Abstract
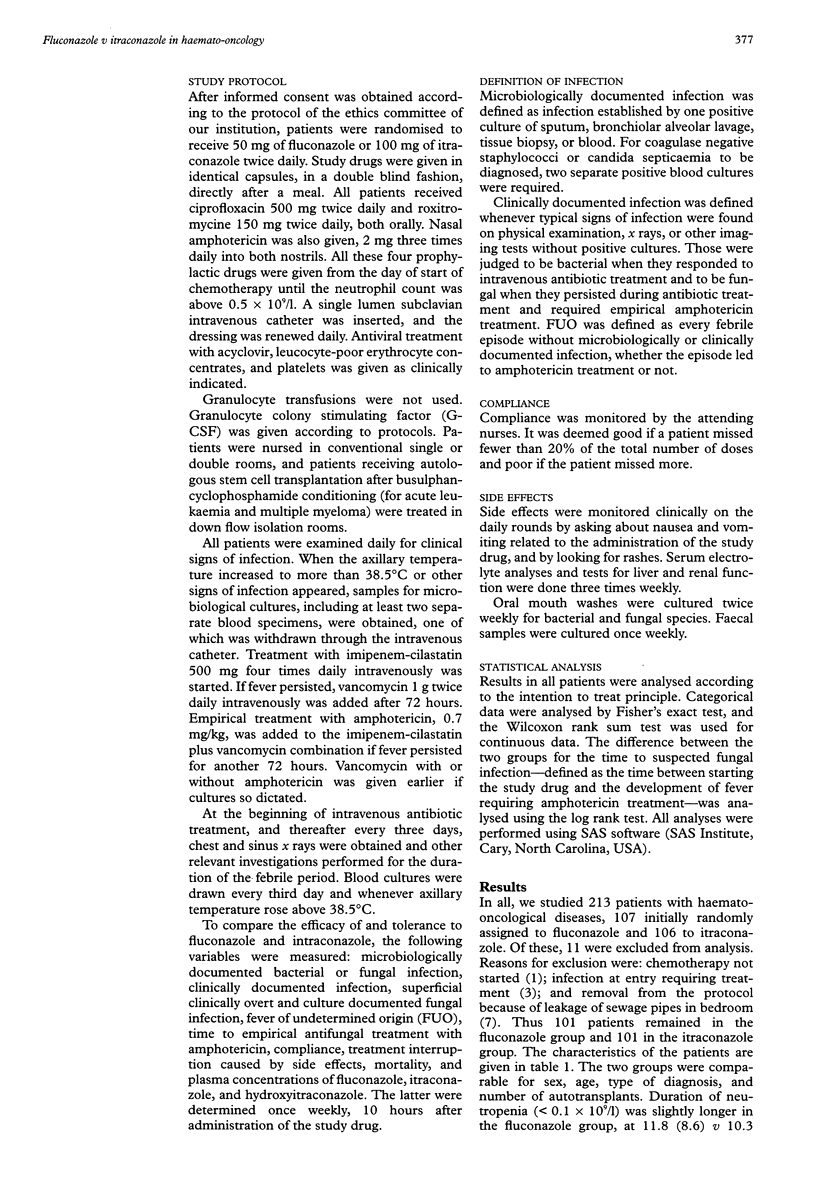
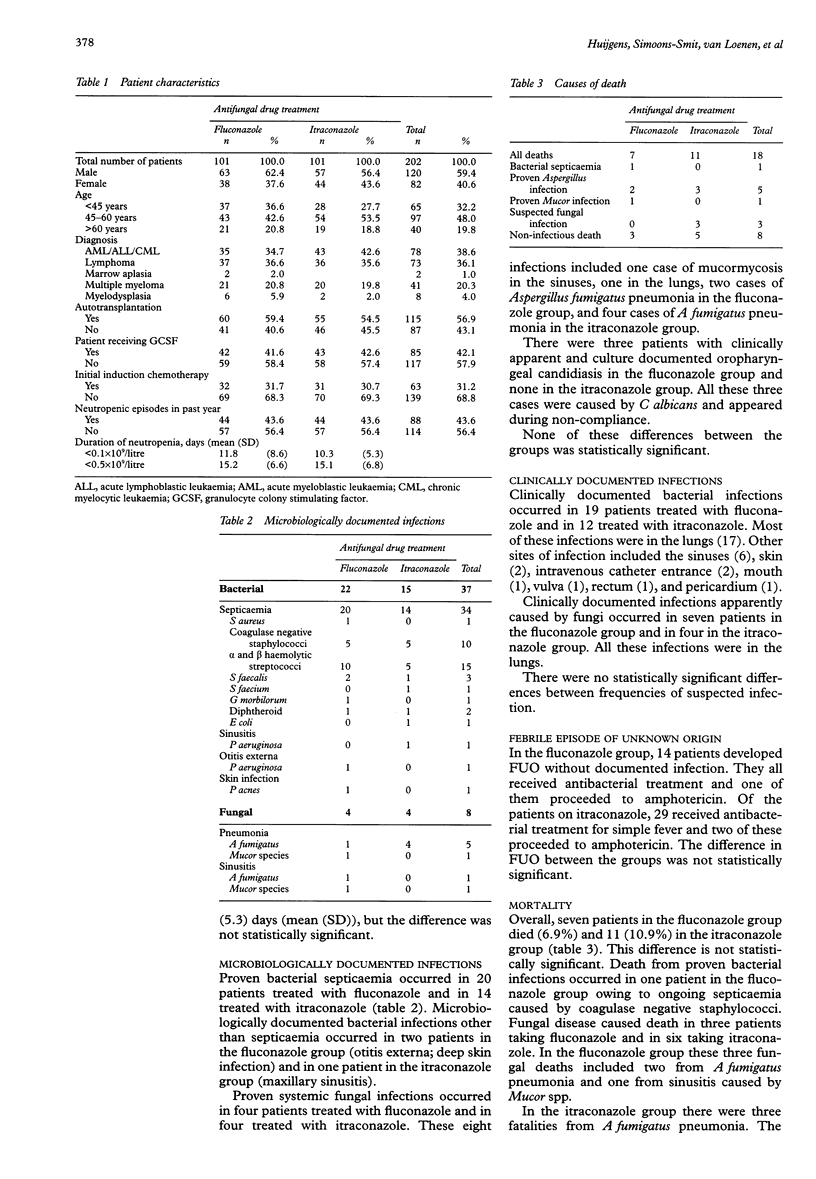
AIMS: To compare the efficacy of and tolerance to oral fluconazole and intraconazole in preventing fungal infection in neutropenic patients with haematological malignancies. PATIENTS: 213 consecutive, afebrile adult patients treated with or without autologous stem cell transplantation for haematological malignancies. METHODS: A randomised, double blind, single centre study. Patients were randomly assigned to receive fluconazole 50 mg or itraconazole 100 mg, both twice daily in identical capsules. An intention to treat analysis was performed on 202 patients, 101 in each group. RESULTS: Microbiologically documented systemic fungal infections occurred in four patients in each group. Clinical fungal infection was thought to be present in seven recipients of fluconazole and four of itraconazole. In all 202 patients, 29 proceeded to intravenous amphotericin (amphotericin B), 16 in the fluconazole group and 13 in the itraconazole group. Superficial fungal infection was seen only in three non-compliant patients in the fluconazole group. All these infections were oral. No major differences were noted in the isolates of fungi in mouth washes and fecal samples. Overall mortality was 8.9% (18 deaths; seven in the fluconazole group, 11 in the itraconazole group). Mortality from microbiologically and clinically documented fungal infection was 4.5% (nine deaths; three in the fluconazole group, six in the itraconazole group). Median time to suspected or proven fungal infection was 16 days in both groups. None of these comparisons reached statistical significance (p < 0.05). No major clinical toxicity was noted and compliance was excellent. CONCLUSIONS: In neutropenic patients treated for haematological malignancies with or without autologous stem cell transplantation, fluconazole and itraconazole in low doses result in a similar low frequency of fungal disease. Fluconazole may be the preferable drug because of the smaller number of capsules and lack of need for timing relative to meals.
Full text
PDF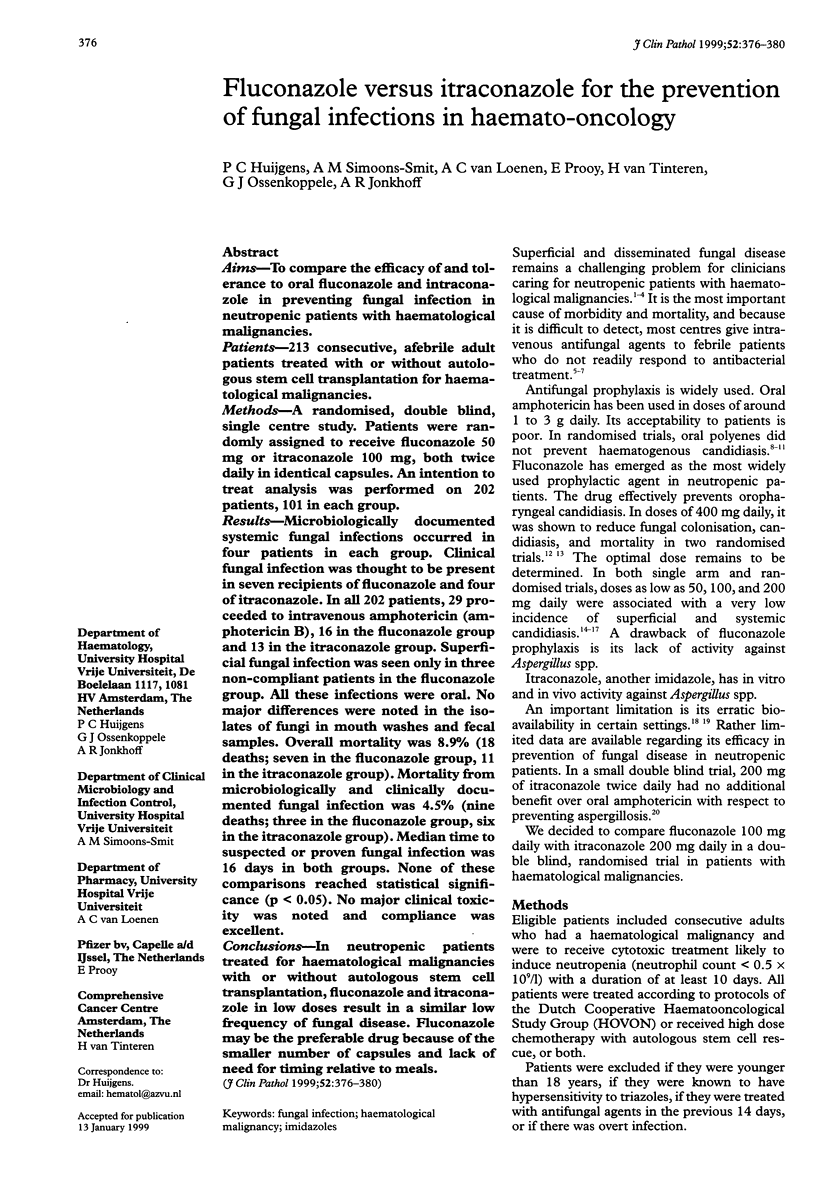

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Alangaden G., Chandrasekar P. H., Bailey E., Khaliq Y. Antifungal prophylaxis with low-dose fluconazole during bone marrow transplantation. The Bone Marrow Transplantation Team. Bone Marrow Transplant. 1994 Dec;14(6):919–924. [PubMed] [Google Scholar]
- Boogaerts M. A., Verhoef G. E., Zachee P., Demuynck H., Verbist L., De Beule K. Antifungal prophylaxis with itraconazole in prolonged neutropenia: correlation with plasma levels. Mycoses. 1989;32 (Suppl 1):103–108. doi: 10.1111/j.1439-0507.1989.tb02299.x. [DOI] [PubMed] [Google Scholar]
- Bow E. J., Mandell L. A., Louie T. J., Feld R., Palmer M., Zee B., Pater J. Quinolone-based antibacterial chemoprophylaxis in neutropenic patients: effect of augmented gram-positive activity on infectious morbidity. National Cancer Institute of Canada Clinical Trials Group. Ann Intern Med. 1996 Aug 1;125(3):183–190. doi: 10.7326/0003-4819-125-3-199608010-00004. [DOI] [PubMed] [Google Scholar]
- Buchanan A. G., Riben P. D., Rayner E. N., Parker S. E., Ronald A. R., Louie T. J. Nystatin prophylaxis of fungal colonization and infection in granulocytopenic patients: correlation of colonization and clinical outcome. Clin Invest Med. 1985;8(2):139–147. [PubMed] [Google Scholar]
- Deaney N. B., Tate H. A meta-analysis of clinical studies of imipenem-cilastatin for empirically treating febrile neutropenic patients. J Antimicrob Chemother. 1996 May;37(5):975–986. doi: 10.1093/jac/37.5.975. [DOI] [PubMed] [Google Scholar]
- Goodman J. L., Winston D. J., Greenfield R. A., Chandrasekar P. H., Fox B., Kaizer H., Shadduck R. K., Shea T. C., Stiff P., Friedman D. J. A controlled trial of fluconazole to prevent fungal infections in patients undergoing bone marrow transplantation. N Engl J Med. 1992 Mar 26;326(13):845–851. doi: 10.1056/NEJM199203263261301. [DOI] [PubMed] [Google Scholar]
- Gøtzsche P. C., Johansen H. K. Meta-analysis of prophylactic or empirical antifungal treatment versus placebo or no treatment in patients with cancer complicated by neutropenia. BMJ. 1997 Apr 26;314(7089):1238–1244. doi: 10.1136/bmj.314.7089.1238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huijgens P. C., Ossenkoppele G. J., Weijers T. F., van Loenen A. C., Simoons-Smit A. M., Wijermans P. W., van Pampus E. C., Langenhuijsen M. M. Imipenem-cilastatin for empirical therapy in neutropenic patients with fever: an open study in patients with hematologic malignancies. Eur J Haematol. 1991 Jan;46(1):42–46. doi: 10.1111/j.1600-0609.1991.tb00512.x. [DOI] [PubMed] [Google Scholar]
- Huijgens P. C., van Loenen A. C., Simoons-Smit A. M., Prooy E., Ossenkoppele G. J. The prophylactic use of fluconazole 50 vs. 100 mg daily in haematological malignancies. Eur J Cancer. 1993;29A(6):926–927. doi: 10.1016/s0959-8049(05)80444-7. [DOI] [PubMed] [Google Scholar]
- Kunová A., Trupl J., Spánik S., Drgona L., Sufliarsky J., Lacka J., Studená V., Hlavácová E., Studená M., Kukucková E. Candida glabrata, Candida krusei, non-albicans Candida spp., and other fungal organisms in a sixty-bed national cancer center in 1989-1993: no association with the use of fluconazole. Chemotherapy. 1995 Jan-Feb;41(1):39–44. doi: 10.1159/000239322. [DOI] [PubMed] [Google Scholar]
- Levine A. S., Siegel S. E., Schreiber A. D., Hauser J., Preisler H., Goldstein I. M., Seidler F., Simon R., Perry S., Bennett J. E. Protected environments and prophylactic antibiotics. A prospective controlled study of their utility in the therapy of acute leukemia. N Engl J Med. 1973 Mar 8;288(10):477–483. doi: 10.1056/NEJM197303082881001. [DOI] [PubMed] [Google Scholar]
- Menichetti F., Del Favero A., Martino P., Bucaneve G., Micozzi A., D'Antonio D., Ricci P., Carotenuto M., Liso V., Nosari A. M. Preventing fungal infection in neutropenic patients with acute leukemia: fluconazole compared with oral amphotericin B. Ann Intern Med. 1994 Jun 1;120(11):913–918. doi: 10.7326/0003-4819-120-11-199406010-00003. [DOI] [PubMed] [Google Scholar]
- Pizzo P. A. Management of fever in patients with cancer and treatment-induced neutropenia. N Engl J Med. 1993 May 6;328(18):1323–1332. doi: 10.1056/NEJM199305063281808. [DOI] [PubMed] [Google Scholar]
- Pizzo P. A., Robichaud K. J., Gill F. A., Witebsky F. G. Empiric antibiotic and antifungal therapy for cancer patients with prolonged fever and granulocytopenia. Am J Med. 1982 Jan;72(1):101–111. doi: 10.1016/0002-9343(82)90594-0. [DOI] [PubMed] [Google Scholar]
- Prentice A. G., Warnock D. W., Johnson S. A., Phillips M. J., Oliver D. A. Multiple dose pharmacokinetics of an oral solution of itraconazole in autologous bone marrow transplant recipients. J Antimicrob Chemother. 1994 Aug;34(2):247–252. doi: 10.1093/jac/34.2.247. [DOI] [PubMed] [Google Scholar]
- Prentice A. G., Warnock D. W., Johnson S. A., Taylor P. C., Oliver D. A. Multiple dose pharmacokinetics of an oral solution of itraconazole in patients receiving chemotherapy for acute myeloid leukaemia. J Antimicrob Chemother. 1995 Oct;36(4):657–663. doi: 10.1093/jac/36.4.657. [DOI] [PubMed] [Google Scholar]
- Preston S. L., Briceland L. L. Fluconazole for antifungal prophylaxis in chemotherapy-induced neutropenia. Am J Health Syst Pharm. 1995 Jan 15;52(2):164–206. doi: 10.1093/ajhp/52.2.164. [DOI] [PubMed] [Google Scholar]
- Rex J. H., Pfaller M. A., Galgiani J. N., Bartlett M. S., Espinel-Ingroff A., Ghannoum M. A., Lancaster M., Odds F. C., Rinaldi M. G., Walsh T. J. Development of interpretive breakpoints for antifungal susceptibility testing: conceptual framework and analysis of in vitro-in vivo correlation data for fluconazole, itraconazole, and candida infections. Subcommittee on Antifungal Susceptibility Testing of the National Committee for Clinical Laboratory Standards. Clin Infect Dis. 1997 Feb;24(2):235–247. doi: 10.1093/clinids/24.2.235. [DOI] [PubMed] [Google Scholar]
- Rozenberg-Arska M., Dekker A. W., Branger J., Verhoef J. A randomized study to compare oral fluconazole to amphotericin B in the prevention of fungal infections in patients with acute leukaemia. J Antimicrob Chemother. 1991 Mar;27(3):369–376. doi: 10.1093/jac/27.3.369. [DOI] [PubMed] [Google Scholar]
- Sable C. A., Donowitz G. R. Infections in bone marrow transplant recipients. Clin Infect Dis. 1994 Mar;18(3):273–284. doi: 10.1093/clinids/18.3.273. [DOI] [PubMed] [Google Scholar]
- Saral R. Candida and Aspergillus infections in immunocompromised patients: an overview. Rev Infect Dis. 1991 May-Jun;13(3):487–492. doi: 10.1093/clinids/13.3.487. [DOI] [PubMed] [Google Scholar]
- Schimpff S. C., Greene W. H., Young V. M., Fortner C. L., Cusack N., Block J. B., Wiernik P. H. Infection prevention in acute nonlymphocytic leukemia. Laminar air flow room reverse isolation with oral, nonabsorbable antibiotic prophylaxis. Ann Intern Med. 1975 Mar;82(3):351–358. doi: 10.7326/0003-4819-82-3-351. [DOI] [PubMed] [Google Scholar]
- Williams C., Whitehouse J. M., Lister T. A., Wrigley P. F. Oral anticandidal prophylaxis in patients undergoing chemotherapy for acut- leukemia. Med Pediatr Oncol. 1977;3(3):275–280. doi: 10.1002/mpo.2950030309. [DOI] [PubMed] [Google Scholar]
- Winston D. J., Chandrasekar P. H., Lazarus H. M., Goodman J. L., Silber J. L., Horowitz H., Shadduck R. K., Rosenfeld C. S., Ho W. G., Islam M. Z. Fluconazole prophylaxis of fungal infections in patients with acute leukemia. Results of a randomized placebo-controlled, double-blind, multicenter trial. Ann Intern Med. 1993 Apr 1;118(7):495–503. doi: 10.7326/0003-4819-118-7-199304010-00003. [DOI] [PubMed] [Google Scholar]


