Abstract
Background
Following sexual abuse, children and young people may develop a range of psychological problems, including anxiety, depression, post‐traumatic stress disorder (PTSD), and a range of behaviour problems. Those working with children and young people experiencing these problems may use one or more of a range of psychological approaches.
Objectives
To assess the relative effectiveness of psychological interventions compared to other treatments or no treatment controls, to overcome psychological consequences of sexual abuse in children and young people up to 18 years of age.
Secondary objectives
To rank psychotherapies according to their effectiveness. To compare different ‘doses’ of the same intervention.
Search methods
In November 2022 we searched CENTRAL, MEDLINE, Embase, PsycINFO, 12 other databases and two trials registers. We reviewed the reference lists of included studies, alongside other work in the field, and communicated with the authors of included studies.
Selection criteria
We included randomised controlled trials comparing psychological interventions for sexually abused children and young people up to 18 years old with other treatments or no treatments. Interventions included: cognitive behavioural therapy (CBT), psychodynamic therapy, family therapy, child centred therapy (CCT), and eye movement desensitisation and reprocessing (EMDR). We included both individual and group formats.
Data collection and analysis
Two review authors independently selected studies, extracted data and assessed the risk of bias for our primary outcomes (psychological distress/mental health, behaviour, social functioning, relationships with family and others) and secondary outcomes (substance misuse, delinquency, resilience, carer distress and efficacy).
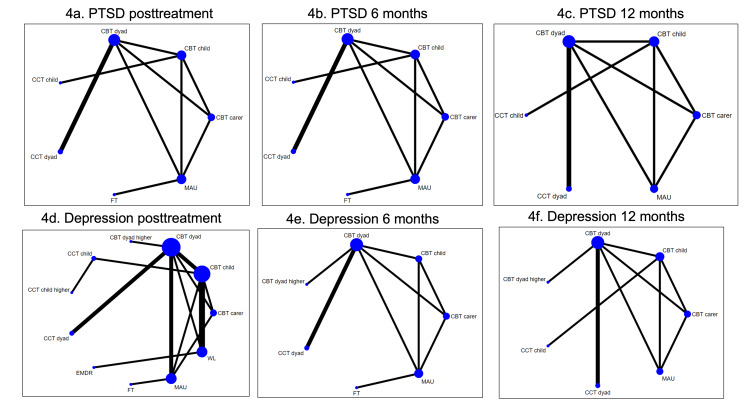
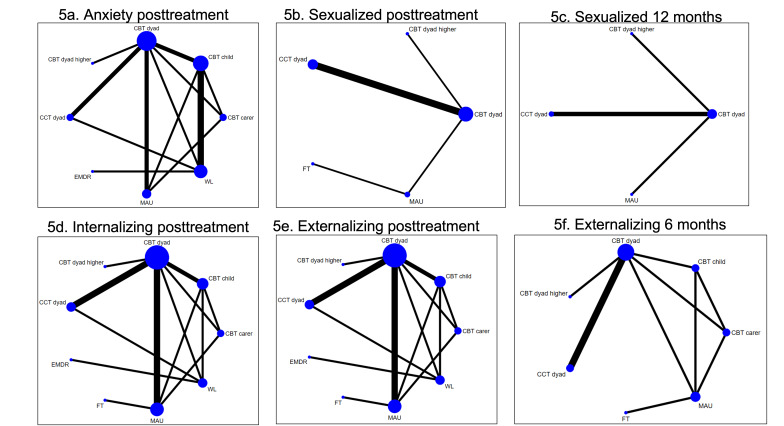
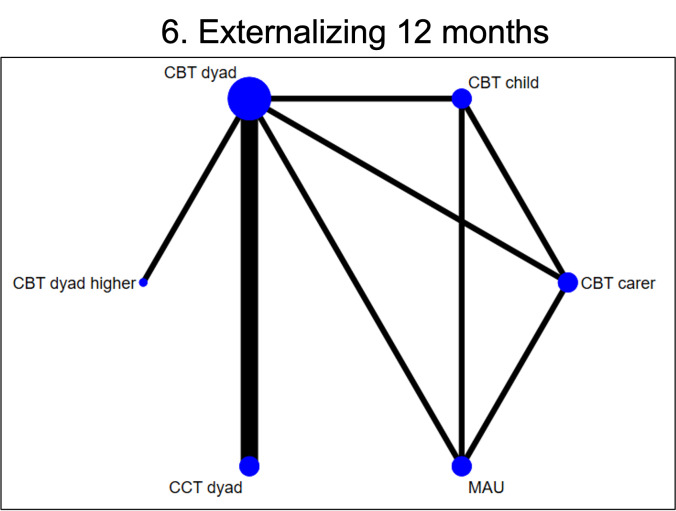
We considered the effects of the interventions on all outcomes at post‐treatment, six months follow‐up and 12 months follow‐up. For each outcome and time point with sufficient data, we performed random‐effects network and pairwise meta‐analyses to determine an overall effect estimate for each possible pair of therapies. Where meta‐analysis was not possible, we report the summaries from single studies. Due to the low number of studies in each network, we did not attempt to determine the probabilities of each treatment being the most effective relative to the others for each outcome at each time point.
We rated the certainty of evidence with GRADE for each outcome.
Main results
We included 22 studies (1478 participants) in this review. Most of the participants were female (range: 52% to 100%), and were mainly white. Limited information was provided on socioeconomic status of participants. Seventeen studies were conducted in North America, with the remaining studies conducted in the UK (N = 2), Iran (N = 1), Australia (N = 1) and Democratic Republic of Congo (N = 1). CBT was explored in 14 studies and CCT in eight studies; psychodynamic therapy, family therapy and EMDR were each explored in two studies. Management as usual (MAU) was the comparator in three studies and a waiting list was the comparator in five studies. For all outcomes, comparisons were informed by low numbers of studies (one to three per comparison), sample sizes were small (median = 52, range 11 to 229) and networks were poorly connected. Our estimates were all imprecise and uncertain.
Primary outcomes At post‐treatment, network meta‐analysis (NMA) was possible for measures of psychological distress and behaviour, but not for social functioning. Relative to MAU, there was very low certainty evidence that CCT involving parent and child reduced PTSD (standardised mean difference (SMD) ‐0.87, 95% confidence intervals (CI) ‐1.64 to ‐0.10), and CBT with only the child reduced PTSD symptoms (SMD ‐0.96, 95% CI ‐1.72 to ‐0.20). There was no clear evidence of an effect of any therapy relative to MAU for other primary outcomes or at any other time point.
Secondary outcomes Compared to MAU, there was very low certainty evidence that, at post‐treatment, CBT delivered to the child and the carer might reduce parents' emotional reactions (SMD ‐6.95, 95% CI ‐10.11 to ‐3.80), and that CCT might reduce parents' stress. However, there is high uncertainty in these effect estimates and both comparisons were informed only by one study. There was no evidence that the other therapies improved any other secondary outcome.
We attributed very low levels of confidence for all NMA and pairwise estimates for the following reasons. Reporting limitations resulted in judgements of 'unclear' to 'high' risk of bias in relation to selection, detection, performance, attrition and reporting bias; the effect estimates we derived were imprecise, and small or close to no change; our networks were underpowered due to the low number of studies informing them; and whilst studies were broadly comparable with regard to settings, the use of a manual, the training of the therapists, the duration of treatment and number of sessions offered, there was considerable variability in the age of participants and the format in which the interventions were delivered (individual or group).
Authors' conclusions
There was weak evidence that both CCT (delivered to child and carer) and CBT (delivered to the child) might reduce PTSD symptoms at post‐treatment. However, the effect estimates are uncertain and imprecise. For the remaining outcomes examined, none of the estimates suggested that any of the interventions reduced symptoms compared to management as usual.
Weaknesses in the evidence base include the dearth of evidence from low‐ and middle‐income countries. Further, not all interventions have been evaluated to the same extent, and there is little evidence regarding the effectiveness of interventions for male participants or those from different ethnicities. In 18 studies, the age ranges of participants ranged from 4 to 16 years old or 5 to 17 years old. This may have influenced the way in which the interventions were delivered, received, and consequently influenced outcomes.
Many of the included studies evaluated interventions that were developed by members of the research team. In others, developers were involved in monitoring the delivery of the treatment. It remains the case that evaluations conducted by independent research teams are needed to reduce the potential for investigator bias.
Studies addressing these gaps would help to establish the relative effectiveness of interventions currently used with this vulnerable population.
Keywords: Adolescent; Child; Child, Preschool; Female; Humans; Male; Cognitive Behavioral Therapy; Cognitive Behavioral Therapy/methods; Network Meta-Analysis; Psychosocial Intervention; Psychotherapy; Psychotherapy/methods; Sex Offenses
Plain language summary
How effective are the psychological interventions used for treating the consequences of sexual abuse in children and adolescents
Key messages
• A number of psychological therapies are used to help children and young people overcome the consequences of sexual abuse.
• There is largely uncertain evidence to suggest that any particular interventions is better than management as usual in helping children and young people recover from sexual abuse.
• We need more and better studies of interventions to establish whether one is better than another in addressing the various consequences of sexual abuse.
What do we mean by psychological interventions?
Psychological interventions are those that try to bring about change in people. They are often referred to as 'talking therapies' but they also include therapies in which communication between therapist and patient is based on activity, such as play, or art.
There is a range of psychological interventions that are used to help children and young people who have been sexually abused to overcome the sorts of difficulties that can develop as a result of the abuse; for example, post‐traumatic stress disorder (PTSD), anxiety, depression, and a range of behaviour problems.
Why is this important for children and young people who have been sexually abused?
Previous systematic reviews suggest that psychological therapies can improve outcomes for children, but we do not know whether some therapies are more effective than others.
What did we want to find out?
We wanted to find out which interventions were best for treating the range of problems that can occur following sexual abuse. We wanted to find out if we could rank them in order of how well they work. For example, we wanted to find out which intervention was the best at helping children who have PTSD, or children who are depressed. Which was second best? And so on.
What did we do?
We searched for studies that examined the effectiveness of a range of psychological therapies, including cognitive‐behavioural therapy (CBT), eye movement desensitisation and reprocessing (known as EMDR), child‐centred therapy (CCT), psychodynamic therapy, and family therapy. We included studies that compared:
• one therapy to another therapy;
• different 'doses' of therapy; for example, eight weeks of a therapy to 16 weeks of the same therapy;
• one version of a therapy with another version; for example, one that involved parents as well as the child with the same therapy that did not;
• one therapy to management as usual; and
• one therapy to no therapy (mainly those on a waiting list).
We used methods that allowed us to compare the effectiveness of each therapy against others, for particular outcomes. We summarised the results of the studies and rated our confidence in the evidence, based on factors such as the number of studies and how large or small they were.
What did we find?
We found 22 studies (1478 participants) and most of them were from North America. Fourteen of these examined the effectiveness of CBT and eight examined the effectiveness of CCT. Psychodynamic therapy, family therapy and EMDR were each examined in two studies. Management as usual was the comparator in three studies and a waiting list was the comparator in five studies.
Main results
On the available evidence it is not clear whether one intervention is more effective than others in helping children and young people who have been sexually abused. There is some evidence, though it is largely uncertain and imprecise, that CBT may be better than management as usual when it comes to reducing the symptoms of PTSD at the end of treatment. No evidence pointed to the effectiveness of other therapies for PTSD, and no therapy appeared to do better than management as usual for the other outcomes we examined.
The evidence base for the effectiveness of other psychotherapeutic interventions for sexually abused children and adolescents is limited, particularly in relation to psychodynamic therapy, family therapy and EMDR.
What are the limitations of the evidence?
Our confidence in the results is not strong. The treatment effects we identified were small or close to 'no change' and not very precise. Whilst the studies were broadly comparable in some respects (settings; the use of a manual to deliver the intervention; the 'amount' of therapy), there was considerable variability in others, such as the age of participants and the format in which the interventions were delivered (individual or group).
The results of further research could differ from the results of this review.
How up to date is this evidence?
The evidence is up to date to 1 November 2022.
Summary of findings
Summary of findings 1. Summary of findings table 1. Results of the indirect evidence for post‐traumatic stress disorder post‐treatment in sexually abused people under 18 years old.
| Estimates of effects, confidence intervals, and certainty of the indirect evidence for post‐traumatic stress disorder post‐treatment in sexually abused people under 18 years old | |||
|
Patient or population: sexually abused people under 18 years old Settings: clinical setting Interventions: WL, FT, EMDR, CCT dyad, CCT child, CBT dyad, CBT child, CBT carer Comparator (reference): MAU | |||
|
Total number of studies: 11 Total number of participants: 627 |
Relative effecta (95% CI) | Quality of the evidence (GRADE) | Interpretations of findings |
| WL | ‐0.15 (‐1.85 to 1.55) | Very low | Uncertain evidence of WL overperforming MAU |
| FT | ‐0.58 (‐1.41 to 0.26) | Very low | Uncertain evidence of FT overperforming MAU |
| EMDR | ‐0.48 (‐1.44 to 0.49) | Very Low | Uncertain evidence of EMDR overperforming MAU |
| CCT dyad | ‐0.87 (‐1.64 to ‐0.10) | Very low | Uncertain evidence of CCT dyad overperforming MAU |
| CCT child | 0.66 (‐0.42 to 1.75) | Very low | Uncertain evidence of CCT child overperforming MAU |
| CBT dyad | ‐0.35 (‐1.55 to 0.85) | Very low | Uncertain evidence of CBT dyad overperforming MAU |
| CBT child | ‐0.96 (‐1.72 to ‐0.20) | Very low | Uncertain evidence of CBT child overperforming MAU |
| CBT carer | ‐0.46 (‐1.22 to 0.29) | Very low | Uncertain evidence of CBT carer overperforming MAU |
| CBT carer: cognitive behavioural therapy delivered only to the carer; CBT child: cognitive behavioural therapy delivered only to the child; CBT dyad: cognitive behavioural therapy delivered to the child and the carer; CCT child: child‐centred therapy delivered only to the child; CCT dyad: child‐centred therapy delivered to the child and the carer; CI: confidence interval; EMDR: eye movement desensitisation and reprocessing; FT: family therapy; MAU: management as usual; NMA: network meta‐analysis; SoF: summary of findings table; WL: waiting list | |||
NMA‐SoF table definitions
aNegative relative effect estimates suggest that the comparator treatments outperformed the reference treatment.
GRADE Working Group grades of evidence High quality: further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: we are very uncertain about the estimate.
We gave a rating of very low confidence to all the estimates of this analysis because of major concerns in 36 effect estimates in the domain 'within‐study bias' (based on the risk of bias assessments), in 28 effect estimates on the domain 'imprecision' (uncertain effect estimates with wide confidence intervals), and concerns about heterogeneity in five estimates (high variability in the results of the studies that contributed to each comparison).
Summary of findings 2. Summary of findings table 2. Results of the indirect evidence for depression post‐treatment in sexually abused people under 18 years old.
| Estimates of effects, confidence intervals, and certainty of the indirect evidence for depression post‐treatment in sexually abused people under 18 years old | |||
|
Patient or population: sexually abused people under 18 years old Settings: clinical setting Interventions: WL, FT, EMDR, CCT dyad, CCT child higher, CCT child, CBT dyad higher, CBT dyad, CBT child, CBT carer Comparison (reference): MAU | |||
|
Total number of studies: 12 Total number of participants: 769 |
Relative effecta (95% CI) | Quality of the evidence (GRADE) | Interpretation of findings |
| WL | ‐1.82 (‐5.04 to 1.40) | Very low | Uncertain evidence of WL overperforming MAU |
| FT | ‐0.42 (‐2.61 to 1.76) | Very low | Uncertain evidence of FT overperforming MAU |
| EMDR | ‐0.72 (‐3.82 to 2.37) | Very low | Uncertain evidence of EMDR overperforming MAU |
| CCT dyad | ‐0.51 (‐3.02 to 2.01) | Very low | Uncertain evidence of CCT dyad overperforming MAU |
| CCT child higher | ‐1.07 (‐3.57 to 1.43) | Very low | Uncertain evidence of CCT child higher overperforming MAU |
| CCT child | ‐0.88 (‐2.69 to 0.94) | Very low | Uncertain evidence of CCT child overperforming MAU |
| CBT dyad higher | 0.98 (‐1.55 to 3.51) | Very low | Uncertain evidence of MAU overperforming CBT dyad higher |
| CBT dyad | 0.07 (‐2.56 to 2.69) | Very low | Uncertain evidence of MAU overperforming CBT dyad |
| CBT child | ‐0.80 (‐2.60 to 1.01) | Very low | Uncertain evidence of CBT child overperforming MAU |
| CBT carer | ‐0.64 (‐2.45 to 1.17) | Very low | Uncertain evidence of CBT carer overperforming MAU |
| CBT carer: cognitive behavioural therapy delivered only to the carer; CBT child: cognitive behavioural therapy delivered only to the child; CBT dyad: cognitive behavioural therapy delivered to the child and the carer; CBT dyad higher: cognitive behavioural therapy delivered to the child and the carer at a higher dose; CCT child: child‐centred therapy delivered only to the child; CCT child higher: child centred therapy delivered only to the child at a higher dose; CCT dyad: child‐centred therapy delivered to the child and the carer; CI: confidence interval; EMDR: eye movement desensitisation and reprocessing; FT: family therapy; MAU: management as usual delivered to the child and the carer; NMA: network meta‐analysis; SoF: summary of findings table; WL: waiting list | |||
NMA‐SoF table definitions
aNegative relative effect estimates suggest that the comparator treatments outperformed the reference treatment.
GRADE Working Group grades of evidence High quality: further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: we are very uncertain about the estimate.
We gave a very low confidence rating for all the estimates as all had major concerns in within‐study bias and imprecision or heterogeneity.
Summary of findings 3. Summary of findings table 3. Results of the indirect evidence for anxiety post‐treatment in sexually abused people under 18 years old.
| Estimates of effects, confidence intervals, and certainty of the indirect evidence for anxiety post‐treatment in sexually abused people under 18 years old | |||
|
Patient or population: sexually abused people under 18 years old Settings: clinical setting Interventions: WL EMDR, CCT dyad, CBT dyad higher, CBT dyad, CBT child, CBT carer Comparison (reference): MAU | |||
|
Total number of studies: 10 Total number of participants: 691 |
Relative effecta (95% CI) | Quality of the evidence (GRADE) | Interpretation of findings |
| WL | 0.50 (‐2.09 to 3.09) | Very Low | Uncertain evidence of MAU overperforming WL |
| EMDR | ‐0.84 (‐2.65 to 0.97) | Very low | Uncertain evidence of EMDR overperforming MAU |
| CCT dyad | ‐0.65 (‐1.97 to 0.67) | Very low | Uncertain evidence of CCT dyad overperforming MAU |
| CBT dyad higher | 0.66 (‐1.18 to 2.50) | Very low | Uncertain evidence of MAU overperforming CBT dyad higher |
| CBT dyad | 0.56 (‐1.44 to 2.55) | Very low | Uncertain evidence of MAU overperforming CBT dyad |
| CBT child | ‐0.13 (‐1.45 to 1.20) | Very low | Uncertain evidence of CBT child overperforming MAU |
| CBT carer | ‐0.01 (‐1.33 to 1.31) | Very low | Uncertain evidence of CBT carer overperforming MAU |
| CBT carer: cognitive behavioural therapy delivered only to the carer; CBT child: cognitive behavioural therapy delivered only to the child; CBT dyad: cognitive behavioural therapy delivered to the child and the carer; CBT dyad higher: cognitive behavioural therapy delivered to the child and the carer at a higher dose; CCT dyad: child‐centred therapy delivered to the child and the carer; CI: confidence interval; EMDR: eye movement desensitisation and reprocessing; MAU: management as usual; NMA: network meta‐analysis; SoF: summary of findings table; WL: waiting list | |||
NMA‐SoF table definitions
aNegative relative effect estimates suggest that the comparator treatments outperformed the reference treatment.
GRADE Working Group grades of evidence High quality: further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: we are very uncertain about the estimate.
We gave a very low rating of confidence in the estimates of these analyses because they had major concerns in three domains: inconsistency, heterogeneity and within‐study bias.
Summary of findings 4. Summary of findings table 4. Results of the indirect evidence for sexualised behaviour post‐treatment in sexually abused people under 18 years old.
| Estimates of effects, confidence intervals, and certainty of the indirect evidence for sexualised behaviour post‐treatment in sexually abused people under 18 years old | |||
|
Patient or population: sexually abused people under 18 years old Settings: clinical setting Interventions: FT, CCT dyad, CBT dyad higher, CBT dyad Comparison (reference): MAU | |||
|
Total number of studies: 7 Total number of participants: 612 |
Relative effecta (95% CI) | Quality of the evidence (GRADE) | Interpretation of findings |
| FT | ‐0.43 (‐1.19 to 0.33) | Very low | Uncertain evidence of FT overperforming MAU |
| CCT dyad | 0.55 (‐0.02 to 1.11) | Very low | Uncertain evidence of MAU overperforming CCT dyad |
| CBT dyad higher | 0.11 (‐0.52 to 0.75) | Very low | Uncertain evidence of MAU overperforming CBT dyad higher |
| CBT dyad | 0.37 (‐0.13 to 0.87) | Very low | Uncertain evidence of MAU overperforming CBT dyad |
| CBT dyad: cognitive behavioural therapy delivered to the child and the carer; CBT dyad higher: cognitive behavioural therapy delivered to the child and the carer at a higher dose; CCT dyad: child‐centred therapy delivered to the child and the carer; CI: confidence interval; FT: family therapy; MAU: management as usual; NMA: network meta‐analysis; SoF: summary of findings table | |||
NMA‐SoF table definitions
aNegative relative effect estimates suggest that the comparator treatments outperformed the reference treatment.
GRADE Working Group grades of evidence High quality: further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: we are very uncertain about the estimate.
We gave a very low confidence rating to all estimates because of major concerns regarding within‐study bias, precision and inconsistency.
Summary of findings 5. Summary of findings table 5. Results of the indirect evidence for internalising behaviour post‐treatment in sexually abused people under 18 years old.
| Estimates of effects, confidence intervals, and certainty of the indirect evidence for internalising behaviour post‐treatment in sexually abused people under 18 years old | |||
|
Patient or population: sexually abused people under 18 years old Settings: clinical setting Interventions: WL, FT, EMDR, CCY dyad, CBT dyad higher, CBT dyad, CBT child, CBT carer Comparator (reference): MAU | |||
|
Total number of studies: 11 Total number of participants: 770 |
Relative effecta (95% CI) | Quality of the evidence (GRADE) | Interpretation of findings |
| WL | 0.22 (‐0.41 to 0.85) | Very low | Uncertain evidence of MAU overperforming WL |
| FT | ‐1.19 (‐2.54 to 0.15) | Very low | Uncertain evidence of FT overperforming MAU |
| EMDR | ‐0.39 (‐1.05 to 0.28) | Very low | Uncertain evidence of EMDR overperforming MAU |
| CCT dyad | ‐0.17 (‐0.76 to 0.42) | Very low | Uncertain evidence of CCT dyad overperforming MAU |
| CBT dyad higher | 0.46 (‐0.24 to 1.17) | Very low | Uncertain evidence of MAU overperforming CBT dyad higher |
| CBT dyad | ‐0.83 (‐1.93 to 0.28) | Very low | Uncertain evidence of CBT dyad overperforming MAU |
| CBT child | ‐0.37 (‐0.97 to 0.23) | Very low | Uncertain evidence of CBT child overperforming MAU |
| CBT carer | ‐0.42 (‐1.03 to 0.18) | Very low | Uncertain evidence of CBT carer overperforming MAU |
| CBT carer: cognitive behavioural therapy delivered only to the carer; CBT child: cognitive behavioural therapy delivered only to the child; CBT dyad: cognitive behavioural therapy delivered to the child and the carer; CBT dyad higher: cognitive behavioural therapy delivered to the child and the carer at a higher dose; CCT dyad: child centred therapy delivered to the child and the carer; CI: confidence interval; EMDR: eye movement desensitisation and reprocessing; FT: family therapy; MAU: management as usual; NMA: network meta‐analysis; SoF: summary of findings table; WL: waiting list | |||
NMA‐SoF table definitions
aNegative relative effect estimates suggest that the comparator treatments outperformed the reference treatment.
GRADE Working Group grades of evidence High quality: further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: we are very uncertain about the estimate.
We gave a very low confidence rating to all the estimates of these analyses because all of them had major concerns in within‐study bias, imprecision, and some concerns regarding inconsistency.
Summary of findings 6. Summary of findings table 6. Results of the indirect evidence for externalising behaviour post‐treatment in sexually abused people under 18 years old.
| Estimates of effects, confidence intervals, and certainty of the indirect evidence for externalising behaviour post‐treatment in sexually abused people under 18 years old | |||
|
Patient or population: sexually abused people under 18 years old Settings: clinical setting Intervention: WL, FT, EMDR, CCT dyad, CBT dyad higher, CBT dyad, CBT child, CBT carer Comparator (reference): MAU | |||
|
Total number of studies: 11 Total number of participants: 749 |
Relative effecta (95% CI) | Quality of the evidence (GRADE) | Interpretation of findings |
| WL | ‐0.01 (‐1.14 to 1.13) | Very low | Uncertain evidence of WL overperforming MAU |
| FT | ‐0.78 (‐2.68 to 1.12) | Very low | Uncertain evidence of FT overperforming MAU |
| EMDR | ‐0.35 (‐1.63 to 0.94) | Very low | Uncertain evidence of EMDR overperforming MAU |
| CCT dyad | ‐0.23 (‐1.25 to 0.79) | Very low | Uncertain evidence of CCT dyad overperforming MAU |
| CBT dyad higher | 0.24 (‐0.99 to 1.47) | Very low | Uncertain evidence of MAU overperforming CBT dyad higher |
| CBT dyad | 0.10 (‐1.41 to 1.62) | Very low | Uncertain evidence of MAU overperforming CBT dyad |
| CBT child | 0.06 (‐0.95 to 1.07) | Very low | Uncertain evidence of MAU overperforming CBT child |
| CBT carer | ‐0.61 (‐1.64 to 0.41) | Very low | Uncertain evidence of CBT carer overperforming MAU |
| CBT carer: cognitive behavioural therapy delivered only to the carer; CBT child: cognitive behavioural therapy delivered only to the child; CBT dyad: cognitive behavioural therapy delivered to the child and the carer; CBT dyad higher: cognitive behavioural therapy delivered to the child and the carer at a higher dose; CCT dyad: child centred therapy delivered to the child and the carer; CI: confidence interval; EMDR: eye movement desensitization and reprocessing; FT: family therapy; MAU: management as usual; NMA: network meta‐analysis; SoF: summary of findings table; WL: waiting list | |||
NMA‐SoF table definitions
aNegative relative effect estimates suggest that the comparator treatments outperformed the reference treatment.
GRADE Working Group grades of evidence High quality: further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: we are very uncertain about the estimate.
We gave a very low confidence rating to all the estimates of this analysis because all of them had major concerns about within‐study bias and imprecision.
Background
Description of the condition
The National Institute for Health and Care Excellence (NICE) in the UK defines child sexual abuse (CSA) as follows.
"[CSA] involves forcing or enticing a child or young person to take part in sexual activities, not necessarily involving a high level of violence, whether or not the child is aware of what is happening. The activities may involve physical contact, including assault by penetration (for example, rape or oral sex) or non‐penetrative acts such as masturbation, kissing, rubbing and touching outside of clothing. They may also include non‐contact activities, such as involving children in looking at, or in the production of, sexual images, watching sexual activities, encouraging children to behave in sexually inappropriate ways, or grooming a child in preparation for abuse (including through the Internet). Sexual abuse is not solely perpetrated by adult males. Women can also commit acts of sexual abuse, as can other children." (NICE 2017, pp 46‐7).
Child sexual exploitation is increasingly recognised as a particular form of child sexual abuse, in which an imbalance of power between a child or young person and others is used "to coerce, manipulate or deceive a child or young person under the age of 18 into sexual activity (a) in exchange for something the victim needs or wants, and/or (b) for the financial advantage of increased status of the perpetrator or facilitator." (NICE 2017, pp 42‐3). Exploitation may occur even in circumstances where the sexual activity appears consensual, and it can occur through the medium of technology.
Prevalence
Estimates of the prevalence of CSA vary widely for a number of reasons. Definitions may differ according to the country where the problem is being studied, data may vary in their availability and quality, and there are methodological differences between studies and differences in the contexts in which victims and perpetrators live; for example, conditions of war and social unrest and injustice; low‐, middle‐ or high‐income countries (Gilbert 2009; Latzman 2017; Singh 2014).
Aiming to describe global prevalence rates of CSA, Barth 2013 conducted a meta‐analysis of studies reporting cases of four predefined types of CSA (forced intercourse, mixed sexual abuse, non‐contact abuse, and contact abuse) in children and adolescents under 18 years of age. Studies were excluded when the country was not reported (indicative of low‐quality reporting) and the sample size was smaller than 1000 (low statistical precision). The 55 included studies were published between 2002 and 2009 and covered 24 countries: 16 studies were conducted in Asia, 14 in North America, 11 in Europe, 9 in Africa and 5 in Central and South America. For girls, the review authors reported pooled prevalence rates for forced intercourse, mixed sexual abuse, non‐contact abuse and contact abuse of 9%, 15%, 31% and 13%, respectively; for boys, the figures were 3%, 8%, 17% and 6%, respectively.
Barth and colleagues also explored contextual variables (geographical region, level of development assessed using the Human Development Index (United Nations Development Programme 2009)) and methodological variables that might explain the heterogeneity of the prevalence estimates between studies (Barth 2013). The reviewers found no statistically significant differences in prevalence rates across studies conducted in different regions or degree of development of the country.
Consequences of CSA
As well as the physical and psychological trauma that may be associated with penetrative sexual abuse (e.g. vulval or anal sores, infections, higher risk of sexually transmitted diseases), children who are sexually abused are at risk of adverse effects in many areas of their development and functioning (Fisher 2017). Child sexual abuse is associated with increased risk of poor physical and mental health, impeded cognitive development, and emotional and behavioural problems. Long and intense experiences of stress during childhood disturb brain architecture, affect metabolic mechanisms and the immune system, and increase the risk of stress‐related chronic illnesses such as hypertension, cardiovascular diseases, and mental ill health (Allnock 2012). Lifetime consequences can include poorer educational outcomes, low socioeconomic status, unemployment, and revictimisation (Allnock 2012; Fisher 2017; Herrmann 2014; McEwen 2007; NSCDC 2007; Woods 2005).
Post‐traumatic stress disorder (PTSD), sexualised behaviour, and internalising and externalising problems are some of the most common psychological problems to affect children and young people following sexual abuse (Fergusson 1999; Harvey 2010; MacMillan 2009; Putnam 2003; Trask 2011). According to the criteria of the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM‐5), a child meets the criteria for a PTSD diagnosis if he or she demonstrates concurrence of at least one symptom of re‐experiencing the traumatic experience, three or more symptoms of avoidant behaviours, and two or more symptoms of autonomic hyperarousal (DSM‐5). Sexualised behaviour is characterised by sexualised play with dolls, putting objects into the anus or vagina, excessive or public masturbation, seductive behaviour, requesting sexual stimulation from adults or other children, and age‐inappropriate sexual knowledge. Internalising problems include social withdrawal, depression, fearfulness, inhibition, and over‐controlled behaviour; while externalising problems include aggression, hyperactivity, and antisocial and under‐controlled behaviour (Kendall‐Tackett 1993; Trask 2011). Infants and children up to six years old are more likely to suffer anxiety, nightmares, PTSD, internalising and externalising problems and sexualised behaviours; children aged 7 to 12 years old are more likely to have school problems, hyperactivity, and aggressive and regressive behaviours; and adolescents (13 to 18 years old) are more likely to harm themselves, suffer depression, and engage in substance abuse and criminal behaviour (Kendall‐Tackett 1993).
Along with the impacts for abused children and their families, societies and governments are impacted too. In the UK, the annual cost of child sexual abuse is GBP 3.2 billion, including (in millions): child depression (GBP 1.6); child suicide (GBP 1.9); adult mental health (GBP 162.7); adult physical health, alcohol and drug misuse (GBP 15.4); criminal justice system (GBP 149); services for children (GBP 124); and productivity losses (GBP 2700) (Saied‐Tessier 2014). In Australia and the USA, the costs of child sexual abuse is included in figures for maltreatment overall. In the USA, the average cost per victim of child maltreatment in 2012 was estimated to be USD 210,200 including: childhood health care costs (USD 32,248), adult medical costs (USD 10,530), productivity losses (USD 144,360), child welfare costs (USD 7720), criminal justice costs (USD 6747) and special education costs (USD 7999) (Fang 2012). In 2016, the lifetime costs attributable to child maltreatment in Australia were estimated at AUD 17.4 billion, including (in millions): health system costs (AUD 3.301), special education costs (AUD 196.4), criminal justice system costs (AUD 904.2), child protection system (AUD 818.2), productivity losses (AUD 2529.9), loss of quality of life related to mental health (AUD 16,601.9) and premature mortality (unfulfilled life expectancy) (AUD 757.2) (McCarthy 2016).
Description of the intervention
Psychological interventions used to treat the consequences of sexual abuse amongst children and young people come from different theoretical orientations: psychodynamic or psychoanalytic, cognitive‐behavioural, systemic, humanistic, and eye movement desensitisation and reprocessing theory (Sánchez‐Meca 2011). The main characteristics of interventions in these groups are described below. Treatment delivery, as well as overall suitability and accessibility, may vary according to the child's age, symptoms, severity of impairment, settings, contexts, training of therapists, availability of mental health services for victims, and other variables.
Systemic therapies
Systemic therapies view families as contexts that ameliorate or reinforce children’s response to the abuse, whether perpetrated inside or outside the family (Carr 2006; Dallos 2010). Generally, systemic therapies maintain that: (1) the children's needs should be addressed within the relational system in which they occur; (2) the system has circular and evolving patterns of behaviour; (3) beliefs and behaviours are the basis of the system's narratives; (4) the members of the system construe what happens from their own frame of reference; (5) meanings emerge from social interactions and context; (6) the therapist should adopt different stances of power with the client's family and the therapeutic relationship; (7) during the therapy, the therapist and the system construct reality; (8) the therapist should be self‐reflective on his or her own constructions; and (9) the therapists should have a positive view of the family and stress its strengths in order to work as a unit (Karakurt 2014; Lorås 2017).
Systemic therapies can be delivered in structured, strategic and social constructivist models. Each model makes different hypotheses about the roots of the family’s problems and thereby the ways in which the therapy is expected to lead to changes (Tickle 2016). However, similar treatment techniques are employed across models, including (Lorås 2017):
adaptive reframing of situations, using metaphors and externalisation of thoughts, feelings and beliefs;
creation of alternative stories of the family’s problems in which the problem is not the dominant trait of the system;
a focus on strengths and solutions: therapists encourage family members to seek change with their own resources and efforts; and
reflecting: the therapy is seen as a safe space where family members feel free to listen, acknowledge and discuss different positions.
The therapy, which can last several weeks to several months, focuses on improving the family’s functioning as a unit, and involves different elements such as psychoeducation, developing maps of family patterns, and narrative techniques (Carr 2006; Dallos 2010; Goepfert 2015; Solomon 2012; Spain 2017).
Child Centred Therapy
Child‐centred therapy emerged in the 1950s and 1960s as a response to the behavioural and psychoanalytic approaches. Humanistic theory proposed a shift from viewing a lack of free will in human actions, behaviours, cognitions and decisions, towards viewing a client capable of self‐determination. Person‐centred therapy is based on the premise that clients have an inherent tendency to develop their potential (termed 'self‐actualisation'), and regards the therapeutic relationship as curative in its own right (Rogers 1951). The manifestation of the problem in the moment and a focus on present feelings is considered the most important focus for therapy. With its fundamental postulate that play is the child’s natural medium of expression, non‐directive play therapy offers the child the opportunity to ‘play out’ their feelings, problems and difficulties, and therefore to develop a more positive image of themselves rather than relying on external ‘conditions of worth’ (Axline 1947). It is by the constant recognition and clarification of the emotions in the non‐directive (play) therapy that the child’s (or young person’s) insights into the feelings that motivate behaviour and self‐definition can emerge.
The children's free expression of themselves is facilitated by communicating three basic therapist attitudes: (1) empathy; (2) genuineness; and (3) unconditional positive regard. The primary therapeutic objective is to provide the children with the maximum opportunity to express their feelings, so that these can be recognised and clarified, and the children is eventually enabled to identify their own feelings. The treatment is delivered in individual format and the length varies on the basis of the children's needs (Cain 2016; Hofmann 2017).
Cognitive behavioural therapy (CBT) interventions and trauma‐focused CBT (TF‐CBT)
CBT interventions are multi‐component interventions that draw primarily on cognitive theories of learning, with particular attention on how the meaning we attribute to events mediates their impact. More broadly, CBT treatments draw on a range of theories, including systems theory, social learning theory, operant and classical conditioning. Treatment is also informed by what is known about the problems it seeks to address. For example, when used in the treatment of maltreated children, therapists also draw on attachment theory and neurodevelopmental theories of trauma, as well as theories of child and adolescent development.
Trauma‐focused CBT (TF‐CBT) is one of the most widely used cognitive behavioural interventions. Developed by Esther Deblinger, Judith Cohen and Anthony Mannarino (see Cohen 2006; Deblinger 1996a), it takes the form of a sequential programme comprising three phases of similar length (see Cohen 2018 for a full description) and summarised in the acronym PRACTICE.
-
Phase 1 Stabilisation and skills enhancement. This includes:
psychoeducation about the impact of sexual abuse (giving parents and children information about sexual abuse, such as why it happens, who is affected, how children feel and the impact it can have on them and their parents), and parenting skills to help parents support their children and manage the ‘fall‐out’ that sexual abuse can have in relation to child behaviour problems;
relaxation training, to reduce and manage stress;
affective skills, to assist in managing the emotional consequences of trauma (i.e. dysregulation or difficulties to manage emotional distress); and
cognitive processing skills, to help parents and children understand the relationship between thoughts, feelings and behaviours, and to develop more accurate and helpful thoughts.
-
Phase 2
Trauma narration and processing. In this phase children and parents are helped to develop a ‘trauma narrative’ and engage in processing it cognitively.
-
Phase 3 Consolidation. This last phase encompasses:
in vivo exposure (e.g. exposure to environmental cues associated with the abuse, like sounds, smells, locations);
conjoint sessions with parents and children to improve communication, both generally and in relation to the sexual abuse; and
enhancing safety.
This structured, yet flexible, programme (e.g. if children are at risk, issues of safety may be dealt with early on in the programme) is typically delivered in 8 to 16 sessions. It may be delivered in either individual or group format, with separate sessions for carer(s) and child, combined with conjoint sessions. When implemented with young people in residential settings, the length of treatment can extend to some 25 sessions.
Psychodynamic therapies
Psychodynamic therapies encompass all forms of psychoanalysis and psychoanalytically‐derived psychotherapy. Psychoanalysis is a clinical and theoretical discipline originating from Sigmund Freud’s proposition that unconscious mental forces, called instincts or ‘instinctual drives’, motivate and shape human perceptions and behaviour (Likierman 1999). Psychoanalysis is based upon exploration of the unconscious, resulting in insights gained by the analysis of the transference relationship. ‘Transference’ refers to the patient’s unconscious motives and personality structure, as expressed in the relationship with the therapist, and can be defined as a re‐enacted memory of earlier situations, developmental stages and relationships. Unconscious traces of these memories and associated ideas and emotions are believed to shape the patient’s perception of the therapist and their behaviour towards him or her (Prochaska 1999; Shemilt 2007). Following Freud, many diverging psychodynamic theories were developed by emphasising different aspects of personal development as the core organising principles for personality and psychopathology.
Psychodynamic child psychotherapies, as modern variants of child psychoanalysis, are briefer and goal directed, incorporating a psychoanalytic understanding of pathology and its development. The primary focus of child psychotherapy is the strengthening of ego defences and the amelioration of specific symptoms or problem areas. Concurrent with individual therapy for the child, the parents or carers may be engaged in psychotherapy. Close attention is paid to contextual or environmental issues and their active modification (Harper 1995; Kegerreis 2010).
Eye movement desensitisation and reprocessing (EMDR)
Eye movement desensitisation and reprocessing (EMDR) is a therapeutic intervention that was originally designed to treat psychological distress associated with trauma (Shapiro 1989). EMDR is one of only two treatments approved by NICE for symptoms of PTSD including children over five years old (NICE 2018). It is recognised by the World Health Organization (WHO) as an effective therapy for people who have experienced trauma (WHO 2013).
During EMDR a three‐pronged approach is used to engage the children with processing: i) the disturbing memory of a traumatic experience that is contributing to the present dysfunction; ii) the triggers that elicit the disturbance (present); and iii) the installation of future templates related to adequately coping with the upsetting events (future) (Shapiro 2001). These are addressed using the following eight phases (Shapiro 2015):
Phase 1 (Children's history): The clinician assesses the children's suitability for the treatment, obtains background information and identifies memory networks that would facilitate the processing of the disturbing memory.
Phase 2 (Preparation): Suitable children are explained about EMDR techniques and processes. The disturbing memory to process is identified. Self‐control techniques are taught to the children for them to use when triggers elicit the disturbing memory.
Phase 3 (Assessment): The memory of the traumatic event is accessed, and its components are disentangled by identifying the physical sensations, emotions, mental images and bad and positive beliefs associated with the memory.
Phase 4 (Desensitisation): Bilateral dual attention stimuli (e.g. eye movements) are utilised to start re‐processing of the disturbing memory.
Phase 5 (Installation): The clinician identifies a children's positive self‐believe and try to link it to positive cognitive networks and to generalise it to the memory that the client has been processing.
Phase 6 (Body scan): The children focus on processing physical discomfort associated to the traumatic event.
Phase 7 (Closure): The focus of the sessions shifts from the disturbing memory to positive memory networks.
Phase 8 (Revaluation): The clinician assesses the psychological status.
Through the bilateral stimulation techniques of EMDR, the distressing memories, sensations and feelings associated with the traumatic experience are surfaced and attempted to be eased by bringing the children to a relaxed state where they can develop coping strategies or positive beliefs about themselves.
During the EMRD session, the children are instructed to focus on recalling a traumatic memory in brief sequential doses, while simultaneously focusing on an external stimulus such as tracking the therapist’s finger being waved back and forth in front of the client in a precisely prescribed manner (though a variety of other stimuli, including hand‐tapping and audio stimulation, are often used) (Shapiro 1993; Shapiro 2007). The process of bilateral stimuli is repeated until the child consigns a positive thought in place of the older negative thought. The number of sessions depends on the severity of traumatic event and negative memories. EMDR therapy can be modified dependent upon the specific needs and developmental stage of the child or adolescent. For some children, especially very young children or those who may struggle to talk about the traumatic event, pictures can be used instead of words. In the course of EMDR therapy, unprocessed memories of traumatic experiences, stored in neural networks, become linked with the adaptively processed memories of positive experiences. This is why it is called 'reprocessing' (Shapiro 2007).
How the intervention might work
Systemic therapies
The treatment includes the following activities: the members of the family are encouraged to share the difficult thoughts and feelings they may be experiencing because of the abuse. They also are encouraged to listen to each other's beliefs and interpretations about what has occurred. Drawings of genograms (family trees) are used to identify system relationships that need to be restored; and solution‐focused ideas and coping skills are used to ease guilt and stress. The understanding of each other’s meanings and the linking of such meanings with beliefs and interpretations about the family’s problems are thought to facilitate the co‐creation of more positive interactions between family members (Lorås 2017).
Structured systemic therapies view family’s difficulties as the result of a disorganised family structure. The therapist will try to restore the system’s boundaries by questioning family members’ interpretations around the dysfunction occurring after the sexual abuse, the structure of the family and the beliefs network of the system. Strategic systemic models attribute families’ difficulties to negative interactions between the family members. The therapist will try to improve these interactions by encouraging the members of the system to assess how the problems influence the system and how each member can contribute to make things better. Social constructivist therapists will prevent the creation of these limitations by offering opportunities for open dialogue and the creation of narratives in which the family’s difficulties are shown as an opportunity for change and moving forward (Tickle 2016).
Child centred therapy
Research about how child‐centred therapy ameliorates a patient's psychological distress is scarce. From a humanistic perspective, the process of change is most accurately conceptualised as a combination of consciousness raising and corrective emotional experiencing, which occurs within the context of a genuine empathic relationship characterised by unconditional positive regard (Cain 2016; Hofmann 2017; Prochaska 1999).
Cognitive behavioural therapy interventions (CBT) and Trauma‐focused CBT (TF‐CBT)
To some extent the description of TF‐CBT provides an indication of how this intervention might work, so we expand a little on the key ‘ingredients’ in this section.
The trauma of sexual abuse, like other trauma, can profoundly and adversely impact the way that children see themselves, the world and their future. Sexual abuse can also adversely impact family cohesiveness and undermine a parent's ability to provide adequate support to affected children. CBT interventions, therefore, include strategies to support or improve family functioning and parenting capacity by addressing parental distress caused by what has happened and how the child is responding.
Psychoeducation is seen as an important component of this support, for both parents and older children, in order to make sense of why children might be thinking, feeling and behaving in particular ways (see Phase 1 of TF‐CBT above under Description of the intervention). Relaxation strategies provide a means of managing the physiological consequences of trauma.
Parenting strategies are designed to help parents managing the behaviour problems that are often associated with sexual abuse, including aggression, withdrawal, anxiety and sexualised behaviours. Teaching children to relax helps to create a context in which they can be helped to express their emotions and acquire cognitive coping skills. Both children (and parents) learn how to label the feelings associated with the abuse and to communicate them to others; they learn to identify maladaptive beliefs and attributions and replace them with those that are more accurate and effective. Depending on their age, children are taught to recognise the signs of anxiety and the internal and external factors that can trigger it, and helped to replace maladaptive responses with adaptive ones.
Unsurprisingly, children and parents may go to some lengths to avoid the reminders of what happened, which may well trigger post‐traumatic stress symptoms or anxiety, but these ‘safety behaviours’ mean that children do not learn that these ‘neutral’ or ‘now neutral’ situations are non‐threatening, and they fail to experience ‘coping’. Gradual exposure (or ‘in vivo mastery’), therefore, is an important component.
TF‐CBT incorporates a specific focus on the trauma itself. This enables the therapist to help the child identify and correct problematic assumptions and concerns that he or she might have as a result of what happened. The explicit focus on the traumatic experience(s) of sexual abuse is thought to help the child to process their experiences in ways that prevent the continuation of intrusive thoughts and flashbacks that can be triggered by current events that themselves carry no threat.
Psychodynamic therapies
In psychodynamic therapies the containment offered by a positive transference relationship with the therapist is thought to facilitate the expression of inner conflicts and the overcoming of resistance. For CSA victims, the defences available to the child to deal with abuse will depend on the maturity of the child at the time of the abuse, as well as the capacity of adults to hear and act on any disclosure. In cases where there has not been suitable intervention at the time, young people are thought to exhibit psychological symptoms and inappropriate behaviour(s), as a result of a reliance on very primitive defence mechanisms (Kegerreis 2010; Lanyado 1999).
The early stages of psychotherapy with sexually abused children focus on building basic trust. The child or young person is encouraged to express their thoughts and fantasies as they occur, and to present them in whatever way they choose (verbally or non‐verbally, or both) using toys, drawings or dramatisation (Harper 1995). While the defences that they have organised must be respected, therapists frequently use a range of psychoanalytic procedures, such as 'clarification' and 'interpretation', to help the child understand the significance of certain behaviours (Horne 1999; Kegerreis 2010). Clarifications may simply involve descriptions of the patient's behaviour or a repetition of the child's statements, to get the child to elaborate on what he or she is doing. At other times they are designed to help the child understand and label feelings of which he or she may be unaware. The technique used by most therapists is 'interpretation' of the child's play or verbal statements, designed to bring unconscious material to awareness. The therapist comments on the relationships between thoughts, feelings and behaviours, or poses tentative hypotheses regarding the 'meaning' of certain behaviours (Harper 1995; Horne 1999; Prochaska 1999).
Through the therapist’s interpretations, unhelpful (i.e. immature) defences can be noted, verbalised and slowly explored, and their meaning analysed when therapy is well established. In the last phases of therapy, the insights that have come about from interpretation of resistance and transference are 'worked through'. The gradual attainment of insight is seen to be a precursor of significant therapeutic change expressed with a strengthened and more mature ego functioning that is better able to cope with the demands of intrapsychic conflicts at the end of therapy (Harper 1995; Horne 1999; Kegerreis 2010).
Eye movement desensitisation and reprocessing (EMDR)
Shapiro’s adaptive information processing (AIP) model posits that mental disorders result from memories of adverse past experiences that were inadequately stored in the memory (Shapiro 2001). Memories stored in a dysfunctional manner can be understood as containing disturbing feelings, thoughts, beliefs and physical sensations that cause continued distress and that may be triggered by present life experiences. Shapiro hypothesises that EMDR therapy facilitates the accessing of the traumatic memory network, so that information processing is enhanced, with new associations forged between the traumatic memory and more adaptive memories or information (Shapiro 1993; Shapiro 2001). These new associations are thought to result in complete information processing, reformulation of associated cognitions, desensitisation of emotional distress, and relief of accompanying physiological arousal, leading to the development of cognitive insights (see Oren 2012; Shapiro 2014; Shapiro 2017).
Common factors and common elements
Although each intervention approach hypothesises a particular set of processes whereby change is brought about, some writers argue that many therapies that appear to be distinct share common elements that account for their impact; for example psychoeducation, exposure, relaxation, etc. (Barth 2012). Others argue that the effectiveness of therapeutic approaches are primarily attributable to nonspecific factors in therapy, such as the nature of the therapeutic relationship (trusting, emotionally charged); the therapeutic context, plus the client's belief that the therapist can help; a narrative that makes sense of the client's problems and a plausible means of dealing with them (see, for example, Frank 1993; Jensen 2005). This review was not designed to explore these factors, but they are discussed in relation to the findings.
Why it is important to do this review
Identifying effective treatments to treat the psychological consequences of child sexual abuse may mitigate the impact of the trauma on the lives of the abused children and youth. Previous systematic reviews assessing the effectiveness of psychotherapeutic interventions to treat the psychological consequences of sexual abuse in children and young people have used pairwise meta‐analyses, which only compare two interventions (Benuto 2015; Corcoran 2008; Harvey 2010; Hetzel‐Riggin 2007; Macdonald 2012; Parker 2013; Reeker 1997; Sánchez‐Meca 2011; Trask 2011). Since not all therapies have been assessed in head‐to‐head comparisons, studies' conclusions may only partially yield information needed to make informed decisions (Tonin 2017).
Network meta‐analysis (NMA) allows comparison of multiple treatments, using direct comparisons of interventions within randomised controlled trials (RCTs) and indirect comparisons across trials based on a common comparator (Hindryckx 2017). NMA provides estimates of the effects of each intervention relative to every other, and allows calculation of the probability of one intervention being the best for a specific outcome (Caldwell 2010). The comparative effectiveness of psychotherapies for adults was already assessed in a previous systematic review with NMA (Wilen 2014). No NMA has been conducted to assess the relative effectiveness of psychotherapeutic interventions drawn from psychodynamic, cognitive behavioural, systemic and humanistic theories, compared to other treatments or no treatment controls, to overcome psychological consequences of sexual abuse in children and young people up to 18 years of age. A likely reason for this is NMA being a relatively new methodology in 2011, when the latest meta‐analyses in the field were conducted. This review aims to bridge this gap, to explore the applicability of NMA in the field and to provide an up‐to‐date account of what is known about what works for whom, for what outcomes, and under what circumstances for this group of children.
Objectives
To assess the relative effectiveness of psychological interventions compared to other treatments or no treatment controls, to overcome psychological consequences of sexual abuse in children and young people up to 18 years of age.
Secondary objectives
To rank psychotherapies according to their effectiveness.
To compare different ‘doses’ of the same intervention.
Methods
Criteria for considering studies for this review
Types of studies
We included randomised controlled trials (RCTs) comparing a psychological intervention with an alternate psychological intervention, management as usual (MAU) or no treatment. Studies comparing alternative doses or formats of the same intervention were also eligible for inclusion. (See Types of interventions for more detail.)
Types of participants
We included studies with participants up to 18 years old who had experienced any form of child sexual abuse (CSA), as described above under Description of the condition.
We excluded studies with participants over the age of 18 years.
Additionally, we excluded trials in which participants who had experienced CSA had experienced physical abuse or other traumatic experiences simultaneously when: 1) separate results for participants experiencing only CSA were not reported; 2) the randomisation was not stratified by the specific type of abuse or traumatic experience; 3) the participants experiencing CSA were less than the 50% of the sample (sample would have been too small to have any statistical power); and 4) individual data were not available.
Network meta‐analysis (NMA) relies on the assumption of transitivity, which refers to a similar distribution of effect modifiers across the comparisons included in the network (Caldwell 2005; Cipriani 2013; Salanti 2012). Although the age group is broad, the age of the participants has not been found to be an effect modifier in treating the consequences of CSA. Thus, with our selection criteria, all the interventions explored in this review are legitimate alternatives for participants and therefore jointly randomisable.
Types of interventions
Interventions of direct interest
We included any psychological intervention, delivered by a trained professional in any setting or any format (individual or group), and at any ‘dose’, designed to alleviate psychological distress amongst children and young people who have experienced CSA. We a priori specified these as ‘experimental’ or ‘control’.
Experimental interventions
Cognitive behavioural therapy (CBT): therapist addressed negative cognitive, emotional and behavioural consequences of sexual abuse; included strategies to support or improve child and family functioning and parenting capacity by addressing parental distress caused by what had happened and how the child was responding.
Psychodynamic therapy (PST): therapist focused on the strengthening of ego defences and the amelioration of specific symptoms or problem areas.
Eye movement desensitisation and reprocessing (EMDR): therapist helped young person to process what had happened to them, identify (surfacing) negative cognitions associated with a traumatic incident and substitute these with a healthy, positive cognition.
Child Centred Therapy (CCT): counsellors sought to facilitate what is believed to be our inherent tendency to develop our potential (termed 'self‐actualisation’).
Family therapy (FT): therapist sought to effect changes in the family that could ameliorate the psychological distress that children experienced following abuse perpetrated either inside or outside the family.
Comparator interventions
An alternate psychological treatment: for example, CBT versus CCT or CBT versus EMDR.
Higher doses of any of the experimental interventions: measured as a greater number of intervention sessions delivered.
MAU: as defined by the trial authors.
Waiting list (WL): participants who were assessed and informed that they would receive the intervention at the end of the waiting list phase.
Types of outcome measures
Primary outcomes
Psychological distress/mental health, including post‐traumatic stress disorder (PTSD; e.g. the Children's PTSD Inventory (Saigh 2000) or the Trauma Symptoms Checklist (Briere 1989)); depression (e.g. the Children's Depression Inventory (Kovacs 1992)); anxiety (e.g. State‐Trait Anxiety Inventory for Children (Spielberger 1973)); and self‐harm (e.g. item nine on the Child Depression Inventory (CDI) (Kovacs 1992)).
Behaviour, including sexualised (e.g. the Child Sexual Behavior Inventory (CSBI) (Friedrich 1992a)), and internalising and externalising behaviours (e.g. the 'Externalising' subscale of the Child Behavior Checklist (CBCL) (Achenbach 1991)).
Social functioning, including attachment (e.g. the Inventory of Parents and Peer Attachment (IPPA) (Armsden 1987)).
Relationships with family and others, cognitive or academic attainment, and quality of life (e.g. the Warwick‐Edinburgh Mental Wellbeing Scale (WEMWBS) (NHS Health Scotland 2006).
Secondary outcomes
Substance misuse (e.g. the Youth Risk Behaviour Survey (Brener 2004)).
Delinquency (e.g. the Youth Risk Behaviour Survey (Brener 2004)).
Resilience (e.g. the Children’s Attributional Style Questionnaire (CASQ) (Thompson 1998)).
Carer distress and efficacy (e.g. the Revised Scale for Caregiving Self‐Efficacy (Steffen 2002)).
Rating scales
A wide range of instruments is available to measure the behavioural and psychological consequences of CSA (Deblinger 1989; DSM‐5; Kendall‐Tackett 1993; Nakamura 2009; Siddons 2004). Due to anticipated heterogeneity in the use of measurement scales across the studies, we did not prespecify a hierarchy for selection of outcomes in advance of data extraction. We included outcome data when/where instruments were reported to be reliable and valid, and either were self‐report, a relative's or assessor's reports. If an outcome was assessed using a measure with subscales, we used the total score, providing the full scale that addressed the outcome of interest. If self‐ and observer‐rated assessments were available, we gave preference to the latter. When more than one measure of the same outcome was reported in a trial, we used the data from the instrument with higher reliability, as reported by the authors of the trial. We anticipated variation in the timing of follow‐ups, so we analysed data in three categories, as per protocol (Caro 2019): short term (one to three months following therapy), medium term (four to six months following therapy), and long term (six to 12 months following therapy).
Search methods for identification of studies
We first ran the searches for this review in April 2019, and updated them in March 2020. A further update was run in November 2022 for all sources apart from AMED, which was unavailable.
Electronic searches
We searched the following databases and trial registers (all years).
Cochrane Central Register of Controlled Trials (CENTRAL; 2022, Issue 10), in the Cochrane Library, which includes the Developmental, Psychosocial and Learning Problems Specialized Register (searched 1 November 2022).
MEDLINE Ovid (1946 to October Week 4 2022).
MEDLINE Ovid In‐Process & Other Non‐Indexed Citations (1946 to 1 November 2022).
MEDLINE Ovid Epub Ahead of Print (1 November 2022).
Embase Ovid (1974 to 1 November 2022).
Allied and Complementary Medicine Database Ovid (AMED; 1985 to 31 March 2020).
PsycINFO Ovid (1806 to October Week 4 2022).
Child Development & Adolescent Studies EBSCOhost (1970 to 2 November 2022).
CINAHL (Cumulative Index to Nursing and Allied Health Literature EBSCOhost; 1937 to 3 November 2022).
Cochrane Database of Systematic Reviews (CDSR, 2022, Issue 11), in the Cochrane Library (searched 1 November 2022).
Conference Proceedings Citation Index ‒ Science Web of Science (CPCI‐S; 1990 to 3 November 2022).
Conference Proceedings Citation Index ‒ Social Science & Humanities Web of Science (CPCI‐SSH; 1990 to 3 November 2022).
SciELO Citation Index Web of Science (2002 to 3 November 2022).
Science Citation Index Web of Science (1970 to 3 November 2022).
Social Sciences Citation Index Web of Science (1970 to 3 November 2022).
ERIC EBSCOhost (Educational Resources Information Center; 1966 to 3 November 2022).
Electronic Theses Online Service, The British Library (EThOS; ethos.bl.uk/Home.do?new=1; 1800 to 4 November 2022).
Health Technology Assessment Database (HTA; current issue; www.crd.york.ac.uk/CRDWeb; searched 4 November 2022).
Epistemonikos (www.epistemonikos.org; searched 4 November 2022).
ClinicalTrials.gov (current issue; clinicaltrials.gov; searched 4 November 2022).
World Health Organization International Clinical Trials Registry Platform (WHO ICTRP; www.who.int/clinical-trials-registry-platform; searched 4 November 2022).
The search strategy for each source can be found in Appendix 1.
Searching other resources
Reference lists
We checked the references of previous reviews, meta‐analyses and included studies to identify missing studies or additional unpublished or ongoing relevant studies.
Personal communication
We contacted the authors of some of the trials to request additional trial data (Dominguez 2001; Monck 1994; Trowell 2002).
Data collection and analysis
In this section, we provide information on all methodological decisions set out in the protocol (Caro 2019) and used in this review. Appendix 2 provides information of the methods set out in our published protocol that were not applied in this, first version of the review.
Selection of studies
Working in pairs, three of the four review authors (WT, PC and GM) independently screened the titles and abstracts of studies retrieved from the searches against the selection criteria (Criteria for considering studies for this review).
We eliminated studies deemed irrelevant by both review authors. We obtained the full text of any title or abstract that one or more review author thought might be potentially eligible and assessed it against the inclusion criteria. We discussed any disagreements with the third review author (GM) and, if agreement was not reached, we sought the information necessary to resolve the issue from the study authors. We record the reasons for excluding studies in the table Characteristics of excluded studies tables.
We present our study selection process (along with the number of records and studies, and reasons for exclusion of records at screening of full‐text reports) in a PRISMA flow diagram.
Data extraction and management
PC and GM independently extracted data and entered them onto a structured, pilot‐tested Excel data collection form, which was based on the data collection form for intervention reviews for RCTs only of the Cochrane Developmental, Psychosocial and Learning Problems Review Group (CDPLP 2014). The form is available here.
Outcome data
From each included study, we extracted relevant details on all primary and secondary outcome measures used, as defined by the review authors, including length of follow‐up and summary data (means, standard deviations (SD), confidence intervals (CI) and significance levels for continuous data, and proportions for dichotomous data).
Data on potential effect modifiers
From each included study, we extracted data on the following characteristics that could have acted as effect modifiers.
Study characteristics (geographical location of study; study design; study duration; details of attrition; risk of bias concerns; service setting (e.g. hospital or community, research facility or community agency); whether the researchers were members of the treatment agency or independent or external; proportion of families referred or approached who agreed to be randomised; and characteristics of the therapists (e.g. discipline, level of qualification or student, years of experience)).
Participant characteristics (number randomised; nature and duration of sexual abuse, including sexual exploitation; age of participants; specific diagnosis; comorbidities; gender distribution; sexual orientation).
Intervention characteristics (intervention components; format and timing of psychological therapy; duration; frequency; concurrent interventions; whether the treatment is manualised, semi‐structured or unstructured treatment; if participants were required to attend a set number of sessions; and if participants were paid).
Comparison characteristics (format, frequency and duration).
Other data
From each included study, we extracted data on the following additional information.
Study author(s), year of publication, citation and contact details.
Sources of funding and other potential commercial interests.
Assessment of risk of bias in included studies
PC and WT judged the risk of bias of each of the included studies in accordance with the guidance provided in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2017) and assigned one of the following three ratings.
High risk of bias (plausible bias that seriously weakens confidence in the results).
Low risk of bias (plausible bias unlikely to seriously alter the results).
Unclear or unknown risk of bias.
We based the risk for bias assessment on the domains outlined in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2017), which are set out in Appendix 3.
Measures of treatment effect
Relative treatment effects
We estimated the pairwise relative treatment effects of the interventions by calculating effect sizes appropriate for the type of outcome data provided. All studies reported continuous outcome data and used different measures to assess the same outcome. We therefore used the standardised mean difference (SMD) with its 95% CI (Higgins 2021a).
If an outcome was assessed using a measure with subscales, we used the total score, providing the full scale that addressed the outcome of interest. In this review, negative SMDs indicated that the treatment condition (or treatment A in the head‐on analyses) was more effective (resulted in greater symptom reduction) than the treatment to which it was compared.
An SMD of 0.2 indicates a small effect, an SMD of 0.5 indicates a moderate effect, and an SMD of 0.8 indicates a large effect (Cohen 1988). We present the 95% CI in brackets for each SMD.
Endpoint versus change data
We used mean final values and not change‐from‐baseline scores for the following reasons.
Change scores do not correct pretest imbalances (Fu 2016).
Change scores can be calculated by subtracting the baseline score from the endpoint score, but standard deviations cannot be calculated this way. These would need to be imputed or approximated. When the studies’ original data are transformed, the change scores across participants are reordered and there is no way to guarantee that the transformation applies to the change score (Clifton 2019; Higgins 2021a).
SMDs from change scores are more likely to show significant results, whilst those from endpoints produce more conservative results (Fu 2016).
Most of the time, baseline and endpoints are reported for different number of participants because of withdrawals or attrition. With change scores, reviewers cannot specify the number of participants reporting baseline and endpoint scores (Higgins 2021a).
Endpoint data typically have no negative effects. This can make it easier for clinicians to interpret (Higgins 2021a).
Standard deviations from endpoint data are usually more readily reported by the authors in the studies, which facilitates the creation of a consistent dataset (Higgins 2021a).
Only one of the included studies reported change‐from‐baseline scores (Trowell 2002). We decided not to include this study in the numerical analyses for the following reasons.
Change and postintervention data cannot be combined in an SMD meta‐analysis/network meta‐analysis. Standard deviations of each data reflect different things. Postintervention scores' SDs reflect between‐person variability at a single point in time; whereas change scores' SDs reflect variation in between‐person changes over time.
To include Trowell 2002, we would have had to transform the endpoints of all the other studies to change scores. We decided not to do so. First, there was no methodological justification to transform the original data, as all the endpoints reported by the other studies were estimated using the pretest outcome measure as a covariate in the regression models (ANCOVA; analysis of covariance), which has been argued to be the preferred statistical approach to account for potential baseline imbalances and to reach precise and least biased interventions' effect estimates (Higgins 2021a). Second, switching from endpoints to changes from baselines because of an observed baseline imbalance across the studies introduces bias rather than removes it (Vickers 2001). And third, utilising change scores does not correct baseline imbalances.
Relative treatment ranking
We estimated the probability that each treatment is the first, second, third, etc. most effective in the network with the surface under the cumulative ranking curve (SUCRA) and mean ranks (Chaimani 2013). However, due to the uncertainty of the effect estimates and the low number of studies informing some of the comparisons, we determined that reporting the rankings could be misleading. We have reported this amendment in the Differences between protocol and review section of the review.
Unit of analysis issues
We did not find cluster‐randomised trials or cross‐over trials. Our plans for managing these if found in future updates of the review are set out in our published protocol and in Appendix 2.
Studies with multiple treatment groups
For both pairwise comparisons and network meta‐analyses, when a study involved more than two treatment arms, we did not combine them. Rather, we kept the arms separate to investigate heterogeneity across intervention arms (e.g. the difference between delivering CBT to the child only, to the non‐offending carer only, or to the child and the non‐offending carer together). For pairwise comparisons and continuous outcomes, we divided the number of participants of the control group evenly between the number of experimental groups to avoid double counting the participants, and used the original means and standard deviations. This was not necessary in the NMA, as it accounted for the correlation between comparisons from the same study and data could be entered from each arm as originally randomised in the study (Higgins 2021a).
Dealing with missing data
We did not exclude studies due to missing data. We tried to contact the study authors for all relevant missing data. The authors contacted and the results of these exchanges are detailed in the section Description of studies. When we could not reach the authors, or the data were not available even after making contact, we dealt with missing data as follows, and as recommended by the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2021a).
Continuous data
We did not collect individual participant data (Appendix 2).
Missing statistics
Where studies had missing summary data, such as missing standard deviations, we obtained them from the standard error of the mean by multiplying by the square root of the sample size. If the standard error was not available, we used the CI. For samples larger than 100 participants we obtained the standard deviation by dividing the length of the CI by 3.92 (CI = 95%); 3.29 (CI = 90%); and 5.15 (CI = 99%) and then multiplying this value by the square root of the sample size. Where sample sizes were smaller than 60, we changed the numbers 3.92, 3.29 and 5.15 to larger numbers specific to the t distribution. These were obtained from tables of the t distribution with degrees of freedom equal to the group sample size minus 1 (Higgins 2021a).
Assessment of reporting biases
We were unable to perform comparison‐adjusted or conventional funnel plots due to the nature and number of the included studies (See Differences between protocol and review). For conclusions from these graphs to be meaningful, all comparisons across studies must be defined in a consistent direction (active versus inactive interventions, newer versus older treatment, or sponsored versus non sponsored treatment). To draw valid conclusions, 10 or more studies are recommended (Higgins 2021a, Chapter 13, section 13.3.5.4 Tests for funnel plot asymmetry), and in no case did we have a sufficient number of studies.
Data synthesis
Methods for direct treatment comparisons
As anticipated in our protocol (Caro 2019), there was considerable clinical heterogeneity between included studies. Therefore, studies making direct (head‐to‐head ) comparisons were synthesised using a random‐effects meta‐analysis in RevMan (Review Manager 2020; Higgins 2021a). See additional details in the section 'Assessment of statistical heterogeneity' below.
For ease of comparison with the NMA results, results for direct treatment comparisons are reported in ‘triangle tables’ (Dias 2019). However, results are also summarised in forest plots, including those comparisons reported only in single studies. The forest plots contain: 1) summary data for each intervention group (number of participants, means and standard deviations); 2) effects estimates (SMDs) and CI; and 3) risk of bias of each included study. All forest plots can be found in the Data and analyses section at the end of the review.
Methods for indirect and mixed comparisons
An NMA allows us to estimate the relative effectiveness of all interventions simultaneously, by combining direct and indirect evidence in one meta‐analysis. For example: an indirect estimate of the effect of the intervention B relative to the intervention A can be derived via the common comparator C, by combining the summary effects from A versus C and B versus C. An NMA is possible for any connected network of treatment comparisons, and network plots are used to display the number of treatments and comparisons contributing to an analysis (see Results).
We conducted a random‐effects NMA, implemented using the network macro in Stata (Stata 2013; White 2015). The reference treatment for analysis was MAU; however, for networks where this was not possible, we selected waiting list. An NMA allows comparisons to be made between all interventions included in the analysis, regardless of whether they have been compared in direct, head‐to‐head trials. If all eligible interventions defined in this review were included in an NMA, this would result in 91 pairwise comparisons (See 'Definitions of Nodes of the Network' under Included studies). As such, to aid readability, we report only the relative effects of each intervention compared to the reference treatment from the NMA. However, the full set of results for each outcome and time point are reported in this repository.
Methods for assessing heterogeneity within comparisons and inconsistency across comparisons are described in the sections below on 'Assessment of statistical heterogeneity', 'Assessment of transitivity across treatment comparisons' and 'Assessment of statistical inconsistency'.
Where appropriate, NMA also allows us to rank the probability that each treatment is the first, second, third, etc. most effective in a network for each outcome (Caldwell 2005; Higgins 2021a). However, as described above in 'Relative treatment ranking' under Measures of treatment effect, we made a retrospective decision not to report treatment rankings in this review, as we considered them potentially misleading given the extent of uncertainty in the evidence base (Salanti 2022).
For networks with five or more studies, we examined the certainty of the evidence using the Confidence in Network Meta‐analysis online tool (CINeMA) (CINeMA 2017; Salanti 2014. CINeMA is based on the approach developed by the GRADE Working Group and allows judgements of high, moderate, low or very low confidence in the evidence to be made by assessing the level of concerns in each of the following GRADE domains (Brignardello‐Petersen 2018).
Within‐study bias: refers to unclear or high risk of bias of the included studies.
Reporting bias: refers to an incomplete or inappropriate inclusion of eligible studies.
Indirectness: refers to the relevance of the included studies to the research question.
Imprecision: based on the width of the CI of the estimates. The wider the CI, the more imprecise the estimate.
Heterogeneity: variability in the results of the studies contributing to the analyses.
Incoherence: refers to the verification of the transitivity and consistency assumptions.
We rated concerns in the evidence base as being major, some, no concerns, or undetected concerns.
The CINeMA tool cannot be used for networks informed by fewer than five studies (Nikolakopoulou 2020).
Assessment of statistical heterogeneity
Assumptions when estimating heterogeneity
We assumed a single estimate for heterogeneity variance across different comparisons for both pairwise comparisons and the NMA in order to: (1) allow that comparisons explored only in one or two trials could borrow information about heterogeneity from comparisons explored in three or more trials; and (2) obtain more precise estimates, as estimates of heterogeneity are more precise when more data contribute to the estimate.
Measures and tests for heterogeneity
We assessed the presence of heterogeneity using the following tests and measures (Higgins 2021a).
CI of the estimated effects: poor overlap between these indicated statistical heterogeneity.
Chi2 statistic: P values < 0.10 indicated statistical heterogeneity.
-
I2 statistic: described the percentage of total variation across studies caused by heterogeneity rather than chance. Interpretation was guided by the following thresholds:
0% to 40%: not important;
30% to 60%: moderate heterogeneity;
50% to 90%: substantial heterogeneity; or
75% to 100%: considerable heterogeneity.
Tau2, an estimate of between‐studies variance.
Assessment of reporting biases
We examined the funnel plots for both direct and indirect comparisons for which at least 10 studies were available.
Assessment of transitivity across treatment comparisons
A valid NMA requires an assumption of transitivity to hold across the network. To assess transitivity, we evaluated the distribution of effect modifiers across the comparisons included in the network (Caldwell 2005; Cipriani 2013; Salanti 2012). We created a table with the characteristics of the included studies, checked the distribution of effect modifiers and assessed the studies to be similar across characteristics that may modify the treatment effect (see Table 4 in the repository, available here).
Assessment of statistical inconsistency
The statistical manifestation of a lack of transitivity is inconsistency. We assessed inconsistency using both local and global approaches.
We used a loop‐specific approach to evaluate inconsistency separately for each quadratic or triangular closed loop of the network (Bucher 1997), by calculating the magnitude of the difference between direct and indirect estimates (inconsistency factors) and their 95% CI (allowing the same variance for all comparisons in a loop). When the lower limits of the CI of the inconsistency factors reach zero, this suggests no evidence for inconsistency (Chaimani 2013). Where possible, we reported the number of inconsistent loops in the network, and results of the tests for inconsistency are presented in inconsistency plots. For a global assessment of inconsistency across the entire network, we used a design × treatment model, based on the Chi2 test. We performed this assessment using the network suite and mvmeta command in STATA (Higgins 2012).
We did not assess the global and local inconsistency of networks formed by two‐armed trials only, or where closed loops were formed by comparisons made within the same multi‐armed trial. Global inconsistency is unlikely in networks consisting of only two‐arm trials and local inconsistency is considered to arise when there are at least three separate sets of studies making different comparisons (closed loops) (Higgins 2012; Veroniki 2013).
Local approaches for evaluating inconsistency
We inferred the presence of inconsistency in each loop of the network by calculating the magnitude of the difference between direct and indirect estimates (inconsistency factors) and their 95% CI. The results of these analyses are presented in a forest plot using the command ifplot in STATA (Chaimani 2015; Veroniki 2013).
Global approaches for evaluating inconsistency
We checked the assumption of consistency of the entire network through the design × treatment model based on the Chi2 test. We performed this analysis through the command mvmeta in STATA, fitting the inconsistency model of NMA (Higgins 2012).
Subgroup analysis and investigation of heterogeneity
We planned to perform subgroup and meta‐regression analyses with the following explanatory variables: children’s age, gender, and intensity of treatment (a combination of frequency × length). However, we could not do so, due to the low number of studies per outcome to form the subgroups (Higgins 2021a).
Sensitivity analysis
We could not perform our preplanned sensitivity analyses due to the low number of studies. See Appendix 2 for details of what we will do if this situation changes in the future.
Summary of findings and assessment of the certainty of the evidence
We included tables reporting the characteristics, risk of bias and treatment effect sizes of the included studies.
We created summary of findings tables at post‐treatment for indirect evidence for the following outcomes.
Psychological distress/mental health, including post‐traumatic stress disorder (PTSD; e.g. the Children's PTSD Inventory (Saigh 2000) or the Trauma Symptoms Checklist (Briere 1989)); depression (e.g. the Children's Depression Inventory (Kovacs 1992)); anxiety (e.g. State‐Trait Anxiety Inventory for Children (Spielberger 1973)); and self‐harm (e.g. item nine on the Child Depression Inventory (CDI) (Kovacs 1992)).
Behaviour, including sexualised (e.g. the Child Sexual Behavior Inventory (CSBI) (Friedrich 1992a)), and internalising and externalising behaviours (e.g. the 'Externalising' subscale of the Child Behavior Checklist (CBCL) (Achenbach 1991)).
Social functioning, including attachment (e.g. the Inventory of Parents and Peer Attachment (IPPA) (Armsden 1987)).
We were not able to perform network meta‐analyses for all outcomes at six or 12 months follow‐up.
Finally, we used the CINeMA tool to examine the certainty of the evidence (CINeMA 2017; Salanti 2009; Salanti 2014). We made judgements of high, moderate, low or very low confidence in the evidence by assessing the level of concerns (major concerns, some concerns, no concerns, or undetected) in each of the following dimensions:
within‐study bias (limitations at study level that may lead to biased estimates);
reporting bias;
indirectness (relevance of the included studies to the research question);
imprecision;
heterogeneity; and
incoherence (transitivity/inconsistency) (Brignardello‐Petersen 2018).
Results
Description of studies
Results of the search
We retrieved a total of 7205 records. Of these, 5721 remained after deduplication. We excluded 5580 records after assessing their titles and abstracts. We retrieved 141 papers for full text inspection. Of these, we:
classified two as ongoing studies (see Ongoing studies);
categorised one as awaiting classification (from latest search; see Studies awaiting classification);
excluded 100 ineligible full‐text reports (see Excluded studies); and
included 22 studies from 38 reports (see Included studies section).
The PRISMA flow diagram depicts the study selection process Figure 1.
1.
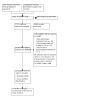
Study flow diagram
Included studies
Details of the 22 included studies are summarised below and in the Characteristics of included studies tables.
We found high variability across studies in terms of the ages of the participants and the format of the therapy (individual or group), but uniformity in terms of the settings in which therapies were delivered, the manualisation of therapies, the gender and ethnicity of the participants, the experience of therapists, length of the sessions, number of sessions and frequency of the sessions.
Study design
All evaluations of the interventions were conducted by the research teams that developed and monitored the delivery of the treatments.
We did not find any cluster‐randomised trials, cross‐over trials, or repeated measurements trials. There were:
two four‐armed trials (Deblinger 1996bDeblinger 2011);
two three‐armed trials (King 2000Perez 1987); and
18 two‐armed trials (Baker 1985; Berliner 1996; Burke 1988; Celano 1996; Cohen 1996; Cohen 1998; Cohen 2004; Costas 1999; Danielson 2012; Deblinger 2001; Dominguez 2001; Farkas 2008; Foa 2013; Jaberghaderi 2004; Monck 1994; O'Callaghan 2013; Thun 2003; Trowell 2002).
Location and setting
Of the 22 studies:
one study was conducted in Canada (Farkas 2008);
two studies were conducted in the UK (Monck 1994; Trowell 2002);
one study was conducted in Iran (Jaberghaderi 2004);
one study was conducted in the Democratic Republic of Congo (O'Callaghan 2013);
one was conducted in Australia (King 2000); and
16 studies were conducted in the USA.
All but one study was conducted in a clinical setting; O'Callaghan 2013 was conducted in a school setting.
Sample size
The smallest sample comprised 11 participants (Jaberghaderi 2004) and the largest sample comprised 229 participants (Cohen 2004). Thirteen studies had fewer than 48 participants, six fewer than 83 participants and three studies had more than 100 participants.
Participants
Age
The age range of participants varied widely across the studies, making it difficult to group them. The following table (Table 1) summarises the age range of participants per study.
Table 1 Summary of the age range of participants per study
| Study | Age range in years | Study | Age range in years | Study | Age range in years |
| Baker 1985 | 13 to 17 | Costas 1999 | 4 to 10 | King 2000 | 5 to 17 |
| Berliner 1996 | 4 to 13 | Danielson 2012; Farkas 2008 | 13 to 17 | Monck 1994 | 4 to 16 |
| Burke 1988; Celano 1996 | 8 to 13 | Deblinger 1996b | 7 to 13 | O'Callaghan 2013 | 12 to 17 |
| Cohen 1996 | 2 to 7 | Deblinger 2001 | 2 to 8 | Perez 1987 | 4 to 9 |
| Cohen 2004 | 8 to 14 | Deblinger 2011 | 4 to 11 | Thun 2003 | 16 to 18 |
| Cohen 1998 | 8 to 15 | Foa 2013 | Mean age 15 | Trowell 2002 | 6 to 14 |
| Dominguez 2001 | 6 to 17 | Jaberghaderi 2004 | 12 to 13 |
Gender
The percentage of female participants was:
56% in Cohen 1996;
61% and 62% in Deblinger 2001 and Deblinger 2011, respectively;
64% in Perez 1987;
68% in Costas 1999;
69% in Cohen 1998 and King 2000;
73% in Farkas 2008;
76% in Dominguez 2001;
79% in Cohen 2004;
83% in Deblinger 1996b;
86% in Monck 1994;
88% in Danielson 2012; and
89% in Berliner 1996.
In the remaining eight studies, it was 100% (Baker 1985; Burke 1988; Celano 1996; Foa 2013; Jaberghaderi 2004; O'Callaghan 2013; Thun 2003; Trowell 2002).
Ethnicity
In Celano 1996 more than 50% of the participants were African‐American.
In Danielson 2012 46% of the participants were African American, 37.5% white, 4.2% Native American, 8.3% bi‐racial, 4% Hispanic; and in Dominguez 2001, 8% of the participants were African‐American, 40% were Hispanic, 48% were Caucasian, and 4% were described as "other".
Nine studies described more than 50% of participants as Caucasian (Baker 1985; Berliner 1996; Cohen 1996; Cohen 1998; Cohen 2004; Deblinger 1996b; Deblinger 2001; Deblinger 2011; Foa 2013).
Seven studies did not report the ethnicity of the participants (Jaberghaderi 2004; King 2000; Monck 1994; O'Callaghan 2013; Perez 1987; Thun 2003; Trowell 2002).
Socioeconomic background
Few studies reported on the sociodemographic background of the participants. Those that did described them as follows: "primarily low income" (Celano 1996); "Mean SES was Hollingshead IV" (Cohen 1996); "Family Income: < USD 25,000 per year (52%) and > USD 25,000 per year (48%)" (Cohen 2004); and "SES mean socioeconomic rating: 6.08" (King 2000). Jaberghaderi 2004 said "All participants were in the same socio‐economic status".
Definition of child sexual abuse
Three studies defined sexual abuse as follows: "sexual touching by anyone at least five years older than the child or by a perpetrator of any age if the victim felt coerced" (Celano 1996; Cohen 1996) and "inappropriate sexual touch" (O'Callaghan 2013).
The remaining 19 studies simply reported that the abuse must have been confirmed by third parties (e.g. Child Protective Services (CPS), law enforcement or professional independent forensic evaluators). The type of sexual abuse experienced by the participants and the characteristics of the perpetrators are summarised in the Characteristics of included studies tables.
Nature of the abuse
Where reported, the sexual abuse experienced by children and young people included: digital penetration, physical injuries, vaginal or anal intercourse, oral sex, and fondling.
Perpetrators of the abuse
The abusers were mainly male parents, step‐parents, other adult relatives or strangers, or older peers.
Criteria to exclude participants
Children were excluded from studies for the following reasons: intellectual disability (often termed 'mental retardation' by the study authors), developmental disorders (e.g. autism), drug misuse of carers, psychotic symptoms and suicidal behaviour. See Characteristics of included studies tables for a summary of the inclusion and exclusion criteria used in each study.
Interventions
We included psychological interventions delivered to a child or young person by, or through, a parent or other carer if the intervention was concerned with addressing the consequences of sexual abuse for the child.
We found two types of interventions that we did not prespecify in the protocol: non‐directive supportive therapy (explored in Cohen 1996; Cohen 1998; Cohen 2004; Deblinger 2001; Dominguez 2001), and play therapy (explored in Costas 1999 and Perez 1987). The trials of supportive therapy and play therapy mentioned the following key ingredients: active listening, unconditional positive regard, reflecting feelings, and empathy. Therefore, we classified these interventions as child centred therapy.
Two studies assessed family therapy (Danielson 2012; Monck 1994); two assessed eye movement desensitisation and reprocessing (Farkas 2008; Jaberghaderi 2004) and two studies assessed psychodynamic therapy (Thun 2003; Trowell 2002).
Fourteen studies explored cognitive behavioural therapy (Berliner 1996; Burke 1988; Celano 1996; Cohen 1996; Cohen 1998; Cohen 2004; Deblinger 1996b; Deblinger 2001; Deblinger 2011; Dominguez 2001; Foa 2013; Jaberghaderi 2004; King 2000; Deblinger 2011); and eight assessed child centred therapy (Baker 1985; Cohen 1996; Cohen 1998; Cohen 2004; Deblinger 2001; Dominguez 2001; Costas 1999; Perez 1987).
Three studies used management as usual (MAU) as the comparator (Berliner 1996; Celano 1996; Danielson 2012), and five used waiting list controls (Costas 1999; Farkas 2008; King 2000; O'Callaghan 2013; Perez 1987). Management as usual was described as the standard care that a CSA victim and family would typically receive when presenting for treatment in the clinic.
Seventeen studies administered interventions to individuals, and 10 studies used a group format. In five studies, the arms compared were the intervention in individual format versus the same intervention in group format, with one arm of treatment delivering more sessions (higher dose) than the other one (Baker 1985; Deblinger 2011; Monck 1994; Perez 1987; Trowell 2002).
All interventions were manualised and were delivered by a range of clinicians trained in the interventions and with previous experience in the treatment of child sexually abuse:
social workers (Berliner 1996; O'Callaghan 2013);
psychologists (Burke 1988; Cohen 1998; Danielson 2012; Dominguez 2001; Jaberghaderi 2004; King 2000);
no more details beyond therapists or counsellors (Baker 1985; Cohen 1996; Deblinger 1996b; Deblinger 2011; Foa 2013; Perez 1987; Thun 2003; Trowell 2002); and
a mix of the above (Celano 1996; Cohen 2004; Deblinger 2001; Farkas 2008).
Some studies did not specify the training or discipline of those delivering the intervention (Costas 1999; Monck 1994).
Number of sessions, frequency, duration and dose
Twenty studies reported the number of sessions, 18 reported the length of sessions, and 19 reported the duration of the intervention. The number of sessions ranged from six to 30. Almost every study administered sessions weekly, and the length of session ranged from 45 to 120 minutes.
Deblinger 2011 compared four variants of CBT. In two arms, CBT was delivered in eight weeks, in one arm with the inclusion of a 'trauma narrative' and in one arm without. In the remaining two arms, CBT was delivered in 16 weeks, again in one arm with a trauma narrative and in one arm without. We classified the two arms that received CBT over 16 weeks as a higher dose of CBT.
Trowell 2002 compared two arms of psychodynamic therapy: one delivered in 18 weeks and the other in 30 weeks. We classified the latter as a higher dose of psychodynamic therapy.
Monck 1994 compared two arms of family therapy: one delivered in four to six weeks and the other one delivered in up to 20 weeks. We classified the second as a higher dose of family therapy.
Finally, Baker 1985 compared two arms of child centred therapy: one delivered in six weeks and the other one in 10 weeks. We classified the latter as CCT higher dose.
Recipients of therapy
Ten studies delivered one of the arms of treatment only to the child (Baker 1985; Burke 1988; Dominguez 2001; Foa 2013; Jaberghaderi 2004; King 2000; O'Callaghan 2013; Perez 1987; Thun 2003; Trowell 2002).
Twelve studies administered one of the arms of treatment to both, the child and his or her carer (Berliner 1996; Celano 1996; Cohen 1996; Cohen 1998; Cohen 2004; Costas 1999; Danielson 2012; Deblinger 1996b; Deblinger 2001; Deblinger 2011; Farkas 2008; King 2000).
Monck 1994 delivered the intervention to the family.
Definition of the nodes of the networks
Thirteen studies compared an active psychological intervention against another active psychological intervention, and nine studies compared against MAU or a no intervention‐WL. There were three two‐armed studies comparing different doses of the same interventions (Baker 1985; Monck 1994; Trowell 2002) and there were three multi‐armed studies (Deblinger 1996b; Deblinger 2011; King 2000) comparing different modalities of CBT (i) delivered to the child only, ii) to the non‐offending carer only, iii) to the child and the non‐offending carer together, and iv) a higher dose of CBT delivered to the child and the non‐offending carer).
We analysed studies comparing different doses as separated nodes in the pairwise comparisons and in the NMA.
To incorporate multi‐armed studies in the networks, we created specific nodes for each arm and differentiated the other treatments of the networks accordingly, where applicable. Appendix 4 describes, in detail, the multi‐armed studies.
The nodes of the networks correspond to the theoretical orientation of the therapies and specify whether the treatment was delivered only to the child, only to the non‐offending carer, or to the child and carer. For inclusion in our analyses we specified the following 14 interventions.
Cognitive behavioural therapy delivered only to the child (CBT child; Burke 1988; Deblinger 1996b; Dominguez 2001; Foa 2013; King 2000; O'Callaghan 2013; Jaberghaderi 2004).
Cognitive behavioural therapy delivered only to the carer (CBT carer; Deblinger 1996b).
Cognitive behavioural therapy delivered to the child and the carer (CBT dyad; Berliner 1996; Celano 1996; Cohen 1996; Cohen 1998; Cohen 2004; Deblinger 1996b; Deblinger 2001; Deblinger 2011; King 2000).
Cognitive behavioural therapy delivered to the child and the carer at a higher dose (CBT dyad higher; Deblinger 2011).
Psychodynamic therapy delivered only to the child (PD child; Trowell 2002).
Psychodynamic therapy delivered only to the child at a higher dose (PD child higher; Trowell 2002).
Eye movement desensitisation and reprocessing (EMDR; Farkas 2008; Jaberghaderi 2004).
Child centred therapy delivered only to the child (CCT child; Baker 1985).
Child centred therapy delivered only to the child at a higher dose (CCT child higher; Baker 1985).
Child centred therapy delivered to the child and the carer (CCT dyad; Costas 1999).
Family therapy (FT; Danielson 2012Monck 1994).
Family therapy at a higher dose (FT higher; Monck 1994).
Management as usual (MAU; Berliner 1996; Celano 1996; Danielson 2012; Deblinger 1996b).
Waiting list (WL; Costas 1999; Farkas 2008; King 2000).
Outcomes
Of the 22 included studies, there were five that we could not include in the numerical analyses for the following reasons.
Dominguez 2001: data could not be derived or imputed, and we could not contact the author.
Monck 1994: data could not be derived or imputed, and although we were able to contact the authors, they were unable to provide the information requested.
Perez 1987 and Thun 2003 reported on outcomes that were not the focus of this review; Perez 1987 reported on self‐concept and locus of control and Thun 2003 reported on self‐esteem and self‐image.
Trowell 2002: we could not obtain endpoint scores at post‐treatment and one‐year follow‐up from the authors.
The outcomes that were the focus of this review were not assessed in all included studies and were measured in a variety of ways. In Appendix 5, we list the studies from which we extracted data and, as the same outcome was measured with different instruments, we specify the instrument used to obtain the data. We chose the instruments with higher reliability where reported by the authors of each study. In the absence of this information, we planned either to choose the instrument whose validity was already reported in the other trials, or to examine the literature on the validity of the instruments and choose accordingly.
Seventeen of the 22 included studies contributed to the numerical analyses (Baker 1985; Berliner 1996; Burke 1988; Celano 1996; Cohen 1996; Cohen 1998; Cohen 2004; Costas 1999; Danielson 2012; Deblinger 1996b; Deblinger 2001; Deblinger 2011; Farkas 2008; Foa 2013; Jaberghaderi 2004; King 2000; O'Callaghan 2013).
Missing data
Burke 1988 neither reported the standard deviations of the groups nor provided enough data to derive them. We could not reach the author by email, so we imputed the standard deviations from a previous meta‐analysis following the imputation method of Furukawa 2006.
Dominguez 2001 did not report the mean of the groups or enough data to derive them. We could not impute the data nor reach the author by email. Therefore, this study is included in the review but does not contribute to the numerical analyses.
Monck 1994 did not report enough data to derive means and standard deviations. We contacted the primary author, but she did not provide us with further details and we could not impute the data. Therefore, this study is included in the review, but it is not included in the numerical analyses.
Trowell 2002 is also included in the review but not in the numerical analyses because we could not obtain the means and standard deviations for the groups at post‐treatment and at one year follow‐up from the authors.
Finally, as indicated above, two studies reported on outcomes that we did not state in our protocol: Perez 1987 and Thun 2003. These studies are included in this review, but they do not contribute to the numerical analyses.
Excluded studies
We excluded 100 ineligible full‐text reports for the following reasons: 66 were not RCTs, 32 did not study sexually abused children and two did not use a psychosocial intervention. Of these 100, we selected 36 and reported them in more detail in the Characteristics of excluded studies tables: 32 of these were excluded because they were not RCTs and four were excluded because the participants were not victims of CSA.
Studies awaiting classification
Danielson 2016 is a two‐arm study comparing risk reduction family therapy with management as usual.
Ongoing studies
Of the 141 full‐text records inspected, we classified two as ongoing studies (Amirzadegan 2018; NCT00073684). Amirzadegan 2018 is a two‐arm study comparing play therapy versus narrative therapy. The remaining study is registered as a clinical trial (NCT00073684). We emailed the authors of both studies for more details on the studies’ current status and the interventions being compared; however, we did not receive responses. See Characteristics of ongoing studies tables for more details.
Risk of bias in included studies
The following section and the risk of bias tables under Characteristics of included studies contain details and reasons for our judgements. Figure 2 and Figure 3 depict a graphical representation of these judgements.
2.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies
3.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study
Allocation
Random sequence generation
We rated three studies at high risk of bias because random sequence generation was not mentioned and was unlikely to have been done (Burke 1988; Costas 1999; Monck 1994).
We rated 11 studies at unclear risk of bias because the authors stated that the participants were randomly allocated, but they did not mention how (Celano 1996; Cohen 2004; Deblinger 1996b; Deblinger 2011; Dominguez 2001; Farkas 2008; Foa 2013; Jaberghaderi 2004; King 2000; Thun 2003; Trowell 2002).
We rated eight studies at low risk of bias because the authors randomised participants using procedures such as computer programmes, random number tables and coin toss (Baker 1985; Berliner 1996; Cohen 1996; Cohen 1998; Danielson 2012; Deblinger 2001; O'Callaghan 2013; Perez 1987).
Allocation concealment
We rated five studies at high risk of bias because concealment of the allocation was not mentioned and seemed unlikely to have been done (Burke 1988; Costas 1999; Danielson 2012; Dominguez 2001; Perez 1987).
We rated 12 studies at unclear risk of bias because the authors did not report information on concealment to make a judgement (Celano 1996; Cohen 1996; Cohen 1998; Cohen 2004; Deblinger 1996b; Deblinger 2001; Deblinger 2011; Farkas 2008; Jaberghaderi 2004; King 2000; Thun 2003; Trowell 2002).
We rated five studies at low risk of bias because the authors specified procedures to conceal allocation to the treatments (Baker 1985; Berliner 1996; Foa 2013; Monck 1994; O'Callaghan 2013).
Blinding
Blinding of participants and personnel
We rated all 22 studies at high risk of performance bias because the blinding of the personnel and the participants was not mentioned and was unlikely to have been done given the intervention.
Blinding of outcome assessment
We rated 19 studies at high risk of detection bias because all the outcomes were children's and parents' self‐reports.
We rated three studies at low risk of detection bias because the outcomes were assessed by "a clinician not involved in the child’s treatment. Additionally, a psychiatrist or psychologist blind to treatment condition rated the child’s overall psychosocial functioning based on child and caretaker interviews” (Celano 1996); "two psychologists, blind to assignment" (Foa 2013, p 2651); and by "two psychologists blind to assignment" (Jaberghaderi 2004, p 362).
Incomplete outcome data
We rated seven studies at high risk of attrition bias due to three weaknesses (Berliner 1996; Cohen 1996; Costas 1999; Farkas 2008; Jaberghaderi 2004; King 2000; Thun 2003). First, attrition was high in some studies and the implications of this on the results were not discussed. Second, although authors sometimes reported non‐significant differences between completers and non‐completers, they did not report whether or not they performed tests with enough statistical power to detect differences. Finally, studies did not report data that would have allowed for the computation of effect sizes for participants who remained in treatment and those who did not remain.
We rated six studies at unclear risk of bias because attrition or dropouts from treatment were not mentioned and there was not enough information to make a judgement (Baker 1985; Celano 1996; Deblinger 1996b; Deblinger 2001; Dominguez 2001; Monck 1994).
We rated nine studies at low risk of attrition bias because they ran intention‐to‐treat analyses or described how they handled the implications of incomplete data on the results (Burke 1988; Cohen 1998; Cohen 2004; Danielson 2012; Deblinger 2011; Foa 2013; O'Callaghan 2013; Perez 1987; Trowell 2002).
Selective reporting
We rated 17 studies at unclear risk of reporting bias because all the outcomes measured were reported, but there was no reference to a protocol.
We rated two studies at high risk of reporting bias (Cohen 1998; Deblinger 2011). Cohen 1998 did not report one measure from their report of initial outcomes, but did report outcomes for all time points at one‐year follow‐up, and Deblinger 2011 only reported the results of analysis of covariance if data sets were complete.
We rated three studies at low risk of reporting bias because all the outcomes measured were reported and there was a reference to a protocol or a registration of the trial (Cohen 2004; Foa 2013; O'Callaghan 2013).
We were unable to assess reporting bias with funnel plots due to nature and low number of studies. At least 10 studies are needed to conduct comparison‐adjusted or conventional funnel plot for the test to detect reporting biases and the results to be meaningful (Higgins 2021a, Chapter 13, section 13.3.5.4 Tests for funnel plot asymmetry).
Other potential sources of bias
We rated all the studies as at low risk of other potential sources of bias.
Effects of interventions
See: Table 1; Table 2; Table 3; Table 4; Table 5; Table 6
In the networks presented below, each node represents an experimental or control condition; comparisons explored in the included trials are represented by lines connecting the nodes. Ideally, the network of this review should consist of 14 nodes, each connected with all the others, meaning that all the listed interventions and each possible comparison among them has been directly compared in at least one trial.
We report NMA and pairwise results by outcome and by time point. The reference treatment for each analysis is specified, as are the number of treatments and head‐to‐head comparisons contributing to each network analysis. However, for readability, network plots are reported for the postintervention time point only.
Where NMA was not possible, only pairwise results are reported. Where pairwise meta‐analyses could be performed, we used a random‐effects meta‐analysis, except where only a single study was available to estimate a comparison, when we report the fixed effect. Results based on a single study are denoted using a. In such cases, I2 is not applicable and this is also indicated by 'na'.
Appendix 6 lists the outcomes and reasons for which we could not perform NMA, global and local inconsistency tests, assess risk of publication with funnel plots or use the CINeMA approach to judge the degree of confidence in the direct and indirect estimates.
The results of the statistical analyses are summarised in this section and interpreted in the Discussion section. Figures that are not incorporated here are available in this repository.
Primary outcomes
In reporting the results of our analyses, we present a 'triangle table' for each outcome at post‐treatment and, where possible, at six and 12 months follow‐up.
The upper diagonal triangle in each table displays the mean differences (MD) for the column intervention versus the row intervention from the NMA. Values < 0 favour the column defining the intervention.
The lower diagonal triangle in each table displays the results from the direct pairwise comparisons and is read as differences for the row intervention versus the column intervention. Values < 0 favour the row defining the intervention.
For Tables 1 to 13 this applies to the lower triangle only. In the triangle tables, 'na' means that there were no studies making a comparison, CI refers to confidence interval, and NMA refers to network meta‐analysis.
Psychological distress: post‐traumatic stress disorder
Post‐treatment
Figure 4 (a) provides the graphical representation of this network. Direct evidence was available for 13 comparisons coming from 11 studies. All NMA results are reported relative to MAU and the number of direct studies given in brackets. Where the number of direct studies is zero, the estimate is based on indirect evidence from the NMA. The full set of pairwise and network meta‐analyses is summarised in Table 2 below.
4.
Network meta‐analysis for post‐traumatic stress disorder and depression at post‐treatment, 6 months follow‐up and 12 months follow‐up
Abbreviations CBT carer: cognitive behavioural therapy delivered to the carer; CBT child: cognitive behavioural therapy delivered to the child; CBT dyad: cognitive behavioural therapy delivered to the carer and the child; CBT dyad higher: cognitive behavioural therapy delivered to the carer and the child at a higher dose; CCT child: child centred therapy delivered to the child; CCT child higher: child centred therapy delivered to the child at a higher dose; CCT dyad: child centred therapy delivered to the carer and the child; EMDR: eye movement desensitization and reprocessing; FT: family therapy; MAU: management as usual; WL: waiting list.
Table 2 Pairwise and network meta‐analyses results (SMD and 95% CI) for PTSD at post‐treatment
| MAU | WL | FT | EMDR | CCT dyad | CCT child | CBT dyad | CBT child | CBT carer | |
| MAU | ‐ | ‐0.15 (‐1.85 to 1.55) | ‐0.58 (‐1.41 to 0.26) | ‐0.48 (‐1.44 to 0.49) | ‐0.87 (‐1.64 to ‐0.10) | 0.66 (‐0.42 to 1.75) | ‐0.35 (‐1.55 to 0.85) | ‐0.96 (‐1.72 to ‐0.20) | ‐0.46 (‐1.22 to 0.29) |
| WL | na | ‐ | ‐0.31 (‐1.78 to 1.16) | ‐1.08 (‐2.56 to 0.39) | ‐0.52 (‐1.77 to 0.73) | ‐0.42 (‐1.57 to 0.73) | ‐0.81 (‐2.02 to 0.39) | ‐0.90 (‐1.89 to 0.08) | ‐0.40 (‐1.61 to 0.80) |
| FT | ‐0.37 (‐1.09 to 0.35)a | na | ‐ | ‐0.77 (‐2.32 to 0.78) | ‐0.21 (‐1.36 to 0.94) | ‐0.11 (‐1.35 to 1.13) | ‐0.50 (‐1.60 to 0.60) | ‐0.59 (‐1.69 to 0.50) | ‐0.09 (‐1.18 to 0.99) |
| EMDR | na | ‐1.24 (‐2.03 to ‐0.45)a | na | ‐ | 0.56 (‐0.77 to 1.90) | 0.66 (‐0.59 to 1.91) | 0.27 (‐1.03 to 1.57) | 0.18 (‐0.92 to 1.27) | 0.68 (‐0.62 to 1.97) |
| CCT dyad | na | na | na | na | ‐ | 0.10 (‐0.87 to 1.07) | ‐0.29 (‐0.63 to 0.04) | ‐0.39 (‐1.15 to 0.38) | 0.11 (‐0.66 to 0.89) |
| CCT child | na | na | na | na | na | ‐ | ‐0.39 (‐1.30 to 0.52) | ‐0.48 (‐1.08 to 0.11) | 0.02 (‐0.89 to 0.93) |
| CBT dyad | ‐0.32 (‐1.36 to 0.72) | ‐1.21 (‐2.21 to ‐0.21)a | na | na | ‐0.40 (‐0.65 to ‐0.16) | na | ‐ | ‐0.09 (‐0.79 to 0.60) | 0.41 (‐0.29 to 1.11) |
| CBT child | ‐0.96 (‐1.68 to ‐0.24)a | ‐1.59 (‐2.45 to ‐0.72) | na | 0.18 (‐0.87 to 1.23)a | na | ‐0.48 (‐0.99 to 0.03)a | ‐0.00 (‐0.52 to 0.52) | ‐ | 0.50 (‐0.19 to 1.19) |
| CBT carer | ‐0.43 (‐1.13 to 0.26)a | na | na | na | na | na | 0.40 (‐0.23 to 1.04)a | 0.50 (‐0.13 to 1.12)a | ‐ |
| aResults based on a single study | |||||||||
For NMA estimates, there was weak evidence for CCT dyad (SMD ‐0.87, 95% CI ‐1.64 to ‐0.10, 0 studies) and CBT child (SMD ‐0.96, 95% CI ‐1.72 to ‐0.20, 1 study) reducing PTSD symptoms at post‐treatment relative to MAU. There was no evidence of an effect for EMDR, FT, CBT dyad and CBT carer in reducing PTSD symptoms at post‐treatment relative to MAU. The Chi2 P value was 0.3, suggesting no evidence of heterogeneity.
For pairwise comparisons, there was weak evidence for CBT child reducing PTSD symptoms at post‐treatment relative to MAU (SMD ‐0.96, 95% CI ‐1.68 to ‐0.24, 1 study). Heterogeneity assessments were not applicable, as there was only one study informing the pairwise comparisons. For the direct comparison of CBT dyad versus MAU, Tau² was 0.43, Chi² = 4.30 and I² = 77%, suggesting considerable heterogeneity.
Using a loop‐based assessment, we found no evidence of inconsistency in the NMA. There were five closed loops in this network and all the lower CI limits of the inconsistency factors reached zero. However, the CI included large values, so we cannot rule out the possibility of inconsistency (see 'Figure 1. Inconsistency plots', available here).
We gave a very low confidence rating to all the estimates of this analysis because the effect estimates had major concerns in the within‐study bias domain (based on the risk of bias assessments), imprecision domain (uncertain effect estimates with wide CI), and in the heterogeneity domain (high variability in the results of the studies that contributed to each comparison).
Six months follow‐up
Figure 4 (b) provides the graphical representation of this network. Direct evidence was available for nine comparisons coming from five studies. All NMA results are reported relative to MAU and the number of direct studies given in brackets. Where the number of direct studies is zero, the estimate is based on indirect evidence from the NMA. The full set of pairwise and network meta‐analyses is summarised in Table 3 below.
Table 3 Pairwise and network meta‐analyses results (SMD and 95% CI) for PTSD at six months follow‐up
| MAU | FT | CCT dyad | CCT child | CBT dyad | CBT child | CBT carer | |
| MAU | ‐ | 0.04 (‐0.67 to 0.76) | ‐0.26 (‐1.02 to 0.49) | ‐0.03 (‐0.90 to 0.85) | ‐0.72 (‐1.42 to ‐0.02) | ‐0.94 (‐1.64 to ‐0.25) | ‐0.49 (‐1.18 to 0.19) |
| FT | 0.04 (‐0.67 to 0.76)a | ‐ | ‐0.31 (‐1.35 to 0.73) | ‐0.07 (‐1.20 to 1.06) | ‐0.76 (‐1.76 to 0.24) | ‐0.99 (‐1.99 to 0.01) | ‐0.54 (‐1.53 to 0.45) |
| CCT dyad | na | na | ‐ | 0.24 (‐0.63 to 1.10) | ‐0.45 (‐0.73 to ‐0.17) | ‐0.68 (‐1.36 to 0.00) | ‐0.23 (‐0.92 to 0.46) |
| CCT child | na | na | na | ‐ | ‐0.69 (‐1.51 to 0.13) | ‐0.92 (‐1.45 to ‐0.39) | ‐0.47 (‐1.28 to 0.35) |
| CBT dyad | na | na | ‐0.46 (‐0.74 to ‐0.17)a | ‐0.92 (‐1.45 to ‐0.39)a | ‐ | ‐0.23 (‐0.85 to 0.39) | 0.22 (‐0.41 to 0.85) |
| CBT child | ‐0.88 (‐1.59 to ‐0.17)a | na | na | na | ‐0.26 (‐0.88 to 0.36)a | ‐ | 0.45 (‐0.17 to 1.07) |
| CBT carer | ‐0.43 (‐1.12 to 0.26)a | na | na | na | 0.23 (‐0.40 to 0.86)a | 0.48 (‐0.14 to 1.10)a | ‐ |
| aResults based on a single study | |||||||
For NMA estimates, there was weak evidence for CBT dyad (SMD ‐0.72, 95% CI ‐1.42 to ‐0.02, 1 study) and CBT child (SMD ‐0.94, 95% CI ‐1.64 to ‐0.25, 1 study) reducing PTSD symptoms at six months follow‐up relative to MAU. For the pairwise comparisons, there was weak evidence for CBT child reducing PTSD symptoms at six months follow‐up relative to MAU (SMD ‐0.88, 95% CI ‐1.59 to ‐0.17, 1 study). Assessments of heterogeneity were not applicable here, as all pairwise comparisons were informed by only one study.
Evidence of inconsistency could not be assessed, as the two closed loops in this network were formed exclusively by multi‐arm trials.
The CINeMA confidence rating assessment cannot be performed when there are less than five studies informing a network. Due to the low number of studies included in this network, the analyses to make judgements on imprecision, heterogeneity and incoherence could not be performed.
12 months follow‐up
Figure 4 (c) provides the graphical representation of this network. Direct evidence was available for eight comparisons coming from four studies. All NMA results are reported relative to MAU and the number of direct studies given in brackets. Where the number of direct studies is zero, the estimate is based on indirect evidence from the NMA. The full set of pairwise and network meta‐analyses is summarised in Table 4 below.
Table 4 Pairwise and network meta‐analyses results (SMD and 95% CI) for PTSD at 12 months follow‐up
| MAU | CCT dyad | CCT child | CBT dyad | CBT child | CBT carer | |
| MAU | ‐ | ‐0.42 (‐1.17 to 0.33) | ‐0.10 (‐0.95 to 0.75) | ‐0.75 (‐1.45 to ‐0.05) | ‐0.54 (‐1.22 to 0.15) | ‐0.33 (‐1.02 to 0.35) |
| CCT dyad | na | ‐ | 0.32 (‐0.53 to 1.16) | ‐0.33 (‐0.59 to ‐0.07) | ‐0.12 (‐0.79 to 0.56) | 0.09 (‐0.60 to 0.77) |
| CCT child | na | na | ‐ | ‐0.65 (‐1.45 to 0.16) | ‐0.43 (‐0.94 to 0.08) | ‐0.23 (‐1.03 to 0.57) |
| CBT dyad | ‐0.68 (‐1.39 to 0.03)a | ‐0.33 (‐0.59 to ‐0.07) | na | ‐ | 0.22 (‐0.41 to 0.84) | 0.42 (‐0.21 to 1.05) |
| CBT child | ‐0.47 (‐1.16 to 0.21)a | na | ‐0.43 (‐0.94 to 0.08)a | 0.21 (‐0.41 to 0.84)a | ‐ | 0.20 (‐0.41 to 0.81) |
| CBT carer | ‐0.33 (‐1.02 to 0.36)a | na | na | 0.47 (‐0.17 to 1.11)a | 0.22 (‐0.40 to 0.83)a | ‐ |
| aResults based on a single study | ||||||
For NMA estimates, there was some evidence for CBT dyad reducing PTSD symptoms at 12 months follow‐up relative to MAU (SMD ‐0.75, 95% CI ‐1.45 to ‐0.05, 1 study). However, there was no evidence of an effect for all other interventions relative to MAU. For the pairwise comparisons, there was no evidence for any therapy reducing PTSD symptoms at 12 months follow‐up compared to MAU. Assessments of heterogeneity were not applicable here, as all pairwise comparisons were informed by only one study.
There were four closed loops in this network, all of which were formed exclusively by multi‐arm trials. As such, evidence of statistical inconsistency could not be assessed.
Due to the low number of studies included in this network, the CINeMA assessments could not be performed.
Psychological distress: depression
Post‐treatment
Figure 4 (d) provides the graphical representation of this network. Direct evidence was available for 14 comparisons coming from 12 studies. All NMA results are reported relative to MAU and the number of direct studies given in brackets. Where the number of direct studies is zero, the estimate is based on indirect evidence from the NMA. The full set of pairwise and network meta‐analyses is summarised in Table 5 below.
Table 5 Pairwise and network meta‐analyses results (SMD and 95% CI) for depression at post‐treatment
| MAU | WL | FT | EMDR | CCT dyad | CCT child higher | CCT child | CBT dyad higher | CBT dyad | CBT child | CBT carer | |
| MAU | ‐ | ‐1.82 (‐5.04 to 1.40) | ‐0.42 (‐2.61 to 1.76) | ‐0.72 (‐3.82 to 2.37) | ‐0.51 (‐3.02 to 2.01) | ‐1.07 (‐3.57 to 1.43) | ‐0.88 (‐2.69 to 0.94) | 0.98 (‐1.55 to 3.51) | 0.07 (‐2.56 to 2.69) | ‐0.80 (‐2.60 to 1.01) | ‐0.64 (‐2.45 to 1.17) |
| WL | na | ‐ | 0.57 (‐2.62 to 3.77) | ‐1.30 (‐3.16 to 0.56) | 0.10 (‐2.79 to 2.98) | ‐0.20 (‐3.36 to 2.95) | 0.02 (‐2.57 to 2.61) | ‐0.54 (‐3.67 to 2.59) | ‐0.35 (‐2.97 to 2.26) | ‐0.27 (‐2.18 to 1.63) | ‐0.12 (‐2.73 to 2.49) |
| FT | 0.05 (‐0.66 to 0.77) | na | ‐ | ‐1.87 (‐5.57 to 1.83) | ‐0.48 (‐3.32 to 2.37) | ‐0.78 (‐4.37 to 2.82) | ‐0.56 (‐3.67 to 2.55) | ‐1.12 (‐4.21 to 1.98) | ‐0.93 (‐3.50 to 1.65) | ‐0.85 (‐3.42 to 1.72) | ‐0.69 (‐3.27 to 1.88) |
| EMDR | na | ‐1.30 (‐2.10 to ‐0.51)a | na | ‐ | 1.40 (‐2.04 to 4.83) | 1.10 (‐2.57 to 4.76) | 1.31 (‐1.88 to 4.50) | 0.75 (‐2.89 to 4.40) | 0.94 (‐2.27 to 4.15) | 1.02 (‐1.64 to 3.69) | 1.18 (‐2.03 to 4.39) |
| CCT dyad | na | na | na | na | ‐ | ‐0.30 (‐3.62 to 3.02) | ‐0.08 (‐2.87 to 2.70) | ‐0.64 (‐2.75 to 1.47) | ‐0.45 (‐1.67 to 0.76) | ‐0.37 (‐2.54 to 1.79) | ‐0.22 (‐2.39 to 1.95) |
| CCT child higher | na | na | na | na | na | ‐ | 0.22 (‐1.58 to 2.02) | ‐0.34 (‐3.87 to 3.19) | ‐0.15 (‐3.24 to 2.93) | ‐0.07 (‐2.59 to 2.44) | 0.08 (‐3.00 to 3.17) |
| CCT child | na | na | na | na | na | 0.22 (‐0.43 to 0.87)a | ‐ | ‐0.56 (‐3.60 to 2.48) | ‐0.37 (‐2.88 to 2.13) | ‐0.29 (‐2.04 to 1.46) | ‐0.14 (‐2.64 to 2.37) |
| CBT dyad higher | na | na | na | na | na | na | na | ‐ | 0.19 (‐1.53 to 1.91) | 0.27 (‐2.21 to 2.75) | 0.42 (‐2.06 to 2.91) |
| CBT dyad | ‐0.33 (‐1.22 to 0.57) | ‐0.28 (‐1.19 to 0.63)a | na | na | ‐0.43 (‐0.68 to ‐0.19) | na | na | 0.19 (‐0.18 to 0.56)a | ‐ | 0.08 (‐1.71 to 1.87) | 0.23 (‐1.56 to 2.03) |
| CBT child | ‐0.73 (‐1.42 to ‐0.05)a | ‐1.05 (‐2.43 to 0.34) | na | na | na | na | ‐0.29 (‐0.79 to 0.21) | na | 0.07 (‐0.45 to 0.58) | ‐ | 0.15 (‐1.63 to 1.94) |
| CBT carer | ‐0.33 (‐1.02 to 0.36)a | na | na | na | na | na | na | na | 0.25 (‐0.38 to 0.88)a | 0.16 (‐0.45 to 0.78)a | ‐ |
| aResults based on a single study | |||||||||||
For NMA, there was no evidence of an effect for any therapy reducing depression symptoms at post‐treatment, compared to MAU. For pairwise comparisons, there was weak evidence for CBT child reducing depression symptoms at post‐treatment, compared to MAU (SMD ‐0.73, 95% CI ‐1.42 to ‐0.05, 1 study).
There were five closed loops. Two of these were formed by a multi‐arm trial, which is consistent by definition. For the other three, an assessment of inconsistency was possible using both global and local approaches. The P value from the global test was 0.67, suggesting no evidence of global inconsistency. For the local, loop‐based assessment of inconsistency, the lower CI of the inconsistency factors reached zero, potentially suggesting no evidence of statistical inconsistency. However, as the upper confidence limits included large values, we caution that some inconsistency is still likely (see 'Figure 1. Inconsistency plots', available here)
CINeMA assessments provided a very low confidence rating for all the estimates from the NMA, on the basis of major concerns for within‐study bias, imprecision and/or heterogeneity domains.
Six months follow‐up
Figure 4 (e) provides the graphical representation of this network. Direct evidence was available for nine comparisons coming from five studies. All NMA results are reported relative to MAU and the number of direct studies given in brackets. Where the number of direct studies is zero, the estimate is based on indirect evidence from the NMA. The full set of pairwise and network meta‐analyses is summarised in Table 6 below.
Table 6 Pairwise and network meta‐analyses results (SMD and 95% CI) for depression at six months follow‐up
| MAU | FT | CCT dyad | CCT dyad higher | CBT dyad | CBT child | CBT carer | |
| MAU | ‐ | ‐0.11 (‐0.83 to 0.60) | 0.18 (‐0.55 to 0.90) | ‐0.25 (‐1.02 to 0.52) | ‐0.09 (‐0.77 to 0.59) | ‐0.56 (‐1.23 to 0.11) | ‐0.23 (‐0.90 to 0.45) |
| FT | ‐0.11 (‐0.83 to 0.60)a | ‐ | 0.29 (‐0.73 to 1.31) | ‐0.14 (‐1.19 to 0.92) | 0.02 (‐0.96 to 1.01) | ‐0.45 (‐1.43 to 0.53) | ‐0.11 (‐1.09 to 0.87) |
| CCT dyad | na | na | ‐ | ‐0.43 (‐0.88 to 0.03) | ‐0.27 (‐0.53 to ‐0.01) | ‐0.74 (‐1.42 to ‐0.06) | ‐0.40 (‐1.08 to 0.28) |
| CCT dyad higher | na | na | na | ‐ | 0.16 (‐0.21 to 0.53) | ‐0.31 (‐1.04 to 0.41) | 0.02 (‐0.71 to 0.75) |
| CBT dyad | ‐0.09 (‐0.77 to 0.59)a | na | ‐0.27 (‐0.53 to ‐0.01) | 0.16 (‐0.21 to 0.53)a | ‐ | ‐0.47 (‐1.10 to 0.16) | ‐0.13 (‐0.76 to 0.49) |
| CBT child | ‐0.61 (‐1.29 to 0.07)a | na | na | na | ‐0.57 (‐1.20 to 0.06)a | ‐ | 0.34 (‐0.28 to 0.95) |
| CBT carer | 0.36 (‐0.26 to 0.98)a | na | na | na | ‐0.12 (‐0.75 to 0.51)a | 0.36 (‐0.26 to 0.98)a | ‐ |
| aResults based on a single study | |||||||
For NMA estimates, there was no evidence of any therapy reducing depression symptoms at six months follow‐up, compared to MAU. For pairwise comparisons, there was no evidence of any therapy reducing depression symptoms at six months follow‐up, compared to MAU. For the direct comparison of CBT dyad versus MAU, Tau² was 0.31, Chi² was 4.00 and I² was 75%, suggesting considerable heterogeneity among the studies.
There were four closed loops in this network, all of which were formed exclusively by multi‐arm trials. As such, evidence of inconsistency could not be assessed.
Due to the low number of studies included in the six‐month follow‐up network, the CINeMA assessments for confidence in the evidence could not be performed for the depression symptoms outcome.
12 months follow‐up
Figure 4 (f) provides the graphical representation of this network. Direct evidence was available for nine comparisons. All NMA results are reported relative to MAU and the number of direct studies given in brackets. Where the number of direct studies is zero, the estimate is based on indirect evidence from the NMA. The full set of pairwise and network meta‐analyses is summarised in Table 7 below.
Table 7 Pairwise and network meta‐analyses results (SMD and 95% CI) for depression at 12 months follow‐up
| MAU | CCT dyad | CCT child | CBT dyad higher | CBT dyad | CBT child | CBT carer | |
| MAU | ‐ | ‐0.01 (‐0.73 to 0.72) | ‐0.19 (‐1.03 to 0.64) | ‐0.11 (‐0.88 to 0.66) | ‐0.18 (‐0.86 to 0.49) | ‐0.56 (‐1.23 to 0.11) | ‐0.38 (‐1.06 to 0.29) |
| CCT dyad | na | ‐ | ‐0.19 (‐1.03 to 0.66) | ‐0.10 (‐0.55 to 0.35) | ‐0.17 (‐0.43 to 0.08) | ‐0.55 (‐1.22 to 0.13) | ‐0.38 (‐1.05 to 0.30) |
| CCT child | na | na | ‐ | 0.08 (‐0.80 to 0.97) | 0.01 (‐0.79 to 0.82) | ‐0.36 (‐0.87 to 0.14) | ‐0.19 (‐0.98 to 0.61) |
| CBT dyad higher | na | na | na | ‐ | ‐0.07 (‐0.44 to 0.30) | ‐0.45 (‐1.17 to 0.28) | ‐0.27 (‐1.00 to 0.46) |
| CBT dyad | ‐0.16 (‐0.84 to 0.52)a | ‐0.18 (‐0.44 to 0.07) | na | ‐0.07 (‐0.44 to 0.30)a | ‐ | ‐0.37 (‐1.00 to 0.25) | ‐0.20 (‐0.83 to 0.43) |
| CBT child | ‐0.59 (‐1.27 to 0.09)a | na | ‐0.36 (‐0.87 to 0.14)a | na | ‐0.42 (‐1.05 to 0.20)a | ‐ | 0.17 (‐0.44 to 0.79) |
| CBT carer | ‐0.34 (‐1.01 to 0.34)a | na | na | na | ‐0.19 (‐0.82 to 0.44)a | 0.20 (‐0.42 to 0.81)a | ‐ |
| aResults based on a single study | |||||||
Relative to MAU, there was no evidence to support a beneficial effect of any therapy reducing depression symptoms at 12 months follow‐up, from either NMA or standard meta‐analyses. Assessments of heterogeneity were not applicable.
There were four closed loops in this network, all of which were formed exclusively by multi‐arm trials. As such, evidence of inconsistency could not be assessed.
Due to the low number of studies included in the 12‐month follow‐up network for the depression symptoms outcome, the CINeMA assessments for confidence in the evidence could not be performed.
Psychological distress: anxiety
Post‐treatment
Figure 5 (a) provides the graphical representation of this network. Direct evidence was available for 12 comparisons coming from 10 studies. All NMA results are reported relative to MAU and the number of direct studies given in brackets. Where the number of direct studies is zero, the estimate is based on indirect evidence from the NMA. The full set of pairwise and network meta‐analyses is summarised in Table 8 below.
5.
Network meta‐analyses for anxiety, sexualised behaviour internalising behaviour and externalising behaviour at post‐treatment; externalising behaviour at 6 months follow‐up and sexualised behaviour at 12 months follow‐up
Abbreviations CBT carer: cognitive behavioural therapy delivered to the carer; CBT child: cognitive behavioural therapy delivered to the child; CBT dyad: cognitive behavioural therapy delivered to the carer and the child; CBT dyad higher: cognitive behavioural therapy delivered to the carer and the child at a higher dose; CCT dyad: child centred therapy delivered to the carer and the child; EMDR: eye movement desensitization and reprocessing; FT: family therapy; MAU: management as usual; WL: waiting list.
Table 8 Pairwise and network meta‐analyses results (SMD and 95% CI) for anxiety at post‐treatment
| MAU | WL | EMDR | CCT dyad | CBT dyad higher | CBT dyad | CBT child | CBT carer | |
| MAU | ‐ | 0.50 (‐2.09 to 3.09) | ‐0.84 (‐2.65 to 0.97) | ‐0.65 (‐1.97 to 0.67) | 0.66 (‐1.18 to 2.50) | 0.56 (‐1.44 to 2.55) | ‐0.13 (‐1.45 to 1.20) | ‐0.01 (‐1.33 to 1.31) |
| WIL | na | ‐ | ‐0.88 (‐2.28 to 0.53) | ‐0.65 (‐2.82 to 1.53) | ‐1.10 (‐3.44 to 1.25) | ‐0.90 (‐2.89 to 1.09) | ‐0.38 (‐1.87 to 1.11) | ‐0.26 (‐2.25 to 1.73) |
| EMDR | na | ‐0.88 (‐1.63 to ‐0.12)a | ‐ | 0.23 (‐2.35 to 2.81) | ‐0.22 (‐2.95 to 2.51) | ‐0.02 (‐2.46 to 2.41) | 0.50 (‐1.55 to 2.54) | 0.61 (‐1.82 to 3.05) |
| CCT dyad | na | ‐0.15 (‐0.92 to 0.62)a | na | ‐ | ‐0.45 (‐1.97 to 1.07) | ‐0.25 (‐1.13 to 0.62) | 0.27 (‐1.32 to 1.85) | 0.38 (‐1.20 to 1.96) |
| CBT dyad higher | na | na | na | na | ‐ | 0.20 (‐1.04 to 1.44) | 0.72 (‐1.09 to 2.53) | 0.83 (‐0.98 to 2.64) |
| CBT dyad | ‐0.34 (‐1.02 to 0.34) | ‐0.31 (‐1.22 to 0.60)a | na | ‐0.25 (‐0.49 to ‐0.01) | 0.20 (‐0.18 to 0.57)a | ‐ | 0.52 (‐0.80 to 1.84) | 0.64 (‐0.68 to 1.96) |
| CBT child | ‐0.13 (‐0.73 to 0.47)a | ‐1.24 (‐2.45 to ‐0.04) | na | na | na | 0.37 (‐0.15 to 0.88) | ‐ | 0.12 (‐1.20 to 1.44) |
| CBT carer | ‐0.01 (‐0.61 to 0.59)a | na | na | na | na | 0.61 (0.02 to 1.21)a | ‐0.13 (‐0.73 to 0.47)a | ‐ |
| aResults based on a single study | ||||||||
Relative to MAU, there was no evidence from either NMA or standard meta‐analyses to indicate a beneficial effect of therapy reducing anxiety symptoms at post‐treatment.
There were six closed loops in the network. One of these was formed by a multi‐arm trial, which is consistent by definition. For the other five, an assessment of inconsistency was possible using both global and local approaches. The global test for inconsistency had a P value of 0.45, suggesting no evidence of inconsistency. For the local, loop‐based assessment of inconsistency, the lower CI of the inconsistency factors reached zero, potentially suggesting no evidence of statistical inconsistency. However, as the upper CI included large values, we caution that some inconsistency is still likely (see 'Figure 1. Inconsistency plots', available here).
CINeMA assessments provided a very low rating of confidence in the estimates of these analyses because they had major concerns in three dimensions: inconsistency, heterogeneity and within‐study bias.
Six months follow‐up
Only two studies reported evidence for anxiety at six months follow‐up (one comparison, Analysis 3.14, Table 9 below). Therefore, we were unable to perform an NMA.
3.14. Analysis.

Comparison 3: CBT dyad versus CCT dyad, Outcome 14: Anxiety 6 months
Table 9 Summary of results for anxiety at six months follow‐up
| Intervention | Control | No. of trials | RE E a | 95% CI | P value | I2 b | Participants | Trials | Link to analysis |
| Cognitive behavioural therapy | Child Centred Therapy | 2 | SMD ‐0.32 | ‐0.58 to ‐0.06 | 0.02 | 0% | 233 | Cohen 1998; Cohen 2004 | Analysis 3.14 |
| aRandom‐effects (more than one trial) or fixed‐effect (one trial) estimates. bAn I2 from a meta‐analysis of less than seven studies has low power and precision to detect heterogeneity (Higgins 2021a). | |||||||||
The estimate from the pairwise comparison from the standard meta‐analysis suggests weak evidence to support a beneficial effect for CBT dyad reducing the anxiety symptoms at six months relative to CCT dyad (SMD ‐0.32, 95% CI ‐0.58 to ‐0.06, 2 studies). The I2 was 0%, Tau² was 0.00 and Chi² was 0.73, suggesting no heterogeneity between the two trials compared.
12 months follow‐up
Only three studies reported evidence for anxiety at 12 months follow‐up (two comparisons, Analysis 2.13; Analysis 3.15 in Table 10 below). Therefore, we were unable to perform an NMA.
2.13. Analysis.

Comparison 2: CBT dyad versus MAU, Outcome 13: Anxiety 12 months
3.15. Analysis.

Comparison 3: CBT dyad versus CCT dyad, Outcome 15: Anxiety 12 months
Table 10 Summary of results for anxiety at 12 months follow‐up
| Experimental | Control | No. of trials | RE or FE Ea | 95% CI | P value | I2 b | Participants | Trials | Link to analysis |
| CBT dyad | MAU | 1 | MD ‐2.40 | ‐6.14 to 1.34 | 0.21 | NA | 65 | Berliner 1996 | Analysis 2.13 |
| CBT dyad | CCT dyad | 2 | SMD ‐0.20 | ‐0.48 to 0.09 | 0.17 | 0% | 194 | Cohen 1998; Cohen 2004 | Analysis 3.15 |
| aRandom‐effects (more than one trial) or fixed‐effect (one trial) estimates. bAn I2 from a meta‐analysis of less than seven studies has low power and precision to detect heterogeneity (Higgins 2021a). | |||||||||
The estimate from the pairwise comparison from the standard meta‐analysis suggests no evidence to support a beneficial effect for CBT dyad reducing anxiety symptoms at 12 months follow‐up relative to CCT dyad (SMD ‐0.20, 95% CI ‐0.48 to 0.09, 2 studies). Tau² was 0.00, Chi² was 0.00 and I² was 0%, suggesting no evidence of heterogeneity was observed between the two trials compared.
Also, there was no evidence for CBT dyad having a beneficial effect in reducing the anxiety symptoms at 12 months follow‐up compared to MAU (MD 2.40, 95% CI ‐6.14 to 1.34, 1 study). Heterogeneity assessments do not apply here, as there is only one study informing the comparison for this outcome.
Behaviour: sexualised behaviour
Post‐treatment
Figure 5 (b) provides the graphical representation of this network. Direct evidence was available for four comparisons coming from seven studies. All NMA results are reported relative to MAU and the number of direct studies given in brackets. Where the number of direct studies is zero, the estimate is based on indirect evidence from the NMA. The full set of pairwise and network meta‐analyses is summarised in Table 11 below.
Table 11 Pairwise and network meta‐analyses results (SMD and 95% CI) for sexualised behaviour at post‐treatment
| MAU | FT | CCT dyad | CBT dyad higher | CBT dyad | |
| MAU | ‐ | ‐0.43 (‐1.19 to 0.33) | 0.55 (‐0.02 to 1.11) | 0.11 (‐0.52 to 0.75) | 0.37 (‐0.13 to 0.87) |
| FT | ‐0.43 (‐1.15 to 0.30)a | ‐ | 0.98 (0.03 to 1.92) | 0.54 (‐0.44 to 1.53) | 0.80 (‐0.11 to 1.71) |
| CCT dyad | na | na | ‐ | ‐0.43 (‐0.90 to 0.03) | ‐0.18 (‐0.44 to 0.09) |
| CBT dyad higher | na | na | na | ‐ | 0.26 (‐0.13 to 0.64) |
| CBT dyad | 0.37 (‐0.08 to 0.82) | na | ‐0.28 (‐0.49 to ‐0.07) | 0.26 (‐0.06 to 0.57)a | ‐ |
| aResults based on a single study | |||||
For both NMA and pairwise analyses, there was no evidence for any therapy reducing sexualised behaviour symptoms at post‐treatment relative to MAU. Heterogeneity assessments were not applicable.
This network consists of two‐arm studies and has no closed loops. Therefore, we were unable to evaluate global and local inconsistency.
We gave a very low CINeMA confidence rating to all estimates because of major concerns about within‐study bias, precision and inconsistency.
Six months follow‐up
Only three studies reported evidence for sexualised behaviour at six months follow‐up (two comparisons, Analysis 3.16; Analysis 6.9 in Table 12 below). Therefore, we were unable to perform network meta‐analysis.
3.16. Analysis.

Comparison 3: CBT dyad versus CCT dyad, Outcome 16: Sexualised behaviour 6 months
6.9. Analysis.

Comparison 6: Family therapy versus MAU, Outcome 9: Sexualised behaviour 6 months
Table 12 Summary of results for sexualised behaviour six months follow‐up
| Intervention | Control | No. of trials | RE or FE Ea | 95% CI | P value | I2 b | Participants | Trials | Link to analysis |
| Cognitive behavioural therapy (CBT) | Child centred therapy (CCT) | 2 | SMD ‐0.35 | ‐0.86 to 0.16 | 0.18 | 27% | 89 | Cohen 1996; Cohen 1998 | Analysis 3.16 |
| Family therapy | Management as usual (MAU) | 1 | MD 0.00 | ‐0.21 to 0.21 | 1.00 | NA | 30 | Danielson 2012 | Analysis 6.9 |
| aRandom‐effects (more than one trial) or fixed‐effect (one trial) estimates. bAn I2 from a meta‐analysis of less than seven studies has low power and precision to detect heterogeneity (Higgins 2021a). | |||||||||
The estimate from the pairwise comparison from the standard meta‐analysis suggests no evidence to support a beneficial effect for CBT dyad reducing the sexualised behaviour symptoms at six months relative to CCT dyad (SMD ‐0.35, 95% CI ‐0.86 to 0.16, 2 studies). Tau² was 0.04, Chi² was 1.37, and I² was 27%, suggesting no important heterogeneity between the two trials compared.
Also, there was no evidence for family therapy having a beneficial effect in reducing the sexualised behaviour symptoms at six months compared to MAU (MD 0.00 95% CI ‐0.21 to 0.21, 1 study).
12 months follow‐up
Figure 5 (c) provides the graphical representation of this network. Direct evidence was available for three comparisons coming from four studies. All NMA results are reported relative to MAU and the number of direct studies given in brackets. Where the number of direct studies is zero, the estimate is based on indirect evidence from the NMA. The full set of pairwise and network meta‐analyses is summarised in Table 13 below.
Table 13 Pairwise and network meta‐analyses results (SMD and 95% CI) for sexualised behaviour at 12 months follow‐up
| MAU | CCT dyad | CBT dyad higher | CBT dyad | |
| MAU | ‐ | 0.71 (0.13 to 1.29) | 0.20 (‐0.35 to 0.75) | 0.30 (‐0.16 to 0.75) |
| CCT dyad | na | ‐ | ‐0.51 (‐0.99 to ‐0.03) | ‐0.41 (‐0.77 to ‐0.05) |
| CBT dyad higher | na | na | ‐ | 0.10 (‐0.22 to 0.41) |
| CBT dyad | 0.30 (‐0.16 to 0.75)a | ‐0.41 (‐0.77 to ‐0.05) | 0.10 (‐0.22 to 0.41)a | ‐ |
| aResults based on a single study | ||||
For both NMA and pairwise analyses, there was no evidence for any therapy reducing sexualised behaviour symptoms at 12 months follow‐up relative to MAU. Heterogeneity assessments were not applicable.
Due to the low number of studies included in the network for sexualised behaviour at 12 months follow‐up, the CINeMA assessments could not be performed.
Behaviour: internalising
Post‐treatment
Figure 5 (d) provides the graphical representation of this network. Direct evidence was available for 14 comparisons coming from 11 studies. All NMA results are reported relative to MAU and the number of direct studies given in brackets. Where the number of direct studies is zero, the estimate is based on indirect evidence from the NMA. The full set of pairwise and network meta‐analyses is summarised in Table 14 below.
Table 14 Pairwise and network meta‐analyses results (SMD and 95% CI) for internalising at post‐treatment
| MAU | WL | FT | EMDR | CCT dyad | CBT dyad higher | CBT dyad | CBT child | CBT carer | |
| MAU | ‐ | 0.22 (‐0.41 to 0.85) | ‐1.19 (‐2.54 to 0.15) | ‐0.39 (‐1.05 to 0.28) | ‐0.17 (‐0.76 to 0.42) | 0.46 (‐0.24 to 1.17) | ‐0.83 (‐1.93 to 0.28) | ‐0.37 (‐0.97 to 0.23) | ‐0.42 (‐1.03 to 0.18) |
| WL | na | ‐ | 0.84 (‐0.46 to 2.14) | ‐0.75 (‐1.50 to ‐0.01) | 0.74 (‐0.35 to 1.84) | 0.13 (‐0.99 to.25) | 0.35 (‐0.72 to 1.42) | 0.15 (‐0.75 to 1.06) | 0.10 (‐0.98 to 1.17) |
| FT | 0.32 (‐0.40 to 1.04)a | na | ‐ | ‐1.59 (‐3.09 to ‐0.09) | ‐0.09 (‐1.05 to 0.86) | ‐0.71 (‐1.69 to 0.28) | ‐0.49 (‐1.42 to 0.44) | ‐0.68 (‐1.62 to 0.26) | ‐0.74 (‐1.68 to 0.20) |
| EMDR | na | ‐0.75 (‐1.50 to ‐0.01)a | na | ‐ | 1.49 (0.17 to 2.82) | 0.88 (‐0.46 to 2.22) | 1.10 (‐0.20 to 2.41) | 0.90 (‐0.26 to 2.07) | 0.85 (‐0.46 to 2.16) |
| CCT dyad | na | ‐0.45 (‐1.23 to 0.33)a | na | na | ‐ | ‐0.61 (‐1.00 to ‐0.22) | ‐0.39 (‐0.62 to‐0.16) | ‐0.59 (‐1.21 to 0.03) | ‐0.65 (‐1.27 to ‐0.02) |
| CBT dyad higher | na | na | na | na | na | ‐ | 0.22 (‐0.10 to 0.53) | 0.02 (‐0.64 to 0.68) | ‐0.03 (‐0.69 to 0.62) |
| CBT dyad | 0.16 (‐0.17 to 0.48) | ‐0.43 (‐1.34 to 0.49)a | na | na | ‐0.40 (‐0.68 to ‐0.12) | 0.22 (‐0.10 to 0.53)a | ‐ | ‐0.20 (‐0.77 to 0.38) | ‐0.25 (‐0.83 to 0.33) |
| CBT child | ‐0.36 (‐0.96 to 0.24)a | 0.18 (‐0.73 to 1.08)a | na | na | na | na | 0.11 (‐0.67 to 0.89) | ‐ | ‐0.06 (‐0.65 to.53) |
| CBT carer | ‐0.40 (‐1.00 to 0.20)a | na | na | na | na | na | ‐0.25 (‐0.83 to 0.33)a | ‐0.07 (‐0.66 to 0.52)a | ‐ |
| aResults based on a single study | |||||||||
Relative to MAU, there was no evidence from either the NMA or standard meta‐analyses to indicate a beneficial effect of therapy in reducing internalising behaviour symptoms at post‐treatment.
There were six closed loops. One of these was formed by a multi‐arm trial, which is consistent by definition. For the other five, an assessment of inconsistency was possible using both global and local approaches. The test for global inconsistency had a P value of 0.09 suggesting global inconsistency. For the local, loop‐based assessment of inconsistency, the lower CI of the inconsistency factors reached zero, potentially suggesting no evidence of statistical inconsistency. However, as the upper CI included large values, we caution that some inconsistency is still likely (see 'Figure 1. Inconsistency plots', available here).
Using the CINeMA tool for assessing confidence in the estimates, we gave a very low confidence rating to all the estimates due to major concerns for within‐study bias, imprecision, and some concerns relating to inconsistency.
Six months follow‐up
Four studies reported evidence for internalising behaviour six months follow‐up (two comparisons, Analysis 3.17; Analysis 6.10 in Table 15 below). There were not enough studies to perform an NMA.
3.17. Analysis.

Comparison 3: CBT dyad versus CCT dyad, Outcome 17: Internalising behaviour 6 months
6.10. Analysis.

Comparison 6: Family therapy versus MAU, Outcome 10: Internalising behaviour 6 months
Table 15 Summary of the results for internalising behaviour at six months follow‐up
| Experimental | Control | No. of trials | RE or FE Ea | 95% CI | P value | I2 b | Participants | Trials | Link to analysis |
| CBT dyad | CCT dyad | 3 | SMD ‐0.27 | ‐0.50 to ‐0.05 | 0.02 | 0% | 304 | Cohen 1996; Cohen 1998; Cohen 2004 | Analysis 3.17 |
| Family Therapy | MAU | 1 | MD 3.30 | ‐1.91 to 8.51 | 1.00 | NA | 30 | Danielson 2012 | Analysis 6.10 |
| aRandom‐effects (more than one trial) or fixed‐effect (one trial) estimates. bAn I2 from a meta‐analysis of less than seven studies has low power and precision to detect heterogeneity (Higgins 2021a). | |||||||||
The estimate from the pairwise comparison from the standard meta‐analysis suggests no evidence to support a beneficial effect for CBT dyad reducing internalising behaviour symptoms at six months follow‐up relative to CCT dyad (SMD ‐0.27, 95% CI ‐0.50 to 0.05, 3 studies). Tau² was 0.00, Chi² was 0.42 and I² was 0%, suggesting no heterogeneity between the three trials compared.
Also, there was no evidence for family therapy having a beneficial effect in reducing internalising behaviour symptoms at six months compared to MAU (MD 3.30, 95% CI ‐1.91 to 8.51, 1 study).
12 months follow‐up
Four studies reported evidence for internalising behaviour 12 months follow‐up (two comparisons, Analysis 2.14; Analysis 3.18 in Table 16 below). There were not enough studies to perform an NMA.
2.14. Analysis.

Comparison 2: CBT dyad versus MAU, Outcome 14: Internalising behaviour 12 months
3.18. Analysis.

Comparison 3: CBT dyad versus CCT dyad, Outcome 18: Internalising behaviour 12 months
Table 16 Summary of the results for internalising behaviour at 12 months follow‐up
| Intervention | Control | No. of trials | RE or FE Ea | 95% CI | P value | I2 b | Participants | Trials | Link to analysis |
| CBT dyad | MAU | 1 | MD 3.00 | 1.41 to 7.41 | 0.03 | NA | 77 | Berliner 1996 | Analysis 2.14 |
| CBT dyad | CCT dyad | 3 | SMD ‐0.26 | ‐0.50 to ‐0.02 | 0.03 | 0% | 271 | Cohen 1996; Cohen 1998; Cohen 2004 | Analysis 3.18 |
| aRandom‐effects (more than one trial) or fixed‐effect (one trial) estimates. bAn I2 from a meta‐analysis of less than seven studies has low power and precision to detect heterogeneity (Higgins 2021a). | |||||||||
The estimate from one trial suggests weak evidence to support a beneficial effect for CBT dyad reducing internalising behaviour symptoms at 12 months follow‐up relative to MAU (MD 3.00, 95% CI 1.41 to 7.41, 1 study). Heterogeneity assessments do not apply here, as there is only one study informing the comparison for this outcome.
There was also weak evidence for CBT dyad having a beneficial effect in reducing internalising behaviour symptoms at 12 months follow‐up compared to CCT dyad (SMD ‐0.26, 95% CI ‐0.50 to ‐0.02, 3 studies). Tau² was 0.00, Chi² was 0.42 and I² was 0%, suggesting no heterogeneity between the three trials compared.
Behaviour: externalising
Post‐treatment
Figure 5 (e) provides the graphical representation of this network. Direct evidence was available for 13 comparisons coming from 11 studies. All NMA results are reported relative to MAU and the number of direct studies given in brackets. Where the number of direct studies is zero, the estimate is based on indirect evidence from the NMA. The full set of pairwise and network meta‐analyses is summarised in Table 17 below.
Table 17 Pairwise and network meta‐analyses results (SMD and 95% CI) for externalising at post‐treatment
| MAU | WL | FT | EMDR | CCT dyad | CBT dyad higher | CBT dyad | CBT child | CBT carer | |
| MAU | ‐ | ‐0.01 (‐1.14 to 1.13) | ‐0.78 (‐2.68 to 1.12) | ‐0.35 (‐1.63 to 0.94) | ‐0.23 (‐1.25 to 0.79) | 0.24 (‐0.99 to 1.47) | 0.10 (‐1.41 to 1.62) | 0.06 (‐0.95 to 1.07) | ‐0.61 (‐1.64 to 0.41) |
| WL | na | ‐ | 0.63 (‐1.21 to 2.47) | ‐0.72 (‐1.75 to 0.31) | 0.40 (‐1.18 to 1.98) | 0.06 (‐1.63 to 1.75) | 0.18 (‐1.32 to 1.68) | 0.47 (‐0.69 to 1.63) | ‐0.21 (‐1.71 to 1.30) |
| FT | 0.23 (‐0.49 to 0.95)± | na | ‐ | ‐1.36 (‐3.46 to 0.75) | ‐0.23 (‐1.75 to 1.29) | ‐0.57 (‐2.21 to 1.06) | ‐0.46 (‐1.89 to 0.98) | ‐0.16 (‐1.59 to 1.27) | ‐0.84 (‐2.28 to 0.60) |
| EMDR | na | ‐0.72 (‐1.47 to 0.02)± | na | ‐ | 1.12 (‐0.76 to 3.01) | 0.78 (‐1.20 to 2.76) | 0.90 (‐0.92 to 2.72) | 1.19 (‐0.36 to 2.74) | 0.51 (‐1.31 to 2.34) |
| CCT dyad | na | ‐0.38 (‐1.16 to 0.40)± | na | na | ‐ | ‐0.34 (‐1.26 to 0.58) | ‐0.22 (‐0.71 to 0.27) | 0.07 (‐1.00 to 1.15) | ‐0.61 (‐1.69 to 0.48) |
| CBT dyad higher | na | na | na | na | na | ‐ | 0.12 (‐0.66 to 0.90) | 0.41 (‐0.82 to 1.65) | ‐0.27 (‐1.51 to 0.98) |
| CBT dyad | 0.11 (‐0.39 to 0.60) | 0.28 (‐0.62 to 1.19)a | na | na | ‐0.23 (‐0.45 to 0.00) | 0.12 (‐0.20 to 0.43)a | ‐ | 0.29 (‐0.67 to 1.25) | ‐0.39 (‐1.36 to 0.58) |
| CBT child | 0.01 (‐0.70 to 0.73)a | 0.53 (‐0.39 to 1.45)a | na | na | na | na | 0.23 (‐0.30 to 0.76) | ‐ | ‐0.68 (‐1.64 to 0.28) |
| CBT carer | ‐0.69 (‐1.45 to 0.06)a | na | na | na | na | na | ‐0.40 (‐1.06 to 0.26)a | ‐0.70 (‐1.36 to ‐0.04)a | ‐ |
| aResults based on a single study | |||||||||
For NMA estimates, there was no evidence of an effect of any therapy reducing externalising behaviour symptoms at post‐treatment compared to MAU. For the pairwise comparisons, there was no evidence of an effect for any therapy reducing externalising behaviours symptoms at post‐treatment compared to MAU.
There were six closed loops. One of these was formed by a multi‐arm trial, which is consistent by definition. For the other five, an assessment of inconsistency was possible using both global and local approaches. The test for global inconsistency had a P value of 0.71, suggesting no evidence against the consistency assumption. For the local, loop‐based assessment of inconsistency, the lower CI of the inconsistency factors reached zero, potentially suggesting no evidence of statistical inconsistency. However, as the upper CI included large values, we caution that some inconsistency is still likely (see 'Figure 1. Inconsistency plots', available here).
We gave a very low confidence rating to all the estimates of this analysis because all of them had major concerns in within‐study bias and imprecision.
Six months follow‐up
Figure 5 (f) provides the graphical representation of this network. Direct evidence was available for nine comparisons coming from six studies. All NMA results are reported relative to MAU and the number of direct studies given in brackets. Where the number of direct studies is zero, the estimate is based on indirect evidence from the NMA. The full set of pairwise and network meta‐analyses is summarised in Table 18 below.
Table 18 Pairwise and network meta‐analyses results (SMD and 95% CI) for externalising at six months follow‐up
| MAU | FT | CCT dyad | CBT dyad higher | CBT dyad | CBT child | CBT carer | |
| MAU | ‐ | ‐0.16 (‐0.88 to 0.55) | 0.04 (‐0.73 to 0.81) | ‐0.05 (‐0.84 to 0.75) | ‐0.03 (‐0.76 to 0.70) | ‐0.21 (‐0.93 to 0.51) | ‐0.41 (‐1.15 to 0.32) |
| FT | ‐0.16 (‐0.88 to 0.55)a | ‐ | 0.20 (‐0.85 to 0.26) | 0.12 (‐0.95 to 1.19) | 0.13 (‐0.89 to 1.16) | ‐0.05 (‐1.06 to 0.97) | ‐0.25 (‐1.28 to 0.78) |
| CCT dyad | na | na | ‐ | ‐0.09 (‐0.48 to.31) | ‐0.07 (‐0.31 to 0.17) | ‐0.25 (‐0.93 to 0.43) | ‐0.46 (‐1.16 to 0.24) |
| CBT dyad higher | na | na | na | ‐ | 0.01 (‐0.30 to 0.33) | ‐0.16 (‐0.88 to 0.55) | ‐0.37 (‐1.10 to 0.36) |
| CBT dyad | ‐0.03 (‐0.76 to 0.70)a | na | ‐0.07 (‐0.31 to 0.17) | 0.01 (‐0.30 to 0.33)a | ‐ | ‐0.18 (‐0.82 to 0.46) | ‐0.38 (‐1.04 to 0.27) |
| CBT child | ‐0.21 (‐0.93 to 0.51)a | na | na | na | ‐0.17 (‐0.81 to 0.47]a | ‐ | ‐0.20 (‐0.84 to 0.43) |
| CBT carer | ‐0.44 (‐1.18 to 0.30)a | na | na | na | ‐0.37 (‐1.03 to 0.29)a | ‐0.21 (‐0.85 to 0.43)a | ‐ |
| aResults based on a single study | |||||||
For NMA estimates, there was no evidence of an effect for any therapy reducing externalising behaviour symptoms at six months relative to MAU. And for the pairwise comparisons, there was no evidence of an effect for any therapy reducing externalising behaviour symptoms at six months relative to MAU.
We gave a very low confidence rating to all the estimates as they all had major concerns in within‐study bias, imprecision and inconsistency.
12 months follow‐up
Figure 6 provides the graphical representation of this network. Direct evidence was available for eight comparisons coming from five studies. All NMA results are reported relative to MAU and the number of direct studies given in brackets. Where the number of direct studies is zero, the estimate is based on indirect evidence from the NMA. The full set of pairwise and network meta‐analyses is summarised in Table 19 below.
6.
Network meta‐analysis for externalising behaviour at 12 months follow‐up
Abbreviations CBT carer: cognitive behavioural therapy delivered to the carer; CBT child: cognitive behavioural therapy delivered to the child; CBT dyad: cognitive behavioural therapy delivered to the carer and the child; CBT dyad higher: cognitive behavioural therapy delivered to the carer and the child at a higher dose; CCT dyad: child centred therapy delivered to the carer and the child; MAU: management as usual.
Table 19 Pairwise and network meta‐analyses results (SMD and 95% CI) for externalising at six months follow‐up
| MAU | CCT dyad | CBT dyad higher | CBT dyad | CBT child | CBT carer | |
| MAU | ‐ | ‐0.05 (‐0.90 to 0.80) | 0.10 (‐0.77 to 0.96) | ‐0.08 (‐0.85 to 0.69) | ‐0.14 (‐0.89 to 0.62) | ‐0.34 (‐1.11 to 0.43) |
| CCT dyad | na | ‐ | 0.15 (‐0.39 to 0.69) | ‐0.02 (‐0.39 to 0.34) | ‐0.08 (‐0.86 to 0.69) | ‐0.29 (‐1.08 to 0.50) |
| CBT dyad higher | na | na | ‐ | ‐0.17 (‐0.57 to 0.22) | ‐0.24 (‐1.02 to 0.55) | ‐0.44 (‐1.24 to 0.36) |
| CBT dyad | ‐0.06 (‐0.79 to 0.67)a | ‐0.04 (‐0.36 to 0.28) | ‐0.17 (‐0.49 to 0.14)a | ‐ | ‐0.06 (‐0.74 to 0.62) | ‐0.26 (‐0.96 to 0.43) |
| CBT child | ‐0.13 (‐0.85 to 0.59)a | na | na | ‐0.27 (‐0.93 to 0.39)a | ‐ | ‐0.20 (‐0.89 to 0.48) |
| CBT carer | ‐0.32 (‐1.05 to 0.42)a | na | na | ‐0.27 (‐0.93 to 0.39)a | ‐0.25 (‐0.89 to 0.39)a | ‐ |
| aResults based on a single study | ||||||
Compared to MAU, there was no evidence of an effect for any therapy reducing externalising behaviour symptoms at 12 months follow‐up, either from the NMA or the pairwise meta‐analyses.
We gave a very low confidence rating to all the estimates of this analysis because they all had major concerns in within‐study bias, imprecision and inconsistency.
Social functioning
Post‐treatment
Four studies reported evidence for social functioning at post‐treatment (two comparisons, Analysis 2.15; Analysis 3.19 in Table 20 below). We were not able to perform an NMA due to the low number of studies.
2.15. Analysis.

Comparison 2: CBT dyad versus MAU, Outcome 15: Social functioning post‐treatment
3.19. Analysis.

Comparison 3: CBT dyad versus CCT dyad, Outcome 19: Social functioning post‐treatment
Table 20 Pairwise meta‐analyses results (SMD and 95% CI) for social functioning at post‐treatment
| Experimental | Control | No. of trials | RE or FE Ea | 95% CI | P value | I2 b | Participants | Trials | Link to analysis |
| CBT dyad | MAU | 1 | MD ‐1.10 | ‐3.26 to 1.06 | 0.32 | NA | 43 | Berliner 1996 | Analysis 2.15 |
| CBT dyad | CCT dyad | 3 | SMD ‐0.25 | ‐0.47 to ‐0.04 | 0.02 | 0% | 325 | Cohen 1996; Cohen 1998; Cohen 2004 | Analysis 3.19 |
| aRandom‐effects (more than one trial) or fixed‐effect (one trial) estimates. bAn I2 from a meta‐analysis of less than seven studies has low power and precision to detect heterogeneity (Higgins 2021a). | |||||||||
The estimate from the pairwise comparison from the standard meta‐analysis suggests no evidence to support a beneficial effect for CBT dyad reducing social functioning symptoms at post‐treatment relative to MAU (MD ‐1.10, 95% CI ‐3.26 to 1.06, 1 study).
There was weak evidence for CBT dyad having a beneficial effect in reducing social functioning symptoms at post‐treatment compared with CCT dyad (SMD ‐0.25, 95% CI ‐0.47 to ‐0.04, 3 studies). Tau² was 0.00, Chi² was 1.84 and I² was 0%, suggesting no heterogeneity between the three trials compared.
Six months follow‐up
Only two studies reported evidence for social functioning at six months follow‐up (one comparison, Analysis 3.20 in Table 21 below). We were not able to perform an NMA due to the low number of studies.
3.20. Analysis.

Comparison 3: CBT dyad versus CCT dyad, Outcome 20: Social functioning 6 months
Table 21 Summary of the results for social functioning at six months follow‐up
| Experimental | Control | No. of trials | RE or FE Ea | 95% CI | P value | I2 b | Participants | Trials | Link to analysis |
| CBT dyad | CCT dyad | 2 | SMD ‐0.10 | ‐0.36 to 0.16 | 0.45 | NA | 224 | Cohen 1998; Cohen 2004 | Analysis 3.20 |
| aRandom‐effects (more than one trial) or fixed‐effect (one trial) estimates. bAn I2 from a meta‐analysis of less than seven studies has low power and precision to detect heterogeneity (Higgins 2021a). | |||||||||
The estimate from the pairwise comparison from the standard meta‐analysis suggests no evidence to support a beneficial effect for CBT dyad reducing social functioning symptoms at six months follow‐up relative to CCT dyad (SMD ‐0.10, 95% CI ‐0.36 to 0.16, 2 studies). In terms of heterogeneity, Tau² was 0.00, Chi² was 0.76 and I² was 0%, suggesting no heterogeneity was observed between the trials.
12 months follow‐up
Three studies reported evidence for social functioning at 12 months follow‐up (two comparisons, analyses Analysis 2.16; Analysis 3.21 in Table 22 below). We were unable to perform an NMA due to the low number of studies.
2.16. Analysis.

Comparison 2: CBT dyad versus MAU, Outcome 16: Social functioning 12 months
3.21. Analysis.

Comparison 3: CBT dyad versus CCT dyad, Outcome 21: Social functioning 12 months
Table 22 Summary of results for social functioning at 12 months follow‐up
| Experimental | Control | No. of trials | RE or FE Ea | 95% CI | P value | I2 b | Participants | Trials | Link to analysis |
| CBT dyad | MAU | 1 | MD ‐2.30 | ‐4.24 to ‐0.36 | 0.02 | NA | 43 | Berliner 1996 | Analysis 2.16 |
| CBT dyad | CCT dyad | 2 | SMD ‐0.16 | ‐0.42 to 0.10 | 0.24 | 0% | 228 | Cohen 1998; Cohen 2004 | Analysis 3.21 |
| aRandom‐effects (more than one trial) or fixed‐effect (one trial) estimates. bAn I2 from a meta‐analysis of less than seven studies has low power and precision to detect heterogeneity (Higgins 2021a). | |||||||||
The estimate from the standard meta‐analysis suggests very weak evidence of a beneficial effect of CBT dyad reducing social functioning symptoms at 12 months relative to CCT dyad (SMD ‐0.16, 95% CI ‐0.42 to 0.10, 2 studies). Tau² was 0.00, Chi² was 0.63 and I² was 0%, suggesting no heterogeneity between the trials compared.
There was evidence of a beneficial effect of CBT dyad relative to MAU (MD ‐2.30, 95% CI ‐4.24 to ‐0.36, 1 study).
Social functioning: attachment
None of the included studies reported on this outcome at any of the time points.
Secondary outcomes
Substance misuse
Post‐treatment
Only one study reported evidence for substance misuse at post‐treatment (one comparison, Analysis 6.11 in Table 23 below). We were unable to perform pairwise meta‐analysis or NMA.
6.11. Analysis.

Comparison 6: Family therapy versus MAU, Outcome 11: Substance misuse post‐treatment
Table 23 Summary of results for substance misuse at post‐treatment
| Experimental | Control | No. of trials | Fixed Effect | 95% CI | P value | I2 | Participants | Trials | Link to analysis |
| Family therapy | Management as usual | 1 | MD 2.20 | ‐0.96 to 5.36 | 0.17 | NA | 30 | Danielson 2012 | Analysis 6.11 |
The estimate suggests no evidence to support a beneficial effect for family therapy reducing substance misuse at post‐treatment relative to management as usual (MD 2.20, 95% CI ‐0.96 to 5.36, 1 study).
Six months follow‐up
Only one study reported evidence for substance misuse at six months follow‐up (one comparison, Analysis 6.12 in Table 24 below). We were unable to perform pairwise meta‐analysis or NMA.
6.12. Analysis.

Comparison 6: Family therapy versus MAU, Outcome 12: Substance misuse 6 months
Table 24 Summary of results for substance misuse at six months follow‐up
| Experimental | Control | No. of trials | Fixed Effect | 95% CI | P value | I2 | Participants | Trials | Link to analysis |
| Family therapy | Management as usual | 1 | MD 2.20 | ‐6.76 to 2.36 | 0.34 | NA | 30 | Danielson 2012 | Analysis 6.12 |
The estimate suggests no evidence to support a beneficial effect for family therapy reducing substance misuse at six months follow‐up relative to management as usual (MD 2.20, 95% CI ‐6.76 to 2.36, 1 study).
12 months follow‐up
None of the included studies reported on substance misuse at 12 months follow‐up.
Delinquency
None of the included studies examined this outcome.
Carer distress and efficacy: parent's belief of child
Post‐treatment
Only two studies reported evidence for parent's belief of child at post‐treatment (two comparisons,Analysis 2.17; Analysis 3.22 in Table 25 below). We were unable to perform pairwise meta‐analysis or NMA.
2.17. Analysis.

Comparison 2: CBT dyad versus MAU, Outcome 17: Parent's belief of child post‐treatment
3.22. Analysis.

Comparison 3: CBT dyad versus CCT dyad, Outcome 22: Parent's belief of child post‐treatment
Table 25 Summary of the results for parent's belief of child at post‐treatment
| Experimental | Control | No. of trials | Fixed Effect | 95% CI | P value | I2 | Participants | Trials | Link to analysis |
| CBT | Management as usual | 1 | MD 0.50 | ‐1.14 to 2.14 | 0.55 | NA | 32 | Cohen 1996 | Analysis 2.17 |
| CBT dyad | CCT dyad | 1 | MD 2.33 | 0.18 to 4.48 | 0.03 | NA | 179 | Cohen 2004 | Analysis 3.22 |
There is no evidence to support a beneficial effect for CBT dyad increasing parent’s belief of child at post‐treatment relative to management as usual (MD 0.50, 95% CI ‐1.14 to 2.14, 1 study). Heterogeneity assessments do not apply here, as there is only one study informing the comparison for this outcome.
Also, the evidence is uncertain to conclude a beneficial effect for CBT dyad increasing the parent’s belief of child at post‐treatment relative to CCT dyad (MD 2.33, 95% CI 0.18 to 4.48, 1 study).
Six months follow‐up
Only one study reported evidence for parent's belief of child at six months follow‐up (one comparison, Analysis 3.23 in Table 26 below). We were unable to perform pairwise meta‐analysis or NMA.
3.23. Analysis.

Comparison 3: CBT dyad versus CCT dyad, Outcome 23: Parent's belief of child 6 months
Table 26 Summary of the results for parent's belief of child at six months follow‐up
| Intervention | Control | No. of trials | Fixed Effect | 95% CI | P value | I2 | Participants | Trials | Link to analysis |
| CBT dyad | CCT dyad | 1 | MD 0.91 | ‐2.99 to 4.81 | 0.65 | NA | 143 | Cohen 2004 | Analysis 3.23 |
There is no evidence to support a beneficial effect for CBT dyad increasing parent’s belief of child at six months follow‐up relative to child centred therapy (MD 0.91, 95% CI ‐2.99 to 4.81, 1 study).
12 months follow‐up
Only one study reported evidence for parent's belief of child at 12 months follow‐up (one comparison, Analysis 3.24 in Table 27 below). We were unable to perform pairwise meta‐analysis or NMA.
3.24. Analysis.

Comparison 3: CBT dyad versus CCT dyad, Outcome 24: Parent's belief of child 12 months
Table 27 Summary of the results for parent's belief of child at 12 months follow‐up
| Experimental | Control | No. of trials | Fixed effect | 95% CI | P value | I2 | Participants | Trials | Link to analysis |
| CBT dyad | CCT dyad | 1 | MD ‐1.31 | ‐5.45 to 2.83 | 0.53 | NA | 148 | Cohen 2004 | Analysis 3.24 |
There is no evidence to support a beneficial effect for CBT dyad (MD 1.31, 95% CI ‐5.45 to 2.38, 1 study) increasing parent’s belief of child at 12 months follow‐up relative to child centred therapy
Carer distress and efficacy: parental attributions
Post‐treatment
Only three studies reported evidence for parenting skills at post‐treatment (seven comparisons, Analysis 2.18; Analysis 3.25; Analysis 4.12; Analysis 10.12 in Table 28 below). There were no studies reporting on parenting skills at six and 12 months follow‐up. We were unable to perform an NMA due to the low number of studies reporting on this outcome. A pairwise meta‐analysis was possible for the CBT dyad versus CCT dyad comparison only.
2.18. Analysis.

Comparison 2: CBT dyad versus MAU, Outcome 18: Parenting skills post‐treatment
3.25. Analysis.

Comparison 3: CBT dyad versus CCT dyad, Outcome 25: Parenting skills post‐treatment
4.12. Analysis.

Comparison 4: CBT child versus CBT dyad, Outcome 12: Parenting skills post‐treatment
10.12. Analysis.

Comparison 10: CBT carer versus CBT dyad, Outcome 12: Parenting skills post‐treatment
Table 28 Summary of the results for parental attributions at post‐treatment
| Experimental | Control | No. of trials | RE or FE Ea | 95% CI | P value | I2 b | Participants | Trials | Link to analysis |
| CBT dyad | MAU | 1 | MD 1.96 | 6.09 to 10.01 | 0.63 | NA | 43 | Deblinger 1996b | Analysis 2.18 |
| CBT carer | CBT dyad | 1 | MD 5.78 | ‐2.19 to 13.75 | 0.16 | NA | 44 | Deblinger 1996b | Analysis 10.12 |
| CBT child | CBT dyad | 1 | MD ‐0.99 | ‐8.43 to 6.45 | 0.79 | NA | 46 | Deblinger 1996b | Analysis 4.12 |
| CBT dyad | CCT dyad | 2 | SMD 0.32 | 0.05 to 0.59 | 0.02 | 0% | 212 | Cohen 2004; Deblinger 2001 | Analysis 3.25 |
| aRandom‐effects (more than one trial) or fixed‐effect (one trial) estimates. bAn I2 from a meta‐analysis of less than seven studies has low power and precision to detect heterogeneity (Higgins 2021a). | |||||||||
There was no evidence that any modality of CBT reduced parental attributions symptoms at post‐treatment compared to MAU or CCT dyad.
Carer distress and efficacy: parent's emotional reaction
Post‐treatment
Two studies reported evidence for parent's emotional reaction at post‐treatment (one comparison, Analysis 3.26 in Table 29 below). We were unable to perform an NMA.
3.26. Analysis.

Comparison 3: CBT dyad versus CCT dyad, Outcome 26: Parent's emotional reaction post‐treatment
Table 29 Summary of the results for parent's emotional reaction at post‐treatment
| Experimental | Control | No. of trials | Random effect | 95% CI | P value | I2 a | Participants | Trials | Link to analysis |
| CBT dyad | CCT dyad | 2 | SMD ‐6.95 | ‐10.11 to ‐3.80 | 0.0001 | 0% | 223 | Cohen 2004; Deblinger 2001 | Analysis 3.26 |
| aAn I2 from a meta‐analysis of less than seven studies has low power and precision to detect heterogeneity (Higgins 2021a). | |||||||||
There was uncertain evidence from a single study for CBT dyad reducing parent's emotional reaction at post‐treatment compared to CCT dyad. The Chi2 was 0.11 and the I2 was 0%, suggesting no evidence of heterogeneity between the two studies.
Six months follow‐up
Only one study reported evidence for parent's emotional reaction at six months follow‐up (one comparison, Analysis 3.27 in Table 30 below). We were unable to perform an NMA or pairwise meta‐analysis.
3.27. Analysis.

Comparison 3: CBT dyad versus CCT dyad, Outcome 27: Parent's emotional reaction 6 months
Table 30 Summary of the results for parent's emotional reaction at six months follow‐up
| Intervention | Control | No. of trials | Fixed Effect | 95% CI | P value | I2 | Participants | Trials | Link to analysis |
| CBT dyad | CCT dyad | 1 | MD ‐3.93 | ‐7.88 to 0.02 | 0.05 | NA | 143 | Cohen 2004 | Analysis 3.27 |
There was weak evidence, from a single study, that CBT dyad reduced parents' emotional reaction at six months follow‐up compared with CCT dyad.
12 months follow‐up
Only one study reported evidence for parent's emotional reaction at 12 months follow‐up (one comparison, Analysis 3.28 in Table 31 below). We were unable to perform an NMA or pairwise meta‐analysis.
3.28. Analysis.

Comparison 3: CBT dyad versus CCT dyad, Outcome 28: Parent's emotional reactions 12 months
Table 31 Summary of the results for parent's emotional reaction at 12 months follow‐up
| Intervention | Control | No. of trials | Fixed effect | 95% CI | P value | I2 | Participants | Trials | Link to analysis |
| CBT dyad | CCT dyad | 1 | MD ‐4.56 | ‐8.37 to ‐0.75 | 0.02 | NA | 148 | Cohen 2004 | Analysis 3.28 |
There was weak evidence, from a single study, for CBT dyad reducing parent's emotional reaction at 12 months follow‐up compared to CCT dyad.
Carer distress and efficacy: parent's acceptance
Post‐treatment
Only one study reported evidence for parent's acceptance at post‐treatment (one comparison, Analysis 1.4 in Table 32 below). There were no studies reporting on parent’s acceptance at six and 12 months follow‐up. We were unable to perform an NMA or pairwise meta‐analysis.
1.4. Analysis.

Comparison 1: CCT dyad vs waiting list, Outcome 4: Parent's acceptance post‐treatment
Table 32 Summary of the results for parent's acceptance at post‐treatment
| Experimental | Control | No. of trials | Fixed Effect | 95% CI | P value | I2 | Participants | Trials | Link to analysis |
| CCT dyad | Waiting list | 1 | MD 12.75 | 2.62 to 22.88 | 0.01 | NA | 31 | Costas 1999 | Analysis 1.4 |
There was some evidence for CCT dyad reducing parent's acceptance of symptoms compared to a waiting list. However, the effect estimate is uncertain and based on a very small sample size, from a single study.
Carer distress and efficacy: parent's stress
One study reported evidence for parent's stress at post‐treatment (one comparison, Analysis 1.5 in Table 33 below). There were no studies reporting on parent’s stress at six and 12 months follow‐up, and we were unable to perform an NMA or pairwise meta‐analysis.
1.5. Analysis.

Comparison 1: CCT dyad vs waiting list, Outcome 5: Parent's stress post‐treatment
Table 33 Summary of the results for parent's stress at post‐treatment
| Intervention | Control | No. of trials | Fixed Effect | 95% CI | P value | I2 | Participants | Trials | Link to analysis |
| CCT dyad | Waiting list | 1 | MD ‐14.36 | ‐37.35 to 8.63 | 0.22 | NA | 31 | Costas 1999 | Analysis 1.5 |
There was no evidence for CCT dyad reducing parent's stress symptoms compared to a waiting list.
Discussion
Summary of main results
The results of this review largely provide imprecise and uncertain evidence to suggest that the psychological interventions assessed in these studies outperformed management as usual in reducing the psychological impairment resulting from sexual abuse. This was the case for both pairwise comparisons and network meta‐analyses (NMA).
Even where there was some evidence of improvement, the effect estimates were very uncertain and imprecise. Therefore, we are unable to ascertain that any of the therapies are consistently superior to the others.
We ranked the therapies for each outcome, but the results of these rankings are not sufficiently reliable to draw strong conclusions about the effectiveness of the therapies, based as they are on underpowered networks with small, imprecise and non‐significant effect estimates.
Regarding the different modalities of cognitive behavioural therapy (CBT) explored in this review (at higher dose, delivered only to the child, delivered only to the carer or delivered to the child and the carer), none appeared to be better than the others, which may suggest that the changes occur irrespective of the dose of CBT and the involvement of the non‐offending carer in the treatment.
Of the five studies examining the impact of therapy on carer efficacy, there is no evidence that CBT or child centred therapy (CCT) was superior. Cognitive behavioural therapy appeared to be better than management as usual in relation to improving parents’ attributions of responsibility for the abuse and better than CCT in addressing parent’s adverse emotional reactions (feelings of anger, distress and embarrassment, resulting from discovering the abuse). However, CCT and management as usual outperformed CBT in relation to both parent’s belief of child (two studies) and parenting skills (three studies).
Important limitations of results
First, the confidence intervals (CI) of both the direct and indirect summary estimates were wide (difference between the lower and the upper limit > 0.33), included zero, and the effect estimates were small (standardised mean differences (SMD) < 0.5). This suggests that more information and precision is needed in order to make decisions about the relative merits of the interventions considered.
Second, our networks were underpowered due to the low number of studies informing them. None of the direct comparisons within the networks were informed by more than three studies and even these exceptional cases did not represent all the interventions equally. Cognitive behavioural therapy and CCT were the interventions more frequently explored.
Third, whilst the studies were broadly comparable in terms of the setting in which the interventions were delivered, the use of a manual to deliver the interventions, the training of the therapists who delivered the interventions, the number of sessions offered, and the duration of the treatments, there was considerable variability across the studies in terms of the age of the participants and the format in which the interventions were delivered (individual or group).
Overall completeness and applicability of evidence
The completeness and applicability of the available evidence is significantly limited in a number of respects. First, not all the psychological consequences associated with child sexual abuse (CSA) have been explored equally in the literature: post‐traumatic stress disorder (PTSD), depression, anxiety, sexualised behaviour, and internalising and externalising problems have more evidence than social competence, attachment, substance misuse, delinquency, resilience and carer’s efficacy. Thus, we have no evidence of effectiveness of the interventions for some of the outcomes at any of the time points.
In the 22 studies included in this review, most participants were white females, although eight studies did not report the ethnicity of the participants and in one study most participants were African‐American. All but one of the studies were conducted in high‐income countries, with 16 conducted in the USA. The age range of participants in the included studies was generally wide (i.e. two to eight years old) and authors rarely provided details on how the interventions were adjusted to account for developmental differences in participants. Such differences may influence the way in which the intervention is delivered, received and ultimately the changes that may result from it.
Evidence of the impact of these interventions in low‐ and middle‐income countries is scarce, and the evidence base for therapies other than CBT for children who have been sexually abused is relatively sparse. The extent to which the findings of this review can be applied to other settings, both geographical and non‐clinical, is unclear.
Quality of the evidence
We rated the degree of confidence in the evidence presented in the summary of findings tables as very low. The main factors undermining the quality of the evidence were that most studies were judged to be at high or unclear risk of bias, either because of no information being provided, or because the information available was unclear about random sequence generation, allocation concealment, blinding of participants and personnel, treatment fidelity monitoring, incomplete data handling and selective outcome reporting. Our analyses were underpowered due to the low number of studies; none of the direct comparisons of our networks were explored in more than three trials; the comparisons available over‐represented CBT and CCT and under‐represented family therapy, psychodynamic therapy and eye movement desensitisation and reprocessing (EMDR); and our direct and indirect effect estimates were small, imprecise and lacked statistical and clinical significance. Additionally, we were unable to test publication bias because there were not enough studies to do so, and we were unable to check whether estimates derived from indirect comparisons reflected the estimates derived from direct comparisons (consistency) because there were not enough direct comparisons for all the interventions explored.
Potential biases in the review process
We took a number of steps to minimise bias. We developed a protocol for this review (Caro 2019), which adhered to the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2021a), and which we published before embarking on the review. We conducted extensive searches of relevant databases and we did not use setting, language, type of publication, year of publication or missing data as reasons for excluding studies. Two review authors, working independently, selected trials for inclusion and extracted data; disagreements were resolved by discussion within the team. We requested additional information from the authors of included studies, when this was missing from reports. Lastly, we assessed risk of bias in all trials according to the recommendations provided in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2017).
The relatively small number of studies suggests that future studies may influence the findings, particularly if more, better designed studies of therapies other than CBT or CCT are conducted. Further, in this review, we could not obtain and incorporate into our numerical analyses data from five studies because:
the required data could not be derived or imputed, and we could not contact the authors (Dominguez 2001);
the required data could not be derived or imputed and although we were able to contact the authors, they were unable to provide the information requested (Monck 1994);
the outcomes reported were not the focus of this review (Perez 1987 and Thun 2003); and
we could not obtain endpoint scores at post‐treatment and one year follow‐up from the authors (Trowell 2002).
This is a potential source of bias undermining the completeness of the evidence because these studies, with the exception of Dominguez 2001, reported on some of the interventions for which there was little evidence available: family therapy and psychodynamic therapy.
This review is one of the components of the doctoral research of one of the authors (PC), which was funded by the Colombian Government and the University of Los Andes in Colombia. Neither of these parties intervened in the definition of the criteria to exclude or include studies in the review nor in the definition of the PICO (population, intervention, comparison, outcome) acronym.
Agreements and disagreements with other studies or reviews
Eight meta‐analyses have explored the effectiveness of psychotherapeutic interventions to ameliorate the psychological impairments that can result from CSA in people up to 18 years old (Corcoran 2008; Harvey 2010; Hetzel‐Riggin 2007; Macdonald 2012; Macdonald 2016; Reeker 1997; Sánchez‐Meca 2011; Trask 2011). To our knowledge, this is the first systematic review that seeks to evaluate the relative effectiveness of different psychological interventions, using network meta‐analysis.
Overall, our findings concur with those previous meta‐analyses. Reeker and colleagues did not report a 'top intervention', and neither did they find significant differences in the overall effect sizes by gender and age of the samples, by outcome and treatment approach, or the source of outcome data (child or parent) (Reeker 1997). The results from Hetzel‐Riggin 2007 suggested that psychological treatment is better than no treatment for the consequences of CSA and that specific treatments are better for specific outcomes. For example: play therapy appeared to be the best treatment for social functioning, CBT and CCT for behaviour problems, and family therapy appeared to be the best for psychological distress (Hetzel‐Riggin 2007). Corcoran and colleagues found small, non‐significant effects of interventions on the outcomes that they analysed and the treatments involving the carer were not superior to those not involving them (Corcoran 2008). Harvey 2010 concluded that CBT led to the largest improvements in PTSD, but did not find statistically significant differences on internalising, externalising, and sexualised behaviours. In Sánchez‐Meca 2011, CBT appeared to be the most effective treatment for sexualised behaviour, anxiety, depression and self‐esteem. Results from Trask and colleagues suggest that CBT outperformed management as usual and waiting list, with small to medium positive effects on PTSD, internalising and externalising problems (Trask 2011). Finally, Macdonald and colleagues found that CBT reached small‐to‐medium effects on depression, PTSD, and anxiety, but the evidence on sexualised and behaviour problems was inconclusive (Macdonald 2012).
The extent of comparability between this review and those conducted earlier, however, is limited by differences in the inclusion criteria adopted. We restricted included studies to RCTs, whilst, excepting Macdonald 2012, the previous reviews also included quasi‐experimental studies (Corcoran 2008; Macdonald 2016; Trask 2011) and observational studies (Harvey 2010; Hetzel‐Riggin 2007; Reeker 1997; Sánchez‐Meca 2011; Trask 2011). We decided to focus on randomised controlled trials in order to minimise possible biased estimates, as high variability across trials in terms of the study’s quality and design has been argued to lead to misleading conclusions and imprecise estimates (Garg 2008).
Authors' conclusions
Implications for practice.
The magnitude, uncertainty, and, in some cases, the lack of significance of our estimates do not allow us to ascertain whether one intervention is clearly more effective than the others. However, in reducing the symptoms of post‐traumatic stress disorder at post‐treatment relative to management as usual, there is a very weak and uncertain trend favouring CBT delivered only to the child and CCT delivered to child plus parent (CCT dyad). From the NMA and pairwise results, there was no evidence of the other explored therapies reducing depression, anxiety, sexualised behaviours, internalising and externalising problems, and carers' outcomes at post‐treatment, six months and 12 months follow‐up relative to management as usual.
The evidence base for the effectiveness of other psychotherapeutic interventions for sexually abused children and adolescents is limited, particularly in relation to psychodynamic therapy, family therapy and eye movement desensitisation and reprocessing.
The paucity of rigorous research on interventions other than CBT means that it is not currently possible to determine the relative effectiveness of the therapies used to treat children who have been sexually abused.
Implications for research.
Our results point to the need for the following.
More studies evaluating the effectiveness of those interventions currently used to treat the consequences of sexual abuse for children and young people, including studies comparing active treatments. In particular, trials are needed that evaluate the effectiveness of child centred therapy, psychodynamic therapy, eye movement desensitisation and reprocessing and family therapy.
More studies that explore the impact of therapy on a wider range of outcomes, including children's social functioning, attachment, substance misuse, delinquency, resilience and carer’s efficacy.
Studies that are sufficiently powered to discern treatment effects, that give due attention to design characteristics that minimise the risk of bias, and have better quality reporting.
More studies that are conducted by research teams independent of those developing and overseeing the delivery of treatments.
More studies conducted in low‐ and middle‐income countries and with a more diverse ethnic composition.
History
Protocol first published: Issue 6, 2019
Acknowledgements
Funding for this research has been provided by the University of Los Andes (Colombia) and the Colombian Administrative Department of Science and Technology.
We thank Cochrane Developmental, Psychosocial and Learning Problems for their advice and support.
Cochrane Developmental, Psychosocial and Learning Problems supported the authors in the development of this review.
The following people conducted the editorial process for this article.
Sign‐off Editor (final editorial decision): Toby J Lasserson, Cochrane Central Executive
Editor (provided editorial guidance to authors): Nuala Livingstone, Cochrane Evidence Production and Methods Directorate
Managing Editor (provided editorial guidance to authors, edited the article, conducted editorial policy checks): Joanne Duffield, Queen's University Belfast
Deputy Managing Editor (provided editorial guidance to authors, edited the article and supported editorial team): Sarah Davies, University of Bristol
Information specialist (supported the authors with the searches and provided editorial guidance): Margaret Anderson
Copy Editor (copy editing and production): Andrea Takeda (Cochrane Central Production Service)
Peer‐reviewers (provided comments and recommended an editorial decision): Dr John Carpenter, Emeritus Professor, School for Policy Studies, University of Bristol, UK (clinical/content review); Dr Donna Peach, University of Salford, UK (clinical/content review); Mbeh Sandrine Diribe, Cameroon (consumer review); Brian Duncan, USA (consumer review); and Theresa Moore, Cochrane Methods Support Unit, University of Bristol, UK (methods review).
Appendices
Appendix 1. Search strategies
Cochrane Central Register of Controlled Trials (CENTRAL) Strategy used up to March 2020.
1 MeSH descriptor: [Child Abuse, Sexual] explode all trees 2 (sex* near/3 (abuse* or assault* or trauma* or victimi*)):ti,ab 3 MeSH descriptor: [Incest] this term only 4 incest*:ti,ab 5 {or #1‐#4} 6 MeSH descriptor: [Infant] explode all trees 7 MeSH descriptor: [Child] explode all trees 8 MeSH descriptor: [Adolescent] this term only 9 MeSH descriptor: [Young Adult] this term only 10 (infant* or child* or baby or babies* or adolescen* or teen* or youth* or young next person* or young next people or young next adult* or pre next school* or preschool* or baby or babies):ti,ab 11 {or #6‐#10} 12 #5 and #11 13 MeSH descriptor: [Psychotherapy] explode all trees 14 MeSH descriptor: [Mind‐Body Therapies] explode all trees 15 (psycho next therap* or psychotherap*):ti,ab 16 (psychoanalytic* or psycho next analytic* or psychodynamic* or psycho next dynamic*):ti,ab 17 MeSH descriptor: [Cognitive Behavioral Therapy] explode all trees 18 ((cognitive next behav* or cognitive or cognition) near/3 (program* or intervention* or therap* or treatment*)):ti,ab 19 ‘CBT’:ti,ab 20 (counselling or counseling):ti,ab 21 (psychodrama or ‘acting out’ or ‘role play’):ti,ab 22 (meditation or mindfulness or ‘mind training’):ti,ab 23 (Relax* near/3 (training* or treatment* or therap*)):ti,ab 24 (multisystemic or multi next systemic):ti,ab 25 ((psychosocial or psycho next social or psycho NEXT education* or psychoeducation*) near/3 (intervention* or program* or support* or therap* or treatment*)):ti,ab 26 ((family or group or systemic* or multimodal* or multi‐modal*) near/3 (program* or intervention* or therap* or treatment*)):ti,ab 27 MeSH descriptor: [Mental Health] this term only 28 MeSH descriptor: [Cognitive Therapy] 1 tree(s) exploded [Search note: This MeSH term was replaced by Cognitive Behavioral Therapy in 2019 and was removed from subsequent searches] 29 (behav* near/3 (program* or intervention* or therap* or treatment*)):ti,ab 30 ((exposure or abreaction or desensitization) near/3 therap*):ti,ab 31 (‘Eye Movement Desensitization and Reprocessing’ or EMDR):ti,ab 32 ((existential or gestalt or humanistic or milieu or person‐centred or residential or process‐experiential or "transactional analysis" or "non‐directive therapies") near therap*):ti,ab 33 (therapeutic adj (alliance or relationship)):ti,ab 34 MeSH descriptor: [Feedback, Psychological] 2 tree(s) exploded 35 ((biofeedback or feedback or imagery) near/3 (intervention* or therap* or treatment* or train*)):ti,ab 36 (hypnosis or hypno next therapy or hypnotherapy or breathing next exercise*):ti,ab 37 MeSH descriptor: [Object Attachment] this term only 38 ((attachment or bond*) near/3 (infant* or child* or mother* or maternal* or father* or paternal* or parental*)):ti,ab 39 ((solution focus* or trauma* or talking) near/3 therap*):ti,ab 40 "dialectical behaviour therapy":ti,ab 41 "acceptance and commitment therapy":ti,ab 42 MeSH descriptor: [Sensory Art Therapies] 1 tree(s) exploded 43 ((art or creative or drama or music or narrative or play* or sensory) near/3 (program* or intervention* or therap*)):ti,ab 44 dramatherapy:ti,ab 45 "Third wave":ti,ab 46 {or #13‐#45} 47 #12 and #46
Cochrane Central Register of Controlled Trials (CENTRAL) Strategy used March 2020 onwards.
#1 MeSH descriptor: [Child Abuse] explode all trees #2 (sex* near/3 (abuse* or assault* or trauma* or victimi*)):ti,ab #3 MeSH descriptor: [Incest] this term only #4 incest*:ti,ab #5 {or #1‐#4} #6 MeSH descriptor: [Infant] explode all trees #7 MeSH descriptor: [Child] explode all trees #8 MeSH descriptor: [Adolescent] this term only #9 MeSH descriptor: [Young Adult] this term only #10 (infant* or child* or baby or babies* or adolescen* or teen* or youth* or young next person* or young next people or young next adult* or pre next school* or preschool* or baby or babies):ti,ab #11 {or #6‐#10} #12 #5 and #11 #13 MeSH descriptor: [Psychotherapy] explode all trees #14 MeSH descriptor: [Mind‐Body Therapies] explode all trees #15 (psycho next therap* or psychotherap*):ti,ab #16 (psychoanalytic* or psycho next analytic* or psychodynamic* or psycho next dynamic*):ti,ab #17 MeSH descriptor: [Cognitive Behavioral Therapy] explode all trees #18 (cognitive next behav* or cognitive or cognition) near/3 (program* or intervention* or therap* or treatment*):ti,ab #19 ‘CBT’:ti,ab #20 (counselling or counseling):ti,ab #21 (psychodrama or ‘acting out’ or ‘role play’):ti,ab #22 (meditation or mindfulness or ‘mind training’):ti,ab #23 (Relax* near/3 (training* or treatment* or therap*)):ti,ab #24 (multisystemic or multi next systemic):ti,ab #25 ((psychosocial or psycho next social or psycho NEXT education* or psychoeducation*) near/3 (intervention* or program* or support* or therap* or treatment*)):ti,ab #26 ((family or group or systemic* or multimodal* or multi‐modal*) near/3 (program* or intervention* or therap* or treatment*)):ti,ab #27 MeSH descriptor: [Mental Health] this term only #28 (behav* near/3 (program* or intervention* or therap* or treatment*)):ti,ab #29 ((exposure or abreaction or desensitization) near/3 therap*):ti,ab #30 (‘Eye Movement Desensitization and Reprocessing’ or EMDR):ti,ab #31 ((existential or gestalt or humanistic or milieu or person‐centred or residential or process‐experiential or "transactional analysis" or "non‐directive therapies") near therap*):ti,ab #32 (therapeutic next (alliance or relationship)):ti,ab #33 MeSH descriptor: [Feedback, Psychological] explode all trees #34 ((biofeedback or feedback or imagery) near/3 (intervention* or therap* or treatment* or train*)):ti,ab #35 (hypnosis or hypno next therapy or hypnotherapy or breathing next exercise*):ti,ab #36 MeSH descriptor: [Object Attachment] this term only #37 ((attachment or bond*) near/3 (infant* or child* or mother* or maternal* or father* or paternal* or parental*)):ti,ab #38 ((solution focus* or trauma* or talking) near/3 therap*):ti,ab #39 dialectical behaviour therapy:ti,ab #40 acceptance and commitment therapy:ti,ab #41 MeSH descriptor: [Sensory Art Therapies] explode all trees #42 ((art or creative or drama or music or narrative or play* or sensory) near/3 (program* or intervention* or therap*)):ti,ab #43 dramatherapy:ti,ab #44 Third wave:ti,ab #45 {or #13‐#44} #46 #12 and #45 in Trials
Medline Ovid
1 child abuse, sexual/ 2 (child$ adj5 sex$).tw,kf. 3 1 or 2 4 sex offenses/ 5 rape/ 6 incest/ 7 (sex$ adj5 abuse$).tw,kf. 8 (sex$ adj5 offen$).tw,kf. 9 (sex$ adj5 assault$).tw,kf. 10 (sex$ adj5 coerc$).tw,kf. 11 (sex$ adj5 exploit$).tw,kf. 12 (sex$ adj5 (in‐appropriate or inappropriate)).tw,kf. 13 (sex$ adj5 victim$).tw,kf. 14 (sex$ adj5 violen$).tw,kf. 15 (incest$ or rape$ or molest$).tw,kf. 16 or/4‐15 17 infant/ 18 exp Child/ 19 Adolescent/ 20 (baby or babies or boys or girls or infant$ or preschool$ or pre‐school$ or child$ or teen$ or adolescen$ or youth$ or young people$ or young person$).tw. 21 or/17‐20 22 16 and 21 23 3 or 22 24 exp psychotherapy/ 25 mind body therapies/ 26 (psycho$ therap$ or psychotherap$).tw,kf. 27 (psychoanalytic$ or psycho‐analytic$ or psychodynamic$ or psycho‐dynamic$).tw,kf. 28 Cognitive Behavioral Therapy/ 29 ((cognitive‐behav$ or cognitive or cognition) adj3 (approach$ or program$ or intervention$ or therap$ or treatment$)).tw,kf. 30 CBT.tw,kf. 31 counsel?ing.tw,kf. 32 (psychodrama or acting out or role play).tw,kf. 33 (meditat$ or mindfulness$ or mind training).tw,kf. 34 (Relax$ adj3 (training$ or treatment$ or therap$)).tw,kf. 35 (multisystemic or multi‐systemic).tw,kf. 36 ((psychosocial or psycho‐social or psychoeducation$ or psycho‐education$) adj3 (approach or intervention$ or program$ or support$ or therap$ or treatment$)).tw,kf. 37 ((family or group or systemic$ or multimodal$ or multi‐modal$) adj3 (program$ or intervention$ or therap$ or treatment$)).tw,kf. 38 exp Behavior Therapy/ 39 (behavio?r$ adj3 (approach$ or program$ or intervention$ or therap$ or treatment$)).tw,kf. 40 ((exposure or abreaction or desensitization) adj3 therap$).tw,kf. 41 ("Eye Movement Desensitization and Reprocessing" or EMDR).tw,kf. 42 ((existential or gestalt or humanistic or milieu or person‐centred or residential) adj therap$).tw,kf. 43 (therapeutic adj (alliance or relationship)).tw,kf. 44 Feedback, Psychological/ 45 ((biofeedback or feedback or imagery) adj3 (intervention$ or therap$ or treatment$ or train$)).tw,kf. 46 (hypnosis or hypno‐therapy or hypnotherapy or breathing exercise$).tw,kf. 47 object attachment/ 48 ((attachment or bond$) adj3 (infant$ or child$ or mother$ or maternal$ or father$ or paternal$ or parental$)).tw,kf. 49 ((solution focus$ or trauma$ or talking) adj3 therap$).tw,kf. 50 "dialectical behavio?r therapy".tw,kf. 51 "acceptance and commitment therapy".tw,kf. 52 sensory art therapies/ 53 ((art or drama or music or narrative or play$ or sensory) adj1 (program$ or intervention$ or therap$)).tw,kf. 54 Third wave.tw,kf. 55 or/24‐54 56 23 and 55 57 randomized controlled trial.pt. 58 controlled clinical trial.pt. 59 randomi#ed.ab. 60 placebo$.ab. 61 drug therapy.fs. 62 randomly.ab. 63 trial.ab. 64 groups.ab. 65 or/57‐64 66 exp animals/ not humans.sh. 67 65 not 66 68 56 and 67 [Annotation: Final search line March 2020] 69 (202003* or 202004* or 202005* or 202006* or 202007* or 202008* or 202009* or 202010* or 202011* or 202012*OR 2021* or 2022*).dt,ez,da. 70 68 and 69 [Annotation: Final search line November 2022]
Medline Ovid In‐Process & Other Non‐Indexed Citations. Strategy used up to March 2020.
1 child abuse, sexual/ 2 (child$ adj5 sex$).tw,kf. 3 1 or 2 4 sex offenses/ 5 rape/ 6 incest/ 7 (sex$ adj5 abuse$).tw,kf. 8 (sex$ adj5 offen$).tw,kf 9 (sex$ adj5 assault$).tw,kf. 10 (sex$ adj5 coerc$).tw,kf. 11 (sex$ adj5 exploit$).tw,kf. 12 (sex$ adj5 (in‐appropriate or inappropriate)).tw,kf. 13 (sex$ adj5 victim$).tw,kf. 14 (sex$ adj5 violen$).tw,kf. 15 (rape$ or molest$).tw,kf. 16 (incest$ or rape$ or molest$).tw,kf. 17 or/4‐16 18 infant/ 19 exp Child/ 20 Adolescent/ 21 (baby or babies or boys or girls or infant$ or preschool$ or pre‐school$ or child$ or teen$ or adolescen$ or youth$ or young people$ or young person$).tw. 22 or/18‐21 23 17 and 22 24 3 or 23 25 exp psychotherapy/ 26 mind body therapies/ 27 (psycho$ therap$ or psychotherap$).tw,kf. 28 (psychoanalytic$ or psycho‐analytic$ or psychodynamic$ or psycho‐dynamic$).tw,kf. 29 Cognitive Therapy/ 30 ((cognitive‐behav$ or cognitive or cognition) adj3 (approach$ or program$ or intervention$ or therap$ or treatment$)).tw,kf. 31 CBT.tw,kf. 32 counsel?ing.tw,kf. 33 (psychodrama or acting out or role play).tw,kf. 34 (meditat$ or mindfulness$ or mind training).tw,kf. 35 ((Relax$) adj3 (training$ or treatment$ or therap$)).tw,kf. 36 (multisystemic or multi‐systemic).tw,kf. 37 ((psychosocial or psycho‐social or psychoeducation$ or psycho‐education$) adj3 (approach or intervention$ or program$ or support$ or therap$ or treatment$)).tw,kf. 38 ((family or group or systemic$ or multimodal$ or multi‐modal$) adj3 (program$ or intervention$ or therap$ or treatment$)).tw,kf. 39 exp Behavior Therapy/ 40 ((behavio?r$) adj3 (approach$ or program$ or intervention$ or therap$ or treatment$)).tw,kf. 41 ((exposure or abreaction or desensitization) adj3 (therap$)).tw,kf. 42 ("Eye Movement Desensitization and Reprocessing" or EMDR).tw,kf. 43 ((existential or gestalt or humanistic or milieu or person‐centred or residential) adj therap$).tw. 44 ((therapeutic) adj (alliance or relationship)).tw,kf. 45 Feedback, Psychological/ 46 ((biofeedback or feedback or imagery) adj3 (intervention$ or therap$ or treatment$ or train$)).tw,kf. 47 (hypnosis or hypno‐therapy or hypnotherapy or breathing exercise$).tw. 48 object attachment/ 49 ((attachment or bond$) adj3 (infant$ or child$ or mother$ or maternal$ or father$ or paternal$ or parental$)).tw,kf. 50 ((solution focus$ or trauma$ or talking) adj3 (therap$)).tw,kf. 51 ("dialectical behaviour therapy").tw,kf. 52 ("acceptance and commitment therapy").tw,kf. 53 sensory art therapies/ 54 ((art or drama or music or narrative or play$ or sensory) adj1 (program$ or intervention$ or therap$)).tw,kf. 55 Third wave.tw,kf. 56 or/25‐55 57 24 and 56 58 randomized controlled trial.pt. 59 controlled clinical trial.pt. 60 randomi#ed.ab. 61 placebo$.ab. 62 drug therapy.fs. 63 randomly.ab. 64 trial.ab. 65 groups.ab. 66 or/58‐65 67 exp animals/ not humans.sh. 68 66 not 67 69 57 and 68
MEDLINE In‐Process & Other Non‐Indexed Citations Ovid. Strategy used March 2020 onwards.
1 (child$ adj5 sex$).tw,kf. 2 (sex$ adj5 abuse$).tw,kf. 3 (sex$ adj5 offen$).tw,kf. 4 (sex$ adj5 assault$).tw,kf. 5 (sex$ adj5 coerc$).tw,kf. 6 (sex$ adj5 exploit$).tw,kf. 7 (sex$ adj5 (in‐appropriate or inappropriate)).tw,kf. 8 (sex$ adj5 victim$).tw,kf. 9 (sex$ adj5 violen$).tw,kf. 10 (incest$ or rape$ or molest$).tw,kf. 11 or/2‐10 12 (baby or babies or boys or girls or infant$ or preschool$ or pre‐school$ or child$ or teen$ or adolescen$ or youth$ or young people$ or young person$).tw. 13 11 and 12 14 1 or 13 15 (psycho$ therap$ or psychotherap$).tw,kf. 16 (psychoanalytic$ or psycho‐analytic$ or psychodynamic$ or psycho‐dynamic$).tw,kf. 17 ((cognitive‐behav$ or cognitive or cognition) adj3 (approach$ or program$ or intervention$ or therap$ or treatment$)).tw,kf. 18 CBT.tw,kf. 19 counsel?ing.tw,kf. 20 (psychodrama or acting out or role play).tw,kf. 21 (meditat$ or mindfulness$ or mind training).tw,kf. 22 (Relax$ adj3 (training$ or treatment$ or therap$)).tw,kf. 23 (multisystemic or multi‐systemic).tw,kf. 24 ((psychosocial or psycho‐social or psychoeducation$ or psycho‐education$) adj3 (approach or intervention$ or program$ or support$ or therap$ or treatment$)).tw,kf. 25 ((family or group or systemic$ or multimodal$ or multi‐modal$) adj3 (program$ or intervention$ or therap$ or treatment$)).tw,kf. 26 (behavio?r$ adj3 (approach$ or program$ or intervention$ or therap$ or treatment$)).tw,kf. 27 ((exposure or abreaction or desensitization) adj3 therap$).tw,kf. 28 ("Eye Movement Desensitization and Reprocessing" or EMDR).tw,kf. 29 ((existential or gestalt or humanistic or milieu or person‐centred or residential) adj therap$).tw,kf. 30 (therapeutic adj (alliance or relationship)).tw,kf. 31 ((biofeedback or feedback or imagery) adj3 (intervention$ or therap$ or treatment$ or train$)).tw,kf. 32 (hypnosis or hypno‐therapy or hypnotherapy or breathing exercise$).tw,kf. 33 ((attachment or bond$) adj3 (infant$ or child$ or mother$ or maternal$ or father$ or paternal$ or parental$)).tw,kf. 34 ((solution focus$ or trauma$ or talking) adj3 therap$).tw,kf. 35 "dialectical behavio?r therapy".tw,kf. 36 "acceptance and commitment therapy".tw,kf. 37 ((art or drama or music or narrative or play$ or sensory) adj1 (program$ or intervention$ or therap$)).tw,kf. 38 Third wave.tw,kf. 39 or/15‐38 40 14 and 39 41 (random$ or trial$ or control$ or group$ or placebo$ or blind$ or prospectiv$ or longitudinal$ or meta‐analys$ or systematic review$).tw. 42 40 and 41
MEDLINE Epub Ahead of Print Ovid. Strategy used March 2020 onwards.
1 (child$ adj5 sex$).tw,kf. 2 (sex$ adj5 abuse$).tw,kf. 3 (sex$ adj5 offen$).tw,kf. 4 (sex$ adj5 assault$).tw,kf. 5 (sex$ adj5 coerc$).tw,kf. 6 (sex$ adj5 exploit$).tw,kf. 7 (sex$ adj5 (in‐appropriate or inappropriate)).tw,kf. 8 (sex$ adj5 victim$).tw,kf. 9 (sex$ adj5 violen$).tw,kf. 10 (incest$ or rape$ or molest$).tw,kf. 1 11 or/2‐10 12 (baby or babies or boys or girls or infant$ or preschool$ or pre‐school$ or child$ or teen$ or adolescen$ or youth$ or young people$ or young person$).tw. 13 11 and 12 14 1 or 13 15 (psycho$ therap$ or psychotherap$).tw,kf. 16 (psychoanalytic$ or psycho‐analytic$ or psychodynamic$ or psycho‐dynamic$).tw,kf. 17 ((cognitive‐behav$ or cognitive or cognition) adj3 (approach$ or program$ or intervention$ or therap$ or treatment$)).tw,kf. 18 CBT.tw,kf. 19 counsel?ing.tw,kf. 20 (psychodrama or acting out or role play).tw,kf. 21 (meditat$ or mindfulness$ or mind training).tw,kf. 22 (Relax$ adj3 (training$ or treatment$ or therap$)).tw,kf. 23 (multisystemic or multi‐systemic).tw,kf. 24 ((psychosocial or psycho‐social or psychoeducation$ or psycho‐education$) adj3 (approach or intervention$ or program$ or support$ or therap$ or treatment$)).tw,kf. 25 ((family or group or systemic$ or multimodal$ or multi‐modal$) adj3 (program$ or intervention$ or therap$ or treatment$)).tw,kf. 26 (behavio?r$ adj3 (approach$ or program$ or intervention$ or therap$ or treatment$)).tw,kf. 27 ((exposure or abreaction or desensitization) adj3 therap$).tw,kf. 28 ("Eye Movement Desensitization and Reprocessing" or EMDR).tw,kf. 29 ((existential or gestalt or humanistic or milieu or person‐centred or residential) adj therap$).tw,kf. 30 (therapeutic adj (alliance or relationship)).tw,kf. 31 ((biofeedback or feedback or imagery) adj3 (intervention$ or therap$ or treatment$ or train$)).tw,kf. 32 (hypnosis or hypno‐therapy or hypnotherapy or breathing exercise$).tw,kf. 33 ((attachment or bond$) adj3 (infant$ or child$ or mother$ or maternal$ or father$ or paternal$ or parental$)).tw,kf. 34 ((solution focus$ or trauma$ or talking) adj3 therap$).tw,kf. 35 "dialectical behavio?r therapy".tw,kf. 36 "acceptance and commitment therapy".tw,kf. 37 ((art or drama or music or narrative or play$ or sensory) adj1 (program$ or intervention$ or therap$)).tw,kf. 38 Third wave.tw,kf. 39 or/15‐38 40 14 and 39 41 (random$ or trial$ or control$ or group$ or placebo$ or blind$ or prospectiv$ or longitudinal$ or meta‐analys$ or systematic review$).tw. 42 40 and 41
Embase Ovid
1 child sexual abuse/ 2 (child$ adj5 sex$).tw. 3 1 or 2 4 sexual crime/ 5 rape/ 6 incest/ 7 (sex$ adj5 abuse$).tw,ti,ab,kw,hw. 8 (sex$ adj5 offen$).tw,ti,ab,kw,hw. 9 (sex$ adj5 assault$).tw,ti,ab,kw,hw. 10 (sex$ adj5 coerc$).tw,ti,ab,kw,hw. 11 (sex$ adj5 exploit$).tw,ti,ab,kw,hw. 12 (sex$ adj5 (in‐appropriate or inappropriate)).tw,ti,ab,kw,hw. 13 (sex$ adj5 victim$).tw,ti,ab,kw,hw. 14 (sex$ adj5 violen$).tw,ti,ab,kw,hw. 15 (incest$ or rape$ or molest$).tw,ti,ab,kw,hw. 16 or/4‐15 17 infant/ 18 exp child/ 19 adolescent/ 20 (baby or babies or boys or girls or infant$ or preschool$ or pre‐school$ or child$ or teen$ or adolescen$ or youth$ or young people$ or young person$).tw. 21 or/17‐20 22 16 and 21 23 3 or 22 24 exp psychotherapy/ or psychodynamic psychotherapy/ 25 "mind body therapies".tw,ti,ab,kw,hw. 26 (psycho$ therap$ or psychotherap$).tw,ti,ab,kw,hw. 27 (psychoanalytic$ or psycho‐analytic$ or psychodynamic$ or psycho‐dynamic$).tw,ti,ab,hw,kw. 28 cognitive therapy/ 29 ((cognitive‐behav$ or cognitive or cognition) adj3 (approach$ or program$ or intervention$ or therap$ or treatment$)).tw,ti,ab,kw,hw. 30 cognitive behavioral therapy/ 31 family therapy/ 32 "CBT".tw,ti,ab,hw,kw. 33 counsel?ing.tw,ti,ab,hw,kw. 34 (psychodrama or acting out or role play).tw,ti,ab,hw,kw. 35 (meditat$ or mindfulness$ or mind training).tw,ti,ab,kw,hw. 36 (Relax$ adj3 (training$ or treatment$ or therap$)).tw,ti,ab,hw,kw. 37 ((family or group or systemic$ or multimodal$ or multi‐modal$) adj3 (program$ or intervention$ or therap$ or treatment$)).tw,ab,ti,hw,kw. 38 exp Behavior Therapy/ 39 (behavio?r$ adj3 (approach$ or program$ or intervention$ or therap$ or treatment$)).tw,ti,ab,kw,hw. 40 ((exposure or abreaction or desensitization) adj3 therap$).tw,ti,ab,kw,hw. 41 ("Eye Movement Desensitization and Reprocessing" or EMDR).tw,ti,ab,kw,hw. 42 ((existential or gestalt or humanistic or milieu or person‐centred or residential) adj therap$).tw. 43 (therapeutic adj (alliance or relationship)).tw,ti,ab,hw,kw. 44 psychological feedback/ 45 ((biofeedback or feedback or imagery) adj3 (intervention$ or therap$ or treatment$ or train$)).tw,ti,ab,hw,kw. 46 (hypnosis or hypno‐therapy or hypnotherapy or breathing exercise$).tw. 47 "object attachment".tw,ti,ab,kw,hw. 48 ((attachment or bond$) adj3 (infant$ or child$ or mother$ or maternal$ or father$ or paternal$ or parental$)).tw. 49 ((solution focus$ or trauma$ or talking) adj3 therap$).tw,ti,ab,kw,hw. 50 "dialectical behavio?r therapy".tw,ti,ab,kw,hw. 51 "acceptance and commitment therapy".tw,ti,ab,hw,kw. 52 "sensory art therapies".tw,ti,ab,kw,hw. 53 art therapy/ 54 ((art or drama or music or narrative or play$ or sensory) adj1 (program$ or intervention$ or therap$)).tw,ti,ab,hw,kw. 55 "Third wave".tw,ti,ab,hw,kw. 56 or/24‐55 57 23 and 56 58 Randomized controlled trial/ 59 controlled clinical trial/ 60 Single blind procedure/ 61 Double blind procedure/ 62 Crossover procedure/ 63 (crossover or cross‐over).tw. 64 ((singl$ or doubl$ or tripl$ or trebl$) adj1 (blind$ or mask$)).tw. 65 Placebo/ 66 placebo.tw. 67 prospective.tw. 68 factorial$.tw. 69 random$.tw. 70 assign$.ab. 71 allocat$.tw. 72 volunteer$.ab. 73 or/58‐72 74 Animal experiment/ not (human experiment/ or human/) 75 73 not 74 76 57 and 75 [Annotation: Final search line March 2020] 77 limit 76 to yr="2020 ‐Current" [Annotation: Final search line November 2022]
Allied and Complementary Medicine Database (AMED) Ovid
1 Child abuse sexual/ 2 ((child$) adj5 (sex$)) 3 1 OR 2 4 Sex offenses/ 5 (sex$ adj5 abuse$).ti,ab,hw. 6 (sex$ adj5 offen$).ti,ab,hw. 7 (sex$ adj5 assault$).ti,ab,hw. 8 (sex$ adj5 coerc$).ti,ab,hw. 9 (sex$ adj5 exploit$).ti,ab,hw. 10 (sex$ adj5 (in‐appropriate or inappropriate)).ti,ab,hw. 11 (sex$ adj5 victim$).ti,ab,hw. 12 (sex$ adj5 violen$).ti,ab,hw. 13 (incest$ or rape$ or molest$).ti,ab,hw. 14 4 or 5 or 6 or 7 or 8 or 9 or 10 or 11 or 12 or 13 15 infant/ 16 exp Child/ 17 Adolescent/ 18 (baby or babies or boys or girls or infant$ or preschool$ or pre‐school$ or child$ or teen$ or adolescen$ or youth$ or young people$ or young person$).ti,ab,hw. 19 15 or 16 or 17 or 18 20 14 and 19 21 3 or 20 22 exp psychotherapy/ 23 ("mind body therapies").ti,ab,hw. 24 ("psycho$ therap$" or psychotherap$ or psychoanalytic$ or psycho‐analytic$ or psychodynamic$ or psycho‐dynamic$).ti,ab,hw. 25 Cognitive therapy/ 26 ((cognitive‐behav$ or cognitive or cognition) adj3 (approach$ or program$ or intervention$ or therap$ or treatment$)).ti,ab,hw. 27 ("CBT").ti,ab,hw. 28 counsel?ing.ti,ab,hw. 29 (psychodrama or "acting out" or "role play" or meditat$ or mindfulness$ or mind training).ti,ab,hw. 30 ((Relax$) adj3 (training$ or treatment$ or therap$)).ti,ab,hw. 31 (multisystemic or multi‐systemic).ti,ab,hw. 32 ((psychosocial or psycho‐social or psychoeducation$ or psycho‐education$) adj3 (approach or intervention$ or program$ or support$ or therap$ or treatment$)).ti,ab,hw. 33 ((family or group or systemic$ or multimodal$ or multi‐modal$) adj3 (program$ or intervention$ or therap$ or treatment$)).ti,ab,hw. 34 exp Behavior Therapy/ 35 ((behavio?r$) adj3 (approach$ or program$ or intervention$ or therap$ or treatment$)).ti,ab,hw. 36 ((exposure or abreaction or desensitization) adj3 (therap$)).ti,ab,hw. 37 ("Eye Movement Desensitization and Reprocessing" or EMDR).ti,ab,hw. 38 ((existential or gestalt or humanistic or milieu or person‐centred or residential) adj therap$).hw. 39 ((therapeutic) adj (alliance or relationship)).ti,ab,hw. 40 ("psychological feebback").ti,ab,hw. 41 ((biofeedback or feedback or imagery) adj3 (intervention$ or therap$ or treatment$ or train$)).ti,ab,hw. 42 Hypnosis/ 43 (hypno‐therapy or hypnotherapy or breathing exercise$).hw. 44 object attachment/ 45 ((attachment or bond$) adj3 (infant$ or child$ or mother$ or maternal$ or father$ or paternal$ or parental$)).ti,ab,hw. 46 ((solution focus$ or trauma$ or talking) adj3 (therap$)).ti,ab,hw. 47 ("dialectical behaviour therapy").ti,ab,hw. 48 ("acceptance and commitment therapy").ti,ab,hw. 49 sensory art therapies/ 50 ((art or drama or music or narrative or play$ or sensory) adj1 (program$ or intervention$ or therap$)).ti,ab,hw 51 ("third wave").ti,ab,hw. 52 22 or 23 or 24 or 25 or 26 or 27 or 28 or 29 or 30 or 31 or 32 or 33 or 34 or 35 or 36 or 37 or 38 or 39 or 40 or 41 or 41 or 42 or 43 or 44 or 45 or 46 or 47 or 48 or 49 or 50 or 51 53 21 AND 52 54 randomized controlled trial.pt. 55 controlled clinical trial.pt. 56 randomi#ed.ab. 57 placebo$.ab. 58 randomly.ab. 59 trial.ab. 60 groups.ab 61 (random$ or placebo$ or single blind$ or double blind$ or triple blind$).ti,ab. 62 54 or 55 or 56 or 56 or 57 or 59 or 60 or 61 63 53 and 62
APA PsycINFO Ovid
1 Child Abuse/ 2 (child$ adj5 sex$).tw. 3 or/1‐2 4 Sexual Abuse/ 5 Sex Offenses/ 6 (sex$ adj5 abuse$).tw. 7 (sex$ adj5 offen$).tw. 8 (sex$ adj5 assault$).tw. 9 (sex$ adj5 coerc$).tw. 10 (sex$ adj5 exploit$).tw. 11 (sex$ adj5 (in‐appropriate or inappropriate)).tw. 12 (sex$ adj5 victim$).tw. 13 (sex$ adj5 violen$).tw. 14 (incest$ or rape$ or molest$).tw. 15 or/4‐14 16 (baby or babies or boys or girls or infant$ or preschool$ or pre‐school$ or child$ or teen$ or adolescen$ or youth$ or young people$ or young person$).mp. 17 15 and 16 18 3 or 17 19 exp Psychotherapy/ 20 Mind Body Therapy/ 21 (psycho$ therap$ or psychotherap$).tw. 22 (psychoanalytic$ or psycho‐analytic$ or psychodynamic$ or psycho‐dynamic$).tw. 23 Cognitive Therapy/ 24 ((cognitive‐behav$ or cognitive or cognition) adj3 (approach$ or program$ or intervention$ or therap$ or treatment$)).tw. 25 CBT.tw. 26 counsel?ing.tw. 27 (psychodrama or acting out or role play).tw. 28 (meditat$ or mindfulness$ or mind training).tw. 29 (Relax$ adj3 (training$ or treatment$ or therap$)).tw. 30 (multisystemic or multi‐systemic).tw. 31 ((psychosocial or psycho‐social or psychoeducation$ or psycho‐education$) adj3 (approach or intervention$ or program$ or support$ or therap$ or treatment$)).tw. 32 ((family or group or systemic$ or multimodal$ or multi‐modal$) adj3 (program$ or intervention$ or therap$ or treatment$)).tw. 33 exp Behavior Therapy/ 34 (behavio?r$ adj3 (approach$ or program$ or intervention$ or therap$ or treatment$)).tw. 35 ((exposure or abreaction or desensitization) adj3 therap$).tw. 36 ("Eye Movement Desensitization and Reprocessing" or EMDR).tw. 37 ((existential or gestalt or humanistic or milieu or person‐centred or residential) adj therap$).tw. 38 (therapeutic adj (alliance or relationship)).tw. 39 psychological feedback.mp. 40 ((biofeedback or feedback or imagery) adj3 (intervention$ or therap$ or treatment$ or train$)).tw. 41 (hypnosis or hypno‐therapy or hypnotherapy or breathing exercise$).tw. 42 attachment behavior/ 43 ((attachment or bond$) adj3 (infant$ or child$ or mother$ or maternal$ or father$ or paternal$ or parental$)).tw. 44 ((solution focus$ or trauma$ or talking) adj3 therap$).tw. 45 "dialectical behavio?r therapy".tw. 46 "acceptance and commitment therapy".tw. 47 Art Therapy/ 48 ((art or drama or music or narrative or play$ or sensory) adj1 (program$ or intervention$ or therap$)).tw. 49 Third wave.tw. 50 or/19‐49 51 18 and 50 52 randomized controlled trials/ 53 clinical trials/ 54 treatment effectiveness evaluation/ 55 exp treatment outcomes/ 56 followup studies/ 57 longitudinal studies/ 58 Placebo/ 59 Experiment Controls/ 60 exp program evaluation/ 61 (randomis$ or randomiz$).tw. 62 (control$ adj (experiment$ or trial$)).tw. 63 (TAU or "treatment as usual" or "wait$ list").ab. 64 or/52‐63 65 exp animals/ 66 64 not 65 67 51 and 66 [Search note: Final line 2020] 68 limit 67 to up=20200330‐20221024 [Search note: Final line 2022]
Child Development and Adolescent Studies (CDAS) EBSCOhost
S1 (ZU "child sexual abuse") S2 TI ((child*) N5 (sex*)) OR AB ((child*) N5 (sex*)) S3 ((ZU "sex crimes")) S4 (ZU "rape") or ((ZU "incest")) S5 TI ((sex*) N5 (abuse* OR offen* OR assault* OR coerc* OR exploit* OR in‐appropriate OR inappropriate OR victim* OR violen* OR rape* OR molest* OR incest*)) OR AB ((sex)* N5 (abuse* OR offen* OR assault* OR coerc* OR exploit* OR in‐appropriate OR inappropriate OR victim* OR violen* OR rape* OR molest* OR incest*)) S6 S1 OR S2 OR) S3 OR S4 OR S5 S7 (ZU "children") or (ZU "infants") or (ZU "teenagers") S8 TI (infant* OR child* OR adolescent* OR babies OR boys OR girls or infant* OR preschool* OR pre‐school* OR child* or teen* or adolescen* OR youth* OR "young people*" OR "young person*") OR AB (infant* OR child* OR adolescent* OR babies OR boys OR girls or infant* OR preschool* OR pre‐school* OR child* or teen* or adolescen* OR youth* OR "young people*" OR "young person*") S9 S7 AND S8 S10 S6 AND S9 S11 (ZU "psychotherapy") S12 TI ("mind body therapies") OR AB ("mind body therapies") S13 TI ((psycho*) N1 (therap* or psychotherapy*)) OR AB ((psycho)* N1 (therap* or psychotherapy*)) S14 TI (psychoanalytic* or psycho‐analytic* or psychodynamic* or psycho‐dynamic*) OR AB (psychoanalytic* or psycho‐analytic* or psychodynamic* or psycho‐dynamic*) S15 (ZU "cognitive therapy*) S16 TI ((cognitive‐behav* or cognitive or cognition) N1 (approach* or program* or intervention* or therap* or treatment*)) OR AB ((cognitive‐behav* or cognitive or cognition) N1 (approach* or program* or intervention* or therap* or treatment*)) S17 ((ZU "cognitive therapy for children") OR (ZU "psychotherapy") or (ZU "psychotherapy") or (ZU "cognitive therapy") S18 ZU ("counseling")) S19 TI (psychodrama or "acting out" or "role play") OR AB (psychodrama* or "acting out" or "role play") S20 TI (meditat* or mindfulness* or "mind training") OR AB (meditat* or mindfulness* or "mind training") S21 TI ((relax*) N3 (training* or treatment* or therap*)) OR AB ((relax*) N3 (training* or treatment* or therap*)) S22 TI (multisystemic or multi‐systemic) OR AB (multisystemic or multi‐systemic) S23 TI ((psychosocial or psycho‐social or psychoeducation* or psycho‐education*) N3 (approach or intervention* or program* or support* or therap*or treatment*)) OR AB ((psychosocial or psycho‐social or psychoeducation* or psycho‐education*) N3 (approach or intervention* or program* or support* or therap*or treatment*)) S24 TI ((family or group or systemic* or multimodal* or multi‐modal*) N3 (program* or interventioin* or therap* or treatment*)) OR AB ((family or group or systemic* or multimodal* or multi‐modal*) N3 (program* or interventioin* or therap* or treatment*)) S25 (ZU "behavior therapy") or (ZU "behavior therapy for children") or (ZU "behavior therapy for teenagers") S26 TI ((behavior*) N3 (approach* or program* or intervention* or therap* or treatment*)) OR AB ((behavior*) N3 (approach* or program* or intervention* or therap* or treatment*)) S27 TI (exposure or abreaction or desensitization N3 therap*) OR AB (exposure or abreaction or desensitization N3 therap*) S28 TI ("Eye Movement Desensitization and Reprocessing" or EMDR) OR AB ("Eye Movement Desensitization and Reprocessing" or EMDR) S29 TI ("existential therap*" or "gestalt therap*" or "humanistic therap*" or "milieu therap*" or "person‐centred therap*" or "residential therap*") OR AB ("existential therap*" or "gestalt therap*" or "humanistic therap*" or "milieu therap*" or "person‐centred therap*" or "residential therap*") S30 TI ("therapeutic alliance" or "therapeutic relationship") or AB ("therapeutic alliance" or "therapeutic relationship") S31 TI ("psychological feedback") OR AB ("psychological feedback") S32 TI ((biofeedback or feedback or imagery) N3 (intervention* or therap* or treatment* or train*)) OR AB ((biofeedback or feedback or imagery) N3 (intervention* or therap* or treatment* or train*)) S33 TI (hypnosis or hypno‐therapy or hypnotherapy or "breathing exercise*") OR AB (hypnosis or hypno‐therapy or hypnotherapy or "breathing exercise*") S34 TI ("object attachment") OR AB ("object attachment") S35 TI ((attachment or bond*) N3 (infant* or child* or mother* or maternal* or father* or paternal* or parental*)) OR AB ((attachment or bond*) N3 (infant* or child* or mother* or maternal* or father* or paternal* or parental*)) S36 TI ((solution focus* or trauma* or talking) N3 (therap*)) OR AB ((solution focus* or trauma* or talking) N3 (therap*)) S37 TI ("dialectical behaviour therapy") OR AB ("dialectical behaviour therapy") S38 TI ("acceptance and commitment therapy") OR AB ("acceptance and commitment therapy") S39 (ZU "art therapy") S40 TI ("sensory art therap*") OR AB ("sensory art therap*") S41 TI ((art or drama or music or narrative or play* or sensory) N1 (program* or intervention* or therap*)) OR AB ((art or drama or music or narrative or play* or sensory) N1 (program* or intervention* or therap*)) S42 TI ("third wave") OR AB ("third wave") S43 S11 OR S12 OR S13 OR S14 OR S15 OR S16 OR S17 OR S18 OR S19 OR S20 OR S21 OR S22 OR S23 OR S24 OR S25 OR S26 OR S27 OR S28 OR S29 OR S30 OR S31 OR S32 OR S33 OR S34 OR S35 OR S36 OR S37 OR S38 OR S39 OR S40 OR S41 OR S42 S44 S10 AND S43 S45 (ZU "randomized controlled trials") S46 TI ("controlled clinical trial*") OR AB ("controlled clinical trial*") S47 TI (randomized) OR AB (randomized) S48 TI (placebo*) OR AB (placebo*) S49 (ZU "drug therapy") S50 TI (randomly) OR AB (randomly) S51 TI (trial) OR AB (trial) S52 S45 OR S46 OR S47 OR S48 OR S49 OR S50 OR S51 S53 S44 AND S52
CINAHL (Cumulative Index to Nursing & Allied Health) EBSCOhost
S1 MH "Child Abuse, Sexual" S2 TI((child*)N5(sex*)) OR AB((child*)N5(sex*)) S3 S1 OR S2 S4 (MH "Rape") OR (MH "incest") or TI(sexual offen*e*) OR AB (sexual offen*e*) S5 TI ((sex*) N5 (abuse* or offen* or assault* or coerc* or exploit* or in‐appropriate or inappropriate or violen* or victim* or molest*)) OR AB ((sex*) N5 (abuse* or offen* or assault* or coerc* or exploit* or in‐appropriate or inappropriate or violen* or molest*)) S6 S4 OR S5 S7 (MH "child") OR (MH "infant") S8 TI (adolescen* OR babies OR boys OR girls OR preschool* OR pre‐school* OR teen* OR youth* OR "young people*" OR "young person*") OR AB (adolescen* OR babies OR boys OR girls OR preschool* OR pre‐school* OR teen* OR youth* OR "young people*" OR "young person*") S9 S7 OR S8 S10 S6 AND S9 S11 S3 OR S10 S12 (MH "psychotherapy") OR (MH "psychotherapy, brief") OR (MH "Psychotherapy, Psychodynamic") OR (MH "Psychotherapy, Group") OR (MH "Cognitive therapy") OR (MH "counseling") OR (MH "mind body techniques") OR (MH "Behavior Therapy") OR (MH "Psychodrama") OR (MH "acting out") OR (MH "Role Playing") OR (MH "meditation") OR (MH "mindfulness") OR (MH "Family therapy") OR (MH "Eye Movement Desensitization and Reprogramming") OR (MH "Hypnosis") OR (MH "art therapy") S13 TI (psychoanalytic* or psycho‐analytic*) OR AB (psychoanalytic* or psycho‐analytic*) S14 TI (cognitive‐behav* or cognitive or cognition) N1 (approach* or program* or intervention* or therap* or treatment*)) OR AB ((cognitive‐behav* or cognitive or cognition) N1 (approach* or program* or intervention* or therap* or treatment*)) S15 TI ((relax*) N3 (training* or treatment* or therap*)) OR AB ((relax*) N3 (training* or treatment* or therap*)) S16 TI (multisystemic or multi‐systemic) OR AB (multisystemic or multi‐systemic) S17 TI ((psychosocial or psycho‐social or psychoeducation* or psycho‐education*) N3 (approach or intervention* or program* or support* or therap*or treatment*)) OR AB ((psychosocial or psycho‐social or psychoeducation* or psycho‐education*) N3 (approach or intervention* or program* or support* or therap*or treatment*)) S18 TI ((family or group or systemic* or multimodal* or multi‐modal*) N3 (program* or interventioin* or therap* or treatment*)) OR AB ((family or group or systemic* or multimodal* or multi‐modal*) N3 (program* or interventioin* or therap* or treatment*)) S19 TI ((behavior*) N3 (approach* or program* or intervention* or therap* or treatment*)) OR AB ((behavior*) N3 (approach* or program* or intervention* or therap* or treatment*)) S20 TI ((exposure or abreaction or desensitization) N3 (therap*)) OR AB ((exposure or abreaction or desensitization) N3 (therap*)) S21 TI (existential or gestalt or humanistic or milieu or person‐centred or residential N1 therap*) OR AB (existential or gestalt or humanistic or milieu or person‐centred or residential N1 therap*) S22 TI ("therapeutic alliance" or "therapeutic relationship") or AB ("therapeutic alliance" or "therapeutic relationship") S23 TI ("psychological feedback") OR AB ("psychological feedback") S24 TI ("psychological feedback") OR AB ("psychological feedback") S25 TI ((biofeedback or feedback or imagery) N3 (intervention* or therap* or treatment* or train*)) OR AB ((biofeedback or feedback or imagery) N3 (intervention* or therap* or treatment* or train*)) S26 TI (hypno‐therapy or hypnotherapy or "breathing exercise*") OR AB (hypno‐therapy or hypnotherapy or "breathing exercise*") S27 TI ("object attachment") OR AB ("object attachment") S28 TI ((attachment or bond*) N3 (infant* or child* or mother* or maternal* or father* or paternal* or parental*)) OR AB ((attachment or bond*) N3 (infant* or child* or mother* or maternal* or father* or paternal* or parental*)) S29 TI (solution focus* or trauma* or talking) N3 (therap*)) OR AB ((solution focus* or trauma* or talking) N3 (therap*)) S30 TI ("dialectical behavio*r therapy") OR AB ("dialectical behavio*r therapy") S31 TI ("acceptance and commitment therapy") OR AB ("acceptance and commitment therapy") S32 TI ("sensory art therap*") OR AB ("sensory art therap*") S33 TI ((art or drama or music or narrative or play* or sensory) N1 (program* or intervention* or therap*)) OR AB ((art or drama or music or narrative or play* or sensory) N1 (program* or intervention* or therap*)) S34 TI ("third wave") OR AB ("third wave") S35 S12 OR S13 OR S14 OR S15 OR S16 OR S17 OR S18 OR S19 OR S20 OR S21 OR S22 OR S23 OR S24 OR S25 OR S26 OR S27 OR S28 OR S29 OR S30 OR S31 OR S32 OR S33 OR S34 S36 S11 AND S35 S37 MH randomized controlled trials S38 MH double‐blind studies S39 MH single‐blind studies S40 MH random assignment S41 MH pretest‐posttest design S42 MH cluster sample S43 TI (randomised OR randomized) S44 AB (random*) S45 TI (trial)02 S46 MH (sample size) AND AB (assigned OR allocated OR control) S47 MH (placebos) S48 PT (randomized controlled trial) S49 AB (control W5 group) S50 MH (crossover design) OR MH (comparative studies) S51 AB (cluster W3 RCT)r S52 MH animals+ S53 MH (animal studies) S54 TI (animal model*) S55 S52 OR S53 OR S54 S56 MH (human) S57 S55 NOT S56 S58 S37 OR S38 OR S39 OR S40 OR S41 OR S42 OR S43 OR S44 OR S45 OR S46 OR S47 OR S48 OR S49 OR S50 OR S51 S59 S58 NOT S57 S60 S36 AND S59 [Search note: Final line 2020] S61 EM 20200301 ‐ S62 S60 AND S61[Search note:Final line 2022]
Cochrane Database of Systematic Reviews
#1 MeSH descriptor: [Child Abuse] explode all trees #2 (sex* near/3 (abuse* or assault* or trauma* or victimi*)):ti,ab #3 MeSH descriptor: [Incest] this term only #4 incest*:ti,ab #5 {or #1‐#4} #6 MeSH descriptor: [Infant] explode all trees #7 MeSH descriptor: [Child] explode all trees #8 MeSH descriptor: [Adolescent] this term only #9 MeSH descriptor: [Young Adult] this term only #10 (infant* or child* or baby or babies* or adolescen* or teen* or youth* or young next person* or young next people or young next adult* or pre next school* or preschool* or baby or babies):ti,ab #11 {or #6‐#10} #12 #5 and #11 #13 MeSH descriptor: [Psychotherapy] explode all trees #14 MeSH descriptor: [Mind‐Body Therapies] explode all trees #15 (psycho next therap* or psychotherap*):ti,ab #16 (psychoanalytic* or psycho next analytic* or psychodynamic* or psycho next dynamic*):ti,ab #17 MeSH descriptor: [Cognitive Behavioral Therapy] explode all trees [Annotation: Previously Cognitive Therapy/] #18 (cognitive next behav* or cognitive or cognition) near/3 (program* or intervention* or therap* or treatment*):ti,ab #19 ‘CBT’:ti,ab #20 (counselling or counseling):ti,ab #21 (psychodrama or ‘acting out’ or ‘role play’):ti,ab #22 (meditation or mindfulness or ‘mind training’):ti,ab #23 (Relax* near/3 (training* or treatment* or therap*)):ti,ab #24 (multisystemic or multi next systemic):ti,ab #25 ((psychosocial or psycho next social or psycho NEXT education* or psychoeducation*) near/3 (intervention* or program* or support* or therap* or treatment*)):ti,ab #26 ((family or group or systemic* or multimodal* or multi‐modal*) near/3 (program* or intervention* or therap* or treatment*)):ti,ab #27 MeSH descriptor: [Mental Health] this term only #28 (behav* near/3 (program* or intervention* or therap* or treatment*)):ti,ab #29 ((exposure or abreaction or desensitization) near/3 therap*):ti,ab #30 (‘Eye Movement Desensitization and Reprocessing’ or EMDR):ti,ab #31 ((existential or gestalt or humanistic or milieu or person‐centred or residential or process‐experiential or "transactional analysis" or "non‐directive therapies") near therap*):ti,ab #32 (therapeutic next (alliance or relationship)):ti,ab #33 MeSH descriptor: [Feedback, Psychological] explode all trees #34 ((biofeedback or feedback or imagery) near/3 (intervention* or therap* or treatment* or train*)):ti,ab #35 (hypnosis or hypno next therapy or hypnotherapy or breathing next exercise*):ti,ab #36 MeSH descriptor: [Object Attachment] this term only #37 ((attachment or bond*) near/3 (infant* or child* or mother* or maternal* or father* or paternal* or parental*)):ti,ab #38 ((solution focus* or trauma* or talking) near/3 therap*):ti,ab #39 dialectical behaviour therapy:ti,ab #40 acceptance and commitment therapy:ti,ab #41 MeSH descriptor: [Sensory Art Therapies] explode all trees #42 ((art or creative or drama or music or narrative or play* or sensory) near/3 (program* or intervention* or therap*)):ti,ab #43 dramatherapy:ti,ab #44 Third wave:ti,ab #45 {or #13‐#44} #46 #12 and #45 in Cochrane Reviews, Cochrane Protocols [Search note: Final line 2020] #47 #12 and #45 with Cochrane Library publication date Between Apr 2020 and Nov 2022, in Cochrane Reviews, Cochrane Protocols [Search note: Final line 2020]2
Web of Science databases (Science Citation Index (SCI); Social Science Citation Index (SSCI);Conference Proceedings Citation Index Science (CPCI‐S); Conference Proceedings Citation Index‐ Social Science & Humanities (CPCI‐SSH); SciELO ) Strategy used up to March 2020.
1 TS="child sexual abuse " 2 TS=rape 3 TS=incest 4 TS=((sex)* near/5 (abuse* or offen* or assault* or coerc* or exploit* or in‐appropriate or inappropriate or victim* or violen* or molest* or incest* or rape*)) 5 #4 or #3 or #2 6 TS=infant 7 TS=Adolescent 8 TS=(baby or babies or boys or girls or infant* or preschool* or pre‐school* or child* or teen* or adolescen* or youth* or "young people" or "young person") 9 #8 OR #7 OR #6 10 #9 AND #5 11 #10 OR #1 12 TS= psychotherapy 13 TS="mind body therapies" 14 TS=("psycho* therap*" or psychotherap*) 15 TS=(psychoanalytic* or psycho‐analytic* or psychodynamic* or psycho‐dynamic*) 16 TS=CBT 17 TS=counselling 18 TS=(psychodrama or "acting out" or "role play") 19 TS=(meditat* or mindfulness* or "mind training") 20 TS=((Relax*) near/5 (training* or treatment* or therap*)) 21 TS=(multisystemic or multi‐systemic) 22 TS=((psychosocial or psycho‐social or psychoeducation* or psycho‐education*) near/3 (approach or intervention* or program* or support* or therap* or treatment*)) 23 TS=((family or group or systemic* or multimodal* or multi‐modal*) NEAR/3 (program* or intervention* or therap* or treatment*)) 24 TS="behavior therapy" 25 TS=(behavior* or behaviour* near/3 (approach* or program* or intervention* or therap* or treatment*)) 26 TS=((exposure or abreaction or desensitization) NEAR/3 therap*) 27 TS=("Eye Movement Desensitization and Reprocessing" or EMDR) 28 TS=((existential or gestalt or humanistic or milieu or person‐centred or residential) near therap*) 29 TS=((existential or gestalt or humanistic or milieu or person‐centred or residential or process‐experiential or "transactional analysis" or non‐directive) NEAR/5 therap*) 30 TS=(therapeutic near (alliance or relationship)) 31 TS="psychological feedback" 32 TS=((biofeedback or feedback or imagery) near/3 (intervention* or therap* or treatment* or train*)) 33 TS=(hypnosis or hypno‐therapy or hypnotherapy or "breathing exercise*") 34 TS="object attachment" 35 TS=((attachment or bond*) near/3 (infant* or child* or mother* or maternal* or father* or paternal* or parental*)) 36 TS=(("solution focus*" or trauma* or talking) near/3 therap*) 37 TS="dialectical behaviour therapy" 38 TS="acceptance and commitment therapy" 39 TS="sensory art therapies" 40 TS=((art or drama or music or narrative or play* or sensory) near/1 (program* or intervention* or therap*)) 41 TS="Third wave" 42 #41 or #40 or #39 or #38 or #37 or #36 or #35 or #34 or #33 or #32 or #31 or #30 or #29 or #28 or #27 or #26 or #25 or #24 or #23 or #22 or #21 or #20 or #19 or #18 or #17 or #16 or #15 or #14 or #13 or #12 43 #42 AND #11 44 TS="randomized controlled trial" 45 TS="controlled clinical trial" 46 TS=randomi?ed 47 TS=(placebo* or random* or control* or group* or "single blind*" or "double blind*" or "triple blind*") 48 TS="drug therapy" 49 TS=randomly 50 TS=trial 51 TS=groups 52 #51 or #50 or #49 or #48 or #47 or #46 or #45 or #44 53 #52 AND #43
Web of Science databases (Science Citation Index (SCI); Social Science Citation Index (SSCI);nConference Proceedings Citation Index Science (CPCI‐S); Conference Proceedings Citation Index‐ Social Science & Humanities (CPCI‐SSH); SciELO ) Strategy used from March 2020 onwards.
22 #20 AND #21 Timespan: 2020‐03‐30 to 2022‐11‐02 (Index Date) #21 #1 AND #19 #20 TS=("child sexual abuse " ) OR (TS= (sex* near/5 (abuse* or offen* or assault* or coerc* or exploit* or in‐appropriate or inappropriate or victim* or violen* or molest*) or rape or incest*) ) AND (TS=(baby or babies or boys or girls or infant* or preschool* or pre‐school* or child* or teen* or adolescen* or youth* or "young people" or "young person")) #19 #2 OR #3 OR #4 OR #5 OR #6 OR #7 OR #8 OR #9 OR #10 OR #11 OR #12 OR #13 OR #14 OR #15 OR #16 OR #17 OR #18 #18 TS=(psychotherap* or "psycho* therap*" or psychoanalytic* or psycho‐analytic* or psychodynamic* or psycho‐dynamic*or "mind body therapies" ) #17 TS=(CBT or counsel*ing or psychodrama or "acting out" or "role play" or meditat* or mindfulness* or "mind training" or (Relax* near/5 (training* or treatment* or therap*)) ) #16 TS=(multisystemic or multi‐systemic or ((psychosocial or psycho‐social or psychoeducation* or psycho‐education*) near/3 (approach or intervention* or program* or support* or therap* or treatment*))) #15 TS=((family or group or systemic* or multimodal* or multi‐modal*) NEAR/3 (program* or intervention* or therap* or treatment*)) #14 TS=((behavior* or behaviour*) near/3 (approach* or program* or intervention* or therap* or treatment*)) #13 TS=((exposure or abreaction or desensitization) NEAR/3 therap*) #12 TS=("Eye Movement Desensitization and Reprocessing" or EMDR) #11 TS=((existential or gestalt or humanistic or milieu or person‐centred or residential or process‐experiential or "transactional analysis" or non‐directive) NEAR/5 therap*) #10 TS=(therapeutic near (alliance or relationship)) #9 TS="psychological feedback" #8 TS=((biofeedback or feedback or imagery) near/3 (intervention* or therap* or treatment* or train*)) #7 TS=(hypnosis or hypno‐therapy or hypnotherapy or "breathing exercise*") #6 TS=("object attachment" OR ((attachment or bond*) near/3 (infant* or child* or mother* or maternal* or father* or paternal* or parental*))) #5 TS=(("solution focus*" or trauma* or talking) near/3 therap*) #4 TS= ("dialectical behavio*r therapy" or "acceptance and commitment therapy" or "sensory art therapies" ) #3 TS= ((art or drama or music or narrative or play* or sensory) near/1 (program* or intervention* or therap*)) #2 TS="Third wave" #1 TS=(placebo* or random* or control* or group* or "single blind*" or "double blind*" or "triple blind* " or RCT or trial* or groups)
Educational Resources Information Center (ERIC)
S1 TI ("sexual abuse" OR rape OR incest OR molest*) OR AB ("sexual abuse" OR rape OR incest OR molest*) S2 TI ((sex*) N5 (abuse* OR offen* OR assault* OR coerc* OR exploit* OR in‐appropriate OR inappropriate OR victim* OR violen* OR molest*)) OR AB ((sex*) N5 (abuse* OR offen* OR assault* OR coerc* OR exploit* OR in‐appropriate OR inappropriate OR victim* OR violen* OR molest*)) S3 S1 OR S2 S4 TI (infant OR child OR adolescent OR baby OR babies OR boys OR girls or infant* OR preschool* OR pre‐school* OR child* or teen* or adolescen* OR youth* OR "young people*" OR "young person*") OR AB (infant OR child OR adolescent OR baby OR babies OR boys OR girls or infant* OR preschool* OR pre‐school* OR child* or teen* or adolescen* OR youth* OR "young people*" OR "young person*") S5 S3 AND S4 S6 TI (psychotherapy OR "mind body therapies" OR "psycho* therap*" OR psychotherap* OR psychoanalytic* OR psycho‐analytic* OR psychodynamic* OR psycho‐dynamic* OR "cognitive therapy" OR "sensory art therapies" OR "acceptance and commitment therapy" OR "dialectical behavior therapy" OR "Behavior Therapy") OR AB (psychotherapy OR "mind body therapies" OR "psycho* therap*" OR psychotherap* OR psychoanalytic* OR psycho‐analytic* OR psychodynamic* OR psycho‐dynamic* OR "cognitive therapy" OR "sensory art therapies" OR "acceptance and commitment therapy" OR "dialectical behavior therapy" OR "Behavior Therapy") S7 TI ((art OR drama OR music OR narrative OR play* OR sensory OR cognitive‐behav* OR cognitive OR cognition OR CBT OR counseling OR psychodrama OR "acting out" OR "role play" OR meditat* OR mindfulness* or "mind training" OR relax* OR multisystemic OR multi‐systemic OR psychosocial OR psycho‐social OR psychoeducation* OR psycho‐education* OR family OR group OR systemic* OR multimodal* OR multi‐modal* OR behavior OR exposure OR abreaction OR desensitization OR "eye movement desensitization and reprocessing" OR EMDR OR existential OR gestalp OR humanistic OR milieu OR person‐centred OR process‐experiential OR "transactional analysis" OR "non‐directive therap*" OR biofeedback OR feedback OR imagery OR hypnosis OR hypno‐therapy OR hypnotherapy OR "breathing exercise*" OR "object attachment" OR "solution focus*" OR trauma OR talking) N3 (approach* OR program* OR intervention* OR therap* OR treatment*)) S8 AB ((art OR drama OR music OR narrative OR play* OR sensory OR cognitive‐behav* OR cognitive OR cognition OR CBT OR counseling OR psychodrama OR "acting out" OR "role play" OR meditat* OR mindfulness* or "mind training" OR relax* OR multisystemic OR multi‐systemic OR psychosocial OR psycho‐social OR psychoeducation* OR psycho‐education* OR family OR group OR systemic* OR multimodal* OR multi‐modal* OR behavior OR exposure OR abreaction OR desensitization OR "eye movement desensitization and reprocessing" OR EMDR OR existential OR gestalp OR humanistic OR milieu OR person‐centred OR process‐experiential OR "transactional analysis" OR "non‐directive therap*" OR biofeedback OR feedback OR imagery OR hypnosis OR hypno‐therapy OR hypnotherapy OR "breathing exercise*" OR "object attachment" OR "solution focus*" OR trauma OR talking) N3 (approach* OR program* OR intervention* OR therap* OR treatment*) S9 S6 OR S7 OR S8 S10 S5 AND S9 S11 (ZU "randomized controlled trials") S12 TI (random* or trial* or experiment* or PROSPECTIVE* OR longitudinal or BLIND* or CONTROL*) OR AB (random* or trial* or experiment* or PROSPECTIVE* OR longitudinal or BLIND* or CONTROL*) S13 (ZU "evaluation research") OR (ZU "control groups) OR (ZU "experimental groups") OR (ZU "longitudinal studies") OR (ZU "followup studies") OR (ZU "program effectiveness") OR (ZU "program evaluation") S14 TI (randomised OR randomized OR placebo* OR randomly OR trial) OR AB (randomised OR randomized OR placebo* OR randomly OR trial) S15 S11 OR S12 OR S13 OR S14 S16 S10 AND S15
Health Technology Assessment Database (HTA; www.crd.york.ac.uk/CRDWeb)
MeSH DESCRIPTOR Child Abuse, Sexual EXPLODE ALL TREES\
Electronic Theses Online Service, The British Library (EThOS)
Any word: child sexual abuse.
Epistemonikos
(title:((title:(child sexual abuse) OR abstract:(child sexual abuse))) OR abstract:((title:(child sexual abuse) OR abstract:(child sexual abuse))))
ClinicalTrials.gov
All studies. Condition or disease: child sexual abuse Study type: interventional studies (clinical trials)
World Health Organization International Clinical Trials Registry Platform (WHO ICTRP)
"Child sexual abuse" Search for clinical trials in children No filters.
Appendix 2. Methods set out in our published protocol that were not applied in this first version of the review
| Method | Reasons for not performing it |
| Measures of treatment effect | Had we obtained binary outcomes, we would have used the odds ratios (OR) with 95% confidence intervals (CI). |
| Unit of analysis issues |
Cluster‐randomised trials Had we retrieved trials in which authors randomised groups rather than individuals, we would have proceeded as recommended in the Cochrane Handbook for Systematic Reviews of Interventions (chapter 23, section 23.1.3 Methods of analysis for cluster‐randomized trialsHiggins 2021b).
|
|
Cross‐over trials Had we found studies in which participants received the control and the intervention but in different order, we would have included these studies but would only have used the data from the first period. | |
| Dealing with missing data |
Continuous data Should we have collected individual patient data, we would have imputed missing continuous data using the last observation carried forward (LOCF) approach. |
| Investigation of heterogeneity and inconsistency |
Subgroup analysis We planned to perform subgroup and meta‐regression analyses with the following explanatory variables: children’s age, gender, and intensity of treatment (a combination of frequency × length). We could not perform them due to the low number of studies. At least 10 studies are needed per characteristic modelled for the investigation to produce useful findings (Higgins 2021a, Chapter 10, section 10.11.5). |
| Sensitivity analyses | We could not perform sensitivity analyses due to the low number of studies. At least 10 studies are needed for the results of the analyses to be meaningful. Had we enough studies, we would have assess the robustness of findings by performing the following reanalyses: reanalysis using a fixed‐effect model, reanalysis without imputing data, reanalysis restricting the analysis only to studies considered to be at low risk of selection and detection bias (i.e. adequate allocation sequence generation, adequate allocation concealment, blinding of assessor), reanalysis excluding group therapy studies, and reanalysis excluding studies in which a concomitant pharmacotherapy is allowed. |
Appendix 3. Domains of risk of bias
| Type of bias being assessed | Criteria for assigning judgements | |
| Selection bias | Random sequence generation (was the allocation sequence adequately generated?) | Where authors reported that the participants were randomly allocated but did not report details on random sequence generation or allocation concealment, we rated the study as being at unclear risk of bias. Where no information was reported about the participants' allocation, sequence generation and allocation concealment, we rated the study as being at high risk of bias. Where authors reported details on random allocation of the participants, random sequence generation and allocation concealment, we rated the studies as being at low risk of bias. |
| Allocation concealment (was allocation adequately concealed?) | ||
| Detection bias | Blinding of participants and personnel (was knowledge of the allocated intervention adequately prevented during the study?) | Where no information about blinding of personnel and participants was explicitly stated in the studies, we rated the studies as high risk of bias and explained that the information was not mentioned, and that blinding was unlikely to have been done. Where not enough details about blinding of personnel and participants were stated in the studies, we rated them as being at unclear risk of bias. Where the authors reported methods for blinding of personnel and participants, we rated them as being at low risk of bias. |
| Blinding of outcome assessors (was knowledge of the allocated intervention adequately prevented during the study?) | ||
| Performance bias | Therapist and researcher allegiance, treatment fidelity (was treatment fidelity adequately monitored?) | Where monitoring of fidelity was not reported by the authors, we rated the studies as being at high risk of performance bias. We rated the studies as being at unclear risk of bias when not enough information on the monitoring of fidelity was reported by the authors. And we rated the studies as being at low risk of bias when methods for monitoring fidelity were reported in detail by the authors. |
| Attrition bias | Incomplete outcome data (were incomplete outcome data adequately addressed?) | We rated the studies as at low risk of attrition bias when the outcomes were measured in all participants; the proportion of incomplete data was low (less than 5% missing outcome data); and when the authors of the trials performed sensitivity analyses to demonstrate that incomplete data did not influence the estimated intervention effect. We rated studies as being at unclear risk of bias when information on the outcomes messured, the proportion of incomplete data, and sensitivity analyses was not enough to make a judgement. We rated studies as being at high risk of bias when the outcomes measured in participants, the proportion of incomplete data and the sensitivity analyses were not reported by the authors at all. |
| Reporting bias | Selective outcome reporting (are reports of the study free of suggestion of selective outcome reporting?) | We rated the studies as being at unclear risk of bias of selective outcome reporting when the authors reported all outcomes measured but did not make any reference to a protocol or trial registration. We rated the studies as being at high risk of bias of selective outcome reporting when the authors did not report all the outcomes measured or did not made any reference to a protocol or trial registration. We rated the studies as being at low risk of bias when the authors reported all the outcomes measured and referred to a protocol or trial registration. |
| Other sources of bias | Was the study apparently free of other problems that could put it at a high risk of bias? | We rated the studies as being at low risk of bias when they seemed to be free of other problems that could put them at risk of bias. We rated the studies at high risk of bias when other sources of risk were evident and no methods to overcome them were reported. We rated the studies at unclear risk of bias when there was not any information to suggest potential biases. |
Appendix 4. Multiarmed trials
Deblinger 1996b is a four‐armed trial that compared: i) CBT for the child only versus ii) CBT for the non‐offending carer only versus iii) CBT delivered to the child and the carer versus iv) MAU. The comparisons made in this trial Informed the nodes: MAU dyad, CBT child, CBT carer and CBT dyad.
King 2000 is a three‐armed trial that compared: i) CBT for the child and carer versus ii) CBT for the child only versus iii) waiting list. The comparisons made in this trial informed the nodes: WL, CB child and CBT dyad.
Deblinger 2011 is a four‐armed trial that compared: i) CBT of eight weeks with trauma narrative versus ii) CBT of eight weeks without trauma narrative versus iii) CBT of 16 weeks with trauma narrative and iv) CBT of 16 weeks without trauma narrative. The four conditions were delivered to the child and carer. For the purposes of this review, we combined the two arms delivered in eight weeks in one arm and compared it with one arm resulting from the combination of the two arms delivered in 16 weeks. We included these comparisons as the nodes: CBT_dyad (for the intervention lasting 8 weeks) and CBT_dyad higher (for the intervention lasting 16 weeks). We did not differentiate the nodes by components of the interventions because it exceeds the scope of this review; which is focused by now only in the theoretical orientation informing the intervention and how each theory has greater or smaller effects. A components network meta‐analyses can be performed to explore the specific components of an intervention as suggested by Caldwell 2016, and this is a possibility that we do not rule out for a future version of this review.
Footnotes
CBT: cognitive behaviour therapy; CBT carer: cognitive behavioural therapy delivered to the carer only; CBT child: cognitive behavioural therapy delivered to the child only; CBT dyad: cognitive behavioural therapy delivered to the child and the carer; CBT dyad: a higher dose of cognitive behavioural therapy delivered to the child and the carer; MAU: Management as usual; MAU dyad: management as usual delivered to the child and the carer; WL: waiting list.
Appendix 5. Outcomes, instruments, reporters and studies
| Outcome | Timing of assessment | Instrument | Reporter | Study |
| Post‐traumatic stress disorder | Post‐treatment, assessed in 10 studies | Children's Impact of Traumatic Events Scale‐Revised (CITES‐R; Wolfe 1991) | Child self‐report | 1 study: Celano 1996 |
| Trauma Symptom Checklist for Children (TSCC; Briere 1996) | Child self‐report | 2 studies: Farkas 2008; Cohen 1998 | ||
| UCLA PTSD Index for DSM‐IV‐Adolescent & Caregiver versions (Steinberg 2004) | Child self‐report | 1 study: Danielson 2012 | ||
| Schedule for Affective Disrders and Schizophrenia for School‐Age Children‐Post‐traumatic Stress Disorder Scale (Kaufman 1997) | Interviewer | 2 studies: Deblinger 1996b; Deblinger 2001 | ||
| Child PTSD Symptom Scale–Interview (CPSS‐I; Gillihan 2013) | Interviewer | 1 study: Foa 2013 | ||
| Parent Report of Post‐traumatic Symptoms (PROPS; Greenwald 1999) | Caretaker | 1 study: Jaberghaderi 2004 | ||
| PTSD section of the ADIS, Child version (Silverman 1996) | Interviewer | 1 study: King 2000 | ||
| University of California– Los Angeles Post‐traumatic Stress Disorder Reaction Index (UCLA‐PTSDR I; Steinberg 2004) | Child self‐report | 1 study: O'Callaghan 2013 | ||
| 6 months follow‐up, assessed in 4 studies | Trauma Symptom Checklist for Children (TSCC; Briere 1996) ‐ PTSD subscale | Child self‐report | 1 study: Cohen 1998 | |
| UCLA PTSD Index for DSM‐IV‐Adolescent & Caregiver versions (Steinberg 2004) | Child self‐report | 1 study: Danielson 2012 | ||
| Schedule for Affective Disrders and Schizophrenia for School‐Age Children‐Post‐traumatic Stress Disorder Scale (Kaufman 1997) | Interviewer | 1 study: Deblinger 1996b | ||
| Child PTSD Symptom Scale–Interview (CPSS‐I; Gillihan 2013) | Interviewer | 1 study: Kaczkurkin 2016 in Foa 2013 | ||
| 12 months follow‐up, assessed in 4 studies | Trauma Symptom Checklist for Children (TSCC; Briere 1996) ‐ PTSD subscale | Child self‐report | 1 study: Cohen 1998 | |
| Schedule for Affective Disrders and Schizophrenia for School‐Age Children‐Post‐traumatic Stress Disorder Scale (Kaufman 1997) | Interviewer | 1 study: Deblinger 1996b | ||
| Child PTSD Symptom Scale–Interview (CPSS‐I; Gillihan 2013) | Interviewer | 1 study: Kaczkurkin 2016 in Foa 2013 | ||
| Kiddies SADS–E Section. Designed to Assess PTSD (Orvaschel 1989) | Children self‐report | 1 study: Trowell 2002 | ||
| Depression | Post‐treatment, assessed in 12 studies | Children’s Depression Inventory (CDI; Kovacs 1992) | Child self‐report | 9 studies: Berliner 1996; Burke 1988; Cohen 1998; Cohen 2004; Danielson 2012; Deblinger 1996b; Deblinger 2011; Foa 2013; King 2000 |
| Child self‐report Trauma Symptom Checklist for Children ‐ Depression subscale (Briere 1996) | Child self‐report | 1 study: Farkas 2008 | ||
| The African Youth Psychosocial Assessment Instrument (AYPA) (Betancourt 2009; Bolton 2007) | Child self‐report | 1 study: O'Callaghan 2013 | ||
| The Institute for Personality and Ability Testing Depression Scale (Buros 1965) | Child self‐report | 1 study: Baker 1985 | ||
| 6 months follow‐up, assessed in 5 studies | Children’s Depression Inventory (CDI; Kovacs 1992) | Child self‐report | 5 studies: Cohen 1998; Cohen 2004; Danielson 2012; Deblinger 1996b; Deblinger 2011 | |
| 12 months follow‐up, assessed in 5 studies | Children’s Depression Inventory (CDI; Kovacs 1992) | Child self‐report | 5 studies: Cohen 1998; Cohen 2004; Danielson 2012; Deblinger 1996b; Deblinger 2011 | |
| Anxiety | Post‐treatment, assessed in 11 studies | The Institute for Personality and Ability Testing Anxiety Scale (Buros 1965) | Child self‐report | 1 study: Baker 1985 |
| Revised Children's Manifest Anxiety Scale (RCMAS; Reynolds 1985) | Child self‐report | 3 studies: Berliner 1996; Burke 1988; King 2000 | ||
| Trauma Symptom Checklist for Children (TSCC; Briere 1996) | Child self‐report | 2 studies: Cohen 1998; Farkas 2008 | ||
| State‐Trait Anxiety Inventory for Children (STAIC; Spielberger 1973) ‐ State | Child self‐report | 2 studies: Cohen 2004; Deblinger 1996b | ||
| Multidimensional Anxiety Scale for Children (MASC; March 1997) | Child self‐report | 1 study: Deblinger 2011 | ||
| The African Youth Psychosocial Assessment Instrument (AYPA; O'Callaghan 2013) | Child self‐report | 1 study: O'Callaghan 2013 | ||
| Child Anxiety Scale (CAS; Gillis 1980) | Child self‐report | 1 study: Costas 1999 | ||
| 6 months follow‐up, assessed in 2 studies | Trauma Symptom Checklist for Children (TSCC; Briere 1996) | Child self‐report | 1 study: Cohen 1998 | |
| State‐Trait Anxiety Inventory for Children (STAIC; Spielberger 1973) ‐ State | Child self‐report | 1 study: Cohen 2004 | ||
| 12 months follow‐up, assessed in 1 study | Revised Children's Manifest Anxiety Scale (RCMAS; Reynolds 1985) | Child self‐report | 1 study: Berliner 1996 | |
| Sexualised behaviour | Post‐treatment, assessed in 7 studies | Child Sexual Behavior Inventory (CSBI; Friedrich 1997) | Caretaker | 6 studies: Berliner 1996; Cohen 1996; Cohen 1998; Cohen 2004; Deblinger 2001; Deblinger 2011 |
| Number of sexual partners (Danielson 2012) | Child self‐report | 1 study: Danielson 2012 | ||
| 6 months follow‐up, assessed in 4 studies | Child Sexual Behavior Inventory (CSBI; Friedrich 1997) | Caretaker | 3 studies: Cohen 1996; Cohen 1998; Deblinger 2011 | |
| Number of sexual partners (Danielson 2012) | Child self‐report | 1 study: Danielson 2012 | ||
| 12 months follow‐up, assessed in 4 studies | Child Sexual Behavior Inventory (CSBI; Friedrich 1997) | Caretaker | 4 studies: Berliner 1996; Cohen 1996; Cohen 1998; Deblinger 2011 | |
| Internalising behaviours | Post‐treatment, assessed in 10 studies | Child Behavior Checklist (CBCL; Achenbach 1991) | Caretaker | 9 studies: Berliner 1996; Celano 1996; Cohen 1998; Cohen 2004; Costas 1999; Deblinger 1996b; Deblinger 2011; Farkas 2008; King 2000 |
| Behavior Assessment System for Children (BASC; Reynolds 1998) | Child self‐report | 1 study: Danielson 2012 | ||
| 6 months follow‐up, assessed in 5 studies | Child Behavior Checklist (CBCL; Achenbach 1991) | Caretaker | 4 studies: Cohen 1996; Cohen 1998; Cohen 2004; Deblinger 2011 | |
| Behavior Assessment System for Children (BASC; Reynolds 1998) | Child self‐report | 1 study: Danielson 2012 | ||
| 12 months follow‐up, assessed in 5 studies | Child Behavior Checklist (CBCL; Achenbach 1991) | Caretaker | 5 studies: Berliner 1996; Cohen 1996; Cohen 1998; Cohen 2004; Deblinger 2011 | |
| Externalising behaviours | Post‐treatment, assessed in 11 studies | Child Behavior Checklist (CBCL; Achenbach 1991) | Caretaker | 11 studies: Berliner 1996; Celano 1996; Cohen 1996; Cohen 1998; Cohen 2004; Costas 1999; Danielson 2012; Deblinger 1996b; Deblinger 2011; Farkas 2008; King 2000 |
| 6 months follow‐up, assessed in 6 studies | Child Behavior Checklist (CBCL; Achenbach 1991) | Caretaker | 6 studies: Cohen 1996; Cohen 1998; Cohen 2004; Danielson 2012; Deblinger 1996b; Deblinger 2011 | |
| 12 months follow‐up, assessed in 5 studies | Child Behavior Checklist (CBCL; Achenbach 1991) | Caretaker | 5 studies: Cohen 1996; Cohen 1998; Cohen 2004; Deblinger 1996b; Deblinger 2011 | |
| Social competence | Post‐treatment, assessed in 4 studies | Child Behavior Checklist (CBCL; Achenbach 1991) | Caretaker | 4 studies: Berliner 1996; Cohen 1996; Cohen 1998; Cohen 2004 |
| 6 months follow‐up, assessed in 2 studies | Child Behavior Checklist (CBCL; Achenbach 1991) | Caretaker | 2 studies: Cohen 1998; Cohen 2004 | |
| 12 months follow‐up, assessed in 3 studies | Child Behavior Checklist (CBCL; Achenbach 1991) | Caretaker | 3 studies: Berliner 1996; Cohen 1998; Cohen 2004 | |
| Attachment | Post‐treatment | None of the included studies reported on this outcome at this time point | ‐ | ‐ |
| 6 months follow‐up | None of the included studies reported on this outcome at this time point | ‐ | ‐ | |
| 12 months follow‐up | None of the included studies reported on this outcome at this time point | ‐ | ‐ | |
| Substance misuse | Post‐treatment, assessed in 1 study | The Time Line Follow Back Interview (TLFB), a well‐established method of assessing SU (Sobell 1996) | Child self‐report | Used in 1 study: Danielson 2012 |
| 6 months follow‐up, assessed in 1 study | The Time Line Follow Back Interview (TLFB), a well‐established method of assessing SU (Sobell 1996) | Child self‐report | Used in 1 study: Danielson 2012 | |
| 12 months follow‐up | None of the included studies reported on this outcome at this time point | ‐ | ‐ | |
| Delinquency | Post‐treatment | None of the included studies reported on this outcome at this time point | ‐ | ‐ |
| 6 months follow‐up | None of the included studies reported on this outcome at this time point | ‐ | ‐ | |
| 12 months follow‐up | None of the included studies reported on this outcome at this time point | ‐ | ‐ | |
| Resilience | Post‐treatment | None of the included studies reported on this outcome at this time point | ‐ | ‐ |
| 6 months follow‐up | None of the included studies reported on this outcome at this time point | ‐ | ‐ | |
| 12 months follow‐up | None of the included studies reported on this outcome at this time point | ‐ | ‐ | |
| Parent's belief of child | Post‐treatment, assessed in 2 studies | The Parent Reaction to Incest Disclosure Scale (PRIDS; Everson 1989) | Clinician | 1 study: Celano 1996 |
| Parental Support Questionnaire (PSQ; Mannarino 1996) | Parent self‐report | 1 study: Cohen 2004 | ||
| 6 months follow‐up, assessed in 1 study | Parental Support Questionnaire (PSQ; Mannarino 1996) | Parent self‐report | 1 study: Cohen 2004 | |
| 12 months follow‐up, assessed in 1 study | Parental Support Questionnaire (PSQ; Mannarino 1996) | Parent self‐report | 1 study: Cohen 2004 | |
| Parental attributions | Post‐treatment, assessed in 1 study | The Parental Attribution Scale (PAS; Celano 1992). | Parent self‐report | 1 study: Celano 1996 |
| 6 months follow‐up | None of the included studies reported on this outcome at this time point | ‐ | ‐ | |
| 12 months follow‐up | None of the included studies reported on this outcome at this time point | ‐ | ‐ | |
| Parenting skills | Post‐treatment, assessed in 3 studies | Parenting Practices Questionnaire (PPQ; Strayhorn 1998) | Parent self‐report | 3 studies: Cohen 2004, Deblinger 1996b, Deblinger 2001 |
| 6 months follow‐up, assessed in 1 study | Parenting Practices Questionnaire (PPQ; Strayhorn 1998) | Parent self‐report | 1 study: Cohen 2004 | |
| 12 months follow‐up, assessed in 2 studies | Parenting Practices Questionnaire (PPQ; Strayhorn 1998) | Parent self‐report | 2 studies: Cohen 2004, Deblinger 1996b | |
| Parent's emotional reaction | Post‐treatment, assessed in 2 studies | Parent’s Emotional Reaction Questionnaire (PERQ; Mannarino 1996) | Parent self‐report | 2 studies: Cohen 2004, Deblinger 2001 |
| 6 months follow‐up, assessed in 1 study | Parent’s Emotional Reaction Questionnaire (PERQ; Mannarino 1996) | Parent self‐report | 1 study: Cohen 2004 | |
| 12 months follow‐up, assessed in 1 study | Parent’s Emotional Reaction Questionnaire (PERQ; Mannarino 1996) | Parent self‐report | 1 study: Cohen 2004 | |
| Parent's stress | Post‐treatment, assessed in 1 study | Parenting Stress Index (PSI; Abidin 1983) | Parent self‐report | 1 study: Costas 1999 |
| 6 months follow‐up | None of the included studies reported on this outcome at this time point | ‐ | ‐ | |
| 12 months follow‐up | None of the included studies reported on this outcome at this time point | ‐ | ‐ | |
| Parental acceptance | Post‐treatment, assessed in 1 study | Porter Parental Acceptance Scale (PPAS; Porter 1954) | Parent self‐report | 1 study: Costas 1999 |
| 6 months follow‐up | None of the included studies reported on this outcome at this time point | ‐ | ‐ | |
| 12 months follow‐up | None of the included studies reported on this outcome at this time point | ‐ | ‐ |
Appendix 6. Assessments that could and could not be performed
| Outcome and timing of assessment | NMA | Inconsistency tests | Publication bias | GRADE |
| Post‐traumatic stress disorder at post‐treatment | Yes | Yes | No | Yes |
| Post‐traumatic stress disorder at 6 months follow‐up | Yes | No | No | No |
| Post‐traumatic stress disorder at 12 months follow‐up | Yes | No | No | No |
| Depression at post‐treatment | Yes | Yes | No | Yes |
| Depression at 6 months follow‐up | Yes | No | No | No |
| Depression at 12 months follow‐up | Yes | No | No | No |
| Anxiety at post‐treatment | Yes | Yes | No | Yes |
| Anxiety at 6 months follow‐up | No | No | No | No |
| Anxiety at 12 months follow‐up | No | No | No | No |
| Sexualised behaviour at post‐treatment | Yes | No | No | Yes |
| Sexualised behaviour at 6 months follow‐up | No | No | No | No |
| Sexualised behaviour at 12 months follow‐up | Yes | No | No | No |
| Internalising behaviours at post‐treatment | Yes | Yes | No | Yes |
| Internalising behaviours at 6 months follow‐up | No | No | No | No |
| Internalising behaviours at 12 months follow‐up | No | No | No | No |
| Externalising behaviours at post‐treatment | Yes | Yes | No | Yes |
| Externalising behaviours at 6 months follow‐up | Yes | No | No | Yes |
| Externalising behaviours at 12 months follow‐up | Yes | No | No | Yes |
| Social competence at post‐treatment | No | No | No | No |
| Social competence at 6 months follow‐up | No | No | No | No |
| Social competence at 12 months follow‐up | No | No | No | No |
| Attachment at post‐treatment | No | No | No | No |
| Attachment at 6 months follow‐up | No | No | No | No |
| Attachment at 12 months follow‐up | No | No | No | No |
| Substance misuse at post‐treatment | No | No | No | No |
| Substance misuse at 6 months follow‐up | No | No | No | No |
| Substance misuse at 12 months follow‐up | No | No | No | No |
| Delinquency at post‐treatment | No | No | No | No |
| Delinquency at 6 months follow‐up | No | No | No | No |
| Delinquency at 12 months follow‐up | No | No | No | No |
| Resilience at post‐treatment | No | No | No | No |
| Resilience at 6 months follow‐up | No | No | No | No |
| Resilience at 12 months follow‐up | No | No | No | No |
| Parent's belief of child at post‐treatment | No | No | No | No |
| Parent's belief of child at 6 months follow‐up | No | No | No | No |
| Parent's belief of child at 12 months follow‐up | No | No | No | No |
| Parental attributions at post‐treatment | No | No | No | No |
| Parental attributions at 6 months follow‐up | No | No | No | No |
| Parental attributions at 12 months follow‐up | No | No | No | No |
| Parenting skills at post‐treatment | No | No | No | No |
| Parenting skills at 6 months follow‐up | No | No | No | No |
| Parenting skills at 12 months follow‐up | No | No | No | No |
| Parent's emotional reaction at post‐treatment | No | No | No | No |
| Parent's emotional reaction at 6 months follow‐up | No | No | No | No |
| Parent's emotional reaction at 12 months follow‐up | No | No | No | No |
| Parent's stress at post‐treatment | No | No | No | No |
| Parent's stress at 6 months follow‐up | No | No | No | No |
| Parent's stress 12 months follow‐up | No | No | No | No |
| Parental acceptance at post‐treatment | No | No | No | No |
| Parental acceptance at 6 months follow‐up | No | No | No | No |
| Parental acceptance at 12 months follow‐up | No | No | No | No |
|
Footnotes NMA: network meta‐analysis | ||||
We could not perform a network meta‐analysis for the following outcomes, due to the low number of studies and the lack of connectedness of the networks:
anxiety at 6 and 12 months follow‐up;
internalising behaviours at 6 and 12 months follow‐up; and
sexualised behaviour at 6 months follow‐up.
We did not perform analyses of global and local inconsistency in the networks of the following outcomes:
post‐traumatic stress disorder (PTSD) at 6 and 12 months follow‐up;
depression at 6 and 12 months follow‐up;
sexualised behaviour at 12 months follow‐up; and
externalising behaviours at 6 and 12 months follow‐up.
These networks consisted of two‐armed trials only or had closed loops formed by comparisons made within the same multi‐armed trial. Global inconsistency is unlikely in networks consisting of only two‐arm trials; and local inconsistency only arises when there are at least three separate sets of studies making different comparisons (closed loops) (Higgins 2012; Veroniki 2013).
We created rankings of therapies for each outcome, but these were based on underpowered networks, and on small, imprecise and non‐significant effect estimates. Therefore, although we decribe the results of the rankograms and the SUCRA (surface under the cumulative ranking curve) tables, we do not take these rankings' results into account when reporting the conclusions of the review.
Finally, we were unable to judge the certainty of the evidence with CINeMA (Confidence in Network Meta‐analysis) for the outcomes below because their networks were informed by too few studies. Networks informed by fewer than five studies do not allow the tool to calculate prediction intervals, without which the analysis of heterogeneity and inconsistency domains cannot be conducted and therefore the quality of evidence cannot be graded:
PTSD at 6 and 12 months follow‐up;
depression at 6 and 12 months follow‐up;
anxiety at 6 and 12 months follow‐up;
sexualised behaviour at 6 and 12 months follow‐up; and
internalising behaviours at 6 and 12 months follow‐up.
As above, these networks consisted of two‐armed trials only or had closed loops formed by comparisons made within the same multi‐armed trial. Global inconsistency is unlikely in networks consisting of only two‐arm trials; and local inconsistency only arises when there are at least three separate sets of studies making different comparisons (closed loops) (Higgins 2012; Veroniki 2013).
Data and analyses
Comparison 1. CCT dyad vs waiting list.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1.1 Anxiety post‐treatment | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 1.2 Internalising post‐treatment | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 1.3 Externalising post‐treatment | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 1.4 Parent's acceptance post‐treatment | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.5 Parent's stress post‐treatment | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected |
1.1. Analysis.

Comparison 1: CCT dyad vs waiting list, Outcome 1: Anxiety post‐treatment
1.2. Analysis.

Comparison 1: CCT dyad vs waiting list, Outcome 2: Internalising post‐treatment
1.3. Analysis.

Comparison 1: CCT dyad vs waiting list, Outcome 3: Externalising post‐treatment
Comparison 2. CBT dyad versus MAU.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 2.1 PTSD post‐treatment | 2 | 65 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.32 [‐1.36, 0.72] |
| 2.2 PTSD 6 months | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 2.3 PTSD 12 months | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 2.4 Depression post‐treatment | 2 | 86 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.33 [‐1.22, 0.57] |
| 2.5 Depression 6 months | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 2.6 Depression 12 months | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 2.7 Anxiety post‐treatment | 2 | 110 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.34 [‐1.02, 0.34] |
| 2.8 Sexualised behaviour post‐treatment | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 2.9 Sexualised behaviour 12 months | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 2.10 Internalising post‐treatment | 3 | 152 | Std. Mean Difference (IV, Random, 95% CI) | 0.16 [‐0.17, 0.48] |
| 2.11 Externalising post‐treatment | 3 | 137 | Std. Mean Difference (IV, Random, 95% CI) | 0.11 [‐0.39, 0.60] |
| 2.12 Externalising 12 months | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 2.13 Anxiety 12 months | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 2.14 Internalising behaviour 12 months | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 2.15 Social functioning post‐treatment | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 2.16 Social functioning 12 months | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 2.17 Parent's belief of child post‐treatment | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 2.18 Parenting skills post‐treatment | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 2.19 Parenting skills 6 months | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected |
2.1. Analysis.

Comparison 2: CBT dyad versus MAU, Outcome 1: PTSD post‐treatment
2.2. Analysis.

Comparison 2: CBT dyad versus MAU, Outcome 2: PTSD 6 months
2.3. Analysis.

Comparison 2: CBT dyad versus MAU, Outcome 3: PTSD 12 months
2.4. Analysis.

Comparison 2: CBT dyad versus MAU, Outcome 4: Depression post‐treatment
2.5. Analysis.

Comparison 2: CBT dyad versus MAU, Outcome 5: Depression 6 months
2.6. Analysis.

Comparison 2: CBT dyad versus MAU, Outcome 6: Depression 12 months
2.7. Analysis.

Comparison 2: CBT dyad versus MAU, Outcome 7: Anxiety post‐treatment
2.8. Analysis.

Comparison 2: CBT dyad versus MAU, Outcome 8: Sexualised behaviour post‐treatment
2.9. Analysis.

Comparison 2: CBT dyad versus MAU, Outcome 9: Sexualised behaviour 12 months
2.10. Analysis.

Comparison 2: CBT dyad versus MAU, Outcome 10: Internalising post‐treatment
2.11. Analysis.

Comparison 2: CBT dyad versus MAU, Outcome 11: Externalising post‐treatment
2.12. Analysis.

Comparison 2: CBT dyad versus MAU, Outcome 12: Externalising 12 months
2.19. Analysis.

Comparison 2: CBT dyad versus MAU, Outcome 19: Parenting skills 6 months
Comparison 3. CBT dyad versus CCT dyad.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 3.1 PTSD post‐treatment | 2 | 262 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.40 [‐0.65, ‐0.16] |
| 3.2 PTSD 6 months | 2 | 200 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.46 [‐0.74, ‐0.17] |
| 3.3 PTSD 12 months | 2 | 235 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.33 [‐0.59, ‐0.07] |
| 3.4 Depression post‐treatment | 2 | 265 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.43 [‐0.68, ‐0.19] |
| 3.5 Depression 6 months | 2 | 233 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.27 [‐0.53, ‐0.01] |
| 3.6 Depression 12 months | 2 | 237 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.18 [‐0.44, 0.07] |
| 3.7 Anxiety post‐treatment | 2 | 265 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.25 [‐0.49, ‐0.01] |
| 3.8 Sexualised behaviour post‐treatment | 4 | 348 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.28 [‐0.49, ‐0.07] |
| 3.9 Sexualised behaviour 12 months | 2 | 125 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.41 [‐0.77, ‐0.05] |
| 3.10 Internalising post‐treatment | 3 | 304 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.40 [‐0.68, ‐0.12] |
| 3.11 Externalising post‐treatment | 3 | 304 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.13 [‐0.49, 0.22] |
| 3.12 Externalising 6 months | 3 | 267 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.07 [‐0.31, 0.17] |
| 3.13 Externalising 12 months | 3 | 271 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.04 [‐0.36, 0.28] |
| 3.14 Anxiety 6 months | 2 | 233 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.32 [‐0.58, ‐0.06] |
| 3.15 Anxiety 12 months | 2 | 194 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.20 [‐0.48, 0.09] |
| 3.16 Sexualised behaviour 6 months | 2 | 89 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.35 [‐0.86, 0.16] |
| 3.17 Internalising behaviour 6 months | 3 | 271 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.23 [‐0.47, 0.01] |
| 3.18 Internalising behaviour 12 months | 3 | 271 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.26 [‐0.50, ‐0.02] |
| 3.19 Social functioning post‐treatment | 3 | 328 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.25 [‐0.47, ‐0.04] |
| 3.20 Social functioning 6 months | 2 | 224 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.10 [‐0.36, 0.16] |
| 3.21 Social functioning 12 months | 2 | 228 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.16 [‐0.42, 0.10] |
| 3.22 Parent's belief of child post‐treatment | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 3.23 Parent's belief of child 6 months | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 3.24 Parent's belief of child 12 months | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 3.25 Parenting skills post‐treatment | 2 | 212 | Std. Mean Difference (IV, Random, 95% CI) | 0.32 [0.05, 0.59] |
| 3.26 Parent's emotional reaction post‐treatment | 2 | 223 | Mean Difference (IV, Fixed, 95% CI) | ‐6.95 [‐10.11, ‐3.80] |
| 3.27 Parent's emotional reaction 6 months | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 3.28 Parent's emotional reactions 12 months | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected |
3.1. Analysis.

Comparison 3: CBT dyad versus CCT dyad, Outcome 1: PTSD post‐treatment
3.2. Analysis.

Comparison 3: CBT dyad versus CCT dyad, Outcome 2: PTSD 6 months
3.3. Analysis.

Comparison 3: CBT dyad versus CCT dyad, Outcome 3: PTSD 12 months
3.4. Analysis.

Comparison 3: CBT dyad versus CCT dyad, Outcome 4: Depression post‐treatment
3.5. Analysis.

Comparison 3: CBT dyad versus CCT dyad, Outcome 5: Depression 6 months
3.6. Analysis.

Comparison 3: CBT dyad versus CCT dyad, Outcome 6: Depression 12 months
3.7. Analysis.

Comparison 3: CBT dyad versus CCT dyad, Outcome 7: Anxiety post‐treatment
3.8. Analysis.

Comparison 3: CBT dyad versus CCT dyad, Outcome 8: Sexualised behaviour post‐treatment
3.9. Analysis.

Comparison 3: CBT dyad versus CCT dyad, Outcome 9: Sexualised behaviour 12 months
3.10. Analysis.

Comparison 3: CBT dyad versus CCT dyad, Outcome 10: Internalising post‐treatment
3.11. Analysis.

Comparison 3: CBT dyad versus CCT dyad, Outcome 11: Externalising post‐treatment
3.12. Analysis.

Comparison 3: CBT dyad versus CCT dyad, Outcome 12: Externalising 6 months
3.13. Analysis.

Comparison 3: CBT dyad versus CCT dyad, Outcome 13: Externalising 12 months
Comparison 4. CBT child versus CBT dyad.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 4.1 PTSD post‐treatment | 2 | 58 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.00 [‐0.52, 0.52] |
| 4.2 PTSD 6 months | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 4.3 PTSD 12 months | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 4.4 Depression post‐treatment | 2 | 58 | Std. Mean Difference (IV, Random, 95% CI) | 0.07 [‐0.45, 0.58] |
| 4.5 Depression 6 months | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 4.6 Depression 12 months | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 4.7 Anxiety post‐treatment | 2 | 64 | Std. Mean Difference (IV, Random, 95% CI) | 0.37 [‐0.15, 0.88] |
| 4.8 Internalising post‐treatment | 2 | 64 | Std. Mean Difference (IV, Random, 95% CI) | 0.11 [‐0.67, 0.89] |
| 4.9 Externalising post‐treatment | 2 | 56 | Std. Mean Difference (IV, Random, 95% CI) | 0.23 [‐0.30, 0.76] |
| 4.10 Externalising 6 months | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 4.11 Externalising 12 months | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 4.12 Parenting skills post‐treatment | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 4.13 Parenting skills 6 months | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected |
4.1. Analysis.

Comparison 4: CBT child versus CBT dyad, Outcome 1: PTSD post‐treatment
4.2. Analysis.

Comparison 4: CBT child versus CBT dyad, Outcome 2: PTSD 6 months
4.3. Analysis.

Comparison 4: CBT child versus CBT dyad, Outcome 3: PTSD 12 months
4.4. Analysis.

Comparison 4: CBT child versus CBT dyad, Outcome 4: Depression post‐treatment
4.5. Analysis.

Comparison 4: CBT child versus CBT dyad, Outcome 5: Depression 6 months
4.6. Analysis.

Comparison 4: CBT child versus CBT dyad, Outcome 6: Depression 12 months
4.7. Analysis.

Comparison 4: CBT child versus CBT dyad, Outcome 7: Anxiety post‐treatment
4.8. Analysis.

Comparison 4: CBT child versus CBT dyad, Outcome 8: Internalising post‐treatment
4.9. Analysis.

Comparison 4: CBT child versus CBT dyad, Outcome 9: Externalising post‐treatment
4.10. Analysis.

Comparison 4: CBT child versus CBT dyad, Outcome 10: Externalising 6 months
4.11. Analysis.

Comparison 4: CBT child versus CBT dyad, Outcome 11: Externalising 12 months
4.13. Analysis.

Comparison 4: CBT child versus CBT dyad, Outcome 13: Parenting skills 6 months
Comparison 5. CBT child versus waiting list.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 5.1 PTSD post‐treatment | 2 | 71 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.59 [‐2.45, ‐0.72] |
| 5.2 Depression post‐treatment | 3 | 96 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.05 [‐2.43, 0.34] |
| 5.3 Anxiety post‐treatment | 3 | 96 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.24 [‐2.45, ‐0.04] |
| 5.4 Internalising post‐treatment | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 5.5 Externalising post‐treatment | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected |
5.1. Analysis.

Comparison 5: CBT child versus waiting list, Outcome 1: PTSD post‐treatment
5.2. Analysis.

Comparison 5: CBT child versus waiting list, Outcome 2: Depression post‐treatment
5.3. Analysis.

Comparison 5: CBT child versus waiting list, Outcome 3: Anxiety post‐treatment
5.4. Analysis.

Comparison 5: CBT child versus waiting list, Outcome 4: Internalising post‐treatment
5.5. Analysis.

Comparison 5: CBT child versus waiting list, Outcome 5: Externalising post‐treatment
Comparison 6. Family therapy versus MAU.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 6.1 PTSD post‐treatment | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 6.2 PTSD 6 months | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 6.3 Depression post‐treatment | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 6.4 Depression 6 months | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 6.5 Sexualised behaviour 6 months follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 6.6 Internalising post‐treatment | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 6.7 Externalising post‐treatment | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 6.8 Externalising 6 months | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 6.9 Sexualised behaviour 6 months | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 6.10 Internalising behaviour 6 months | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 6.11 Substance misuse post‐treatment | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 6.12 Substance misuse 6 months | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected |
6.1. Analysis.

Comparison 6: Family therapy versus MAU, Outcome 1: PTSD post‐treatment
6.2. Analysis.

Comparison 6: Family therapy versus MAU, Outcome 2: PTSD 6 months
6.3. Analysis.

Comparison 6: Family therapy versus MAU, Outcome 3: Depression post‐treatment
6.4. Analysis.

Comparison 6: Family therapy versus MAU, Outcome 4: Depression 6 months
6.5. Analysis.

Comparison 6: Family therapy versus MAU, Outcome 5: Sexualised behaviour 6 months follow‐up
6.6. Analysis.

Comparison 6: Family therapy versus MAU, Outcome 6: Internalising post‐treatment
6.7. Analysis.

Comparison 6: Family therapy versus MAU, Outcome 7: Externalising post‐treatment
6.8. Analysis.

Comparison 6: Family therapy versus MAU, Outcome 8: Externalising 6 months
Comparison 7. CBT carer versus MAU.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 7.1 PTSD post‐treatment | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 7.2 PTSD 6 months | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 7.3 PTSD 12 months | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 7.4 Depression post‐treatment | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 7.5 Depression 6 months | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 7.6 Depression 12 months | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 7.7 Anxiety post‐treatment | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 7.8 Internalisiing post‐treatment | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 7.9 Externalising post‐treatment | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 7.10 Externalising 6 months | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 7.11 Externalising 12 months | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected |
7.1. Analysis.

Comparison 7: CBT carer versus MAU, Outcome 1: PTSD post‐treatment
7.2. Analysis.

Comparison 7: CBT carer versus MAU, Outcome 2: PTSD 6 months
7.3. Analysis.

Comparison 7: CBT carer versus MAU, Outcome 3: PTSD 12 months
7.4. Analysis.

Comparison 7: CBT carer versus MAU, Outcome 4: Depression post‐treatment
7.5. Analysis.

Comparison 7: CBT carer versus MAU, Outcome 5: Depression 6 months
7.6. Analysis.

Comparison 7: CBT carer versus MAU, Outcome 6: Depression 12 months
7.7. Analysis.

Comparison 7: CBT carer versus MAU, Outcome 7: Anxiety post‐treatment
7.8. Analysis.

Comparison 7: CBT carer versus MAU, Outcome 8: Internalisiing post‐treatment
7.9. Analysis.

Comparison 7: CBT carer versus MAU, Outcome 9: Externalising post‐treatment
7.10. Analysis.

Comparison 7: CBT carer versus MAU, Outcome 10: Externalising 6 months
7.11. Analysis.

Comparison 7: CBT carer versus MAU, Outcome 11: Externalising 12 months
Comparison 8. CBT child versus MAU.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 8.1 PTSD post‐treatment | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 8.2 PTSD 6 months | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 8.3 PTSD 12 months | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 8.4 Depression post‐treatment | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 8.5 Depression 6 months | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 8.6 Depression 12 months | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 8.7 Anxiety post‐treatment | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 8.8 Internalising post‐treatment | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 8.9 Externalising post‐treatment | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 8.10 Externalising 6 months | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 8.11 Externalisiing 12 months | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected |
8.1. Analysis.

Comparison 8: CBT child versus MAU, Outcome 1: PTSD post‐treatment
8.2. Analysis.

Comparison 8: CBT child versus MAU, Outcome 2: PTSD 6 months
8.3. Analysis.

Comparison 8: CBT child versus MAU, Outcome 3: PTSD 12 months
8.4. Analysis.

Comparison 8: CBT child versus MAU, Outcome 4: Depression post‐treatment
8.5. Analysis.

Comparison 8: CBT child versus MAU, Outcome 5: Depression 6 months
8.6. Analysis.

Comparison 8: CBT child versus MAU, Outcome 6: Depression 12 months
8.7. Analysis.

Comparison 8: CBT child versus MAU, Outcome 7: Anxiety post‐treatment
8.8. Analysis.

Comparison 8: CBT child versus MAU, Outcome 8: Internalising post‐treatment
8.9. Analysis.

Comparison 8: CBT child versus MAU, Outcome 9: Externalising post‐treatment
8.10. Analysis.

Comparison 8: CBT child versus MAU, Outcome 10: Externalising 6 months
8.11. Analysis.

Comparison 8: CBT child versus MAU, Outcome 11: Externalisiing 12 months
Comparison 9. CBT carer versus CBT child.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 9.1 PTSD post‐treatment | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 9.2 PTSD 6 months | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 9.3 PTSD 12 months | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 9.4 Depression post‐treatment | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 9.5 Depression 6 months | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 9.6 Depression 12 months | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 9.7 Anxiety post‐treatment | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 9.8 Internalising post‐treatment | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 9.9 Externalising post‐treatment | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 9.10 Externalising 6 months | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 9.11 Externalising 12 months | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected |
9.1. Analysis.

Comparison 9: CBT carer versus CBT child, Outcome 1: PTSD post‐treatment
9.2. Analysis.

Comparison 9: CBT carer versus CBT child, Outcome 2: PTSD 6 months
9.3. Analysis.

Comparison 9: CBT carer versus CBT child, Outcome 3: PTSD 12 months
9.4. Analysis.

Comparison 9: CBT carer versus CBT child, Outcome 4: Depression post‐treatment
9.5. Analysis.

Comparison 9: CBT carer versus CBT child, Outcome 5: Depression 6 months
9.6. Analysis.

Comparison 9: CBT carer versus CBT child, Outcome 6: Depression 12 months
9.7. Analysis.

Comparison 9: CBT carer versus CBT child, Outcome 7: Anxiety post‐treatment
9.8. Analysis.

Comparison 9: CBT carer versus CBT child, Outcome 8: Internalising post‐treatment
9.9. Analysis.

Comparison 9: CBT carer versus CBT child, Outcome 9: Externalising post‐treatment
9.10. Analysis.

Comparison 9: CBT carer versus CBT child, Outcome 10: Externalising 6 months
9.11. Analysis.

Comparison 9: CBT carer versus CBT child, Outcome 11: Externalising 12 months
Comparison 10. CBT carer versus CBT dyad.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 10.1 PTSD post‐treatment | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 10.2 PTSD 6 months | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 10.3 PTSD 12 months | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 10.4 Depression post‐treatment | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 10.5 Depression 6 months | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 10.6 Depression 12 months | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 10.7 Anxiety post‐treatment | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 10.8 Internalising post‐treatment | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 10.9 Externalising post‐treatment | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 10.10 Externalising 6 months | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 10.11 Externalising 12 months | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 10.12 Parenting skills post‐treatment | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 10.13 Parenting skills 6 months | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected |
10.1. Analysis.

Comparison 10: CBT carer versus CBT dyad, Outcome 1: PTSD post‐treatment
10.2. Analysis.

Comparison 10: CBT carer versus CBT dyad, Outcome 2: PTSD 6 months
10.3. Analysis.

Comparison 10: CBT carer versus CBT dyad, Outcome 3: PTSD 12 months
10.4. Analysis.

Comparison 10: CBT carer versus CBT dyad, Outcome 4: Depression post‐treatment
10.5. Analysis.

Comparison 10: CBT carer versus CBT dyad, Outcome 5: Depression 6 months
10.6. Analysis.

Comparison 10: CBT carer versus CBT dyad, Outcome 6: Depression 12 months
10.7. Analysis.

Comparison 10: CBT carer versus CBT dyad, Outcome 7: Anxiety post‐treatment
10.8. Analysis.

Comparison 10: CBT carer versus CBT dyad, Outcome 8: Internalising post‐treatment
10.9. Analysis.

Comparison 10: CBT carer versus CBT dyad, Outcome 9: Externalising post‐treatment
10.10. Analysis.

Comparison 10: CBT carer versus CBT dyad, Outcome 10: Externalising 6 months
10.11. Analysis.

Comparison 10: CBT carer versus CBT dyad, Outcome 11: Externalising 12 months
10.13. Analysis.

Comparison 10: CBT carer versus CBT dyad, Outcome 13: Parenting skills 6 months
Comparison 11. CBT child versus CCT child.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 11.1 PTSD post‐treatment | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 11.2 PTSD 6 months | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 11.3 PTSD 12 months | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 11.4 Depression post‐treatment | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 11.5 Depression 12 months | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected |
11.1. Analysis.

Comparison 11: CBT child versus CCT child, Outcome 1: PTSD post‐treatment
11.2. Analysis.

Comparison 11: CBT child versus CCT child, Outcome 2: PTSD 6 months
11.3. Analysis.

Comparison 11: CBT child versus CCT child, Outcome 3: PTSD 12 months
11.4. Analysis.

Comparison 11: CBT child versus CCT child, Outcome 4: Depression post‐treatment
11.5. Analysis.

Comparison 11: CBT child versus CCT child, Outcome 5: Depression 12 months
Comparison 12. CBT child versus EMDR.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 12.1 PTSD post‐treatment | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected |
12.1. Analysis.

Comparison 12: CBT child versus EMDR, Outcome 1: PTSD post‐treatment
Comparison 13. CBT dyad versus waiting list.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 13.1 PTSD post‐treatment | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 13.2 Depression post‐treatment | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 13.3 Anxiety post‐treatment | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 13.4 Internalising post‐treatment | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 13.5 Externalising post‐treatment | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected |
13.1. Analysis.

Comparison 13: CBT dyad versus waiting list, Outcome 1: PTSD post‐treatment
13.2. Analysis.

Comparison 13: CBT dyad versus waiting list, Outcome 2: Depression post‐treatment
13.3. Analysis.

Comparison 13: CBT dyad versus waiting list, Outcome 3: Anxiety post‐treatment
13.4. Analysis.

Comparison 13: CBT dyad versus waiting list, Outcome 4: Internalising post‐treatment
13.5. Analysis.

Comparison 13: CBT dyad versus waiting list, Outcome 5: Externalising post‐treatment
Comparison 14. EMDR vs waiting list.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 14.1 PTSD post‐treatment | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 14.2 Depression post‐treatment | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 14.3 Anxiety post‐treatment | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 14.4 Internalising post‐treatment | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 14.5 Externalising post‐treatment | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected |
14.1. Analysis.

Comparison 14: EMDR vs waiting list, Outcome 1: PTSD post‐treatment
14.2. Analysis.

Comparison 14: EMDR vs waiting list, Outcome 2: Depression post‐treatment
14.3. Analysis.

Comparison 14: EMDR vs waiting list, Outcome 3: Anxiety post‐treatment
14.4. Analysis.

Comparison 14: EMDR vs waiting list, Outcome 4: Internalising post‐treatment
14.5. Analysis.

Comparison 14: EMDR vs waiting list, Outcome 5: Externalising post‐treatment
Comparison 15. CBT dyad vs CBT dyad higher.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 15.1 Depression post‐treatment | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 15.2 Depression 6 months | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 15.3 Depression 12 months | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 15.4 Anxiety post‐treatment | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 15.5 Sexualised behaviour post‐treatment | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 15.6 Sexualised behaviour 12 months | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 15.7 Internalising post‐treatment | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 15.8 Externalising post‐treatment | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 15.9 Exernalising 6 months | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 15.10 Externalising 12 months | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected |
15.1. Analysis.

Comparison 15: CBT dyad vs CBT dyad higher, Outcome 1: Depression post‐treatment
15.2. Analysis.

Comparison 15: CBT dyad vs CBT dyad higher, Outcome 2: Depression 6 months
15.3. Analysis.

Comparison 15: CBT dyad vs CBT dyad higher, Outcome 3: Depression 12 months
15.4. Analysis.

Comparison 15: CBT dyad vs CBT dyad higher, Outcome 4: Anxiety post‐treatment
15.5. Analysis.

Comparison 15: CBT dyad vs CBT dyad higher, Outcome 5: Sexualised behaviour post‐treatment
15.6. Analysis.

Comparison 15: CBT dyad vs CBT dyad higher, Outcome 6: Sexualised behaviour 12 months
15.7. Analysis.

Comparison 15: CBT dyad vs CBT dyad higher, Outcome 7: Internalising post‐treatment
15.8. Analysis.

Comparison 15: CBT dyad vs CBT dyad higher, Outcome 8: Externalising post‐treatment
15.9. Analysis.

Comparison 15: CBT dyad vs CBT dyad higher, Outcome 9: Exernalising 6 months
15.10. Analysis.

Comparison 15: CBT dyad vs CBT dyad higher, Outcome 10: Externalising 12 months
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Baker 1985.
| Study characteristics | ||
| Methods | Study design: randomised controlled trial | |
| Participants |
Inclusion criteria: not reported Exclusion criteria: not reported Gender: female participants Age: range = 13 to 17 years Type of abuse: “The type and extent of abuse varied from fondling to intercourse, with six participants having been subject to sexual intercourse.” (p 36) Onset of abuse: not reported Length of abuse: not reported Perpetrator of abuse: natural father (n = 8); step father (n = 14), step uncle (n = 3), babysitters (n = 2); neighbour (n = 1); schoolmates (n = 2); foster fathers (n = 2); brothers (n = 3); male friends of the family (n = 4) |
|
| Interventions | Participants (n = 39) randomly assigned to one of two groups
|
|
| Outcomes |
Time points for assessment: baseline and post‐treatment Measures (outcomes) : Piers Harris Children's Self Concept Scale (self‐concept), Institute for Personality and Ability Testing Anxiety Scale (anxiety), and Institute for Personality and Ability Testing Depression Scale (depression). The following outcomes were used for the quantitative analyses:
|
|
| Notes |
Start and end date: not reported Funding sources: not reported Study’s limitations as reported by the study's authors: “Generalization of the results is limited to sexually abused female adolescents in a rural population. Perhaps the major limitation of this study was the lack of a control group for comparison. This was not possible as treatment could not be withheld from these clients. An additional limitation was the small number of subjects available at one time, which limited the number of groups that could not be conducted. It is possible that the small number of groups may have magnified the significance of the outcome. More groups would have provided greater distribution of any differences that may have existed and increased the reliability of the results. The use of three separate assessment instruments may have been a limitation. Reading levels may have been a contributing factor as well as the time involved in completing the tests. The wide range of ages, i.e., 13 to 17, was reported by therapists as a somewhat limiting, as it was difficult, at times, to achieve group interaction due to the level of immaturity of the younger subjects and to the difference in selection of topics for discussion. The variations of kinds of abuse also entered into the limiting factors, since some subjects had been abused for long periods of tome while others had been abused only occasionally. Based on therapists’ reports this aspect was limiting only in as much as some discussions seemed to be diluted for younger subjects. The fact that subjects represented a variety of kinds of abuse seemed to stimulate discussion and exchange. It is possible that some other means of grouping subjects other than by random assignment may be worth investigating. In addition, more groups would eliminate the need for grouping subjects across such wide age ranges and developmental levels. Court proceedings may have significant effects on adolescent’s emotional states, and investigation of thus variable may determine whether it is beneficial for victims to be involved in court testimony, which is currently a controversial issue, especially for young children” (p 61‐2) |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: “Random assignment of subjects was achieved by placing 8 slips of paper each for group I, group II, group III, and five slips of paper each for therapist I, therapist II, and Therapist III in one box and having subjects draw one slip at a time until all subjects has been assigned. Therapist assignment was achieved by placing three slips of paper indicating group I, Group II, and Group III in a box having each therapist draw one until all were assigned” (p 37) |
| Allocation concealment (selection bias) | Low risk | Quote: “Therapists were randomly assigned to groups. Subjects were randomly assigned to individual or group therapy. Random assignment of subjects was achieved by placing eight slips of paper each for Group I, Group II, Group III and five slips of paper each for Therapist I, Therapist II, and Therapist III in one box and having subjects draw one slip at a time until all subjects had been assigned. Therapist assignment was achieved by placing three slips of paper indicating Group I, Group II, and Group III in a box and having each therapist draw one until all were assigned”. (p 37) |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: not mentioned and unlikely to have been prevented |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Comment: children's self‐reports and parents’ reports |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Comment: no dropouts were mentioned. Not enough information to make a judgement |
| Selective reporting (reporting bias) | Unclear risk | Comment: all the outcomes measured were reported, but there was no reference to a protocol. |
| Other bias | Low risk | Comment: no other potential sources of bias were identified. |
Berliner 1996.
| Study characteristics | ||
| Methods | Study design: randomised controlled trial | |
| Participants |
Inclusion criteria: “Children were required to complete a minimum of 8 of 10 sessions to remain in the study, and children assigned to the index condition had to be present for the unique experimental treatment sessions” (p 299) Exclusion criteria: not reported Gender: 88% of participants were girls. "A significant subgroup was reported to have been neglected by a primary caretaker. PTSD was the chart diagnosis in 81% of cases.” (p 297) Age: range = 4 to 13 years Type of abuse: almost half had experienced penetration offences, about 15% had been physically injured, and one fourth had been threatened with physical injury. In three fourths of the cases, children had experienced multiple incidents of sexual abuse. About one fifth of the children had experienced other forms of violence or abuse, including physical assault, or had witnessed sexual or physical violence towards a parent or non‐family member. Onset of abuse: not reported Length of abuse: not reported Perpetrator of abuse: male adults in most cases: parents in more than one third of cases, strangers in slightly more than 10% of cases, and relatives and people known to the children in the remainder of cases. |
|
| Interventions | Participants (n = 154) randomly assigned to one of two groups
|
|
| Outcomes |
Time points for assessment: baseline, post‐treatment, 1‐year follow‐up, and 2‐year follow‐up Measures (outcomes): Fear Survey Schedule for Children‐Revised (FSSC‐R; fear), Sexual Abuse Fear Evaluation Scales (SAFE; fear of sexual abuse), Children Manifest Anxiety Scale (RCMAS; anxiety), Children's Depression Inventory (CDI; depression), Child Behaviour Checklist‐Parent version (CBCL; internalising and externalising behaviour), and Child Sexual Behaviour Inventory (CSBI; sexualised behaviour). The following outcomes were used for the quantitative analyses:
|
|
| Notes |
Start and end dates: not reported Funding sources: "This study was funded by the National Center on Child Abuse and Neglect, Grant #90‐CA‐1447, Department of Health and Human Services, Washington, DC." (p 309) Study's limitations as reported by the study's authors: “Without a no‐treatment or community comparison sample, it is not possible to conclude from this study that participation in abuse‐specific treatment produces greater improvement than a natural recovery process” (p 305) |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: “Groups rather than individuals were randomly assigned to either the index or comparison conditions using a random number table generated at the beginning of the project” (p 299) |
| Allocation concealment (selection bias) | Low risk | Quote: “Assigned therapists and other staff were blind to the random assignment schedule and were not informed of the condition of the group they would be running until all children were referred” (p 299) |
| Blinding of participants and personnel (performance bias) All outcomes | High risk |
Quote: “To prevent selective referring and staff manipulation of the assignment schedule, assigned therapists and other staff were blind to the random assignment schedule and were not informed of the condition of the group they would be running until all children were referred” (p 299) Comment: the authors only state that the intervention’s staff were blind. They do not report if the participants were blind. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Comment: children's self‐reports and parents’ reports |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Comment: there was substantial attrition. Whilst there were no significant differences between participants who completed the treatment versus participants who dropped out, the authors did not report if they performed tests with enough statistical power to detect meaningful differences. Also, the authors did not report data that would allow for computation of effect sizes of participants who remained in treatment and those who did not remain. |
| Selective reporting (reporting bias) | Unclear risk | Comment: all the outcomes measured were reported, but there was no reference to a protocol. |
| Other bias | Low risk | Comment: no other potential sources of bias were identified. |
Burke 1988.
| Study characteristics | ||
| Methods | Study design: randomised controlled trial | |
| Participants |
Inclusion criteria: “To be accepted in this study, a subject must have acknowledged that abuse had occurred and enough evidence must have been presented to the referring agency (Department of Family and Children Services, Department of Social Services, the Navy Family Service Center, and private practitioners) for the abuse to be considered "confirmed" by this agency. One county agency in Georgia and two agencies in South Carolina provided referrals. Additional criteria for inclusion included (1) reports of behavioral difficulties in subjects indicated in records of assigned child protection case workers, (2) a pretreatment score on the Children's Depression Inventory of at least one standard deviation above the mean score obtained from a normative sample of girls aged 8 to 13, and (3) abuse must have occurred within the last two years” (p 26) Exclusion criteria: “Subjects were excluded if they were not within one year of their age appropriate grade level in school or if they participated in special education classes. No child missed more than one consecutive session of treatment.” (p 26‐7) Gender: all participants were girls Age: range = 8 to 13 years Type of abuse: not reported Onset of abuse: not reported Length of abuse: not reported Perpetrator of abuse: not reported |
|
| Interventions | Participants (n = 25) randomly assigned to one of two groups
|
|
| Outcomes |
Time points for assessment: baseline, post‐treatment, and 6‐week follow‐up Measures (outcomes): Children's Depression Inventory (CDI; depression), Revised Children's Manifest Anxiety Scale (RCMAS; anxiety), Achenbach Child Behaviour Checklist and Profile (CBP; behaviour), Revised Fear Survey Schedule for Children (FSSC‐R; fear) The following outcomes were used for the quantitative analyses:
|
|
| Notes |
Start and end dates: not reported Funding sources: not reported Study's limitations as reported by the study's authors: “[The study] did not involve any placebo treatment comparison group or any comparison group which received different component parts of the treatment package” (p 49‐50) |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Comment: not mentioned and unlikely to have been done |
| Allocation concealment (selection bias) | High risk | Comment: not mentioned and unlikely to have been done |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: not mentioned and unlikely to have been done |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Comment: all the outcomes were self‐reports. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: there were no missing data, or there were no outcomes where data was incomplete. |
| Selective reporting (reporting bias) | Unclear risk | Comment: all the outcomes measured were reported, but there was no reference to a protocol. |
| Other bias | Low risk | Comment: no other potential sources of bias were identified. |
Celano 1996.
| Study characteristics | ||
| Methods | Study design: randomised controlled trial | |
| Participants |
Inclusion criteria: “Children were eligible for the study if they were 8 to 13 years old, had experienced contact sexual abuse within the past 3‐year period, and could disclose the abuse to the clinician during the evaluation” (p 5) Exclusion criteria: “Mentally retarded, psychotic, or drug‐addicted children or parents were ineligible” (p 5) Gender: all participants were girls Age: range = 8 to 13 years Type of abuse: digital penetration of the vagina, oral sex, or attempted intercourse (~25%); and fondling (~25%) Onset of abuse: not reported Length of abuse: not reported. However, "In a third of the cases, the perpetrator still had contact by phone or in person with the child at intake.” (p 5) Perpetrator of abuse: all males; family members (56%): 25% in a paternal caregiver role (e.g. father, mother's boyfriend), other family members (31%); acquaintances (31%); and strangers (13%) |
|
| Interventions | Participants (n = 49) randomly assigned to one of two groups
|
|
| Outcomes |
Time points for assessments: baseline and post‐treatment Measures (outcomes): Child Behaviour Check List (CBCL; internalising and externalising), Children's Impact of Traumatic Events Scales‐Revised (CITES‐R; PTSD), Children's Global Assessment Scale (CGAS; social competence), Parent Reaction to Incest Disclosure Scale (PRIDS; parents' reaction to incest disclosure), Parental Attribution Scale (PAS; parents' attribution of responsibility of the abuse). The following outcomes were used for the quantitative analyses:
|
|
| Notes |
Start and end dates: not reported Funding sources: not reported Study's limitations as reported by the study's authors: "The lack of a no‐treatment control group and the use of multiple statistical tests with a relatively small sample, which may have contributed to Type I errors" (p 15) |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: authors only stated that the participants were randomly allocated. |
| Allocation concealment (selection bias) | Unclear risk | Comment: there is no information on the way in which allocation was performed. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: not mentioned and unlikely to have been done |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: “standardised measures were administered by a clinician not involved in the child’s treatment. Additionally, a psychiatrist or psychologist blind to treatment condition rated the child’s overall psychosocial functioning based on child and caretaker interviews” (p 6) |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Comment: although there were no significant differences between participants who completed the treatment versus participants who dropped out of it, the authors did not report if they performed tests with enough statistical power to detect meaningful differences. Also, the authors did not report data that would allow for computation of effect sizes of participants who remained in treatment and those who did not remain. |
| Selective reporting (reporting bias) | Unclear risk | Comment: all the outcomes stated at the beginning and measured were reported, but there was no reference to a protocol. |
| Other bias | Low risk | Comment: no other potential sources of bias were identified. |
Cohen 1996.
| Study characteristics | ||
| Methods | Study design: randomised controlled trial | |
| Participants |
Inclusion criteria: “Inclusionary criteria included the following. The child had to have experienced some form of sexual abuse as defined above, with the most recent episode of sexual abuse having occurred no more than 6 months before referral to the study. Both males and females were included in the study. Where applicable, the sexual abuse had to have been reported to Child Protective Services before the child's acceptance into the study. In all cases, a child was included only if the abuse had been indicated by Child Protective Services, if there had been independent confirmation of abuse by the agency in Pittsburgh with recognized expertise in conducting investigative evaluations, or if there was physical evidence diagnostic of sexual abuse. Because the primary goal of treatment in the study was symptom reduction, subjects had to reach a minimal level of symptomatology in order to be included. Minimal symptomatology was defined as either a Weekly Behavior Record (WBR) Total Behavior score of more than 7, or any sexually inappropriate behavior report ed on the Child Sexual Behavior Inventory (CSBI).” (p 44) Exclusion criteria: “Exclusionary criteria included mental retardation or pervasive developmental disorder, psychotic symptoms, a serious medical illness, psychotic disorder or active substance abuse in the parent participating in treatment, or the lack of a long‐term caretaker to participate in the study (i.e., if a child was expected to remain with the present caretaker for less than 12 months, the subject was not included).” (p 44) Gender: 56% of participants were girls Age: range = 3 to 6 years Type of abuse*: genital fondling only (46%); vaginal or anal intercourse, or both (26%); oral‐genital contact (22%); fondling of breasts (3%); and other or unknown (3%); more than one type of abuse (34%) Onset of abuse: not reported Length of abuse: once (25%), 2 to 5 times (26%), 6 to 10 times (15%), more than 10 times (29%), and not known (5%) Perpetrator of abuse: biological father (15%), biological mother (2%), mother's paramour (10%), uncle (7%), baby‐sitter (7%), older child/adolescent (13%), and multiple abusers or other (46%) *Percentages reflect the most intrusive type of abuse experienced by the participant |
|
| Interventions | Participants (n = 86) randomly assigned to one of two groups
|
|
| Outcomes |
Time points for assessments: baseline, 6‐month follow‐up, and 1‐year follow‐up Measures (outcomes): Child Behaviour Checklist (CBCL; internalising and externalising), Child Sexual Behaviour Inventory (CSBI; sexualised behaviour), Weekly Behaviour Report (WBR; weekly behaviour), and Preschool Symptom Self‐Report (PRESS; global functioning) The following outcomes were used for the quantitative analyses:
|
|
| Notes |
Start and end dates: not reported Funding sources: "This research was funded by the National Center on Child Abuse and Neglect (grant 90‐CA‐1526)." (p 42) Study’s limitations as reported by the study's authors: none reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: “Treatment assignment was randomised with the use of Efron's biased coin toss (Efron, 1980), to ensure that the two groups would be balanced with respect to the identity of the perpetrator, type of sexual abuse experienced, gender, and age.” (p 45) |
| Allocation concealment (selection bias) | Unclear risk | Comment: did not report enough information to make a judgement |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: not mentioned and unlikely to have been done |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Comment: children’s self‐reports and parent’s reports |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Comment: 19 of the 86 participants dropped out. Although the authors show that there were no statistical differences between completers and no completers, they do not report if they performed tests with enough statistical power to detect meaningful differences, or data that would allow computation of the effect sizes of completers and non‐completers. |
| Selective reporting (reporting bias) | Unclear risk | Comment: all the outcomes measured were reported, but there was no reference to a protocol. |
| Other bias | Low risk | Comment: no other potential sources of bias were identified. |
Cohen 1998.
| Study characteristics | ||
| Methods | Study design: randomised controlled trial | |
| Participants |
Inclusion criteria: “contact sexual abuse within the past 6 months which had been validated by CPS or an independent forensic evaluation prior to entry into the study, significant symptomatology related to the sexual abuse experience (as documented by a score in the clinical range on any of the self‐report instruments or the presence of sexually inappropriate behavior as reported by the parent), and availability of a non‐offending parent or primary caregiver who was able to participate in treatment.” (p 138) Exclusion criteria: “active psychotic symptoms or substance abuse, or mental retardation or pervasive developmental delay in the child, or active psychosis in the parent or primary caretaker participating in the treatment.” (p 139) Gender: 69% of participants were girls Age: range = 7 to 15 years Type of abuse*: anal or vaginal intercourse or both (54%); oral intercourse (2%); and genital fondling only (44%) Onset of abuse: not reported Length of abuse: single episode of sexual abuse (36%); 2 to 5 episodes (21%); 6 to 10 episodes (8%); more than 10 episodes (33%); not reported (2%) Perpetrator of abuse: not reported *Reflects the most severe type of abuse experienced (many experienced more than one type) |
|
| Interventions | Participants (n = 82) randomly assigned to one of two groups
|
|
| Outcomes |
Time points for assessment: baseline, 6‐month follow‐up, and 1‐year follow‐up Measures (outcomes): Child Behaviour Checklist (CBCL)‐Parent Form (internalising and externalising), State‐Trait Anxiety Inventory for Children (STAIC; anxiety), Children's Depression Inventory (CDI; depression) and Child Sexual Behaviour Inventory (CSBI; sexualised behaviour) The following outcomes were used for the quantitative analyses:
|
|
| Notes |
Start and end dates: not reported Funding sources: "This study was supported by the National Center on Child Abuse and Neglect, Grant No. 90‐CA‐1545" (p 17). It is not clear if support means funding. Study’s limitations as reported by the study's authors: “Inadequate sample size and lack of pre‐treatment symptomatology; relatively high drop‐out rate, particularly for the NST group, which diminished the study's power to detect statistically significant differences between the two treatment groups and may have implications regarding the generalizability of the study findings; failure to administer assessment instruments (particularly the CSBI) to removed participants at the time of their removal from the study; and the lack of child‐rated client satisfaction questionnaires” (p 25‐6) |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: “Efron’s biased coin toss was used to ensure that the two groups were balanced with respect to (a) Child Behaviour Checklist CBCL Total Behavior Problems, (b) gender, and (c) age” (p 22) |
| Allocation concealment (selection bias) | Unclear risk | Comment: no information to make a judgement |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: not mentioned and unlikely to have been done |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Comment: children's self‐reports and parents’ reports |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: authors analysed data on an intention‐to‐treat (ITT) basis |
| Selective reporting (reporting bias) | High risk | Comment: although the authors reported outcomes for all time points at 1‐year follow‐up, they did not report one measure from their report of initial outcomes. Also, there was no reference to a protocol. |
| Other bias | Low risk | Comment: No other potential sources of bias were identified. |
Cohen 2004.
| Study characteristics | ||
| Methods | Study design: randomised controlled trial | |
| Participants |
Inclusion criteria: “children had to meet at least 5 criteria for sexual abuse‐related DSMIV‐defined PTSD, including at least one symptom in each of the three PTSD clusters (reexperiencing, avoidance or numbing, and hyperarousal). In addition, children were required to have a parent or other caretaker (including long‐term foster parents) who was willing and able to participate in the parental treatment component of the study” (p 3) Exclusion criteria: “children were excluded if they had an active psychotic disorder or an active substance use disorder which resulted in significant impairment in adaptive functioning, or if the parent or primary caretaker who would be participating in the treatment had such a disorder. Additionally, children were excluded if they were not fluent in English, and/or had a documented developmental disorder (e.g., autism). Children who were currently on psychotropic medication had to have been on a stable medication regimen for at least two months prior to admission to the study. Children in the study could not be receiving psychotherapy for sexual abuse outside of the study” (p 3) Gender: 79% of participants were girls Age: range = 8 to 14 years Type of abuse*: sexual touching over clothes (n = 6, 2.9%); non‐genital touching under clothes (n = 9; 4.4%); digital penetration (n = 45; 22%); simulated intercourse (n = 21; 10.3%); oral‐genital abuse (n = 41; 20.1%); penile penetration (n = 76; 37.4%); other (n = 8 3.9%). Abuse initiated via: playful/coaxing (n = 22; 10.8%); bribes (n = 8; 3.9%); command (n = 40; 19.7%); verbal threats (n = 38; 18.7%); physical threats (n = 10; 4.9%); and physical force (n = 74; 36.5%) Onset of abuse: not reported Length of abuse: not reported Perpetrator of abuse: not reported *Most intrusive types of sexual abuse |
|
| Interventions | 229 participants were randomly assigned to one of two groups
|
|
| Outcomes |
Time points for assessments: baseline and post‐treatment Measures (outcomes): Kiddie‐Schedule for Affective Disorders and Schizophrenia‐Present and Lifetime Version (K‐SADS‐PL; affective disorders), Children’s Depression Inventory (CDI; depression), State‐Trait Anxiety Inventory for Children (STAIC; anxiety), Children’s Attributions and Perceptions Scale (CAPS; child's attributions and perceptions), Child Behaviour Checklist (CBCL; internalising and externalising), Parent’s Emotional Reaction Questionnaire (PERQ; emotional reactions of the parents), and Parental Support Questionnaire (PSQ; supportive parenting) The following outcomes were used for the quantitative analyses
|
|
| Notes |
Start and end dates: not reported Funding sources: "This research was funded by the National Institute of Mental Health, grants R10 MH55963 and R10 MH56224." (p 1) Study's limitations as reported by the study's authors: “The lack of a no treatment control group; the study did not elucidate which specific TFCBT components underlie its superior effectiveness; relatively few Hispanic and no Asian families were included in the study.” (p 8) |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: the authors only state that the participants were randomly allocated. |
| Allocation concealment (selection bias) | Unclear risk | Comment: not enough information reported to make a judgement |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: not mentioned and unlikely to have been done |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Comment: children's self‐reports and parents’ reports |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: the authors analysed data on an intention‐to‐treat (ITT) basis and multiple imputation procedures were employed to estimate the sample’s missing, post‐test scale scores. |
| Selective reporting (reporting bias) | Low risk | Comment: all the outcomes measured were reported and it is a registered trial with protocol. |
| Other bias | Low risk | Comment: no other potential sources of bias were identified. |
Costas 1999.
| Study characteristics | ||
| Methods | Study design: randomised controlled trial | |
| Participants |
Inclusion criteria: "(a) must be a significant caregiver of a child between 4 and 10 years of age who has experienced sexual abuse; (b) must be a nonoffender; (c) child must be identified by an investigating agency as having been sexually abused; (d) must be able to speak, read, and write the English language; (e) must not be involved in classes that exclusively address parenting issues; (f) must be able to attend the 10 weeks of filial therapy training; (g) must be able to attend a pretraining session to complete pretest instruments and be videotaped playing with their child; (h) must be able to attend a posttraining session to complete posttest instruments and be videotaped playing with their child; (f) must agree to participate in weekly 30‐minute home play sessions with their child; and (g) must be willing to sign the consent‐to‐participate form." (p 48) Exclusion criteria: not reported Gender: 68% of participants were girls Age: range = 4 to 10 years Type of abuse: intervention = intrafamilial abuse (85%); extrafamilial abuse (7.5%); and unknown (7.5%) Onset of abuse: mean age 5.4 years (range 18 months to 9.5 years) Length of abuse: not reported Perpetrator of abuse: not reported |
|
| Interventions | 31 participants were randomly assigned to one of two groups
|
|
| Outcomes |
Time points for assessments: baseline and post‐treatment Measures (outcomes): Porter Parental Acceptance Scale (parents' acceptance), Parenting Stress Index (parents' stress), Child Behaviour Checklist (internalising and externalising), Child Anxiety Scale (anxiety), Joseph Preschool and Primary Self‐Concept Screening Test (self‐concept), Draw a Person: Screening Procedure for Emotional Disturbance (child's emotional disturbance) The following outcomes were used for the quantitative analyses:
|
|
| Notes |
Start and end dates: not reported Funding sources: not reported Study’s limitations as reported by the study's authors: none reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Comment: no methods for randomisation mentioned |
| Allocation concealment (selection bias) | High risk | Comment: not mentioned and unlikely to have been done |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: not mentioned and unlikely to have been done |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Comment: children's self‐reports and parents’ reports |
| Incomplete outcome data (attrition bias) All outcomes | High risk |
Quote: "Over the course of the 10‐week treatment period, 1 subject from the experimental group and 4 subjects from the control group dropped out of the study. Thus, 26 subjects completed the present study, 14 in the experimental group and 12 in the control group." (p 48) Comment: no further details given |
| Selective reporting (reporting bias) | Unclear risk | Comment: all the outcomes measured were reported, but there was no reference to a protocol. |
| Other bias | Low risk | Comment: no other potential sources of bias were identified. |
Danielson 2012.
| Study characteristics | ||
| Methods | Study design: randomised controlled trial | |
| Participants |
Inclusion criteria: “Inclusion criteria were youth who: a) were aged 12–17; b) had experienced at least one lifetime CSA that could be recollected by the youth (defined as unwanted/forced vaginal or anal penetration by an object, finger, or penis; oral sex; or touching of one’s genitalia); and c) were not mentally retarded” (p 2) Exclusion criteria: not reported Gender: 88% of participants were girls Age: range = 13 to 17 years Type of abuse: not reported Onset of abuse: not reported Length of abuse: not reported Perpetrator of abuse: not reported “30 treatment seeking adolescent CSA victims and their caregivers (72.6% biological parents, 17.1% other family members, 10.3% non‐familial guardians). 70% received Medicaid' 'Nine (30%) reported 2nd, 3rd, and 4th CSA revictimization experiences; age of first/only CSA experience ranged from 4–15; and 23 (67.7%) reported having experienced other traumatic events. Mean time since most recent assault was 3.7 years (SD = 3.8).” (p 2) |
|
| Interventions | Participants (n = 30) randomly assigned to one of two groups
|
|
| Outcomes |
Time points for assessment: baseline, post‐treatment, 3‐month follow‐up, and 6‐month follow‐up Measures (outcomes): UCLA PTSD Index for DSM‐IV‐Adolescent & Caregiver versions (PTSD), Child Depression Inventory (CDI; depression), Behavioural Assessment System for Children (BASC‐2; internalising and externalising behaviour), Timeline Follow Back Interview (TLFB; substance misuse), Cohesion and Conflict subscales of the Family Environment Scale (FES; family environment), and the following two items to measure risky sexual behaviour: “1) number of consensual sexual intercourse partners over the past 3 months (including new sexual partners), and 2) whether or not the youth had been diagnosed with a sexually transmitted disease in the past 3 months” (p 4) The following outcomes were used for the quantitative analyses:
|
|
| Notes |
Start and end dates: not reported Funding sources: "The study was supported by grant award K23DA018686 from the National Institute on Drug Abuse (NIDA; PI: Danielson) and a Young Investigator Award from NARSAD (PI: Danielson)." (p 7) Study's limitations as reported by the study's authors: “There were baseline differences existed between RRFT and TAU across most variables and dosage differences, where RRFT youth received more sessions on average than TAU youth.” (p 6‐7) |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Comment: randomised participants using computerised blocked randomisation |
| Allocation concealment (selection bias) | High risk | Comment: did not report enough information to make a judgement |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: not mentioned and unlikely to have been done |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Comment: children's self‐reports and parents’ reports |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: the authors analysed data on an intention‐to‐treat (ITT) basis. |
| Selective reporting (reporting bias) | Unclear risk | Comment: the authors reported the primary outcomes specified in the trial registration and two of the three secondary outcomes. However, there is no reference to a protocol. |
| Other bias | Low risk | Comment: no other sources of bias were identified. |
Deblinger 1996b.
| Study characteristics | ||
| Methods | Study design: randomised controlled trial | |
| Participants |
Inclusion criteria: “Inclusion criteria were as follows: (a) contact CSA substantiated by an investigation conducted by DYFS or the prosecutor's office, (b) children between the ages of 7 and 13, (c) human subject consent to participate in the study completed by the child and the child's legal guardian, and (d) presence of a total of three posttraumatic stress symptoms, including at least one symptom of avoidance or reexperiencing phenomenon. Based on previous research and clinical experience, the investigators decided to include in the current study both children who met full DSM‐IIIR criteria for PTSD and those with partial PTSD symptoms, as. described previously. Because PTSD often presents with delayed onset or an episodic course, the exclusion of children who did not meet full PTSD criteria at the time of the initial assessment seemed unwarranted. Children exhibiting partial PTSD symptoms might develop the full‐blown disorder with time.” (p 312) Exclusion criteria: “Exclusion criteria were as follows: (a) severe developmental delay; (b) psychosis; (c) ongoing, unsupervised contact with the alleged perpetrator; (d) female caretaker not willing to participate; or (e) dangerousness to themselves (i.e., suicidal) or others (i.e., dangerous aggressive behavior). Children identified as suicidal or dangerously aggressive were referred for crisis intervention or hospitalization at any time during the investigation. They were excluded from the sample only if they were referred for such treatment during the initial evaluation. Other clinical and legal issues were also considered, on a case‐by‐case basis, in evaluating the appropriateness of potential subjects' participation in this treatment outcome investigation” (p 312) Gender: 83% of participants were girls Age: range = 7 to 13 years Type of abuse: sexual touching (45%); simulated intercourse (7%); oral‐genital contact (17%); and penile penetration of the vagina or anus (33%) Onset of abuse: not reported Length of abuse: range 1 day to 5 years of repeated abuse; 1 one sexually abusive incident (18%), 2 to 10 episodes (47%), 11 to 50 episodes (22%), and more than 50 abusive incidents (13%). Last incident: 6 months before baseline measurements (66%), 6 months to 2 years before baseline measurements (16%), and 2 or more years before baseline measurements (18%) Perpetrator of abuse: fathers or stepfathers (32%); other adult relatives (19%); adult nonrelatives (22%); older peers (20%); multiple offenders (7%) |
|
| Interventions | Participants (n = 100) randomly assigned to one of four groups
|
|
| Outcomes |
Time points for assessment: baseline, post‐treatment, 3‐month follow‐up, 6‐month follow‐up, 1‐year follow‐up, and 2‐year follow‐up Measures (outcomes): PTSD section of the Schedule for Affective Disorders and Schizophrenia for School‐Age Children (K‐SADS‐E; PTSD), State/Trait Anxiety Inventory for Children (STAIC; anxiety), Child Depression Inventory (CDI; depression), Child Behaviour Checklist (CBCL; internalising and externalising behaviour), Parenting Practices Questionnaire (PPQ; parenting) The following outcomes were used for the quantitative analyses:
|
|
| Notes |
Start and end dates: not reported Funding source: not reported Study's limitations as reported by the study's authors: “The heterogeneity of the community treatment condition and that some of the measures used in the investigation, such as the STAIC Inventory, may have had limited sensitivity in detecting the types of symptoms suffered by sexually abused children” (p 319) |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: the authors only report that the participants were allocated randomly. |
| Allocation concealment (selection bias) | Unclear risk | Comment: not enough information is provided to make a judgement. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: not mentioned and unlikely to have been done |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Comment: children's self‐reports and parents’ reports |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Comment: there was not enough information about the impact of missing data on the results to make a judgement. |
| Selective reporting (reporting bias) | Unclear risk | Comment: All the outcomes measured were reported, but there was no reference to a protocol. |
| Other bias | Low risk | Comment: no other sources of bias were identified. |
Deblinger 2001.
| Study characteristics | ||
| Methods | Study design: randomised controlled trial | |
| Participants |
Inclusion criteria: "All child participants had made a credible disclosure of contact sexual abuse (Russell, 1983) to a professional prior to their participation in group." (p 333) Exclusion criteria: 'Parents and/ or children who suffered psychotic disorders, severe developmental delays, and/ or behaviours that were dangerous to themselves or others were excluded." (p 333) Gender: 61% of participants were girls Age: range = 2 to 8 years Type of abuse: penile penetration (n = 7; 16%); no penile penetration (n = 37; 84%) Onset of abuse: not reported Length of abuse: not reported Perpetrator of abuse: adults aged 18 years old or older (n = 16; 36%): fathers or step fathers (n = 4; 9%), other adult relatives (n = 6; 13.6%), other adult nonrelatives (n = 6; 13.6%); adolescents or older children aged 17 years old or younger (n = 28; 64%): siblings (n = 2; 4.5%) related older peers (n = 11; 25%), and not related older peers (n = 15; 34%) |
|
| Interventions | Participants (n = 54) randomly assigned to one of two groups
|
|
| Outcomes |
Time points for assessment: baseline, post‐treatment, and 3‐month follow‐up Measures (outcomes): Impact of Events Scale (IES; trauma), Parent Emotional Reaction Questionnaire (PERQ; emotional reaction of the parents), Parent Practices Questionnaire (PPQ; parenting), Social Support Questionnaire (SSQ; parents' support networks), Child Sexual Behaviour Inventory (sexualised behaviour), Kiddie Schedule for Affective Disorders and Schizophrenia for School‐Age Children‐Epidemiologic Version (affective disorders), and the What If Situations Test (WIST; children's reactions to risky situations). The following outcomes were used for the qualitative analyses:
|
|
| Notes |
Start and end dates: not reported Funding source: "This study was funded by the National Institute of Mental Health, Grant #IR2IMH53241" (p 332) Study's limitations as reported by the study's authors: “The majority of children in this sample did not demonstrate clinically significant behaviour problems at pre‐treatment, making the detection of differential treatment effects difficult. In addition, the 3‐month follow‐up was not long enough to examine the long‐term maintenance of the treatment effects or the preventive potential of these interventions” (p 340‐1) |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: “Assignment was randomly determined by computer program” (p 335) |
| Allocation concealment (selection bias) | Unclear risk | Comment: did not report enough information to make a judgement |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: not mentioned and unlikely to have been done |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Comment: children's self‐reports and parents’ reports |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Comment: although there were no significant differences between participants who completed the treatment versus the participants who dropped out of it, and relatively low percentage of attrition, the authors did not report the impact of the dropouts on the results. |
| Selective reporting (reporting bias) | Unclear risk | Comment: all the outcomes measured were reported, but there was no reference to a protocol or registration of the trial. |
| Other bias | Low risk | Comment: no other sources of bias were identified. |
Deblinger 2011.
| Study characteristics | ||
| Methods | Study design: randomised controlled trial | |
| Participants |
Inclusion criteria: “To be eligible for the study, children must have experienced contact sexual abuse, which was confirmed by NJ’s Division of Youth' Page 68 'and Family Services, PA’s Department of Children, Youth, and Families, a law enforcement official, or a professional with recognized expertise in conducting evaluations of CSA. Children who were allegedly sexually abused by other children were only accepted into the study when their abuse was verified by an independent child abuse professional as indicated above, and the abuse involved an age or size differential, and some indication that the child perpetrating the abuse had utilized physical force, verbal threats, and/or coercion to engage and/or maintain the child’s cooperation and silence. Children had to have at least five PTSD symptoms, including at least one symptom representing, respectively, avoidance, reexperiencing, and hyperarousal” (p 68‐9) Exclusion criteria: “children with significant developmental disabilities (IQ < 70) were excluded. A child or a parent could not have a serious medical or mental health illness (i.e., psychosis) that would interfere with his or her participation in treatment but no children were excluded for these reasons.” (p 69) Gender: 62% of participants were girls. "Participating parents were most frequently the child’s biological mother (84%), who was either currently married or cohabiting with a partner (67%) and who was employed either full‐ or part‐time (60%). Thirty‐five percent of the parents reported that they had also experienced contact CSA” (p 69) Age: range = 4 to 11 years Type of abuse: oral–genital contact or penile penetration, or both (61%) Onset of abuse: not reported Length of abuse: not reported Perpetrator of abuse: related or unrelated adult (51%); older children or teens (49%) |
|
| Interventions | 210 participants were randomly assigned to one of two groups
|
|
| Outcomes |
Time points for assessment: baseline, post‐treatment, 6 months follow‐up and 12 months follow‐up Measures (outcomes): Schedule for Affective Disorders and Schizophrenia for School‐Age Children‐Present and Lifetime Version (post‐traumatic stress disorder), Child Behavior Checklist (CBCL, internalising, externalising), Child Sexual Behavior Inventory (CSBI, sexualised behaviour)), Parent Emotional Reaction Questionnaire (PERQ, emotional reaction of the parents), Parent Practices Questionnaire (PPQ, parenting), Children’s Depression Inventory (depression), Multidimensional Anxiety Scale for Children (MASC, anxiety). The following outcomes were used for quantitative analyses:
|
|
| Notes |
Start and end dates: not reported Funding sources: "The authors disclose the following financial relationships within the past 3 years: Contract grant sponsor: NIMH; Contract grant numbers: R01‐MH064776; R01‐MH064635." (p 67) Study's limitations as stated by the study's authors: “The study was limited by the relatively small numbers of children in each condition (barely enough power to detect differences among conditions for most outcomes) and the lack of self‐report instruments to assess depressive and anxiety outcomes in younger children” (p 239) |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: the authors only reported that participants were randomly allocated. |
| Allocation concealment (selection bias) | Unclear risk | Comment: not mentioned and unlikely to have been done |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: not mentioned and unlikely to have been done |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Comment: children's self‐reports and parents’ reports |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: 31 children and their parents dropped out. Differences between completers and non‐completers were not statistically significant. Authors analysed data on an intention‐to‐treat (ITT) basis. |
| Selective reporting (reporting bias) | High risk | Comment: The authors only reported the results of analysis of covariance (ANCOVA) for complete sets of data. |
| Other bias | Low risk | Comment: no other potential sources of bias were identified. |
Dominguez 2001.
| Study characteristics | ||
| Methods | Study design: randomised controlled trial | |
| Participants |
Inclusion criteria: no further details than "Participants were referred by local community agencies, district attorneys, school personnel, and law enforcement officers" (p 34) Exclusion criteria: "Exclusionary criteria included mental retardation, gross organic brain damage, psychotic or autistic behavior, learning disabilities, perpetrators of violence, substance abusers, gang members, and conduct disordered children." (p 34) Gender: 76% (n = 32) of participants were girls Age: range = 6 to 17 years Type of abuse: fondled (32%); attempted penetration (12%); successfully penetrated (56%) Onset of abuse: not reported Length of abuse: not reported Perpetrator of abuse: older child (52%); adult stranger (16%); adult acquaintance (8%); non‐caregiving adult well known to the child (8%); someone who had previously served in the caregiving role (16%) |
|
| Interventions | Participants (n = 25) randomly assigned to one of two groups
|
|
| Outcomes |
Time points for assessment: baseline and post‐treatment Measures (outcomes): Impact of Events Scale‐Revised (IES‐R; trauma) and Children’s Depression Inventory (CDI; depression) We could not use the data from this study because no mean values or standard deviations of the outcome measures or the number of participants for whom the outcomes were measured were reported by the authors, and neither were other statistics to calculate or impute the data (e.g. standard errors, confidence intervals and P values). We tried to contact the authors but did not get a response. |
|
| Notes |
Start and end dates: not reported Funding sources: not reported Study's limitations as reported by the study's authors: “The current study had limited power due to the sample size of 25. Due to the nature of the design (i.e., no‐treatment control group) and the lack of differential treatment effectiveness, threats to the overall treatment effect finding include the passage of time and non‐specifics of treatment. Second, threats to the finding that there were no differential treatment effects include overlapping active treatment components (i.e., supportive treatment was contaminated with CBT elements) and a lack of power to detect differences. Another potential limitation in this study is the use of the Impact of Events Scale‐Revised (Horowitz, 1979). This measure was originally developed as a tool to be used with adults, not with children. Other limitation is that the study did not involve a follow‐up assessment. Generalizability of the results is another limitation of this study. The participants in this study were a very particular subset of children who experienced sexual abuse.” (p 72‐4) |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: the author only states that the participants were randomly allocated to the conditions. |
| Allocation concealment (selection bias) | High risk | Comment: not mentioned and unlikely to have been done |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: not mentioned and unlikely to have been done |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Comment: children's self‐reports and parents’ reports |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Comment: the author reported that there were no statistically significant differences between completers and non‐completers. However, due to the small size of the sample, the tests have very low statistical power to detect imbalances between groups, if any. |
| Selective reporting (reporting bias) | Unclear risk | Comment: all the outcomes measured were reported, but there was no reference to a protocol. |
| Other bias | Low risk | Comment: no other potential sources of bias were identified. |
Farkas 2008.
| Study characteristics | ||
| Methods | Study design: randomised controlled trial | |
| Participants |
Inclusion criteria: not reported Exclusion criteria: “presenting at least one trauma had affected and who still affects them, do not present a psychotic disorder, suicidal thoughts or cognitive deficits” (p 10‐8) Gender: 73% of participants were girls Age: range = 7 to 13 years Type of abuse: penetration (in 40% or more of cases) Onset of abuse: beginning of adolescence, between 11 and 15 years old (for 50% of participants) Length of abuse: more than 40% experienced multiple episodes Perpetrator of abuse: 40% of assaults committed by same person, usually a relative other than parents |
|
| Interventions | Participants (n = 30) randomly assigned to one of two groups
|
|
| Outcomes |
Time points for assessments: baseline, post‐treatment, and 3‐month follow‐up Measures (outcomes): Trauma Symptom Checklist for Children (TSCC; PTSD, depression and anxiety) and Child Behavior Checklist (CBCL; internalising and externalising behaviour) The following outcomes were used for the quantitative analyses:
|
|
| Notes |
Start date: May 2005. End date: November 2006 Funding sources: not reported Study's limitations as reported by the study's authors: the majority of participants were girls, which represents the reality of sexual assault involving more women than men; the results of this study do not allow to separate the specific effect of the EMDR treatment components of the treatment MASTR; It would be interesting to resume the study by adding some additional EMDR treatment sessions since the adolescents presented, in addition to incidents of sexual assault, many other traumas that could not be treated given the time spent (4 sessions) at this part of treatment; and finally, it would be interesting to check the impact of a component systemic treatment that aims to support the parent or guardian to the difficulties he experiences to help the young to regulate emotions (translated from French; p 18) Original text:"Toutefois, la majorité des participants sont des filles, ce qui représente la réalité des agressions sexuelles qui impliquent un nombre plus important de femmes que d'hommes. Les résultats de la présente étude ne permettent pas de départager l'effet spécifique des composantes du traitement EMDR de celles du traitement MASTR Il serait également intéressant de reprendre l'étude en ajoutant quelques séances supplémentaires de traitement EMDR puisque les adolescents présentaient, en plus des incidents d'agressions sexuelles, de nombreux autres traumatismes qui n'ont pu être traités étant donné le temps consacré (4 séances) à cette partie du traitement. Finalement, il serait intéressant de vérifier l'impact d'une composante systémique au traitement qui viserait à soutenir le parent ou tuteur pour les difficultés qu'il éprouve à aider le jeune à réguler ses émotions" (p 83) |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: not enough information to make a judgement |
| Allocation concealment (selection bias) | Unclear risk | Comment: not enough information to make a judgement |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: neither participants nor personnel were blinded |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Comment: children's self‐reports and parents’ self‐reports |
| Incomplete outcome data (attrition bias) All outcomes | High risk |
Quote: “Of the 35 participants who were selected at the beginning of the study, five (three girls and two boys), three of whom were in the treatment group, gave up study and did not participate in the second measurement time”. (Translated from French; p 75) Comment: no further details given |
| Selective reporting (reporting bias) | Unclear risk | Comment: all the outcomes measured were reported, but there was no reference to a protocol. |
| Other bias | Low risk | Comment: no other sources of bias were identified. |
Foa 2013.
| Study characteristics | ||
| Methods | Study design: randomised controlled trial | |
| Participants |
Inclusion criteria: “Inclusion criteria were female sex, age 13 to 18 years, and a primary diagnosis from the Diagnostic and Statistical Manual of Mental Disorders (Fourth Edition, Text Revision) of chronic or subthreshold PTSD related to sexual abuse that occurred at least 3months prior to assessment for the study. Subthreshold PTSD was defined as: 1 or more re‐experiencing symptoms, 2 or more avoidance symptoms, 2 or more arousal symptoms, and a total score of 14 or greater on the Child PTSD Symptom Scale–Interview.” (p 2651) Exclusion criteria: “current suicidal ideation with intent, uncontrolled bipolar disorder, schizophrenia, conduct disorder, pervasive developmental disorder, initiation of psychotropic medication within the previous 12 weeks, and current inpatient psychiatric treatment. Adolescents with substance use or suicidality without imminent threat were not excluded” (p 2651) Gender: all participants were girls Age: range = 7 to 13 years Type of abuse: not reported Onset of abuse: not reported Length of abuse: not reported Perpetrator of abuse: not reported |
|
| Interventions | Participants (n = 61) randomly assigned to one of two groups
|
|
| Outcomes |
Time points for assessment: baseline, mid‐treatment, post‐treatment, 3‐month follow‐up, 6‐month follow‐up, and 12‐month follow‐up Measures (outcomes): Child PTSD Symptom Scale–Interview (CPSS‐I; PTSD), Children’s Global Assessment Scale (CGAS; PTSD), Children Depression Inventory (CDI; depression), and Expectancy of Therapeutic Outcome for Adolescents (ETO‐A, satisfaction with treatment). The following outcomes were used for the quantitative analyses:
|
|
| Notes |
Start and end dates: no more information than "Data collection lasted from February 2006 through March 2012." (p 2650) Funding sources: "This study was conducted with support from the National Institute of Mental Health (R01 MH074505) awarded to Dr Foa." (p 2656) Study’s limitations as reported by the study's authors: “First, the pre‐randomization preparatory sessions may reduce generalizability to treatment studies in which participants are randomized immediately after the baseline evaluation. Second, the preparatory sessions occurred prior to randomization, which may have biased the sample by excluding inappropriate participants and including more motivated ones. Third, because the sample comprised female adolescents whose PTSD was related to sexual abuse, the results may not generalize to PTSD related to other types of traumas or to males” (p 2656) |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: the authors only report that participants were randomly assigned. |
| Allocation concealment (selection bias) | Low risk | Quote: “On completing the preparatory phase but prior to the patient beginning treatment, a research assistant consulted the randomisation table and notified the therapist of the patient’s treatment condition” (p 2651). |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: not mentioned and unlikely to have been done |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: “assessment was conducted by two psychologists blind to assignment” (p 2651) |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: the authors analysed data on an intention‐to‐treat (ITT) basis. |
| Selective reporting (reporting bias) | Low risk | Comment: all the outcomes reported in the trial registration were reported. |
| Other bias | Low risk | Comment: no other sources of bias were identified. |
Jaberghaderi 2004.
| Study characteristics | ||
| Methods | Study design: randomised controlled trial | |
| Participants |
Inclusion criteria: "Participants were eligible for inclusion if they met sexual abuse victimization criteria, whether or not they had experienced additional trauma as well" (p 366) Exclusion criteria: not reported Gender: all participants were girls Age: range = 12 to 13 years Type of abuse not reported Onset of abuse: not reported Length of abuse: not reported Perpetrator of abuse: not reported |
|
| Interventions | Participants (n = 14) randomly assigned to one of two groups
|
|
| Outcomes |
Time points for assessment: baseline and post‐treatment Measures (outcomes): Child Report of Post‐traumatic Symptoms (CROPS, post‐traumatic stress disorder), Children’s self‐report and Parent Report of Post‐traumatic Symptoms (PROPS, post‐traumatic stress disorder) , Rutter Teacher Scale, and Subjective Units of Distress Scale (SUDS) (children's distress). The following outcomes were used for the quantitative analyses:
|
|
| Notes |
Start and end dates: not reported Funding sources: not reported Study's limitations as reported by the study's authors: “Limitations include small N, single therapist for each treatment condition, no independent verification of treatment fidelity, and no long‐term follow‐up.” (p 358) |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: the authors only report that the participants were randomly allocated, not how randomisation was completed. |
| Allocation concealment (selection bias) | Unclear risk | Comment: not enough information to make a judgement |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: not mentioned and unlikely to have been done |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: “The assessment was by two psychologists, blind to assignment’ (p 362) |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Comment: the author did not perform analyses comparing completers and non‐completers. |
| Selective reporting (reporting bias) | Unclear risk | Comment: all the outcomes measured were reported, but there was no reference to a protocol. |
| Other bias | Low risk | Comment: no other sources of bias were identified. |
King 2000.
| Study characteristics | ||
| Methods | Study design: randomised controlled trial | |
| Participants |
Inclusion criteria: “Inclusion criteria were as follows: (1) The child and his or her nonoffending parents had to be English‐speaking. The term “parent” is used to indicate the primary caregiver and includes biological/ adoptive parents, foster parents, and other guardians. (2) There had to be a history of contact sexual abuse such as sexual touching, oral genital contact, or penile penetration of the vagina or anus, with or without physical force. For those cases in which the perpetrator was a child, he or she had to be 5 years older than the victimized child. (3) Independent validation of sexual abuse was required. In all cases a child was included only if the abuse had been substantiated by the sexual assault center, Department of Health and Community Services, or professionals/agencies with recognized expertise in conducting investigative evaluations. (4) The child’s symptoms met diagnostic criteria for PTSD or fell short of the diagnostic criteria for PTSD by several symptoms, but the child still experienced severe stress reactions. Deblinger et al. (1996, p. 312) noted that such children “might develop the full‐blown disorder in time” and are in need of treatment. Similar to the subjects of Deblinger et al. (1996), these children had to exhibit a total of 3 posttraumatic stress symptoms including at least one of avoidance or reexperiencing phenomena.” (p 1348) Exclusion criteria: “(1) ongoing, unsupervised contact with the alleged perpetrator; (2) severe intellectual disability, psychosis, or suicidal behavior; (3) taking antidepressant or antianxiety medication; and (4) child or parents not willing to participate” (p 1348) Gender: 69% of participants were girls Age: range = 5 to 17 years Type of abuse: genital fondling only (n = 5); vaginal/anal intercourse only (n = 7); digital penetration of anus/vagina only (n = 4); multiple types of abuse (n = 20) Onset of abuse: not reported Length of abuse: mean number of abusive episodes 7.64 (SD 3.84, range 1 to 33); time since last abusive experience: mean 4.54 years (SD 3.11, range 3 months to 8 years 10 months) Perpetrator of abuse: biological father (n = 4); stepfather (n = 3); family friend (n = 5); neighbor (n = 5); professional (n = 3); acquaintance (n = 8); older youth (n = 4); other (n = 4) |
|
| Interventions | Participants (n = 36) randomly assigned to one of three groups
|
|
| Outcomes |
Time points used for assessment: baseline, post‐treatment and 12‐week follow‐up Measures (outcomes): PTSD section of the Anxiety Disorders Interview Schedule for the DSM‐IV (ADIS; PTSD), Fear Thermometer for Sexually Abused Children (fear), Coping Questionnaire for Sexually Abused Children (children's coping strategies towards sexual abuse risk), Revised Children’s Manifest Anxiety Scale (R‐CMAS; anxiety), Children’s Depression Inventory (CDI; depression), Child Behaviour Checklist (CBCL; internalising and externalising behaviour), Global Assessment Functioning (GAF; children's global functioning). The following outcomes were used for the quantitative analyses:
|
|
| Notes |
Start and end dates: not reported Funding sources: not reported Study's limitations as reported by the study's authors: "The relatively small sample size is probably the most important methodological limitation, but several other constraints also deserve emphasis. First, the WLC controls for history and some of the demand characteristics and unreliability of the assessments but not the demand characteristics of the active treatments. Second, the multimeasure assessments were conducted by the therapists. Inasmuch as the therapists were aware of the child’s group assignment, we must acknowledge the possibility of experimenter bias. Third, 12‐week follow‐up assessments were carried out on the 3 groups.” (p 1354) |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: the authors only report that the participants were randomly allocated. |
| Allocation concealment (selection bias) | Unclear risk | Comment: not information to make a judgement |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: not mentioned and unlikely to have been done |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Comment: children's self‐reports and parents’ reports |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Comment: attrition at post‐test was not considered in the statistical analyses. |
| Selective reporting (reporting bias) | Unclear risk | Comment: all the outcomes measured were reported, but there was no reference to a protocol. |
| Other bias | Low risk | Comment: no other sources of bias were identified. |
Monck 1994.
| Study characteristics | ||
| Methods | Study design: randomised controlled trial | |
| Participants |
Inclusion criteria: '"All children between 4 and 16 years were included when sexual abuse had occurred more than once in the previous 2 years, disclosure was in the previous 12 months, and the abuser was a close family member or resident with the child" (p 1388 of the linked study Hyde 1995) Exclusion criteria: not reported Gender: 85% of participants were girls Age: range = 4 to 16 years Type of abuse: not penetrative (38%); penetrative (62%) Onset of abuse: not reported Length of abuse: up to 2 months (6%); 2 to 18 months (31%); 19 to 36 months (31%); 37 to 60 months (8%); 61 + months (15%) Perpetrator of abuse: biological parent (46%); surrogate parent (18%); brother (11%); other (25%) |
|
| Interventions | Participants (n = 47) randomly assigned to one of two groups
|
|
| Outcomes |
Time points for assessment: baseline and post‐treatment Measures (outcomes): Great Ormond Street Self‐image Profile (children's self‐image); General Health Questionnaire (GHQ; children's general health); Teacher's Behaviour Checklist (general behaviour of the child); An interview to the carer to identify somatic symptoms and behaviour disorder (general behaviour of the children); Self‐Esteem Checklist (children's self‐esteem), developed at the Institute of Child Health, based in part, on domains identified for children; Children's Depression Inventory (depression); Pictorial Scale of Perceived Competence and Social Acceptance for Children (children's acceptance and social competence); and Family Relations Test (FRT; family relations) We could not use the data from this study because no mean values or standard deviations of the outcome measures or the number of participants for whom the outcomes were measured were reported by the authors, and neither were other statistics to calculate or impute the data (e.g. standard errors, confidence intervals and P values). We tried to contact the authors but did not get a response. |
|
| Notes |
Start and end dates: not reported Funding sources: "The study was supported with a three‐year grant to Dr Arnon Bentovim from the Department of Health, and three‐month extension to Elizabeth Monck to lead on the analysis and writing of the report" (p 8) Study's limitations as reported by the study's authors: none reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk |
Quote: “Once it had been agreed that a family would take part in treatment, they were randomly allocated to one of two treatment modes” (p 12) Comment: no further details provided |
| Allocation concealment (selection bias) | Low risk | Quote: “Once it had been agreed that a family would take part in treatment, they were randomly allocated to one of two treatment modes: family treatment only or family treatment plus group treatment. This allocation was made without the direct involvement of the researchers or the clinical team and was achieved by blind choice of marked cards drawn from an envelope.” (p 12) |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Quote: “Although the original intention had been that the interviewer would also be blind to the treatment, this proved unrealistic as it usually became apparent at an early stage in this final interview.” (p 12) |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Comment: children's self‐report and parents’ self‐reports |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Comment: the authors did not report dropouts. Not information to make a judgement |
| Selective reporting (reporting bias) | Unclear risk | Comment: all the outcomes measured were reported, but there was no reference to a protocol. |
| Other bias | Low risk | Comment: no other sources of bias were identified. |
O'Callaghan 2013.
| Study characteristics | ||
| Methods | Study design: randomised controlled trial | |
| Participants |
Inclusion criteria: “'the researchers were advised to use the more general and less intrusive criteria of either having witnessed or having personally experienced rape or inappropriate sexual touch as the eligibility criteria" (p 360) Exclusion criteria: "Intellectual disability, psychosis, or severe emotional and behavioral problems (e.g. physical violence towards staff) that prevented group participation were the exclusion criteria." (p 360) Gender: all participants were girls. The sample for this study was "drawn from a group of 60 girls comprising minors rescued from brothels by a local non‐governmental organization (NGO; Conference Regionale del Afrique de l’ Ouest Francophone [CERAO]), victims of military and militia sexual violence and relatives of CERAO workers" (p 360) Age: range = 12 to 17 years Type of abuse: not reported. However, sexual abuse was defined as inappropriate sexual touch. Onset of abuse: not reported Length of abuse: not reported Perpetrator of abuse: not reported |
|
| Interventions | Participants (n = 52) randomly assigned to one of two groups
|
|
| Outcomes |
Time point for assessment: baseline and post‐treatment Measures (outcomes): University of California, Los Angeles‐Post‐traumatic Stress Disorder Reaction Index (UCLA‐PTSDR I; PTSD) and African Youth Psychosocial Assessment Instrument (AYPA), formerly known as Acholi Psychosocial Assessment Instrument (depression and anxiety) The following outcomes were used for the quantitative analyses:
|
|
| Notes |
Start and end dates: No more information than "Data were collected by the same outcome assessors at preintervention (May, 2011), 7 weeks later at postintervention (July, 2011), and at a 3‐month follow‐up (October, 2011)" (p 361) Funding sources: "This project was funded by World Vision, and by family and friends who contributed toward the carpentry and mechanics tools and the hygiene kits given to every girl in the study" (p 369) Study's limitations as reported by the authors: "The use of self‐reports, small sample size, and the use of exposure to a traumatic event (e.g., rape or sexual abuse) rather than the existence of disabling levels of distress." (p 365) |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Participants were randomly assigned to either the intervention or control group using a computer‐generated random sequence of numbers (www.random.org)." (p 362) |
| Allocation concealment (selection bias) | Low risk | Quote: "Selection bias was reduced by ensuring that treatment allocation was concealed from those responsible for participant enrolment and by ensuring that the person responsible for assigned participants had met none of the participants before the group allocation" (p 361‐2) |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: only the staff were blind. No information on the participants. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Comment: children's self‐reports |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: the authors analysed data on an intention‐to‐treat (ITT) basis. |
| Selective reporting (reporting bias) | Low risk | Comment: all the outcomes measured and stated in the registration of the trial were reported. |
| Other bias | Low risk | Comment: no other sources of bias were identified. |
Perez 1987.
| Study characteristics | ||
| Methods | Study design: randomised controlled trial | |
| Participants |
Inclusion criteria: “(a) the children were between the ages of four and nine, (b) the children were victims of incest or extrafamilial sexual abuse, (c) the abuse had come to the attention of the social service and/or police agency within a six month period of time, (d) the children were not currently in therapy or had not taken part in any kind of therapy in the past, (e) the children were available for twelve sessions of therapy, and (f) the children took part in the pre‐ and posttesting.” (p 37) Exclusion criteria: not reported Gender: 64% of participants were girls Age: range = 4 to 9 years Type of abuse: not reported Onset of abuse: not reported Length of abuse: not reported Perpetrator of abuse: not reported |
|
| Interventions | Participants (n = 55) randomly assigned to one of three groups
|
|
| Outcomes |
Time points for assessments: baseline and post‐treatment Outcomes: self concept and self‐mastery* Measures (outcomes): Primary Self‐Concept Inventory (PSCI; children's self‐concept) and Locus of Control Scale (LCS; children's locus of control) *Self‐concept and self‐mastery were not identified outcomes for this review. |
|
| Notes |
Start and end dates: not reported Funding sources: not reported Study’s limitations as reported by the study's authors: “This study was limited to children in the City and County of Denver# Colorado# who were diagnosed as having been victims of either incest or extrafamilial sexual abuse. Hence, the results and conclusions are restricted to similar geographical areas. This study was limited to child victims of sexual abuse between the ages of four and nine. Hence, the results and conclusions are suitable only to children within this age span. This study was further limited in that the sample was drawn from a pre‐selected group of children who were known to be victims of sexual abuse as determined through a social service and/or police investigation. Children who were suspected of being victims of sexual abuse were not included; therefore/ the results are valid only for known victims. Most of the victims in this study were involved with the juvenile court system and possibly the criminal court system. This limits the results to sexually abused children involved with outside legal systems. A further limitation was the similar socioeconomic status of the families participating in this study. Because families involved with the juvenile court systems tend to be from lower income families, the results of this study are valid for only these children. Similarly, because a large percentage of families from lower socioeconomic backgrounds are from minority (Hispanic and Black) descent, the results of this study are valid only for populations high in minority density. Another limitation of this study was the size of the population being studied. A larger population would allow for more confidence that the results of the sample are representative of the larger population. A final limitation was that this study evaluated only testing outcomes and did not measure the dynamics within the therapy that might have been different for each child.” (p 11‐3) |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: “Each child for whom permission was granted was matched according to gender and age using a random‐block technique (Johnson & Solso, 1971). Once matched, the children were randomly assigned to one of two treatment groups; group play therapy or individual play therapy; or to a control group receiving no therapy” (p 38) |
| Allocation concealment (selection bias) | High risk | Comment: not reported and unlikely to have been done |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: not reported and unlikely to have been done |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Comment: not reported and unlikely to have been done |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: no attrition reported |
| Selective reporting (reporting bias) | Unclear risk | Comment: all the outcomes measured were reported, but there was no reference to a protocol. |
| Other bias | Low risk | Comment: no other potential sources of bias were identified. |
Thun 2003.
| Study characteristics | ||
| Methods | Study design: randomised controlled trial | |
| Participants |
Inclusion criteria: not reported Exclusion criteria: not reported Gender: all participants were female adolescents, who had been identified as “at risk” youth: "They had dropped out of school and had volunteered for a military based residential program designed to assist them in getting their Graduate Equivalency Degree" (p 6) Age: range = 16 to 18 years Type of abuse: not reported. However, in this study "sexual abuse was defined as having a sexual experience with someone at least five years older if the subject was 13 or younger, or having a sexual experience with someone 10 years older if the subject was 14 or older." (p 7) Onset of abuse: not reported Length of abuse: not reported Perpetrator of abuse: not reported |
|
| Interventions | Participants (n = 13) randomly assigned to one of two groups
|
|
| Outcomes |
Time points for assessments: baseline and post‐treatment Measures (outcomes): Personal History Questionnaire (children's personal history) and Offer Self‐Image Questionnaire‐Revised (OSIQ‐R; children's self‐image) Self‐image is not an outcome of interest in this review. Therefore, we did not incorporated these data in the review. |
|
| Notes |
Start and end dates: not reported Funding sources: not reported Study’s limitations as reported by the study's authors: “A lack of statistical support in this pilot study for the effect of group therapy on sexually abused adolescent females may be due to the small sample size and the resulting limited statistical power. It is possible that a larger sample size would have revealed significant findings. In addition, it is possible that the participants in this study are not representative of the general population of female adolescent survivors of sexual abuse, since all the participants in this study were “at risk” high school dropouts. Therefore, these results cannot be generalized to female adolescent survivors of sexual abuse who do not drop out of school.” (p 12) |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: the authors only reported that participants were randomly allocated. |
| Allocation concealment (selection bias) | Unclear risk | Comment: not enough information to make a judgement |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: not mentioned and unlikely to have been done |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Comment: participants' self‐reports |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Comment: no further details than two of the six participants allocated to the experimental condition dropped out. The authors did not mention the implications of the dropouts in the results. |
| Selective reporting (reporting bias) | Unclear risk | Comment: all the outcomes measured were reported, but there was no reference to a protocol. |
| Other bias | Low risk | Comment: no other potential sources of bias were identified. |
Trowell 2002.
| Study characteristics | ||
| Methods | Study design: randomised controlled trial | |
| Participants |
Inclusion criteria: "Contact sexual abuse had occurred on the basis of balance of probabilities verified by social services and/or court procedure; 6 to 14 years old; consent from the child and the legal guardian; symptoms of behavioural disturbance; abuse disclosed 2 years before referral” (p 235) Exclusion criteria: “Developmental delay, psychosis, lack of reasonable confidence that further abuse would not occur and necessity for hospitalization at the time of initial assessment” (p 235) Gender: all participants were girls Age: range = 6 to 14 years Type of abuse: touching without or with clothes (16.90%), genital touching or simulated intercourse (38.02%), oral anal or vaginal penetration (45.07%) Onset of abuse: not reported Length of abuse: more than 10 abusive incidents (54.92%); more than 2 years duration (38.02%) Perpetrator of abuse: parent (42.25%); more than one abuser (35.21%) |
|
| Interventions | Participants (n = 71) randomly assigned to one of two groups
|
|
| Outcomes |
Time points for assessments: baseline, 1‐year follow‐up, and 2 year follow‐up Measures: Orvaschel’s scales for PTSD and the Kiddie Global Assessment Scale (K‐GAS) (both for PTSD). The following outcomes were used for the quantitative analyses:
|
|
| Notes |
Start and end dates: not reported Funding sources: "The research was funded by the Department of Health and the Mental Health Foundation. The Tavistock Centre has provided additional support and resources" (p 246) Study’s limitations as reported by the study's authors: “The design consisted of a comparison of two active treatment groups; and the treatment groups were small which resulted in reduced power in statistical analysis” (p 245) |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: the authors only reported that the participants were randomly allocated and did not provide specific information. |
| Allocation concealment (selection bias) | Unclear risk | Comment: not enough information to make a judgement |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: the authors stated that it was not possible to blind participants. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Comment: the authors stated that blinding of assessors was compromised because the children and the carers identified the specific therapy during the assessments. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: the authors analysed participants based on ‘assigned treatment’ rather than ‘treatment completed’ to try to minimise the potential attrition bias. |
| Selective reporting (reporting bias) | Unclear risk | Comment: all the outcomes measured were reported, but there was no reference to a protocol. |
| Other bias | Low risk | Comment: no other potential sources of bias were identified. |
ADIS: Anxiety Disorders Interview Schedule for the DSM‐IV. ANCOVA: analysis of covariance. AYPA: African Youth Psychosocial Assessment Instrument (formerly known as Acholi Psychosocial Assessment Instrument). CAPS: Children’s Attributions and Perceptions Scale. CBCL: Child Behaviour Checklist. CBP: Achenbach Child Behaviour Checklist and Profile. CBT: cognitive behaviour therapy. CCT: child centered therapy. CDI: Children's Depression Inventory. CERAO: Conference Regionale del Afrique de l’ Ouest Francophone. CGAS: Children's Global Assessment Scale. CITES‐R: Children's Impact of Traumatic Events Scales‐‐Revised. CMAS: Children's Manifest Anxiety Scale. CPS: Child Protection System CPSS‐I: Child PTSD Symptom Scale–Interview. CROPS: Child Report of Post‐traumatic Symptoms. CSA: child sexual abuse. CSBI: Child Sexual Behaviour Inventory. DSM‐III‐R: Diagnostic and Statistical Manual of Mental Disorders, Third Edition, Revised. DSM‐IV: Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition. DYFS: Division of Youth and Family Services EMDR: eye movement desensitisation and reprocessing. ETOA: Expectancy of Therapeutic Outcome for Adolescents. FES: Family Environment Scale. FRT: Family Relations Test. FSSC‐R: Fear Survey Schedule for Children‐Revised. FT: family therapy. GAF: Global Assessment Functioning. GHQ: General Health Questionnaire. IES: Impact of Events Scale. IES‐R: Impact of Events Scale‐Revised. IQ: intelligence quotient. ITT: intention‐to‐treat. K‐GAS: Kiddie Global Assessment Scale. K‐SADS‐E: Kiddie‐Schedule for Affective Disorders and Schizophrenia for School‐Age Children. K‐SADS‐PL: Kiddie‐Schedule for Affective Disorders and Schizophrenia‐Present and Lifetime Version. LCS: Locus of Control Scale. MASC: Multidimensional Anxiety Scale for Children. MASTR: motivation‐adaptive skills‐trauma resolution. MASTR‐EMDR: motivation‐adaptive skills‐trauma resolution and eye movement desensitisation and reprocessing. MAU: management as usual. n: number. NARSAD: National Alliance for Research on Schizophrenia & Depression NGO: non‐governmental organisation. NIDA: National Institute on Drug Abuse. OSIQ‐R: Offer Self‐Image Questionnaire‐Revised. P: page number. PAS: Parental Attribution Scale. PD: Psychodynamic Therapy. PERQ: Parent’s Emotional Reaction Questionnaire. PI: principal investigator. PPQ: Parenting Practices Questionnaire. PRESS: Preschool Symptom Self‐Report. PRIDS: Parent Reaction to Incest Disclosure Scale. PROPS: Children’s self‐report and Parent Report of Post‐traumatic Symptoms. PSCI: Primary Self‐Concept Inventory. PSQ: Parental Support Questionnaire. PTSD: post‐traumatic stress disorder. R‐CMAS: Revised Children’s Manifest Anxiety Scale. RRFT: Risk Reduction Family Therapy SAFE: Sexual Abuse Fear Evaluation Scales. SD: standard deviation. SSQ: Social Support Questionnaire. STAIC: State‐Trait Anxiety Inventory for Children (STAIC). SUDS: Subjective Units of Distress Scale. TAU: treatment as usual. TFCBT: Trauma Focused Cognitive Behavioural Therapy TLFB: Timeline Follow Back Interview. TSCC: Trauma Symptom Checklist for Children. UCLA PTSD Index for DSM‐IV‐Adolescent & Caregiver versions: University of California Posttraumatic Stress Disorder Index UCLA‐PTSD R I: University of California, Los Angeles‐Post‐Traumatic Stress Disorder Reaction Index. WBR: Weekly Behavior Report. WIST: What If Situations Test. WL: waiting list. WLC: wait‐list control.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Ancha 2003 | Not a randomised controlled trial |
| Bagley 2000 | Not a randomised controlled trial |
| Bicanic 2014 | Not a randomised controlled trial |
| Bowers 1992 | Not a randomised controlled trial |
| Cloitre 2004 | Not a randomised controlled trial. Summary of Cohen 2004 |
| Crugnola 2014 | Not a randomised controlled trial |
| De luca 1995 | Not a randomised controlled trial |
| Echeburúa 1997 | Not a randomised controlled trial |
| Friedrich 1992b | Not a randomised controlled trial |
| Gouweloos 2011 | Not a randomised controlled trial |
| Habigzang 2013 | Not a randomised controlled trial |
| Hahn 2016 | Not a randomised controlled trial |
| Hall‐Marley 1993 | Not a randomised controlled trial |
| Homstead 1986 | Not a randomised controlled trial |
| Hubel 2014 | Not a randomised controlled trial |
| Hébert 2010 | Not a randomised controlled trial |
| Karatzias 2014 | Not sexually abused children. Participants older than 18 years old. |
| Liotta 2015 | Not a randomised controlled trial |
| McGain 1995 | Not a randomised controlled trial |
| Misurell 2014 | Not a randomised controlled trial |
| Nolan 2002 | Not a randomised controlled trial |
| NTR6678 | Not sexually abused children. Participants older than 18 years old. |
| Osen 2007 | Not a randomised controlled trial |
| Reeker 1998 | Not a randomised controlled trial |
| Resick 2003 | Not a randomised controlled trial |
| Robinson 1989 | Not a randomised controlled trial |
| Roos 2021 | Not sexually abused children. Mixed sample (less than the 50% of the sample experienced sexual abuse). |
| Rosner 2019 | Mixed sample. Less than the 50% of the sample were child sexual abused children. |
| Silveria 1993 | Not a randomised controlled trial |
| Simoneau 2008 | Not a randomised controlled trial |
| Stauffer 1996 | Not a randomised controlled trial |
| Steil 2015 | Not a randomised controlled trial |
| Sullivan 1992 | Not a randomised controlled trial |
| Tourigny 1998 | Not a randomised controlled trial |
| Waters 1998 | Not a randomised controlled trial |
| Wolf 1993 | Not a randomised controlled trial |
Characteristics of studies awaiting classification [ordered by study ID]
Danielson 2016.
| Methods | Design: randomised controlled trial |
| Participants | "To date, 96 adolescents aged 13–18 years (mean 15.4, SD 1.2; 87 percent girls; 42 percent ethnic/racial minority; 81 percent sexual abuse; 30 percent physical abuse; 45 percent witnessed violence; > 50 percent multiple forms of child maltreatment) have been randomized to receive RRFT or treatment as usual (TAU)." (p S293) |
| Interventions |
Intervention: risk reduction family therapy Comparator: treatment as usual |
| Outcomes |
"Youth and caregivers completed interviews and questionnaires at pretreatment baseline" (p S293) Timing of outcome assessment: 3‐, 6‐, 12‐, and 18‐month follow‐up |
| Notes |
Funding sources: supported by NIDA Grants R01 DA031285 and K24 029783. Current status of the study: unknown. We tried to contact the authors but did not get a response. |
NIDA: National Institute on Drug Abuse; RRFT: risk reduction family therapy; SD: standard deviation
Characteristics of ongoing studies [ordered by study ID]
Amirzadegan 2018.
| Study name | Comparison the efficiency of play and narrative therapy on decreasing depression, anxiety and aggression of sexually abused children in Tehran |
| Methods | Design: randomised controlled trial |
| Participants |
Sample size: 45 participants Age range: children between 7 and 12 years old Setting: Rooyesh Nahal Tehran Institute Study date: 2017 |
| Interventions |
Intervention (n = 30)
Comparator (n = 15): waiting list |
| Outcomes |
Timing of outcome assessment: baseline and post‐treatment |
| Starting date | Not reported |
| Contact information |
Name: S Ghahari (corresponding author) Address: Department of Mental Health, School of Behavioral Sciences and Mental Health, Tehran Institute of Psychiatry, Iran University of Medical Sciences (IUMS), Tehran, Iran; Psychiatry and Behavioral Sciences Research Center, Addiction Institute, Mazandaran University of Medical Sciences, Sari, Iran, Tehran, Iran Telephone: not reported Email: not reported |
| Notes |
Funding sources: not reported Current status of the study: unknown. We tried to contact the authors but did not get a response. |
NCT00073684.
| Study name |
Public title: Optimal treatment strategies for sexually abused children Official title: Young sexually abused children: optimal cognitive behavioural strategies |
| Methods | Design: randomised controlled trial |
| Participants |
Sample size: 210 sexually abused children aged between 4 to 11 years old Inclusion criteria
Exclusion criteria
|
| Interventions |
Interventions to compare: 4 variations of trauma focused cognitive behavioral therapy:
|
| Outcomes |
Primary outcome(s)
Secondary outcome(s)
Timing of outcome assessment: months 6 and 12 |
| Starting date | August 2003. Registered on ClinicalTrials.Gov on 2 December 2003 |
| Contact information |
Name: not reported Address: not reported Telephone: not reported Email: not reported |
| Notes |
Funding sources: No further information than "Sponsors and collaborators: Rowan University and the National Institute of Mental Health (NIMH))" Current status of the study: not reported |
DSM‐IV: Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition; IQ: intelligence quotient; n: number of participants;
Differences between protocol and review
In the table below, we list post‐protocol changes per section of the review. Methods that we were not able to use in this version of the review are reported in Table 34 below.
Table 34 Differences between protocol and review
| Section | Protocol | Review |
| Objectives | To assess the relative effectiveness of psychological therapies, compared to other treatments or no treatment controls, to overcome psychological consequences of sexual abuse in children and young people up to 18 years of age. Secondary objectives
|
"To assess the relative effectiveness of psychological interventions compared to other treatments or no treatment controls, to overcome psychological consequences of sexual abuse in children and young people up to 18 years of age using network meta‐analysis. Secondary objectives
We were unable to address one of the secondary objectives because there were not enough studies to conduct the proposed analysis: subgroup analyses to assess the impact of moderator variables on treatment outcomes. If this is possible in later versions of the review, we will use the methods set out in the protocol. |
| Types of participants | All children and adolescents up to 18 years of age who have experienced any kind of sexual abuse (see Description of the condition). | "We included studies with participants aged 0 to 18 years old of both sexes, who had experienced any form of child sexual abuse, as described under Description of the condition. We limited the syntax of our searches to randomised controlled trials assessing the effectiveness of psychotherapies for the consequences of child sexual abuse/rape/incest/molestation and similar terms in children and adolescents up to 18 years old. However, the searches found some trials with mixed samples (e.g. participants that experienced child sexual abuse with physical abuse or other traumatic experiences simultaneously). We excluded these studies for the following reasons: 1) separate results for participants experiencing only child sexual abuse were not reported; 2) the randomisation was not stratified by the specific type of abuse or traumatic experience; 3) the participants experiencing CSA were less than the 50% of the sample; and 4) individual data were not available. We excluded studies with participants over the age of 18, unless data for children and adolescents aged 18 or under were reported separately. We also excluded studies whose participants included children and young people who had experienced a range of maltreatment, unless the data for those who had been sexually abused were available or reported separately." We have included these additional details to clarify why we excluded studies with mixed types of abuse and with participants older than 18 years old. We expanded on these criteria to clarify how we handled mixed samples. |
| Measures of treatment effects > Relative treatment rankings | We will also estimate the ranking probabilities for each treatment. This is the probability that each treatment is the first, second, third, etc., best in the network. We will obtain a treatment hierarchy using the surface under the cumulative ranking curve (SUCRA) and mean ranks. SUCRA can also be expressed as percentage and interpreted as the percentage of efficacy or safety of treatment that would be ranked first without uncertainty (Chaimani 2013). | We were advised not to report the rankings as they could be misleading due to the uncertainty of the effect estimates and the low number of studies informing the networks. |
| Unit of analysis issues > Studies with multiple treatment groups | For studies including multiple treatment groups, we will include each pairwise comparison separately. When variables are binary, we will divide the shared intervention group evenly among the comparisons (only in pairwise comparisons); when variables are continuous, we will divide only the total number of participants ‐ we will leave the means and standard deviations unchanged. This will avoid double counting the participants in the pooled estimate of treatment effect, while retaining information from each arm of the trial. The network meta‐analysis will consider the correlation between the effect sizes from multi‐arm studies (Higgins 2021a). | "For both pairwise comparisons and network meta‐analyses, when a study involved more than two treatment arms, we did not combine them. Rather, we kept the arms separate, to investigate heterogeneity across intervention arms (e.g. the difference between delivering CBT to the child only, to the non‐offending carer only, or to the child and the non‐offending carer together). For pairwise comparisons and continuous outcomes, we divided the number of participants of the control group evenly between the number of experimental groups to avoid double counting of participants and used the original means and standard deviations. An NMA accounts for the correlation between correlated comparisons from the same study. Therefore, each arm can be differentiated in separated nodes to be included in the networks and there is no need to divide the number of participants of the control group (Higgins 2021a)." We added additional details to justify why we kept the arms separated when analysing multiple treatment groups. We did this to investigate heterogeneity across intervention arms (e.g. the difference between delivering CBT to the child only, to the non‐offending carer only, or to the child and the non‐offending carer together). |
| Assessment of reporting biases | Not included in the protocol. | For each comparison where we had more than 10 trials reporting on an outcome, we planned to explore if the studies with larger effect sizes were more likely to be published than studies with smaller effect sizes (publication bias) (Higgins 2021a). For this, we would have used an extension of the funnel plot scatter used for meta‐analysis (comparison‐adjusted funnel plots), which accounts for the different treatment comparisons included in the networks (Chaimani 2012; Chaimani 2013; White 2015). The X axis of the graph represents the size of the effect estimates and the Y axis represents a measure of dispersion (the standard error of the effect estimate). The effect estimates from larger studies (larger samples) are more precise than those from smaller studies. The former are expected to scatter more narrowly at the top of the inverted funnel and the latter to scatter more widely at the bottom of the funnel. In the absence of publication bias, effect estimates spread symmetrically (Higgins 2021a). We were unable to perform comparison‐adjusted or conventional funnel plots due to the nature and number of the included studies (Differences between protocol and review). For conclusions from these graphs to be meaningful, all the comparisons across studies must be defined in a consistent direction (active versus inactive interventions, newer versus older treatment, or sponsored versus non sponsored treatment). For none of these cases there were at least 10 studies to plot the graphs (10 or more studies are recommended to draw valid conclusions) (Higgins 2021a, Chapter 13, section 13.3.5.4 Tests for funnel plot asymmetry). |
| Summary of findings and assessment of the certainty of the evidence | We will include tables reporting the characteristics, risk of bias and treatment effect sizes of the included studies. We will create summary of findings tables for the comparisons and outcomes marked with an asterisk under the Types of outcome measures section at two time points: immediately and up to one year after the treatment. Finally, we will use the Confidence in Network Meta‐Analysis online tool (CINeMA) based on the GRADE approach proposed by the GRADE Working Group, to make judgements about how the statistical contributions of the direct comparisons contribute to the credibility of NMA treatment effects (CINeMA 2017; Salanti 2014). |
We included tables reporting the characteristics, risk of bias and treatment effect sizes of the included studies. We created summary of findings tables for multiple comparisons for the outcomes marked with an asterisk under the Types of outcome measures section, only at post‐treatment as we were not able to perform network meta‐analyses for all outcomes at six or 12 months follow‐up. Finally, we used the Confidence in Network Meta‐analysis online tool (CINeMA) based on the approach developed by the GRADE Working Group to examine the quality of the evidence (CINeMA 2017; Salanti 2014). We made judgements of high, moderate, low or very low confidence in the evidence by assessing the level of concerns (major concerns, some concerns, no concerns, or undetected) in each of the following dimensions:
We changed the original time points proposed for summary of findings tables because we were not able to perform network meta‐analyses for all outcomes at six or 12 months follow‐up. Also, we provided more details on the specific criteria on which the GRADE analysis is based. |
Contributions of authors
PC, WT and GM were involved in the conception, design and co‐ordination of the review; PC searched the electronic databases and other resources for studies; the three authors screened and selected studies for inclusion; PC and GM extracted the data from the studies and compared them with data extracted for previous reviews that included some of the trials included in this review; PC and WT assessed the risk of bias of the included studies; PC and DC undertook the statistical analysis of the data and the assessment of the certainty in the body of evidence; and PC, WT, DC and GM interpreted the data and participated in the writing of the review.
GM and WT both have relevant clinical expertise in systematic reviews, and knowledge of the relevant literature. DC has relevant statistical expertise in systematic reviews, meta‐analyses and network meta‐analyses. PC has expertise in network meta‐analysis, which she gained from completing a network meta‐analysis course as part of her doctoral studies and from contributing to other network meta‐analyses in her working as research assistant.
Sources of support
Internal sources
There were no internal sources of support, Other
External sources
-
University of Los Andes, Colombia
Provided financial support to cover the living costs and tuition fees for the first year of Paola Caro's PhD degree
-
Administrative Department of Science and Technology, Colombia
Provided finanicial support to cover the living costs and tuition fees for the second to fourth years of Paola Caro's PhD degre
Declarations of interest
Paola Caro reports that she has no conflicts of interest.
William Turner is an Editor with Cochrane Developmental, Psychosocial and Learning Problems (CDPLP). He was not involved in the editorial process for this review.
Deborah Caldwell reports that she has no conflicts of interest.
Geraldine Macdonald is the Co‐ordinating Editor of CDPLP. She was not involved in the editorial process for this review.
New
References
References to studies included in this review
Baker 1985 {published data only}
- Baker CR. A Comparison of Individual and Group Therapy as Treatment of Sexually Abused Adolescent Females. Maryland (MD): University of Maryland, College Park, 1985. [Google Scholar]
Berliner 1996 {published data only}
- Berliner L, Saunders BE. Treating fear and anxiety in sexually abused children: results of a controlled 2-year follow-up study. Child Maltreatment 1996;1(4):294-309. [DOI: 10.1177/1077559596001004002] [DOI] [Google Scholar]
Burke 1988 {published data only}
- Burke, M. Short-Term Group Therapy for Sexually Abused Girls: A Learning Theory Based Treatment for Negative Affect. PhD thesis 1988.
Celano 1996 {published data only}
- Celano M, Hazzard A, Webb C, McCall C. Treatment of traumagenic beliefs among sexually abused girls and their mothers: an evaluation study. Journal of Abnormal Child Psychology 1996;24(1):1-17. [DOI: 10.1007/BF01448370] [PMID: ] [DOI] [PubMed] [Google Scholar]
Cohen 1996 {published data only}
- Cohen JA, Mannarino AP. A treatment outcome study for sexually abused preschool children: initial findings. Journal of the American Academy of Child & Adolescent Psychiatry 1996;35(1):42-50. [DOI: 10.1097/00004583-199601000-00011] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Cohen JA, Mannarino AP. A treatment study for sexually abused preschool children: outcome during a one-year follow-up. Journal of the American Academy of Child & Adolescent Psychiatry 1997;36(9):1228-35. [DOI: 10.1097/00004583-199709000-00015] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Cohen JA, Mannarino AP. Factors that mediate treatment outcome of sexually abused preschool children. Journal of the American Academy of Child & Adolescent Psychiatry 1996;35(10):1402-10. [DOI: 10.1097/00004583-199610000-00028] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Cohen JA, Mannarino AP. Factors that mediate treatment outcome of sexually abused preschool children: six- and 12-month follow-up. Journal of the American Academy of Child & Adolescent Psychiatry 1998;37(1):44-51. [DOI: 10.1097/00004583-199801000-00016] [PMID: ] [DOI] [PubMed] [Google Scholar]
Cohen 1998 {published data only}
- Cohen JA, Mannarino AP, Knudsen K. Treating sexually abused children: 1 year follow-up of a randomized controlled trial. Child Abuse & Neglect 2005;29(2):135-45. [DOI: 10.1016/j.chiabu.2004.12.005] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Cohen JA, Mannarino AP. Interventions for sexually abused children: initial treatment outcome findings. Child Maltreatment 1998;3(1):17-26. [DOI: 10.1177/1077559598003001002] [DOI] [Google Scholar]
- Cohen JA, Mannarino AP. Predictors of treatment outcome in sexually abused children. Child Abuse & Neglect 2000;24(7):983-94. [DOI: 10.1016/s0145-2134(00)00153-8] [PMID: ] [DOI] [PubMed] [Google Scholar]
Cohen 2004 {published data only}
- Cohen JA, Deblinger E, Mannarino AP, Steer RA. A multisite, randomized controlled trial for children with sexual abuse-related PTSD symptoms. Journal of the American Academy of Child & Adolescent Psychiatry 2004;43(4):393-402. [DOI: 10.1097/00004583-200404000-00005] [PMCID: PMC1201422] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deblinger E, Mannarino AP, Cohen JA, Steer RA. A follow-up study of a multisite, randomized, controlled trial for children with sexual abuse-related PTSD symptoms. Journal of the American Academy of Child & Adolescent Psychiatry 2006;45(12):1474-84. [DOI: 10.1097/01.chi.0000240839.56114.bb] [PMID: ] [DOI] [PubMed] [Google Scholar]
Costas 1999 {published data only}
- Costas M, Landreth G. Filial therapy with nonoffending parents of children who have been sexually abused. International Journal of Play Therapy 1999;8(1):43-66. [DOI: 10.1037/h0089427] [DOI] [Google Scholar]
Danielson 2012 {published data only}
- Danielson CK, McCart MR, Walsh K, De Arellano MA, White D, Resnick HS. Reducing substance use risk and mental health problems among sexually assaulted adolescents: a pilot randomized controlled trial. Journal of Family Psychology 2012;26(4):628-35. [DOI: 10.1037/a0028862] [PMCID: PMC3419329] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Deblinger 1996b {published data only}
- Deblinger E, Lippmann J, Steer R. Sexually abused children suffering posttraumatic stress symptoms: initial treatment outcome findings. Child Maltreatment 1996;1(4):310-21. [DOI: 10.1177/1077559596001004003] [DOI] [Google Scholar]
- Deblinger E, Steer RA, Lippmann J. Two-year follow-up study of cognitive behavioral therapy for sexually abused children suffering post-traumatic stress symptoms. Child Abuse & Neglect 1999;23(12):1371-8. [DOI: 10.1016/s0145-2134(99)00091-5] [PMID: ] [DOI] [PubMed] [Google Scholar]
Deblinger 2001 {published data only}
- Deblinger E, Stauffer LB, Steer RA. Comparative efficacies of supportive and cognitive behavioral group therapies for young children who have been sexually abused and their nonoffending mothers. Child Maltreatment 2001;6(4):332-43. [DOI: 10.1177/1077559501006004006] [PMID: ] [DOI] [PubMed] [Google Scholar]
Deblinger 2011 {published data only}
- Deblinger E, Mannarino AP, Cohen JA, Runyon MK, Steer RA. Trauma-focused cognitive behavioral therapy for children: impact of the trauma narrative and treatment length. Depression & Anxiety 2011;28(1):65-75. [DOI: 10.1002/da.20744] [PMCID: PMC6675414] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mannarino AP, Cohen JA, Deblinger E, Runyon MK, Steer RA. Trauma-focused cognitive-behavioral therapy for children: sustained impact of treatment 6 and 12 months later. Child Maltreatment 2012;17(3):231-41. [DOI: 10.1177/1077559512451787] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Dominguez 2001 {published data only}
- Dominguez RZ. Evaluation of Cognitive-Behavioral and Supportive Treatments for Sexually Abused Children: Analyzing the Process of Change Using Individual Growth Curve Analyses [PhD thesis]. Houston (TX): University of Houston, 2001. [Google Scholar]
Farkas 2008 {published data only}
- Farkas L, Lebeau T, McDuff P, Cyr M, Lemay J. Treatment Effectiveness of MASTR-EMDR Therapy for Sexually Abused Adolescents [L’efficacité de l’approche MASTR-EMDR auprès d’adolescent(e)s qui ont été agressé(e)s sexuellement]. Revue Québécoise de Psychologie 2008;29(3):101-15. [Google Scholar]
- Farkas L. The Effects of Motivation-Adaptive Skills-Trauma Resolution (MASTR) - Eye Movement Desensitization and Reprocessing (EMDR) on Traumatized Adolescents with Conduct Problems [PhD thesis]. Montréal (QC): Université de Montréal, 2008. [URL: core.ac.uk/download/pdf/55649056.pdf] [Google Scholar]
Foa 2013 {published data only}
- Brown LA, Belli G, Suzuki N, Capaldi S, Foa EB. Reduction in suicidal ideation from prolonged exposure therapy for adolescents. Journal of Clinical Child & Adolescent Psychology 2020;49(5):651-9. [DOI: 10.1080/15374416.2019.1614003] [PMCID: PMC6885098] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Capaldi S, Asnaani A, Zandberg LJ, Carpenter JK, Foa EB. Therapeutic alliance during prolonged exposure versus client-centered therapy for adolescent posttraumatic stress disorder. Journal of Clinical Psychology 2016;72(10):1026-36. [DOI: 10.1002/jclp.22303] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Foa EB, McLean CP, Capaldi S, Rosenfield D. Prolonged exposure vs supportive counseling for sexual abuse-related PTSD in adolescent girls: a randomized clinical trial. JAMA 2013;310(24):2650-7. [DOI: 10.1001/jama.2013.282829] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Kaczkurkin AN, Asnaani A, Zhong J, Foa EB. The moderating effect of state anger on treatment outcome in female adolescents with PTSD. Journal of Traumatic Stress 2016;29(4):325-31. [DOI: 10.1002/jts.22116] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLean CP, Su Y-J, Carpenter JK, Foa EB. Changes in PTSD and depression during prolonged exposure and client-centered therapy for PTSD in adolescents. Journal of Clinical Child & Adolescent Psychology 2017;46(4):500-10. [DOI: 10.1080/15374416.2015.1012722] [PMCID: PMC4564358] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zandberg L, Kaczkurkin AN, McLean CP, Rescorla L, Yadin E, Foa EB. Treatment of adolescent PTSD: the impact of prolonged exposure versus client-centered therapy on co-occurring emotional and behavioral problems. Journal of Traumatic Stress 2016;28(6):507-14. [DOI: 10.1002/jts.22138] [PMCID: PMC7367099] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Jaberghaderi 2004 {published data only}
- Jaberghaderi N, Greenwald R, Rubin A, Zand SO, Dolatabadi S. A comparison of CBT and EMDR for sexually-abused Iranian girls. Clinical Psychology & Psychotherapy 2004;11(5):358-68. [DOI: 10.1002/cpp.395] [DOI] [Google Scholar]
King 2000 {published data only}
- King NJ, Tonge BJ, Mullen P, Myerson N, Heyne D, Rollings S, et al. Treating sexually abused children with posttraumatic stress symptoms: a randomized clinical trial. Journal of the American Academy of Child & Adolescent Psychiatry 2000;39(11):1347-55. [DOI: 10.1097/00004583-200011000-00008] [PMID: ] [DOI] [PubMed] [Google Scholar]
Monck 1994 {published data only}
- Hyde C, Bentovim A, Monck E. Some clinical and methodological implications of a treatment outcome study of sexually abused children. Child Abuse & Neglect 1995;19(11):1387-99. [DOI: 10.1016/0145-2134(95)00096-q] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Monck E, Bentovim A, Goodall G, Hyde C, Lewin B, Sharland E. Child Sexual Abuse: A Descriptive and Treatment Outcome Study. London, UK: Her Majesty's Stationary Office (HMSO), 1994. [Google Scholar]
O'Callaghan 2013 {published data only}
- O'Callaghan P, McMullen J, Shannon C, Rafferty H, Black A. A randomized controlled trial of trauma-focused cognitive behavioral therapy for sexually exploited, war-affected Congolese girls. Journal of the American Academy of Child & Adolescent Psychiatry 2013;52(4):359-69. [DOI: 10.1016/j.jaac.2013.01.013] [PMID: ] [DOI] [PubMed] [Google Scholar]
Perez 1987 {published data only}
- Perez CL. A Comparison of Group Play Therapy and Individual Play Therapy for Sexually Abused Children [EdD thesis]. Greenley (CO): University of Northern Colorado, 1987. [Google Scholar]
Thun 2003 {published data only}
- Thun D, Sims PL, Adams MA, Webb T. Effects of group therapy on female adolescent survivors of sexual abuse: a pilot study. Journal of Child Sexual Abuse 2003;11(4):1-16. [DOI: 10.1300/J070v11n04_01] [PMID: ] [DOI] [PubMed] [Google Scholar]
Trowell 2002 {published data only}
- McCrone P, Weeramanthri T, Knapp M, Rushton A, Trowell J, Miles G, et al. Cost-effectiveness of individual versus group psychotherapy for sexually abused girls. Child and Adolescent Mental Health 2005;10(1):26-31. [DOI: 10.1111/j.1475-3588.2005.00113.x] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Trowell J, Kolvin I, Weeramanthri T, Sadowski H, Berelowitz M, Glaser D, et al. Psychotherapy for sexually abused girls: psychopathological outcome findings and patterns of change. British Journal of Psychiatry 2002;180:234‐47. Erratum in: British Journal of Psychiatry 2002;180(6):553. DOI: 10.1192/S0007125000161306. [DOI: 10.1192/bjp.180.3.234] [PMID: ] [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Ancha 2003 {published data only}
- Ancha AJ. Program evaluation of a time-limited, abuse-focused treatment for child and adolescent sexual abuse victims and their families [PsyD thesis]. Ann Arbor (MI): Argosy University, 2003. [Google Scholar]
Bagley 2000 {published data only}
- Bagley C, LaChance M. Evaluation of a family-based programme for the treatment of child sexual abuse. Child & Family Social Work 2000;5(3):205-13. [DOI: 10.1046/j.1365-2206.2000.00162.x] [DOI] [Google Scholar]
Bicanic 2014 {published data only}
- Bicanic I, De Roos C, Van Wesel F, Sinnema G, Van de Putte E. Rape-related symptoms in adolescents: short- and long-term outcome after cognitive behavior group therapy. European Journal of Psychotraumatology 2014;5:22969. [DOI: 10.3402/ejpt.v5.22969] [PMCID: PMC4048594] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Bowers 1992 {published data only}
- Bowers JJ. Therapy through art. Facilitating treatment of sexual abuse. Journal of Psychosocial Nursing and Mental Health Services 1992;30(6):15-24. [DOI: 10.3928/0279-3695-19920601-07] [PMID: ] [DOI] [PubMed] [Google Scholar]
Cloitre 2004 {published data only}
- Cloitre M, Stovall-McClough KC, Miranda R, Chemtob CM. Therapeutic alliance, negative mood regulation, and treatment outcome in child abuse-related posttraumatic stress disorder. Journal of Consulting and Clinical Psychology 2004;72(3):411-6. [DOI: 10.1037/0022-006X.72.3.411] [PMID: ] [DOI] [PubMed] [Google Scholar]
Crugnola 2014 {published data only}
- Crugnola CR, Ferro V, Ierardi E, Tadele T, Orlandini A. Assessment of the effectiveness of a psycho-pedagogical and counselling intervention program with Ethiopian young girls who were victims of sexual violence [Valutazione dell’efficacia di un intervento di supporto psicopedagogico e counselling rivolto a bambine etiopi vittime di violenza sessuale]. Maltrattamento e Abuso All'Infanzia: Rivista Interdisciplinare 2014;16(2):81-96. [DOI: 10.3280/MAL2014-002005] [DOI] [Google Scholar]
De luca 1995 {published data only}
- De Luca RV, Boyes DA, Grayston AD, Romano E. Sexual abuse: effects of group therapy on pre-adolescent girls. Child Abuse Review 1995;4(4):263-77. [DOI: 10.1002/car.2380040406] [DOI] [Google Scholar]
Echeburúa 1997 {published data only}
- Echeburúa E, De Corral P, Zubizarreta I, Sarasua B. Psychological treatment of chronic posttraumatic stress disorder in victims of sexual aggression. Behavior Modification 1997;21(4):433-56. [DOI: 10.1177/01454455970214003] [PMID: ] [DOI] [PubMed] [Google Scholar]
Friedrich 1992b {published data only}
- Friedrich WN, Luecke WJ, Beilke RL, Place V. Psychotherapy outcome of sexually abused boys: an agency study. Journal of Interpersonal Violence 1992;7(3):396–409. [DOI: 10.1177/088626092007003008] [DOI] [Google Scholar]
Gouweloos 2011 {published data only}
- Gouweloos J, Kremers A, Sadat A, Bicanic I. Trauma treatment after single rape. How to reduce dropout amongst Moroccan and Turkish girls? Psychologie & Gezondheid 2011;39(3):175-9. [URL: Available at www.researchgate.net/publication/297912441_Trauma_treatment_after_single_rape_How_to_reduce_dropout_amongst_Moroccan_and_Turkish_girls] [Google Scholar]
Habigzang 2013 {published data only}
- Habigzang LF, Damásio BF, Koller SH. Impact evaluation of a cognitive behavioral group therapy model in Brazilian sexually abused girls. Journal of Child Sexual Abuse 2013;22(2):173-90. [DOI: 10.1080/10538712.2013.737445] [PMID: ] [DOI] [PubMed] [Google Scholar]
Hahn 2016 {published data only}
- Hahn H, Oransky M, Epstein C, Smith Stover C, Marans S. Findings of an early intervention to address children's traumatic stress implemented in the child advocacy center setting following sexual abuse. Journal of Child & Adolescent Trauma 2016;9(1):55-66. [DOI: 10.1007/s40653-015-0059-7] [DOI] [Google Scholar]
Hall‐Marley 1993 {published data only}
- Hall-Marley SE, Damon L. Impact of structured group therapy on young victims of sexual abuse. Journal of Child and Adolescent Group Therapy 1993;3(1):41-8. [DOI: 10.1007/BF00973642] [DOI] [Google Scholar]
Hébert 2010 {published data only}
- Hébert M, Tourigny M. Effects of a psychoeducational group intervention for children victims of sexual abuse. Journal of Child & Adolescent Trauma 2010;3(2):143-60. [DOI: 10.1080/19361521003726930] [DOI] [Google Scholar]
Homstead 1986 {published data only}
- Homstead K. An investigation of a sexual abuse group treatment program for female adolescent victims of sexual abuse [EdD thesis]. Ann Arbour (MI): University of Massachusetts, 1986. [Google Scholar]
Hubel 2014 {published data only}
- Hubel GS, Campbell C, West T, Friedenberg S, Schreier A, Flood MF, et al. Child advocacy center based group treatment for child sexual abuse. Journal of Child Sexual Abuse 2014;23(3):304-25. [DOI: 10.1080/10538712.2014.888121] [PMID: ] [DOI] [PubMed] [Google Scholar]
Karatzias 2014 {published data only}
- Karatzias T, Ferguson S, Chouliara Z, Gullone A, Cosgrove K, Douglas A. Effectiveness and acceptability of group psychoeducation for the management of mental health problems in survivors of child sexual abuse (CSA). International Journal of Group Psychotherapy 2014;64(4):492-514. [DOI: 10.1521/ijgp.2014.64.4.492] [PMID: ] [DOI] [PubMed] [Google Scholar]
Liotta 2015 {published data only}
- Liotta L, Springer C, Misurell JR, Block-Lerner J, Brandwein D. Group treatment for child sexual abuse: treatment referral and therapeutic outcomes. Journal of Child Sexual Abuse 2015;24(3):217-37. [DOI: 10.1080/10538712.2015.1006747] [PMID: ] [DOI] [PubMed] [Google Scholar]
McGain 1995 {published data only}
- McGain B, McKinzey RK. The efficacy of group treatment in sexually abused girls. Child Abuse & Neglect 1995;19(9):1157-69. [DOI: 10.1016/0145-2134(95)00076-k] [PMID: ] [DOI] [PubMed] [Google Scholar]
Misurell 2014 {published data only}
- Misurell J, Springer C, Acosta L, Liotta L, Kranzler A. Game-based cognitive–behavioral therapy individual model (GB-CBT-IM) for child sexual abuse: a preliminary outcome study. Psychological Trauma: Theory, Research, Practice, and Policy 2014;6(3):250-8. [DOI: 10.1037/a0033411] [DOI] [Google Scholar]
Nolan 2002 {published data only}
- Nolan M, Carr A, Fitzpatrick C, O'Flaherty A, Keary K, Turner R, et al. A comparison of two programmes for victims of child sexual abuse: a treatment outcome study. Child Abuse Review 2002;11(2):103-23. [DOI: 10.1002/car.727] [DOI] [Google Scholar]
NTR6678 {published data only}
- NTR6678. The effectiveness of a 12-week clinical trauma therapy program for victims suffering from post-traumatic stress disorder after childhood sexual abuse. www.trialregister.nl/trial/6491 (first received 4 September 2017).
Osen 2007 {published data only}
- Osen B, Zoellner T. Trauma-focused group therapy with sexually traumatized women [Traumafokussierte gruppentherapie für sexuell traumatisierte frauen]. Zeitschrift für Psychiatrie Psychologie und Psychotherapie 2007;55(2):111-21. [DOI: 10.1024/1661-4747.55.2.111] [DOI] [Google Scholar]
Reeker 1998 {published data only}
- Reeker J, Ensing D. An evaluation of a group treatment for sexually abused young children. Journal of Child Sexual Abuse 1998;7(2):65-85. [DOI: 10.1300/J070v07n02_04] [DOI] [Google Scholar]
Resick 2003 {published data only}
- Resick PA, Nishith P, Griffin MG. How well does cognitive-behavioral therapy treat symptoms of complex PTSD? An examination of child sexual abuse survivors within a clinical trial. CNS Spectrums 2003;8(5):340-55. [DOI: 10.1017/s1092852900018605] [PMCID: PMC2970926] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Robinson 1989 {published data only}
- Robinson D. Evaluating intrafamilial child sexual abuse treatment: group process and outcomes in multi-site programs [EdD thesis]. Cambridge (MA): Harvard University, 1989. [Google Scholar]
Roos 2021 {published data only}
- Roos, C, Zijlstra, B, Perrin, S, van der Oord, S, Lucassen, S, Emmelkamp, P, de Jongh, A. Predictors and moderators of treatment outcome for single incident paediatric PTSD: a multi-centre randomized clinical trial. Euoropean Journal of Psychotraumatology 2021;12(1):1968138. [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Rosner 2019 {published data only}
- Rosner, R, Rimane, E, Frick, U, Gutermann, J, Hagl, M, Renneberg, B, Schreiber, F, Vogel, A, Steil, R. Effect of Developmentally Adapted Cognitive Processing Therapy for Youth With Symptoms of Posttraumatic Stress Disorder After Childhood Sexual and Physical Abuse: A Randomized Clinical Trial. JAMA Psychiatry 2019;76(5):484-491. [DOI: 10.1001/jamapsychiatry.2018.4349] [DOI] [PMC free article] [PubMed] [Google Scholar]
Silveria 1993 {published data only}
- Silveria D. Cognitive-behaviroral group therapy for sexually abused adolescent males [PhD thesis]. Los Angeles (CA): University of Southern California, 1993. [Google Scholar]
Simoneau 2008 {published data only}
- Simoneau AC, Hebert M, Tourigny M. Evaluation of a group therapy for 6-13 year old sexually abused children. Revue Quebecoise de Psychologie 2008;29(3):27-43. [Google Scholar]
Stauffer 1996 {published data only}
- Stauffer LB, Deblinger E. Cognitive behavioral groups for nonoffending mothers and their young sexually abused children: a preliminary treatment outcome study. Child Maltreatment 1996;1(1):65-76. [DOI: 10.1177/1077559596001001007] [DOI] [Google Scholar]
Steil 2015 {published data only}
- Steil R, Benner A, Müller-Engelmann M, Hadouch K. Cognitive restructuring and imagery modification. Psychotherapeut 2015;60(4):310-14. [DOI: 10.1007/s00278-015-0041-8] [DOI] [Google Scholar]
Sullivan 1992 {published data only}
- Sullivan PM, Scanlan JM, Brookhouser PE, Schulte LE, Knutson JF. The effects of psychotherapy on behavior problems of sexually abused deaf children. Child Abuse & Neglect 1992;16(2):297-307. [DOI: 10.1016/0145-2134(92)90036-Q] [DOI] [PubMed] [Google Scholar]
Tourigny 1998 {published data only}
- Tourigny M, Péladeau N, Doyon M, Bouchard C. Effectiveness of a treatment program for sexually abused children. Child Abuse & Neglect 1998;22(1):25-43. [DOI: 10.1016/s0145-2134(97)00117-8] [PMID: ] [DOI] [PubMed] [Google Scholar]
Waters 1998 {published data only}
- Waters KT. Program evaluation of group treatment of sexually abused children [EdD thesis]. Cincinnati (OH): University of Cincinnati, 1998. [Google Scholar]
Wolf 1993 {published data only}
- Wolf VB. Group therapy of young latency age sexually abused girls. Journal of Child and Adolescent Group Therapy 1993;3(1):25-39. [DOI: 10.1007/BF00973641] [DOI] [Google Scholar]
References to studies awaiting assessment
Danielson 2016 {published data only}
- Danielson CK. 22.4 Reducing risk for substance use problems among adolescents with a child maltreatment history. Journal of the American Academy of Child & Adolescent Psychiatry 2016;55(Suppl 10):S293. [DOI: 10.1016/j.jaac.2016.07.247] [DOI] [Google Scholar]
References to ongoing studies
Amirzadegan 2018 {published data only}
- Amirzadegan M, Ghahari S, Asgharnejad Farid AA. PW0008 Comparison the efficiency of play and narrative therapy on decreasing depression, anxiety and aggression of sexually abused children in Tehran. European Psychiatry 2018;48(Suppl 1):S143. [DOI: 10.1016/j.eurpsy.2017.12.016] [DOI] [Google Scholar]
NCT00073684 {published data only}
- NCT00073684. Optimal treatment strategies for sexually abused children [Young sexually abused children: optimal CBT strategies]. clinicaltrials.gov/ct2/show/NCT00073684 (first received 2 December 2003).
Additional references
Abidin 1983
- Abidin RR. Parenting Stress Index: Manual, Administration Booklet, [and] Research Update. Charlottesville (VA): Pediatric Psychology Press, 1983. [Google Scholar]
Achenbach 1991
- Achenbach TM. Manual for the Child Behavior Checklist 4-18 and 1991 Profile. Burlington (VT): University of Vermont, 1991. [ISBN: 0938565087] [Google Scholar]
Allnock 2012
- Allnock D, Hynes P. Therapeutic Services for Sexually Abused Children and Young People: Scoping the Evidence Base. London (UK): NSPCC, 2012. [www.nspcc.org.uk/globalassets/documents/research-reports/therapeutic-services-sexually-abused-children-evidence-review.pdf] [Google Scholar]
Armsden 1987
- Armsden GC, Greenberg MT. The Inventory of Parent and Peer Attachment: individual differences and their relationship to psychological well-being in adolescence. Journal of Youth and Adolescence 1987;16(5):427–54. [DOI: 10.1007/BF02202939] [DOI] [PubMed] [Google Scholar]
Axline 1947
- Axline VM. Play Therapy. New York (NY): Ballantine Books, 1947. [Google Scholar]
Barth 2012
- Barth RP, Lee BR, Lindsey MA, Collins KS, Strieder F, Chorpita BF, et al. Evidence-based practice at a crossroads: the timely emergence of common elements and common factors. Research on Social Work Practice 2012;22(1):108-19. [DOI: 10.1177/1049731511408440] [DOI] [Google Scholar]
Barth 2013
- Barth J, Bermetz L, Heim E, Trelle S, Tonia T. The current prevalence of child sexual abuse worldwide: a systematic review and meta-analysis. International Journal of Public Health 2013;58(3):469–83. [DOI: 10.1007/s00038-012-0426-1] [PMID: ] [DOI] [PubMed] [Google Scholar]
Benuto 2015
- Benuto LT, O’Donohue W. Treatment of the sexually abused child: review and synthesis of recent meta-analyses. Children and Youth Services Review 2015;56:52-60. [DOI: 10.1016/j.childyouth.2015.06.009] [DOI] [Google Scholar]
Betancourt 2009
- Betancourt TS, Bass J, Borisova I, Neugebauer R, Speelman L, Onyango G, et al. Assessing local instrument reliability and validity: a field-based example from northern Uganda. Social Psychiatry and Psychiatric Epidemiology 2009;44(8):685-92. [DOI: 10.1007/s00127-008-0475-1] [PMCID: PMC2716434] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Bolton 2007
- Bolton P, Bass J, Betancourt T, Speelman L, Onyango G, Clougherty KF, et al. Interventions for depression symptoms among adolescent survivors of war and displacement in northern Uganda: a randomized controlled trial. JAMA 2007;298(5):519-27. [DOI: 10.1001/jama.298.5.519] [PMID: ] [DOI] [PubMed] [Google Scholar]
Brener 2004
- Brener ND, Kann L, Kinchen SA, Grunbaum JA, Whalen L, Eaton D, et al. Methodology of the youth risk behavior surveillance system. MMWR. Recommendations and Reports 2004;53(RR-12):1-13. [PMID: ] [PubMed] [Google Scholar]
Briere 1989
- Briere J, Runtz M. The Trauma Symptom Checklist (TSC-33): early data on a new scale. Journal of Interpersonal Violence 1989;4(2):151-63. [DOI: 10.1177/088626089004002002] [DOI] [Google Scholar]
Briere 1996
- Briere JN. Trauma Symptom Checklist for Children (TSCC): Professional Manual. Odessa (FL): Psychological Assessment Resources, 1996. [Google Scholar]
Brignardello‐Petersen 2018
- Brignardello-Petersen R, Bonner A, Alexander PE, Siemieniuk RA, Furukawa TA, Rochwerg B, et al. Advances in the GRADE approach to rate the certainty in estimates from a network meta-analysis. Journal of Clinical Epidemiology 2018;93:36-44. Erratum in: Journal of Clinical Epidemiology 2018;98:162. DOI:10.1016/j.jclinepi.2018.04.013. [DOI: ] [PMID: 29051107]29051107 [Google Scholar]
Bucher 1997
- Bucher HC, Guyatt GH, Griffith LE, Walter SD. The results of direct and indirect treatment comparisons in meta-analysis of randomized controlled trials. Journal of Clinical Epidemiology 1997;50(6):683-91. [PMID: ] [DOI] [PubMed] [Google Scholar]
Buros 1965
- Buros OK. The Sixth Mental Measurements Yearbook. Highland Park (NJ): Gryphon Press, 1965. [Google Scholar]
Cain 2016
- Cain DJ, Keenan K, Rubin S. Humanistic Psychotherapies: Handbook of Research and Practice. 2nd edition. Washington (DC): American Psychological Association, 2016. [Google Scholar]
Caldwell 2005
- Caldwell DM, Ades AE, Higgins JP. Simultaneous comparison of multiple treatments: combining direct and indirect evidence. BMJ 2005;331(7521):897-900. [DOI: 10.1136/bmj.331.7521.897] [PMCID: PMC1255806] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Caldwell 2010
- Caldwell DM, Welton NJ, Ades AE. Mixed treatment comparison analysis provides internally coherent treatment effect estimates based on overviews of reviews and can reveal inconsistency. Journal of Clinical Epidemiology 2010;63(8):875-82. [DOI: 10.1016/j.jclinepi.2009.08.025] [PMID: ] [DOI] [PubMed] [Google Scholar]
Caldwell 2016
- Caldwell DM, Welton NJ. Approaches for synthesising complex mental health interventions in meta-analysis. Evidence-Based Mental Health 2016;19(1):16-21. [DOI: 10.1136/eb-2015-102275] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Carr 2006
- Carr A. Family Therapy: Concepts, Process and Practice. 2nd edition. Hoboken (NJ): John Wiley and Sons Ltd, 2006. [ISBN: 9780470713051] [Google Scholar]
CDPLP 2014
- CDPLP. Data collection form for intervention reviews: RCTs only. dplp.cochrane.org/data-extraction-forms (accessed 21 August 2021).
Celano 1992
- Celano M, Webb C, Hazzard A. Parental attributions of responsibility for child sexual abuse. In: Paper presented at the National Symposium on Child Victimization; 1992 May; Washington (DC). 1992.
Chaimani 2012
- Chaimani A, Salanti G. Using network meta‐analysis to evaluate the existence of small‐study effects in a network of interventions. Research Synthesis Methods 2012;3(2):161-76. [DOI: 10.1002/jrsm.57] [PMID: ] [DOI] [PubMed] [Google Scholar]
Chaimani 2013
- Chaimani A, Higgins JP, Mavridis D, Spyridonos P, Salanti G. Graphical tools for network meta-analysis in STATA. PLoS One 2013;8(10):e76654. [DOI: 10.1371/journal.pone.0076654] [PMCID: PMC3789683] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Chaimani 2015
- Chaimani A, Salanti G. Visualizing assumptions and results in network meta-analysis: the network graphs package. Stata Journal 2015;15(4):905-50. [DOI: 10.1177/1536867X150150040] [DOI] [Google Scholar]
CINeMA 2017 [Computer program]
- CINeMA: Confidence in Network Meta-Analysis. Bern (CH): Institute of Social and Preventive Medicine, University of Bern, 2017. Available at cinema.ispm.unibe.ch.
Cipriani 2013
- Cipriani A, Higgins JP, Geddes JR, Salanti G. Conceptual and technical challenges in network meta-analysis. Annals of Internal Medicine 2013;159(2):130-7. [DOI: 10.7326/0003-4819-159-2-201307160-00008] [PMID: ] [DOI] [PubMed] [Google Scholar]
Clifton 2019
- Clifton L, Clifton DA. The correlation between baseline score and post-intervention score, and its implications for statistical analysis. Trials 2019;20(1):43. [DOI: 10.1186/s13063-018-3108-3] [PMCID: PMC6330413] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Cohen 1988
- Cohen J. Statistical Power Analysis for the Behavioral Sciences. Hillsdale (NJ): Lawrence Erlbaum Associates, 1988. [Google Scholar]
Cohen 2006
- Cohen JA, Mannarino AP, Delinger E. Treating Trauma and Traumatic Grief in Children and Adolescents. New York (NY): Guilford Press, 2006. [Google Scholar]
Cohen 2018
- Cohen JA, Deblinger E, Mannarino AP. Trauma-focused cognitive behavioural therapy for children and families. Psychotherapy Research 2018;28(1):47-57. [DOI: 10.1080/10503307.2016.1208375] [PMID: ] [DOI] [PubMed] [Google Scholar]
Corcoran 2008
- Corcoran J, Pillai V. A meta-analysis of parent-involved treatment for child sexual abuse. Research on Social Work Practice 2008;15(5):453-64. [DOI: 10.1177/1049731507313980] [DOI] [Google Scholar]
Dallos 2010
- Dallos R. An Introduction to Family Therapy: Systematic Theory and Practice. Maidenhead (UK): Open University Press, 2010. [ISBN: 0-33-526454-9] [Google Scholar]
Deblinger 1989
- Deblinger E, McLeer SV, Atkins MS, Ralphe D, Foa E. Post-traumatic stress in sexually abused, physically abused, and nonabused children. Child Abuse & Neglect 1989;13(3):403-8. [PMID: ] [DOI] [PubMed] [Google Scholar]
Deblinger 1996a
- Deblinger E, Heflin AH. Treating Sexually Abused Children and their Nonoffending Parents: A Cognitive Behavioral Approach. London (UK): Sage Publications, Inc, 1996. [Google Scholar]
Dias 2019
- Dias S, Caldwell DM. Network meta-analysis explained. Archives of Disease in Childhood - Fetal and Neonatal Edition 2019;104(1):F8-F12. [DOI: 10.1136/archdischild-2018-315224] [PMCID: PMC6761999] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
DSM‐5
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5 edition. Washington (DC): American Psychiatric Association, 2013. [ISBN: 8123923791] [Google Scholar]
Everson 1989
- Everson MD, Hunter WM, Runyon DK, Edelsohn GA, Coulter ML. Maternal support following disclosure of incest. American Journal of Orthopsychiatry 1989;59(2):197–207. [DOI: 10.1111/j.1939-0025.1989.tb01651.x] [PMID: ] [DOI] [PubMed] [Google Scholar]
Fang 2012
- Fang X, Brown DS, Florence CS, Mercy JA. The economic burden of child maltreatment in the United States and implications for prevention. Child Abuse & Neglect 2012;36(2):156-65. [DOI: 10.1016/j.chiabu.2011.10.006] [PMCID: PMC3776454] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Fergusson 1999
- Fergusson DM, Mullen PE. Childhood Sexual Abuse An Evidence Based Perspective. London (UK): Sage Publications Inc, 1999. [DOI: 10.4135/9781452205540] [DOI] [Google Scholar]
Fisher 2017
- Fisher C, Goldsmith A, Hurcombe R, Soares C. The Impacts of Child Sexual Abuse: A Rapid Evidence Assessment. London (UK): Independent Inquiry Into Child Sexual Abuse, 2017. [URL: tinyurl.com/y74o5c6h] [Google Scholar]
Frank 1993
- Frank JD, Frank JB. Persuasion and Healing: A Comparative Study of Psychotherapy. 3rd edition. Baltimore (MD): John Hopkins University Press, 1993. [Google Scholar]
Friedrich 1992a
- Friedrich WN, Grambsch P, Damon L, Hewitt SK, Koverola C, Lang RA, et al. Child Sexual Behavior Inventory: normative and clinical comparisons. Psychological Assessment 1992;4(3):303-11. [DOI: 10.1037/1040-3590.4.3.303] [DOI] [Google Scholar]
Friedrich 1997
- Friedrich WN. CSBI: Child Sexual Behavior Inventory: Professional Manual. Odessa (FL): Psychological Assessment Resources, 1997. [Google Scholar]
Fu 2016
- Fu R, Holmer HK. Change score or follow-up score? Choice of mean difference estimates could impact meta-analysis conclusions. Journal of Clinical Epidemiology 2016;76:108-17. [DOI: 10.1016/j.jclinepi.2016.01.034] [PMID: ] [DOI] [PubMed] [Google Scholar]
Furukawa 2006
- Furukawa TA, Barbui C, Cipriani A, P Brambilla, Watanabe N. Imputing missing standard deviations in meta-analyses can provide accurate results. Journal of Clinical Epidemiology 2006;59(1):7-10. [DOI: 10.1016/j.jclinepi.2005.06.006] [PMID: ] [DOI] [PubMed] [Google Scholar]
Garg 2008
- Garg AX, Hackam D, Tonelli M. Systematic review and meta-analysis: when one study is just not enough. Clinical Journal of the American Society of Nephrology 2008;3(1):253-60. [DOI: 10.2215/CJN.01430307] [PMID: ] [DOI] [PubMed] [Google Scholar]
Gilbert 2009
- Gilbert R, Widom CS, Browne K, Fergusson D, Webb E, Janson S. Burden and consequences of child maltreatment in high-income countries. Lancet 2009;373(9657):68-81. [DOI: 10.1016/S0140-6736(08)61706-7] [PMID: ] [DOI] [PubMed] [Google Scholar]
Gillihan 2013
- Gillihan SJ, Aderka IM, Conklin PH, Capaldi S, Foa EB. The Child PTSD Symptom Scale: psychometric properties in female adolescent sexual assault survivors. Psychological Assessment 2013;25(1):23-31. [DOI: 10.1037/a0029553] [PMCID: PMC3779054] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Gillis 1980
- Gillis JS. Child Anxiety Scale (CAS). Manual. Champaign (IL): Institute for Personality and Ability Testing Inc, 1980. [Google Scholar]
Goepfert 2015
- Goepfert E, Mulé C, Hahn E, Visco Z, Siegel M. Family system interventions for families of children with autism spectrum disorder. Child and Adolescent Psychiatric Clinics of North America 2015;24(3):571-83. [DOI: 10.1016/j.chc.2015.02.009] [PMID: ] [DOI] [PubMed] [Google Scholar]
Greenwald 1999
- Greenwald R‚ Rubin A. Assessment of posttraumatic symptoms in children: development and preliminary validation of parent and child scales. Research on Social Work Practice 1999;9(1):61-75. [DOI: 10.1177/104973159900900105] [DOI] [Google Scholar]
Harper 1995
- Harper P. A spectrum of psychological therapies for children. In: Clarkson P, Pokorny M, editors(s). The Handbook of Psychotherapy. London (UK): Routledge, 1995:158-71. [Google Scholar]
Harvey 2010
- Harvey ST, Taylor JE. A meta-analysis of the effects of psychotherapy with sexually abused children and adolescents. Clinical Psychology Review 2010;30(5):517-35. [DOI: 10.1016/j.cpr.2010.03.006] [PMID: ] [DOI] [PubMed] [Google Scholar]
Herrmann 2014
- Herrmann B, Banaschak S, Csorba R, Navratil F, Dettmeyer R. Physical examination in child sexual abuse. Deutsches Ärzteblatt International 2014;111(41):692-703. [DOI: 10.3238/arztebl.2014.0692] [PMCID: PMC4215093] [DOI] [Google Scholar]
Hetzel‐Riggin 2007
- Hetzel-Riggin MD, Brausch AM, Montgomery BS. A meta-analytic investigation of therapy modality outcomes for sexually abused children and adolescents: an exploratory study. Child Abuse & Neglect 2007;31(2):125-41. [DOI: 10.1016/j.chiabu.2006.10.007] [PMID: ] [DOI] [PubMed] [Google Scholar]
Higgins 2012
- Higgins JP, Jackson D, Barrett JK, Lu G, Ades AE, White IR. Consistency and inconsistency in network meta-analysis: concepts and models for multi-arm studies. Research Synthesis Methods 2012;3(2):98-110. [DOI: 10.1002/jrsm.1044] [PMCID: PMC4433772] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2017
- Higgins JP, Altman DG, Sterne JA, editor(s). Chapter 8: Assessing risk of bias in included studies. In: Higgins JP, Churchill R, Chandler J, Cumpston MS, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.2.0 (updated June 2017). Cochrane, 2017. Available from training.cochrane.org/handbook/archive/v5.2.
Higgins 2021a
- Higgins, JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 6.2 (updated February 2021). Cochrane, 2021. Available from training.cochrane.org/handbook.
Higgins 2021b
- Higgins JP, Eldridge S, Li T, editor(s). Chapter 23: Including variants on randomized trials. In: Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 6.2 (updated February 2021). Cochrane, 2021. Available from training.cochrane.org/handbook.
Hindryckx 2017
- Hindryckx P, Zou GY, Feagan B, Garg S, Singh L, Lobaton T, et al. Biologic drugs for induction and maintenance of remission in Crohn's disease: a network meta-analysis. Cochrane Database of Systematic Reviews 2017, Issue 8. Art. No: CD012751. [DOI: 10.1002/14651858.CD012751] [DOI] [Google Scholar]
Hofmann 2017
- Hofmann SG editor(s). International Perspectives on Psychotherapy. Boston (MA): Springer, 2017. [ISBN: 978-3-319-56193-6] [Google Scholar]
Horne 1999
- Horne A. Sexual abuse and sexual abusing in childhood and adolescence. In: Lanyado M, Horne A, editors(s). The Handbook of Child & Adolescent Psychotherapy: Psychoanalytic Approaches. London (UK): Routledge, 1999:347-68. [Google Scholar]
Jensen 2005
- Jensen PS, Weersing R, Hoagwood KE, Goldman E. What is the evidence for evidence-based treatments? A hard look at our soft underbelly. Mental Health Services Research 2005;7(1):53-74. [PMID: ] [DOI] [PubMed] [Google Scholar]
Karakurt 2014
- Karakurt G, Silver KE. Therapy for childhood sexual abuse survivors using attachment and family systems theory orientations. American Journal of Family Therapy 2014;42(1):79-91. [DOI: 10.1080/01926187.2013.772872] [PMCID: PMC3891673] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Kaufman 1997
- Kaufman J, Birmaher B, Brent D, Rao U, Flynn C, Moreci P, et al. Schedule for Affective Disorders and Schizophrenia for School-Age Children-Present and Lifetime Version (K-SADS-PL): initial reliability and validity data. Journal of the American Academy of Child and Adolescent Psychiatry 1997;36(7):980-8. [DOI: 10.1097/00004583-199707000-00021] [PMID: ] [DOI] [PubMed] [Google Scholar]
Kegerreis 2010
- Kegerreis S. Psychodynamic Counselling with Children and Young People: An Introduction. Basingstoke (UK): Palgrave Macmillan, 2010. [Google Scholar]
Kendall‐Tackett 1993
- Kendall-Tackett KA, Williams LM, Finkelhor D. Impact of sexual abuse on children: a review and synthesis of recent empirical studies. Psychological Bulletin 1993;113(1):164-80. [DOI: 10.1037/0033-2909.113.1.164] [PMID: ] [DOI] [PubMed] [Google Scholar]
Kovacs 1992
- Kovacs M. CDI: Children’s Depression Inventory. A Measure of Depressive Symptoms in Young Persons. North Tonawanda (NY): MHS Inc, 1992. [Google Scholar]
Lanyado 1999
- Lanyado M. The treatment of traumatisation in children. In: Lanyado M, Horne A, editors(s). The Handbook of Child & Adolescent Psychotherapy: Psychoanalytic Approaches. London (UK): Routledge, 1999:275-92. [Google Scholar]
Latzman 2017
Likierman 1999
- Likierman M, Urban E. The roots of child and adolescent psychotherapy in psychoanalysis. In: Lanyado M, Horne A, editors(s). The Handbook of Child and Adolescent Psychotherapy: Psychoanalytic Approaches. London (UK): Routledge, 1999:19-30. [Google Scholar]
Lorås 2017
- Lorås L, Bertrando P, Ness O. Researching systemic therapy history: in search of a definition. Journal of Family Psychotherapy 2017;28(2):134-49. [DOI: 10.1080/08975353.2017.1285656] [DOI] [Google Scholar]
Macdonald 2012
- Macdonald G, Higgins JP, Ramchandani P, Valentine JC, Bronger LP, Klein P, et al. Cognitive-behavioural interventions for children who have been sexually abused. Cochrane Database of Systematic Reviews 2012, Issue 5. Art. No: CD001930. [DOI: 10.1002/14651858.CD001930.pub3] [PMCID: PMC7061273] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Macdonald 2016
- Macdonald G, Livingstone N, Hanratty J, McCartan C, Cotmore R, Cary M, et al. The effectiveness, acceptability and cost-effectiveness of psychosocial interventions for maltreated children and adolescents: an evidence synthesis. Health Technology Assessment 2016;20(69):1-508. [DOI: 10.3310/hta20690] [PMCID: PMC5056338] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
MacMillan 2009
- MacMillan HL, Wathen CN, Barlow J, Fergusson DM, Leventhal JM, Taussig HN. Interventions to prevent child maltreatment and associated impairment. Lancet 2009;373(9659):250–66. [DOI: 10.1016/S0140-6736(08)61708-0] [PMID: ] [DOI] [PubMed] [Google Scholar]
Mannarino 1996
- Mannarino AP, Cohen JA. Family-related variables and psychological symptom formation in sexually abused girls. Journal of Child Sexual Abuse 1996;5(1):105-20. [DOI: 10.1300/J070v05n01_06] [DOI] [Google Scholar]
March 1997
- March JS, Parker JD, Sullivan K, Stallings P, Conners CK. The Multidimensional Anxiety Scale for Children (MASC): factor structure, reliability, and validity. Journal of the American Academy of Child and Adolescent Psychiatry 1997;36(4):554-65. [DOI: 10.1097/00004583-199704000-00019] [PMID: ] [DOI] [PubMed] [Google Scholar]
McCarthy 2016
- McCarthy MM, Taylor P, Norman RE, Pezzullo L, Tucci J, Goddard C. The lifetime economic and social costs of child maltreatment in Australia. Children and Youth Services Review 2016;71:217-26. [DOI: 10.1016/j.childyouth.2016.11.014] [DOI] [Google Scholar]
McEwen 2007
- McEwen BS. Physiology and neurobiology of stress and adaptation: central role of the brain. Physiological Reviews 2007;87(3):873-904. [DOI: 10.1152/physrev.00041.2006] [PMID: ] [DOI] [PubMed] [Google Scholar]
Nakamura 2009
- Nakamura BJ, Ebesutani C, Bernstein A, Chorpita BF. A psychometric analysis of the Child Behavior Checklist DSM-Oriented Scales. Journal of Psychopathology and Behavioral Assessment 2009;31(3):178–89. [DOI: 10.1007/s10862-008-9119-8] [DOI] [PMC free article] [PubMed] [Google Scholar]
NHS Health Scotland 2006
- NHS Health Scotland, University of Warwick, University of Edinburgh. Warwick–Edinburgh Mental Well-being Scale (WEMWBS); 2006. www2.uwe.ac.uk/services/Marketing/students/pdf/Wellbeing-resources/well-being-scale-wemwbs.pdf (accessed 3 June 2019).
NICE 2017
- National Institute for Health and Care Excellence. Child Abuse and Neglect: NICE Guideline. London (UK): National Institute for Health and Care Excellence, 2017. [URL: www.nice.org.uk/guidance/ng76/resources/child-abuse-and-neglect-pdf-1837637587141] [Google Scholar]
NICE 2018
- NICE. Post-Traumatic Stress Disorder. London (UK): National Institute for Health and Care Excellence, 2018. [URL: www.nice.org.uk/guidance/ng116/resources/posttraumatic-stress-disorder-pdf-66141601777861] [PubMed] [Google Scholar]
Nikolakopoulou 2020
- Nikolakopoulou A, Higgins JP, Papakonstantinou T, Chaimani A, Del Giovane C, Egger M, et al. CINeMA: an approach for assessing confidence in the results of a network meta-analysis. PLoS Medicine 2020;17(4):e1003082. [DOI: 10.1371/journal.pmed.1003082] [PMCID: PMC7122720] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
NSCDC 2007
- National Scientific Council on the Developing Child. The Timing and Quality of Early Experiences Combine to Shape Brain Architecture. Working Paper 5. Cambridge (MA): National Scientific Council on the Developing Child, 2007. [URL: developingchild.harvard.edu/wp-content/uploads/2007/05/Timing_Quality_Early_Experiences-1.pdf] [Google Scholar]
Oren 2012
- Oren E, Solomon R. EMDR therapy: an overview of its development and mechanisms of action [La thérapie EMDR: un aperçu de ses développements et mécanismes d’action]. Revue européenne de psychologie appliquée 2012;62(4):197-203. [DOI: 10.1016/j.erap.2012.08.005] [DOI] [Google Scholar]
Orvaschel 1989
- Orvaschel H. Kiddies SADS–E Section. Designed to Assess PTSD. Philadelphia (PA): Medical College of Philadelphia, 1989. [Google Scholar]
Parker 2013
- Parker B, Turner W. Psychoanalytic/psychodynamic psychotherapy for children and adolescents who have been sexually abused. Cochrane Database of Systematic Reviews 2013, Issue 7. Art. No: CD008162. [DOI: 10.1002/14651858.CD008162.pub2] [PMID: ] [DOI] [PubMed] [Google Scholar]
Porter 1954
- Porter BM. Measurement of parental acceptance of children. Journal of Home Economics 1954;46(3):176–82. [APA RECORD: 1955-00619-001] [Google Scholar]
Prochaska 1999
- Prochaska JO, Norcross JC. Psychoanalytic therapies. In: Prochaska JO, Norcross JC, editors(s). Systems of Psychotherapy: A Transtheoretical Analysis. Pacific Grove (CA): Brooks/Cole Publishing, 1999:25-68. [Google Scholar]
Putnam 2003
- Putnam FW. Ten-year research update review: child sexual abuse. Journal of the American Academy of Child and Adolescent Psychiatry 2003;42(3):269-78. [DOI: 10.1097/00004583-200303000-00006] [PMID: ] [DOI] [PubMed] [Google Scholar]
Reeker 1997
- Reeker J, Ensing D, Elliott R. A meta-analytic investigation of group treatment outcomes for sexually abused children. Child Abuse & Neglect 1997;21(7):669-80. [DOI: 10.1016/s0145-2134(97)00024-0] [PMID: ] [DOI] [PubMed] [Google Scholar]
Review Manager 2020 [Computer program]
- Review Manager 5 (RevMan 5). Version 5.4.1. Copenhagen: Nordic Cochrane Centre, The Cochrane Collaboration, 2020.
Reynolds 1985
- Reynolds CR, Richmond BO. Revised Children's Manifest Anxiety Scale (RCMAS). Manual. Los Angeles (CA): Western Psychological Services, 1985. [Google Scholar]
Reynolds 1998
- Reynolds CR, Kamphaus RW. BASC: Behavior Assessment System for Children: Manual. Circle Pines (MN): American Guidance Service, 1998. [Google Scholar]
Rogers 1951
- Rogers C. Client Centered Therapy. Oxford (UK): Houghton Mifflin, 1951. [Google Scholar]
Saied‐Tessier 2014
- Saied-Tessier A. Estimating the Costs of Child Sexual Abuse in the UK. London (UK): NSPCC, 2014. [Google Scholar]
Saigh 2000
- Saigh PA, Yasik AE, Oberfield RA, Green BL, Halamandaris PV, Rubenstein H, et al. The Children’s PTSD Inventory: development and reliability. Journal of Traumatic Stress 2000;13(3):369–80. [DOI: 10.1023/A:1007750021626] [PMID: ] [DOI] [PubMed] [Google Scholar]
Salanti 2009
- Salanti G, Marinho V, Higgins JP. A case study of multiple-treatments meta-analysis demonstrates that covariates should be considered. Journal of Clinical Epidemiology 2009;62(8):857-64. [DOI: 10.1016/j.jclinepi.2008.10.001] [PMID: ] [DOI] [PubMed] [Google Scholar]
Salanti 2012
- Salanti G. Indirect and mixed-treatment comparison, network, or multiple-treatments meta-analysis: many names, many benefits, many concerns for the next generation evidence synthesis tool. Research Synthesis Methods 2012;3(2):80-97. [DOI: 10.1002/jrsm.1037] [PMID: ] [DOI] [PubMed] [Google Scholar]
Salanti 2014
- Salanti G, Del Giovane C, Chaimani A, Caldwell DM, Higgins JP. Evaluating the quality of evidence from a network meta-analysis. PLoS One 2014;9(7):e99682. [DOI: 10.1371/journal.pone.0099682] [PMCID: PMC4084629] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Salanti 2022
- Salanti G, Nikolakopoulou A, Efthimiou O, Mavridis D, Egger M, White I. Introducing the treatment hierarchy question in network meta-analysis. American Journal of Epidemiology 2022;191(5):930-8. [DOI: 10.1093/aje/kwab278] [PMCID: PMC9071581] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Shapiro 1989
- Shapiro F. Efficacy of the eye movement desensitization procedure in the treatment of traumatic memories. Journal of Traumatic Stress 1989;2(2):199-223. [DOI: 10.1002/jts.2490020207] [DOI] [Google Scholar]
Shapiro 1993
- Shapiro F. Eye movement desensitization and reprocessing (EMDR) in 1992. Journal of Traumatic Stress 1993;6(3):417–21. [DOI: 10.1002/jts.2490060312] [DOI] [Google Scholar]
Shapiro 2001
- Shapiro F. Eye Movement Desensitization and Reprocessing: Basic Principles, Protocols, and Procedures. 2nd edition. New York (NY): Guilford Press, 2001. [Google Scholar]
Shapiro 2007
- Shapiro F. EMDR, adaptive information processing, and case conceptualization. Journal of EMDR Practice and Research 2007;1(2):68-87. [DOI: 10.1891/1933-3196.1.2.68] [DOI] [Google Scholar]
Shapiro 2014
- Shapiro F. The role of eye movement desensitization and reprocessing (EMDR) therapy in medicine: addressing the psychological and physical symptoms stemming from adverse life experiences. Permanente Journal 2014;18(1):71-7. [DOI: 10.7812/TPP/13-098] [PMCID: PMC3951033] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Shapiro 2015
- Shapiro F, Solomon R. Eye movement desensitization and reprocessing therapy. In: Neukrug ES, editors(s). The SAGE Encyclopedia of Theory in Counseling and Psychotherapy. Thousand Oaks (CA): SAGE Publications, 2015:389-94. [Google Scholar]
Shapiro 2017
- Shapiro F. Eye Movement Desensitization and Reprocessing (EMDR) Therapy: Basic Principles, Protocols and Procedures. 3rd edition. New York (NY): Guilford Press, 2017. [Google Scholar]
Shemilt 2007
- Shemilt J, Naismith J. Psychodynamic theories I. In: Naismith J, Grant S, editors(s). Seminars in the Psychotherapies. Glasgow (UK): Royal College of Psychiatrists, 2007:28-62. [Google Scholar]
Siddons 2004
- Siddons H, Lancaster S. An Overview of the Use of the Child Behavior Checklist within Australia. Camberwell (VI): ACER Press, 2004. [Google Scholar]
Silverman 1996
- Silverman WK, Albano AM. Anxiety Disorders Interview Schedule (ADIS-IV): Child and Parent Interview Schedules. New York (NY): Graywind Publications, 1996. [Google Scholar]
Singh 2014
- Singh MM, Parsekar SS, Nair SN. An epidemiological overview of child sexual abuse. Journal of Family Medicine and Primary Care 2014;3(4):430-5. [DOI: 10.4103/2249-4863.148139] [PMCID: PMC4311357] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Sobell 1996
- Sobell LC, Sobell M. Timeline followback method (drugs, cigarettes, and marijuana); June 1996. Available at www.emcdda.europa.eu/drugs-library/timeline-followback-method-drugs-cigarettes-and-marijuana_en.
Solomon 2012
- Solomon AH, Chung B. Understanding autism: how family therapists can support parents of children with autism spectrum disorders. Family Process 2012;51(2):250-64. [DOI: 10.1111/j.1545-5300.2012.01399.x] [PMID: ] [DOI] [PubMed] [Google Scholar]
Spain 2017
- Spain D, Sin J, Paliokosta E, Furuta M, Chalder T, Murphy D, et al. Family therapy for autism spectrum disorders. Cochrane Database of Systematic Reviews 2017, Issue 5. Art. No: CD011894. [DOI: 10.1002/14651858.CD011894.pub2] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Spielberger 1973
- Spielberger CD. Manual for the State-Trait Anxiety Inventory for Children for Children. Palo Alto (CA): Consulting Psychologists Press, 1973. [Google Scholar]
Stata 2013 [Computer program]
- Stata. Version 13. College Station, TX, USA: StataCorp, 2013. Available at www.stata.com.
Steffen 2002
- Steffen AM, McKibbin C, Zeiss AM, Gallagher-Thompson D, Bandura A. The Revised Scale for Caregiving Self-Efficacy: reliability and validity studies. Journals of Gerontology. Series B, Psychological Sciences and Social Sciences 2002;57(1):P74-86. [DOI: 10.1093/geronb/57.1.P74] [PMID: ] [DOI] [PubMed] [Google Scholar]
Steinberg 2004
- Steinberg AM, Brymer MJ, Decker KB, Pynoos RS. The University of California at Los Angeles Post-traumatic Stress Disorder Index. Current Psychiatry Reports 2004;6(2):96-100. [DOI: 10.1007/s11920-004-0048-2] [PMID: ] [DOI] [PubMed] [Google Scholar]
Strayhorn 1998
- Strayhorn JM, Weidman CS. A Parent Practices Scale, and its relation to parent and child mental health. Journal of the American Academy of Child and Adolescent Psychiatry 1988;27(5):613−8. [DOI: 10.1097/00004583-198809000-00016] [PMID: ] [DOI] [PubMed] [Google Scholar]
Sánchez‐Meca 2011
- Sánchez-Meca J, Rosa-Alcázar A, López-Soler C. The psychological treatment of sexual abuse in children and adolescents: a meta-analysis. International Journal of Clinical and Health Psychology 2011;11(1):67-93. [ISSN: 1697-2600] [URL: www.aepc.es/ijchp/articulos_pdf/ijchp-371.pdf] [Google Scholar]
Thompson 1998
- Thompson M, Kaslow NJ, Weiss B, Nolen-Hoeksema S. Children's Attributional Style Questionnaire—Revised: psychometric examination. Psychological Assessment 1998;10(2):166-70. [DOI: 10.1037/1040-3590.10.2.166] [DOI] [Google Scholar]
Tickle 2016
- Tickle A, Rennoldson M. Systemic family therapy. In: Dawson DL, Moghaddam NG, editors(s). Formulation in Action. Applying Psychological Theory to Clinical Practice. Berlín (DE): De Gruyter Open, 2016:123-41. [Google Scholar]
Tonin 2017
- Tonin FS, Rotta I, Mendes AM, Pontarolo R. Network meta-analysis: a technique to gather evidence from direct and indirect comparisons. Pharmacy Practice 2017;15(1):943-54. [DOI: 10.18549/PharmPract.2017.01.943] [PMCID: PMC5386629] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Trask 2011
- Trask EV, Walsh K, DiLillo D. Treatment effects for common outcomes of child sexual abuse: a current meta-analysis. Aggression and Violent Behavior 2011;16(1):6-19. [DOI: 10.1016/j.avb.2010.10.001] [NIHMSID: NIHMS254267] [PMCID: PMC3095890] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
United Nations Development Programme 2009
- United Nations Development Programme. Human Development Report 2009. Overcoming Barriers: Human Mobility and Development. New York (NY): United Nations Development Programme, 2009. [Google Scholar]
Veroniki 2013
- Veroniki AA, Vasiliadis HS, Higgins JP, Salanti G. Evaluation of inconsistency in networks of interventions. International Journal of Epidemiology 2013;42(1):332–45. [DOI: 10.1093/ije/dys222] [PMCID: PMC5411010] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Veroniki 2016b
- Veroniki AA, Straus SE, Soobiah C, Elliott MJ, Tricco AC. A scoping review of indirect comparison methods and applications using individual patient data. BMC Medical Research Methodology 2016;16:47. [DOI: 10.1186/s12874-016-0146-y] [PMCID: PMC4847203] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Vickers 2001
- Vickers AJ, Altman DG. Statistics notes: analysing controlled trials with baseline and follow up measurements. BMJ 2001;323(7321):1123-4. [DOI: 10.1136/bmj.323.7321.1123] [PMCID: PMC1121605] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
White 2015
- White IR. Network meta-analysis. Stata Journal 2015;15(4):951-85. [DOI: 10.1177/1536867X1501500403] [DOI] [Google Scholar]
WHO 2013
- World Health Organization. Guidelines for the Management of Conditions Specifically Related to Stress. Geneva (CH): WHO, 2013. [PubMed] [Google Scholar]
Wilen 2014
- Wilen JS. A systematic review and network meta-analysis of psychosocial interventions for adults who were sexually abused as children [PhD thesis]. Bryn Mawr (PA): Bryn Mawr College, 2014. [Google Scholar]
Wolfe 1991
- Wolfe VV, Gentile C. Children's Impact of Traumatic Events Scale - Revised. University of Western Ontario 1991.
Woods 2005
- Woods CR. Sexually transmitted diseases in prepubertal children: mechanisms of transmission, evaluation of sexually abused children, and exclusion of chronic perinatal viral infections. Seminars in Pediatric Infectious Diseases 2005;16(4):317-25. [DOI: 10.1053/j.spid.2005.06.012] [PMID: ] [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
Caro 2019
- Caro P, Turner W, Macdonald G. Comparative effectiveness of interventions for treating the psychological consequences of sexual abuse in children and adolescents. Cochrane Database of Systematic Reviews 2019, Issue 6. Art. No: CD013361. [DOI: 10.1002/14651858.CD013361] [DOI] [PMC free article] [PubMed] [Google Scholar]