Abstract
Older adults are a high priority population for smoking cessation. This study observed the influence of older age on the relationship between quitting predictors and cessation. Secondary analysis was conducted of a primary care trial of adults who smoke cigarettes randomized to standard advice to quit or advice plus two-week supply of nicotine replacement therapy. Logistic regressions assessed interactions of age (<60 vs. ≥ 60 years) by predictors in relation to quit attempts and six-month cessation controlling for treatment. Predicting quit attempts, there was an interaction of age by motivation (p=.025), and trend of age by nicotine dependence (p=.057). Predicting six-month cessation, an interaction of age by motivation was observed (p=.020) and a trend of age by dependence (p=.067). For those with high nicotine dependence, older adults had less successful outcomes compared to younger counterparts. Yet, among participants unmotivated to quit, older adults had more successful outcomes than those younger.
Keywords: tobacco cessation, geriatric health, primary care, smoking cessation
Introduction
Cigarette smoking prevalence among U.S. adults ≥ 65 years has not changed in 15 years (currently 9%), although younger ages have seen drastic reductions (Cornelius et al., 2022; Isenberg et al., 2016; Kleykamp & Kulak, 2022; Warren et al., 2014). Notably, older adults experience a disproportionate impact of tobacco morbidity and mortality compared to their younger counterparts (Warren et al., 2014). Annual smoking-related mortality (392K) is higher for older adults who smoke cigarettes compared to those aged 35 - 64 years who smoke (163.5K), despite a lower prevalence of cigarette smoking in the older age group comparatively (i.e., 9% vs. 14-15%) (Warren et al., 2014). Tobacco use also exacerbates health conditions (e.g., diabetes, chronic pain) which are more common in older age (Dahlhamer et al., 2018; Rimer et al., 1990; Warren et al., 2014). Further, cigarette smoking is a risk factor for Alzheimer’s disease, dementia, and cognitive decline, all of which increase in prevalence with advancing age (Alzheimer’s Association, 2022; Baumgart et al., 2015; Durazzo et al., 2014). Thus, older adults are a population at high risk of the negative health consequences of cigarette smoking.
Although there are increased health risks of cigarette smoking in older age, older adults are less interested in quitting than younger adults (53.7% vs. 62.3-72.7%) and less likely to make a quit attempt per annum (Arancini et al., 2021; Babb et al., 2017). In a nationally representative sample, about 47% of older adults who smoked cigarettes made a 24-hour quit attempt, and 5.4% had quit (≥ six months) in the past year, compared to 58.7% and 8.2% among younger adults, respectively (Babb et al., 2017). Despite less interest in quitting in older age, over half (53.7%) of older adults who smoke cigarettes do want to quit (Babb et al., 2017). Yet, only a third (37%) of these older adults receive an evidence-based cessation resource, and only 5% successfully quit annually (Henley et al., 2019). Lower quit success and cessation treatment utilization is likely attributed to various factors including misinformation about the health benefits of quitting in older age and false beliefs that older adults are unwilling or unlikely to be successful quitting. In fact, there are substantial health benefits of quitting cigarettes across the lifespan (Adams, 2020) and evidence suggests older adults quit at comparable, or higher, rates in cessation treatment compared to those younger (Chen et al., 2015).
Despite the public health need to promote tobacco cessation in older age, an age group expected to double between 2012 and 2050 (Ortman et al., 2019), older adults are routinely underrepresented in the cessation literature (Chen et al., 2015; McAfee et al., 2021). More commonly, treatment trials will simply report age-group differences in outcomes (Chen et al., 2015). Fewer studies examine factors that facilitate quitting within samples specifically of older adults who smoke cigarettes (Chen et al., 2015). In community samples of older adults who smoke cigarettes, lower nicotine dependence, social support, and greater quitting self-efficacy predicted long-term abstinence (Cohen-Mansfield et al., 2016; Donze et al., 2007). For older adults in treatment (i.e., cessation clinics, self-help materials, telephone counseling), lower nicotine dependence predicted long-term success (Hsu et al., 2018; Tait et al., 2007). However, many of these studies included a wide definition for “older” (i.e., ≥ 50 years), which does not capture the developmental period of older age (60 or 65 years of age and older by World Health Organization) [World Health Organization (WHO) 2019]. Older adulthood is a period with unique considerations relevant to cessation treatment (e.g., reductions in social functioning, changes in cognition, polypharmacy, underdiagnosis and undertreatment of other substance use disorders [Substance Abuse and Mental Health Services Administration (SAMHSA), 2020]. To our knowledge, only one study assessed if and how predictors of quitting were differentially related to cessation, based on age group (Arancini et al., 2021). Arancini and colleagues (2021) found age-related differences in quit attempts and success (30-day abstinence) were influenced by motivation to quit and nicotine dependence (Arancini et al., 2021). However, older age was more widely defined (≥ 55 years). An older and narrower age range to define older adults who smoke cigarettes could better account for unique aging considerations. Further, this general population sample of adults who smoked cigarettes had not necessarily received cessation treatment, resources, or advice to quit. Thus, it is unknown how predictors of quitting are impacted by age in relationship to cessation outcomes following advice to quit.
This study examined if and how established predictors of cessation were uniquely related to quitting among older (vs. younger) adults who smoke cigarettes after receiving standard cessation care (i.e., brief advice to quit). Secondary analysis was conducted on data from a trial (Carpenter et al. 2020) in which adults smoking cigarettes in primary care were randomized to either brief physician advice to quit or to the same quit advice plus brief supply of nicotine replacement (NRT). This study focused on potential interactions between age group (<60 vs. ≥ 60 years) and known predictors of cessation: a) motivation to quit, b) nicotine dependence, and c) quitting self-efficacy, each in relation to both 24-hour quit attempts and success 6-months later (7-day point prevalence abstinence at six-months). We hypothesized that each of these factors would be more strongly related to quit outcomes among an older (vs. younger) age group.
Methods
Procedure
The parent study recruited adults who smoke cigarettes from South Carolina primary care clinics (2014 - 2017) (Carpenter et al, 2020). Inclusion criteria included: ≥18 years of age, smoking ≥ five cigarettes daily for ≥ 25 days of past 30, and English speaking. Exclusion criteria included FDA contraindications for NRT use. Prior to study initiation, tobacco cessation certified study staff delivered a one-time (60-90 minute) training of study procedures, review of clinical practice cessation guidelines for physicians (i.e., Ask, Advise, and Refer standard care), and review of NRT to study staff and providers. Providers did not receive study scripts (e.g., explicit prompts to initiate a quit date) but were encouraged to deliver standard care for cessation. Participants provided written informed consent and completed baseline questionnaires while visiting the clinic. Individuals were randomized to 1) standard care of brief physician advice to quit (i.e., Ask, Advise, Refer) or 2) standard care plus two-week supply of NRT (patch and lozenge). All participants received a standard brochure about smoking cessation (National Cancer Institute brochure), which included general information about NRT, and referral information to the state tobacco quitline. Thus, all participants received standard care of advice to quit from their providers and take-home cessation information. For those randomized to NRT sampling, providers could discuss these medications to the extent that they wished. All participants were given detailed information of both NRT products, including information about how to access more of these medications if needed. Follow-up measures were completed via phone at one, three, and six-months. Detailed procedural information is published elsewhere (Dahne et al., 2018).
Measures
Relevant Baseline Measures
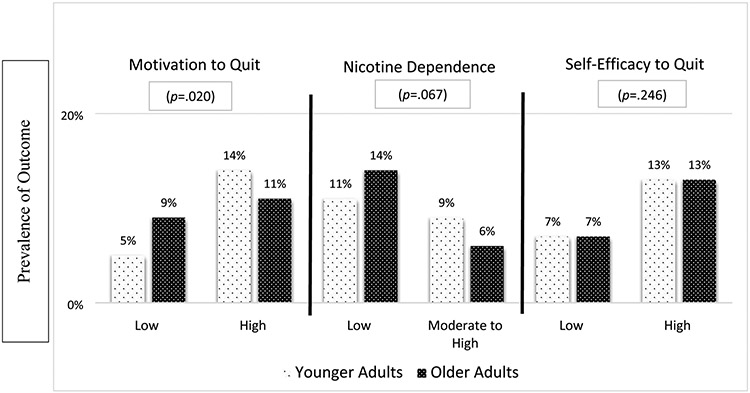
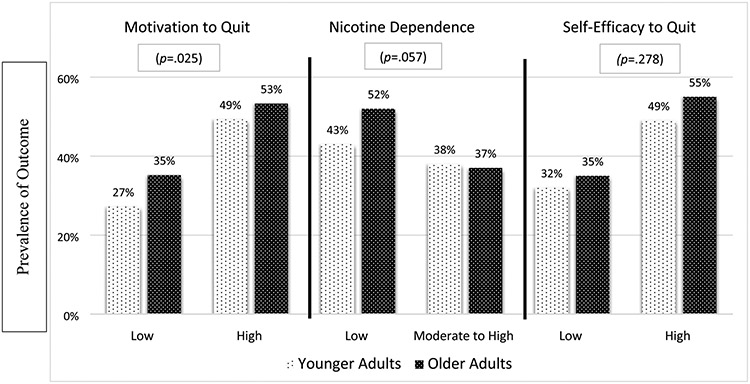
Participants completed Heaviness of Smoking Index (HSI) (range 0-6) to assess nicotine dependence (Borland et al., 2010). For visual representation in Figures 1-2, scores were dichotomized: low (0-1) versus moderate/high (2-6). Motivation to quit and self-efficacy to quit were measured with 0-10 scales (Burris et al., 2015; Heatherton et al., 1989). For Figures 1-2, scores were dichotomized low (0-5) vs. high (6-10). Individuals also reported the average number of cigarettes they smoked per day, a quit attempt in the past 12 months (yes vs. no), and use of NRT at their last quit attempt (yes vs. no).
Figure 1. Interactions of Age Group by Predictors in Relationship to Any 24 Hour Quit Attempt.
Note: Predictors dichotomized solely for visual representation; p-values represent the overall test of the interaction of continuous predictors and age group in relationship to likelihood of outcome, as presented in text. Older adults (≥60 years) compared to younger adults (<60 years).
Figure 2. Interactions of Age Group by Predictors in Relationship to Six-Month Point Prevalence.
Note: Predictors dichotomized solely for visual representation; p-values represent the overall test of the interaction of continuous predictors and age group in relationship to likelihood of outcome, as presented in text. Older adults (≥60 years) compared to younger adults (<60 years).
Cessation Outcomes
At one, three, and six-month follow-ups, participants identified any quit attempt sustained ≥ 24 hours. Incidence of quit attempts was defined across the entire six-months (i.e., any point of assessment). At six-months, participants reported abstinence: no smoking, not even a puff, ≥ seven days (i.e., point prevalence) at the time of six-month follow-up.
Data Analysis
Descriptive statistics assessed demographics by age group (i.e., <60 years vs. ≥60 years). Chi-square analyses compared age group in relationship to demographic characteristics [i.e., gender, race, ethnicity, employment status, insurance status, educational level, and income]. In preliminary analyses, independent t-tests and chi-square analyses assessed age group differences (<60 years vs. ≥60 years) in the baseline measures of quitting history (i.e., past year quit attempt, NRT use at last quit attempt), cigarettes per day, and predictors of cessation (i.e., motivation to quit, self-efficacy to quit, nicotine dependence). Next, binary logistic regression models assessed relationship between age group and each outcome: 24-hour quit attempt (yes vs. no) and six-months point prevalence (yes vs. no). Regression analyses controlled for treatment (standard care vs. standard care plus NRT sample). Quit outcomes were based on intent-to-treat principles, in which missing data was assigned as smoking or no quit attempt at follow-up. Intent-to-treat approach is the most conservative and recommended by the Society of Research on Nicotine and Tobacco (Hughes et al., 2003). We also tested the interaction of age group (<60 years vs. ≥ 60 years) and treatment group in relationship to both outcomes. Final logistic regression models included main effects of age group (<60 years vs. ≥60 years) and continuous predictors (i.e., motivation to quit, nicotine dependence, self-efficacy for quitting), as well as the interactions between age group and predictors. We opted against analyses of age as a continuous predictor given interest in comparing other ages to the distinct developmental period of older adulthood.
Results
Demographics
Demographics for younger (N=917) and older adults (N=328) are presented (Table 1). Full sample demographics (N=1245) have been previously published (Carpenter et al., 2020). Older adults were more likely to have health insurance [χ2 (1) = 25.9, p<.001], and less likely to be employed [χ2 (5) = 516. 9, p<.001] compared to younger adults. Educational background differed by age group [χ2 (2) = 7.0, p=.031], with older adults having a lower rate of post high school education. Race (i.e., Black/African American, White, Other race), ethnicity, gender, and income did not differ by age group.
Table 1.
Demographic Characteristics of Younger and Older Samples
| Younger Adults (N=917) | Older Adults (N=328) | p | |
|---|---|---|---|
| N (%) | N (%) | ||
| Gender | .27 | ||
| Men | 351 (38.3) | 137 (41.8) | |
| Women | 566 (61.7) | 191 (58.2) | |
| Race | .172 | ||
| White/Caucasian | 585 (63.8) | 191 (58.2) | |
| Black/African American | 315 (34.4) | 131 (39.9) | |
| Asian American | 4 (0.4) | 0 | |
| Multiracial | 4 (0.4) | 1 (0.3) | |
| American Indian/Alaskan Native | 5 (0.5) | 1 (0.3) | |
| Other | 4 (0.4) | 3 (0.9) | |
| Native Hawaiian/Other Pacific Islander | 1 (0.1) | 1 (0.3) | |
| Ethnicity | .52 | ||
| Non-Hispanic/Latino | 900 (98.1) | 320 (97.6) | |
| Hispanic/Latino | 17 (1.9) | 8 (2.4) | |
| Employment Status | <.001 | ||
| Employed Full or Part Time | 491 (53.5) | 50 (15.2) | |
| Not Employed Full or Part Time | 426 (46.5) | 278 (84.8) | |
| Insurance Status | <.001 | ||
| Currently have health care coverage | 763 (83.2) | 310 (94.5) | |
| No health care coverage | 154 (16.8) | 18 (5.5) | |
| Highest Education Level | |||
| Highschool/GED or less | 570 (62.2) | 226 (68.9) | .031 |
| Some College | 280 (30.5) | 75 (22.9) | |
| College Graduate | 67 (7.3) | 27 (8.2) | |
| Income | .078 | ||
| < $25,000 | 378 (51.8) | 148 (59.4) | |
| $25,000 to < $50,000 | 195 (26.7) | 61 (24.5) | |
| ≥$50,000 | 157 (21.5) | 40 (16.1) |
Note: Older adults (≥60 years) compared to younger adults (<60 years) P-values based on chi-square analyses. Age-group comparison of race compared groups: White/Caucasian, Black/African American, Other race
Age-Group Differences in Quitting History, Cessation Predictors, and Outcomes
T-tests indicated age group differences in nicotine dependence (p=.04), such that older adults who smoked cigarettes were less dependent (M=2.55, SD=1.54) than younger adults (M=2.76, SD=1.47) (Table 2). Older adults were less motivated to quit cigarettes (M=5.77; SD=3.87 vs. M=6.47; SD=3.58; p=.004) and less likely to have made a quit attempt in the past year (31.0% vs. 36.8%) ([χ2 (1) = 3.86, p=.05] compared to those younger. Quitting self-efficacy, cigarettes per day, and prevalence of NRT use did not differ by age (Table 2). After controlling for treatment, age group was not associated with likelihood of quit attempt (p=.21; 43.6% for older vs. 39.8% for younger) nor cessation (p=0.92; 9.5% for older vs. 9.9% for younger).
Table 2.
Age Group Differences in Quitting History, Cessation Predictors and Outcomes
| Younger Adults (N=917) | Older Adults (N=328) | p | |
|---|---|---|---|
| Baseline Variables | M (SD) | M (SD) | |
| Nicotine Dependence | 2.76 (1.47) | 2.55 (1.54) | .04 |
| Motivation to Quit | 6.47 (3.58) | 5.77 (3.87) | .004 |
| Quitting Self-Efficacy | 5.93 (3.34) | 5.74 (3.40) | .38 |
| Cigarettes Per Day | 15.12 (9.03) | 15.25 (8.83) | .82 |
| n (%) | n (%) | ||
| Past Year Quit Attempt | 337 (36.8) | 101 (31.0) | .05 |
| NRT Use During Last Quit Attempt | 193 (22.2) | 73 (21.0) | .65 |
| Six-Month Follow-Up Outcomes | n (%) | n (%) | |
| Any Quit Attempt | 365 (39.8) | 143 (43.6) | .21 |
| Cessation | 91 (9.9) | 31 (9.5) | .92 |
Note: Analyses based on independent t-tests, chi-square analyses, and logistic regressions; Bolded significant p-values (p<.05) Analyses for cessation outcomes controlled for treatment assignment; NRT= nicotine replacement therapy
Final Models Predicting Cessation Outcomes
Interactions of age group and treatment group in relationship to any 24-hour quit attempt and six-month cessation were non-significant (p>.05’s). Given age-group differences in certain sociodemographic characteristics (i.e., education, employment status, insurance status), a sensitivity analysis was conducted adjusting for these covariates in both final models. No difference in effects were observed and therefore simpler models are subsequently presented for clarity.
In the final model predicting incidence of any quit attempt, there was an interaction of age group by motivation to quit (p=.025) (Figure 1). Specifically, among those who reported lowest motivation (i.e., those reporting 0 out of 10), older adults were more than twice as likely to attempt to quit than younger adults (OR=2.17; 95% CI: 1.29 to 3.64). Yet, among those who reported highest motivation (i.e., 10 out of 10), older adults were about equally likely to make a quit attempt compared to those younger (OR=0.96; 95% CI: 0.66 to 1.40). There was a trend in the interaction of age group by nicotine dependence (p=.057). Specifically, among those who scored lowest in dependence (i.e., scored 0 out of 6), older adults were almost two times more likely to attempt to quit compared to younger adults (OR=1.77; 95% CI: 1.06 to 2.96). For those who scored highest (i.e., 6 out of 6), older adults were less likely to make a quit attempt compared to those younger (OR=0.64; 95% CI: 0.33 to 1.24). Age group did not interact with self-efficacy (p=.278).
In the final model predicting cessation, interaction of age group by motivation was observed (p=.020) (Figure 2). Specifically, for those lowest in motivation (i.e., reporting 0 out of 10), older adults were three times more likely to quit compared to younger adults (OR=3.01; 95% CI: 1.14 to 7.94). For those who scored highest (i.e., 10 out of 10), older adults were less likely to quit compared to those younger (OR=0.68; 95% CI: 0.37 to 1.23). There was a trend in the interaction of age group by nicotine dependence (p=.067). For those scoring lowest in dependence (i.e., scored 0 out of 6), older adults were almost two times more likely to quit (OR=1.77; 95% CI: 0.82 to 3.83). However, among those who scored highest (i.e., 6 out of 6), older adults were less likely to quit compared to those younger (OR=0.34; 95% CI: 0.10 to 1.15). Age group and self-efficacy did not interact (p=.246).
Discussion
Among a discrete group of older adults (≥60 years) who smoke cigarettes (vs. younger), known predictors of quitting (motivation to quit, nicotine dependence, and quitting self-efficacy) were differentially related to cessation outcomes within a pragmatic primary care cessation trial. For those with initially low levels of nicotine dependence, older adults were more likely to make a quit attempt and be quit at six-months after standard cessation care compared to their younger counterparts. Yet, for adults with moderate to high levels of dependence, older age predicted less successful quit outcomes. Among participants initially not motivated to quit, older adults were more likely to make a quit attempt and be quit at six-months after advice to quit compared to younger adults. Yet, for those with initially stronger motivation, older adults were about equally likely to make a quit attempt and less likely to be quit at six-months compared to those younger. Results suggest differences between younger and older adults in how key factors predict cessation behaviors following advice to quit.
In previous studies, higher nicotine dependence negatively impacted outcomes among older adults receiving cessation treatment (Hsu et al., 2018; Tait et al., 2007). In this study, nicotine dependence was a stronger cessation barrier following advice to quit for older adults with high dependence compared to those who were younger with high dependence. Given the burden of tobacco morbidity and mortality among older adults who smoke cigarettes and among heavily nicotine dependent adults of all ages, older adults who are more dependent (e.g., smoke heavily) might need more intensive and tailored cessation intervention (Rojewski et al., 2018; Warren et al., 2014). Generally, older adults who smoke cigarettes are less likely to access cessation resources compared to younger adults (Huddlestone et al., 2015; Kaufman et al., 2010; Kulak et al., 2018). For example, older adults have the lowest awareness of tobacco cessation quit lines or websites (31.2%) compared to other age groups (41-54%) and are less likely to access quit lines compared to those in mid-life (Kaufman et al., 2010). Notably, Medicare does not cover the cost of over-the-counter NRT (Medicare.gov, 2022). Although Medicare does cover alternative pharmacotherapy (i.e., bupropion, varenicline), beneficiaries still need to obtain a prescription and cover potential co-payments for these medications (Medicare.gov, 2022). Thus, older adults might have multiple financial and logistical barriers that make it challenging to access cessation pharmacotherapy. Findings also highlight concern about the lack of high-quality (i.e., randomized, controlled) treatment trials specifically among older adults who smoke cigarettes (Cawkwell et al., 2015). For adults of all ages, pharmacotherapies are known to be beneficial for quitting among those heavily nicotine dependent (Cawkwell et al., 2015; Lindson et al., 2019). Although varenicline and bupropion have been deemed safe for use in older adulthood (Cawkwell et al., 2015; Lindson et al., 2019), the effectiveness of these medications in this population is understudied, with no placebo-controlled trials conducted within exclusively older adult samples (Cawkwell et al., 2015; Lindson et al., 2019; McAfee et al., 2021). Brief screening for nicotine dependence could be an efficient way to identify older adults who need more intensive cessation intervention and extra support accessing appropriate resources.
Although motivation is a known predictor of quitting among adults of all ages (Hyland et al. 2006), older adults with initially low motivation to quit experienced cessation success even more so than younger adults with low motivation. Provision of standard cessation advice for older adults who smoke cigarettes but not motivated to quit may still perhaps increase quitting. This is consistent with research in which brief cessation treatment and NRT medication sampling increased likelihood of quitting behaviors regardless of initial motivation among adults (Burris et al. 2015; Jardin et al. 2014). Yet, older adults who smoke are less likely to receive advice to quit from medical providers and less likely to be referred to counseling or prescribed NRT compared to younger adults (Huddlestone et al., 2015; Kaufman et al., 2010; Kulak et al., 2018). Lack of cessation advice and referrals for older adults might be attributed to the widely held misperception that quitting smoking is less beneficial in older age (McAfee et al., 2021). Findings emphasize the importance of providing cessation care to older smokers in medical settings regardless of their initial motivation to quit.
After controlling for treatment type, older adults did not differ in quit success (attempts or cessation) at six-months from those younger. This finding is consistent with previous research indicating older adults within cessation trials are similarly successful in quit outcomes compared to younger age groups (Chen & Wu, 2015). Treatment type (i.e., standard advice to quit vs. standard advice to quit plus NRT sampling) did not interact with age group in relationship to outcomes, suggesting both age groups were similarly impacted by the type of treatment.
This study utilized a secondary analysis of a larger parent study and future studies should replicate findings within larger samples of older adults who smoke cigarettes. Because older adults are generally less likely to access cessation resources (Huddlestone et al., 2015; Kaufman et al., 2010; Kulak et al., 2018), it is possible that older adults were less aware of NRT than younger adults in this study. However, at baseline, older adults reported using NRT at a comparable rate during their last quit attempt compared to those younger and were similarly impacted by the NRT sampling treatment regarding quit outcomes. Although there is some evidence that the six-item Fagerstrom Test for Nicotine Dependence has better psychometric properties among those with lighter cigarette use (Pérez-Ríos et al., 2009), the Heaviness of Smoking Index is a widely used reliable measure of nicotine dependence (Borland et al., 2010). Despite these limitations, this study used secondary analysis of a large pragmatic clinical trial to explore the understudied and important topic of tobacco cessation in older age.
Conclusion
Well-known predictors of quit success were differentially associated with quitting in older age (≥60 years) after receiving standard cessation care in primary care. Although older adults in this sample were less nicotine dependent than those younger overall, older adults with high nicotine dependence were less likely to make a quit attempt or successfully quit compared to their younger counterparts. Nicotine dependence could be an important consideration in cessation treatment with older populations; such that older adults with higher dependence might need more intensive treatment including proactive approaches to ensure ease of access to nicotine replacement therapy or other cessation pharmacotherapy. Following standard cessation advice, older adults attempted to quit and succeeded at a similar rate as those younger. Further, older adults unmotivated to quit were more likely to quit compared to unmotivated younger adults.
What this paper adds:
Older adults are disproportionally impacted by tobacco morbidity and mortality, less interested and less likely to attempt quitting smoking, but underrepresented in the cessation literature.
This study uniquely examines how well-known predictors of quitting impact cessation outcomes differentially in older compared to younger age groups.
Findings provide age-group considerations in the provision of standard advice to quit.
Applications of study findings:
Older adults who smoked cigarettes were differentially impacted by well-known predictors of quitting than younger adults within the context of standard cessation advice in primary care.
Older adults with high nicotine dependence might need additional support and more intensive intervention when quitting, even more so than younger adults with high dependence.
Older adults with initially low motivation to quit had more successful outcomes than unmotivated younger adults. Findings underscore the importance of providing cessation support to older adults, regardless of initial motivation to quit.
Funding
Funding for this research was provided by National Institute on Drug Abuse (R01 DA021619), (K23 DA045766), (T32 DA007288). Clinical Trials registration number NCT02096029.
Footnotes
Declaration of Conflicting Interests
Authors declare no conflicts of interest.
IRB Number
Medical University of South Carolina Institutional Review Board Approval Number: Pro00019201
References
- Adams JM (2020). Smoking Cessation-Progress, Barriers, and New Opportunities: The Surgeon General's Report on Smoking Cessation. JAMA, 323(24), 2470–2471. 10.1001/jama.2020.6647 [DOI] [PubMed] [Google Scholar]
- Alzheimer’s Association. (2022). Alzheimer’s Disease Facts and Figures. Alzheimers Dement; 2022;18. https://www.alz.org/media/documents/alzheimers-facts-and-figures.pdf [DOI] [PubMed] [Google Scholar]
- Arancini L, Borland R, Le Grande M, Mohebbi M, Dodd S, Dean OM, … & Cummings KM (2021). Age as a predictor of quit attempts and quit success in smoking cessation: findings from the International Tobacco Control Four-Country survey (2002–14). Addiction, 116(9), 2509–2520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Babb S, Malarcher A, Schauer G, Asman K, & Jamal A (2017). Quitting smoking among adults—United States, 2000–2015. Morbidity and Mortality Weekly Report, 65(52), 1457–1464. [DOI] [PubMed] [Google Scholar]
- Baumgart M, Snyder HM, Carrillo MC, Fazio S, Kim H, & Johns H (2015). Summary of the evidence on modifiable risk factors for cognitive decline and dementia: a population-based perspective. Alzheimer's & Dementia, 11(6), 718–726. [DOI] [PubMed] [Google Scholar]
- Borland R, Yong HH, O'Connor RJ, Hyland A, & Thompson ME (2010). The reliability and predictive validity of the Heaviness of Smoking Index and its two components: findings from the International Tobacco Control Four Country study. Nicotine & Tobacco Research, 12 (suppl_1), S45–S50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burris JL, Heckman BW, Mathew AR, & Carpenter MJ (2015). A mechanistic test of nicotine replacement therapy sampling for smoking cessation induction. Psychology of Addictive Behaviors, 29(2), 392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carpenter MJ, Wahlquist AE, Dahne J, Gray KM, Garrett-Mayer E, Cummings KM, Davis R & Egan BM (2020). Nicotine replacement therapy sampling for smoking cessation within primary care: results from a pragmatic cluster randomized clinical trial. Addiction, 115(7), 1358–1367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cawkwell PB, Blaum C, & Sherman SE (2015). Pharmacological smoking cessation therapies in older adults: a review of the evidence. Drugs & Aging, 32(6), 443–451. [DOI] [PubMed] [Google Scholar]
- Chen D, & Wu LT (2015). Smoking cessation interventions for adults aged 50 or older: a systematic review and meta-analysis. Drug and Alcohol Dependence, 154, 14–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen-Mansfield J (2016). Predictors of smoking cessation in old–old age. Nicotine & Tobacco Research, 18(7), 1675–1679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cornelius ME, Loretan CG, Wang TW, Jamal A, & Homa DM (2022). Tobacco product use among adults—United States, 2020. Morbidity and Mortality Weekly Report, 71(11), 397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dahlhamer J, Lucas J, Zelaya C, Nahin R, Mackey S, DeBar L, … & Helmick C (2018). Prevalence of chronic pain and high-impact chronic pain among adults—United States, 2016. Morbidity and Mortality Weekly Report, 67(36), 1001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dahne J, Wahlquist AE, Boatright AS, Garrett-Mayer E, Fleming DO, Davis R, Egan B & Carpenter MJ (2018). Nicotine replacement therapy sampling via primary care: methods from a pragmatic cluster randomized clinical trial. Contemporary Clinical Trials, 72, 1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donze J, Ruffieux C, & Cornuz J (2007). Determinants of smoking and cessation in older women. Age and Ageing, 36(1), 53–57. [DOI] [PubMed] [Google Scholar]
- Durazzo TC, Mattsson N, Weiner MW, & Alzheimer's Disease Neuroimaging Initiative. (2014). Smoking and increased Alzheimer's disease risk: a review of potential mechanisms. Alzheimer's & Dementia, 10, S122–S145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heatherton TF, Kozlowski LT, Frecker RC, Rickert W, & Robinson J (1989). Measuring the heaviness of smoking: using self-reported time to the first cigarette of the day and number of cigarettes smoked per day. British journal of addiction, 84(7), 791–800. [DOI] [PubMed] [Google Scholar]
- Henley SJ, Asman K, Momin B, Gallaway MS, Culp MB, Ragan KR, Richards TB & Babb S (2019). Smoking cessation behaviors among older US adults. Preventive Medicine Reports, 16, 100978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hsu CL, Hsueh KC, Chou MY, Yu HC, Mar GY, Chen HJ, & West R (2018). Long-term smoking cessation rates in elderly versus other adult smokers: A 3-year follow-up study in Taiwan. Addictive Behaviors Reports, 8, 62–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes JR, Keely JP, Niaura RS, Ossip-Klein DJ, Richmond RL, & Swan GE (2003). Measures of abstinence in clinical trials: issues and recommendations. Nicotine & Tobacco Research, 5(1), 13–25. [PubMed] [Google Scholar]
- Huddlestone L, Walker GM, Hussain-Mills R, & Ratschen E (2015). Treating tobacco dependence in older adults: a survey of primary care clinicians’ knowledge, attitudes, and practice. BMC family practice, 16(1), 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hyland A, Borland R, Li Q, Yong HH, McNeill A, Fong GT, O’Connor RJ & Cummings KM (2006). Individual-level predictors of cessation behaviours among participants in the International Tobacco Control (ITC) Four Country Survey. Tobacco control, 15(suppl 3), iii83–iii94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Isenberg JY, Quiñones AR, Slatore CG, Bryson WC, & Thielke SM (2016). Trends in cigarette smoking and cessation among Medicare managed care recipients, 2005–2012. Addictive Behaviors, 58, 155–160. [DOI] [PubMed] [Google Scholar]
- Jardin BF, Cropsey KL, Wahlquist AE, Gray KM, Silvestri GA, Cummings KM, & M. J. (2014). Evaluating the effect of access to free medication to quit smoking: a clinical trial testing the role of motivation. Nicotine Tob Res, 16(7), 992–999. 10.1093/ntr/ntu025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaufman A, Augustson E, Davis KIA, & Finney Rutten LJ (2010). Awareness and use of tobacco quitlines: evidence from the Health Information National Trends Survey. Journal of Health Communication, 15(sup3), 264–278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kleykamp BA, & Heishman SJ (2011). The older smoker. Jama, 306(8), 876–877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kleykamp BA, & Kulak JA (2022). Cigarette Use Among Older Adults: A Forgotten Population. American Journal of Public Health, (0), e1–e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kulak JA, & LaValley S (2018). Cigarette use and smoking beliefs among older Americans: findings from a nationally representative survey. Journal of Addictive Diseases, 37(1-2), 46–54. [DOI] [PubMed] [Google Scholar]
- Lindson N, Chepkin SC, Ye W, Fanshawe TR, Bullen C, & Hartmann-Boyce J (2019). Different doses, durations and modes of delivery of nicotine replacement therapy for smoking cessation. Cochrane Database of Systematic Reviews, (4). [DOI] [PMC free article] [PubMed] [Google Scholar]
- McAfee T, Malone RE, & Cataldo J (2021). Ignoring our elders: tobacco control’s forgotten health equity issue. Tobacco Control, 30(5), 479–480. [DOI] [PubMed] [Google Scholar]
- Medicare.gov. (2022, July 20). Counseling to prevent tobacco use & tobacco-caused disease. https://www.medicare.gov/coverage/counseling-to-prevent-tobacco-use-tobacco-caused-disease#:~:text=Counseling%20to%20prevent%20tobacco%20use%20%26%20tobacco%2Dcaused%20disease
- Ortman JM, Velkoff VA, & Hogan H (2014). An aging nation: The older population in the United States, current population reports, P25-1140. Washington, DC: US Census Bureau. [Google Scholar]
- Pérez-Ríos M, Santiago-Pérez MI, Alonso B, Malvar A, Hervada X, & de Leon J (2009). Fagerstrom test for nicotine dependence vs heavy smoking index in a general population survey. BMC public health, 9(1), 1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rimer BK, Orleans CT, Keintz MK, Cristinzio S, & Fleisher L (1990). The older smoker: status, challenges and opportunities for intervention. Chest, 97(3), 547–553 [DOI] [PubMed] [Google Scholar]
- Rojewski AM, Tanner NT, Dai L, Ravenel JG, Gebregziabher M, Silvestri GA, & Toll BA (2018). Tobacco dependence predicts higher lung cancer and mortality rates and lower rates of smoking cessation in the National Lung Screening Trial. Chest, 154(1), 110–118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration (2020). Treating substance use disorder in older adults. Treatment Improvement Protocol (TIP 26). [PubMed] [Google Scholar]
- Tait RJ, Hulse GK, Waterreus A, Flicker L, Lautenschlager NT, Jamrozik K, & Almeida OP (2007). Effectiveness of a smoking cessation intervention in older adults. Addiction, 102(1), 148–155. [DOI] [PubMed] [Google Scholar]
- Warren GW, Alberg AJ, Kraft AS, & Cummings KM (2014). The 2014 Surgeon General's report:“The Health Consequences of Smoking–50 Years of Progress”: a paradigm shift in cancer care. Cancer, 120(13), 1914–1916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization (2019, March 29). Ageing. https://www.who.int/health-topics/ageing#tab=tab_1.