Abstract
Background
While previous studies have identified a range of factors associated with mask wearing in the US, little is known about drivers of mask-wearing among racial and ethnic minority groups. This analysis assessed whether factors positively associated with wearing a mask early in the pandemic differed between participants grouped by race/ethnicity (Hispanic, non-Hispanic Black, non-Hispanic Asian, and non-Hispanic White).
Method
Data were obtained from a US internet panel survey of 3217 respondents during May–November 2020 (weighted by race/ethnicity, age, gender, and education to the US national population). Within each of the four available racial/ethnic groups, crude and adjusted odds ratios (COR and AOR) were calculated using logistic regression to assess factors positively associated with wearing a mask. Adjusted models were controlled for age, gender, education, county COVID-19 case count, presence of a state-issued mask mandate, and interview month.
Results
The following variables were most strongly positively associated with mask wearing (p<0.05) in each racial/ethnic group: Hispanic—seeing others wearing masks (AOR: 6.7), importance of wearing a mask combined with social distancing (AOR: 3.0); non-Hispanic Black—belief that wearing a mask would protect others from coronavirus (AOR: 5.1), reporting hearing that one should wear a mask (AOR: 3.6); non-Hispanic Asian—belief that people important to them believe they should wear a mask (COR: 5.1, not statistically significant); and non-Hispanic White—seeing others wearing masks (AOR: 3.1), importance of wearing a mask (AOR: 2.3).
Conclusion
Public health efforts to encourage mask wearing should consider the diversity of behavioral influences within different population groups.
Keywords: SARS cov-2, COVID-19, Masks, Health equity, Hispanic health, Black/African American
Throughout much of the COVID-19 pandemic in the USA, Hispanic, non-Hispanic Black, and American Indian or Alaska Native persons have been at significantly higher risk of experiencing serious illness and mortality compared to non-Hispanic White persons [1, 2]. From early in the pandemic, there have been calls to address the racial and ethnic health disparities driving increased COVID-19 mortality [3–5]. One way to accomplish this goal is to prioritize the promotion of protective measures such as mask wearing among groups at elevated risk of exposure to the virus and of worse outcomes when infected.
Health Behavior Theory Applied to Mask Wearing Promotion During COVID-19
“Health behavior theory” is a term that refers collectively to numerous theoretical models that help explain why individuals engage in behaviors that may positively or negatively affect their health and what factors contribute to those behaviors [6]. Although health behavior theory encompasses a wide range of explanatory models, together, it represents a consistent approach to understanding (and potentially influencing) health-related behavior, and it assumes that behaviors are the predictable result of individual, interpersonal, social, cultural, and societal factors. While there is no one model that explains all behavior, applying one or more models to situations in which people’s behavior can either protect them or put them at increased risk for disease can help clarify what is driving behavior [7]. Some examples of factors examined in behavioral theory models are the perceived risk from a disease [8], one’s attitude (positive, negative) towards a behavior, confidence that one can perform a behavior (self-efficacy) [9], and a belief that others perform the behavior and believe that you should also (social norms) [10].
In order to measure the presence or absence of these factors, behavioral scientists often conduct surveys in which they provide statements that express an attitude or perception, and ask participants to rate the extent to which they agree with the statement. Ideally, scientists are able to present multiple variations of a statement, including some versions that present the statement in the negative. With responses to multiple statements factored together, we can “construct” a measure of an attitude or perception. For this reason, the resulting measures are called “behavioral theory constructs.” However, there is no established consensus on the number of statements to use to represent a behavioral theory construct.
Prior Behavioral Theory-Based Analysis of Predictors of Mask Wearing During COVID-19
Prior research by Barile et al. [11], applied behavioral theory to mask wearing behavior during COVID-19. They identified associations between behavioral theory-based predictors and self-reported mask wearing frequency using survey data collected during May and June of 2020. They used predictors primarily derived from the theory of planned behavior: attitudes, perceived subjective norms, and perceived behavioral control [9]. In the context of mask wearing during COVID-19, “attitudes” refer to an individual’s feelings about mask-wearing, “perceived subjective norms” are the perceived social pressures to wear a mask, and “perceived behavioral control” refers to an individual’s belief in their ability to successfully wear a mask. Another behavioral theory construct of interest was how intention to wear a mask may be more or less likely to result in a mask being actually worn based on other factors. The team used data from a cross-sectional panel survey of US adults conducted in May and June 2020 (N = 1004).
Barile et al. found that perceived subjective norms, perceived behavioral control, and attitudes toward the behavior were all positively associated with intention to wear a face covering in public. They further found that the intention to wear a face covering was positively associated with self-reported wearing of a face covering if other people were observed wearing face coverings in public, although this effect appeared slightly stronger with cloth face coverings than other types of masks. They concluded that the intention to wear face coverings and observing other people wearing them are important behavioral predictors of adherence to the CDC recommendation to wear face coverings in public.
Behavioral Theory Model Featuring Race/Ethnic Group as a Social Environment
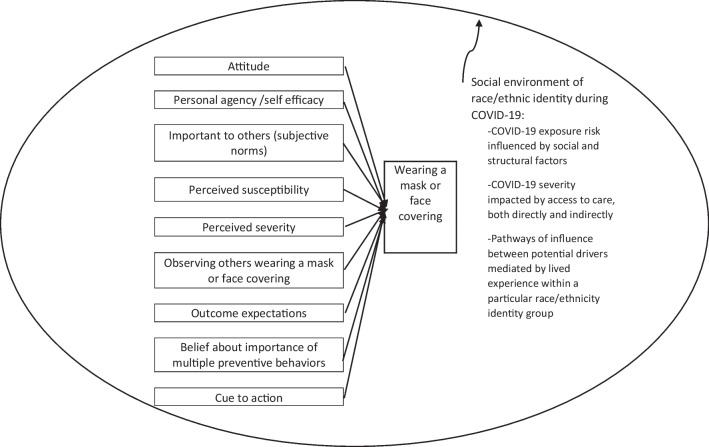
In this analysis, we analyze the same survey data, but with several more months added (July–November 2020). We build on the approach of Barile and colleagues, using many of the same behavioral constructs, but we also have added a new “social environment” element that comes from social ecological theory [12]. This theory focuses on the influence that social environments at multiple levels can have on an individual’s behavior. In the context of COVID-19, belonging to a particular racial/ethnic group can result in experiencing a different social environment around mask wearing, whether due to race-based bias, limited access to health care that leaves one more vulnerable to COVID-19 effects, or a concern about how one will be viewed when wearing a mask. Framed this way, identifying as a member of a particular racial/ethnic group suggests exposure to a particular social environment that might influence mask wearing behavior and might even affect the ways that different behavior theory-based constructs influence this behavior.
Figure 1 below provides a graphic illustration of the analytic model which incorporates both theories. This model is different from that of Barile et al. [11] in a few important ways. The current model takes a less granular view of the relationship between intention and behavior and also defines the outcome of interest as wearing a mask of any type (not distinguishing between cloth and other types). This model also incorporates three additional behavioral theory constructs: outcome expectations, belief about the importance of multiple preventive behaviors, and cues to action. The most significant revision is the addition of the social environment (represented by the circle) of racial/ethnic group membership as a context within which mask wearing behavior occurs [12].
Fig. 1.
Theory-based model for associations assessed for mask wearing within four distinct social environments (lived experiences of race/ethnicity during COVID-19)
Several social environmental factors around race/ethnicity are particularly salient in the COVID-19 context: the heightened risk of infection with SARS-CoV-2 for individuals within some racial/ethnic groups due to differences in employment opportunities; poorer health outcomes after COVID-19, both due to poor access to treatment and access to preventive health care over the life cycle; and a range of race/ethnicity-specific experiences that may influence a person’s likelihood of wearing a mask.
While it is not possible with available data to test the effects of social environment directly, by testing associations between behavioral theory constructs within four groups of race/ethnicity separately we can get an indirect indication of whether social environment may influence behavior. With four separate models, controlling for a large number of demographic factors, we see whether positively correlated behavioral theory constructs are similar across all groups, or different. We hypothesize that analyses conducted separately for each major group of race/ethnicity using the same protocol will result in different behavior theory-based constructs being positively associated with mask wearing behavior. In order to make this analysis possible, data from seven monthly survey rounds were pooled, and respondents were grouped by race/ethnicity regardless of survey month. This significantly larger sample size makes it possible to evaluate behavior theory-based constructs within four major groups of race/ethnicity: Hispanic, non-Hispanic Black (“Black”), non-Hispanic Asian (“Asian”), and non-Hispanic White (“White”). This analysis looks at what COVID-19-related behavior theory constructs are most strongly associated with mask wearing behavior in each of these groups and also at whether applying a similar process separately in four different social environments results in similar results in each group.
While a growing body of evidence exists regarding attitudes, beliefs, and perceived social norms associated with mask wearing behavior for the US population as a whole [11, 13–24], far less is known about drivers and barriers within racial and ethnic minority groups [25–30]. It is important to distinguish studies about what drives mask wearing behavior (or impedes it) from studies that simply describe differences in mask wearing frequency by racial and ethnic group [31]. The latter does not provide any guidance for community-based communication strategies to increase mask wearing. In other health fields (e.g., cancer screening, exercise intentions, and arthritis treatment), studies of barriers and drivers to self-protective behaviors have revealed different behavioral drivers and barriers to exist in different racial/ethnic groups [32–35].
While this work is grounded in theory, our goal is also practical. In addition to exploring relationships between behavioral theory constructs and mask wearing behaviors in four separate social environments of race/ethnicity, we seek to demonstrate a process by which actionable drivers of mask wearing can be identified and used for intervention development. We do not intend for the specific results obtained from this national online survey to be used to develop mask promotion interventions, but rather that the process be replicated in each local community to guide evidence-based intervention development.
Methods
The analytic dataset came from a series of on-line panel surveys collected for the CDC COVID-19 response by an internet panel survey company [36]. The primary purpose of the surveys was to periodically assess a national sample of adults on their experiences, beliefs, and attitudes about COVID-19 and self-protection and to use results to guide COVID-19 response activities. One of the self-protection behaviors measured was wearing a mask or face covering. The survey data was weighted to represent the 2010 US population in terms of age, sex, race/ethnicity, and education.
The surveys were administered monthly to an opt-in new sample of approximately 500 adults (not surveyed previously) from the continental US aged ≥18 years. Quota sampling and statistical weighting were employed to reflect the US population by gender, age, region, race/ethnicity, and education. Participants were recruited to participate in an on-line survey via mail and other publicity and, once enrolled, were screened to assure that the participant had not participated in another online survey within the last six weeks. As the survey was intended to “take the pulse” of the national population during the pandemic, data was collected exclusively through a self-administered internet-based survey. This activity was reviewed by CDC and was conducted consistent with applicable federal law and CDC policy [39, 40].
In order analyze the survey data by race/ethnicity, the seven monthly surveys were merged, creating a single dataset in which month of survey completion was a variable. Five additional county-level variables were added to the dataset: COVID-19 case and death counts (each for the previous day and cumulatively from the first local case) [37] and whether a state-issued mask mandate was in effect in the respondent’s county on the date of interview [38].
To match the county-level variables with respondents, the zip code provided by respondents was assigned a county FIPS code using the US Department of Housing and Urban Development-US Postal Service zip code crosswalk file [41]. For the 879 (27%) respondents whose zip code matched multiple counties, the county with the highest proportion of the zip code’s residential addresses was assigned as the county of residence.
Categorization of Race/Ethnicity Group
To analyze data by race and ethnicity, mutually exclusivegroups of participants were created: Hispanic, Black, Asian, White, and “multiple or other race.” First, any respondent indicating Hispanic ethnicity was classified as Hispanic, regardless of race. Next, the remaining participants (non-Hispanic) who reported Black, Asian, or White as their race were classified accordingly. All non-Hispanic respondents reporting race as American Indian or Alaska Native, Native Hawaiian, other Pacific Islander or reporting more than one race were classified as “multiple or other race.” Due to the small sample size and heterogeneity of the “multiple or other race” category, this group was excluded from the analysis.
Outcome Variable
The main outcome of interest was “always” wearing a mask when going out in public in the previous week. Since the survey asked two separate questions about wearing a cloth mask and about wearing any other kind of mask, a response of “always” to either question constituted “always” wearing a mask. Both questions contained the same format: “In the past week, when you have gone outside of your home for work, grocery shopping, or other activities that involved interacting with other people, how often did you wear [a cloth face covering/paper disposable mask, surgical mask, dust mask, or other respirator, such as an N95] that covered your nose and mouth?” “Always” by itself was selected for the outcome because “always” wearing a mask was the intended behavior and because a very large proportion of respondents reported “always” wearing a mask. The comparison of the intended response versus all other responses was both advantageous because it would be the goal of any future intervention and reasonable analytically because it provided sufficient sample size in both response groups to make modelling of the relatively small racial/ethnic groups possible.
Independent Variables: Attitudes, Beliefs, and Perceptions About COVID-19 and Mask Wearing
As described by Barile et al. (2020) [11], the surveys were designed to include measures of several COVID-19-related attitudes, beliefs, and perceptions recognized in behavioral theory to often influence behavior [42]. Consistent with theory, these attitudes, beliefs, and perceptions (“behavioral theory constructs”) [43] were measured by presenting construct-related statements and asking participants to rate their level of agreement (“disagree,” “neither agree nor disagree,” and “agree”) with the statement. For example, a participant’s level of agreement with the statement, “I would protect others from coronavirus if I wear a mask when I go out in public” is an indicator of whether they hold positive or negative outcome expectations for mask wearing. When agreement (or disagreement) is correlated with mask-wearing behavior, we can uncover what influences mask wearing behavior.
In addition to outcome expectations, six other behavioral constructs were assessed using these types of statements: perceived (COVID-19) susceptibility, perceived (COVID-19) severity, attitude toward (mask wearing) behavior, subjective social norms (what you believe others think you should do), belief about the importance of multiple preventive behaviors, and personal agency (belief in your ability to act). However, for the construct descriptive (or observed) social norms, respondents were asked to rate the frequency of having seen others wearing a cloth or other face covering (“rarely/never, sometimes, often/always”), and for the cue to action construct, respondents were asked to identify any from a list of messages they had heard about in public or in the media. If they selected “wear a face/covering/mask in public” as a message they had heard, then they were coded as having heard this message.
Several other types of independent variables were analyzed: COVID-19 case and fatality counts (per respondent county), presence/absence of a state-wide mask wearing mandate at time of survey, gender, age, education, geographic region, urban/rural status, employment status, household income, and responses to questions about participants personal experiences with COVID-19. Frequencies for mask wearing behavior questions and all of the independent variables were displayed by a racial/ethnic group.
Statistical Analysis
Since the primary goal of the analysis was to identify the relationships between behavioral theory constructs and mask wearing frequency within each race/ethnicity group, mask wearing behavior was modelled separately for each racial/ethnic group. The nine behavioral theory constructs described above were included in each of four separate binary logistic regression models, as well as age, sex, education, cumulative COVID-19 case count, presence of a state-issued mask mandate, and survey month. This is a fundamentally different approach from creating a single model with race/ethnicity as a covariate, one which is more consistent with a health equity perspective, because it seeks to identify drivers of mask wearing behavior within different racial/ethnic groups, rather than treating race/ethnicity as a potentially causal factor. Within each of the four racial/ethnic groups, crude and adjusted odds ratios (“COR,” “AOR”) were calculated. All analyses were weighted using the provided survey weights. Statistical analyses were performed using IBM SPSS, version 29.0.
As explained above, behavioral theory constructs are sometimes formulated using multiple agree/disagree type statements. Since the seven surveys that constitute the analysis data set were not originally intended for analysis as a merged dataset, many of the behavioral theory construct statements were not included in all seven months. Consequently, analysts used a single statement for each construct in order to be consistent across all constructs. However, for five of the nine behavioral theory constructs, there was more than one statement for which data had been collected in all seven months. For example, for the construct, attitude toward behavior, one statement was, “I think it is a good idea for everyone to wear a face covering/mask while out in public,” while a second statement was, “I think it is a good idea for me to wear a face covering/mask while out in public.” In these cases, bivariate correlations were calculated between each statement and “always” wearing a mask for each racial/ethnic group. The statement with the strongest correlation within that group was chosen for inclusion in logistic regression modelling for that group.
Results
Demographic and County Characteristics by Respondent Racial/Ethnic Group
The 3,217 respondents who left their home at least once in the past seven days included: 2,240 White respondents (63%1), 381 Hispanic respondents (16%), 345 Black respondents (12%), 158 Asian respondents (5%), and 93 respondents of non-Hispanic, and other or multiple race (3%). Weighted frequencies of demographic characteristics of these respondent groups are shown in Table 1. Hispanic respondents were more likely to report being employed (66% (348/528)) than any other group (range: 53–56%). All groups had their greatest proportion of respondents in the two middle income categories, (“$25,000–$49,999” and “$50,000–$99,999”); however, 31% (123/397) of Black respondents were reported being in the lowest income group (“$25,000 or below”), more than ten percentage points higher than any other group.
Table 1.
Self-reported demographic characteristics of survey respondentsa by racial/ethnic group United States, May–November 2020 (N= 3,217)
| Hispanic (n=381) | Non-Hispanic Asian (n=158) | Non-Hispanic Black (n=345) | Non-Hispanic White (n=2,240) | Non-Hispanic multiple or other raceb (n=93) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| % | % | % | % | % | ||||||
| Gender | Nc | (95% CI) | Nc | (95% CI) | Nc | (95% CI) | Nc | (95% CI) | Nc | (95% CI) |
| Female | 192 | 50.2 | 92 | 56.5 | 185 | 52.9 | 1,059 | 49.8 | 67 | 69.9 |
| (45.9, 54.4) | (48.8, 64.1) | (48.0, 57.8) | (47.6, 51.9) | (60.3, 77.5) | ||||||
| Male | 189 | 49.8 | 66 | 43.5 | 160 | 47.1 | 1,181 | 50.2 | 26 | 30.1 |
| (45.6, 54.1) | (35.9, 51.2) | (42.2, 52.0) | (48.0, 52.4) | (22.5, 39.7) | ||||||
| Age group (years) | ||||||||||
| 18–29 | 159 | 40.0 | 53 | 32.0 | 95 | 25.0 | 309 | 12.3 | 33 | 34.0 |
| (35.8, 44.2) | (25.2, 39.6) | (20.9, 29.4) | (10.9, 13.7) | (25.8, 43.5) | ||||||
| 30–39 | 96 | 22.5 | 39 | 24.2 | 77 | 18.7 | 488 | 17.0 | 18 | 19.5 |
| (19.1, 26.2) | (17.8, 31.0) | (15.0, 22.7) | (15.4, 18.7) | (12.8, 27.7) | ||||||
| 40–49 | 54 | 15.6 | 24 | 15.3 | 43 | 12.2 | 447 | 18.1 | 8 | 10.8 |
| (12.6, 18.8) | (10.2, 21.3) | (9.2, 15.6) | (16.5, 19.9) | (6.2, 18.1) | ||||||
| 50–64 | 59 | 17.5 | 25 | 14.6 | 95 | 29.8 | 582 | 27.2 | 29 | 29.4 |
| (14.5, 21.0) | (9.7, 20.6) | (25.4, 34.4) | (25.3, 29.2) | (21.6, 38.7) | ||||||
| ≥65 | 13 | 4.4 | 17 | 13.8 | 35 | 14.4 | 414 | 25.4 | 5 | 6.3 |
| (2.9, 6.4) | (9.1, 19.8) | (11.2, 18.1) | (23.6, 27.4) | (2.9, 12.3) | ||||||
| Census regiond | ||||||||||
| Northeast | 66 | 16.5 | 25 | 15.5 | 54 | 16.6 | 436 | 18.6 | 11 | 11.7 |
| (13.5, 19.8) | (10.7, 22.0) | (13.2, 20.5) | (16.9, 20.3) | (6.9, 19.2) | ||||||
| Midwest | 37 | 10.2 | 22 | 15.2 | 64 | 18.6 | 527 | 25.1 | 18 | 21.1 |
| (7.9, 13.0) | (10.2, 21.3) | (15.0, 22.7) | (23.3, 27.1) | (14.4, 29.7) | ||||||
| South | 138 | 37.2 | 33 | 20.9 | 194 | 55.3 | 807 | 35.6 | 41 | 44.5 |
| (33.3, 41.5) | (15.0, 27.6) | (50.5, 60.3) | (33.5, 37.7) | (35.3, 53.9) | ||||||
| West | 140 | 36.1 | 78 | 48.4 | 33 | 9.6 | 470 | 20.7 | 23 | 22.8 |
| (32.2, 40.3) | (40.7, 56.2) | (7.0, 12.8) | (18.9, 22.5) | (16.0, 31.7) | ||||||
| Community type | ||||||||||
| Urban | 187 | 48.2 | 67 | 41.3 | 161 | 45.7 | 703 | 27.2 | 28 | 29.7 |
| (44.1, 52.6) | (34.1, 49.3) | (41.0, 50.8) | (25.3, 29.2) | (21.6, 38.7) | ||||||
| Suburban | 156 | 41.4 | 81 | 52.2 | 122 | 35.2 | 979 | 45.2 | 38 | 40.1 |
| (37.3, 45.7) | (44.5, 59.9) | (30.7, 40.1) | (43.0, 47.3) | (31.0, 49.2) | ||||||
| Rural | 38 | 10.4 | 10 | 6.5 | 62 | 19.1 | 558 | 27.6 | 27 | 30.2 |
| (8.0, 13.2) | (3.3, 10.9) | (15.5, 23.2) | (25.7, 29.6) | (22.5, 39.7) | ||||||
| Employmente | ||||||||||
| Employed | 259 | 65.8 | 86 | 53.0 | 208 | 56.1 | 1,351 | 53.4 | 49 | 49.7 |
| (61.8, 69.9) | (45.1, 60.5) | (51.3, 61.0) | (51.2, 55.6) | (40.7, 59.3) | ||||||
| Household income | ||||||||||
| ≤$25,000 | 65 | 17.6 | 25 | 14.3 | 99 | 30.8 | 333 | 17.2 | 27 | 30.0 |
| (14.5, 21.0) | (9.7, 20.6) | (26.6, 35.7) | (15.6, 18.9) | (21.6, 38.7) | ||||||
| $25,000-$49,999 | 116 | 33.2 | 35 | 23.1 | 114 | 31.9 | 568 | 29.2 | 32 | 34.3 |
| (29.2, 37.2) | (17.2, 30.3) | (27.5, 36.7) | (27.2, 31.2) | (25.8, 43.5) | ||||||
| $50,000-$99,999 | 128 | 32.5 | 63 | 43.6 | 81 | 22.8 | 698 | 30.3 | 19 | 22.1 |
| (28.5, 36.5) | (35.9, 51.2) | (18.8, 27.0) | (28.3, 32.3) | (15.2, 30.7) | ||||||
| ≥$100,000 | 72 | 16.7 | 35 | 19.0 | 51 | 14.5 | 641 | 23.3 | 15 | 13.7 |
| (13.7, 20.0) | (13.4, 25.5) | (11.4, 18.3) | (21.5, 25.2) | (8.3, 21.3) | ||||||
| Education | ||||||||||
| High school graduate or less | 132 | 39.2 | 22 | 15.3 | 144 | 46.9 | 674 | 38.5 | 44 | 51.9 |
| (35.1, 43.4) | (10.2, 21.3) | (42.0, 51.8) | (36.3, 40.6) | (42.5, 61.1) | ||||||
| Some college or degree | 186 | 46.1 | 103 | 63.8 | 165 | 43.9 | 1,021 | 43.2 | 43 | 43.3 |
| (41.8, 50.3) | (55.9, 70.7) | (39.0, 48.7) | (41.0, 45.3) | (34.4, 52.9) | ||||||
| Some graduate school or degree | 63 | 14.7 | 33 | 20.9 | 36 | 9.3 | 545 | 18.4 | 6 | 4.8 |
| (11.9, 18.0) | (15, 27.6) | (6.8, 12.5) | (16.7, 20.1) | (1.8, 9.8) | ||||||
CI confidence interval
aRespondents to a survey (May–November, 2020) stating that they left their home at least one day in the prior week
bNon-Hispanic multiple or other race included American Indian or Alaska Native, Native Hawaiian or other Pacific Islander, multiple race, and other race
cN’s are unweighted, while frequencies (%) and 95% confidence intervals are weighted by race/ethnicity, age, gender, and education to the US national population, as provided by the panel survey data company
dNortheast: ME, NH, VT, MA, RI, CT, NY, NJ, and PA; Midwest: WI, IL, MI, IN, OH, ND, SD, NE, KS, MN, IA, and MO; West: MT, ID, WY, NV, UT, CO, AZ, NM, WA, OR, CA, AK, and HI; West: MT, ID, WY, NV, UT, CO, AZ, NM, WA, OR, CA, AK, and HI
eEmployed: full-time part-time, and self-employed; not employed: student, homemaker, and not employed
Table 2 shows the county characteristics of survey respondents grouped by race/ethnicity for: Hispanic, Asian, Black, and White respondents. Regarding county COVID-19 cases and deaths per 100,000 population, Hispanic respondents resided in counties with the highest mean values for cumulative cases (2009), deaths (66), and cases in the prior day (21). For Black respondents, the values for these three indicators were slightly lower (1,899, 65, and 18), but still higher than Asian or White respondents. Nearly 70% (110/158) of Asian respondents lived in counties with state-issued mask mandates at the time of survey while the other three groups ranged from 58% to 61%.
Table 2.
Survey respondenta county characteristics by racial/ethnic group (N=3217), United States, May–November 2020
| Hispanic (n=381) | Non-Hispanic Asian (n=158) | Non-Hispanic Black (n=345) | Non-Hispanic White (n=2,240) | |||||
|---|---|---|---|---|---|---|---|---|
| COVID-19 cases and death counts at the time of survey |
Meanb (95% CI) |
Mean (95% CI) |
Mean (95% CI) |
Mean (95% CI) |
||||
| Cumulative cases since beginning of outbreak |
2,009 (1869, 2,149) |
1,513 (1325, 1702) |
1,898 (1771, 2026) |
1,516 (1460, 1572) |
||||
| Cumulative deaths since beginning of outbreak |
66.1 (59.7, 72.5) |
55.6 (43.7, 67.5) |
65.1 (57.8, 72.3) |
46.6 (44.4, 48.9) |
||||
| Number of cases reported for day prior to interview |
21.1 (18.2, 24.0) |
17.8 (14.1, 21.6) |
18.4 (16.3, 20.4) |
15.6 (14.6, 16.6) |
||||
| Number of deaths reported for day prior to interview |
0.3 (0.3, 0.4) |
0.2 (0.1, 0.3) |
0.4 (0.3, 0.5) |
0.3 (0.2, 0.33) |
||||
| Presence of mask mandates at the time of survey | Nc |
% (95% CI) |
N |
% (95% CI) |
N |
% (95% CI) |
N |
% (95% CI) |
| State-issued public mask mandate in effect in county of respondent | 226 |
61.2 (56.8, 65.2) |
108 |
69.7 (62.1, 76.4) |
203 |
59.8 (55.0, 64.6%) |
1,345 |
58.7 (56.5, 60.8) |
CI confidence interval
aRespondents to a survey (May–November, 2020) stating that they left their home at least one day in the prior week
bMeans are per 100,000 population
cN’s are unweighted, while frequencies (%) and 95% confidence intervals are weighted by race/ethnicity, age, gender and education to the US national population, as provided by the panel survey data company
Self-Reported Mask Use
Asian respondents had the highest percentage of respondents reporting “always” wearing a mask when going out in the prior week (60% (96/159)), slightly more than the Hispanic (58% (304/528)), White (57% (1,141/2,018)), and Black (54% (213/397)) respondents (p<.05).
Table S1 shows survey response frequencies by race/ethnicity group to four questions about people’s personal experiences with COVID-19. These were not included in the main analysis because the questions were only asked between May and October. Hispanic respondents had the highest frequency of “yes” responses to questions about knowing someone who had been diagnosed (32%), hospitalized (28%), or had died (26%) from COVID-19. A separate analysis using models for the shorter time period did not reveal any statistically significant associations between a “yes” response to any of the five questions and always wearing a mask (data not shown).
Behavioral Theory Constructs–Frequencies
Table 3 shows frequencies of agreement with behavioral theory construct statements within four groups of race/ethnicity as well as the association between the construct and “always” wearing a mask. Eight of the nine constructs were positively associated (p<.05) with “always” wearing a mask in at least one group, while four (observed social norm, outcome expectations, personal agency, and cue to action) were positively associated (p<.05) in two of the four groups.
Table 3.
Agreement with behavioral theory construct statements and association between agreement and “always” wearing a maska by race/ethnicity, United States, May–November 2020
| Hispanic respondentsb (n=381) | Non-Hispanic Black respondentsc (n=385) | Non-Hispanic Asian respondentsd (n=158) | Non-Hispanic White respondentse (n=2,240) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| % | Crude OR | AORf | % | Crude OR | AOR | % | Crude OR | AOR | % | Crude OR | AOR | |
| Descriptive (observed) social norm—when going out, seeing others wearing cloth or other face coveringg,h | ||||||||||||
| Sometimes | 19.3 | 3.6 | 3.4 | 23.2 | 0.8 | 0.3 | 18.7 | 0.5 | – | 18.4 | 1.4 | 1.5 |
| (16.1, 22.8) | (1.4, 8.8) | (1.1, 10.0) | (19.2, 27.5) | (0.3, 2.1) | (0.1, 1.3) | (13.4, 25.5) | (0, 6.0) | (16.8, 20.2) | (0.8, 2.7) | (0.7, 3.1) | ||
| Often/always | 73.4 | 8.4 | 6.7 | 71.8 | 2.2 | 0.8 | 79.3 | 0.7 | – | 79.1 | 3.8 | 3.1 |
| (69.6, 77.1) | (3.6, 19.7) | (2.5, 18.3) | (67.2, 76.0) | (0.9, 5.6) | (0.2, 2.8) | (72.4, 85.0) | (0.1, 8.2) | (77.3, 80.8) | (2.1, 7.1) | (1.6, 6.1) | ||
| Subjective (perceived) social norm—People who are important to me believe that I should wear a mask when I go out in publici,j | ||||||||||||
| Neutral | 13.9 | 1.3 | 0.6 | 14.7 | 2.1 | 1.9 | 14.3 | 2.4 | – | 17.4 | 1.7 | 0.8 |
| (11.1, 17.0) | (0.7, 2.7) | (0.2, 1.6) | (11.4, 18.3) | (0.6, 7.3) | (0.4, 9.5) | (9.7, 20.6) | (0.3, 22.3) | (15.8, 19.1) | (1.1, 2.5) | (0.5, 1.3) | ||
| Agree/strongly agree | 73.6% | 5.0 | 0.9 | 80.2 | 7.0 | 3.4 | 82.7 | 5.1 | – | 72.4 | 7.0 | 1.4 |
| (69.8, 77.3) | (2.8, 8.9) | (0.4, 2.1) | (76.2, 84.0 | (2.2, 22.4) | (0.8, 15) | (75.9, 87.7) | (0.6, 41.9) | (70.5, 74.4) | (4.9, 9.9) | (0.9, 2.2) | ||
| Attitude toward behavior—It is important for me to wear a mask when I am out in publick | ||||||||||||
| Neutral | 13.1 | 1.1 | 0.6 | 13.7 | 0.5 | 0.4 | 13.6 | 0.2 | – | 12.8 | 1.7 | 1.2 |
| (10.4, 16.1) | (0.5, 2.5) | (0.2, 1.8) | (10.7, 17.5) | (0.2, 1.5) | (0.1, 1.4) | (9.1, 19.8 | (0.0, 2.0) | (11.4, 14.3) | (1.1, 2.5) | (0.7, 2.1) | ||
| Agree/strongly agree | 76.6 | 6.7 | 1.8 | 77.3 | 3.9 | 1.6 | 83.8 | 0.4 | – | 74.9 | 8.5 | 2.3 |
| (72.8, 80.0) | (3.5, 13.0) | (0.7, 4.6) | (73.0, 81.2) | (1.8, 8.2) | (0.5, 4.5) | (77.3, 88.8) | (0.0, 4.9) | (72.9, 76.7) | (6.1, 11.9) | (1.4, 3.6) | ||
| Belief about importance of multiple preventive behaviors—it is important to use both social distancing and mask wearing to prevent the spread of coronavirus | ||||||||||||
| Neutral | 13.4 | 1.5 | 0.9 | 14.6 | 0.8 | 0.6 | 9.6 | 0.9 | – | 11.8 | 1.5 | 0.8 |
| (10.7, 16.6) | (0.7, 3.5) | (0.3, 2.6) | (11.4, 18.3) | (0.3, 2) | (0.2, 2.3) | (5.6, 14.7) | (0.1, 6.7) | (10.4, 13.3) | (1.0, 2.3) | (0.5, 1.5) | ||
| Agree/strongly agree | 75.8 | 8.0 | 3.0 | 78.4 | 3.0 | 0.4 | 87.0 | 2.3 | – | 79.2 | 6.0 | 1.0 |
| (72.0, 79.3) | (4.1, 15.7) | (1.1, 8.1) | (74.1, 82.2) | (1.3, 6.8) | (0.1, 1.5) | (80.9, 91.4) | (0.4, 13.1) | (77.4, 80.9) | (4.2, 8.6) | (0.6, 1.7) | ||
| Outcome expectations—I would protect others from coronavirus if I wear a mask when I go out in public l | ||||||||||||
| Neutral | 15.4 | 2.4 | 2.5 | 13.5 | 1.3 | 2.1 | 14.1 | 0.3 | – | 15.3 | 2.2 | 1.6 |
| (12.5, 18.6) | (1.1, 5.2) | (0.9, 6.9) | (10.5, 17.2) | (0.5, 3.7) | (0.6, 7.7) | (9.1, 19.8) | (0, 3.8) | (13.8, 16.9) | (1.5, 3.2) | (1.0, 2.6) | ||
| Agree/strongly agree | 74.2 | 6.7 | 1.6 | 77.7 | 6.8 | 5.1 | 84.0 | 0.7 | – | 72.1 | 6.8 | 1.7 |
| (70.4, 77.8) | (3.5, 13.1) | (0.6, 4.1) | (73.6, 81.7) | (2.9, 16) | (1.8, 15.0) | (78.0, 89.3) | (0.1, 8.4) | (70.2, 74.1) | (5.0, 9.4) | (1.1, 2.8) | ||
| Personal agency—I am confident that I can wear a mask when out in public to prevent the spread of coronavirus | ||||||||||||
| Neutral | 13.5 | 1.9 | 2.1 | 13.9 | 1.1 | 2.8 | 11.4 | 0.6 | – | 13.6 | 1.8 | 1.1 |
| (10.7, 16.6) | (0.9, 3.9) | (0.8, 5.7) | (10.7, 17.5) | (0.3, 3.3) | (0.7, 11.9) | (7.1, 16.9) | (0.1, 4.2) | (12.2, 5.2) | (1.1, 2.7) | (0.7, 1.9) | ||
| Agree/strongly agree | 74.7 | 4.7 | 1.9 | 79.8 | 5.4 | 3.8 | 84.8 | 2.5 | – | 76.1 | 8.4 | 2.1 |
| (71.0, 78.4) | (2.6, 8.4) | (0.9, 4.3) | (75.7, 83.6) | (2.1, 14.4) | (1.1, 13.9) | (78.7, 89.8 | (0.5, 13.1) | (74.2, 7.9) | (5.9, 12.1) | (1.3, 3.5) | ||
| Cue to action—Which of the following actions have you heard are important things to do to protect yourself and others from coronavirus?…Wear a mask in public.m | ||||||||||||
| Yes | 77.1 | 2.1 | 0.9 | 79.5 | 4.1 | 3.6 | 84.3 | 1.3 | – | 87.2 | 2.8 | 1.6 |
| (73.4, 80.5) | (1.4, 3.1) | (0.5, 1.5) | (75.4, 83.3) | (2.4, 7.0) | (1.7, 7.3) | (78.0, 89.3) | (0.5, 3.0) | (85.7, 88.6) | (2.1, 3.6) | (1.1, 2.2) | ||
| Perceived severity of infection—I’m worried I would become seriously ill if I became infected with COVID-19. | ||||||||||||
| Neutral | 20.0 | 0.9 | 0.8 | 21.2% | 0.7 | 0.7 | 25.5 | 0.4 | – | 19.1 | 1.7 | 1.5 |
| (16.8, 23.7 | (0.5, 1.5) | (0.4, 1.6) | (17.4, 25.4 | (0.4, 1.4) | (0.3, 1.6) | (18.9, 32.3) | (0.1, 1.3) | (17.5, 20.9) | (1.3, 2.3) | (1.1, 2.2) | ||
| Agree/strongly agree | 60.6 | 2.0 | 0.9 | 61.7 | 1.4 | 0.7 | 63.3 | 0.8 | – | 59.3 | 3.1 | 1.5 |
| (56.4, 64.7) | (1.3, 3.2) | (0.5, 1.7) | (56.9, 66.4 | (0.8, 2.4) | (0.3, 1.4) | (55.9, 70.7) | (0.3, 2.3) | (57.1, 61.4) | (2.5, 3.9) | (1.1, 1.9) | ||
| Perceived susceptibility to infection - I think it is likely that I will become infected with COVID-19. | ||||||||||||
| Neutral | 32.7 | 1.2 | 1.0 | 32.5 | 1.0 | 1.6 | 31.6 | 1.1 | – | 33.2 | 1.1 | 0.9 |
| (28.9, 36.9) | (0.8, 1.9) | (0.6, 1.8) | (28.0, 37.2) | (0.6, 1.6) | (0.9, 2.9) | (24.6, 38.9) | (0.5, 2.4) | (31.2, 35.3) | (0.9, 1.3) | (0.7, 1.2) | ||
| Agree/strongly agree | 36.0 | 1.6 | 1.3 | 24.6 | 0.9 | 1.3 | 27.7 | 0.9 | – | 24.0 | 1.2 | 0.9 |
| (32.0, 40.1) | (1.0, 2.4) | (0.8, 2.2) | (20.6, 29.1) | (0.6, 1.5) | (0.6, 2.5) | (21.2, 35.0) | (0.4, 2.0) | (22.2, 25.9) | (1.0, 1.5) | (0.7, 1.2) | ||
Values in bold indicate statistically significant associations at p < .05
aWhen leaving the home in the prior week
bHispanic respondents; model chi sq: 142.8; p<.001
cNon-Hispanic Black respondents; model chi-sq: 115.9; p<.001
dNon-Hispanic Asian respondents; model chi-sq: 32.4; p=.594 (model did not converge)
eNon-Hispanic White respondents; model chi-sq: 474.4; p<.001
fAdjusted odds ratios were estimated controlling for all other behavioral construct variables, as well as age, gender, education, presence of a mask mandate in respondent’s county, cumulative COVID-19 cases in the county the day prior to the interview, and interview month. None of the demographic, county, or time variables were statistically significant in models
g“Never/rarely” is the referent level
hIn May and June, survey items referred to a “cloth face covering.” From July forward, all items were revised to refer to “face covering/mask.” After examination of frequency time trends revealed general consistency in responses between the slight wording differences, the questions were merged, and the term “mask” was used for all of the merged items
iUnless otherwise noted, “Strongly disagree/disagree” is the referent level
jFor non-Hispanic White respondents, the statement was: “People who are important to me want me to wear a face covering/mask when I go out in public”
kFor Hispanic respondents the statement was: “It is important for everyone to wear a face covering/mask when they are out in public”
lFor non-Hispanic White respondents, the statement was: “I can help stop the coronavirus outbreak in my community if I wear a face covering/mask while out in public”
m“No” is the referent level
Hispanic Respondents
The construct, descriptive (observed) norm, had the highest adjusted odds ratio for mask wearing among all the constructs in the regression model using data from Hispanic respondents (AOR: 6.7 (2.5, 18.3)). The survey question used to measure this construct (reported frequency of “When going out, seeing others wearing cloth or other face covering”) was also reported with high frequency in comparison to the other three groups (38% vs. 27%–31%). The only other statistically significant construct for this model was belief about multiple preventive behaviors (AOR: 3.0 (1.1, 8.1)). More than half of Hispanic respondents (56.5%) agreed with the survey item used to measure this construct, “It is important to use both social distancing and face coverings/mask to prevent the spread of coronavirus.”
Asian Respondents
Logistic regression models did not converge for Asian respondents due to a combination of small sample size and a high percentage of respondents reporting “always” wearing a mask (60% (96/159)). Therefore, only crude odds ratios (COR) were reported. Among these, the constructs: subjective norm (COR=5.1), personal agency (COR=2.5), and beliefs about performing multiple preventive behaviors (COR=2.3) had the largest crude associations with mask wearing; however, none were statistically significant (p<.05). On most of the construct statements, over 50% of this group reported agreement, with the exception of descriptive (observed) norm, perceived severity, and perceived susceptibility to infection, which were lower. This group had a notably higher agreement than the non-Hispanic White group to the statement, “It is important for me to wear a face covering/mask when I am out in public” (attitude toward behavior: 65% (103/159) vs. 56% (1126/2018)).
Black Respondents
Three behavioral theory constructs were found to be significant among Black respondents: outcome expectations (AOR=5.1), personal agency (AOR=3.8), and cue to action (AOR=3.6). Frequency of agreement with the statement representing outcome expectations (“I would protect others from coronavirus if I wear a face covering/mask when I go out in public,” (53.3%)) is notably higher than that of the non-Hispanic White group (46.0%), although the question for that group was worded slightly differently (“I can help stop the coronavirus outbreak in my community if I wear a face covering/mask while out in public”). The construct, personal agency, was not only significantly associated with mask wearing frequency but had a higher agreement frequency for the non-Hispanic Black group than other groups (57.8% vs. 49.6-55.2%). With regard to cue to action, this group has a somewhat lower frequency of reporting having heard messaging about wearing a mask than the non-Hispanic Asian or non-Hispanic White groups; however, it has a higher AOR for mask wearing than these other two groups.
White Respondents
There were six constructs that were significantly associated with “always” wearing a mask for this group: descriptive norm (AOR=3.1), attitude toward the behavior (AOR=2.3), personal agency (AOR=2.1), outcome expectations (AOR=1.7), cue to action (AOR=1.6), and perceived severity (AOR=1.5). Among these, the White group had a high frequency of responding, “Wear a face covering/mask in public,” in response to the question, “Which of the following actions have you heard are important things to do to protect yourself and others from coronavirus?” (cue to action: 87% (1,760/2,018) vs. 77%–84%). Within the White group, there was also a notably lower frequency of agreement for the personal agency-related statement, “Wearing a face covering/mask while out in public is easy for me” (38% (769/2,018) vs. 43%–49%). While outcome expectations was significantly associated with mask wearing (AOR=1.7), agreement with the outcome expectations statement was low (46.0%) in comparison to that of the other groups (53%–55%).
Discussion
While the separate modelling of the four groups does not lend itself to statistical comparison between the groups, the results suggest that different behavioral theory constructs are more common and more influential in some groups than others. If one were to develop mask wearing promotion interventions with a diversity of results such as these, mask promotion efforts might emphasize social norms for some population groups, emphasizing the merit of the behavior for others, and for other groups, a more successful approach might be focusing on developing people’s sense of personal agency by assisting them in making mask wearing less challenging.
Hispanic Respondents
Among Hispanic respondents, seeing others wear a mask and believing in the importance of both social distancing and masks were the strongest drivers of always wearing a mask. Taken together, these factors suggest the role of social environment in mask wearing behavior, since both seeing others wearing a mask and awareness of multiple types of infection prevention methods contribute to an atmosphere of prevention. The interpersonal influence and the salience of multiple strategies is consistent with the socio-ecologic theory [12, 44], which emphasizes the influences of multiple social environmental factors simultaneously: within the individual, among friends and family, between local groups and organizations, across the larger community, and finally at broad societal levels. In the published literature, there are several studies that identify seeing others wearing masks as influential (but these do not specifically refer to Hispanic individuals) [11, 13, 18, 44–51]. No other group was found to be significantly influenced by the idea that mask wearing combined with social distancing was important. The most similar findings in prior studies were that mask wearing did not reduce engagement in other types of preventive measures and, in one instance, increased it [52, 53].
Black respondents
The combination of three psychosocial factors most strongly associated with mask wearing among Black respondents (outcome expectations, personal agency, and cue to action) corresponds to a pattern suggested by behavioral theory [42], in which behavior is driven by a combination of motivation, capability, and contextual opportunities to act. In this case, outcome expectations (protecting others) is the motivation, personal agency is the sense of capability, and cue to action (having heard messaging about the importance of masks) is the contextual opportunity to act. This is consistent with a recent qualitative study that found both a desire to protect others and cues to action as related to mask wearing among Black participants [54]. Direct communication with Black communities (cue to action) was also found to be an effective strategy for promoting COVID-19 vaccine uptake among Black populations, in contrast to vaccination mandates or incentive-based programs [55]. The three factors have been identified separately as positively associated with mask wearing in populations not specified by race/ethnicity [16, 17, 20, 56, 57].
Asian Respondents
Within the Asian respondent group, the variable with the strongest association (but not statistically significant) was, “people who are important to me believe that I should wear a face covering/mask when I go out in public” (subjective (perceived) norm). Behavioral theory distinguishes this internalized sense of expectation from the influence of seeing others wearing masks [42, 43]. Other studies have found perceived social norms to be influential in mask wearing, but not specifically with Asian groups [10, 11, 19].
White Respondents
As with the Hispanic group, the White respondent group was influenced by seeing others wearing masks (descriptive (observed) norm). However, believing that mask wearing was important (attitude toward the behavior) was unique for this group. This suggests a more individualistic perspective, with one influence coming from others and the second being one’s own determination that the behavior was important. These two variables were also identified as being positively associated with mask wearing in a prior analysis of a subset of the current dataset (May and June 2020, all races and ethnicities combined) [11]. Other published studies have looked at perceived efficacy of mask wearing rather than perceived importance [58, 59] and found it to be positively associated.
It is important to emphasize that these results suggest that participants in different social environments during COVID-19 generally have different drivers to mask-wearing; one should not conclude from this that all members of each particular group are motivated to wear masks this way. Prior to implementing any mask promotion efforts, surveys like the one performed with a national sample should be repeated in the local community to identify drivers and barriers for those populations, since there are likely to be variations in importance of different constructs at different times, in different locations and within different sub-groups.
It is also interesting to note that for behavioral constructs that were represented by more than one statement (for example, with outcome expectations had two), different statements were more strongly associated with mask wearing behavior in different racial/ethnic groups. For example, within the group of non-Hispanic Black respondents, the statement, “I would protect others from coronavirus if I wear a mask when I go out in public” was more predictive of wearing a mask, while among non-Hispanic White participants, the statement “I can help stop the coronavirus outbreak in my community if I wear a face covering/mask while out in public” was more strongly associated. This raises the question of whether the wording of behavioral theory construct statements may affect how strongly it resonates with different groups. Further research is needed to determine whether variations in wording to represent theoretical constructs to different groups might be useful [60].
Limitations
This analysis is a first step in applying behavioral science theory towards mask-wearing behaviors using a health equity lens, and the results should be interpreted cautiously. Data were collected for monthly program monitoring, which was not intended to be merged or stratified by race/ethnicity. This resulted in small sample sizes for three of the four groups, as well as the exclusion of some psychosocial factors and survey questions that were not collected every month. Despite these challenges, this analysis identified clear differences in factors associated with mask wearing between the Hispanic, Black, Asian, and White respondent groups.
In addition to the limitations already described, the following important limitations should be considered. Survey data are self-reported and subject to biases, including social desirability and recall bias. Second, the data were collected online, which is limited to internet users and to users who speak English and are familiar with the survey system. Third, because mask wearing behavior was measured at the same time as the behavioral constructs, we cannot ascertain that the attitudes and perceptions preceded the mask wearing behavior. Thus, we must consider whether any of these beliefs, attitudes, and perceptions formed as a result of mask wearing (or not wearing a mask) that was in fact driven by something else. Lastly, the representativeness of the samples is unknown. Although the data collection service weighted the datasets so that overall age, sex, education, region, and racial/ethnic composition matched the national US population at the time of the survey, this did not assure representativeness within each of the racial/ethnic groups. It was also not possible to examine other racial/ethnic groups such as American Indian, Alaska Native, Native Hawaiian, and Pacific Islander groups, who are known to experience some of the highest rates of COVID-19 morbidity and mortality. Lastly, other published studies have identified a range of social and individual factors that were not considered in this analysis (for example, use of reason [61], belief in science [61, 62], political orientation [62], and social identity [30, 63]).
Conclusion
These results suggest that analyzing behavioral theory constructs separately for different racial and ethnic groups reveals different potential avenues for community efforts to promote mask wearing during COVID-19 outbreaks, or during other future health emergencies. This approach need not be limited to mask promotion, however. Indeed, behavioral theory-based messaging tailored to specific audiences is being developed to promote COVID-19 vaccination uptake [64]. Surveying specific social identity groups in terms of behavioral theory-based constructs and measuring relationships with desired behaviors can be used by any community program wishing to increase self-protective behaviors quickly and effectively. This theory-based approach can be validated in the field and can be used for monitoring program effectiveness over time.
Acknowledgements
The authors would like to thank Fred Fridinger, John O’Connor, CDC, Deanne Weber, Porter Novelli.
Author Contribution
Christine E. Prue conceived the original behavioral theory constructs and statements used by the survey company. All authors contributed to the analysis conception and design. Dataset merging was performed by Giulia Earle-Richardson, Rieza H. Soelaeman, and Patricia Reese. Data analysis was performed by Giulia Earle-Richardson, Kiva A. Fisher, Rieza H. Soelaeman, and Daiva Yee. The first draft of the manuscript was written by Giulia Earle-Richardson. All authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Data Availability
For more information regarding data availability, contact the corresponding author.
Declarations
Ethics Approval
The dataset was created from a previously collected opt-in survey that contained no identifiers and from publicly available county level case and fatality counts. This activity was reviewed by CDC and was found to be consistent with applicable federal law and CDC ethics policy.
Consent to Participate
The survey datasets were obtained from a commercial internet panel survey company [33], through a subscription license. Porter Novelli Public Services panel surveys have been determined to be consistent with standard informed consent practices for this type of market research [34].
Competing Interests
The authors declare no competing interests.
Disclaimer
The findings and conclusions in this article are those of the authors and do not necessarily represent the official position of CDC.
Footnotes
Percentages were calculated using weighted n’s; for example, for White respondents, there were a total 2018 participants after weighting, divided by the weighted total sample of 3210 participants. 2018/3210 is 63%. Unless otherwise noted, all frequencies are calculated using weighting by race/ethnicity, age, gender, and education to the US national population, as provided by the panel survey data company.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Hill L, Artiga S, Ndugga N. COVID-19 cases, deaths, and vaccinations by race/ethnicity as of winter 2022. Kaiser Family Foundation. 2023. www.kff.org/coronavirus-covid-19/issue-brief/covid-19-cases-deaths-and-vaccinations-by-race-ethnicity-as-of-winter-2022/. Accessed 14 Apr 2023
- 2.Truman BI, Chang MH, Moonesinghe R. Provisional COVID-19 age-adjusted death rates, by race and ethnicity - United States, 2020–2021. Morb Mortal Wkly Rep. 2022;71(17):601–605. doi: 10.15585/mmwr.mm7117e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Johnson-Agbakwu CE, Ali NS, Oxford CM, Wingo S, Manin E, Coonrod DV. Racism, COVID-19, and health inequity in the USA: a call to action. J Racial Ethn Health Disparities. 2022;9:52–58. 10.1007/s40615-020-00928-y. [DOI] [PMC free article] [PubMed]
- 4.Laurencin CT, McClinton A. The COVID-19 pandemic: a call to action to identify and address racial and ethnic disparities. J Racial Ethn Health Disparities. 2020;7(3):398–402. doi: 10.1007/s40615-020-00756-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pilecco FB, Leite L, Góes EF, Diele-Viegas LM, Aquino EM. Addressing racial inequalities in a pandemic: data limitations and a call for critical analyses. Lancet Glob Health. 2020;8(12):e1461–e1462. doi: 10.1016/S2214-109X(20)30360-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.West R, Michie S, Rubin GJ, et al. Applying principles of behaviour change to reduce SARS-CoV-2 transmission. Nat Hum Behav. 2020;4:451–459. doi: 10.1038/s41562-020-0887-9. [DOI] [PubMed] [Google Scholar]
- 7.Glanz, K. Social and behavioral theories. e-source behavioral & social sciences research website. National Institutes of Health, Office of Behavioral and Social Science Research website. obssr.od.nih.gov/sites/obssr/files/Social-and-Behavioral-Theories.pdf. Accessed 27 Jun 2023.
- 8.Ferrer R, Klein WM. Risk perceptions and health behavior. Curr Opin Psychol. 2015;1(5):85–89. doi: 10.1016/j.copsyc.2015.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ajzen I. The theory of planned behavior. Organ Behav Hum Decis Process. 1991;50:179–211. https://www.sciencedirect.com/science/article/pii/074959789190020T. Access 14 Apr 2023.
- 10.Cislaghi Beniamino, Heise Lori. Using social norms theory for health promotion in low-income countries. Health Promotion International. 2019;34(3):616–623. doi: 10.1093/heapro/day017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Barile JP, Guerin RJ, Fisher KA, Tian LA, Okun AH, Vanden Esschert KL, Jeffers A, Gurbaxani BM, Thompson WW, Prue CE. Theory-based behavioral predictors of self-reported use of face coverings in public settings during the COVID-19 pandemic in the United States. Ann Behav Med. 2021;55(1):82–88. doi: 10.1093/abm/kaaa109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Casola AR, Kunes B, Cunningham A, Motley RJ. Mask use during COVID-19: a social-ecological analysis. Health Promotion Practice. 2021;22(2):152–155. doi: 10.1177/1524839920983922. [DOI] [PubMed] [Google Scholar]
- 13.Mallinas SR, Maner JK, Plant EA. What factors underlie attitudes regarding protective mask use during the COVID-19 pandemic? Pers Individ Dif. 2021;111038. 10.1016/j.paid.2021.111038. [DOI] [PMC free article] [PubMed]
- 14.Milad E, Bogg T. Spring 2020 COVID-19 surge: prospective relations between demographic factors, personality traits, social cognitions and guideline adherence, mask wearing, and symptoms in a US sample. Ann Behav Med. 2021;55(7):665–76. 10.1093/abm/kaab039. [DOI] [PMC free article] [PubMed]
- 15.Fisher KA, Barile JP, Guerin RJ, et al. Factors associated with cloth face covering use among adults during the COVID-19 pandemic—United States, April and May 2020. Morb Mortal Wkly Rep. 2020;69(28):933–937. doi: 10.15585/mmwr.mm6928e3. [DOI] [PubMed] [Google Scholar]
- 16.Davis RE, Sharma M, Simon KE, Wilkerson AH. Conceptualization of college students’ COVID-19 related mask-wearing behaviors using the multi-theory model of health behavior change. Health Promot Perspect. 2021;11(2):194–201. doi: 10.34172/hpp.2021.24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Koebele EA, Albright EA, Dickinson KL, et al. Perceptions of efficacy are key determinants of mask-wearing behavior during the COVID-19 pandemic. Nat Haz Rev. 2021;22(3):6021002. doi: 10.1061/(ASCE)NH.1527-6996.0000489. [DOI] [Google Scholar]
- 18.Carbon CC. About the acceptance of wearing face masks in times of a pandemic. i-Perception. 2021;12(3):1–14. doi: 10.1177/20416695211021114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Graupensperger S, Lee CM, Larimer ME. Young adults underestimate how well peers adhere to COVID-19 preventive behavioral guidelines. J Prim Prev. 2021;43(3):309–318. doi: 10.1007/s10935-021-00633-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Asri A, Asri V, Renerte B, et al. Wearing a mask—for yourself or for others? Behavioral correlates of mask wearing among COVID-19 frontline workers. PloS One. 2021;16(7):e0253621. doi: 10.1371/journal.pone.0253621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Clements JM. Knowledge and behaviors toward COVID-19 among US residents during the early days of the pandemic: cross-sectional online questionnaire. JMIR Public Health Surveill. 2020;6(2):e19161. doi: 10.2196/19161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Liu Y, Mattke S. Association between state stay-at-home orders and risk reduction behaviors and mental distress amid the COVID-19 pandemic. Prev Med. 2020;141:106299. doi: 10.1016/j.ypmed.2020.106299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lu JG, Jin P, English AS. Collectivism predicts mask use during COVID-19. Proc Natl Acad Sci USA. 2021;118(23):e2021793118. doi: 10.1073/pnas.2021793118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chen CY-C, Lei M. Psychosocial factors associated with mask-wearing behavior during the COVID-19 pandemic. Psych Health Med. 2022;27(9):1996–2006. doi: 10.1080/13548506.2021.1998562. [DOI] [PubMed] [Google Scholar]
- 25.Orom HA, Kiviniemi NC, Hay MT, Waters JL, Schofield EA, Thomas E, Tuman SN, M, Racial/ethnic differences in prosocial beliefs and prevention behavior during the COVID-19 pandemic. Research Support Non-U.S. Gov't. J Racial Ethn Health Disparities. 2022;9(5):1807–1817. doi: 10.1007/s40615-021-01117-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Franz B, Milner A, Braddock IIJH. Do black lives matter in the American public’s mitigation responses to the COVID-19 pandemic? An analysis of mask wearing and racial/ethnic disparities in deaths from COVID-19. J Racial Ethn Health Disparities. 2022;9:1577–1583. 10.1007/s40615-021-01097-2. [DOI] [PMC free article] [PubMed]
- 27.Vereen RN, Lazard AJ, Frank SC, et al. Motivations, barriers, and communication recommendations for promoting face coverings during the COVID-19 pandemic: survey findings from a diverse sample. PloS One. 2021;16(5):e0251169. doi: 10.1371/journal.pone.0251169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ma Y, Zhan N. To mask or not to mask amid the COVID-19 pandemic: how Chinese students in America experience and cope with stigma. Chin Sociol Rev. 2020;1–26. 10.1080/21620555.2020.1833712.
- 29.Karout L, Serwat A, El Mais H, Kassab M, Khalid F, Mercedes BR. COVID-19 prevalence, risk perceptions, and preventive behavior in asymptomatic Latino population: a cross-sectional study. Cureus. 2020;12(9):e10707. doi: 10.7759/cureus.10707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Webber, K. T., Stifano, S., Davis, S. M., Stifano, S. C. Considering social identity threat alongside the health belief model to examine mask-wearing intentions of Black, Latinx, and Asian individuals in the U.S. during COVID-19. J Health Commun. 2022;1–13. Advance online publication. 10.1080/10410236.2022.2067384. [DOI] [PubMed]
- 31.Hearne NH, Brittany N, Niño MD. Understanding how race, ethnicity, and gender shape mask-wearing adherence during the COVID-19 pandemic: evidence from the COVID impact survey. J Racial Ethn Health Disparities. 2022;9(1):176–183. doi: 10.1007/s40615-020-00941-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Davis JL, Buchanan KL, Green BL. Racial/ethnic differences in cancer prevention beliefs: applying the health belief model framework. Am J Health Promot. 2013;27(6):384–389. doi: 10.4278/ajhp.120113-QUAN-15. [DOI] [PubMed] [Google Scholar]
- 33.Kim JE, Zane N. Help-seeking intentions among Asian American and White American students in psychological distress: application of the health belief model. Cultur Divers Ethnic Minor Psychol. 2016;22(3):311–321. doi: 10.1037/cdp0000056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ang DC, Monahan PO, Cronan TA. Understanding ethnic disparities in the use of total joint arthroplasty: application of the health belief model. Arthritis Rheum. 2008;59(1):102–108. doi: 10.1002/art.23243. [DOI] [PubMed] [Google Scholar]
- 35.Blanchard CM, Rhodes RE, Nehl E, Fisher J, Sparling P, Courneya KS. Ethnicity and the theory of planned behavior in the exercise domain. Am J Health Behav. 2003;27(6):579–591. doi: 10.5993/ajhb.27.6. [DOI] [PubMed] [Google Scholar]
- 36.Porter Novelli Public Services and ENGINE Insights through PN View 360 website. http://styles.porternovelli.com/pn-view-panels. Accessed 20 Jan 2023.
- 37.USA Facts, US COVID-19 cases and deaths by state. USA Facts website. usafacts.org/visualizations/coronavirus-covid-19-spread-map. Accessed 10 Jan 2021.
- 38.US Centers for Disease Contol and Prevention, U.S. State and Territorial Public Mask Mandates From April 10, 2020 through August 15, 2021 by County by Day Centers for Disease Control website. data.cdc.gov/Policy-Surveillance/U-S-State-and-Territorial-Public-Mask-Mandates-Fro/62d6-pm5i. Accessed 10 Jan 2021.
- 39.Insights Association, Code of Standards website. https://www.insightsassociation.org/Resources/Code-of-Standards. Accessed 24 May 2023.
- 40.US Department of Health and Human Services, Office for Human Subjects Protections website. Code of Federal Regulations, 45 part 46.102(I)(2), 21 C.F.R. part 56; 42 U.S.C. §241(d); 5 U.S.C. §552a; 44 U.S.C. §3501 et seq. https://www.hhs.gov/ohrp/regulations-and-policy/regulations/45-cfr-46/index.html. Accessed 24 May 2023.
- 41.HUD Office of Policy Development and Research (PD&R), HUDS USPS Zip Code Crosswalk Files. U.S. Department of Housing and Urban Development website. www.huduser.gov/portal/datasets/usps_crosswalk.html. Accessed 10 Jan 2021.
- 42.Glanz K, Bishop DB. The role of behavioral science theory in development and implementation of public health interventions. Annu Rev Public Health. 2010;31:399–418. doi: 10.1146/annurev.publhealth.012809.103604. [DOI] [PubMed] [Google Scholar]
- 43.National Cancer Institute, Division of Cancer Control and Population Sciences, Behavioral research program website. Constructs and measures for health behavior. cancercontrol.cancer.gov/brp/research/constructs. Accessed 19 Oct 2021.
- 44.Eaton LA, Kalichman SC. Social and behavioral health responses to COVID-19: lessons learned from four decades of an HIV pandemic. J Behav Med. 2020;43(3):341–345. doi: 10.1007/s10865-020-00157-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Bokemper SE, Cucciniello M, Rotesi TE, et al. Beliefs about mask efficacy and the effect of social norms on mask wearing intentions for COVID-19 risk reduction. PLoS One. 2021;16(10):e0258282. doi: 10.1371/journal.pone.0258282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.DeJonckheere M, Waselewski M Amaro, X, Frank A, Chua KP, Views on COVID-19 and use of face coverings among US youth. J Adolesc Health. 2021;68(5):873–881. doi: 10.1016/j.jadohealth.2021.02.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Gette JA, Stevens AK, Littlefield AK, Hayes KL, White HR, Jackson KM. Individual and COVID-19-specific indicators of compliance with mask use and social distancing: the importance of norms, perceived effectiveness, and state response. Int J Environ Res Public Health. 2021;18(16):8715. doi: 10.3390/ijerph18168715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Chen CY-C, Lei M. Psychosocial factors associated with mask-wearing behavior during the COVID-19 pandemic. Psychol Health Med. 2022;27(9):1996–2006. 10.1080/13548506.2021.1998562. [DOI] [PubMed]
- 49.Latkin CA, Dayton L, Kaufman MR, Schneider KE, Strickland JC, Konstantopoulos A. Social norms and prevention behaviors in the United States early in the COVID-19 pandemic. Psychol Health Med. 2022;27(1):162–177. doi: 10.1080/13548506.2021.2004315.10(1080/13548506),pp.2004315,2021. [DOI] [PubMed] [Google Scholar]
- 50.Rose JP, Edmonds KA. Social comparisons for following health recommendations and their relation to worry and intentions during COVID-19. European Journal of Health Psychology. 2021;28(4):141–151. doi: 10.1027/2512-8442/a000080. [DOI] [Google Scholar]
- 51.Wilson RF, Sharma AJ, Schluechtermann S, et al. Influencing risk for COVID-19 exposure among young adults aged 18–23 years - Winnebago County, Wisconsin March-July 2020. Morb Mortal Wkly Rep. 2020;69(41):1497–1502. doi: 10.15585/mmwr.mm6941e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Hutchins HJ, Wolff B, Leeb R, Ko JY, Odom E, Willey J, Friedman A, Bitsko RH. COVID-19 mitigation behaviors by age group—United States, April–June 2020. Morb Mortal Wkly Rep. 2020;69(43):1584–1590. doi: 10.15585/mmwr.mm6943e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.MacIntyre CR, Nguyen PY, Chughtai AA, Trent M, Gerber B, Steinhofel K, Seale H. Mask use, risk-mitigation behaviours and pandemic fatigue during the COVID-19 pandemic in five cities in Australia, the UK and USA: a cross-sectional survey. Int J Infect Dis. 2021;106:199–207. doi: 10.1016/j.ijid.2021.03.056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Moss J, Alexander L, Barré I, Parham I, Gillyard T, Davis J, Cunningham-Erves J. Understanding physical distancing and face mask use across high-risk African American subgroups during the COVID-19 pandemic: application of health belief model. Health Promot Pract. 2023;0(0). 10.1177/15248399221151176. [DOI] [PMC free article] [PubMed]
- 55.Adeagbo M, Olukotun M, Musa S, Alaazi D, Allen U, Renzaho AMN, Sekyi-Otu A, Salami B. Improving COVID-19 vaccine uptake among Black populations: a systematic review of strategies. Int J Environ Res Public Health. 2022;19(19):11971. doi: 10.3390/ijerph191911971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Salimi A, El Hawary H, Diab N, Smith L. The North American Layman’s understanding of COVID-19: are we doing enough? Front Public Health. 2020;8:358. doi: 10.3389/fpubh.2020.00358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Kasting ML, Head KJ, Hartsock JA, Sturm L, Zimet GD. Public perceptions of the effectiveness of recommended non-pharmaceutical intervention behaviors to mitigate the spread of SARS-CoV-2. PloS One. 2020;15(11):e0241662. doi: 10.1371/journal.pone.0241662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Taylor S, Asmundson GJG. Negative attitudes about facemasks during the COVID-19 pandemic: the dual importance of perceived ineffectiveness and psychological reactance. PloS One. 2021;16(2):e0246317. doi: 10.1371/journal.pone.0246317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Broomell SB, Chapman GB, Downs JS. Psychological predictors of prevention behaviors during the COVID-19 pandemic. Behav Sci Policy. 2020;43–50. 10.1353/bsp.2020.0014.
- 60.Warnecke RB, Johnson TP, Chávez N, et al. Improving question wording in surveys of culturally diverse populations. Ann Epidemiol. 1997;7(5):334–342. doi: 10.1016/s1047-2797(97)00030-6. [DOI] [PubMed] [Google Scholar]
- 61.Capraro V, Barcelo H. Telling people to “rely on their reasoning” increases intentions to wear a face covering to slow down COVID-19 transmission. Appl Cogn Psychol. 2021;35:693– 699. 10.1002/acp.3793. [DOI] [PMC free article] [PubMed]
- 62.Cunningham GB, Nite C. Demographics, politics, and health factors predict mask wearing during the COVID-19 pandemic: a cross-sectional study. BMC Public Health. 2021;21(1):1403. doi: 10.1186/s12889-021-11424-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Powdthavee N, Riyanto YE, Wong ECL, Yeo JXW, Chan QY. When face masks signal social identity: explaining the deep face-mask divide during the COVID-19 pandemic. PLoS ONE. 2021;16(6):e0253195. doi: 10.1371/journal.pone.0253195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Cunningham-Erves J, Brandt HM, Sanderson M, Clarkson K, Lee O, Schlundt D, Bonnet K, Davis J. Development of a theory-based, culturally appropriate message library for use in interventions to promote COVID-19 vaccination among African Americans: formative research. JMIR Form Res. 2022;6(7):e38781. doi: 10.2196/38781. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
For more information regarding data availability, contact the corresponding author.