Abstract
BACKGROUND
Young adults may have high long-term atherosclerotic cardiovascular disease (ASCVD) risk despite low short-term risk.
OBJECTIVES
In this study, we sought to compare the performance of short-term and long-term ASCVD risk prediction tools in young adults and evaluate ASCVD incidence associated with predicted short-term and long-term risk.
METHODS
We included adults aged 18 to 39 years, from 2008 to 2009 in a U.S. integrated health care system, and followed them through 2019. We calculated 10-year and 30-year ASCVD predicted risk and assessed ASCVD incidence.
RESULTS
Among 414,260 young adults, 813 had an incident ASCVD event during a median of 4 years (maximum 11 years). Compared with 10-year predicted risk, 30-year predicted risk improved reclassification (net reclassification index: 16%) despite having similar discrimination (Harrell’s C: 0.749 vs 0.726). Overall, 1.0% and 2.2% of young adults were categorized as having elevated 10-year (≥7.5%) and elevated 30-year (≥20%) predicted risk, respectively, and 1.6% as having low 10-year (<7.5%) but elevated 30-year predicted risk. The ASCVD incidence rate per 1,000 person-years was 2.60 (95% CI: 1.92–3.52) for those with elevated 10-year predicted risk, 1.87 (95% CI: 1.42–2.46) for those with low 10-year but elevated 30-year predicted risk, and 0.32 (95% CI: 0.30–0.35) for those with low 10-year and 30-year predicted risk. The age- and sex-adjusted incidence rate ratio was 3.04 (95% CI: 2.25–4.10) comparing those with low 10-year but elevated 30-year predicted risk and those with low 10-year and 30-year predicted risk.
CONCLUSIONS
Long-term ASCVD risk prediction tools further discriminate a subgroup of young adults with elevated observed risk despite low estimated short-term risk.
Keywords: ASCVD, cardiovascular risk, young adults
To guide lipid-lowering treatment decisions, the 2018 American Heart Association (AHA)/American College of Cardiology (ACC) cholesterol guideline recommends using pooled cohort equations (PCEs) to estimate 10-year atherosclerotic cardiovascular disease (ASCVD) risk.1 However, the PCEs are not directly applicable to young adults because they were developed in and recommended only for adults 40 to 75 years of age.2 The 2018 AHA/ACC cholesterol guideline recommends the estimation of lifetime or 30-year ASCVD risk for adults younger than 40 years of age.1
A few studies have reported that some adults may have a low 10-year but a high lifetime predicted ASCVD risk.3–5 Because age is the strongest contributor to 10-year predicted risk,6 young adults generally have a low 10-year ASCVD predicted risk even if their risk factor profile indicates high lifetime risk.7 Individuals with a low 10-year but a high lifetime predicted ASCVD risk have a higher incidence of subclinical ASCVD compared with those with both low 10-year and lifetime predicted risk,3 suggesting this subgroup as one that would benefit from preventive measures.
Existing lifetime or 30-year ASCVD risk tools were derived from a single cohort of non-Hispanic Whites aged 20 to 59 years.8,9 It is unclear how well these long-term ASCVD risk prediction tools, along with the PCE 10-year risk equation, discriminate high vs low ASCVD risk among young adults, especially among those who are not non-Hispanic White. In the present study, we compared the performance of 10-year, 30-year, and lifetime ASCVD risk prediction tools recommended by the 2018 AHA/ACC cholesterol guideline in a large diverse sample of young adults. We evaluated characteristics of young adults with elevated short-term or long-term predicted ASCVD risk and the incidence of ASCVD associated with short-term and long-term predicted risk categories.
METHODS
STUDY COHORT.
We included adults aged 18 to 39 years from January 1, 2008, to December 31, 2009, at Kaiser Permanente Southern California, a large U.S. integrated health care system serving a diverse population. Kaiser Permanente Southern California provides medical services to its members through 15 hospitals and more than 200 outpatient facilities that it owns. All interactions with the system are captured in comprehensive electronic health records. Medical care provided to its members outside of the system are captured through medical claims.
For each person, we defined their index date as the first day in this period that they had at least 6 months of continuous eligibility as a Kaiser Permanente Southern California member. We excluded individuals with a history of myocardial infarction, acute coronary syndrome, stable or unstable angina, coronary revascularization, stroke, or peripheral arterial disease before their index date. We required at least 1 low-density lipoprotein cholesterol (LDL-C) measurement up to 6 years before or on their index date. We further excluded individuals who had a statin prescription up to 6 years before their index date, individuals without any measurements of total cholesterol, high-density lipoprotein cholesterol (HDL-C), systolic blood pressure, or diastolic blood pressure measured in an outpatient setting before their index date, and individuals without smoking history information. We followed the identified individuals from their index date until disenrollment from Kaiser Permanente Southern California, ASCVD event, death, statin initiation, or December 31, 2019, whichever occurred first. This study was approved by the Kaiser Permanente Southern California institutional review committees, and the requirement to obtain informed consent was waived.
SHORT-TERM AND LONG-TERM PREDICTED ASCVD RISK.
To estimate short-term ASCVD risk, we used the PCEs for 10-year predicted risk.2 The race- (self-reported Black and non-Black) and sex-specific equations incorporated age, smoking, systolic blood pressure, antihypertensive medication use, total cholesterol, HDL-C, and diabetes (Supplemental Table 1). Because the PCEs are applicable only to individuals aged 40 to 79 years, we applied age as 40 years to every participant when calculating the PCEs10 while the actual age remained when calculating long-term predicted risk.
To estimate long-term predicted ASCVD risk, we used the 30-year ASCVD risk prediction tool as the primary analysis.8 For 30-year risk prediction, there are 4 different equations depending on outcomes and risk factors (Supplemental Table 1). Two equations were used to estimate hard ASCVD risk and the other 2 equations were used to estimate an expanded range of cardiovascular risks including coronary insufficiency and angina pectoris, transient ischemic attack, intermittent claudication, and heart failure. The primary equation for hard ASCVD risk prediction included sex, age, systolic blood pressure, antihypertensive medication use, total cholesterol, HDL-C, diabetes, and smoking.8 The other risk prediction equations included sex, age, systolic blood pressure, antihypertensive medication use, diabetes, smoking, and body mass index (BMI) instead of total cholesterol and HDL-C as predictors.8
We also used a lifetime risk prediction tool to estimate long-term predicted ASCVD risk.9 This tool assigns men and women to 1 of 5 risk categories depending on the number of risk factors present. The 5 risk categories were all optimal risk factors, ≥1 nonoptimal risk factor, ≥1 elevated risk factor, 1 major risk factor, and ≥2 major risk factors based on levels of total cholesterol, systolic blood pressure, diastolic blood pressure, smoking, and diabetes (Supplemental Table 2).
OUTCOMES OF INTERESTS.
The outcomes of interest were incident ASCVD events during study follow-up. Consistent with the outcomes used in the PCEs and 30-year hard ASCVD risk prediction tools, ASCVD events were defined as nonfatal myocardial infarction (MI), death from coronary heart disease, and fatal or nonfatal ischemic stroke. We used principal hospital discharge diagnoses to identify MI (ICD-9 codes 410.x0 and 410.x1, ICD-10 codes I21.x and I22.x)11 and ischemic stroke (ICD-9 codes 433.x1, 434.x1, and 436.xx, ICD-10 codes I63.x, G46.3, and G46.4).12,13 Death from coronary heart disease and stroke was identified by ICD-10 codes (I20-I25 and I60–69) from hospital records and California State death files.14
STATISTICAL ANALYSIS.
To assess the performance of the 10-year and 30-year model in young adults, first we calculated ASCVD incidence rates as the number of ASCVD events per 1,000 person-years per decile of estimated 10-year and 30-year risk. Second, we used Harrell’s C-statistic to assess discrimination ability of 10-year and 30-year risk models. We required nonmissing values for all necessary predictors for both 10-year and 30-year risk and calculated 95% CIs and differences in Harrell’s C-statistic by performing 500 bootstrap resamplings. Third, we evaluated whether using long-term predicted risk helps to correctly categorize young adults into groups of predicted ASCVD risk. Using the 10-year risk categories of <2.5%, 2.5% to <7.5%, and ≥7.5% and the 30-year risk categories of <7.5%, 7.5% to <20%, and ≥20%, the categoric net reclassification improvement (NRI) was calculated. The upper cutoff points were chosen based on earlier publications and clinical recommendations (10-year risk of 7.5% and 30-year risk of 20%) 15,16 and lower cutoff points were chosen based on the distribution of the predicted risk. We also calculated the continuous NRI without considering specific cutoff points. Fourth, we compared the estimated 10-year and 30-year predicted risk between those who had an ASCVD event and those who did not have an ASCVD event.
We used mean ± SD and n (%) to describe demographic and clinical characteristics of young adults by short-term and long-term predicted risk categories according to previously used cutoff points.5,15,16 For 10-year and 30-year risks, individuals were categorized as having: 1) low 10-year (<7.5%) and low 30-year (<20%) risks; 2) low 10-year (<7.5%) and elevated 30-year (≥20%) risks; or 3) elevated 10-year (≥7.5%) risk. Because of the small number, individuals with elevated 10-year but low 30-year risk were included in the elevated 10-year risk group. Analysis of variance or chi-square tests were conducted to compare demographic and clinical characteristics across different risk categories. We calculated Pearson’s correlation coefficients and investigated correlations among estimated 10-year and 30-year predicted risks.
To assess the incremental predictive value for ASCVD risk by using long-term predicted risk in addition to short-term predicted risk, we compared ASCVD incidence rates during follow-up between the short-term and long-term predicted risk categories. We used Poisson regression to calculate crude as well as age- and sex-adjusted incident rate ratios (IRRs) with 95% CIs using the low short-term and low long-term predicted risk categories as the reference group.17 We also calculated changes in sensitivity and specificity by using both long-term and short-term tools together compared with the short-term or long-term prediction tool alone.
As a secondary analysis, we used the lifetime risk equation to estimate long-term predicted risk. For 10-year and lifetime predicted risk, individuals were categorized as having: 1) low 10-year (<7.5%) and low lifetime (<39%) predicted risks; 2) low 10-year (<7.5%) and elevated lifetime (≥39%) predicted risk; or 3) elevated 10-year (≥7.5%) predicted risk. Men and women with ≥1 elevated risk factor, 1 major risk factor, or ≥2 major risk factors were estimated as having ≥39% lifetime predicted risk, which was associated with a greater risk of subclinical atherosclerosis.3 We used all optimal risk factors, ≥1 nonoptimal risk factor, and ≥1 elevated risk factor or higher risk categories to calculate the NRI.
We performed several sensitivity analyses. First, we applied different categories of 10-year and 30-year risk: 1) 4 groups of low/low, low/elevated, elevated/low, and elevated/elevated 10-year and 30-year predicted risks; 2) 2 groups of low or elevated 10-year predicted risk; and 3) 2 groups of low or elevated 30-year predicted risk. Second, we applied alternative versions of the 30-year risk prediction algorithms (Supplemental Table 1).8 Finally, instead of considering statin initiation as a censoring event, we continued follow-up until disenrollment from Kaiser Permanente Southern California, outcomes of interests, or death.
RESULTS
We included a total of 414,260 young adults (mean age 29.8 years, 60.6% women). Median (IQR) 10-year predicted ASCVD risk was 0.6% (0.3%–1.3%) and median 30-year predicted risk was 3.1% (1.5%–6.2%) (Supplemental Table 3). The correlation of 10-year and 30-year estimated risks was 0.73 (Supplemental Table 4).
Over a median of 4.0 years (IQR: 1.2–11.0 years) of follow-up, 813 young adults had incident ASCVD events. The highest deciles of estimated 10-year and 30-year risk had the highest observed ASCVD incidence (Figure 1). The Harrell’s C-statistics for 10-year and 30-year risk equations were 0.726 (95% CI: 0.689–0.765) and 0.749 (0.714–0.784), respectively, with a difference of 0.023 (−0.005 to 0.047) (Table 1). The overall NRI using the 30-year risk equation compared with the 10-year risk equation was 16.0% (Table 2). The net percentage of young adults with ASCVD correctly categorized upward was 26.7%, and the net percentage of young adults without ASCVD correctly assigned a lower risk category decreased by 10.7%. The net continuous NRI using the 30-year risk equation compared with the 10-year risk equation was 22.4% (95% CI: 17.1%–27.6%) (event NRI of 64.8% and nonevent NRI of −42.4%). Among young adults who had an ASCVD during follow-up, 5.2% had elevated 10-year risk and 10.6% had elevated 30-year predicted risk (Supplemental Table 5).
FIGURE 1. ASCVD Event Rates Per Estimated 10-Year and 30-Year Cardiovascular Risks.
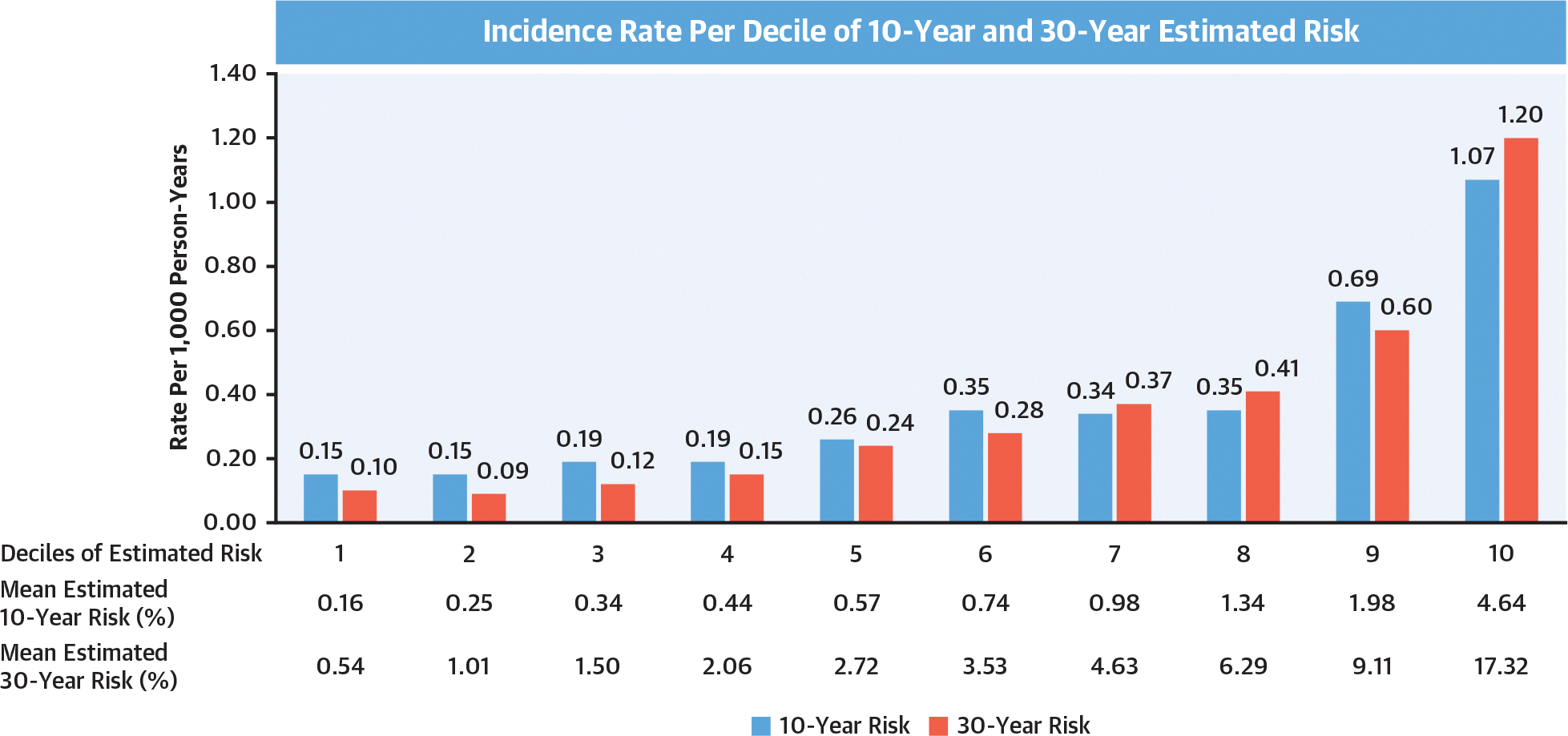
This figure shows the incidence rate of ASCVD (per 1,000 person-years) per each decile of estimated 10-year and 30-year risk. We applied both 10-year and 30-year risk prediction tools to young adults aged 18–39 years in the Kaiser Permanente Southern California health care system. The observed ASCVD incidence increased at the higher deciles of estimated 10-year and 30-year risk. ASCVD = atherosclerotic cardiovascular disease.
TABLE 1.
Harrell’s C-Statistics of 10-Year and 30-Year Cardiovascular Risk Prediction Tools
| Prediction | Harrell’s C-Statistic (95% CI) | Difference (95% CI) |
|---|---|---|
|
| ||
| 10-year risk | 0.726 (0.689 to 0.765) | Reference |
| 30-year risk | ||
| Hard ASCVD outcome model (without BMI)a | 0.749 (0.714 to 0.784) | 0.023 (−0.005 to 0.047) |
| Hard ASCVD outcome model (with BMI) | 0.738 (0.704 to 0.775) | 0.011 (−0.018 to 0.040) |
| Expanded CVD outcome model (without BMI) | 0.755 (0.720 to 0.789) | 0.028 (0.001 to 0.053)b |
| Expanded CVD Outcome Mode (with BMI) | 0.740 (0.705 to 0.776) | 0.014 (−0.016 to 0.043) |
See Supplemental Table 1 for risk factors and outcomes used for each risk prediction.
Primary analysis.
Statistically significant.
ASCVD = atherosclerotic cardiovascular disease; BMI = body mass index; CVD = cardiovascular.
TABLE 2.
Reclassification of Young Adults by the 30-Year vs the 10-Year Risk Prediction Tools
| 30-Year Predicted Risk |
|||||||||
|---|---|---|---|---|---|---|---|---|---|
| 0 to <7.5% |
7.5 to <20% |
≥20% |
|||||||
| 10-y Predicted Risk | N | ASCVD | n | ASCVD | n | ASCVD | n | ASCVD | Net Reclassification Index |
|
| |||||||||
| 0.0% to <2.5% | 371,903 | 600 (0.16) | 320,544 | 398 (0.12) | 50,780 | 198 (0.39) | 579 | 4 (0.69) | 16.0% |
| 2.5% to <7.5% | 38,201 | 171 (0.45) | 11,575 | 25 (0.22) | 20,780 | 99 (0.48) | 5,846 | 47 (0.80) | 26.7% (ASCVD) |
| ≥7.5% | 4,156 | 42 (1.01) | 133 | 0 (0.00) | 1,237 | 7 (0.57) | 2,786 | 35 (1.26) | −10.7% (no ASCVD) |
| Total | 414,260 | 813 (0.20) | 332,252 | 423 (0.13) | 72,797 | 304 (0.42) | 9,211 | 86 (0.93) | |
Values are n (%) unless otherwise indicated.
ASCVD = atherosclerotic cardiovascular disease.
Applying the 10-year and 30-year ASCVD risk prediction tools separately, 1.0% of the young adults were categorized as having elevated (≥7.5%) 10-year predicted risk and 2.2% were categorized as having elevated (≥20%) 30-year predicted risk (Table 3). Overall, 1.6% individuals were categorized as having low 10-year but elevated 30-year predicted risk of ASCVD and 0.3% were categorized as having elevated 10-year but low 30-year predicted risk. Young adults with elevated 10-year ASCVD risk were more likely to self-report being Black (16.9%), and a higher percentage were current smokers (84.8%) and had higher mean systolic blood pressure, BMI, and LDL-C compared with other groups. Young adults with low 10-year but elevated 30-year risk were more likely to be taking antihypertensive medication (32.7%) and have diabetes (22.1%) compared with other groups. Compared with young adults with low 10-year and 30-year predicted risks, the percentage of current smoking (38.2%) as well as mean systolic blood pressure, BMI, and LDL-C were higher among young adults with low 10-year but elevated 30-year predicted risk.
TABLE 3.
Characteristics of Young Adults Stratified by Estimated 10-Year and 30-Year Cardiovascular Risk
| Low 10-Year/Low 30-Year Risk (n = 403,679) | Low 10-Year/Elevated 30-Year Risk (n = 6,425) | Elevated 10-Year Riska (n = 4,156) | |
|---|---|---|---|
|
| |||
| Age, y | 29.6 ± 6.5 | 37.0 ± 2.2 | 32.7 ± 5.2 |
| Sex | |||
| Women | 249,955 (61.9) | 418 (6.5) | 742 (17.9) |
| Men | 153,724 (38.1) | 6,007 (93.5) | 3,414 (82.1) |
| Race/ethnicity | |||
| White | 99,639 (24.7) | 1,739 (27.1) | 1,183 (28.5) |
| Black | 32,265 (8.0) | 435 (6.8) | 704 (16.9) |
| Hispanic | 186,621 (46.2) | 2,950 (45.9) | 1,476 (35.5) |
| Asian/Pacific Islander | 40,667 (10.1) | 547 (8.5) | 288 (6.9) |
| Other | 44,487 (11.0) | 754 (11.7) | 505 (12.2) |
| Systolic blood pressure, mm Hg | 118.6 ± 14.1 | 137.1 ± 16.1 | 139.0 ± 18.1 |
| Diastolic blood pressure, mm Hg | 71.7 ± 10.2 | 83.6 ± 11.3 | 83.6 ± 12.3 |
| Body mass index, kg/m2 | 28.5 ± 6.9 | 33.1 ± 6.8 | 34.2 ± 7.4 |
| Total cholesterol, mg/dL | 181.8 ± 34.8 | 223.5 ± 42.2 | 234.5 ± 57.6 |
| HDL cholesterol, mg/dL | 50.6 ± 13.0 | 39.4 ± 9.1 | 35.5 ± 8.5 |
| LDL cholesterol, mg/dL | 109.3 ± 30.0 | 137.4 ± 37.7 | 140.2 ± 43.0 |
| <100 | 160,477 (39.8) | 980 (15.3) | 668 (16.1) |
| 100–129 | 148,818 (36.9) | 1,746 (27.2) | 982 (23.6) |
| 130–159 | 71,390 (17.7) | 2,054 (32.0) | 1,242 (29.9) |
| 160–190 | 19,085 (4.7) | 1,147 (17.9) | 867 (20.9) |
| ≥190 | 3,909 (1.0) | 498 (7.8) | 397 (9.6) |
| Current smoking | 32,982 (8.2) | 2,452 (38.2) | 3,524 (84.8) |
| Treated hypertension | 11,354 (2.8) | 2,103 (32.7) | 1,126 (27.1) |
| Diabetes | 4,989 (1.2) | 1,422 (22.1) | 655 (15.8) |
| 10-year risk, % | 1.0 ± 1.0 | 4.5 ± 1.6 | 11.1 ± 5.9 |
| ≥7.5 | 0 (0.0) | 0 (0.0) | 4,156 (100.0) |
| <7.5 | 403,679 (100.0) | 6,425 (100.0) | 0 (0.0) |
| 30-year risk, % | 4.3 ± 3.9 | 25.1 ± 5.2 | 26.9 ± 13.3 |
| ≥20 | 0 (0.0) | 6,425 (100.0) | 2,786 (67.0) |
| <20 | 403,679 (100.0) | 0 (0.0) | 1,370 (33.0) |
| Lifetime risk, % | 29.7 ± 14.9 | 52.5 ± 8.1 | 57.7 ± 10.7 |
| ≥39 | 162,636 (40.3) | 6,373 (99.2) | 4,139 (99.6) |
| <39 | 241,043 (59.7) | 52 (0.8) | 17 (0.4) |
Values are mean ± SD or n (%). Definitions for elevated and low cardiovascular risk: 10-year risk: elevated ≥7.5%, low <7.5%; 30-year risk: elevated ≥20%, low <20%. All P values <0.001 from analysis of variance (ANOVA) tests for continuous variables and chi-square tests for categoric variables across low 10-year/low 30-year risk vs low 10-year/ elevated 30-year risk vs elevated 10-year risk categories.
A total of 1,370 young adults had elevated 10-year but low 30-year risk, and they were included in the elevated 10-year risk group.
ASCVD = atherosclerotic cardiovascular disease; HDL = high-density lipoprotein; LDL = low-density lipoprotein.
The incidence rates of ASCVD per 1,000 person-years were 2.60 (95% CI: 1.92–3.52) for those with elevated 10-year ASCVD predicted risk, 1.87 (95% CI: 1.42–2.46) for those with low 10-year but elevated 30-year predicted risk, and 0.32 (95% CI: 0.30–0.35) for those with low 10-year and 30-year predicted risk (Table 4). Compared with those with low 10-year and 30-year predicted risks, age- and sex-adjusted IRRs were 5.98 (95% CI: 4.36–8.22) for those with elevated 10-year predicted risk and 3.04 (95% CI: 2.25–4.10) for those with low 10-year but elevated 30-year predicted risk (Central Illustration). Using both 10-year and 30-year risk prediction tools increased sensitivity from 5.2% to 11.4% while specificity decreased from 99.0% to 97.5% compared with the 10-year risk prediction tool only (Supplemental Table 6).
TABLE 4.
Atherosclerotic Cardiovascular Disease Rates and Incidence Rate Ratios Stratified by Estimated 10-Year and 30-Year Risk
| Young Adults, n (%) | Total Person-Years | ASCVD Events | Rate per 1,000 Person-Years (95% CI) | Crude IRR (95% CI) | Age-adjusted IRR (95% CI) | Age- and Sex-Adjusted IRR (95% CI) | |
|---|---|---|---|---|---|---|---|
|
| |||||||
| Elevated 10-year risk | 4,156 (1.0) | 16,144 | 42 | 2.60 (1.92–3.52) | 8.05 (5.89–10.98) | 7.02 (5.14–9.59) | 5.98 (4.36–8.22) |
| Low 10-year/elevated 30-year risk | 6,425 (1.6) | 27,235 | 51 | 1.87 (1.42–2.46) | 5.79 (4.36–7.69) | 3.74 (2.80–4.99) | 3.04 (2.25–4.10) |
| Low 10-year/low 30-year risk | 403,679 (97.4) | 2,226,787 | 720 | 0.32 (0.30–0.35) | Reference | Reference | Reference |
Definitions for elevated and low risk: 10-year risk: elevated ≥7.5%, low <7.5%; 30-year risk: elevated ≥20%, low <20%.
ASCVD = atherosclerotic cardiovascular disease.
CENTRAL ILLUSTRATION. ASCVD Associated With Low 10-Year But Elevated 30-Year Predicted Risk.

The percentage of young adults categorized as having elevated 10-year (≥7.5%) risk, low 10-year (<7.5%) but elevated 30-year (≥20%) predicted risk, and low 10-year (<7.5%) and low 30-year (<20%) predicted risks, and age- and sex-adjusted incidence rate ratios (IRRs) for ASCVD compared with young adults with low 10-year (<7.5%) and low 30-year (<20%) predicted risk. Also shown is the better performance of the 30-year risk prediction tool compared with the 10-year risk prediction tool.
Sensitivity analyses using different risk categories showed that the age- and sex-adjusted IRR for young adults with elevated 10-year but low 30-year predicted risk was 4.30 (95% CI: 2.04–9.08) compared with those with low 10-year and 30-year predicted risks (Supplemental Tables 7 and 8). Sensitivity analysis using modified versions of 30-year risk prediction algorithms identified a group of young adults with low 10-year and elevated 30-year predicted risks who had ASCVD incidence ranges from 0.93 to 1.28 per 1,000 person-years, which are higher than those with low 10-year and 30-year predicted risks (from 0.26 to 0.32 per 1,000 person-years) (Supplemental Table 9). Sensitivity analyses that did not consider statin initiation as a censoring event also showed a higher ASCVD incidence rate for those with low 10-year but elevated 30-year predicted risk (2.34 per 1,000 person-years) compared with low 10-year and 30-year predicted risk (0.38 per 1,000 person-years) (Supplemental Table 10).
With the use of the lifetime risk equation for long-term ASCVD risk estimation, the prediction tools categorized 40.8% of young adults as having low 10-year but elevated (≥39%) lifetime predicted ASCVD risk (Supplemental Table 11). The incidence rate was 0.42 per 1,000 person-years for those with elevated (≥39%) lifetime predicted ASCVD risk (Supplemental Table 12). The overall NRI with the use of the lifetime risk equation was 7.8% compared with the 10-year risk equation. The net percentage of young adults with ASCVD correctly categorized upward was 80.4% and the net percentage of young adults without ASCVD correctly assigned a lower predicted risk was −72.7% (Supplemental Table 13). The age- and sex-adjusted IRRs were 8.23 (95% CI: 5.91–11.45) among those with elevated 10-year predicted risk and 1.96 (95% CI: 1.69–2.27) among those with low 10-year but elevated lifetime predicted risk compared with those with low 10-year and lifetime predicted risk (Supplemental Table 14).
DISCUSSION
This study compared the performance of the short-term and long-term ASCVD prediction tools recommended by the 2018 AHA/ACC cholesterol guideline in a large cohort of contemporary young adults. A very low percentage of young adults were estimated to have elevated 10-year predicted ASCVD risk, and a higher percentage were estimated to have elevated 30-year predicted ASCVD risk. With the use of the 30-year risk prediction tool, 1.6% of young adults were identified as having low 10-year but elevated 30-year predicted risk. The 30-year risk prediction tool had better classification compared with the 10-year risk prediction tool in young adults. Young adults with low 10-year but elevated 30-year predicted risk had a higher incidence of ASCVD events compared with those with both low 10-year and low 30-year predicted risks. These findings suggest the potential benefit of using long-term prediction tools in addition to short-term risk estimation to identify at-risk young adults.
The 10-year risk prediction models are commonly recommended in patients aged over 40 years.2,15 This is mainly because the original PCEs were developed among adults aged 40 to 75 years who are most abundantly represented in U.S. cardiovascular disease epidemiology cohort studies, and the PCEs are recommended for only this age group.2 The incidence of MI and ischemic stroke hospitalization has increased among young adults in recent years.18,19 The major contributors of ASCVD risk in young adults include tobacco use, hypercholesterolemia, hypertension, and/or diabetes.20 In particular, the prevalence of elevated lipid levels is high during young adulthood,21 and evidence suggests that elevated LDL-C during young adulthood contributes to the onset of ASCVD independently from LDL-C levels in later life.22 Together, these data support earlier ASCVD risk assessment, detection, and intervention of these high-risk young adults and potentially early initiation of lipid-lowering therapy in higher-risk young adults.23
The best approach to ASCVD risk prediction among young adults is currently unknown. The present study suggests that the 30-year risk prediction tools have an overall better performance compared with the 10-year risk models and may help to further identify subgroups of young adults with elevated ASCVD risk despite low estimated 10-year risk. Based on these findings, health system approaches incorporating the 30-year risk prediction tool together with the 10-year risk prediction tool into electronic health records to identify young adult candidates for intervention will help form the basis for a discussion between clinicians and patients. Kaiser Permanente Southern California has built population-based care management programs using clinical information systems and decision support tools, including the Kaiser Permanente ASCVD Risk Estimator (10-year risk prediction), for routine patient care.24,25 Further incorporating a 30-year risk prediction tool into the existing estimator may be the reasonable next step.
The present study found that both 30-year and lifetime ASCVD risk prediction tools discriminate a group of young adults with elevated observed ASCVD events. However, the lifetime risk prediction tool identified that more than 40% of additional young adults had low 10-year but elevated lifetime risk while only 1.6% of additional young adults had low 10-year but elevated 30-year risk. This large discrepancy may be because the 30-year risk model predicts risk on a continuous scale whereas each individual is assigned into 1 of the 5 possible risk categories in the lifetime risk model. In the present analysis, all young adults with ≥1 elevated risk factor were categorized as having elevated predicted lifetime risk, representing about 41% of the study population. These percentages are similar to earlier findings. For example, Marma et al5 reported that 59.2% to 65.6% of men aged 20 to 39 years, and 43.0% to 55.2% of women aged 20 to 39 years had low 10-year but elevated lifetime ASCVD risk according to National Health and Nutrition Examination Survey data. From this analysis, the prevalence of young adults with elevated 10-year predicted risk was estimated to be between 0.4% to 2.4% depending on age group (20–29 years or 30–39 years) and sex. The present study findings suggest that incorporating the 30-year ASCVD risk prediction tool into clinical practice would be translated into a lower number needed to treat to avoid 1 ASCVD event compared with the lifetime risk prediction model. Given that the eventual goal of applying these tools is to identify at-risk young adults for intervention, the 30-year risk prediction tool may be better than the lifetime risk prediction tool. A comprehensive approach to ASCVD prevention, including lipid-lowering therapy, tobacco cessation, and treatment for hypertension and diabetes, may be needed.
The present study confirmed that a low percentage of young adults (5.2% based on 10-year risk, 10.6% based on 30-year risk) who developed ASCVD events were categorized as having elevated predicted ASCVD risk. The median (IQR) 10-year predicted risk among those who had an ASCVD event was only 1.3% (0.6%–2.6%), which is in line with recent findings among adults aged 40 to 55 years who experienced their first MI.7 These findings suggest that many individuals would not have qualified for statin therapy before their ASCVD events. Moreover, the present study showed that the 30-year risk prediction tool classified 249 individuals with ASCVD events into a higher risk category, but also up-classified more than 56,000 individuals without ASCVD events. This yielded a high ratio of individuals who were up-classified per ASCVD event. These findings suggest that more refined risk prediction models are needed to better identify at-risk young adults. To further improve the current risk prediction tools, ongoing efforts incorporating other important risk factors such as social determinants of health, polygenic risk scores, metabolomics, and/or proteomics may provide important insights and move more toward precision risk prediction in young adults.26–29 In addition, further studies are needed to evaluate alternative approaches to select young adults who may benefit from lipid-lowering therapies based on predicted absolute risk reduction rather than an absolute risk-based approach.30,31
STUDY STRENGTHS AND LIMITATIONS.
We evaluated a large contemporary cohort of young adults aged 18 to 39 years of diverse racial/ethnic groups in an integrated U.S. health care system. We examined the distribution of calculated ASCVD risk according to various short-term and long-term risk prediction algorithms recommended in the 2018 AHA/ACC cholesterol guideline, and further linked those calculated risks to observed ASCVD events during follow-up with the use of relatively complete electronic health records. However, our study population had a relatively short follow-up (median 4 years). These are the challenges of studying young adults with the use of electronic health records from a U.S. health care system, because they frequently change their health plans. This study used the ASCVD risk cutoffs used in previous studies for older age groups. Although the 10-year and lifetime risk tools validated their cutoffs, they were not specific for young adults and this study did not evaluate age-specific cutoffs or age-based discrimination. There were no validation studies regarding cutoffs for 30-year ASCVD risk. Although this study compared the observed ASCVD event rates per estimated short-term and long-term risk, future studies with longer follow-ups will be necessary to evaluate the calibration of long-term risk prediction models among young adults. We applied the age of 40 years to estimate 10-year predicted risk with the use of the PCEs, which overestimated the 10-year predicted risk in this population aged 18 to 39 years.
CONCLUSIONS
Young adults enrolled in a large integrated U.S. health care system with either high short-term or low short-term but elevated long-term predicted risk had higher incidence of ASCVD events compared with those with both low short-term and long-term predicted risk, suggesting that current risk assessment practices miss the opportunity to identify young adults eligible for preventive measures. Further practical clinical research is needed to test the efficacy, feasibility, and acceptability of implementing risk assessment tools in young adult patients. For the time being, using the 30-year risk prediction tool to identify additional at-risk young adults for lipid-lowering therapy and ASCVD prevention may be important.
Supplementary Material
PERSPECTIVES.
COMPETENCY IN PATIENT CARE AND PROCEDURAL SKILLS:
A subgroup of young adults at low 10-year predicted atherosclerotic risk have high 30-year risk and a 3-fold higher incidence of disease than those with both low 10-year and 30-year predicted risks after adjustment for age and sex.
TRANSLATIONAL OUTLOOK:
Using the 30-year risk prediction tool to identify young adults as candidates for lipid-lowering therapy and other preventive measures may represent an important opportunity to improve patient care.
FUNDING SUPPORT AND AUTHOR DISCLOSURES
This work was supported by the National Institutes of Health (R01HL155081 to Drs An and Zhang), which had no role in the design and conduct of the study; the collection, management, analysis, and interpretation of the data; the preparation, review, or approval of the manuscript; or the decision to submit the manuscript for publication. The authors have reported that they have no relationships relevant to the contents of this paper to disclose.
ABBREVIATIONS AND ACRONYMS
- ASCVD
atherosclerotic cardiovascular disease
- BMI
body mass index
- HDL-C
high-density lipoprotein cholesterol
- IRR
incident rate ratios
- LDL-C
low-density lipoprotein cholesterol
- MI
myocardial infarction
- NRI
net reclassification improvement
- PCE
pooled cohort equations
Footnotes
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the Author Center.
APPENDIX For supplemental tables, please see the online version of this paper.
REFERENCES
- 1.Lloyd-Jones DM, Braun LT, Ndumele CE, et al. Use of risk assessment tools to guide decision-making in the primary prevention of atherosclerotic cardiovascular disease: a special report from the American Heart Association and American College of Cardiology. Circulation. 2019;139(25):e1162–1177. [DOI] [PubMed] [Google Scholar]
- 2.Goff DC Jr, Lloyd-Jones DM, Bennett G, et al. 2013 ACC/AHA guideline on the assessment of cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;63(25 Pt B):2935–2959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Berry JD, Liu K, Folsom AR, et al. Prevalence and progression of subclinical atherosclerosis in younger adults with low short-term but high lifetime estimated risk for cardiovascular disease: the Coronary Artery Risk Development in Young Adults study and Multi-Ethnic Study of Atherosclerosis. Circulation. 2009;119(3):382–389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kandula NR, Kanaya AM, Liu K, et al. Association of 10-year and lifetime predicted cardiovascular disease risk with subclinical atherosclerosis in South Asians: findings from the Mediators of Atherosclerosis in South Asians Living in America (MASALA) study. J Am Heart Assoc. 2014;3(5):e001117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Marma AK, Berry JD, Ning H, Persell SD, Lloyd-Jones DM. Distribution of 10-year and lifetime predicted risks for cardiovascular disease in US adults: findings from the National Health and Nutrition Examination Survey 2003 to 2006. Circ Cardiovasc Qual Outcomes. 2010;3(1):8–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nanna MG, Peterson ED, Wojdyla D, Navar AM. The accuracy of cardiovascular pooled cohort risk estimates in U.S. older adults. J Gen Intern Med. 2020;35(6):1701–1708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zeitouni M, Nanna MG, Sun JL, Chiswell K, Peterson ED, Navar AM. Performance of guideline recommendations for prevention of myocardial infarction in young adults. J Am Coll Cardiol. 2020;76(6):653–664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pencina MJ, d’Agostino RB Sr, Larson MG, Massaro JM, Vasan RS. Predicting the 30-year risk of cardiovascular disease: the Framingham heart study. Circulation. 2009;119(24):3078–3084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lloyd-Jones DM, Leip EP, Larson MG, et al. Prediction of lifetime risk for cardiovascular disease by risk factor burden at 50 years of age. Circulation. 2006;113(6):791–798. [DOI] [PubMed] [Google Scholar]
- 10.Singh A, Collins BL, Gupta A, et al. Cardiovascular risk and statin eligibility of young adults after an MI: Partners YOUNG-MI Registry. J Am Coll Cardiol. 2018;71(3):292–302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Reynolds K, Go AS, Leong TK, et al. Trends in incidence of hospitalized acute myocardial infarction in the Cardiovascular Research Network (CVRN). Am J Med. 2017;130(3):317–327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Go AS, Hylek EM, Chang Y, et al. Anticoagulation therapy for stroke prevention in atrial fibrillation: how well do randomized trials translate into clinical practice? JAMA. 2003;290(20):2685–2692. [DOI] [PubMed] [Google Scholar]
- 13.Singer DE, Chang Y, Borowsky LH, et al. A new risk scheme to predict ischemic stroke and other thromboembolism in atrial fibrillation: the ATRIA study stroke risk score. J Am Heart Assoc. 2013;2(3):e000250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chen W, Petitti DB, Enger S. Limitations and potential uses of census-based data on ethnicity in a diverse community. Ann Epidemiol. 2004;14(5):339–345. [DOI] [PubMed] [Google Scholar]
- 15.Grundy SM, Stone NJ, Bailey AL, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA guideline on the management of blood cholesterol: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2019;73(24):e285–e350. [DOI] [PubMed] [Google Scholar]
- 16.Clark CJ, Alonso A, Spencer RA, Pencina M, Williams K, Everson-Rose SA. Predicted long-term cardiovascular risk among young adults in the national longitudinal study of adolescent health. Am J Public Health. 2014;104(12):e108–115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Xu Y, Cheung YB, Lam KF, Tan SH, Milligan P. A simple approach to the estimation of incidence rate difference. Am J Epidemiol. 2010;172(3):334–343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gupta A, Wang Y, Spertus JA, et al. Trends in acute myocardial infarction in young patients and differences by sex and race, 2001 to 2010. J Am Coll Cardiol. 2014;64(4):337–345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ramirez L, Kim-Tenser MA, Sanossian N, et al. Trends in acute ischemic stroke hospitalizations in the United States. J Am Heart Assoc. 2016;5(5). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Stone NJ, Smith SC Jr, Orringer CE, et al. Managing atherosclerotic cardiovascular risk in young adults: JACC state-of-the-art review. J Am Coll Cardiol. 2022;79(8):819–836. [DOI] [PubMed] [Google Scholar]
- 21.Zhang Y, An J, Reynolds K, Safford MM, Muntner P, Moran AE. Trends of elevated low-density lipoprotein cholesterol, awareness, and screening among young adults in the US, 2003–2020. JAMA Cardiol. 2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zhang Y, Vittinghoff E, Pletcher MJ, et al. Associations of blood pressure and cholesterol levels during young adulthood with later cardiovascular events. J Am Coll Cardiol. 2019;74(3):330–341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Razavi AC, Mehta A, Sperling LS. Statin therapy for the primary prevention of cardiovascular disease: pros. Atherosclerosis. 2022;356:41–45. [DOI] [PubMed] [Google Scholar]
- 24.Kanter MH, Lindsay G, Bellows J, Chase A. Complete care at Kaiser Permanente: transforming chronic and preventive care. Jt Comm J Qual Patient Saf. 2013;39(11):484–494. [DOI] [PubMed] [Google Scholar]
- 25.Go AS, Tabada G, Reynolds K, et al. A new ASCVD risk estimator is more accurate than the ACC/AHA pooled cohort equation in four diverse community-based populations in the U.S. and Canada [abstract]. Circulation. 2018;138(suppl 1):A12623. [Google Scholar]
- 26.Javed Z, Valero-Elizondo J, Dudum R, et al. Development and validation of a polysocial risk score for atherosclerotic cardiovascular disease. Am J Prev Cardiol. 2021;8:100251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mosley JD, Gupta DK, Tan J, et al. Predictive accuracy of a polygenic risk score compared with a clinical risk score for incident coronary heart disease. JAMA. 2020;323(7):627–635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Elliott J, Bodinier B, Bond TA, et al. Predictive accuracy of a polygenic risk score-enhanced prediction model vs a clinical risk score for coronary artery disease. JAMA. 2020;323(7):636–645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Whelton SP, Post WS. Importance of traditional cardiovascular risk factors for identifying high-risk persons in early adulthood. Eur Heart J. 2022;43(30):2901–2903. [DOI] [PubMed] [Google Scholar]
- 30.Kohli-Lynch CN, Lewsey J, Boyd KA, et al. Beyond 10-year risk: a cost-effectiveness analysis of statins for the primary prevention of cardiovascular disease. Circulation. 2022;145(17):1312–1323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Thanassoulis G, Williams K, Altobelli KK, Pencina MJ, Cannon CP, Sniderman AD. Individualized statin benefit for determining statin eligibility in the primary prevention of cardiovascular disease. Circulation. 2016;133(16):1574–1581. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


