Abstract
OBJECTIVE
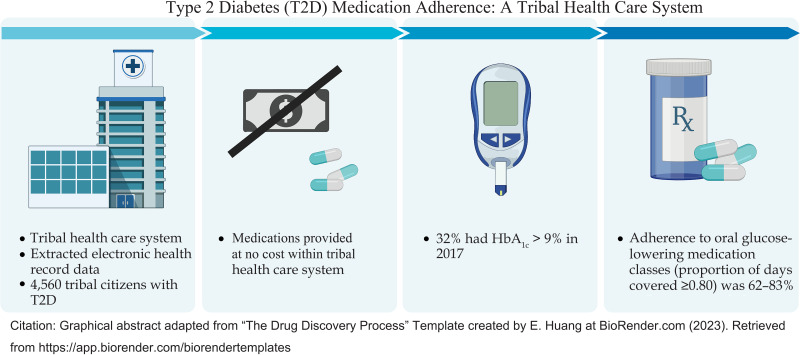
To examine HbA1c levels and adherence to oral glucose-lowering medications and their association with future HbA1c levels among American Indian adults with type 2 diabetes (T2D) receiving medications at no cost from a tribal health care system.
RESEARCH DESIGN AND METHODS
Tribal citizens with T2D who used Choctaw Nation Health Services Authority (CNHSA) and Pharmacies and had HbA1c data during 2017–2018 were included in this study. Medication adherence (proportion of days covered [PDC] ≥0.80) was calculated using 2017 CNHSA electronic health record data.
RESULTS
Of the 74,000 tribal citizens living on tribal lands, 4,560 were eligible; 32% had HbA1c at or below target (≤7%), 36% were above target (>7 to ≤9%), and 32% were uncontrolled (>9%) in 2017. The percentage of patients with PDC ≥0.80 was 66% for those using biguanides, 72% for sulfonylureas, 75% for dipeptidyl peptidase 4 inhibitors, and 83% for sodium–glucose cotransporter 2 inhibitors. The proportion of patients with HbA1c at or below target increased slightly from 32% in 2017 to 42% in 2018. Higher average PDC in 2017 was associated with lower HbA1c levels in 2018 (β = −1.143; P < 0.001).
CONCLUSIONS
Medication adherence was higher than that found in previous studies using self-report methods in American Indian populations, although a smaller proportion of patients had HbA1c at or below target relative to U.S. adults with T2D. Medication adherence was associated with improved HbA1c levels for most oral glucose-lowering medication classes. Future studies of American Indians should use both longitudinal prescription data from both electronic health records and pharmacy refills.
Graphical Abstract
Introduction
Type 2 diabetes (T2D) disproportionately affects American Indian (AI) individuals (1,2); however, little is known about medication adherence or hemoglobin A1c (HbA1c) levels in this population. AI individuals are >2.5 times as likely to have T2D (1,2) and have poorer glycemic control (higher HbA1c values) compared with their White counterparts, putting them at increased risk of developing diabetes-related complications (3,4). Few studies have addressed medication adherence in the AI population; none have used a large sample size to examine medication adherence among those who use the Indian Health Service (IHS) or tribal health care systems and receive medications at no cost (5,6). Here, we examine HbA1c levels, adherence to oral glucose-lowering medications, and glycemic control in AI adults with T2D using tribal health services.
Adherence to glucose-lowering medications can substantially improve HbA1c and decrease mortality (7–9). Although initial approaches to improving HbA1c are frequently nonpharmacological, such as lifestyle changes, these approaches often do not suffice as the disease progresses, and glucose-lowering medications are commonly required long term to improve HbA1c. Cost has been cited as a common cause of medication nonadherence (10–12). Authors of a multiyear investigation of the National Health Interview Survey found that 15% of patients with diabetes reported cost-related nonadherence (12). However, the degree of adherence to glucose-lowering medications is virtually unknown among AI patients who primarily receive care and medications at no cost from IHS/tribal facilities.
We identified only four studies of AI adults with T2D that focused on medication adherence. In one study (N = 166) using a self-reported adherence scale (scores ranged from 0 to 4, with higher scores indicating higher adherence), 72% of participants reported low to moderate medication adherence (score ≤3) (13). Being female was associated with higher levels of diabetes distress and depressive symptoms and lower medication adherence (13). In two separate studies with small samples (N = 40 and N = 16), a majority of participants had extremely low levels of self-reported medication adherence (score ≤1 of 4) (14,15). In a large cohort study within nine U.S. commercial integrated delivery systems (N = 5,831; <2% AI participants), AI patients in non-IHS/tribal health care settings had significantly lower diabetes medication adherence compared with their non-Hispanic White counterparts (16). Although these findings are important, they may not be generalizable to AI patients who use IHS/tribal health care and do not pay for medications.
To improve understanding related to adherence to medications among AI patients with T2D, we extracted electronic health record (EHR) data to examine HbA1c levels, adherence to oral glucose-lowering medications, and their association with future HbA1c levels among AI adults with T2D who receive medication at no cost from a tribal health care system.
Research Design and Methods
Design
We conducted a descriptive association study of EHR data from 2017 and 2018 that included visit-level data for HbA1c levels and dispensed glucose-lowering medications. The University of Florida and Choctaw Nation Institutional Review Boards approved this study.
Choctaw Nation is a federally recognized tribe located in rural southeastern Oklahoma. There are >223,000 tribal citizens throughout the U.S., making Choctaw Nation the third-largest federally recognized AI tribe (17). Choctaw Nation Tribal Health Services Authority (CNHSA) is a tribal health system that partners with IHS to deliver health care services to >74,000 Choctaw citizens and their families who predominately live in southeastern Oklahoma, Arkansas, and Texas (A. Randolph, personal communication, 1 March 2022). IHS is an agency of the Department of Health and Human Services that provides health care services to >2 million AI and Alaska Native patients from 574 federally recognized tribes in 37 states (18). CNHSA provides citizens with a wide range of health care services, including primary care, specialists (e.g., endocrinologists), diagnostic services, mental health services, surgical services, labor and delivery, nutritional services, and diabetes wellness programs.
Sample
Tribal citizens enrolled in any federally recognized tribe were included in the sample if they had a T2D ICD-10 diagnosis code in the EHR, were age ≥18 years, had used CNHSA Health Services and Pharmacies, were dispensed glucose-lowering medications (other than insulin) by CNHSA Pharmacies, and had HbA1c measures recorded during 2017, the year we were provided access to the data via an executed data use agreement. Individuals diagnosed with end-stage renal disease were excluded because of the frequent medication and dosage changes that are often required. Individuals prescribed insulin were also excluded because of the need for frequent dosage adjustments.
Data Extraction
From the Choctaw Nation EHR database, Choctaw Nation program staff members extracted pharmacy prescription refill data for medications, applicable diagnosis codes, demographic data, and laboratory data for 2017 and 2018. Raw deidentified EHR data were securely transferred electronically for storage on a password-protected file server at the University of Florida. Access was given only to authorized members of the research team.
HbA1c Measure
The HbA1c target was defined as ≤7% based on the American Diabetes Association guidelines (19); above target was defined as >7 to ≤9% and uncontrolled as >9%. For our analysis, we used the first HbA1c measure in each study year (2017 and 2018). HbA1c levels labeled as too low (<4.5%) or too high (>14%) to be measured accurately were recorded as values of 4.5 or 14%, respectively. This affected a very small percentage (0.5% in 2017 and 0.4% in 2018) of HbA1c measures.
Medication Adherence Measure
To examine the percentage of medication adherence, we focused on patients with medication refills in 2017 for seven different glucose-lowering medication classes: biguanides, dipeptidyl peptidase 4 (DPP-4) inhibitors, sulfonylureas, α-glucosidase inhibitors, sodium–glucose cotransporter 2 (SGLT2) inhibitors, thiazolidinediones (TZDs), and meglitinides. We estimated medication adherence by calculating a prescription refill-based proportion of days covered (PDC). An acceptable adherence threshold to medication was defined as PDC ≥0.80. The Pharmacy Quality Alliance offers this claims-based adherence measure (20) and recommends that insulin be excluded from medication adherence PDC calculations because insulin requires titration and frequent dosage adjustments, and despite directions to discard insulin vials after 30 days, many patients continue to use the insulin beyond 30 days. We did not have access to complete prescription data, such as when a physician may have discontinued a medication or when medications were not used during hospitalization. Therefore, for the denominator, we used the window from the first dispensing date in 2017 to when the last refill in 2017 was scheduled to run out or the end of 2017, whichever date was earlier. For the numerator, we used the days a medication was supplied to a patient in 2017. We calculated PDC for each medication class separately. For patients who had been dispensed multiple glucose-lowering medications in the same class, a day was considered covered if at least one of the medications was available. Medication adherence was operationalized as a continuous measure of PDC for the year with a range of 0–1.
Statistical Analysis
The data were imported into R (r-project.org) for analysis. Demographic and clinical variables were summarized using descriptive statistics, including mean, SD, percentile, frequency, percentage, and Pearson correlation. Within-subject year-to-year HbA1c comparison was performed using the paired t test. Comparison between patients to whom a medication class was dispensed and those to whom it was not was performed using an independent t test. Regression analysis was used to examine the association between 2017 PDC and 2018 HbA1c of patients, adjusting for their 2017 HbA1c. Statistical significance was set at a two-sided α of 0.05.
Results
Of the 74,000 tribal citizens who use CNHSA health care services, 7,264 patients, representing ∼10% of tribal citizens, had a T2D ICD-10 diagnosis code in 2017. Of these, 87 (1.2%) were excluded for having end-stage renal disease, and 1,199 (16.5%) were excluded because of a lack of HbA1c data in 2017. Of the remaining 5,978 patients, 899 (15.0%) did not have a prescription filled by CNHSA in 2017, and 519 (8.7%) had only insulin in 2017. After applying exclusion criteria, there were 4,560 eligible tribal citizens whose EHR data were available for this study (Supplementary Fig. 1). This sample represents 63% of all the tribal citizens with an EHR record of T2D in 2017. The sample (N = 4,560) lived in 317 communities; all patients had T2D and received health care and pharmacy services at CNHSA. Most patients were tribal citizens; however, immediate non-Native family members (e.g., spouse or children age ≤19 years) of tribal citizens are eligible to use some Choctaw Nation Health Services; therefore, a small portion (n = 15; 0.03%) of the sample is non-Native. The mean age of the cohort was 56.8 ± 13.0 years; 52% of the sample was female; 99.7% was AI (Table 1).
Table 1.
Patient demographic data (N = 4,560)
| Characteristic | n (%) |
|---|---|
| Mean age (SD), years | 56.8 ± 13.0 |
| Sex | |
| Male | 2,184 (47.9) |
| Female | 2,376 (52.1) |
| Race/ethnicity | |
| AI | 4,545 (99.7) |
| Other | 15 (0.3) |
HbA1c Levels
In 2017, patients had a mean HbA1c of 8.0 ± 1.9%, with a median of 7.5% and first and third quartiles of 6.6 and 9.1%, respectively. The percentages with below-target, above-target, and uncontrolled HbA1c measures were 32%, 36%, and 32%, respectively. In 2018, 11% of patients did not have an HbA1c measure. In 2018, mean HbA1c was 7.8 ± 1.8%, and the median and first and third quartiles were 7.4, 6.5, and 8.7%, respectively. The 2018 HbA1c levels were below target, above target, and uncontrolled for 42, 37, and 21%, respectively.
HbA1c measures for 2017 and 2018 were highly correlated (r = 0.60; P < 0.001). The difference between the 2 years was statistically significant (P < 0.001). On average, 2018 HbA1c levels were 0.20 ± 1.63% (95% CI 0.15, 0.25%) lower than 2017 HbA1c levels.
Medication Adherence
Table 2 shows medications dispensed and adherence (PDC) by medication class in 2017. Of the seven glucose-lowering medication classes, biguanides and sulfonylureas were the two most commonly dispensed, at 85.5 and 40.8%, respectively, and had similar PDC adherence levels (mean 0.81 ± 0.17 for biguanides and 0.84 ± 0.16 for sulfonylureas). Patients dispensed SGLT2 inhibitors and meglitinides were very likely to be adherent, with 83 and 81% showing PDC percentage ≥0.8, respectively, whereas only 66 and 72% of biguanide and sulfonylurea users, respectively, were adherent (PDC percentage ≥0.8). Table 2 presents additional details regarding individual medications dispensed and related PDC statistics.
Table 2.
Percentage of patients dispensed each medication class and adherence statistics for PDC with medication dispensed in 2018
| Patients to whom medication dispensed, % | PDC adherence statistics in 2018 | ||||
|---|---|---|---|---|---|
| Mean ± SD | Range | Median (25, 75%) | ≥0.8, % | ||
| Medication class | |||||
| Biguanides | 85.8 | 0.81 ± 0.17 | 0.17–1 | 0.88 (0.73, 0.95) | 66 |
| DPP-4 inhibitors | 14.8 | 0.86 ± 0.15 | 0.20–1 | 0.91 (0.80, 0.97) | 75 |
| Sulfonylureas | 40.8 | 0.84 ± 0.16 | 0.16–1 | 0.90 (0.78, 0.95) | 72 |
| α-Glucosidase inhibitors | 1.6 | 0.82 ± 0.19 | 0.20–1 | 0.87 (0.73, 1) | 62 |
| SGLT2 inhibitors | 4.3 | 0.89 ± 0.13 | 0.33–1 | 0.93 (0.84, 0.98) | 83 |
| TZDs | 13.8 | 0.86 ± 0.16 | 0.20–1 | 0.92 (0.81, 0.97) | 76 |
| Meglitinides | 0.4 | 0.89 ± 0.12 | 0.60–1 | 0.94 (0.84, 0.97) | 81 |
| Medication | |||||
| Metformin | 85.8 | 0.81 ± 0.17 | 0.17–1 | 0.88 (0.73, 0.95) | 66 |
| Saxagliptin | 14.7 | 0.86 ± 0.15 | 0.20–1 | 0.91 (0.80, 0.97) | 75 |
| Glipizide | 26.6 | 0.84 ± 0.16 | 0.16–1 | 0.90 (0.79, 0.96) | 73 |
| Glyburide | 4.0 | 0.85 ± 0.15 | 0.28–1 | 0.90 (0.79, 0.96) | 75 |
| Glimepiride | 10.8 | 0.83 ± 0.16 | 0.27–1 | 0.89 (0.76, 0.95) | 70 |
| Acarbose | 1.6 | 0.82 ± 0.19 | 0.20–1 | 0.87 (0.73, 1) | 62 |
| Canagliflozin | 2.7 | 0.89 ± 0.12 | 0.50–1 | 0.94 (0.83, 0.99) | 81 |
| Empagliflozin | 3.7 | 0.90 ± 0.11 | 0.49–1 | 0.94 (0.87, 0.99) | 85 |
| Pioglitazone | 13.8 | 0.86 ± 0.16 | 0.20–1 | 0.92 (0.81, 0.97) | 76 |
| Repaglinide | 0.4 | 0.89 ± 0.12 | 0.60–1 | 0.94 (0.84, 0.97) | 81 |
HbA1c by Adherence
Table 3 shows findings for patients dispensed a class of glucose-lowering medication and their HbA1c (mean, SD, and percentage meeting the 7% target) in 2017 and 2018. Patients who were dispensed medications in all classes except biguanides, α-glucosidase inhibitors, and meglitinides had higher initial HbA1c in 2017 (P < 0.001 for all) than those to whom the corresponding medications were not dispensed. We also present the mean and 95% CI of year-to-year HbA1c change as well as P values comparing the changes among patients dispensed and not dispensed medications from a class. Being dispensed an SGLT2 inhibitor or TZD class of medication was associated with improvement in HbA1c (P = 0.004 and 0.03, respectively), whereas being dispensed an α-glucosidase inhibitor was associated with worsening of HbA1c (P = 0.01).
Table 3.
Change in HbA1c between first measurement in 2017 and first measurement in 2018 for patients dispensed and not dispensed medication class
| Class | Dispensed | HbA1c | P* | ||
|---|---|---|---|---|---|
| Mean ± SD, %, meeting target | Change (95% CI) | ||||
| 2017 | 2018 | ||||
| Biguanides | No | 8.2 ± 1.9, 34 | 8.0 ± 1.8, 36 | −0.12 (−0.26, 0.01) | 0.22 |
| Yes | 8.0 ± 1.9, 39 | 7.8 ± 1.8, 43 | −0.21 (−0.27, −0.16) | ||
| DPP-4 inhibitors | No | 8.0 ± 1.9, 41 | 7.7 ± 1.8, 45 | −0.21 (−0.26, −0.15) | 0.46 |
| Yes | 8.4 ± 1.7, 24 | 8.2 ± 1.7, 27 | −0.15 (−0.29, −0.02) | ||
| Sulfonylureas | No | 7.8 ± 1.9, 47 | 7.6 ± 1.8, 50 | −0.17 (−0.23, −0.10) | 0.12 |
| Yes | 8.4 ± 1.8, 26 | 8.1 ± 1.7, 31 | −0.25 (−0.33, −0.17) | ||
| α-Glucosidase inhibitors | No | 8.0 ± 1.9, 39 | 7.8 ± 1.8, 42 | −0.21 (−0.26, −0.16) | 0.01 |
| Yes | 8.1 ± 2.0, 36 | 8.3 ± 1.9, 28 | 0.21 (−0.11, 0.54) | ||
| SGLT2 | No | 8.0 ± 1.9, 40 | 7.8 ± 1.8, 43 | −0.18 (−0.23, −0.13) | 0.004 |
| Yes | 9.1 ± 1.8, 9 | 8.6 ± 1.7, 17 | −0.56 (−0.81, −0.31) | ||
| TZDs | No | 7.9 ± 1.9, 41 | 7.7 ± 1.7, 44 | −0.17 (−0.23, −0.12) | 0.03 |
| Yes | 8.7 ± 2.0, 22 | 8.4 ± 1.9, 27 | −0.36 (−0.53, −0.20) | ||
| Meglitinides | No | 8.0 ± 1.9, 39 | 7.8 ± 1.8, 42 | −0.20 (−0.25, −0.15) | 0.91 |
| Yes | 8.3 ± 1.6, 12 | 8.2 ± 1.7, 25 | −0.17 (−0.63, 0.28) | ||
P values obtained using t tests comparing the year-to-year change of HbA1c of patients dispensed and those not dispensed a class of medication.
Multiple linear regression was used to examine the association between the 2017 PDC adherence and 2018 HbA1c levels, adjusting for the 2017 HbA1c levels. We examined both the PDC adherence average across classes and class-specific PDC adherence (Table 4). The higher average PDC in 2017 was associated with lower HbA1c levels in 2018 (β = −1.143; P < 0.001). For most classes (except α-glucosidase inhibitors and meglitinides), adherence was associated with improved 2018 HbA1c levels.
Table 4.
Associations between 2017 adherence and 2018 HbA1c levels, adjusting for 2017 HbA1c levels
| PDC | Estimate | SE | t | P |
|---|---|---|---|---|
| Average across classes | −1.143 | 0.144 | −7.947 | <0.001 |
| Biguanides | −1.071 | 0.141 | −7.604 | <0.001 |
| DPP-4 inhibitors | −1.328 | 0.388 | −3.419 | 0.001 |
| Sulfonylureas | −1.277 | 0.230 | −5.558 | <0.001 |
| α-Glucosidase inhibitors | 0.545 | 0.830 | 0.656 | 0.51 |
| SGLT2 inhibitors | −3.166 | 0.802 | −3.947 | <0.001 |
| TZDs | −1.434 | 0.472 | −3.036 | 0.003 |
| Meglitinides | −1.918 | 1.955 | −0.981 | 0.34 |
Conclusions
To our knowledge, we are the first to use tribal EHR data to examine HbA1c levels and medication adherence to glucose-lowering medications in AI adults with T2D. Using EHR dispensing data for the 4,560 AI patients with T2D who received Choctaw Nation of Oklahoma (CNO) tribal health care, we found higher adherence to oral glucose-lowering medications than seen in previous studies with self-report measures in the AI population (13–16). Although glycemic control improved from 2017 to 2018, it was lower than glycemic control typically reported in individuals with T2D, despite higher rates of medication adherence (21). We found an association between medication adherence (PDC) and improved glycemic control, which is consistent with prior research (22). Regarding classes of glycemic control medications, we also identified two classes (SGLT2 inhibitors and TZDs), the dispensing of which was associated with lower future HbA1c, and one (α-glucosidase inhibitor) associated with higher future HbA1c. Finally, average adherence to glycemic control medications in 2017 was associated with improved 2018 HbA1c levels for most medication classes, except α-glucosidase inhibitors and meglitinides. This may be due to the smaller sample sizes of these two classes (1.6 and 0.4% of total glucose-lowering medications dispensed, respectively). If not a result of small sample size, this effect reinforces current diabetes management guidelines (also relevant for the time frame being studied) in which these medication classes are not preferred as first-line options because of more efficacious available options.
Medication Adherence
Our findings, using PDC, noted higher medication adherence than that reported in prior studies of AI individuals, which revealed low to moderate medication adherence using the patient self-reported four-item Morisky Medication Adherence self-report scale (13–15). Findings from studies with prescription claims–based methods for measuring adherence can lead to different results compared with those using patient self-report measures (23). Self-reported adherence measures are prone to bias (24) but are widely adopted, likely because of ease of use (25). PDC has been recognized by the Pharmacy Quality Alliance as the preferred claims-based adherence measure (20). However, there is no gold-standard measure, and using more than one adherence measure is often recommended (26). Although there is not an established gold standard, there is a need for further research using adherence measures to improve our understanding of adherence to glucose-lowering medications in AI populations. It is also important to point out we did not have access to the duration of T2D diagnosis. We know that variations in the duration of T2D may negatively affect medication adherence as well as the responsiveness to oral glucose-lowering treatment. However, we did control for 2017 HbA1c as a proxy for disease severity.
Adherence to medication in our study was also higher than that previously reported in other studies using the PDC threshold of ≥80%. Most studies using a threshold of 80% reported between 40 and 56% of patients as adherent (27–29). A distinguishing feature in our study was that cost was removed as a potential barrier to medication adherence, which may explain the elevated rates of medication adherence. To our knowledge, no previous studies have examined medication adherence rates in AI populations living on tribal lands and receiving medications at no cost.
Medications with the lowest percentage of patients meeting the medication adherence target (PDC >80%) were metformin (66%) and acarbose (62%); however, metformin was more commonly dispensed (85.8%) compared with acarbose (1.6%). A plausible explanation for reduced adherence for both medications may include potential adverse effects, such as gastrointestinal symptoms (30). Both medications may also be less convenient for patients than many other oral glucose medication classes because they are required to be taken with food and are typically prescribed to be taken more than once daily (31).
Although the 1-year PDC data may not be representative of longitudinal trends, if adherence is high, it may reflect the CNHSA removal of an important barrier (i.e., cost), because CNHSA patients do not have a copay for medications. Our study, however, did not include complete prescription data, such as when a physician may have discontinued a medication, or medication dispensing data during hospitalization, which is important for accurate adherence data. Future studies should focus on examining prescription and pharmacy refill data longitudinally.
HbA1c Levels
Despite high adherence rates, the patients’ mean HbA1c level for our study was 8%, which is above the recommended target of ≤7% (19). Thirty-two percent of patients met the recommended HbA1c target in 2017 compared with 50% of adults with diabetes in the U.S., as published in the National Diabetes Statistics Report 2020 (1). It has been noted, however, that the accepted adherence threshold (PDC >80%) may be insufficient for predicting HbA1c ≤7% (32). In a recently published study, authors proposed that a threshold of >90% may be better for predicting glycemic control (HbA1c ≤7%) (32).
Another reason for suboptimal HbA1c levels in the presence of good medication adherence rates may be therapeutic inertia (i.e., the failure to initiate or intensify glucose-lowering therapy in a timely manner) (33). Delays in oral glucose-lowering treatment intensification >4 months from elevated glycemic targets have been reported to range from 28 to 73% and can lead to elevated HbA1c levels (34). In this study, we know only that patients receiving a glucose-lowering medication but do not know the dose or interval. Future studies should examine prescription data to better understand if therapeutic inertia is a factor in elevated HbA1c levels.
Strengths and Limitations
This is an innovative study with a large sample size that examines medication adherence and HbA1c levels in a population using tribal health care services and receiving medications at no cost to them. We also used a claims-based, validated, quasi-objective method to calculate medication adherence.
This study is not without limitations. Pharmacy refill data were used to calculate medication adherence (PDC), but we did not have access to EHR data describing when a medication may have been discontinued, paused, or switched to another agent, all of which would have improved the accuracy of the measure of medication adherence. Additionally, we did not have data on hospital medication dispensing or on whether patients were actually taking their medications, only that the medications were dispensed. It should also be pointed out that although citizens mainly fill their prescriptions within CNHSA, there are occasions when it is necessary to fill prescriptions outside CNHSA. For example, the provider may order a medication that is not available from the CNHSA pharmacy or the patient may have traveled outside the CNHSA service area. The study was limited to 1 year of pharmacy refill data (2017); however, we plan to conduct a multiyear longitudinal analysis that will more accurately represent medication adherence and HbA1c indicator levels in the CNO population. It will also help confirm, clarify, and enhance the findings of this study. Insulin was not included in the analysis, potentially excluding patients with more advanced T2D. Currently, there is no reliable standardized method for assessing adherence to insulin using prescription EHR data (35). Additionally, patients who were taking multiple glucose-lowering medications in the same class only needed to be covered by one medication each day in the treatment period to be considered adherent. Taking multiple glucose-lowering medications may be a factor related to adherence and should be explored further in future studies. Finally, we could not assess adherence among the 27% of tribal citizens with an EHR diagnostic code of T2D who were excluded. Research is particularly needed to understand the context of T2D management for the 16.5% excluded because of the lack of an HbA1c value in 2017, which limits our ability to generalize findings to the entire population of those with T2D.
In conclusion, this study provides insight into medication adherence and HbA1c levels among patients with T2D using CNO health care services at no cost. Medication adherence findings from this EHR-based study are higher than those from several previous studies in the AI population that used self-report methods. There was an association between medication adherence in 2017 with improved 2018 HbA1c levels for all classes of oral glucose-lowering medications except α-glucosidase inhibitors and meglitinides. Although the proportions of patients with an HbA1c at or below target increased slightly from 32% in 2017 to 42% in 2018, these proportions were smaller compared with the 50% in 2020 for U.S. adults with diabetes (1). Future studies should include a multiyear longitudinal analysis that uses both prescription data from the EHR and pharmacy refill data to calculate medication adherence. Future studies should also further examine barriers and facilitators that affect medication adherence from the patient’s perspective in AI individuals residing on or near tribal lands and receiving IHS or tribal health services.
Article Information
Acknowledgments. The authors thank the CNO for their collaboration and support in this study. The authors also appreciate the support of Thomas M. Danielson and Jordan Everett of the Choctaw Nation’s Information Management Services for their assistance with data retrieval.
Funding. This research was supported by grants 1R01NR020386-01 and U54CA233444 from the National Institute of Nursing Research (NINR) and National Cancer Institute (NCI), National Institutes of Health, respectively. S.M.M. was supported by grant 1P30DK092923 from the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK).
The contents are solely the responsibility of the authors and do not necessarily represent the official views of the NINR, NCI, or NIDDK.
Duality of Interest. No potential conflicts of interest relevant to this article were reported.
Author Contributions. L.S. and T.N.N. led the writing of the manuscript. L.S., Y.Y., and D.J.W. designed the study. Y.Y. conducted the statistical analysis and created the tables. L.S., Y.Y., A.D.-C., A.B.L., W.T.D., R.S., and D.J.W. contributed to the interpretation of results. Y.Y., A.D.-C., A.B.L., R.T.G., S.M.M., and D.J.W. reviewed and edited the manuscript. All authors critically revised the manuscript for intellectual content and approved the final manuscript. L.S. and Y.Y. are the guarantors of this work and, as such, had full access to all the data in this study and take responsibility for the integrity of the data and accuracy of the data analysis.
Prior Presentation. Parts of this study were presented in a poster presentation at the 82nd Annual American Diabetes Association Conference, New Orleans, LA, 3–7 June 2022.
Footnotes
This article contains supplementary material online at https://doi.org/10.2337/figshare.22358056.
References
- 1. Centers for Disease Control and Prevention . National Diabetes Statistics Report 2020. Accessed 6 April 2023. Available from https://www.cdc.gov/diabetes/pdfs/data/statistics/national-diabetes-statistics-report.pdf
- 2. Centers for Disease Control and Prevention . Summary Health Statistics: National Health Interview Survey 2018—Table A-4a. Accessed 6 April 2023. Available from https://www.cdc.gov/nchs/nhis/shs/tables.htm
- 3. Quandt SA, Bell RA, Snively BM, et al. Ethnic disparities in glycemic control among rural older adults with type 2 diabetes. Ethn Dis 2005;15:656–663 [PMC free article] [PubMed] [Google Scholar]
- 4. Hall ME, do Carmo JM, da Silva AA, Juncos LA, Wang Z, Hall JE. Obesity, hypertension, and chronic kidney disease. Int J Nephrol Renovasc Dis 2014;7:75–88 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Schroeder EB, Moore KR, Manson SM, et al. A randomized clinical trial of an interactive voice response and text message intervention for individuals with hypertension. J Clin Hypertens (Greenwich) 2020;22:1228–1238 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Fort MP, Steiner JF, Santos C, et al. Opportunities, challenges, and strategies for engaging family in diabetes and hypertension management: a qualitative study. J Health Care Poor Underserved 2020;31:827–844 [DOI] [PubMed] [Google Scholar]
- 7. Kim YY, Lee JS, Kang HJ, Park SM. Effect of medication adherence on long-term all-cause-mortality and hospitalization for cardiovascular disease in 65,067 newly diagnosed type 2 diabetes patients. Sci Rep 2018;8:12190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Farmer AJ, Rodgers LR, Lonergan M, et al. Adherence to oral glucose-lowering therapies and associations with 1-year HbA1c: a retrospective cohort analysis in a large primary care database. Diabetes Care 2016;39:258–263 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Lawrence DB, Ragucci KR, Long LB, Parris BS, Helfer LA. Relationship of oral antihyperglycemic (sulfonylurea or metformin) medication adherence and hemoglobin A1c goal attainment for HMO patients enrolled in a diabetes disease management program. J Manag Care Pharm 2006;12:466–471 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. McHorney CA, Spain CV. Frequency of and reasons for medication non-fulfillment and non-persistence among American adults with chronic disease in 2008. Health Expect 2011;14:307–320 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Cohen RA, Cha AE. Strategies used by adults with diagnosed diabetes to reduce their prescription drug costs, 2017-2018. NCHS Data Brief 2019;(349):1–8 [PubMed] [Google Scholar]
- 12. Van Alsten SC, Harris JK. Cost-related nonadherence and mortality in patients with chronic disease: a multiyear investigation, National Health Interview Survey, 2000-2014. Prev Chronic Dis 2020;17:E151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Aronson BD, Sittner KJ, Walls ML. The mediating role of diabetes distress and depressive symptoms in type 2 diabetes medication adherence gender differences. Health Educ Behav 2020;47:474–482 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Jacobs A, Kemppainen JK, Taylor JS, Hadsell C. Beliefs about diabetes and medication adherence among Lumbee Indians living in rural southeastern North Carolina. J Transcult Nurs 2014;25:167–175 [DOI] [PubMed] [Google Scholar]
- 15. Shiyanbola OO, Nelson J. Illness perceptions, beliefs in medicine and medication non-adherence among South Dakota minority women with diabetes: a pilot study. S D Med 2011;64:365–368 [PubMed] [Google Scholar]
- 16. Schmittdiel JA, Steiner JF, Adams AS, et al. Diabetes care and outcomes for American Indians and Alaska Natives in commercial integrated delivery systems: a SUrveillance, PREvention, and ManagEment of Diabetes Mellitus (SUPREME-DM) study. BMJ Open Diabetes Res Care 2014;2:e000043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. National Congress of American Indians . The Choctaw Nation in Oklahoma 2017. Accessed 6 April 2023. Available from https://www.ncai.org/tribal-vawa/sdvcj-today/the-choctaw-nation-in-oklahoma
- 18. Indian Health Service . The Federal Health Program for American Indians and Alaska Natives. Accessed 6 April 2023. Available from https://www.ihs.gov/
- 19. American Diabetes Association . 6. Glycemic targets: Standards of Medical Care in Diabetes—2021. Diabetes Care 2021;44(Suppl. 1):S73–S84 [DOI] [PubMed] [Google Scholar]
- 20. Pharmacy Quality Alliance . PQA Measures Overview. Accessed 6 April 2023. Available from https://www.pqaalliance.org/pqa-measures
- 21. Krass I, Schieback P, Dhippayom T. Adherence to diabetes medication: a systematic review. Diabet Med 2015;32:725–737 [DOI] [PubMed] [Google Scholar]
- 22. Zhu VJ, Tu W, Rosenman MB, Overhage JM. A comparison of data driven-based measures of adherence to oral hypoglycemic agents in Medicaid patients. AMIA Annu Symp Proc 2014;2014:1294–1301 [PMC free article] [PubMed] [Google Scholar]
- 23. Stephenson JJ, Shinde MU, Kwong WJ, Fu AC, Tan H, Weintraub WS. Comparison of claims vs patient-reported adherence measures and associated outcomes among patients with nonvalvular atrial fibrillation using oral anticoagulant therapy. Patient Prefer Adherence 2018;12:105–117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Stirratt MJ, Dunbar-Jacob J, Crane HM, et al. Self-report measures of medication adherence behavior: recommendations on optimal use. Transl Behav Med 2015;5:470–482 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Pednekar PP, Ágh T, Malmenäs M, et al. Methods for measuring multiple medication adherence: a systematic review—report of the ISPOR Medication Adherence and Persistence Special Interest Group. Value Health 2019;22:139–156 [DOI] [PubMed] [Google Scholar]
- 26. Lam WY, Fresco P. Medication adherence measures: an overview. BioMed Res Int 2015;2015:217047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Huber CA, Rapold R, Brüngger B, Reich O, Rosemann T. One-year adherence to oral antihyperglycemic medication and risk prediction of patient outcomes for adults with diabetes mellitus: an observational study. Medicine (Baltimore) 2016;95:e3994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Horii T, Momo K, Yasu T, Kabeya Y, Atsuda K. Determination of factors affecting medication adherence in type 2 diabetes mellitus patients using a nationwide claim-based database in Japan. PLoS One 2019;14:e0223431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Oung AB, Kosirog E, Chavez B, Brunner J, Saseen JJ. Evaluation of medication adherence in chronic disease at a federally qualified health center. Ther Adv Chronic Dis 2017;8:113–120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Mertes G. Efficacy and safety of acarbose in the treatment of type 2 diabetes: data from a 2-year surveillance study. Diabetes Res Clin Pract 1998;40:63–70 [DOI] [PubMed] [Google Scholar]
- 31. Bonnet F, Scheen A. Understanding and overcoming metformin gastrointestinal intolerance. Diabetes Obes Metab 2017;19:473–481 [DOI] [PubMed] [Google Scholar]
- 32. Lim MT, Ab Rahman N, Teh XR, et al. Optimal cut-off points for adherence measure among patients with type 2 diabetes in primary care clinics: a retrospective analysis. Ther Adv Chronic Dis 2021;12:2040622321990264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Khunti K, Davies MJ. Clinical inertia—Time to reappraise the terminology? Prim Care Diabetes 2017;11:105–106 [DOI] [PubMed] [Google Scholar]
- 34. Ruiz-Negrón N, Wander C, McAdam-Marx C, Pesa J, Bailey RA, Bellows BK. Factors associated with diabetes-related clinical inertia in a managed care population and its effect on hemoglobin A1c goal attainment: a claims-based analysis. J Manag Care Spec Pharm 2019;25:304–313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Stolpe S, Kroes MA, Webb N, Wisniewski T. A systematic review of insulin adherence measures in patients with diabetes. J Manag Care Spec Pharm 2016;22:1224–1246 [DOI] [PMC free article] [PubMed] [Google Scholar]