Abstract
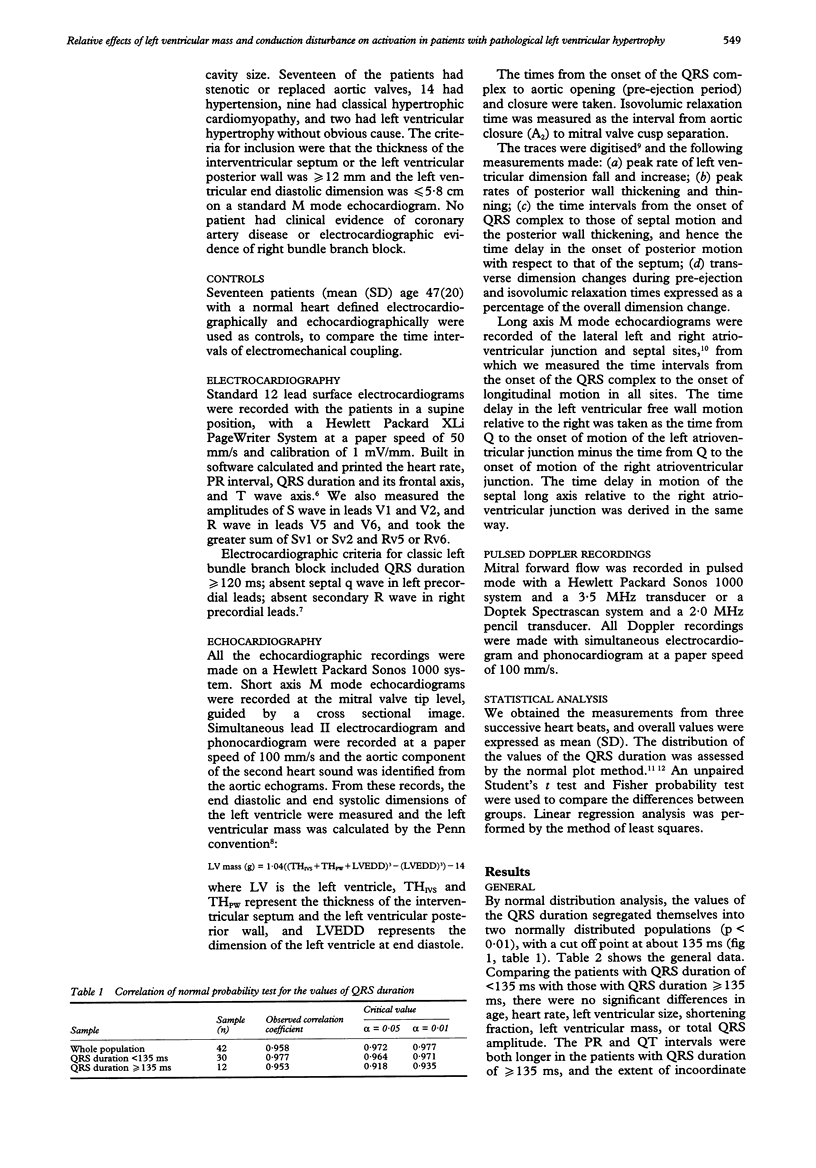
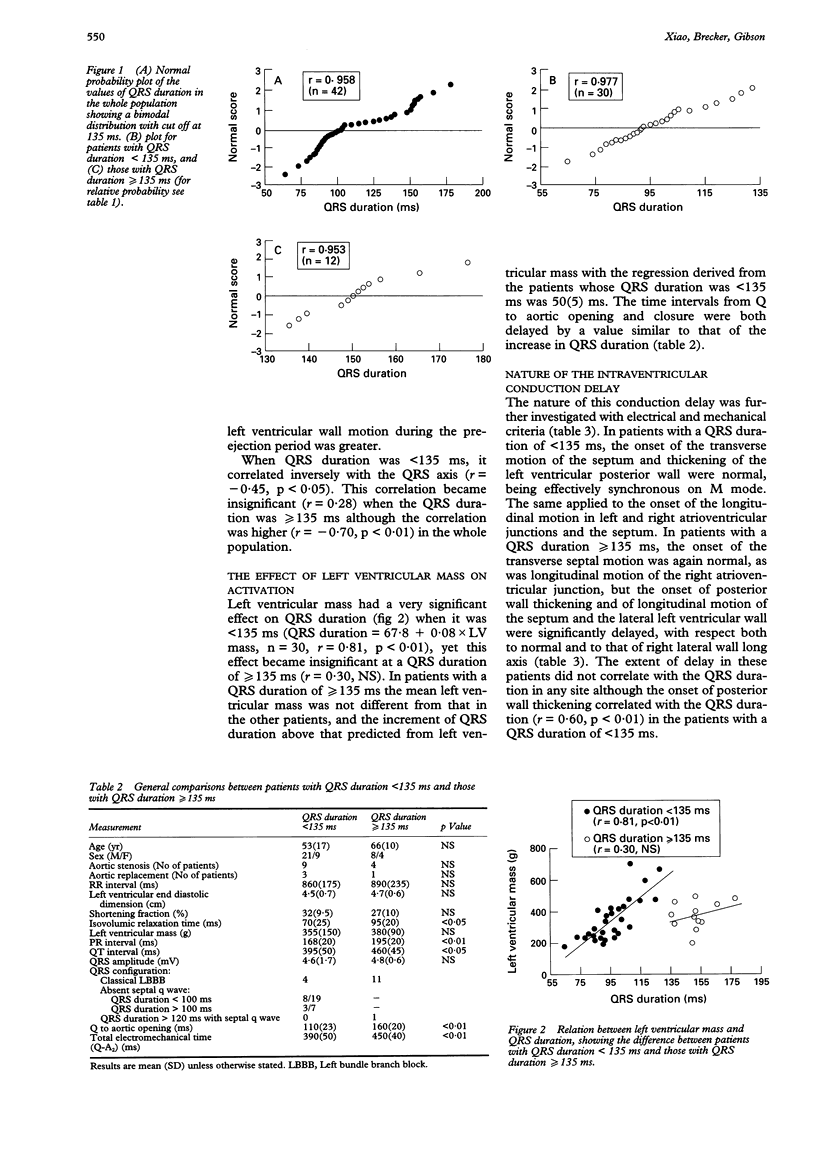
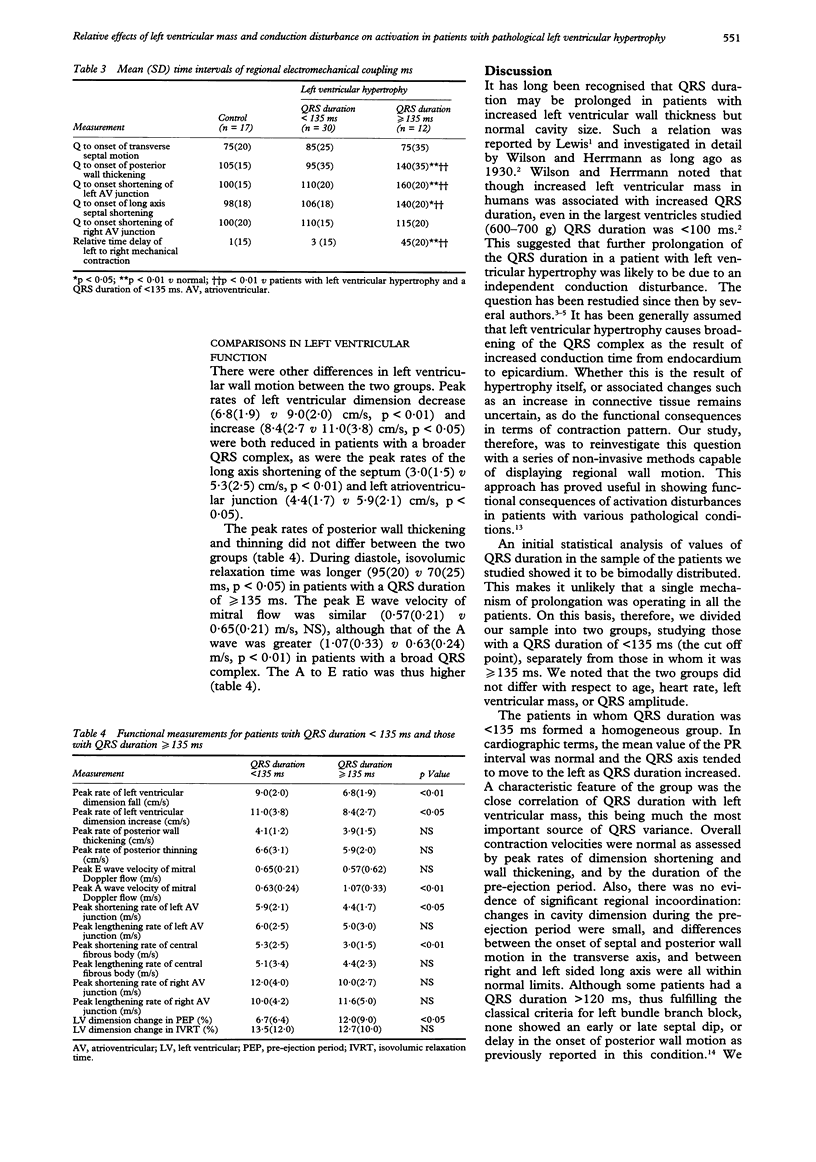
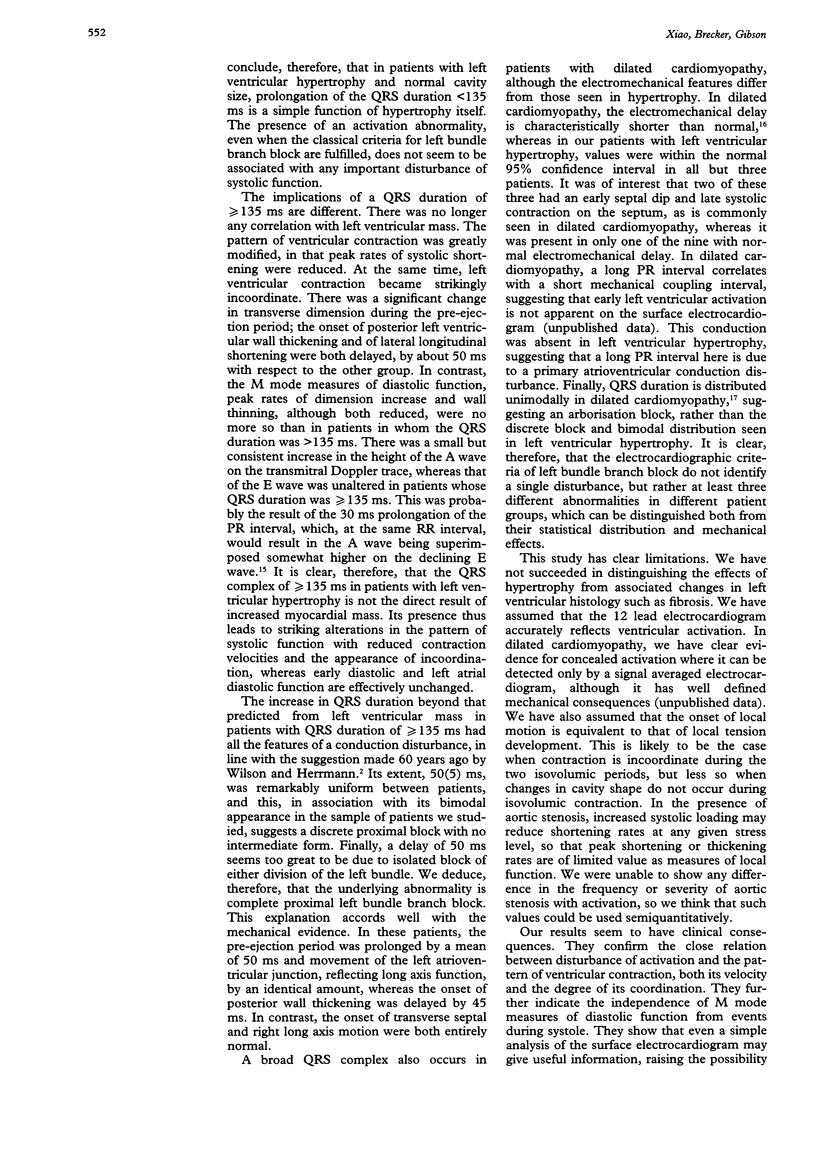
OBJECTIVE--To investigate the relative effects of left ventricular mass and conduction disturbance on the duration and axis of the QRS complex in patients with left ventricular hypertrophy and a normal cavity size. STUDY DESIGN--Retrospective and prospective study of 42 patients with pathological left ventricular hypertrophy and 17 normal controls by electrocardiography, echocardiography, and pulsed Doppler recordings. SETTING--Tertiary cardiac referral centre. PATIENTS--42 patients (mean (SD) age 58(16)) with left ventricular hypertrophy and normal cavity size. 17 had stenotic or replaced aortic valves, 14 had hypertension, 9 had hypertrophic cardiomyopathy and 2 had left ventricular hypertrophy without obvious cause. 17 normal people (mean (SD) age 47(20)) were used as controls. RESULTS--The values of QRS duration segregated into two normally distributed populations, with a cut off point at 135 ms. When patients with QRS duration of < 135 ms (n = 30) were compared with those with QRS duration of > or = 135 ms (n = 12), there were no significant differences in age, heart rate, left ventricular size, shortening fraction, left ventricular mass and total QRS amplitude. Both the PR and QT intervals were, however, longer in patients with a QRS duration of > or = 135 ms, and the extent of incoordinate left ventricular wall motion during the preejection period was greater. When it was < 135 ms the QRS duration was strikingly correlated with left ventricular mass (r = 0.81, p < 0.01). The onsets of transverse septal motion and of posterior wall thickening were normal, as were the onsets of the longitudinal motion of left, septal, and right atrioventricular junctions. When the QRS duration was > or = 135 ms the onset of transverse septal motion and of the longitudinal right atrioventricular junction were both normal, but that of the posterior wall thickening (p < 0.01) and the longitudinal motion of the septum (p < 0.05) and lateral left ventricular wall (p < 0.01) were significantly delayed. Peak rates of left ventricular dimension decrease (p < 0.01) and increase (p < 0.01) were both reduced, as were the peak rates of the long axis shortening of the septum (p < 0.01) and left atrioventricular junction (p < 0.05), whereas the peak rates of posterior wall thickening and thinning did not differ between the two groups. Mean isovolumic relaxation time was longer (p < 0.05) in patients with QRS duration of > or = 135 ms and the peak velocity of the A wave and thus the A to E ratio was greater than in patients with a QRS duration of < 135 ms and that of the E wave was similar in the two groups. CONCLUSION--In patients with left ventricular hypertrophy the values of QRS duration are bimodally distributed, with a cut off point at 135 ms. When QRS duration is < 135 ms, left ventricular mass seems to be closely related to QRS duration, making it the dominant factor determining the activation time. Once QRS duration reaches > or = 135 ms the correlation with mass no longer exists. The statistical distribution, electrocardiographic characteristics, and incoordination pattern of left ventricular wall motion all suggest the development of a proximal left bundle branch block.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Casale P. N., Devereux R. B., Alonso D. R., Campo E., Kligfield P. Improved sex-specific criteria of left ventricular hypertrophy for clinical and computer interpretation of electrocardiograms: validation with autopsy findings. Circulation. 1987 Mar;75(3):565–572. doi: 10.1161/01.cir.75.3.565. [DOI] [PubMed] [Google Scholar]
- Devereux R. B., Reichek N. Echocardiographic determination of left ventricular mass in man. Anatomic validation of the method. Circulation. 1977 Apr;55(4):613–618. doi: 10.1161/01.cir.55.4.613. [DOI] [PubMed] [Google Scholar]
- GRANT R. P., DODGE H. T. Mechanisms of QRS complex prolongation in man; left ventricular conduction disturbances. Am J Med. 1956 Jun;20(6):834–852. doi: 10.1016/0002-9343(56)90204-2. [DOI] [PubMed] [Google Scholar]
- Jones C. J., Raposo L., Gibson D. G. Functional importance of the long axis dynamics of the human left ventricle. Br Heart J. 1990 Apr;63(4):215–220. doi: 10.1136/hrt.63.4.215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDonald I. G. Echocardiographic demonstration of abnormal motion of the interventricular septum in left bundle branch block. Circulation. 1973 Aug;48(2):272–280. doi: 10.1161/01.cir.48.2.272. [DOI] [PubMed] [Google Scholar]
- Molloy T. J., Okin P. M., Devereux R. B., Kligfield P. Electrocardiographic detection of left ventricular hypertrophy by the simple QRS voltage-duration product. J Am Coll Cardiol. 1992 Nov 1;20(5):1180–1186. doi: 10.1016/0735-1097(92)90376-x. [DOI] [PubMed] [Google Scholar]
- Pearson A. C., Janosik D. L., Redd R. R., Buckingham T. A., Blum R. I., Labovitz A. J. Doppler echocardiographic assessment of the effect of varying atrioventricular delay and pacemaker mode on left ventricular filling. Am Heart J. 1988 Mar;115(3):611–621. doi: 10.1016/0002-8703(88)90812-5. [DOI] [PubMed] [Google Scholar]
- Upton M. T., Gibson D. G. The study of left ventricular function from digitized echocardiograms. Prog Cardiovasc Dis. 1978 Mar-Apr;20(5):359–384. doi: 10.1016/0033-0620(78)90003-8. [DOI] [PubMed] [Google Scholar]
- Xiao H. B., Brecker S. J., Gibson D. G. Differing effects of right ventricular pacing and left bundle branch block on left ventricular function. Br Heart J. 1993 Feb;69(2):166–173. doi: 10.1136/hrt.69.2.166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiao H. B., Brecker S. J., Gibson D. G. Effects of abnormal activation on the time course of the left ventricular pressure pulse in dilated cardiomyopathy. Br Heart J. 1992 Oct;68(4):403–407. doi: 10.1136/hrt.68.10.403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiao H. B., Lee C. H., Gibson D. G. Effect of left bundle branch block on diastolic function in dilated cardiomyopathy. Br Heart J. 1991 Dec;66(6):443–447. doi: 10.1136/hrt.66.6.443. [DOI] [PMC free article] [PubMed] [Google Scholar]


