Abstract
Discussion of diversity, equity, and inclusion (DEI) has moved to the forefront in medical education, and in particular, efforts toward gender equity have emphasized the need for more women faculty and physicians. Gender parity was recently achieved for medical students matriculating into US allopathic schools during the 2017–2018 academic year1. However, this documented increase in women attending medical school as students is not matched by an increase in women teaching in the undergraduate medical education (UME) curriculum. In 2020, the faculty employed by medical schools across the USA (totaling 186,311) includes 43% women; this percentage drops significantly when considering the rank of full professor, of which only 26% are women [1]. For faculty representing graduate programs in science, technology, engineering, and math (STEM), many of which teach in the pre-clerkship phase of UME, less than 25% are women [2], according to the 2019 AAMC statement of gender equity.
Supplementary Information
The online version contains supplementary material available at 10.1007/s40670-023-01776-1.
Background
Discussion of diversity, equity, and inclusion (DEI) has moved to the forefront in medical education, and in particular, efforts toward gender equity have emphasized the need for more women faculty and physicians. Gender parity was recently achieved for medical students matriculating into US allopathic schools during the 2017–2018 academic year [1]. However, this documented increase in women attending medical school as students is not matched by an increase in women teaching in the undergraduate medical education (UME) curriculum. In 2020, the faculty employed by medical schools across the USA (totaling 186,311) includes 43% women; this percentage drops significantly when considering the rank of full professor, of which only 26% are women [1]. Faculty representing graduate programs in science, technology, engineering, and math (STEM), many of which teach in the pre-clerkship phase of UME face their own barriers [2], and less than 25% are women [3], according to the 2019 AAMC statement of gender equity.
The lack of female faculty early in UME has an impact beyond equity in numbers. Gender-related experiences that negatively impact medical students disproportionately exist in females, who report feelings of “fatigue, frustration, isolation, and self-doubt,” particularly in the pre-clinical years [3]. In some, these sentiments resulted in a diminished sense of belonging within the medical profession, indicating that “imposter syndrome” is present early in medical training. To alleviate this sentiment and create a more inclusive environment, female medical students intentionally seek out female peers and faculty [4]. This highlights a need for strong support and mentorship of female medical students.
Effective faculty do far more than provide information to their students; they serve in several capacities (“roles”) including as a mentor, facilitator, resource, and role model to students [5]. These roles are an important and impactful part of the student experience. In particular, mentorship improves the medical student experience [6]. Research shows that students internalize traits from their mentors [7], and it has been shown that exposure to role models has a strong impact on medical students’ choice of specialty [8]. Students are more likely to pursue a specialty or career in which they have a mentor. Recent studies demonstrate that, during the pre-clinical years of UME, faculty gender can impact medical student development positively by fostering a sense of community [4, 7, 8]. Interestingly, gender differences in teaching are also noted at the student level, as studies have reported female medical students make more effective facilitators than their male counterparts [9, 10].
Unfortunately, there is a historic trend in which female medical students report challenges in finding same-sex role models and mentors (significantly more than their male peers) [11]. This problem likely remains unresolved, given the disparity in the representation of women faculty coupled with the increased population of women as students in medical school [1]. Thus, it is reasonable to expect that, for female faculty, the duties of “mentor” and “role model” would be desired and deemed important by female medical students. To our knowledge, the gender-specific roles of faculty and the influence this has on the medical education experience are yet to be explicitly described. This work sought to understand whether the medical education experience was different for male versus female students. Specifically, we sought to understand how medical students appraise the contribution(s) of male and female faculty during the first year of the UME curriculum.
Finally, we note that the language used here related to sex and gender refers most typically to biological and socio-cultural differences, respectively. In this study, we are using the self-reported, biological sex (male or female). Thus, most of our language will use the terms “male” or “female.” Other studies may have identified cohorts using the “man” or “woman” designation, and in referencing that research, we may also utilize that language.
Activity
First-year medical students (189 students: 51% male and 49% female) at the University of Cincinnati College of Medicine (UCCoM class of 2023) were invited to participate in an optional, anonymous online survey upon completion of their first year of medical school (June, 2020). The anonymous survey link was provided via email to the student cohort and was part of a survey conducted biannually by medical student curriculum representatives, which included broad questions about the student learning experience. For this study, we utilized a subset of unique questions created by medical education faculty specifically to understand the role of male versus female faculty. These questions were unique to this survey iteration (June 2020) and were approved by the UCCoM Office of Medical Education evaluation team and the institutional IRB. Student participants were informed that participation in the survey was optional, anonymous, and uncompensated.
Student participants self-identified their gender (male, female, non-binary) and were asked to evaluate their own perception of faculty in the first-year, foundational science courses. All students were asked whether female faculty presence in the pre-clinical UME courses was important in medical education broadly, as well as to the participant, personally. Participants were asked to indicate (5-point Likert scale; “never” to “always”) whether they personally experienced male and female faculty in the following roles, adapted from Harden and Crosby [6]: role model, scholarly leader, content expert, mentor, resource, information provider, facilitator (helps me achieve my learning), evaluator (assesses my learning), and agent of change (improves the curriculum). Students were also asked for the broader curriculum whether gender had an important influence in these roles (in addition to a new role — “agent of change”) and whether female faculty, specifically, were an important influence in these roles. Responses were analyzed by chi-square (two-variable questions) and by t test (multi-variable questions) using SPSS statistical software.
Results
The UME program at UCCoM is an integrated, organ-system–based curriculum with a 2-year pre-clerkship phase followed by 2 years of clinical clerkship experiences. The first-year (M1) foundational courses involve 90 faculty members in total (68% male and 32% female). Of the roughly 312 total lectures given in the first year, 271 were given by male faculty (86.9%) and only 41 lectures given by female faculty (13.1%). Of the 189 M1 students asked to evaluate their experience with these faculty lecturers, 130 students completed the survey (68.7% response rate). Just over half of student participants self-identified as female (55%), a gender ratio which approximates the M1 cohort. Two respondents identified as non-binary (data not included in this analysis).
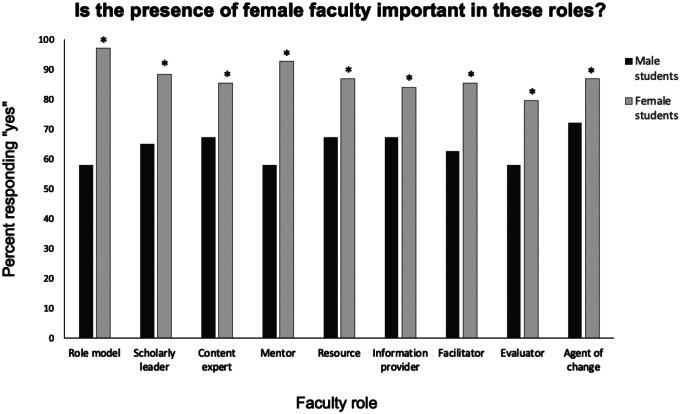
When considering how all medical students experience early UME, female medical students tended to view female lecturers as more important than did their male student peers, although statistical significance was not achieved (5-point Likert scale; male students = 4.39; female students 4.64; p = 0.064, t test male vs. female students). When asked how students were affected personally, both male and female medical students reported that a female faculty presence in UME is important (Pearson’s Chi-square analysis; x [2] = 1.845; 1, N = 119, p = 0.174). However, when asked whether it is important for female faculty to serve in specific faculty roles [6], female medical students were significantly more likely to respond, “yes,” than their male student peers (Fig. 1; Pearson’s chi-square analysis; p ≤ 0.001). Details for this statistical analysis are found in Supplemental Table S1.
Fig. 1.
Female medical students say that female faculty play many important roles in medical education. First-year medical students were asked whether, in the broad context of medical education, representation of female faculty was important in the specific faculty roles listed. For each role, female students responded “yes” significantly more than their male peers (chi-square analysis “yes” versus “no” for each role, *p < 0.01; ***p < 0.001)
To better understand what specific ways students viewed UME faculty of different genders, we asked students to report how often they personally experienced faculty in various roles that have been previously described for medical teachers [6] (using a 5-point Likert scale; see supplemental materials). Male students regard male and female faculty similarly, primarily experiencing faculty as “information providers” and not as “mentors.” Table 1 shows non-significant p values for comparison of faculty gender in each specified faculty role, representing the experience of male medical students (t test analysis). Interestingly, female students reported significant differences in their experience of faculty of different genders (Table 2). Female medical students were significantly more likely to regard male faculty in the roles of “content expert” (p = 0.05) and “evaluator” (p < 0.001), while they experienced female faculty significantly more in the roles of “mentor” (p < 0.001) and “role model” (p < 0.001) (t test analysis; male versus female faculty).
Table 1.
Influence of faculty gender on male medical students’ experience of faculty
| Averagea ± SD | |||
|---|---|---|---|
| Faculty role | Male faculty | Female faculty | p valueb |
| Role model | 3.26 ± 0.77 | 3.19 ± 0.83 | 0.641 |
| Scholarly leader in field | 3.66 ± 0.74 | 3.63 ± 0.69 | 0.791 |
| Content expert | 3.96 ± 0.65 | 3.88 ± 0.61 | 0.457 |
| Mentor | 2.65 ± 1.10 | 2.61 ± 1.12 | 0.866 |
| Resource | 3.45 ± 1.08 | 3.33 ± 1.20 | 0.557 |
| Information provider | 4.14 ± 0.87 | 4.03 ± 0.77 | 0.487 |
| Facilitator of learning | 3.66 ± 0.82 | 3.52 ± 0.89 | 0.374 |
| Evaluator | 3.51 ± 0.86 | 3.21 ± 0.94 | 0.078 |
aNumbers reflect average responses ± standard deviation to the question, “Please rate the degree to which the [MALE/FEMALE] faculty you encountered in your basic science and organ-system courses served in the following roles for you as a medical student.” (5-point Likert scale: 1 = never, 2 = seldom, 3 = sometimes, 4 = often, 5 = always)
bStatistical comparison of student responses for male versus female faculty, analyzed by t test for each individual role
Table 2.
Influence of faculty gender on female medical students’ experience of faculty
| Averagea ± SD | |||
|---|---|---|---|
| Faculty role | Male faculty | Female faculty | p valueb |
| Role model | 2.90 ± 0.91 | 3.51 ± 0.92 | < 0.001 |
| Scholarly leader in field | 3.79 ± 0.69 | 3.60 ± 0.78 | 0.116 |
| Content expert | 3.90 ± 0.65 | 3.61 ± 0.83 | < 0.05 |
| Mentor | 2.46 ± 1.01 | 3.03 ± 1.07 | < 0.001 |
| Resource | 3.22 ± 0.91 | 3.36 ± 0.98 | 0.380 |
| Information provider | 4.01 ± 0.78 | 3.74 ± 0.98 | 0.061 |
| Facilitator of learning | 3.56 ± 0.89 | 3.42 ± 0.98 | 0.139 |
| Evaluator | 3.68 ± 0.96 | 2.83 ± 1.06 | < 0.001 |
aNumbers reflect average responses ± standard deviation to the question, “Please rate the degree to which the [MALE/FEMALE] faculty you encountered in your basic science and organ-system courses served in the following roles for you as a medical student.” (5-point Likert scale: 1 = never, 2 = seldom, 3 = sometimes, 4 = often, 5 = always)
bStatistical comparison of student responses for male versus female faculty, analyzed by t test for each individual role
Discussion
These data demonstrate the unique roles that female faculty serve for female medical students. As medical school cohorts continue to grow in their diversity, it is important to consider the medical education experience of learners, particularly for historically marginalized groups. Here, we show that there is indeed a gendered difference in how medical students encounter the faculty in the pre-clerkship curriculum. Overall, while male students report that female faculty are an important presence, they personally experience UME faculty uniformly across a variety of roles. For female medical students, however, it is the female faculty who bring added value as role models and mentors.
This is perhaps not surprising. The importance of mentors is reflected in a refrain echoed across minoritized populations: “You can’t be what you can’t see.” It is important to note that the unique value associated with the indirect roles that female faculty assume (i.e., mentorship) did not come at the cost of their value as an educator. We demonstrate that medical students personally value male and female faculty equally as a resource, information provider, and facilitator of student learning.
Across undergraduate and graduate medical education, gender biases in learning and teaching have been documented, impacting students [12, 13] and faculty [14, 15], respectively. On faculty teaching evaluations, these biases exist in the evaluation of teaching materials [16] as well as in qualitative comments [12, 13, 15]. For example, female instructors are more often described as “compassionate,” while males are described as “exemplary” or “intelligent” [12]. Indeed, biased experiences are reflected in our data, as female students but not male students are more likely to view male faculty as content experts and evaluators. The latter is particularly interesting and may be related to the “stereotype threat” that women, more so than men, have been shown to experience, which can negatively impact the perceived environment in academic medicine [17]. On the other hand, both biases could be a product of the limited exposure that our participant cohort had to female faculty in their first-year curriculum, as the number of total lectures given by women was less than fifteen percent.
Considering these uniquely positive experiences that female medical students have when interacting with female faculty, it is important to consider representation in medical teaching faculty. The stark contrast between the numbers of female medical students versus faculty in advanced positions who identify as female is not insignificant. As we approach the 5-year mark of gender parity in medical school matriculants, one might imagine that the trend will soon follow in the faculty arena, as students graduate residency programs. This is a tempting assumption that the under-representation of women physicians and educators is a time-limited problem. However, it ignores the discrepancies that continue to flourish due to complex implicit biases against female faculty created from centuries of societal norms [18]. While some suggest that there is no sex difference in intention to leave academic medicine [19], recent studies recount many reasons that discrepancy in advanced faculty titles or leadership positions exists [20–22]. The latter reflects a continuation of historical reports of women leaving academic medicine careers due to challenges in professional advancement, low salary, and issues with departmental leadership [22, 23].
One contributor to disparities among academic medicine faculty could be a lack of programming to foster a gender equitable environment within the institution [6]. Most programming that is available falls under professional development, focusing more on personal improvement rather than institution-wide interventions to address the recruitment, promotion, or retention of women [18]. While recommendations for both male and female mentors have been published [24], a recent review suggests that, across a variety of programs offered, mentorship experiences explicitly designed for women more significantly improve the retention of women faculty [8]. In addition, women faculty desire mentorship programs [25]. In this study, we highlight that this very population is also needed to serve in a mentoring capacity to female medical students. Respectively, this creates a need for both time to be mentored and programs to train faculty to be an effective student mentor.
Considering the unique role women educators serve, our study demonstrates yet another reason to recruit and retain female faculty. On promotion dossiers, mentorship is most likely listed under the “service” category, which is often allotted only a small percent effort toward promotion and has been reported to contribute to faculty fatigue [23, 26]. For some, mentorship is part of the “hidden work” disproportionately assigned to women [27]. This study shows a direct, positive impact of female faculty on the learner experience, thus serving as a call to action for medical teaching centers to protect time for women educators to devote to this important work.
This study demonstrates that all medical students view female faculty as an important presence in early medical education, both personally and for the broader medical curriculum. Given that the female medical student cohort currently has an equal presence in medical school, the lack of a female faculty presence is a problem worthy of attention now. In considering who is called upon to teach in the UME curriculum, medical institutions should assess the diversity of their faculty cohort, noting that a strong female faculty presence will bolster the medical student experience and perhaps serve as a feed-forward mechanism for mentorship of women in academic medicine.
Study Limitations
The data analyzed in our brief study represents one cohort of medical students from a single institution. It would be interesting to see if the data shift over time or whether such a trend is present at other academic medical institutions. We also acknowledge that our surveys include binary gender, as this was the data available for our faculty. As institutions expand their collection and reporting of genders beyond the binary, studies like this should be repeated to be more inclusive.
Supplementary Information
Below is the link to the electronic supplementary material.
Declarations
Ethics Approval
This work was designated non-human subject research by the IRB at the University of Cincinnati College of Medicine.
Competing Interests
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Heather R. Christensen, Email: heather.christensen@uc.edu
Ellie Sidler Bognar, Email: sidleree@mail.uc.edu.
References
- 1.AAMC Board of Directors. Applicants and Matriculants Data. Association of American Medical Colleges. https://www.aamc.org/data-reports/students-residents/interactive-data/2020-facts-applicants-and-matriculants-data. 2021. Accessed 18 Jul 2021.
- 2.Webster TL, Honeycutt KJ, Bekcer BJ, Haggar FL, Kennel VL, McBrien SB. Fix your leaky pipelines: support women in pursuit of advanced degrees. Med Sci Ed. 2021;31:795–804. doi: 10.1007/s40670-020-01184-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.AAMC Board of Directors. AAMC statement on gender equity. Association of American Medical Colleges. 2020. https://www.aamc.org/about-us/equity-diversity-inclusion/aamc-statement-gender-equity. Accessed 18 July 2020.
- 4.Babaria P, Bernheim S, Nunez-Smith M. Gender and the pre-clinical experiences of female medical students: a taxonomy. Med Educ. 2011;45(3):249–260. doi: 10.1111/j.1365-2923.2010.03856.x. [DOI] [PubMed] [Google Scholar]
- 5.Crosby RMH, Harden J. AMEE Guide No 20: The good teacher is more than a lecturer - the twelve roles of the teacher. Med Teach. 2000;22(4):334–347. doi: 10.1080/014215900409429. [DOI] [Google Scholar]
- 6.Farkas AH, Allenbaugh J, Bonifacino E, Turner R, Corbelli JA. Mentorship of US medical students: a systematic review. J Gen Intern Med. 2019;34(11):2602–2609. doi: 10.1007/s11606-019-05256-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Maudsley RF. Role models and the learning environment: essential elements in effective medical education. Acad Med. 2001;76(5):432–434. doi: 10.1097/00001888-200105000-00011. [DOI] [PubMed] [Google Scholar]
- 8.Wright S, Wong A, Newill C. The impact of role models on medical students. J Gen Intern Med. 1997;12(1):53–56. doi: 10.1007/s11606-006-0007-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tribune H. Gender matters in medical education introduction : the gender shift in medicine. 2017:111–126. 10.1007/978-3-319-02487-5.
- 10.Kassab S, Abu-Hijleh M, Al-Shboul Q, Hamdy H. Gender-related differences in learning in student-led PBL tutorials. Educ Heal. 2005;18(2):272–282. doi: 10.1080/13576280500148577. [DOI] [PubMed] [Google Scholar]
- 11.Bright CM, Duefield CA, Stone VE. Perceived barriers and biases in the medical education experience by gender and race. J Natl Med Assoc. 1998;90(11):681–688. [PMC free article] [PubMed] [Google Scholar]
- 12.Vu C, Farez R, Simpson P, Kaljo K. Gendered differences in teaching performance evaluations of obstetrics and gynecology residents. J Surg Educ. 2021;34(11):2602–2609. doi: 10.1016/j.jsurg.2021.04.011. [DOI] [PubMed] [Google Scholar]
- 13.Riese A, Rappaport L, Alverson B, Park S, Rockney RM. Clinical performance evaluations of third-year medical students and association with student and evaluator gender. Acad Med. 2017;92(6):835–840. doi: 10.1097/ACM.0000000000001565. [DOI] [PubMed] [Google Scholar]
- 14.Morgan HK, Purkiss JA, Porter AC, et al. Student evaluation of faculty physicians: gender differences in teaching evaluations. J Women’s Heal. 2016;25(5):453–456. doi: 10.1089/jwh.2015.5475. [DOI] [PubMed] [Google Scholar]
- 15.Heath JK, Weissman GE, Clancy CB, Shou H, Farrar JT, Dine CJ. Assessment of gender-based linguistic differences in physician trainee evaluations of medical faculty using automated text mining. JAMA Netw Open. 2019;2(5):e193520. 10.1001/jamanetworkopen.2019.3520. [DOI] [PMC free article] [PubMed]
- 16.Özgümüs A, Rau HA, Trautmann ST, König-Kersting C. Gender bias in the evaluation of teaching materials. Front Psychol. 2020;11. 10.3389/fpsyg.2020.01074. [DOI] [PMC free article] [PubMed]
- 17.Fassiotto M, Hamel EO, Ku M, et al. Women in academic medicine: measuring stereotype threat among junior faculty. J Women’s Heal. 2016;25(3):292–298. doi: 10.1089/jwh.2015.5380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Azam TU, Oxentenko AS. Gender parity in medical school does not equal gender parity in medical school leadership. J Women’s Heal. 2019;28(5):563–564. doi: 10.1089/jwh.2019.7762. [DOI] [PubMed] [Google Scholar]
- 19.Pololi LH, Krupat E, Civian JT, Ash AS, Brennan RT. Why are a quarter of faculty considering leaving academic medicine? A study of their perceptions of institutional culture and intentions to leave at 26 representative U.S. medical schools. Acad Med. 2012;87(7):859–869. 10.1097/ACM.0b013e3182582b18. [DOI] [PubMed]
- 20.Weavind L, Jobin MT. Women mentoring women in academic medicine: pathways to success. Int Anesthesiol Clin. 2018;56(3):110–120. doi: 10.1097/AIA.0000000000000192. [DOI] [PubMed] [Google Scholar]
- 21.Carr PL, Gunn CM, Kaplan SA, Raj A, Freund KM. Inadequate progress for women in academic medicine: findings from the national faculty study. J Women’s Heal. 2015;24(3):190–199. doi: 10.1089/jwh.2014.4848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cropsey KL, Masho SW, Shiang R, Sikka V, Kornstein SG, Hampton CL. Why do faculty leave? Reasons for attrition of women and minority faculty from a medical school: four-year results. J Women’s Heal. 2008;17(7):1111–1118. doi: 10.1089/jwh.2007.0582. [DOI] [PubMed] [Google Scholar]
- 23.Roper RL. Does gender bias still affect women in science? Microbiol Mol Biol Rev. 2019;83(3). 10.1128/MMBR.00018-19. [DOI] [PMC free article] [PubMed]
- 24.Marshall AL, Dversdal RK, Murphy M, Prill DM, Zhang T, Jain S. WOMENtorship: The #WomenInMedicine perspective. Med Teach. 2020;42(2):228–230. doi: 10.1080/0142159X.2019.1671967. [DOI] [PubMed] [Google Scholar]
- 25.Blood EA, Ullrich NJ, Hirshfeld-Becker DR, et al. Academic women faculty: are they finding the mentoring they need? J Women’s Heal. 2012;21(11):1201–1208. doi: 10.1089/jwh.2012.3529. [DOI] [PubMed] [Google Scholar]
- 26.Poole EL, Spies MA. Relationship among faculty fatigue, academic rank, and scholarship and service productivity. J Adv Nurs. July 2021:jan.14990. 10.1111/jan.14990. [DOI] [PubMed]
- 27.Delp L. Women’s hidden work Linda Delp. NEW Solut A J Environ Occup Heal Policy. 2011;20(4):415–419. doi: 10.2190/NS.20.4.b. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.