Abstract
Pulmonary rehabilitation has established a status of evidence-based therapy for patients with symptomatic COPD in the stable phase and after acute exacerbations. Rehabilitation should have the possibility of including different disciplines and be offered in several formats and lines of healthcare. This review focusses on the cornerstone intervention, exercise training, and how training interventions can be adapted to the limitations of patients. These adaptations may lead to altered cardiovascular or muscular training effects and/or may improve movement efficiency. Optimising pharmacotherapy (not the focus of this review) and oxygen supplements, whole-body low- and high-intensity training or interval training, and resistance (or neuromuscular electrical stimulation) training are important training modalities for these patients in order to accommodate cardiovascular and ventilatory impairments. Inspiratory muscle training and whole-body vibration may also be worthwhile interventions in selected patients. Patients with stable but symptomatic COPD, those who have suffered exacerbations and patients waiting for or who have received lung volume reduction or lung transplantation are good candidates. The future surely holds promise to further personalise exercise training interventions and to tailor the format of rehabilitation to the individual patient's needs and preferences.
Short abstract
Pulmonary rehabilitation that includes individualised exercise training is effective in patients with stable COPD and those who have suffered an exacerbation. Remaining challenges are to increase uptake and access to and personalisation of programmes. https://bit.ly/3M0kPu2
Introduction: COPD a disease with extrapulmonary consequences
COPD is a respiratory disease that develops over several decades through exposure to noxious gases, typically cigarette smoke. It is characterised by airflow obstruction, hyperinflation and poor pulmonary gas exchange. COPD is often punctuated by exacerbations that contribute to the morbidity of the disease. First-line treatment includes preventive strategies such as smoking cessation and vaccination as well as respiratory pharmacotherapy to reduce airflow limitation and hyperinflation in order to improve symptoms of dyspnoea and to reduce the probability of exacerbations [1].
Dyspnoea is “a subjective experience of breathing discomfort that consists of qualitatively distinct sensations that vary in intensity” [2]. Its intensity typically increases when ventilatory requirements increase and approach the maximum ventilatory capacity (for a comprehensive review see [3]). This happens when patients with COPD engage in exercise or physical activities that require increased energy production in the metabolism. In addition, poor gas exchange and increased dead-space ventilation, also observed in early stages of COPD, increase the ventilatory requirements for a given exercise and lead to even more symptoms of dyspnoea. As a natural response, patients avoid exercise, the trigger for these unpleasant and frightening symptoms.
While the strategy of exercise avoidance provides immediate comfort, it is a fatal strategy for the human body in the long term. Avoidance of exercise and physical activity leads to deleterious effects outside the lungs and perhaps accelerates the inflammatory cascade in the lungs of patients [4]. One of the consequences of a reduction in physical activity is observed in skeletal muscle, where deconditioning leads to adaptations in skeletal muscle metabolism, function and muscle fibre type composition, leading to an undesired increase of pulmonary ventilation and dyspnoea for a given exercise through early onset of lactic acid release, aggravated by early symptoms of skeletal muscle fatigue during exercise [5]. This leads to further physical activity avoidance. Furthermore, the cardiovascular system, the metabolic system, the brain and the immune system all suffer from a chronic lack of physical activity. In the human body, all these systems work well in an environment that includes a healthy dose of physical activity and a lack of it inevitably leads to the development of comorbidities. These nonrespiratory consequences of COPD are discussed elsewhere [6, 7]. Exacerbations further impact disease progression and the more rapid development of comorbidity, not only through acute bursts of inflammation but also by reducing physical activity.
In addition to the physiological consequences, physical activity avoidance has consequences in terms of participation in social interactions. This further contributes to the development of mental health problems as well as social isolation and loneliness [8].
For decades it has been known that the day-to-day problems encountered by patients suffering from COPD are not only caused by the respiratory symptoms, but also, directly or indirectly, related to the nonrespiratory problems these patients develop as a consequence of their lung disease. Similarly, symptoms are not limited to dyspnoea, but also include muscle fatigue in some 17–95% of patients (depending on the studied population and methodology). Fatigue contributes significantly to the physiological and psychological burden of COPD [9].
The net result is that the burden of COPD for an individual patient is often uncoupled from the initial respiratory problem, combined with a history of long-standing inactivity and emerging comorbidities. Only treating the respiratory problems in these patients leads to an unsatisfactory result from the patient's perspective. Pulmonary rehabilitation aims to tackle nonrespiratory problems by taking a holistic approach, with a focus the prevention of further respiratory disease progression (by optimising pharmacotherapy and adherence to therapy) and the initiation of therapies geared towards improving the patient's physical and mental health as well as ensuring that patients maximise physical activity and other health-enhancing behaviours, including smoking cessation and nutrition [10].
The aim of the current review is to provide a contemporary review of the definition of pulmonary rehabilitation and discuss how exercise interventions exert positive effects on patients with COPD. In addition, the clinical case scenarios for rehabilitation are discussed, i.e. the stable patient, the patient that undergoes a (surgical) procedure and the patient during or after an exacerbation. Selection of appropriate interventions and access are two important challenges facing pulmonary rehabilitation interventions in the future.
Definition of (modern) pulmonary rehabilitation
For many years, it has been recognised that comprehensive treatment of patients with COPD should go beyond respiratory treatment and tackle nonrespiratory and behavioural treatable traits as well [11]. In fact, pulmonary rehabilitation is among the most successful treatments for patients with remaining symptoms and/or excessive utilisation of healthcare resources. The European Respiratory Society and the American Thoracic Society (ATS) define rehabilitation as “a comprehensive intervention based on a thorough patient assessment followed by patient-tailored therapies, which include, but are not limited to, exercise training, education, and behaviour change, designed to improve the physical and psychological condition of people with chronic respiratory disease and to promote the long-term adherence of health-enhancing behaviours” [10]. Similar definitions are given by other professional organisations [12–14]. More recently, attention has been paid to the process of pulmonary rehabilitation [15]. This process consists of a comprehensive assessment prior to the prescription of a dedicated rehabilitation programme addressing the pulmonary and nonpulmonary physiological problems, as well as mental, motivational and social ones. After the assessment, a personalised programme can be proposed, which takes into account the individual's needs and preferences. In addition, a trajectory for follow-up needs to be established when the initial programme comes to an end. When patients can continue some form of continued exercise training as part of their disease management, outcomes are considerably better [16]. Such a maintenance programme completes the pulmonary rehabilitation process.
A comprehensive and personalised approach to patients' problems is highlighted in all guidance on pulmonary rehabilitation. Such personalised programmes can theoretically be implemented in all lines of healthcare, although comprehensive and multidisciplinary programmes are easier to implement in second- or third-line care in most current healthcare systems. Multi- or interdisciplinary concepts are integrated in most contemporary definitions of rehabilitation. A recent systematic review, however, highlighted that, while deconditioning was addressed in almost all the randomised controlled studies on pulmonary rehabilitation, other treatable traits were addressed much less frequently (e.g. obesity/cachexia in 18% of studies, anxiety/depression in 10% of studies and encouragement to engage independently in exercise only in 46% of reported studies) [17]. Nevertheless, these traits are very prevalent in individuals with COPD. In a recent study from Portugal, including 102 patients referred for pulmonary rehabilitation, ≈30% had symptoms of anxiety and 42% had symptoms of depression using a cut-off in the Hospital Anxiety and Depression Scale (HADS) of ≥8 points [18]. Using slightly more rigorous cut-offs (≥10 points) these proportions were 21% and 16% in a large study from the Netherlands [19]. In the latter study, the prevalence of obesity was 23% and underweight prevalence was observed in 14% of patients. In a sample of 339 patients (forced expiratory volume in 1 s of 46±17% pred, 6-min walk distance (6MWD) 392±112 m) referred to our pulmonary rehabilitation programme in whom physical activity was assessed with triaxial accelerometry, we confirmed the prevalence of anxiety and depression with the HADS questionnaire ≥10 points to be 32% and 23%, respectively. In this cohort, 24% of patients were obese and 24% were underweight. 75% of patients presented with severe inactivity (<5000 steps per day measured with a triaxial accelerometer following recommended methodology [20]). The prevalence of the treatable traits clearly depends on the instruments and thresholds used as well as the patient population typically referred. Irrespective of the thresholds, however, a good fraction of patients need to pay attention to these treatable traits and, hence, comprehensive programmes need to address mental health, nutritional and social issues, as well as behavioural aspects, next to exercise training.
It has become clear that, in order to ensure the quality of pulmonary rehabilitation, such programmes should undergo quality control audits and be delivered by well-trained staff. A recent workshop document of the ATS as well as an audit report from the British Thoracic Society stressed the need to ensure quality control of rehabilitation programmes in order to maintain and further optimise their efficacy [15].
The cornerstone of pulmonary rehabilitation is exercise training. The exercise training component of rehabilitation directly tackles deconditioning and its associated symptoms of dyspnoea and fatigue, the main reasons for referral. Indirectly, participation in exercise training programmes may have additional effects on comorbidities, health-related quality of life and general health. Exercise training is therefore considered an essential component of pulmonary rehabilitation [15]. Other interventions may also confer significant effects on their specific outcomes in selected patients. For example, psychosocial support interventions showed measurable improvements in mental health [21], which may be of particular benefit to patients with impaired psychosocial status at baseline. Up to half of patients included in cardiac or pulmonary rehabilitation report “fear” of exercise and nearly 70% of patients indicate that specific interventions to tackle these fears would be beneficial [22].
Reversing physiological problems
Exercise training is a potent intervention to reverse several nonrespiratory physiological consequences. When fine-tuned, exercise training can have profound effects on the skeletal muscle, cardiovascular, metabolic, bone and mental health consequences of chronic diseases.
Skeletal muscle dysfunction and impaired cardiorespiratory fitness contribute to the burden of COPD as it is experienced by patients [5]. Muscle dysfunction contributes to excess pulmonary ventilation and early contractile muscle fatigue. Along with reduced ventilatory capacity, dynamic hyperinflation and poor gas exchange further contribute to exercise intolerance. Improving skeletal muscle function delays fatigue and reduces the ventilatory requirements during exercise, and hence reduces dynamic hyperinflation and symptoms. In addition, whole-body exercise at an appropriate intensity may also improve cardiac output during exercise [23]. This leads to enhanced functional exercise capacity as well as enhanced whole-body endurance. Improvements in cardiac output may be the direct effect of improved cardiac systolic function as a consequence of the exercise training stimulus. It may, however, also be the consequence of the reduced ventilatory requirements and consequent improvements in dynamic hyperinflation [24], leading to a better end diastolic volume and stroke volume, as is also observed with bronchodilator therapy [25–27].
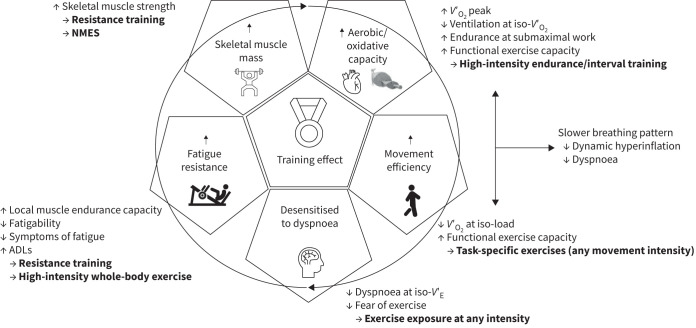
The mechanisms through which exercise training can help to enhance exercise tolerance are summarised in figure 1.
FIGURE 1.
The effects of exercise training on different systems of the body. Different exercise types and intensities (→ are mechanisms) may have different effects on the body. Arrows (↑, ↓) are indicative of the direction of effects. The reader is referred to the text for the magnitude of the effects, where relevant. ADL: activities of daily living; NMES: neuromuscular electrical stimulation; V′E: pulmonary ventilation; V′O2: oxygen uptake.
Different training modalities have different effects on clinical outcomes in patients. Resistance training, for example, leads to larger increases in skeletal muscle strength compared to whole-body exercise training. In addition, there is substantial crossover between training forms and improvements in one feature may impact other outcomes (e.g. improvements in strength may lead to better functional exercise tolerance [28]). That is why contemporary programmes mix different training approaches in order to maximise their effects.
These physiological benefits obey the “training laws” dictated by the exercise training frequency, intensity, time (duration) of exercise exposure and type of exercise (FITT principles). The link between training volume and training effect can be demonstrated [29] but it is not as robust as in other diseases or healthy cohorts. Peak oxygen uptake (V′O2peak) is not the most sensitive outcome to capture the increase in exercise tolerance in patients with COPD due to the constraints in the maximum pulmonary ventilation that are not affected by exercise training per se. Indeed, while exercise training nearly doubles the submaximal endurance time in COPD, the effect on V′O2peak across all studies is rather modest, as peak ventilation cannot increase much in ventilatory-limited patients. One study compared the effect of a similar programme in patients with heart failure and reduced ejection fraction (New York Heart Association 2–3) and patients with (very) severe COPD [30]. In patients with heart failure, V′O2peak increased by 19% whereas in patients with COPD the increase in V′O2peak seemed blunted (12%). At submaximal testing, both groups showed similar improvements. Similarly, a recent meta-analysis of improvements in V′O2peak showed a standardised mean difference (SMD) of 0.41 (0.25–0.58) in COPD [29], whereas in heart failure an SMD of 0.77 (0.39–1.14) was reported for enhanced V′O2peak [31].
Despite the limited improvement in V′O2peak, largely due to the inability to expand peak ventilation in many patients, the clinical relevance of taking part in a well-designed and properly executed exercise programme is, however, undisputed [32].
In general, two broad categories of exercise training can be used in patients with COPD, namely whole-body (aerobic) exercise training and local muscle exercises, typically prescribed as resistance training (i.e. weight lifting).
The effect of exercise training
General FITT principles
The American College of Sport Medicine guidelines on whole-body (aerobic) exercise training in elderly people propose to include training at least three times per week (frequency) at minimally 60% of pre-training V′O2peak (intensity) of whole-body aerobic exercise (e.g. walking, cycling, stepping, type) for 20–60 min over a period of 12–16 weeks (time) in order to increase exercise tolerance and elicit cardiovascular improvements [33]. In patients with COPD, effects are observed after as little as 6–8 weeks, but longer programmes provide somewhat larger effects. The effects of training programmes that adhere to these principles are well documented in terms of cardiovascular function [23, 34, 35], ventilatory requirements for a given oxygen consumption [36], skeletal muscle oxidative capacity [37, 38] and skeletal muscle fatigability [39]. These effects spin off in relevant clinical outcomes such as improved exercise tolerance, improved symptoms of dyspnoea and fatigue, and improved health-related quality of life [40]. Whole-body exercise can be offered on land as well as in water/swimming pools as long as an appropriate intensity can be guaranteed [41].
Modifications to accommodate COPD patient limitations
While the effect of exercise training in patients are well established, it is equally known that whole-body endurance training is difficult for many patients with COPD. High-intensity exercise training may not be achievable for large groups of patients and such training can be perceived by patients as extremely difficult [42, 43], particularly when ventilatory limitation is high. Patients may also develop dynamic hyperinflation and/or exercise-induced hypoxemia/hypercapnia. While training at low intensities may still lead to significant improvements in movement efficiency and desensitisation to dyspnoea, some of the physiological effects on skeletal muscle may be less achievable at such low loads when muscles are not fatigued during the exercise training [44]. Several avenues have been explored to make exercise training using more effective higher loads more comfortable for patients with limited ventilatory reserve. These can be summarised as interventions that increase the ventilatory capabilities in patients and interventions that reduce the ventilatory needs during exercise.
Interventions that increase the ventilatory abilities of patients
A first and obvious avenue is to maximise the ventilatory capacity of patients using optimal bronchodilator therapy. In many patients, bronchodilators increase the pulmonary ventilation during exercise and lower dynamic hyperinflation, hence reducing symptoms of dyspnoea during exercise [45]. When patients are prescribed exercise training, it is advised to optimise pharmacotherapy with the perspective of allowing more comfortable exercise. A review of pharmacologic strategies to enhance pulmonary ventilation and symptoms during exercise is beyond the scope of the present review and can be found elsewhere [46, 47].
Nonpharmacologic interventions can also improve ventilatory capacity in selected patients with COPD. Volume reduction using endobronchial valves or coils, or volume reduction surgery certainly improve peak ventilation in patients with pulmonary emphysema that qualify for the intervention [48]. After volume reduction interventions and with enhanced ventilatory capacity, patients are good candidates for exercise training. This exercise training will help to maximise the benefits of the newly acquired ventilatory capacity. Alternatively, exercise training can be offered using mixtures of inhaled lower-density air, also allowing for higher ventilation (e.g. helium+oxygen mixtures) [49]. The latter, however, is rather costly and large quantities of the scarce gas helium are needed. Its use should therefore be limited to more essential medical applications and should not be advised in routine clinical exercise training.
Noninvasive ventilation (NIV) using a nose or nose–mouth interface also reduces the work of breathing and acutely improves the exercise tolerance of patients with COPD. It allows for a slightly higher training intensity [50] and may render somewhat larger improvements in exercise tolerance after an exercise training programme [51], particularly in very severe patients. The application of NIV requires expertise and training, appropriate equipment and patients who are willing to get accustomed to the oronasal interfaces, making this not a mainstream technique for use in large amounts of patients [52] but an attractive option for those patients using nocturnal NIV to try.
Interventions that reduce the ventilatory burden of exercise
A second approach is to modify the training interventions such that the prescribed exercise yields a low pulmonary ventilation, yet still puts a high-intensity work stimulus on the patient.
Oxygen supplements reduce ventilatory requirements and hence dynamic hyperinflation during exercise in patients with COPD – even in patients that maintain saturation during exercise [53]. In patients with more pronounced desaturation during exercise [54, 55], but not those with mild hypoxia [56], oxygen supplements also lead to reduced lactate levels during exercise. Hence both chemoreceptor inhibition as well as lower lactate may cause lower ventilatory needs during exercise in patients with COPD. Oxygen supplements may thus help to make exercise training easier to cope with or allow increased exercise training intensity [57]. Several studies have investigated the effect of using oxygen supplements during exercise training and results have been conflicting. In patients with modest desaturation on exercise, some studies found differences in favour of patients that trained with oxygen in terms of enhanced exercise tolerance [58], some found mixed effects [57] and others showed no effect [59]. A recent systematic review pooling all studies found no general effect of oxygen supplements during rehabilitation [60]. While it is clear that no overwhelming effect of oxygen supplements during exercise training is seen, many clinicians provide oxygen for safety reasons and for patient comfort (i.e. less dyspnoea during exercise training). Proper patient selection (see below) may allow to identify patients for whom oxygen supplements may indeed greatly contribute to the training effect. One such study looked at a patient with normal saturation at rest and significant desaturation upon exercise, and an improvement of exercise endurance time of more than 10% was achieved when oxygen was administered [61]. This study, however, had some methodologic shortcomings that preclude firm conclusions and would require replication. Nevertheless, such patient selection may be crucial, particularly when oxygen would be required in a setting where it is not easily available.
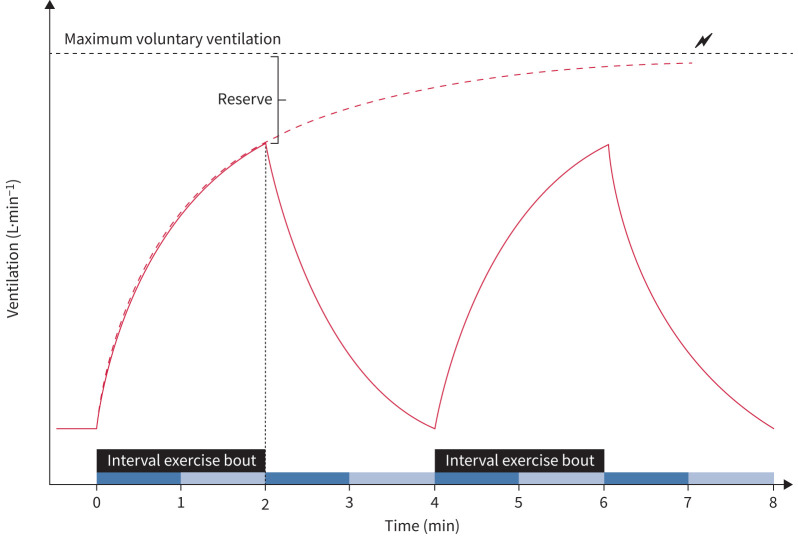
Interval training is a form of whole-body (aerobic) exercise training where the same exercises as whole-body endurance training are offered, but in shorter bouts (30 s to 2 min) alternating with rest (either lower or no load) periods. This blunts the ventilatory requirements and allows for more comfortable training with fewer symptoms [62] and unexpected interruptions of the training programme [42]. This form of exercise training makes use of the slow kinetic change in pulmonary ventilation upon the start of an exercise bout. In the example shown in figure 2, the exercise is interrupted after 2 min. This is before a high pulmonary ventilation is reached if the high intense work rate would be continued longer (dotted red line in figure 2). A resting period (typically of equal duration) is then interposed until the next high load bout starts, as depicted in figure 2.
FIGURE 2.
Change in pulmonary ventilation during constant high-intensity exercise (dashed red line) and interval training at the same work rate (red solid line) as a function of time of exercise. With constant exercise at high intensity, patients often reach maximum voluntary ventilation and have to stop the exercise. With shorter bouts of exercise, the pulmonary ventilation remains further from the maximum pulmonary ventilation and hence patients experience fewer symptoms during exercise.
A recent systematic review suggests slightly larger effects of interval training over whole-body endurance training when compared across a broad range of respiratory diseases [63]. In COPD, the clinical effects of interval training are not different from high-intensity endurance training, but the training programme is easier for patients to cope with or the only, relatively easy, alternative to deliver high loads for some of them (e.g. exercise induced hypoxia/hypercapnia, dynamic hyperinflation). High-intensity interval training, where bouts of exercise at near peak exercise intensities are interspersed with rest, is becoming increasingly more popular in many chronic conditions, including COPD [64]. In other chronic diseases important benefits were also noted in terms of improved glycaemic control, vascular health and systemic inflammatory markers [65]. Such benefits would also be potentially interesting in patients with COPD. To date, research is lacking to confirm such effects in patients with lung disease. Modifications to an interval training programme have been proposed using sinusoidal exercise training [66], where exercise intensity oscillates between higher and lower intensities and leads to lower (but more steady) pulmonary ventilation and fewer symptoms despite moments of higher work rate.
Eccentric muscle contractions, as elicited by eccentric cycling [67] or downhill walking [68], have the ability to place a significant workload on the peripheral muscles with less metabolic and ventilatory burden [69]. Significant benefits of eccentric training have been demonstrated on skeletal muscle function [70–73]. The metabolic load, however, may be too low to elicit cardiorespiratory effects [67] and effects on mitochondrial function are also uncertain [73]. Hence this form of exercise training may be of particular benefit to impact on skeletal muscle function in patients where conventional exercise training fails to elicit a significant training stimulus [71].
One-legged cycling is another way to reduce the ventilatory burden of exercise. By focussing the exercise on a single leg, the metabolic burden of exercise is reduced and allows for a higher workload on the leg at work [74]. A simple adaptation to an ergometer bicycle needs to be made to allow cycling with one leg, while the other leg is resting. This adaptation allows a higher (supramaximal) work rate when corrected for the amount of working muscle mass, while the ventilatory challenge and whole-body metabolic load remain below the maximum, rendering it an interesting exercise stimulus in an attempt to improve skeletal muscle function [75].
Resistance training (weightlifting) reduces the amount of skeletal muscle contractile units at work and requires a low whole-body metabolic load, as typically only a limited amount of high-intensity skeletal muscle contractions are made (e.g. three sets of eight contractions at 70% of the maximum contraction). To that end, resistance training machines can be used. Alternatives are to use free weights or elastic bands [76]. Elastic bands can be easily integrated in training programmes in hospital wards or at home. It is important to note that the resistance by elastic bands is limited and more repetitions are often needed in order to produce overload on the skeletal muscles trained. Such overload is important to ensure physiological effects [77].
Several studies have shown that with resistance training a high muscular workload can be offered with a low ventilatory burden [78, 79]. Besides the metabolic advantage of resistance training, this form of training is also directed specifically at the skeletal muscle. When resistance training is embedded in the exercise regimen, effects can be expected on skeletal muscle strength and skeletal muscle mass [80] as well as on skeletal muscle fibre oxidative capacity [77]. In healthy elderly people, a dose–response relation with training parameters as well as with protein intake has been observed [81, 82]. In patients with COPD, there is currently insufficient data to confirm this, although it is likely to be similar [83] as the overall response in muscle biology to resistance training in COPD is generally comparable with the response in healthy participants [84]. Importantly, resistance training also has effects on whole-body functional exercise tolerance and health-related quality of life in patients with COPD [85].
Neuromuscular electrical stimulation (NMES) is a modality of muscle stimulation with low ventilatory requirements [86]. The training consists of externally applied trains of electrical stimuli, delivered at a pre-determined frequency with a pre-defined stimulus duration alternating with a period of rest. In stable patients, a higher stimulus frequency (75 Hz) was suggested to be more effective than lower stimulation frequency (15 Hz) [87]. Another study that compared 50 Hz and 35 Hz stimulations in patients after acute exacerbations did not observe differences [88]. The effect of NMES observed in stable patients with COPD with a transfer beyond muscle function on functional exercise tolerance has been confirmed in a recent Cochrane analysis [89]. During [90] and after [91] acute exacerbations (when ventilatory capabilities are reduced), NMES can positively affect skeletal muscle function. NMES has been used as a standalone therapy or as an adjunct to regular exercise training. In both scenarios the addition of NMES led to a greater increase in skeletal muscle force and improved functional exercise tolerance [89]. In patients with disabling skeletal muscle dysfunction and those with very limited ventilatory capacity, the addition of NMES with a stimulation frequency of more than 50 Hz seems justified. Importantly, while NMES may be adequate to improve muscle function it is advised to combine this form of muscle stimulation with a functional exercise stimulus in order to engage skeletal muscle in meaningful contractions and improve mechanical efficiency (see figure 1).
Other interventions
Besides adaptations that have an impact on ventilatory capacity and training forms that require less ventilation, other exercise interventions been used to improve function in patients with COPD.
Whole-body vibration (WBV) is an intervention whereby patients perform low-intensity exercises on a vibrating platform. The vibrations cause a small mechanical stretch and subsequent reflex muscle contractions organised at a spinal level. This additional stimulus is proposed to result in additional beneficial effects in skeletal muscle function. In patients with COPD, WBV training showed significant improvements in functional exercise capacity in stable patients [92] and patients during an acute exacerbation [93]. In addition, the mechanical vibrations have a small beneficial effect on bone health in health subjects, an effect which has not been studied in COPD. A mechanism through which WBV may exert beneficial effects is through its effect on proprioception and postural balance. WBV training was shown to be as effective as an intervention to improve postural balance in patients with COPD [94]. Hence this form of treatment seems to be particularly interesting for frail patients with impaired postural balance and elevated risk for traumatic falls.
Inspiratory muscle training is a dedicated intervention targeting the inspiratory muscles that aims to enhance inspiratory muscle function and alleviate dyspnoea. The training programme obeys the physiological principles of exercise training, namely progressive overload, specificity, individual differences and reversibility. In order to achieve an overload stimulus on the respiratory muscles, patients have to breathe against an additional load that increases the work of breathing. Typically, this external load is imposed by a threshold valve or a (variable) resistance. Titrating the training intensity is done by expressing the inspiratory pressure as a proportion of the maximal inspiratory pressure. More advanced training equipment can monitor the inspiratory flow, inspiratory volume and pressure, and provides an assessment of inspiratory power and inspiratory work. In the past, inspiratory muscle training was typically prescribed as an endurance training modality whereby patients performed many inspirations against a relatively low load (e.g. 15 min at 40% of maximal inspiratory pressure). In an attempt to ensure adherence to the training programme, more recent studies have adopted a training scheme with fewer repetitions at a higher relative load [95, 96].
While there has been a lot of debate on the utility of inspiratory muscle training, it is certain that this form of training improves inspiratory muscle function. A recent systematic review also showed a clinically relevant improvement in the 6MWD after inspiratory muscle training (36 (26–46) m) [97]. The benefits on other, more comprehensive, outcomes, including physical activity and health-related quality of life, are less certain or are just (not) reaching the threshold of clinical relevance. In addition, when inspiratory muscle training is added to conventional pulmonary rehabilitation, its additional effects are less clear and may be diluted by the overwhelming effect of exercise training in general [97]. Nevertheless, in this scenario, studies conducted in patients with inspiratory muscle weakness had better inspiratory muscle function, exercise endurance time and dyspnoea during exercise [98].
In recent years, the benefits of inspiratory muscle training on breathing pattern [99] have become better understood and new devices have been introduced that allow for a more physiologic breathing pattern during inspiration [95]. Smaller studies have suggested alternative benefits of inspiratory muscle training in COPD. First, one small study showed a possible benefit on postural balance [100], which fits with earlier associations of inspiratory muscle weakness and impaired postural control in COPD [101]. Second, improved autonomic function was observed after inspiratory muscle training [102]. Similar observations were made in healthy subjects [103], people with hypertension [104] and patients with obstructive sleep apnoea [105]. While such effects are possibly important for the prevention of cardiovascular morbidity, the effects are transient and disappear when the training is interrupted. Third, one study also suggested improvements in oxygenation at night in patients that followed inspiratory muscle training, compared to controls [106]. These studies need further confirmation, but altogether provide rationale to include inspiratory muscle training in the management of selected patients, particularly those with impaired inspiratory muscle function.
Scenarios for pulmonary rehabilitation in patients with COPD
The stable patient
In patients with stable COPD, the importance of a rehabilitation programme that contains exercise training for a minimum period of 8–12 weeks is undisputed. After the latest Cochrane update, an editorial accompanying the Cochrane meta-analysis stated that no further research was needed to prove the clinical effectiveness of pulmonary rehabilitation [32]. The Global Strategy for Management of Obstructive Lung Disease advocates the use of rehabilitation and a recent Lancet commission highlighted the impact of rehabilitation in patients with COPD [107]. The contemporary discussion is therefore not whether rehabilitation should be offered, but rather how it can be offered to all patients that need it. Alternative programme settings tuned to the needs of patients in the community or in the primary care setting and telerehabilitation have been advocated as ways to make rehabilitation accessible to more patients. In all scenarios, it is important that patients are properly evaluated and their individual needs are addressed. Exercise training is offered applying the principles for exercise training outlined above. The quality and effect of the programme is assessed and the staff delivering the programme are properly trained [15]. After the core programme, it is important that a maintenance programme is set up in order to maintain its benefits and result in a sustained improvement in utilisation of healthcare resources [108]. Such programmes can be organised in the community or in primary care [16].
After a (surgical) procedure
Pulmonary rehabilitation following lung volume reduction procedures or after lung transplantation is typically advised, but few studies have formally investigated its effects [10]. After these procedures, the ventilatory capacity of patients is acutely improved and this may be the best moment to achieve a training stimulus that enhances physical fitness in these patients. It is tempting to speculate that in these patients exercise training and sustained increases in physical activity may also contribute to optimal maintenance of general health after these procedures. The best timing for rehabilitation interventions in patients receiving volume reduction remains an important question in search for resolution [109]. In patients who have undergone lung transplantation, there is less doubt as these patients acutely lose functional exercise capacity and muscle strength [110] and pulmonary rehabilitation facilitates recovery. However, the strength of the evidence is low due to the low number of studies [111]. In these patients, exercise training is also important to tackle the systemic consequences of sustained inactivity in combination with the immune suppression regimen. Exercise training can be successful in reversing these consequences. For example, a recent study showed improved bone health after exercise training in patients after lung transplantation [112] and another study showed promising results in terms of improved blood pressure [113].
During and after exacerbations of COPD
Patients that have suffered from exacerbations deserve special attention. Besides an acute increase in symptoms and acute reductions in lung function, exacerbations cause an acute decline in skeletal muscle function, functional exercise tolerance and quality of life [114]. Pulmonary rehabilitation is thus a potent intervention to improve outcome after an acute exacerbation. Programmes that include patients after exacerbations should pay attention to the specific needs of these patients. Skeletal muscle weakness, a limited ventilatory capacity, remaining gas exchange problems, anxiety and the acquisition of self-management skills to prevent further exacerbations or act appropriately are specific points of attention. After exacerbations, patients should be referred to pulmonary rehabilitation programmes [115]. Exercise training programmes should be adapted to take into account the frailty and reduced ventilatory capacity of the patients and therapists should be aware of possible relapses. The main problem in this scenario seems to be the accessibility of programmes for this group of patients. A recent health database investigation identified that only 1.5% of patients initiated rehabilitation within 3 months of discharge [116]. Innovative programme formats and better patient and clinician education could perhaps improve access in the future.
In summary
Pulmonary rehabilitation containing exercise training is a powerful intervention to improve exercise tolerance, skeletal and respiratory muscle function, efficiency of movement, symptoms of dyspnoea and fatigue, and health-related quality of life. The selection of training type as well as components of the rehabilitation programme should be individually tailored. Further research could focus on the personalisation of training types and add-on interventions to maximise the effects of the training component of rehabilitation. Pulmonary rehabilitation should be considered in stable patients in the context of volume reduction procedures and lung transplantation and in patients who have suffered exacerbations. For clinical practice, the main challenge is to ensure that accessibility and proximity of rehabilitation is secured in all healthcare systems. In addition, patient as well as clinician awareness of rehabilitation should be further enhanced. This will require more rehabilitation programmes, but also, existing programmes should offer, and payors should reimburse, different options for effective rehabilitation to tap into patient preferences.
Questions for future research
Pulmonary rehabilitation has generally shown its effectiveness across different settings and patient types. Two main research questions remain open on personalisation of rehabilitation programmes:
Identify patient phenotypes that benefit most from specific interventions so that personalised rehabilitation can be practiced in an evidence-based way by selecting patient types.
Similarly, rehabilitation has shown to be effective in different formats; however, it is likely that when formats (outpatient, centre-based, community-based, home-based, telerehabilitation or hybrid forms) are tailored to individual patients, their effectiveness could be even further optimised. It is currently unclear which patients would benefit from each of these formats. Such selection should likely take patient characteristics, contextual (e.g. social, geographic) and preference factors into account.
Points for clinical practice
Pulmonary rehabilitation should be prescribed to those patients that remain symptomatic despite optimal pharmacotherapy and to patients that suffer from exacerbations.
Exercise training in the context of pulmonary rehabilitation should be tailored to the patient's limitations, possibilities, goals and preferences. When group training is offered, different patients should still receive individualised programmes with accents to tackle patient-specific training goals.
Clinicians in all lines of healthcare should have knowledge of the rehabilitation programmes available in their area so they can effectively prescribe pulmonary rehabilitation.
Footnotes
Provenance: Commissioned article, peer reviewed.
Previous articles in this series: No. 1: Montes de Oca M, Laucho-Contreras ME. Smoking cessation and vaccination. Eur Respir Rev 2023; 32: 220187. No. 2: Volpato E, Farver-Vestergaard I, Brighton LJ, et al. Nonpharmacological management of psychological distress in people with COPD. Eur Respir Rev 2023; 32: 220170. No. 3: Owens RL, Derom E, Ambrosino N. Supplemental oxygen and noninvasive ventilation. Eur Respir Rev 2023; 32: 220159. No. 4: Verleden GM, Gottlieb J. Lung transplantation for COPD/pulmonary emphysema. Eur Respir Rev 2023; 32: 220116.
This article has an editorial commentary: https://doi.org/10.1183/16000617.0028-2023
Number 5 in the Series “Nonpharmacological interventions in COPD: state of the art and future directions” Edited by Geert M. Verleden and Wim Janssens
Conflict of interest: None declared.
Support statement: T. Troosters, H. Demeyer and W. Janssens are funded by grants of the Flemish Research Foundation (#12ZW822N, #G0C0720N) for their work related to pulmonary rehabilitation and COPD. Funding information for this article has been deposited with the Crossref Funder Registry.
References
- 1.Singh D, Donohue JF, Boucot IH, et al. Future concepts in bronchodilation for COPD: dual- versus monotherapy. Eur Respir Rev 2021; 30: 210023. doi: 10.1183/16000617.0023-2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Parshall MB, Schwartzstein RM, Adams L, et al. An official American Thoracic Society statement: update on the mechanisms, assessment, and management of dyspnea. Am J Respir Crit Care Med 2012; 185: 435–452. doi: 10.1164/rccm.201111-2042ST [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dempsey JA, Neder JA, Phillips DB, et al. The physiology and pathophysiology of exercise hyperpnea. Handb Clin Neurol 2022; 188: 201–232. doi: 10.1016/B978-0-323-91534-2.00001-1 [DOI] [PubMed] [Google Scholar]
- 4.Garcia-Aymerich J, Lange P, Benet M, et al. Regular physical activity modifies smoking-related lung function decline and reduces risk of chronic obstructive pulmonary disease: a population-based cohort study. Am J Respir Crit Care Med 2007; 175: 458–463. doi: 10.1164/rccm.200607-896OC [DOI] [PubMed] [Google Scholar]
- 5.Maltais F, Decramer M, Casaburi R, et al. An official American Thoracic Society/European Respiratory Society statement: update on limb muscle dysfunction in chronic obstructive pulmonary disease. Am J Respir Crit Care Med 2014; 189: e15–e62. doi: 10.1164/rccm.201402-0373ST [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Franssen FM, Rochester CL. Comorbidities in patients with COPD and pulmonary rehabilitation: do they matter? Eur Respir Rev 2014; 23: 131–141. doi: 10.1183/09059180.00007613 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Burke H, Wilkinson TMA. Unravelling the mechanisms driving multimorbidity in COPD to develop holistic approaches to patient-centred care. Eur Respir Rev 2021; 30: 210041. doi: 10.1183/16000617.0041-2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Witt LJ, Wroblewski KE, Pinto JM, et al. Beyond the lung: geriatric conditions afflict community-dwelling older adults with self-reported chronic obstructive pulmonary disease. Front Med 2022; 9: 814606. doi: 10.3389/fmed.2022.814606 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ebadi Z, Goërtz YMJ, Van Herck M, et al. The prevalence and related factors of fatigue in patients with COPD: a systematic review. Eur Respir Rev 2021; 30: 200298. doi: 10.1183/16000617.0298-2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Spruit MA, Singh SJ, Garvey C, et al. An official American Thoracic Society/European Respiratory Society statement: key concepts and advances in pulmonary rehabilitation. Am J Respir Crit Care Med 2013; 188: e13–e64. doi: 10.1164/rccm.201309-1634ST [DOI] [PubMed] [Google Scholar]
- 11.Agusti A, Bafadhel M, Beasley R, et al. Precision medicine in airway diseases: moving to clinical practice. Eur Respir J 2017; 50: 1701655. doi: 10.1183/13993003.01655-2017 [DOI] [PubMed] [Google Scholar]
- 12.Cosio BG, Hernández C, Chiner E, et al. Spanish COPD guidelines (GesEPOC 2021): non-pharmacological treatment update. Arch Bronconeumol 2022; 58: 345–351. doi: 10.1016/j.arbres.2021.08.010 [DOI] [PubMed] [Google Scholar]
- 13.Bolton CE, Bevan-Smith EF, Blakey JD, et al. British Thoracic Society guideline on pulmonary rehabilitation in adults. Thorax 2013; 68: Suppl. 2, ii1–ii30. doi: 10.1136/thoraxjnl-2013-203808 [DOI] [PubMed] [Google Scholar]
- 14.Russi EW, Karrer W, Brutsche M, et al. Diagnosis and management of chronic obstructive pulmonary disease: the Swiss guidelines. Official guidelines of the Swiss Respiratory Society. Respiration 2013; 85: 160–174. doi: 10.1159/000346025 [DOI] [PubMed] [Google Scholar]
- 15.Holland AE, Cox NS, Houchen-Wolloff L, et al. defining modern pulmonary rehabilitation. An Official American Thoracic Society workshop report. Ann Am Thorac Soc 2021; 18: e12–e29. doi: 10.1513/AnnalsATS.202102-146ST [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Silva L, Maricoto T, Costa P, et al. A meta-analysis on the structure of pulmonary rehabilitation maintenance programmes on COPD patients’ functional capacity. NPJ Prim Care Respir Med 2022; 32: 38. doi: 10.1038/s41533-022-00302-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Holland AE, Wageck B, Hoffman M, et al. Does pulmonary rehabilitation address treatable traits? A systematic review. Eur Respir Rev 2022; 31: 220042. doi: 10.1183/16000617.0042-2022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Souto-Miranda S, Rocha V, Mendes MA, et al. The presence of extra-pulmonary treatable traits increases the likelihood of responding to pulmonary rehabilitation. Respir Med 2023; 206: 107086. doi: 10.1016/j.rmed.2022.107086 [DOI] [PubMed] [Google Scholar]
- 19.Vanfleteren LE, Spruit MA, Groenen M, et al. Clusters of comorbidities based on validated objective measurements and systemic inflammation in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med 2013; 187: 728–735. doi: 10.1164/rccm.201209-1665OC [DOI] [PubMed] [Google Scholar]
- 20.Demeyer H, Mohan D, Burtin C, et al. Objectively measured physical activity in patients with COPD: recommendations from an international task force on physical activity. Chronic Obstr Pulm Dis 2021; 8: 528–550. doi: 10.15326/jcopdf.2021.0213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Farver-Vestergaard I, Danielsen JTT, Løkke A, et al. Psychosocial intervention in chronic obstructive pulmonary disease: meta-analysis of randomized controlled trials. Psychosom Med 2022; 84: 347–358. doi: 10.1097/PSY.0000000000001043 [DOI] [PubMed] [Google Scholar]
- 22.Farris SG, Abrantes AM, Bond DS, et al. Anxiety and fear of exercise in cardiopulmonary rehabilitation: patient and practitioner perspectives. J Cardiopulm Rehabil Prev 2019; 39: E9–E13. doi: 10.1097/HCR.0000000000000401 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nasis I, Kortianou E, Vasilopoulou M, et al. Hemodynamic effects of high intensity interval training in COPD patients exhibiting exercise-induced dynamic hyperinflation. Respir Physiol Neurobiol 2015; 217: 8–16. doi: 10.1016/j.resp.2015.06.006 [DOI] [PubMed] [Google Scholar]
- 24.Porszasz J, Emtner M, Goto S, et al. Exercise training decreases ventilatory requirements and exercise-induced hyperinflation at submaximal intensities in patients with COPD. Chest 2005; 128: 2025–2034. doi: 10.1378/chest.128.4.2025 [DOI] [PubMed] [Google Scholar]
- 25.Herth F, Hohlfeld JM, Haas J, et al. The effect of tiotropium/olodaterol versus fluticasone propionate/salmeterol on left ventricular filling and lung hyperinflation in patients with COPD. BMJ Open Respir Res 2020; 7: e000741. doi: 10.1136/bmjresp-2020-000741 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hohlfeld JM, Vogel-Claussen J, Biller H, et al. Effect of lung deflation with indacaterol plus glycopyrronium on ventricular filling in patients with hyperinflation and COPD (CLAIM): a double-blind, randomised, crossover, placebo-controlled, single-centre trial. Lancet Respir Med 2018; 6: 368–378. doi: 10.1016/S2213-2600(18)30054-7 [DOI] [PubMed] [Google Scholar]
- 27.Stone IS, Barnes NC, James WY, et al. Lung deflation and cardiovascular structure and function in chronic obstructive pulmonary disease. A randomized controlled trial. Am J Respir Crit Care Med 2016; 193: 717–726. doi: 10.1164/rccm.201508-1647OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ferte JB, Boyer FC, Taiar R, et al. Impact of resistance training on the 6-minute walk test in individuals with chronic obstructive pulmonary disease: a systematic review and meta-analysis. Ann Phys Rehabil Med 2022; 65: 101582. doi: 10.1016/j.rehab.2021.101582 [DOI] [PubMed] [Google Scholar]
- 29.Ward TJC, Plumptre CD, Dolmage TE, et al. Change in V′O2peak in response to aerobic exercise training and the relationship with exercise prescription in people with COPD: a systematic review and meta-analysis. Chest 2020; 158: 131–144. doi: 10.1016/j.chest.2020.01.053 [DOI] [PubMed] [Google Scholar]
- 30.Gudjonsdottir M, Thoroddsen E, Karlsdottir AE, et al. Evaluating the benefits of exercise training in HFrEF or COPD patients: ISO-level comparison can add valuable information to V′O2peak. J Cardiopulm Rehabil Prev 2020; 40: 421–426. doi: 10.1097/HCR.0000000000000528 [DOI] [PubMed] [Google Scholar]
- 31.Righi GA, Schuch FB, Tolves T, et al. Combined aerobic and strength training for fitness outcomes in heart failure: meta-analysis and meta-regression. Disabil Rehabil 2022; 44: 4149–4160. doi: 10.1080/09638288.2021.1900411 [DOI] [PubMed] [Google Scholar]
- 32.Lacasse Y, Cates CJ, McCarthy B, et al. This Cochrane Review is closed: deciding what constitutes enough research and where next for pulmonary rehabilitation in COPD. Cochrane Database Syst Rev 2015; 2015: ED000107. doi: 10.1002/14651858.ED000107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.American College of Sports Medicine , Chodzko-Zajko WJ, Proctor DN, et al. American College of Sports Medicine position stand. Exercise and physical activity for older adults. Med Sci Sports Exerc 2009; 41: 1510–1530. doi: 10.1249/MSS.0b013e3181a0c95c [DOI] [PubMed] [Google Scholar]
- 34.Bronstad E, Tjonna AE, Rognmo Ø, et al. Aerobic exercise training improves right- and left ventricular systolic function in patients with COPD. COPD 2013; 10: 300–306. doi: 10.3109/15412555.2012.745843 [DOI] [PubMed] [Google Scholar]
- 35.Merlo C, Bernardi E, Bellotti F, et al. Supervised exercise training improves endothelial function in COPD patients: a method to reduce cardiovascular risk? ERJ Open Res 2020; 6: 00304-2019. doi: 10.1183/23120541.00304-2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Casaburi R, Patessio A, Ioli F, et al. Reductions in exercise lactic acidosis and ventilation as a result of exercise training in patients with obstructive lung disease. Am Rev Respir Dis 1991; 143: 9–18. doi: 10.1164/ajrccm/143.1.9 [DOI] [PubMed] [Google Scholar]
- 37.Maltais F, LeBlanc P, Simard C, et al. Skeletal muscle adaptation to endurance training in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med 1996; 154: 442–447. doi: 10.1164/ajrccm.154.2.8756820 [DOI] [PubMed] [Google Scholar]
- 38.Sala E, Roca J, Marrades RM, et al. Effects of endurance training on skeletal muscle bioenergetics in chronic obstructive pulmonary disease. Am J Respir Crit Care Med 1999; 159: 1726–1734. doi: 10.1164/ajrccm.159.6.9804136 [DOI] [PubMed] [Google Scholar]
- 39.Mador MJ, Kufel TJ, Pineda LA, et al. Effect of pulmonary rehabilitation on quadriceps fatiguability during exercise. Am J Respir Crit Care Med 2001; 163: 930–935. doi: 10.1164/ajrccm.163.4.2006125 [DOI] [PubMed] [Google Scholar]
- 40.McCarthy B, Casey D, Devane D, et al. Pulmonary rehabilitation for chronic obstructive pulmonary disease. Cochrane Database Syst Rev 2015; 2015: CD003793. doi: 10.1002/14651858.CD003793.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.McNamara RJ, McKeough ZJ, McKenzie DK, et al. Water-based exercise training for chronic obstructive pulmonary disease. Cochrane Database Syst Rev 2013; 2013: CD008290. doi: 10.1002/14651858.CD008290.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Puhan MA, Büsching G, Schünemann J, et al. Interval versus continuous high-intensity exercise in chronic obstructive pulmonary disease: a randomized trial. Ann Intern Med 2006; 145: 816–825. doi: 10.7326/0003-4819-145-11-200612050-00006 [DOI] [PubMed] [Google Scholar]
- 43.Maltais F, LeBlanc P, Jobin J, et al. Intensity of training and physiologic adaptation in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med 1997; 155: 555–561. doi: 10.1164/ajrccm.155.2.9032194 [DOI] [PubMed] [Google Scholar]
- 44.Burtin C, Saey D, Saglam M, et al. Effectiveness of exercise training in patients with COPD: the role of muscle fatigue. Eur Respir J 2012; 40: 338–344. doi: 10.1183/09031936.00111811 [DOI] [PubMed] [Google Scholar]
- 45.Di Marco F, Sotgiu G, Santus P, et al. Long-acting bronchodilators improve exercise capacity in COPD patients: a systematic review and meta-analysis. Respir Res 2018; 19: 18. doi: 10.1186/s12931-018-0721-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Puente-Maestu L, Palange P, Casaburi R, et al. Use of exercise testing in the evaluation of interventional efficacy: an official ERS statement. Eur Respir J 2016; 47: 429–460. doi: 10.1183/13993003.00745-2015 [DOI] [PubMed] [Google Scholar]
- 47.Maltais F, de la Hoz A, Casaburi R, et al. Effects of tiotropium/olodaterol on activity-related breathlessness, exercise endurance and physical activity in patients with COPD: narrative review with meta-/pooled analyses. Adv Ther 2021; 38: 835–853. doi: 10.1007/s12325-020-01557-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Armstrong HF, Dussault NE, Thirapatarapong W, et al. Ventilatory efficiency before and after lung volume reduction surgery. Respir Care 2015; 60: 63–71. doi: 10.4187/respcare.03233 [DOI] [PubMed] [Google Scholar]
- 49.Palange P, Valli G, Onorati P, et al. Effect of heliox on lung dynamic hyperinflation, dyspnea, and exercise endurance capacity in COPD patients. J Appl Physiol 2004; 97: 1637–1642. doi: 10.1152/japplphysiol.01207.2003 [DOI] [PubMed] [Google Scholar]
- 50.Menadue C, Piper AJ, van't Hul AJ, et al. Non-invasive ventilation during exercise training for people with chronic obstructive pulmonary disease. Cochrane Database Syst Rev 2014; 2014: CD007714. 10.1002/14651858.CD007714.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Xiang G, Wu Q, Wu, X, et al. Non-invasive ventilation intervention during exercise training in individuals with chronic obstructive pulmonary disease: a systematic review and meta-analysis. Ann Phys Rehabil Med 2021; 64: 101460. doi: 10.1016/j.rehab.2020.101460 [DOI] [PubMed] [Google Scholar]
- 52.Bonnevie T, Gravier FE, Fresnel E, et al. NIV is not adequate for high intensity endurance exercise in COPD. J Clin Med 2020; 9: 1054. doi: 10.3390/jcm9041054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Somfay A, Porszasz J, Lee SM, et al. Dose-response effect of oxygen on hyperinflation and exercise endurance in nonhypoxaemic COPD patients. Eur Respir J 2001; 18: 77–84. doi: 10.1183/09031936.01.00082201 [DOI] [PubMed] [Google Scholar]
- 54.Miki K, Maekura R, Hiraga T, et al. Effects of oxygen on exertional dyspnoea and exercise performance in patients with chronic obstructive pulmonary disease. Respirology 2012; 17: 149–154. doi: 10.1111/j.1440-1843.2011.02086.x [DOI] [PubMed] [Google Scholar]
- 55.Megaritis D, Wagner PD, Vogiatzis I. Ergogenic value of oxygen supplementation in chronic obstructive pulmonary disease. Intern Emerg Med 2022; 17: 1277–1286. doi: 10.1007/s11739-022-03037-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Somfay A, Pórszász J, Lee S-M, et al. Effect of hyperoxia on gas exchange and lactate kinetics following exercise onset in nonhypoxemic COPD patients. Chest 2002; 121: 393–400. doi: 10.1378/chest.121.2.393 [DOI] [PubMed] [Google Scholar]
- 57.Emtner M, Porszasz J, Burns M, et al. Benefits of supplemental oxygen in exercise training in nonhypoxemic chronic obstructive pulmonary disease patients. Am J Respir Crit Care Med 2003; 168: 1034–1042. doi: 10.1164/rccm.200212-1525OC [DOI] [PubMed] [Google Scholar]
- 58.Neunhauserer D, Steidle-Kloc E, Weiss G, et al. supplemental oxygen during high-intensity exercise training in nonhypoxemic chronic obstructive pulmonary disease. Am J Med 2016; 129: 1185–1193. doi: 10.1016/j.amjmed.2016.06.023 [DOI] [PubMed] [Google Scholar]
- 59.Alison JA, McKeough ZJ, Leung RWM,et al. Oxygen compared to air during exercise training in COPD with exercise-induced desaturation. Eur Respir J 2019; 53: 1802429. doi: 10.1183/13993003.02429-2018 [DOI] [PubMed] [Google Scholar]
- 60.Freitag N, Doma K, Neunhaeuserer D, et al. Is structured exercise performed with supplemental oxygen a promising method of personalized medicine in the therapy of chronic diseases? J Pers Med; 2020; 10: 135. doi: 10.3390/jpm10030135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Dyer F, Callaghan J, Cheema K, et al. Ambulatory oxygen improves the effectiveness of pulmonary rehabilitation in selected patients with chronic obstructive pulmonary disease. Chron Respir Dis 2012; 9: 83–91. doi: 10.1177/1479972312438702 [DOI] [PubMed] [Google Scholar]
- 62.Vogiatzis I, Nanas S, Roussos C. Interval training as an alternative modality to continuous exercise in patients with COPD. Eur Respir J 2002; 20: 12–19. doi: 10.1183/09031936.02.01152001 [DOI] [PubMed] [Google Scholar]
- 63.Alexiou C, Ward L, Hume E, et al. Effect of interval compared to continuous exercise training on physiological responses in patients with chronic respiratory diseases: a systematic review and meta-analysis. Chron Respir Dis 2021; 18: 14799731211041506. doi: 10.1177/14799731211041506 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Sawyer A, Cavalheri V, Hill K. Effects of high intensity interval training on exercise capacity in people with chronic pulmonary conditions: a narrative review. BMC Sports Sci Med Rehabil 2020; 12: 22. doi: 10.1186/s13102-020-00167-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Martland R, Mondelli V, Gaughran F, et al. Can high-intensity interval training improve physical and mental health outcomes? A meta-review of 33 systematic reviews across the lifespan. J Sports Sci 2020; 38: 430–469. doi: 10.1080/02640414.2019.1706829 [DOI] [PubMed] [Google Scholar]
- 66.Porszasz J, Rambod M, van der Vaart H, et al. Sinusoidal high-intensity exercise does not elicit ventilatory limitation in chronic obstructive pulmonary disease. Exp Physiol 2013; 98: 1102–1114. doi: 10.1113/expphysiol.2012.070375 [DOI] [PubMed] [Google Scholar]
- 67.Ward TJC, Lindley MR, Ferguson RA, et al. Submaximal eccentric cycling in people with COPD: acute whole-body cardiopulmonary and muscle metabolic responses. Chest 2021; 159: 564–574. doi: 10.1016/j.chest.2020.08.2082 [DOI] [PubMed] [Google Scholar]
- 68.Camillo CA, Burtin C, Hornikx M, et al. Physiological responses during downhill walking: a new exercise modality for subjects with chronic obstructive pulmonary disease? Chron Respir Dis 2015; 12: 155–164. doi: 10.1177/1479972315575717 [DOI] [PubMed] [Google Scholar]
- 69.Rooyackers JM, Berkeljon DA, Folgering HT. Eccentric exercise training in patients with chronic obstructive pulmonary disease. Int J Rehabil Res 2003; 26: 47–49. doi: 10.1097/01.mrr.0000054807.81886.9E [DOI] [PubMed] [Google Scholar]
- 70.Inostroza M, Valdés O, Tapia G, et al. Effects of eccentric vs concentric cycling training on patients with moderate COPD. Eur J Appl Physiol 2022; 122: 489–502. doi: 10.1007/s00421-021-04850-x [DOI] [PubMed] [Google Scholar]
- 71.Camillo CA, Osadnik CR, Burtin C, et al. Effects of downhill walking in pulmonary rehabilitation for patients with COPD: a randomised controlled trial. Eur Respir J 2020; 56: 2000639. doi: 10.1183/13993003.00639-2020 [DOI] [PubMed] [Google Scholar]
- 72.Bourbeau J, De Sousa Sena R, Taivassalo T, et al. Eccentric versus conventional cycle training to improve muscle strength in advanced COPD: a randomized clinical trial. Respir Physiol Neurobiol 2020; 276: 103414. doi: 10.1016/j.resp.2020.103414 [DOI] [PubMed] [Google Scholar]
- 73.MacMillan NJ, Kapchinsky S, Konokhova Y, et al. Eccentric ergometer training promotes locomotor muscle strength but not mitochondrial adaptation in patients with severe chronic obstructive pulmonary disease. Front Physiol 2017; 8: 114. doi: 10.3389/fphys.2017.00114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Dolmage TE, Goldstein RS. Response to one-legged cycling in patients with COPD. Chest 2006; 129: 325–332. doi: 10.1378/chest.129.2.325 [DOI] [PubMed] [Google Scholar]
- 75.Ribeiro F, Oueslati F, Saey D, et al. Cardiorespiratory and muscle oxygenation responses to isokinetic exercise in chronic obstructive pulmonary disease. Med Sci Sports Exerc 2019; 51: 841–849. doi: 10.1249/MSS.0000000000001856 [DOI] [PubMed] [Google Scholar]
- 76.de Lima FF, Cavalheri V, Silva BSA, et al. Elastic resistance training produces benefits similar to conventional resistance training in people with chronic obstructive pulmonary disease: systematic review and meta-analysis. Phys Ther 2020; 100: 1891–1905. doi: 10.1093/ptj/pzaa149 [DOI] [PubMed] [Google Scholar]
- 77.Nyberg A, Martin M, Saey D, et al. Effects of low-load/high-repetition resistance training on exercise capacity, health status, and limb muscle adaptation in patients with severe COPD: a randomized controlled trial. Chest 2021; 159: 1821–1832. doi: 10.1016/j.chest.2020.12.005 [DOI] [PubMed] [Google Scholar]
- 78.Robles P, Araujo T, Brooks D, et al. Cardiorespiratory responses to short bouts of resistance training exercises in individuals with chronic obstructive pulmonary disease: a comparison of exercise intensities. J Cardiopulm Rehabil Prev 2017; 37: 356–362. doi: 10.1097/HCR.0000000000000282 [DOI] [PubMed] [Google Scholar]
- 79.Nyberg A, Saey D, Martin M, et al. Cardiorespiratory and muscle oxygenation responses to low-load/high-repetition resistance exercises in COPD and healthy controls. J Appl Physiol 2018; 124: 877–887. doi: 10.1152/japplphysiol.00447.2017 [DOI] [PubMed] [Google Scholar]
- 80.De Brandt J, Spruit MA, Hansen D, et al. Changes in lower limb muscle function and muscle mass following exercise-based interventions in patients with chronic obstructive pulmonary disease: a review of the English-language literature. Chron Respir Dis 2018; 15: 182–219. doi: 10.1177/1479972317709642 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Morton RW, Murphy KT, McKellar SR, et al. A systematic review, meta-analysis and meta-regression of the effect of protein supplementation on resistance training-induced gains in muscle mass and strength in healthy adults. Br J Sports Med 2018; 52: 376–384. doi: 10.1136/bjsports-2017-097608 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Tagawa R, Watanabe D, Ito K, et al. Synergistic effect of increased total protein intake and strength training on muscle strength: a dose-response meta-analysis of randomized controlled trials. Sports Med Open 2022; 8: 110. doi: 10.1186/s40798-022-00508-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Huhn A, Flenker U, Diel P. Effects of carbohydrate and protein administration by food items on strength response after training in stable COPD. Nutrients 2022; 14: 3565. doi: 10.3390/nu14173565 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Molmen KS, Hammarström D, Falch GS, et al. Chronic obstructive pulmonary disease does not impair responses to resistance training. J Transl Med 2021; 19: 292. doi: 10.1186/s12967-021-02969-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Spruit MA, Gosselink R, Troosters T, et al. Resistance versus endurance training in patients with COPD and peripheral muscle weakness. Eur Respir J 2002; 19: 1072–1078. doi: 10.1183/09031936.02.00287102 [DOI] [PubMed] [Google Scholar]
- 86.Sillen MJ, Franssen FM, Vaes AW, et al. Metabolic load during strength training or NMES in individuals with COPD: results from the DICES trial. BMC Pulm Med 2014; 14: 146. doi: 10.1186/1471-2466-14-146 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Sillen MJ, Franssen FM, Delbressine JM, et al. Efficacy of lower-limb muscle training modalities in severely dyspnoeic individuals with COPD and quadriceps muscle weakness: results from the DICES trial. Thorax 2014; 69: 525–531. doi: 10.1136/thoraxjnl-2013-204388 [DOI] [PubMed] [Google Scholar]
- 88.Chaplin EJ, Houchen L, Greening NJ, et al. Neuromuscular stimulation of quadriceps in patients hospitalised during an exacerbation of COPD: a comparison of low (35 Hz) and high (50 Hz) frequencies. Physiother Res Int 2013; 18: 148–156. doi: 10.1002/pri.1541 [DOI] [PubMed] [Google Scholar]
- 89.Hill K, Cavalheri V, Mathur S, et al. Neuromuscular electrostimulation for adults with chronic obstructive pulmonary disease. Cochrane Database Syst Rev 2018; 5: CD010821. doi: 10.1002/14651858.CD010821.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Giavedoni S, Deans A, McCaughey P, et al. Neuromuscular electrical stimulation prevents muscle function deterioration in exacerbated COPD: a pilot study. Respir Med 2012; 106: 1429–1434. doi: 10.1016/j.rmed.2012.05.005 [DOI] [PubMed] [Google Scholar]
- 91.Abdellaoui A, Préfaut C, Gouzi F, et al. Skeletal muscle effects of electrostimulation after COPD exacerbation: a pilot study. Eur Respir J 2011; 38: 781–788. doi: 10.1183/09031936.00167110 [DOI] [PubMed] [Google Scholar]
- 92.Berner K, Albertyn SCS, Dawnarain S, et al. The effectiveness of combined lower limb strengthening and whole-body vibration, compared to strengthening alone, for improving patient-centred outcomes in adults with COPD: a systematic review. S Afr J Physiother 2020; 76: 1412. doi: 10.4102/sajp.v76i1.1412 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Dobler CC, Morrow AS, Farah MH, et al. Nonpharmacologic therapies in patients with exacerbation of chronic obstructive pulmonary disease: a systematic review with meta-analysis. Mayo Clin Proc 2020; 95: 1169–1183. doi: 10.1016/j.mayocp.2020.01.018 [DOI] [PubMed] [Google Scholar]
- 94.Gloeckl R, Schneeberger T, Leitl D, et al. Whole-body vibration training versus conventional balance training in patients with severe COPD–a randomized, controlled trial. Respir Res 2021; 22: 138. doi: 10.1186/s12931-021-01688-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Langer D, Charususin N, Jácome C, et al. Efficacy of a novel method for inspiratory muscle training in people with chronic obstructive pulmonary disease. Phys Ther 2015; 95: 1264–1273. doi: 10.2522/ptj.20140245 [DOI] [PubMed] [Google Scholar]
- 96.Hill K, Cecins NM, Eastwood PR, et al. Inspiratory muscle training for patients with chronic obstructive pulmonary disease: a practical guide for clinicians. Arch Phys Med Rehabil 2010; 91: 1466–1470. doi: 10.1016/j.apmr.2010.06.010 [DOI] [PubMed] [Google Scholar]
- 97.Ammous O, Feki W, Lotfi T, et al. Inspiratory muscle training, with or without concomitant pulmonary rehabilitation, for chronic obstructive pulmonary disease (COPD). Cochrane Database Syst Rev 2023; 1: CD013778. doi: 10.1002/14651858.CD013778.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Charususin N, Gosselink R, Decramer M, et al. Randomised controlled trial of adjunctive inspiratory muscle training for patients with COPD. Thorax 2018; 73: 942–950. doi: 10.1136/thoraxjnl-2017-211417 [DOI] [PubMed] [Google Scholar]
- 99.Langer D, Ciavaglia C, Faisal A, et al. Inspiratory muscle training reduces diaphragm activation and dyspnea during exercise in COPD. J Appl Physiol 2018; 125: 381–392. doi: 10.1152/japplphysiol.01078.2017 [DOI] [PubMed] [Google Scholar]
- 100.Tounsi B, Acheche A, Lelard T, et al. Effects of specific inspiratory muscle training combined with whole-body endurance training program on balance in COPD patients: randomized controlled trial. PLoS ONE 2021; 16: e0257595. doi: 10.1371/journal.pone.0257595 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Janssens L, Brumagne S, McConnell AK, et al. Proprioceptive changes impair balance control in individuals with chronic obstructive pulmonary disease. PLoS One 2013; 8: e57949. doi: 10.1371/journal.pone.0057949 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Cutrim ALC, Duarte AAM, Silva-Filho AC, et al. Inspiratory muscle training improves autonomic modulation and exercise tolerance in chronic obstructive pulmonary disease subjects: a randomized-controlled trial. Respir Physiol Neurobiol 2019; 263: 31–37. doi: 10.1016/j.resp.2019.03.003 [DOI] [PubMed] [Google Scholar]
- 103.Rodrigues GD, Dal Lago P, da Silva Soares PP. Time-dependent effects of inspiratory muscle training and detraining on cardiac autonomic control in older women. Exp Gerontol 2021; 150: 111357. doi: 10.1016/j.exger.2021.111357 [DOI] [PubMed] [Google Scholar]
- 104.Ferreira JB, Plentz RD, Stein C, et al. Inspiratory muscle training reduces blood pressure and sympathetic activity in hypertensive patients: a randomized controlled trial. Int J Cardiol 2013; 166: 61–67. doi: 10.1016/j.ijcard.2011.09.069 [DOI] [PubMed] [Google Scholar]
- 105.Ramos-Barrera GE, DeLucia CM, Bailey EF. Inspiratory muscle strength training lowers blood pressure and sympathetic activity in older adults with OSA: a randomized controlled pilot trial. J Appl Physiol 2020; 129: 449–458. doi: 10.1152/japplphysiol.00024.2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Heijdra YF, Dekhuijzen PN, van Herwaarden CL, et al. Nocturnal saturation improves by target-flow inspiratory muscle training in patients with COPD. Am J Respir Crit Care Med 1996; 153: 260–265. doi: 10.1164/ajrccm.153.1.8542126 [DOI] [PubMed] [Google Scholar]
- 107.Stolz D, Mkorombindo T, Schumann DM, et al. Towards the elimination of chronic obstructive pulmonary disease: a Lancet commission. Lancet 2022; 400: 921–972. doi: 10.1016/S0140-6736(22)01273-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Jenkins AR, Gowler H, Curtis F, et al. Efficacy of supervised maintenance exercise following pulmonary rehabilitation on health care use: a systematic review and meta-analysis. Int J Chron Obstruct Pulmon Dis 2018; 13: 257–273. doi: 10.2147/COPD.S150650 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Hartman JE, Vanfleteren LEGW, van Rikxoort EM, et al. Endobronchial valves for severe emphysema. Eur Respir Rev 2019; 28: 180121. doi: 10.1183/16000617.0121-2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Maury G, Langer D, Verleden G, et al. Skeletal muscle force and functional exercise tolerance before and after lung transplantation: a cohort study. Am J Transplant 2008; 8: 1275–1281. doi: 10.1111/j.1600-6143.2008.02209.x [DOI] [PubMed] [Google Scholar]
- 111.Gutierrez-Arias R, Martinez-Zapata MJ, Gaete-Mahn MC, et al. Exercise training for adult lung transplant recipients. Cochrane Database Syst Rev 2021; 7: CD012307. doi: 10.1002/14651858.CD012307.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Ulvestad M, Godang K, Durheim MT, et al. Effect of high-intensity training on bone health and body composition in lung transplant recipients: a secondary analysis of a randomized controlled trial. Clin Transplant 2021; 35: e14375. doi: 10.1111/ctr.14375 [DOI] [PubMed] [Google Scholar]
- 113.Langer D, Burtin C, Schepers L, et al. Exercise training after lung transplantation improves participation in daily activity: a randomized controlled trial. Am J Transplant 2012; 12: 1584–1592. doi: 10.1111/j.1600-6143.2012.04000.x [DOI] [PubMed] [Google Scholar]
- 114.Machado A, Barusso M, De Brandt J, et al. Impact of acute exacerbations of COPD on patients’ health status beyond pulmonary function: a scoping review. Pulmonology 2022; in press [ 10.1016/j.pulmoe.2022.04.004]. [DOI] [PubMed] [Google Scholar]
- 115.Wedzicha JA, Miravitlles M, Hurst JR, et al. Management of COPD exacerbations: a European Respiratory Society/American Thoracic Society guideline. Eur Respir J 2017; 49: 1600791. doi: 10.1183/13993003.00791-2016 [DOI] [PubMed] [Google Scholar]
- 116.Lindenauer PK, Stefan MS, Pekow PS, et al. Association between initiation of pulmonary rehabilitation after hospitalization for COPD and 1-year survival among medicare beneficiaries. JAMA 2020; 323: 1813–1823. doi: 10.1001/jama.2020.4437 [DOI] [PMC free article] [PubMed] [Google Scholar]