Abstract
We examined media exposure, psychological fear and worry, perceptions of risk, and health protective behaviors surrounding the 2014 Ebola virus outbreak in a probability-based, representative, national sample of Americans (N = 3447). Structural equation models examined relationships between amount (hours/day) and content (e.g., graphic images of dead bodies) of media exposure and counts of self-reported health protective behaviors that participants performed or would perform if Ebola spread to their community. Ebola-related risk perceptions and fear and worry were potential mediators. Greater total hours and more graphic media exposure positively correlated with more fear and worry; greater total hours of media exposure also positively correlated with higher perceived risk. Higher risk perceptions were associated with more health protective behaviors performed and intended. Greater fear and worry were associated with more behaviors performed. Amount and content of media exposure exhibited indirect effects on behaviors performed; amount of media exposure had indirect effects on intentions. Media may help promote health protective behaviors during public health threats; the amount and content should be congruent with threat to minimize distress and maximize resources.
Keywords: Ebola virus, Media, Risk perceptions, Health protective behaviors, Public health crisis
1. Introduction
As demonstrated throughout the ongoing COVID-19 pandemic, seasonal influenza outbreaks, and more localized outbreaks such as H1N1 in 2009 and SARS in 2002–2003, effective media communications pose challenges to public health officials tasked with conveying accurate information to the public and encouraging appropriate health protective behaviors. This is particularly important with fluctuating risks and evolving mitigation efforts. Since 2020, the COVID-19 crisis has dominated the news cycle: but this is neither the first nor the last highly publicized public health threat facing society. For example, in Fall 2014, the Ebola epidemic commanded much of the U.S. media cycle [1], even though, in contrast to the COVID-19 pandemic, there were only 4 confirmed cases of Ebola in the United States. At that time, though, the potential toll of Ebola was unknown and accompanied by staggering initial estimates of reach for the disease - along with vivid stories and images from devastated areas in West Africa. Yet, although Ebola spreads less easily than COVID-19, it is more deadly [2,3]. How did the populace respond to that emerging threat?
During Fall 2014, The New York Times reported more than 350 Ebola stories, including more than 70 on the front page [4]. Analyses of social media reports on Twitter found more Ebola-related tweets in the U.S. compared to countries where the virus was vastly more prevalent, with frequency of these tweets positively associated with negative emotions [5]. Herein, we present secondary data analyses derived from a representative, probability-based sample of Americans, assessed in the immediate aftermath of the Ebola 2014 outbreak. The overarching goal was to examine how media exposure to a potential threat was associated with performance of health protective behaviors. We employ a multi-disciplinary approach, bridging together perspectives from disaster psychology, communication science, decision science, health psychology, and stress and coping.
During public health crises, accurate public perceptions of risks are vital to achieving appropriate public policies and promoting personal protective behaviors. As described in Media Dependency Theory, in information-based societies, the media is the primary means by which individuals seek out and obtain information, particularly during times of crisis [6,7]. Despite the relatively low objective threat of contracting Ebola in the United States, analyses of Ebola-related tweets from 2014 found that 42% of Ebola-related Twitter posts involved risk-elevating messaging likely to contribute to increased risk perceptions [8]. While 96% of print and television coverage of Ebola contained risk-elevating messaging, only 55% and 53% contained risk-minimizing messages or both risk-minimizing and risk-elevating messaging, respectively [9]. As evidenced in research during the COVID-19 pandemic, heavier reliance on the media was associated with increased perception of risk, with both traditional media (e.g., television and print) and Facebook exposure associated with the highest risk perceptions [10].
Despite the proliferation of risk-elevating messaging during the Ebola crisis, Fischhoff et al. [11] found that by early 2015, when the Ebola threat had ebbed for an indeterminate period, Americans had reasonably coherent perceptions of the risk, with large individual variation (e.g., females and individuals with lower incomes perceived greater risk of becoming sick from Ebola). Here, we analyze cognitive, affective, experiential, and demographic predictors that guided adoption of health protective behaviors during that outbreak. During many public health crises (e.g., Zika epidemic, reemergence of measles in the U.S.), many individuals’ primary exposure to the illness is through the news media. That coverage can provide valuable information about the nature of the risk and appropriate health protective behaviors [12]. Yet it can also evoke stress responses among individuals facing little direct threat [13, 14]. This psychological activation of the stress response system can itself have negative health consequences downstream: thus the benefits of mitigation efforts must be carefully weighed against the deleterious consequences of increased stress in the populace [15].
As evidenced during the ongoing COVID-19 pandemic, encouraging individuals to take appropriate health protective behaviors during public health threats is critical to mitigating potential crises [16]. As outlined in leading theories of health behavior, two of these motivations, risk appraisals and fear, can encourage health protective actions in response to threats [17]. Herein, we examine how the type and amount of media communications are related to self-protective behavior, contrasting both cognitive (risk perception) and affective (fear) processes as potential mediators of this relationship. In our model, we theorize that media exposure (both type and amount) elicits both cognitive and affective psychological responses. These, in turn, motivate people to act in ways that can reduce fear and mitigate risk.
1.1. Conceptual model: media, perception of risk, and health-protective action
In constructing our model, we integrate Media Dependency Theory with key constructs from the Health Belief Model (HBM) [18], Theory of Planned Behavior (TPB) [19,20], and Protection Motivation Theory (PMT) [21]. These theories provide frameworks for using media risk communications to encourage protective actions or anticipating their damage. The HBM posits value-expectancy constructs that explain decisions to take protective actions; namely, as perceived susceptibility and severity increase, so does perceived threat [22]. These factors, along with external cues to action, then trigger health protective behaviors. The TPB, an extension of the Theory of Reasoned Action [23], states that intentions to perform a behavior follow reasonably (but not always rationally) from specific behavior-related beliefs. Prior research integrating TPB with Media Dependency Theory found high media exposure, regardless of self-reported dependency, was associated with increased protective behaviors [24]. In addition, people tend to act on these intentions when required skills are present and situational factors do not impede action. PMT posits that a combination of severity, probability, and both self- and response efficacy lead to the adoption of health protective behaviors, all of which are can be communicated to individuals via the media. From these frameworks, we infer that people may be most willing to engage in health protective behaviors when these actions are relatively easy (e.g., washing hands, using sanitizer), the threat is severe, and people perceive themselves at risk.
These perspectives suggest that media exposure to a public health crisis may shape subsequent health protective behaviors. Indeed, research conducted during COVID-19 found that COVID-19-related media exposure was associated with increased risk perceptions, and in turn increased health protective behaviors (staying home and social distancing) [25]. Through the TPB lens, the media provides critical input to the beliefs that shape intentions to perform health protective behaviors. These inputs are interpreted in the context of individuals’ demographics, socioeconomic status, and prior personal experiences [23]. For example, research using the TPB model found that increased risk perception was a mediating factor between information received from trusted inputs (e.g., the media) and intentions to engage in food safety behaviors [26]. Similarly with HBM, the media may be an informational source shaping individuals’ risk perceptions [27].
1.2. Psychological responses to media exposure and resulting health protective behaviors
Media communications can influence self-protective behaviors through affective responses (e.g., fear, distress) [28,29], as well as cognitive ones (e.g., perception of risk). Affective responses can motivate valuable individual health protective behavior [30]. Fear-based reactions and disgust may prompt adaptive behaviors such as quitting smoking [31] or intending to exercise [32]. Increased fear in response to influenza threat resulted in increases in intentions to obtain a flu vaccine [33]. Consequently, fear may serve as a mediator between media exposure (both amount and content) and health-protective behaviors.
However, affective responses can also lead societies to misallocate resources [34], if they amplify societal perceptions of risk for low-probability events [35,36]. For example, early in the COVID-19 pandemic, panic buying diverted protective gear needed by healthcare workers; during prior threats emergency departments were swamped by “worried well” [15]. Media exposure can also produce psychological distress [37–39], with potential physical and mental health problems [40].
Two components of media exposure have been linked to both affective and cognitive responses: the amount and the content. The amount of media exposure has been associated with posttraumatic responses to the September 11, 2001 terrorist attacks (9/11) [37] and the Boston Marathon bombings [39]. Similarly, the content of graphic images (e.g., television scenes of people jumping from the World Trade Center) was associated with increased incidence of PTSD following 9/11 [40]. Likewise, increased exposure to images depicting blood or gore was associated with increased fear and worry regarding terrorism following the Boston Marathon bombings [38].
1.3. The present study
Collective events provide opportunities to observe how these complex processes play out in populations that vary in their exposures and responses. We were able to study diverse Americans’ psychological and behavioral responses to the 2014 Ebola outbreak, with a representative sample, drawn from participants in an ongoing, longitudinal study. We examined media exposure as a potential source of Ebola-related cognitive and affective processes and, in turn, whether those processes affected health protective behaviors. Specifically, we asked if both cognitive processes (self-reported perceptions of Ebola risk) and affective processes (self-reported fear and worry) were mediators of the relationship between media exposure and health protective behaviors, both intended and performed. Intentions are central to models of health protective behaviors and, empirically, are typically good, if imperfect, predictors of subsequent actual behavior [20]. Hence, they indicate what behavior might have been, had Ebola become more prevalent.
We had three hypotheses: 1) Exposure to more hours of Ebola-related media exposure and more Ebola-related graphic images will be positively associated with reporting more health protective behaviors (intended and performed). 2) Exposure to more hours of Ebola-related media exposure and more Ebola-related graphic images will be positively associated with perceptions of Ebola-related risk and Ebola-related fear and worry. 3) Higher perceptions of Ebola-related risk and greater Ebola-related fear and worry will mediate the link between media exposure (both amount and content) and health protective behaviors (intended and performed).
2. Method
2.1. Design, sample, and data collection
Participants were drawn from a longitudinal study of Americans’ responses to negative life events and collective trauma; 4675 were initially surveyed in 2013 shortly after the Boston Marathon bombings (79.1% participation rate), including representative samples from metropolitan Boston (n = 846), New York City (n = 941), and the remainder of the U.S. (n = 2888). The initial sampling design was generated to oversample populations exposed to domestic terrorism (i.e., the Boston Marathon bombings, the 9/11 terrorist attacks) because such communities might exhibit increased psychological vulnerability to collective threats. Participants were recruited from the GfK (now Ipsos) KnowledgePanel, which used address-based sampling methods to randomly sample and recruit individuals within U.S. households. Starting December 29, 2014, 4336 participants who had agreed to be contacted for future surveys were invited to participate in a study of their responses to the Ebola outbreak. The final sample had 3447 participants (79.5% participation). Overall, 3114 (90.3%) completed the survey online and 333 (9.7%) completed a paper and pencil version. All procedures were approved by the Institutional Review Board of the University of California, Irvine.
Panel selection methods provide statistical control of the representativeness of KnowledgePanel samples and ensure samples’ comparability to the target population. Panel design weights were calculated to reflect unequal selection probabilities (according to demographic categories) for each sampled member of the KnowledgePanel. Design weights were post-stratified to benchmarks from the most recent U.S. government statistics for each sampling area (Boston, New York, and the remainder of U.S.) to compensate for differential nonresponse. Thus, the weighted composition of the sample closely matched that of the target population as defined by the benchmarks from the American Community Survey of the U.S. Department of Commerce [41], allowing for population-based inferences. (See Ref. [11] for details of weight construction.) Comparisons between the KnowledgePanel, the adult U.S. population, and the Ebola study presented herein are outlined in Supplemental Table 1. Of note, the Ebola sample weight preserved the oversampling in New York and Boston that were part of the initial design of the study [39].
2.2. Measures
2.2.1. Predictor variables
Hours of Ebola-related media exposure.
Participants reported the average number of hours they spent per day consuming Ebola-related media from all sources [“(TV, radio, videos or text on Internet news sites, social media, mobile phones, newspapers and other print media)”] in October 2014. We used ranges based on previous research on media exposure to community adversity [39]: less than 1 h, 1–3 h, 4–6 h, or more than 6 h of Ebola media per day, across all sources. Data were analyzed both continuously and as a three-level categorical value to test for quadratic effects, combining the two highest groups due to small cell size. We present analyses treating exposure as a continuous variable in the main text and provide the categorical analyses as supplemental material.
Exposure to graphic images of the Ebola crisis.
Participants reported how often they saw media images of 1) bloody sites where Ebola patients had been, 2) bloody Ebola patients, and 3) dead bodies of people who had died from Ebola, on 5-point scales with endpoints (1 = never; 5 = very often). As reliability was very good (α = 0.87), we used their mean value.
2.2.2. Covariates
Demographics and prior mental health.
Upon enrollment to the KnowledgePanel, all participants provided demographic (e.g., age, gender, ethnicity, education, income, and marital status) and mental health information (updated regularly). Prior mental health difficulties were assessed using two items modeled after the U.S. Centers for Disease Control and Prevention’s National Center for Health Statistics annual National Health Interview Survey [42]: Respondents reported whether a physician had ever diagnosed them with depression or anxiety disorders (coded 0 for no prior diagnoses, 1 for either anxiety or depression, 2 for both). Over 94% of respondents had provided mental health histories prior to the Ebola outbreak. To retain sample representativeness, missing values for depression and anxiety were imputed using Sequential Hot-Deck imputation.
2.2.3. Outcome variables
Performance of Ebola-related health-protective behaviors.
Participants were provided a list of four behaviors “someone might do in response to Ebola” and were asked to check behaviors they had performed: 1) avoided public places, 2) washed hands or used hand sanitizer more often, 3) wore a face mask, and/or 4) avoided public transportation. We summed the number of reported behaviors (0–4).
Intention to perform Ebola-related health-protective behaviors.
Participants were provided a list of four behaviors “someone might do in response to Ebola” and were asked to check behaviors they would do if they knew someone in their area had the Ebola virus: 1) avoid public places, 2) wash hands or use hand sanitizer more often, 3) wear a face mask, and/or 4) avoid public transportation. We summed the number of intended behaviors (0–4).
2.2.4. Mediators
Ebola-related risk perceptions.
A composite measure of risk perceptions related to Ebola was generated by averaging six items assessing different aspects of risk. (Fischhoff and colleagues [11] report more fully on this measure, called the transmissibility index.) The first three items asked participants to report “the percent chance that you will catch Ebola,” if you “spend a day working in the same office as someone who has the Ebola virus” a) “but has no symptoms at all?“, b) “and is beginning to feel badly?“, and c) “and is seriously ill?” The second three items asked for “the percent chance that you will catch Ebola if you spend half an hour riding on a bus or in a subway car with someone who has the Ebola virus” a) “but has no symptoms at all?” b) “and is beginning to feel badly?” and c) “and is seriously ill?” Participants were asked to “provide a number between 0 and 100.” These six judgments were highly correlated: α = 0.93; items were averaged.
Ebola-related fear and worry.
Two items assessed how often respondents had experienced Ebola-related fear and worry in the preceding week on scales from 1 (never) to 5 (all the time): “I worry that Ebola will personally affect me or someone in my family in the future” and “How often in the past week have you had fears about the possibility of Ebola affecting your community?” Items were based on prior post-9/11 research [43]. Reliability was α = 0.84; items were averaged.
2.3. Analytic strategy
We calculated bivariate relationships between study variables, then used logistic regression to predict intended and reported health protective behaviors. We then constructed two path models with amount (total hours) and type (graphic) of media exposure as independent variables. Perceived Ebola-related risk and Ebola-related fear and worry were hypothesized mediators. We used demographic indicators and prior mental health as covariates. As missing data were rare, we used row mean substitution for all continuous composites with data available from more than 66% of items.
Path analyses used the generalized structural equation modeling program (GSEM) in STATA 16, an extension of the Structural Equation Modeling program that accommodates survey sampling weights. Path analysis incorporates multiple equations simultaneously and is a parsimonious method to test hypothesized indirect and direct effects while reducing Type 1 error [44]. It is recommended over the classic mediation model when testing for complementary mediation (i.e., both mediated and direct effects are in the same direction) [45]. Since sampling weights correct for standard errors, we did not use the bootstrapping method common in testing mediation in structural equation modeling as its performance in such situations is unclear [46]. We controlled for key covariates (region of residence, demographics, prior mental health) for each exogenous variable [47]. Gaussian and Poisson distributions were specified for continuous (i.e., fear, risk) and count (i.e., number of health protective behaviors) outcomes, respectively. We present unstandardized coefficients, which represent the actual scaling of the individual variables.
3. Results
3.1. Descriptive statistics
The demographic composition of the final weighted sample closely matched benchmarks for the target population in Boston, New York, and the remainder of the U.S [11]. See Supplemental Table 1 for detailed demographic descriptive statistics. Of the sample, 11.60% reported a prior diagnosis of either depression or anxiety (n = 400), 7.47% reported both diagnoses (n = 257), and 80.93% reported neither mental health diagnosis (n = 2787). Table 1 presents bivariate relationships between key study variables.
Table 1.
Bivariate relationships between key study variables.
| Dependent Variables | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 16 | 17 | 18 | |
| Predictor Variables | ||||||||||||||
| 1. Health protective behaviors | – | – | ||||||||||||
| 2. Intention to preform health behaviors | −.40*** | – | ||||||||||||
| 3. Ebola worry | .33*** | .09*** | – | |||||||||||
| 4. Risk perception | .01*** | .01*** | .01*** | – | ||||||||||
| 5. Media exposure | .22*** | .06* | .37*** | 5.39** | – | |||||||||
| 6. Graphic images | .12** | .01 | .14*** | −.53 | .10*** | – | ||||||||
| 7. Prior mental health ailments | −.02 | .01 | .09** | 2.98* | .07** | −.02 | – | |||||||
| 8. Income | −.08*** | −.01 | −.05*** | −1.51*** | −.03*** | .02* | −.16*** | – | ||||||
| 9. Age | −.001 | .003*** | .00 | −.06 | .002 | .001 | .003 | −.01** | – | |||||
| 10. College | −.37*** | −.08** | −.17*** | −7.22*** | −.11*** | .03 | −.43*** | 1.51*** | −2.07** | – | ||||
| 11. Gender | −.06 | −.10** | −.04 | −4.17** | −.06* | .13** | .06* | .20* | −1.19 | .003 | – | – | – | – |
| 12. White, non-Hispanic | −.30*** | .01 | −.29*** | −1.45 | −.17*** | −.12* | .11 | .55*** | 6.50*** | .08 | .05 | .77*** | −.69*** | .06 |
| 13. Black | .21 | .10 | .19* | −2.73 | .31*** | .11 | −.03 | −.72*** | −1.57 | −.74*** | −.22 | −.81* | .31 | .18 |
| 14. Other, non-Hispanic | −.02 | .05 | .30** | −1.56 | −.06 | .14 | −.21 | .08 | −3.92* | 1.07*** | −.13 | −.04 | .48 | −.33 |
| 15. Hispanic | .37*** | −.14* | .21** | 5.79* | .10* | .06 | .11 | −.50** | −8.41*** | −.39* | .17 | −.92** | .66*** | −.05 |
| 16. Boston Metro Area | −.13 | −.10* | −.13** | −5.22* | −.02 | −.02 | −.03 | .38** | 1.93 | .48*** | −.11 | – | – | |
| 17. New York Metro Area | −.08 | −.11* | .09 | .02 | .07 | .09 | −.09 | .37** | .46 | .30* | −.06 | – | – | – |
| 18. National sample | .13 | .14*** | .02 | 3.27* | −.03 | −.05 | .08 | −.49*** | −1.53 | −.53*** | .11 | – | – | − |
Male gender = 1; Female gender = 0.
College education = 1; Less than a college education = 0.
Note: Variables are unstandardized. Count variables (1, 2, 7) are in the Poisson distribution; continuous variables (3–6, 8, 9) are in the Gaussian distribution; dichotomous variables (10–18) are in the Logit distribution. Variables entered into the equations as predictor variables are indicated in the rows, with the dependent variables indicated in the columns.
p < .05,
p < .01,
p < .001.
Exposure to Ebola-related media.
Overall, 72.12% (n = 2484) reported exposure to less than 1 h per day of Ebola-related media; 22.05% (n = 760) 1–3 h per day; and 4.09% (n = 141) more than 4 h per day. Of the sample, 13.52% (n = 466) reported seeing graphic Ebola-related images sometimes, often, or very often. The most common graphic image was bodies of people who died from Ebola (M = 1.78, SD = 0.99). Hours per day of Ebola-related media exposure and exposure to graphic Ebola-related images were weakly positively correlated (r = 0.16, p < .001).
Ebola-related risk perception and fear and worry.
Among the six risk perception items, the highest mean probability was for catching Ebola if “you spend a day working in the same office as someone who has the Ebola virus who is seriously ill” (M = 55.17%; median = 50%, SD = 37.1%). The lowest risk perception was for catching Ebola if “you spend a half hour on a bus or subway car as someone who has the Ebola virus but has no symptoms at all” (M = 21.90%; median = 7%; SD = 28.6%).
On average, participants reported similar low values for “worry that Ebola will personally affect me or someone in my family in the future” (M = 1.56, SD = 0.76) and “how often in the past week have you had fears about the possibility of Ebola affecting you or your family?” (M = 1.48, SD = 0.76). The combined fear and worry score was associated with pre-Ebola outbreak doctor-diagnosed anxiety (b = 0.15, p = .008, 95% CI, 0.04, 0.27) and cumulative mental health ailments (b = 0.09, p = .008, 95% CI, 0.02, 0.16) in bivariate analyses, although not when controlling for other factors in multivariate models.
Behaviors and intentions.
Overall, 45.15% (n = 1555) of participants reported performing at least one health protective behavior, with 7.94% (n = 274) performing two, 3.42% (n = 118) performing three, and 1.84% (n = 63) performing all four. The most common behavior was washing hands or using hand sanitizer more than usual, 43.85% (n = 1510); the least common was wearing a face mask, 4.87%, (n = 168). However, participants were more likely to report intentions to perform these behaviors if they “knew that someone in my area had the Ebola virus,” with 83.99% (n = 2893) reporting that they would perform at least one, 19.37% (n = 667) two, 24.03% (n = 828) three, and 22.72% (n = 782) reporting that they would engage in all four. Table 2 presents logistic regression examining the roles of the two primary independent variables (hours of media exposure and frequency of exposure to graphic images) and two mediators (Ebola-related risk perception and Ebola-related fear and worry) in predicting self-reports of performing or intending to perform each of the four protective behaviors. Ebola-related fear and worry and risk perceptions were strong predictors in almost all cases. Media exposure was a modest predictor in most cases; frequency of exposure to graphic images was only significant for having avoided public places and worn a face mask.
Table 2.
Bivariate predictors of performance and intentions to perform health protective behaviors.
| Performance of Health Protective Behaviors | ||||
|---|---|---|---|---|
| Avoid public places | Wash my hands or use sanitizer more often | Wear a face mask | Avoid public transportation | |
| OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | |
| Risk perception | 1.01 (1.01, 1.02)*** | 1.01 (1.01, 1.01)*** | 1.00 (0.99, 1.01) | 1.01 (1.01, 1.02)*** |
| Ebola-related fear and worry | 1.44 (1.30, 1.61)*** | 1.24 (1.14, 1.34)*** | 1.37 (1.10, 1.57)*** | 1.29 (1.16, 1.42)*** |
| Media exposure | 1.58 (1.17, 2.15)** | 1.26 (1.04, 1.52)* | 1.61 (1.11, 2.34)* | 1.52 (1.12, 2.05)** |
| Graphic images | 1.40 (1.16, 1.70)** | 1.07 (0.95, 1.19) | 1.65 (1.29, 2.10)*** | 1.14 (0.95, 1.37) |
| Intentions to Perform Health Protective Behaviors | ||||
| Avoid public places | Wash my hands or use sanitizer more often | Wear a face mask | Avoid public transportation | |
| OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | |
| Risk perception | 1.02 (1.02, 1.03)*** | 0.99 (0.99, 0.99)* | 1.02 (1.02, 1.02)*** | 1.02 (1.01, 1.02)*** |
| Ebola-related fear and worry | 1.31 (1.20, 1.43)*** | 0.86 (0.80, 0.94)*** | 1.24 (1.13, 1.36)*** | 1.16 (1.07, 1.26)*** |
| Media exposure | 1.25 (1.03, 1.51)* | 0.90 (0.74, 1.10) | 1.41 (1.14, 1.73)** | 1.13 (0.92, 1.37) |
| Graphic images | 1.01 (0.90, 1.13) | 0.94 (0.84, 1.04) | 1.08 (0.96, 1.22) | 1.04 (0.92, 1.17) |
p < .05,
p < .01,
p < .001.
3.2. Path models examining direct and mediator effects on performance and intentions to perform health protective behaviors
The left-hand side of Table 3 presents full results of analyses of the predictive value of the exposure variables (hours per day of media exposure and frequency of exposure to graphic images), mediators (Ebola-related risk perception and fear and worry), and covariates on performance of protective behaviors (SEM 1) and intentions to perform protective behaviors (SEM 2). The right-hand side analyzes the predictive value of the exposure variables and covariates on the mediators.
Table 3.
Direct effects of path models predicting performance of and intentions to perform health protective behaviors (N = 3394)a.
| VARIABLE | Outcome Variables | Mediators | ||||||
|---|---|---|---|---|---|---|---|---|
| SEM 1: Performance of Health Protective Behaviorsb | SEM 2: Intentions to Perform Health Protective Behaviorsb | Ebola-related Risk Perceptions | Ebola-related Worry and Fear | |||||
| b | (95% CI) | b | (95% CI) | b | (95% CI) | b | (95% CI) | |
| Ebola-related Media Exposure | ||||||||
| Hours per Day | 0.04 | −0.09, 0.18 | 0.01 | −0.05, 0.07 | 5.08 | 1.96, 8.21** | 0.30 | 0.22, 0.39*** |
| Graphic Images | 0.08 | 0.01, 0.15* | 0.01 | −0.03, 0.04 | −0.68 | −2.59, 1.22 | 0.11 | 0.06, 0.16*** |
| Mediators | ||||||||
| Ebola-related Risk Perceptions | 0.01 | 0.002, 0.01*** | 0.01 | 0.004, 0.01*** | – | – | – | – |
| Ebola-related Worry and Fear | 0.23 | 0.13, 0.33*** | 0.04 | −0.004, 0.08 | – | – | – | – |
| Covariates | ||||||||
| Prior Mental Health Diagnosis | −0.10 | −0.21, 0.003 | −0.03 | −0.08, 0.02 | 1.57 | −1.06, 4.20 | 0.06 | −0.01, 0.12 |
| Age | 0.00 | 0.00, 0.00 | 0.003 | 0.001, 0.01** | −0.08 | −0.16, 0.01 | 0.00 | 0.00, 0.00 |
| Male genderc | −0.03 | −0.16, 0.10 | −0.07 | −0.13, −0.01* | −3.80 | −6.72, −0.87* | −0.02 | −0.10, 0.05 |
| Income | −0.03 | −0.07, 0.01 | 0.002 | −0.01, 0.02 | −0.85 | −1.63, −0.07* | −0.02 | −0.04, −0.01** |
| College Educationd | −0.23 | −0.40, −0.06** | −0.02 | −0.08, 0.04 | −5.10 | −8.39, −1.80** | −0.11 | −0.18, −0.04** |
| Ethnicitye | ||||||||
| Black | 0.12 | −0.12, 0.36 | 0.08 | −0.03, 0.18 | −5.88 | −11.69, −0.06* | 0.09 | −0.07, 0.25 |
| Hispanic | 0.28 | 0.10, 0.47** | −0.14 | −0.25, −0.03* | 3.28 | −1.88, 8.45 | 0.18 | 0.06, 0.31** |
| Mixed Race/Other, Non-Hispanic | 0.04 | −0.27, 0.34 | 0.05 | −0.08, 0.19 | −0.16 | −6.32, 5.99 | 0.39 | 0.23, 0.55*** |
| Regionf | ||||||||
| Boston | −0.03 | −0.23, 0.18 | −0.11 | −0.19, −0.02* | −4.78 | −8.99, −0.57* | −0.06 | −0.15, 0.02 |
| New York | −0.17 | −0.34, 0.01 | −0.13 | −0.22, −0.05** | −0.87 | −4.99, 3.26 | 0.03 | −0.07, 0.13 |
| Constant | −1.02 | −1.35, −0.68*** | 0.43 | 0.28, 0.59*** | 43.53 | 36.59, 50.46*** | 0.98 | 0.81, 1.14*** |
p < .05,
p < .01,
p < .001.
Ns vary due to missing data.
Results may be interpreted as log odds increases in counts.
Female = 0 (reference group).
Less than college education = 0 (reference group).
White = 0 (reference group).
National sample = 0 (reference group).
Frequency of exposure to graphic images was positively associated with performance of health protective behaviors, as were the two mediator variables: Ebola-related risk perceptions and Ebola-related fear and worry (see Fig. 1 and Table 3). Hours per day of media exposure were indirectly associated with performance of health protective behaviors through both higher Ebola-related risk perceptions and greater Ebola-related fear and worry (see Fig. 1). Exposure to graphic images was also indirectly associated with performance of health protective behaviors through greater Ebola-related fear and worry, suggesting partial mediation (see Fig. 1).
Fig. 1.
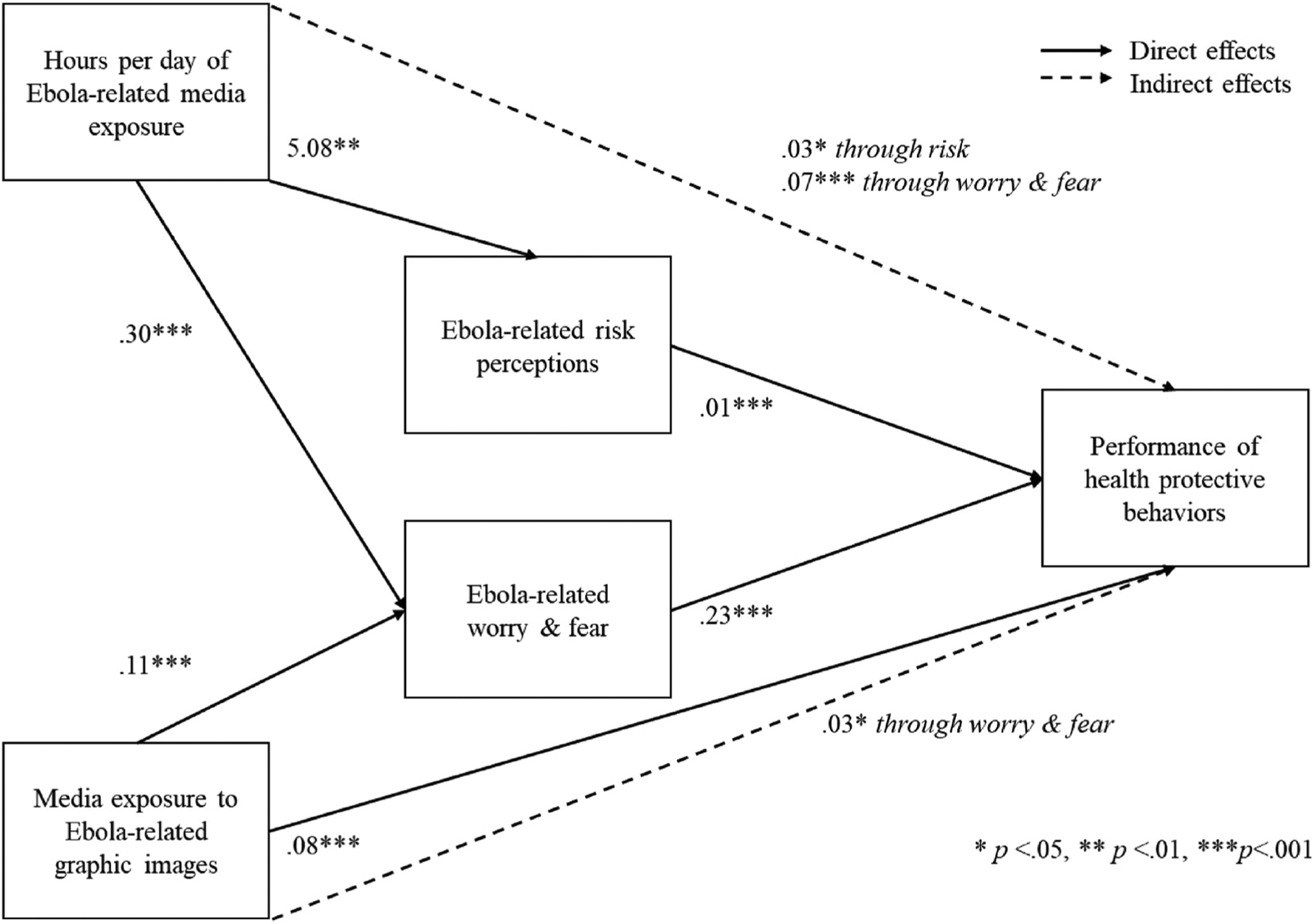
Path model depicting health protective behaviors performed in response to the Ebola virus in the U.S.
Although hours per day of Ebola-related media exposure had no direct effect on behavioral intentions (SEM 2), it did have a significant direct effect on both mediators (see Table 3). As seen in Fig. 2, a significant indirect effect was found between hours per day of Ebola-related media exposure and behavioral intentions through higher Ebola-related risk perceptions. Exposure to Ebola-related graphic images had no direct effects on behavioral intentions or Ebola-related risk perceptions. There was a direct effect of exposure to graphic images on Ebola-related fear and worry.
Fig. 2.
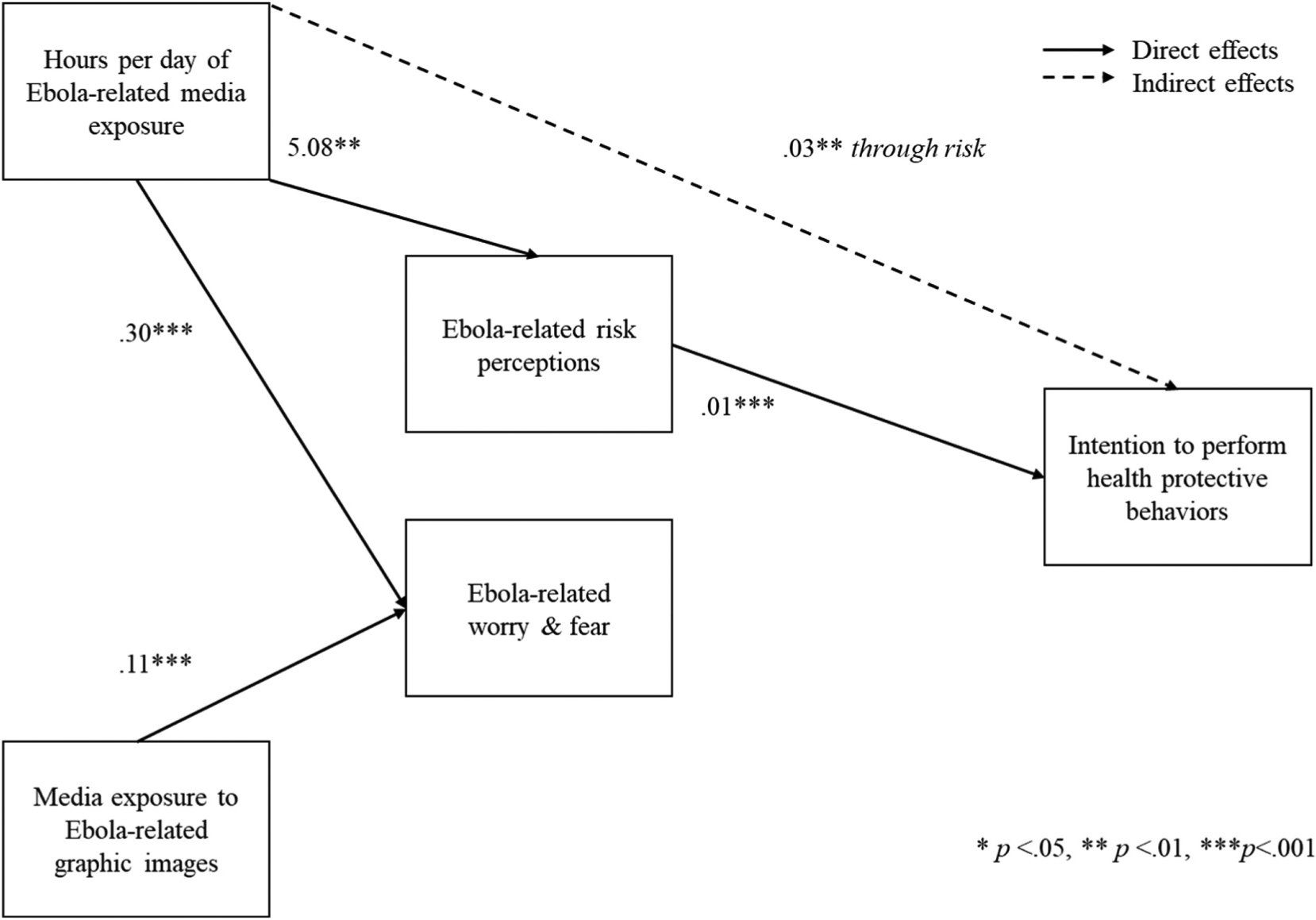
Path model depicting intention to perform health protective behaviors in response to the Ebola virus in the U.S.
Given the significant right skew of the predictor variables (p < .001), all analyses were also run using log transformations. The pattern of results for both SEM 1 and SEM 2 was consistent, except that when using log transformed variables exposure to graphic images did not exhibit a direct effect on behaviors performed (b = 0.08, 95% CI, −0.06, 0.23); the effect sizes were similar and interpretation of all indirect effects remained identical.
Path models were also tested for potential reciprocal relationships between Ebola-related risk perception and Ebola-related fear and worry, as risk and fear and worry may serve as reinforcing processes. The relationship was not significant in either direction, nor did it statistically alter any other paths in the model or improve model fit. Thus, this path was not included in the models.
Finally, exploratory analyses evaluated the potential for curvilinear relationships between media exposure and outcomes by treating media exposure as a three-level categorical variable (less than 1 h, 1–3 h, 4+ hours). As with the continuous variable, the categorical variable did not indicate a direct relationship between hours of media exposure and performance or intention to preform health protective behaviors related to Ebola. However, there was a curvilinear relationship between categorical media exposure and risk perceptions: a significant relationship was found between 1 and 3 h per day of exposure (b = 7.53, 95% CI, 3.96, 11.09) although not 4+ hours per day of exposure (b = 2.14, −7.70, 11.99) when compared to less than 1 h of daily exposure. See Supplemental Table 2 for full results of indirect and direct effects.
4. Discussion
Although the 2014 Ebola outbreak posed little threat in the U.S., almost half of a representative sample of Americans reported performing at least one health protective behavior in response to Ebola, while the great majority said that they would do so if someone in their community were infected with Ebola. Although Ebola was one of the most widely reported stories at the time, only a minority reported spending many hours engaging with Ebola-related media or seeing many graphic images. This is in stark contrast to the high levels of media exposure reported during the early phase of the COVID-19 outbreak, which had an immediate, direct relationship with U.S. residents’ mental health [38]. Another major difference in the experiences is the high transmissibility of COVID-19, which resulted in severe movement restrictions during the outbreak that impacted daily life, leading to more time spent online and increased media consumption [48].
We found that both cognitive (risk perception) and affective (fear) processes mediated the link between media exposure and health protective behaviors. As expected, people who reported more media exposure also reported greater perceptions of risk, which, in turn, predicted more health protective behavior. Risk perceptions also mediated the association between amount of Ebola-related media exposure and intentions to perform health protective behaviors. This was the only significant path in the SEM model predicting those intentions. Fear and worry mediated associations between both the amount and the content of media exposure and protective behaviors, consistent with prior research on fear-based reactions to health threats [31,33]. Contrary to our hypotheses, fear and worry did not mediate the associations between media exposure and intentions to perform health protective behaviors. Perhaps those affective responses tended to govern immediate action, while cognitive responses tended to govern intentions to act if the threat increased (i.e., someone in close proximity becoming infected with Ebola). Also notable, some of the health protective behaviors assessed (i.e., washing hands, hand sanitizing) were both low effort and good public health practices generally, supporting the notion that people perform health protective behaviors based on external cues (e.g., media exposure) when the required effort is low and the perceived response efficacy high.
4.1. Graphic media exposure
Our results found exposure to graphic images was associated with protective behaviors performed through worry and fear but not risk. Prior research has found that viewing graphic images is associated with greater distress in response to terrorism [40,49]. While risk judgments exhibit reciprocal relationships with affective states [50,51], graphic images appeared to target primarily an emotional response. Such images can evoke adaptive affective responses, such as disgust, promoting avoidance of danger [52]. These affective responses target automatic fear-based processes in the amygdala, which have been found to precede and operate independent of cognitive processes, including perceptions of risk [53]. Thus, graphic images may elicit an affective response (e.g., fear and worry), but not necessarily a cognitive one.
4.2. Amount of media exposure
We found higher risk perceptions among people who reported greater media exposure, consistent with prior research, suggesting that sensationalized media coverage [54,55] can amplify health risks for low-probability, high-consequence threats like Ebola [56]. By enhancing the availability of negative events [57], even accurate reporting of population-level risk can lead to exaggerated perception of personal risk [58], as previously found for infectious diseases [56]. Protective behaviors based on such exaggerated perceptions could be rational, but unwarranted. Our results show some evidence of an over-saturation effect of media exposure on risk perception, whereby the highest amounts of exposure were not associated with protective behavior through risk perceptions. However, given the small sample size in the highest group, we cautiously interpret this finding and suggest it as an area for future research. Finally, we note evidence that a substantial minority of U.S. residents may have had their perceptions of risk and resulting behaviors influenced by incorrect knowledge about Ebola transmission: 24.5% of U.S. residents incorrectly stated Ebola was spread through airborne droplets [59]. Indeed, since knowledge and attitudes, in addition to risk perception, were associated with protective behaviors during COVID-19 [60], such factors should be integrated in future research on the impact of media exposure on health protective behavior during viral outbreaks and other threats.
The link between amount of media exposure and fear and worry is consistent with previous studies regarding the Boston Marathon bombings and other collective trauma [39,61,62]. This may be due to activation of fear circuitry in the brain [63], which then leads to the maintenance of ruminative processes such as ongoing fear and worry. Data suggest these thought patterns can lead to anxiety [64] and motivated avoidance to reduce this anxiety [65]: health protective behaviors may serve as an active coping method to alleviate this fear-related distress [66].
4.3. Implications for promoting public health
It may be advantageous to capitalize on these cognitive and affective processes to promote health protective behaviors during public health crises. Mathematical models suggest that fear-inspired flight can encourage social distancing and other behaviors that may help reduce disease spread [67]. Graphic images, in particular, can be utilized to promote adaptive behaviors. This has been effectively employed in prior public health campaigns: for example, cigarette warning labels that contain graphic images have been linked with emotional responses including fear and disgust that predict subsequent smoking cessation [68]; warnings that elicit strong emotional reactions may be particularly effective at promoting positive anti-smoking behavior [31,69]. Measured incorporation of graphic images to promote health protective behaviors during critical outbreaks may help minimize the impact of epidemics. This may be particularly true when trying to elicit higher effort behavior, such as vaccination during COVID-19 and other viral outbreaks (e.g., seasonal influenza): effective communication strategies are critical given the high degree of vaccine hesitancy in the U.S. and elsewhere [70]. Future research should explore the efficacy of incorporating such imagery into public health messaging.
Nonetheless, the benefits of capitalizing on the media to elicit affective and cognitive responses should be cautiously weighed against the potential for triggering unnecessary distress throughout the population. During a low-threat situation, these affective responses could lead to distress, fear, and anxiety that could negatively impact psychological and physical health [71,72], overburden healthcare facilities [37], or lead to maladaptive responses [73]. Our results show some evidence of this phenomenon: some participants reported high risk perceptions for activities such as riding in a bus or sharing an office space, although Ebola is generally spread through bodily fluid and contact with dead bodies [74]. Yet since Ebola is also spread (albeit to a lesser degree) through fomites, hand hygiene (the most frequently performed behavior) is a rational and potentially effective way to prevent Ebola contraction, and is particularly useful to engage in since it is a low effort behavior. Thus, it may be advantageous to judiciously utilize images in the highest threat circumstances to avoid saturation, “wear out effects,” or engagement in behaviors that are not necessary. “Wear out effects,” in particular, can occur when messages promote health protective behavior initially and then decline in effectiveness [75]. This has occurred during the COVID-19 pandemic, as evidenced by reports of “pandemic burnout” [76], potentially leading to decreased health protective behavior.
4.4. Limitations
Our study has a large, representative sample, with measures of pre-event mental health and other demographic variables that provided relevant covariates. One potential limit is combining traditional and social media, which may have differential effects on outcomes [77] and exposure [78]. For example, after the Boston Marathon bombings, older individuals tended to obtain information regarding the bombings from traditional media, while younger individuals used social media more often than older adults [78]. Although we drew from an ongoing longitudinal study, our primary analyses were cross-sectional. We were not able to test these relationships with longitudinal data, using intentions as a potential mediator for subsequent behaviors [79]. Without such observations, we cannot fully parse directionality. As noted by Weinstein and Nicholich [80], health protective behaviors may reflect higher initial risk perceptions and lead to lower ones. Similarly, people with higher fear, worry, and risk perceptions may have sought more media exposure, which could, in turn, heighten those responses [81]. As noted in the introduction, although we treat risk perceptions as primarily cognitive and fear/worry as primarily affective, the two interact, with emotions and beliefs informing one another [58, 82]. Nonetheless, as suggested by prior authors [28], we were able to assess both cognitive and affective processes concurrently in the context of a public health epidemic. This is important as meta-analytic findings have indicated that appeals targeting multiple processes at once tend to exhibit stronger effect sizes [29]. While we were able to test key constructs in theories of health protective behavior, we could not test them all (e.g., self-efficacy, social norms). Although we pretested our measures extensively, we did not conduct the kind of mixed-methods study needed to elucidate the reasons that people give for their decisions regarding these behaviors and intentions.
5. Conclusions
Our findings provide a picture of how the amount and type of media exposure can influence the cognitive and affective responses that shape intended and actual health protective behaviors during a highly publicized public health crisis. The effect of amount of media exposure (hours per day) was mediated by both cognitive and affective processes; the effect of type of exposure (graphic images) was mediated affectively. With the ever-present social media and 24/7 news coverage of health emergencies, understanding these processes is essential to securing appropriate health protective behavioral responses during public health crises [83,84]. These media can provide vital information and stimulate psychological responses that motivate engagement in health protective behaviors. However, they can also distort perceptions of risk and create unwarranted fear and worry [15,85]. Employing media effectively means addressing both cognitive and affective processes. Moreover, it must be done so in a way that promotes positive health protective action without over-activating the psychological stress response. This is a delicate, yet critical, risk communication task during large-scale public health crises.
Supplementary Material
Acknowledgments
This work was funded by National Science Foundation grants SBE 1760764 Drs. Roxane Cohen Silver, E. Alison Holman, and Mansour Fahimi. Dr. Dana Rose Garfin was supported by National Institute of Health K01 MD013910.
Footnotes
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Appendix A. Supplementary data
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ijdrr.2022.103059.
References
- [1].Hamel L, Firth J, Brodie M, Kaiser Health Policy News Index: Special Focus on Ebola, 2014. http://kff.org/global-health-policy/poll-finding/kaiser-health-policy-news-index-special-focus-on-ebola/.
- [2].Sahni B, Yadav AK, Bala K, Jena PK, Kumar D, Basic reproduction number (R naught) and case fatality rate of COVID-19: a Conceptual Approach, J. Clin. Diagn. Res 2 (2020) 1–5, 10.7860/jcdr/2020/45502.14054. [DOI] [Google Scholar]
- [3].WHO Ebola Response Team, Ebola virus disease in West Africa — the first 9 months of the epidemic and forward projections, N. Engl. J. Med 371 (2014) 1481–1495, 10.1056/NEJMoa1411100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Sullivan M, Journalism in the Time of Ebola, New York Times, 2014. [Google Scholar]
- [5].Gui X, Kou Y, Pine KH, Chen Y, Managing uncertainty: using social media for risk assessment during a public health crisis, in: Conference on Human Factors in Computing Systems - Proceedings, 2017-May(June 2018), 2017, pp. 4520–4533, 10.1145/3025453.3025891.. [DOI] [Google Scholar]
- [6].Ball-Rokeach SJ, DeFleur ML, A dependency model of mass-media effects, Commun. Res 3 (1) (1976) 3–21, 10.1177/009365027600300101. [DOI] [Google Scholar]
- [7].Jung J, Media dependency theory, in: The International Encyclopedia of Media Effects, 2017, 10.1002/9781118783764.wbieme0063. [DOI] [Google Scholar]
- [8].Sell TK, Hosangadi D, Trotochaud M, Misinformation and the US Ebola communication crisis: analyzing the veracity and content of social media messages related to a fear-inducing infectious disease outbreak, BMC Publ. Health 20 (1) (2020) 1–10, 10.1186/s12889-020-08697-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Sell TK, Boddie C, McGinty EE, Pollack K, Smith KC, Burke TA, Rutkow L, Media messages and perception of risk for Ebola virus infection, United States, Emerg. Infect. Dis 23 (1) (2017) 108–111, 10.3201/eid2301.160589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Muñiz C, Media system dependency and change in risk perception during the COVID-19 pandemic, Tripod 1 (47) (2020) 11–26, 10.51698/tripodos.2020.47p11-26. [DOI] [Google Scholar]
- [11].Fischhoff B, Wong-Parodi G, Garfin DR, Holman EA, Silver RC, Public understanding of Ebola risks: mastering an unfamiliar threat, Risk Anal. 38 (1) (2018) 71–83, 10.1111/risa.12794. [DOI] [PubMed] [Google Scholar]
- [12].Glik DC, Risk communication for public health emergencies, Annu. Rev. Publ. Health 28 (2007) 33–54, 10.1146/annurev.publhealth.28.021406.144123. [DOI] [PubMed] [Google Scholar]
- [13].Dillard J, Yang C, Personal, interpersonal, and media predictors of fear of Ebola, J. Int. Crisis Risk Commun. Res 2 (2) (2019) 181–206, 10.30658/jicrcr.2.2.2. [DOI] [Google Scholar]
- [14].Thompson RR, Garfin DR, Holman EA, Silver RC, Distress, worry, and functioning following a global health crisis: a national study of Americans’ responses to Ebola, Clin. Psychol. Sci 5 (3) (2017) 513–521, 10.1177/2167702617692030. [DOI] [Google Scholar]
- [15].Garfin DR, Silver RC, Holman EA, The Novel Coronavirus (COVID-2019) Outbreak: Amplification of Public Health Consequences by Media Exposure, Health Psychology, 2020, 10.1037/hea0000875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Matrajt L, Leung T, Evaluating the Effectiveness of Social Distancing Interventions to Delay or Flatten the Epidemic Curve of Coronavirus Disease, Emerging Infectious Diseases, 2020, 10.3201/eid2608.201093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Sheeran P, Maki A, Montanaro E, Avishai-Yitshak A, Bryan A, Klein WMP, Miles E, Rothman AJ, The impact of changing attitudes, norms, and self-efficacy on health-related intentions and behavior: a meta-analysis, Health Psychol. (2016), 10.1037/hea0000387. [DOI] [PubMed] [Google Scholar]
- [18].Hochbaum G, Public participation in medical screening programs: a socio-psychological study (No. 572), in: US Department of Health, Education, and Welfare, Public Health Service, Bureau of State Services, Division of Special Health Services, Tuberculosis Program, 1958. [Google Scholar]
- [19].Ajzen I, The theory of planned behavior, Organ. Behav. Hum. Decis. Process 50 (2) (1991) 179–211, 10.1016/0749-5978(91)90020-T. [DOI] [Google Scholar]
- [20].Armitage CJ, Conner M, Social cognition models and health behaviour: a structured review, Psychol. Health 15 (2) (2000) 173–189, 10.1080/08870440008400299. [DOI] [Google Scholar]
- [21].Maddux JE, Rogers RW, Protection motivation and self-efficacy: a revised theory of fear appeals and attitude change, J. Exp. Soc. Psychol 19 (5) (1983) 469–479, 10.1016/0022-1031(83)90023-9. [DOI] [Google Scholar]
- [22].Champion VL, Skinner CS, The health belief model, Health Behav. Health Educ.: Theor. Res. Practice 4 (45–65) (2008). [Google Scholar]
- [23].Yzer M, Theory of reasoned action and theory of planned behavior, in: The International Encyclopedia of Media Effects, 2017, 10.1002/9781118783764.wbieme0075. [DOI] [Google Scholar]
- [24].Ho SS, Liao Y, Rosenthal S, Applying the theory of planned behavior and media dependency theory: predictors of public pro-environmental behavioral intentions in Singapore, Environ. Commun 9 (1) (2015) 77–99, 10.1080/17524032.2014.932819. [DOI] [Google Scholar]
- [25].Ranjit YS, Shin H, First JM, Houston JB, COVID-19 protective model: the role of threat perceptions and informational cues in influencing behavior, J. Risk Res 24 (3–4) (2021) 449–465, 10.1080/13669877.2021.1887328. [DOI] [Google Scholar]
- [26].Lobb AE, Mazzocchi M, Traill WB, Modelling risk perception and trust in food safety information within the theory of planned behaviour, Food Qual. Prefer 18 (2) (2007) 384–395, 10.1016/j.foodqual.2006.04.004. [DOI] [Google Scholar]
- [27].Yzzer M, Reasoned Action Theory, The SAGE Handbook of Persuasion: Developments in Theory and Practice, 2017, pp. 1–7. [Google Scholar]
- [28].Liao Q, Cowling BJ, Lam WWT, Ng DMW, Fielding R, Anxiety, worry and cognitive risk estimate in relation to protective behaviors during the 2009 influenza A/H1N1 pandemic in Hong Kong: ten cross-sectional surveys, BMC Infect. Dis 14 (1) (2014) 169, 10.1186/1471-2334-14-169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Sheeran P, Harris PR, Epton T, Does heightening risk appraisals change people’s intentions and behavior? A meta-analysis of experimental studies, Psychol. Bull 140 (2) (2014) 511–543, 10.1037/a0033065. [DOI] [PubMed] [Google Scholar]
- [30].Consedine NS, Moskowitz JT, The role of discrete emotions in health outcomes: a critical review, Appl. Prev. Psychol 12 (2) (2007) 59–75, 10.1016/j.appsy.2007.09.001. [DOI] [Google Scholar]
- [31].Hammond D, Health warning messages on tobacco products: a review, Tobac. Control 20 (5) (2011) 327–337, 10.1136/tc.2010.037630. [DOI] [PubMed] [Google Scholar]
- [32].Hollands GJ, Marteau TM, The impact of using visual images of the body within a personalized health risk assessment: an experimental study, Br. J. Health Psychol 18 (2) (2013) 263–278, 10.1111/bjhp.12016. [DOI] [PubMed] [Google Scholar]
- [33].Dillard JP, Anderson JW, The role of fear in persuasion, Psychol. Market 21 (11) (2004) 909–926, 10.1002/mar.20041. [DOI] [Google Scholar]
- [34].Chang HJ, Huang N, Lee CH, Hsu YJ, Hsieh CJ, Chou YJ, The impact of the SARS epidemic on the utilization of medical Services: SARS and the fear of SARS, Am. J. Publ. Health 94 (4) (2004) 562–564, 10.2105/AJPH.94.4.562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Frewer LJ, Miles S, Marsh R, The media and genetically modified foods: evidence in support of social amplification of risk, Risk Anal 22 (4) (2002) 701–711, 10.1111/0272-4332.00062. [DOI] [PubMed] [Google Scholar]
- [36].Gore ML, Siemer WF, Shanahan JE, Schuefele D, Decker DJ, Effects on risk perception of media coverage of a black bear-related human fatality, Wildl. Soc. Bull 33 (2) (2005) 507–516, 10.2193/0091-7648(2005)33[507:EORPOM]2.0.CO;2. [DOI] [Google Scholar]
- [37].Bernstein KT, Ahern J, Tracy M, Boscarino JA, Vlahov D, Galea S, Television watching and the risk of incident probable posttraumatic stress disorder: a prospective evaluation, J. Nerv. Ment. Dis 195 (1) (2007) 41–47, 10.1097/01.nmd.0000244784.36745.a5. [DOI] [PubMed] [Google Scholar]
- [38].Alison Holman E, Thompson RR, Garfin DR, Silver RC, The unfolding COVID-19 pandemic: a probability-based, nationally representative study of mental health in the U.S, Sci. Adv 5390 (2020), eabd5390, 10.1126/sciadv.abd5390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Alison Holman E, Garfin DR, Silver RC, Media’s role in broadcasting acute stress following the Boston Marathon bombings, Proc. Natl. Acad. Sci. USA 111 (2014) 93–98, 10.1073/pnas.1316265110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Ahern J, Galea S, Resnick H, Television images and psychological symptoms after the September 11 terrorist attacks, Psychiatry 65 (4) (2002), 10.1521/psyc.65.4.289.20240. [DOI] [PubMed] [Google Scholar]
- [41].United States Census Bureau, American Community Survey (ACS), 2012.
- [42].U.S. Department of Health and Human Services, National Center for Health Statistics: National Health Interview Survey Questionnaire 2000, U.S. Department of Health and Human Services, 2001. [Google Scholar]
- [43].Silver RC, Holman EA, McIntosh DN, Poulin M, Gil-Rivas V, Nationwide longitudinal study of psychological responses to September 11, JAMA 288 (10) (2002) 1235–1244. [DOI] [PubMed] [Google Scholar]
- [44].Kline RB, Principles and Practice of Structural Equation Modeling (Second), The Guliford Press, 2005. [Google Scholar]
- [45].Zhao X, Lynch JG Jr., Chen Q, Reconsidering baron and kenny: myths and truths about mediation analysis, J. Consum. Res 37 (2) (2010) 197–206, 10.1086/651257. [DOI] [Google Scholar]
- [46].Bollen KA, Tueller S, Oberski D, Issues in the structural equation modeling of complex survey data (2013), in: Proceedings of the 59th World Statistics Congress. Hong Kong, 2013, http://www.statistics.gov.hk/wsc/STS010-P1-S.pdf. [Google Scholar]
- [47].Gunzler D, Chen T, Wu P, Zhang H, Introduction to mediation analysis with structural equation modeling, Shanghai Arch. Psychiatr 25 (6) (2013) 390–394, 10.3969/j.issn.1002-0829.2013.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [48].Christie A, Brooks JT, Hicks LA, Sauber-Schatz EK, Yoder JS, Honein MA, Guidance for implementing COVID-19 prevention strategies in the context of varying community transmission levels and vaccination coverage, MMWR. Morbid. Mortal. Wkly. Rep 70 (30) (2021) 1044–1047, 10.15585/mmwr.mm7030e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [49].Alison Holman E, Garfin DR, Lubens P, Silver RC, Media Exposure to Collective Trauma, Mental Health, and Functioning: Does it Matter what You See? Clinical Psychological Science, 2019. [Google Scholar]
- [50].Kobbeltvedt T, Wolff K, The Risk-as-feelings hypothesis in a Theory-of-planned-behaviour perspective, Judgment Decis. Making 4 (7) (2009) 567–586. [Google Scholar]
- [51].Slovic P, Finucane ML, Peters E, MacGregor DG, Risk as analysis and risk as feelings, Risk Anal. 24 (2) (2004). [DOI] [PubMed] [Google Scholar]
- [52].Olatunji BO, Disgust: characteristic features, social manifestations, and clinical implications, J. Soc. Clin. Psychol 24 (7) (2005) 932–962. [Google Scholar]
- [53].Phelps EA, Emotion and cognition: insights from studies of the human amygdala, Annu. Rev. Psychol 57 (2006) 27–53, 10.1146/annurev.psych.56.091103.070234. [DOI] [PubMed] [Google Scholar]
- [54].Wahlberg AE, Sjöberg L, Risk perception and the media, J. Risk Res 3 (1) (2000) 31–50, 10.1080/136698700376699. [DOI] [Google Scholar]
- [55].Wilson K, Code C, Dornan C, Ahmad N, Hébert P, Graham I, The reporting of theoretical health risks by the media: Canadian newspaper reporting of potential blood transmission of Creutzfeldt-Jakob disease, BMC Publ. Health 4 (2004) 1, 10.1186/1471-2458-4-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [56].Young ME, King N, Harper S, Humphreys KR, The influence of popular media on perceptions of personal and population risk in possible disease outbreaks, Health Risk Soc. 15 (1) (2013) 103–114, 10.1080/13698575.2012.748884. [DOI] [Google Scholar]
- [57].Tversky A, Kahneman D, Availability: a heuristic for judging frequency and probability, Cognit. Psychol (1973), 10.1016/0010-0285(73)90033-9. [DOI] [Google Scholar]
- [58].Slovic P, Peters E, Risk perception and affect, Curr. Dir. Psychol. Sci 15 (6) (2006) 322–325, 10.1177/03063127067078012. [DOI] [Google Scholar]
- [59].Gesser-Edelsburg A, Shir-raz Y, Mph SH, Lev OS, The public’s risk perceptions regarding the current Ebola outbreak in an as-yet unaffected country, Am. J. Infect. Control 43 (7) (2015) 669–675, 10.1016/j.ajic.2015.03.005. [DOI] [PubMed] [Google Scholar]
- [60].Garfin DR, Fischhoff B, Holman EA, Silver RC, Risk perceptions and health behaviors as COVID-19 emerged in the United States: results from a probability-based nationally representative sample, J. Exp. Psychol. Appl 27 (4) (2021) 584–598, 10.1037/xap0000374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [61].Pfefferbaum B, Nixon S, Tivis RD, Doughty DE, Pynoos RS, Gurwitch Robin H., Foy DW, Television exposure in children after a terrorist incident, Psychiatry 64 (3) (2001) 202–211, 10.1521/psyc.64.3.202.18462. [DOI] [PubMed] [Google Scholar]
- [62].Silver RC, Holman E, Andersen J, Poulin M, Mcintosh D, Gil-Rivas V, Mental- and physical-health effects of acute exposure to media images of the September 11, 2001, attacks and the Iraq War, Psychol. Sci 24 (2013) 1623–1634, 10.1177/0956797612460406. [DOI] [PubMed] [Google Scholar]
- [63].Bourne C, Mackay CE, Holmes EA, The neural basis of flashback formation: the impact of viewing trauma, Psychol. Med 43 (2013) 1521–1532, 10.1017/S0033291712002358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [64].Gana K, Martin B, Canouet MD, Worry and anxiety: is there a casual relationship? Psychopathology 34 (2001) 221–229. [DOI] [PubMed] [Google Scholar]
- [65].Borkovec TD, Inz J, The nature of worry in generalized anxiety disorder: a predominance of thought activity, Behav. Res. Ther 28 (2) (1990) 153–158, 10.1016/0005-7967(90)90027-G. [DOI] [PubMed] [Google Scholar]
- [66].Cohen F, Lazarus RS, Active coping processes, coping dispositions, and recovery from surgery, Psychosom. Med 35 (5) (1973) 375–389. [DOI] [PubMed] [Google Scholar]
- [67].Epstein JM, Parker J, Cummings D, Hammond RA, Coupled Contagion Dynamics of Fear and Disease: Mathematical and Computational Explorations, PLoS ONE, 2008, 10.1371/journal.pone.0003955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [68].Hammond D, Fong GT, McDonald PW, Brown KS, Cameron R, Graphic Canadian cigarette warning labels and adverse outcomes: evidence from Canadian smokers, Am. J. Publ. Health 94 (2004) 1442–1445, 10.2105/AJPH.94.8.1442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [69].Noar SM, Hall MG, Francis DB, Ribisl KM, Pepper JK, Brewer NT, Pictorial Cigarette Pack Warnings: a Meta-Analysis of Experimental Studies, Tobacco Control, 2015, 10.1136/tobaccocontrol-2014-051978 tobaccocontrol-2014–051978-. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [70].Dror AA, Eisenbach N, Taiber S, Morozov NG, Mizrachi M, Zigron A, Srouji S, Sela E, Vaccine hesitancy: the next challenge in the fight against COVID-19, Eur. J. Epidemiol 35 (8) (2020) 775–779, 10.1007/s10654-020-00671-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [71].Garfin DR, Thompson RR, Holman EA, Acute stress and subsequent health outcomes: a systematic review, J. Psychosom. Res 112 (107–113) (2019), 10.1016/j.jpsychores.2018.05.017. [DOI] [PubMed] [Google Scholar]
- [72].Holman EA, Silver RC, Poulin M, Andersen J, Gil-Rivas V, McIntosh DN, Terrorism, acute stress, and cardiovascular health, Arch. Gen. Psychiatr 65 (1) (2008) 73–80. [DOI] [PubMed] [Google Scholar]
- [73].Wong-Parodi G, Feygina I, Factors influencing (mal) adaptive responses to natural disasters : the case of hurricane matthew, Weather Clim. Soc 10 (4) (2018) 747–768, 10.1175/WCAS-D-17-0138.1. [DOI] [Google Scholar]
- [74].Judson S, Prescott J, Munster V, Understanding Ebola virus transmission, Viruses 7 (2) (2015) 511–521, 10.3390/v7020511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [75].Bornstein RF, Exposure and affect: overview and meta-analysis of research, 1968–1987, Psychol. Bull 106 (2) (1989) 265–289, 10.1037/0033-2909.106.2.265. [DOI] [Google Scholar]
- [76].Mion G, Hamann P, Saleten M, Plaud B, Baillard C, Psychological impact of the COVID-19 pandemic and burnout severity in French residents: a national study, Eur. J. Psychiatr 35 (3) (2021) 173–180, 10.1016/j.ejpsy.2021.03.005. [DOI] [Google Scholar]
- [77].Chan MPS, Winneg K, Hawkins L, Farhadloo M, Jamieson KH, Albarracín D, Legacy and social media respectively influence risk perceptions and protective behaviors during emerging health threats: a multi-wave analysis of communications on Zika virus cases, Soc. Sci. Med 212 (2018) 50–59, 10.1016/j.socscimed.2018.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [78].Jones NM, Garfin DR, Holman EA, Silver RC, Media Use and exposure to graphic content in the week following the Boston Marathon bombings, Am. J. Community Psychol (2016) 47–59, 10.1002/ajcp.12073. [DOI] [PubMed] [Google Scholar]
- [79].Schwarzer R, Models of health behaviour change: intention as mediator or stage as moderator? Psychol. Health 23 (3) (2008) 259–263, 10.1080/08870440801889476. [DOI] [PubMed] [Google Scholar]
- [80].Weinstein ND, Nicolich M, Correct and incorrect interpretations of correlations between risk perceptions and risk behaviors, Health Psychol. (1993), 10.1037/0278-6133.12.3.235. [DOI] [PubMed] [Google Scholar]
- [81].Thompson RR, Jones NM, Holman EA, Silver RC, Media exposure to mass violence events can fuel a cycle of distress, Sci. Adv (2019), 10.1126/sciadv.aav3502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [82].Borkovec TD, Ray WJ, Stober J, Worry: a cognitive phenomenon intimately linked to affective, physiological, and interpersonal behavioral processes, Cognit. Ther. Res 22 (6) (1998) 561–576, 10.1023/A:1018790003416. [DOI] [Google Scholar]
- [83].Korda H, Itani Z, Harnessing social media for health promotion and behavior change, Health Promot. Pract 15–23 (2011), 10.1177/1524839911405850. [DOI] [PubMed] [Google Scholar]
- [84].Luca NR, Suggs LS, Theory and model use in social marketing health interventions, J. Health Commun 730 (January) (2012) 1–21, 10.1080/10810730.2012.688243. [DOI] [PubMed] [Google Scholar]
- [85].Majumder MS, Kluberg S, Santillana M, Mekaru S, Brownstein JS, 2014. Ebola Outbreak: Media Events Track Changes in Observed Reproductive Number, PLOS Current Outbreaks, 2015, pp. 1–6, 10.1371/currents.outbreaks.e6659013c1d7f11bdab6a20705d1e865. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


