Abstract
Natural environments have been linked to decreased risk of cardiovascular disease (CVD) and respiratory disease (RSD) mortality. However, few cohort studies have looked at associations of natural environments with CVD or RSD hospitalization. The aim of this study was to evaluate these associations in a cohort of U.S. Medicare beneficiaries (~63 million individuals). Our open cohort included all fee-for-service Medicare beneficiaries (2000–2016), aged ≥65, living in the contiguous U.S. We assessed zip code-level park cover based on the United States Geological Survey Protected Areas Database, average greenness (Normalized Difference Vegetation Index, NDVI), and percent blue space cover based on Landsat satellite images. Cox-equivalent Poisson models were used to estimate associations of the exposures with first CVD and RSD hospitalization in the full cohort and among those living in urban zip codes (≥1000 persons/mile2). NDVI was weakly negatively correlated with percent park cover (Spearman ρ = − 0.23) and not correlated with percent blue space (Spearman ρ = 0.00). After adjustment for potential confounders, percent park cover was not associated with CVD or RSD hospitalization in the full or urban population. An IQR (0.27) increase in NDVI was negatively associated with CVD (HR: 0.97, 95%CI: 0.96, 0.97), but not with RSD hospitalization (HR: 0.99, 95%CI: 0.98, 1.00). In urban zip codes, an IQR increase in NDVI was positively associated with RSD hospitalization (HR: 1.02, 95%CI: 1.00, 1.03). In stratified analyses, percent park cover was negatively associated with CVD and RSD hospitalization for Medicaid eligible individuals and individuals living in low socioeconomic status neighborhoods in the urban population. We observed no associations of percent blue space cover with CVD or RSD hospitalization. This study suggests that natural environments may benefit cardiorespiratory health; however, benefits may be limited to certain contexts and certain health outcomes.
Keywords: Built environment, Cardiorespiratory health, Nature
1. Introduction
Numerous studies have reported potential beneficial health effects of exposure to natural environments (Fong et al., 2018; Twohig-Bennett and Jones, 2018). Several potential pathways underlying associations of natural environments to health have been suggested. Natural environments may reduce exposure to harmful environmental exposures (e.g., air pollution, noise), can be a resource for stress reduction and attention restoration, and can encourage physical activity and social interactions (Fong et al., 2018; Markevych et al., 2017). On the other hand, vegetation may adversely affect health by releasing pollen and volatile organic compounds (VOCs) (Fan et al., 2020; Markevych et al., 2017).
Many measures of the natural environment have been used in epidemiologic studies. Most studies focus on availability of greenness, measured by satellite-based vegetation indices such as the Normalized Difference Vegetation Index (NDVI) (Labib et al., 2020). These vegetation indices assess the quantity of green vegetation but do not differentiate vegetation quality or green space type. Parks, agricultural lands, uncultivated lands, and private yards are generally captured by vegetation indices but may differ in their impact on health. Parks, for example, provide suitable spaces for physical activities and social gatherings and are publicly accessible, in contrast to agricultural or private lands. Exposure to blue space (e.g. rivers, lakes, oceans) has received less attention in comparison to green space but can be potentially helpful to de-stress, calm and relax (McDougall et al., 2020; White et al., 2020).
Exposure to green space has been linked to decreased risk of cardiovascular disease (CVD) and respiratory disease (RSD) mortality in several large cohort studies (Bauwelinck et al., 2021; Bereziartua et al., 2022; Crouse et al., 2017; Klompmaker et al., 2021; Vienneau et al., 2017). Only a few cohort studies evaluated associations between greenness and CVD incidence (Chen et al., 2020; Dalton and Jones, 2020; Ponjoan et al., 2022; Seo et al., 2019). Chen et al. (2020), Dalton and Jones (2020), Ponjoan et al. (2022) and Seo et al. (2019) observed negative associations between greenness and CVD incidence. To the best of our knowledge, there are no cohort studies that have evaluated associations of green space with RSD incidence in adults. Some cross-sectional studies reported a beneficial association between residential greenness and RSD, such as asthma or COPD, in adults (Alcock et al., 2017; Maas et al., 2009; Sarkar et al., 2019; Xiao et al., 2022). However, a study from China observed positive associations between neighborhood greenness and COPD prevalence (Fan et al., 2020). Evidence of associations between blue space exposure and CVD outcomes and all-cause mortality is not consistent (Georgiou et al., 2021). A study in Spain observed an increased risk between exposure to blue space and all-cause mortality (Nieuwenhuijsen et al., 2018), whereas a study in Canada observed decreased risks between exposure to blue space and all-cause, CVD and RSD mortality (Crouse et al., 2018).
Our aim was to evaluate associations of features of natural environments with first CVD and RSD hospitalization in a cohort of all fee-for-service Medicare beneficiaries living in the contiguous U.S. from 2000 through 2016 (~63 million individuals). We assessed percent park cover, greenness and percent blue space cover for each zip code in the contiguous U.S. As reviews reported stronger effects of natural environments in urban areas and among low socioeconomic status (SES) individuals (Browning et al., 2022; Fong et al., 2018; Rigolon et al., 2021), we also evaluated associations in beneficiaries living in urban zip codes (≥1000 persons/mile2) and in different neighborhood SES (nSES) zip codes.
2. Methods
2.1. Study population
To create an open cohort, data were derived from the Medicare denominator and Medicare Provider Analysis and Review (MEDPAR) files. Medicare is a national health insurance program that provides health insurance for Americans aged 65 and older and for younger people with disability status. Our cohort included all fee-for-service Medicare beneficiaries, aged ≥65 years, living in the contiguous U.S. from January 1, 2000–December 31, 2016. For each beneficiary, follow-up started on January 1st, 2000 or January 1st of the year following entry into the cohort. Moving during follow-up was included in the analyses on an annual time scale. Each beneficiary was followed until the first hospital admission for the outcome of interest, censoring, end of the follow-up, or death.
2.2. Outcome definition
Hospital admissions for all Medicare fee-for-service beneficiaries from 2000 through 2016 were available in MEDPAR. From 2000 through the third quarter of 2015, the International Classification of Disease, Ninth Edition (ICD-9) codes were used. From the fourth quarter of 2015, ICD-10 (from the Tenth Edition) codes were used. We looked at first hospital admission with a primary discharge diagnosis of CVD (ICD-9: 390–459, ICD-10: I00–I99) or RSD (ICD-9: 460–519, ICD-10: J00-J99). Separate cohorts for CVD and RSD hospitalizations were created.
2.3. Exposure assessment
We assessed percent park cover, greenness and percent blue space cover for each zip code in the contiguous U.S. Exposures were assessed on zip code level because we only had information about the residential zip code of each beneficiary. The median area of all zip codes included in our cohort (in 2016) was 92.8 km2 and in urban zip codes it was 17.5 km2 (Table S1).
2.3.1. Park cover
We created a park cover dataset based on the United States Geological Survey Protected Areas Database of the U.S. (PAD-US). The PAD-US strives to be a complete inventory of public land and other protected areas in the US by compiling the “best available” data provided by land managing agencies and organizations. (U.S. Geological Survey (USGS) and Gap Analysis U.S. Geological Survey, Gap Analysis Project, 2020) As PAD-US differentiates between multiple types of public lands, we selected all land types that are likely to be known and used by the general public for outdoor recreation from PAD-US V2.1 (2020) to create a cross-sectional park cover dataset. This included only open and restricted access areas to provide an accessible and recreational version of the PAD-US (“PAD-US-AR”). To assess zip code-level park cover, we converted the park dataset to a raster image and calculated percent park cover for each zip code.
The following designations were included in the park cover dataset:
Parks and open spaces open for public access or restricted access (i.e., seasonally open, fees required, or permits required) including but not limited to lands managed by the National Park Service, U.S. Forest Service, Bureau of Land Management, U.S. Fish & Wildlife, Army Corps of Engineers, State Parks, State Departments of Conservation, State Departments of Natural Resources, State Departments of Land, State Fish and Wildlife Departments, State Forest Service, State Park and Recreation Departments, Tennessee Valley Authority, and city and county park and recreation departments.
Conservation easements
The following designations were excluded from the park cover dataset:
Department of Energy, Department of Defense, and Bureau of Reclamation lands
Marine areas managed as/by Marine Protected Areas, National Oceanic and Atmospheric Administration, Bureau of Ocean Energy Management, etc.
Proclamation areas, which are boundaries of national lands used for administrative purposes that overlap with large areas of public lands that are not all available to the public
Fish hatcheries and other lands used for water rights with regulated hunting
National Park easements (i.e., lands paralleling but not including the Appalachian Trail and not used by the public)
Joint management areas (i.e., university research stations)
Non-governmental organization lands (aside from conservation easements)
State trust/land survey lands
American Indian Lands
Other areas with unknown access or closed public access (i.e., limited to coordinated programs and research)
2.3.2. Greenness
The Normalized Difference Vegetation Index (NDVI), an indicator of greenness, was estimated using satellite imagery. The NDVI is calculated as the ratio between the red and near infrared values (NASA). NDVI ranges from − 1 to 1 and values close to 1 correspond to areas with complete coverage by live vegetation, values close to zero correspond to areas without live vegetation and negative values correspond to water. To assess greenness, we used images from Landsat 7 and Landsat 8 (Collection 1 Tier 1 DN values, representing scaled, calibrated at sensor radiance) for the contiguous U.S. from June 1, up to August 31 (summer), for each year (2000–2016). Landsat 7 and Landsat 8 images are generated every 16 days at 30 m resolution. Using Google Earth Engine (Gorelick et al., 2017), we made cloud-free NDVI composite maps (based on Landsat 7 and Landsat 8 images) for the contiguous U.S. After setting negative NDVI values to zero, we calculated the spatially-weighted mean summer NDVI for each zip code in the U.S. for each year.
2.3.3. Blue space cover
We estimated blue space using satellite imagery based on the Joint Research Centre’s Global Surface Water Dataset (Pekel et al., 2016). This dataset contains information about the location of surface water, based on Landsat 5, 7, and 8 images from 1984 to 2018 (30 m spatial resolution). Information was aggregated over the entire time period and not available for each year. To classify each pixel into water or non-water, we used the “Occurrence” band. This band indicates the frequency with which water was present in each pixel during the time period. We used a 50% threshold (water was present 50% or more of the time) to classify pixels into blue space and no blue space. As zip codes are used for postal services, adjacent water bodies such as rivers, lakes and oceans are not always included in zip code areas. Therefore, we calculated spatially weighted blue space cover of zip codes with a 1000 m buffer around each zip code.
2.4. Covariates
For each beneficiary, information about year of entry, age at year of Medicare entry, sex, race, Medicaid eligibility (a proxy for low socioeconomic status), and zip code of residence for all Medicare beneficiaries were derived from the Medicare beneficiary file. As a proxy for nSES, we used eight zip code-level covariates from the U.S. Census and American Community Survey (median home value, median household income, population density, percent Hispanic, percent Black, percent of the population with less than a high school degree, percent below the poverty level, and percent of owner-occupied housing units). We linked percent of the population that were ever smokers (based on the county level), derived from the nationwide Behavioural Risk Factor Surveillance System (BRFSS). BRFSS is the nation’s premier system of surveys that collect information about health-related risk behaviours of U.S. residents. The average population size of all counties in the contiguous U.S. in 2010 was 98,670 (min: 82, max: 9,818,605) (United States Census Bureau, 2022). U.S. census (2000, 2009–2016) and BRFSS (2000–2011) variables were available for some years but not all. Temporal interpolation using a moving average algorithm within each zip code was performed for missing years, as described previously (Di et al., 2017). Further, U.S. census regions (West, Midwest, Northeast, and South) were linked to account for regional differences.
We also assessed zip code-level air pollution (particulate matter less than 2.5 μm (PM2.5) and nitrogen dioxide (NO2)), and meteorological indicators (maximum daily temperature, specific humidity, and precipitation). Briefly, annual PM2.5 and NO2 concentrations across the contiguous U.S. for 2000–2016 were estimated based on predictions from well-validated spatio-temporal ensemble models (Di et al., 2019b, 2019a; Requia et al., 2020). Detailed information about air pollution models can be found elsewhere (Di et al., 2019b, 2019a; Requia et al., 2020). For each zip code, the annual average concentrations were estimated by averaging the estimations at grid cells whose centroids fall within the boundary of that ZIP code. Average summer maximum temperature, ambient specific humidity and total precipitation were estimated for each year for each zip code using daily data from the Gridded Surface Meteorological dataset (Abatzoglou, 2013).
2.5. Statistical analyses
We applied a Cox-equivalent re-parameterized Poisson model to overcome computational challenges due to our large cohort. We aggregated all beneficiaries within the same zip code in a specific year, with the same age (2-year categories), sex, race, Medicaid eligibility and year of follow-up and treated them as one single grid cell. We fitted a stratified quasi-Poisson model to estimate associations with the rate of first CVD and RSD hospitalizations. The count of CVD and RSD related first hospitalizations in each grid cell was the dependent variable, using the corresponding total person-time in each grid cell as the offset. To account for within zip code correlated observations across years, an m-out-n bootstrap method using zip code units was used to calculate statistically robust confidence intervals (CIs). All hazard ratios (HRs) were expressed per IQR increase (based on the full CVD cohort). The Cox-equivalent re-parameterized Poisson approach is described in more detail elsewhere (Shi et al., 2020).
To evaluate the impact of potential confounders, we fitted models with increasing degrees of covariate adjustment. Model 1 included percent park cover, NDVI, percent blue space cover, calendar year, region, an offset for total person-time, and strata for all possible combinations of sex, race, Medicaid eligibility, age at study entry (2-year categories) and follow-up year. In Model 2, all U.S. census covariates (except population density) were added. In Model 3, population density was added, in Model 4 percent ever smoked was added, and in Model 5 average summer temperature, specific humidity and total precipitation were added. A directed acyclic graph (DAG) outlining the conceptual relations between all variables is shown in Fig. S1. We evaluated the shape of the exposure-response curves for each exposure with natural splines. We a priori specified 2 or 3 degrees of freedom to visually evaluate deviations from linearity.
In addition, we estimated associations of park cover, greenness and blue space cover for individuals living in urban zip codes (population density ≥1000 persons/mile2). To evaluate whether associations were modified by individual demographics, region, nSES and air pollution, we stratified our analyses by sex (male, female), age (<75 years, 75–84 years, ≥85 years), race (White, Black, other/unknown), Medicaid eligibility (eligible, not eligible), region (West, Midwest, Northeast, South) and tertiles of zip code-level percent below the poverty level, median home value, median household income, PM2.5 and NO2. For sensitivity analyses, we excluded beneficiaries who had their first CVD or RSD hospital admission within the first year of their follow-up and all records in the year 2000, to exclude potential prevalent CVD or RSD cases. We ran single-exposure models and additionally adjusted for zip code level NO2 and PM2.5. We also examined percent blue space cover without a 1000 m buffer. In addition, we stratified our analyses by deciles of zip code-level area.
R software (R Project for Statistical Computing) version 3.6.1 were used for our analyses. The analyses were conducted on the Harvard Research Computing Environment, which is supported by the Institute for Quantitative Social Science at Harvard University.
2.6. Informed consent
This study was approved by the institutional review board at the Harvard T H Chan School of Public Health and was exempt from informed consent requirements as a study of existing administrative data.
3. Results
In total 63,009,173 Medicare beneficiaries were included in the full cohort. We observed 18,610,833 first CVD hospital admissions in 401,315,016 person years and 9,741,992 first RSD hospital admissions in 453,244,756 person years. The vast majority of the individuals in the cohorts were White, not eligible for Medicaid, and between 65 and 74 years of age when they entered the study (Table 1). Percent park cover was highest in the western U.S., while greenness was highest in the eastern U.S. (Fig. 1). Median percent park cover was lower in the full cohort (7.5%) than the urban cohort (11.4%), while median greenness was higher in the full cohort (0.52) than the urban cohort (0.39, Table S2). Greenness was weakly negatively correlated with percent park cover (Spearman ρ = − 0.23) and not correlated with percent blue space cover (Spearman ρ = 0.00, Fig. S2). In the urban cohort, greenness was not correlated with percent park cover (Spearman ρ = 0.03).
Table 1.
Descriptive statistics of all U.S. Medicare fee-for-service beneficiaries (n = 63,009,173) from 2000 through 2016.a
| Individual-level covariates | Demographics at study entry | N (%) |
|---|---|---|
|
| ||
| Sex | Female | 34,725,534 (55.1) |
| Age entry | 65–74 years | 48,240,802 (76.6) |
| 75–84 years | 10,819,118 (17.2) |
|
| 85+ years | 3,949,253 (6.3) |
|
| Race | White | 53,262,938 (84.5) |
| Black | 5,511,612 (8.7) |
|
| Other/unknown | 4,234,623 (6.7) |
|
| Medicaid eligibility | Not eligible | 55,164,043 (87.5) |
| Eligible | 7,845,130 (12.5) |
|
| Region | Northeast | 12,374,875 (19.6) |
| South | 24,085,710 (38.2) |
|
| Midwest | 15,254,270 (24.2) |
|
| West | 11,294,318 (17.9) |
|
| Zip code-level covariates a | Aggregated data (2000–2016) | Median (IQR) |
| Natural environment measures | % Park cover NDVI % Blue space cover (1000 m buffer) % Blue space cover (no buffer) |
7.5 (15.9) 0.52 (0.27) 0.5 (3.2) 0.3 (1.3) |
| U.S. census covariates | Population density (persons/mile2) Median home value ($1000) Median household income ($1000) % with less than a high school degree % below the poverty level % owner-occupied housing units % Black % Hispanic |
517.4 (2919.0) 139.4 (145.3) 46.0 (24.9) 24.7 (21.6) 8.6 (8.2) 71.8 (21.4) 3.7 (13.5) 5.0 (14.0) |
| BRFSS covariate | % ever smoked | 46.2 (9.1) |
| Other environmental exposures | summer temperature (°C) summer specific humidity (g of water vapor/kg of dry air) summer total precipitation (mm, daily total) PM2.5 (ĝ/m3) NO2 (ppb) |
29.9 (5.2) 12.0 (4.0) 3.1 (2.3) 9.7 (4.0) 16.3 (13.9) |
Descriptive statistics of the zip code level covariates are given for the strata (aggregated data based on zip code, year, sex, race, Medicaid eligibility, 2-year categories of age at study entry and year of follow-up) based on the CVD cohort. Descriptive statistics of the zip code level covariates for the RSD cohort are shown in Table S2.
Fig. 1.
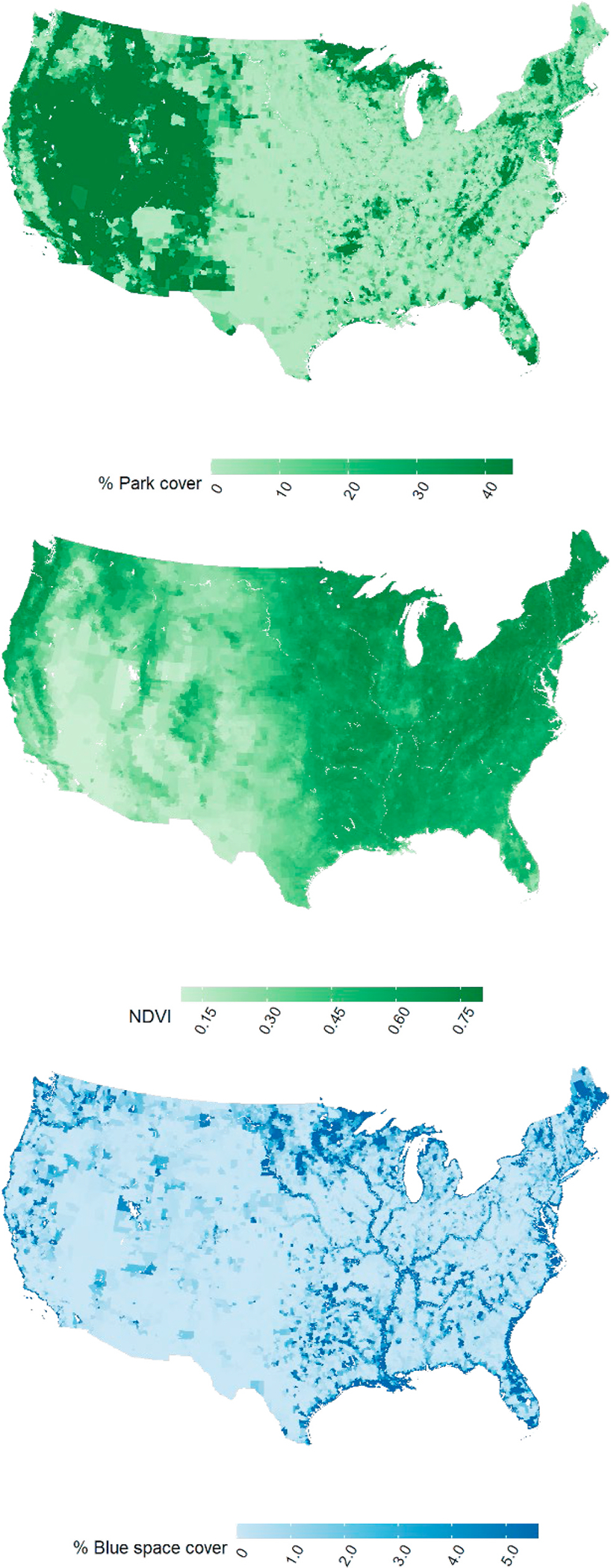
The spatial variation of zip code level % Park cover, NDVI (2008), and % Blue space cover in the contiguous U.S.a.
a To aid in visualization, the % Park cover map was truncated at 44.0%, the NDVI map was truncated at 0.1 and 0.8 and the % Blue space cover map was truncated at 5.6%.
3.1. Associations in the full cohort
Splines showed no or small deviations from linearity for the exposure-response curves (Fig. S3). We observed negative associations of percent park cover with CVD and RSD hospitalizations in our minimally adjusted model (Model 1, Fig. S4). After adjustment for potential confounders, associations of percent park cover attenuated to null (Table 2). For greenness, we observed weak positive associations with CVD and RSD hospitalization in our minimally adjusted model. In the fully adjusted model (Model 5), we found negative associations of greenness with CVD hospitalization (HR: 0.965, 95%CI: 0.959, 0.971, per IQR increase) but not with RSD hospitalization (HR: 0.987, 95%CI: 0.977, 0.997, per IQR increase). Percent blue space cover was not associated with CVD or RSD hospitalization.
Table 2.
HRs of percent park cover, NDVI and percent blue space cover with CVD and RSD hospitalization in the full and urban cohort of U.S. Medicare fee-for-service beneficiaries aged ≥65 years living in the contiguous U.S. from 2000 through 2016 (n = 63,009,173).a, b.
| Exposure (IQR) | CVD hospitalization |
RSD hospitalization |
||
|---|---|---|---|---|
| Full cohort |
Urban cohort |
Full cohort |
Urban cohort |
|
| HR (95% CI) | HR (95% CI) | HR (95% CI) | HR (95% CI) | |
|
| ||||
| % Park cover (15.9) | 0.997 (0.995, 1.000) | 0.991 (0.987, 0.996) | 0.995 (0.991, 0.999) | 0.995 (0.989, 1.002) |
| NDVI (0.27) | 0.965 (0.959, 0.971) | 0.979 (0.970, 0.989) | 0.987 (0.977, 0.997) | 1.018 (1.004, 1.032) |
| % Blue space cover (3.2) | 0.999 (0.998, 1.000) | 1.001 (1.000, 1.002) | 0.997 (0.995, 0.998) | 1.001 (0.999, 1.002) |
Associations are expressed per IQR increase of the CVD hospitalization (full) cohort. Models included percent park cover, NDVI and percent blue space cover simultaneously. Models were adjusted for calendar year, region, U.S. census covariates, % ever smoked, summer temperature, summer specific humidity, summer total precipitation, an offset for total person-time and strata for all possible combinations of sex, race, Medicaid Eligibility, age at study entry (2-year categories), and follow-up year. Urban cohorts included all person years in zip codes with a population density of 1000+ persons/mile2.
In the full cohorts, we observed 18, 610, 833 first CVD hospital admissions in 401, 315, 016 person years, 9,741,992 first respiratory disease hospital admissions in 453, 244, 756 person years. In the urban cohorts, we observed 8,354,677 first CVD hospital admissions in 185, 252, 789 person years, 4,387,395 first respiratory disease hospital admissions in 208, 437, 165 person years.
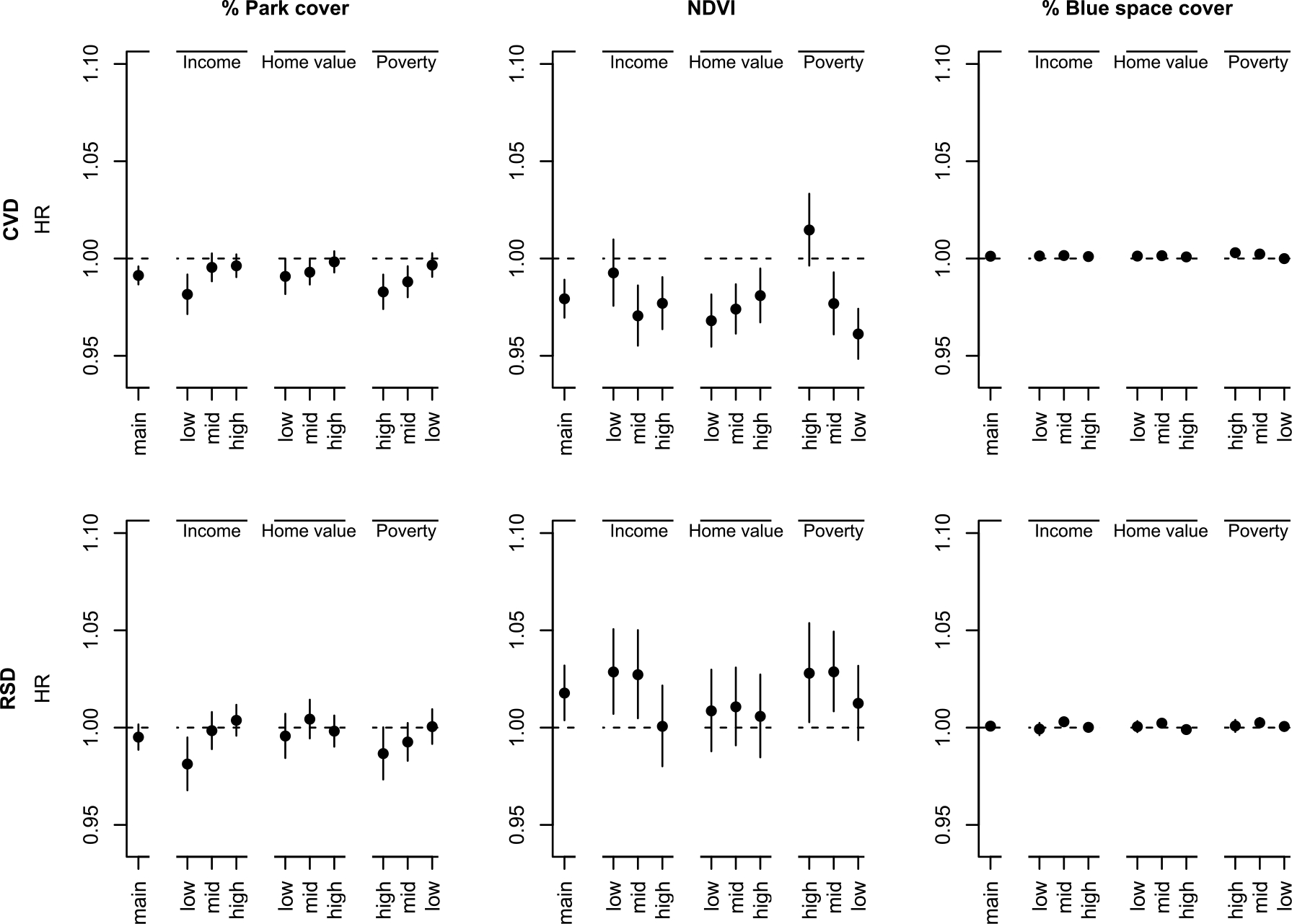
In general, for percent park cover and percent blue space cover, we did not observe a clear pattern of effect modification by individual demographics (Fig. 2) or nSES (Fig. 3) for CVD and RSD hospitalization. Negative associations of greenness with CVD hospitalization were stronger for individuals 85+ compared to 65+ or 75+ years, and for individuals not eligible for Medicaid compared to individuals eligible. We observed negative associations of greenness with CVD hospitalization for White and Black individuals, but positive associations for individuals of unknown/other race. Further, negative associations were observed for individuals living in the West and Northeast and positive in the South. For RSD hospitalization, we observed negative associations of greenness for females, Black individuals, and individuals living in the West or Midwest. Associations of greenness with CVD hospitalization became stronger with decreasing percent below the poverty levels (Fig. 3). Associations of greenness with CVD hospitalization were positive in the lowest NO2 tertile, null in the lowest PM2.5 tertile, and negative in the highest NO2 and PM2.5 tertiles (Table S3). No negative associations were observed between greenness and RSD hospitalization in any of the NO2 tertiles.
Fig. 2.
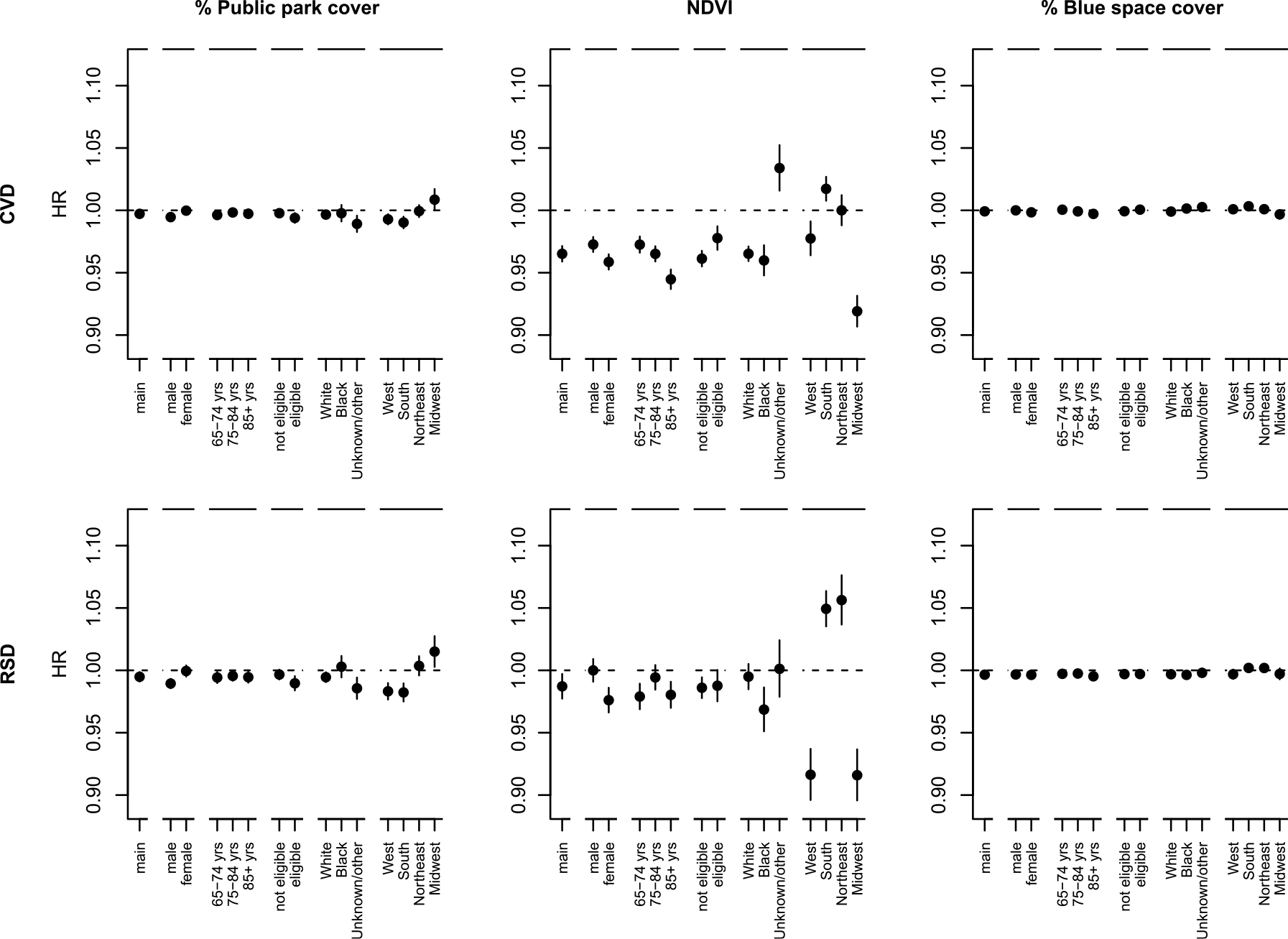
Associations of percent park cover, NDVI and percent blue space cover with CVD and RSD hospitalization in the full cohort in stratified analyses by sex (male, female), age (65–74, 75–84, 85+ years), Medicaid eligibility (not eligible, eligible), race (White, Black, unknown/other) and region (West, South, Northeast, Midwest).a
a Associations are expressed per IQR increase of the CVD hospitalization (full) cohort (IQR Percent park cover: 15.9, NDVI: 0.27, Percent blue space cover: 3.2). Models included park, NDVI, blue space and were adjusted for calendar year, region, U.S. census covariates, % ever smoked, summer temperature, summer specific humidity and summer total precipitation, an offset for total person-time and strata for all possible combinations of sex, race, Medicaid Eligibility, age at study entry (2-year categories), and follow-up year.
Fig. 3.
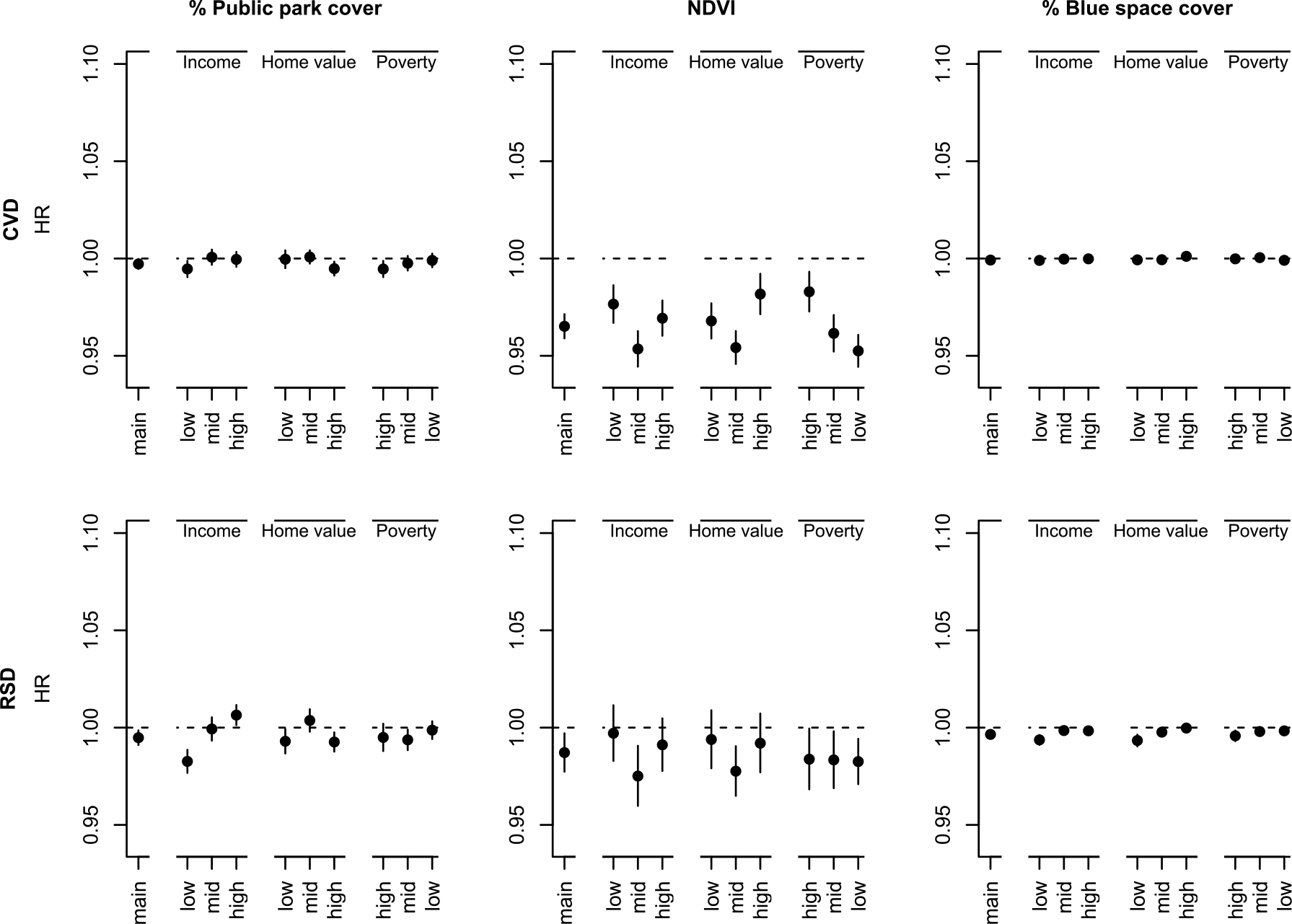
Associations of percent park cover, NDVI and percent blue space cover with CVD and RSD hospitalization in the full cohort in stratified analyses by median household income, median home value and percent below the poverty level.a, b
b To define strata, we used the following quantiles (q33.3, q66.7) for the CVD cohort: median household income ($1000): 39.9, 55.6; median home value ($1000): 107.4, 196.3; percent below the poverty level (%): 6.4, 11.4; for the RSD cohort: median household income ($1000): 40.0, 55.7; median home value ($1000): 107.7, 196.3; percent below the poverty level (%): 6.4, 11.4.
3.2. Associations in the urban cohort
Associations of percent park cover with CVD and RSD hospitalization in urban areas were negative in our minimally adjusted model and attenuated after adjustment for potential confounders (Fig. 4, Table 2). Greenness was negatively associated with CVD hospitalization and positively associated with RSD hospitalization in our fully adjusted model. No associations for percent blue space cover were observed in urban areas.
Fig. 4.
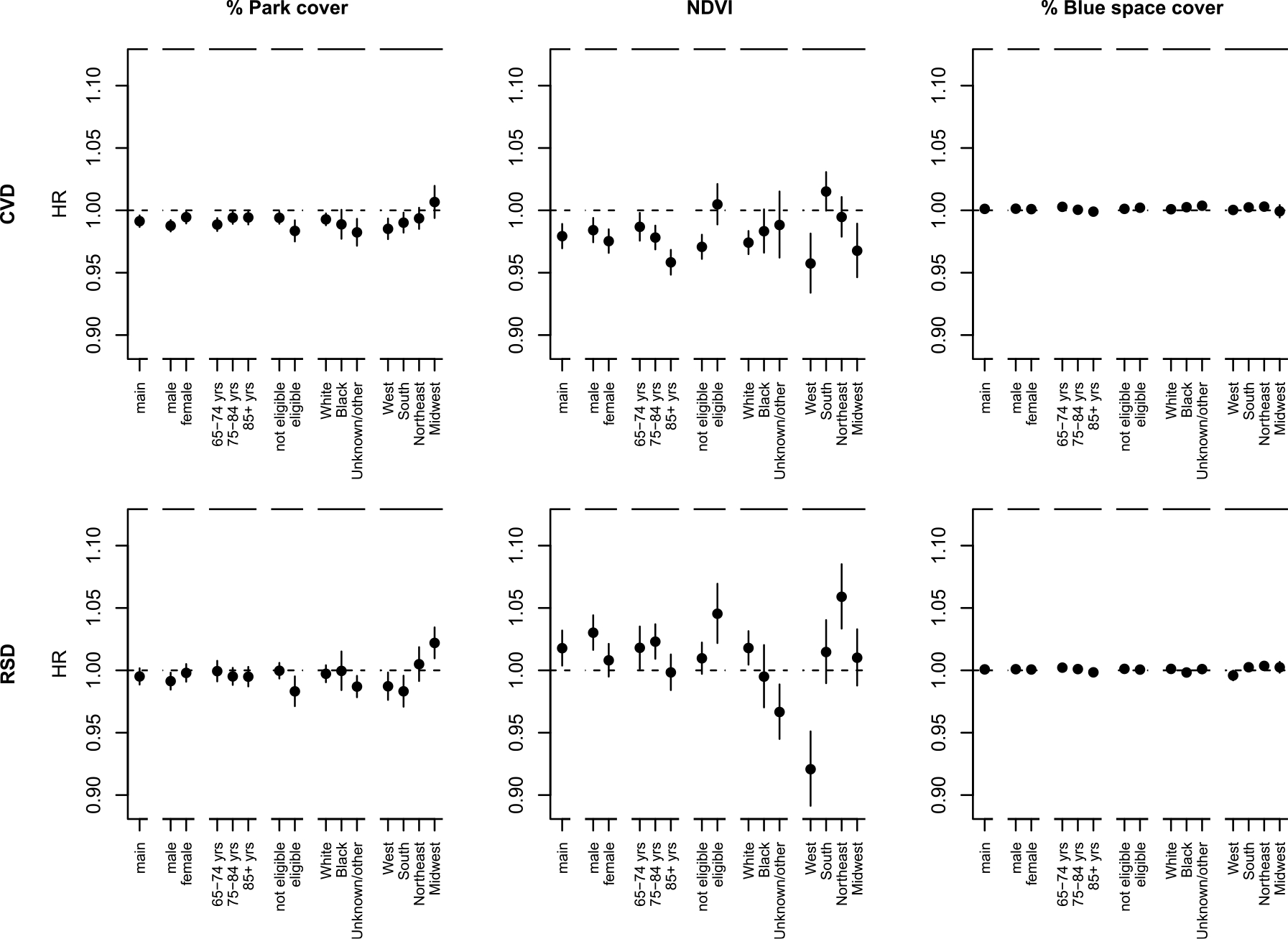
Associations of percent park cover, NDVI and percent blue space cover with CVD and RSD hospitalization in the urban population in stratified analyses by sex (male, female), age (65–74, 75–84, 85+ years), Medicaid eligibility (not eligible, eligible), race (White, Black, unknown/other) and region (West, South, Northeast, Midwest).a.
a Associations are expressed per IQR increase of the CVD hospitalization (full) cohort (IQR Percent park cover: 15.9, NDVI: 0.27, Percent blue space cover: 3.2). Models included percent park cover, NDVI, percent blue space cover and were adjusted for calendar year, region, U.S. census covariates, % ever smoked, summer temperature, summer specific humidity and summer total precipitation, an offset for total person-time and strata for all possible combinations of sex, race, Medicaid Eligibility, age at study entry (2-year categories), and follow-up year.
In urban areas, percent park cover was negatively associated with CVD and RSD hospitalization for Medicaid eligible individuals, individuals with an unknown or other race, and individuals living in the lowest median household income tertile and in the highest percent below poverty tertile (Figs. 4 and 5). Negative associations of greenness with CVD hospitalization were stronger for the elderly and individuals not eligible for Medicaid, no association was observed for individuals eligible for Medicaid. We observed positive associations of greenness with RSD hospitalization for males, younger, Medicaid eligible, and White individuals. We observed negative associations of greenness in the West (for CVD and RSD hospitalization) and in the Midwest (for CVD hospitalization). No associations of greenness with RSD hospitalization were observed in zip codes with a high median household income and low percent below the poverty level. Associations of greenness with CVD hospitalization were null or weakly positive in the lowest NO2 and PM2.5 tertiles and negative in the middle and highest tertiles (Table S4).
Fig. 5.
Associations of percent park cover, NDVI and percent blue space cover with CVD and RSD hospitalization in the urban population in stratified analyses by median household income, median home value and percent below the poverty level.a, b.
a Associations are expressed per IQR increase of the CVD hospitalization (full) cohort (IQR Percent park cover: 15.9, NDVI: 0.27, Percent blue space cover: 3.2). Models included park cover, NDVI, percent blue space cover and were adjusted for calendar year, region, U.S. census covariates, % ever smoked, summer temperature, summer specific humidity and summer total precipitation, an offset for total person-time and strata for all possible combinations of sex, race, Medicaid Eligibility, age at study entry (2-year categories), and follow-up year. b To define strata, we used the following quantiles (q33.3, q66.7) for the CVD cohort: median household income ($1000): 42.5, 62.4; median home value ($1000): 146.8, 276.8; percent below the poverty level (%): 6.5, 11.7; for the RSD cohort: median household income ($1000): 42.6, 62.5; median home value ($1000): 147.0, 276.7; percent below the poverty level (%): 6.5, 11.6.
3.3. Sensitivity analyses
In the full and urban cohort, we observed that associations were generally robust to additional adjustments for PM2.5, exclusion of potentially prevalent cases, and parameterizations of blue space (Table S5). Associations of single-exposure models were also similar. Additional adjustment for NO2 substantially attenuated associations of greenness with CVD hospitalization and resulted in positive associations of greenness with RSD hospitalizations. Stratified analyses by zip code area deciles showed no clear trend for stronger associations in smaller zip codes (Fig. S5).
4. Discussion
In this study of over 63 million Medicare beneficiaries, we observed protective associations between greenness and CVD, but not RSD, hospitalizations. In the urban cohort, associations of greenness with RSD hospitalization were positive. There was no protective association between percent park or blue space cover and CVD or RSD hospitalization in the full cohort. However, percent park cover was negatively associated with CVD and RSD hospitalization for low-SES individuals in urban areas.
We observed a weak negative correlation between percent park cover and greenness, indicating that greenness does not represent parks well at the zip code level. This is likely because NDVI captures total greenness, and therefore includes all types of green areas, such as agriculture, forests, lawns, and yards. Moreover, not all parks contain dense vegetation, especially in the west of the U.S. In urban areas, the correlation between percent park cover and greenness was close to null. This was somewhat unexpected as some urban greenness can be found in parks; however, urban parks may include paved paths and playgrounds that do not contain vegetation. Moreover, NDVI captures street and private greenery, which may constitute a large portion of the total greenness in urban areas. Not all types of greenery contribute equally to the NDVI, as it depends on the amount of aboveground photosynthetic biomass. Further, we note that correlations of percent park cover and NDVI with some covariates, such as median home value, population density and NO2, differ in direction.
We observed negative associations of greenness with CVD hospitalization, in line with previous studies (Chen et al., 2020; Dalton and Jones, 2020; Ponjoan et al., 2022; Seo et al., 2019). Park cover was not associated with CVD hospitalization. This is contrary to our expectations as park cover could be expected to be a better indicator for green spaces suitable for physical activity and social gatherings, and therefore may have a stronger impact on health. However, after adjustment for NO2, the negative association of greenness with CVD hospitalization almost completely disappeared. We note that NO2 could be a confounder, but it could also suggest mediation of the greenness – CVD hospitalization relation.
We observed positive associations of greenness with RSD hospitalization in the urban cohort, and in the full cohort after adjustment for NO2. This is in contrast to findings of some (Alcock et al., 2017; Maas et al., 2009; Sarkar et al., 2019; Xiao et al., 2022), but not all studies (Fan et al., 2020). In stratified analyses, we also observed positive associations of greenness with RSD hospitalization in zip codes with low NO2 concentrations in the full cohort, indicating complex relationships between greenness and air pollutants. The positive association with RSD hospitalization might be because vegetation can be a source of pollen, ozone and other respiratory irritants, such as VOCs (Hanigan and Johnston, 2007). Emission of VOCs might be more strongly related to greenness compared to percent park cover. Dominant vegetation types likely differ between regions; this may explain the differences of our findings with other studies and also the differences between the regional effect estimates for greenness. In the eastern U.S., isoprene and monoterpene emission from vegetation is generally high (Millet et al., 2008; Ying et al., 2015), and could explain the positive associations of greenness with RSD hospitalization in the South and Northeast. The stronger positive association in the urban cohort compared to the full cohort could be partly due to a lower tolerance to pollen. It has been hypothesized that urban dwellers are exposed to reduced pathogen levels compared to rural dwellers and therefore have an increased risk of allergy (Linneberg, 2005).
We observed no protective association between percent park or blue space cover and CVD or RSD hospitalization. This could be due to the absence of true associations in this study population, or methodological issues, such as our use of zip code-level exposure, characteristics of our study population, and adjustment for potential confounders. As we do not have information about the exact residential address of each beneficiary, we used zip code-level exposures. The median area of a zip code in the contiguous U.S. (in 2016) was about 93 km2 and in urban areas it was about 18 km2. This is substantially larger than the 300 m (area: 0.28 km2), and 1000 m (area: 3.14 km2) buffers commonly used in natural environment and health studies. Moreover, greenness and percent park cover can differ substantially within a zip code, and beneficiaries living close to the border of their zip code can be exposed to greenness in neighboring zip codes. The lack of associations for percent blue space cover may be related to the limited variability. Moreover, we note that there could be several air pollution sources in/close to blue spaces that may balance out potential beneficial effects of blue space.
In the urban population, percent park cover was generally negatively associated with CVD and RSD hospitalization for low SES individuals (Medicaid eligible individuals, individuals living in the lowest nSES tertile), but not for mid or high SES individuals. Associations of greenness with CVD hospitalization, on the other hand, were weaker/absent for low SES individuals and positive associations with RSD hospitalization were stronger for low SES individuals in the urban cohort. These findings are not consistent with a recent review that reported that beneficial effects of green space are stronger for low SES individuals than for high SES individuals and that protective effects for low SES groups were stronger for green space than greenness (Rigolon et al., 2021). As parks are freely accessible, individuals of low SES may go there to work out, relax, and socially interact.
Our study has multiple strengths. We assessed park cover, greenness and blue space for each zip code in the U.S. Percent park cover, greenness and blue space were included simultaneously in our models, to estimate associations for each exposure independent of the other exposures. We included approximately 63 million Medicare fee-for-service beneficiaries living in the contiguous U.S. in our cohorts. The Medicare study population is a fairly representative sample of individuals aged 65+ years across the U.S. However, during our follow-up period, Medicare beneficiaries may have switched to managed care plans and back, which could have resulted in some missed cases in our data. We note that elderly may experience, perceive, and use nature differently than other age groups. Hence, findings may not be generalizable to younger populations. Our study also has some limitations, in addition to those discussed above. Natural environment indicators were assessed at the zip code level, which likely resulted in exposure measurement error. We had no information about quality and safety of parks, greenness and blue spaces and on whether blue spaces could be used for recreation. Moreover, NDVI captures all green vegetation and does not differentiate between types of vegetation (e.g. trees, shrubs, grass). Blue space was based on satellite images from 1984 to 2018 years and park cover was based on data from 2020. We assumed that the spatial distribution of these exposures was stable over time. Further, we note that PM2.5 and NO2 were predicted by ensemble models that included natural environment indicators (Di et al., 2019b, 2019a). This could potentially lead to an overestimation of the true relation between these pollutants and the natural environments indicators. However, the relative importance of these indicators in the ensemble models was low. Therefore, we do not think that the use of natural environment indicators as predictors in the air pollution models have substantially affected the correlations between these variables in our cohort. We were unable to adjust for individual-level SES (other than Medicaid eligibility) and lifestyle factors, which may have resulted in an overestimation of the associations. However, we included various nSES measures that are likely related to individual SES. Further, we note that some individuals may have had their first CVD or RSD hospitalization before they were eligible for Medicare.
5. Conclusions
We observed a protective association of greenness on CVD hospitalization and indications of a harmful association on RSD hospitalization. Associations of greenness with both outcomes were sensitive to adjustment for NO2. For individuals of low SES, we observed that percent park cover, but not greenness, was negatively associated with CVD and RSD hospitalization in urban areas. Blue space was not associated with CVD or RSD hospitalization. These results suggest that natural environments may benefit health; however, benefits may be limited to certain contexts and certain health outcomes.
Supplementary Material
Funding
This study was supported by the National Institute of Environmental Health Sciences (R01 ES028033, R01 ES028033-S1, R01 ES026217, 1R01 ES030616, 1R01 ES029950, P30 ES000002), the National Heart, Lung and Blood Institute (R01 HL150119), the National Institute on Aging (5R01 AG060232-03, 1R01 AG066793, 3R01 AG066793-02S1, 1RF1 AG071024, 1RF1 AG074372-01A1), and the National Institute on minority Health and Health Disparities (R01 MD012769).
Footnotes
Declaration of competing interest
The authors declare the following financial interests/personal relationships which may be considered as potential competing interests:
This paper has been recommended for acceptance by Dr. Payam Dadvand.
Appendix A. Supplementary data
Supplementary data to this article can be found online at https://doi.org/10.1016/j.envpol.2022.120046.
Data availability
The data that has been used is confidential.
References
- Abatzoglou JT, 2013. Development of gridded surface meteorological data for ecological applications and modelling. Int. J. Climatol 33, 121–131. 10.1002/joc.3413. [DOI] [Google Scholar]
- Alcock I, White M, Cherrie M, Wheeler B, Taylor J, McInnes R, Otte im Kampe E, Vardoulakis S, Sarran C, Soyiri I, Fleming L, 2017. Land cover and air pollution are associated with asthma hospitalisations: a cross-sectional study. Environ. Int 109, 29–41. 10.1016/J.ENVINT.2017.08.009. [DOI] [PubMed] [Google Scholar]
- Bauwelinck M, Casas L, Nawrot TS, Nemery B, Trabelsi S, Thomas I, Aerts R, Lefebvre W, Vanpoucke C, Van Nieuwenhuyse A, Deboosere P, Vandenheede H, 2021. Residing in urban areas with higher green space is associated with lower mortality risk: a census-based cohort study with ten years of follow-up. Environ. Int 148, 106365 10.1016/J.ENVINT.2020.106365. [DOI] [PubMed] [Google Scholar]
- Bereziartua A, Chen J, de Hoogh K, Rodopoulou S, Andersen ZJ, Bellander T, Brandt J, Fecht D, Forastiere F, Gulliver J, Hertel O, Hoffmann B, Arthur Hvidtfeldt U, Verschuren WMM, Jöckel K-H, Jørgensen JT, Katsouyanni K, Ketzel M, Hjertager Krog N, Brynedal B, Leander K, Liu S, Ljungman P, Faure E, Magnusson PKE, Nagel G, Pershagen G, Peters A, Raaschou-Nielsen O, Renzi M, Rizzuto D, Samoli E, van der Schouw YT, Schramm S, Severi G, Stafoggia M, Strak M, Sørensen M, Tjønneland A, Weinmayr G, Wolf K, Zitt E, Brunekreef B, Hoek G, 2022. Exposure to surrounding greenness and natural-cause and cause-specific mortality in the ELAPSE pooled cohort. Environ. Int 166, 107341 10.1016/J.ENVINT.2022.107341. [DOI] [PubMed] [Google Scholar]
- Browning MHEM, Rigolon A, McAnirlin O, Yoon H, Violet), 2022. Where greenspace matters most: a systematic review of urbanicity, greenspace, and physical health. Landsc. Urban Plann 217, 104233 10.1016/J.LANDURBPLAN.2021.104233. [DOI] [Google Scholar]
- Chen H, Burnett RT, Bai L, Kwong JC, Crouse DL, Lavigne E, Goldberg MS, Copes R, Benmarhnia T, Ilango SD, Donkelaar A van, Martin, R.V., Hystad, P., 2020. Residential greenness and cardiovascular disease incidence, readmission, and mortality. Environ. Health Perspect 128, 1–11. 10.1289/EHP6161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crouse DL, Balram A, Hystad P, Pinault L, van den Bosch M, Chen H, Rainham D, Thomson EM, Close CH, van Donkelaar A, Martin RV, Ménard R, Robichaud A, Villeneuve PJ, 2018. Associations between living near water and risk of mortality among urban Canadians. Environ. Health Perspect 126 10.1289/EHP3397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crouse DL, Pinault L, Balram A, Hystad P, Peters PA, Chen H, van Donkelaar A, Martin RV, Ménard R, Robichaud A, Villeneuve PJ, 2017. Urban greenness and mortality in Canada’s largest cities: a national cohort study. Lancet Planet. Health 1, e289–e297. 10.1016/S2542-5196(17)30118-3. [DOI] [PubMed] [Google Scholar]
- Dalton AM, Jones AP, 2020. Residential neighbourhood greenspace is associated with reduced risk of cardiovascular disease: a prospective cohort study. PLoS One 15, e0226524. 10.1371/JOURNAL.PONE.0226524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Di Q, Amini H, Shi L, Kloog I, Silvern R, Kelly J, Benjamin Sabath M, Choirat C, Koutrakis P, Lyapustin A, Wang Y, Mickley LJ, Schwartz J, Paulson JA, 2019a. Assessing NO 2 concentration and model uncertainty with high spatiotemporal resolution across the contiguous United States using ensemble model averaging. ACS Publ 54, 1372–1384. 10.1021/acs.est.9b03358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Di Q, Amini H, Shi L, Kloog I, Silvern R, Kelly J, Sabath MB, Choirat C, Koutrakis P, Lyapustin A, Wang Y, Mickley LJ, Schwartz J, 2019b. An ensemble-based model of PM2.5 concentration across the contiguous United States with high spatiotemporal resolution. Environ. Int 130, 104909 10.1016/j.envint.2019.104909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Di Q, Wang Yan, Zanobetti A, Wang Yun, Koutrakis P, Choirat C, Dominici F, Schwartz JD, 2017. Air pollution and mortality in the Medicare population. N. Engl. J. Med 376, 2513–2522. 10.1056/NEJMoa1702747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fan J, Guo Y, Cao Z, Cong S, Wang N, Lin H, Wang Chongjian, Bao H, Lv X, Wang B, Gao Y, Chen Y, Yang T, Wang L, Wang Chen, Ruan Z, Fang L, 2020. Neighborhood greenness associated with chronic obstructive pulmonary disease: a nationwide cross-sectional study in China. Environ. Int 144, 106042 10.1016/J.ENVINT.2020.106042. [DOI] [PubMed] [Google Scholar]
- Fong KC, Hart JE, James P, 2018. A review of epidemiologic studies on greenness and health: updated literature through 2017. Curr. Environ. Heal reports 5 (1), 77–87. 10.1007/s40572-018-0179-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Georgiou M, Morison G, Smith N, Tieges Z, Chastin S, 2021. Mechanisms of impact of blue spaces on human health: a systematic literature review and meta-analysis. Int. J. Environ. Res. Publ. Health 18, 1–41. 10.3390/ijerph18052486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gorelick N, Hancher M, Dixon M, Ilyushchenko S, Thau D, Moore R, 2017. Google Earth engine: planetary-scale geospatial analysis for everyone. Remote Sens. Environ 202, 18–27. 10.1016/j.rse.2017.06.031. [DOI] [Google Scholar]
- Hanigan IC, Johnston FH, 2007. Respiratory hospital admissions were associated with ambient airborne pollen in Darwin, Australia, 2004–2005. Clin. Exp. Allergy 37, 1556–1565. 10.1111/J.1365-2222.2007.02800.X. [DOI] [PubMed] [Google Scholar]
- Klompmaker JO, Janssen NAH, Bloemsma LD, Marra M, Lebret E, Gehring U, Hoek G, 2021. Effects of exposure to surrounding green, air pollution and traffic noise with non-accidental and cause-specific mortality in the Dutch national cohort. Environ. Health 20, 1–16. 10.1186/S12940-021-00769-0, 2021 201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Labib SM, Lindley S, Huck JJ, 2020. Spatial dimensions of the influence of urban green-blue spaces on human health: a systematic review. Environ. Res 180, 108869 10.1016/J.ENVRES.2019.108869. [DOI] [PubMed] [Google Scholar]
- Linneberg A, 2005. Hypothesis: urbanization and the allergy epidemic – a reverse case of immunotherapy? Allergy 60, 538–539. 10.1111/J.1398-9995.2005.00721.X. [DOI] [PubMed] [Google Scholar]
- Maas J, Verheij RA, De Vries S, Spreeuwenberg P, Schellevis FG, Groenewegen PP, 2009. Morbidity is related to a green living environment. J. Epidemiol. Community Health 63, 967–973. 10.1136/JECH.2008.079038. [DOI] [PubMed] [Google Scholar]
- Markevych I, Schoierer J, Hartig T, Chudnovsky A, Hystad P, Dzhambov AM, de Vries S, Triguero-Mas M, Brauer M, Nieuwenhuijsen MJ, Lupp G, Richardson EA, Astell-Burt T, Dimitrova D, Feng X, Sadeh M, Standl M, Heinrich J, Fuertes E, 2017. Exploring pathways linking greenspace to health: theoretical and methodological guidance. Environ. Res 158, 301–317. 10.1016/J.ENVRES.2017.06.028. [DOI] [PubMed] [Google Scholar]
- McDougall CW, Quilliam RS, Hanley N, Oliver DM, 2020. Freshwater blue space and population health: an emerging research agenda. Sci. Total Environ 737, 140196 10.1016/J.SCITOTENV.2020.140196. [DOI] [PubMed] [Google Scholar]
- Millet DB, Jacob DJ, Folkert Boersma K, Fu T-M, Kurosu Thomas P., Chance Kelly, Heald Colette, L., Guenther Alex, Jacob DBJ, Boersma KF, Fu TM, Kurosu TP, Chance K, Heald CL, Guenther A, 2008. Spatial distribution of isoprene emissions from North America derived from formaldehyde column measurements by the OMI satellite sensor. J. Geophys. Res. Atmos 113, 2307. 10.1029/2007JD008950. [DOI] [Google Scholar]
- NASA. Measuring Vegetation (NDVI & EVI) [WWW Document]. URL https://earthobservatory.nasa.gov/features/MeasuringVegetation/measuring_vegetation_2.php (accessed 6.16.20).
- Nieuwenhuijsen MJ, Gascon M, Martinez D, Ponjoan A, Blanch J, Garcia-Gil MDM, Ramos R, Foraster M, Mueller N, Espinosa A, Cirach M, Khreis H, Dadvand P, Basagaña X, 2018. Air pollution, noise, blue space, and green space and premature mortality in barcelona: a mega cohort. Int. J. Environ. Res. Publ. Health 15 (2405 15), 2405. 10.3390/IJERPH15112405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pekel JF, Cottam A, Gorelick N, Belward AS, 2016. High-resolution mapping of global surface water and its long-term changes. Nature 540, 418–422. 10.1038/nature20584. [DOI] [PubMed] [Google Scholar]
- Ponjoan A, Blanch J, Alves-Cabratosa L, Martí-Lluch R, Comas-Cufí M, Cirach M, Nieuwenhuijsen M, Garcia-Gil M, del M, Ramos R, 2022. Impact of residential greenness on myocardial infarction in the population with diabetes: a sex-dependent association? Environ. Res. 205, 112449 10.1016/J.ENVRES.2021.112449. [DOI] [PubMed] [Google Scholar]
- Requia WJ, Di Q, Silvern RF, Kelly JT, Koutrakis P, Mickley LJ, Sulprizio MP, Amini H, Shi L, Schwartz J, 2020. An ensemble learning approach for estimating high spatiotemporal resolution of ground-level ozone in the contiguous United States. Environ. Sci. Technol 54, 11037–11047. 10.1021/acs.est.0c01791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rigolon A, Browning MHEM, McAnirlin O, Yoon H, 2021. Green space and health equity: a systematic review on the potential of green space to reduce health disparities. Int. J. Environ. Res. Publ. Health 18, 1–29. 10.3390/ijerph18052563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sarkar C, Zhang B, Ni M, Kumari S, Bauermeister S, Gallacher J, Webster C, 2019. Environmental correlates of chronic obstructive pulmonary disease in 96 779 participants from the UK Biobank: a cross-sectional, observational study. Lancet Planet. Health 3, e478–e490. 10.1016/S2542-5196(19)30214-1. [DOI] [PubMed] [Google Scholar]
- Seo S, Choi S, Kim K, Kim SM, Park SM, 2019. Association between urban green space and the risk of cardiovascular disease: a longitudinal study in seven Korean metropolitan areas. Environ. Int 125, 51–57. 10.1016/J.ENVINT.2019.01.038. [DOI] [PubMed] [Google Scholar]
- Shi L, Wu X, Danesh Yazdi M, Braun D, Abu Awad Y, Wei Y, Liu P, Di Q, Wang Y, Schwartz J, Dominici F, Kioumourtzoglou M-A, Zanobetti A, 2020. Long-term effects of PM2·5 on neurological disorders in the American Medicare population: a longitudinal cohort study. Lancet Planet. Health 4, e557–e565. 10.1016/s2542-5196(20)30227-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Twohig-Bennett C, Jones A, 2018. The health benefits of the great outdoors: a systematic review and meta-analysis of greenspace exposure and health outcomes. Environ. Res 166, 628–637. 10.1016/j.envres.2018.06.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Geological Survey (USGS), Gap Analysis Project, 2020. Protected Areas Database of the United States (PAD-US) 2.1: U.S. Geological Survey Data Release [WWW Document]. 10.5066/P92QM3NT. [DOI]
- United States Census Bureau, 2022. County Population Totals: 2010–2019.
- Vienneau D, Hoogh K. de, Faeh D, Kaufmann M, Wunderli JM, Röösli M, Group SS, 2017. More than clean air and tranquillity: residential green is independently associated with decreasing mortality. Environ. Int 108, 176–184. 10.1016/j.envint.2017.08.012. [DOI] [PubMed] [Google Scholar]
- White MP, Elliott LR, Gascon M, Roberts B, Fleming LE, 2020. Blue space, health and well-being: a narrative overview and synthesis of potential benefits. Environ. Res. 191, 110169. 10.1016/j.envres.2020.110169. [DOI] [PubMed] [Google Scholar]
- Xiao Y, Gu X, Niu H, Meng X, Zhang L, Xu J, Yang L, Zhao J, Zhang Xiangyan, Bai C, Kang J, Ran P, Shen H, Wen F, Huang K, Chen Y, Sun T, Shan G, Lin Y, Wu S, Zhu J, Wang R, Shi Z, Xu Y, Ye X, Song Y, Wang Q, Zhou Y, Ding L, Li D, Yao W, Guo Y, Xiao F, Lu Y, Peng X, Zhang B, Xiao D, Wang Z, Zhang H, Bu X, Zhang Xiaolei, An L, Zhang S, Cao Z, Zhan Q, Yang Y, Liang L, Cao B, Dai H, Wu T, He J, Kan H, Chen R, Yang T, Wang C, 2022. Associations of residential greenness with lung function and chronic obstructive pulmonary disease in China. Environ. Res 209, 112877 10.1016/J.ENVRES.2022.112877. [DOI] [PubMed] [Google Scholar]
- Ying Q, Li J, Kota SH, 2015. Significant contributions of isoprene to summertime secondary organic aerosol in eastern United States. Environ. Sci. Technol 49, 7834–7842. 10.1021/ACS.EST.5B02514/SUPPL_FILE/ES5B02514_SI_001.PDF. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data that has been used is confidential.


