Abstract
Purpose:
To investigate the knowledge of myopia and its natural history including complications and clinical approaches for management adopted by optometrists across India.
Methods:
An online survey was distributed to Indian optometrists. A pre-validated questionnaire was adopted from previous literature. Respondents provided information about their demographics (gender, age, practice location, and modality), myopia knowledge, self-reported practice behaviors relating to childhood myopia, the information and evidence base used to guide their practice, and perceived extent of adult caregiver engagement in making management decisions for myopic children.
Results:
A total of 302 responses were collected from different regions of the country. Most respondents demonstrated knowledge of the association between high myopia and retinal breaks, retinal detachment and primary open-angle glaucoma. Optometrists used a range of techniques to diagnose childhood myopia, with a preference for non-cycloplegic refractive measures. The most common approaches to management were single-vision distance despite most optometrists identifying orthokeratology and low-dose (0.01%) topical atropine as two potentially more effective therapeutic interventions for controlling childhood myopia progression. Almost 90% of respondents considered increasing the time spent outdoors to be beneficial for reducing the rate of myopia progression. The main sources of information used to guide clinical practice were continuing education conferences, seminars, research articles, and workshops.
Conclusion:
Indian optometrists appear to be aware of emerging evidence and practices, but are not routinely adopting measures. Clinical guidelines, regulatory approval, and sufficient consultation time may be of value for assisting practitioners in making clinical decisions based on the current available research evidence.
Keywords: Indian optometrists, knowledge, myopia, myopia control, myopia progression
Myopia is a major challenge worldwide, giving rise to an epidemic in certain regions.[1] According to the World Health Organization (WHO), myopia is defined as a spherical equivalent refractive error of ≤ −0.5 D and about half of the world population is estimated to become myopic by 2050. High myopia is defined as a spherical equivalent refractive error of ≤ –5.00 D and is estimated to affect about 10% of the world population by 2050.[2] In 2010, it was estimated that uncorrected refractive error was the most common cause of distance vision impairment, affecting 1 billion population, and the second most common cause of blindness globally.[3] A recent systematic review and meta-analysis estimate that the percentage of the world’s population with myopia will increase from 22.9% in 2000 to 49.8% in 2050.[4] Additionally, by 2050, almost 1 billion people, or 9.8% of the world’s population, will have high myopia.[4] Similarly, a systematic review of myopia prevalence in India predicts that the prevalence of myopia in India will increase to 31.89% in 2030, 40.01% in 2040, and 48.14% in 2050.[5]
Tideman et al.[6] demonstrated that visual impairment is associated with axial length and spherical equivalent. Similarly, strategies should also be developed to prevent the development of myopia and its complication. Although myopia is a refractive error and is conventionally managed by optical or surgical correction, high myopia can result in visual morbidity. The risk of myopic complications increases with age and the progression of refractive error.[7] The pathological complications of myopia can range from vision impairment from uncorrected refractive error, reduced quality of life, increased risk of cataract, and open-angle glaucoma to the potentially blinding conditions of retinal detachment and myopic macular degeneration (MMD).[8,9]
There has been rising scientific interest in approaches that may prevent myopia development and/or reduce the rate of myopic progression, particularly in children. Several of these interventions are being implemented within eyecare practice based on promising research evidence and in the absence of regulatory approval. There is therefore a need to better understand the knowledge and comprehension of practitioners concerning myopia, and their clinical practices, as related to the diagnosis and management of childhood myopia.[10,11]
A wide range of these prevention strategies has been studied and proven to be effective in myopia control including spectacles (single-vision, bifocal, multifocal and peripheral aberration control), contact lenses (soft and rigid lens designs, including orthokeratology), pharmaceutical intervention (Atropine) and lifestyle changes (increasing time spent outdoors).[10,11]
Balaji and Vishwanathan have also shown that the anti-myopia strategies in India are only limited to single vision spectacles and lifestyle changes (increasing outdoor activities).[12] Additionally, the authors have also highlighted that lack of awareness and training could be the reason for the low uptake of myopia prevention strategies.[12]
To date, only three studies have evaluated and reported different clinical practice trends in myopia. The first was a cross-sectional survey of 971 eyecare practitioners, including optometrists, dispensing opticians and ophthalmologists, across Asia, Australasia, Europe, North America and South America,[13] the second was a survey of 173 eye care providers across different cities of Pakistan[14] and third being an online survey of 239 practitioners in different cities of Australia.[15]
To our knowledge, there are no published data in India that have reported the knowledge and clinical approaches in managing childhood myopia. Additionally, the interaction between optometrists and the adult caregivers of children with myopia, including what topics are discussed or how clinical decisions are made for myopia management strategies are also unknown or limited. The purpose of the present study was to investigate the knowledge of myopia, its natural history including complications and clinical approaches for the management adopted by optometrists across India.
Methods
A cross-sectional survey was conducted among optometrists practicing in India. The study was approved by the Institutional Review Board (IRB number: CLGEI-IEC/21-222/22) date of approval was 19/07/2022 and also adhered to the declarations of tenets of Helsinki. Informed consent was obtained from all participants before participating in the survey. A self-administered, electronic questionnaire (Google form) with a cover letter explaining the aim of the study was distributed through social media platforms such as WhatsApp (Facebook, Inc., USA) and Gmail (Google Corp., USA) asking each respondent to contribute to the survey by completing the questionnaire and also share with their social contacts. Invitations were sent either to phone numbers or email IDs.
Study questionnaire
A validated, well-structured questionnaire was adopted from previous literature.[15] Apart from demographic details, the following parameters were assessed:
-
(1)
Practitioner’s understanding of myopia, including its natural history and the associated risk of other eye diseases.
-
(2)
Self-reported clinical practice behaviors of practitioners, as related to myopia diagnosis and management in children (16 years of age or younger)
-
(3)
Information and evidence base used by clinicians to guide their clinical practice
-
(4)
Perception of optometrists of the extent of adult caregiver involvement in the decision-making process, as related to childhood myopia management.
Statistical analysis
Statistical analysis was performed using the SPSS software (Statistical Package for Social Sciences [IBM SPSS Statistics for Windows, Version 25.0. Armonk, NY: IBM Corp]). Demographic characteristics were summarized using descriptive statistics (frequencies, percentage, mean, and standard deviation). Survey questions comprising Likert scales were analyzed using ordinal logistic regression, with years of practice classified into an early career (0–5 years) and experienced clinicians (6 + years), practitioner interest in managing childhood myopia and primary practice location. Similarly, binomial logistic regression was used for dichotomous questions, with years of practice and practitioner interest in managing childhood myopia as independent factors. A P value of 0.05 or less was considered statistically significant.
Results
A total of 302 responses were collected from different regions. The ratio between males and females was 0.94:1. Similarly, the majority of the optometrists have experience between 0 and 5 years (77.5%). Almost three-fourths of the participants indicated their primary place of practice was a hospital (67.2%) followed by academic institutions (24.2%). Almost half of the respondents indicated providing clinical care to 5 or fewer every week. Most respondents were working in the state of Uttar Pradesh (44.3%), followed by Jharkhand (15.2%), Delhi (12%), and Punjab (6.6%). Additionally, 15 in every 20 participants possessed a research/clinical interest in managing childhood myopia.
Clinical procedure
Table 1 describes the routine clinical procedures for the examination of school-aged children, on initial presentation. The majority of participants indicated that they would prefer to take patient family history of myopia, undertake non-cycloplegic retinoscopy, non-cycloplegics subjective refraction, cycloplegic retinoscopy, and cover test for distance and near. More than half of the respondents indicated dilated subjective refraction (53.31%) and cycloplegic subjective refraction (55.63%). Additionally, almost 4 in 10 respondents preferred dynamic retinoscopy during the initial presentation. Lastly, peripheral refraction, stereopsis, retinal photography-periphery, optical coherence tomography (OCT), pupil size measurement, and corneal topography were unlikely to be preferred by respondents at the initial presentation of children with myopia.
Table 1.
Percentage of respondents who indicated performing each clinical procedure routinely on all school-aged children with myopia on initial presentation
| Clinical Procedure | % of respondents |
|---|---|
| Note patient family history of myopia | 85.76 |
| Non-cycloplegic (manifest) subjective refraction | 77.15 |
| Non-cycloplegic (manifest) retinoscopy | 66.89 |
| Cover test (distance and near phoria) | 64.24 |
| Cycloplegic retinoscopy | 63.58 |
| Cycloplegic subjective refraction | 55.63 |
| Dilated retinal fundus examination | 53.31 |
| Intraocular pressure | 49.01 |
| AC/A ratio | 43.38 |
| Axial length measurement | 41.06 |
| Dynamic retinoscopy (for example, MEM, Nott retinoscopy) | 40.07 |
| Cycloplegic autorefraction | 34.11 |
| Non-cycloplegic (manifest) autorefraction | 33.77 |
| Retinal fundus photography - posterior pole | 31.79 |
| Stereopsis | 29.47 |
| Un-dilated retinal evaluation | 25.50 |
| Corneal topography | 21.85 |
| Pupil size measurement | 21.52 |
| Peripheral refraction | 15.23 |
| Optical coherence tomography | 12.58 |
| Retinal fundus photography - peripheral | 11.26 |
AC/A: Accommodative Convergence/Accommodation), MEM: Monocular Estimation Method
Knowledge of ocular complication of high myopia
Practitioners were asked about their understanding of the association between high myopia (≥ −6.00 D) and the risk of incident ocular pathologies. Each of the correct responses (that is, retinal breaks, rhegmatogenous retinal detachment, and primary open-angle glaucoma) was selected by at least half of the respondents with retinal breaks being the maximum. However, knowledge regarding choroidal neovascularization and foveoschisis were found to be significantly low (1 in every 10 participants) [Table 2].
Table 2.
Percentage of respondents with ocular complications of high myopia
| Ocular conditions | % of respondents |
|---|---|
| Retinal breaks | 84.44 |
| Primary open-angle glaucoma | 49.34 |
| Rhegmatogenous retinal detachment | 45.03 |
| Foveoschisis | 15.89 |
| Cataract | 15.89 |
| Choroidal neo-vascularization | 15.56 |
| Exudative retinal detachment | 13.25 |
| Primary angle closure glaucoma | 10.93 |
| Diabetic retinopathy | 6.95 |
Management of myopia in children
Majority of the practitioners indicated increasing outdoor activity (86.42%) as effective approach to manage childhood myopia. Almost half of the respondents considered low-dose (0.01%) topical Atropine (49.01%) and visual hygiene (49.01%) as the other two most effective modalities [Table 3].
Table 3.
Percentage of respondents who indicated the most effective options for the management of Myopia
| Management approaches | % of respondents |
|---|---|
| Advice to increase time spent outdoors | 86.42 |
| Visual hygiene (for example, taking regular breaks with prolonged near work, maintaining appropriate working distance and good lighting) | 49.01 |
| Atropine (low-dose: 0.01%) eye drops | 49.01 |
| Single vision spectacles | 40.40 |
| Atropine (moderate dose: 0.1-0.5%) eye drops | 34.11 |
| Orthokeratology | 32.78 |
| Soft contact lenses (for example, distance-center, multifocal soft contact lenses) | 25.50 |
| Progressive addition spectacle lenses (multifocals) | 24.83 |
| Peripheral defocus | 23.18 |
| Bifocal spectacle lenses | 18.21 |
| Atropine (high dose >0.5%) eye drops | 6.95 |
| Cyclopentolate (1%) eye drops | 3.64 |
| Bifocal with prism | 3.64 |
Factors influencing management approaches
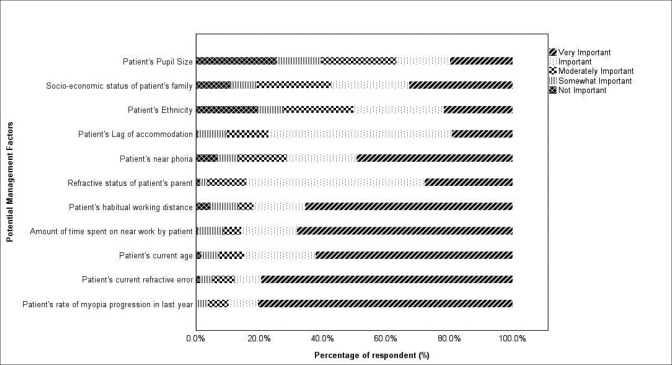
A number of factors that were considered important when deciding the myopia management strategy for children. These factors were from the patient’s [Fig. 1] and practitioner’s end [Fig. 2]. The rate of myopia progression of a child in the past 1 year along with the patient’s current refractive errors was the essential consideration, with almost 80%of optometrists rating it as very important. We found that the individuals who possessed an interest in managing myopia were more likely to indicate a rate of myopia progression (OR 4.63, 95% CI 2.52–8.50, P < 0.05) and current refractive error (OR 6.04, 95% CI 3.31–11.02, P < 0.05) as key factors for management. Similarly, Over 80% of participants indicated that the age of patients, patient’s habitual working distance, and the amount of time spent performing near work were important or very important. Pupil size of the patient (20%), socio-economic status of the family (37%), ethnicity of the patient (21%), and lag of accommodation (20%) were considered as least important factors in managing childhood myopia.
Figure 1.
Percentage of respondents (%) rating the relative importance of each factor when deciding upon the management approach for a child with myopia
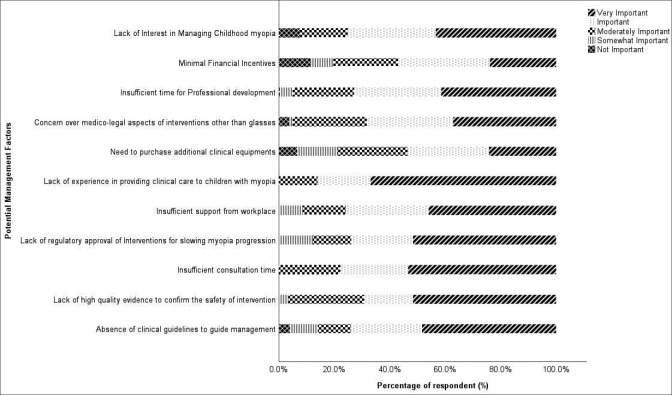
Figure 2.
Percentage of respondents (%) who rated the relative importance of each potential factor as a barrier limiting their ability to provide optimal clinical care to children with myopia
Regarding potential barriers to provide optimal myopia care [Fig. 2], the factors considered most important were lack of experience in providing clinical care to children with myopia, insufficient consultation time, lack of high-quality evidence to confirm the safety of interventions and lack of regulatory approval of intervention for slowing myopia progression. Individuals having a research and/or clinical interest in managing myopia indicated insufficient consultation time (OR 3.59, 95% CI 2.17–5.96, P < 0.05) and lack of high-quality evidence to confirm the safety of interventions (OR 1.97 95% CI 1.23–2.63, P < 0.05) were more likely to be most important barriers. Additionally, 4 in 10 participants indicated insufficient support from the workplace to be the most important potential barrier in managing myopia. Medico-legal aspects were less likely to be important for more experienced practitioners (OR 0.35, 95% CI 0.20–0.89, P = 0.08).
Source of information
Continued Educational activities (65.7%), continued educational conferences (62.7%), and original research articles (64.8%) were the three most useful sources of information in participants’ current approach in managing childhood myopia. Additionally, textbooks (22.5%) and industry information (15.2%) were indicated as least important source of information by respondents.
Topic of discussion with adult caregiver/parents
The majority of the participants were found to be engaged on the potential cause of myopia, options other than glasses for managing a child’s myopia, longer term risk of eye disease associated with myopia, and what myopia is.
Discussion
The purpose of the present study was to evaluate the understanding and knowledge of childhood myopia among optometrists practicing in India and their self-reported clinical practice pattern for diagnosis and management of myopia. The present study also considered the information used by eye care practitioners to guide their clinical practice. Additionally, this study also presumed that the optometrists/eye care practitioners will take help in discussing different topics on myopia with adult caregivers when discussing the management for children in India.
The self-reported survey was distributed on social platforms and had diversified respondents from different states of the country. However, the response rate in the present study was unknown as we could not able to measure the number of eye care practitioners who had received the questionnaire. However, it may be presumed that questionnaires were completed in the majority by practitioners interested in myopia control.
Experimental, epidemiological, and clinical research has shown that refractive development is influenced by both environmental and genetic factors. The eye growth and refractive maturation during infancy are tightly regulated by visually guided mechanisms as observed with an animal model, whereas observational data in human populations provide compelling evidence that environmental influences myopia susceptibility.[16,17]
The majority of the participants indicated they would note the patient’s family history of myopia during the initial presentation, followed by non-cycloplegics (manifest) retinoscopy, non-cycloplegics (manifest) subjective refraction, cover test, and cycloplegic retinoscopy. Lag of accommodation and peripheral refraction are known to be weakly associated with myopia progression.[18,19] The findings from the current study had also shown that these clinical examinations were opted for by a few eye care practitioners (MEM-4 in 10 participants; peripheral refraction-3 in 20 participants). A similar survey among Australian optometrists also reported a greater percentage of the similar procedure as our current study except for cycloplegic refraction.[15] In our study, we found more than one-half of the respondent indicated cycloplegic refraction because the previous study has also reported that cycloplegic refraction prevents the over-correction of myopia in children less than 12 years old.[20] Additionally, consensus-based American Optometric Association’s guidelines for comprehensive pediatric eye and vision examination also stated that cycloplegic refraction is the preferred procedure and is also used to quantify the refractive errors in the presence of visual conditions such as strabismus, amblyopia, and anisometropia. However, there had been a lack of published data to support or rebut the recommendations.[21]
Concerning knowledge regarding ocular complications, the majority of respondents were aware of incident risks of retinal breaks, rhegmatogenous retinal detachment and primary open-angle glaucoma associated with high myopia. However, 3 in 20 participants were aware of foveoschisis and choroidal neovascularization. Similar findings were noted in Douglass et al.’s[15] study where a majority of participants were not aware of ocular complications such as foveoschisis and choroidal neovascularization.
Given that there is a strong association between higher myopia and longer axial length.[22] ocular biometry is considered an important clinical parameter, particularly for monitoring the potential effects of interventions on axial elongation. In 2016, the US Food and Drug Administration Public Workshop on ‘Controlling the Progression of Myopia: Contact Lenses and Future Medical Devices’ recommended for axial length be adopted as a key outcome measure in myopia intervention trials. However, the current study revealed 4 in 10 respondents indicated axial length measurement.[23]
With regard to effective methods for the management of myopia and its progression, outdoor activity was indicated by most of the respondents in the current study. In a recent study, Bhandary et al.[24] also found that outdoor activity with an illuminance level of greater than 1000 lux significantly reduced the progression of myopia. Similarly, a recent meta-analysis consisting of data from three randomized controlled trials and six cohort studies reported that orthokeratology significantly reduced axial elongation relative to a control (single-vision distance) intervention.[25] Additionally, two studies named Atropine in the Treatment of Myopia (ATOM)[26] and ATOM 2[27] compared the safety and efficacy of different concentrations of Atropine eye drops in controlling myopia progression. The result of the study suggested that low-dose Atropine (0.01%) showed promising results as an effective intervention for slowing myopia progression with fewer side effects than the higher dose (0.1%, 0.5%). However, the current study found that orthokeratology was less likely indicated as an effective method compared with low-dose Atropine (0.01%).
Similarly, 1-year follow-up data from the Low-Concentration Atropine for Myopia Progression (LAMP) study, which was a double-masked placebo-controlled trial, has questioned the efficacy of 0.01% topical Atropine, relative to a 0.05% concentration, for slowing axial elongation.[28] A similar study done among Australian optometrists found that Ortho-k lenses and low-dose Atropine were more likely indicated methods for managing myopia.[15]
Most practitioners indicated the potential value of a range of resources to support their practice, including seminars, workshops, conferences, and original research articles. These findings suggest that optometrists prefer pre-appraised and synthesized evidence, over independently accessing primary sources and undertaking their appraisal and interpretation of research studies. These preferences mirror those reported for other areas of optometric practice, including dry eye disease[29,30] and age-related macular degeneration.[31]
The result of the study can be interpreted with some limitations. Firstly, the respondents were maximally limited to one state (Uttar Pradesh), which restrict the current study to generalize the results. Secondly, the survey was self-reported, which might have some possibilities of overestimation of knowledge and practice of childhood myopia.
Conclusion
The majority of participants indicated patient family history of myopia, undertake non-cycloplegic retinoscopy, non-cycloplegics subjective refraction, cycloplegic retinoscopy, and cover test for distance and near as routine clinical procedure during initial presentation. Similarly, axial length measures and dilated retinal fundus examinations were not routinely performed on initial presentation. Single-vision distance spectacle correction remained the first choice of myopia correction in school-aged children, despite practitioner awareness of the potential efficacy of other interventions, such as outdoor activities, orthokeratology, and low-dose atropine, for controlling myopia progression. Lastly, continued educational activities, continued educational conferences, and original research articles were the three most useful sources of information.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Congdon N, Burnett A, Frick K. The impact of uncorrected myopia on individuals and society. Community Eye Health. 2019;32:7–8. [PMC free article] [PubMed] [Google Scholar]
- 2.Holden B, Mariotti S, Kocur I. The impact of myopia and high myopia: Report of the Joint WHO–Brien Holden Vision Institute. Paper presented at: Global Scientific Meeting on Myopia 2015 [Google Scholar]
- 3.Bourne RR, Stevens GA, White RA, Smith JL, Flaxman SR, Price H, et al. Causes of vision loss worldwide, 1990–2010: A systematic analysis. Lancet Glob Health. 2013;1:e339–49. doi: 10.1016/S2214-109X(13)70113-X. [DOI] [PubMed] [Google Scholar]
- 4.Holden BA, Fricke TR, Wilson DA, Jong M, Naidoo KS, Sankaridurg P, et al. Global prevalence of myopia and high myopia and temporal trends from 2000 through 2050. Ophthalmology. 2016;123:1036–42. doi: 10.1016/j.ophtha.2016.01.006. [DOI] [PubMed] [Google Scholar]
- 5.Priscilla JJ, Verkicharla PK. Time trends on the prevalence of myopia in India–A prediction model for 2050. Ophthalmic Physiol Opt. 2021;41:466–74. doi: 10.1111/opo.12806. [DOI] [PubMed] [Google Scholar]
- 6.Tideman JW, Snabel MC, Tedja MS, Van Rijn GA, Wong KT, Kuijpers RW, et al. Association of axial length with risk of uncorrectable visual impairment for Europeans with myopia. JAMA Ophthalmol. 2016;134:1355–63. doi: 10.1001/jamaophthalmol.2016.4009. [DOI] [PubMed] [Google Scholar]
- 7.Saw S-M, Matsumura S, Hoang QV. Prevention and management of myopia and myopic pathology. Invest Ophthalmol Vis Sci. 2019;60:488–99. doi: 10.1167/iovs.18-25221. [DOI] [PubMed] [Google Scholar]
- 8.Haarman AEG, Enthoven CA, Tideman JWL, Tedja MS, Verhoeven VJM, Klaver CCW, et al. The complications of myopia:A review and meta-analysis. Invest Ophthalmol Vis Sci. 2020;61:49. doi: 10.1167/iovs.61.4.49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Choudhury F, Meuer SM, Klein R, Torres M, McKean-Cowdin R, Varma R, et al. Axial length and myopic macular degeneration prevalence among Chinese-Americans:The Chinese American Eye Study (CHES) Invest Ophthalmol Vis Sci. 2018;59:3958. [Google Scholar]
- 10.Walline JJ. Myopia control:A review. Eye Contact Lens. 2016;42:3–8. doi: 10.1097/ICL.0000000000000207. [DOI] [PubMed] [Google Scholar]
- 11.Huang J, Wen D, Wang Q, McAlinden C, Flitcroft I, Chen H, et al. Efficacy comparison of 16 interventions for myopia control in children:A network meta-analysis. Ophthalmology. 2016;123:697–708. doi: 10.1016/j.ophtha.2015.11.010. [DOI] [PubMed] [Google Scholar]
- 12.Balaji JJ, Viswanathan S. Practice patterns in managing myopia differs among Indian eye care practitioners. Indian J Ophthalmol. 2022;70:1848–9. doi: 10.4103/ijo.IJO_2486_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wolffsohn JS, Calossi A, Cho P, Gifford K, Jones L, Li M, et al. Global trends in myopia management attitudes and strategies in clinical practice. Cont Lens Anterior Eye. 2016;39:106–16. doi: 10.1016/j.clae.2016.02.005. [DOI] [PubMed] [Google Scholar]
- 14.Shahzad MA, Khan HA, Arshad MS, Sharjeel M, Yasin N, Jahangir S, et al. Knowledge, perspectives and practice patterns of eye care providers in Pakistan regarding myopia. Pak J Med Health Sci. 2022;16:746–50. [Google Scholar]
- 15.Douglass A, Keller PR, He M, Downie LE. Knowledge, perspectives and clinical practices of Australian optometrists in relation to childhood myopia. Clin Exp Optom. 2020;103:155–66. doi: 10.1111/cxo.12936. [DOI] [PubMed] [Google Scholar]
- 16.Wojciechowski R. Nature and nurture:The complex genetics of myopia and refractive error. Clin Genet. 2011;79:301–20. doi: 10.1111/j.1399-0004.2010.01592.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sherwin JC, Mackey DA. Update on the epidemiology and genetics of myopic refractive error. Expert Rev Ophthalmol. 2013;8:63–87. [Google Scholar]
- 18.Koomson NY, Amedo AO, Opoku-Baah C, Ampeh PB, Ankamah E, Bonsu K, et al. Relationship between reduced accommodative lag and myopia progression. Optom Vis Sci. 2016;93:683–91. doi: 10.1097/OPX.0000000000000867. [DOI] [PubMed] [Google Scholar]
- 19.Radhakrishnan H, Allen PM, Calver RI, Theagarayan B, Price H, Rae S, et al. Peripheral refractive changes associated with myopia progression. Invest Ophthalmol Vis Sci. 2013;54:1573–81. doi: 10.1167/iovs.12-10278. [DOI] [PubMed] [Google Scholar]
- 20.Fotedar R, Rochtchina E, Morgan I, Wang JJ, Mitchell P, Rose KA, et al. Necessity of cycloplegia for assessing refractive error in 12-year-old children:A population-based study. Am J Ophthalmol. 2007;144:307–9. doi: 10.1016/j.ajo.2007.03.041. [DOI] [PubMed] [Google Scholar]
- 21.Evidence based clinical practice guidelines. Comprehensive Pediatric eye and Vision Examination. “American Optometric Association (AOA)”. [[Last accessed on 2022 Sep 15]]. Available from: https://www.aoa.org/AOA/Documents/Practice%20Management/Clinical%20Guidelines/EBO%20Guidelines/Comprehensive%20Pediatric%20Eye%20and%20Vision%20Exam.pdf .
- 22.Ip JM, Huynh SC, Kifley A, Rose KA, Morgan IG, Varma R, et al. Variation of the contribution from axial length and other oculometric parameters to refraction by age and ethnicity. Invest Ophthalmol Vis Sci. 2007;48:4846–53. doi: 10.1167/iovs.07-0101. [DOI] [PubMed] [Google Scholar]
- 23.Food and Drug Administration. Controlling the Progression of Myopia: Contact Lenses and Future Medical Devices; Public Workshop. In: FDA. White Oak Campus: Silver Spring, MD: 2016. [Google Scholar]
- 24.Bhandary SK, Dhakal R, Sanghavi V, Verkicharla PK. Ambient light level varies with different locations and environmental conditions:Potential to impact myopia. PloS One. 2021;16:e0254027. doi: 10.1371/journal.pone.0254027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Li SM, Kang MT, Wu SS, Liu LR, Li H, Chen Z, et al. Efficacy, safety and acceptability of orthokeratology on slowing axial elongation in myopic children by meta-analysis. Curr Eye Res. 2016;41:600–8. doi: 10.3109/02713683.2015.1050743. [DOI] [PubMed] [Google Scholar]
- 26.Chua WH, Balakrishnan V, Chan YH, Tong L, Ling Y, Quah BL, et al. Atropine for the treatment of childhood myopia. Ophthalmology. 2006;113:2285–91. doi: 10.1016/j.ophtha.2006.05.062. [DOI] [PubMed] [Google Scholar]
- 27.Chia A, Chua WH, Cheung YB, Wong WL, Lingham A, Fong A, et al. Atropine for the treatment of childhood myopia:Safety and efficacy of 0.5%, 0.1%, and 0.01% doses (Atropine for the Treatment of Myopia 2) Ophthalmology. 2012;119:347–54. doi: 10.1016/j.ophtha.2011.07.031. [DOI] [PubMed] [Google Scholar]
- 28.Yam JC, Jiang Y, Tang SM, Law AK, Chan JJ, Wong E, et al. Low-concentration atropine for myopia progression (LAMP) study:A randomized, double-blinded, placebo-controlled trial of 0.05%, 0.025%, and 0.01% atropine eye drops in myopia control. Ophthalmology. 2019;126:113–24. doi: 10.1016/j.ophtha.2018.05.029. [DOI] [PubMed] [Google Scholar]
- 29.Downie LE, Rumney N, Gad A, Keller PR, Purslow C, Vingrys AJ, et al. Comparing self-reported optometric dry eye clinical practices in Australia and the United Kingdom:Is there scope for practice improvement? Ophthalmic Physiol Opt. 2016;36:140–51. doi: 10.1111/opo.12280. [DOI] [PubMed] [Google Scholar]
- 30.Downie L, Keller P, Vingrys A. An evidence-based analysis of Australian optometrists'dry eye practices. Optom Vis Sci. 2013;90:1385–95. doi: 10.1097/OPX.0000000000000087. [DOI] [PubMed] [Google Scholar]
- 31.Downie L, Keller P. The self-reported clinical practice behaviors of Australian optometrists as related to smoking, diet and nutritional supplementation. PLoS One. 2015;10:e0124533. doi: 10.1371/journal.pone.0124533. [DOI] [PMC free article] [PubMed] [Google Scholar]