Abstract
Background
Intranasally administered insulin has shown promise in both rodent and human studies in Alzheimer's disease; however, both effects and mechanisms require elucidation.
Objective
We assessed the effects of intranasally administered insulin on white matter health and its association with cognition and cerebral spinal fluid biomarker profiles in adults with mild cognitive impairment or Alzheimer's disease in secondary analyses from a prior phase 2 clinical trial (NCT01767909).
Design
A randomized (1:1) double-blind clinical trial.
Setting
Twelve sites across the United States.
Participants
Adults with mild cognitive impairment or Alzheimer's disease.
Intervention
Participants received either twice daily placebo or insulin (20 IU Humulin R U-100 b.i.d.) intranasally for 12 months. Seventy-eight participants were screened, of whom 49 (32 men) were enrolled.
Measurements
Changes from baseline in global and regional white matter hyperintensity volume and gray matter volume were analyzed and related to changes in cerebral spinal fluid biomarkers, Alzheimer's Disease Assessment Scale-Cognition, Clinical Disease Rating-Sum of Boxes, Alzheimer's Disease Cooperative Study-Activities of Daily Living Scale, and a memory composite.
Results
The insulin-treated group demonstrated significantly reduced changes in white matter hyperintensity volume in deep and frontal regions after 12 months, with a similar trend for global volume. White matter hyperintensity volume progression correlated with worsened Alzheimer's disease cerebral spinal fluid biomarker profile and cognitive function; however, patterns of correlations differed by treatment group.
Conclusion
Intranasal insulin treatment for 12 months reduced white matter hyperintensity volume progression and supports insulin's potential as a therapeutic option for Alzheimer's disease.
Key words: Alzheimer's disease, clinical trial, intranasal insulin, white matter, CSF
Introduction
Alzheimer's disease (AD) is the leading cause of dementia and, as there are currently no disease modifying treatments, its prevalence is expected to increase in response to an aging population (1). AD is characterized by aggregation of amyloid beta (Aβ) plaques and tau neurofibrillary tangles (NFT). Clinical trials have attempted to reduce accumulation of these proteins in the brain and prevent further cognitive decline; however, although some amyloid antibody trials have successfully reduced plaque load, none have been successful to date in halting the progression of AD symptoms (2, 3). Positron Emission Tomography (PET) measures AD pathology by quantifying the load of Aβ and NFT in the brain, and a number of studies have demonstrated relationships between PET measures and concentrations of these proteins in cerebral spinal fluid (CSF) (4, 5). CSF Aβ42 decreases as amyloid accumulation in brain increases, suggesting it is being sequestered in the brain parenchyma, while hyperphosphorylated tau (p-tau) in CSF increases with increased propagation of NFT (6). Utilizing ratios of Aβ42 to Aβ40, p-tau, and total tau (t-tau) has been found to further improve specificity and sensitivity to identify AD dementia (7, 8). There remains a clear need for a pharmacological intervention to prevent or slow AD progression.
As AD progresses, gray matter volume is reduced. While this is also true of non-pathological aging, adults with AD exhibit a far greater reduction in overall gray matter associated with a predictable pattern (9). The hippocampus and entorhinal cortex are perhaps the most easily detected regions affected by AD (10); however, an AD-defined meta region including the hippocampus and other regions such as entorhinal, inferior temporal, middle temporal, inferior parietal, fusiform, and precuneus has recently been utilized in order to increase sensitivity (11). Cortical thickness has also been postulated to be a more reliable marker of AD progression as it is less affected by total intracranial volume which can vary greatly between patients (11). While progression of the disease and corresponding gray matter reduction have been well established, its utility as a clinical trial endpoint needs to be validated. Interventions that have successfully removed amyloid or even allayed cognitive decline have also been associated with reduced gray matter volume (12, 13). These findings illustrate a complex relationship between brain health and gray matter volumetrics which is not fully understood.
White matter integrity can be reflected by the presence of white matter hyperintensities (WMH) detected with magnetic resonance imaging (MRI); however, the relationship of WMHs and AD progression has not been characterized in detail. WMHs are detected using fluid-attenuated inversion recovery (FLAIR) MRI, are presumed to indicate cerebrovascular pathology (14), and are associated with gliosis, demyelination, axonal loss, and arteriosclerosis (15). It is postulated that WMHs reflect a number of factors including hypoxia, amyloid angiopathy, blood brain barrier damage, degeneration, hypoperfusion, and inflammation (15). WMH volume (WMHV) increases with age and some studies have found WMHV to be independent of Aβ burden, leading to the proposal that WMHs should be considered a co-pathology that do not directly contribute to AD (16, 17). Other studies have found correlations between WMHs and cortical tau load in AD (18). It has been proposed that cerebrovascular pathology represented by WMHs precedes and therefore could initiate Aβ aggregation (19, 20, 21). Conversely, other investigators claim that Aβ induces vascular damage through neuroinflammation, formation of reactive oxygen species, and oxidative stress (22, 23). It is possible that vascular and AD-specific pathology form a vicious cycle giving rise to these differing viewpoints, or that the precise time course of the association differs for subgroups of patients with AD.
Identification of the nature of the association of WMHs and AD is hindered by lack of a commonly-accepted standardized approach to measurement of WMHs (24). Methods evaluating WMHs range from semi-quantitative visual reads using one of 3 established rating scales (Manolio, Fazekas and Schmidt, Scheltens) to fully automated lesion segmentation (25, 26). Representation of the data is also not consistent, with some studies reporting global ratings or volumes and others focusing on spatial patterns (27, 28). There are also many ways to spatially segment WMHs such as periventricular versus deep (29); however, deep can also be further split in to juxtacortical and non-juxtacortical[30]. Studies in which WMHs are segmented in classical lobular fashion have reported that AD is associated with temporal WMHs (31), or with global and parietal/occipital volumes (32). Volumes can also be displayed as raw volumes (33), log transformed values (33), or percent change ratios (34, 35). As the field progresses automated techniques generating quantitative spatially accurate information may prove the best way to track WMH progression in AD. It is clear that WMHs are associated with poor cognitive outcomes and preventing progression is a clinically relevant marker.
A promising area of research in the treatment and prevention of AD focuses on metabolism, inflammation and, in particular, the role of insulin in the central nervous system. With respect to metabolism, although insulin does not appear to impact global transport of glucose into the brain, it has been shown to increase glucose uptake via the glucose transporter GLUT4 in selected regions such as the hippocampus (36). Further, insulin increases glycogen storage in astrocytes, thereby providing an alternate energy source during glucose deprivation or intense neuronal activity (37). Insulin has long been implicated in AD and several reviews have highlighted both its importance and therapeutic potential (38, 39, 40). In short, insulin has been demonstrated to modulate both Aβ and pathological tau formation, and improves neuronal health, dendritic spine proliferation, and white matter integrity. Insulin can be administered intranasally where it is detectible in perivascular spaces with PET imaging (41) and in the CSF in less than 30 minutes (42). A promising pilot trial documented improvements in delayed memory recall, preserved Alzheimer's Disease Assessment Scale (ADAS-Cog) scores, and functional abilities assessed by the Alzheimer's Disease Cooperative Study-Activities of Daily Living Scale (ADCS-ADL) after 4 months of treatment with intranasal insulin compared to placebo (43). A recent large 18-month phase II clinical trial of INI treatment in AD and MCI patients found differing patterns of results depending on the device used to administer the insulin (13). For the device used by the primary intent-to-treat cohort, no significant differences in rates of decline measured by the ADAS-Cog13, Clinical Disease Rating-Sum of Boxes (CDR-SOB), ADCS-ADL, or CSF Aβ and tau were observed between placebo and insulin groups. In a secondary cohort, a different device showed better performance on ADAS-Cog13 in the insulin-treated group compared to placebo at 6 months with a similar trend at 12 months. In open-label analyses, the early-start secondary device cohort treated with insulin performed better on the ADAS-Cog13 and ADL-MCI at 18 months than the delayed start secondary group. The insulin-treated group using this device also demonstrated an improvement in CSF Aβ42/Aβ40 and Aβ42/t-tau ratios at 12 months. This study highlights the need for additional investigation to definitively determine the potential for intranasal insulin as a therapeutic for AD.
In the present study, we assessed the effects of INI on white matter health in the secondary cohort of participants using the device associated with improved cognition and AD biomarker profiles. There are several mechanisms through which insulin could act directly to improve white matter health and prevent WMH progression (44). Reduced insulin levels or activity impair oligodendrocyte myelin survival and maintenance, and increase ceramides and decreases sulfatides, leading to oxidative stress, inflammation, and lipid peroxidation. These factors all contribute to myelin damage and subsequent WMHs. Insulin resistance impairs vascular responsiveness, causing luminal narrowing and fibrosis, which cause decreased blood flow and blood brain barrier damage. These effects lead to ischemia and inflammation and promote the formation of WMHs. As mentioned previously, insulin reduces Aβ and p-tau levels in the brain, both of which can cause inflammation, neuronal and glial damage, and vascular impairment (45). These distinct pathways could all culminate in the formation and progression of WMHs, thus poising insulin at a convergence point in several potential cascades, and raising the possibility that providing insulin to the brain to overcome deficient insulin availability or activity may have therapeutic benefit in AD.
Based on this evidence, we examined the effect of 12 months of INI treatment vs. placebo on change in WMHs. We also examined the relationships among changes in WMHs, cognition, and AD CSF biomarkers.
Methods
The study was overseen by the Alzheimer's Therapeutic Research Institute (P. Aisen, Director) together with the Principal Investigator (S. Craft). Eligibility and recruitment for this study have been described previously (13). Two devices were used in the parent study; however, only one device demonstrated cognitive benefits or changes in AD CSF biomarkers across the 18-month long study. For this reason, we evaluated only the group using the device that showed potential beneficial effects. Briefly, participants with AD (n=31) or amnestic MCI (n=18) were recruited from 12 sites. Participants received baseline testing including CDR, MMSE, ADAS-Cog13, a lumbar puncture, and an MRI, then were randomized on a 1:1 basis to receive either 20 IU intranasal insulin (n=24) or placebo (n=25) twice daily for 12 months. After 12 months the cognitive battery was readministered, a lumbar puncture was performed, and another MRI was obtained. There were a total of 40 participants (insulin n=20; placebo n=20) with MRI data that passed quality control measures at baseline and month 12.
T1 and Fluid Attenuated Inversion Recovery images were collected with 1.5 or 3T MRI. T1 weighed images were processed using FreeSurfer 6.0.0 to produce participant specific gray matter volume, thickness, and area. FLAIR images were segmented by the lesion growth algorithm[46] as implemented in the LST toolbox version 3.0.0 (www.statisticalmodelling.de/lst.html) for SPM. The algorithm first segments the T1 images into the three main tissue classes (CSF, GM and WM). This information is then combined with the coregistered FLAIR intensities in order to calculate lesion belief maps. By thresholding these maps with a pre-chosen initial threshold (κ= 0.3) an initial binary lesion map is obtained which is subsequently grown along voxels that appear hyperintense in the FLAIR image. The result is a lesion probability map. The lesion probability maps were then warped to MNI space and lobular volume was extracted using Mayo Clinic Adult Lifespan Template (47). A temporal-parietal volume meta-ROI was created to examine volume and was defined as bilateral entorhinal, inferior temporal, middle temporal, inferior parietal, fusiform, and precuneus (11). Cortical thickness was similarly defined by Jack (48) as the surface area weighted thickness of the entorhinal, inferior temporal, middle temporal, and fusiform.
CSF was collected in the morning after an overnight fast and was immediately placed on dry ice and was shipped overnight to the central biomarker laboratory. AD biomarkers Aβ42, Aβ40, total tau, and tau phosphorylated at threonine 181 were quantified with the Meso Scale Discovery platform (Meso Scale Diagnostics). Blood was collected for APOE genotyping using established protocols.
Cross sectional analysis was performed to assess group differences at baseline in age, cognitive status, sex, baseline surface weighted cortical thickness, AD signature region volume, total WMHV, and regional WMHV at baseline using general linear models or chi squared tests when appropriate. Change variables for gray matter and WMHV were defined as percentage change from baseline as previously described (35). General linear modeling was performed in SAS v 9.4 with covariates age, ApoE4 status, study site, and sex included in all initial models. Baseline volumes were also included for GMV and WMHV models, and total intracranial volume was included in models analyzing data in native space. Non-contributing covariates (p>0.15) were dropped from the model. No adjustments were made for multiple comparisons; rather, results are reported as mean estimates and corresponding 95% confidence intervals. In exploratory analyses, we examined whether individual treatment groups showed reliable change in WMHV over time with within-group LSMEANS t-tests. Change variables for WMHV, cognitive scores, and CSF values were subjected to Pearson's r correlations to determine inter-relationships.
Results
Participants
For the parent study secondary cohort that utilized the device associated with cognitive benefit, 78 participants were screened, of whom 49 (32 men [65.3%]) were enrolled. Twenty-four were randomized to the insulin arm and 25 were randomized to the placebo arm (Figure 1). Of those 49, 40 participants (insulin n=20, placebo n=20) had usable MRI data at both time points and were analyzed for this study. There were no demographic or other notable clinical differences between participants with usable and unusable data. There were also no differences in demographic characteristics between arms at baseline (Table 1).
Figure 1.

CONSORT diagram
Table 1.
Descriptive characteristics of cohort
| Placebo n = 20 | Insulin n = 20 | Combined n = 40 | |
|---|---|---|---|
| Gender | |||
| Male | 14 (70%) | 11 (55%) | 25 (62%) |
| Female | 6 (30%) | 9 (45%) | 15 (38%) |
| Diagnosis | |||
| AD | 15 (75%) | 11 (55%) | 26 (65%) |
| MCI | 5 (25%) | 9 (45%) | 14 (35%) |
| Racial Categories | |||
| Black or African American | 0 (0%) | 1 (5%) | 1 (2%) |
| White | 20 (100%) | 19 (95%) | 39 (98%) |
| APOE-ε4 Carriage | |||
| No | 4 (20%) | 5 (25%) | 9 (23%) |
| Yes | 16 (80%) | 15 (75%) | 31 (77%) |
| Age, years (SD) | 70.88 (5.69) | 71.69 (8.25) | 71.28 (7.01) |
| Education, years (SD) | 17.2 (2.48) | 16.05 (2.87) | 16.62 (2.71) |
| Baseline ADAS-cog | 24.75 (8.75) | 24.15 (7.36) | 24.45 (7.99) |
| Baseline ADL | 39.65 (7.35) | 42.65 (7.23) | 41.15 (7.35) |
| Baseline CDR-SOB | 3.15 (1.65) | 2.7 (1.36) | 2.92 (1.51) |
MRI Results
The temporal-parietal meta-ROI decreased in volume over time as did the surface weighted cortical thickness (both ps<.001, Figure 2). There was no interaction between treatment arm and rate of decline of gray matter or cortical thickness (Supplementary Table 1).
Figure 2.

Changes in gray matter A) volume and B) surface weighted thickness in the temporal-parietal meta-ROI
There were no significant differences between treatment group and placebo. Error bars represent 95% confidence intervals.
An interaction between treatment arm and global WMHV was observed such that the insulin-treated arm tended to have less global WMH volume increase over the 12 month intervention compared to the placebo group (insulin lsmeans [95% CI]=18.98 [−1.38,39.33] and placebo 42.21 [21.70,62.72], p=0.064, Figure 3). Given this trend, exploratory analyses were conducted for comparisons of individual ROIs between treatment arms. Insulin significantly reduced WMHV change over the 12 month intervention in both the frontal lobe and deep white matter compared to placebo (frontal insulin lsmeans [95% CI]=15.14 [−3.84,34.12] and placebo=39.18 [20.05,58.30], p=0.042; deep WM insulin lsmeans [95% CI]=56.94 [−20.20,134.08] and placebo=161.37 [81.68, 241.05], p=0.042, Figure 3). Change in WMHV was less in the insulin arm than the placebo arm for all other regions, although these comparisons did not reach statistical significance.
Figure 3.
White Matter Hyperintensity Volume (WMHV) as percent change from baseline both globally and regionally split by MCALT (excluding cerebellum and midbrain regions)
There were significant differences between the degree of change for insulin and placebo groups in the deep white matter and frontal regions with a similar trend for global change (+ p<0.10, * p<0.05). The placebo group showed significantly increased change from baseline WMHV in all regions, whereas the insulin group showed significant change only in temporal lobe with a trend for global change (# <0.10, ## p<0.05). Error bars represent 95% confidence intervals.
When we examined whether individual treatment groups showed reliable change in WMHV over time with within-group LSMEANS t-tests, the placebo group showed significantly increased WMHVs across all regions (all ps<0.05, Figure 3; raw means for baseline and month 12 for all regions are presented in Supplementary Table 2), whereas WMHV was unchanged following insulin treatment in the deep white matter, corpus callosum, occipital, parietal, and frontal regions (all p>0.1, Figure 3). Temporal WMHV increased slightly over the 12 month intervention with insulin treatment with a similar trend in global WMHV (temporal p=0.033; global p=0.066), although to a lesser degree than with placebo.
Correlation between MRI and Cognitive Outcomes
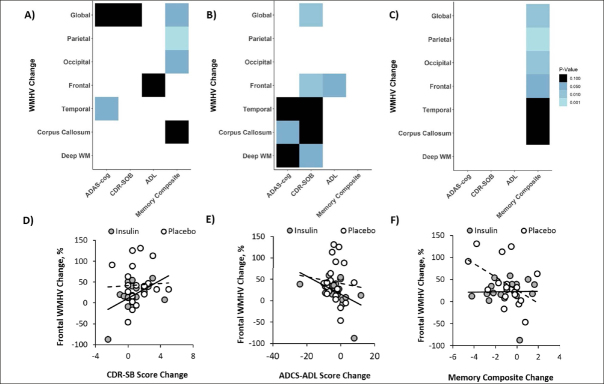
For the combined cohort including both insulin and placebo groups, increased global WMHV correlated with lowered memory composite scores (r=−0.38, p=0.024, Figure 4A) and similar trends were observed for the ADAS-Cog13 and CDR-SOB (r=0.297, p=0.062; r=0.278, p=0.081, figure 4A). Regional analysis revealed a significant correlation between the memory composite score and parietal and occipital WMHVs and a trend correlation for the corpus callosum (r=−0.536, p=0.001; r=−0.405, p=0.015; r=0.31, p=0.069, Figure 4A). Increased temporal WMHV was associated with worsened (higher) scores for the ADAS-Cog13 (r=0.313, p=0.049, Figure 4A). A similar trend correlation was observed between frontal WMHV and ADCS-ADL scores (r=−0.267, p=0.095, Figure 4A).
Figure 4.
Changes in global and regional White Matter Hyperintensity Volume (WMHV) correlate with changes in ADAS-cog, CDR-SB, ADCS-ADL, and a memory composite
Analyses were performed for both insulin and placebo groups combined (A) and for the insulin treatment arm (B) and placebo (C) groups independently. Light colors represent correlations with lower p values (ps range from <0.001 to 0.10 from light to dark). Exemplar scatterplots are shown that demonstrate relationships between change in frontal WMHVs (which differed between insulin and placebo groups) and change in (D) CDR-SB, (E) ADCS-ADL, and (F) memory composite scores.
When analyzed by treatment group, the insulin group showed a significant correlation between change in ADAS-Cog13 scores and WMHVs change in the corpus callosum, and trending correlations for the deep white matter and temporal regions (r=0.459, p=0.041; r=0.409, p=0.073; r=0.368, p=0.092, Figure 4B). Increased (worsened) CDR-SOB scores correlated significantly with increased frontal and global WMHV with trends noted for deep white matter, temporal, and the corpus callosum regions (r=0.535, p=0.014; r=0.537, p=0.014; r=0.439, p=0.052; r=0.426, p=0.059; r=0.409, p=0.061, Figure 4B). Smaller increases in frontal WMHV also correlated with smaller increases in ADCS-ADL scores (r=−0.475, p=0.034). In the placebo group, declines in memory composite scores only correlated with increased WMHV in global, parietal, and occipital regions with trends for frontal, corpus callosum, and temporal regions (r=−0.639, p=0.005; r=−0.773, p=0.001; r=−0.585, p=0.013; r=−0.48, p=0.05; r=0.435, p=0.08; r=−0.425, p=0.088, Figure 4C).
Correlation between MRI and CSF outcomes
For the combined cohort including both insulin and placebo groups, global WMHV increase correlated with a decrease in CSF Aβ42 and with a similar trend for the Aβ42/Aβ40 ratio (r=−0.375, p=0.028; r=−0.328, p=0.058, Figure 5A). Frontal WMHV increases also correlated with decreases in both Aβ42 and Aβ42/Aβ40 ratio (r=−0.355, p=0.039; r=−0.44, p=0.009, Figure 5A). Increases in both corpus callosum and deep white matter WMHV correlated with decreases in Aβ42/tau ratio (r=−0.397, p=0.001; r=−0.734, p=0.001, figure 5A).
Figure 5.
Changes in global and regional White Matter Hyperintensity Volume (WMHV) correlate with changes in CSF AD biomarkers
Analyses were performed for both insulin and placebo groups combined (A) and for the insulin treatment arm (B) and placebo (C) groups independently. Light colors represent correlations with lower p values (ps range from <0.001 to 0.10 from light to dark). Exemplar scatterplots are shown that demonstrate relationships between change in frontal WMHVs (which differed between insulin and placebo groups) and change in CSF (D) Aβ42, (E) Aβ42/Aβ40 ratio, and (F) Aβ42/T-tau ratio.
When analyzed by treatment group, there was a significant correlation between increased parietal WMHV and decreased Aβ40 in the insulin group (r=−0.525, p=0.036, figure 5B). There were trending relationships between increased global WMHV and decreased Aβ42/ Aβ40 ratio, increased frontal WMHV and decreased Aβ42/Aβ40 ratio and Aβ42/t-tau ratio changes, and increased corpus callosum and decreased Aβ42 levels (r=−0.443, p=0.085; r=−0.467, p=0.067; r=−0.477, p=0.061; r=−0.446, p=0.083, figure 5B). In the placebo group, increases in both corpus callosum and deep white matter WMHV correlated with decreases in Aβ42/t-tau ratio (r=−0.733, p=0.001; r=−0.724, p=0.001, figure 5C). Temporal WHV change positively correlated with ptau-181/t-tau ratio (r=0.481, p=0.043, figure 5C). There was a trend for both global and frontal WMHV change to negatively correlate with Aβ42 change (r=−0.431, p=0.073; r=−0.408, p=0.092, figure 5C).
Discussion
The present study found that increased WMHV correlated with greater declines in cognition and worsening of CSF AD biomarker profiles, and that INI treatment for 12 months reduced WMHV progression in key brain regions. White matter hyperintensities represent cerebral small vessel disease and white matter damage resulting from degraded myelin, and have been shown to increase with aging. Some studies have suggested that regional, and not global WMHV may best predict, or correlate, with AD progression (49). While there are numerous ways to segregate WMHs the most promising research has suggested a division between frontal and posterior regions in differentiating normal versus pathological aging, with lobular divisions further increasing the regional specificity (32, 50). We observed that INI treatment for 12 months slowed the progression of WMHs globally and in deep WM and frontal regions compared to placebo assignment. This finding supports previous studies linking frontal WMHs and pathological aging and suggests that INI may reduce AD-related WMH progression in these key areas. Exploratory analysis also demonstrated that for all other regions, with the exception of the temporal lobe, progression of WMHs were stabilized following insulin treatment. These findings may be considered clinically significant as growing research has shown that WMHVs correlate with numerous pathological outcomes such as ependymal loss, cerebral ischemia, and demyelination (51). Insulin could be acting through a number of pathways to preserve white matter health (44). Insulin resistance impairs oligodendrocyte myelin maintenance and survival, while also leading to reduced vascular smooth muscle responsiveness. Increasing insulin availability could ameliorate these deficiencies thereby reducing WMH progression.
Previous research has shown that higher baseline WMHV predicts worse cognitive outcomes measured by the ADAS-Cog (52) and CDR (53). We demonstrated in the combined cohort that over 12 months, longitudinal increases in WMHV correlate with decreases in cognition measured by the ADAS-Cog, CDR-SOB, ADCS-ADL, and a memory composite. We also found that correlations differed depending on treatment group. The placebo group showed correlations only between WMHV and memory composite scores, while the insulin treated group showed associations between WMHs and both the ADAS-Cog13 and CDR-SOB, as well as the ADCS-ADL. Of note, in the parent study, insulin treatment was shown to benefit performance on the ADAS-Cog13, CDR, and ADCS-ADL for the secondary cohort (13). The present findings raise the possibility that insulin's effects on these measures are mediated in part by factors associated with WMHV. These findings suggest that preventing or even delaying progression of white matter damage could prevent global cognitive and functional decline.
Increased CSF Aβ42 levels and decreased hyperphosphorylated tau concentrations have been proposed as markers demonstrating improvement in AD pathology (54, 55). Studies have shown that greater Aβ load, indicated by lower CSF Aβ42 concentration and increased Aβ PET, correlates with greater WMH burden (56, 57, 58, 59); however, the findings regarding p-tau and total tau are less consistent, with some studies reporting correlations (18, 60) while other do not (59, 61, 62). In the parent study, insulin treatment was associated with improved (increased) Aβ42/Aβ 40 and Aβ42/tau ratios (13) for the secondary cohort treated with the device which was associated with cognitive benefit. The present study adds to these findings by demonstrating that WMHV changes inversely correlate with changes in Aβ40, Aβ42, Aβ42/Aβ40 ratio, and Aβ42/t-tau ratio; however, these associations differ by region and CSF metric. The relationship between WMHV and tau and Aβ may change throughout the course of the disease as Aβ pathology is stabilized and tau pathology increases; however, this hypothesis is still in contention (59). Insulin affects the regulation of both Aβ and hyperphosphorylated tau (63). Both Aβ40 (64) and Aβ42 (65) cause inflammation via production of reactive oxygen species. Aβ42 aggregates and starts seeding points which grow to plaques leading to death in several cell types including oligodendrocytes (66, 67), while Aβ40 is more prone to form deposits on vessels walls where it damages pericytes (68, 69). Hyperphosphorylated tau also leads to neurovascular dysfunction resulting in reduced energy supply due to aberrant vessel dilation (70). Insulin may act indirectly to stop WMH progression by preventing damage caused by hyperphosphorylated tau, Aβ40, and Aβ42 to both the blood brain barrier and myelin producing oligodendrocytes. Further research needs to be done to elucidate patterns behind regional WMH load and CSF AD biomarkers of Aβ and tau.
Numerous studies have sought to identify the temporal and spatial patterns of gray matter volume loss in typical AD progression (71). While there is not a consensus across all studies, several vulnerable regions have been highlighted (11, 72). Measures of gray matter volume and thickness were unchanged by 12 months of INI administration. It is possible that our region of interest, while widely accepted, failed to capture subtle differences between treatment groups. Other regions of the brain that were excluded from our analysis may be more sensitive to changes specific to this intervention. Previous interventions have shown decreased rates of atrophy in patients with MCI treated with other noninsulin interventions; however, these findings were over a 2-year period (73). It is possible that our intervention was not long enough to detect subtle changes in gray matter volume. Cognitive improvement has been observed without halting gray matter atrophy. A phase II clinical trial testing daily administration of resveratrol showed greater reduction in brain volume in the treatment group compared to placebo after one year of treatment, but the resveratrol-treated group also showed less decline on the ADCS-ADL suggesting interventions can still be beneficial independent of apparent reduction of gray matter volume (74).
Our study had several limitations. Our small sample size may have contributed to our inability to detect preservation of gray matter volume and cortical thickness by INI treatment, and may also have reduced our ability to detect relationships between WMHVs and other measures. Our cohort was predominantly white (93%) and male (62%) and thus results may not generalize to a more diverse population. A number of participants did not complete the trial or had usable data at either baseline or follow up. These missing datapoints could result in a completer bias; however, this is unlikely as those with incomplete data did not differ demographically or in any baseline measures from completers. It is also possible that a longer intervention may be needed to observe a divergence between groups on our measures. These results need to be replicated in a larger, longer study in order to determine the effects of insulin on the brain WM health and the mechanistic pathways underlying these effects.
In conclusion, we found that treating MCI and AD patients with 12 months of INI significantly reduced WMH progression without affecting gray matter volume or cortical thickness, and that increases in WMHV correlated with both worsening in AD CSF biomarker profile and cognitive/functional measures. These findings support insulin's potential as a therapeutic option for AD; however, more research needs to be conducted to elucidate mechanism through which insulin may impact white matter integrity.
Acknowledgments
Funding and acknowledgments: This study was supported by the National Institute on Aging (NIA RF1AG041845). Eli Lilly provided diluent placebo for the blinded phase of the trial, and insulin for the open label portion at no cost; they had no input into the design, conduct or interpretation of trial results or in the preparation of this manuscript. The authors would like to thank the site personnel, and the following Site Prinicipal Investigators for their perseverance throughout the trial: Deniz Erten-Lyons, David Knopman, Joseph Kass, Rachelle Doody, Hillel Grossman, Neelum Aggarwal, Esther Oh, Gregory Jicha, Anton Porsteinsson, Aimee Pierce, Gaby Thai, Ruth Mulnard, Allan Levey, Jeffrey Burns, Neill Graff-Radford, Jared Brosch, Martin Farlow, Christopher van Dyck, Marek-Marsel Mesulam, Ian Grant, Raymond Scott Turner, Scott McGinnis, Thomas Obisesan, Alan Lerner, Allison Perrin, Laura Baker, Elaine Peskind, Henry Querfurth, Brian Ott, Ralph Richter, Jacobo Mintzer, Marwan Sabbagh, Jiong Shi, Daniel Press, Shauna Yuan, David Carr, Nupar Ghoshal, Amanda Smith, James Galvin, and Kyle Womack. We are particularly grateful to the trial participants for their dedication.
Electronic supplementary material
Supplementary material is available for this article at https://doi.org/10.14283/jpad.2021.14 and is accessible for authorized users.
Supplemental Table 1. Raw means and confidence intervals for temporal-parietal ROI volume and thickness change split by treatment group.
Supplemental Table 2. Raw means for global and regional white matter hyperintensity volumes at screening and month 12 follow-up for insulin and placebo groups.
Conflict of interest: The authors have no conflict of interest to report.
Ethical Standards: The study was approved by the Institutional Review Boards of all participating institutions. All participants provided written informed consent to participate in the study.
References
- 1.Association, A.s. 2019 Alzheimer's disease facts and figures. Alzheimer's & Dementia. 2019;15(3):321–387. 10.1016/j.jalz.2019.01.010 [Google Scholar]
- 2.Sevigny J, Chiao P, Bussiere T, et al. The antibody aducanumab reduces Abeta plaques in Alzheimer's disease. Nature. 2016;537(7618):50–56. doi: 10.1038/nature19323. 10.1038/nature19323 PubMed PMID: 27582220. [DOI] [PubMed] [Google Scholar]
- 3.Klein G, Delmar P, Kerchner GA, et al. Thirty-Six-Month Amyloid Positron Emission Tomography Results Show Continued Reduction in Amyloid Burden with Subcutaneous Gantenerumab. J Prev Alzheimers Dis. 2021;8(1):3–6. doi: 10.14283/jpad.2020.68. PubMed PMID: 33336218. [DOI] [PubMed] [Google Scholar]
- 4.La Joie R, Bejanin A, Fagan AM, et al. Associations between [(18)F]AV1451 tau PET and CSF measures of tau pathology in a clinical sample. Neurology. 2018;90(4):e282–e290. doi: 10.1212/WNL.0000000000004860. 10.1212/WNL.0000000000004860 PubMed PMID: 29282337, PMCID 5798657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Schipke CG, Koglin N, Bullich S, et al. Correlation of florbetaben PET imaging and the amyloid peptide Ass42 in cerebrospinal fluid. Psychiatry Res Neuroimaging. 2017;265:98–101. doi: 10.1016/j.pscychresns.2016.10.011. 10.1016/j.pscychresns.2016.10.011 PubMed PMID: 28024844. [DOI] [PubMed] [Google Scholar]
- 6.Olsson B, Lautner R, Andreasson U, et al. CSF and blood biomarkers for the diagnosis of Alzheimer's disease: a systematic review and meta-analysis. Lancet Neurol. 2016;15(7):673–684. doi: 10.1016/S1474-4422(16)00070-3. 10.1016/S1474-4422(16)00070-3 PubMed PMID: 27068280. [DOI] [PubMed] [Google Scholar]
- 7.Hansson O, Lehmann S, Otto M, Zetterberg H, Lewczuk P. Advantages and disadvantages of the use of the CSF Amyloid beta (Abeta) 42/40 ratio in the diagnosis of Alzheimer's Disease. Alzheimers Res Ther. 2019;11(1):34. doi: 10.1186/s13195-019-0485-0. 10.1186/s13195-019-0485-0 PubMed PMID: 31010420, PMCID 6477717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Blennow K, Hampel H. CSF markers for incipient Alzheimer's disease. Lancet Neurol. 2003;2(10):605–613. doi: 10.1016/s1474-4422(03)00530-1. 10.1016/S1474-4422(03)00530-1 PubMed PMID: 14505582. [DOI] [PubMed] [Google Scholar]
- 9.Driscoll I, Davatzikos C, An Y, et al. Longitudinal pattern of regional brain volume change differentiates normal aging from MCI. Neurology. 2009;72(22):1906–1913. doi: 10.1212/WNL.0b013e3181a82634. 10.1212/WNL.0b013e3181a82634 PubMed PMID: 19487648, PMCID 2690968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jack CR, Jr., Barkhof F, Bernstein MA, et al. Steps to standardization and validation of hippocampal volumetry as a biomarker in clinical trials and diagnostic criterion for Alzheimer's disease. Alzheimers Dement. 2011;7(4):474–485. doi: 10.1016/j.jalz.2011.04.007. 10.1016/j.jalz.2011.04.007 PubMed PMID: 21784356, PMCID 3396131, e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Schwarz CG, Gunter JL, Wiste HJ, et al. A large-scale comparison of cortical thickness and volume methods for measuring Alzheimer's disease severity. Neuroimage Clin. 2016;11:802–812. doi: 10.1016/j.nicl.2016.05.017. 10.1016/j.nicl.2016.05.017 PubMed PMID: 28050342, PMCID 5187496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sur, C., J. Kost, D. Scott, et al., BACE inhibition causes rapid, regional, and non-progressive volume reduction in Alzheimer's disease brain. Brain, 2020. [DOI] [PMC free article] [PubMed]
- 13.Craft S, Raman R, Chow TW, et al. Safety, Efficacy, and Feasibility of Intranasal Insulin for the Treatment of Mild Cognitive Impairment and Alzheimer Disease Dementia: A Randomized Clinical Trial. JAMA Neurol. 2020;77(9):1099–1109. doi: 10.1001/jamaneurol.2020.1840. 10.1001/jamaneurol.2020.1840 PubMed PMID: 32568367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Raman MR, Kantarci K, Murray ME, Jack CR, Jr., Vemuri P. Imaging markers of cerebrovascular pathologies: Pathophysiology, clinical presentation, and risk factors. Alzheimers Dement (Amst) 2016;5:5–14. doi: 10.1016/j.dadm.2016.12.006. 10.1016/j.dadm.2016.12.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Abraham HM, Wolfson L, Moscufo N, Guttmann CR, Kaplan RF, White WB. Cardiovascular risk factors and small vessel disease of the brain: Blood pressure, white matter lesions, and functional decline in older persons. J Cereb Blood Flow Metab. 2016;36(1):132–142. doi: 10.1038/jcbfm.2015.121. 10.1038/jcbfm.2015.121 PubMed PMID: 26036933, PMCID 4758547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Roseborough A, Ramirez J, Black SE, Edwards JD. Associations between amyloid beta and white matter hyperintensities: A systematic review. Alzheimers Dement. 2017;13(10):1154–1167. doi: 10.1016/j.jalz.2017.01.026. 10.1016/j.jalz.2017.01.026 PubMed PMID: 28322203. [DOI] [PubMed] [Google Scholar]
- 17.Villeneuve S, Jagust WJ. Imaging Vascular Disease and Amyloid in the Aging Brain: Implications for Treatment. J Prev Alzheimers Dis. 2015;2(1):64–70. doi: 10.14283/jpad.2015.47. PubMed PMID: 25844350, PMCID 4381867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.McAleese KE, Firbank M, Dey M, et al. Cortical tau load is associated with white matter hyperintensities. Acta Neuropathol Commun. 2015;3:60. doi: 10.1186/s40478-015-0240-0. 10.1186/s40478-015-0240-0 PMCID 4589169, PubMed PMID: 26419828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Thal DR. The pre-capillary segment of the blood-brain barrier and its relation to perivascular drainage in Alzheimer's disease and small vessel disease. ScientificWorldJournal. 2009;9:557–563. doi: 10.1100/tsw.2009.72. 10.1100/tsw.2009.72 PubMed PMID: 19578713, PMCID 5823174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Iturria-Medina Y, Sotero RC, Toussaint PJ, Mateos-Perez JM, Evans AC, I. Alzheimer's Disease Neuroimaging Early role of vascular dysregulation on late-onset Alzheimer's disease based on multifactorial data-driven analysis. Nat Commun. 2016;7:11934. doi: 10.1038/ncomms11934. 10.1038/ncomms11934 PubMed PMID: 27327500, PMCID 4919512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Honjo K, Black SE, Verhoeff NP. Alzheimer's disease, cerebrovascular disease, and the beta-amyloid cascade. Can J Neurol Sci. 2012;39(6):712–728. doi: 10.1017/s0317167100015547. 10.1017/S0317167100015547 PubMed PMID: 23227576. [DOI] [PubMed] [Google Scholar]
- 22.Snyder HM, Corriveau RA, Craft S, et al. Vascular contributions to cognitive impairment and dementia including Alzheimer's disease. Alzheimers Dement. 2015;11(6):710–717. doi: 10.1016/j.jalz.2014.10.008. 10.1016/j.jalz.2014.10.008 PubMed PMID: 25510382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yamada M. Predicting cerebral amyloid angiopathy-related intracerebral hemorrhages and other cerebrovascular disorders in Alzheimer's disease. Front Neurol. 2012;3:64. doi: 10.3389/fneur.2012.00064. 10.3389/fneur.2012.00064 PubMed PMID: 22539931, PMCID 3336108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wardlaw JM, Smith EE, Biessels GJ, et al. Neuroimaging standards for research into small vessel disease and its contribution to ageing and neurodegeneration. The Lancet Neurology. 2013;12(8):822–838. doi: 10.1016/S1474-4422(13)70124-8. 10.1016/S1474-4422(13)70124-8 PubMed PMID: 23867200, PMCID 3714437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.van den Heuvel DM, ten Dam VH, de Craen AJ, et al. Measuring longitudinal white matter changes: comparison of a visual rating scale with a volumetric measurement. AJNR Am J Neuroradiol. 2006;27(4):875–878. PubMed PMID: 16611781, PMCID 8134007. [PMC free article] [PubMed] [Google Scholar]
- 26.Kapeller P, Barber R, Vermeulen RJ, et al. Visual rating of age-related white matter changes on magnetic resonance imaging: scale comparison, interrater agreement, and correlations with quantitative measurements. Stroke. 2003;34(2):441–445. doi: 10.1161/01.str.0000049766.26453.e9. 10.1161/01.STR.0000049766.26453.E9 PubMed PMID: 12574557. [DOI] [PubMed] [Google Scholar]
- 27.Ramirez J, McNeely AA, Scott CJM, Masellis M, Black SE, I., Alzheimer's Disease Neuroimaging White matter hyperintensity burden in elderly cohort studies: The Sunnybrook Dementia Study, Alzheimer's Disease Neuroimaging Initiative, and Three-City Study. Alzheimers Dement. 2016;12(2):203–210. doi: 10.1016/j.jalz.2015.06.1886. 10.1016/j.jalz.2015.06.1886 PubMed PMID: 26208292. [DOI] [PubMed] [Google Scholar]
- 28.Rizvi B, Narkhede A, Last BS, et al. The effect of white matter hyperintensities on cognition is mediated by cortical atrophy. Neurobiol Aging. 2018;64:25–32. doi: 10.1016/j.neurobiolaging.2017.12.006. 10.1016/j.neurobiolaging.2017.12.006 PubMed PMID: 29328963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.DeCarli C, Fletcher E, Ramey V, Harvey D, Jagust WJ. Anatomical mapping of white matter hyperintensities (WMH): exploring the relationships between periventricular WMH, deep WMH, and total WMH burden. Stroke. 2005;36(1):50–55. doi: 10.1161/01.STR.0000150668.58689.f2. 10.1161/01.STR.0000150668.58689.f2 PubMed PMID: 15576652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lindemer ER, Greve DN, Fischl B, Augustinack JC, Salat DH, I. Alzheimer's Disease Neuroimaging Differential Regional Distribution of Juxtacortical White Matter Signal Abnormalities in Aging and Alzheimer's Disease. J Alzheimers Dis. 2017;57(1):293–303. doi: 10.3233/JAD-161057. 10.3233/JAD-161057 PubMed PMID: 28222518, PMCID 5534349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Guzman VA, Carmichael OT, Schwarz C, et al. White matter hyperintensities and amyloid are independently associated with entorhinal cortex volume among individuals with mild cognitive impairment. Alzheimers Dement. 2013;9(5):S124–S131. doi: 10.1016/j.jalz.2012.11.009. PubMed PMID: 23375566, PMCID 3663926, Suppl. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lee S, Viqar F, Zimmerman ME, et al. White matter hyperintensities are a core feature of Alzheimer's disease: Evidence from the dominantly inherited Alzheimer network. Ann Neurol. 2016;79(6):929–939. doi: 10.1002/ana.24647. 10.1002/ana.24647 PubMed PMID: 27016429, PMCID 4884146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Garnier-Crussard A, Bougacha S, Wirth M, et al. White matter hyperintensities across the adult lifespan: relation to age, Abeta load, and cognition. Alzheimers Res Ther. 2020;12(1):127. doi: 10.1186/s13195-020-00669-4. 10.1186/s13195-020-00669-4 PubMed PMID: 33032654, PMCID 7545576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Birdsill AC, Koscik RL, Jonaitis EM, et al. Regional white matter hyperintensities: aging, Alzheimer's disease risk, and cognitive function. Neurobiol Aging. 2014;35(4):769–776. doi: 10.1016/j.neurobiolaging.2013.10.072. 10.1016/j.neurobiolaging.2013.10.072 PubMed PMID: 24199958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Taylor WD, Steffens DC, MacFall JR, et al. White matter hyperintensity progression and late-life depression outcomes. Arch Gen Psychiatry. 2003;60(11):1090–1096. doi: 10.1001/archpsyc.60.11.1090. 10.1001/archpsyc.60.11.1090 PubMed PMID: 14609884. [DOI] [PubMed] [Google Scholar]
- 36.McNay EC, Pearson-Leary J. GluT4: A central player in hippocampal memory and brain insulin resistance. Exp Neurol. 2020;323:113076. doi: 10.1016/j.expneurol.2019.113076. 10.1016/j.expneurol.2019.113076 PubMed PMID: 31614121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Muhic M, Vardjan N, Chowdhury HH, Zorec R, Kreft M. Insulin and Insulin-like Growth Factor 1 (IGF-1) Modulate Cytoplasmic Glucose and Glycogen Levels but Not Glucose Transport across the Membrane in Astrocytes. J Biol Chem. 2015;290(17):11167–11176. doi: 10.1074/jbc.M114.629063. 10.1074/jbc.M114.629063 PubMed PMID: 25792745, PMCID 4409273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.de la Monte SM. Insulin resistance and Alzheimer's disease. BMB Rep. 2009;42(8):475–481. doi: 10.5483/bmbrep.2009.42.8.475. 10.5483/BMBRep.2009.42.8.475 PubMed PMID: 19712582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Arnold SE, Arvanitakis Z, Macauley-Rambach SL, et al. Brain insulin resistance in type 2 diabetes and Alzheimer disease: concepts and conundrums. Nat Rev Neurol. 2018;14(3):168–181. doi: 10.1038/nrneurol.2017.185. 10.1038/nrneurol.2017.185 PubMed PMID: 29377010, PMCID 6098968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Suzanne M. Insulin resistance and neurodegeneration: progress towards the development of new therapeutics for Alzheimer's disease. Drugs. 2017;77(1):47–65. doi: 10.1007/s40265-016-0674-0. 10.1007/s40265-016-0674-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lochhead JJ, Wolak DJ, Pizzo ME, Thorne RG. Rapid transport within cerebral perivascular spaces underlies widespread tracer distribution in the brain after intranasal administration. J Cereb Blood Flow Metab. 2015;35(3):371–381. doi: 10.1038/jcbfm.2014.215. 10.1038/jcbfm.2014.215 PubMed PMID: 25492117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Born J, Lange T, Kern W, McGregor GP, Bickel U, Fehm HL. Sniffing neuropeptides: a transnasal approach to the human brain. Nat Neurosci. 2002;5(6):514–516. doi: 10.1038/nn849. 10.1038/nn0602-849 PubMed PMID: 11992114. [DOI] [PubMed] [Google Scholar]
- 43.Craft S, Baker LD, Montine TJ, et al. Intranasal insulin therapy for Alzheimer disease and amnestic mild cognitive impairment: a pilot clinical trial. Arch Neurol. 2012;69(1):29–38. doi: 10.1001/archneurol.2011.233. 10.1001/archneurol.2011.233 PubMed PMID: 21911655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.de la Monte, S.M. and P. Grammas, Insulin Resistance and Oligodendrocyte/ Microvascular Endothelial Cell Dysfunction as Mediators of White Matter Degeneration in Alzheimer's Disease, in Alzheimer's Disease, T. Wisniewski, Editor. 2019: Brisbane (AU). [PubMed]
- 45.Ashrafian H, Zadeh EH, Khan RH. Review on Alzheimer's disease: Inhibition of amyloid beta and tau tangle formation. Int J Biol Macromol. 2020;167:382–394. doi: 10.1016/j.ijbiomac.2020.11.192. 10.1016/j.ijbiomac.2020.11.192 PubMed PMID: 33278431. [DOI] [PubMed] [Google Scholar]
- 46.Schmidt P, Gaser C, Arsic M, et al. An automated tool for detection of FLAIR-hyperintense white-matter lesions in Multiple Sclerosis. Neuroimage. 2012;59(4):3774–3783. doi: 10.1016/j.neuroimage.2011.11.032. 10.1016/j.neuroimage.2011.11.032 PubMed PMID: 22119648. [DOI] [PubMed] [Google Scholar]
- 47.Schwarz, C., J. Gunter, C. Ward, et al. The mayo clinic adult lifespan template (MCALT): better quantification across the lifespan. in Alzheimer's Association International Conference.[Google Scholar]. 2017.
- 48.Jack CR, Jr., Wiste HJ, Therneau TM, et al. Associations of Amyloid, Tau, and Neurodegeneration Biomarker Profiles With Rates of Memory Decline Among Individuals Without Dementia. JAMA. 2019;321(23):2316–2325. doi: 10.1001/jama.2019.7437. 10.1001/jama.2019.7437 PubMed PMID: 31211344, PMCID 6582267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Brickman AM, Provenzano FA, Muraskin J, et al. Regional white matter hyperintensity volume, not hippocampal atrophy, predicts incident Alzheimer disease in the community. Arch Neurol. 2012;69(12):1621–1627. doi: 10.1001/archneurol.2012.1527. 10.1001/archneurol.2012.1527 PubMed PMID: 22945686, PMCID 3597387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Tubi MA, Feingold FW, Kothapalli D, et al. White matter hyperintensities and their relationship to cognition: Effects of segmentation algorithm. Neuroimage. 2020;206:116327. doi: 10.1016/j.neuroimage.2019.116327. 10.1016/j.neuroimage.2019.116327 PubMed PMID: 31682983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Gouw AA, Seewann A, van der Flier WM, et al. Heterogeneity of small vessel disease: a systematic review of MRI and histopathology correlations. J Neurol Neurosurg Psychiatry. 2011;82(2):126–135. doi: 10.1136/jnnp.2009.204685. 10.1136/jnnp.2009.204685 PubMed PMID: 20935330. [DOI] [PubMed] [Google Scholar]
- 52.Carmichael O, Schwarz C, Drucker D, et al. Longitudinal changes in white matter disease and cognition in the first year of the Alzheimer disease neuroimaging initiative. Arch Neurol. 2010;67(11):1370–1378. doi: 10.1001/archneurol.2010.284. 10.1001/archneurol.2010.284 PubMed PMID: 21060014, PMCID 3082636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Heo JH, Lee ST, Kon C, Park HJ, Shim JY, Kim M. White matter hyperintensities and cognitive dysfunction in Alzheimer disease. J Geriatr Psychiatry Neurol. 2009;22(3):207–212. doi: 10.1177/0891988709335800. 10.1177/0891988709335800 PubMed PMID: 19433863. [DOI] [PubMed] [Google Scholar]
- 54.Mitchell AJ. CSF phosphorylated tau in the diagnosis and prognosis of mild cognitive impairment and Alzheimer's disease: a meta-analysis of 51 studies. J Neurol Neurosurg Psychiatry. 2009;80(9):966–975. doi: 10.1136/jnnp.2008.167791. 10.1136/jnnp.2008.167791 PubMed PMID: 19465413. [DOI] [PubMed] [Google Scholar]
- 55.Hampel H, Goernitz A, Buerger K. Advances in the development of biomarkers for Alzheimer's disease: from CSF total tau and Abeta(1–42) proteins to phosphorylated tau protein. Brain Res Bull. 2003;61(3):243–253. doi: 10.1016/s0361-9230(03)00087-x. 10.1016/S0361-9230(03)00087-X PubMed PMID: 12909294. [DOI] [PubMed] [Google Scholar]
- 56.Kandel BM, Avants BB, Gee JC, et al. White matter hyperintensities are more highly associated with preclinical Alzheimer's disease than imaging and cognitive markers of neurodegeneration. Alzheimers Dement (Amst) 2016;4:18–27. doi: 10.1016/j.dadm.2016.03.001. 10.1016/j.dadm.2016.03.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Marnane M, Hsiung GY. Could Better Phenotyping Small Vessel Disease Provide New Insights into Alzheimer Disease and Improve Clinical Trial Outcomes? Curr Alzheimer Res. 2016;13(7):750–763. doi: 10.2174/1567205013666160222112634. 10.2174/1567205013666160222112634 PubMed PMID: 26899579. [DOI] [PubMed] [Google Scholar]
- 58.Pietroboni AM, Carandini T, Colombi A, et al. Amyloid PET as a marker of normal-appearing white matter early damage in multiple sclerosis: correlation with CSF beta-amyloid levels and brain volumes. Eur J Nucl Med Mol Imaging. 2019;46(2):280–287. doi: 10.1007/s00259-018-4182-1. 10.1007/s00259-018-4182-1 PubMed PMID: 30343433. [DOI] [PubMed] [Google Scholar]
- 59.Walsh P, Sudre CH, Fiford CM, et al. CSF amyloid is a consistent predictor of white matter hyperintensities across the disease course from aging to Alzheimer's disease. Neurobiol Aging. 2020;91:5–14. doi: 10.1016/j.neurobiolaging.2020.03.008. 10.1016/j.neurobiolaging.2020.03.008 PubMed PMID: 32305782. [DOI] [PubMed] [Google Scholar]
- 60.Tosto G, Zimmerman ME, Hamilton JL, Carmichael OT, Brickman AM, I. Alzheimer's Disease Neuroimaging The effect of white matter hyperintensities on neurodegeneration in mild cognitive impairment. Alzheimers Dement. 2015;11(12):1510–1519. doi: 10.1016/j.jalz.2015.05.014. 10.1016/j.jalz.2015.05.014 PubMed PMID: 26079417, PMCID 4677059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Kester MI, Goos JD, Teunissen CE, et al. Associations between cerebral small-vessel disease and Alzheimer disease pathology as measured by cerebrospinal fluid biomarkers. JAMA Neurol. 2014;71(7):855–862. doi: 10.1001/jamaneurol.2014.754. 10.1001/jamaneurol.2014.754 PubMed PMID: 24818585. [DOI] [PubMed] [Google Scholar]
- 62.Osborn KE, Liu D, Samuels LR, et al. Cerebrospinal fluid beta-amyloid42 and neurofilament light relate to white matter hyperintensities. Neurobiol Aging. 2018;68:18–25. doi: 10.1016/j.neurobiolaging.2018.03.028. 10.1016/j.neurobiolaging.2018.03.028 PubMed PMID: 29702372, PMCID 6085839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Kellar D, Craft S. Brain insulin resistance in Alzheimer's disease and related disorders: mechanisms and therapeutic approaches. Lancet Neurol. 2020;19(9):758–766. doi: 10.1016/S1474-4422(20)30231-3. 10.1016/S1474-4422(20)30231-3 PubMed PMID: 32730766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Parks JK, Smith TS, Trimmer PA, Bennett JP, Jr., Parker WD., Jr. Neurotoxic Abeta peptides increase oxidative stress in vivo through NMDA-receptor and nitric-oxide-synthase mechanisms, and inhibit complex IV activity and induce a mitochondrial permeability transition in vitro. J Neurochem. 2001;76(4):1050–1056. doi: 10.1046/j.1471-4159.2001.00112.x. 10.1046/j.1471-4159.2001.00112.x PubMed PMID: 11181824. [DOI] [PubMed] [Google Scholar]
- 65.Kim HC, Yamada K, Nitta A, et al. Immunocytochemical evidence that amyloid beta (1–42) impairs endogenous antioxidant systems in vivo. Neuroscience. 2003;119(2):399–419. doi: 10.1016/s0306-4522(02)00993-4. 10.1016/S0306-4522(02)00993-4 PubMed PMID: 12770555. [DOI] [PubMed] [Google Scholar]
- 66.Xu J, Chen S, Ahmed SH, et al. Amyloid-beta peptides are cytotoxic to oligodendrocytes. J Neurosci. 2001;21(1):RC118. doi: 10.1523/JNEUROSCI.21-01-j0001.2001. 10.1523/JNEUROSCI.21-01-j0001.2001 PubMed PMID: 11150354, PMCID 6762453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Pak K, Chan SL, Mattson MP. Presenilin-1 mutation sensitizes oligodendrocytes to glutamate and amyloid toxicities, and exacerbates white matter damage and memory impairment in mice. Neuromolecular Med. 2003;3(1):53–64. doi: 10.1385/NMM:3:1:53. 10.1385/NMM:3:1:53 PubMed PMID: 12665676. [DOI] [PubMed] [Google Scholar]
- 68.Verbeek MM, Ruiter DJ, de Waal RM. The role of amyloid in the pathogenesis of Alzheimer's disease. Biol Chem. 1997;378(9):937–950. doi: 10.1515/bchm.1997.378.9.937. PubMed PMID: 9348103. [DOI] [PubMed] [Google Scholar]
- 69.Schultz N, Brannstrom K, Byman E, et al. Amyloid-beta 1–40 is associated with alterations in NG2+ pericyte population ex vivo and in vitro. Aging Cell. 2018;17(3):e12728. doi: 10.1111/acel.12728. 10.1111/acel.12728 PubMed PMID: 29453790, PMCID 5946076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Park L, Hochrainer K, Hattori Y, et al. Tau induces PSD95-neuronal NOS uncoupling and neurovascular dysfunction independent of neurodegeneration. Nat Neurosci. 2020;23(9):1079–1089. doi: 10.1038/s41593-020-0686-7. 10.1038/s41593-020-0686-7 PubMed PMID: 32778793, PMCID 7896353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Frisoni GB, Fox NC, Jack CR, Jr., Scheltens P, Thompson PM. The clinical use of structural MRI in Alzheimer disease. Nat Rev Neurol. 2010;6(2):67–77. doi: 10.1038/nrneurol.2009.215. 10.1038/nrneurol.2009.215 PubMed PMID: 20139996, PMCID 2938772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Wirth M, Bejanin A, La Joie R, et al. Regional patterns of gray matter volume, hypometabolism, and beta-amyloid in groups at risk of Alzheimer's disease. Neurobiol Aging. 2018;63:140–151. doi: 10.1016/j.neurobiolaging.2017.10.023. 10.1016/j.neurobiolaging.2017.10.023 PubMed PMID: 29203090. [DOI] [PubMed] [Google Scholar]
- 73.Smith AD, Smith SM, de Jager CA, et al. Homocysteine-lowering by B vitamins slows the rate of accelerated brain atrophy in mild cognitive impairment: a randomized controlled trial. PLoS One. 2010;5(9):e12244. doi: 10.1371/journal.pone.0012244. 10.1371/journal.pone.0012244 PubMed PMID: 20838622, PMCID 2935890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Turner RS, Thomas RG, Craft S, et al. A randomized, double-blind, placebo-controlled trial of resveratrol for Alzheimer disease. Neurology. 2015;85(16):1383–1391. doi: 10.1212/WNL.0000000000002035. 10.1212/WNL.0000000000002035 PubMed PMID: 26362286, PMCID 4626244. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Table 1. Raw means and confidence intervals for temporal-parietal ROI volume and thickness change split by treatment group.
Supplemental Table 2. Raw means for global and regional white matter hyperintensity volumes at screening and month 12 follow-up for insulin and placebo groups.