Abstract
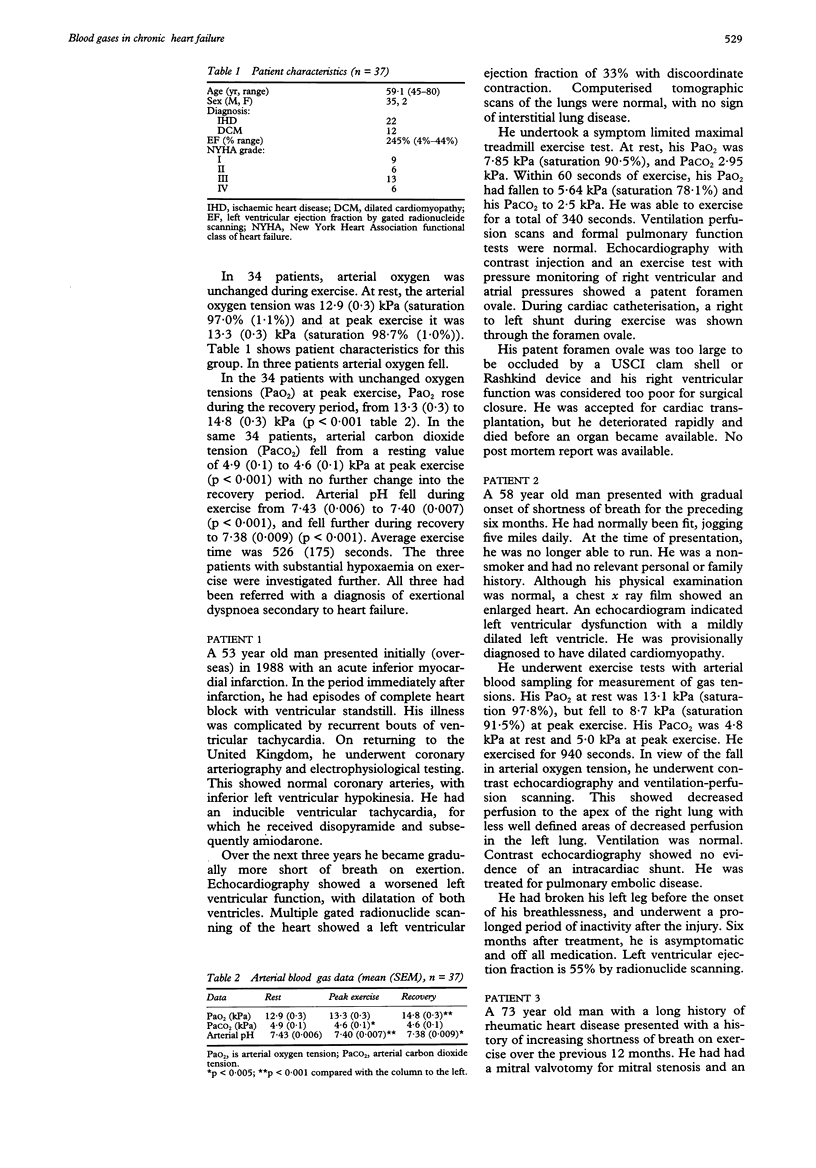
BACKGROUND--Coexisting cardiorespiratory disease may contribute in individual cases to the increased ventilatory response to exercise in patients with chronic heart failure. OBJECTIVE--To characterise further the arterial blood gas response to exercise and to explore the possible uses of blood gas sampling in clinical practice in patients with chronic heart failure. METHODS--37 patients with a primary diagnosis of chronic heart failure (age (range) 59 (45-80); left ventricular ejection fraction 24.5% (4%-44%)) underwent exercise testing with arterial blood gas analysis during exercise. RESULTS--In 34 patients there was a small fall in arterial carbon dioxide tension from a mean (SEM) of 4.9 (0.1) kPa at rest to 4.6 (0.1) kPa at peak exercise (p < 0.001). There was no significant change in arterial oxygen tension. During the recovery period arterial oxygen tension rose from 13.3 (0.3) kPa at peak exercise to 14.8 (0.3) kPa three minutes into recovery (p < 0.001). Arterial carbon dioxide tension was unchanged. In the remaining three patients there was considerable arterial hypoxaemia on exercise, from 10.4 kPa at rest to 7.7 kPa at peak exercise. All of these patients had an alternative diagnosis (patent foramen ovale with right to left shunt during exercise, pulmonary embolic disease, and clinically unsuspected obstructive airways disease). CONCLUSION--Patients with a presumptive diagnosis of chronic heart failure should undergo exercise testing with arterial blood gas analysis. Arterial hypoxaemia on exercise is rare in stable chronic heart failure. If hypoxia on exercise is detected, an alternative diagnosis should be sought.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Buller N. P., Poole-Wilson P. A. Mechanism of the increased ventilatory response to exercise in patients with chronic heart failure. Br Heart J. 1990 May;63(5):281–283. doi: 10.1136/hrt.63.5.281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark A., Coats A. The mechanisms underlying the increased ventilatory response to exercise in chronic stable heart failure. Eur Heart J. 1992 Dec;13(12):1698–1708. doi: 10.1093/oxfordjournals.eurheartj.a060127. [DOI] [PubMed] [Google Scholar]
- Franciosa J. A., Leddy C. L., Wilen M., Schwartz D. E. Relation between hemodynamic and ventilatory responses in determining exercise capacity in severe congestive heart failure. Am J Cardiol. 1984 Jan 1;53(1):127–134. doi: 10.1016/0002-9149(84)90696-9. [DOI] [PubMed] [Google Scholar]
- Higginbotham M. B., Morris K. G., Conn E. H., Coleman R. E., Cobb F. R. Determinants of variable exercise performance among patients with severe left ventricular dysfunction. Am J Cardiol. 1983 Jan 1;51(1):52–60. doi: 10.1016/s0002-9149(83)80010-1. [DOI] [PubMed] [Google Scholar]
- Moore D. P., Weston A. R., Hughes J. M., Oakley C. M., Cleland J. G. Effects of increased inspired oxygen concentrations on exercise performance in chronic heart failure. Lancet. 1992 Apr 4;339(8797):850–853. doi: 10.1016/0140-6736(92)90288-e. [DOI] [PubMed] [Google Scholar]
- Rubin S. A., Brown H. V., Swan H. J. Arterial oxygenation and arterial oxygen transport in chronic myocardial failure at rest, during exercise and after hydralazine treatment. Circulation. 1982 Jul;66(1):143–148. doi: 10.1161/01.cir.66.1.143. [DOI] [PubMed] [Google Scholar]
- Rubin S. A., Brown H. V. Ventilation and gas exchange during exercise in severe chronic heart failure. Am Rev Respir Dis. 1984 Feb;129(2 Pt 2):S63–S64. doi: 10.1164/arrd.1984.129.2P2.S63. [DOI] [PubMed] [Google Scholar]
- Sullivan M. J., Higginbotham M. B., Cobb F. R. Increased exercise ventilation in patients with chronic heart failure: intact ventilatory control despite hemodynamic and pulmonary abnormalities. Circulation. 1988 Mar;77(3):552–559. doi: 10.1161/01.cir.77.3.552. [DOI] [PubMed] [Google Scholar]


