disproportionate risk of probable comorbid PTSD/HD relative to heterosexual women. SMW were more than four times as likely as heterosexual women to meet criteria for probable comorbid PTSD/HD.
These findings underscore the need to assess and monitor PTSD and comorbid PTSD/HD among SMW and rapidly connect at-risk SMW to evidence-based, scalable interventions targeting these highly prevalent mental and behavioral health conditions. Our results indicated markedly elevated rates of probable PTSD among SMW, which may be due partly to the increased likelihood of experiencing early, severe, and multiple forms of trauma (Porsch et al., 2022; Salim et al., 2022). In addition, prior evidence suggests that inadequate social support, help-seeking barriers, and self-blame are associated with SMW’s increased risk of negative trauma sequelae, including PTSD (Salim et al., 2022; Sigurvinsdottir & Ullman, 2016). Moreover, SMW face minority-specific stressors (Brooks, 1981; Dyar et al., 2018; Meyer, 2003; Pachankis et al., 2017, 2020), chronic-threat vigilance, and threats to social safety (Diamond & Alley, 2022). These cumulative life stressors may contribute to prolonged and sensitized stress responses, such as blunted cortisol levels, lowering thresholds for tolerating threats and contributing to PTSD risk among SMW (Diamond & Alley, 2022; Juster et al., 2019).
We also found that SMW reported significantly greater PTSD symptom severity than heterosexual women. Differences in PTSD symptom severity levels between SMW and heterosexual women were consistent across measures assessing Diagnostic and Statistical Manual of Mental Disorders (DSM-IV, DSM-5) criteria. These findings are notable given that greater PTSD symptom severity, even among those who do not meet criteria for PTSD (i.e., subthreshold PTSD), is associated with greater functional impairment, alcohol use disorders, and other psychiatric comorbidities (Morgan-López et al., 2020). If left untreated, 20% of those with subthreshold PTSD developed full PTSD within two years (Breslau et al., 2004). As such, early intervention for those with subthreshold PTSD is important, especially for SMW.
Consistent with some prior research (Balsam et al., 2015; Cerezo & Ramirez, 2020; Evans-Polce & McCabe, 2020; Sigurvinsdottir & Ullman, 2016; Veldhuis et al., 2022), this study found that SMW of color, and transgender and gender diverse people were more likely to meet criteria for probable PTSD and report greater PTSD symptom severity levels than White SMW and cisgender SMW, respectively. Bi+ participants also reported greater mean levels of PTSD symptom severity than gay/lesbian SMW. These intragroup disparities in PTSD may be explained by greater exposure to traumatic events that are highly predictive of PTSD, such as assaultive interpersonal violence and “corrective rape” (Pittman et al., 2022; Porsch et al., 2022). Moreover, cumulative adversity may contribute to fewer coping resources that are integral to managing stress among SMW of color, transgender and gender diverse people, and bi+ women (Batchelder et al., 2022; Cerezo & Ramirez, 2020; Jhe et al., 2021; Page et al., 2021).
Other factors compounding risk of PTSD among SMW of color, transgender and gender diverse people, and bi+ women are intersectional minority stressors, such as gendered racism and monosexism (Cerezo & Ramirez, 2020; Dworkin et al., 2018; Jackson et al., 2021; Sarno et al., 2021). For example, Black women are sometimes viewed as oversexualized, stoic, and sexually deviant; these stereotypes increase risk of sexual assault and negatively impact stress and coping (Leath et al., 2022). For SMW who identify as transgender or gender diverse, experiences of sexism might be experienced as incongruent or dysphoric (Scheer et al., 2021), potentially exacerbating mental health issues, such as PTSD. Future research should consider whether higher rates of sexual and gender identity outness among SMW who identify as transgender or gender diverse predict greater adversity and subsequent PTSD (Pachankis et al., 2020). Furthermore, SMW who face multiple forms of social and systemic subordination based on unique combinations of social identities (i.e., negative intersectional experiences; Jackson et al., 2021) also report difficulty accessing adequate services and being dissatisfied with treatment (Scheer, Batchelder, et al., 2022), impeding timely intervention (Livingston et al., 2020).
Notably, meta-analyses examining differences in probable PTSD between racial/ethnic SMW and White SMW, and between bi+ SMW and gay/lesbian SMW demonstrated some publication bias. When including potentially missing effect sizes using the trim-and-fill method, we found inconsistent patterns of effect sizes for race/ethnicity and sexual identity comparisons. After correcting for bias, SMW’s rates of probable PTSD no longer varied across race/ethnicity but did vary across sexual identity. Publication bias did not seem evident in other analyses.
Our findings also provide compelling evidence of frequent comorbidity between PTSD and HD among SMW; 17% met criteria for probable comorbid PTSD/HD. This estimate is higher than previous research using a representative sample of sexual minority people (7.4%; Simpson et al., 2019). In the general U.S. population, estimates of comorbid PTSD/HD vary widely (9.8% to 61.3%; Debell et al., 2014). Strikingly, we also found that SMW were more than four times as likely as heterosexual women to meet criteria for probable comorbid PTSD/HD. Extant research in the general population and among SMW show robust associations between PTSD and HD (Dworkin et al., 2020; Helminen et al., 2021; Hien et al., 2021). According to the self-medication hypothesis (Khantzian, 1985) and consistent with social learning theory (Bandura, 1977), alcohol is used to reduce distressing threat-related symptoms (Patel et al., 2022) and interoceptive cues, such as affect and cognitions (Hawn et al., 2020). Indeed, drinking-to-cope can increase risk of re-victimization and contribute to greater incidence and persistence of PTSD and HD by reducing the ability to accurately detect threat (Kaysen et al., 2017; Steele & Josephs, 1990); diminishing fear extinction learning, leading to dysregulated arousal responses; and, disrupting habituation to trauma-related memory reconsolidation and cues (Straus et al., 2022). Additional work is needed to clarify processes central to the etiology of PTSD/HD among SMW (e.g., permissive beliefs, instrumental thoughts, memory processing, cue reactivity, social influence risk factors; Dyar & Kaysen, 2022; Palmisano et al., 2022) given their unique drinking norms, expectancies, and motives (Ehlke et al., 2022; Hughes et al., 2020).
Clinical and Future Research Implications
While SMW are more likely than heterosexual women to seek mental health treatment (Cochran et al., 2003)—likely because of greater burden of health risks (Evans-Polce & McCabe, 2020; Hughes et al., 2020; Pharr et al., 2019)—they are also more likely to delay needed care and miss appointments because of access barriers, including being uninsured, experiencing and anticipating stigma, and feeling dissatisfied with treatment (Batchelder et al., 2021; Lynch et al., 2021; Pachankis et al., 2021; Scheer, Batchelder, et al., 2022). SMW may seek help when facing severe symptoms and thus may have increased vulnerability to acute PTSD- and alcohol-attributable harm, including death (Lehavot et al., 2017; Livingston et al., 2022; Lynch et al., 2021). Further, nearly 75% of individuals with comorbid PTSD/HD do not seek treatment (Blanco et al., 2013); among those who do, attrition is high (Roberts et al., 2015). Thus, providers have less time to identify and treat SMW with PTSD/HD (Livingston et al., 2022).
SMW may not benefit from existing interventions to the same extent as heterosexual women (Beard et al., 2017; Pachankis et al., 2022). Current evidence-based treatment models targeting PTSD and HD (e.g., prolonged exposure, motivational interviewing) do not explicitly consider SMW’s comorbid health needs, barriers to treatment access and retention in care, or unique risk factors of PTSD and HD, such as enacted, anticipated, and internalized stigma (Pachankis et al., 2022; Scheer, Clark, et al., 2022). In fact, <1% of alcohol interventions have examined sexual identity differences and <18% of substance use facilities in the U.S. have sexual minority-specific programming (Helminen et al., 2022; Williams & Fish, 2020).
Findings from this meta-analysis underscore the importance of effectively screening SMW for PTSD and comorbid PTSD/HD. It is critical for providers to center SMW’s needs and experiences when screening for PTSD and comorbid PTSD/HD, for example, by gathering information about whether SMW’s PTSD-related disruptions in cognition and mood are exacerbated by salient stigma-related experiences, thoughts, and beliefs (Livingston et al., 2020). When delivering treatment involving exposure to trauma stimuli, clinicians should consider safety concerns or reasons for feared consequences that might be salient for SMW, including ongoing violence exposure, family rejection, and likelihood of identity-related assault (Scheer, Clark, et al., 2022). Providers working from a cognitive behavioral therapy (CBT) framework might assess SMW-specific high-risk situations leading to permissive beliefs about using alcohol to cope with stigma- or trauma-related distress (Hien et al., 2021). Clinicians might also assess for PTSD and comorbid PTSD/HD etiologic and maintenance mechanisms (e.g., under- vs. over-modulating negative affect) to improve diagnostic clarity in PTSD symptoms, identify treatment needs, match SMW to personalized treatment, and predict treatment response (Ressler, 2018).
Results from this meta-analysis highlight the importance of increasing access to treatment targeting PTSD and comorbid PTSD/HD, reducing dropout rates among treatment seekers, and improving treatment outcomes among SMW. Recent research suggests that lowering structural stigma, such as systemic discrimination and inadequate government funding, promotes availability of tailored programming for sexual and gender minority people (Cascalheira et al., 2022). Other research has shown that motivational enhancement therapy (MET) increases treatment attendance and retention among individuals seeking treatment targeting PTSD, substance use disorders, and comorbid PTSD/substance use disorders (Kaysen et al., 2022). Moreover, training clinicians to incorporate cultural humility approaches (i.e., accepting feedback about how one’s identities and experiences may bias awareness of clients’ identities and experiences and repairing cultural ruptures within therapeutic relationships; Gonzalez et al., 2021) has led to improved treatment engagement among minoritized clients (Hook et al., 2013). Future research should extend prior research by examining whether training providers in applying cultural humility frameworks and employing culturally tailored MET could lead to increases in SMW’s initiation and retention in treatment targeting PTSD and PTSD/HD.
Recent evidence suggests preliminary efficacy of integrated treatments that combine trauma-focused therapy with cognitive-behavioral approaches to treating substance use disorders (Flanagan et al., 2016). For instance, one meta-analysis (Foa et al., 2007) found that prolonged exposure for PTSD delivered alongside relapse prevention therapy for substance use disorders resulted in greater reductions in PTSD symptoms and substance misuse compared to non-trauma-focused interventions (e.g., mutual-aid groups). Concurrent Treatment of PTSD and Substance Use Disorders Using Prolonged Exposure (COPE; Back et al., 2014) represents one promising integrated CBT-based treatment that has demonstrated initial efficacy (compared to relapse prevention for substance use disorders and an active monitoring control group) in reducing PTSD symptom severity and frequency of recent primary substance use (Persson et al., 2017; Ruglass et al., 2017). To our knowledge, only one known study has demonstrated efficacy of COPE in reducing women’s PTSD and HD severity (Persson et al., 2017). None of this research is specific to SMW with comorbid PTSD/HD and no current evidence-based integrated treatment has been adapted for SMW with PTSD and HD. Nevertheless, meta-analytic findings indicate that culturally adapted interventions produce better outcomes than other conditions, including non-culturally adapted treatments (Hall et al., 2016). Thus, research should develop evidence-based, culturally adapted, and scalable treatments for SMW with probable PTSD, who report severe PTSD symptoms, and with probable comorbid PTSD/HD.
Limitations of this Meta-Analysis
Several limitations of this meta-analysis should be noted. First, most studies used scales measuring past-month PTSD, however a few studies used past-week, past-year, and lifetime timeframes. Research is needed to determine potential sexual identity-related disparities in probable PTSD across various impairment and functioning levels to refine our understanding of PTSD in this population (Sullivan et al., 2016). Moreover, despite heterogeneity in clinical presentations of PTSD (Neria, 2021), the present study did not account for variation in symptom weighting, such as whether symptom clusters (e.g., negative alterations in cognitions and mood vs. marked alteration in arousal and reactivity) may be more heavily connected to PTSD symptom severity in SMW than in heterosexual women or across certain SMW subgroups (Morgan-López et al., 2020). Examining symptom cluster and relevance, such as frequency and intensity, could increase accuracy in using dimensional approaches to examine PTSD disparities among SMW and between SMW and heterosexual women (Ruglass et al., 2020). Attending to heterogeneity in PTSD symptom clusters could improve treatment efficacy, track temporal changes in clinical outcomes, and provide greater diagnostic specificity for PTSD (Neria, 2021). Given inclusion criteria for this meta-analysis, results may overrepresent SMW with PTSD and HD. Thus, future studies should identify the population prevalence of probable PTSD, PTSD symptom severity, and comorbid PTSD/HD among SMW.
Moreover, SMW subgroup differences in PTSD were not examined across other general sociodemographic characteristics, such as income, age, and location, and those specific to SMW (e.g., outness). Further, studies did not assess or report demographic characteristics (e.g., race/ethnicity, sexual identity, gender identity) in consistent ways. Finally, selection bias should be considered (Ahmed et al., 2012). For example, papers from other countries may not have been identified given the English-language criterion of this study. Future work should consider potential cultural differences in studies of PTSD and comorbid PTSD/HD disparities among women and transgender populations. Research is also needed to clarify sexual identity-related disparities in specific PTSD symptoms (e.g., alterations in cognition and mood, persistent avoidance) and comorbid alcohol use disorder and other drug use disorders, such as opioid use disorder, among women (Schuler et al., 2019). Finally, we also did not examine findings from unpublished work, potentially inflating associations found in the present study.
Conclusion
The current meta-analysis clarifies the magnitude of disparities in probable PTSD, PTSD symptom severity, and comorbid PTSD/HD between SMW and heterosexual women. Findings also provide robust evidence that SMW of color, transgender and gender diverse people, and bi+ women are at greatest risk of probable PTSD, PTSD symptom severity, and probable comorbid PTSD/HD. Results emphasize the importance of improving diagnostic assessment of trauma-related sequalae and examining mechanisms influencing the etiology and maintenance of PTSD and comorbid PTSD/HD among SMW. Further, these findings underscore the need to develop, disseminate, and implement culturally sensitive, integrated treatments to increase treatment utilization and retention and reduce risk of PTSD and co-occurring HD among SMW.
Supplementary Material
Highlights.
SMW were more likely than heterosexual women to meet criteria for probable PTSD.
SMW reported significantly greater PTSD symptom severity than heterosexual women.
Probable PTSD rates and PTSD symptom severity levels varied across SMW subgroups.
Among SMW, 17% met criteria for probable comorbid PTSD/HD.
Rates of probable comorbid PTSD/HD were higher among SMW than heterosexual women.
Role of Funding Sources
Jillian R. Scheer acknowledges support from the National Institute on Alcohol Abuse and Alcoholism, K01AA028239–01A1. Cory Cascalheira acknowledges support as a National Institutes of Health RISE Fellow, R25GM061222. Abigail Batchelder acknowledges support from the National Institute on Drug Abuse, K23DA043418. Tonda L. Hughes is supported by funding from NIAAA (R01AA013328, R01AA029088, and R01AA029088). Information in this report is the authors’ own and does not represent the views of the funders, including the National Institutes of Health.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest
All authors declare that they have no conflicts of interest.
References
- Ahmed I, Sutton AJ, & Riley RD (2012). Assessment of publication bias, selection bias, and unavailable data in meta-analyses using individual participant data: A database survey. BMJ, 344, d7762. 10.1136/bmj.d7762 [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association (APA). (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Washington, DC. [Google Scholar]
- Babor TF, Higgins-Biddle JC, Saunders JB, & Monteiro MG (2001). AUDIT: The Alcohol Use Disorders Identification Test: Guidelines for use in primary care (2nd ed.). World Health Organization. [Google Scholar]
- Back SE, Foa EB, Killeen TK, & Mills KL (2014). Concurrent treatment of PTSD and substance use disorders using prolonged exposure (COPE): Therapist guide Oxford University Press. [Google Scholar]
- Balduzzi S, Rücker G, & Schwarzer G (2019). How to perform a meta-analysis with R: A practical tutorial. Evidence-Based Mental Health, 22(4), 153–160. 10.1136/ebmental-2019-300117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Balsam KF, Molina Y, Blayney JA, Dillworth T, Zimmerman L, & Kaysen D (2015). Racial/ethnic differences in identity and mental health outcomes among young sexual minority women. Cultural Diversity & Ethnic Minority Psychology, 21(3), 380–390. 10.1037/a0038680 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bandura A (1977). Social learning theory Prentice-Hall. [Google Scholar]
- Batchelder AW, Foley JD, Stanton AM, Gorman KR, Morris JC, & Scheer JR (2022). Facets of gender expression and discriminationd in relation to alcohol and other drug use severity among sexual minority women and gender diverse individuals assigned female at birth. LGBT Health. Advanced online publication 10.1089/lgbt.2022.0138 [DOI] [PMC free article] [PubMed]
- Batchelder AW, Stanton AM, Kirakosian N, King D, Grasso C, Potter J, Mayer KH, & O’Cleirigh C (2021). Mental health and substance use diagnoses and treatment disparities by sexual orientation and gender in a community health center sample. LGBT Health, 8(4), 290–299. 10.1089/lgbt.2020.0293 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beard C, Kirakosian N, Silverman AL, Winer JP, Wadsworth LP, & Björgvinsson T (2017). Comparing treatment response between LGBQ and heterosexual individuals attending a CBT- and DBT-skills-based partial hospital. Journal of Consulting and Clinical Psychology, 85(12), 1171–1181. 10.1037/ccp0000251 [DOI] [PubMed] [Google Scholar]
- Blanco C, Hoertel N, Wall MM, Franco S, Peyre H, Neria Y, Helpman L, & Limosin F (2018). Toward understanding sex differences in the prevalence of posttraumatic stress disorder: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. The Journal of Clinical Psychiatry, 79(2), 19420. 10.4088/JCP.16m11364 [DOI] [PubMed] [Google Scholar]
- Blanco C, Xu Y, Brady K, Pérez-Fuentes G, Okuda M, & Wang S (2013). Comorbidity of posttraumatic stress disorder with alcohol dependence among US adults: Results from National Epidemiological Survey on Alcohol and Related Conditions. Drug and Alcohol Dependence, 132(3), 630–638. 10.1016/j.drugalcdep.2013.04.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bostwick WB, Hughes TL, Steffen A, Veldhuis CB, & Wilsnack SC (2019). Depression and victimization in a community sample of bisexual and lesbian women: An intersectional approach. Archives of Sexual Behavior, 48(1), 131–141. 10.1007/s10508-018-1247-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bovin MJ, Marx BP, Weathers FW, Gallagher MW, Rodriguez P, Schnurr PP, & Keane TM (2016). Psychometric properties of the PTSD Checklist for Diagnostic and Statistical Manual of Mental Disorders–Fifth Edition (PCL-5) in veterans. Psychological Assessment, 28(11), 1379–1391. 10.1037/pas0000254 [DOI] [PubMed] [Google Scholar]
- Breslau N, Lucia VC, & Davis GC (2004). Partial PTSD versus full PTSD: An empirical examination of associated impairment. Psychological Medicine, 34(7), 1205–1214. 10.1017/S0033291704002594 [DOI] [PubMed] [Google Scholar]
- Briere J, & Spinazzola J (2005). Phenomenology and psychological assessment of complex posttraumatic states. Journal of Traumatic Stress, 18(5), 401–412. 10.1002/jts.20048 [DOI] [PubMed] [Google Scholar]
- Brooks V (1981). Minority stress and lesbian women Lexington Books. [Google Scholar]
- Bush K (1998). The AUDIT Alcohol Consumption Questions (AUDIT-C)An Effective Brief Screening Test for Problem Drinking. Archives of Internal Medicine, 158(16), 1789. 10.1001/archinte.158.16.1789 [DOI] [PubMed] [Google Scholar]
- Cascalheira CJ, Helminen EC, Shaw TJ, & Scheer JR (2022). Structural determinants of tailored behavioral health services for sexual and gender minorities in the United States, 2010 to 2020: A panel analysis. BMC Public Health, 22(1), 1908. 10.1186/s12889-022-14315-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Castillo-Carniglia A, Keyes KM, Hasin DS, & Cerdá M (2019). Psychiatric comorbidities in alcohol use disorder. The Lancet Psychiatry, 6(12), 1068–1080. 10.1016/S2215-0366(19)30222-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cerezo A, & Ramirez A (2020). Perceived discrimination, alcohol use disorder and alcohol-related problems in sexual minority women of color. Journal of Social Service Research, 47(33–46). 10.1080/01488376.2019.1710657 [DOI] [Google Scholar]
- Christ NM, Elhai JD, Forbes CN, Gratz KL, & Tull MT (2021). A machine learning approach to modeling PTSD and difficulties in emotion regulation. Psychiatry Research, 297, 113712. 10.1016/j.psychres.2021.113712 [DOI] [PubMed] [Google Scholar]
- Cochran SD, Sullivan JG, & Mays VM (2003). Prevalence of mental disorders, psychological distress, and mental health services use among lesbian, gay, and bisexual adults in the United States. Journal of Consulting and Clinical Psychology, 71(1), 53–61. 10.1037/0022-006X.71.1.53 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J (1988). Statistical Power Analysis for the Behavioral Sciences (2nd ed.). Routledge. 10.4324/9780203771587 [DOI] [Google Scholar]
- Cusack SE, Hicks TA, Bourdon J, Sheerin CM, Overstreet CM, Kendler KS, Dick DM, & Amstadter AB (2019). Prevalence and predictors of PTSD among a college sample. Journal of American College Health, 67(2), 123–131. 10.1080/07448481.2018.1462824 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Debell F, Fear NT, Head M, Batt-Rawden S, Greenberg N, Wessely S, & Goodwin L (2014). A systematic review of the comorbidity between PTSD and alcohol misuse. Social Psychiatry and Psychiatric Epidemiology, 49(9), 1401–1425. 10.1007/s00127-014-0855-7 [DOI] [PubMed] [Google Scholar]
- Diamond LM, & Alley J (2022). Rethinking minority stress: A social safety perspective on the health effects of stigma in sexually-diverse and gender-diverse populations. Neuroscience & Biobehavioral Reviews, 138, 104720. 10.1016/j.neubiorev.2022.104720 [DOI] [PubMed] [Google Scholar]
- Drabble LA, Wootton AR, Veldhuis CB, Perry E, Riggle EDB, Trocki KF, & Hughes TL (2020). It’s complicated: The impact of marriage legalization among sexual minority women and gender diverse individuals in the United States. Psychology of Sexual Orientation and Gender Diversity, 7(4), 396–406. 10.1037/sgd0000375 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duval S, & Tweedie R (2000). Trim and fill: A simple funnel‐plot–based method of testing and adjusting for publication bias in meta‐analysis. Biometrics 10.1111/j.0006-341X.2000.00455.x [DOI] [PubMed]
- Dworkin ER, Gilmore AK, Bedard-Gilligan M, Lehavot K, Guttmannova K, & Kaysen D (2018). Predicting PTSD severity from experiences of trauma and heterosexism in lesbian and bisexual women: A longitudinal study of cognitive mediators. Journal of Counseling Psychology, 65(3), 324–333. 10.1037/cou0000287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dworkin ER, Jaffe AE, Fitzpatrick S, Rhew IC, & Kaysen D (2020). Daily relationships between posttraumatic stress symptoms, drinking motives, and alcohol consumption in trauma-exposed sexual minority women. Psychology of Addictive Behaviors, 35(1), 3–15. 10.1037/adb0000680 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dyar C, Feinstein BA, Eaton NR, & London B (2018). The mediating roles of rejection sensitivity and proximal stress in the association between discrimination and internalizing symptoms among sexual minority women. Archives of Sexual Behavior, 47(1), 205–218. 10.1007/s10508-016-0869-1 [DOI] [PubMed] [Google Scholar]
- Dyar C, & Kaysen D (2022). Multiple diverse drinking trajectories among sexual minority women: Unique and joint prediction by minority stress and social influence risk factors. Addictive Behaviors, 129, 107273. 10.1016/j.addbeh.2022.107273 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Egger M, Smith GD, Schneider M, & Minder C (1997). Bias in meta-analysis detected by a simple, graphical test. BMJ, 315(7109), 629–634. 10.1136/bmj.315.7109.629 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ehlke SJ, Kelley ML, Lewis RJ, & Braitman AL (2022). The role of alcohol demand on daily microaggressions and alcohol use among emerging adult bisexual+ women. Psychology of Addictive Behaviors, 36(2), 209–219. 10.1037/adb0000754 [DOI] [PubMed] [Google Scholar]
- Estrada F, Cerezo A, & Ramirez A (2021). An examination of posttraumatic stress disorder-related symptoms among a sample of Latinx sexual- and gender-minority immigrants. Journal of Traumatic Stress, 34(5), 967–976. 10.1002/jts.22714 [DOI] [PubMed] [Google Scholar]
- Evans-Polce RJ, & McCabe SE (2020). Alcohol, tobacco, and comorbid psychiatric disorders and associations with sexual identity and stress-related correlates. American Journal of Psychiatry, 177(11), 1073–1081. 10.1176/appi.ajp.2020.20010005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flanagan JC, Korte KJ, Killeen TK, & Back SE (2016). Concurrent treatment of substance use and PTSD. Current Psychiatry Reports, 18(8), 70. 10.1007/s11920-016-0709-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foa E, Hembree E, & Rothbaum BO (2007). Prolonged exposure therapy for PTSD: Emotional processing of traumatic experiences therapist guide Oxford University Press, USA. [Google Scholar]
- Goldstein RB, Smith SM, Chou SP, Saha TD, Jung J, Zhang H, Pickering RP, Ruan WJ, Huang B, & Grant BF (2016). The epidemiology of DSM-5 posttraumatic stress disorder in the United States: Results from the National Epidemiologic Survey on Alcohol and Related Conditions-III. Social Psychiatry and Psychiatric Epidemiology, 51(8), 1137–1148. 10.1007/s00127-016-1208-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonzalez E, Sperandio KR, Mullen PR, & Tuazon VE (2021). Development and initial testing of the multidimensional cultural humility scale. Measurement and Evaluation in Counseling and Development, 54(1), 56–70. 10.1080/07481756.2020.1745648 [DOI] [Google Scholar]
- Grant BF, Goldstein RB, Smith SM, Jung J, Zhang H, Chou SP, Pickering RP, Ruan WJ, Huang B, Saha TD, Aivadyan C, Greenstein E, & Hasin DS (2015). The Alcohol Use Disorder and Associated Disabilities Interview Schedule-5 (AUDADIS-5): Reliability of substance use and psychiatric disorder modules in a general population sample. Drug and Alcohol Dependence, 148, 27–33. 10.1016/j.drugalcdep.2014.11.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halberstam J (2012). Global female masculinities. Sexualities, 15(3–4), 336–354. 10.1177/1363460712436480 [DOI] [Google Scholar]
- Hall GCN, Ibaraki AY, Huang ER, Marti CN, & Stice E (2016). A meta-analysis of cultural adaptations of psychological interventions. Behavior Therapy, 47(6), 993–1014. 10.1016/j.beth.2016.09.005 [DOI] [PubMed] [Google Scholar]
- Hatzenbuehler ML, Slopen N, & McLaughlin KA (2014). Stressful life events, sexual orientation, and cardiometabolic risk among young adults in the United States. Health Psychology, 33(10), 1185–1194. 10.1037/hea0000126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawn SE, Bountress KE, Sheerin CM, Dick DM, & Amstadter AB (2020). Trauma-related drinking to cope: A novel approach to the self-medication model. Psychology of Addictive Behaviors, 34(3), 465–476. 10.1037/adb0000552 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawn SE, Cusack SE, & Amstadter AB (2020). A systematic review of the self-medication hypothesis in the context of posttraumatic stress disorder and comorbid problematic alcohol use. Journal of Traumatic Stress, 33(5), 699–708. 10.1002/jts.22521 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Helminen EC, Cascalheira CJ, Shaw TJ, Zollweg S, Hughes TL, & Scheer JR (2022). A latent class analysis of tailored substance use treatment programs: Implications for treating syndemic conditions facing sexual and gender minority populations. Drug and Alcohol Dependence, 238, 109550. 10.1016/j.drugalcdep.2022.109550 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Helminen E, Scheer JR, Jackson SD, Brisbin CD, Batchelder AW, Cascalheira C, & Sullivan TP (2021). PTSD symptoms and hazardous drinking indicators among trauma-exposed sexual minority women during heightened societal stress. Behavioral Medicine. Advance online publication 10.1080/08964289.2021.2006132 [DOI] [PMC free article] [PubMed]
- Hien DA, López-Castro T, Fitzpatrick S, Ruglass LM, Fertuck EA, & Melara R (2021). A unifying translational framework to advance treatment research for comorbid PTSD and substance use disorders. Neuroscience & Biobehavioral Reviews, 127, 779–794. 10.1016/j.neubiorev.2021.05.022 [DOI] [PubMed] [Google Scholar]
- Hook JN, Davis DE, Owen J, Worthington EL Jr., & Utsey SO (2013). Cultural humility: Measuring openness to culturally diverse clients. Journal of Counseling Psychology, 60, 353–366. 10.1037/a0032595 [DOI] [PubMed] [Google Scholar]
- Hughes TL, Veldhuis CB, Drabble LA, & Wilsnack SC (2020). Research on alcohol and other drug (AOD) use among sexual minority women: A global scoping review. PLOS ONE, 15(3), e0229869. 10.1371/journal.pone.0229869 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackson SD, Mohr JJ, & Kindahl AM (2021). Intersectional experiences: A mixed methods experience sampling approach to studying an elusive phenomenon. Journal of Counseling Psychology, 68(3), 299–315. 10.1037/cou0000537 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jhe GB, Mereish EH, Gordon AR, Woulfe JM, & Katz-Wise SL (2021). Associations between anti-bisexual minority stress and body esteem and emotional eating among bi+ individuals: The protective role of individual- and community-level factors. Eating Behaviors, 43, 101575. 10.1016/j.eatbeh.2021.101575 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones AL, Rafferty J, Cochran SD, Abelson J, Hanna MR, & Mays VM (2022). Prevalence, severity and burden of post-traumatic stress disorder in Black men and women across the adult life span. Journal of Aging and Health, 34(3), 401–412. 10.1177/08982643221086071 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Juster RP, de Torre MB, Kerr P, Kheloui S, Rossi M, & Bourdon O (2019). Sex differences and gender diversity in stress responses and allostatic load among workers and LGBT oeople. Current Psychiatry Reports, 21(11), 110. 10.1007/s11920-019-1104-2 [DOI] [PubMed] [Google Scholar]
- Karatzias T, & Cloitre M (2019). Treating adults with complex posttraumatic stress disorder using a modular approach to treatment: Rationale, evidence, and directions for future research. Journal of Traumatic Stress, 32(6), 870–876. 10.1002/jts.22457 [DOI] [PubMed] [Google Scholar]
- Kaysen D, Bedard-Gilligan M, & Stappenbeck CA (2017). PTSD and alcohol associations among trauma-exposed women: Critical questions for the field. Clinical Psychology, 24(1), 23–26. 10.1111/cpsp.12168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaysen D, Jaffe AE, Shoenberger B, Walton TO, Pierce AR, & Walker DD (2022). Does effectiveness of a brief substance use treatment depend on PTSD? An evaluation of motivational enhancement therapy for active-duty army personnel. Journal of Studies on Alcohol and Drugs, 83(6), 924–933. 10.15288/jsad.22-00011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelley ML, Ehlke SJ, Braitman AL, & Stamates AL (2018). Testing a model of binegativity, drinking-to-cope motives, alcohol use, and sexual coercion among self-identified bisexual women. Journal of Bisexuality, 18(4), 478–496. 10.1080/15299716.2018.1481482 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kerridge BT, Pickering RP, Saha TD, Ruan WJ, Chou SP, Zhang H, Jung J, & Hasin DS (2017). Prevalence, sociodemographic correlates and DSM-5 substance use disorders and other psychiatric disorders among sexual minorities in the United States. Drug and Alcohol Dependence, 170, 82–92. 10.1016/j.drugalcdep.2016.10.038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khantzian E (1985). The self-medication hypothesis of addictive disorders: Focus on heroin and cocaine dependence. The American Journal of Psychiatry, 142, 1259–1264. 10.1176/ajp.142.11.1259 [DOI] [PubMed] [Google Scholar]
- Krueger EA, & Upchurch DM (2019). Are sociodemographic, lifestyle, and psychosocial characteristics associated with sexual orientation group differences in mental health disparities? Results from a national population-based study. Social Psychiatry and Psychiatric Epidemiology, 54(6), 755–770. 10.1007/s00127-018-1649-0 [DOI] [PubMed] [Google Scholar]
- Leath S, Jones M, Jerald MC, & Perkins TR (2022). An investigation of Jezebel stereotype awareness, gendered racial identity and sexual beliefs and behaviours among Black adult women. Culture, Health & Sexuality, 24(4), 517–532. 10.1080/13691058.2020.1863471 [DOI] [PubMed] [Google Scholar]
- Lehavot K, Beckman KL, Chen JA, Simpson TL, & Williams EC (2019). Race/ethnicity and sexual orientation disparities in mental health, sexism, and social support among women veterans. Psychology of Sexual Orientation and Gender Diversity, 6(3), 347–358. 10.1037/sgd0000333 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lehavot K, Blosnich JR, Glass JE, & Williams EC (2017). Alcohol use and receipt of alcohol screening and brief intervention in a representative sample of sexual minority and heterosexual adults receiving health care. Drug and Alcohol Dependence, 179, 240–246. 10.1016/j.drugalcdep.2017.07.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lehavot K, Browne KC, & Simpson TL (2014). Examining sexual orientation disparities in alcohol misuse among women veterans. American Journal of Preventive Medicine, 47(5), 554–562. 10.1016/j.amepre.2014.07.002 [DOI] [PubMed] [Google Scholar]
- Lehavot K, Katon JG, Chen JA, Fortney JC, & Simpson TL (2018). Post-traumatic stress disorder by gender and veteran status. American Journal of Preventive Medicine, 54(1), e1–e9. 10.1016/j.amepre.2017.09.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lehavot K, Molina Y, & Simoni JM (2012). Childhood trauma, adult sexual assault, and adult gender expression among lesbian and bisexual women. Sex Roles, 67(5), 272–284. 10.1007/s11199-012-0171-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lehavot K, Stappenbeck CA, Luterek JA, Kaysen D, & Simpson TL (2014). Gender differences in relationships among PTSD severity, drinking motives, and alcohol use in a comorbid alcohol dependence and PTSD sample. Psychology of Addictive Behaviors, 28(1), 42–52. 10.1037/a0032266 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levitt HM, Puckett JA, Ippolito MR, & Horne SG (2012). Sexual minority women’s gender identity and expression: Challenges and supports. Journal of Lesbian Studies, 16(2), 153–176. 10.1080/10894160.2011.605009 [DOI] [PubMed] [Google Scholar]
- Lin L (2018). Bias caused by sampling error in meta-analysis with small sample sizes. PLOS ONE, 13(9), e0204056. 10.1371/journal.pone.0204056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lipsey MW, & Wilson DB (2001). Practical meta-analysis (pp. ix, 247). Sage Publications, Inc. [Google Scholar]
- Livingston NA, Berke D, Scholl J, Ruben M, & Shipherd JC (2020). Addressing diversity in PTSD treatment: Clinical considerations and guidance for the treatment of PTSD in LGBTQ populations. Current Treatment Options in Psychiatry, 7(2), 53–69. 10.1007/s40501-020-00204-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Livingston NA, Lynch KE, Hinds Z, Gatsby E, DuVall SL, & Shipherd JC (2022). Identifying posttraumatic stress disorder and disparity among transgender veterans using nationwide Veterans Health Administration electronic health record data. LGBT Health, 9(2), 94–102. 10.1089/lgbt.2021.0246 [DOI] [PubMed] [Google Scholar]
- López G, & Yeater EA (2021). Comparisons of sexual victimization experiences among sexual minority and heterosexual women. Journal of Interpersonal Violence, 36(7–8), 4250–4270. 10.1177/0886260518787202 [DOI] [PubMed] [Google Scholar]
- Lynch KE, Viernes B, Schliep KC, Gatsby E, Alba PR, DuVall SL, & Blosnich JR (2021). Variation in sexual prientation documentation in a national electronic health record system. LGBT Health, 8(3), 201–208. 10.1089/lgbt.2020.0333 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCabe SE, Hughes TL, West BT, Evans-Polce RJ, Veliz PT, Dickinson K, McCabe VV, & Boyd CJ (2020). Sexual orientation, adverse childhood experiences, and comorbid DSM-5 substance use and mental health disorders. The Journal of Clinical Psychiatry, 81(6), 19478. 10.4088/JCP.20m13291 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCabe SE, Hughes T, Beal S, Evans-Polce R, Kcomt L, Engstrom C, West B, Veliz P, Leary K, McCabe V, & Boyd C (2022). Sexual orientation differences in childhood sexual abuse, suicide attempts, and DSM-5 alcohol, tobacco, other drug use, and mental health disorders in the US. Child Abuse & Neglect, 123, 10.1016/j.chiabu.2021.105377 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mereish EH, Katz-Wise SL, & Woulfe J (2017). Bisexual-specific minority stressors, psychological distress, and suicidality in bisexual individuals: The mediating role of loneliness. Prevention Science, 18(6), 716–725. 10.1007/s11121-017-0804-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer I (2003). Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: Conceptual issues and research evidence. Psychological Bulletin, 129(5), 674–697. 10.1037/0033-2909.129.5.674 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morgan-López AA, Killeen TK, Saavedra LM, Hien DA, Fitzpatrick S, Ruglass LM, & Back SE (2020). Crossover between diagnostic and empirical categorizations of full and subthreshold PTSD. Journal of Affective Disorders, 274, 832–840. 10.1016/j.jad.2020.05.031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Institutes of Health Sexual and Gender Minority Research Coordinating Committee. (2015). NIH FY 2016–2020 strategic plan to advance research on the health and well-being of sexual and gender minorities http://edi.nih.gov/sites/default/files/EDI_Public_files/sgm-strategic-plan.pdf
- Neria Y (2021). Functional neuroimaging in PTSD: From discovery of underlying mechanisms to addressing diagnostic heterogeneity. American Journal of Psychiatry, 178(2), 128–135. 10.1176/appi.ajp.2020.20121727 [DOI] [PubMed] [Google Scholar]
- National Heart, Lung, and Blood Institute. (2014). Quality assessment tool for observational cohort and cross-sectional studies Accessed September 5, 2022. https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools
- Olff M, Langeland W, Draijer N, & Gersons BPR (2007). Gender differences in posttraumatic stress disorder. Psychological Bulletin, 133(2), 183–204. 10.1037/0033-2909.133.2.183 [DOI] [PubMed] [Google Scholar]
- Ovrebo E, Brown EL, Emery HE, Stenersen M, Schimmel-Bristow A, & Steinruck RE (2018). Bisexual invisibility in trauma: PTSD symptomology, and mental healthcare experiences among bisexual women and men versus lesbians and gay men. Journal of Bisexuality, 18(2), 168–185. 10.1080/15299716.2018.1458682 [DOI] [Google Scholar]
- Pachankis JE, Clark KA, Jackson SD, Pereira K, & Levine D (2021). Current capacity and future implementation of mental health services in U.S. LGBTQ community centers. Psychiatric Services, 72(6), 669–676. 10.1176/appi.ps.202000575 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pachankis JE, Hatzenbuehler ML, Wang K, Burton CL, Crawford FW, Phelan JC, & Link BG (2017). The burden of stigma on health and well-being: A taxonomy of concealment, course, disruptiveness, aesthetics, origin, and peril across 93 stigmas: Personality and Social Psychology Bulletin, 44(4), 451–474. 10.1177/0146167217741313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pachankis JE, Mahon CP, Jackson SD, Fetzner BK, & Bränström R (2020). Sexual orientation concealment and mental health: A conceptual and meta-analytic review. Psychological Bulletin, 146(10), 831–871. 10.1037/bul0000271 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pachankis JE, Soulliard ZA, Morris F, & Seager van Dyk I (2022). A model for adapting evidence-based interventions to be LGBQ-affirmative: Putting minority stress principles and case conceptualization into clinical research and practice. Cognitive and Behavioral Practice Advance online publication. 10.1016/j.cbpra.2021.11.005 [DOI]
- Page KV, Cerezo A, & Ross A (2021). Creating space for ourselves: Black sexual minority women and gender diverse individuals countering anti-Black racism and heterosexism. Psychology of Sexual Orientation and Gender Diversity, 9(2), 131–140. 10.1037/sgd0000470 [DOI] [Google Scholar]
- Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, Chou R, Glanville J, Grimshaw JM, Hróbjartsson A, Lalu MM, Li T, Loder EW, Mayo-Wilson E, McDonald S, … Moher D (2021). The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Systematic Reviews, 10(1), 89. 10.1186/s13643-021-01626-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palmisano AN, Norman SB, Panza KE, Petrakis IL, & Pietrzak RH (2022). PTSD symptom heterogeneity and alcohol-related outcomes in U.S. military veterans: Indirect associations with coping strategies. Journal of Anxiety Disorders, 85, 102496. 10.1016/j.janxdis.2021.102496 [DOI] [PubMed] [Google Scholar]
- Patel H, O’Connor C, Andrews K, Amlung M, Lanius R, & McKinnon MC (2022). Dissociative symptomatology mediates the relation between posttraumatic stress disorder severity and alcohol-related problems. Alcoholism: Clinical and Experimental Research, 46(2), 289–299. 10.1111/acer.14764 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pérez-Stable EJ (2016). Sexual and gender minorities formally designated as a health disparity population for research purposes NIMHD. https://www.nimhd.nih.gov/about/directors-corner/messages/message_10-06-16.html [Google Scholar]
- Persson A, Back SE, Killeen TK, Brady KT, Schwandt ML, Heilig M, & Magnusson Å (2017). Concurrent treatment of PTSD and substance use disorders using prolonged exposure (COPE): A pilot study in alcohol-dependent women. Journal of Addiction Medicine, 11(2), 119–125. 10.1097/ADM.0000000000000286 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pharr JR, Kachen A, & Cross C (2019). Health disparities among sexual gender minority women in the United States: A population-based study. Journal of Community Health: The Publication for Health Promotion and Disease Prevention, 44(4), 721–728. 10.1007/s10900-019-00631-y [DOI] [PubMed] [Google Scholar]
- Pittman DM, Riedy Rush C, Hurley KB, & Minges ML (2022). Double jeopardy: Intimate partner violence vulnerability among emerging adult women through lenses of race and sexual orientation. Journal of American College Health, 70(1), 265–273. 10.1080/07448481.2020.1740710 [DOI] [PubMed] [Google Scholar]
- Porsch LM, Xu M, Veldhuis CB, Bochicchio LA, Zollweg SS, & Hughes TL (2022). Intimate partner violence among sexual minority women: A scoping review. Trauma, Violence, & Abuse, Advanced online publication. 10.1177/15248380221122815 [DOI] [PMC free article] [PubMed]
- Possemato K, Maisto SA, Wade M, Barrie K, McKenzie S, Lantinga LJ, & Ouimette P (2015). Ecological momentary assessment of PTSD symptoms and alcohol use in combat veterans. Psychology of Addictive Behaviors, 29(4), 894–905. 10.1037/adb0000129 [DOI] [PubMed] [Google Scholar]
- Puckett J, Maroney M, Levitt H, & Horne S (2016). Relations between gender expression, minority stress, and mental health in cisgender sexual minority women and men. Psychology of Sexual Orientation and Gender Diversity, 3(4), 489–498. 10.1037/sgd0000201 [DOI] [Google Scholar]
- Ralevski E, Olivera-Figueroa LA, & Petrakis I (2014). PTSD and comorbid AUD: A review of pharmacological and alternative treatment options. Substance Abuse and Rehabilitation, 5, 25–36. 10.2147/SAR.S37399 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ressler KJ (2018). Alpha-Adrenergic receptors in PTSD: Failure or time for precision medicine? The New England Journal of Medicine, 378(6), 575–576. 10.1056/NEJMe1716724 [DOI] [PubMed] [Google Scholar]
- Roberts AL, Austin SB, Corliss HL, Vandermorris AK, & Koenen KC (2010). Pervasive trauma exposure among US sexual orientation minority adults and risk of posttraumatic stress disorder. American Journal of Public Health, 100(12), 2433–2441. 10.2105/AJPH.2009.168971 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts NP, Roberts PA, Jones N, & Bisson JI (2015). Psychological interventions for post-traumatic stress disorder and comorbid substance use disorder: A systematic review and meta-analysis. Clinical Psychology Review, 38, 25–38. 10.1016/j.cpr.2015.02.007 [DOI] [PubMed] [Google Scholar]
- Ruglass LM, Lopez-Castro T, Papini S, Killeen T, Back SE, & Hien DA (2017). Concurrent treatment with prolonged exposure for co-occurring full or subthreshold posttraumatic stress disorder and substance use disorders: A randomized clinical trial. Psychotherapy and Psychosomatics, 86(3), 150–161. 10.1159/000462977 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruglass LM, Morgan-López AA, Saavedra LM, Hien DA, Fitzpatrick S, Killeen TK, Back SE, & López-Castro T (2020). Measurement nonequivalence of the clinician-administered PTSD Scale by race/ethnicity: Implications for quantifying posttraumatic stress disorder severity. Psychological Assessment, 32(11), 1015–1027. 10.1037/pas0000943 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salim SR, McConnell AA, & Messman T (2022). Sexual victimization outcomes and adjustment among bisexual women: A review of the quantitative literature. Trauma, Violence, & Abuse Advance online publication. 10.1177/15248380211073837 [DOI] [PubMed]
- Sarno EL, Swann G, Newcomb ME, & Whitton SW (2021). Intersectional minority stress and identity conflict among sexual and gender minority people of color assigned female at birth. Cultural Diversity & Ethnic Minority Psychology, 27(3), 408–417. 10.1037/cdp0000412 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scheer JR, Batchelder AW, Bochicchio LA, Kidd JD, & Hughes TL (2022). Alcohol use, behavioral and mental health help-seeking, and treatment satisfaction among sexual minority women. Alcoholism, Clinical and Experimental Research, 46(4), 641–656. 10.1111/acer.14789 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scheer JR, Batchelder AW, Wang K, & Pachankis JE (2021). Mental health, alcohol use, and substance use correlates of sexism in a sample of gender-diverse sexual minority women. Psychology of Sexual Orientation and Gender Diversity, 9(2), 222–235. 10.1037/sgd0000477 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scheer JR, Clark KA, McConocha E, Wang K, & Pachankis JE (2022). Toward cognitive-behavioral therapy for sexual minority women: Voices from stakeholders and community members. Cognitive and Behavioral Practice Advance online publication. 10.1016/j.cbpra.2022.02.019 [DOI] [PMC free article] [PubMed]
- Schein J, Houle C, Urganus A, Cloutier M, Patterson-Lomba O, Wang Y, King S, Levinson W, Guérin A, Lefebvre P, & Davis LL (2021). Prevalence of post-traumatic stress disorder in the United States: A systematic literature review. Current Medical Research and Opinion, 37(12), 2151–2161. 10.1080/03007995.2021.1978417 [DOI] [PubMed] [Google Scholar]
- Schuler MS, Dick AW, & Stein BD (2019). Sexual minority disparities in opioid misuse, perceived heroin risk and heroin access among a national sample of US adults. Drug and Alcohol Dependence, 201, 78–84. 10.1016/j.drugalcdep.2019.04.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sigurvinsdottir R, & Ullman SE (2016). Sexual orientation, race, and trauma as predictors of sexual assault recovery. Journal of Family Violence, 31(7), 913–921. 10.1007/s10896-015-9793-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sigurvinsdottir R, & Ulman SE (2015). The role of sexual orientation in the victimization and recovery of sexual assault survivors. Violence and Victims, 30(4), 636–648. 10.1891/0886-6708.VV-D-13-00066 [DOI] [PubMed] [Google Scholar]
- Simpson TL, Rise P, Browne KC, Lehavot K, & Kaysen D (2019). Clinical presentations, social functioning, and treatment receipt among individuals with comorbid life-time PTSD and alcohol use disorders versus drug use disorders: Findings from NESARC-III. Addiction, 114(6), 983–993. 10.1111/add.14565 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith NDL, & Cottler LB (2018). The epidemiology of post-traumatic stress disorder and alcohol use disorder. Alcohol Research: Current Reviews, 39(2), 113–120. [PMC free article] [PubMed] [Google Scholar]
- Steel Z, Chey T, Silove D, Marnane C, Bryant RA, & van Ommeren M (2009). Association of torture and other potentially traumatic events with mental health outcomes among populations exposed to mass conflict and displacement: A systematic review and meta-analysis. JAMA, 302(5), 537–549. 10.1001/jama.2009.1132 [DOI] [PubMed] [Google Scholar]
- Steele CM, & Josephs RA (1990). Alcohol myopia: Its prized and dangerous effects. American Psychologist, 45(8), 921–933. 10.1037/0003-066X.45.8.921 [DOI] [PubMed] [Google Scholar]
- Straus E, Worley MJ, Lyons R, Kline AC, Tripp JC, Davis BC, Haller M, Angkaw AC, Trim RS, & Norman SB (2022). Examining attendance patterns across integrated therapies for posttraumatic stress disorder and alcohol use disorder. Journal of Anxiety Disorders, 85, 102498. 10.1016/j.janxdis.2021.102498 [DOI] [PubMed] [Google Scholar]
- Sullivan TP, Armeli S, Tennen H, Weiss NH, & Hansen NB (2020). Fluctuations in daily PTSD symptoms are related to proximal alcohol use: A micro-longitudinal study of women victims of intimate partner violence. The American Journal of Drug and Alcohol Abuse, 46(1), 98–108. 10.1080/00952990.2019.1624765 [DOI] [PubMed] [Google Scholar]
- Sullivan TP, Weiss NH, Flanagan JC, Willie TC, Armeli S, & Tennen H (2016). PTSD and daily co-occurrence of drug and alcohol use among women experiencing intimate partner violence. Journal of Dual Diagnosis, 12(1), 36–42. 10.1080/15504263.2016.1146516 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Veldhuis CB, Juster R-P, Corbeil T, Wall M, Poteat T, & Hughes TL (2022). Testing whether the combination of victimization and minority stressors exacerbate PTSD risks in a diverse community sample of sexual minority women. Psychology & Sexuality Advance online publication. 10.1080/19419899.2022.2106147 [DOI] [PMC free article] [PubMed]
- Viechtbauer W (2010). Conducting meta-analyses in R with the metafor package. Journal of Statistical Software, 36(03), 1–48. [Google Scholar]
- Williams ND, & Fish JN (2020). The availability of LGBT-specific mental health and substance abuse treatment in the United States. Health Services Research, 55(6), 932–943. 10.1111/1475-6773.13559 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wisco BE, Miller MW, Wolf EJ, Kilpatrick D, Resnick HS, Badour CL, Marx BP, Keane TM, Rosen RC, & Friedman MJ (2016). The impact of proposed changes to ICD-11 on estimates of PTSD prevalence and comorbidity. Psychiatry Research, 240, 226–233. 10.1016/j.psychres.2016.04.043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wisco BE, Nomamiukor FO, Marx BP, Krystal JH, Southwick SM, & Pietrzak RH (2022). Posttraumatic stress disorder in US military veterans: Results from the 2019–2020 National Health and Resilience in veterans study. The Journal of Clinical Psychiatry, 83(2), 39779. 10.4088/JCP.20m14029 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


