Abstract
Background
Older adults experience age-related declines in physical and cognitive functions due to interactions between aging and chronic diseases. Tai Chi and Qigong (TCQ) might be beneficial in improving the physical function and delaying the cognitive decline of this population. The potential underlying mechanism was explored to determine the effects of TCQ on cognitive function via direct or indirect pathways.
Purpose
The objective of this systematic review was to determine the effects of TCQ on cognitive and physical functions in older adults using meta-analysis, and to determine the impact of TCQ on cognitive function while controlling for physical function using a meta-regression approach.
Methods
A systematic search of 13 electronic databases (in English, Korean, and Chinese languages) identified 10,292 potentially eligible studies published between inception and May 2022. The bias in individual studies was assessed using the Cochrane Risk of Bias (version 2.0) tool. The heterogeneity of the studies was evaluated using a 95% prediction interval, and the meta-analysis and meta-regression were implemented using the Comprehensive Meta-Analysis (version 3) software.
Results
Our search identified 17 randomized studies (n = 2,365, mean age = 70.3 years). The results of the meta-analysis that used a random-effects model indicated that TCQ had significant effects on both cognitive (Hedges' g = 0.29, 95% confidence interval [CI] = 0.17 to 0.42) and physical (Hedges' g = 0.32, 95% CI = 0.19 to 0.44) functions. We used meta-regression to explore the effect size of TCQ in association with physical function level. The regression model was significant (Q = 25.01, p = .070), and 55% of the heterogeneity was explained by physical function as a moderator variable. The effects of TCQ on cognitive function remained significant in this model when controlling for the effect of physical function (β = 0.46, p = .011).
Conclusion
This meta-regression of 17 randomized studies strongly suggests that TCQ has beneficial effects on physical and cognitive functions in older adults. The effect of TCQ on cognitive function remained significant after taking into account the significant effects of physical function as a moderator. The findings imply the potential health benefits of TCQ by promoting cognitive function in older adults directly and indirectly through enhancing physical function.
PROSPERO registration number
*PROSPERO international prospective register of systematic reviews, registration ID CRD42023394358.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12877-023-04070-2.
Keywords: Tai Chi and Qigong, Cognitive function, Physical function, Older adults, Meta-analysis, Meta-regression
Background
Aging is the progressive accumulation of time-related changes, and age-related cognitive decline has become a global public health problem [1, 2]. Older adults remember less and walk more slowly than younger adults, which is associated with generalized impairments of physical and cognitive functions [3]. As people age, some experience age-related declines in physical and cognitive functioning from interactions between aging and disease [4], which increases their risks of dependence and premature death [5].
Tai Chi and Qigong (TCQ) is a popular mind–body intervention that shares the core features of Chinese martial arts and meditative movements through smooth and continuous body movements and breathing [6, 7]. There are many similarities between Tai Chi and Qigong in how they focus on the body (posture and movement), breath, and mind (meditation and mindfulness) [8, 9]. The mind–body exercise component of TCQ is a potent lifestyle factor playing a critical role in preserving and promoting healthy cognitive aging [8, 9]. Therefore, Tai Chi and Qigong were considered equivalent interventions and were grouped together in the present review.
A key neurotrophin that influences cognitive function is brain-derived neurotrophic factors (BDNFs). In the cerebral cortex and hippocampus, BDNFs are shown to facilitate neurogenesis and promote synaptic plasticity [10]. Exercise has the potential to directly or indirectly affect the synthesis and release of hippocampal BDNFs’ production [11, 12]. TCQ as an alternative aerobic exercise might be beneficial for delaying cognitive decline in older adults [13], possibly via the upregulation of BDNFs [14]. A randomized controlled trial (RCT) involving people with mild dementia found that a TCQ program might improve cognitive function and mental well-being in this population [15]. A previous meta-analysis indicated that TCQ might improve the cognitive function of middle-aged and older adults with mild cognitive impairment (MCI) [16].
TCQ could affect neural processes and cognitive performance via various pathways, such as aerobic exercises, by engaging learning processes through meditative aspects and from a potential mechanism underlined in East Asian traditions. First, TCQ comprises mild-to-moderate exercise levels depending on specific features [17–19] that are known to have clear cognitive benefits [20, 21]. Aerobic exercise has been found to induce changes in neurotransmitters, neural growth factors, and functional network properties that strengthen neuroplasticity [22, 23] and improve brain perfusion [24]. Consistent with these expectations, several systematic reviews of Tai Chi have shown structural [25, 26] and functional [25, 27, 28] changes as a result of neuroimaging techniques, including in cortical thickness, functional connectivity, and homogeneity of the brain, and executive network neural function [21]. Previous intervention studies also demonstrated that TCQ improved cognitive functioning by changing neural activity [28, 29]. A randomized trial reported that 15 min of Qigong training increased EEG alpha activity, leading to a relaxed state of mind, and theta activity, resulting in internalized attention [28]. Compared to general aerobic exercise, Tai Chi exercise improved cognitive flexibility among healthy adults by affecting brain functional specialization [29].
Second, because TCQ requires practitioners to learn and perform highly coordinated sequences of whole-body postures and movements, cognitive and neural processes involved in attention, sequence learning, and body coordination are heavily involved. TCQ may enhance the neural mechanisms activated during the learning and practice of those exercises and enhance the learning of other sequencing and body coordination activities controlled by the same brain areas. Indeed, learning TCQ enhances growth-factor levels, such as those of BDNFs [22, 30], which in turn enhances learning [22, 31]. TCQ may strengthen specialized areas of the brain responsible for declarative and procedural learning that are utilized when learning the action sequences [32, 33].
Third, the meditative state is a central and unique aspect of mind–body exercises such as TCQ. Meditation improves attention and executive functions [34, 35]. The meditative aspect of TCQ would be expected to benefit older adults since meditation is associated with cognitive benefits in those with cognitive decline [36, 37] and structural brain changes in neurodegenerative disease [38]. The calm mental-focus characteristic of TCQ is conducive to reducing stress, which negatively affects memory in both Tai Chi [39, 40] and Qigong [28, 41]. The meditative aspect of TCQ may affect cognition by enhancing mood [42, 43], which influences perception, attention, and memory [44, 45]. The mindfulness and mental focus characteristics in TCQ would benefit cognition beyond what would be expected in other exercises with similar intensity.
Finally, TCQ was developed based on Taoist philosophy and Traditional Chinese Medicine (TCM) and was designed to stimulate the flow of qi—a form of physical and mental energy—in the internal organs, musculature, and system of qi pathways, or meridians, and thereby improve physiological function [46]. Together, meditation and movements are postulated to stimulate acupuncture points and affect the qi and the efficiency of qi flow through the meridians [47]. Both Taoist theories about 'life-nurturing' and TCM postulate that strengthening the qi leads to mental and spiritual clarity as well as improved body health and well-being [48, 49]. However, the potential association between the cultivation and enhanced circulation of qi and cognitive benefits requires further exploration.
Recent empirical investigations of the benefits of TCQ have primarily focused on physical functions such as maintaining physical aerobic endurance, lower body strength, balance, mobility, gait speed [50, 51], and motor performance [52]. However, exercise-induced benefits on physical and cognitive functions are generally interrelated. For example, previous cross-sectional studies found that older adults with better physical function, frequently indicated by the stronger grip and faster gait, may present better cognitive performance in executive function, memory, and processing speed [53–58]. In addition, a previous meta-analysis also supported the associations between cognitive and physical functions and the impact of exercise training, indicating that exercise-induced improvements in physical function are often accompanied by improvements in cognitive function [59].
As a mind–body exercise that is safely applicable to older adults with impaired physical and cognitive functions, TCQ has been found to be beneficial for delaying impairments in these functions in older adults [60]. Several meta-analysis studies have reported that TCQ is effective in improving cognitive functions [16, 61] and physical functions [62], but no studies have focused on the relationship between physical and cognitive functions. Based on the close association between physical and cognitive functions, we hypothesized that the effects of TCQ on cognitive function could be induced both directly and indirectly via physical functions. While there is promising evidence for cognitive improvement from practicing TCQ, the potential mechanisms underlying the effect of TCQ on cognitive function via indirect or direct pathways have yet to be explored.
Meta-regression involves the integration of meta-analysis and linear regression and aims to explain heterogeneity at the study level rather than at the individual level [63]. Meta-regression can identify multiple covariates, including categorical and continuous variables, and both linear and nonlinear relationships with effect sizes can be assessed [64]. The present systematic review therefore aimed to use meta-regression to determine the effectiveness of TCQ in improving cognitive and physical functions in older adults and to determine if the effect of TCQ on cognitive function remains significant after controlling for physical function.
Methods
Search strategy
The electronic literature published up to May 2022 was searched: six English literature databases (PubMed, Embase, Cochrane Library, CINAHL, ProQuest, and OVID), seven Korean databases (Research Information Sharing Service [RISS], Korean Studies Information Service System [KISS], National Digital Science Library, DBpia, Korea Scholar, National Assembly Library, and Korean Citation Index), and four Chinese databases (Wanfang, China Science and Technology Journal Database [VIP], and Chinese National Knowledge Infrastructure [CNKI]). Three search term groups (Tai Chi, clinical trials, and cognition) were used to find studies that yielded results on both physical and cognitive functions. These search terms were used in combination with their Medical Subject Headings (MeSH) terms, keywords, and synonyms in the search.
The main search terms applied to the Chinese databases were CNKI terms and simplified Chinese characters: “Taichi (太极)” OR “Qigong (气功)” OR “Taiji Quan(太极拳)” OR “Baduan jin (八段锦)”. All articles extracted from each database were screened for duplicates and organized using EndNote (version 20) reference management software. The following characteristics of the included studies were summarized in a Microsoft Excel spreadsheet: publication year, language, population, intervention types, outcome measurements, and comparison groups.
Eligibility criteria
Only RCTs were included in our analysis. The eligibility criteria included studies in which (1) participants are older adults (≥ 60 years) who lived in community settings (i.e., nursing homes, assisted living facilities, or their own homes), (2) participants did not have any disease that affected cognitive function or only had MCI, (3) the intervention included Tai Chi or Qigong, (4) the article included results on both physical (ADL, balance, walking ability, muscle strength, flexibility, and physical health) and cognitive functions (cognitive performance, attention/executive function, memory, and linguistic competence), and (5) the article was published in English, Korean, or Chinese. We excluded articles in which participants were hospitalized or residing in a rehabilitation facility or had neurodegenerative disorders, such as cancer, dementia, Parkinson’s disease, or Alzheimer’s disease. We considered studies that included control groups participating in alternative exercises, usual care, or no treatment.
Data extraction and synthesis
The data that we extracted from the studies were general information (authors, publication year, language), basic characteristics (sample size, intervention type: Tai Chi or Qigong), and intervention length and duration (duration of one session or frequency of sessions). The primary outcome for this review was cognitive function (i.e., global cognitive function, memory and learning, visuospatial ability, and executive function), control condition (active or inactive), and physical function. Outcome data (e.g., means and standard deviations of raw data) were extracted and summarized to evaluate the effects of TCQ on cognitive and physical function.
Quality and risk-of-bias assessments
The quality and risk of bias for all included articles were assessed using the Cochrane’ Risk of Bias (version 2.0) tool (RoB 2.0) [65]. The Cochrane RoB 2.0 contains five domains of bias: bias arising from the randomization process, bias due to deviations from intended interventions, bias due to missing outcome data, bias in the outcome measurements, and bias in the selection of the reported result. An algorithm judged the risk of bias that arose from each domain, leading to a final decision on ‘low risk of bias,’ ‘some concerns,’ or ‘high risk of bias’ [65]. All authors independently assessed the quality and risk of bias of all articles included in the final review. After dividing the authors into two groups, the outcomes of the review by each group’ were compared. Any disagreements between two independent reviewers were resolved by the reviewers or, if necessary, a third expert reviewer to obtain a consensus.
Data analysis
Comprehensive Meta-Analysis (CMA V3.0, Biostat, USA) was used to combine effect sizes and assess heterogeneity and publication bias. The random-effects model was employed for the analysis to allow its results to be generalized to comparable studies [66]. Continuous variables were estimated using Hedges’s g effect sizes with 95% confidence intervals (CIs). The absolute heterogeneity level among the effect estimates was assessed by calculating the between-studies standard deviation and 95% prediction interval (PI). The 95% PIs described the expected range of true effects if a new study was conducted. As the between-studies standard deviation and lower and upper limits of the 95% PI were in the same metric as the effect estimates, they offer a reasonable quantification of the heterogeneity level [63, 67–69]. A subgroup analysis was conducted to compare the effects of TCQ according to the intervention duration: short-term (≤ 12 weeks) vs. long-term (> 12 weeks). The moderators of interest included physical function, which was judged to have an influence on the effect size based on an outcome measure of cognitive function. We conducted meta-regression analyses to investigate the potential moderators of the effects of Tai Chi on cognitive function with physical functioning as a covariate. The publication bias was analyzed by constructing funnel plots to explore the possibility of publication bias resulting from the preferential publication of prevalence reports with positive findings and amongst small studies that estimated high prevalence rates [70]. Egger’s regression test was used to evaluate the relationship between the effect size and the standard error [71] to determine the significance of asymmetry.
Results
Study selection
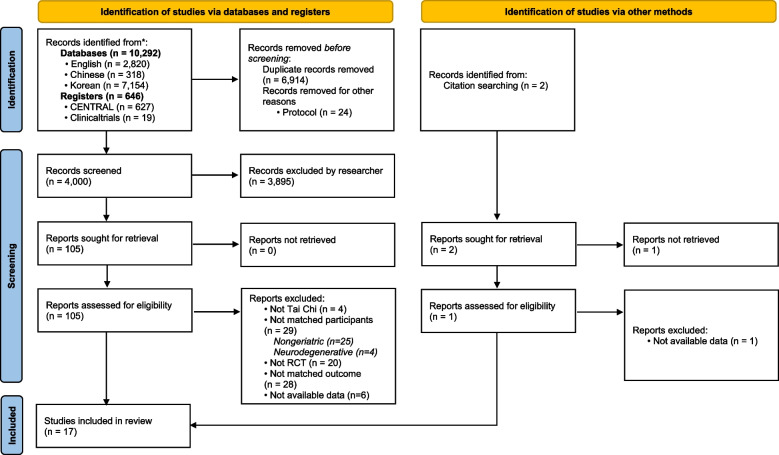
A literature search was performed from inception through May 2022 in accordance with the PRISMA 2020 guidelines [72]. Of the 10,292 citations identified in the databases, 2,820 were from English databases (Embase, PubMed, OVID, ProQuest, and CINAHL), 7,154 from Korean databases (KISS, RISS, DBpia, Korea Scholar, and National Assembly Library), and 318 from Chinese databases (Wanfang, VIP, and CNKI). Of the 646 citations identified in the registers, 627 were from CENTRAL and 19 from ClinicalTrials. Manual searches identified two additional citations.
Duplicate documents were removed using EndNote, and 105 studies were selected according to the inclusion criteria by reviewing titles and abstracts. These 105 studies were screened to exclude non-geriatric (k = 25) or neurodegenerative (e.g. Alzheimer’s disease, Parkinson’s disease, or stroke survivors) studies (k = 4), non-RCTs (k = 20), non-Tai-Chi intervention studies (k = 5), studies that did not evaluate cognitive or physical function as outcomes (k = 28), studies for which data were not available (k = 6), and studies with duplicate participants (k = 1), leaving 17 studies for inclusion in the final analysis. Among the 17 RCTs, one study had two comparison groups (the usual-care and active-control groups); the data of each comparison group were separately entered into the analysis. Two additional studies were found through manual searches, but both were subsequently excluded due to a lack of specific data or not matching the eligibility of the present study. In summary, the qualitative synthesis and quantitative analysis were conducted on 17 studies (Fig. 1).
Fig. 1.
Flow diagram of the study selection process
Quality of studies and risk of bias
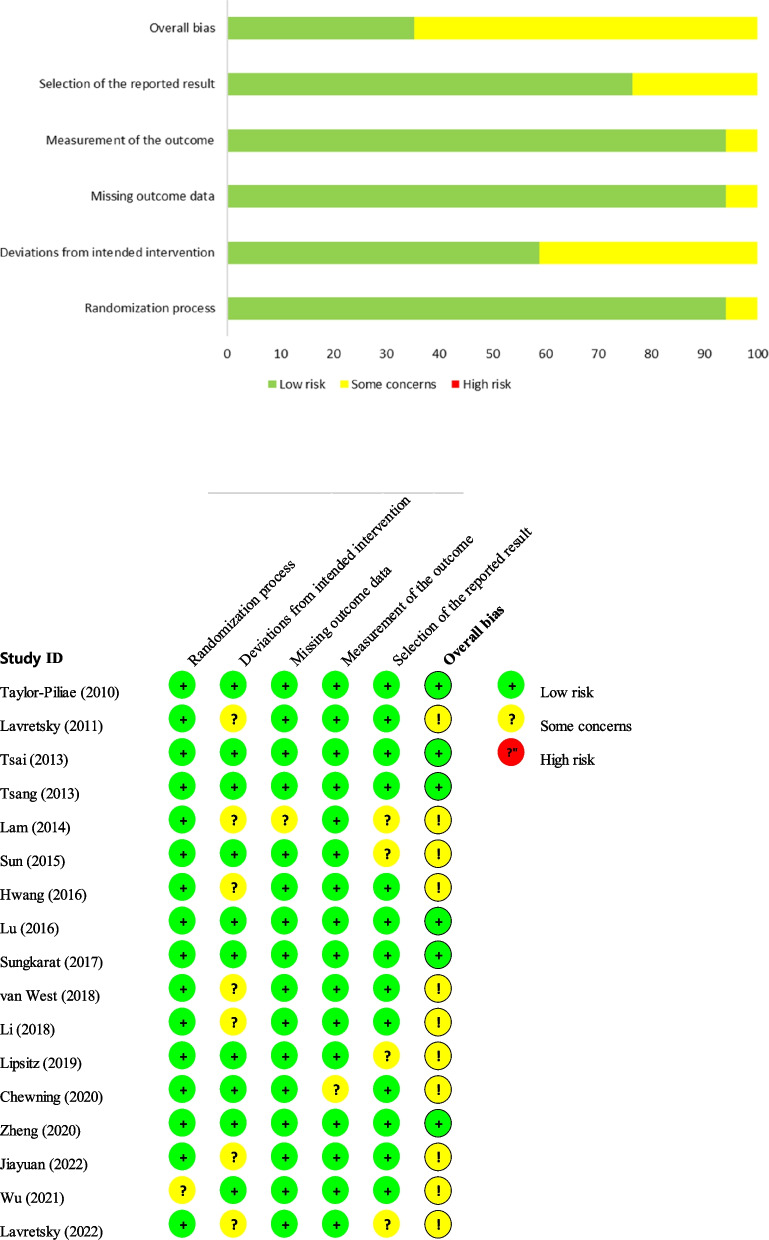
The quality assessment of the 17 included studies revealed that 6 were low risk (35%) and 11 had some concerns (65%); none were considered high risk. When analyzed by domain, 16 studies (94%) were low risk, and 1 (6%) was considered to have some concerns in the domain that presented the bias, according to the ‘randomization process.’ For the ‘deviation from intended intervention’ domain, there were 10 low-risk studies (58.8%) and 7 with some concerns (41.2%). The risks of bias in the ‘missing outcome data’ and ‘measurement of the outcome’ domains were low in 16 studies (94.1%) and uncertain in 1 (5.9%). Among ‘the selection of the reported result’ domain, there were 13 low-risk studies (76.5%) and 4 (23.5%) with some concerns (Fig. 2).
Fig. 2.
Assessment of risk of bias in the included studies
Modality and medium
The 17 included RCTs involved 2,235 participants, with 20–456 in each trial, and their mean age was 61–84 years (overall mean age = 70.9 years and 71.8% females). The main characteristics of the studies are listed in Table 1. The subjects included older adults who were healthy (k = 6), prefrail or frail (k = 2), with MCI or amnestic MCI (k = 5), with geriatric depression (k = 2), and who had a risk of falls (k = 2). The intervention was Tai Chi (k = 14) or Qigong (k = 3) applied for a mean duration of 19.7 weeks (range = 4–52 weeks). The control groups received either an alternative intervention (k = 13, health education or alternative exercise) or no treatment (k = 4, usual care or no treatment). All but one study was reported in English (k = 16), with the remaining report written in Chinese. Most intervention settings (k = 12) for older adults were in the community. The non-community settings were described as an elderly service unit from a hospital (k = 1), and a residential home or housing facility (k = 2), or the intervention setting was not reported (k = 2).
Table 1.
Characteristics of the included studies
| Study author, year (Country/Language) |
Population | Intervention | Comparison | Outcome measurement | Safety monitoring |
||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Disease-related characteristics | E (M:F) | C (M:F) | Age, years (group)b | TCQ type | Intensity (time × session/W × duration) |
Setting | Physical function | Cognitive function | |||
|
Taylor-Piliae, 2010 [40] (USA/English)a |
Age ≥ 60 years, healthy | 37 (13:24) |
AC: 39 (11:28) UC: 56 (16:40) |
70.6 ± 5.9 (E) 68.5 ± 5.0 (AC) 68.2 ± 6.2 (UC) |
Tai Chi, 12-form Yang style |
1) Adoption phase: 1 h × 5/W (group × 2 + home × 3) × 12 Ws 2) Maintenance phase: 1 h × 4/W(group × 1 + home × 3) × 12 Ws |
Community |
1) Western exercise 2) Healthy-aging education |
OLS FRT Arm curls Chair-stand test Back-scratch test Sit-and-reach test |
Animal-naming test Digit span forward Digit span backward |
NI |
|
Lavretsky, 2011 [73] (USA/English) |
Age ≥ 60 years, geriatric depression | 36 (13:23) | 37 (15:22) |
69.1 ± 7.0 (E) 72.0 ± 7.4 (C) |
Tai Chi | Group: 2 h × 1/W × 10 Ws | Community | Health education | SF-36 (physical health) |
MMSE CVLT TMT B–A |
No adverse events |
|
Tsai, 2013 [74] (USA/English) |
Age ≥ 60 years, mild-to-moderate CI with knee OA | 28 (6:22) | 27 (9:18) |
78.9 ± 6.9 (E) 78.9 ± 8.3 (C) |
Tai Chi, 12-form Sun style | Group: 20–40 min × 3/W × 20 W | Community | Health education, culture-related activities, and social activities |
WOMAC (physical functioning) TUG test Sit-to-stand test |
MMSE | No adverse events |
|
Tsang, 2013 [75] (Hong Kong/English) |
Age ≥ 60 years, frail |
61 (14:47) | 55 (15:40) |
83.3 ± 6.3 (E) 84.9 ± 6.0 (C) |
Novel health Qigong | Group: 1 h × 2/W × 12 Ws | Elderly service unit at hospital | Newspaper reading |
Handgrip strength TUG test |
LOTCA-G | No adverse events |
|
Lam, 2014 [76] (Hong Kong/English) |
Age ≥ 65 years, MCI or amnestic MCI | 171 (46:125) | 218 (46:172) |
77.2 ± 6.3 (E) 78.3 ± 6.6 (C) |
Tai Chi, 24 style |
1) Adoption phase: group, 30 min × 3/W × 4–6Ws 2) Maintenance phase: home, 30 min × 3/W × 46–48 Ws, refresher lessons every month |
Residential home | Stretching and relaxation exercises | BBS |
ADA MMSE Digit span backward Visual span backward Delay recall Verbal fluency |
NI |
|
Sun, 2015 [77] (China/English) |
Age ≥ 60 years, healthy | 72 (14:48) | 66 (20:46) |
68.3 ± 5.9 © 70.1 ± 5.7 (C) |
Tai Chi, 24-form Yang style | Group: 1 h × 2/W × 6 Ms | Community | Nonathletic care |
OLS 5-m high walking speed 10-m normal walking speed Handgrip strength (both) |
MMSE | NI |
|
Hwang, 2016 [78] (Taiwan/English) |
Age ≥ 60 years, fall risk | 228 (75:153) | 228 (77:151) |
72.0 ± 8.1 (E) 72.7 ± 8.1 (C) |
Tai Chi, 18-form Yang style | Individual: 1 h × 1/W × 6 Ms, self-practice every day | Community | Lower extremity training |
Handgrip strength (right hand) Tinetti balance test Tinetti gait test |
MMSE | No adverse events |
|
Lu, 2016 [79] (Hong Kong/English) |
Healthy female older adults | 15 (0:15) | 16 (0:16) |
72.8 ± 6.7 (E) 67.3 ± 6.6 (C) |
Tai Chi, 12-form Yang style | Group: 90 min × 3/W × 16 Ws | Community | Usual care | Computerized gait analysis | Auditory Stroop test: single/dual task | No adverse events |
|
Sungkarat, 2017 [21] (Thailand/English) |
Age ≥ 60 years, MCI | 33 (2:31) | 33 (7:26) |
68.3 ± 6.7 (E) 67.5 ± 7.3 (C) |
Tai Chi, 10-form style |
1) Group: 50 min × 3/W × 3 Ws 2) Home: 50 min × 3/W × 12 Ws |
Community | Educational material | PPA |
Wechsler Memory Scale; delayed recall Block-design test Digit span forward/backward TMT B–A |
No adverse events |
|
van West, 2018 [80] (New Zealand/English) |
Age ≥ 60 years, healthy | 43 (11:32) | 36 (7:29) |
69.1 [60-86] (E) 67.6 [60-80] (C) |
Tai Chi, 18-form Yang style | Group:1 h × 2/W × 4 Ws | NI | International POI |
FRT Four-stage balance test Pinch and handgrip strength Chair-stand test ROM; wrist, elbow, and shoulder |
NCI; average of five domain scores (composite memory, psychomotor speed, reaction time, complex attention, and cognitive flexibility) | NI |
|
Li, 2018 [81] (China/Chinese) |
Age 60–70 years, MCI | 10 | 10 |
61.4 ± 1.84 (E) 62.1 ± 2.08 (C) |
Qigong, Baduanjin |
1) Adoption phase: group 60 min × 5/W × 2 Ws 2) Maintenance phase: group 60 min × 5/W × 14 Ws |
Community | Usual care |
CM-PPT Computerized gait analysis |
Erikson flanker task More-odd shifting task 2-back task |
Adjust the exercise intensity according to heart rate |
|
Lipsitz, 2019 [82] (USA/English) |
Age ≥ 60 years, healthy | 93 (30:63) | 87 (30:57) |
75.9 ± 9.1 (E) 74.6 ± 8.6 (C) |
Tai Chi, 9-form Yang style |
Group intervention × 2/W and home practice 20 min × 3/W × 52 Ws (6-month effect reported as a recommendation to end the trial by the Data and Safety Monitoring Board) |
Housing facility | Health education (monthly) |
SPPB SF-12 (physical health) PASE Gait velocity |
TMT: B–A | Minor musculoskeletal complaints |
|
Chewning, 2020 [83] (USA/English) |
Age ≥ 65 years, Fall risk | 94 (18:76) | 103 (13:90) |
75.0 ± 7.4 (E) 72.8 ± 7.0 (C) |
Tai Chi, Yang style |
Group: 1.5 h × 2/W × 6 Ws and home-practice coaching |
Community | No treatment |
TUG test Chair-stand test Four-stage balance test |
TMT B | NI |
|
Zheng, 2020 [84] (China/English) |
Age 45–75 years, stroke survivors with MCI | 24 (19:5) | 24 (22:2) |
61.6 ± 9.2 (E) 62.8 ± 6.4 (C) |
Qigong, Baduanjin | Group: 40 min × 3/W × 24 Ws | Community | No treatment | MBI |
MoCA TMT: B–A AVLT TAP DSC CDT |
No adverse events |
|
Wu, 2021 [85] (China/English) |
Age 50–85 years, Healthy | 19 (4:15) | 19 (1:18) |
63.6 ± 4.0 (E) 63.2 ± 4.4 (C) |
Tai Chi, 24-form Yang style | Group: 60 min × tri-weekly × 12 Ws | NI | Telephone consultation (every other week) |
Knee extensor strength, 6MWT |
IED | NI |
|
Jiayuan, 2022 [86] (China,/English) |
Age ≥ 65 years, Prefrail and frail |
31 (11:18) | 30 (13:17) |
71.7 ± 3.9 (E) 70.8 ± 4.2 (C) |
Tai Chi, 24-form Yang style |
1) 1st stage: Group 60 min × 2/W × 3 Ms 2) 2nd stage: Individual practice 60 min × 2/W × 3 Ms |
Community | Booklet about mindfulness skill |
SPPB TUG test Chair-stand test |
MMSE | NI |
|
Lavretsky, 2022 [87] (USA/English) |
Age ≥ 60 years, geriatric depression | 89 (27:62) | 89 (22:67) |
69.2 ± 6.9 (E) 69.4 ± 6.2 (C) |
Tai Chi |
1) Group: 60 min × 1/W × 6 Ws and home practice for 20 min/day using handouts 2) Virtual: 60 min × 1/W × 6 Ws and home practice for 20 min/day using handouts |
Community | Health education and wellness training | SF-36 |
CVLT ROCFT TMT: B–A Stroop interference COWAT Animal fluency Boston Naming Test |
No adverse events |
Abbreviations: M Male, F Female, E Experimental group, C Control group, AC Active control group, UC Usual care group, TCQ Tai Chi and Qigong, M Month, W Week, NI No information, MCI Mild cognitive impairment, 6MWT 6-min walk test, ADA Alzheimer’s Disease Assessment Scale, AVLT Rey Auditory Verbal Learning Test, BBS Berg Balance Scale, CDT Clock-drawing task, CI Cerebral infarction, CM-PPT Chinese Mini Physical Performance Test, COWAT Controlled Oral Word Association Test, CVLT California Verbal Learning Test, DSC Digit symbol coding, FRT Functional reach test, IED Intra-Extra Dimensional Set Shift, LOTCA-G Loewenstein Occupational Therapy Cognitive Assessment–Geriatric, MBI Modified Barthel Index, MCI Mild cognitive impairment, MMSE Mini Mental Status Examination, MoCA Montreal Cognitive Assessment, NCI Neurocognition index, OA Osteoarthritis, OLS One-leg-standing test, PASE Physical Activity Scale for the Elderly, PPA Physiological profile assessment, ROCFT Rey Complex Figure Test, ROM Range of motion, SF-12 12-Item Short-Form Health Survey, SF-36 36-Item Short-Form Health Survey, SPPB Short Physical Performance Battery, TAP Test of Attention Performance, TMT Trail-Making Test, TUG Timed Up-and-Go Test, WOMAC Western Ontario and McMaster Universities Osteoarthritis Index
a Analyzed for each control group;
b Data are mean ± standard-deviation [range] values
The physical-function outcomes were activities of daily living (ADLs), dynamic balance, static balance, walking ability, muscle strength, flexibility, and physical health. ADLs were measured using the modified Barthel Index, and dynamic balance was measured using the Berg Balance Scale, Tinetti balance test, or functional reach test. Walking ability was measured using the Timed Up-and-Go test, computerized gait analysis, 6-min walk tests, gait velocity, Tinetti gait test, and 5-m or 10-m walking speed test. Static balance was measured using the one-leg-standing test or four-stage balance test. Muscle strength was measured using arm curls, chair-stand test, sit-to-stand test, pinch or handgrip strength, or knee extensor strength. Flexibility was measured using a back-scratch test, sit-and-reach test, or range of motion. Physical health was measured using the physical health domains of the 36- or 12-Item Short-Form Health Survey, or the physical functioning domains of the Western Ontario and McMaster Universities Osteoarthritis Index, Physiological Profile Assessment, Short Physical Performance Battery, Physical Activity Scale for the Elderly, or Chinese Mini Physical Performance Test.
The cognitive-function outcomes were cognitive performance, attention/executive function, memory, and linguistic competence. Cognitive performance was measured using the Mini-Mental State Examination (MMSE), Montreal Cognitive Assessment (MoCA), Loewenstein Occupational Therapy Cognitive Assessment–Geriatric (LOTCA-G), or the cognitive subscale of the Alzheimer’s Disease Assessment Scale (ADA). Attention/executive functions were measured using the animal-naming test, digit span (forward/backward), visual span, Trail-Making Test, Test of Attentional Performance, digit symbol coding, clock-drawing task, Eriksen flanker task, More-odd shifting task, or Stroop test. Memory was measured using the California Verbal Learning Test, Rey Auditory Verbal Learning Test, 2-back task, Intra-Extra Dimensional Set Shift, or delayed recall (e.g., Wechsler Memory Scale or Rey Complex Figure Test). Linguistic competence was measured using verbal fluency, the Controlled Oral Word Association Test, the animal-naming test (fluency), or Boston Naming Test.
Safety monitoring
Safety monitoring was reported in 10 of the 17 studies (58.8%). There were no adverse events in eight studies and minor musculoskeletal complaints in one. In another study, exercise intensity was adjusted according to the monitored heart rate. There were no safety monitoring reports in 7 studies.
Meta-analysis: synthesis of results
Effects of TCQ on cognitive function
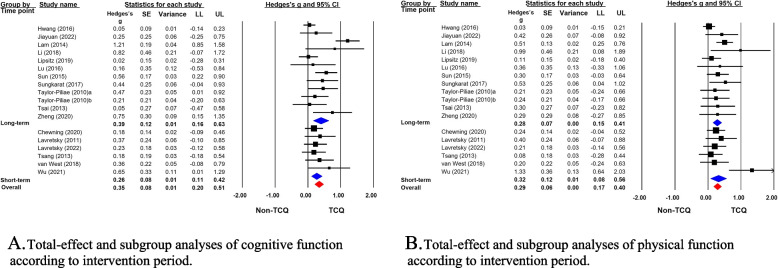
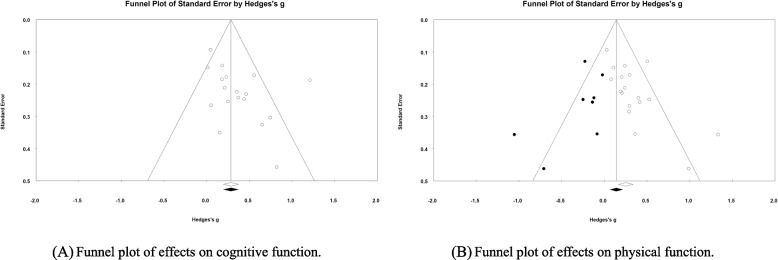
The meta-analysis of the 17 studies using the random-effects model indicated that TCQ had a small effect size in improving cognitive function (Hedges’ g = 0.35, 95% CI = 0.20 to 0.51) (Fig. 3A). Potential heterogeneity was indicated by a 95% PI of − 0.21 to 0.92. There was a risk of publication bias according to the funnel plots and Egger’s regression test (p = 0.049) (Fig. 4A).
Fig. 3.
Forest plots of the effects of TCQ on cognitive and physical functions. SE, standard error; CI, confidence interval; LL, lower limit; UL, upper limit
Fig. 4.
Publication bias in the included studies
A subgroup comparison was conducted between long-term (k = 11) and short-term (k = 6) interventions. The effect sizes of TCQ on cognitive function were indicated by Hedges’ g values of 0.39 (95% CI = 0.16 to 0.63; 95% PI = − 0.40 to 1.19) and 0.26 (95% CI = 0.11 to 0.42; 95% PI = 0.04 to 0.49) for long- and short-term interventions, respectively. No significant differences were found between the effect sizes according to the intervention duration (Q = 0.82, p = 0.364) (Fig. 3A). The funnel plot of the overall effect size for cognitive function was symmetrical, and there was no publication bias for long-term interventions according to Egger’s regression test (p = 0.152). However, the funnel plot for short-term interventions was asymmetrical, so publication bias may have been present.
Effects of TCQ on physical function
The meta-analysis of the 17 studies using the random-effects model indicated that TCQ had a small effect size in improving physical function (Hedges’ g = 0.29, 95% CI = 0.17 to 0.40) (Fig. 3B). Potential heterogeneity was indicated by a 95% PI of − 0.02 to 0.60. Publication bias was suspected according to the funnel plots and Egger’s regression test (p = 0.004) (Fig. 4B).
A subgroup comparison was conducted between long-term (k = 11) and short-term (k = 7) interventions. The effect sizes of TCQ on physical function were indicated by Hedges’ g values of 0.28 (95% CI = 0.15 to 0.41; 95% PI = − 0.02 to 0.57) and 0.32 (95% CI = 0.08 to 0.56; 95% PI = − 0.37 to 1.01) for long- and short-term interventions, respectively. No significant differences were found between the effect sizes according to the intervention duration (Q = 0.081, p = 0.776) (Fig. 3B). The funnel plot of the overall effect size for physical function was symmetrical, but Egger’ s regression test indicated publication bias for the long-term interventions (p = 0.042). The funnel plot for short-term interventions was asymmetrical, suggesting publication bias.
Meta-regression analysis of the effect of TCQ on cognitive function
Since TCQ had significant effects on cognitive and physical functions, we used meta-regression to explore the effect size of TCQ on cognitive function in association with the level of physical functions. The regression model was significant (Q = 9.06, p = 0.002), indicating that physical function significantly impacts the effects of TCQ on cognitive function. The variance that was explained by the model was 0.035 within the total of 0.056, indicating that 63% of the heterogeneity was explained by the model that used physical function as a moderator (Table 2). This confirmed that changes in physical function were associated with changes in cognitive function. The goodness-of-fit test also addressed whether there was heterogeneity that could not be explained by physical function as a covariate. Qresid was used to estimate the variance of the unexplained heterogeneity. The variance that was not explained by the model was 0.021, and the goodness-of-fit test indicated that the unexplained variance was not zero (Q = 26.04, df = 16, p = 0.05). In conclusion, the effects of TCQ on cognitive function remained significant when controlling for the effect of physical function in this model.
Table 2.
Meta regression random-effects model: test of the model
|
Simultabneous test that all coefiicients (excluding intercept) are zero Qmodel = 9.06, df = 1, p = 0.0026 |
|
Goodness of fit: Test that unexplained variance is zero T2 = 0.0208, Tau = 0.1442, I2 = 38.56%, Qresid = 30.766, df = 16, p = 0.0534 |
|
Proportion of total between-study variance explained by the model R2 = T2explained/T2total = 0.0352/0.0560 = 0.63 |
Discussion
This study evaluated the effect of TCQ on cognitive function with physical function as a covariate among older adults with cognitive impairments. The obtained evidence supported the beneficial effects of TCQ on cognitive functions, including global, memory, and executive functions in individuals with or without cognitive impairments [16, 88]. Tai Chi or Qigong was administered for at least 12 weeks and was considered to be a promising alternative mind–body intervention for older adults with MCI [61]. The present review included 17 studies (14 Tai Chi and 3 Qigong interventions) with a mean duration of 19.7 weeks (range = 4–52 weeks). The meta-analysis with the random-effects model also confirmed the significant effects of TCQ on cognitive function for short-term (≤ 12 weeks) and long-term interventions. The difference in effect sizes between the intervention durations was also not significant in our study.
A recent meta-analysis of 14 studies on the effect of aerobic or resistance exercise on older adults with MCI confirmed the beneficial effects of TCQ, including improvement in cognitive function, and in the grip strength of physical function [13]. The association between cognitive and physical functions under the impact of exercise training indicates that exercise-induced improvements in physical function are associated with improved cognitive function [59]. One of the common mechanisms underlying exercise-induced benefits in cognitive function is related to neuroplasticity being facilitated in certain brain structures by physical activity [23]. Rogers and colleagues [24] conducted a 4-year prospective longitudinal study to examine the effects of different physical activity levels on cerebral perfusion and found that physically inactive, retired older adults presented significant declines in cerebral blood flow throughout four years of follow-up compared with those who regularly engaged in physical activity. It is well established that physical activity can increase circulating levels of a BDNF with cognitively beneficial properties. However, the type, intensity, and duration of physical exercise that would induce this mechanism are still under debate [89].
The typical features of TCQ as a mind–body exercise are physical and cognitive-stimulating activities [90]. A previous systematic review based on seven randomized trials proposed that changes in cognitive function during TCQ training may be associated with structural and functional changes in the cortex related to cognition [88]. In addition to the common mechanism through conventional exercise, TCQ as a mind–body exercise could also induce improvements in brain neuroplasticity through its motor complexity and multiple components combined with meditation training and relaxation practice [91, 92]. The aerobic exercise components of TCQ can delay age-related brain atrophy and improve cerebral blood circulation [23, 24], while the tranquility of mindfulness and Qigong breathing can improve attentional focus and executive function [34, 36]. A randomized trial compared the effects of Tai Chi with conventional exercise on cognitive function, and found a significant improvement in older adults from the Tai Chi group at 12 weeks. Both groups achieved clinically relevant improvements at 24 weeks [91].
Given that exercise-induced benefits on physical and cognitive functions are interrelated, TCQ intervention has been hypothesized as a beneficial mind–body exercise that may affect cognitive function either directly or indirectly via improving physical function. In order to confirm the direct pathway of TCQ on cognitive function, the present study used meta-regression analysis to explore further the effect of TCQ on cognitive function with physical function as a moderator. This meta-regression was conducted on the 17 studies in the review, since the recommended minimum number of studies for meta-regression analysis is 10 [63]. Including physical function as a moderator in the model resulted in explaining 63% of the variance in the true effects of TCQ. In other words, physical function as a moderator was significantly related to the effect size from TCQ. Although no previous study has examined the effect of TCQ on cognitive function using meta-regression, the available evidence supports the effect of TCQ on physical function in various populations including older adults with or without chronic conditions [93]. The next step was to explore whether the model with physical function as a moderator explained all of the variance in the effect size. The unexplained variance was still significant, leading to the conclusion that TCQ still have significant effects on cognitive function even after controlling for the effects from physical function.
The meta-regression suggested that TCQ acts beneficially on cognitive function via various mechanisms, not just in its aerobic components but also in the cognitive process of memorizing movements and paying attention to meditation. Therefore, further studies are warranted to explore the underlying mechanisms of TCQ-induced health benefits on physical and cognitive functions. This might reveal the rationale for exercise interventions such as TCQ to improve quality of life by slowing down the decline in cognitive function among those with cognitive impairment.
Some strengths and limitations should be considered when interpreting the present results. The strengths of the study were that we included 17 randomized trials searched from databases in 3 different languages with both cognitive and physical functions as outcomes, which enabled us to conduct the meta-regression analysis. However, the heterogeneity of the studies was also noted due to the range of older adults with varying health and cognitive statuses. The types of Tai Chi or Qigong, although all based on theoretical principles of traditional Chinese medicine, were different in intervention durations or intensity. Moreover, physical and cognitive functions were assessed using various measurement methods. Considering the heterogeneity of the studies, we used random-effect model for the main analysis and subgroup analysis on intervention duration with more than 5 studies. The sensitivity analysis with excluding outliers was also conducted to confirm the effects of TCQ.
Conclusions
The findings of this review suggest that TCQ effectively improves cognitive and physical functions among older adults with or without cognitive impairment when implemented as both short-term and long-term programs. The effect of TCQ on cognitive function remained significant after taking into account the significant effects of physical function as a moderator. The findings imply the potential health benefits of TCQ by promoting cognitive function in older adults directly and indirectly through enhancing physical function.
Supplementary Information
Additional file 1: Appendix. Search Strategy; Pubmed.
Acknowledgements
Not applicable.
Abbreviations
- TCQ
Tai Chi and Qigong
- BDNF
Brain-derived neurotrophic factor
- MCI
Mild cognitive impairment
- RoB
Risk of bias
- PI
Prediction interval
Authors’ contributions
RS, MP, KJ and JCS designed the study, and all authors in 3 teams were involved in the data collection and review process. JS, XF, AR, and YL prepared the tables and figures. RS, KJ, MP, and JCS wrote the main manuscript text, and all authors reviewed the manuscript. All authors meet authorship criteria and read and approved the final manuscript.
Funding
This work was supported by the National Research Foundation of Korea (NRF-2022R1A2C2011502).
Availability of data and materials
The datasets used and analyzed during the current study are available from the corresponding author upon reasonable request.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Moonkyoung Park, Email: lunarnr@cnu.ac.kr.
Rhayun Song, Email: songry@cnu.ac.kr.
Kyoungok Ju, Email: jko2080@hanmail.net.
Jacqueline C. Shin, Email: Jacqueline.shin@indstate.edu
Jisu Seo, Email: jisu45@cnu.ac.kr.
Xing Fan, Email: lsxyfanxing@qq.com.
Xianqi Gao, Email: gaoxianqi1217@gmail.com.
Ahyun Ryu, Email: ryuah@cnu.ac.kr.
Yuelin Li, Email: raylinlee@o.cnu.ac.kr.
References
- 1.Jessen F, Amariglio RE, Buckley RF, van der Flier WM, Han Y, Molinuevo JL, Rabin L, Rentz DM, Rodriguez-Gomez O, Saykin AJ. The characterisation of subjective cognitive decline. Lancet Neurol. 2020;19(3):271–278. doi: 10.1016/S1474-4422(19)30368-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Harman D. The aging process. Proc Natl Acad Sci. 1981;78(11):7124–7128. doi: 10.1073/pnas.78.11.7124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Clouston SA, Brewster P, Kuh D, Richards M, Cooper R, Hardy R, Rubin MS, Hofer SM. The dynamic relationship between physical function and cognition in longitudinal aging cohorts. Epidemiol Rev. 2013;35(1):33–50. doi: 10.1093/epirev/mxs004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cooper R, Hardy R, Aihie Sayer A, Ben-Shlomo Y, Birnie K, Cooper C, Craig L, Deary IJ, Demakakos P, Gallacher J. Age and gender differences in physical capability levels from mid-life onwards: the harmonisation and meta-analysis of data from eight UK cohort studies. PLoS ONE. 2011;6(11):e27899. doi: 10.1371/journal.pone.0027899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dewey ME, Saz P. Dementia, cognitive impairment and mortality in persons aged 65 and over living in the community: a systematic review of the literature. Int J Geriatr Psychiatry. 2001;16(8):751–761. doi: 10.1002/gps.397. [DOI] [PubMed] [Google Scholar]
- 6.Nyman SR, Ingram W, Sanders J, Thomas PW, Thomas S, Vassallo M, Raftery J, Bibi I, Barrado-Martín Y. Randomised controlled trial of the effect of Tai Chi on postural balance of people with dementia. Clin Interv Aging. 2019;14:2017–2029. doi: 10.2147/CIA.S228931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wayne PM, Lee MS, Novakowski J, Osypiuk K, Ligibel J, Carlson LE, Song R. Tai Chi and Qigong for cancer-related symptoms and quality of life: a systematic review and meta-analysis. J Cancer Surviv. 2018;12(2):256–267. doi: 10.1007/s11764-017-0665-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jahnke R. The healing promise of qi: creating extraordinary wellness through qigong and tai chi. UK: McGraw Hill Professional; 2002.
- 9.Larkey L, Jahnke R, Etnier J, Gonzalez J. Meditative movement as a category of exercise: implications for research. J Phys Act Health. 2009;6(2):230–238. doi: 10.1123/jpah.6.2.230. [DOI] [PubMed] [Google Scholar]
- 10.Schinder AF, Poo MM. The neurotrophin hypothesis for synaptic plasticity. Trends Neurosci. 2000;23(12):639–645. doi: 10.1016/S0166-2236(00)01672-6. [DOI] [PubMed] [Google Scholar]
- 11.Manuela Crispim Nascimento C, Rodrigues Pereira J, Pires de Andrade L, Garuffi M, Leme Talib L, Vicente Forlenza O, Maria Cancela J, Regina Cominetti M, Stella F. Physical exercise in MCI elderly promotes reduction of pro-inflammatory cytokines and improvements on cognition and BDNF peripheral levels. Curr Alzheimer Res. 2014;11(8):799–805. doi: 10.2174/156720501108140910122849. [DOI] [PubMed] [Google Scholar]
- 12.Nascimento CMC, Pereira JR, Pires de Andrade L, Garuffi M, Ayan C, Kerr DS, Talib LL, Cominetti MR, Stella F. Physical exercise improves peripheral BDNF levels and cognitive functions in mild cognitive impairment elderly with different bdnf Val66Met genotypes. J Alzheimers Dis. 2015;43(1):81–91. doi: 10.3233/JAD-140576. [DOI] [PubMed] [Google Scholar]
- 13.Lee J. Effects of aerobic and resistance exercise interventions on cognitive and physiologic adaptations for older adults with mild cognitive impairment: a systematic review and meta-analysis of randomized control trials. Int J Environ Res Public Health. 2020;17(24):9216. doi: 10.3390/ijerph17249216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sungkarat S, Boripuntakul S, Kumfu S, Lord SR, Chattipakorn N. Tai Chi improves cognition and plasma BDNF in older adults with mild cognitive impairment: a randomized controlled trial. Neurorehabil Neural Repair. 2018;32(2):142–149. doi: 10.1177/1545968317753682. [DOI] [PubMed] [Google Scholar]
- 15.Huang N, Li W, Rong X, Champ M, Wei L, Li M, Mu H, Hu Y, Ma Z, Lyu J. Effects of a modified Tai Chi program on older people with mild dementia: a randomized controlled trial. J Alzheimers Dis. 2019;72(3):947–956. doi: 10.3233/JAD-190487. [DOI] [PubMed] [Google Scholar]
- 16.Liu F, Chen X, Nie P, Lin S, Guo J, Chen J, Yu L. Can Tai Chi improve cognitive function? A systematic review and meta-analysis of randomized controlled trials. J Altern Complement Med. 2021;27(12):1070–1083. doi: 10.1089/acm.2021.0084. [DOI] [PubMed] [Google Scholar]
- 17.Chen X, Marrone G, Olson TP, Lundborg CS, Zhu H, Wen Z, Lu W, Jiang W. Intensity level and cardiorespiratory responses to Baduanjin exercise in patients with chronic heart failure. ESC Heart Fail. 2020;7:3782–91. [DOI] [PMC free article] [PubMed]
- 18.Lan C, Chen SY, Lai JS. The exercise intensity of Tai Chi Chuan. Med Sport Sci. 2008;52:12–19. doi: 10.1159/000134225. [DOI] [PubMed] [Google Scholar]
- 19.Lan C, Chen SY, Lai JS, Wong MK. Heart rate responses and oxygen consumption during Tai Chi Chuan practice. Am J Chin Med. 2001;29(3–4):403–410. doi: 10.1142/S0192415X01000423. [DOI] [PubMed] [Google Scholar]
- 20.Kramer AF, Hahn S, Cohen NJ, Banich MT, McAuley E, Harrison CR, Chason J, Vakil E, Bardell L, Boileau RA, et al. Ageing, fitness and neurocognitive function. Nature. 1999;400(6743):418–419. doi: 10.1038/22682. [DOI] [PubMed] [Google Scholar]
- 21.Sungkarat S, Boripuntakul S, Chattipakorn N, Watcharasaksilp K, Lord SR. Effects of Tai Chi on cognition and fall risk in older adults with mild cognitive impairment: a randomized controlled trial. J Am Geriatr Soc. 2017;65(4):721–727. doi: 10.1111/jgs.14594. [DOI] [PubMed] [Google Scholar]
- 22.Cotman CW, Berchtold NC. Exercise: a behavioral intervention to enhance brain health and plasticity. Trends Neurosci. 2002;25(6):295–301. doi: 10.1016/S0166-2236(02)02143-4. [DOI] [PubMed] [Google Scholar]
- 23.Hotting K, Roder B. Beneficial effects of physical exercise on neuroplasticity and cognition. Neurosci Biobehav Rev. 2013;37(9 Pt B):2243–2257. doi: 10.1016/j.neubiorev.2013.04.005. [DOI] [PubMed] [Google Scholar]
- 24.Rogers RL, Meyer JS, Mortel KF. After reaching retirement age physical activity sustains cerebral perfusion and cognition. J Am Geriatr Soc. 1990;38(2):123–128. doi: 10.1111/j.1532-5415.1990.tb03472.x. [DOI] [PubMed] [Google Scholar]
- 25.Pan Z, Su X, Fang Q, Hou L, Lee Y, Chen CC, Lamberth J, Kim ML. The effects of Tai Chi intervention on healthy elderly by means of neuroimaging and EEG: a systematic review. Front Aging Neurosci. 2018;10:110. doi: 10.3389/fnagi.2018.00110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Yu AP, Tam BT, Lai CW, Yu DS, Woo J, Chung KF, Hui SS, Liu JY, Wei GX, Siu PM. Revealing the neural mechanisms underlying the beneficial effects of Tai Chi: a neuroimaging perspective. Am J Chin Med. 2018;46(2):231–259. doi: 10.1142/S0192415X18500131. [DOI] [PubMed] [Google Scholar]
- 27.Cui L, Tao S, Yin HC, Shen QQ, Wang Y, Zhu LN, Li XJ. Tai Chi Chuan alters brain functional network plasticity and promotes cognitive flexibility. Front Psychol. 2021;12:665419. doi: 10.3389/fpsyg.2021.665419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Henz D, Schollhorn WI. EEG brain activity in dynamic health qigong training: same effects for mental practice and physical training? Front Psychol. 2017;8:154. doi: 10.3389/fpsyg.2017.00154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ladawan S, Klarod K, Philippe M, Menz V, Versen I, Gatterer H, Burtscher M. Effect of Qigong exercise on cognitive function, blood pressure and cardiorespiratory fitness in healthy middle-aged subjects. Complement Ther Med. 2017;33:39–45. doi: 10.1016/j.ctim.2017.05.005. [DOI] [PubMed] [Google Scholar]
- 30.Chen J, Kitanishi T, Ikeda T, Matsuki N, Yamada MK. Contextual learning induces an increase in the number of hippocampal CA1 neurons expressing high levels of BDNF. Neurobiol Learn Mem. 2007;88(4):409–415. doi: 10.1016/j.nlm.2007.07.009. [DOI] [PubMed] [Google Scholar]
- 31.Tokuyama W, Okuno H, Hashimoto T, Xin Li Y, Miyashita Y. BDNF upregulation during declarative memory formation in monkey inferior temporal cortex. Nat Neurosci. 2000;3(11):1134–1142. doi: 10.1038/80655. [DOI] [PubMed] [Google Scholar]
- 32.Clark D, Ivry RB. Multiple systems for motor skill learning. Wiley Interdiscip Rev Cogn Sci. 2010;1(4):461–467. doi: 10.1002/wcs.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Nakahara H, Doya K, Hikosaka O. Parallel cortico-basal ganglia mechanisms for acquisition and execution of visuomotor sequences - a computational approach. J Cogn Neurosci. 2001;13(5):626–647. doi: 10.1162/089892901750363208. [DOI] [PubMed] [Google Scholar]
- 34.Pratzlich M, Kossowsky J, Gaab J, Krummenacher P. Impact of short-term meditation and expectation on executive brain functions. Behav Brain Res. 2016;297:268–276. doi: 10.1016/j.bbr.2015.10.012. [DOI] [PubMed] [Google Scholar]
- 35.Tsai MH, Chou WL. Attentional orienting and executive control are affected by different types of meditation practice. Conscious Cogn. 2016;46:110–126. doi: 10.1016/j.concog.2016.09.020. [DOI] [PubMed] [Google Scholar]
- 36.Gard T, Holzel BK, Lazar SW. The potential effects of meditation on age-related cognitive decline: a systematic review. Ann N Y Acad Sci. 2014;1307:89–103. doi: 10.1111/nyas.12348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wong WP, Coles J, Chambers R, Wu DB, Hassed C. The effects of mindfulness on older adults with mild cognitive impairment. J Alzheimers Dis Rep. 2017;1(1):181–193. doi: 10.3233/ADR-170031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Dwivedi M, Dubey N, Pansari AJ, Bapi RS, Das M, Guha M, Banerjee R, Pramanick G, Basu J, Ghosh A. Effects of meditation on structural changes of the brain in patients with mild cognitive impairment or Alzheimer's disease dementia. Front Hum Neurosci. 2021;15:728993. doi: 10.3389/fnhum.2021.728993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Esch T, Duckstein J, Welke J, Braun V. Mind/body techniques for physiological and psychological stress reduction: stress management via Tai Chi training - a pilot study. Med Sci Monit. 2007;13(11):CR488–497. [PubMed] [Google Scholar]
- 40.Taylor-Piliae RE, Newell KA, Cherin R, Lee MJ, King AC, Haskell WL. Effects of Tai Chi and Western exercise on physical and cognitive functioning in healthy community-dwelling older adults. J Aging Phys Act. 2010;18(3):261–279. doi: 10.1123/japa.18.3.261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Jin P. Efficacy of Tai Chi, brisk walking, meditation, and reading in reducing mental and emotional stress. J Psychosom Res. 1992;36(4):361–370. doi: 10.1016/0022-3999(92)90072-A. [DOI] [PubMed] [Google Scholar]
- 42.Jahnke R, Larkey L, Rogers C, Etnier J, Lin F. A comprehensive review of health benefits of qigong and tai chi. Am J Health Promot. 2010;24(6):e1–e25. doi: 10.4278/ajhp.081013-LIT-248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wang W, Sawada M, Noriyama Y, Arita K, Ota T, Sadamatsu M, Kiyotou R, Hirai M, Kishimoto T. Tai Chi exercise versus rehabilitation for the elderly with cerebral vascular disorder: a single-blinded randomized controlled trial. Psychogeriatrics. 2010;10(3):160–166. doi: 10.1111/j.1479-8301.2010.00334.x. [DOI] [PubMed] [Google Scholar]
- 44.Forgas JP. Mood effects on cognition: affective influences on the content and process of information processing and behavior. Cambridge: Academic press; 2017. [Google Scholar]
- 45.Paul K, Pourtois G, Harmon-Jones E. Modulatory effects of positive mood and approach motivation on reward processing: two sides of the same coin? Cogn Affect Behav Neurosci. 2020;20(2):236–249. doi: 10.3758/s13415-019-00764-6. [DOI] [PubMed] [Google Scholar]
- 46.Zhang NN, Lü XB, Ni W, Mao WQ. Effect of long-term Tai Chi exercise on cognitive function of middle-aged and old people. Chin J Clin Rehab. 2006;10(26):7–9. [Google Scholar]
- 47.Klein P, Picard G, Baumgarden J, Schneider R. Meditative movement, energetic, and physical analyses of three qigong exercises: unification of eastern and western mechanistic exercise theory. Medicines (Basel) 2017;4(4):69. doi: 10.3390/medicines4040069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Pei H, Ma L, Cao Y, Wang F, Li Z, Liu N, Liu M, Wei Y, Li H. Traditional Chinese medicine for Alzheimer's disease and other cognitive impairment: a review. Am J Chin Med. 2020;48(3):487–511. doi: 10.1142/S0192415X20500251. [DOI] [PubMed] [Google Scholar]
- 49.Zhuang Y. Qi-gong life-nurturing. Baton Rouge: Yajun Zhuang; 2009. [Google Scholar]
- 50.Hsieh CC, Lin PS, Hsu WC, Wang JS, Huang YC, Lim AY, Hsu YC. The effectiveness of a virtual reality-based Tai Chi exercise on cognitive and physical function in older adults with cognitive impairment. Dement Geriatr Cogn Disord. 2018;46(5–6):358–370. doi: 10.1159/000494659. [DOI] [PubMed] [Google Scholar]
- 51.Zhou S, Zhang Y, Kong Z, Loprinzi PD, Hu Y, Ye J, Liu S, Yu JJ, Zou L. The effects of Tai Chi on markers of atherosclerosis, lower-limb physical function, and cognitive ability in adults aged over 60: a randomized controlled trial. Int J Environ Res Public Health. 2019;16(5):753. doi: 10.3390/ijerph16050753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Solianik R, Mickevičienė D, Žlibinaitė L, Čekanauskaitė A. Tai chi improves psychoemotional state, cognition, and motor learning in older adults during the COVID-19 pandemic. Exp Gerontol. 2021;150:111363. doi: 10.1016/j.exger.2021.111363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.El Said SMS, Adly NN, Abdul-Rahman SA. Executive function and physical function among community-dwelling egyptian older adults. J Alzheimers Dis. 2021;80(4):1583–1589. doi: 10.3233/JAD-201423. [DOI] [PubMed] [Google Scholar]
- 54.Fitzpatrick AL, Buchanan CK, Nahin RL, Dekosky ST, Atkinson HH, Carlson MC, Williamson JD. Associations of gait speed and other measures of physical function with cognition in a healthy cohort of elderly persons. J Gerontol A Biol Sci Med Sci. 2007;62(11):1244–1251. doi: 10.1093/gerona/62.11.1244. [DOI] [PubMed] [Google Scholar]
- 55.Gatto NM, Garcia-Cano J, Irani C, Liu T, Arakaki C, Fraser G, Wang C, Lee GJ. Observed physical function is associated with better cognition among elderly adults: the adventist health study-2. Am J Alzheimers Dis Other Demen. 2020;35:1533317520960868. doi: 10.1177/1533317520960868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.George KM, Gilsanz P, Peterson RL, Glymour MM, Mayeda ER, Mungas DM, Miles SQ, Whitmer RA. Physical performance and cognition in a diverse cohort: Kaiser Healthy Aging and Diverse Life Experiences (KHANDLE) Study. Alzheimer Dis Assoc Disord. 2021;35(1):23–29. doi: 10.1097/WAD.0000000000000428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Sprague BN, Phillips CB, Ross LA. Age-varying relationships between physical function and cognition in older adulthood. J Gerontol B Psychol Sci Soc Sci. 2019;74(5):772–784. doi: 10.1093/geronb/gbx126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Zhao X, Jin L, Sun SB. The bidirectional association between physical and cognitive function among chinese older adults: a mediation analysis. Int J Aging Hum Dev. 2021;92(2):240–263. doi: 10.1177/0091415020940214. [DOI] [PubMed] [Google Scholar]
- 59.Falck RS, Davis JC, Best JR, Crockett RA, Liu-Ambrose T. Impact of exercise training on physical and cognitive function among older adults: a systematic review and meta-analysis. Neurobiol Aging. 2019;79:119–130. doi: 10.1016/j.neurobiolaging.2019.03.007. [DOI] [PubMed] [Google Scholar]
- 60.Solloway MR, Taylor SL, Shekelle PG, Miake-Lye IM, Beroes JM, Shanman RM, Hempel S. An evidence map of the effect of Tai Chi on health outcomes. Syst Rev. 2016;5(1):126. doi: 10.1186/s13643-016-0300-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Wei L, Chai Q, Chen J, Wang Q, Bao Y, Xu W, Ma E. The impact of Tai Chi on cognitive rehabilitation of elder adults with mild cognitive impairment: a systematic review and meta-analysis. Disabil Rehabil. 2022;44(11):2197–2206. doi: 10.1080/09638288.2020.1830311. [DOI] [PubMed] [Google Scholar]
- 62.Zou L, Han J, Li C, Yeung AS, Hui SSC, Tsang WW, Ren Z, Wang L. Effects of Tai Chi on lower limb proprioception in adults aged over 55: a systematic review and meta-analysis. Arch Phys Med Rehab. 2019;100(6):1102–1113. doi: 10.1016/j.apmr.2018.07.425. [DOI] [PubMed] [Google Scholar]
- 63.Borenstein M, Hedges LV, Higgins JPT, Rothstein HR. Introduction to meta-analysis. UK: John Wiley & Sons, Ltd.; 2009.
- 64.Baker WL, Michael White C, Cappelleri JC, Kluger J, Coleman CI, From the Health Outcomes P. Group EC Understanding heterogeneity in meta-analysis: the role of meta-regression. Int J Clin Pract. 2009;63(10):1426–1434. doi: 10.1111/j.1742-1241.2009.02168.x. [DOI] [PubMed] [Google Scholar]
- 65.Sterne JAC, Savovic J, Page MJ, Elbers RG, Blencowe NS, Boutron I, Cates CJ, Cheng HY, Corbett MS, Eldridge SM, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:l4898. doi: 10.1136/bmj.l4898. [DOI] [PubMed] [Google Scholar]
- 66.Borenstein M, Hedges LV, Higgins JP, Rothstein HR. A basic introduction to fixed-effect and random-effects models for meta-analysis. Res Synth Methods. 2010;1(2):97–111. doi: 10.1002/jrsm.12. [DOI] [PubMed] [Google Scholar]
- 67.Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA. The Cochrane Collaboration. 2020. Cochrane handbook for systematic reviews of interventions version 6.1. [Google Scholar]
- 68.IntHout J, Ioannidis JP, Rovers MM, Goeman JJ. Plea for routinely presenting prediction intervals in meta-analysis. BMJ Open. 2016;6(7):e010247. doi: 10.1136/bmjopen-2015-010247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Stijnen T, White IR, Schmid CH. Analysis of univariate study-level summary data using normal models. FL, USA: CRC Press; 2021. [Google Scholar]
- 70.Adcock M, Fankhauser M, Post J, Lutz K, Zizlsperger L, Luft AR, Guimarães V, Schättin A, de Bruin ED. Effects of an in-home multicomponent exergame training on physical functions, cognition, and brain volume of older adults: a randomized controlled trial. Front Med (Lausanne) 2019;6:321. doi: 10.3389/fmed.2019.00321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Adcock M, Thalmann M, Schättin A, Gennaro F, de Bruin ED. A pilot study of an in-home multicomponent exergame training for older adults: feasibility, usability and pre-post evaluation. Front Aging Neurosci. 2019;11:304. [DOI] [PMC free article] [PubMed]
- 72.Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Lavretsky H, Alstein LL, Olmstead RE, Ercoli LM, Riparetti-Brown M, Cyr NS, Irwin MR. Complementary use of Tai Chi Chih augments escitalopram treatment of geriatric depression: a randomized controlled trial. Am J Geriatric Psychiatry. 2011;19(10):839–850. doi: 10.1097/JGP.0b013e31820ee9ef. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Tsai PF, Chang JY, Beck C, Kuo YF, Keefe FJ. A pilot cluster-randomized trial of a 20-week tai chi program in elders with cognitive impairment and osteoarthritic knee: effects on pain and other health outcomes. J Pain Symptom Manage. 2013;45(4):660–669. doi: 10.1016/j.jpainsymman.2012.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Tsang HW, Lee JL, Au DW, Wong KK, Lai K. Developing and testing the effectiveness of a novel health qigong for frail elders in Hong Kong: a preliminary study. Evid Based Complement Altern Med. 2013;2013:827392. doi: 10.1155/2013/827392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Lam L, Chan W, Kwok T, Chiu H. Effectiveness of Tai Chi in maintenance of cognitive and functional abilities in mild cognitive impairment: a randomised controlled trial. Hong Kong Med J. 2014;20(3 Suppl 3):20–23. [PubMed] [Google Scholar]
- 77.Sun J, Kanagawa K, Sasaki J, Ooki S, Xu H, Wang L. Tai chi improves cognitive and physical function in the elderly: a randomized controlled trial. J Phys Ther Sci. 2015;27(5):1467–1471. doi: 10.1589/jpts.27.1467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Hwang HF, Chen SJ, Lee-Hsieh J, Chien DK, Chen CY, Lin MR. Effects of home-based tai chi and lower extremity training and self-practice on falls and functional outcomes in older fallers from the emergency department—a randomized controlled trial. J Am Geriatr Soc. 2016;64(3):518–525. doi: 10.1111/jgs.13952. [DOI] [PubMed] [Google Scholar]
- 79.Lu X, Siu KC, Fu SN, Hui-Chan CW, Tsang WW. Effects of Tai Chi training on postural control and cognitive performance while dual tasking–a randomized clinical trial. J Complement Integr Med. 2016;13(2):181–187. doi: 10.1515/jcim-2015-0084. [DOI] [PubMed] [Google Scholar]
- 80.van West KR, Stinear C, Buck R. The effects of poi on physical and cognitive function in healthy older adults. J Aging Phys Act. 2018;27(1):44–52. doi: 10.1123/japa.2017-0273. [DOI] [PubMed] [Google Scholar]
- 81.Li QS. Effect of Health Qigong Baduanjin on executive function and physical function in patients with Mild cognitive impairment [dissertation]. China: Shenyang Sport University; 2018.
- 82.Lipsitz LA, Macklin EA, Travison TG, Manor B, Gagnon P, Tsai T, Aizpurúa II, Lo OY, Wayne PM. A cluster randomized trial of Tai chi vs health education in subsidized housing: the MI-WiSH study. J Am Geriatr Soc. 2019;67(9):1812–1819. doi: 10.1111/jgs.15986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Chewning B, Hallisy KM, Mahoney JE, Wilson D, Sangasubana N, Gangnon R. Disseminating tai chi in the community: promoting home practice and improving balance. Gerontologist. 2020;60(4):765–775. doi: 10.1093/geront/gnz006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Zheng G, Zheng Y, Xiong Z, Ye B. Effect of Baduanjin exercise on cognitive function in patients with post-stroke cognitive impairment: a randomized controlled trial. Clin Rehabil. 2020;34(8):1028–1039. doi: 10.1177/0269215520930256. [DOI] [PubMed] [Google Scholar]
- 85.Wu MT, Tang PF, Tseng WYI, Hsu YC, Chen YJ, Goh JO, Chou TL, Chang YK, Gau SSF, Lan C. Integrity of the Prefronto-striato-thalamo-prefrontal loop predicts Tai Chi Chuan training effects on cognitive task-switching in middle-aged and older adults. Front Aging Neurosci. 2021;12:602191. [DOI] [PMC free article] [PubMed]
- 86.Jiayuan Z, Xiang-Zi J, Li-Na M, Jin-Wei Y, Xue Y. Effects of mindfulness-based tai chi chuan on physical performance and cognitive function among cognitive frailty older adults: a six-month follow-up of a randomized controlled trial. J Prev Alzheimers Dis. 2022;9(1):104–112. doi: 10.14283/jpad.2021.40. [DOI] [PubMed] [Google Scholar]
- 87.Lavretsky H, Milillo MM, Kilpatrick L, Grzenda A, Wu P, Nguyen SA, Ercoli LM, Siddarth P. A randomized controlled trial of Tai Chi Chih or health education for geriatric depression. Am J Geriatr Psychiatry. 2022;30(3):392–403. doi: 10.1016/j.jagp.2021.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Lin R, Cui S, Yang J, Yang H, Feng Z, Wahner-Roedler DL, Zhou X, Salinas M, Mallory MJ, Do A, et al. Effects of Tai Chi on patients with mild cognitive impairment: a systematic review and meta-analysis of randomized controlled trials. Biomed Res Int. 2021;2021:5530149. doi: 10.1155/2021/5530149. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 89.Walsh EI, Smith L, Northey J, Rattray B, Cherbuin N. Towards an understanding of the physical activity-BDNF-cognition triumvirate: a review of associations and dosage. Ageing Res Rev. 2020;60:101044. doi: 10.1016/j.arr.2020.101044. [DOI] [PubMed] [Google Scholar]
- 90.Siu MY, Lee DTF. Effects of tai chi on cognition and instrumental activities of daily living in community dwelling older people with mild cognitive impairment. BMC Geriatr. 2018;18(1):37. doi: 10.1186/s12877-018-0720-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Yu AP, Chin EC, Yu DJ, Fong DY, Cheng CP, Hu X, Wei GX, Siu PM. Tai Chi versus conventional exercise for improving cognitive function in older adults: a pilot randomized controlled trial. Sci Rep. 2022;12(1):8868. doi: 10.1038/s41598-022-12526-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Ji Z, Li A, Feng T, Liu X, You Y, Meng F, Wang R, Lu J, Zhang C. The benefits of Tai Chi and brisk walking for cognitive function and fitness in older adults. PeerJ. 2017;5:e3943. [DOI] [PMC free article] [PubMed]
- 93.Choo YT, Jiang Y, Hong J, Wang W. Effectiveness of Tai Chi on quality of life, depressive symptoms and physical function among community-dwelling older adults with chronic disease: a systematic review and meta-analysis. Int J Nurs Stud. 2020;111:103737. doi: 10.1016/j.ijnurstu.2020.103737. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Appendix. Search Strategy; Pubmed.
Data Availability Statement
The datasets used and analyzed during the current study are available from the corresponding author upon reasonable request.