Abstract
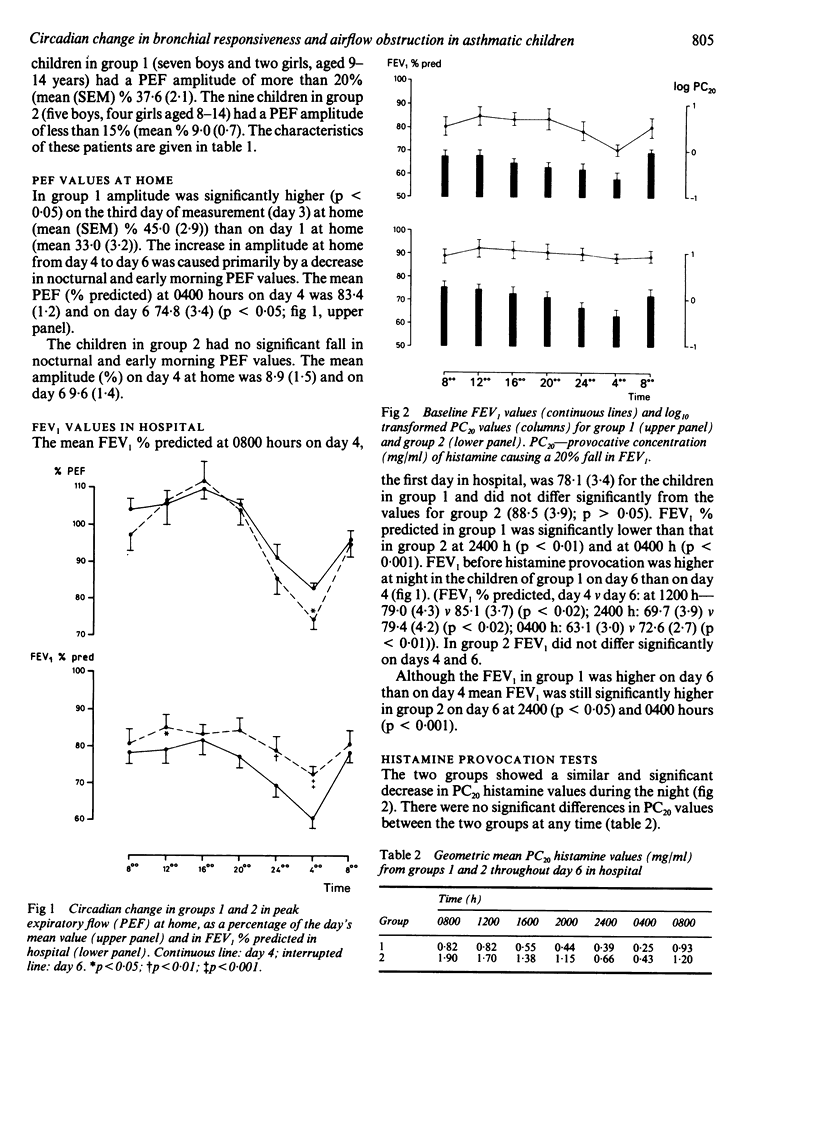
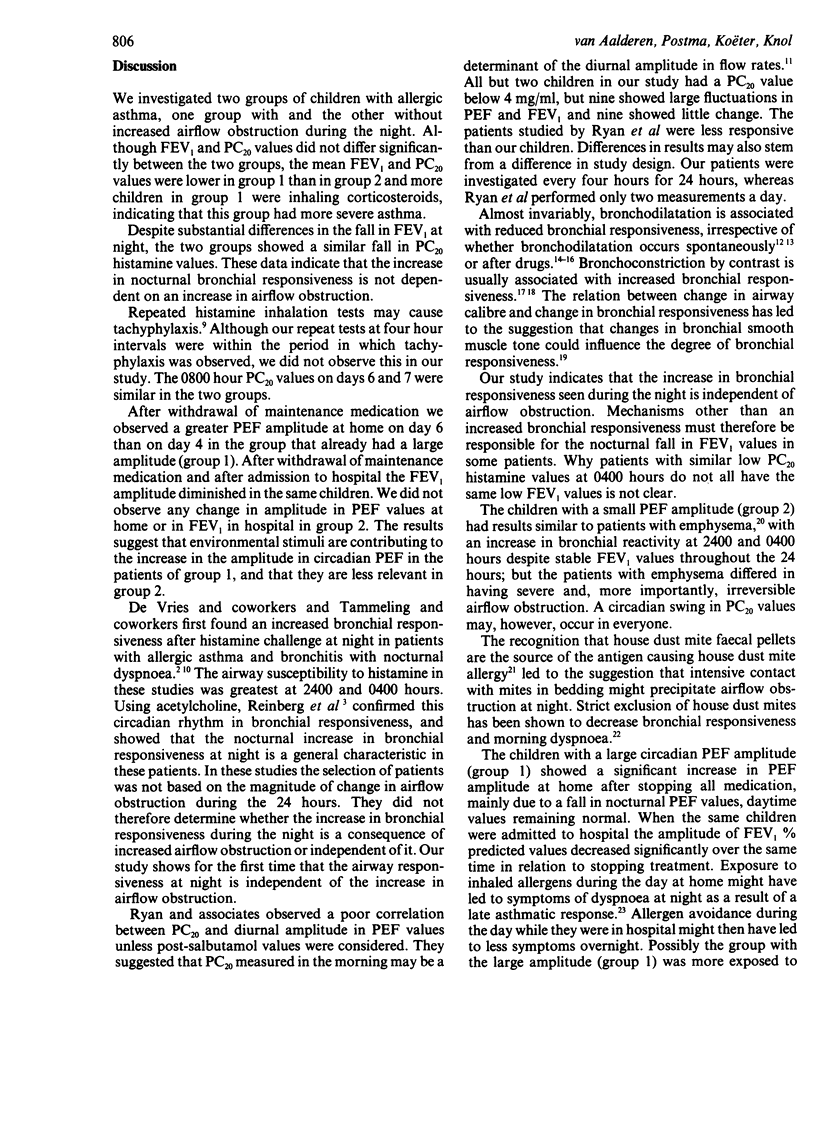
To throw light on the question of whether the increase in bronchial responsiveness seen during the night is due to increased airflow obstruction, nine asthmatic children with increased airflow obstruction at night (group 1) were compared with nine without (group 2). The mean fall in forced expiratory volume in one second (FEV1) between 16.00 and 04.00 hours was 21.9% in group 1 and 2.3% in group 2. Selection of patients was based on the amplitude of change in peak expiratory flow (PEF) measured every four hours for three consecutive days at home. The study was performed in hospital on four consecutive days. Medication was withheld for three days before and during the measurements at home and in hospital. On the first day in hospital (day 4) FEV1 was measured every four hours for 24 hours. On day 6 inhaled histamine provocation tests were performed at the same times as the FEV1 measurements on day 4. Both groups showed a nocturnal fall in the provocative dose of histamine causing a 20% fall in FEV1 (PC20). The mean change in histamine PC20 from 16.00 to 04.00 hours was 1.1 doubling doses of histamine in group 1 and 1.5 doubling doses in group 2. The results indicate that the increase in nocturnal bronchial responsiveness that occurs at night is not due to an increase in airflow obstruction.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Barnes P., FitzGerald G., Brown M., Dollery C. Nocturnal asthma and changes in circulating epinephrine, histamine, and cortisol. N Engl J Med. 1980 Jul 31;303(5):263–267. doi: 10.1056/NEJM198007313030506. [DOI] [PubMed] [Google Scholar]
- Benson M. K. Bronchial hyperreactivity. Br J Dis Chest. 1975 Oct;69(0):227–239. doi: 10.1016/0007-0971(75)90090-x. [DOI] [PubMed] [Google Scholar]
- Cockcroft D. W., Killian D. N., Mellon J. J., Hargreave F. E. Protective effect of drugs on histamine-induced asthma. Thorax. 1977 Aug;32(4):429–437. doi: 10.1136/thx.32.4.429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cockcroft D. W., Ruffin R. E., Dolovich J., Hargreave F. E. Allergen-induced increase in non-allergic bronchial reactivity. Clin Allergy. 1977 Nov;7(6):503–513. doi: 10.1111/j.1365-2222.1977.tb01481.x. [DOI] [PubMed] [Google Scholar]
- Connolly C. K. Diurnal rhythms in airway obstruction. Br J Dis Chest. 1979 Oct;73(4):357–366. [PubMed] [Google Scholar]
- Gerritsen J., Koëter G. H., Akkerboom H. J., Knol K. Recovery of FEV1 after histamine challenge in asthmatic children. Clin Allergy. 1987 Mar;17(2):119–126. doi: 10.1111/j.1365-2222.1987.tb02329.x. [DOI] [PubMed] [Google Scholar]
- Hartley J. P., Nogrady S. G. Effect of an inhaled antihistamine on exercise-induced asthma. Thorax. 1980 Sep;35(9):675–679. doi: 10.1136/thx.35.9.675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Juniper E. F., Syty-Golda M., Hargreave F. E. Histamine inhalation tests: inhalation of aerosol via a facemask versus a valve box with mouthpiece. Thorax. 1984 Jul;39(7):556–557. doi: 10.1136/thx.39.7.556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manning P. J., Jones G. L., O'Byrne P. M. Tachyphylaxis to inhaled histamine in asthmatic subjects. J Appl Physiol (1985) 1987 Oct;63(4):1572–1577. doi: 10.1152/jappl.1987.63.4.1572. [DOI] [PubMed] [Google Scholar]
- Orehek J., Gayrard P. Les tests de provocation bronchique non-spécifiques dans l'asthme. Bull Eur Physiopathol Respir. 1976 Jul-Aug;12(4):565–598. [PubMed] [Google Scholar]
- Orehek J., Massari J. P., Gayrard P., Grimaud C., Charpin J. Effect of short-term, low-level nitrogen dioxide exposure on bronchial sensitivity of asthmatic patients. J Clin Invest. 1976 Feb;57(2):301–307. doi: 10.1172/JCI108281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Platts-Mills T. A., Tovey E. R., Mitchell E. B., Moszoro H., Nock P., Wilkins S. R. Reduction of bronchial hyperreactivity during prolonged allergen avoidance. Lancet. 1982 Sep 25;2(8300):675–678. doi: 10.1016/s0140-6736(82)90709-7. [DOI] [PubMed] [Google Scholar]
- Postma D. S., Koëter G. H., vd Mark T. W., Reig R. P., Sluiter H. J. The effects of oral slow-release terbutaline on the circadian variation in spirometry and arterial blood gas levels in patients with chronic airflow obstruction. Chest. 1985 May;87(5):653–657. doi: 10.1378/chest.87.5.653. [DOI] [PubMed] [Google Scholar]
- Reinberg A., Gervais P., Morin M., Abulker C. Rythme circadien humain du seuil de la réponse bronchique à l'acétylcholine. C R Acad Sci Hebd Seances Acad Sci D. 1971 Apr 5;272(14):1879–1881. [PubMed] [Google Scholar]
- Ryan G., Latimer K. M., Dolovich J., Hargreave F. E. Bronchial responsiveness to histamine: relationship to diurnal variation of peak flow rate, improvement after bronchodilator, and airway calibre. Thorax. 1982 Jun;37(6):423–429. doi: 10.1136/thx.37.6.423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sterk P. J., Plomp A., Crobach M. J., van de Vate J. F., Quanjer P. H. The physical properties of a jet-nebulizer and their relevance for the histamine provocation test. Bull Eur Physiopathol Respir. 1983 Jan-Feb;19(1):27–36. [PubMed] [Google Scholar]
- Taylor A. J., Davies R. J., Hendrick D. J., Pepys J. Recurrent nocturnal asthmatic reactions to bronchial provocation tests. Clin Allergy. 1979 May;9(3):213–219. doi: 10.1111/j.1365-2222.1979.tb01544.x. [DOI] [PubMed] [Google Scholar]
- de VRIES, GOEI J. T., BOOY-NOORD H., ORIE N. G. Changes during 24 hours in the lung function and histamine hyperreactivity of the bronchial tree in asthmatic and bronchitic patients. Int Arch Allergy Appl Immunol. 1962;20:93–101. doi: 10.1159/000229248. [DOI] [PubMed] [Google Scholar]


