Abstract
Digital psychological interventions have been widely used clinically in recent years, but the methodological quality and quality of evidence of related studies are unclear, thus interfering with the translation of practice outcomes and the application of clinical decisions. We searched for meta-analyses of randomized controlled trials in the PubMed, Web of Science, Embase, Cochrane Library, JBI Database, CINAHL, and PsycINFO databases as well as some databases containing gray literature up to 27 April 2022 using a combination of keywords. After two researchers independently screened and extracted data from the literature, the methodological quality of the included literature was evaluated by the AMSTAR 2 scale, and the evidence quality of the outcome index was graded by the Grading of Recommendations, Assessment, Development, and Evaluation system. A total of 12 meta-analyses reporting the positive impact of digital psychological interventions in the prevention and/or treatment of depressive symptoms in perinatal women were included, but the methodological quality and evidence level of the included studies were low. Digital psychological interventions are effective in reducing perinatal depression, but the methodological quality and reliability of outcome indicators are mostly low. Improving study designs, using higher-quality clinical evidence, conducting systematic evaluation studies strictly following the procedures, and standardizing the reporting of study results are recommended.
Keywords: Perinatal depression, Digital, Psychological interventions, Systematic review, Meta-analysis
Introduction
The World Health Organization (WHO) reports that approximately 140 million women worldwide give birth each year (World Health Organization 2018). During pregnancy, childbirth, and lactation, women undergo tremendous physical, psychological, social, familial, and role changes, and these changes may affect psychological and physical resources, leading to an increased susceptibility to psychological problems, such as major depressive disorder (MDD), anxiety disorders, and psychotic disorders (Howard and Khalifeh 2020; van Ravesteyn et al. 2017). Perinatal depression (PND) refers to depressive episodes of different degrees occurring from pregnancy to 12 months after delivery, including prenatal and postnatal depression, which mainly manifests as depressed mood, sadness, agitation, and irritability. In severe cases, psychotic symptoms such as hallucinations or suicidal thoughts may occur (Simas et al. 2018). The incidence of perinatal depression ranges from 5 to 38.8% (Lara et al. 2014; Silveira et al. 2015; Huang et al. 2019), the incidence of perinatal depression is as high as 40% in high-risk women (e.g., family history of depression, major life events, or socioeconomically disadvantaged groups) (Parameswaran et al. 2022), and the recurrence rate of postpartum depression is as high as 30–50% in women with a second pregnancy and delivery (Josefsson et al. 2002).
The harms of perinatal depression are multifaceted; it affects not only maternal quality of life, marital relationships, and social functioning status (Wonch et al. 2016) but also pregnancy outcomes (e.g., preterm birth, low birth weight) (Jarde et al. 2016); the emotional, intellectual, cognitive, and behavioral development of infants and children (Herba et al. 2016; Hannigan et al. 2018; Duan et al. 2019); and in severe cases, even suicidal or infanticidal behavior (Khalifeh et al. 2016). In addition, the children of women with perinatal depression also suffer from depression in childhood to adulthood that is more difficult to treat, has a longer duration, and can even last for multiple generations, which is known as intergenerational transmission (Grundwald and Brunton 2015; Bowers and Yehuda 2016).
Perinatal depression has a high incidence and is harmful, and effective interventions are the key to reducing perinatal depression. Studies have shown that pharmacotherapy is only indicated for moderate to severe illness, whereas behavioral interventions are recommended for the initial treatment of mild to moderate depression (Ladyman et al. 2022). Generally, non-pharmacological treatments to reduce depression, such as psychological interventions, are preferred by those who are pregnant (Zhang et al. 2021), possibly due to the adverse effects of antidepressants, which impact the gastrointestinal, cardiovascular, and central nervous systems (Lei et al. 2019). These adverse effects may affect patient tolerance and compliance, and antidepressant exposure during pregnancy is associated with adverse pregnancy outcomes and offspring development (Rommel et al. 2020, 2022). Psychological intervention is a planned and step-by-step process guided by psychological theories to influence the mental activities, personality characteristics, or psychological problems of certain subjects so that patients progress toward the desired goal. Psychological interventions are performed in a variety of ways (e.g., cognitive behavioral therapy (CBT), interpersonal therapy (IPT), mindfulness intervention, behavioral activation (BA), and psychological education intervention) (Martín-Gómez et al. 2020). Studies have shown that psychological interventions have a positive impact on perinatal depression (Dolan et al. 2022; Sockol 2018), but previous psychological interventions were mostly face-to-face (individual or group) (Sangsawang et al. 2019), and some women were unable to access psychotherapy due to temporal and financial barriers, stigma, and self-stigma (Cacciola and Psouni 2020). With the rapid development of networked information technology, digital health is revolutionizing the delivery of medical services and has rapidly become an important tool for providing care during the COVID-19 pandemic (Meyer 2020). Digital psychological interventions are being increasingly examined.
Psychological interventions are considered digital when they are delivered by methods, including the internet, computers, mobile phones or tablets, and short message services (SMSs) (Fu et al. 2020). Digital psychological interventions (a) overcome spatial and temporal constraints and increase access and convenience (Brearly et al. 2017), (b) improve the connectivity and flexibility of psychological interventions (Gordon et al. 2016), (c) reduce personnel costs (Osborne et al. 2019), and (d) benefit individuals who are reluctant to seek help due to the stigma of mental illness (Mannarini and Rossi 2018). Studies have shown that digital psychological interventions can significantly reduce the degree of depression in affected individuals (Gilbody et al. 2017).
Several meta-analyses have examined the efficacy of digital psychological interventions in reducing perinatal depressive symptoms, and these meta-analyses varied in terms of purpose, type of intervention, and study quality, hindering overall findings. A systematic re-evaluation is a new approach to synthesizing high-quality evidence based on the same or similar interventions, which supports summing up treatment effects in a broader context (Smith et al. 2011) and can provide useful and up-to-date evidence for practitioners and clinicians. Currently, there are no systematic reviews of meta-analyses and/or systematic reviews on the effectiveness of digital psychological interventions to reduce perinatal depression. Therefore, we aimed to (a) comprehensively evaluate the meta-analyses on the effects of digital psychological interventions on perinatal depression and (b) synthesize results from past meta-analyses to guide health policies and research.
Methods
Protocol and registration
This systematic review was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (Page et al. 2021). The study protocol was registered in the PROSPERO database (CRD42022356820).
Eligibility criteria
Studies were selected for review if they fulfilled the following criteria:
Population: women aged ≥ 18 years in the perinatal period (during pregnancy and the first 12 months postpartum);
Intervention: Intervention conditions must include at least one digital psychological intervention group (e.g., ICBT or IPT);
Comparison: any comparison condition (e.g., active control, usual care, or waitlist);
Outcomes: perinatal depression (from pregnancy to the first 12 months postpartum);
Study design: meta-analyses of the effectiveness of digital psychological interventions in reducing perinatal depression.
Studies were excluded for the following reasons: (a) non-English literature, (b) full text was not available, (c) data reporting was incomplete, (d) research content was the development or feasibility evaluation of the telemedicine system, and (e) others (e.g., primary outcome indicator is not depression, non-psychological interventions, conference abstracts).
Search procedures and information sources
A systematic search of electronic databases (PubMed, Web of Science, Embase, Cochrane Library, JBI Database, CINAHL, PsycINFO, and some databases containing gray literature) was conducted from the inception of the databases until April 27, 2022. The database search was conducted independently by two authors (CC and XW).
The search terms and strategy were as follows: [(postpartum) OR (postnatal) OR (puerper*) OR (pregnan*) OR (antenatal) OR (antepartum) OR (prenatal) OR (perinatal) OR (peripartum) OR (maternal*)] AND [(depress*) OR (“mental health”) OR (“mental disorder*”) OR (“depressive disorder*”)] AND [(m-health) OR (mhealth) OR (e-health) OR (ehealth) OR (telehealth) OR (telemedicine) OR (teleconsultation) OR (“information service”) OR (telephone) OR (“cell phone”) OR (“mobile phone”) OR (“mobile application”) OR (“mobile health”) OR (“text messaging”) OR (telemonitoring) OR (“social media”) OR (“reminder system”) OR (computer*) OR (online) OR (internet) OR (web-based) OR (technolog*)] AND [(“meta-analysis”) OR (“meta synthesis”) OR (“systematic review”)]. In addition, the references of the included literature were traced to supplement the acquisition of relevant literature.
The search results were imported to EndNote X9.3.3, and duplicates were deleted. Two authors (CC and XW) independently screened the titles and abstracts according to the inclusion and exclusion criteria; then, potentially eligible articles were screened by full-text reading. Reasons for excluding papers in the full-text screening stage were recorded. Each article was cross-checked after completion, and any disagreements were discussed and resolved or referred to a third author (HX).
Data extraction
Data extraction from the included articles was completed independently by two authors (CC and XW) using a data extraction form. Extracted data included the first author, year of publication, country, aims, type and number of included studies, sample size, intervention description, depression measurement, main findings, funding sources, and risk of bias assessment. If the literature data were missing or could not be extracted, the original author was contacted to obtain the data. Any discrepancies in this process were discussed and resolved with the third author (HX).
Quality assessment
The methodological quality and quality of evidence were evaluated independently by two authors (CC and XW) for each meta-analysis included, with a third author (HX) joining to resolve any disagreements.
Methodological quality
Evaluation was performed using the AMSTAR 2 assessment tool, which was adapted for both randomized and non-randomized studies of healthcare interventions and provided a more comprehensive assessment of methodological quality (Shea et al. 2017).
Quality of evidence
With perinatal depression as the evidence body, the Grading of Recommendations, Assessment, Development, and Evaluation (GRADE) system was used for evaluation (Guyatt et al. 2008). The certainty of the evidence could increase or decrease for several reasons: certainty could be rated lower due to the risk of bias, imprecision, inconsistency, indirectness, or publication bias; certainty could be rated higher for a large magnitude of effect and dose‒response gradient, and all residual confounders would decrease the magnitude of effect (in situations with an effect).
Results
Study selection
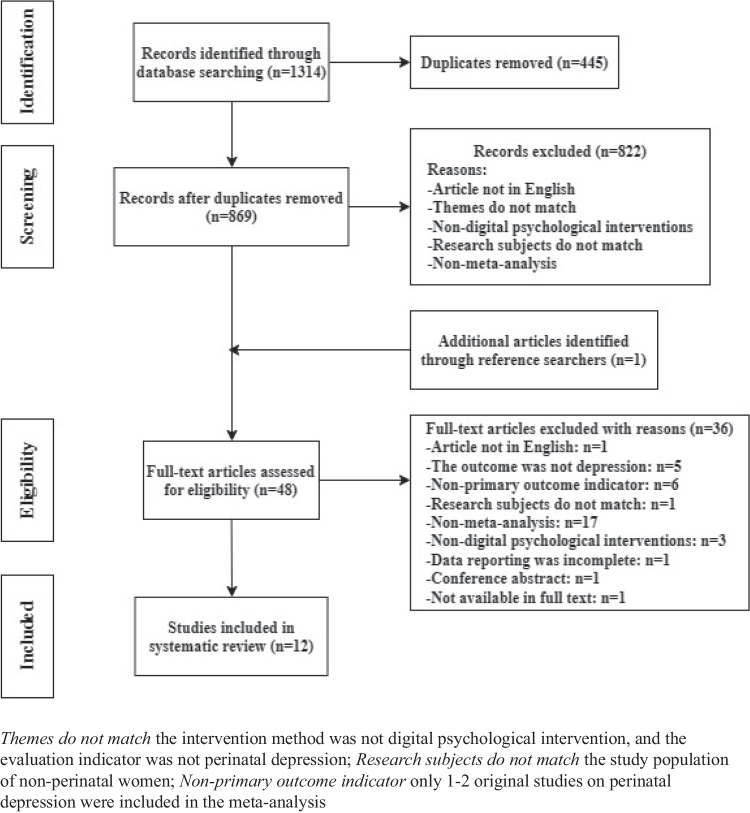
According to the search strategy, a total of 1314 articles were retrieved, and 869 articles remained after removing duplicates. Forty-seven articles were screened after reading the titles and abstracts, and 1 additional article was included after screening the references. A total of 48 papers were rescreened after reading the full text in detail, and 36 papers were excluded. Finally, 12 articles were included in the systematic review of meta-analyses. The literature screening process and results are shown in Fig. 1.
Fig. 1.
Study selection flow diagram
Study characteristics
Table 1 presents a summary of the included meta-analyses following the PICO search strategy. All of the studies were conducted between 2017 and 2022; the number of included original studies ranged from 5 to 19 articles; the sample size of one study was not reported completely, and the remaining studies ranged from 567 to 2277. Of the 12 meta-analyses, 7 reviews examined the treatment of perinatal depression, and 5 reviews examined both the prevention and treatment of perinatal depression (Chae and Kim 2021; Nair et al. 2018; Neo et al. 2022; Lau et al. 2020, 2022). Among the 12 meta-analyses, 11 were conducted with article quality evaluation and a description of the quality evaluation tool, and 1 study (Roman et al. 2019) did not mention whether quality evaluation was performed. The quality evaluation tools for each of the 11 articles were as follows: 7 studies (Lau et al. 2017, 2020, 2022; Liu et al. 2022; Loughnan et al. 2019; Neo et al. 2022; Zhao et al. 2021) used the Cochrane Risk of Bias tool (Higgins et al. 2011), 1 study (Chae and Kim 2021) used the Cochrane Risk of Bias 2.0 (Sterne et al. 2019), 2 studies (Nair et al. 2018; Dol et al. 2020) used the JBI (Lockwood et al. 2015), and 1 study (Mu et al. 2021) used the Jadad scale (Jadad et al. 1996). GRADE (Guyatt et al. 2008) was used to evaluate the evidence quality of four articles (Dol et al. 2020; Lau et al. 2020, 2022; Neo et al. 2022). Almost all the included papers, except for three (Liu et al. 2022; Nair et al. 2018; Roman et al. 2019), were supported by grants.
Table 1.
Characteristics of the included systematic reviews
| First author (year of publication) | Country | Aims | Type and number of included studies/total number of participants | Type of research of included studies | Intervention characteristics: (a) type (e.g., CBT, IBA), (b) delivery format (e.g., app, telephone, Web), (c) range of the number of sessions (mean), (d) range of duration of treatments (mean), (e) time of intervention (pregnancy, postpartum or both), and (f) follow-up | Outcome measures | Main findings | Funding sources | Risk of bias assessment |
|---|---|---|---|---|---|---|---|---|---|
| Dol et al. (2020) | Canada | To evaluate the effectiveness of mother-targeted mobile health (mHealth) education interventions during the perinatal period on maternal psychosocial outcomes in high-income countries | N = 5*/195 (full report not available) (5 quasi-experimental; the single asterisk indicates that a total of 21 studies were included in the review, but we only report the data from the studies focused on perinatal depression and psychological intervention) | Treatment (n = 5) |
a. Peer support (n = 2), peer support + mindfulness therapy (n = 1), CBT (n = 1), PST + IPT (n = 1) b. Telephone (n = 1), app (n = 3), SMS (n = 1) c. Not reported d. 3 to 12 weeks e. Postnatal (n = 3), antenatal and postnatal (n = 1), and not reported (n = 1) f. Not reported |
EPDS (n = 4), PHQ-9 (n = 1) | Mothers who received an mHealth intervention targeting postpartum depression showed a decreased score on the Edinburgh Postnatal Depression Scale at postintervention (OR = − 6.01; 95% CI: − 8.34 to − 3.67; p < 0.00001) | Doctoral Award (FRN154341) and Canadian Child Health Clinician Scientist Program Career Development and Canadian Institute of Health Research New Investigator | JBI/GRADE |
| Chae and Kim (2021) | South Korea | This study investigated the effect of internet-based prenatal interventions among pregnant women | N = 6*/1834 (6 = RCTs; the single asterisk indicates that a total of 9 studies were included in the review, but we only report the data from the studies focused on perinatal depression) | Prevention (n = 3) + treatment (n = 3) |
a. CBT (n = 3), metacognitive therapy and positive psychology (n = 1), PST (n = 1), psychoeducation (n = 1) b. Website + e-mail (n = 2), website (n = 1), website + e-mail + telephone (n = 1), website + e-mail + telephone + SMS (n = 1), app + telephone (n = 1) c. 2 to 16 sessions d. 2 to 24 weeks e. Antenatal (n = 4), antenatal and postnatal (n = 2) f. After intervention to 6 months |
EPDS (n = 5), CES-D (n = 1), PHQ-9 (n = 2), HDRS (n = 1), IDAS (n = 1), MADRS-S (n = 1), WSAS (n = 1)—some articles applied multiple scales | Meta-analysis of standardized mean differences showed that 6 studies had an effect on postpartum depression, with an effect size of − 0.16 (95% CI: − 0.26 to − 0.05) | NRF grant (2020R1F1A1048449) | Cochrane Risk of Bias 2.0 |
| Loughnan et al. (2019) | Australia | To analyze the effectiveness and acceptability of internet-based intervention for depression and anxiety in perinatal women | N = 6*/567 (5 RCTs + 1 open uncontrolled pilot study; the single asterisk indicates that a total of 7 studies were included in the review, but we only report the data from the studies focused on perinatal depression) | Treatment (n = 6) |
a. CBT (n = 4), BA (n = 2) b. Telephone (n = 3), website (n = 2), e-mail (n = 1) c. 6 to 12 sessions d. 6 to 15 weeks e. Postnatal (n = 4), antenatal (n = 2) f. Not reported |
EPDS (n = 4), BDI-II (n = 1), MADRS-S (n = 1), PHQ-9 (n = 1)—some articles applied 2 scales | Preliminary findings indicate large improvements in depression (Hedges g = 1.67; 95% CI: 1.38 to 1.96). However, between-group differences between interventions and control conditions were only moderate for depression (Hedges g = 0.60; 95% CI: 0.43 to 0.78) | PhD scholarship and NHMRC grant (1,145,382) | Cochrane Risk of Bias tool |
| Nair et al. (2018) | Australia | To assess the extent to which telemedicine may be an effective way to provide services to sufferers of maternal depression | N = 10/1138 (10 RCTs) | Prevention (n = 2) + treatment (n = 8) |
a. CBT (n = 6), BA (n = 2), psychoeducation (n = 1), mood tracking (n = 1) b. Website (n = 8), app (n = 2) c. Not reported d. 2 to 17 weeks e. Postnatal (n = 6), perinatal (n = 2), antenatal (n = 2) f. 4 weeks to 12 months, not reported from all studies |
EPDS (n = 5), BDI-II (n = 2), WSAS (n = 2), PHQ-9 (n = 1), PHQ-4 (n = 1), CES-D (n = 1), MADRS-S (n = 1)—some articles applied multiple scales | We found that interventions delivered via telemedicine have been shown to effectively alleviate MD symptoms, improving treatment efficacy | No external funding | JBI |
| Roman et al. (2019) | Romania | To identify, synthesize, and analyze the empiric studies regarding the online cognitive behavioral therapy effectiveness for postpartum depression | N = 6/635 (6 RCTs) | Treatment (n = 6) |
a. CBT (n = 6) b. Website (n = 4), website + telephone (n = 2) c. 6 to 12 sessions d. Not reported e. Postnatal (n = 6) f. 10 weeks to 16 months |
EPDS | Online guided cognitive behavioral therapy can be recommended for postpartum depression as an alternative or adjunct to psychotherapy (d = − 0.54; 95% CI: − 0.716 to − 0.423) | Not mentioned | Not mentioned |
| Lau et al. (2017) | Singapore | To evaluate the efficacy of therapist-supported ICBT in improving stress, anxiety, and depressive symptoms among postpartum women | N = 8/1523 (8 RCTs) | Treatment (n = 8) |
a. CBT (n = 8) b. Website (n = 3), website + telephone (n = 2), website + telephone + e-mail (n = 2), telephone + e-mail (n = 1) c. 6 to 12 sessions d. 5 to 17 weeks e. Postnatal (n = 8) f. Not reported |
EPDS (n = 3), BDI-II (n = 3), BSI-GSI (n = 2) | Therapist-supported ICBT significantly improved depressive symptoms (d = − 0.63; 95% CI: − 0.77 to − 0.50) of the intervention group compared with those of the control group at postintervention | NUHSRO/2013/147/SU/01 grant (R545-000–055-133 and R545-000–055-750) and HSS Seed Fund | Cochrane Risk of Bias tool |
| Neo et al. (2022) | Singapore | To investigate the effectiveness of internet-based psychological intervention in reducing depressive, anxiety, and stress symptoms and fear of childbirth among pregnant women at postintervention and follow-up | N = 12*/2162 (12 RCTs; the single asterisk indicates that a total of 16 studies were included in the review, but we only report the data from the studies focused on perinatal depression | Prevention (n = 7) + treatment (n = 5) |
a. CBT (n = 5), mindfulness therapy (n = 2), metacognitive therapy and positive psychology (n = 1), PST (n = 1), psychoeducation (n = 1), mindfulness behavioral cognitive therapy (n = 1), mindfulness-based stress reduction therapy (n = 1) b. Website (n = 9), app (n = 3) c. 3 to 44 sessions d. 3 to 46 weeks e. Antenatal (n = 11), antenatal and postnatal (n = 1) f. 4 to 18 weeks, not reported from all studies |
EPDS (n = 10), PHQ-9 (n = 2) | Internet-delivered psychological interventions were found to significantly reduce depressive symptoms (g = − 0.32; 95% CI: − 0.53 to − 0.11; p < 0.05) | AcRF grant (NUHSRO/2017/054/T1) | Cochrane Risk of Bias tool/GRADE |
| Liu et al. (2022) | China | To evaluate the effectiveness of telemedicine intervention in women with postpartum depression | N = 7*/1338 (7 RCTs; the single asterisk indicates that a total of 20 studies were included in the review, but we only report the data from the studies that focused on psychological intervention and performed meta-analysis) | Treatment (n = 7) |
a. CBT (n = 5), BA (n = 2) b. Internet (n = 4), website (n = 1), app (n = 1), online (n = 1) c. Not reported d. Not reported e. Postnatal (n = 7) f. 4 to 17 weeks |
EPDS (n = 4), BDI-II (n = 2), PHQ-9 (n = 1) | The results of the meta-analysis revealed that internet-based CBT was found to have a significant effect on PPD (SMD = − 1.62; 95% CI: − 2.42 to − 0.80; p < 0.00001) and internet-based behavioral activation did not have a significant effect on PPD (SMD = − 0.55; 95% CI: − 0.68 to − 0.43; p = 0.67) | Not mentioned | Cochrane Risk of Bias tool |
| Lau et al. (2022) | Singapore | To evaluate the effectiveness of digital CBT on psychological symptoms (depression, anxiety, and stress symptoms) | N = 15*/1455 (15 RCTs; the single asterisk indicates that a total of 18 studies were included in the review, but we only report the data from the studies focused on perinatal depression) | Prevention (n = 6) + treatment (n = 9) |
a. CBT (n = 12), BA (n = 3) b. Website (n = 5), website + e-mail (n = 3), app (n = 2), website + e-mail + telephone (n = 2), website + e-mail + telephone + SMS (n = 2), website/app (n = 1) c. 3 to 16 sessions d. 4 to 15 weeks e. Postnatal (n = 9), antenatal (n = 6) f. 4 weeks to 12 months, not reported from all studies |
EPDS (n = 9), PHQ-8 (n = 1), PHQ-9 (n = 1), BDI-II (n = 1), GSI-D (n = 2), DASS-21-D (n = 1) | Digital CBT significantly reduced depression (g = − 0.56, 95% CI: − 0.85 to − 0.27, p < 0.001) compared with the control group. The perinatal women were gradual responders who may have needed up to 8 sessions and exposure to more than 6 weeks to attain significant improvement in depression symptoms | AcRF grant (NUHSRO/2017/054/T1) | Cochrane Risk of Bias tool/GRADE |
| Zhao et al. (2021) | China | To evaluate the effectiveness of telehealth interventions in reducing depressive symptoms and anxiety in women with PPD | N = 9/1958 (9 RCTs) | Treatment (n = 9) |
a. Peer support (n = 3), CBT + BA (n = 5), interpersonal therapy (n = 1) b. Telephone (n = 4), website (n = 2), app (n = 1), telephone + app (n = 1), telephone + website (n = 1) c. Not reported d. Not reported e. Postnatal (n = 9) f. 4 to 36 weeks |
EPDS (n = 9) | The EPDS (MD = − 2.99, 95% CI: − 4.52 to − 1.46; p < 0.001) scores were significantly lower in the telehealth group than in the control group | Grant numbers: FDN-148438, LC2019ZD019, YNKT201802, and Z2019001 | Cochrane Risk of Bias tool |
| Mu et al. (2021) | China | To determine the efficacy of internet-based interventions in decreasing the prevalence of postpartum depression in perinatal women | N = 7/2277 (7 RCTs) | Treatment (n = 7) |
a. CBT (n = 5), BA (n = 2) b.Website (n = 7) c. Not reported d. Not reported e. Not reported f. 10 weeks to 6 months |
EPDS (n = 3), BDI-II (n = 2), CES-D (n = 1), MADRS-S (n = 1) | Internet-based interventions significantly improved postpartum depression (d = 0.642, 95% CI: 0.508 to 0.813) | Grant numbers: kj2017a191 and 2020zryb06 | Jadad scale |
| Lau et al. (2020) | Singapore | To evaluate the effectiveness of digital psychotherapeutic intervention on improving psychological outcomes among perinatal women and identify its essential features | N = 19*/1736 (19 RCTs; the single asterisk indicates that a total of 25 studies were included in the review, but we only report the data from the studies focused on perinatal depression) | Prevention (n = 9) + treatment (n = 10) |
a.CBT (n = 6), CBT + BA (n = 3), psychoeducation (n = 3), CBT + psychoeducation (n = 1), CBT + problem-solving component (n = 1), PST + psychoeducation (n = 1), CBT + problem-solving component + psychoeducation (n = 1), mindfulness therapy (n = 1), stress reduction therapy (n = 1), mindfulness therapy + stress reduction component (n = 1) b.Website (n = 7), website + e-mail (n = 3), website + e-mail + telephone (n = 5), website + e-mail + telephone + SMS (n = 1), website + SMS (n = 1), app (n = 1), app + telephone (n = 1) c. 3 to 16 sessions, not reported from all studies d. 3 to 15 weeks, not reported from all studies e. Antenatal (n = 8), postnatal (n = 11) f. 4 weeks to 12 months, not reported from all studies |
EPDS (n = 10), BDI-II (n = 3), GSI-D (n = 2), PHQ-8 (n = 1), PHQ-9 (n = 2), HDRS (n = 1), MADRS-S (n = 1), CES-D (n = 1), HADS-D (n = 1), DASS-21-D (n = 1)—some articles applied 2 scales | Meta-analysis results revealed that digital psychotherapeutic intervention had a medium-sized effect (g = 0.49) on alleviating depression symptoms (Z = − 3.75, p < 0.001) compared with the control | AcRF grant (NUHSRO/2017/054/T1) | Cochrane Risk of Bias tool/GRADE |
RCT randomized control trial; app application; PST problem-solving therapy; EPDS Edinburgh Postnatal Depression Scale; BDI-II Beck Depression Inventory II; DASS-21-D Depression, Anxiety and Stress Scale 21-Depression Subscale; CES-D Center for Epidemiologic Scale-Depression Scale; PHQ-9 Patient Health Questionnaire-9; HDRS Hamilton Depression Rating Scale; IDAS Inventory of Depression Rating Scale; MADRS-S Montgomery-Åsberg Depression Rating Scale-Self-Report; WSAS Work and Social Adjustment Scale-depression/pregnancy version; PHQ-4 Patient Health Questionnaire-4; BSI-GSI Brief Symptom Inventory-Global Severity Index; GSI-D Global Severity Index-Depression subscale; PHQ-8 Patient Health Questionnaire-8; HADS-D Hospital Anxiety and Depression Scale-Depression Subscale; ICBT internet-based cognitive behavioral therapy; AcRF Academic Research Fund
Characteristics of digital psychological interventions
Regarding digital psychological interventions, the studies included a variety of interventions: 7 reviews included BA (Nair et al. 2018; Loughnan et al. 2019; Lau et al. 2020, 2022; Mu et al. 2021; Zhao et al. 2021; Liu et al. 2022), 4 reviews included psychoeducation (Nair et al. 2018; Lau et al. 2020; Chae and Kim 2021; Neo et al. 2022), 4 reviews included problem-solving therapy (Dol et al. 2020; Chae and Kim 2021; Lau et al. 2022; Neo et al. 2022), and all studies included CBT. In addition, interventions such as peer support (Dol et al. 2020; Zhao et al. 2021), mindfulness therapy (Dol et al. 2020; Lau et al. 2020; Neo et al. 2022), mood tracking (Nair et al. 2018), metacognitive therapy and positive psychology (Chae and Kim 2021; Neo et al. 2022), and stress reduction therapy (Lau et al. 2020) have also been described. The studies included different types of intervention delivery formats, with 8 reviews being telephone-based (Chae and Kim 2021; Dol et al. 2020; Lau et al. 2017, 2020, 2022; Loughnan et al. 2019; Roman et al. 2019; Zhao et al. 2021) and 8 reviews being app-based (Nair et al. 2018; Dol et al. 2020; Lau et al. 2020, 2022; Chae and Kim 2021; Zhao et al. 2021; Liu et al. 2022; Neo et al. 2022), and all but 1 review (Dol et al. 2020) reported on the effectiveness of website-based psychological interventions. Of the 12 meta-analyses, five reviews did not report the number of sessions (Nair et al. 2018; Dol et al. 2020; Mu et al. 2021; Zhao et al. 2021; Liu et al. 2022), and seven articles reported the number of sessions to be between 2 and 44 sessions. Among the 7 studies, two had between 3 and 16 sessions (Lau et al. 2020, 2022), and three had between 6 and 12 sessions (Lau et al. 2017; Loughnan et al. 2019; Roman et al. 2019). Regarding the duration of treatment, 4 articles did not report this information (Roman et al. 2019; Mu et al. 2021; Zhao et al. 2021; Liu et al. 2022), and 8 articles reported that the treatment duration was between 2 and 46 weeks. The duration of follow-up ranged from 4 weeks to 16 months. The primary outcome measure in all studies was depression, which was measured by the EPDS in 12 studies. Other frequently reported measures in the reviews were the BDI-II, PHQ-9, and CES-D. The control group mainly used measures such as treatment as usual (TAU), placebo, and waitlist.
Effectiveness of digital psychological interventions
All 12 reviews evaluated the effectiveness of digital psychological interventions in the reduction of depressive symptoms. Regarding the type of intervention, both mindfulness therapy (Neo et al. 2022) and CBT (Lau et al. 2017; Roman et al. 2019) significantly improved the depressive symptoms of patients in the intervention group compared with those in the control group postintervention. In one study (Liu et al. 2022), the subgroup analysis of BA intervention and CBT intervention revealed that internet-based CBT had a significant effect on perinatal and postpartum depression (PPD) (standardized mean difference (SMD) = − 1.62; 95% CI: − 2.42 to − 0.80; p < 0.00001), but in the internet behavioral activation group, there was no significant difference in PPD scores after intervention between the experimental group and the control group (SMD = − 0.55; 95% CI: − 0.68 to − 0.43; p = 0.67). In addition, a study by Lau et al. (2020) showed that a website platform with ≥ 8 therapist-guided sessions using the theoretical principle of cognitive behavioral therapy was more effective than other treatments in improving depression symptoms in postnatal women. Regarding the delivery format of intervention, 1 article subgroup analyzed the effect of website-based, application-based, and telephone-based psychological interventions on perinatal depression. The results showed that all three intervention platforms had a positive effect on reducing perinatal depression, and application-based interventions (g = 4.02) were more effective than telephone-based interventions (g = 2.18) and website-based interventions (g = 1.62) (Liu et al. 2022). One article compared website-based interventions with application-based interventions and found that the effect sizes were greater among application-based interventions (g = 1.18) than website-based interventions (g = 0.45) (Lau et al. 2022). Subgroups of 2 studies analyzed the effect of digital psychological interventions on the prevention and treatment of perinatal depression and concluded that digital psychological interventions have a positive impact on the treatment of perinatal depression but differed with regard to the prevention of perinatal depression; however, no significant subgroup differences in prevention or treatment were found in either study (p > 0.05) (Lau et al. 2020, 2022). Regarding the duration of the intervention, studies showed that the postpartum depression scores of the intervention group were reduced at follow-up after 6–8 weeks, 4–7 weeks, and 8–14 weeks (Dol et al. 2020; Neo et al. 2022). The results of Mu et al. (2021) revealed that the effect of internet-based interventions weakened in studies with a follow-up duration over 12 weeks after intervention (0.727, 95% CI: 0.637 to 0.831). Lau et al. (2022) found that preferable features of intervention should be more than eight sessions and longer than 6 weeks in postnatal women.
Evaluation of the methodological quality of the included literature
Table 2 presents an item-by-item quality assessment for each study using the AMSTAR 2 instrument. Of the 12 articles, 2 were rated as low quality (Lau et al. 2017, 2020), and the rest were rated as critically low quality. Critical item 7 and non-critical items 3 and 10 were more frequently reported missing. In addition, some articles did not report and/or discuss the impact of the risk of bias on the results.
Table 2.
AMSTAR 2 evaluation results of the included literature
| Study | AMSTAR 2 items | Quality rating | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1a | 2b | 3c | 4d | 5e | 6f | 7 g | 8 h | 9i | 10j | 11 k | 12 l | 13 m | 14n | 15o | 16p | ||
| Dol et al. (2020) | Y | N | N | Y | Y | Y | Y | PY | N | N | N | N | N | N | N | PY | Critically low |
| Chae and Kim (2021) | Y | N | N | PY | N | N | N | PY | Y | N | Y | N | N | Y | Y | Y | Critically low |
| Loughnan et al. (2019) | PY | Y | N | Y | Y | Y | N | PY | Y | N | N | N | Y | N | Y | Y | Critically low |
| Nair et al. (2018) | N | Y | Y | Y | N | N | N | PY | N | N | Y | Y | Y | Y | Y | Y | Critically low |
| Roman et al. (2019) | Y | N | N | PY | N | N | N | PY | N | N | Y | Y | Y | Y | Y | N | Critically low |
| Lau et al. (2017) | Y | Y | Y | PY | Y | Y | N | Y | Y | N | Y | Y | Y | Y | Y | Y | Low |
| Neo et al. (2022) | Y | Y | N | PY | Y | Y | N | Y | Y | N | Y | N | N | N | Y | Y | Critically low |
| Liu et al. (2022) | Y | Y | N | PY | N | Y | N | PY | Y | N | Y | N | N | Y | Y | N | Critically low |
| Lau et al. (2022) | Y | Y | N | Y | Y | Y | Y | Y | Y | N | Y | Y | Y | Y | Y | Y | Moderate |
| Zhao et al. (2021) | PY | Y | N | Y | Y | Y | N | PY | Y | N | Y | N | N | Y | N | Y | Critically low |
| Mu et al. (2021) | Y | N | N | PY | N | N | N | PY | N | N | Y | Y | Y | Y | N | Y | Critically low |
| Lau et al. (2020) | Y | Y | Y | Y | Y | Y | N | Y | Y | N | Y | Y | Y | Y | Y | Y | Low |
Y yes, PY partial yes, N no
aDid the research questions and inclusion criteria for the review include the components of PICO?
bDid the report of the review contain an explicit statement that the review methods were established before the conduct of the review, and did the report justify any significant deviations from the protocol?
cDid the review authors explain their selection of the study designs for inclusion in the review?
dDid the review authors use a comprehensive literature search strategy?
eDid the review authors perform study selection in duplicate?
fDid the review authors perform data extraction in duplicate?
gDid the review authors provide a list of excluded studies and justify the exclusions?
hDid the review authors describe the included studies in adequate detail?
iDid the review authors use a satisfactory technique for assessing the risk of bias (RoB) in individual studies included in the review?
jDid the review authors report on funding sources for the studies included in the review?
kIf meta-analysis was performed, did the review authors use appropriate methods for statistical combination of results?
lIf meta-analysis was performed, did the review authors assess the potential impact of RoB in individual studies on the results of the meta-analysis or other evidence synthesis?
mDid the review authors account for RoB in individual studies when interpreting/discussing the results of the review?
nDid the review authors provide a satisfactory explanation for, and discussion of, any heterogeneity observed in the results of the review?
oIf they performed quantitative synthesis, did the review authors carry out an adequate investigation of publication bias (small study bias) and discuss its likely impact on the review results?
pDid the review authors report any potential sources of conflict of interest, including any funding they received for conducting the review?
Evaluation of the quality of evidence for inclusion in the literature
Table 3 shows the results of the quality grading of the outcome indicators according to the GRADE, with 2 high-level evidence papers, 1 moderate-level evidence paper, 4 low-level evidence papers, and 5 critically low-level evidence papers. Among the downgrading factors, inconsistency was the main downgrading factor, with most studies showing a high degree of heterogeneity between studies. The next most common downgrading factor was limitations, with 9 articles being downgraded because of limitations. Most of the articles only mentioned randomization but did not describe the method of generating random numbers, and most of the literature did not use blinding and allocation concealment. Finally, funnel plots or tests for publication bias were not produced in parts of the literature, leading to a high risk of publication bias.
Table 3.
Qualities of the evidence measuring major outcomes rated by the GRADE system
| Study | Risk of bias | Inconsistency | Indirectness | Imprecision | Publication bias | Quality rating |
|---|---|---|---|---|---|---|
| Dol et al. (2020) | − 1a | − 2b | 0 | 0 | − 1 | Critically low |
| Chae and Kim (2021) | − 1a | 0 | 0 | 0 | 0 | Moderate |
| Loughnan et al. (2019) | − 1a | − 1c | 0 | 0 | 0 | Low |
| Nair et al. (2018) | − 1a | − 1c | 0 | 0 | 0 | Low |
| Roman et al. (2019) | 0 | 0 | 0 | 0 | 0 | High |
| Lau et al. (2017) | 0 | 0 | 0 | 0 | 0 | High |
| Neo et al. (2022) | − 1a | − 1c | 0 | 0 | 0 | Low |
| Liu et al. (2022) | − 1a | − 2b | 0 | 0 | 0 | Critically low |
| Lau et al. (2022) | − 1a | − 2b | 0 | 0 | 0 | Critically low |
| Zhao et al. (2021) | − 1a | − 2b | 0 | 0 | − 1 | Critically low |
| Mu et al. (2021) | 0 | − 1c | 0 | 0 | − 1 | Low |
| Lau et al. (2020) | − 1a | − 2b | 0 | 0 | 0 | Critically low |
0, not downgraded; − 1, downgrade one level; − 2, downgrade two levels
aThe included studies were at high risk of bias for randomization, blinding, allocation concealment, completeness of outcome data, or selective reporting
bOf the included studies, 75% ≤ I2 ≤ 100%
cOf the included studies, 50% ≤ I2 < 75%
Discussion
Digital psychological interventions have a positive impact on reducing perinatal depression
The purpose of this study was to conduct a systematic review of previous meta-analyses addressing the effects of digital psychological interventions on PND symptoms. Of the 12 included meta-analyses, one meta-analysis reported that there was no significant difference between the internet behavioral activation and control groups in PPD scores after intervention (Liu et al. 2022). This may have been because only two articles were integrated for analysis in this subgroup, and the results may be somewhat biased. Second, one of the two studies included a population of women meeting Diagnostic and Statistical Manual of Mental Disorders criteria for major depressive disorder and one of women with depressive symptoms. Major depressive disorder requires a combination of formal psychotherapy and pharmacotherapy (Langan and Goodbred 2016), and psychological intervention alone may have little effect in treating major depressive disorder. While postpartum depression mostly occurs within 2 weeks after delivery, the symptoms are obvious 4–6 weeks after delivery (Li 2020), the incidence of perinatal depression decreases and symptoms gradually resolve as the postpartum period progresses (Banti et al. 2011; Underwood et al. 2016), and a longer assessment time (15 weeks) may lead to less pronounced postpartum depressive symptoms. These factors may have caused no obvious difference in the evaluation results between the two groups. In addition, this subgroup of articles analyzed internet-based CBT, and the results showed that internet-based CBT had a significant effect on PPD. The remaining 11 reviews reported the positive effects of digital psychological interventions in reducing perinatal depression. Psychotherapeutic interventions mainly include CBT, IPT, mindfulness intervention, BA, psychoeducational intervention, problem-solving therapy, stress reduction therapy, or a combination of therapies. A meta-analysis integrating 20 randomized controlled trials found that CBT effectively improved the symptoms and progression of postnatal depression (Huang et al. 2018). At present, the role of psychotherapeutic interventions in the prevention and treatment of perinatal depression has been generally verified (Nillnia et al. 2018; Ponting et al. 2020). With the rapid development of information technology, digital psychological intervention has gradually become a research hotspot in technology, psychology, nursing, and other fields. Digital interventions are diverse, with most studies focusing on telephone-based interventions, but recent studies have also demonstrated the superiority and effectiveness of SMS and smartphone applications (Lamont et al. 2016; Sun et al. 2021). The literature included in this study suggests that digital interventions, whether website-based psychological interventions, telephone-based psychological interventions, or application-based psychological interventions, have a positive impact on perinatal depression, but the effect size of other delivery forms of psychological intervention on reducing perinatal depression was not specifically compared. We recommend that this is expanded in future studies to identify the best form of delivery and improve the effectiveness of the intervention. In addition, the effectiveness of digital psychological interventions in preventing perinatal depression needs to be further validated. The effectiveness of the different digital psychological intervention methods varied depending on the duration of the intervention, intensity, intervention provider, and depth of follow-up; however, in general, digital psychological interventions had a positive impact on improving perinatal depression.
Quality of studies in meta-analyses of the effectiveness of digital psychological interventions in reducing perinatal depression
The results of the AMSTAR 2 quality evaluation showed that the methodological quality of the 12 included meta-analyses was low, with items 3, 7, and 10 more frequently reported as missing and some articles not reporting and/or discussing the impact of the risk of bias on the results. Our recommendations for further research are as follows: (a) Considering that the inclusion of RCTs alone may result in the inclusion of non-comprehensive studies, the types of included studies should be limited, and the reasons for inclusion should be explained; (b) to avoid researchers being influenced by their preferences when screening and including studies, researchers should make a list of excluded literature and give reasons for exclusion; (c) given the influence of commercial funding, researchers should report whether the included studies receive funding and the source of that funding; (d) note the heterogeneity and impact of the risk of bias (e.g., selection bias, publication bias) of the included literature on the results; subgroup analysis, sensitivity analysis, and detailed discussion and interpretation of the results should be included.
The GRADE evaluation showed that the included literature had a low strength of evidence; inconsistency was the main downgrading factor, followed by limitations and publication bias. The above analysis showed that many of the existing studies have deficiencies, such as poor design and incomplete analysis. Therefore, the conclusions of the meta-analysis need to be further validated. More high-quality original studies, especially high-quality randomized controlled trials, need to be conducted in the future to provide better evidence to support the use of digital psychological interventions.
Limitations and future directions
Despite these important findings, this study also had the following limitations. First, the current systematic evaluation and re-evaluation could only descriptively evaluate the elements included in the meta-analysis based on existing studies, and it was difficult to re-evaluate the previous research process comprehensively. The quality of meta-analysis is influenced by the quality of the original article and the quality of the methodology, and bias objectively exists; therefore, large-scale and high-quality research and reviews are needed. Second, the heterogeneity among the included studies was large, which was mainly due to the inconsistency of intervention methods, frequency, duration, and time of measurement (ranging from 2 weeks to 16 months, mostly ≤ 12 weeks) of perinatal depression of digital psychological interventions. Therefore, we did not combine the original articles included in the 12 meta-analyses to provide a pooled effect size of digital psychological interventions on perinatal depression and only performed a descriptive analysis. Finally, the selected meta-analyses included overlapping trials, so these studies were considered more than once in our synthesis, which may have skewed some of the results. We comprehensively examined the original literature in 12 meta-analyses, and a total of 110 original studies were included, leaving 50 remaining after removing duplicates.
In the future, large-scale and high-quality studies should be conducted to establish evidence-based digital psychological intervention methods in terms of structure, content, and providers to lay the foundation for the development of scientific, rigorous, and standardized systematic evaluations and promote the development of the evidence-based practice of digital psychological interventions in perinatal depression. Literature included in systematic reviews and meta-analyses should also strictly follow the PRISMA statement to improve the quality of the review and the level of evidence and to provide a scientific basis for advancing the clinical translation of research results.
Conclusion
This study is an early systematic re-evaluation focusing on digital psychological interventions for reducing perinatal depression and provides a reference for promoting an evidence-based practice of digital psychological interventions in women with perinatal depression. This review suggests that digital psychological interventions have a positive effect on reducing perinatal depression, and the use of digital psychological interventions for the treatment and care of women in the perinatal period should be considered in medical practice to increase the accessibility of medical care and reduce women’s sense of stigma.
However, the methodological quality and level of evidence of the current meta-analyses are low, the outcome indicators of the studies mostly used scales based on subjective evaluation, and there was a lack of objective quantitative analysis, which may have impacted the reliability and accuracy of the results of this study. Therefore, the effectiveness of digital psychological interventions in reducing perinatal depression needs to be supported by higher-level evidence. More high-quality, large-sample, multicenter clinical trials should be conducted in the future to compare different intervention forms and durations; provide the best level of support; lay the foundation for developing scientific, rigorous, standardized systematic evaluations; maximize long-term effects; and promote the development of evidence-based digital psychological interventions for perinatal depression.
Acknowledgements
We would like to thank the authors of the included studies in this study for sharing their research.
Author contribution
CC designed the study and wrote the first draft of the manuscript.
YL assessed the quality of the studies and reviewed and proofread the papers.
CC and XW developed the search strategy and screened titles and abstracts.
CC, XW, and HX evaluated the papers for inclusion and extracted data.
All authors contributed to and have seen and approved the final version of the manuscript being submitted. We warrant that the article is our original work, has not received prior publication, and is not under consideration for publication elsewhere.
Funding
This review was supported by Anhui Provincial Natural Science Foundation (grant number: 2108085MG242).
Data Availability
Any other questions about the data can be communicated by contacting the corresponding author.
Declarations
Competing interests
The authors declare no competing interests. They did not use any non-original material except for the references cited in this study.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Caifeng Chen, Email: ccf08020603@163.com.
Xiaoying Wang, Email: w1878744460@163.com.
Han Xu, Email: 376652033@qq.com.
Yuhong Li, Email: liyuhong@ahmu.edu.cn.
References
- Banti S, Mauri M, Oppo A, Borri C, Rambelli C, Ramacciotti D, Montagnani MS, Camilleri V, Cortopassi S, Rucci P, Cassano GB. From the third month of pregnancy to 1 year postpartum. Prevalence, incidence, recurrence, and new onset of depression. Results from the perinatal depression-research & screening unit study. Compr Psychiatry. 2011;52:343–351. doi: 10.1016/j.comppsych.2010.08.003. [DOI] [PubMed] [Google Scholar]
- Bowers ME, Yehuda R. Intergenerational transmission of stress in humans. Neuropsychopharmacology. 2016;41:232–244. doi: 10.1038/npp.2015.247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brearly TW, Shura RD, Martindale SL, Lazowski RA, Luxton DD, Shenal BV, Rowland JA. Neuropsychological test administration by videoconference: a systematic review and meta-analysis. Neuropsychol Rev. 2017;27:174–186. doi: 10.1007/s11065-017-9349-1. [DOI] [PubMed] [Google Scholar]
- Cacciola E, Psouni E. Insecure attachment and other help-seeking barriers among women depressed postpartum. Int J Environ Res Public Health. 2020;17:3887. doi: 10.3390/ijerph17113887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chae J, Kim HK. Internet-based prenatal interventions for maternal health among pregnant women: a systematic review and meta-analysis. Child Youth Serv Rev. 2021;127:106079. doi: 10.1016/j.childyouth.2021.106079. [DOI] [Google Scholar]
- Dol J, Richardson B, Murphy GT, Aston M, McMillan D, Campbell-Yeo M. Impact of mobile health interventions during the perinatal period on maternal psychosocial outcomes. JBI Evid Synth. 2020;18:30–55. doi: 10.11124/JBISRIR-D-19-00191. [DOI] [PubMed] [Google Scholar]
- Dolan N, Grealish A, Tuohy T, Bright A. Are mindfulness-based interventions as effective as cognitive behavioral therapy in reducing symptoms of complicated perinatal grief? A systematic review. J Midwifery Wom Heal. 2022;67:209–225. doi: 10.1111/jmwh.13335. [DOI] [PubMed] [Google Scholar]
- Duan C, Hare M, Staring M, Deligiannidis KM. Examining the relationship between perinatal depression and neurodevelopment in infants and children through structural and functional neuroimaging research. Int Rev Psychiatr. 2019;31:264–279. doi: 10.1080/09540261.2018.1527759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fu Z, Burger H, Arjadi R, Bockting CLH. Effectiveness of digital psychological interventions for mental health problems in low-income and middle-income countries: a systematic review and meta-analysis. Lancet Psychiat. 2020;7:851–864. doi: 10.1016/S2215-0366(20)30256-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilbody S, Brabyn S, Lovell K, Kessler D, Devlin T, Smith L, Araya R, Barkham M, Bower P, Cooper C, Knowles S, Littlewood E, Richards DA, Tallon D, White D, Worthy G, Collaborative REEACT. Telephone-supported computerised cognitive–behavioural therapy: REEACT-2 large-scale pragmatic randomised controlled trial. Brit J Psychiat. 2017;210:362–367. doi: 10.1192/bjp.bp.116.192435. [DOI] [PubMed] [Google Scholar]
- Gordon M, Henderson R, Holmes JH, Wolters MK, Bennett IM, SPIRIT (Stress in Pregnancy: Improving Results with Interactive Technology) Group Participatory design of ehealth solutions for women from vulnerable populations with perinatal depression. J Am Med Inform Assoc. 2016;23:105–109. doi: 10.1093/jamia/ocv109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grundwald NJ, Brunton PJ. Prenatal stress programs neuroendocrine stress responses and affective behaviors in second generation rats in a sex-dependent manner. Psychoneuroendocrino. 2015;62:204–216. doi: 10.1016/j.psyneuen.2015.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, Schunemann HJ. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ-Brit Med J. 2008;336:924–926. doi: 10.1136/bmj.39489.470347.AD. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hannigan LJ, Eilertsen EM, Gjerde LC, Reichborn-Kjennerud T, Eley TC, Rijsdijk FV, Ystrom E, McAdams TA. Maternal prenatal depressive symptoms and risk for early-life psychopathology in offspring: genetic analyses in the Norwegian Mother and Child Birth Cohort Study. Lancet Psychiat. 2018;5:808–815. doi: 10.1016/S2215-0366(18)30225-6. [DOI] [PubMed] [Google Scholar]
- Herba CM, Glover V, Ramchandani PG, Rondon MB. Maternal depression and mental health in early childhood: an examination of underlying mechanisms in low-income and middle-income countries. Lancet Psychiat. 2016;3:983–992. doi: 10.1016/S2215-0366(16)30148-1. [DOI] [PubMed] [Google Scholar]
- Higgins JPT, Altman DG, Gotzsche PC, Juni P, Moher D, Oxman AD, Savovic J, Schulz KF, Weeks L, Sterne JAC. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ-Brit Med J. 2011;343:d5928. doi: 10.1136/bmj.d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howard LM, Khalifeh H. Perinatal mental health: a review of progress and challenges. World Psychiatry. 2020;19:313–327. doi: 10.1002/wps.20769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang L, Zhao Y, Qiang C, Fan B. Is cognitive behavioral therapy a better choice for women with postnatal depression? A systematic review and meta-analysis. PLoS One. 2018;13:e205243. doi: 10.1371/journal.pone.0205243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang RR, Lei BM, Fu B, Zhang LJ, Chen ZH, Xiao ML, Yang DQ, Yan CL, Lei J. Research progress in perinatal depression assessment. Chin Nursing Manag. 2019;19:1105–1109. doi: 10.3969/j.issn.l672-1756.2019.07.031. [DOI] [Google Scholar]
- Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJM, Gavaghan DJ, McQuay HJ. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials. 1996;17:1–12. doi: 10.1016/0197-2456(95)00134-4. [DOI] [PubMed] [Google Scholar]
- Jarde A, Morais M, Kingston D, Giallo R, MacQueen GM, Giglia L, Beyene J, Wang Y, McDonald SD. Neonatal outcomes in women with untreated antenatal depression compared with women without depression: a systematic review and meta-analysis. JAMA Psychiat. 2016;73:826–837. doi: 10.1001/jamapsychiatry.2016.0934. [DOI] [PubMed] [Google Scholar]
- Josefsson A, Angelsiöö L, Berg G, Ekström C, Gunnervik C, Nordin C, Sydsjö G. Obstetric, somatic, and demographic risk factors for postpartum depressive symptoms. Obstet Gynecol. 2002;2:223–228. doi: 10.1016/s0029-7844(01)01722-7. [DOI] [PubMed] [Google Scholar]
- Khalifeh H, Hunt IM, Appleby L, Howard LM. Suicide in perinatal and non-perinatal women in contact with psychiatric services: 15 year findings from a UK national inquiry. Lancet Psychiat. 2016;3:233–242. doi: 10.1016/S2215-0366(16)00003-1. [DOI] [PubMed] [Google Scholar]
- Ladyman C, Sweeney B, Sharkey K, Bei B, Wright T, Mooney H, Huthwaite M, Cunningham C, Firestone R, Signal TL. A scoping review of non-pharmacological perinatal interventions impacting maternal sleep and maternal mental health. BMC Pregnancy Childb. 2022;22:659. doi: 10.1186/s12884-022-04844-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lamont K, Sliwa K, Stewart S, Carrington M, Pretorius S, Libhaber E, Wiysonge CS, Adebayo EF, Klipstein-Grobusch K. Short message service (SMS) as an educational tool during pregnancy: a literature review. Health Educ J. 2016;75:540–552. doi: 10.1177/0017896915607910. [DOI] [Google Scholar]
- Langan R, Goodbred AJ. Identification and management of peripartum depression. Am Fam Physician. 2016;93:852–858. [PubMed] [Google Scholar]
- Lara MA, Navarrete L, Nieto L, Barba Martín JP, Navarro JL, Lara-Tapia H. Prevalence and incidence of perinatal depression and depressive symptoms among Mexican women. J Affect Disorders. 2014;175:18–24. doi: 10.1016/j.jad.2014.12.035. [DOI] [PubMed] [Google Scholar]
- Lau Y, Cheng J, Wong S, Yen K, Cheng L. Effectiveness of digital psychotherapeutic intervention among perinatal women: a systematic review and meta-analysis of randomized controlled trials. World J Psychiatr. 2020;11:133–152. doi: 10.5498/wjp.v11.i4.133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lau Y, Htun TP, Wong SN, Tam W, Klainin-Yobas P. Therapist-supported Internet-based cognitive behavior therapy for stress, anxiety, and depressive symptoms among postpartum women: a systematic review and meta-analysis. J Med Internet Res. 2017;19:e138. doi: 10.2196/jmir.6712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lau Y, Yen KY, Wong SH, Cheng JY, Cheng LJ. Effect of digital cognitive behavioral therapy on psychological symptoms among perinatal women in high income-countries: a systematic review and meta-regression. J Psychiatr Res. 2022;146:234–248. doi: 10.1016/j.jpsychires.2021.11.012. [DOI] [PubMed] [Google Scholar]
- Lei BM, Xiao ML, Huang RR, Yang DQ, Fu B, Tang GX, Zhang LJ, Chen ZH, Lei J. Research progress in perinatal depression interventions. Chin Nursing Manag. 2019;19:784–789. doi: 10.3969/j.issn.1672-1756.2019.05.030. [DOI] [Google Scholar]
- Li YH. Review of risk factors screening of postpartum depression and its interventions. Chin General Pract. 2020;23:266–271. doi: 10.12114/j.issn.1007-9572.2019.00.773. [DOI] [Google Scholar]
- Liu X, Huang S, Hu Y, Wang G. The effectiveness of telemedicine interventions on women with postpartum depression: a systematic review and meta-analysis. Worldv Evid-Based Nu. 2022;19:175–190. doi: 10.1111/wvn.12576. [DOI] [PubMed] [Google Scholar]
- Lockwood C, Munn Z, Porritt K. Qualitative research synthesis: methodological guidance for systematic reviewers utilizing meta-aggregation. Int J Evid-Based Hea. 2015;13:179–187. doi: 10.1097/XEB.0000000000000062. [DOI] [PubMed] [Google Scholar]
- Loughnan SA, Joubert AE, Grierson A, Andrews G, Newby JM. Internet-delivered psychological interventions for clinical anxiety and depression in perinatal women: a systematic review and meta-analysis. Arch Womens Ment Health. 2019;22:737–750. doi: 10.1007/s00737-019-00961-9. [DOI] [PubMed] [Google Scholar]
- Mannarini S, Rossi A. Assessing mental illness stigma: a complex issue. Front Psychol. 2018;9:2722. doi: 10.3389/fpsyg.2018.02722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martín-Gómez C, Moreno-Peral P, Bellón JA, Cerón SC, Campos-Paino H, Gómez-Gómez I, Rigabert A, Benítez I, Motrico E. Effectiveness of psychological, psychoeducational and psychosocial interventions to prevent postpartum depression in adolescent and adult mothers: study protocol for a systematic review and meta-analysis of randomised controlled trials. BMJ Open. 2020;10:e34424. doi: 10.1136/bmjopen-2019-034424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer MA. COVID-19 pandemic accelerates need to improve online patient engagement practices to enhance patient experience. J Patient Experience. 2020;7:657–664. doi: 10.1177/2374373520959486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mu TY, Li YH, Xu RX, Chen J, Wang YY, Shen CZ. Internet-based interventions for postpartum depression: a systematic review and meta-analysis. Nurs Open. 2021;8:1125–1134. doi: 10.1002/nop2.724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nair U, Armfield NR, Chatfield MD, Edirippulige S. The effectiveness of telemedicine interventions to address maternal depression: a systematic review and meta-analysis. J Telemed Telecare. 2018;24:639–650. doi: 10.1177/1357633X18794332. [DOI] [PubMed] [Google Scholar]
- Neo HS, Tan JH, Ang WHD, Lau Y. Internet-delivered psychological interventions for reducing depressive, anxiety symptoms and fear of childbirth in pregnant women: a meta-analysis and meta-regression. J Psychosom Res. 2022;157:110790. doi: 10.1016/j.jpsychores.2022.110790. [DOI] [PubMed] [Google Scholar]
- Nillnia YI, Mehralizadec A, Mayerb L, Milanovic S. Treatment of depression, anxiety, and trauma-related disorders during the perinatal period: a systematic review. Clin Psychol Rev. 2018;66:136–148. doi: 10.1016/j.cpr.2018.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Osborne D, Meyer D, Moulding R, Kyrios M, Bailey E, Nedeljkovic M. Cost-effectiveness of internet-based cognitive-behavioural therapy for obsessive-compulsive disorder. Internet Interv. 2019;18:100277. doi: 10.1016/j.invent.2019.100277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, Chou R, Glanville J, Grimshaw JM, Hróbjartsson A, Lalu MM, Li T, Loder EW, Mayo-Wilson E, McDonald S, McGuinness LA, Stewart LA, Thomas J, Tricco AC, Welch VA, Whiting P, Moher D (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ-Brit Med J n71. 10.1136/bmj.n71
- Parameswaran UD, Pentecost R, Williams M, Smid M, Latendresse G. Experiences with use of technology and telehealth among women with perinatal depression. BMC Pregnancy Childb. 2022;22:1–571. doi: 10.1186/s12884-022-04889-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ponting C, Mahrer NE, Zelcer H, Schetter CD, Chavira DA. Psychological interventions for depression and anxiety in pregnant Latina and Black women in the United States: a systematic review. Clin Psychol Psychot. 2020;27:249–265. doi: 10.1002/cpp.2424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roman M, Constantin T, Bostan CM. The efficiency of online cognitive-behavioral therapy for postpartum depressive symptomatology: a systematic review and meta-analysis. Women Health. 2019;60:99–112. doi: 10.1080/03630242.2019.1610824. [DOI] [PubMed] [Google Scholar]
- Rommel A, Bergink V, Liu X, Munk-Olsen T, Molenaar NM. Long-term effects of intrauterine exposure to antidepressants on physical, neurodevelopmental, and psychiatric outcomes: a systematic review. J Clin Psychiat. 2020;81:19r–12965r. doi: 10.4088/JCP.19r12965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rommel AS, Momen NC, Molenaar NM, Agerbo E, Bergink V, Munk-Olsen T, Liu X. Antidepressant use during pregnancy and risk of adverse neonatal outcomes: a comprehensive investigation of previously identified associations. Acta Psychiat Scand. 2022;145:544–556. doi: 10.1111/acps.13409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sangsawang B, Wacharasin C, Sangsawang N. Interventions for the prevention of postpartum depression in adolescent mothers: a systematic review. Arch Womens Ment Health. 2019;22:215–228. doi: 10.1007/s00737-018-0901-7. [DOI] [PubMed] [Google Scholar]
- Shea BJ, Reeves BC, Wells G, Thuku M, Hamel C, Moran J, Moher D, Tugwell P, Welch V, Kristjansson E, Henry DA (2017) AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ-Brit Med J j4008. 10.1136/bmj.j4008 [DOI] [PMC free article] [PubMed]
- Silveira ML, Ertel KA, Dole N, Chasan-Taber L. The role of body image in prenatal and postpartum depression: a critical review of the literature. Arch Womens Ment Health. 2015;18:409–421. doi: 10.1007/s00737-015-0525-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simas TAM, Flynn MP, KrollDesrosiers AR, Carvalho SM, Levin LL, Biebel K, Byatt N. A systematic review of integrated care interventions addressing perinatal depression care in ambulatory obstetric care settings. Clin Obstet Gyneco. 2018;61:573–590. doi: 10.1097/GRF.0000000000000360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith V, Devane D, Begley CM, Clarke M. Methodology in conducting a systematic review of systematic reviews of healthcare interventions. BMC Med Res Methodol. 2011;11:15. doi: 10.1186/1471-2288-11-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sockol LE. A systematic review and meta-analysis of interpersonal psychotherapy for perinatal women. J Affect Disorders. 2018;232:316–328. doi: 10.1016/j.jad.2018.01.018. [DOI] [PubMed] [Google Scholar]
- Sterne JAC, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, Cates CJ, Cheng H, Corbett MS, Eldridge SM, Emberson JR, Hernán MA, Hopewell S, Hróbjartsson A, Junqueira DR, Jüni P, Kirkham JJ, Lasserson T, Li T, McAleenan A, Reeves BC, Shepperd S, Shrier I, Stewart LA, Tilling K, White IR, Whiting PF, Higgins JPT (2019) RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ-Brit Med J l4898. 10.1136/bmj.l4898 [DOI] [PubMed]
- Sun Y, Li Y, Wang J, Chen Q, Bazzano AN, Cao F (2021) Effectiveness of smartphone-based mindfulness training on maternal perinatal depression: randomized controlled trial. J Med Internet Res 23: e23410. 10.2196/23410 [DOI] [PMC free article] [PubMed]
- Underwood L, Waldie K, D'Souza S, Peterson ER, Morton S. A review of longitudinal studies on antenatal and postnatal depression. Arch Womens Ment Health. 2016;19:711–720. doi: 10.1007/s00737-016-0629-1. [DOI] [PubMed] [Google Scholar]
- van Ravesteyn LM, Lambregtse-van DBM, Hoogendijk WJ, Kamperman AM. Interventions to treat mental disorders during pregnancy: a systematic review and multiple treatment meta-analysis. PLoS One. 2017;12:e173397. doi: 10.1371/journal.pone.0173397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wonch KE, de Medeiros CB, Barrett JA, Dudin A, Cunningham WA, Hall GB, Steiner M, Fleming AS. Postpartum depression and brain response to infants: differential amygdala response and connectivity. Soc Neurosci-Uk. 2016;11:600–617. doi: 10.1080/17470919.2015.1131193. [DOI] [PubMed] [Google Scholar]
- World Health Organization ed. (2018) Intrapartum care for a positive childbirth experience WHO recommendations. World Health Organization, Geneva, Switzerland. 10.1080/09638237.2021.1952947
- Zhang X, Lin P, Sun J, Sun Y, Shao D, Cao D, Cao F. Prenatal stress self-help mindfulness intervention via social media: a randomized controlled trial. J Ment Health. 2021;32:206–215. doi: 10.1080/09638237.2021.1952947. [DOI] [PubMed] [Google Scholar]
- Zhao L, Chen J, Lan L, Deng N, Liao Y, Yue L, Chen I, Wen SW, Xie R. Effectiveness of telehealth interventions for women with postpartum depression: systematic review and meta-analysis. JMIR Mhealth Uhealth. 2021;9:e32544. doi: 10.2196/32544. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Any other questions about the data can be communicated by contacting the corresponding author.