Objectives
Contingency management (CM) is one of the most effective treatments for stimulant use disorder but has not been leveraged for people with stimulant-associated cardiomyopathy (SA-CMP), a chronic health condition with significant morbidity and mortality. We aimed to determine the feasibility and acceptability of a multidisciplinary addiction/cardiology clinic with CM for patients with SA-CMP and to explore barriers and facilitators to engagement and recovery.
Methods
We recruited patients with a hospitalization in the past 6 months, heart failure with reduced ejection fraction (<40%) and stimulant use disorder to participate in Heart Plus, a 12-week addiction/cardiology clinic with CM in an urban, safety-net, hospital-based cardiology clinic, which took place March 2021 through June 2021. Contingency management entailed gift card rewards for attendance and negative point-of-care urine drug screens. Our mixed-methods study used the Reach, Effectiveness, Adoption, Implementation, and Maintenance framework. We obtained data from the medical record, staff surveys, and qualitative interviews with participants.
Results
Thirty-eight patients were referred, 17 scheduled an appointment, and 12 attended the intake appointment and enrolled in the study. Mean treatment duration was 8 of 12 weeks. Of the 9 participants who attended more than one visit, the median attendance was 82% of available visits for in-person visits and 83% for telephone visits, and all patients reported decreased stimulant use.
Conclusions
Delivering CM through a multidisciplinary addiction/cardiology clinic for patients with SA-CMP was feasible and engaged patients in care. Further research is needed to assess whether this program is associated with improved heart failure outcomes.
Key Words: heart failure, stimulant use disorder, methamphetamine, contingency management
Stimulant use, especially that of methamphetamine, is increasing with a corresponding rise in adverse health effects.1–4 It is associated with a myriad of cardiovascular conditions, including cardiomyopathy.5–7 Patients with stimulant-associated cardiomyopathy (SA-CMP) have high rates of morbidity, mortality, and acute care presentations related to heart failure (HF).8,9 From 2008 to 2018, there was a 600% increase in hospitalizations for methamphetamine-associated HF in California.10 The use of guideline directed medical therapy (GDMT) for patients with HF improves mortality and decreases hospitalizations but requires engagement in outpatient care, which is low among patients with SA-CMP.11,12
Stimulant abstinence improves cardiac function and reduces hospital admissions in patients with SA-CMP.13,14 Although no Food and Drug Administration–approved medications for stimulant use disorder exist, there are highly effective behavioral treatments, including contingency management (CM).15–18 Contingency management involves reinforcing a target behavior through a reward-based system.18–20 A meta-analysis demonstrates that CM has the greatest effect size out of all psychosocial treatments for substance use disorders.21 Although CM is cost-effective and increases abstinence and retention in treatment, most insurance programs do not provide reimbursement.22–24
It is recommended that patients with SA-CMP discontinue stimulant use, but there is no published literature on stimulant use disorder treatment for this high-risk population.8 Traditionally, addiction and cardiology care are siloed, and patients access services independently. To improve access and care integration, we created a multidisciplinary addiction/cardiology clinic with CM named Heart Plus.
This study aims to use mixed methods to determine the feasibility and acceptability of an addiction/cardiology clinic with CM for patients with SA-CMP.
METHODS
Setting
This study took place at a safety-net, hospital-based cardiology clinic located in San Francisco, CA. Patients have public insurance (Medicaid and/or Medicare) or are uninsured.
Program Description
We initially designed Heart Plus to be a 12-week program with twice weekly in-person visits to coincide with the half-life of stimulants in urine (approximately 48 hours) with a reward system adapted from conventional CM programs.25 Because of a COVID-19 hospital directive to reduce in-person visits, we pivoted to include one in-person visit and one telephone visit weekly, with each visit separated by 3 days. At each visit, the patient met with an addiction medicine physician (E.A. or S.A.) to discuss substance use, HF symptoms, and medication adherence. In-person visits also included vital signs, a cardiovascular examination, and an optional point-of-care urine drug screen (POC UDS) with the Accutest Drug Test Cup 12 Panel (CLIA Waived Product # JANDS823). If the POC UDS was inconsistent with the patient’s reported stimulant use, the physician ordered confirmatory urine toxicology via mass spectrometry. Because confirmatory results were not immediately available, CM was still based on the POC UDS results. During each visit, the addiction physician provided CM using a variable magnitude of reinforcement (eg, “fishbowl”) system.25 Participants earned increasing numbers of prize draws for attendance or POC UDS negative for stimulants. These were decoupled so participants could earn increasing draws for attendance, regardless of whether they submitted a POC UDS. Rewards included affirmations and gift cards ranging from $5 to $100 (Fig. 1).
FIGURE 1.
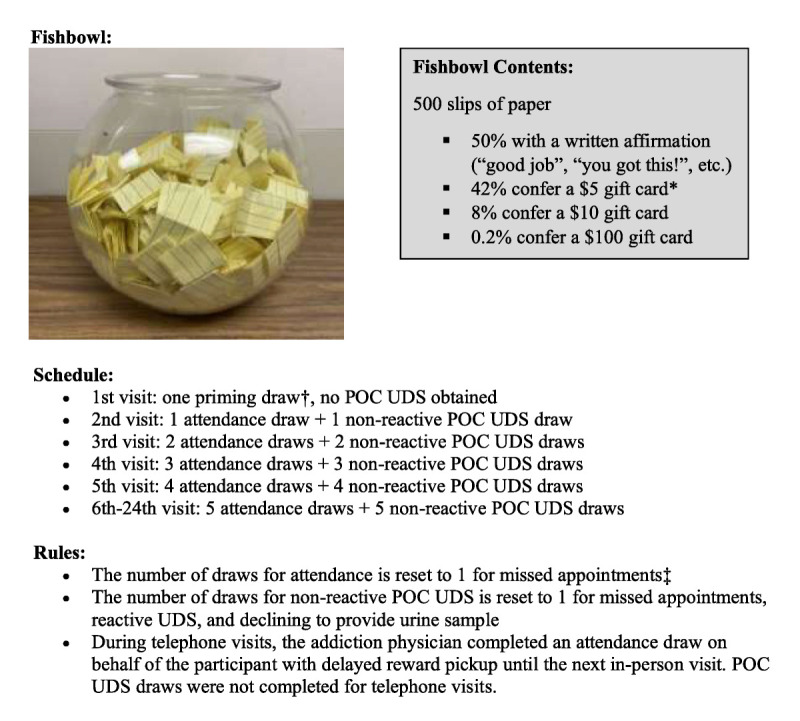
Fishbowl contents and schedule of maximum rewards for attendance and POC UDS.
We scheduled patients to see the cardiologist (J.D.) for medication management every other week; however, the addiction physician could refer for immediate care if necessary.
Patient Participants
We included participants with HF with reduced ejection fraction (ejection fraction <40%), stimulant use disorder (diagnosed via Diagnostic and Statistical Manual of Mental Disorders criteria), hospitalization in the last 6 months, and interest in reducing or discontinuing stimulant use. We excluded participants residing in skilled nursing facilities and residential treatment programs, and those without a telephone.
We recruited participants by asking clinicians to refer eligible patients to the Heart Plus lead, an addiction medicine physician. The addiction physician called or visited the patient in the hospital for screening and scheduled patients for an intake visit. We recruited patients from September of 2020 to February 2021, and we conducted the Heart Plus pilot March to June 2021. We consented all participants at the initial clinic visit. The institutional review board of the University of California, San Francisco, approved this study.
Program Evaluation
We completed a mixed-methods study, using the Reach, Effectiveness, Adoption, Implementation, and Maintenance framework (Table 1).26
TABLE 1.
Reach, Effectiveness, Adoption, Implementation, Maintenance Framework Applied to Heart Plus: A Multidisciplinary Addiction/Cardiology Clinic for Patients with Active Stimulant Use Disorder and SA-CMP
| Framework | Question | Results |
|---|---|---|
| Reach | Will adults with SA-CMP and stimulant use disorder enroll in Heart Plus? | 17 of patients (45%) who were referred for the program were reachable and chose to enroll |
| Will adults with SA-CMP and stimulant use disorder scheduled for a Heart Plus visit attend their initial appointment? | 12 of patients (71%) scheduled for a Heart Plus visit attended their initial appointment | |
| Effectiveness | Will adults with SA-CMP and stimulant use disorder engage in treatment with Heart Plus? | Before Heart Plus, none of the participants were engaged in care (defined as 3 or more visits in a 3-mo period.) During Heart Plus, 75% of participants were engaged in care. The mean treatment duration was 8 of 12 weeks. |
| Will engaged patients reduce or stop stimulant use? | All participants who attended >1 Heart Plus visit reported reduced stimulant use A median of 2 POC UDS were submitted per patient (out of 12 opportunities to submit a test); 89% of submitted POC UDS were nonreactive for stimulants. |
|
| Adoption | Will providers refer their eligible patients to Heart Plus? | 95% of surveyed staff and providers reported that a combined addiction/cardiology program would be moderately or extremely useful for patients with SA-CMP |
| Implementation | What were the costs and adaptations made to Heart Plus? | Cost of CM = $1690 total. Over the duration of the 3-mo program, the cost was $1.56 per patient per day. No adaptations were made during this initial pilot |
| Maintenance | Not evaluated in this pilot study | |
SA-CMP indicates stimulant-associated cardiomyopathy.
We used several data sources. First, we distributed a survey January 2020 to February 2020 to clinicians and staff to assess acceptability of our program (Appendix 1, http://links.lww.com/JAM/A394). We asked leadership in each department to distribute the survey via email listservs.
Second, we extracted data from the medical record. Demographics included the following: age, gender, sex, and race/ethnicity. Other data included the following: comorbid health status using the Charlson Comorbidity Index (CCI), cardiology clinic attendance (number of visits attended in the 3 months preceding, during, and after the pilot), acute care utilization (number of emergency department and hospital admissions in the 3 months preceding, during, and after the pilot), comorbid cardiovascular diseases, cardiac ejection fraction, and American College of Cardiology and New York Heart Association class designation. Substance use history was collected during the intake visit. We also determined Heart Plus outcomes, including percent of in-person visits with UDS nonreactive for stimulants and CM earnings. We defined engagement in care as 3 or more visits attended in a three-month period.
Third, we conducted 30- to 60-minute interviews to assess patient perspectives on Heart Plus, including acceptability, feasibility, effectiveness, and appropriateness of the program. Researchers (L.W.S., A.M.) contacted all participants to schedule an in-person, audio-recorded, semistructured interview, and made at least 3 attempts to contact participants. Interviews used a semistructured guide (see Appendix 3, http://links.lww.com/JAM/A394) to probe for participants’ experience.
Data Analysis
We analyzed descriptive statistics using Stata 16 (College Station, TX). For qualitative analysis, we used a matrix-based analysis technique.27,28 Three analysts (AM, LS, SL) separately completed a templated matrix organized by pre-determined topics while listening to audio-recordings of the interview. Topics included care experiences before, during, and after Heart Plus, barriers to engagement, and suggestions for improvement. Analysts identified relevant domains from the interview, recorded quotations for each domain, and created a summary for each interview. At least 2 analysts coded each interview. The research team then compared completed matrices, discussed themes, reconciled differences, and refined data based on consensus.
RESULTS
Reach: Participant Enrollment and Participant Demographics
Clinicians referred 38 patients to Heart Plus in 2021; 17 were reachable, agreed to participate, and scheduled an intake visit. Twelve patients attended their intake visit and provided informed consent (Table 2). At least 3 attempts were made to reschedule patients who missed their initial appointment.
TABLE 2.
Demographic Characteristics of Individuals with Active Stimulant Use Disorder and Stimulant-Associated Cardiomyopathy Who Attended at Least One Heart Plus Visit (n = 12)
| Characteristic | Median (IQR) or n (%) |
|---|---|
| Age, yr | 59 (12.8) |
| Gender | |
| Cisgender female | 1 (8%) |
| Cisgender male | 11 (92%) |
| Race/ethnicity | |
| Asian/Pacific Islander/Filipinx | 4 (33%) |
| Black/African-American | 6 (50%) |
| Hispanic/Latinx | 0 (0%) |
| White | 2 (17%) |
| Housing status | |
| Stably housed (eg, living in a house or apartment) | 2 (17%) |
| Marginally housed (eg, living in a Shelter-In-Place hotel* or in transitional housing) | 8 (75%) |
| Staying with friends/relatives | 1 (8%) |
| Staying in a shelter | 1 (8%) |
| Unsheltered (eg, living in a vehicle or outside) | 0 (0%) |
| Documented comorbidities | |
| Diabetes | 4 (33%) |
| History of myocardial infarction | 4 (33%) |
| History of stroke | 4 (33%) |
| Hypertension (stage 2 or higher) | 11 (92%) |
| Chronic kidney disease (stage 2 or higher) | 3 (25%) |
| CCI | 4.5 (2.5) |
| NYHA Class at baseline | |
| Class I | 0 (0%) |
| Class II | 2 (17%) |
| Class III | 10 (83%) |
| Class IV | 0 (0%) |
| Ejection Fraction at Baseline | 29 (15.3) |
| Stimulant use at baseline | |
| Predominantly methamphetamine | 9 (75%) |
| Predominantly cocaine | 3 (25%) |
| Co-occurring substance use | |
| Alcohol | 1 (8%) |
| Heroin | 2 (17%) |
| Tobacco | 5 (42%) |
*Shelter-in-Place hotels were provided by the city of San Francisco starting March 2020 to temporarily house people living unsheltered and isolate people in overcrowded congregate settings (shelters) during the COVID-19 pandemic.
IQR indicates interquartile range; NYHA, New York Heart Association
Among the 12 participants, the mean age was 56 years, and the majority (92%) were male and identified as people of color (50% Black, 33% Filipinx, and 17% White). Most (83%) were marginally housed or experiencing homelessness. Three-quarters of participants used methamphetamine and 25% used cocaine. The median cardiac ejection fraction at baseline was 29%. Participants had multiple comorbidities, with median CCI of 4.5. All participants had American College of Cardiology Class C, with 83% with New York Heart Association Stage III, and 17% with Stage II (Table 2).
Effectiveness: Participant Engagement, Acceptability, and Stimulant Use
Heart Plus Clinic Attendance
All but one participant had been referred to outpatient cardiology in the past. In the 3 months before Heart Plus, only 3 participants (25%) attended visits in cardiology clinic, and none met engagement criteria (3 or more visits during a 3-month period). During Heart Plus, mean treatment duration was 8 of 12 weeks. Three participants (25%) attended only the intake visit, 2 of whom were discharged from an admission and escorted by staff directly to Heart Plus clinic. Seventy-five percent (n = 9) of participants met criteria for care engagement during the 3-month Heart Plus pilot with a median of 18 visits attended (9 telephone visits and 9 in-person visits.) Two participants attended all available visits. The 9 participants who attended more than 1 visit had median attendance of 83% for telephone visits and 82% for in-person visits. Participants saw the cardiologist a median of 2 visits. In the 3 months after Heart Plus, 5 participants (42%) attended at least one cardiology visit and 1 participant (8%) met engagement criteria with 3 visits (Fig. 2.)
FIGURE 2.
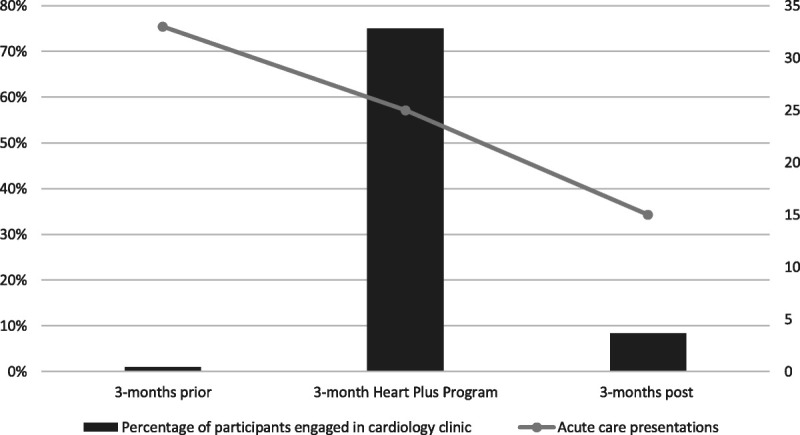
Percentage of participants engaged in outpatient cardiology care (defined as attending 3 or more visits during a three-month period) and acute care presentations (ie, hospitalizations or emergency department visits) before, during, and after the Heart Plus pilot clinic.
Stimulant Use Outcomes
During the Heart Plus pilot, one participant reported abstinence from stimulants with consistently nonreactive POC UDS, while all patients who attended more than 1 visit reported reduced use. Participants infrequently chose to submit POC UDS; a median of 2 tests were submitted per patient out of a median of 12 possible in-person visits (16.7% of visits). Four participants chose not to submit any POC UDS. Of those POC UDS submitted, 89% were nonreactive for stimulants. No samples were sent for confirmatory testing.
Acute Care Utilization (Emergency Department or Hospital Admissions)
In the 3 months before Heart Plus, all 12 participants had a total number of 33 acute care presentations. During Heart Plus, 7 participants used acute care services (25 presentations). Almost two-thirds of the acute care presentations during Heart Plus were from the 3 participants who only attended the intake visit. In the 3 months after Heart Plus, 9 participants used acute care services with a total of 15 presentations (Fig. 2).
Patient Perspectives
Half of the participants completed qualitative interviews. The interviews revealed the following themes (see Table 3 for representative quotes):
TABLE 3.
Themes From In-depth Qualitative Interviews with Participants with Active Stimulant Use Disorder and Stimulant-associated Cardiomyopathy Who Attended at Least One Heart Plus Visit (n = 6)
| Theme #1: Nonstigmatizing patient-provider relationships are essential and ameliorate prior negative experiences with the healthcare system to increase trust and build self-efficacy | “This program helped me to start trusting in hospitals more and trusting in doctors more because I used to think, they used to use people like me like guinea pigs. Like throw medication at me and don’t really know what it’s going to do, stuff like that.” (Participant A) “It’s like, here’s a group of people who don’t even know me. They’re just meeting me. They have this program. Are they full of shit or are they on some real shit? And, I was like, okay, let’s find out. And, we’re all characters, or actors, so it’s like, to have a people who give a damn, and don’t judge you, because of what you do or your lifestyle, that’s a miracle and a blessing in itself. Because, like I said, it’s like “hey we’re here for you. We can help you, but you gotta help us…” And to see people give a damn, it’s like wait a minute. They care so much about me, maybe I should care about me.” (Participant B) “Before [Heart Plus], I don’t think about hope. I don’t believe in hope. Before, I was like, oh man, I’m gonna die here. I’m thinking about, like, jumping into the Bridge or the Golden Gate Bridge. Because there’s no more tomorrow for me. But when I came here, I see hope for me, you know? There’s change, there’s a chance to change, to be saved.” (Participant C) |
| Theme #2: Heart Plus led to increased medication adherence, decreased substance use, and improved symptom control | “I have a better outlook about some things now…. Like I have to remember every day to take my meds now. Before, it was like, I take them or I don’t. I don’t like when something is in control of me. Definitely don’t want to be anybody’s tool.” (Participant B) “[My doctor] said now [that] I’m getting old, I’m not young anymore, and no one can take care of me. I have to take care of myself... I told her, “I promise you, I want to take out [all of the drugs], step by step.” And, I took out smoking, drugs, I don’t drink... I appreciate what [my doctor] did for my life.” (Participant D) “I’ve found that my cravings for using drugs is fading away. I didn’t know that I would be like that. When I came here [to Heart Plus clinic], I noticed that “Oh, I don’t crave that much. Today I’m clean. I’m supposed to be getting high.” You know, this is not me, right? I noticed that my using is fading away. Hopefully it’ll be for good.” (Participant C) “Before I couldn’t even walk half a block. Now I could walk two blocks. I could go walking or riding the bike or riding the bus, you know? Before I can’t walk half a block, I gotta catch my breath. I’ll be hella tired. I’m like, “What’s going on?” The doctor explained: your heart is very tired, your heart is weak. You need to take this medicine to let your heart go back to what it used to be.” (Participant C) |
| Theme #3: Participants want a longer program with more frequent visits | “I’m not indulging as much. I’m still on a path to where I’m trying to eliminate it. I think if it had been longer I probably woulda been stopped by now.” (Participant E) “Every week I was coming up here being seen, where now I gotta wait a month or two to see my primary doctor. It was too short. It should be as long as you pretty much allow it to be. It [shouldn’t] have no cutoff point or no graduation really. That program was real good, I hate that it ended like that.” (Participant A) “Would be better if it was 5 days a week. You only give me 2 days, you know? It’d be better if it was 5 days… just 2 days, that’s not enough. We have 7 days a week, right? And then, we only be here 1 hour, 2 hours, and the rest is free. What do you do with your life? Whatever happen in the street, you know? Wish it was five, or four, you know?” (Participant C) |
| Theme #4: Targeting social determinants of health and substance use (stress, poverty, trauma, etc) is necessary to help patients achieve their goals around substance use | “Sometimes I want to just disappear. Cause umm. Being responsible is hard. Like I said this life is hard. Struggling to survive is hard. Everything is a hustle. A hustle is how you survive to live every day. And, things shouldn’t be as hard as they are. There should be nobody in this country or in this world that is hungry….” (Participant B) “I was having a lot of issues. I’d almost make it [to the next clinic visit without using], and then issues showed up. Stressful issues, and it sent me back to do what I do.” (Participant E) Participant: “I need [drugs] to function. I’m not a nice person. [laughs] I’m not a nice person when I’m stressed out, anxiety, it’s like I don’t want to talk, I don’t want to think. And, I think we all need some type of escape…. I’ve been coping my entire life.” (Participant B) |
Theme #1: Nonstigmatizing patient-clinician relationships increase trust, build self-efficacy, and ameliorate prior negative experiences with the healthcare system
All 6 participants identified trusting relationships with clinicians, not CM, as the most essential component of Heart Plus. Patients experienced a strong connection with the addiction physician. The nonstigmatizing care they received increased their trust in the healthcare system and motivated them to engage. Most participants preferred in-person visits to telephone visits because it was challenging to build trusting relationships over the phone.
Theme #2: Heart Plus led to increased medication adherence, decreased substance use, and improved symptom control.
Multiple participants were hesitant to take medications because of mistrust in the healthcare system, and as trusting relationships formed during the clinic, they began taking medications regularly. Five participants described decreased cravings and less stimulant use with a desire to continue to work toward abstinence. One participant completely stopped using stimulants and quit smoking cigarettes. Several participants noted positive changes in their diet, quality of life, and symptom control.
Theme #3: Participants want a longer program with more frequent visits.
All participants desired a longer program with more frequent visits. In addition to receiving medical care, Heart Plus was a way for participants to get support and separate themselves from people and situations that trigger substance use.
Theme #4: Targeting social determinants of health is necessary to help patients achieve their goals around substance use.
Although participants were highly motivated to decrease stimulant use, multiple participants described difficulty doing so because of major life stressors, including homelessness, poverty, trauma, and racism. They found Heart Plus helpful but, without greater psychosocial stability, they were not confident they could achieve their goals.
Adoption: Provider Perspectives and Acceptability
Clinician/Staff Survey
Of the 90 respondents who completed the online survey, the majority were physicians (Appendix 2, http://links.lww.com/JAM/A394). Approximately half of respondents were extremely or somewhat dissatisfied with the existing care for patients with SA-CMP. Seventy-nine percent reported that an addiction/cardiology clinic would be moderately or extremely useful, and 78% reported CM as moderately or extremely useful. Seventy-two percent strongly agreed that the program would align with the mission values of the hospital.
Implementation: Program Costs
Individual participants earned between $5 and $400, with a median of $147.50. In total, participants received $1690 in gift cards. The cost was $1.56 per patient per day during the 3-month pilot.
DISCUSSION
Patients with SA-CMP experience significant morbidity and mortality, and there is increasing recognition of the need to provide addiction treatment alongside cardiology care. Our study demonstrates that a pilot addiction/cardiology clinic with CM for patients with SA-CMP is feasible and acceptable to patients and staff. This is the first published attempt to provide integrated, multispecialty care to patients with SA-CMP.
Despite their relatively young age (median, 59 years), participants had advanced HF and significant medical and psychosocial comorbidities. The median CCI score of 4.5 translates to a 10-year survival of only 37%.29 Most patients were experiencing homelessness or marginally housed. Despite historically poor engagement and numerous barriers to care, attendance was comparable to the landmark Veterans Affairs study of CM, which included a more medically and psychosocially stable cohort of patients.25 Mean treatment duration was 8 of 12 possible visits, similar to a multisite randomized trial of CM in community-based outpatient treatment programs.30 Similar to most CM programs, engagement was high during the program and steeply dropped in the months following.31 However, we found that acute care visits decreased steadily during and after Heart Plus participation, and engagement in care in the 3 months after Heart Plus was still higher than in the 3-month period preceding the program.
One patient stopped using stimulants and all patients who attended more than 1 Heart Plus clinic reported decreased use. Point-of-care UDS were optional and infrequently collected, presumably because participants anticipated that the results would be reactive for stimulants. Because one of the main goals of the clinic was to increase engagement, prize draws were available for attendance alone. Future research should explore alternative behaviors to incentivize for patients who aim to cut down or use more safely rather than abstain (eg, participation in harm reduction services, reduced use via buccal swabs, or improvement in volume overload as measured by serial basic natriuretic peptide testing). Harm reduction literature shows that oftentimes behavioral change is incremental; thus, providing appropriately tailored CM to “meet patients where they are at” may be more effective in improving overall health than focusing on abstinence.32
Engagement in clinic allowed GDMT to be titrated. Guideline-directed medical therapy is associated with decreased HF hospitalizations and mortality.11 We did not objectively measure medication adherence, but during interviews, participants described increased trust in the healthcare system leading to regular use of medications. The decrease in acute care presentations in our study is promising, and future research should include controlled studies with the power to detect differences in cardiovascular outcomes, such as basic natriuretic peptide, ejection fraction, HF hospitalizations, and mortality.
Because of COVID-19, half of visits were conducted via phone. Multiple participants reported that trusting relationships were harder to build over the phone. Lost phones and inadequate reception led to decreased participation. Furthermore, telephone visits delayed the receipt of rewards, which may have decreased the efficacy of CM.33 Future iterations of this program will aim to have entirely in-person visits, COVID-19 hospital policies permitting.
Participants desired more frequent visits. It is possible that for this high-risk population, an intensive-outpatient program (more than 9 hours of treatment per week occurring several days of the week, typically in groups) would better meet patients’ needs. Other support could include care from social work, case management, pharmacy, and nursing colleagues.
There were several limitations. Given the high-risk population, the results are unlikely to be generalizable to all settings. The survey distributed to healthcare staff and clinicians may have been subject to response bias, because most respondents were physicians. Although participants reported decreased substance use and increased medication adherence, these were not objectively assessed. Finally, we did not evaluate program maintenance and sustainability.
CONCLUSIONS
The Heart Plus pilot, a multidisciplinary addiction/cardiology clinic with CM for patients with SA-CMP, was feasible and acceptable to patients and staff. Participants were highly engaged in care, and while few patients discontinued stimulant use, most patients decreased drug use and described other positive impacts, such as increased trust in the healthcare system and regular use of medications. This initial pilot should inform larger, controlled studies powered to detect differences in cardiovascular outcomes.
Supplementary Material
ACKNOWLEDGMENTS
The authors thank the patients who participated, San Francisco General Hospital’s Addiction Medicine Patient Navigators, and Richard Fine People’s Clinic.
Footnotes
Supplemental digital content is available for this article. Direct URL citation appears in the printed text and is provided in the HTML and PDF versions of this article on the journal’s Web site (www.journaladdictionmedicine.com).
Supported by the University of San Francisco California Committee of Interns and Residents/Service Employee International Union Patient Care Fund and Centers for Disease Control and Prevention via Public Health Foundation Enterprises grant (#NU50CK000482-03-01).
The authors report no conflicts of interest.
Presented virtually at the national AMERSA Conference in November 8, 2020 and November 4, 2021.
Contributor Information
Elizabeth Abbs, Email: Elizabeth.abbs@sfdph.org.
Leslie W. Suen, Email: leslie.suen@ucsf.edu.
Marlene Martin, Email: marlene.martin@ucsf.edu.
Andreas Mitchell, Email: andreas.mitchell@ucsf.edu.
Jonathan Davis, Email: jonathan.davis@ucsf.edu.
Soraya Azari, Email: soraya.azari@ucsf.edu.
REFERENCES
- 1.Han B Compton WM Jones CM, et al. Methamphetamine use, methamphetamine use disorder, and associated overdose deaths among US adults. JAMA Psychiat. 2021;78(12):1329–1342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hedegaard H Miniño AM Spencer MR, et al. Drug overdose deaths in the United States, 1999–2020. NCHS Data Brief. 2021;426:1–8. [PubMed] [Google Scholar]
- 3.Han B Cotto J Etz K, et al. Methamphetamine overdose deaths in the US by sex and race and ethnicity. JAMA Psychiat. 2021;78(5):564–567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Han B. Key substance use and mental health indicators in the united states: Results from the 2019 National Survey on Drug Use and Health. Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration; 2020. HHS Publication No. PEP20-07-01-001, NSDUH Series H-55.
- 5.Middlekauff HR, Cooper ZD, Strauss SB. Drugs of misuse: Focus on vascular dysfunction. Can J Cardiol. 2022;38(9):1364–1377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dominic P Ahmad J Awwab H, et al. Stimulant drugs of abuse and cardiac arrhythmias. Circ Arrhythm Electrophysiol. 2022;15(1):e010273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gagnon LR Sadasivan C Perera K, et al. Cardiac complications of common drugs of abuse: Pharmacology, toxicology, and management. Can J Cardiol. 2022;38(9):1331–1341. [DOI] [PubMed] [Google Scholar]
- 8.Reddy PKV Ng TMH Oh EE, et al. Clinical characteristics and management of methamphetamine-associated cardiomyopathy: State-of-the-art review. J Am Heart Assoc. 2020;9(11):e016704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Thomas IC Nishimura M Ma J, et al. Clinical characteristics and outcomes of patients with heart failure and methamphetamine abuse. J Card Fail. 2020;26(3):202–209. [DOI] [PubMed] [Google Scholar]
- 10.Zhao SX Deluna A Kelsey K, et al. Socioeconomic burden of rising methamphetamine-associated heart failure hospitalizations in California from 2008 to 2018. Circ Cardiovasc Qual Outcomes. 2021;14(7):e007638. [DOI] [PubMed] [Google Scholar]
- 11.Espinoza C, Alkhateeb H, Siddiqui T. Updates in pharmacotherapy of heart failure with reduced ejection fraction. Ann Transl Med. 2021;9(6):516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.DesJardin J, Leyde S, Davis J. Weathering the perfect storm: Management of heart failure in patients with substance use disorders. Heart. 2021;107(16):1353–1354. [DOI] [PubMed] [Google Scholar]
- 13.Bhatia HS Nishimura M Dickson S, et al. Clinical and echocardiographic outcomes in heart failure associated with methamphetamine use and cessation. Heart. 2021;107(9):741–747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Schürer S Klingel K Sandri M, et al. Clinical characteristics, histopathological features, and clinical outcome of methamphetamine-associated cardiomyopathy. JACC: Heart Failure. 2017;5(6):435–445. [DOI] [PubMed] [Google Scholar]
- 15.Buchholz J, Saxon AJ. Medications to treat cocaine use disorders: Current options. Curr Opin Psychiatry. 2019;32(4):275–281. [DOI] [PubMed] [Google Scholar]
- 16.Siefried KJ Acheson LS Lintzeris N, et al. Pharmacological treatment of methamphetamine/amphetamine dependence: A systematic review. CNS Drugs. 2020;34(4):337–365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ronsley C Nolan S Knight R, et al. Treatment of stimulant use disorder: A systematic review of reviews. Plos One. 2020;15(6):e0234809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Brown HD, DeFulio A. Contingency management for the treatment of methamphetamine use disorder: A systematic review. Drug Alcohol Depend. 2020;216:108307. [DOI] [PubMed] [Google Scholar]
- 19.Davis DR Kurti AN Skelly JM, et al. A review of the literature on contingency management in the treatment of substance use disorders, 2009–2014. Prev Med. 2016;92:36–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tardelli VS Lago MPPD Mendez M, et al. Contingency management with pharmacologic treatment for stimulant use disorders: A review. Behav Res Ther. 2018;111:57–63. [DOI] [PubMed] [Google Scholar]
- 21.Dutra L Stathopoulou G Basden SL, et al. A meta-analytic review of psychosocial interventions for substance use disorders. Am J Psychiatry. 2008;165(2):179–187. [DOI] [PubMed] [Google Scholar]
- 22.Kirby KC, Benishek LA, Tabit MB. Contingency management works, clients like it, and it is cost-effective. Am J Drug Alcohol Abuse. 2016;42(3):250–253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Olmstead TA, Petry NM. The cost-effectiveness of prize-based and voucher-based contingency management in a population of cocaine- or opioid-dependent outpatients. Drug Alcohol Depend. 2009;102(1–3):108–115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Glass J, Nunes E, Bradley K. Contingency management: A highly effective treatment for substance use disorders and the legal barriers that stand in its way. Health Affairs Blog Published March 11, 2020. Available at: https://www.healthaffairs.org/do/10.1377/forefront.20200305.965186/full/. Accessed September 1, 2022.
- 25.Petry NM DePhilippis D Rash CJ, et al. Nationwide dissemination of contingency management: The veterans administration initiative: Nationwide dissemination of contingency management. Am J Addict. 2014;23(3):205–210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gaglio B, Shoup JA, Glasgow RE. The RE-AIM framework: A systematic review of use over time. Am J Public Health. 2013;103(6):e38–e46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Vindrola-Padros C, Johnson GA. Rapid techniques in qualitative research: A critical review of the literature. Qual Health Res. 2020;30(10):1596–1604. [DOI] [PubMed] [Google Scholar]
- 28.Purcell N Zamora K Bertenthal D, et al. How VA whole health coaching can impact veterans’ health and quality of life: A mixed-methods pilot program evaluation. Glob Adv Health Med. 2021;10:216495612199828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Radovanovic D Seifert B Urban P, et al. Validity of Charlson Comorbidity Index in patients hospitalised with acute coronary syndrome. Insights from the nationwide AMIS plus registry 2002–2012. Heart. 2014;100(4):288–294. [DOI] [PubMed] [Google Scholar]
- 30.Petry NM Peirce JM Stitzer ML, et al. Effect of prize-based incentives on outcomes in stimulant abusers in outpatient psychosocial treatment programs: A National Drug Abuse Treatment Clinical Trials Network Study. Arch Gen Psychiatry. 2005;62(10):1148–1156. [DOI] [PubMed] [Google Scholar]
- 31.Sayegh CS Huey SJ Zara EJ, et al. Follow-up treatment effects of contingency management and motivational interviewing on substance use: A meta-analysis. Psychol Addict Behav. 2017;31(4):403–414. [DOI] [PubMed] [Google Scholar]
- 32.Hawk M Coulter RWS Egan JE, et al. Harm reduction principles for healthcare settings. Harm Reduct J. 2017;14(1):70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lattal KA. Delayed reinforcement of operant behavior. J Exp Anal Behav. 2010;93(1):129–139. [DOI] [PMC free article] [PubMed] [Google Scholar]


