Abstract
Background:
The childhood family environment can influence long-term well-being in part by modifying how individuals’ respond to and cope with stress across the lifespan. Theoretical models propose that childhood stress will either exacerbate (stress sensitization) or attenuate (steeling effect) the effects of adult stress on mental health. This study tests whether childhood family stress modifies the association between stressful life events and depressive symptoms in pregnancy and consecutive postpartum periods.
Methods:
A sample of 127 women reported on depressive symptoms after one birth, during a subsequent pregnancy, and postpartum following that birth. Childhood family stress was assessed with the Risky Families Questionnaire. Stressful life events were measured at all three timepoints to capture the number of life events during both pregnancies and between pregnancies.
Results:
Associations between stressful life events and depressive symptoms varied as a function of childhood family stress. At the between-persons level, more stressful life events were associated with greater depressive symptoms among women who reported infrequent exposure to childhood family stress in this sample, but not among women who reported more frequent exposure to childhood family stress.
Conclusions:
Results provides novel evidence that moderate exposure to childhood family stress may attenuate the association between stressful life events and depressive symptoms in the perinatal period, consistent with a steeling effect. That is, some degree of childhood family stress may promote resilience to perinatal stress. Findings underscore the utility of examining the interaction of risk factors across the lifespan in predicting perinatal mental health.
Keywords: stress, family stress, depressive symptoms, pregnancy, postpartum
Depressive symptoms among women during the perinatal period (pregnancy and postpartum) are prevalent and have adverse implications for long-term maternal health, child development, and family functioning (Gavin et al., 2005; Haight et al., 2019; Meaney, 2018). A life course perspective proposes that maternal mental health during and after pregnancy is influenced by the interaction between risk and protective factors across the lifespan (Bernstein & Merkatz, 2010; Lu & Halfon, 2003), highlighting the importance of childhood experiences in predicting perinatal well-being. Childhood is a developmental period characterized by rapid development of biological stress response systems and heightened sensitivity to the social environment (Gunnar & Hostinar, 2015; Gunnar & Quevedo, 2007) such that experiences in childhood can have enduring effects on responses to stress and risk for mental health problems across the lifespan (Del Giudice et al., 2011; Repetti et al., 2002; Stroud, 2020). For example, the strength of the association between stress and mental health symptoms in adulthood varies as a function of childhood stress (e.g., Seery et al., 2010; Shapero et al., 2015; Stroud et al., 2020). However, the role of childhood stress in modifying the association between stress and mental health symptoms in the perinatal period remains unclear despite strong evidence that childhood stress and stressful life events in the perinatal period increase risk for perinatal depressive symptoms (Ertel et al., 2011; Racine et al., 2021; Yim et al., 2015). The current study utilizes a life course approach to test if childhood family stress modifies the association of stressful life events with depressive symptoms in pregnancy and postpartum.
As one of the primary contexts in which children’s development unfolds, the family environment serves a particularly important role in calibrating responses to stress and risk for mental health problems (del Giudice et al., 2012; Ellis et al., 2017; Repetti et al., 2002). Childhood family environments characterized by high aggression, high conflict, low support, or low warmth has been found to disrupt emotion processing, social competence, and the development of biological stress response systems (Repetti et al., 2002). Theory and evidence diverge, however, in whether such experiences in childhood increase vulnerability or resilience to mental health problems after later stress (Ellis & Boyce, 2008; Hostinar & Gunnar, 2013; Shakiba et al., 2017; Stroud, 2020). The stress sensitization model posits that childhood experiences of stress will increase sensitivity to later stress and increase susceptibility to mental health problems after later stress (Stroud, 2020). Studies consistent with sensitization effects of childhood stress have found that individuals who were exposed to family dysfunction, parental psychopathology, family violence, or abuse in childhood report greater depressive symptoms following recent stressors when compared to individuals who have not experienced childhood stress (see Stroud, 2020 for a review).
Contrasting theories developed from evolutionary psychology and resilience research propose that some early stress exposures, such as exposure to a family environment that is neither highly threatening nor highly supportive (i.e., moderate childhood stress), may increase resistance to later stressful experiences and decrease vulnerability to mental health problems after later stress, referred to as a steeling effect (Ellis et al., 2020; del Giudice et al., 2011; Rutter, 2012; Seery, 2011). Consistent with steeling effects, studies have found that individuals who experienced some stressful life events in childhood were at lower risk for emotional distress after later stress exposure compared to individuals exposed to no early life stress or extreme early life stress (Seery et al., 2010; Shapero et al., 2015). Such evidence from non-pregnant samples indicates that childhood experiences serve a critical role in modifying the association between stress and mental health symptoms across the lifespan by either sensitizing or steeling individuals to adult stress. To date, the role of childhood family stress in modifying associations of stress with depressive symptoms in the perinatal period is unclear. Further investigations in this area are necessary given the implications of perinatal depressive symptoms for long-term child and family health (Meaney, 2018).
In addition to being critical windows whereby maternal stress exposure and depressive symptoms can influence long-term family health, pregnancy and postpartum also represent periods in which childhood experiences are more salient. For example, individuals often draw on memories of childhood, attachment representations, and experiences with caregivers to prepare for parenthood (Aparicio, 2017; Davis & Narayan, 2020; Narayan et al., 2020, 2021). Therefore, childhood family social environment may play a particularly important role in predicting well-being after stress in the perinatal period. Accumulating evidence in recent years has indicates that childhood adversity, such as family dysfunction, abuse, and neglect, predicts lower well-being in the perinatal period (for a review, see Racine et al., 2021). In contrast, other evidence indicates that the perinatal period may be a time of resilience for individuals with a history of childhood family stress in which individuals draw on stress-adapted coping skills and social support to break the cycle of adversity (Atzl et al., 2019a; Chamberlain et al., 2019; Ellis et al., 2020; Davis & Narayan, 2020). Although such evidence highlights the centrality of childhood experiences to perinatal well-being, it remains unclear the extent to which childhood experiences modify associations between perinatal stress and well-being.
To our knowledge, only one study has evaluated the interactive effect of childhood and perinatal stress on psychological distress in the perinatal period. In a community sample of 200 pregnant women, there was a significant interactive effect of early life stress and prenatal intimate partner violence in predicting emotional distress in pregnancy (Tung et al., 2019). Specifically, there was a U-shaped association between harsh parenting and prenatal distress in the context of prenatal intimate partner violence such that moderate levels of harsh parenting in childhood were associated with lower emotional distress compared to low or high levels of harsh parenting among women who experienced intimate partner violence during pregnancy. Conversely, exposure to traumatic violence in childhood, regardless of the level, was associated with greater emotional distress in the context of intimate partner violence. These results suggest differences in steeling and sensitization effects in pregnancy depending on the type of childhood stress, with steeling effects of moderate harsh parenting but sensitization effects of traumatic violence. Additional work is necessary to elucidate whether childhood experiences confer susceptibility or resilience to depressive symptoms in pregnancy and extend examination to the postpartum period.
The Current Study
In a prospective cohort study conducted in a racially and ethnically diverse and mostly low-income sample, we evaluate the interactive effects of childhood family environment and stressful life events in predicting perinatal depressive symptoms across consecutive births. This study focuses centrally on the perinatal period as a key window for long-term family health, as well as a time in which childhood experiences may be especially salient to stress responses and well-being (Davis & Narayan, 2020; Meaney, 2018). Using multilevel modeling, we test whether childhood family environment modifies the association between stressful life events and depressive symptoms in mothers postpartum of one birth, during a subsequent pregnancy, and postpartum of that subsequent birth. Stress is conceptualized as stressors and stress responses, including acute events and chronic conditions that may be interrelated (Epel et al., 2018). Stressful life events encompass one possible form of stressor that can occur in the perinatal period that include events such as death of someone close, loss of a job, and relationship problems. Of note, stressful life events are common in pregnancy and postpartum, with up to 70% of pregnant individuals reporting experiencing at least one stressful life event, and are associated with perinatal depressive symptoms (e.g., Baron et al., 2017; Salm Ward et al., 2017). Family social environment in childhood was evaluated as the mean frequency of exposure to low warmth, low support, high conflict, and high aggression (hereafter, childhood family stress) (Repetti et al., 2002).
We hypothesized that more frequent exposure to family stress in childhood and more perinatal stressful life events would each be associated with greater perinatal depressive symptoms, consistent with prior research (Baron et al., 2017; Ertel et al., 2011; Racine et al., 2021; Yim et al., 2015). However, we predicted that these main effects would be qualified by an interaction between childhood family stress and stressful life events such that the effect of perinatal stress on depressive symptoms will depend on childhood family stress. Prior theory and evidence diverge as to whether childhood stress confers vulnerability or resilience to depressive symptoms after later stress and only one study to our knowledge has tested this in the perinatal period (Tung et al., 2019). Thus, we had no specific hypotheses regarding the manner in which childhood family stress would modify the association between stressful life events and depressive symptoms.
Methods
Journal Article Reporting Standards
We report how we determined our sample size, all data exclusions (if any), all manipulations, and all measures in the study. Study data, materials, and analysis code is available from the first author upon request. The study was not pre-registered.
Participants and Procedure
Participants in this study were enrolled in the multi-site Community Child Health Network (CCHN; conducted from 2007 to 2012) designed to gain insights into the reasons for disparities in maternal and child health that sampled only Hispanic/Latina, Black/African American and non-Hispanic White women. Participants were recruited following a birth (index birth) in five study sites and completed visits postpartum of that birth and through a subsequent pregnancy and postpartum period. Participants who were enrolled at three eligible CCHN study sites were invited to enroll in a follow-up study of the subsequent child’s development. Participants enrolled in the follow-up study completed additional home visits four and five years after the subsequent birth. Further details on CCHN and the follow up study are reported elsewhere (Mahrer et al., 2020; Morgan et al., 2020). The current sample includes all participants enrolled in the follow-up study (n = 127). An overview of study visits is presented in Figure 1. Trained interviewers conducted structured interviews during in-home visits. The study was approved by the Institutional Review Boards at each site. All participants provided written and informed consent and were compensated for study visits.
Figure 1.
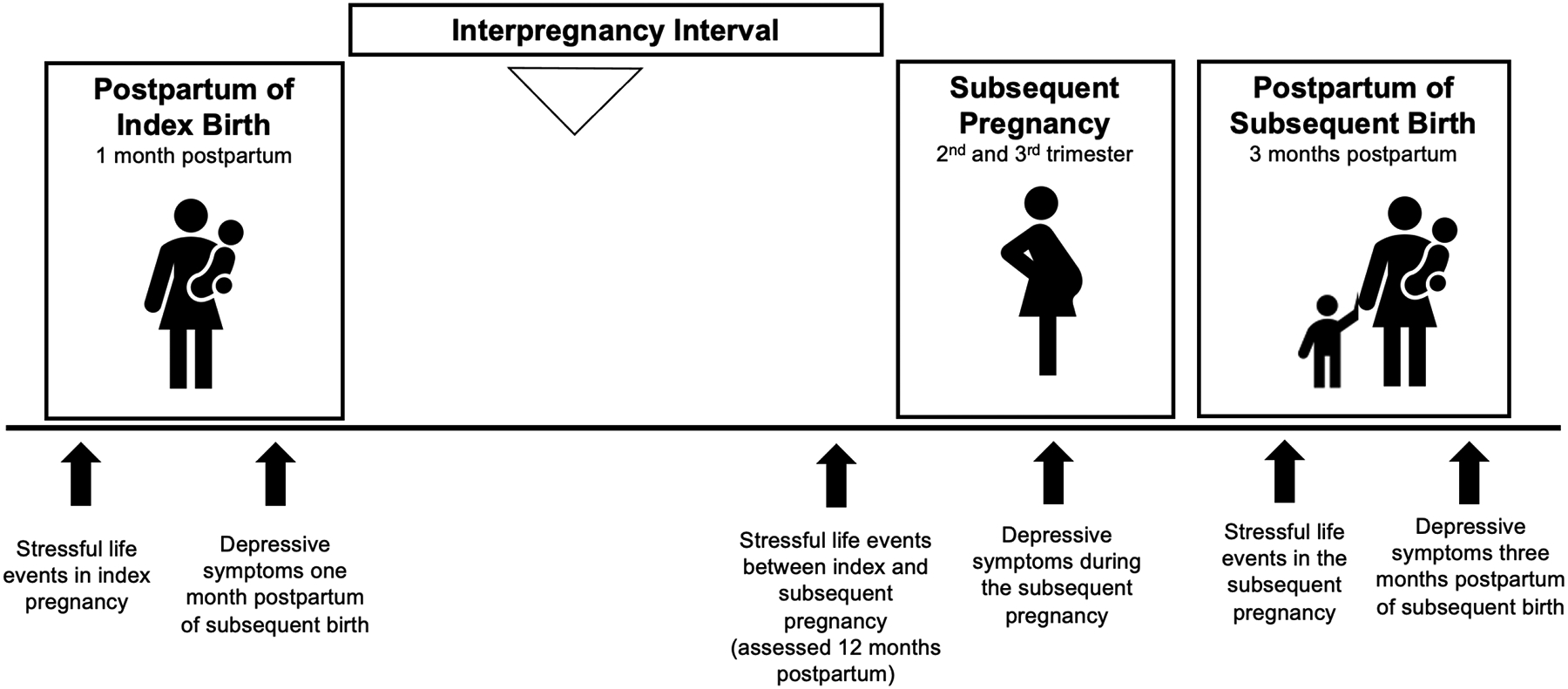
Study Overview
Measures
Sociodemographic and Medical Variables
Participants reported their age, education, household income, household size, racial/ethnic identity, relationship status, and number of previous live births at the time of enrollment in CCHN. Updates to income and relationship status were collected at each study visit. Data on interpregnancy interval was obtained from medical records. Per capita income was calculated as household income divided by household size, adjusted for cost of living in each study site.
Childhood family stress
Participants reported on childhood family stress with the 10-item Risky Families Questionnaire four years following the subsequent birth. This measure assesses childhood family environment and dysfunction between ages 5 and 15 years (Repetti et al., 2002; Taylor et al., 2004; e.g., “how often did a parent or other adult in the household swear at you, insult you, put you down, or act in a way that made you feel threatened?”). Participants reported the frequency of which each item occurred on a scale of 1 (not at all) to 5 (very often). An average of the items was calculated with higher scores indicating a greater mean frequency of exposure to a family social environment characterized by low warmth, low support, high conflict, and/or high aggression. Cronbach’s alpha indicated good reliability in the current sample (α = .88).
Stressful life events
Stressful life events were assessed with the Life Events Inventory at three study visits (Dominguez et al., 2005). Participants retrospectively reported whether or not they had experienced 24 possible life events over a given period at each visit (e.g., “you were threatened with physical harm”, “serious arguments several times with any one person”, “you or someone close had a serious injury, illness, or hospitalization”). These items were used to calculate indices that reflected: (1) the number of life events that occurred in the index pregnancy (reported one month after the index birth); (2) the number of life events that occurred in the interpregnancy interval between the index birth and the subsequent birth (reported 12 months after the index birth); and (3) the number of life events that occurred in the subsequent pregnancy (reported three months after the subsequent birth).
Depressive Symptoms
Two instruments were used to assess maternal depressive symptoms to be appropriate to the time periods administered. The Edinburgh Postpartum Depression Scale (EPDS) was used to assess depressive symptoms during postpartum periods after the index and subsequent births (Cox et al., 1987). The EPDS consists of 10 items that assess severity of depressive symptoms over the past week on a scale of 0 to 3 and is validated for use in the first year postpartum in Spanish and English (Garcia-Esteve et al., 2003). The Center for Epidemiological Studies Depression Scale 9-item version (CES-D) was administered during the second and third trimesters of pregnancy (Santor & Coyne, 1997). The CES-D assesses frequency of symptoms in the past week on a scale of 1 (none of the days) to 4 (most or all days) and is validated for use in pregnancy (Marcus et al., 2003). CES-D scores in the second and third trimester of pregnancy were intercorrelated and scored as an average (r = .53, p < .001). Mean scores were used in analyses. Cronbach’s alpha indicated acceptable reliability for the EPDS (α = .82–.83) and CES-D (α =.75–.86).
There is substantial overlap between the EPDS and CES-D as demonstrated in prior studies in perinatal samples (Tandon et al., 2012). In the current sample, the measures were also positively correlated (r’s = 0.28–0.50, see Table 2). Depressive symptoms were scaled as the proportion of maximum score (POMS) to account for differences in instruments across study visits. POMS scores represent the proportion of the total possible scale score between 0 and 1, with higher scores indicating greater symptoms. This method maintains the proportion of absolute differences between observed response scores and is the recommended scale transformation for longitudinal data (Moeller, 2015).
Table 2.
Descriptive statistics and bivariate correlations of primary study variables
| Variable | M | SD | 1 | 2 | 3 | 4 | 5 | 6 |
|---|---|---|---|---|---|---|---|---|
| 1. Childhood family stress | 1.92 | 0.86 | ||||||
| 2. Stressful life events: Index pregnancy | 2.95 | 2.87 | .17 [−.02, .34] |
|||||
| 3. Stressful life events: Interpregnancy interval | 3.73 | 3.21 | .13 [−.06, .31] |
48** [.32, .61] |
||||
| 4. Stressful life events: Subsequent pregnancy | 2.54 | 2.80 | .27* [.06, .46] |
.43** [.24, .59] |
.58** [.42, .71] |
|||
| 5. Depressive symptoms postpartum index birth (EPDS) | 5.05 | 4.00 | .20 [−.00, .38] |
.12 [−.08, .31] |
.09 [−.11, .28] |
.31** [.09, .50] |
||
| 6. Depressive symptoms subsequent pregnancy (CES-D) | 17.07 | 4.90 | .20* [.00, .38] |
.24* [.04, .42] |
.38** [.19, .54] |
.50** [.32, .64] |
.28** [.07, .46] |
|
| 7. Depressive symptoms postpartum subsequent birth (EPDS) | 4.04 | 4.27 | .21* [.01, .39] |
.12 [−.08, .31] |
.17 [−.03, .35] |
.19 [−.03, .39] |
.31** [.11, .49] |
.50** [.32, .64] |
Note. M and SD are used to represent mean and standard deviation, respectively. Values in square brackets indicate the 95% confidence interval for each correlation.
p < .05.
p < .01.
Data Analytic Plan
We conducted analyses in R Version 3.6.1. Prior to analysis, we examined the primary study variables for normality (skewness < 3; kurtosis < 7) and outliers (> 3 standard deviations from sample mean). We accounted for non-normality by log-transformation and outliers by winsorizing to three standard deviations from the mean. None of the primary study variables violated assumptions of normality. Data included one outlier on depressive symptoms in pregnancy, one outlier on depressive symptoms postpartum of the subsequent birth, three outliers on stressful life events in the index pregnancy, one outlier on stressful life events between pregnancies, and three outliers on stressful life events in the subsequent pregnancy. Results were robust to outliers and did not change with or without winsorization; we present models with outliers winsorized.
Primary Analysis
We tested study hypotheses using multilevel modeling to account for the nested structure of the longitudinal data and repeated assessment of stressful life events and depressive symptoms. Multilevel modeling accounts for repeated measurements within individuals and allows for the examination of both within- and between-person sources of variability in the outcome (Luke, 2019). Focal predictors and covariates were mean centered prior to analysis to ease interpretation of results (Aiken & West, 1991). Childhood family stress was grand mean centered (Level 2). Stressful life events were grand mean centered (Level 2) and centered within each individual (Level 1) to evaluate within- and between-person effects (Snijders & Bosker, 2011). Between-person effects test whether an individual who reports more stressful life events is predicted to report greater depressive symptoms than an individual who reports fewer stressful life events. Within-person effects test whether an individual is predicted to report greater depressive symptoms at study visits when they report more stressful life events than their average number of stressful life events. Models testing interactive effects included two interactive terms to test whether (1) childhood family stress modified the between-person association of stressful life events (average level of stressful life events across participants) with depressive symptoms and (2) childhood family stress modified the within-person association of stressful life events (changes in stressful life events at a given time point relate to an individual’s average level of stressful life events) with depressive symptoms.
Multilevel modeling was conducted with a series of linear mixed models using the lme4 and lmerTest packages in R (Bates et al., 2007; Kuznetsova et al., 2015). To confirm whether multilevel modeling was the most appropriate analysis for the current data, we first ran an unconditional (empty) model to evaluate systematic variability in depressive symptoms at the within- and between-persons level and evaluated the intraclass coefficient (ICC). ICC values reflect nonindependence of observations and the proportion of variation in the outcome explained by between-person variation (Musca et al., 2011), with higher values indicating greater between-person variability. We also tested an unconditional slope model that evaluated the linear effect of time on depressive symptoms, given that time could be an important contributor to depressive symptoms over the study period (study period length M = 4.79 years, SD = 0.53 years) (Bolger & Laurenceau, 2013).
To test primary research questions, we added predictors to the models to test the main and interactive effects of childhood family stress and stressful life events on perinatal depressive symptoms. First, we tested a random intercept model that tested the effect of childhood stress and stressful life events on depressive symptoms to evaluate main effects. We then tested a random intercept model with the within-level and cross-level interaction, which allows for the intercept, but not the slope, to vary across individuals. Finally, we tested a random slope model that included a within- and cross-level interaction. The random slope model extends the random intercept and allows for both the intercept and slope to vary across individuals. We tested both a random intercept and random slope model for theoretical and methodological reasons. Theoretically, it is not only plausible that stress could predict average depressive symptoms across this period but also that the effect of stress on depressive symptoms varies across individuals (Snijders & Bosker, 2011). For example, individuals who report more stressful life events may report higher levels of depressive symptoms on average, but there may be some individuals for whom the associations between stressful life events and depressive symptoms are stronger or weaker. The latter can be captured with random slopes. Methodologically, modeling random slopes is recommended in the context of cross-level interactions as failure to do so may disregard cluster-driven heteroskedasticity and autocorrelation, thereby violating model assumptions and introducing systematic bias in model estimates (see Heisig & Schaeffer, 2018). The best fitting model of the random intercept and random slope model was determined with the log-likelihood ratio test (Snijders & Bosker, 2011). We interpret coefficients from the best fitting model.
We conducted simple effects analyses to probe significant interactions at the mean and one standard deviation above and below the mean of the moderator (Aiken & West, 1991). Additionally, we explored regions of significance using Johnson-Neyman analyses to determine the values of the moderator (childhood family stress) where the relation between stressful life events and depressive symptoms moved from non-significance to significance (Preacher et al., 2006). Significant main effects were interpreted if interactions were not statistically significant (alpha = .05).
Covariates.
Models adjusted for covariates based on potential confounding influences. In primary analysis models, time since start of the study was included as a covariate, as is recommended in multilevel models (Bolger & Laurenceau, 2013). Number of previous live births at time of enrollment (primiparity; no previous live births vs. one or more previous life births) and interpregnancy interval were included as covariates given associations with perinatal depressive symptoms in prior studies. Sociodemographic characteristics of age, education, per capita household income, racial/ethnic identity, and relationship status were evaluated as covariates and included if significantly associated with depressive symptoms at any study visit (α = .05). Participants who were single reported significantly higher depressive symptoms than participants who were not single at each study visit. Higher per capita household income was associated with lower depressive symptoms in the subsequent pregnancy (r = −0.21, p = .04). Thus, all models adjusted for relationship status (dummy coded; married or not married but cohabiting with a partner [partnered] vs. neither married nor cohabiting with a partner [not partnered]), income (mean centered), primiparity (dummy coded; no previous live births vs. one or more previous live births), and interpregnancy interval (mean centered).
Results
Sample description
A complete sample description is presented in Table 1. Mean participant age at enrollment was 26.6 years (SD = 6.1 years). Participants identified as Hispanic/Latina (48.8%), non-Hispanic White (31.5%), and Black/African American (21.3%). The modal level of educational attainment was high school, GED, or technical degree and the mean per capita household income was $15,307 (SD = $18,384). A majority of participants were either married (46.5%) or not married but cohabiting with their partner (30.7%) one month postpartum of the index birth. The index birth was the first birth for half of the participants (51.8%).
Table 1.
Sample Description (n = 127)
| M (SD) or % (n) | |
|---|---|
| Age at enrollment (years) | 26.6 (6.1) |
| Per capita household income ($) | 15,307 (18,384) |
| Interpregnancy interval (months) | 17.6 (13.0) |
| Education level | |
| Less than high school | 22.8 (29) |
| High school/GED/Technical | 40.9 (52) |
| Some college | 10.2 (13) |
| College or higher degree | 22.8 (29) |
| Other | 3.1 (4) |
| Relationship status | |
| Married | 46.5 (59) |
| Cohabiting, not married | 30.7 (38) |
| Single | 23.6 (30) |
| Race/Ethnicity | |
| Hispanic/Latina | 48.8 (62) |
| Non-Hispanic White | 31.5 (40) |
| Black or African American | 21.3 (27) |
| Parity at index birth | |
| First birth | 51.8 (65) |
| Not first birth | 49.6 (63) |
| Study Site | |
| Chicago | 77.2 (98) |
| Washington, D.C. | 14.2 (18) |
| Eastern North Carolina | 8.7 (11) |
Note. Per capita income adjusted for cost of living at each study site. Some percentages do not add to 100 due to missing data.
Descriptive statistics
Table 2 presents descriptive statistics and bivariate associations of primary study variables. On average, participants reported mean frequency of exposure (averaged across all items) to family stress in childhood as occurring “rarely” (M = 1.92, SD = 0.86). Across all items, most of the sample (84%) reported mean frequency of exposure to childhood family stress as “never” or “rarely” whereas 12% reported mean frequency of exposure to childhood family stress as occurring “sometimes” and 4% reported exposure to childhood family stress as occurring “often” or “very often”. Mean levels of exposure to childhood family stress were mostly low with some variation and comparable to levels in other community samples (Felitti et al., 1998; Lehman et al., 2009). Additional information on the frequency of childhood family stress is presented in the Supplemental Materials. Number of stressful life events were similar during the index pregnancy (M = 2.95, SD = 2.87, range = 0–15) and subsequent pregnancy (M = 2.54, SD = 2.80, range = 0–12), but slightly higher during the interpregnancy interval (M = 3.73, SD = 3.21, range = 0–22). Across study visits, between 76.8% to 83.2% of the sample experienced at least one stressful life event, indicating slightly higher rates in the current sample compared to other community samples (e.g., Salm-Ward et al., 2017).
In bivariate associations, more frequent childhood family stress was associated with higher depressive symptoms in the subsequent pregnancy and postpartum of the subsequent birth. More frequent childhood family stress was also positively associated with reporting more stressful life events in pregnancy but was not associated with stressful life events in the index pregnancy or between pregnancies. More stressful life events were associated with greater depressive symptoms at each timepoint (r’s = 0.12–0.38).
Primary analysis
We used multilevel modeling to evaluate the interactive effect of childhood family stress and perinatal stressful life events on depressive symptoms in pregnancy and postpartum. In the unconditional (empty) model, the estimated mean of depressive symptoms across the three timepoints was 0.19 and the ICC indicated that a substantial proportion (19%) of the variation in depressive symptoms was due to variability between-persons. Thus, multilevel modeling is the most appropriate analytic method to account for the nested longitudinal data structure and avoid inflation of the Type I error rate (Musca et al., 2011). In the unconditional slope model evaluating the effect of time on depressive symptoms, we found that time significantly predicted depressive symptoms such that time positively predicted depressive symptoms. Complete coefficients from each model are presented in Table 3.
Table 3.
Mixed Linear Model Results
| Unconditional Model, Intercept Only | Unconditional Model, Linear Effect of Time | Random Intercept Model with Main Effects Only | Random Intercept Model with Main and Interactive Effects | Random Slope Model with Main and Interactive Effects | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| B | SE | 95% CI | B | SE | 95% CI | B | SE | 95% CI | B | SE | 95% CI | B | SE | 95% CI | |
| Fixed Components | |||||||||||||||
| Intercept | 0.190*** | 0.011 | 0.169, 0.212 | 0.173*** | 0.014 | 0.145, 0.200 | 0.198 | 0.028 | 0.145, 0.251 | 0.204*** | 0.027 | 0.151, 0.256 | 0.205*** | 0.027 | 0.153, 0.256 |
| Level 1 | |||||||||||||||
| Stressful life events | −0.002 | 0.007 | −0.016, 0.011 | −0.007 | 0.007 | −0.020, 0.007 | −0.006 | −0.008 | −0.022, 0.009 | ||||||
| Stressful life events x childhood family stress | −0.003 | 0.008 | −0.018, 0.012 | 0.002 | 0.009 | −0.015, 0.021 | |||||||||
| Time | 0.003** | 0.009 | 0.008, 0.044 | 0.032** | 0.010 | 0.012, 0.052 | 0.032** | 0.010 | 0.013, 0.052 | 0.032** | 0.010 | 0.013, 0.050 | |||
| Level 2 | |||||||||||||||
| Stressful life events | 0.017*** | 0.005 | 0.012, 0.052 | 0.018*** | 0.005 | 0.009, 0.027 | 0.018*** | 0.005 | 0.009, 0.027 | ||||||
| Childhood family stress | 0.014 | 0.014 | −0.012, 0.040 | 0.026^ | 0.014 | −0.001, 0.053 | 0.026^ | 0.014 | −0.001, 0.005 | ||||||
| Stressful life events x childhood family stress | −0.011* | 0.005 | −0.020, −0.003 | −0.011* | 0.005 | −0.020, −0.002 | |||||||||
| − 1 SD | 0.028*** | 0.007 | 0.016, 0.041 | 0.028*** | 0.006 | 0.015, 0.041 | |||||||||
| Mean | 0.019*** | 0.005 | 0.009, 0.028 | 0.018*** | 0.005 | 0.009, 0.027 | |||||||||
| + 1 SD | 0.009 | 0.006 | −0.003, 0.020 | 0.008 | 0.006 | −0.003, 0.020 | |||||||||
| Interpregnancy interval | −0.002^ | 0.001 | −0.004, 0.000 | −0.002^ | 0.001 | −0.004, 0.000 | −0.002^ | 0.001 | −0.004, −0.000 | ||||||
| Relationship status | −0.013 | 0.027 | −0.065, 0.039 | −0.018 | 0.027 | −0.069, 0.033 | −0.022 | 0.027 | −0.070, −0.031 | ||||||
| Primiparity | −0.031 | 0.023 | −0.076, 0.014 | −0.025 | 0.023 | −0.070, 0.019 | −0.025 | 0.023 | −0.070, 0.019 | ||||||
| Per capita income | −0.010 | 0.014 | −0.036, 0.016 | −0.011 | 0.013 | −0.036, 0.015 | −0.011 | 0.013 | −0.036, 0.014 | ||||||
| Variance Components | Variance | SD | Variance | SD | Variance | SD | Variance | SD | Variance | SD | |||||
| Intercept | 0.006 | 0.077 | 0.006 | 0.080 | 0.005 | 0.070 | 0.005 | 0.070 | 0.007 | 0.081 | |||||
| Residual | 0.023 | 0.153 | 0.024 | 0.154 | 0.023 | 0.152 | 0.022 | 0.150 | 0.018 | 0.132 | |||||
| Stressful life events | 0.001 | 0.033 | |||||||||||||
| ICC | 0.19 | 0.19 | 0.18 | 0.18 | 0.30 | ||||||||||
| Deviance | −250.53 | −252.54 | −219.42 | −230.73 | −238.01 | ||||||||||
| Log-likelihood ratio test | 7.30*a | ||||||||||||||
p < .10;
p < .05;
p < .01;
p < .001
Log-likelihood ratio test of whether the random slope model significantly improved model fit from the random intercept model.
Note. B = unstandardized coefficient; SE = standard error; CI = confidence interval; ICC = intraclass coefficient. Simple slopes were probed if interaction term was significant. For visual clarity, covariates are not included in the table. Models adjusted for time since study start, primiparity, income, relationship status, and interpregnancy interval. All continuous predictors and covariates were mean centered for ease of interpretation. Stressful life events were centered within cluster (Level 1) and grand mean centered (Level 2).
First, we tested the main effects of childhood family stress and stressful life events on depressive symptoms in the perinatal period. Childhood family stress was not significantly associated with depressive symptoms, but more stressful life events were significantly associated with greater depressive symptoms. When including interactive effects in the model, we found that the random slope model significantly improved model fit from the random intercept model based on the log-likelihood test; therefore, we interpret coefficients from the random slope model. In the random slope model that included main and interactive effects of childhood stress and stressful life events, more frequent exposure to family stress in childhood and more stressful life events were independently associated with greater depressive symptoms in the perinatal period. However, these effects were qualified by a significant between-person interactive effect of childhood family stress and average levels of stressful life events (Level 2) on depressive symptoms such that the association between stressful life events and depressive symptoms varied across individuals depending on childhood family stress at the between-person level.
Simple slopes analyses (Figure 2) revealed that more stressful life events were associated with greater depressive symptoms among individuals who experienced low (Intercept = 0.18, B = 0.028, SE = 0.006, p < .001) or mean (Intercept = 0.20, B = 0.018, SE = 0.005, p < .001) frequency of exposure to childhood family stress in the current sample. Stressful life events were not significantly associated with depressive symptoms among individuals who reported high frequency of exposure to childhood family stress in the current sample (Intercept = 0.22, B = 0.008, SE = 0.006, p = .19). Simple slopes in the current sample corresponded to mean frequency of exposure to childhood stress as never (low), rarely (sample mean), and sometimes (high), respectively. Johnson-Neyman region of significance analyses (Figure 3) indicated that the association between average stressful life events and depressive symptoms was positive and significant for individuals who reported mean frequency of exposure to childhood family stress at a mean centered value less than 0.66 (observed range = −0.93 to 2.67), which corresponded to a mean frequency of less often than “sometimes”.
Figure 2.
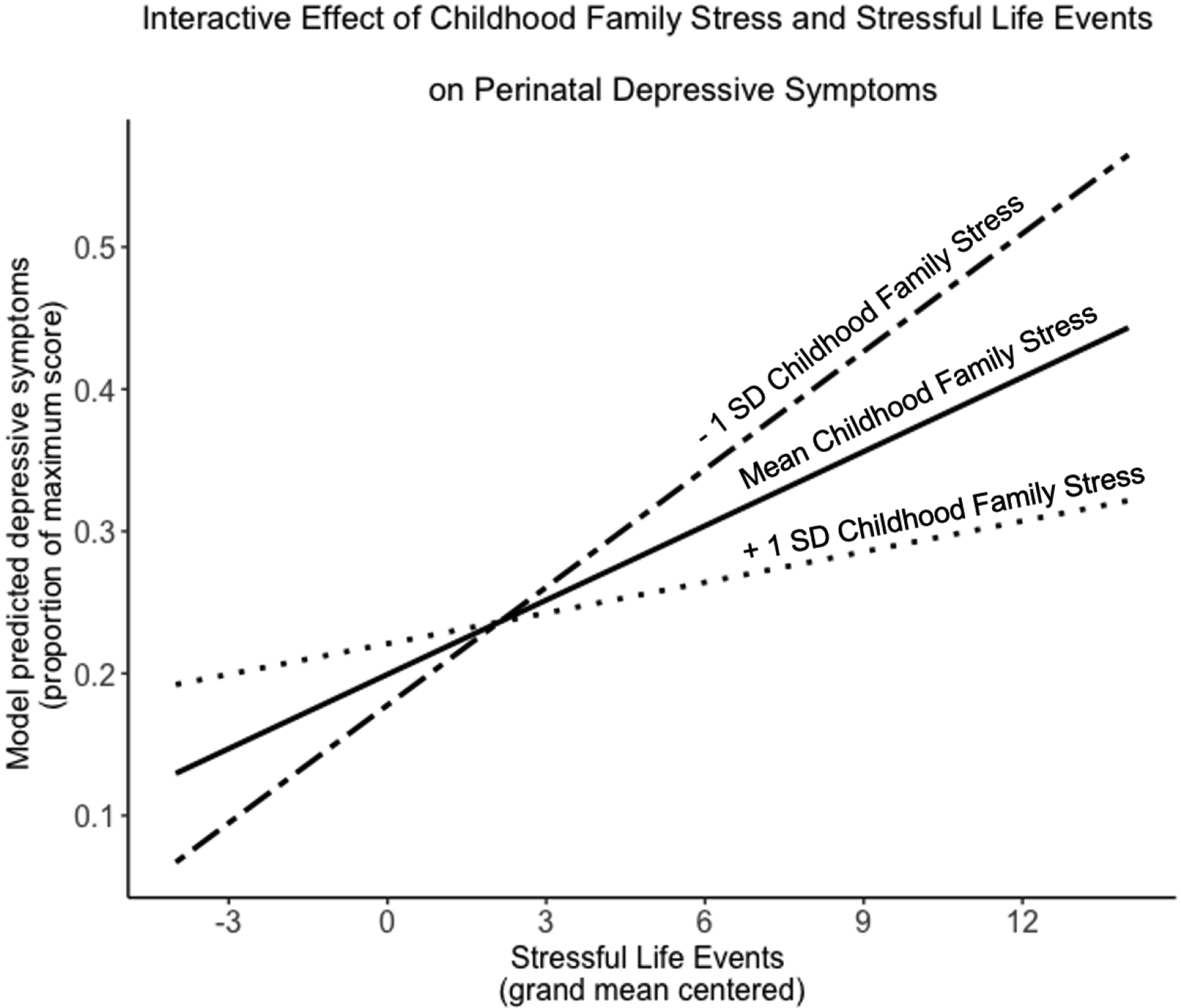
Simple slopes analysis of the association between stressful life events and depressive symptoms by childhood family stress
Figure 3.
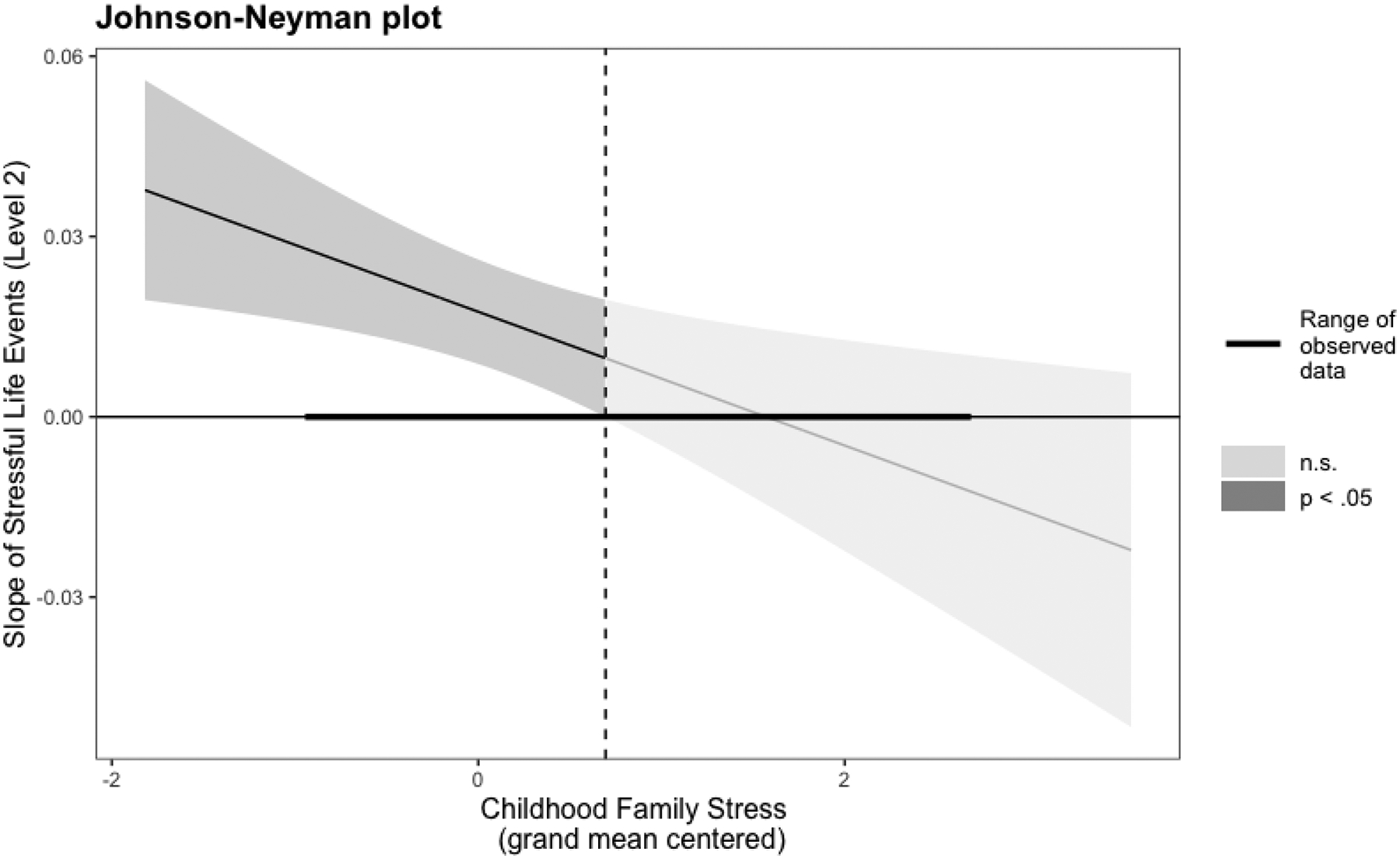
Johnson-Neyman region of significance analyses
Within-person changes in stressful life events were not associated with depressive symptoms nor did association between within-person changes in stressful life events and depressive symptoms vary depending on childhood family stress. That is, depressive symptoms did not vary across study visits as a function of whether stressful life events deviated from an individual’s average levels of stressful life events and frequency of childhood family stress did not modify this association.
Discussion
A life course perspective underscores the importance of the cumulative and interactive effects of risk and resilience factors across the lifespan on maternal mental health during and after pregnancy (Bernstein & Merkatz, 2010; Lu & Halfon, 2003), yet the interactive effects of childhood and perinatal stress on perinatal depressive symptoms are understudied. To our knowledge, this is the first study test childhood family environment as a moderator of the association between stressful life events and depressive symptoms in pregnancy and across consecutive postpartum periods. In the current study, mean frequency of exposure to family stress was low on average but there was considerably variability in the sample. Rates in this sample were also similar to rates of childhood family stress in other community samples (e.g., Felitti et al., 1998; Lehman et al., 2009). Within this context, more frequent exposure to a childhood family environment characterized by low warmth and support and high conflict and dysfunction was associated with greater depressive symptoms in pregnancy and postpartum. More stressful life events in the perinatal period were also independently associated with greater depressive symptoms. However, the association between stressful life events and depressive symptoms was conditional on childhood family stress. More stressful life events were associated with greater depressive symptoms among individuals who reported a never or rarely experiencing childhood family stress. However, stressful life events were not associated with depressive symptoms among individuals who reported experiencing childhood family stress sometimes or more often. These results suggest that moderate levels of family stress in childhood may promote resilience to depressive symptoms in the context of perinatal stress.
The present findings add to small but growing evidence that childhood family experiences play an important role in modifying responses to stress and subsequent risk for depressive symptoms in the perinatal period. This pattern of findings may be consistent with a steeling effect of childhood stress (Rutter, 2012), which refers to evidence that early life stress may serve to increase resistance to later stress thereby reducing vulnerability to depressive symptoms (Seery, 2011; Seery et al., 2010; Shapero et al., 2019). Consistent with the present findings, evidence in non-pregnant samples suggests that the childhood family stress serves an especially important role in calibrating responses to stress across development compared to other forms of stress in childhood (del Giudice et al., 2012; Ellis et al., 2017). In the context of the perinatal period, another recent study reported a steeling effect of moderate levels of harsh parenting in childhood to emotional distress in pregnancy among individuals experiencing prenatal intimate partner violence (Tung et al., 2019). Together with the current results, these findings indicate moderate levels of childhood family stress (e.g., harsh parenting, low parental warmth and support) in particular may contribute to a steeling effect in the context of perinatal stress.
There are several pathways in which moderate childhood family stress could protect against depressive symptoms after stressful life events in the perinatal period. Moderate family stress may promote the development of stress-adapted coping abilities, social skills, and cognitive resources that are advantageous in the face of later stressors (i.e., “hidden talents”; Ellis et al., 2020). The perinatal period has been conceptualized as a potential period of resilience for individuals with a history of early life stress (Davis & Narayan, 2020). Therefore, the perinatal period may be a time in which individuals who experienced childhood stress actively draw on coping skills and social support to break the cycle of adversity (Atzl et al., 2019a; Chamberlain et al., 2019). Moreover, the transition to parenthood may be a time of positive posttraumatic growth and positive social role change for individuals with a history of childhood stress (Aparicio, 2017; Fava et al., 2016). These factors may allow individuals to cope with stressful events in the perinatal period and mitigate risk for depressive symptoms after stressful life events.
This is not to say that more frequent exposure to family stress in childhood is beneficial in all circumstances in pregnancy and postpartum. For example, in the current sample higher family stress in childhood was associated with more stressful life events in pregnancy and postpartum. In this sense, childhood stress may indirectly increase vulnerability to depressive symptoms by contributing to higher levels of stressful life events, potentially through stress generation pathways (Davis & Narayan, 2020; Liu et al., 2013). Furthermore, growing evidence indicates a significant, positive association of childhood family stress with depressive symptoms in pregnancy and postpartum (for a review, see Racine et al., 2021). Consistent with such evidence, childhood stress was positively associated with perinatal depressive symptoms in this sample. Moreover, individuals who reported greater frequency of exposure to childhood family stress had greater depressive symptoms at low levels of perinatal stress as compared to individuals who reported less frequent exposure to childhood family stress. Therefore, this pattern of results suggests that moderate frequency of exposure to family stress may promote resilience to depressive symptoms when faced with later stressful events. Rather than adopting a deficit-focused lens to childhood stress and lifespan mental health, future research should aim to identify the contexts in which early experiences of stress may be resilience-promoting and the pathways through which this might occur.
Resilience is a dynamic concept involving the interaction between multiple systems (Masten, 2018; Masten & Barnes, 2018) and we cannot conclude whether childhood family stress modifies the association between perinatal stress and other health outcomes. While moderate exposure to family stress in childhood may protect again depressive symptoms in the context of perinatal stress, there may be a cost to physiological systems. Skin deep resilience refers to the observation that some individuals who appear to be psychosocially resilient (e.g., more favorable mental health) in the face of stress demonstrate high allostatic load and accelerated epigenetic aging (Brody et al., 2016). For example, childhood stress is associated with dampened cortisol reactivity in pregnancy and postpartum (Epstein et al., 2021). Dampened cortisol reactivity may protect against depressive symptoms in the context of perinatal stress but can hold adverse implications for health behaviors and physical health outcomes (Obradović, 2012; Saxbe et al., 2012). Future assessment of psychological and physiological functioning in perinatal samples is necessary.
Strengths and Limitations
The current study has notable strengths including the use of validated measures of stress and depressive symptoms administered during structured, in-home interviews. Moreover, study visits occurred across consecutive births, thus extending prior work evaluating the interactive effects of childhood and perinatal stress in predicting perinatal well-being in pregnancy only. The sample included representation from three study sites and was racially and ethnically diverse. Furthermore, measures of perinatal stress were based on report of objective occurrence of life events rather than subjective evaluation of their impact thereby reducing the risk of mood bias in reporting. Reports of depressive symptoms and early life adversity were collected at separate study timepoints and therefore retrospective report of early life stress may be less strongly influenced by mood. Employing multilevel modeling as the analytic method of the current study accounted for repeated measurements within individuals and prevented inflation of the Type I error rate (Musca, 2011).
There are also several limitations that warrant mention. Due to low to moderate frequency of exposure to family stress in most of our sample, the current study was limited in its ability to test the association between stressful life events and depressive symptoms among individuals with higher frequencies of exposure to family stress. Furthermore, we only tested the moderating role of childhood family stress which may not capture other forms of early life stress. The type, timing, and chronicity of childhood stress may also have differential associations with perinatal mental health and serve different roles in modifying the associations between perinatal stress and mental health (Tung et al., 2019). Although rates of childhood family stress were similar to other community samples, future tests in perinatal samples with a wider range of exposure to childhood stress are necessary to replicate these findings. The use of different measures of depressive symptoms is another possible limitation. Although both are validated and show strong correspondence, there may be differences in the degree of symptom severity necessary to score a certain proportion of the maximum score across measures. Additionally, reports of early life stress were limited to retrospective report. This method is validated and commonly used in empirical studies of early life stress, but there is some evidence of disagreement between retrospective and prospective results (Baldwin et al., 2019). All measures in the current sample were self-report, thus increasing risk of shared method bias and precluding causal inference.
Conclusions
The current study used a life course perspective to examine the interactive effects of childhood family social environment and stressful life events in predicting depressive symptoms during pregnancy and postpartum. We found that there was a positive association between stressful life events and depressive symptoms in the perinatal period among individuals with a low frequency of exposure to family stress in childhood, but not among individuals with more frequent exposure to childhood family stress. This study provides novel evidence that childhood experiences modifying risk for mental health problems in pregnancy and postpartum and highlight the utility of considering the interaction between risk factors across the lifespan in predicting perinatal mental health.
Supplementary Material
Acknowledgements:
We thank Jennifer A. Somers for critical feedback on an earlier draft of this manuscript.
Funding Sources:
This work was supported through the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD; U HD44207, U HD44219, U HD44226, U HD44245, U HD44253, U HD54791, U HD54019, U HD44226-05S1, U HD44245-06S1, R03 HD59584, 5R01HD072021-05) and the National Institute of Nursing Research (NINR; U NR008929).
Footnotes
The ideas and data presented in this manuscript have not been previously disseminated. Study data, materials, and analysis code are available from the first author upon request. The study was not pre-registered.
References
- Aiken LS, & West SG (1991). Multiple regression: Testing and interpreting interactions. Sage Publications. [Google Scholar]
- Aparicio EM (2017). ‘I want to be better than you:’ Lived experiences of intergenerational child maltreatment prevention among teenage mothers in and beyond foster care. Child and Family Social Work, 22(2), 607–616. 10.1111/cfs.12274 [DOI] [Google Scholar]
- Atzl VM, Grande LA, Davis EP, & Narayan AJ (2019). Perinatal promotive and protective factors for women with histories of childhood abuse and neglect. Child Abuse and Neglect, 91, 63–77. 10.1016/j.chiabu.2019.02.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baldwin JR, Reuben A, Newbury JB, & Danese A (2019). Agreement between prospective and retrospective measures of childhood maltreatment: A systematic review and meta-analysis. JAMA Psychiatry, 76(6), 584–593. 10.1001/jamapsychiatry.2019.0097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bates D, Sarkar D, Bates MD, & Matrix L (2007). The lme4 package. R package version, 2(1), 74. [Google Scholar]
- Bernstein PS, & Merkatz IR (2010). A life course perspective on women’s reproductive health and the outcome of pregnancy. Journal of Women’s Health, 19(3), 555–560. 10.1089/jwh.2009.1397 [DOI] [PubMed] [Google Scholar]
- Bolger N, & Laurenceau JP (2013). Intensive longitudinal methods: An introduction to diary and experience sampling research. Guilford press. [Google Scholar]
- Brody GH, Yu T, & Beach SRH (2016). Resilience to adversity and the early origins of disease. Development and Psychopathology, 28(4), 1347–1365. 10.1017/S0954579416000894 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chamberlain C, Gee G, Harfield S, Campbell S, Brennan S, Clark Y, Mensah F,Arabena K, Herrman H, Brown S, Atkinson J, Nicholson J, Gartland D, Glover K, Mitchell A, Atkinson C, McLachlan H, Andrews S, Hirvoven T, … Dyall D (2019). Parenting after a history of childhood maltreatment: A scoping review and map of evidence in the perinatal period. PLoS ONE, 14(3), 18. 10.1371/journal.pone.0213460 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cox JL, Holden JM, & Sagovsky R (1987). Edinburgh postnatal depression scale (EPDS). British Journal of Psychiatry, 150(6), 782–786. [DOI] [PubMed] [Google Scholar]
- Davis EP, & Narayan AJ (2020). Pregnancy as a period of risk, adaptation, and resilience for mothers and infants. Development and Psychopathology, 32(5), 1625–1639. 10.1017/S0954579420001121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- del Giudice M, Ellis BJ, & Shirtcliff EA (2011). The Adaptive Calibration Model of stress responsivity. Neuroscience and Biobehavioral Reviews, 35(7), 1562–1592. 10.1016/j.neubiorev.2010.11.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- del Giudice M, Benjamin Hinnant J, Ellis BJ, & El-Sheikh M (2012). Adaptive Patterns of Stress Responsivity: A Preliminary Investigation. Development and Psychopathology, 48(3), 775–790. 10.1037/a0026519 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dominguez TP, Dunkel Schetter C, Mancuso R, Rini CM, & Hobel C (2005). Stress in African American pregnancies: Testing the roles of various stress concepts in prediction of birth outcomes. Annals of Behavioral Medicine, 29(1), 12–21. 10.1207/s15324796abm2901_3 [DOI] [PubMed] [Google Scholar]
- Duthie L, & Reynolds RM (2013). Changes in the maternal hypothalamic-pituitary-adrenal axis in pregnancy and postpartum: Influences on maternal and fetal outcomes. Neuroendocrinology, 98(2), 106–115. 10.1159/000354702 [DOI] [PubMed] [Google Scholar]
- Ellis BJ, Abrams LS, Masten AS, Sternberg RJ, Tottenham N, & Frankenhuis WE (2020). Hidden talents in harsh environments. Development and Psychopathology, 1–19. 10.1017/S0954579420000887 [DOI] [PubMed] [Google Scholar]
- Ellis BJ, & Boyce WT (2008). Biological Sensitivity to Context. Current Directions in Psychological Science, 17(3), 183–187. 10.1111/j.1467-8721.2008.00571.x [DOI] [Google Scholar]
- Ellis BJ, Oldehinkel AJ, & Nederhof E (2017). The adaptive calibration model of stress responsivity: An empirical test in the Tracking Adolescents’ Individual Lives Survey study. Development and Psychopathology, 29(3), 1001–1021. 10.1017/S0954579416000985 [DOI] [PubMed] [Google Scholar]
- Epel ES, Crosswell AD, Mayer SE, Prather AA, Slavich GM, Puterman E, & Mendes WB (2018). More than a feeling: A unified view of stress measurement for population science. Frontiers in Neuroendocrinology, 49, 146–169. 10.1016/J.YFRNE.2018.03.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Epstein CM, Houfek J, Rice MJ, & Weiss SJ (2021). Integrative Review of Early Life Adversity and Cortisol Regulation in Pregnancy. Journal of Obstetric, Gynecologic & Neonatal Nursing, 0(0). 10.1016/j.jogn.2020.12.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ertel KA, Rich-Edwards JW, & Koenen KC (2011). Maternal depression in the United States: Nationally representative rates and risks. Journal of Women’s Health, 20(11), 1609–1617. 10.1089/jwh.2010.2657 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fava NM, Simon VA, Smith E, Khan M, Kovacevic M, Rosenblum KL, Menke R, & Muzik M (2016). Perceptions of general and parenting-specific posttraumatic change among postpartum mothers with histories of childhood maltreatment. Child Abuse and Neglect, 56, 20–29. 10.1016/j.chiabu.2016.04.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garcia-Esteve L, Ascaso C, Ojuel J, & Navarro P (2003). Validation of the Edinburgh Postnatal Depression Scale (EPDS) in Spanish mothers. Journal of Affective Disorders, 75(1), 71–76. 10.1016/S0165-0327(02)00020-4 [DOI] [PubMed] [Google Scholar]
- Gavin NI, Gaynes BN, Lohr KN, Meltzer-Brody S, Gartlehner G, & Swinson T(2005). Perinatal depression: A systematic review of prevalence and incidence. Obstetrics and Gynecology, 106(5), 1071–1083. 10.1097/01.AOG.0000183597.31630.db [DOI] [PubMed] [Google Scholar]
- Glynn LM, Howland MA, & Fox M (2018). Maternal programming: Application of a developmental psychopathology perspective. Development and Psychopathology, 30(3), 905–919. 10.1017/S0954579418000524 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gunnar MR, & Quevedo K (2007). The Neurobiology of Stress and Development. Annual Review of Psychology, 58, 145–173. 10.1146/ANNUREV.PSYCH.58.110405.085605 [DOI] [PubMed] [Google Scholar]
- Haight SC, Byatt N, Moore Simas TA, Robbins CL, & Ko JY (2019). Recorded diagnoses of depression during delivery hospitalizations in the United States, 2000–2015. Obstetrics & Gynecology, 133(6), 1216–1223. 10.1097/AOG.0000000000003291 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heisig JP, & Schaeffer M (2019). Why you should always include a random slope for the lower-level variable involved in a cross-level interaction. European Sociological Review, 35(2), 258–279. [Google Scholar]
- Hostinar CE, & Gunnar MR (2013). The Developmental Effects of Early Life Stress: An Overview of Current Theoretical Frameworks. Current Directions in Psychological Science, 22(5), 400–406. 10.1177/0963721413488889 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuznetsova A, Brockhoff PB, & Christensen RHB (2015). Package ‘lmertest’. R package version, 2(0), 734. [Google Scholar]
- Lehman BJ, Taylor SE, Kiefe CI, & Seeman TE (2009). Relationship of early life stress and psychological functioning to blood pressure in the CARDIA study. Health Psychology, 28(3), 338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Little TD, Jorgensen TD, Lang KM, & Moore EWG (2014). On the joys of missing data. Journal of Pediatric Psychology, 39(2), 151–162. 10.1093/jpepsy/jst048 [DOI] [PubMed] [Google Scholar]
- Liu RT, Choi JY, Boland EM, Mastin BM, & Alloy LB (2013). Childhood abuse and stress generation: The mediational effect of depressogenic cognitive styles. Psychiatry Research, 206(2–3), 217–222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu MC, & Halfon N (2003). Racial and Ethnic Disparities in Birth Outcomes: A Life-Course Perspective. Maternal and Child Health Journal 2003 7:1, 7(1), 13–30. 10.1023/A:1022537516969 [DOI] [PubMed] [Google Scholar]
- Luke DA (2019). Multilevel modeling. Sage Publications. [Google Scholar]
- Mahrer NE, Ramos IF, Guardino C, Davis EP, Ramey SL, Shalowitz M, & Dunkel Schetter C (2020). Pregnancy anxiety in expectant mothers predicts offspring negative affect: The moderating role of acculturation. Early Human Development, 141, 104932. 10.1016/j.earlhumdev.2019.104932 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marcus SM, Flynn HA, Blow FC, & Barry KL (2003). Depressive symptoms among pregnant women screened in obstetrics settings. Journal of Women’s Health, 12(4), 373–380. 10.1089/154099903765448880 [DOI] [PubMed] [Google Scholar]
- Masten AS (2018). Resilience Theory and Research on Children and Families: Past, Present, and Promise. Journal of Family Theory & Review, 10(1), 12–31. 10.1111/JFTR.12255 [DOI] [Google Scholar]
- Masten AS, & Barnes A (2018). Resilience in Children: Developmental Perspectives. Children, 5(7), 98. 10.3390/children5070098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meaney MJ (2018). Perinatal maternal depressive symptoms as an issue for population health. American Journal of Psychiatry, 175(11), 1084–1093. 10.1176/appi.ajp.2018.17091031 [DOI] [PubMed] [Google Scholar]
- Moeller J (2015). A word on standardization in longitudinal studies: don’t. Frontiers in Psychology, 6, 1389. 10.3389/FPSYG.2015.01389 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moog N, Buss C, Entringer S, Shahbaba B, Gillen DL, Hobel CJ, & Wadhwa PD (2016). Maternal exposure to childhood trauma is associated during pregnancy with placental-fetal stress physiology. Biological Psychiatry, 79(10), 831–839. 10.1016/j.biopsych.2015.08.032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morgan JE, Lee SS, Mahrer NE, Guardino CM, Davis EP, Shalowitz MU, Ramey SL, & Dunkel Schetter C (2020). Prenatal maternal C‐reactive protein prospectively predicts child executive functioning at ages 4–6 years. Developmental Psychobiology, 00, 1–13. 10.1002/dev.21982 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Musca SC, Kamiejski R, Nugier A, Méot A, Er-Rafiy A, & Brauer M (2011). Data with hierarchical structure: Impact of intraclass correlation and sample size on Type-I error. Frontiers in Psychology, 2(APR), 74. 10.3389/FPSYG.2011.00074/BIBTEX [DOI] [PMC free article] [PubMed] [Google Scholar]
- Narayan AJ, Atzl VM, Merrick JS, Harris WW, & Lieberman AF (2020). Developmental Origins of Ghosts and Angels in the Nursery: Adverse and Benevolent Childhood Experiences. Adversity and Resilience Science, 1(2), 121–134. 10.1007/s42844-020-00008-4 [DOI] [Google Scholar]
- Narayan AJ, Lieberman AF, & Masten AS (2021). Intergenerational transmission and prevention of adverse childhood experiences (ACEs). Clinical Psychology Review, 85. 10.1016/j.cpr.2021.101997 [DOI] [PubMed] [Google Scholar]
- Obradović J (2012). How can the study of physiological reactivity contribute to our understanding of adversity and resilience processes in development?. Development and psychopathology, 24(2), 371–387. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Curran PJ, & Bauer DJ (2006). Computational tools for probing interactions in multiple linear regression, multilevel modeling, and latent curve analysis. Journal of Educational and Behavioral Statistics, 31(4), 437–448. [Google Scholar]
- Racine N, Devereaux C, Cooke JE, Eirich R, Zhu J, & Madigan S (2021). Adverse childhood experiences and maternal anxiety and depression: a meta-analysis. BMC Psychiatry, 21(1), 28. 10.1186/s12888-020-03017-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- Repetti RL, Taylor SE, & Seeman TE (2002). Risky families: Family social environments and the mental and physical health of offspring. Psychological Bulletin, 128(2), 330–366. 10.1037/0033-2909.128.2.330 [DOI] [PubMed] [Google Scholar]
- Rutter M (2012). Resilience as a dynamic concept. Development and Psychopathology, 24(2), 335–344. 10.1017/S0954579412000028 [DOI] [PubMed] [Google Scholar]
- Salm Ward T, Kanu FA, & Robb SW (2017). Prevalence of stressful life events during pregnancy and its association with postpartum depressive symptoms. Archives of women’s mental health, 20(1), 161–171. [DOI] [PubMed] [Google Scholar]
- Santor DA, & Coyne JC (1997). Shortening the CES-D to improve its ability to detect cases of depression. Psychological Assessment, 9(3), 233–243. 10.1037/1040-3590.9.3.233 [DOI] [Google Scholar]
- Saxbe DE, Margolin G, Spies Shapiro LA, & Baucom BR (2012). Does dampened physiological reactivity protect youth in aggressive family environments? Child Development, 83(3), 821–830. 10.1111/j.1467-8624.2012.01752.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shakiba N, Ellis BJ, Bush NR, & Thomas Boyce W (2017). Biological sensitivity to context: A test of the hypothesized U-shaped relation between early adversity and stress responsivity. Development and Psychopathology, 32, 641–660. 10.1017/S0954579419000518 [DOI] [PubMed] [Google Scholar]
- Seery MD (2011). Resilience: A silver lining to experiencing adverse life events? Current Directions in Psychological Science, 20(6), 390–394. 10.1177/0963721411424740 [DOI] [Google Scholar]
- Seery MD, Holman EA, & Silver RC (2010). Whatever Does Not Kill Us: Cumulative Lifetime Adversity, Vulnerability, and Resilience. Journal of Personality and Social Psychology, 99(6), 1025–1041. 10.1037/A0021344 [DOI] [PubMed] [Google Scholar]
- Shapero BG, Hamilton JL, Stange JP, Liu RT, Abramson Y, L., & Alloy LB (2015). Moderate Childhood Stress Buffers Against Depressive Response to Proximal Stressors: A Multi-Wave Prospective Study of Early Adolescents. Journal of Abnormal Child Psychology, 43(8), 1403. 10.1007/S10802-015-0021-Z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Snijders TA, & Bosker RJ (2011). Multilevel analysis: An introduction to basic and advanced multilevel modeling. Sage Publications. [Google Scholar]
- Taylor SE, Lerner JS, Sage RM, Lehman BJ, & Seeman TE (2004). Early environment, emotions, responses to stress, and health. Journal of Personality, 72(6), 1365–1394. 10.1111/j.1467-6494.2004.00300.x [DOI] [PubMed] [Google Scholar]
- Tandon SD, Cluxton-Keller F, Leis J, Le HN, & Perry DF (2012). A comparison of three screening tools to identify perinatal depression among low-income African American women. Journal of Affective Disorders, 136(1–2), 155–162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tung I, Keenan K, Stepp SD, & Hipwell AE (2019). The moderating effects of traumatic stress on vulnerability to emotional distress during pregnancy. Development and Psychopathology, 1–14. 10.1017/S0954579419000531 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yim IS, Tanner Stapleton LR, Guardino CM, Hahn-Holbrook J, & Dunkel Schetter C (2015). Biological and psychosocial predictors of postpartum depression: Systematic review and call for integration. Annual Review of Clinical Psychology, 11(1), 99–137. 10.1146/annurev-clinpsy-101414-020426 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


