Abstract
Study Design
Systematic review and meta-analysis
Objectives
This study’s objective is to provide a critical review of the current literature regarding the changes in pulmonary function (PF) in Adolescent idiopathic scoliosis (AIS) patients who have undergone posterior spinal fusion and instrumentation (PSF), with and without thoracoplasty (TP).
Methods
A comprehensive search was performed using the following databases: EMBASE, PubMed, EBSCOhost (CINAHL and Medline) and OpenGrey. Our focus was on studies that compared pre-and postoperative percent-predicted values of forced vital capacity (%FVC) or forced expiratory volume in 1 second (%FEV1) in AIS patients who had undergone PSF, with and without TP, with a minimum 2-year follow-up. The risk of bias for included studies was assessed using the ROBINS-I (“Risk Of Bias In Non-randomised Studies - of Interventions”) tool. Mean change scores were depicted using forest plots.
Results
Fifteen studies met our inclusion criteria. The results of our analysis suggest that PSF with TP caused a significant deterioration of %FVC in individuals with moderate AIS, with no significant effect on %FEV1. It also showed a minor improvement of FEV1% in individuals with moderate AIS after PSF only, but no significant change in %FVC.
Conclusions
PSF with TP caused a significant deterioration of % FVC while PSF alone caused a minor improvement of FEV1% in individuals with moderate AIS with a minimum 2-year follow-up.
Keywords: adolescent idiopathic scoliosis, spinal fusion, respiratory function tests, thoracoplasty, forced expiratory volume, vital capacity
Introduction
The development and awareness of progressive spinal deformity in adolescent idiopathic scoliosis (AIS) patients oft relates to the perception of significant change in thoracic and shoulder symmetry. With more severe deformity, where surgery is indicated, asymmetry often manifests with unilateral rib prominence, waist, chest wall and shoulder asymmetry. Increased rib prominence has been associated with lower self-reported patient outcome scores and self-image scores among affected individuals.1-6 Posterior spinal deformity correction and fusion (PSF) is currently the gold standard for deformity correction in AIS.7,8 Previous studies have reported that Harrington and Cotrel-Dubousset instrumentation had little effect on rib hump deformity despite other advantages, and thus the argument for Thoracoplasty (TP) to improve chest wall deformity was introduced.9-11 The addition of TP to correct residual rib prominence can reduce rib hump height, improve self-image scores and provide additional autograft for fusion.5,6,12,13 TP usually involves the excision of the involved ribs from the costovertebral junction up to the posterior axillary line. Several modifications of the technique have been described in the literature including Schollner costoplasty, Convex Short Length Rib Resection, the rib-end-to-transverse process thoracoplasty, and short apical rib resection.14-16 The introduction of all (pedicle) screw and hybrid constructs which utilise techniques such as direct vertebral derotation and posteromedial translation have resulted in decreased use of TP due to their success in reducing deformity without violating the chest wall.1,3,5,13,17,18 Thoracoplasty has also drawn criticism for causing a deterioration in pulmonary function of patients who have undergone PSF.19,20 Despite these claims, there have been contrasting findings by authors reporting improvement or decline in pulmonary function test values (PFTs) in participants after PSF with TP.3,5,12,19,21,22
Two recent systematic reviews have analysed the effects of corrective surgery on pulmonary function in AIS patients. Lee et al reported on changes in absolute PFTs after corrective surgery. They concluded that Anterior spinal fusion/instrumentation results in a moderate/large reduction in absolute PFTs in the first 3 months post-surgery but normalizes at 2-year post-surgery. They also concluded that TP in conjunction with any surgical approach did not significantly affect absolute PFTs, while PSF had mild to moderate positive effects on absolute PFTs. 20 In contrast, Kato et al 23 concluded that PSF did not affect percent-predicted pulmonary function test values (%PFTs) at 2-year follow-up. Pulmonary development occurs rapidly during childhood into adolescence, and height, age, sex, and ethnicity must be considered when interpreting PFTs.24-27 Consequently, the use of %PFTs can help distinguish whether any measured changes in pulmonary function could be attributed to surgery or form part of normal development.23,25,26 To the best of our knowledge, no review in the literature has compared the effects of PSF alone vs PSF with TP on %PFTs in patients with AIS. This study aims to provide a critical review of the current literature regarding the changes in pulmonary function in AIS patients who have undergone posterior spinal deformity correction and fusion, with or without thoracoplasty.
Methods
Study Selection
The following inclusion criteria were defined: AIS participants who underwent PSF only, AIS participants who underwent PSF with TP, participants aged 10-22 years, studies with pre-and postoperative %PFTs reported, minimum 2-year follow-up, minimum reported statistics of sample size, mean and standard deviations (SD) of %PFTs. Studies were excluded if they included patients with non-idiopathic diagnoses, including neuromuscular, congenital, syndromic or secondary scoliosis, and studies with participants who underwent conversion to PSF from growing rods or had staged surgery. Case reports, literature reviews, conference abstracts and technique reports were excluded from this review. All other prospective and retrospective study types were included. Study subjects were placed into 2 groups for analysis: Patients who underwent PSF without TP (PSF) vs patients who underwent PSF with TP (PSF and TP).
Search Strategy
A comprehensive systematic search was performed using the following databases: EMBASE, PubMed, EBSCO (CINAHL and Medline) and OpenGrey. Medical Subject Heading (MeSH) terms and Emtree (Subject headings) were used to identify variances in subject terms, along with a variation of our search terms with reference to the guidelines set out in Chapter 4 of the Cochrane handbook. 28 The key search terms and combinations were standardised across all 4 databases. The 3 key search terms were “Idiopathic Scoliosis, Surgery and Pulmonary function. The combined and individual database searches were recorded in preferred reporting items for systematic reviews and meta-analyses (PRISMA) (2009) flow diagrams. 29 Finally, a “hand search” of reference lists and citations was completed to avoid the omission of any relevant studies. All databases were searched from inception to March 2021. The search was restricted to human subjects and English language publications due to resource constraints rendering the timely and accurate translation of studies impossible. The complete search strategies for all databases are presented in Appendix 1.
Data Collection and Analysis
Two independent reviewers performed study screening. Key variables were defined as percent predicted forced vital capacity (%FVC), and percent predicted forced expiratory volume in 1 second (%FEV1). The following data was collected for meta-analysis: The sample size, mean and standard deviations of pre-and postoperative per cent predicted forced vital capacity (%FVC), and per cent predicted forced expiratory volume in 1 second (%FEV1). Where postoperative %PFTs over multiple time points were available, the latest complete values were chosen for analysis. Descriptive data for scoliosis cobb angle (SCA), thoracic kyphosis angle (TKA), curve type and length of follow-up were also collected. The effects of SCA curve magnitude on PFTs are controversial and grading the severity of the SCA is challenging. It has been reported that an SCA above 80° may lead to increased shortness of breath, thus we deemed any SCA above 80° as severe, between 45° and 79° as moderate, and curves below 45° as mild.30-33 If any missing data was encountered, the authors were contacted to try and obtain further information. If missing data could not be obtained, the group was excluded from the analysis. The risk of bias for included studies was assessed using the ROBINS-I (“Risk Of Bias In Non-randomised Studies - of Interventions”) tool 34 and presented using the Risk-of-bias VISualization (robvis) tool. 35 The level of evidence for each study was determined using the rating advocated by Marx and Wilson in the Journal of Bone and Joint Surgery. 36 The grades of recommendation assessment, development, and evaluation (GRADE) system 37 were used to determine each outcome’s level of evidence.
Statistical Analysis
Statistical analysis was performed using Stata 16 (StataCorp. 2019. Stata Statistical Software: Release 16. College Station, TX: StataCorp LLC.) The mean change scores (preoperative and follow-up time points) of PFTs were analysed for the PSF and PSF and TP groups. Using a random-effects meta-analysis, these data were pooled together to obtain the summary effect estimate, 95% confidence interval, and P-value. Heterogeneity between studies was explored by visual inspection of the forest plots and quantified using the I2 statistic. The I2 statistic is a quantitative expression (percentage) of total variation that is due to between-study differences rather than sampling error or chance. A value of 0% indicates no observed heterogeneity while 0-40%, 30-60%, 50-90% and >75% may represent non-significant, moderate, substantial, and considerable heterogeneity, respectively. 28 A funnel plot and Egger’s test were used to assess publication bias risk. For studies where the standard deviations of the mean change scores were not reported, authors were contacted to obtain the information. In instances where missing data were not obtainable, correlation coefficients were calculated from the studies providing SDs and used to impute correlation coefficients for the studies with missing data, as described in Chapter 6 of the Cochrane Handbook. 28 Following this, we used the imputed correlation coefficients to calculate SDs for analysis. Sensitivity analysis was performed to explore the effects of changing correlation coefficient values on SD imputation in the following ways: using an independent conservative correlation coefficient (.4), using the median correlation coefficient (.70216), using the smallest correlation coefficient (.5688), and using the largest correlation coefficient (.81639) calculated from included studies that reported SDs.
Results
Study Selection and Characteristics
A total of 6938 studies were identified for initial screening. After duplicates were removed, 5691 studies remained. Screening by title and abstract excluded a further 5591 studies. The remaining 100 studies were identified that discussed pulmonary function changes in AIS patients who have undergone spinal corrective surgery with or without thoracoplasty. These studies underwent full-text screening. From this group, 39 studies were identified that discussed posterior-only surgical approaches with or without thoracoplasty. After final exclusions, a total of 15 studies met the eligibility criteria and were deemed suitable for meta-analysis.3,5,12,19,21,22,38-46 If the findings of multiple surgical techniques were reported in one study, only the group(s) who underwent PSF with or without TP (PSF +/− TP) were extracted for meta-analysis. A PRISMA 29 screening flow chart for study selection is presented in Figure 1, and flow charts for each database are presented in Appendix 2(a)-(d). Table 1 summarises the included studies, their patient demographics and assigned evidence strength levels. 36 Studies were excluded for the following reasons: Only absolute PFTs reported, relevant results could not be extracted from studies with multiple surgical techniques, participant overlap with other included studies could not be ruled out, less than 2 years follow up, incorrect age of subjects, participants with non-idiopathic scoliosis, and participants who underwent staged surgery. The authors were contacted for clarification where participant overlap between studies could not be ruled out. If no clarification was received, the study with the largest number of participants was included and the other studies excluded. A table of excluded studies with reasons can be viewed in Appendix 3: Supplementary Material.
Figure 1.
PRISMA 29 Screening flowchart of study screening for all databases.
Table 1.
Summary of included studies.
| ID | Authors | PublishedYear | Additional Note | EL | Surgical Approach | n | M | F | Age (SD or Range) | Follow up (years) | Curve Types | Cobb Pre-operative (SD) | Cobb Follow-up (SD) | TK Pre-operative (SD) | TK Follow-up (SD) | %FVC Pre-operative (SD) | %FVC Follow-up (SD) | %FEV1 Pre-operative (SD) | %FEV1 Follow-up (SD) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 01 | Vedantam et al | 2000 | PSF only group excluded due to possible overlap with another included study. | 3 | PSF + TP | 33 | NA | NA | 14.2 (2.3) | 3.21 | King 1-5 | 64 (14) | 36 (11) | 24 (15) *T3-T12 | 27 (10) *T3-T12 | 84.5 (17.2) | 77.3 (14.3) | 78.5 (15.9) | 71.9 (13.4) |
| 02 | Pehrsson et al | 2001 | VC used instead of FVC. Only FEV1 used for analysis. | 3 | PSF | 141 | 10 | 131 | 15 (1.8) | 25 | Double Primary, Thoracic and Thoracolumbar | 62 (13) | 37 (10) | NA | NA | 67 (13) **%VC used | 84 (13) **%VC used | 71 (14) | 84 (14) |
| 03 | Kim et al | 2007 | 3 | PSF | 139 | 25 | 114 | 14.6(2.2) | 2 | Lenke 1-4 | 60 (11.7) | 26 (13.3) | 21 (13.5) | 19(8.8) | 79 (16.6) | 81 (16.7) | 75 (16.1) | 77 (15.5) | |
| 04 A | Suk et al | 2008 | 3 | PSF | 37 | 5 | 32 | 14.7 (11-19) | 6.0 | Lenke 1 & 2 | 53.2 (9.1) | 16.3 (6) | 14.3 (8.4) | 22 (8.2) | 81.7 (13.5) | 78.5(15.6) | 74.8(13.1) | 72.7(13) | |
| 04 B | Suk et al | 2008 | Non direct vertebral rotation (N-DVR) group |
3 | PSF + TP | 20 | 2 | 18 | 14.2 (11–17) | 4.8 | Lenke 1 & 2 | 55.4 (11.2) | 17.7(6.3) | 16.6 (7.6) | 21.3 (7.8) | 84.3 (12.3) | 73.5 (12.3) | 74.8 (9.9) | 70.5(9) |
| 04 C | Suk et al | 2008 | Direct vertebral rotation (DVR) group |
3 | PSF + TP | 30 | 4 | 26 | 14.1 (11–17) | 2.5 | Lenke 1 & 2 | 53.6 (12.3) | 10(4.6) | 15(9) | 22.4 (8.5) | 76.8 (15.8) | 70.3 (14.4) | 71.1 (15.3) | 67.4 (15.2) |
| 05 A | Chunguang et al | 2011 | 3 | PSF | 24 | NA | NA | 14.7 (10–17) | 2 | Lenke 1 & 2 | 66.8 (11.5) | 19.2 (7.1) | 20.1 (7.6) | 24.6 (7.5) | 81.4 (13.2) | 81.7 (13.5) | 74.5 (13) | 75.5 (13.5) | |
| 05 B | Chunguang et al | 2011 | Conventional Thoracoplasty (CT) group | 3 | PSF + TP | 20 | NA | NA | 14.5 (10–17) | 2 | Lenke 1 & 2 | 67.5 (12) | 19.2 (7.1) | 21.2 (8) | 26.3 (8) | 81.5 (13.5) | 75.7 (9.7) | 74.8 (13.6) | 70.5 (8.3) |
| 05 C | Chunguang et al | 2011 | Convex short length rib resection (CSLRR) group |
3 | PSF + TP | 26 | NA | NA | 14.2 (10–17) | 2 | Lenke 1 & 2 | 68.4 (12.9) | 17.7 (7.4) | 20.4 (7.8) | 28.8 (8.6) | 80.8 (13) | 80.5 (13.1) | 74.7 (13.2) | 74.5 (13.3) |
| 06 A | Greggi et al | 2011 | 3 | PSF | 40 | 5 | 35 | 15.2(1.9) | 8.3 | Lenke 1-3 | 63 (13) | 35 (13) | 35.2(12.5) | 32.4 (10.6) | 84 (14) | 87 (18) | 80(13) | 83 (17) | |
| 06 B | Greggi et al | 2011 | 3 | PSF + TP | 40 | 6 | 34 | 16.3(2) | 8.3 | Lenke 1-3 | 66(14) | 31 (11.2) | 35.3 (10.1) | 28.4 (9.8) | 85 (15) | 83(14) | 82(12) | 80 (11.5) | |
| 07 | Verma et al | 2011 | 1 x thoracoplasty patient included in the PSF cohort. Included due to expected minimal effect on results. | 3 | PSF | 70 | 23 | 47 | 15.6(2.3) | 2 | Lenke 1-3 | 50 (7.5) | 11 (4.5) | NA | NA | 81.4 (12.4) | 82.66 (0.72) | 80.3 (13.6) | 78.76 (0.60) |
| 08 | Nohara et al | 2015 | VC used instead of FVC. Authors contacted. Only use FEV1. SD's obtained from Authors. | 3 | PSF | 30 | 0 | 30 | 15.7(3) | 14.2 | Lenke 1 & 2 | 58(7) | 26(8.4) | 25.6 (9.1) | 35.2 (8.8) | 81.0 (14.5) **%VC used | 86.4 (12) **%VC used | 84.3 (8.4) | 86.7 (5.5) |
| 09 | Jeans et al | 2017 | 3 | PSF | 37 | 7 | 30 | 14.5 (1.8) | 2.3 | Lenke 1,2,4,5,6 | 59.8 (10.7) | 28.1 (17.7) | 22.7 (13.2) | 32.3 (15) | 82 (15.5) | 82.2 (13.4) | 77.8 (15.3) | 78.3 (14.5) | |
| 10 | Min et al | 2018 | 3 | PSF | 11 | 2 | 9 | 15.2( 2.6) | 6.4 | Double major | 62.3 (15) | 20.3(10.7) | 32.4(10) | 35.6(15.3) | 80(16) | 71(11) | NA | NA | |
| 11 A | Duray et al | 2019 | Additional data obtained from Authors. | 4 | PSF + TP | 36 | 4 | 32 | NA (13-17) | 2 | Lenke 1 & 2 | 51 (29) | 21(16) | 33(16) *T1-T12 | 42(16) *T1-T12 | 84(15) | 83(16) | 83(15) | 84(15) |
| 11 B | Duray et al | 2019 | Additional data obtained from Authors. | 4 | PSF | 60 | 14 | 46 | NA (13-17) | 2 | Lenke 1 & 2 | 50(17) | 22(12) | 29(13) *T1-T12 | 36(21) *T1-T12 | 87(15) | 87(14) | 84(14) | 88(16) |
| 12 | Fujita et al | 2019 | VC used instead of FVC. Only FEV1 used for analysis. SD's obtained from authors. | 3 | PSF | 111 | 8 | 103 | 14.8(2.1) | 2 | Lenke 1,2,3,4,6 | 54.9 (10.4) | 17.4(7.5) | 15.2 (10.6) | 28.8 ( 8.6) | 80.0 (15.9) **%VC used | 80.5 (13.1) **%VC used | 85.8 (7.6) | 74.5 (13.3) |
| 13 | Yaszay et al | 2019 | 3 | PSF | 165 | NA | NA | NA (11-20) | 5 | Lenke 1-6 | NA | NA | NA | NA | 86(15) | 85(12) | 80(14) | 82(13) | |
| 14 | Byun et al | 2020 | 3 | PSF | 35 | 7 | 28 | 14.9 (12–19) | 15.1 | Lenke 1-4 | 68.1 (18.6) | 28.9 (2.2) | 16.2 (8.8) | 21.3 (8.2) | 74.0 (19.8) | 76.4 (16) | 91.8 (42.6) | 82.8 (12.5) | |
| 15 A | Akazawa et al | 2021 | Additional data obtained from Authors. | 3 | PSF | 21 | 3 | 18 | 15.4(1.9) | 7.2 | Lenke 1-3 | 53.5(9.5) | 21.1(5.7) | 16.4 (11.5) | 22.1(8) | 82.7 (17.7) | 87.2 (17.9) | 68.2 (14.7) | 76.6 (15.7) |
| 15 B | Akazawa et al | 2021 | Additional data obtained from Authors. | 3 | PSF + TP | 24 | 1 | 23 | 15.5(2) | 7.2 | Lenke 1 & 2 | 56.4 (9.7) | 25.8(7.9) | 15.1 (9.4) | 19.8(8) | 74.5 (18.6) | 76.4 (16.4) | 57.1 (16) | 66.2 (13.9) |
Results are depicted as means. Abbreviations: SD-Standard deviation, PSF -Posterior Spinal Fusion, TP- Thoracoplasty, TK-Thoracic Kyphosis, VC- Vital Capacity, FVC -Forced Vital Capacity, FEV1- Forced expiratory volume in 1 second, NA-Not available, n=number, M=Male, F=Female, EL = Evidence Level
*Thoracic Kyphosis Measurement Deviation from standard T5-T12
** VC Reported instead of FVC
Risk of Bias Within Studies
Eleven of the included studies were deemed to be at moderate risk of bias, and 4 were considered to be at serious risk of bias. No studies were considered to be at critical risk of bias. The full results are presented in Figure 2 using the robvis tool as advocated by the authors of the ROBINS-I risk of bias of tool.34,35
Figure 2.
Results of risk of bias assessment within studies illustrated with the robvis 35 tool.
Radiographic Results and Follow-Up
The mean reported preoperative scoliosis cobb angle (SCA) ranged from 50° to 68.4°, and the mean preoperative thoracic kyphosis angle (TKA) ranged from 14.3° to 35.3°. The largest reported SCA was 122°. With regards to curve types, 9 studies included patients with variations of thoracic and thoracolumbar curve types,21,22,38-42,44,45 4 studies focused on patients with thoracic-only curves3,5,12,43 and 2 studies reported on all curve types.19,46 Nine studies had a minimum of 2 years of follow-up,3,5,12,19,39-42,45 and 6 studies had a minimum 5-year follow-up.21,22,38,43,44,46 The longest reported mean follow-up period was 25 years by Pehrsson et al. 44
Pulmonary Function Results
The mean reported preoperative %FVC ranged from 67% to 87.7%, and the mean reported preoperative %FEV1 from 57.1% to 91.8%. Three studies reported Vital Capacity (VC) rather than Forced Vital Capacity (FVC).39,43,44 It has been shown that VC cannot be assumed to be equivalent to FVC if measured in subjects with potential airway obstruction or narrowing. 47 Consequently, we could not reliably infer that the FVC and VC values would be similar in the patients in these studies, and their reported %VC values were excluded from the %FVC part of the meta-analysis. One study did not report pre-and postoperative %FEV1 values, and only %FVC values. 42 Two studies compared different thoracoplasty techniques with PSF against PSF only and were analysed as separate groups in the statistical analysis.5,12 The results discussed are based on the analysis using the median correlation coefficient (.70) with associated forest plots presented in Figures 3-6. Forest plots for the complete sensitivity analysis are available in Appendix 4: Supplementary material.
Figure 3.
Forest plot depicting %FVC change in the PSF Group.
Figure 6.
Forest Plot depicting %FEV1 Change is PSF & TP Group.
%FVC Change in the PSF Group
Eleven studies were included in this analysis.3,5,12,21,22,38,40-42,45,46 There was no evidence of a statistically significant difference in %FVC between preoperative and follow-up measurements in the PSF group (Mean change score: 0.34, 95%CI: −1.01 to 1.69, I2 = 47.77%, see Figure 3). A funnel plot (Figure 7) showed no significant evidence of publication bias and was backed up by Egger’s test (P = .5456). The GRADE 37 level for this outcome in this group was deemed to be VERY LOW since all the studies were non-randomised with some inter-study inconsistency. Results remained consistent with sensitivity analysis.
Figure 7.
Funnel plot used to investigate publication bias in the 11 included studies for the %FVC change in the PSF Group.
%FVC Change in the PSF &TP Group
This analysis included 6 studies with 8 groups.3,5,12,19,21, and 22 This showed a statistically significant decrease in %FVC between preoperative and follow-up measurements in the PSF and TP group (Mean change score: −3.96, 95%CI: −6.87 to −1.06, I2 = 75.23%, see Figure 4). A funnel plot (Figure 8) showed no significant evidence of publication bias and was backed up by Egger’s test (P = .9621). The GRADE 37 level for this outcome in this group was deemed to be VERY LOW since all the studies were non-randomised with some inter-study inconsistency. Results remained consistent with sensitivity analysis.
Figure 4.
Forest plot depicting %FVC change in the PSF & TP Group.
Figure 8.
Funnel plot used to investigate publication bias in the 6 included studies with 8 groups for the %FVC change in the PSF & TP Group.
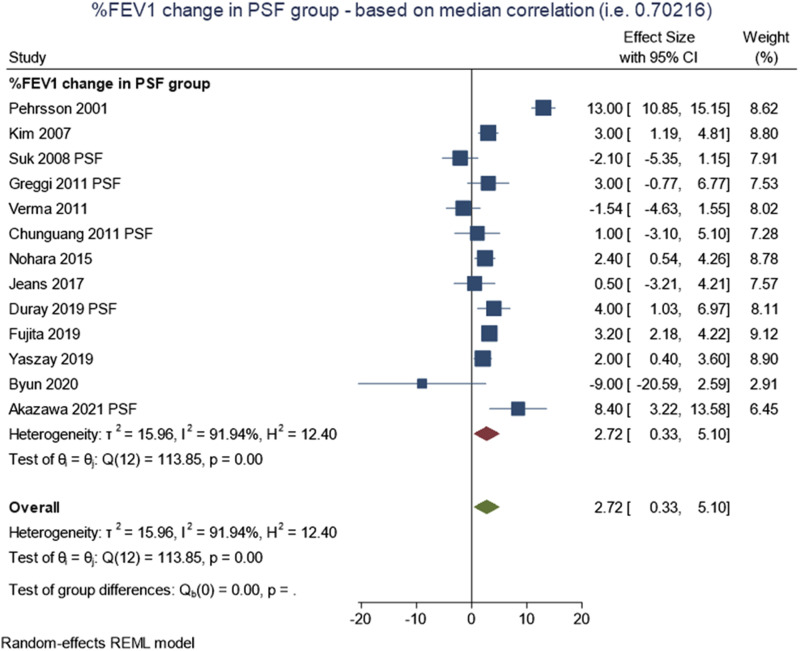
%FEV1 Change in the PSF Group
Thirteen studies were included in this analysis.3,5,12,21,22,38-41,43-46 The results showed a statistically significant increase in %FEV1 for the PSF group between preoperative and follow-up measurements (Mean change score: 2.72, 95%CI: .33 to 5.1, I2 =91.94%, see Figure 5). A funnel plot (Figure 9) showed no significant evidence of publication bias and was backed up by Egger’s test (P= .1503). The GRADE 37 level for this outcome in this group was deemed to be VERY LOW since all the studies were non-randomised with some inter-study inconsistency and considerable statistical heterogeneity. Results remained consistent with sensitivity analysis.
Figure 5.
Forest Plot depicting %FEV1 Change in the PSF Group.
Figure 9.
Funnel plot used to investigate publication bias in the 13 included studies for the %FEV1 change in the PSF Group.
% FEV1 Change in the PSF & TP Group
Six studies with a total of 8 groups were included in this analysis.3,5,12,19,21,22 The analysis revealed no evidence of a statistically significant difference in %FEV1 between preoperative and follow-up measurements in the PSF and TP group (Mean change score: −1.48, 95%CI: −4.69 to 1.73, I2 = 82.76%, see Figure 6). A funnel plot (Figure 10) showed no significant evidence of publication bias and was backed up by Egger’s test (P= .2705). The GRADE 37 level for this outcome in this group was deemed to be VERY LOW since all the studies were non-randomised with some inter-study inconsistency and substantial statistical heterogeneity. Results remained consistent with sensitivity analysis.
Figure 10.
Funnel plot used to investigate publication bias in the 6 included studies with 8 groups for the %FEV1 change in the PSF & TP Group.
Discussion
The use of thoracoplasty to correct rib hump deformity in AIS has been controversial. This is mainly due to its deleterious effect on patient PFTs after surgery and the higher incidence of perioperative complications and postoperative chest wall neuralgia.14,19,20,22,48-50 There have, however, been reports of improvement or non-significant changes in PFTs after TP in several studies.3,5,12,21,22 There are also the reported benefits to consider, such as improved rib hump correction, improved self-image scores and the additional provision of autograft for fusion.5,6,12,13,51
The results of this systematic review and meta-analysis suggest that PSF with TP causes a significant deterioration of %FVC in individuals with moderate AIS.8,30-33 We did not find any significant effect on %FEV1 in this group. Furthermore, our analysis shows a small but significant improvement of FEV1% after PSF only, but no statistically significant change in %FVC. These results refer to a minimum follow-up of 2 years after surgery.
Our findings differ somewhat from the 2016 systematic review by Lee et al, 20 who found that thoracoplasty in conjunction with any surgical approach caused an initial postoperative decline in absolute PFT values, which later normalised at 2 years post-surgery. They also showed an improvement in absolute PFTs at 2 and 6 years after posterior-only corrective surgery. They stressed that these findings be interpreted in the context of the known rapid increase of PFTs in adolescent boys and girls and that any surgical procedure that led to non-significant increases in PFTs 2 years after surgery may impair pulmonary function. 27 A recently published systematic review by Kato et al 23 found no significant improvement in %FVC or %FEV1 at minimum 2 years after posterior surgical correction without TP in patients with mild to moderate AIS. These reviews have commented on the significance of reporting absolute vs percent predicted of normal PFTs.20,23 It is reported that values that have been compared to those of the normal population provide a more accurate representation of the actual changes in pulmonary function.24,25 Unfortunately, various studies were excluded from our analysis because they only reported absolute values of PFTs.
It is important to note the varying levels of heterogeneity identified between the included studies in our meta-analysis. Despite this, the results proved consistent with sensitivity analysis, and we were able to conclude that PSF and TP caused a significant reduction in %FVC in AIS patients in the short to medium term. We can also conclude that AIS patients experienced a small but significant increase in %FEV1 after PSF only. Finally, we can deduce that PSF alone and PSF and TP do not significantly affect %FVC and %FEV1 in AIS, respectively.
This Systematic review has Several Limitations and Complexities
Firstly, 9 studies focused on 2 to 5 year follow-up, and only 6 studies had a minimum of 5 years follow-up. Further studies are needed to accurately determine the effects of surgery on PFTs in AIS patients in the long term.
Secondly, multiple factors could not be fully controlled for in this analysis. These include age at surgery, type of instrumentation utilised during surgery, preoperative and postoperative physical therapy regimes, activity and fitness levels of participants across studies and whether participants were smokers or not. Further high-quality studies are needed with strict protocols for preoperative and postoperative treatment and fitness regimes within a homogenous AIS patient cohort.
Thirdly, various techniques of thoracoplasty were utilised by different authors, and the number of ribs resected, and their location (upper, middle or lower region) within the thoracic cage differed according to the apex of curves in each patient. There is a possibility these factors might have influenced PFTs in such a way that was not accounted for in the included studies.
Fourthly, the included studies had participants with SCA’s within a wide range from curves of all types. It can only be postulated whether the preoperative deformity or the magnitude of the correction of the coronal deformity affects the degree of change in pulmonary function after surgery. Further studies are needed that would be able to classify these effects according to curve severity, curve type and magnitude of deformity correction.
Fifth, we could not account for the impact of kyphosis restoration on pulmonary function changes due to insufficient data in the included studies. Thoracic hypokyphosis has been associated with pulmonary function impairment in AIS, and the mean TKAs of participants in the included studies ranged from hypokyphotic to normal.52,53 Our findings should be interpreted with this in mind.
Sixth, our analysis focused on %PFTs instead of absolute PFT values and consequently excluded a significant number of studies from the meta-analysis. The calculation methods for %PFTs differ between studies, and adjustment formulas for height loss and gain due to scoliosis and its subsequent correction vary widely.27,54,55 Consequently, the possibility exists of some variation in %FVC and %FEV1 results if these adjustments have been performed using different formulas. Nevertheless, %PFTs still allow us to compare any changes to average values in the general population and better represent the actual effects of surgery.23,25,26
Seventh, because the SD’s for the change of %PFTs between preoperative and follow-up measurements could not be obtained for several studies, imputation was needed to calculate these for the analysis. This practice is common in meta-analyses due to the varying consistency in reporting results in observational studies and randomised control trials. 56 Despite the limitations of imputation, our results did not vary with sensitivity analysis using a wide range of correlation coefficients. This illustrates that the results were robust to a wide range of possible real-world SDs in the relevant studies.
Finally, there have been inconsistent findings regarding the effects of surgery on lung volumes in AIS patients.57-59 Fujita et al 39 provided more specific recommendations, concluding that a fusion area of more than 11 vertebral segments may lead to a reduction in postoperative lung volume in AIS patients undergoing PSF. The effects of the coronal, sagittal and rotational deformities in AIS on the static and dynamic aspects of respiration are challenging to measure in isolation.50,52,60-63 Consequently, it can be argued that inadequate deformity correction may contribute to the impairment of PFTs. The addition of TP to improve rib hump height might also indicate insufficient major deformity correction after the primary procedure. It is unclear whether the deterioration in PFTs could be attributed to inadequate correction and derotation of the deformity or the effects of thoracoplasty. Our analysis cannot shed any further light on this question, and further studies are needed to explore these issues.
Conclusion
In conclusion, this systematic review and meta-analysis showed significant deterioration in %FVC after Posterior Spinal Fusion with Thoracoplasty and a small but significant improvement in %FEV1 after Posterior Spinal Fusion only. Posterior Spinal Fusion only and Posterior Spinal Fusion with Thoracoplasty had no significant effects on %FVC and %FEV1, respectively. This was noted in AIS patients with moderate curves with a minimum 2-year follow-up. Based on these findings, we recommend that the use of thoracoplasty be restricted in any patient with underlying cardiopulmonary illness. We also recommend that future studies include participants with longer follow-ups, similar perioperative physical therapy regimes, and treatment with similar techniques and instrumentation. These factors may help reduce heterogeneity amongst the current literature and provide surgeons and patients with better evidence to choose the most suitable treatment option.
Supplemental Material
Supplemental Material for What Are the Effects of Posterior Corrective Surgery, With or Without Thoracoplasty, on Pulmonary Function in Adolescent Idiopathic Scoliosis? A Systematic Review and Meta-analysis by Henry Turner, Robin McManus, and Pat Kiely
Supplemental Material for What Are the Effects of Posterior Corrective Surgery, With or Without Thoracoplasty, on Pulmonary Function in Adolescent Idiopathic Scoliosis? A Systematic Review and Meta-analysis by Henry Turner, Robin McManus, and Pat Kiely
Acknowledgments
The authors would like to thank Fiona Boland, PhD for her assistance with the statistical analysis in this review.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Data Access and Responsibility: The principal investigator, Henry Turner, had full access to all of the data in the study and takes responsibility for the integrity and the data analysis accuracy.
Supplemental Material: Supplemental material for this article is available online.
ORCID iD
Henry Turner https://orcid.org/0000-0002-9023-5377
References
- 1.Wang L, Wang YP, Yu B, et al. Relation between self-image score of SRS-22 with deformity measures in female adolescent idiopathic scoliosis patients. J Orthop Traumatol: Surgery & Research. 2014;100(7):797-801. [DOI] [PubMed] [Google Scholar]
- 2.Erkula G, Sponseller PD, Kiter AE. European spine journal : official publication of the European Spine Society, the European Spinal Deformity Society; 2003:281-287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Duray C, Ferrero E, Julien-Marsollier F, et al. Pulmonary Function After Convex Thoracoplasty in Adolescent Idiopathic Scoliosis Patients Treated by Posteromedial Translation. Spine Deform. 2019;7(5):734-740. [DOI] [PubMed] [Google Scholar]
- 4.Chen SH, Huang TJ, Lee YY, Hsu RW. Pulmonary function after thoracoplasty in adolescent idiopathic scoliosis. Clin Orthop Relat Res. 2002;399:152-161. [DOI] [PubMed] [Google Scholar]
- 5.Suk SI, Kim JH, Kim SS, Lee JJ, Han YT. Thoracoplasty in thoracic adolescent idiopathic scoliosis. Spine. 2008;33(10):1061-1067. [DOI] [PubMed] [Google Scholar]
- 6.Geissele AE, Ogilvie JW, Cohen M, Bradford DS. Thoracoplasty for the treatment of rib prominence in thoracic scoliosis. Spine. 1994;19(14):1636-1642. [DOI] [PubMed] [Google Scholar]
- 7.Cheng JC, Castelein RM, Chu WC, et al. Adolescent idiopathic scoliosis. Nat Rev Dis Prim. 2015;1:15030. [DOI] [PubMed] [Google Scholar]
- 8.Weinstein SL, Dolan LA, Cheng JC, Danielsson A, Morcuende JA. Adolescent idiopathic scoliosis. Lancet. 2008;371(9623):1527-1537. [DOI] [PubMed] [Google Scholar]
- 9.Bjerkreim I, Steen H, Brox JI. Idiopathic scoliosis treated with Cotrel-Dubousset instrumentation: evaluation 10 years after surgery. Spine. 2007;32(19):2103-2110. [DOI] [PubMed] [Google Scholar]
- 10.Harvey CJ, Jr., Betz RR, Clements DH, Huss GK, Clancy M. Are there indications for partial rib resection in patients with adolescent idiopathic scoliosis treated with Cotrel-Dubousset instrumentation? Spine (Phila Pa. 1976;18(12):1593-1598. [DOI] [PubMed] [Google Scholar]
- 11.Głowacki M, Misterska E. Comparison of results of Cotrel-Dubousset instrumentation with partial rib resection at curve apex and without resection treatment based on the Scoliosis Research Society questionnaire. Ortop Traumatol Rehabil. 2009;11(6):520-529. [PubMed] [Google Scholar]
- 12.Chunguang Z, Yueming S, Limin L, et al. Convex short length rib resection in thoracic adolescent idiopathic scoliosis. J Pediatr Orthop. 2011;31(7):757-763. [DOI] [PubMed] [Google Scholar]
- 13.Samdani AF, Hwang SW, Miyanji F, et al. Direct Vertebral Body Derotation, Thoracoplasty, or Both: Which Is Better With Respect to Inclinometer and Scoliosis Research Society-22 Scores? Spine. 2012;37(14). [DOI] [PubMed] [Google Scholar]
- 14.Yang JH, Bhandarkar AW, Modi HN, et al. Short apical rib resections thoracoplasty compared to conventional thoracoplasty in adolescent idiopathic scoliosis surgery. Eur Spine J. 2014;23(12):2680-2688. [DOI] [PubMed] [Google Scholar]
- 15.Yu B, Zhao D, Wang F, et al. Effectiveness and safety of a modified (rib ends fixed under transverse process) thoracoplasty for rib hump deformity in adults with severe thoracic scoliosis: A retrospective study. Medicine (Baltim). 2020;99(39):e22426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Harding IJ, Chopin D, Charosky S, Vialle R, Carrizo D, Delecourt C. Long-term results of Schollner costoplasty in patients with idiopathic scoliosis. Spine. 2005;30(14):1627-1631. [DOI] [PubMed] [Google Scholar]
- 17.Mazda K, Ilharreborde B, Even J, Lefevre Y, Fitoussi F, Penneçot GF. Efficacy and safety of posteromedial translation for correction of thoracic curves in adolescent idiopathic scoliosis using a new connection to the spine: the Universal Clamp. Eur Spine J. 2009;18(2):158-169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Min K, Waelchli B, Hahn F. Primary thoracoplasty and pedicle screw instrumentation in thoracic idiopathic scoliosis. Eur Spine J. 2005;14(8):777-782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Vedantam R, Lenke LG, Bridwell KH, Haas J, Linville DA. A prospective evaluation of pulmonary function in patients with adolescent idiopathic scoliosis relative to the surgical approach used for spinal arthrodesis. Spine (Phila Pa. 1976;25(1):82-90. [DOI] [PubMed] [Google Scholar]
- 20.Lee ACH, Feger MA, Singla A, Abel MF. Effect of Surgical Approach on Pulmonary Function in Adolescent Idiopathic Scoliosis Patients: A Systemic Review and Meta-analysis. Spine (Phila Pa. 1976;41(22):43-55. [DOI] [PubMed] [Google Scholar]
- 21.Akazawa T, Kotani T, Sakuma T, et al. Pulmonary Function Improves in Patients with Adolescent Idiopathic Scoliosis who Undergo Posterior Spinal Fusion Regardless of Thoracoplasty: A Mid-Term Follow-Up. Spine Surg Relat Res. 2021;5(1):22-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Greggi T, Bakaloudis G, Fusaro I, et al. Pulmonary function after thoracoplasty in the surgical treatment of adolescent idiopathic scoliosis. J Spinal Disord Tech. 2010;23(8):e63-e69. [DOI] [PubMed] [Google Scholar]
- 23.Kato S, Murray JC, Ganau M, Tan Y, Oshima Y, Tanaka S. Does Posterior Scoliosis Correction Improve Respiratory Function in Adolescent Idiopathic Scoliosis? A Systematic Review and Meta-analysis. Global Spine J. 2019;9(8):866-873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Piccioni P, Tassinari R, Carosso A, Carena C, Bugiani M, Bono R. Lung function changes from childhood to adolescence: a seven-year follow-up study. BMC Pulm Med. 2015;15:31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Quanjer PH, Stanojevic S, Cole TJ, et al. Multi-ethnic reference values for spirometry for the 3-95-yr age range: the global lung function 2012 equations. Eur Respir J. 2012;40(6):1324-1343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Stanojevic S, Wade A, Stocks J. Reference values for lung function: past, present and future. Eur Respir J. 2010;36(1):12-19. [DOI] [PubMed] [Google Scholar]
- 27.Wang X, Dockery DW, Wypij D, et al. Pulmonary function growth velocity in children 6 to 18 years of age. Am Rev Respir Dis. 1993;148(6 Pt 1):1502-1508. [DOI] [PubMed] [Google Scholar]
- 28.Cumpston M, Li T, Page MJ, et al. Updated guidance for trusted systematic reviews: a new edition of the Cochrane Handbook for Systematic Reviews of Interventions. Cochrane Database Syst Rev. 2019;10:Ed000142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Agabegi SS, Kazemi N, Sturm PF, Mehlman CT. Natural History of Adolescent Idiopathic Scoliosis in Skeletally Mature Patients: A Critical Review. J Am Acad Orthop Surg. 2015;23(12):714-723. [DOI] [PubMed] [Google Scholar]
- 31.Weinstein SL. The Natural History of Adolescent Idiopathic Scoliosis. J Pediatr Orthop. 2019;39(Issue 6 Suppl 1):4-6. [DOI] [PubMed] [Google Scholar]
- 32.Weinstein SL, Dolan LA. The Evidence Base for the Prognosis and Treatment of Adolescent Idiopathic Scoliosis: The 2015 Orthopaedic Research and Education Foundation Clinical Research Award. J Bone Joint Surg Am. 2015;97(22):1899-1903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Weiss H-R, Karavidas N, Moramarco M, Moramarco K. Long-Term Effects of Untreated Adolescent Idiopathic Scoliosis: A Review of the Literature. Asian spine journal. 2016;10(6):1163-1169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sterne JA, Hernán MA, Reeves BC, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 2016;355:i4919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.McGuinness LA, Higgins JPT. Risk-of-bias VISualization (robvis): An R package and Shiny web app for visualizing risk-of-bias assessments. Res Synth Methods. 2021;12(1):55-61. [DOI] [PubMed] [Google Scholar]
- 36.Marx RG, Wilson SM, Swiontkowski MF. Updating the assignment of levels of evidence. J Bone Joint Surg Am. 2015;97(1):1-2. [DOI] [PubMed] [Google Scholar]
- 37.Guyatt GH, Oxman AD, Vist GE, et al. GRADE: An emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336(7650):924-926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Byun YM, Iida T, Yamada K, et al. Long-term pulmonary function after posterior spinal fusion in main thoracic adolescent idiopathic scoliosis. PLoS One. 2020;15(6):e0235123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Fujita N, Yagi M, Michikawa T, et al. Impact of fusion for adolescent idiopathic scoliosis on lung volume measured with computed tomography. Eur Spine J. 2019;28(9):2034-2041. [DOI] [PubMed] [Google Scholar]
- 40.Jeans KA, Lovejoy JF, Karol LA, McClung AM. How Is Pulmonary Function and Exercise Tolerance Affected in Patients With AIS Who Have Undergone Spinal Fusion? Spine Deform. 2017;5(6):416-423. [DOI] [PubMed] [Google Scholar]
- 41.Kim YJ, Lenke LG, Bridwell KH, Cheh G, Whorton J, Sides B. Prospective pulmonary function comparison following posterior segmental spinal instrumentation and fusion of adolescent idiopathic scoliosis: is there a relationship between major thoracic curve correction and pulmonary function test improvement? Spine (Phila Pa. 1976;32(24):2685-2693. [DOI] [PubMed] [Google Scholar]
- 42.Min K, Jud L, Farshad M. Dual Sequential Short Anterior Correction in Double Major Adolescent Idiopathic Scoliosis. Spine Deform. 2018;6(5):545-551. [DOI] [PubMed] [Google Scholar]
- 43.Nohara A, Kawakami N, Saito T, et al. Comparison of Surgical Outcomes Between Anterior Fusion and Posterior Fusion in Patients With AIS Lenke Type 1 or 2 that Underwent Selective Thoracic Fusion -Long-term Follow-up Study Longer Than 10 Postoperative Years. Spine (Phila Pa. 1976;40(21):1681-1689. [DOI] [PubMed] [Google Scholar]
- 44.Pehrsson K, Danielsson A, Nachemson A. Pulmonary function in adolescent idiopathic scoliosis: a 25 year follow up after surgery or start of brace treatment. Thorax. 2001;56(5):388-393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Verma K, Lonner BS, Kean KE, Dean LE, Valdevit A. Maximal pulmonary recovery after spinal fusion for adolescent idiopathic scoliosis: how do anterior approaches compare? Spine (Phila Pa. 1976;36(14):1086-1095. [DOI] [PubMed] [Google Scholar]
- 46.Yaszay B, Jankowski PP, Bastrom TP, et al. Progressive decline in pulmonary function 5 years post-operatively in patients who underwent anterior instrumentation for surgical correction of adolescent idiopathic scoliosis. Eur Spine J. 2019;28(6):1322-1330. [DOI] [PubMed] [Google Scholar]
- 47.Yuan W, He X, Xu Q-F, Wang H-Y, Casaburi R. Increased difference between slow and forced vital capacity is associated with reduced exercise tolerance in COPD patients. BMC Pulm Med. 2014;14:16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Lenke LG, Bridwell KH, Blanke K, Baldus C. Analysis of pulmonary function and chest cage dimension changes after thoracoplasty in idiopathic scoliosis. Spine (Phila Pa. 1976;20(12):1343-1350. [PubMed] [Google Scholar]
- 49.Gitelman Y, Lenke LG, Bridwell KH, Auerbach JD, Sides BA. Pulmonary function in adolescent idiopathic scoliosis relative to the surgical procedure: a 10-year follow-up analysis. Spine (Phila Pa. 1976;36(20):1665-1672. [DOI] [PubMed] [Google Scholar]
- 50.Vedantam R, Crawford AH. The role of preoperative pulmonary function tests in patients with adolescent idiopathic scoliosis undergoing posterior spinal fusion. Spine (Phila Pa. 1976;22(23):2731-2734. [DOI] [PubMed] [Google Scholar]
- 51.Sherman B, Madi P, Aminian A. The effects of thoracoplasty on immediate post-operative recovery in adolescent idiopathic scoliosis. Eur Spine J. 2021;30(3):733-739. [DOI] [PubMed] [Google Scholar]
- 52.Newton PO, Faro FD, Gollogly S, Betz RR, Lenke LG, Lowe TG. Results of preoperative pulmonary function testing of adolescents with idiopathic scoliosis. A study of six hundred and thirty-one patients. J Bone Joint Surg Am. 2005;87(9):1937-1946. [DOI] [PubMed] [Google Scholar]
- 53.Farrell J, Garrido E. Effect of idiopathic thoracic scoliosis on the tracheobronchial tree. BMJ Open Respir Res. 2018;5(1):e000264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Kono K, Asazuma T, Suzuki N, Ono T. Body Height Correction in Scoliosis Patients for Pulmonary Function Test. J Orthop Surg. 2000;8(1):19-26. [DOI] [PubMed] [Google Scholar]
- 55.Bjure J, Grimby G, Nachemson A. Correction of body height in predicting spirometric values in scoliotic patients. Scand J Clin Lab Invest. 1968;21(2):190-192. [PubMed] [Google Scholar]
- 56.Weir CJ, Butcher I, Assi V, et al. Dealing with missing standard deviation and mean values in meta-analysis of continuous outcomes: a systematic review. BMC Med Res Methodol. 2018;18(1):25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Fu J, Liu C, Zhang YG, et al. Three-dimensional computed tomography for assessing lung morphology in adolescent idiopathic scoliosis following posterior spinal fusion surgery. Orthop Surg. 2015;7(1):43-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Sarwahi V, Sugarman EP, Wollowick AL, Amaral TD, Harmon ED, Thornhill B. Scoliosis surgery in patients with adolescent idiopathic scoliosis does not alter lung volume: a 3-dimensional computed tomography-based study. Spine (Phila Pa. 1976;39(6):E399-E405. [DOI] [PubMed] [Google Scholar]
- 59.Wood KB, Schendel MJ, Dekutoski MB, Boachie-Adjei O, Heithoff KH. Thoracic volume changes in scoliosis surgery. Spine. 1996;21(6):718-723. [DOI] [PubMed] [Google Scholar]
- 60.Kotani T, Minami S, Takahashi K, et al. An analysis of chest wall and diaphragm motions in patients with idiopathic scoliosis using dynamic breathing MRI. Spine (Phila Pa. 1976;29(3):298-302. [DOI] [PubMed] [Google Scholar]
- 61.Chu WC, Li AM, Ng BK, et al. Dynamic magnetic resonance imaging in assessing lung volumes, chest wall, and diaphragm motions in adolescent idiopathic scoliosis versus normal controls. Spine. 2006;31(19):2243-2249. [DOI] [PubMed] [Google Scholar]
- 62.Romberg K, Fagevik Olsén M, Kjellby-Wendt G, Lofdahl Hallerman K, Danielsson A. Thoracic mobility and its relation to pulmonary function and rib-cage deformity in patients with early onset idiopathic scoliosis: a long-term follow-up. Spine Deform. 2020;8(2):257-268. [DOI] [PubMed] [Google Scholar]
- 63.Johnston CE, Richards BS, Sucato DJ, Bridwell KH, Lenke LG, Erickson M. Correlation of preoperative deformity magnitude and pulmonary function tests in adolescent idiopathic scoliosis. Spine (Phila Pa. 1976;36(14):1096-1102. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material for What Are the Effects of Posterior Corrective Surgery, With or Without Thoracoplasty, on Pulmonary Function in Adolescent Idiopathic Scoliosis? A Systematic Review and Meta-analysis by Henry Turner, Robin McManus, and Pat Kiely
Supplemental Material for What Are the Effects of Posterior Corrective Surgery, With or Without Thoracoplasty, on Pulmonary Function in Adolescent Idiopathic Scoliosis? A Systematic Review and Meta-analysis by Henry Turner, Robin McManus, and Pat Kiely