Abstract
Growth of abdominal aortic aneurysms (AAAs) is often described as erratic and discontinuous. This study aimed at describing growth patterns of AAAs with respect to maximal aneurysm diameter (Dmax) and aneurysm volume, and to characterize changes in the intraluminal thrombus (ILT) and biomechanical indices as AAAs grow. 384 computed tomography angiographies (CTAs) from 100 patients (mean age 70.0, standard deviation, SD = 8.5 years, 22 women), who had undergone at least three CTAs, were included. The mean follow-up was 5.2 (SD = 2.5) years. Growth of Dmax was 2.64 mm/year (SD = 1.18), volume 13.73 cm3/year (SD = 10.24) and PWS 7.3 kPa/year (SD = 4.95). For Dmax and volume, individual patients exhibited linear growth in 87% and 77% of cases. In the tertile of patients with the slowest Dmax-growth (< 2.1 mm/year), only 67% belonged to the slowest tertile for volume-growth, and 52% and 55% to the lowest tertile of PWS- and PWRI-increase, respectively. The ILT-ratio (ILT-volume/aneurysm volume) increased with time (2.6%/year, p < 0.001), but when adjusted for volume, the ILT-ratio was inversely associated with biomechanical stress. In contrast to the notion that AAAs grow in an erratic fashion most AAAs displayed continuous and linear growth. Considering only change in Dmax, however, fails to capture the biomechanical risk progression, and parameters such as volume and the ILT-ratio need to be considered.
Subject terms: Health care, Cardiovascular diseases
Introduction
Abdominal aortic aneurysms (AAAs) are irreversible dilatations of the abdominal aorta that are associated with a risk of rupture1. Rupture is often a fatal event2, and currently the only effective treatment is elective surgery prior to rupture, by either open surgical repair or endovascular repair1,3. As AAAs are only effectively treated before rupture, but are in general asymptomatic, they are either found through incidental detection on radiological examinations, or specifically designed screening programs. Once an AAA is found, patients are put under surveillance, with primarily ultrasound, and followed until the AAA reaches the surgical-threshold diameter1,3.
Diameter growth of aneurysms has been described as discontinuous, erratic and nonlinear4–7. The inter-observer variability of maximal aneurysm diameter (Dmax) measurements, between both computed tomography (CT) and ultrasonography are significant8–10. Even for a CT of a single patient with an AAA, many ways of measuring the maximal aneurysm diameter have been described8. The fastest diameter growth in an AAA does not always occur at the Dmax location11, and it has been suggested that volume growth is a more sensitive marker of aneurysm disease progression12,13. Semi-automatic measurements, where a diameter is computationally measured from a segmented aneurysm may be more accurate compared to manual diameter readings, and may contribute to improved growth prediction of AAAs14.
Biomechanical analysis has shown potential to improve prediction of both AAA rupture and growth. Peak wall stress (PWS) is higher in ruptured AAAs15,16, and peak wall rupture index (PWRI), is increased in AAAs prior to rupture17. Further, PWRI correlates to aneurysm volume-growth13. However, only small studies have reported on the development over time of these biomechanical parameters18,19.
The primary aim was to investigate the growth pattern of AAAs with respect to semi-automatic Dmax and volume assessment in a cohort of patients that had undergone at least three CT angiograms (CTAs). The secondary aim was to characterize the changes in intraluminal thrombus (ILT) and biomechanical properties (PWS and PWRI) in relation to AAA growth.
Methods
Study cohort
Patients who presented with intact AAA (ICD code I71.4) to the Department of Vascular Surgery at Karolinska University Hospital between the years 2012–2013 were screened for inclusion. Patients were included if they had undergone ≥ 3 CTAs, that were at least 3 months apart, at any point. At our centre patients with AAAs are in general surveyed with ultrasound, and many of the CTs included may have been performed for indications other than AAA. Patients with mycotic, infectious or thoracoabdominal AAAs were excluded. CTAs were extracted from the hospital picture archiving and communications systems. Patient characteristics including age, sex and smoking status were collected from the electronic medical records.
Geometric characterization and finite element analysis
For 3D-segmentation and Finite element analysis, A4Clinics (VASCOPS GmbH, Graz, Austria) was used. The program is commercially available, and the methods are detailed elsewhere20,21.
In short, the analysis is initiated by segmentation of the AAA, including lumen, ILT and vessel wall. The segmentation is semi-automatic, and based on deformable balloon models which generate a hexahedral dominated mesh for the finite element analysis20. The model is given constitutive properties that represent the stress and strain relation of the tissue. These are assigned based on data from ex-vivo biaxial tensile testing. The wall and the thrombus were both model as hyperelastic, isotropic and incompressible22,23. The wall strength of the AAA is inhomogeneous and estimated based on geometric characteristics (relative expansion of the aorta, the thickness of overlying thrombus), and can be adjusted with patient characteristics (sex, age and heredity for rupture, long-term blood pressure)24. The model is fixed at the boundaries, the renal arteries and the aortic bifurcation, and no interaction with the surrounding tissue was considered.
All patients were simulated with the same patient characteristics (65 years old, male, blood pressure 140/80 mmHg and no heredity for rupture). These patient characteristics were used to neutralize their effect on the wall strength model and thereby study the effects of changing aneurysm morphology on the biomechanical parameters. For all geometric and biomechanical parameters, the aneurysm was considered between the lowest renal artery (excluding polar arteries) and the aortic bifurcation. For each segmented CTA, the software outputs the following parameters that are considered in this paper: maximal aneurysm diameter (Dmax), total aneurysm volume, ILT volume, lumen volume, peak wall stress (PWS) and peak wall rupture index (PWRI). PWS denotes the maximum von Mises stress at any point in the AAA, and PWRI is the maximum ratio of wall stress to wall strength25. The maximal diameter is measured perpendicular to the vessel centreline and corresponds to the maximal diameter in any direction within the cross-section. ILT ratio is defined as ILT volume / total aneurysm volume.
CTA images with a slice thickness of > 5 mm were excluded. If slice thickness was > 3 mm (n = 25), images were resampled isotropically with b-splines using the 3D slicer software (version 4.11.0–2020-07–09)26 to allow for more detailed reconstruction.
Statistical analysis
All statistical analyses were performed using R version 4.04 (R Foundation for Statistical Computing, Vienna, Austria)27. Statistical significance was defined as p < 0.05.
To account for repeated observations for each patient, data were modelled using mixed-effects models fitted with the R packages lmerTest28. Mixed-effects models allow for the specification of patient-level random slopes and intercepts. For all models in this paper random intercepts and slopes are specified. The influence of patient characteristics on the time-dependent change of the analysed geometric and biomechanical parameters are modelled with an interaction term between time and the specified patient characteristic. The presented estimates represent the marginal effects and are calculated using the margins package29, and the corresponding p-value denotes the statistical significance of the time-interaction variable. Patient-level growth rates for Dmax, aneurysm volume, lumen volume and ILT volume, as well as relative growth rates for Dmax and volume represent patient-level conditional estimates from the corresponding mixed-effects model.
To evaluate the fit of a simple time-dependent linear model to the data, each patient was fitted with a linear regression with the morphological or biomechanical variable as the outcome and time as the independent variable. An r-squared value above 0.90 was considered as appropriate to describe the growth of the individual patient as linear, this definition was also used by others30. Difference in correlation coefficients was tested with the Dunn and Clark’s test, as implemented in the cocor-package.
Ethical considerations
The study was approved by the Regional Ethical Review Board in Stockholm and conformed to the principles outlined in the Declaration of Helsinki. Informed consent was not considered necessary. Individual patient data will not be made publicly available since it was not part of the Ethical approval for this study.
Results
Patient cohort
For all 100 included patients and 384 CTAs, FEA and geometric characterization was performed. Patients had a mean age of 70.0 (SD = 8.5) years, were mostly male (78%) and a majority (87%) had a history of smoking. Fifty-two patients had 3 CTs, 26 had 4 CTs and 22 patients had 5 or more CTs included. The mean total follow-up (time between first and last included CT) was 5.2 (SD = 2.5) years, and the mean time between CTs was 2.7 (SD = 1.5) years. At baseline, Dmax was 43.9 (SD = 6.8) mm and PWS was 169 (SD = 44) kPa. The mean growth rate of the Dmax in the cohort was 2.64 (SD = 1.18) mm / year, mean aneurysm volume growth was 14.3 (SD = 10.2) cm3 / year and the mean PWS increased 7.4 (SD = 5.0) kPa/year (Table 1).
Table 1.
Summary of baseline patient characteristics.
| Patient characteristics (n = 100) | ||
|---|---|---|
| Age at baseline -yrs | 70.0 (8.5) | |
| Sex = Male | 78 (78%) | |
| Current smoker | 36 (36%), Missing: 1 | |
| Ever smoker | 86 (87%), Missing: 1 | |
| Height -cm | 174.0 (8.8), Missing: 5 | |
| Weight -kg | 82.6 (16.6), Missing: 6 | |
| BSA -m2 | 1.97 (0.22), Missing: 6 | |
| BMI -kg/m2 | 27.1 (4.5), Missing: 6 |
| CTAs (n = 384) | ||
|---|---|---|
|
Median No. of CTA s per patient –n |
3.0 (3.0–4.0) | |
| Mean time between CTAs -years | 2.7 (1.5) | |
| Mean total follow-up time -years | 5.2 (2.5) |
| Measurements (n = 100) |
Baseline Mean (sd) |
Crude growth rate– estimate (/year) (sd) † |
|---|---|---|
| Dmax -mm | 43.9 (6.8) | 2.64 (1.18) |
| Aneurysm volume -cm3 | 94 (33) | 14.28 (10.24) |
| Lumen volume -cm3 | 53 (19) | 5.05 (6.04) |
| ILT volume -cm3 | 23 (20) | 8.00 (7.24) |
| Peak wall stress -kPa | 169 (44) | 7.39 (4.95) |
| Peak wall rupture index -% | 29.6 (8.1) | 2.38 (2.14) |
BSA = body surface area, BMI = body mass index, CTA = computed tomography angiography, Dmax = maximal aneurysm diameter, ILT = intraluminal thrombus. Values denote n (%), mean (standard deviation) or median (interquartile range). † Estimates refer to estimates from mixed effects models, where the variable is a function of time with random intercepts and slopes. Standard deviation refers to the variability in the random slopes.
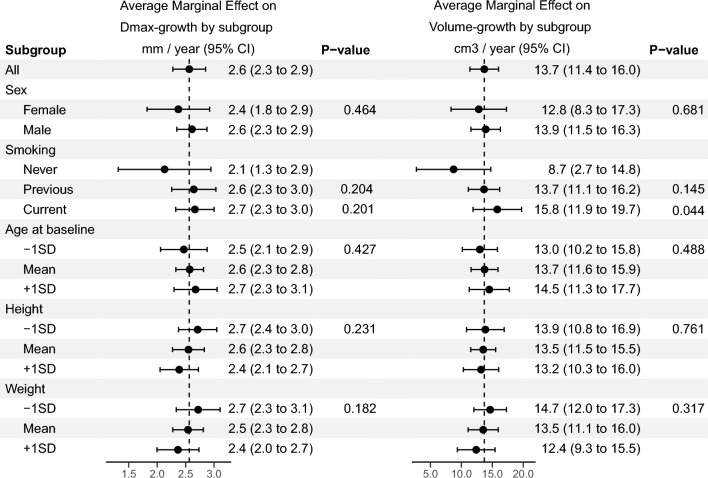
Women and men displayed similar growth rates for Dmax (2.4, 95% CI 1.8–2.9 mm/year vs 2.6, 2.3–2.9 mm/year, p = 0.46) and aneurysm volume (12.8, 8.3–17.3 cm3/year vs 13.9, 11.5–16.3 cm3/year, p = 0.68) (Fig. 1). Current smokers had a significantly higher volume growth rate compared to never smokers, (p < 0.044). Increasing age at baseline was associated with a slower increase in PWRI (p = 0.036). Other patient characteristics had no significant interaction with time for Dmax and Aneurysm volume (Fig. 1), or, PWS and PWRI (Supplementary Fig. 1).
Figure 1.
Subgroup analysis of AAA growth over time for Dmax (maximal aneurysm diameter) and aneurysm volume. Average marginal effect and 95% confidence interval around the estimate refer to estimate growth for patients belonging to the subcategory. P-value refers to the significance of the interaction term between time and the subgroup.
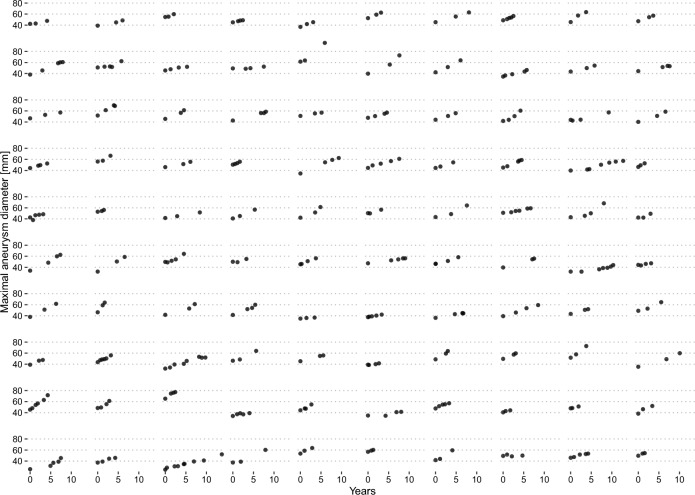
Dmax-growth appeared qualitatively continous and mostly linear (Fig. 2). Individual linear-regression models fitted to each patient revealed an excellent fit (r-squared > 0.90) for 87% of patients, and a mean r-squared of 0.94 ± 0.12. A simple linear-time model for aneurysm volume had an excellent fit in 77% of cases. Growth curves for aneurysm volume over time for the included patients in the study are presented in Supplementary Fig. 2. For Lumen volume, ILT-volume, PWS and PWRI the r-squared value was above 0.90 in 39%, 61%, 38% and 35% of cases respectively (Table 2). Despite this, the mean r-squared values for all fits was above 0.65.
Figure 2.
Maximum aneurysm diameter over time for all patients that are included in the study. A single plot represents one patient, and a dot represents one CTA examination. Y axis denotes the maximum aneurysm diameter (mm), and the x-axis time (in years) from inclusion into the study.
Table 2.
Goodness of fit for individual linear regression models fitted to each patient.
| R-squared | |||
|---|---|---|---|
| Mean | SD | > .90 (n)† | |
| Dmax | 0.94 | 0.12 | 87 |
| Aneurysm volume | 0.91 | 0.16 | 77 |
| Lumen volume | 0.72 | 0.29 | 39 |
| ILT-volume | 0.81 | 0.26 | 60 |
| Peak wall stress | 0.66 | 0.33 | 38 |
| Peak wall rupture index | 0.72 | 0.30 | 35 |
SD = standard deviation, Dmax = maximal aneurysm diameter, ILT = intraluminal thrombus. †The number of patients where the r-squared value for the model exceeds 0.90.
For twelve selected patients, Dmax measurements collected from the electronic medical records, measured with various modalities, are presented in Supplementary Fig. 3, together with the semi-automatic maximal diameter measurements. There is substantial variation, depending on which modality is used for measuring. In some cases, such as for the fifth patient, the clinical CT diameter appears stagnant, until it suddenly increases, in contrast to the semi – automatic diameter which increases continuously.
Comparison of maximal aneurysm diameter, aneurysm volume and peak wall stress growth rates
Patients were divided into groups based on tertiles of Dmax-growth (less than 2.11 mm/year, 2.11 mm/year–3.04 mm/year and more than 3.04 mm/year), Volume, PWS and PWRI (Table 3). Dmax-growth tertiles were not directly related to the corresponding aneurysm volume, PWS or PWRI growth distributions. For patients in the lowest Dmax-growth tertile, only 67% belong to the lowest tertile of aneurysm volume growth, and 52% belong to the lowest PWS-increase tertile and 55% to the lowest tertile of PWRI-increase (Table 3).
Table 3.
Patients categorized according to growth in tertiles (slow, intermediate, and fast) by Maximal Aneurysm Diameter (Dmax), volume and peak wall stress (PWS), peak wall rupture index (PWRI).
| Dmax-growth (mm/year) | |||
|---|---|---|---|
| Slow (< 2.11), N = 331 |
Intermediate (2.11–3.03), N = 341 |
Fast (> 3.03), N = 331 |
|
| Volume-growth (cm3/year) | |||
| Slow (< 9.6) | 22 (67%) | 11 (32%) | 0 (0%) |
| Intermediate (9.6–16.74) | 10 (30%) | 14 (41%) | 10 (30%) |
| Fast (> 16.74) | 1 (3.0%) | 9 (26%) | 23 (70%) |
| PWS-growth (kPa/year) | |||
| Slow (< 5.38) | 17 (52%) | 10 (29%) | 6 (18%) |
| Intermediate (5.38–8.48) | 10 (30%) | 15 (44%) | 9 (27%) |
| Fast (> 8.48) | 6 (18%) | 9 (26%) | 18 (55%) |
| PWRI-growth (ratio/year) | |||
| Slow (< 0.01) | 18 (55%) | 11 (32%) | 4 (12%) |
| Intermediate (0.01–0.03) | 11 (33%) | 14 (41%) | 9 (27%) |
| Fast (> 0.03) | 4 (12%) | 9 (26%) | 20 (61%) |
1n (%).
Lumen and ILT volume changes
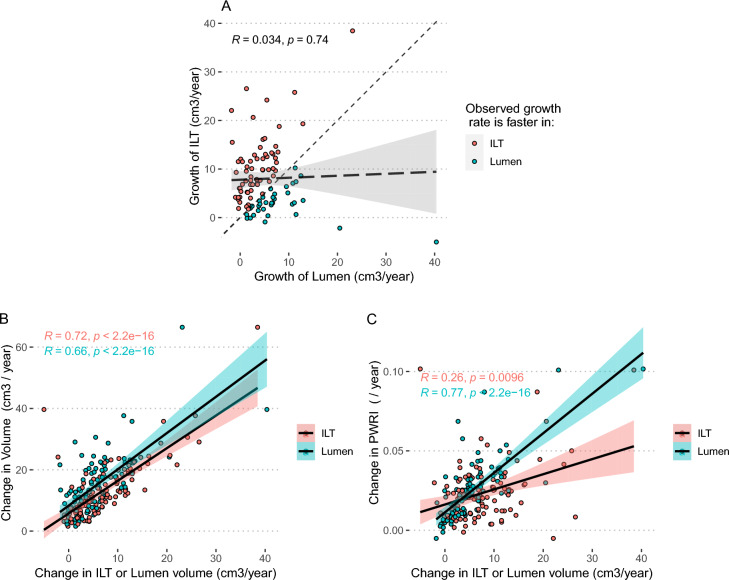
In the majority of patients ILT-volume increased faster than lumen volume, and consequently the ILT-ratio (ILT-volume / aneurysm volume) in aneurysms increased over time (2.63%, 2.13–3.14% / year, p < 0.01) (Supplementary table 1). There was, however, no correlation between the growth of ILT and the growth of the lumen (r = 0.034, p = 0.74) (Fig. 3A). Both ILT and lumen volume change correlated with change in volume (r = 0.72, p < 0.001, and r = 0.66, p < 0.001), there was no evidence of difference in the correlations (p = 0.39) (Fig. 3B). Change in lumen volume correlated significantly stronger with change in PWRI (r = 0.77, p < 0.001) compared to change in ILT volume (r = 0.26, p = 0.001, p for difference in correlations coefficients < 0.001) (Fig. 3C).
Figure 3.
Scatter and correlation plots. (A) Change of intraluminal thrombus (ILT) volume plotted against change of lumen volume, (B) Change of Aneurysm Volume plotted against change of ILT volume (red dots), or lumen volume (blue dots). (C) Change in PWRI plotted against change of ILT volume (red dots), or lumen volume (blue dots). Correlation coefficients and respective p-values are shown in the figure.
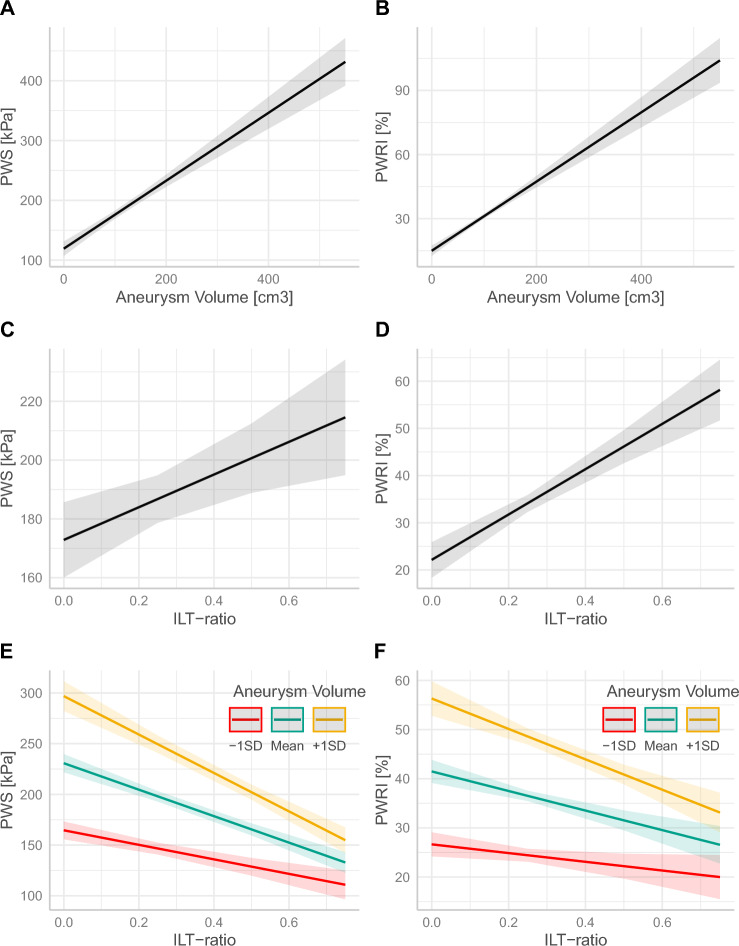
Aneurysm volume and ILT ratio were both associated with increasing PWS and PWRI, when modelling them separately (Fig. 4A–D). However, when introducing an interaction term between aneurysm volume and ILT-ratio, PWS and PWRI still increase for any given aneurysm volume, but they instead decreased with increasing ILT-ratio (Fig. 4E–F and Supplementary table 2).
Figure 4.
Relation between biomechanical indices (PWS and PWRI) and aneurysm volume (A, B), ILT ratio (C, D) and ILT-ratio adjusted for aneurysm volume and their interaction (E, F) Coloured lines indicate the relation of biomechanical stress to ILT-ratio at different levels (-1sd, mean and +1sd) of aneurysm volume.
Discussion
The present study shows that Dmax and volume growth, generally, do not appear to be erratic or discontinuous. Dmax-growth is, in many cases, adequately described as linear. A slow Dmax growth, however, does not harmonize with a sometimes more rapid volume growth and biomechanical increase. The proportion of ILT increased with time but was related to lower biomechanical stress.
Maximal aneurysm diameter and volume growth
Previous studies have described that AAA growth is erratic and discontinuous4–7. Contrary to this notion, where aneurysm growth largely is considered as unpredictable, our results instead indicate that aneurysms mostly grow continuously, and for many patients, growth patterns can adequately be described by a linear model. This is in line with recently published results by Olson et al., who reported from the Non-Invasive Treatment of Abdominal Aortic Aneurysm Clinical Trial (N-TA3CT) that most patients included therein displayed continuous and linear Dmax-growth patterns30. The follow up of patients was between 18 and 30 months in the N-TA3CT trial, in this study we show similar growth patterns but importantly also during longer follow up time (mean 5.2 years). In the current study, volume growth could also, in most patients, be adequately described by a linear model. There may be several explanations for these previous observations of erratic aneurysm growth. Studies that are based on manual measurements from a clinical setting may suffer from certain biases and methodological errors. Semi-automatic diameter measurements for instance are not affected by rounding or so-called ‘terminal digit preference’, which is reported in standard diameter measurements31. Further, in the clinical setting, especially regarding ultrasound, the observer may be unaware of the exact location and method of the previous measurement. In this study, the AAAs were segmented semi-automatically and measurements were extracted from the resulting 3D model. This may overcome many of the potential sources of bias in manual measurement and be more representative of the true biological growth.
While the growth of most patients could be described as linear, for Dmax and volume growth 13% and 23% of patients respectively did not confer to the linear model. The current surveillance strategy with increasing frequency of measurements as the aneurysm grows32, is motivated by the notion of non-linear, exponential, growth. Further work is needed to predict the growth pattern of individual aneurysms, as those growing exponentially should be monitored with increasing frequency and the surveillance intervals of those growing linearly could be extended. The continuous nature of AAA growth described in this study, however, reveals potential for optimized growth prediction from taking more than one observation into account.
Patients with slow Dmax-growth rates in some cases exhibit higher aneurysm volume and PWS/PWRI change rates. Conversely, some patients with a high Dmax-growth rate exhibit lower aneurysm volume and biomechanical change rates. These findings support previous notions that there is a clear difference between surveillance of Dmax and aneurysm volume33. Also, aneurysm biomechanics may evolve independent from aneurysm diameter change. This points to potentially added value of 3D surveillance of AAAs, perhaps particularly in the research setting to for instance interpret the effect of pharmacological therapy. Further studies are, however, required to determine the clinical role of AAA volume or biomechanical parameters in surveillance.
The role of the ILT
There are conflicting reports in the literature regarding the role of the ILT in AAA growth and rupture. The wall of the aneurysm directly affected by the ILT is more degraded, thinner, and weaker34,35. The ILT, however, seems to cushion stress from the wall36. The proportion of the ILT in an AAA has been associated with AAA growth37,38, especially a thick ILT seems to preclude growth39, and the growth of the ILT has been implicated in rupture40. Conversely, ruptured AAAs appear to have less thrombus41,42.
It is suggested that an interplay of the different effects of the ILT lead to an U-shaped association between ILT thickness and aneurysm growth, where a thin ILT does not provide a cushioning effect, while a thick ILT has a greater cushioning effect but a larger effect on wall degradation and therefore also leads to AAA growth39. The present study observes that the proportion of ILT (ILT-ratio) increases as aneurysms grow, but when adjusting for aneurysm volume, ILT-ratio is associated with decreased biomechanical stress. Thus, given an aneurysm of certain size, biomechanical rupture risk appears to be inversely related to the proportion of thrombus. Together with the literature, these results point to a two-fold role of the ILT, where the ILT potentiates growth of AAAs, and the continuous deterioration of the aneurysm wall, whereas it provides biomechanical support. The positive association between the amount of ILT and the size of the AAAs, may in some cases cause confounding. Further, in the case of rupture of the ILT, biomechanical stress may be transmitted through the thrombus to the underlying wall which likely negates the protective effects of ILT. Overall, the net effect of the ILT on growth and rupture likely depends on a number of factors.
Limitations
The nature of this data is retrospective, and there is selection bias in the AAAs that are included. In addition, to be able to study CTA-based growth rates we included only patients that had undergone a minimum of three examinations. However, the overall growth rate of AAAs was 2.6 mm/y, and this is comparable with previously reported growth rates43,44. For some patients, it is obvious that they were deemed as unfit for elective repair, as there are several aneurysms that grow beyond the current operative threshold recommendations and this patient group may represent a comparatively more comorbid patient-group compared to AAA patients in general.
Conclusions
Dmax and volume growth, generally, do not appear to be erratic or discontinuous. Dmax-growth can in most cases adequately be described as linear. Patients with slow Dmax growth do, however, sometimes display relatively more rapid volume growth and PWS increase. The proportion of ILT increased with time but was related to lower biomechanical stress.
Supplementary Information
Author contributions
Concept and design: A.S., J.R. Analysis and interpretation: A.S., M.B., M.L.L., T.C.G., R.H., J.R. Data collection: A.S., M.B., M.L.L. Writing the article: A.S. Critical revision of the article: A.S., M.B., M.L.L., T.C.G., R.H., J.R. Final approval of the article: A.S., M.B., M.L.L., T.C.G., R.H., J.R. Statistical analysis: A.S. Funding: J.R., R.H., T.C.G. Overall responsibility: J.R.
Funding
Open access funding provided by Karolinska Institute. This research was supported by the Swedish Heart–Lung Foundation (20180596, 20180506, 20190553, 20210550, 20220451), the Stockholm County Council HMT and ALF (20180072) projects, and the Swedish Research Council (12660).
Data availability
The data comes from patients, where informed consent has been waived by the Stockholm Ethical Review Board. Individual patient data will not be made publicly available since it was not part of the Ethical approval for this study. Data is available from Antti Siika (antti.siika@ki.se) or Joy Roy (joy.roy@ki.se), upon reasonable request with appropriate ethical permission.
Competing interests
T.C.G. is a scientific advisor and shareholder of VASCOPS GmbH, Graz, Austria. The other authors report no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
The online version contains supplementary material available at 10.1038/s41598-023-36204-2.
References
- 1.Wanhainen A, Verzini F, Van Herzeele I, Allaire E, Bown M, Cohnert T, et al. European society for vascular surgery (ESVS) 2019 clinical practice guidelines on the management of abdominal Aorto-iliac artery aneurysms. Eur. J. Vasc. Endovasc. Surg. 2018;57(8):93. doi: 10.1016/j.ejvs.2018.09.020. [DOI] [PubMed] [Google Scholar]
- 2.Bengtsson H, Bergqvist D. Ruptured abdominal aortic aneurysm: A population-based study. J. Vasc. Surg. 1993;18(1):74–80. doi: 10.1067/mva.1993.42107. [DOI] [PubMed] [Google Scholar]
- 3.Sakalihasan N, Michel JB, Katsargyris A, Kuivaniemi H, Defraigne JO, Nchimi A, et al. Abdominal aortic aneurysms. Nat. Rev. Dis. Primers. 2018;4:34. doi: 10.1038/s41572-018-0030-7. [DOI] [PubMed] [Google Scholar]
- 4.Sweeting MJ, Thompson SG. Making predictions from complex longitudinal data, with application to planning monitoring intervals in a national screening programme. J. R. Stat. Soc. Ser. A Stat. Soc. 2012;175(2):569–86. doi: 10.1111/j.1467-985X.2011.01005.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Stonebridge PA, Draper T, Kelman J, Howlett J, Allan PL, Prescott R, et al. Growth rate of infrarenal aortic aneurysms. Eur. J. Vasc. Endovasc. Surg. 1996;11(1):70–3. doi: 10.1016/S1078-5884(96)80137-7. [DOI] [PubMed] [Google Scholar]
- 6.Hirose Y, Hamada S, Takamiya M. Predicting the growth of aortic aneurysms: A comparison of linear vs exponential models. Angiology. 1995;46(5):413–419. doi: 10.1177/000331979504600508. [DOI] [PubMed] [Google Scholar]
- 7.Kurvers H, Veith FJ, Lipsitz EC, Ohki T, Gargiulo NJ, Cayne NS, et al. Discontinuous, staccato growth of abdominal aortic aneurysms. J. Am. Coll. Surg. 2004;199(5):709–15. doi: 10.1016/j.jamcollsurg.2004.07.031. [DOI] [PubMed] [Google Scholar]
- 8.Long A, Rouet L, Lindholt JS, Allaire E. Measuring the maximum diameter of native abdominal aortic aneurysms: Review and critical analysis. Eur. J. Vasc. Endovasc. Surg. 2012;43(5):515–24. doi: 10.1016/j.ejvs.2012.01.018. [DOI] [PubMed] [Google Scholar]
- 9.Beales L, Wolstenhulme S, Evans JA, West R, Scott DJA. Reproducibility of ultrasound measurement of the abdominal aorta. Br. J. Surg. 2011;98(11):1517–1525. doi: 10.1002/bjs.7628. [DOI] [PubMed] [Google Scholar]
- 10.Foo FJ, Hammond CJ, Goldstone AR, Abuhamdiah M, Rashid ST, West RM, et al. Agreement between computed tomography and ultrasound on abdominal aortic aneurysms and implications on clinical decisions. Eur. J. Vasc. Endovasc. Surg. 2011;42(5):608–614. doi: 10.1016/j.ejvs.2011.07.003. [DOI] [PubMed] [Google Scholar]
- 11.Martufi G, Auer M, Roy J, Swedenborg J, Sakalihasan N, Panuccio G, et al. Multidimensional growth measurements of abdominal aortic aneurysms. J. Vasc. Surg. 2013;58(3):748–55. doi: 10.1016/j.jvs.2012.11.070. [DOI] [PubMed] [Google Scholar]
- 12.Parr A, Jayaratne C, Buttner P, Golledge J. Comparison of volume and diameter measurement in assessing small abdominal aortic aneurysm expansion examined using computed tomographic angiography. Eur. J. Radiol. 2011;79(1):42–47. doi: 10.1016/j.ejrad.2009.12.018. [DOI] [PubMed] [Google Scholar]
- 13.Lindquist Liljeqvist M, Hultgren R, Gasser TC, Roy J. Volume growth of abdominal aortic aneurysms correlates with baseline volume and increasing finite element analysis-derived rupture risk. J. Vasc. Surg. 2016;63(6):1434–1442.e3. doi: 10.1016/j.jvs.2015.11.051. [DOI] [PubMed] [Google Scholar]
- 14.Lindquist Liljeqvist M, Bogdanovic M, Siika A, Gasser TC, Hultgren R, Roy J. Geometric and biomechanical modeling aided by machine learning improves the prediction of growth and rupture of small abdominal aortic aneurysms. Sci. Rep. 2021;11(1):1–10. doi: 10.1038/s41598-021-96512-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Khosla S, Morris DR, Moxon JV, Walker PJ, Gasser TC, Golledge J. Meta-analysis of peak wall stress in ruptured, symptomatic and intact abdominal aortic aneurysms. Br. J. Surg. 2014;101(11):1350–7. doi: 10.1002/bjs.9578. [DOI] [PubMed] [Google Scholar]
- 16.Indrakusuma R, Jalalzadeh H, Planken RN, Marquering HA, Legemate DA, Koelemay MJW, et al. Biomechanical imaging markers as predictors of abdominal aortic aneurysm growth or rupture: A systematic review. Eur. J. Vasc. Endovasc. Surg. 2016 doi: 10.1016/j.ejvs.2016.07.003. [DOI] [PubMed] [Google Scholar]
- 17.Erhart P, Roy J, de Vries JPPM, Liljeqvist ML, Grond-Ginsbach C, Hyhlik-Dürr A, et al. Prediction of rupture sites in abdominal aortic aneurysms after finite element analysis. J. Endovasc. Ther. 2016;23(1):115–20. doi: 10.1177/1526602815612196. [DOI] [PubMed] [Google Scholar]
- 18.Stevens RRF, Grytsan A, Biasetti J, Roy J, Lindquist Liljeqvist M, Gasser TC. Biomechanical changes during abdominal aortic aneurysm growth. PLoS ONE. 2017;12(11):e0187421. doi: 10.1371/journal.pone.0187421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Washington CB, Shum J, Muluk SC, Finol EA. The association of wall mechanics and morphology: A case study of abdominal aortic aneurysm growth. J. Biomech. Eng. 2011;133(10):104501. doi: 10.1115/1.4005176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Auer M, Gasser TC. Reconstruction and finite element mesh generation of abdominal aortic aneurysms from computerized tomography angiography data with minimal user interactions. IEEE Trans. Med. Imaging. 2010;29(4):1022–8. doi: 10.1109/TMI.2009.2039579. [DOI] [PubMed] [Google Scholar]
- 21.Gasser TC, Auer M, Labruto F, Swedenborg J, Roy J. Biomechanical rupture risk assessment of abdominal aortic aneurysms: Model complexity versus predictability of finite element simulations. Eur. J. Vasc. Endovasc. Surg. 2010;40(2):176–85. doi: 10.1016/j.ejvs.2010.04.003. [DOI] [PubMed] [Google Scholar]
- 22.Gasser TC, Görgülü G, Folkesson M, Swedenborg J. Failure properties of intraluminal thrombus in abdominal aortic aneurysm under static and pulsating mechanical loads. J. Vasc. Surg. 2008;48(1):179–88. doi: 10.1016/j.jvs.2008.01.036. [DOI] [PubMed] [Google Scholar]
- 23.Raghavan ML, Vorp DA. Toward a biomechanical tool to evaluate rupture potential of abdominal aortic aneurysm: Identification of a finite strain constitutive model and evaluation of its applicability. J. Biomech. 2000;33(4):475–482. doi: 10.1016/S0021-9290(99)00201-8. [DOI] [PubMed] [Google Scholar]
- 24.Vande Geest JP, Wang DHJ, Wisniewski SR, Makaroun MS, Vorp DA. Towards a noninvasive method for determination of patient-specific wall strength distribution in abdominal aortic aneurysms. Ann. Biomed. Eng. 2006;34(7):1098–106. doi: 10.1007/s10439-006-9132-6. [DOI] [PubMed] [Google Scholar]
- 25.van de Geest JP, di Martino ES, Bohra A, Makaroun MS, Vorp DA. A biomechanics-based rupture potential index for abdominal aortic aneurysm risk assessment: Demonstrative application. Ann. N. Y. Acad. Sci. 2006;1085(1):11–21. doi: 10.1196/annals.1383.046. [DOI] [PubMed] [Google Scholar]
- 26.Fedorov A, Beichel R, Kalpathy-Cramer J, Finet J, Fillion-Robin JC, Pujol S, et al. 3D Slicer as an image computing platform for the Quantitative imaging network. Magn. Reson. Imaging. 2012;30(9):1323–1341. doi: 10.1016/j.mri.2012.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.R Core Team. R: A language and enviornment for statistical computing [Internet]. Vienna, Austria: R Foundation for Statistical Computing; 2021. Available from: https://www.r-project.org/.
- 28.Kuznetsova A, Brockhoff PB, Christensen RHB. lmerTest Package: Tests in Linear Mixed Effects Models. J Stat Softw. 2017;82(13):36. doi: 10.18637/jss.v082.i13. [DOI] [Google Scholar]
- 29.Leeper, T. J. Margins: Marginal effects for model objects. 2021.
- 30.Olson SL, Wijesinha MA, Panthofer AM, Blackwelder WC, Upchurch GR, Terrin ML, et al. Evaluating growth patterns of abdominal aortic aneurysm diameter with serial computed tomography surveillance. JAMA Surg. 2021;156(4):363–70. doi: 10.1001/jamasurg.2020.7190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lederle FA, Wilson SE, Johnson GR, Reinke DB, Littooy FN, Acher CW, et al. Variability in measurement of abdominal aortic aneurysms. Abdominal aortic aneurysm detection and management Veterans administration cooperative study group. J. Vasc. Surg. 1995;21(6):945–52. doi: 10.1016/S0741-5214(95)70222-9. [DOI] [PubMed] [Google Scholar]
- 32.Chaikof EL, Dalman RL, Eskandari MK, Jackson BM, Lee WA, Mansour MA, et al. The society for vascular surgery practice guidelines on the care of patients with an abdominal aortic aneurysm. J. Vasc. Surg. 2018;67(1):2–7. doi: 10.1016/j.jvs.2017.10.044. [DOI] [PubMed] [Google Scholar]
- 33.Ghulam Q, Bredahl K, Eiberg J, Bal L, van Sambeek MR, Kirksey L, et al. Three-dimensional ultrasound is a reliable alternative in endovascular aortic repair surveillance. J. Vasc. Surg. 2021;74:979–987. doi: 10.1016/j.jvs.2021.02.031. [DOI] [PubMed] [Google Scholar]
- 34.Kazi M, Thyberg J, Religa P, Roy J, Eriksson P, Hedin U, et al. Influence of intraluminal thrombus on structural and cellular composition of abdominal aortic aneurysm wall. J. Vasc. Surg. 2003;38(6):1283–1292. doi: 10.1016/S0741-5214(03)00791-2. [DOI] [PubMed] [Google Scholar]
- 35.van de Geest JP, Wang DHJ, Wisniewski SR, Makaroun MS, Vorp DA. Towards a noninvasive method for determination of patient-specific wall strength distribution in abdominal aortic aneurysms. Ann. Biomed. Eng. 2006;34(7):1098–106. doi: 10.1007/s10439-006-9132-6. [DOI] [PubMed] [Google Scholar]
- 36.Speelman L, Schurink GWH, Bosboom EMH, Buth J, Breeuwer M, van de Vosse FN, et al. The mechanical role of thrombus on the growth rate of an abdominal aortic aneurysm. J. Vasc. Surg. 2010;51(1):19–26. doi: 10.1016/j.jvs.2009.08.075. [DOI] [PubMed] [Google Scholar]
- 37.Behr-Rasmussen C, Grøndal N, Bramsen MB, Thomsen MD, Lindholt JS. Mural thrombus and the progression of abdominal aortic aneurysms: A large population-based prospective cohort study. Eur. J. Vasc. Endovasc. Surg. 2014;48(3):301–7. doi: 10.1016/j.ejvs.2014.05.014. [DOI] [PubMed] [Google Scholar]
- 38.Aghayev A, Giannopoulos AA, Gronsbell J, George E, Cai T, Steigner ML, et al. Common first-pass CT angiography findings associated with rapid growth rate in abdominal aorta aneurysms between 3 and 5 cm in largest diameter. Am. J. Roentgenol. 2018;210(2):431–437. doi: 10.2214/AJR.17.18094. [DOI] [PubMed] [Google Scholar]
- 39.Martufi G, Lindquist Liljeqvist M, Sakalihasan N, Panuccio G, Hultgren R, Roy J, et al. Local diameter, wall stress, and thrombus thickness influence the local growth of abdominal aortic aneurysms. J. Endovasc. Ther. 2016;23:957–966. doi: 10.1177/1526602816657086. [DOI] [PubMed] [Google Scholar]
- 40.Stenbaek J, Kalin B, Swedenborg J. Growth of thrombus may be a better predictor of rupture than diameter in patients with abdominal aortic aneurysms. Eur. J. Vasc. Endovasc. Surg. 2000;20(5):466–469. doi: 10.1053/ejvs.2000.1217. [DOI] [PubMed] [Google Scholar]
- 41.Kontopodis N, Koncar I, Tzirakis K, Tavlas E, Davidovic L, Ioannou CV. Intraluminal thrombus deposition is reduced in ruptured compared to diameter-matched intact abdominal aortic aneurysms. Ann. Vasc. Surg. 2019;55:189–195. doi: 10.1016/j.avsg.2018.07.048. [DOI] [PubMed] [Google Scholar]
- 42.Siika A, Lindquist Liljeqvist M, Hultgren R, Gasser TC, Roy J. Aortic lumen area is increased in ruptured abdominal aortic aneurysms and correlates to biomechanical rupture risk. J. Endovasc. Ther. 2018;25(6):750–756. doi: 10.1177/1526602818808292. [DOI] [PubMed] [Google Scholar]
- 43.Wanhainen A, Mani K, Kullberg J, Svensjö S, Bersztel A, Karlsson L, et al. The effect of ticagrelor on growth of small abdominal aortic aneurysms-a randomized controlled trial. Cardiovasc. Res. 2020;116(2):450–456. doi: 10.1093/cvr/cvz133. [DOI] [PubMed] [Google Scholar]
- 44.Sillesen H, Eldrup N, Hultgren R, Lindeman J, Bredahl K, Thompson M, et al. Randomized clinical trial of mast cell inhibition in patients with a medium-sized abdominal aortic aneurysm. Br. J. Surg. 2015;102(8):894–901. doi: 10.1002/bjs.9824. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data comes from patients, where informed consent has been waived by the Stockholm Ethical Review Board. Individual patient data will not be made publicly available since it was not part of the Ethical approval for this study. Data is available from Antti Siika (antti.siika@ki.se) or Joy Roy (joy.roy@ki.se), upon reasonable request with appropriate ethical permission.