Abstract
Background
There is a dearth of high-quality evidence from digital health interventions in routine program settings in low- and middle-income countries. We previously conducted a randomized controlled trial (RCT) in Zimbabwe, demonstrating that 2-way texting (2wT) was safe and effective for follow-up after adult voluntary medical male circumcision (VMMC).
Objective
To demonstrate the replicability of 2wT, we conducted a larger RCT in both urban and rural VMMC settings in South Africa to determine whether 2wT improves adverse event (AE) ascertainment and, therefore, the quality of follow-up after VMMC while reducing health care workers’ workload.
Methods
A prospective, unblinded, noninferiority RCT was conducted among adult participants who underwent VMMC with cell phones randomized in a 1:1 ratio between 2wT and control (routine care) in North West and Gauteng provinces. The 2wT participants responded to a daily SMS text message with in-person follow-up only if desired or an AE was suspected. The control group was requested to make in-person visits on postoperative days 2 and 7 as per national VMMC guidelines. All participants were asked to return on postoperative day 14 for study-specific review. Safety (cumulative AEs ≤day 14 visit) and workload (number of in-person follow-up visits) were compared. Differences in cumulative AEs were calculated between groups. Noninferiority was prespecified with a margin of −0.25%. The Manning score method was used to calculate 95% CIs.
Results
The study was conducted between June 7, 2021, and February 21, 2022. In total, 1084 men were enrolled (2wT: n=547, 50.5%, control: n=537, 49.5%), with near-equal proportions of rural and urban participants. Cumulative AEs were identified in 2.3% (95% CI 1.3-4.1) of 2wT participants and 1.0% (95% CI 0.4-2.3) of control participants, demonstrating noninferiority (1-sided 95% CI −0.09 to ∞). Among the 2wT participants, 11 AEs (9 moderate and 2 severe) were identified, compared with 5 AEs (all moderate) among the control participants—a nonsignificant difference in AE rates (P=.13). The 2wT participants attended 0.22 visits, and the control participants attended 1.34 visits—a significant reduction in follow-up visit workload (P<.001). The 2wT approach reduced unnecessary postoperative visits by 84.8%. Daily response rates ranged from 86% on day 3 to 74% on day 13. Among the 2wT participants, 94% (514/547) responded to ≥1 daily SMS text messages over 13 days.
Conclusions
Across rural and urban contexts in South Africa, 2wT was noninferior to routine in-person visits for AE ascertainment, demonstrating 2wT safety. The 2wT approach also significantly reduced the follow-up visit workload, improving efficiency. These results strongly suggest that 2wT provides quality VMMC follow-up and should be adopted at scale. Adaptation of the 2wT telehealth approach to other acute follow-up care contexts could extend these gains beyond VMMC.
Trial Registration
ClinicalTrials.gov NCT04327271; https://www.clinicaltrials.gov/ct2/show/NCT04327271
Keywords: SMS text messaging–based telehealth, 2-way texting, voluntary medical male circumcision, South Africa, mobile health, mHealth for quality improvement, digital health innovation in low- and middle-income countries, male engagement in care, COVID-19, mobile phone
Introduction
Background
In sub-Saharan Africa (SSA), direct provider-to-client communication approaches, including 2-way texting (2wT) and telehealth, are being deployed in HIV prevention, treatment, and care services with promising results, to improve patient engagement in care, including adherence [1-6]. However, not all interventions are effective in all populations at all times [7]. Rapid responses to COVID-19 accelerated telehealth innovation in SSA to maintain critical service delivery while reducing the spread of the infection [8-12]. However, despite consistent growth in the digital health arena and available tools to guide the assessment of mobile health (mHealth) interventions [13-15], rigorous evidence of mHealth success cannot keep pace with the speed of, and demand for, innovation. A gap remains in high-quality evidence on successful mHealth approaches in routine program settings in SSA [16-18]. A greater understanding of where, when, how, and for whom a digital intervention works is needed to address critical equity issues in mHealth access [19,20] and inform mHealth impact at scale [21-24]. This is particularly important for males who may find using digital health more appealing than engaging in traditional care [25, 26]. With the global progress toward ending AIDS by 2030 threatened [27], additional effort is needed to improve the identification and replication of effective digital health interventions that increase access to critical HIV prevention, treatment, and care services.
Since 2007, voluntary medical male circumcision (VMMC) has been recognized by the Joint United Nations Programme on HIV/AIDS and World Health Organization (WHO) as a critical component of combination HIV prevention, reaching almost 30 million males in SSA by 2022 [28]. To cement the progress in HIV prevention, robust political and financial support from Ministries of Health and donor agencies, including the US President’s Emergency Plan for AIDS Relief (PEPFAR), continues to push for VMMC, with the goal of reaching 80% of eligible males in SSA [27,29-34]. VMMC programs follow global guidelines on service delivery to ensure the delivery of quality VMMC care [35]. Routine VMMC monitoring and evaluation indicators encourage the early diagnosis of adverse events (AEs) and ensure quality data for decision-making. In addition to a number of VMMC procedures, core monitoring and evaluation indicators measure the quality of care, including the number of clients with ≥1 postoperative follow-up visits within 14 days and the number of AEs by severity (moderate or severe) [3,33,36]. Over a decade of data show that VMMC is safe: across large-volume VMMC programs in SSA, the mean combined moderate and severe AE rate is below 2% [37-47], the commonly accepted threshold for safety [48]. Adherence to recommended in-person postoperative reviews by a clinician remains a PEPFAR priority [3,49]. However, with low AE rates, making postoperative reviews a requirement for all males may deter VMMC uptake and waste time for both providers and patients [50]. Moreover, the reported follow-up rates may be overestimated, and men with potential AEs may still be missed [51].
Requiring postoperative visits for all males when the risk of AEs is low suggests program inefficiencies at scale, making VMMC an excellent candidate for digital health innovation. Therefore, in 2019, the International Training and Education Center for Health at the University of Washington conducted a randomized controlled trial (RCT) in Harare, Zimbabwe, to test 2-way texting (2wT)–based telehealth for postoperative follow-up after VMMC [52]. The 2wT approach allowed males healing without complication to opt out of routine postoperative visits while engaging males with concerns in 2-way SMS text messaging with a VMMC nurse who referred them to in-person visits when needed or desired. The 2wT approach maintained patient safety by focusing on those with potential AEs while reducing unnecessary postoperative visits by 85% [50]. The 2wT approach saved US $2.0 per patient [53] and was highly acceptable to both patients and providers [54]. Results from the adaptation and scale-up of the 2wT approach in Zimbabwe from RCT to routine VMMC service delivery show similar safety and efficiency advantages, supporting its continued expansion for males aged ≥15 years [55]. An important implementation science research question is as follows: Could 2wT be replicated and scaled in different routine program settings?
In South Africa, with support from the PEPFAR, approximately 500,000 VMMCs are conducted annually as part of the National Department of Health (NDoH) HIV prevention efforts [31,56]. At this level of productivity and with low AE rates [44], >400,000 unnecessary VMMC reviews may be conducted annually. Urban sites are overwhelmed by high VMMC and review volumes, especially during seasonal high-demand periods. In rural sites, where 90% of VMMCs occur, follow-up requires multiple, sometimes multi-hour trips, eroding health care worker (HCW) productivity. The reported AE rates in South Africa are low, but AE underreporting is also common, reducing the quality of VMMC services and compromising patient care [57]. South Africa’s ambitious VMMC goals and health system constraints, combined with good cell phone coverage and existing mHealth efforts [58-60], converge to suggest that 2wT’s impact would be substantial. Greater efficiency could compensate for VMMC losses owing to the COVID-19 pandemic, reduce unnecessary costs, and maintain the quality of services.
Rationale of This Study
To amplify and strengthen previous 2wT findings via adaptation and replication in a new country and new context, the International Training and Education Center for Health, Aurum Institute, Centre for HIV-AIDS Prevention Studies (CHAPS), and technology partner Medic conducted a 2wT RCT in routine VMMC settings in both urban and rural areas in South Africa. In this primary analysis, our objective was to determine whether 2wT improved the ascertainment of AEs and, therefore, the quality of post-VMMC follow-up while reducing HCWs’ workload. We conducted an unblinded, noninferiority RCT comparing two markers of VMMC quality: (1) moderate or severe AE rate ≤day 14 after VMMC and (2) the mean number of in-person postoperative follow-ups in the control and intervention arms. We hypothesized that 2wT would reduce the follow-up visit workload and improve AE ascertainment, reaffirming the evidence that 2wT-based VMMC follow-up is both safe and efficient. If confirmed, this additional evidence for 2wT’s advantages would support efforts to scale 2wT for VMMC follow-up in South Africa and beyond while also supporting the possibility of using 2wT-based telehealth for other acute or postoperative follow-up in routine low- and middle-income country settings.
Methods
Technology Overview
Digital Tool Design and Development
The 2wT approach is SMS text messaging–based conversational messaging between HCWs and clients. For this study, we adapted the Zimbabwe 2wT digital app that was built on the Community Health Toolkit (CHT) [61], an open-source global public good [62] that is highly secure, highly configurable, runs offline, supports use in multiple languages, and has >40,000 users across 16 countries [63-66]. Medic, a nonprofit organization, is the technical steward of the CHT. The 2wT app can be accessed on desktop computers, tablets, and mobile devices with or without an internet connection [50,55]. The CHT offers advantages in portability via local hosting and the ability to engage across multiple community health system hierarchies (districts, facilities, supervisors, HCWs, and patients). The CHT allows integration with health information systems (District Health Information Software 2) and facility-based electronic medical record systems such as OpenMRS. Engagement with the wider digital health literature and community is core to 2wT’s design, implementation, scale-up, and replication in other settings. The 2wT app aligns with the client-, provider-, manager-, and data-focused components of the WHO Classification of Digital Health Interventions [67].
We conducted Zoom (Zoom Video Communications)-based and in-person user acceptance testing and feedback sessions with patients and providers from routine VMMC program settings. The People, Messages, and Reports tabs (Figures 1-3) were updated through an iterative human-centered design process [68,69] that solicited user feedback from HCWs, nurses, and managers from all study sites to reflect local preferences and priorities, in accordance with the Principles of Digital Development [70]. SMS text message timing and content in English, isiZulu, and Setswana were pretested, modified, and optimized with clients, whereas similar feedback cycles with HCWs informed improvements for naming tasks and 2wT-based documentation. In March 2021, feedback from a small pilot with 50 males enrolled in texting further improved language clarity, smoothed patient referrals, and simplified 2wT reporting to reduce data duplication between the study and routine reporting forms. The pilot feedback also showed that clients often had 2 primary phone numbers. Improvements made before the launch of the study allowed clients to register for 2wT with multiple phone numbers from dual SIM cards or across multiple mobile networks, improving the data quality and continuity of client follow-up.
Figure 1.
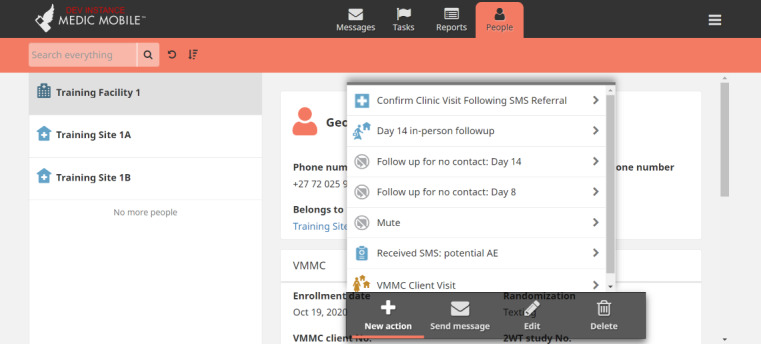
Community Health Toolkit People tab (CC BY 4.0 [55]). AE: adverse event; VMMC: voluntary medical male circumcision.
Figure 3.
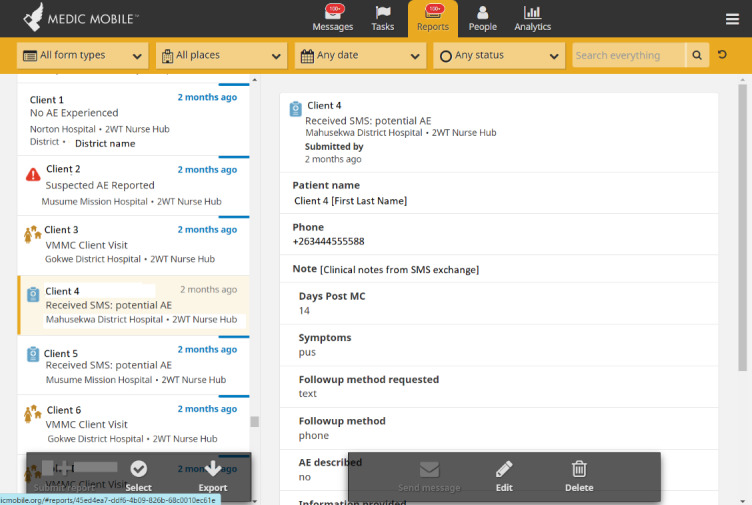
Community Health Toolkit Reports tab (CC BY 4.0 [55]). 2wT: 2-way texting; AE: adverse event; MC: male circumcision; VMMC: voluntary medical male circumcision.
Figure 2.
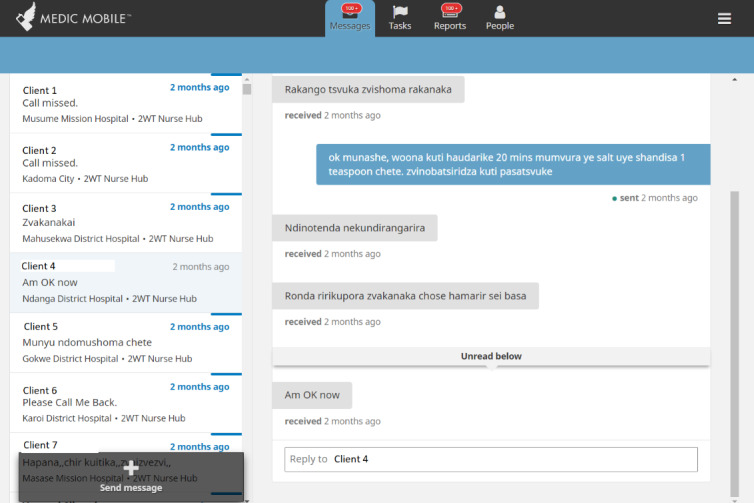
Community Health Toolkit Messages tab (CC BY 4.0 [55]).
2wT System Architecture
For this study, we enrolled 2wT clients directly in the VMMC app (running on the CHT) and stored and managed data using CouchDB and a PostgreSQL database system (Figure 4). We sent the clients SMS text messages via RapidPro [71], an open-source software developed by the United Nations International Children's Emergency Fund (UNICEF), to create more streamlined 2-way messaging flows and benefit from default integrations with a wide range of messaging platforms. An SMS text message aggregator service and a short code (Africa’s Talking) channel linked to RapidPro streamlined the incoming and outgoing 2wT SMS text messages.
Figure 4.
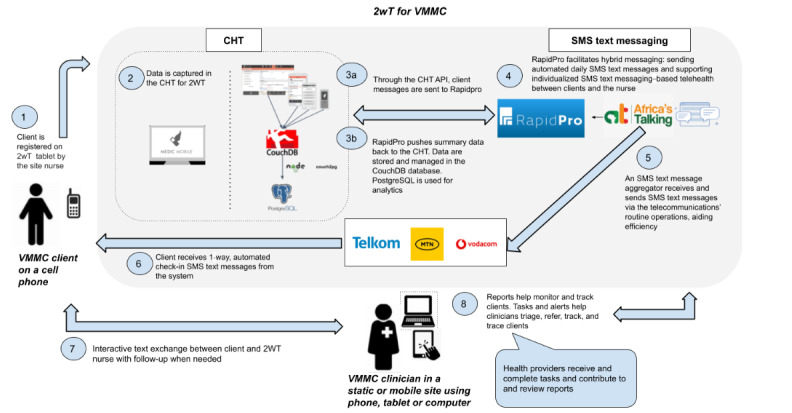
System architecture of 2-way texting (2wT) for voluntary medical male circumcision (VMMC) postoperative care. API: application programming interface; CHT: Community Health Toolkit.
Study Design
We conducted a 2-arm, prospective, unblinded, noninferiority RCT in 3 urban VMMC facilities in the Ekurhuleni district (Gauteng province) and 4 rural VMMC outreach sites in the Bojanala district (North West province) in South Africa. We purposively selected high–VMMC volume sites in urban and rural locations within 1 day of travel from the Aurum headquarters to ease supervision, represent different service delivery models, and consider limited study resources. The unit of randomization was individuals receiving VMMC. The participants were randomized in a 1:1 ratio and divided equally into urban and rural participants. Across all settings, we compared 2 groups of adult participants with cell phones: (1) participants who received routine care via in-person follow-up visits on days 2 and 7 (control) and (2) participants who received and responded to a daily SMS text message (2wT). The 2wT group had in-person follow-up only if desired or if an AE was suspected.
Eligibility
Men were eligible for enrollment if they (1) were aged ≥18 years, (2) possessed a cell phone at the time of enrollment, (3) provided contact information (phone, address, and next of kin), (4) had surgical VMMC, (5) had no intraoperative AE on the day of enrollment, (6) were willing to follow NDoH VMMC protocols, (7) were willing to come to the clinic on day 14 after VMMC, (8) were willing to respond to a questionnaire administered via SMS text message 21 days after circumcision, (9) provided written informed consent, and (10) received a text confirming study enrollment.
Recruitment
Urban recruitment occurred in the Gauteng province at 3 static VMMC sites in the Ekurhuleni district (Tembisa, Tsakane, and Katlehong North), each with its own VMMC team. Rural recruitment was conducted in the Bojanala district across outreach sites served by one VMMC team (Mogwase, Bafokeng, Bapong, and Letlhabile). All sites operated under routine VMMC service delivery provided by CHAPS and adhered to the NDoH VMMC guidance [36]. On the day of their VMMC, the participants were recruited; informed about the study on 2wT-based follow-up; and, if eligible and willing to participate, underwent informed consent by the study team at each site.
Enrollment
All consented men were registered in a custom 2wT software app built using an open-source CHT. Consented men who did not receive text confirming study enrollment were immediately withdrawn from the study and resumed routine VMMC follow-up. Enrollment data included the name, phone number, and alternative phone number of the participants. Men were also asked to provide information on their wage (daily, weekly, monthly, or none) as well as the costs to come to the facility (food and transportation) for future consideration of patient VMMC costs.
Randomization
A total of 1160 opaque security envelopes (580 intervention and 580 control) were used to randomize participants in a 1:1 ratio by following a randomized block design in groups of 10. Blocks were distributed equally between the urban and rural sites. This block design reduced variability within treatment conditions and potential confounding, allowing for interim analysis with near equal–size groups and more certain randomization within sites. The site coordinators were unaware of the envelope’s contents until the participant opened and revealed the group assignment to the coordinator. Randomization affected participant intervention only after routine VMMC surgical procedure and recovery. The study design required that the participants and clinic staff be aware of the allocation after the assignment.
2wT Training
The RCT study team, both researchers and implementation teams, was trained on 2wT through a 3-day hands-on 2wT study training session and an additional week of on-site support during the study launch at each site. For approximately 1 month, the 2wT system was reviewed daily by the central study team, providing brief feedback to the site teams via WhatsApp (Meta Platforms Inc) on areas for improvement. Throughout the RCT, the study team provided follow-up coaching and mentoring to the site teams via email, WhatsApp, and phone calls. The 2wT daily task sheets and quick guides provided reminders, whereas quarterly in-person refresher training ensured adherence to the 2wT study protocol. The study team provided additional support to the VMMC teams via weekly study calls, identifying problems and collaboratively resolving concerns with the 2wT system or VMMC program implementation. The study team visited the sites weekly for the first 3 months and monthly thereafter for quality improvement.
Interventions
Overview
Most 2wT intervention activities in both routine and 2wT arms were maintained from the previous study [52]. Table 1 lists the major South African study activities by arm.
Table 1.
Interventions for the 2-way texting (2wT) and routine arms.
| Specific activities | Control | 2wT | |
| Day 0 (day of VMMCa) | |||
|
|
Routine VMMC eligibility, consent, preoperative counseling, surgery, and completion of the NDoHb client intake forms | ✓ | ✓ |
|
|
Study-specific consent | ✓ | ✓ |
|
|
Routine postoperative care, including wound care instructions, bandage removal guidance, and AEc identification counseling | ✓ | ✓ |
|
|
Additional postoperative education on using the 2wT system, including review of labeled photos of potential AEs named in the daily SMS text message |
|
✓ |
| Scheduled in-person follow-up | |||
|
|
Routinely scheduled day 2 and day 7 visits | ✓ |
|
|
|
Study-specific day 14 visit (US $7 provided as phone credit) | ✓ | ✓ |
|
|
Active client follow-up for missed visits | Day 2 only | Day 14 onlyd |
| 2wT-specific processes | |||
|
|
Daily texts on days 1 to 13 |
|
✓ |
|
|
Phone tracing if there is no SMS text message response by day 8 |
|
✓ |
| NDoH routine AE procedures | |||
|
|
In-person review for AE concerns on any day | ✓ | ✓ |
|
|
Emergency VMMC after-hours care | ✓ | ✓ |
|
|
AE identification, grading, management, and treatment | ✓ | ✓ |
|
|
AE reporting on routine NDoH forms | ✓ | ✓ |
aVMMC: voluntary medical male circumcision.
bNDoH: National Department of Health.
cAE: adverse event.
dDay 14 active tracing for 2wT participants with whom there was no SMS text message, phone, or in-person contact from the day of VMMC.
Routine VMMC Care (Control Arm)
All VMMC care, from the assessment of AEs through complete healing, is provided free of charge by CHAPS in NDoH facilities. CHAPS follows all NDoH protocols based on the WHO guidelines and recommendations [29,36]. In the rural sites, according to standard operating procedures, 1 dedicated CHAPS VMMC team scheduled day 2 and day 7 postsurgery visits in response to either provider or patient considerations, either (1) meeting at a central, convenient location for the patient; (2) by sending a car to the patient’s home; or (3) by sending a driver to transport the patient to a central clinic location to meet the CHAPS VMMC team. In the urban settings, most patients independently returned for scheduled day 2 and day 7 visits, with only a few clients requiring transport support or home visits. In any setting, the patients could seek care outside scheduled visits at any Department of Health or private facility upon suspicion of AEs, but most patients returned to their VMMC site or contacted the CHAPS VMMC team for home visits. Sites used the standardized PEPFAR approach to identify, assess, and record the timing, type, and severity of AEs [48]. The COVID-19 pandemic disrupted VMMC service delivery several times over the course of the study, with travel restrictions and other infection prevention efforts resulting in a complete or partial reduction in scheduled follow-up visits, especially in rural areas. In both the urban and rural settings, the patients who missed the day 2 postsurgery visit were traced via phone call; if the patients missed both day 2 and day 7 visits and were not reachable by phone, up to 3 home visits were attempted to review the clients, when feasible.
2wT Procedures (Intervention Arm)
On day 0 (day of VMMC), a 2wT study team member registered all the intervention participants in the app. The 2wT arm participants received up to 10 minutes of enhanced postoperative counseling using the 2wT flip-book on how to respond to the daily SMS text message and reviewed photos that illustrated the terms in the daily SMS text message: “How are you? Are you experiencing any bleeding, swelling, pus, pain, redness or wound opening? Enter 1=Yes, 0=No and press send.” The 2wT participants received the automated daily SMS text message on days 1 to 13 in 1 of 3 predominant languages of the area, English, Setswana, or isiZulu. The participants could respond via an SMS text message in any language. The clients were expected to respond to the daily SMS text message with a single numeric (0 or 1) response; they could respond to any daily SMS text message at any time. They could also initiate an unrestricted, freely-worded text response at any time, instead of or in addition to the daily numeric response. A free text response was any text-based SMS text message interaction with the VMMC nurse (eg, “Can I come to the clinic?” “I need some help” or “I’m in pain”). The 2wT nurse took no action for the participants who reported no concerns in their response to the daily SMS text message (0=no concerns). However, if a 2wT participant responded to any daily SMS text message with suspicion of a complication (1=yes concerns) or sent a free text reporting an issue, the 2wT VMMC nurse first interacted with the participant via SMS text message, providing education and reassurance. For participants with a potential AE or with need for further reassurance, the nurse triaged the participants, asking them to return to the clinic for a review (urban) or sending a clinical team to review the participants (rural) the following day or earlier if an emergency was suspected. The clients could request a call back to speak with the nurse at any time; the nurse could also initiate calls when desired. If the 2wT patients did not respond to texts on days 2 or 7, NDoH tracing was activated. The 2wT message flow is presented in Figure 5.
Figure 5.
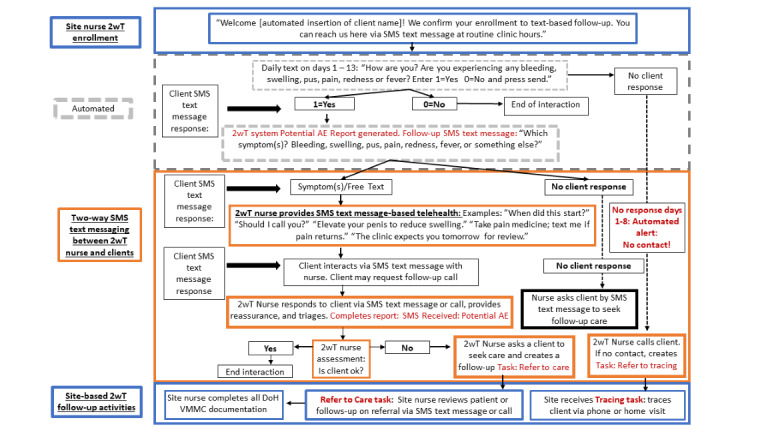
The 2-way texting (2wT) hybrid SMS text message flow (CC BY 4.0 [55]). AE: adverse event; VMMC: voluntary medical male circumcision.
All Study Participants
The 2wT participants in both arms were asked to return to the clinic (urban) or had a visit arranged at their home or an outreach site (rural) for a study-specific, day 14 follow-up to review healing and verify AEs. Day 14 was chosen for verification because 95% of AEs are reported by day 14 [72]. On the day 14 visit, whether on time or delayed and whether the visit took place at the clinic, outreach site, or client’s home, a cell phone credit worth US $7 (100 Rands) was given to all the participants to compensate for time and travel. The control arm VMMC participants were not traced for missing the day 14 visit. The 2wT arm participants with whom there had been no contact by day 14 were actively traced via phone and home visits.
Power and Sample Size
The sample size was calculated based on the AE ascertainment (moderate or severe) occurring between the postoperative days 1 and 14. The noninferiority margin of −0.25% was set as the lower bound of a 95% CI for the maximum mean difference in the rate of cumulative AEs between the control and 2wT arms to conclude that 2wT is noninferior. This margin was set considering the mean AE rate of 0.5% in routine SSA VMMC programs at scale [40,42,46] and assuming that 2wT increases AE ascertainment to 2%, similar to the 1.9% AE ascertainment in the Zimbabwe RCT [50] and the widely accepted safety standard of 2% AE rate [35,48]. With a 10% loss to follow-up (LTFU), a sample size of 1104 men would provide at least 80% power to rule out a decrease in AE ascertainment of >0.25% based on the lower bound of the 1-sided 95% CI. The 1-tailed α value was set as.05.
Outcomes
The primary outcomes of interest were safety and workload. The primary safety outcome was the cumulative AE rate (moderate or severe) ≤day 14 and was calculated per arm as follows: (sum of moderate and severe AEs) / (total number of 2wT participants who had a clinic visit before or on day 14). Similar to the preceding RCT, the safety outcome of cumulative AE rate reported before or on the final study visit on day 14 included a range of 13 to 22 days after VMMC to provide a reasonable margin for participant delays [50]. The primary workload outcome was mean follow-up visits, which was calculated as the mean number of in-person visits, excluding the study-specific visit on day 14. The secondary outcomes included AE rates identified at the day 14 visit, SMS text message response (including daily response, 0=no AE or 1=potential AE, or any freely written text), AE timing, and the severity of AEs. The timing of actions resulting from potential AEs was described as a process measure for care continuity. Variables were created to capture in-person clinic visits and included the following ranges: day 2 visit included visits on days 1 to 4, day 7 visit included visits on days 5 to 10, and day 14 visit included days 13 to 22 after VMMC. All enrollment data on participant wage and visit costs were collected in South African Rand and converted to $US at the exchange rate of US $1=15.68 Rands (June 19, 2022).
Statistical Analyses
Data were exported from the 2wT web-based database and verified using the NDoH paper-record system. Descriptive statistics were calculated to describe the baseline characteristics and number of in-person clinic visits in each study arm. They included median and inter-quartile range (IQR) for the number of clinic visits and frequency for the number of in-person clinic visits. Cumulative AEs and the mean difference in proportions were compared by study arm using the Wilson score method and Manning score method, respectively, and 95% CI for proportions were calculated for both methods. The population for the primary safety outcome analysis (cumulative AEs) included all participants who made at least 1 visit between days 1 and 22. Secondary outcome analysis (AEs identified on day 14) included all participants who made a visit between days 13 and 22. The mean number of in-person clinic visits, excluding study visits, was compared between the 2 arms using a 2-tailed t test. The proportion of potential AEs was calculated as the number of potential AE responses divided by the total number of daily responses (no AE and potential AE). A superiority test was performed on the safety outcome using a 2-sided 95% CI and P value using Fisher exact test. The analyses were performed using Stata (version 17, StataCorp LLC) [73] and SAS (version 9.4, SAS Institute Inc) [74].
Ethics Approval
This multiple principal investigator study was approved by the internal review boards of the University of Washington (study 00009703; principal investigator: CF) and the University of Witwatersrand, Human Research Ethics Committee (ethics reference number: 200204; principal investigator: GS). Written informed consent was obtained from all the participants before enrollment. A 5-person data and safety monitoring board was convened for this study and provided safety oversight, reporting at the conclusion of the study, on May 31, 2022, that the study was safely conducted according to the approved protocols.
Results
Enrollment and Demographics
The CONSORT (Consolidated Standards of Reporting Trials) flow diagram (Multimedia Appendix 1) shows the participant enrollment, assignment, follow-up, and analysis. Study recruitment began on June 7, 2021, and enrollment was completed on February 3, 2022. Follow-up concluded on February 21, 2022. In total, 1084 men were enrolled and randomized in the study. Among the 547 participants in the 2wT arm, 274 (50.1%) were from an urban setting, and 273 (49.9%) were from a rural setting. Of the 537 control participants, 269 (50.1%) were from an urban setting, and 268 (49.9%) were from a rural setting (Table 2). The median participant age was 31 (IQR 24-37) years. The majority of the participants (854/1084, 78.78%) opted for texts in the English language, followed by isiZulu (146/1084, 13.47%) and Setswana (83/1084, 7.66%). Vodacom (Vodacom Group Limited) was the most common mobile carrier (451/1084, 41.6%), followed by MTN (MTN Group Limited; 404/1084, 37.27%). Approximately 60.45% (648/1072) of the participants reported no wages. Among the 39.55% (424/1072) of participants who reported a wage, the median daily wage was US $19.1 (IQR US $12.76-US $28.70).
Table 2.
Description of the voluntary medical male circumcision 2-way texting (2wT) cohort at enrollment by study arm.
| Characteristic | Control (n=537) | 2wT (n=547) | Full sample (N=1084) | |
| Age (years), median (IQRa) | 31 (25-36) | 31 (24-37) | 31 (24-37) | |
| Site, n (%) | ||||
|
|
Urban | 269 (50.1) | 274 (50.1) | 543 (50.1) |
|
|
Rural | 268 (49.9) | 273 (49.9) | 541 (49.9) |
| Language, n (%) | ||||
|
|
English | 429 (79.9) | 425 (77.7) | 854 (78.8) |
|
|
IsiZulu | 71 (13.2) | 75 (13.7) | 146 (13.5) |
|
|
Setswana | 37 (6.9) | 47 (8.6) | 84 (7.7) |
| Mobile carrier, n (%) | ||||
|
|
Cell C | 55 (10.2) | 49 (9) | 104 (9.6) |
|
|
MTN | 193 (35.9) | 211 (38.6) | 404 (37.3) |
|
|
Telcom | 64 (11.9) | 60 (11) | 124 (11.4) |
|
|
Vodacom | 224 (41.7) | 227 (41.5) | 451 (41.6) |
|
|
Other | 1 (0.2) | 0 (0) | 1 (0.1) |
| Daily wage (US $)a | ||||
|
|
None, n (%) | 333 (62.8) | 315 (58.1) | 648 (60.4) |
|
|
Yes, n (%) | 197 (37.2) | 227 (41.9) | 424 (39.6) |
|
|
Value, median (IQR) | 19.13 (12.76-29.34) | 19.13 (12.76-28.70) | 19.13 (12.76-28.70) |
| Transport cost (US $) | ||||
|
|
Value, median (IQR) | 1.66 (0-2.55) | 1.66 (0-2.30) | 1.66 (0-2.55) |
| Food cost (US $) | ||||
|
|
None, n (%) | 479 (89.2) | 482 (88.1) | 961 (88.7) |
|
|
Yes, n (%) | 59 (11) | 65 (11.9) | 123 (11.3) |
|
|
Value, median (IQR) | 1.50 (0.96-2.87) | 1.28 (0.77-2.23) | 1.28 (0.89-2.55) |
aInformation for wages was missing for 7 clients in the routine group and 5 clients in the 2wT group.
2wT Safety
Among participants who had an in-person visit by day 22 after VMMC, AEs were reported in 11 (n=477, 2.3%) 2wT participants and 5 (n=494, 1%) control participants (Table 3). The mean difference in proportions was +1.2% (95% CI −0.09 to +∞). As the lower limit of the 95% CI from the noninferiority comparison was above −0.25%, the 2wT intervention was noninferior to routine in-person follow-up care for AE ascertainment. The cumulative AE rates did not differ between the arms (P=.13). On the day 14 visit, 4 (0.9%) AEs were identified among the control participants and 1 AE (0.2%) was identified among the 2wT participants—a nonsignificant difference (P=.37).
Table 3.
Comparison of combined moderate or severe adverse events (AEs) among circumcised males in South Africa by arm.
|
|
Routine (n=537) | Two-way texting (n=547) | Difference in proportions, % | Noninferiority comparison | Superiority comparison | |||||||
|
|
n | Proportion (95% CI)a, % | n | Proportion (95% CI)a, % |
|
1-sided 95% CIb | 2-sided 95% CIb | 2-sided P valuec | ||||
| Cumulative AEs ≤day 14d | 5/494 | 1.0 (0.4 to 2.3) | 11/477 | 2.3 (1.3 to 4.1) | +1.2 | −0.09 to +∞ | −0.35 to 2.85 | .13 | ||||
| AEs on day 14e | 4/438 | 0.9 (0.4 to 2.3) | 1/463 | 0.2 (0.03 to 1.2) | −0.7 | N/Af | −1.61 to +∞ | .37 | ||||
aCI for binomial proportions were calculated using the Wilson score method.
bCI in binomial proportions were calculated using the Farrington–Manning score method.
cP value comparison group is by Fisher exact test.
dCumulative moderate and severe AEs reported during study visits from days 1 to 22 among the participants with at least 1 postoperative visit.
eCumulative moderate and severe AEs reported during study visits from days 13 to 22 among participants.
fN/A: not applicable.
Follow-up Visit Workload
The texting intervention group reported a mean of 0.22 (SD 0.65) nonstudy visits per person (median 0) compared with 1.34 (SD 0.85) nonstudy visits per person (median 2) in the control group over the 14-day postoperative period—a significant difference of 1.12 visits between the means (P<.001; Table 4). There was an 84% reduction in the follow-up visit workload using 2wT compared with routinely scheduled visits. The participants in the control group were each expected to return for 2 scheduled visits; they returned for 719 visits, total (median 2, IQR 1-2), excluding the study-specific day 14 visit. Among the 537 control participants, 105 (19.6%), 159 (29.6%), and 266 (49.5%) returned for 0, 1, and 2 visits, respectively, and 432 (80.4%) returned for at least 1 visit, excluding the study-specific visit. Among the 2wT participants, there were 118 visits, total (median 0, IQR 0-0), not including the study-specific day 14 visit. Among the 547 participants in the 2wT arm, 60 (11%) and 18 (3.3%) returned for 1 and 2 visits, respectively (Table 3). Excluding the day 14 visit, most 2wT participants (n=464, 84.8%) did not return for any postoperative visits.
Table 4.
Comparison of the workload outcome by arm (excluding the study-specific day 14 visit).
|
|
Control (n=537) | 2wTa (n=547) | Difference in means (95% CI) | 2-sided P value | |||
| Number of clinic visitsb | |||||||
|
|
Value, mean (SD) | 1.34 (0.85) | 0.22 (0.65) | 1.12 (1.03-1.21) | <.001 | ||
|
|
Value, median (IQR) | 2 (1-2) | 0 (0-0) | N/Ac | N/A | ||
| Males with ≥1 in-person follow-up visits within 14 daysd, n (%) | 431 (80.3) | 83 (15.2) | N/A | N/A | |||
| Total visits per client, n (%) | N/A | N/A | |||||
|
|
0 | 105 (19.6) | 464 (84.8) |
|
|
||
|
|
1 | 159 (29.6) | 60 (11) |
|
|
||
|
|
2 | 266 (49.5) | 18 (3.3) |
|
|
||
|
|
3 | 4 (0.7) | 3 (0.5) |
|
|
||
|
|
4 | 1 (0.2) | 1 (0.2) |
|
|
||
|
|
5 | 1 (0.2) | 0 (0) |
|
|
||
|
|
6 | 0 (0) | 0 (0) |
|
|
||
|
|
7 | 1 (0.2) | 0 (0) |
|
|
||
|
|
8 | 0 (0) | 0 (0) |
|
|
||
|
|
9 | 0 (0) | 1 (0.2) |
|
|
||
a2wT: 2-way texting.
bThere were a total of 719 clinic visits in the control group and 118 clinical visits in the 2-way texting group.
cN/A: not applicable.
dThe US President’s Emergency Plan for AIDS Relief indicator.
Comparison within arms (stratified by location [urban vs rural], not shown) identified similar, significant differences in workload between arms. Among the control participants only, visit attendance was nearly 10% higher among the urban participants than among the rural participants on day 2 (200/269, 74.3% vs 175/268, 65.3%; P=.02). LTFU was also significantly higher among the urban participants (23/269, 8.6%) than among the rural participants (6/268, 2.2%) in the control arm (P=.002). Among the 2wT participants only, more urban participants (28/274, 10.2%) than rural participants (11/273, 4%) made a visit on day 2 (P=.01). LTFU was higher among the urban 2wT participants but not significantly (30/274, 10.9% vs 17/273, 6.2%; P=.07). The follow-up visit workload reduction was 79% in the urban setting and 89% in the rural setting.
Secondary Process Outcomes
Texting Response Rates
Response rates were high among the 2wT participants, ranging from a maximum of 86% (468/547) on day 3 to a minimum of 74% (407/547) on day 13. On days 2 and 7, 85% (463/547) and 79% (433/547) of the participants responded, respectively. Among the 547 participants, 514 (94%) responded at least once in 13 days. Only 6.4% (33/514) participants never responded to a daily text. Of the 547 participants in the 2wT arm, 301 (55%) sent at least 1 potential AE text over the 13 days. On an average day, 44% (241/547) responded with “No AE,” 8% (44/547) responded with “potential AE,” 28% (153/547) responded with a free text, and 20% (109/547) did not respond (Figure 6). Among those with an expected 0 or 1 response to the daily SMS text message (no AE or potential AE), a mean of 15% (n=43) responded with a potential AE each day. On day 3, a total of 21% (115/547) of the participants responded with a potential AE, but only 12% (66/547) responded similarly on day 13.
Figure 6.
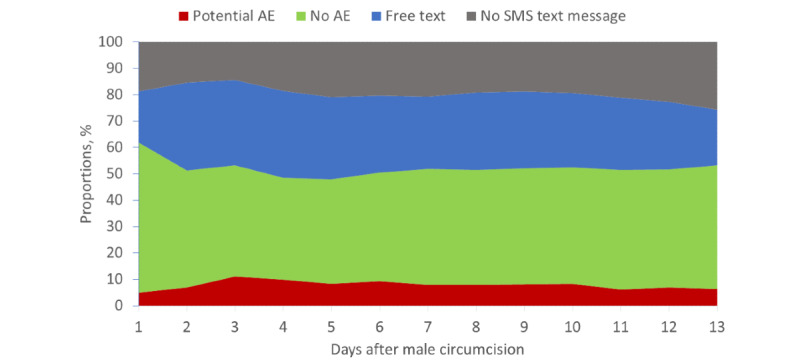
Daily SMS text message responses among 2-way texting participants. AE: adverse event.
Timing and Severity of AEs
Among the 2wT participants, there were a total of 11 AEs, with 9 moderate (2 bleeding, 4 infections, and 3 wound disruptions) and 2 severe bleeding AEs (Table 5). Among the control participants, there were a total of 5 AEs, all moderate (2 infections, 2 wound disruptions, and 1 other [swelling]). The 2wT participants were identified with AEs earlier than the control participants. Among the 2wT participants, 64% (7/11) AEs were identified on or before day 7, whereas only 20% (1/5) AEs among the control participants were identified during this early period. Late AEs (>day 14) were identified among 2 (0.4%) out of 537 control participants. All AEs were related to VMMC, and all occurred on or before day 22. Mild AEs were not included in the study outcomes.
Table 5.
Adverse event (AE) severity and type by arm, postoperative day, and location.
| AE severity | Postoperative day | AE type | Study arm | Location | |||
|
|
|
|
2wTa (n=11) | Control (n=5) | Urban (n=14) | Rural (n=2) | |
| Severe | 1 | Bleeding | ✓ |
|
|
✓ | |
| Severe | 3 | Bleeding | ✓ |
|
✓ |
|
|
| Moderate | 2 | Bleeding | ✓ |
|
✓ |
|
|
| Moderate | 2 | Bleeding | ✓ |
|
✓ |
|
|
| Moderate | 4 | Infection | ✓ |
|
✓ |
|
|
| Moderate | 5 | Infection | ✓ |
|
✓ |
|
|
| Moderate | 7 | Infection | ✓ |
|
✓ |
|
|
| Moderate | 7 | Swelling |
|
✓ | ✓ |
|
|
| Moderate | 10 | Wound disruption | ✓ |
|
✓ |
|
|
| Moderate | 10 | Wound disruption | ✓ |
|
|
✓ | |
| Moderate | 12 | Infection | ✓ |
|
✓ |
|
|
| Moderate | 14 | Infection |
|
✓ | ✓ |
|
|
| Moderate | 14 | Wound disruption |
|
✓ | ✓ |
|
|
| Moderate | 14 | Wound disruption | ✓ |
|
✓ |
|
|
| Moderate | 17 | Wound disruption |
|
✓ | ✓ |
|
|
| Moderate | 22 | Infection |
|
✓ | ✓ |
|
|
a2wT: 2-way texting.
Time Between Potential AE Text and Follow-up
Among the 2wT participants, there were 7111 responses to the daily SMS text message, of which 559 (7.9%) responses were a 1, or a potential AE. The nurse completed 704 potential AE forms, which included reports stemming from men who conveyed issues or concerns first via a free text and not the daily response; 649 potential AE forms were completed and were unique to 1 client per day. Potential AE forms included the documentation of concerns (AE type or severity) and triage (education, reassurance, wound care instructions, etc). The nurse could refer with or without suspicion of an AE, allowing them flexibility to assess each client individually. Referrals to care created a task for the site team to complete an in-person review. From the 649 filled potential AE forms, 50 (7.7%) referrals were made (including for 3 moderate and 1 severe potential AEs): 32 returned within 3 days, and 4 AEs were ascertained (moderate: 3/4, 75% and severe: 1/4, 25%).
LTFU Rate
There were 47 (8.6%) out of the 547 participants in the 2wT arm who did not return for any in-person follow-up and were considered LTFU; of the 47 participants, 45 (96%) were successfully contacted by phone and reported no concerns, 1 (2%) had a physical visit before day 13 and was observed to be healing on schedule, and 1 (2%) had no postoperative contact. Among the 537 control participants, 29 (5.4%) were LTFU; of the 29 participants, 10 (34%) were successfully contacted by phone and reported no concerns, 2 (7%) had visits, and 17 (59%) had no postoperative contact.
Discussion
Principal Safety and Workload Findings
The study conclusively demonstrated that in South Africa, 2wT for VMMC follow-up is noninferior to in-person reviews for AE ascertainment, providing rigorous evidence in support of 2wT safety in routine settings. The 2wT approach also dramatically reduced in-person visits, allowing the clinical team to focus on, and care for, those with potential complications rather than conducting scheduled follow-ups for all men, demonstrating clear efficiency gains. Most 2wT participants interacted via 2wT and elected to heal independently at home rather than return for an in-person review. The South African 2wT RCT adhered to best practices in the monitoring and evaluation of digital health innovations [14,70,75], adding to the evidence from both the Zimbabwe RCT and routine scale-up that 2wT is as safe as, and more efficient than, routine in-person reviews for postoperative follow-up [50,55]. The 2wT results also indicate some of the advantages of telehealth for safe and efficient surgical follow-up [76-78]. As this pragmatic RCT took place within NDoH VMMC settings and largely with routine HCWs, these results strongly suggest that the 2wT telehealth approach to VMMC follow-up should be rolled out as an option for providers and patients. We discuss several advantages of and barriers for 2wT to scale successfully.
First, recent findings from usability testing among 2wT HCWs [79] showed that 2wT responded well to the expressed needs of HCWs and clients, increasing the likelihood of sustained use and widespread adoption [80,81]. From inception, 2wT adaptation, testing, and optimization processes adhered to the common principles for mHealth optimization focused on both patient and provider users, the engagement of broad stakeholders, providing training (and refresher training) to users via hands-on methods, using a simple technology with a familiar user interface, addressing a recognized need for updated VMMC policy, and using widely available SMS text messaging technology [82]. The 2wT approach complements the efficiency of automation with alerts for nurses to engage in direct client messaging when needed, thereby enhancing the nurse-patient relationship. Nurses who refer clients to care trigger an alert for follow-up, requiring an HCW to document subsequent visits, confirm patient-reported improvement, or initiate additional tracing efforts. The embedded system alerts escalate clients without responses to tracing and remind providers to close referral loops when clients are found. The engagement of an SMS text message aggregator in South Africa also increased the efficiency of automated SMS text messages, easing the identification and resolution of any systematic message delays or failures and enhancing user experience. With 2wT’s inclusion of core CHT features, such as longitudinal patient records, task management, and reporting support, 2wT adaptation could transform other postoperative or other acute follow-ups outside the VMMC context.
The 2wT approach improved the quality of postoperative follow-up, as evidenced by consistent and correct AE identification, a standard indicator of quality VMMC postoperative care. Improvements are likely owing to both patient and provider engagement. In 2wT, 5 moderate AEs were identified on or before day 7, after the men were first triaged by the 2wT nurse. This early AE ascertainment suggests that direct 2wT communication between the nurse and the patient encouraged men to return promptly for review when needed. By contrast, 4 men in the control group arm were identified with AEs at the day 14 visit or later, suggesting that they may have delayed care, or not received care, in the absence of the study. This care-seeking behavior suggests that 2wT improves patient health literacy and care engagement, placing the responsibility for healthy healing into the patient's hands and shifting the power balance toward the individual rather than the formal health sector. Furthermore, within the study context, providers promptly documented AEs, including the cascade from potential AEs, through AE clinical management. Although AE ascertainment is a priority indicator of quality VMMC care [35], AEs are chronically underreported in routine settings [45,46,51], including in South Africa [40,44]. The 2wT approach appears to improve AE ascertainment and reporting, contributing to improved patient management and program outcomes.
Similar to the findings from Zimbabwe that showed that 2wT improved efficiency and reduced costs [53], 2wT reduced the follow-up visit workload in South Africa by 79% in urban and 89% in rural settings, leading to program cost savings in both settings [83]. These visit reductions were observed in the already-reduced in-person visits implemented for COVID-19 precautions. Whether VMMC follow-up visits return to prepandemic levels, reducing unnecessary visits would likely have a greater impact in rural settings where the VMMC service model is predominantly outreach, reducing travel time. The benefits of fewer visits could also have a positive impact on VMMC client demand, reducing barriers to VMMC such as transportation costs or time away from work [84]. Moreover, in the future, 2wT could strengthen the continuum of referrals even outside participating VMMC clinics or clinicians by engaging directly with patients. Participants enrolled in 2wT in a central location could seek care at NDoH sites outside the 2wT catchment area and self-report visits, AE diagnoses, and treatments via 2wT. This information pathway could further contribute to improved AE reporting and visit documentation while reducing the burden on HCWs. Advocating for formal PEPFAR approval of 2wT-based follow-up in lieu of in-person visits could fulfill the PEPFAR indicator of at least 1 postoperative visit within 14 days [3] while simultaneously reducing the HCW burden and improving patient care.
Despite these benefits, there are challenges to scaling 2wT successfully. First, digital literacy among HCWs remains low [85]. Patients only need to be comfortable with basic SMS text messaging technology, but HCWs interacting with 2wT must be able to manage the app at a comparable level to WhatsApp, a nonnegligible challenge in some settings or for some HCWs. Patient demand must also increase. For success, 2wT education and outreach are needed to raise awareness around 2wT advantages for both quality care and reduced patient costs [86]. In addition, some patients may lack confidence in telehealth owing to persistent network and infrastructure challenges [87], stymying 2wT growth. The 2wT approach also suffers, in part, by a perception of increased workload. HCWs save time by conducting far fewer routinely scheduled follow-up reviews and by reducing travel for the reviews. However, that time gained is reallocated to interactions with men via 2wT and to other routine duties. The time and cost savings of 2wT are likely to be more appreciated at the health services level as overall efficiency gains across VMMC or routine service delivery, and not as reduced workload during duty hours. As with all postoperative care, patients may require care at any time. Although clients were informed that 2wT is not for emergencies, nurses were required to review 2wT SMS text messages in evenings and on weekends, an issue that should be addressed via the rotation of duties and flexible work hours. Moreover, the 2wT dashboards and data analytics support routine VMMC program reporting. However, approvals of digital documentation for the NDoH and implementing partners, in lieu of and not in addition to paper reporting, will be needed to facilitate scale-up. Finally, as with all digital health interventions, there are concerns regarding sustainability. However, as 2wT specifically targets patients in need of a brief but intensive interaction with a provider, and not a repeated interaction with a health care unit, the benefits of immediate scale-up offset the concerns for long-term eHealth integration.
Limitations
This study has several limitations. As for clients, men without their own phones or those who shared phones were excluded. The 2wT approach would also not work in remote settings without at least some cell connectivity. Using SMS text messaging for 2wT makes it more equitable and accessible for those with basic phones [20] but could reduce uptake for those with feature or smartphones or those who prefer WhatsApp. The 2wT automated SMS text messages were only scripted in 3 predominant languages of the area, potentially excluding men whose preferred language was not offered. Notifiable AEs could be underreported in either group. Both arms received enhanced AE identification education; however, men in the 2wT arm received additional counseling using illustrative photos to explain the words of the daily SMS text message, a bias that could have increased AE identification in the 2wT arm. The RCT study team provided quality assurance throughout the study to ensure adherence to the protocols, increasing supervision and support. However, continued success with 2wT in Zimbabwe within routine, nonresearch settings suggests that 2wT would have similar results outside RCT structures. Complementary usability assessment from both HCW and client perspectives and costing results are forthcoming and, therefore, not included in this paper. Finally, in the context of the COVID-19 pandemic, this RCT emphasized pragmatism and flexibility, a limitation that also facilitated the implementation of the study in challenging times. During the RCT enrollment period, there were 3 waves of the COVID-19 pandemic, causing various levels of clinic closures, service delivery restrictions that affected follow-up, and increased turnover in health care personnel. During the COVID-19 pandemic, the PEPFAR guidelines were changed to allow for phone-based VMMC follow-up when feasible [88]. As a result, in-person visits in the control group likely declined by an unknown percentage. Even in this context, the 2wT study identified a significant reduction in follow-up visit workload with maintained quality of care, reinforcing these dual advantages of 2wT for routine VMMC settings.
Conclusions
Over 4 years of rigorous implementation science research and evaluation in both South Africa and Zimbabwe, 2wT-based telehealth successfully provided quality VMMC follow-up for over 24,000 males, aged ≥15years, in both rural and urban settings [50,53-55]. These studies respond to global calls for robust evidence generation in digital health interventions [82,89,90] and support the recent global VMMC policy changes allowing for the use of postoperative telehealth, in lieu of scheduled visits, for low-risk post-VMMC clients [88]. The 2wT care model, specifically, improved more than safety. The 2wT approach motivated males to actively assume care-seeking responsibility for potential AEs, strengthening relationships between males and nurses and creating a partnership in healing. The 2wT approach also added value in the context of the COVID-19 pandemic by providing dual SMS text messaging–based telehealth and infection prevention benefits. SSA is ready for a 2wT telemedicine approach based on widespread SMS text messaging technology. Therefore, in recognition of scarce health care resources and strong evidence from this rigorously tested intervention, 2wT should be scaled in both rural and urban VMMC programs. Further consideration of simple telehealth approaches such as 2wT could also provide powerful pathways to improve care and reduce workload beyond VMMC, bringing similar benefits for other acute follow-up care contexts, including COVID-19, acute respiratory infection, and other short-term postoperative care.
Acknowledgments
The authors would like to thank the Departments of Health of the Gauteng and North West provinces; implementing partner, Right to Care, for enabling participation of the clinical teams; and the Centre for HIV-AIDS Prevention Studies (CHAPS) study implementation team for their dedication and skills in study recruitment, data management, and data capture. The authors would like to thank the Medic team, specifically Dr Raymond Mugwanya, for their technical skills and invaluable commitment to the success of the project. Research reported in this publication was supported by the National Institute of Nursing Research of the National Institutes of Health (NIH) under award number 5R01NR019229 (“Expanding and Scaling Two-way Texting to Reduce Unnecessary Follow-Up and Improve Adverse Event Identification Among Voluntary Medical Male Circumcision Clients in the Republic of South Africa”). Grant submission preparation was supported by the University of Washington and its Fred Hutch Center for AIDS Research, an NIH-funded program under award number AI027757 that is supported by the following NIH Institutes and Centers: National Institute of Allergy and Infectious Diseases, National Cancer Institute, National Institute of Mental Health, National Institute on Drug Abuse, Eunice Kennedy Shriver National Institute of Child Health and Human Development, National Heart, Lung and Blood Institute, National Investigation Agency, National Institute of General Medical Sciences, and National Institute of Diabetes and Digestive and Kidney Diseases. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Abbreviations
- 2wT
2-way texting
- AE
adverse event
- CHAPS
Centre for HIV-AIDS Prevention Studies
- CHT
Community Health Toolkit
- CONSORT
Consolidated Standards of Reporting Trials
- HCW
health care worker
- LTFU
loss to follow-up
- mHealth
mobile health
- NDoH
National Department of Health
- PEPFAR
US President’s Emergency Plan for AIDS Relief
- RCT
randomized controlled trial
- SSA
sub-Saharan Africa
- VMMC
voluntary medical male circumcision
- WHO
World Health Organization
CONSORT eHealth Checklist.
Data Availability
The data sets generated in the randomized controlled trial and analyzed during this study, including demographics, SMS text messaging response rates, clinic visits, and adverse events, are available from the corresponding author upon reasonable request.
Footnotes
Conflicts of Interest: None declared.
References
- 1.Amankwaa I, Boateng D, Quansah DY, Akuoko CP, Evans C. Effectiveness of short message services and voice call interventions for antiretroviral therapy adherence and other outcomes: a systematic review and meta-analysis. PLoS One. 2018;13(9):e0204091. doi: 10.1371/journal.pone.0204091. https://dx.plos.org/10.1371/journal.pone.0204091 .PONE-D-17-00352 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Demena BA, Artavia-Mora L, Ouedraogo D, Thiombiano BA, Wagner N. A systematic review of mobile phone interventions (SMS/IVR/Calls) to improve adherence and retention to antiretroviral treatment in low-and middle-income countries. AIDS Patient Care STDS. 2020 Feb;34(2):59–71. doi: 10.1089/apc.2019.0181. [DOI] [PubMed] [Google Scholar]
- 3.PEPFAR Monitoring, Evaluation, and Reporting (MER 2.0) Indicator Reference Guide. PEPFAR. 2017. Jan, [2020-09-11]. https://srhrindex.srhrforall.org/uploads/2018/11/2017_PEPFAR-Monitoring-Evaluation-and-Reporting-Indicator-Reference-Guide_MER-2.0-Version-2.1.pdf .
- 4.Pintye J, Rogers Z, Kinuthia J, Mugwanya KK, Abuna F, Lagat H, Sila J, Kemunto V, Baeten JM, John-Stewart G, Unger JA. Two-way short message service (SMS) communication may increase pre-exposure prophylaxis continuation and adherence among pregnant and postpartum women in Kenya. Glob Health Sci Pract. 2020 Mar 05;8(1):55–67. doi: 10.9745/ghsp-d-19-00347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Saragih ID, Tonapa SI, Osingada CP, Porta CM, Lee B. Effects of telehealth-assisted interventions among people living with HIV/AIDS: a systematic review and meta-analysis of randomized controlled studies. J Telemed Telecare. 2021 Dec 30;:1357633X2110707. doi: 10.1177/1357633x211070726. [DOI] [PubMed] [Google Scholar]
- 6.Ødegård ES, Langbråten LS, Lundh A, Linde DS. Two-way text message interventions and healthcare outcomes in Africa: systematic review of randomized trials with meta-analyses on appointment attendance and medicine adherence. PLoS One. 2022;17(4):e0266717. doi: 10.1371/journal.pone.0266717. https://dx.plos.org/10.1371/journal.pone.0266717 .PONE-D-21-10098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kruse C, Betancourt J, Ortiz S, Valdes Luna SM, Bamrah IK, Segovia N. Barriers to the use of mobile health in improving health outcomes in developing countries: systematic review. J Med Internet Res. 2019 Oct 09;21(10):e13263. doi: 10.2196/13263. https://www.jmir.org/2019/10/e13263/ v21i10e13263 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dodoo JE, Al-Samarraie H, Alzahrani AI. Telemedicine use in Sub-Saharan Africa: barriers and policy recommendations for Covid-19 and beyond. Int J Med Inform. 2021 Jul;151:104467. doi: 10.1016/j.ijmedinf.2021.104467. https://europepmc.org/abstract/MED/33915421 .S1386-5056(21)00093-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mitgang EA, Blaya JA, Chopra M. Digital health in response to COVID-19 in low- and middle-income countries: opportunities and challenges. Glob Policy. 2021 Mar 17;12(Suppl 6):107–9. doi: 10.1111/1758-5899.12880. https://europepmc.org/abstract/MED/34230840 .GPOL12880 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bitar H, Alismail S. The role of eHealth, telehealth, and telemedicine for chronic disease patients during COVID-19 pandemic: a rapid systematic review. Digit Health. 2021;7:20552076211009396. doi: 10.1177/20552076211009396. https://journals.sagepub.com/doi/10.1177/20552076211009396?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub0pubmed .10.1177_20552076211009396 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gunasekeran DV, Tseng RM, Tham Y, Wong TY. Applications of digital health for public health responses to COVID-19: a systematic scoping review of artificial intelligence, telehealth and related technologies. NPJ Digit Med. 2021 Feb 26;4(1):40. doi: 10.1038/s41746-021-00412-9. doi: 10.1038/s41746-021-00412-9.10.1038/s41746-021-00412-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mbunge E, Batani J, Gaobotse G, Muchemwa B. Virtual healthcare services and digital health technologies deployed during coronavirus disease 2019 (COVID-19) pandemic in South Africa: a systematic review. Glob Health J. 2022 Jun;6(2):102–13. doi: 10.1016/j.glohj.2022.03.001. https://linkinghub.elsevier.com/retrieve/pii/S2414-6447(22)00023-9 .S2414-6447(22)00023-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Labrique A, Agarwal S, Tamrat T, Mehl G. WHO digital health guidelines: a milestone for global health. NPJ Digit Med. 2020 Sep 18;3(1):120. doi: 10.1038/s41746-020-00330-2. doi: 10.1038/s41746-020-00330-2.10.1038/s41746-020-00330-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Monitoring and Evaluating Digital Health Interventions: A Practical Guide to Conducting Research and Assessment2016 Cited 2021. Geneva: World Health Organization; 2016. [Google Scholar]
- 15.WHO Guideline Recommendations on Digital Interventions for Health System Strengthening. Geneva: World Health Organization; 2019. [PubMed] [Google Scholar]
- 16.McCool J, Dobson R, Whittaker R, Paton C. Mobile health (mHealth) in low- and middle-income countries. Annu Rev Public Health. 2022 Apr 05;43:525–39. doi: 10.1146/annurev-publhealth-052620-093850. https://www.annualreviews.org/doi/abs/10.1146/annurev-publhealth-052620-093850?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub0pubmed . [DOI] [PubMed] [Google Scholar]
- 17.Guo C, Ashrafian H, Ghafur S, Fontana G, Gardner C, Prime M. Challenges for the evaluation of digital health solutions-a call for innovative evidence generation approaches. NPJ Digit Med. 2020;3:110. doi: 10.1038/s41746-020-00314-2. doi: 10.1038/s41746-020-00314-2.314 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Manby L, Aicken C, Delgrange M, Bailey JV. Effectiveness of eHealth interventions for HIV prevention and management in sub-Saharan Africa: systematic review and meta-analyses. AIDS Behav. 2022 Feb;26(2):457–69. doi: 10.1007/s10461-021-03402-w. https://europepmc.org/abstract/MED/34427813 .10.1007/s10461-021-03402-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Were MC, Sinha C, Catalani C. A systematic approach to equity assessment for digital health interventions: case example of mobile personal health records. J Am Med Inform Assoc. 2019 Aug 01;26(8-9):884–90. doi: 10.1093/jamia/ocz071. https://europepmc.org/abstract/MED/31188438 .5514214 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nittas V, Ameli V, Little M, Humphreys DK. Exploring the equity impact of mobile health-based human immunodeficiency virus interventions: a systematic review of reviews and evidence synthesis. Digit Health. 2020;6:2055207620942360. doi: 10.1177/2055207620942360. https://journals.sagepub.com/doi/10.1177/2055207620942360?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub0pubmed .10.1177_2055207620942360 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Swartz A, LeFevre AE, Perera S, Kinney MV, George AS. Multiple pathways to scaling up and sustainability: an exploration of digital health solutions in South Africa. Global Health. 2021 Jul 06;17(1):77. doi: 10.1186/s12992-021-00716-1. https://globalizationandhealth.biomedcentral.com/articles/10.1186/s12992-021-00716-1 .10.1186/s12992-021-00716-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Marcolino MS, Oliveira JA, D'Agostino M, Ribeiro AL, Alkmim MB, Novillo-Ortiz D. The impact of mHealth interventions: systematic review of systematic reviews. JMIR Mhealth Uhealth. 2018 Jan 17;6(1):e23. doi: 10.2196/mhealth.8873. https://mhealth.jmir.org/2018/1/e23/ v6i1e23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Paul ME, Castillo M, Emmanuel P, Bauermeister JA, Mena LA, Sullivan PS, Hightow-Weidman LB. Scale up mHealth HIV interventions: site and public health perspectives and lessons learned from P3. Mhealth. 2021;7:38. doi: 10.21037/mhealth-20-65. https://europepmc.org/abstract/MED/33898607 .mh-07-20-65 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.McCool J, Dobson R, Muinga N, Paton C, Pagliari C, Agawal S, Labrique A, Tanielu H, Whittaker R. Factors influencing the sustainability of digital health interventions in low-resource settings: lessons from five countries. J Glob Health. 2020 Dec;10(2):020396. doi: 10.7189/jogh.10.020396. https://europepmc.org/abstract/MED/33274059 .jogh-10-020396 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Perrier T, Harrington E, Ronen K, Matemo D, Kinuthia J, John-Stewart G, Anderson R, Unger J. Male partner engagement in family planning SMS conversations at Kenyan health clinics. Proceedings of the 1st ACM SIGCAS Conference on Computing and Sustainable Societies; COMPASS '18: ACM SIGCAS Conference on Computing and Sustainable Societies; Jun 20 - 22, 2018; Menlo Park and San Jose, CA, USA. 2018. [DOI] [Google Scholar]
- 26.Sileo KM, Fielding-Miller R, Dworkin SL, Fleming PJ. A scoping review on the role of masculine norms in men's engagement in the HIV care continuum in sub-Saharan Africa. AIDS Care. 2019 Nov 25;31(11):1435–46. doi: 10.1080/09540121.2019.1595509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.IN DANGER: UNAIDS Global AIDS Update 2022. UNAIDS. [2022-06-06]. https://www.unaids.org/sites/default/files/media_asset/2022-global-aids-update_en.pdf .
- 28.Uneven progress on the voluntary medical male circumcision. UNAIDS and WHO. 2022. Apr, [2023-03-17]. https://cdn.who.int/media/docs/default-source/hq-hiv-hepatitis-and-stis-library/who-unaids-male-circumcision-progress-brief-2022.pdf?sfvrsn=2852eedf_1&ua=1 .
- 29.Considerations for implementing models for optimizing the volume and efficiency of male circumcision services. World Health Organization. 2010. Feb, https://www.malecircumcision.org/sites/default/files/document_library/Considerations%20models.pdf .
- 30.World Health Organization . Preventing HIV Through Safe Voluntary Medical Male Circumcision for Adolescent Boys and Men in Generalized HIV Epidemics Recommendations and Key Considerations. Geneva: World Health Organization; 2020. [PubMed] [Google Scholar]
- 31.Voluntary medical male circumcision — Steady progress in the scaleup of VMMC as an HIV prevention intervention in 15 eastern and southern African countries before the SARS-CoV2 pandemic. UNAIDS. 2021. Feb 28, [2022-12-16]. https://www.unaids.org/en/resources/documents/2021/ voluntary-medical-male-circumcision-15-eastern-southern-african-countries .
- 32.2022 Country Operational Plan Guidance. The United States President’s Emergency Plan for AIDS Relief. [2022-12-16]. https://www.state.gov/2022-country-operational-plan-guidance/
- 33.Manual for male circumcision under local anaesthesia and HIV prevention services for adolescent boys and men. World Health Organization. 2018. [2019-02-01]. https://www.who.int/publications/i/item/manual-for-male-circumcision-under-local-anaesthesia-and-hiv-prevention-services-for-adolescent-boys-and-men .
- 34.World Health Organization, Joint United Nations Programme on HIV/AIDS WHO/UNAIDS Technical Consultation on Male Circumcision and HIV Prevention: Research Implications for Policy and Programming. UNIADS. 2007. [2022-12-16]. http://www.unaids.org/sites/default/files/media_asset/mc_recommendations_en_1.pdf .
- 35.Chapter seven. Managing, monitoring, and reporting VMMC adverse events PEPFAR’s best practices for voluntary medical male circumcision site operations. PEPFAR. [2022-12-16]. https://www.malecircumcision.org/sites/default/files/document_library/2017.9.26_ch7_vmmc-site-ops.pdf .
- 36.South African national guidelines for medical male circumcision. National Department of Health. 2015. [2022-12-16]. https://www.knowledgehub.org.za/elibrary/south-african-national-guidelines-medical-male-circumcision .
- 37.Ford N, Chu K, Mills EJ. Safety of task-shifting for male medical circumcision: a systematic review and meta-analysis. AIDS. 2012 Mar 13;26(5):559–66. doi: 10.1097/QAD.0b013e32834f3264. [DOI] [PubMed] [Google Scholar]
- 38.Kitara DL, Ocero A, Lanyero J, Ocom F. Roll-out of medical male circumcision (MMC) for HIV prevention in non-circumcising communities of Northern Uganda. Pan Afr Med J. 2013;15:100. doi: 10.11604/pamj.2013.15.100.2338. https://europepmc.org/abstract/MED/24198894 .PAMJ-15-100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Frajzyngier V, Odingo G, Barone M, Perchal P, Pavin M. Safety of adult medical male circumcision performed by non-physician clinicians in Kenya: a prospective cohort study. Glob Health Sci Pract. 2014 Feb;2(1):93–102. doi: 10.9745/GHSP-D-13-00120. http://www.ghspjournal.org/cgi/pmidlookup?view=long&pmid=25276565 .GHSP-D-13-00120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Phili R, Abdool-Karim Q, Ngesa O. Low adverse event rates following voluntary medical male circumcision in a high HIV disease burden public sector prevention programme in South Africa. J Int AIDS Soc. 2014;17(1):19275. doi: 10.7448/IAS.17.1.19275. https://europepmc.org/abstract/MED/25406951 .19275 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Brito A, Korn A, Monteiro L, Mudender F, Maiela A, Come J, Barnhart S, Feldacker C. Need for improved detection of voluntary medical male circumcision adverse events in Mozambique: a mixed-methods assessment. BMC Health Serv Res. 2019 Nov 21;19(1):855. doi: 10.1186/s12913-019-4604-1. https://bmchealthservres.biomedcentral.com/articles/10.1186/s12913-019-4604-1 .10.1186/s12913-019-4604-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hellar A, Plotkin M, Lija G, Mwanamsangu A, Mkungume S, Christensen A, Mushi J, Machaku M, Maokola T, Mlanga E, Curran K. Adverse events in a large-scale VMMC programme in Tanzania: findings from a case series analysis. J Int AIDS Soc. 2019 Jul;22(7):e25369. doi: 10.1002/jia2.25369. https://europepmc.org/abstract/MED/31368235 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Bochner AF, Feldacker C, Makunike B, Holec M, Murenje V, Stepaniak A, Xaba S, Balachandra S, Tshimanga M, Chitimbire V, Barnhart S. Adverse event profile of a mature voluntary medical male circumcision programme performing PrePex and surgical procedures in Zimbabwe. J Int AIDS Soc. 2017 Feb 21;19(1):21394. doi: 10.7448/IAS.20.1.21394. https://europepmc.org/abstract/MED/28362066 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Muchiri E, Charalambous S, Ginindza S, Maraisane M, Maringa T, Vranken P, Loykissoonlal D, Muturi-Kioi V, Chetty-Makkan CM. Description of adverse events among adult men following voluntary medical male circumcision: findings from a circumcision programme in two provinces of South Africa. PLoS One. 2021 Aug 17;16(8):e0253960. doi: 10.1371/journal.pone.0253960. https://dx.plos.org/10.1371/journal.pone.0253960 .PONE-D-20-25732 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.O'Bryan G, Feldacker C, Ensminger A, Nghatanga M, Brandt L, Shepard M, Billah I, Aupokolo M, Mengistu AT, Forster N, Zemburuka B, Sithole E, Mutandi G, Barnhart S, O'Malley G. Adverse event profile and associated factors following surgical voluntary medical male circumcision in two regions of Namibia, 2015-2018. PLoS One. 2021;16(10):e0258611. doi: 10.1371/journal.pone.0258611. https://dx.plos.org/10.1371/journal.pone.0258611 .PONE-D-21-20649 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Victor O, Phiona M, Vernon M, Thoko M, Paidamoyo G, Farai G, Joseph H, Munyaradzi T, Olbarn R, Pesanai C, Mufuta T, Vuyelwa S, Sinokuthemba X, Batsirai M, Marrianne H, Scott B, Feldacker C. Adverse event trends within a large-scale, routine, voluntary medical male circumcision program in Zimbabwe, 2014-2019. J Acquir Immune Defic Syndr. 2021 Oct 01;88(2):173–80. doi: 10.1097/QAI.0000000000002751. https://europepmc.org/abstract/MED/34173789 .00126334-202110010-00008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Lucas T, Cooney C, Prainito A, Godfrey C, Kiggundu V, Thomas AG, Ridzon R, Toledo C. Consolidated overview of notifiable adverse events in the U.S. President's emergency plan for AIDS relief's voluntary medical male circumcision program through 2020. Curr HIV/AIDS Rep. 2022 Dec 08;19(6):508–15. doi: 10.1007/s11904-022-00636-8. https://europepmc.org/abstract/MED/36348185 .10.1007/s11904-022-00636-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Adverse Event Action Guide for VMMC by Surgery or Device, 2nd Edition, Updated December 2020. Clearinghouse on Male Circumcision for HIV Prevention. 2020. [2022-12-16]. https://www.malecircumcision.org/resource/adverse-event-action-guide-vmmc-surgery-or-device-2nd-edition-updated-december-2020-new .
- 49.Davis SM, Hines JZ, Habel M, Grund JM, Ridzon R, Baack B, Davitte J, Thomas A, Kiggundu V, Bock N, Pordell P, Cooney C, Zaidi I, Toledo C. Progress in voluntary medical male circumcision for HIV prevention supported by the US President's Emergency Plan for AIDS Relief through 2017: longitudinal and recent cross-sectional programme data. BMJ Open. 2018 Sep 01;8(8):e021835. doi: 10.1136/bmjopen-2018-021835. https://bmjopen.bmj.com/lookup/pmidlookup?view=long&pmid=30173159 .bmjopen-2018-021835 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Feldacker C, Murenje V, Holeman I, Xaba S, Makunike-Chikwinya B, Korir M, Gundidza PT, Holec M, Barnhart S, Tshimanga M. Reducing provider workload while preserving patient safety: a randomized control trial using 2-way texting for postoperative follow-up in Zimbabwe's voluntary medical male circumcision program. J Acquir Immune Defic Syndr. 2020 Jan 01;83(1):16–23. doi: 10.1097/QAI.0000000000002198. https://europepmc.org/abstract/MED/31809358 .00126334-202001010-00003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Marongwe P, Gonouya P, Madoda T, Murenje V, Tshimanga M, Balachandra S, Mandisarisa J, Sidile-Chitimbire V, Xaba S, Makunike-Chikwinya B, Holec M, Barnhart S, Feldacker C. Trust but verify: is there a role for active surveillance in monitoring adverse events in Zimbabwe's large-scale male circumcision program? PLoS One. 2019 Jun 10;14(6):e0218137. doi: 10.1371/journal.pone.0218137. https://dx.plos.org/10.1371/journal.pone.0218137 .PONE-D-19-07338 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Feldacker C, Murenje V, Barnhart S, Xaba S, Makunike-Chikwinya B, Holeman I, Tshimanga M. Reducing provider workload while preserving patient safety via a two-way texting intervention in Zimbabwe's voluntary medical male circumcision program: study protocol for an un-blinded, prospective, non-inferiority, randomized controlled trial. Trials. 2019 Jul 23;20(1):451. doi: 10.1186/s13063-019-3470-9. https://trialsjournal.biomedcentral.com/articles/10.1186/s13063-019-3470-9 .10.1186/s13063-019-3470-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Babigumira JB, Barnhart S, Mendelsohn JM, Murenje V, Tshimanga M, Mauhy C, Holeman I, Xaba S, Holec MM, Makunike-Chikwinya B, Feldacker C. Cost-effectiveness analysis of two-way texting for post-operative follow-up in Zimbabwe's voluntary medical male circumcision program. PLoS One. 2020;15(9):e0239915. doi: 10.1371/journal.pone.0239915. https://dx.plos.org/10.1371/journal.pone.0239915 .PONE-D-19-34591 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Feldacker C, Holeman I, Murenje V, Xaba S, Korir M, Wambua B, Makunike-Chikwinya B, Holec M, Barnhart S, Tshimanga M. Usability and acceptability of a two-way texting intervention for post-operative follow-up for voluntary medical male circumcision in Zimbabwe. PLoS One. 2020;15(6):e0233234. doi: 10.1371/journal.pone.0233234. https://dx.plos.org/10.1371/journal.pone.0233234 .PONE-D-19-27561 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Marongwe P, Wasunna B, Gavera J, Murenje V, Gwenzi F, Hove J, Mauhy C, Xaba S, Mugwanya R, Makunike-Chikwinya B, Munyaradzi T, Korir M, Oni F, Khaemba A, Barasa M, Holec M, Sidile-Chitimbire V, Tshimanga M, Holeman I, Barnhart S, Feldacker C. Transitioning a digital health innovation from research to routine practice: two-way texting for male circumcision follow-up in Zimbabwe. PLOS Digit Health. 2022 Jun 15;1(6):e0000066. doi: 10.1371/journal.pdig.0000066. https://europepmc.org/abstract/MED/36812548 .PDIG-D-22-00019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.South Africa Country Operational Plan (COP/ROP) 2020 Strategic Direction Summary. PEPFAR. 2020. Mar 5, [2022-12-16]. https://www.state.gov/wp-content/uploads/2020/07/COP-2020-South-Africa-SDS-FINAL.pdf .
- 57.Rech D, Spyrelis A, Frade S, Perry L, Farrell M, Fertziger R, Toledo C, Castor D, Njeuhmeli E, Loykissoonlal D, Bertrand JT. Implications of the fast-evolving scale-up of adult voluntary medical male circumcision for quality of services in South Africa. PLoS One. 2014;9(5):e80577. doi: 10.1371/journal.pone.0080577. https://dx.plos.org/10.1371/journal.pone.0080577 .PONE-D-13-36124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Anstey Watkins JO, Goudge J, Gómez-Olivé FX, Griffiths F. Mobile phone use among patients and health workers to enhance primary healthcare: a qualitative study in rural South Africa. Soc Sci Med. 2018 Feb;198:139–47. doi: 10.1016/j.socscimed.2018.01.011. https://linkinghub.elsevier.com/retrieve/pii/S0277-9536(18)30011-X .S0277-9536(18)30011-X [DOI] [PubMed] [Google Scholar]
- 59.Barron P, Pillay Y, Fernandes A, Sebidi J, Allen R. The MomConnect mHealth initiative in South Africa: early impact on the supply side of MCH services. J Public Health Policy. 2016 Nov;37(Suppl 2):201–12. doi: 10.1057/s41271-016-0015-2.10.1057/s41271-016-0015-2 [DOI] [PubMed] [Google Scholar]
- 60.Mehl GL, Tamrat T, Bhardwaj S, Blaschke S, Labrique A. Digital health vision: could MomConnect provide a pragmatic starting point for achieving universal health coverage in South Africa and elsewhere? BMJ Glob Health. 2018 Apr 24;3(Suppl 2):e000626. doi: 10.1136/bmjgh-2017-000626. https://gh.bmj.com/lookup/pmidlookup?view=long&pmid=29713512 .bmjgh-2017-000626 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Community Health Toolkit. 2022. [2023-03-22]. https://communityhealthtoolkit.org/
- 62.Global Goods Guidebook. Digital Square. [2022-12-16]. https://digitalsquare.org/resourcesrepository/global-goods-guidebook .
- 63.Karlyn A, Odindo S, Onyango R, Mbindyo C, Mberi T, Too G, Dalley J, Holeman I, Wasunna B. Testing mHealth solutions at the last mile: insights from a study of technology-assisted community health referrals in rural Kenya. Mhealth. 2020 Oct;6:43. doi: 10.21037/mhealth-19-261. https://europepmc.org/abstract/MED/33437839 .mh-06-19-261 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Augustin C, Holeman I, Salomon E, Olsen H, Azar P, Ayyangar M. Pathways to increasing trust in public health data. CHANCE. 2021 Sep 30;34(3):24–32. doi: 10.1080/09332480.2021.1979808. [DOI] [Google Scholar]
- 65.COVID-19 update: CHT-powered app supporting COVID-19 surveillance in Kenya. Medic. [2022-12-16]. https://medic.org/stories/covid-19-update-community-health-toolkit-cht-powered-app-supporting-covid-19-surveillance-in-kenya/
- 66.Yang JE, Lassala D, Liu JX, Whidden C, Holeman I, Keita Y, Djiguiba Y, N'Diaye SI, Fall F, Kayentao K, Johnson AD. Effect of mobile application user interface improvements on minimum expected home visit coverage by community health workers in Mali: a randomised controlled trial. BMJ Glob Health. 2021 Nov;6(11):e007205. doi: 10.1136/bmjgh-2021-007205. https://gh.bmj.com/lookup/pmidlookup?view=long&pmid=34815242 .bmjgh-2021-007205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Classification of digital health interventions v1:a shared language to describe the uses of digital technology for health. World Health Organization. [2019-10-01]. https://apps.who.int/iris/bitstream/handle/10665/260480/WHO-RHR-18.06-eng.pdf .
- 68.Holeman I, Kane D. Human-centered design for global health equity. Inf Technol Dev. 2019 Sep 29;26(3):477–505. doi: 10.1080/02681102.2019.1667289. https://europepmc.org/abstract/MED/32982007 .1667289 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Wasunna B, Holeman I. Training for Community Health: Bridging the Global Health Care Gap. Oxford, United Kingdom: Oxford University Press; 2021. 5 digital health interventions for community health worker training, ongoing education, and supportive supervision: insights from a human-centred design approach. [Google Scholar]
- 70.Principles for digital development. Digital Principles Homepage. [2022-08-01]. https://digitalprinciples.org/
- 71.RapidPro. UNICEF. [2022-12-16]. https://community.rapidpro.io/
- 72.Feldacker C, Bochner AF, Murenje V, Makunike-Chikwinya B, Holec M, Xaba S, Balachandra S, Mandisarisa J, Sidile-Chitimbire V, Barnhart S, Tshimanga M. Timing of adverse events among voluntary medical male circumcision clients: implications from routine service delivery in Zimbabwe. PLoS One. 2018 Sep 7;13(9):e0203292. doi: 10.1371/journal.pone.0203292. https://dx.plos.org/10.1371/journal.pone.0203292 .PONE-D-18-01630 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Stata Statistical Software: Release 17. College Station, TX: StataCorp; 2021. [Google Scholar]
- 74.SAS® software. SAS. 2013. [2023-03-17]. https://www.sas.com/en_us/legal/editorial-guidelines.html .
- 75.Holst C, Sukums F, Radovanovic D, Ngowi B, Noll J, Winkler AS. Sub-Saharan Africa—the new breeding ground for global digital health. Lancet Digital Health. 2020 Apr;2(4):e160–2. doi: 10.1016/s2589-7500(20)30027-3. [DOI] [PubMed] [Google Scholar]
- 76.Baniasadi T, Ghazisaeedi M, Hassaniazad M, Niakan Kalhori SR, Shahi M, Esmaeili M. Surgical patients follow-up by smartphone-based applications: a systematic literature review. Stud Health Technol Inform. 2020 Jun 23;271:85–92. doi: 10.3233/SHTI200079.SHTI200079 [DOI] [PubMed] [Google Scholar]
- 77.McMaster T, Wright T, Mori K, Stelmach W, To H. Current and future use of telemedicine in surgical clinics during and beyond COVID-19: a narrative review. Ann Med Surg (Lond) 2021 Jun;66:102378. doi: 10.1016/j.amsu.2021.102378. https://linkinghub.elsevier.com/retrieve/pii/S2049-0801(21)00328-9 .S2049-0801(21)00328-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Sandberg CE, Knight SR, Qureshi AU, Pathak S. Using telemedicine to diagnose surgical site infections in low- and middle-income countries: systematic review. JMIR Mhealth Uhealth. 2019 Aug 19;7(8):e13309. doi: 10.2196/13309. https://mhealth.jmir.org/2019/8/e13309/ v7i8e13309 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Day S, Ncube V, Maja L, Wasunna B, Pienaar J, Setswe G, Waweru E, Feldacker C. Centering frontline health care workers in digital innovation design: qualitative usability study to inform the optimization of an app for improved male circumcision follow-up in South Africa. JMIR Formative Res. 2023 Feb 5;:44122. doi: 10.2196/44122. (forthcoming) https://preprints.jmir.org/preprint/44122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Owoyemi A, Osuchukwu JI, Azubuike C, Ikpe RK, Nwachukwu BC, Akinde CB, Biokoro GW, Ajose AB, Nwokoma EI, Mfon NE, Benson TO, Ehimare A, Irowa-Omoregie D, Olaniran S. Digital solutions for community and primary health workers: lessons from implementations in Africa. Front Digit Health. 2022;4:876957. doi: 10.3389/fdgth.2022.876957. https://europepmc.org/abstract/MED/35754461 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.WHO guideline: recommendations on digital interventions for health system strengthening: web supplement 2 2019. World Health Organization. [2022-12-16]. https://apps.who.int/iris/bitstream/handle/10665/324998/WHO-RHR-19.7-eng.pdf . [PubMed]
- 82.Labrique AB, Wadhwani C, Williams KA, Lamptey P, Hesp C, Luk R, Aerts A. Best practices in scaling digital health in low and middle income countries. Global Health. 2018 Nov 03;14(1):103. doi: 10.1186/s12992-018-0424-z. https://globalizationandhealth.biomedcentral.com/articles/10.1186/s12992-018-0424-z .10.1186/s12992-018-0424-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Su Y, Mukora R, Ndebele F, Pienaar J, Khumalo C, Xu X, Tweya H, Sardini M, Day S, Sherr K, Setswe G, Feldacker C. Cost savings in male circumcision post-operative care continuum in rural and urban South Africa: evidence on the importance of initial counselling and daily SMS. medRxiv. 2023 Feb 11;:4877. doi: 10.1101/2023.02.08.23284877. doi: 10.1101/2023.02.08.23284877.2023.02.08.23284877 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Tchuenche M, Haté V, McPherson D, Palmer E, Thambinayagam A, Loykissoonlal D, Njeuhmeli E, Forsythe S. Estimating client out-of-pocket costs for accessing voluntary medical male circumcision in South Africa. PLoS One. 2016;11(10):e0164147. doi: 10.1371/journal.pone.0164147. https://dx.plos.org/10.1371/journal.pone.0164147 .PONE-D-16-12494 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Bakibinga-Gaswaga E, Bakibinga S, Bakibinga DB, Bakibinga P. Digital technologies in the COVID-19 responses in sub-Saharan Africa: policies, problems and promises. Pan Afr Med J. 2020;35(Suppl 2):38. doi: 10.11604/pamj.supp.2020.35.2.23456. https://europepmc.org/abstract/MED/33623563 .PAMJ-SUPP-35-2-38 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Chitungo I, Mhango M, Dzobo M, Denhere K, Chimene M, Musuka G, Dzinamarira T. Towards virtual doctor consultations: a call for the scale-up of telemedicine in sub-Saharan Africa during COVID-19 lockdowns and beyond. Smart Health (Amst) 2021 Jul;21:100207. doi: 10.1016/j.smhl.2021.100207. https://europepmc.org/abstract/MED/36570120 .S2352-6483(21)00029-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Chitungo I, Mhango M, Mbunge E, Dzobo M, Musuka G, Dzinamarira T. Utility of telemedicine in sub-Saharan Africa during the COVID-19 pandemic. A rapid review. Hum Behav Emerg Technol. 2021 Dec 02;3(5):843–53. doi: 10.1002/hbe2.297. https://europepmc.org/abstract/MED/34901772 .HBE2297 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.PEPFAR 2022 Country and Regional Operational Plan (COP/ROP) Guidance for all PEPFAR-Supported Countries. PEPFAR. [2022-05-23]. https://www.state.gov/wp-content/uploads/2022/02/COP22-Guidance-Final_508-Compliant-3.pdf .
- 89.Labrique A, Vasudevan L, Weiss W, Wilson K. Establishing standards to evaluate the impact of integrating digital health into health systems. Glob Health Sci Pract. 2018 Oct 10;6(Supplement 1):S5–17. doi: 10.9745/ghsp-d-18-00230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Agarwal S, Lefevre AE, Labrique AB. A call to digital health practitioners: new guidelines can help improve the quality of digital health evidence. JMIR Mhealth Uhealth. 2017 Oct 06;5(10):e136. doi: 10.2196/mhealth.6640. https://mhealth.jmir.org/2017/10/e136/ v5i10e136 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
CONSORT eHealth Checklist.
Data Availability Statement
The data sets generated in the randomized controlled trial and analyzed during this study, including demographics, SMS text messaging response rates, clinic visits, and adverse events, are available from the corresponding author upon reasonable request.


