Abstract
Glomus tumors, which account for less than 2% of soft tissue tumors, are a rare benign soft tissue neoplasm. They originated from neuro-myo-arterial glomus tissue whose primary function is regulation of the body temperature. This tissue is commonly located in the dermis or subcutis in the subungual region; however, it can be extracutaneous such as in bones, the genitourinary tract, the gastrointestinal tract, and the respiratory tract. Histologically, a glomus tumor is made of proliferating rounded or cuboidal epithelioid cells in a meshwork of blood vessels. Although a benign growth, they can rarely show malignant features with infiltration of surrounding tissue with the rapid multiplication of cells in which case it is labeled as a malignant glomus tumor. Pulmonary glomus tumors are extremely rare and most commonly occur in middle-aged men. They are mostly asymptomatic, but a small percentage of patients may present with hemoptysis and cough if there is large airway involvement. We present an interesting case of a middle-aged man presenting with cough and occasional hemoptysis, found to have an endobronchial nodular lesion, and subsequently diagnosed with a pulmonary glomus tumor.
Keywords: benign lung nodule, isolated lung nodule, endobronchial nodule, pulmonary glomus tumor, glomus tumor
Introduction
Glomus tumors are rare benign soft tissue neoplasms that originate from glomus bodies that function as temperature-regulating organs [1]. Pulmonary glomus tumors are extremely rare and most commonly occur in middle-aged men [2-4]. Glomus tumors originating from the pulmonary tract are usually asymptomatic, but rarely, patients may present with hemoptysis and cough if there is large airway involvement [5,6]. We present an interesting case of an endobronchial pulmonary glomus tumor diagnosed with bronchoscopy and treated with electrocautery snare resection and argon plasma coagulation.
This article was presented as a meeting abstract at the 2022 American College of Chest Physicians meeting on October 17, 2022.
Case presentation
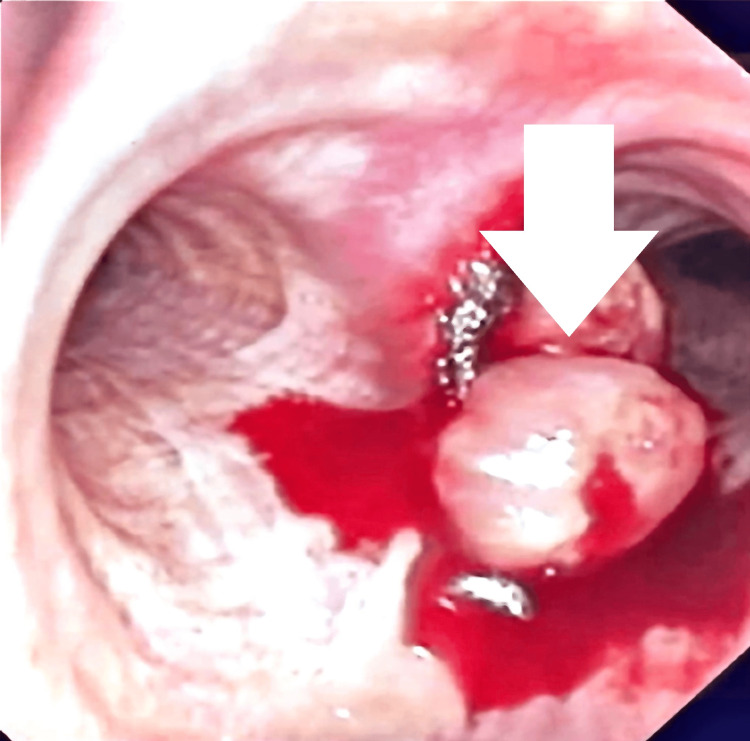
A 52-year-old male presented to the outpatient clinic with a chronic productive cough (yellowish sputum) and hemoptysis. He had a significant history of smoking (10 pack years) and had quit approximately 14 years before the current presentation. The computed tomography (CT) of the chest revealed a right mainstem endobronchial lesion, which was further explored with bronchoscopy, to be defined as a rounded lesion within the right mainstem bronchus (Figure 1).
Figure 1. Bronchoscopic view of the right mainstem bronchus.
A rounded lesion within the right mainstem bronchus was noted (arrowhead).
The endobronchial biopsy results showed findings consistent with a glomus tumor. A positron emission tomography (PET) CT for metastasis workup was obtained, which was negative for any other metastatic foci. A repeat bronchoscopy was performed for electrocautery snare resection and argon plasma coagulation to successfully remove the tumor without complication.
Discussion
Glomus tumors in the pulmonary tract are very uncommon findings. These are often benign growths comprising perivascular cells [7,8]. In the respiratory tract, the glomus tumors can affect the mainstem bronchi and pulmonary parenchyma. It is described as the protruding, polypoidal mass in the bronchial tract and nodular mass in the parenchymal tissue. A variety of other conditions can mimic pulmonary glomus tumors such as carcinoid tumors, leiomyoma, pulmonary sclerosing pneumocytoma, lymphoma, solitary fibrous tumor, or peripheral primitive neuroectodermal tumor [9-12]. Immunohistochemical staining is beneficial in the diagnosis of glomus tumors and in differentiating them from other conditions. Glomus tumor cells are round or oval in shape and stain-positive for type IV collagen, vimentin, and smooth muscle actin [13,14]. The mainstay of treatment of glomus tumors is surgical resection, but there is an increased utilization of endoscopic resection with successful results, as noted in our case [15]. However, it is also important to take into consideration tumor location and malignant potential in deciding between open versus endoscopic resection [16,17].
Conclusions
Glomus tumors are benign tumors, which have been rarely described in the respiratory tract. Although these growths have very limited malignant potential, they should be investigated in pathology and imaging studies. These tumors can be managed with resection, which should be given consideration, as these vascular tumors can cause complications such as massive hemoptysis if not removed. With this case report, we intend to increase awareness among medical professionals about this rare condition.
The authors have declared that no competing interests exist.
Human Ethics
Consent was obtained or waived by all participants in this study
References
- 1.Pulmonary glomus tumor. Dalfior D, Parisi A, Cannizzaro C, et al. Int J Surg Pathol. 2008;16:81–84. doi: 10.1177/1066896907304520. [DOI] [PubMed] [Google Scholar]
- 2.Two cases of glomus tumor arising in large airway: well organized radiologic, macroscopic and microscopic findings. Choi IH, Song DH, Kim J, Han J. Tuberc Respir Dis (Seoul) 2014;76:34–37. doi: 10.4046/trd.2014.76.1.34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Primary pulmonary glomus tumor of uncertain malignant potential: a case report with literature review focusing on current concepts of malignancy grade estimation. Oide T, Yasufuku K, Shibuya K, Yoshino I, Nakatani Y, Hiroshima K. Respir Med Case Rep. 2016;19:143–149. doi: 10.1016/j.rmcr.2016.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tracheal glomus tumor: a case report and review of literature. Venegas O, Newton A, Vergara N, Singhal S, Predina JD. Rare Tumors. 2017;9:6848. doi: 10.4081/rt.2017.6848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.A primary pulmonary glomus tumor: a case report and review of the literature. Ariizumi Y, Koizumi H, Hoshikawa M, et al. Case Rep Pathol. 2012;2012:782304. doi: 10.1155/2012/782304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Primary pulmonary glomus tumor, diagnosed by preoperative needle biopsy: report of one case and literature review. Kim MJ, Sung WJ. https://www.jpatholtm.org/upload/pdf/kjp-42-1-37.pdf Korean J Pathol. 2008;42:37–40. [Google Scholar]
- 7.Behavior of primary tracheal glomus tumor, uncertain malignant potential subtype. Jin Y, Al Sawalhi S, Zhao D, Cai H, Odeh AM, Xie H, Song J. Gen Thorac Cardiovasc Surg. 2019;67:991–995. doi: 10.1007/s11748-019-01085-8. [DOI] [PubMed] [Google Scholar]
- 8.Bronchial glomus tumor: report of 2 cases and review of the literature. Zhang X, Zhu Y, Wang X, Miao J, Li H, Tong Z. https://pubmed.ncbi.nlm.nih.gov/25537412/ Zhonghua Jie He He Hu Xi Za Zhi. 2014;37:758–763. [PubMed] [Google Scholar]
- 9.Glomus tumor of uncertain malignant potential of the lung: a case report and review of literature. Wan PZ, Han Q, Wang EH, Lin XY. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4713688/ Int J Clin Exp Pathol. 2015;8:15402–15406. [PMC free article] [PubMed] [Google Scholar]
- 10.Malignant glomus tumor of the lung with multiple metastasis: a rare case report. Wang S, Ding C, Tu J. http://10.1186/s12957-014-0423-3. World J Surg Oncol. 2015;13:22. doi: 10.1186/s12957-014-0423-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Malignant glomus tumor of the lung with multiorgan metastases: case report and literature review. Dong LL, Chen EG, Sheikh IS, Jiang ZN, Huang AH, Ying KJ. Onco Targets Ther. 2015;8:1909–1914. doi: 10.2147/OTT.S89396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Glomus tumor of uncertain malignant potential arising in the bronchus. Zhu YZ, Li WP, Wang ZY, Yang HF, He QL, Zhu HG, Zheng GJ. J Cardiothorac Surg. 2013;8:146. doi: 10.1186/1749-8090-8-146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Clinical and histopathological diagnosis of glomus tumor: an institutional experience of 138 cases. Mravic M, LaChaud G, Nguyen A, Scott MA, Dry SM, James AW. Int J Surg Pathol. 2015;23:181–188. doi: 10.1177/1066896914567330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Features of gastric glomus tumor: a clinicopathologic, immunohistochemical and molecular retrospective study. Wang ZB, Yuan J, Shi HY. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4014223/#__ffn_sectitle. Int J Clin Exp Pathol. 2014;7:1438–1448. [PMC free article] [PubMed] [Google Scholar]
- 15.Tracheobronchial glomus tumor. Lange TH, Magee MJ, Boley TM, Bell SW, Hazelrigg SR. Ann Thorac Surg. 2000;70:292–295. doi: 10.1016/s0003-4975(00)01274-1. [DOI] [PubMed] [Google Scholar]
- 16.One very rare and one new tracheal tumour found by electron microscopy: glomus tumour and acinic cell tumour resembling carcinoid tumours by light microscopy. Heard BE, Dewar A, Firmin RK, Lennox SC. Thorax. 1982;37:97–103. doi: 10.1136/thx.37.2.97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.A rare case of bronchial glomus tumor. Oizumi S, Kon Y, Ishida T, et al. Respiration. 2001;68:95–98. doi: 10.1159/000050471. [DOI] [PubMed] [Google Scholar]