Abstract
目的
探究室内总挥发性有机物(total volatile organic compounds,TVOC)短期暴露与年轻女性夜间心率变异性(heart rate variability,HRV)的关联。
方法
采用定组研究设计,于2021年12月至2022年4月期间对北京市某高校50名年轻女性进行两次重复调查。每次调查期间,使用室内空气质量检测仪对研究对象室内TVOC浓度进行实时监测。室内温湿度、噪声、二氧化碳和颗粒物浓度分别采用温湿度仪、噪声监测仪、二氧化碳仪及多通道颗粒物监测仪进行实时监测,并采用12导联动态心电图仪测量HRV指标。采用混合效应模型分析TVOC与HRV指标的关联及暴露-反应关系,并使用双污染物模型检验结果的稳定性。
结果
50名女性的平均年龄为(22.5±2.3)岁,平均体重指数为(20.4±1.9) kg/m2。研究期间室内TVOC浓度的中位数(四分位间距)为0.069(0.046) mg/m3,室内温度、相对湿度、二氧化碳浓度、噪声水平及细颗粒物浓度的中位数(四分位间距)分别为24.3(2.7) ℃、38.5%(15.0%)、0.1%(0.1%)、52.7(5.8) dB(A)及10.3(21.5) μg/m3。室内TVOC短期暴露与研究对象HRV的时域及频域指标改变显著相关,且多数HRV指标发生最显著改变的暴露时间窗为1 h。室内TVOC的1 h滑动平均浓度每增加0.01 mg/m3,研究对象心跳间期标准偏差(standard deviation of all normal to normal intervals,SDNN)、连续5 min心跳间期平均标准偏差(standard deviation of average normal to normal intervals,SDANN)及相邻心跳差值超过50 ms与总正常心跳间距个数比值(percentage of adjacent normal to normal intervals differing by more than 50 ms,pNN50)分别降低1.89%(95%CI:-2.28%~-1.50%)、1.92%(95%CI:-2.32%~-1.51%)及0.64%(95%CI:-1.13%~-0.14%),而总功率(total power,TP)、极低频功率(very low frequency power,VLF)及低频功率(low frequency power,LF)分别降低3.52%(95%CI:-4.30%~-2.74%)、5.01%(95%CI:-6.21%~-3.79%)及4.36%(95%CI:-5.16%~-3.55%)。暴露-反应关系曲线显示,当浓度超过0.1 mg/m3时,室内TVOC与SDNN、SDANN、TP、VLF线性负相关。双污染物模型提示,在控制室内噪声及细颗粒物因素后上述结果稳健。
结论
室内TVOC短期暴露与年轻女性的夜间HRV改变存在负相关,本研究为相关防控措施提供了重要的科学依据。
Keywords: 空气污染,室内, 挥发性有机化合物, 心率变异性, 女性, 定组研究
Abstract
Objective
To investigate the association between short-term exposure to indoor total volatile organic compounds (TVOC) and nocturnal heart rate variability (HRV) among young female adults.
Methods
This panel study recruited 50 young females from one university in Beijing, China from December 2021 to April 2022. All the participants underwent two sequential visits. During each visit, real time indoor TVOC concentration was monitored using an indoor air quality detector. The real time levels of indoor temperature, relative humidity, noise, carbon dioxide and fine particulate matter were monitored using a temperature and humidity meter, a noise meter, a carbon dioxide meter and a particulate counter, respectively. HRV parameters were measured using a 12-lead Holter. Mixed-effects models were used to evaluate the association between the TVOC and HRV parameters and establish the exposure-response relationships, and two-pollutant models were applied to examine the robustness of the results.
Results
The mean age of the 50 female subjects was (22.5±2.3) years, and the mean body mass index was (20.4±1.9) kg/m2. During this study, the median (interquartile range) of indoor TVOC concentrations was 0.069 (0.046) mg/m3, the median (interquartile range) of indoor temperature, relative humidity, carbon dioxide concentration, noise level and fine particulate matter concentration were 24.3 (2.7) ℃, 38.5% (15.0%), 0.1% (0.1%), 52.7 (5.8) dB(A) and 10.3 (21.5) μg/m3, respectively. Short-term exposure to indoor TVOC was associated with significant changes in time-domain and frequency-domain HRV parameters, and the exposure metric for most HRV parameters with the most significant changes was 1 h-moving average. Along with a 0.01 mg/m3 increment in 1 h-moving average concentration of indoor TVOC, this study observed decreases of 1.89% (95%CI: -2.28%, -1.50%) in standard deviation of all normal to normal intervals (SDNN), 1.92% (95%CI: -2.32%, -1.51%) in standard deviation of average normal to normal intervals (SDANN), 0.64% (95%CI: -1.13%, -0.14%) in percentage of adjacent NN intervals differing by more than 50 ms (pNN50), 3.52% (95%CI: -4.30%, -2.74%) in total power (TP), 5.01% (95%CI: -6.21%, -3.79%) in very low frequency (VLF) power, and 4.36% (95%CI: -5.16%, -3.55%) in low frequency (LF) power. The exposure-response curves showed that indoor TVOC was negatively correlated with SDNN, SDANN, TP, and VLF when the concentration exceeded 0.1 mg/m3. The two-pollutant models indicated that the results were generally robust after controlling indoor noise and fine particulate matter.
Conclusion
Short-term exposure to indoor TVOC was associated with significant negative changes in nocturnal HRV of young women. This study provides an important scientific basis for relevant prevention and control measures.
Keywords: Air pollution, indoor; Volatile organic compounds; Heart rate variability; Female; Panel study
人的一生80%以上的时间是在室内度过的[1],因此,室内环境与人群健康密切相关。挥发性有机物是近年我国城镇建筑中最常见且受到广泛关注的室内污染物,其主要来源于室内建筑材料、护理产品、装修装饰材料、燃料燃烧释放以及室外挥发性有机物的渗透等[2-3]。挥发性有机物在常温下即可挥发,通过呼吸道吸入等途径对健康造成不良影响[2]。
心率变异性(heart rate variability,HRV)是连续心跳间隔时间的变化特征,可反映心脏自主神经系统(autonomic nervous system,ANS)响应外界刺激以适应环境变化的能力[4-5]。有研究指出夜间HRV指标(总功率、低频和低频/高频比)与女性睡眠质量呈负相关[6]。年轻群体中,许多HRV指标对性别存在普遍依赖性,女性中一些HRV指标相较男生更低[7]。
既往研究表明,总挥发性有机物(total volatile organic compounds,TVOC)短期暴露与HRV改变显著相关,Ma等[8]在我国台北开展的研究发现,短期TVOC职业暴露与HRV降低存在关联,在我国北京和日本的研究也有相似结果[9-10]。然而,国内外有关TVOC与HRV关联的报道较为有限,且相关结果因研究环境、研究设计、人群特征等差异并不一致[9, 11-12]。此外,既往研究主要关注职业暴露和交通污染,很少关注人群夜间睡眠期间HRV的变化及其对环境因素的易感性。本研究旨在探索室内TVOC与年轻女性夜间HRV的关联,从而为室内环境对女性心脏自主神经功能的影响及相关防控措施提供科学依据。
1. 资料与方法
1.1. 研究设计与研究对象的选取
采用定组研究设计[13],于2021年11月至2022年4月期间,招募北京市某高校在读的年轻女性作为研究对象。研究的纳入标准为:(1)年龄在18~28周岁;(2)体重指数(body mass index,BMI) < 28 kg/m2;(3)在北京居住至少1年;(4)身体健康。排除标准为:(1)有吸烟、饮酒史者;(2)有胸部创伤或手术史者;(3)患有呼吸系统、心血管系统相关慢性疾病或服用能够影响心率药物者;(4)临床诊断为睡眠障碍、抑郁、焦虑等其他神经精神性疾病者;(5)正在参与其他药物临床试验或干预性研究的受试者;(6)不能配合研究实施,或不愿签署知情同意书的受试者。本研究已通过北京大学生物医学伦理委员会审批(批准号:IRB00001052-21109),所有研究对象均在研究正式开始前签署知情同意书。
以宿舍为单位对研究对象进行两次调查,于每次调查期间(均为周日晚至周一早)监测研究对象睡眠期间的室内环境中TVOC、温湿度、噪声、二氧化碳(carbon dioxide,CO2)和颗粒物等环境因素暴露水平及HRV指标。
1.2. 室内环境监测
采用室内空气质量检测仪(美国GrayWolf公司)对研究对象睡眠期间室内TVOC浓度进行实时监测[14],测量时间为周日晚22点至下周一凌晨6点,地点为研究对象所在宿舍。室内温湿度、噪声、二氧化碳和颗粒物浓度分别采用温湿度仪(WSZY-1B,北京天建华仪公司)、噪声监测仪(ASV5910+,杭州爱华公司)、二氧化碳仪(WEZY-1B,北京天建华仪公司)及多通道颗粒物监测仪(Handheld PC3016,美国GrayWolf公司)进行实时监测。研究选取每次HRV记录前的5、10、15、30 min及1、2、3 h作为室内TVOC的暴露时间窗,并计算时间窗内各环境因素的滑动平均值作为环境暴露水平。
1.3. 心率变异性监测
采用12导联动态心电图仪(型号MGY-H12,美国DM Software公司)监测研究对象睡眠期间的HRV水平,测量记录间隔为5 min,测量时间为周日晚22点至下周一凌晨6点,地点为研究对象所在宿舍。本研究收集的主要指标为4种时域指标,包括心跳间期标准偏差(standard deviation of all normal to normal intervals,SDNN)、连续5 min心跳间期平均标准偏差(standard deviation of average normal to normal intervals,SDANN)、相邻正常心跳间期差值平方和的均方根(square root of the mean squared dif-ferences of successive normal to normal intervals,rMSSD)、相邻心跳差值超过50 ms与总正常心跳间距个数比值(percentage of adjacent normal to normal intervals differing by more than 50 ms,pNN50),以及4种频域指标,包括总功率(total power,TP)、极低频功率(very low frequency power,VLF)、低频功率(low frequency power,LF)、高频功率(high frequency po-wer,HF)。为了控制混杂,在基线调查时,使用中文版匹兹堡睡眠质量指数(Pittsburgh sleep quality index,PSQI)量表评估研究对象长期睡眠状况。PSQI问卷包含18个自评条目,总分范围为0~21分,得分越高提示总体睡眠质量越差,以PSQI量表得分表示睡眠状况。每次HRV测量前,采用14条目中文版压力知觉量表(perceived stress scale,PSS)评估研究对象近1周心理压力水平。PSS量表总分范围为0~56分,得分越高提示压力水平越高,以PSS量表得分表示心理压力水平。采用自填式问卷收集研究对象的宿舍编号、年龄、身高、体质量、体力活动情况和是否有饮用咖啡习惯等信息,体力活动参考既往研究分为低水平活动、轻度活动和中度或高水平活动三组[15],低水平活动指轻度体力活动 < 2 h/周,轻度活动指轻度体力活动2~4 h/周,中度或高水平活动指轻度体力活动超过4 h/周或剧烈活动超过2 h/周。是否有饮用咖啡习惯以从不饮用或饮用频率低于1次/月定义为“否”,反之为“是”。
1.4. 统计分析方法
使用R 3.6.3软件,主要使用nlme包进行统计学分析。根据既往文献,将HRV指标进行对数转换以改善分布的正态性[16]。建立线性混合效应模型评估室内TVOC暴露与研究对象HRV的关联。模型的随机效应项为每位研究对象的截距项,固定效应项为研究对象所在宿舍(宿舍编号)、年龄、BMI、动态心率、体力活动情况水平(低水平活动/轻度活动/中度或高水平活动)、饮用咖啡习惯(是/否)、睡眠状况、心理压力水平等混杂因素。为控制室内其他环境因素的潜在混杂,模型纳入同暴露时间窗的温度、相对湿度及二氧化碳浓度的滑动平均值。此外,模型纳入季节(供暖季:12~2月;非供暖季:3~4月)、研究日序及研究日序的平方项,以控制季节因素及长期趋势的潜在混杂[17]。
为进一步评估室内不同浓度TVOC暴露与上述主效应具有统计学意义的HRV指标的关联,研究将线性混合效应模型中TVOC的线性效应项替换为自然样条函数(自由度=3)平滑项,以刻画室内TVOC与HRV指标的暴露-反应关系[18]。此外,研究通过建立双污染物模型,即在线性混合效应模型中进一步纳入同时间窗的噪声及细颗粒物(fine particulate matter,PM2.5)水平,以评估TVOC与HRV关联的稳健性。
本研究线性混合效应模型的结果表示为室内TVOC每增加0.01 mg/m3,相应HRV指标的百分比变化及95%置信区间(confidence interval,CI),检验水准为α=0.05。
2. 结果
2.1. 研究对象的基本特征
研究共纳入50名女性作为研究对象,研究对象均完成两次随访,共7 713次HRV监测结果,平均年龄为(22.5±2.3)岁,平均BMI为(20.4±1.9) kg/m2。体力活动水平为较少活动、低水平活动和中等及高水平活动的人数分别为12(24.0%)、22(44.0%)及16(32.0%)人;具有饮用咖啡习惯的人数为22(44.0%)人。研究对象的平均睡眠PSQI为4.9±2.1,压力PSS量表两次随访得分分别为23.1±7.6和23.6±8.5。
2.2. 研究对象的室内环境暴露水平
如表 1所示,研究期间室内TVOC浓度的中位数(四分位间距)为0.069(0.046) mg/m3。此外,研究期间室内温度、相对湿度、二氧化碳浓度、噪声水平及PM2.5浓度的中位数(四分位间距)分别为24.3(2.7) ℃、38.5%(15.0%)、0.1%(0.1%)、52.7(5.8) dB(A)及10.3(21.5) μg/m3。
表 1.
研究期间研究对象所处室内环境污染物监测结果
The monitoring results of indoor environmental pollutants of the study subjects during the research period
| Indicator | First visit | Second visit | All |
| Data are expressed as median (interquartile range). TVOC, total volatile organic compounds; PM2.5, fine particulate matter; CO2, carbon dioxide. | |||
| TVOC/(×10-2 mg/m3) | 7.8 (10.1) | 6.9 (4.4) | 6.9 (4.6) |
| Noise/dB(A) | 52.8 (7.1) | 52.7 (5.2) | 52.7 (5.8) |
| PM2.5/(μg/m3) | 16.0 (25.9) | 4.24 (10.8) | 10.3 (21.5) |
| CO2/% | 0.1 (0.1) | 0.1 (0.1) | 0.1 (0.1) |
| Temperature/℃ | 25.0 (2.2) | 23.9 (2.7) | 24.3 (2.7) |
| Relative humidity/% | 38.2 (11.5) | 39.1 (17.1) | 38.5 (15.0) |
2.3. 研究对象的HRV指标分布
监测期间研究对象心率中位数(四分位间距)为62.0(11.0)次/min,SDNN及TP中位数(四分位间距)分别为65.0(43.0) ms及3 153.4(4 293.1) ms2。相关HRV指标的具体水平详见表 2。
表 2.
研究期间研究对象HRV各指标水平(n=50)
The level of HRV indicators of the research subjects during the research period (n=50)
| Indicator | First visit | Second visit | All |
| Data are expressed as median (interquartile range). SDNN, standard deviation of all normal to normal intervals; SDANN, standard deviation of average normal to normal intervals; rMSSD, square root of the mean squared differences of successive normal to normal intervals; pNN50, percentage of adjacent normal to normal intervals differing by more than 50 ms; TP, total power; VLF, very low frequency power; LF, low frequency power; HF, high frequency power. | |||
| Heart rate/(beats/min) | 62.0 (11.00) | 62.0 (12.0) | 62.0 (11.0) |
| SDNN/ms | 65.0 (42.0) | 64.0 (43.0) | 65.0 (43.0) |
| SDANN/ms | 64.0 (43.0) | 64.0 (43.0) | 64.0 (44.0) |
| rMSSD/ms | 31.0 (16.0) | 31.0 (16.0) | 31.0 (16.0) |
| pNN50/% | 35.0 (36.0) | 34.0 (38.0) | 34.0 (37.0) |
| TP/ms2 | 3 175.1 (4 355.6) | 3 136.5 (4 188.2) | 3 153.4 (4 293.1) |
| VLF/ms2 | 1 211.4 (2 857.7) | 1 196.5 (2 700.2) | 1 205.8 (2 785.7) |
| LF/ms2 | 639.1 (852.1) | 623.1 (915.1) | 633.0 (882.8) |
| HF/ms2 | 697.6 (901.9) | 649.9 (950.9) | 674.6 (928.3) |
2.4. 室内TVOC与HRV指标的关联
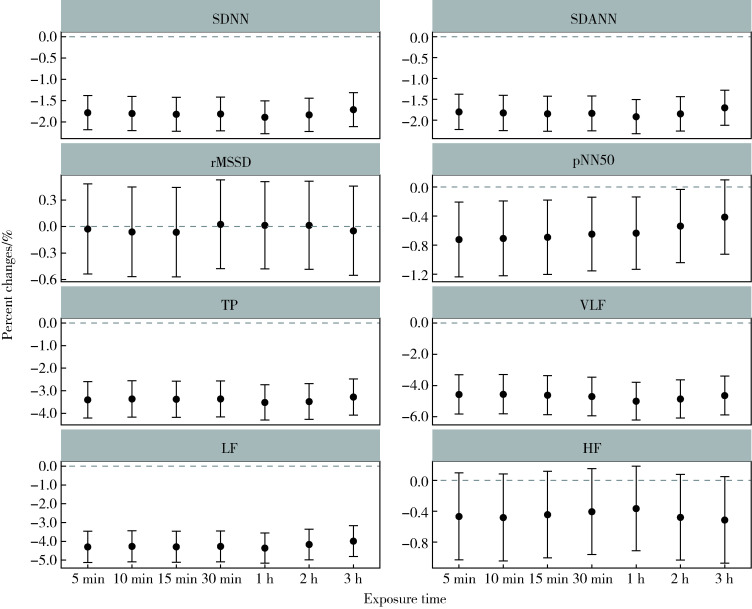
如图 1所示,室内TVOC短期暴露与研究对象HRV的时域及频域指标改变显著相关,且多数HRV指标发生最显著改变的暴露时间窗为1 h。室内TVOC的1 h滑动平均浓度每增加0.01 mg/m3,研究对象SDNN、SDANN及pNN50分别降低1.89%(95%CI:-2.28%~-1.50%)、1.92%(95%CI:-2.32%~-1.51%)及0.64%(95%CI:-1.13%~ -0.14%),而TP、VLF及LF分别降低3.52%(95%CI:-4.30%~-2.74%)、5.01%(95%CI:-6.21%~-3.79%)及4.36%(95%CI:-5.16%~ -3.55%)。室内TVOC暴露与rMSSD和HF的关联不具有统计学意义。
图 1.
室内TVOC每增加0.01 mg/m3与研究对象HRV指标百分比改变的关联及95%置信区间
Percent changes and 95% confidence intervals associated with a 0.01 mg/m3 increase in indoor TVOC exposure concentrations
TVOC, total volatile organic compounds; HRV, heart rate variability. Other abbreviations as in Table 2.
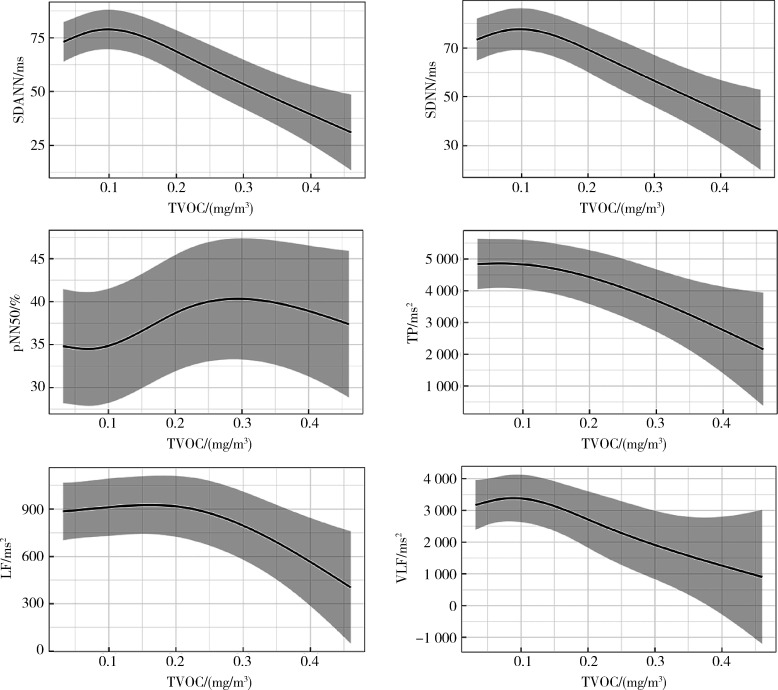
2.5. TVOC与HRV暴露-反应关系
为了进一步探索TVOC浓度变化和HRV指标改变潜在的非线性变化,将混合效应模型中的线性项改为限制性立方样条绘制暴露-反应关系曲线,如图 2所示,当浓度超过0.1 mg/m3时,室内TVOC与SDNN、SDANN、TP、VLF线性负相关。
图 2.
室内TVOC与研究对象HRV指标的暴露-反应曲线
Exposure-response curves for the associations between indoor TVOC and HRV of the study subjects
2.6. 双污染物模型
双污染物模型结果显示,在控制研究对象同时间窗噪声与PM2.5暴露后,上述主效应结果基本稳健(表 3)。
表 3.
室内TVOC的1 h滑动平均浓度每增加0.01 mg/m3与研究对象HRV指标百分比改变(95%置信区间)关联的双污染物模型结果
Percent changes (95% confidence intervals) associated with a 0.01 mg/m3 increase in 1 h moving average concentration of indoor TVOC in two-pollutant models
| Indicator | Main-effects model | Noise-two-pollutant model | PM2.5-two-pollutant model |
| Abbreviations as in Table 2 and Figure 1. | |||
| SDNN | -1.89% (-2.28%, -1.50%) | -1.88% (-2.36%, -1.41%) | -1.97% (-2.77%, -1.17%) |
| SDANN | -1.92% (-2.32%, -1.51%) | -1.85% (-2.35%, -1.34%) | -2.18% (-3.02%, -1.33%) |
| pNN50 | -0.64% (-1.13%, -0.14%) | -0.39% (-1.00%, 0.22%) | -1.49% (-2.46%, -0.51%) |
| TP | -3.52% (-4.30%, -2.74%) | -3.21% (-4.18%, -2.24%) | -4.14% (-5.75%, -2.50%) |
| VLF | -5.01% (-6.21%, -3.79%) | -4.18% (-5.68%, -2.65%) | -4.97% (-7.48%, -2.39%) |
| LF | -4.36% (-5.16%, -3.55%) | -3.63% (-4.63%, -2.62%) | -5.71% (-7.37%, -4.02%) |
3. 讨论
本研究采用定组研究设计,探讨年轻女性人群夜间TVOC与HRV的关联,每个研究对象都可作为自身前后指标比较的对照,无需设置对照组,可控制个体变异性对研究结果造成的潜在混杂,降低某些混杂因素影响[13]。我国《室内空气质量标准》(GB/T 18883—2022)中对室内TVOC的要求是8 h平均浓度不超过0.6 mg/m3,在我国8个城市开展的住宅调查发现TVOC浓度为0.10~1.15 mg/m3[19],在山西大同和上海住宅开展的研究发现TVOC浓度为0.22~1.72 mg/m3和0.37~1.59 mg/m3[20-21],本研究中TVOC浓度为0.03~0.46 mg/m3,较既往研究而言处于较低水平。本研究发现,低水平TVOC浓度暴露数分钟至数小时与年轻女性的HRV改变显著相关,具体指标表现为SDNN、SDANN、pNN50、TP、VLF及LF的降低,提示即使低于当前室内空气质量标准浓度的TVOC短期暴露也可能影响心脏自主神经功能。HRV可以反映交感神经系统和副交感神经系统的活动。不同HRV参数生理意义如下:TP和SDNN是HRV的全局指标,反映了整体自主神经活动;pNN50、HF、rMSSD与副交感神经密切相关[5];LF、SDNN和SDANN受交感与副交感神经活动影响;SDNN反映了长期循环差异和昼夜节律,较低的SDNN值表示较高的压力反应;VLF被认为与全因死亡率和其他疾病密切相关。
睡眠是一种与白天意识完全不同的生理状态,它构成了所有生物体的基本行为机制,是一个复杂的生物生理昼夜节律过程,与人体的许多日常身心功能直接和间接相关。大量证据表明睡眠对于维持身体健康以及良好的认知功能、记忆、情绪等至关重要[22]。此外,睡眠或睡眠相关机制对心血管系统施加调节控制,因为ANS的调节深受睡眠-觉醒周期的影响[23]。有研究表明,睡眠时间短、睡眠质量差和睡眠效率低与HF较低相关[24],睡眠质量差与HRV降低有显著关联[25]。
总体而言,目前国内外关于TVOC与HRV的研究结果并不一致。一项基于我国台湾地区300名20~65岁健康成年人的研究发现,室内TVOC短期暴露与人群SDNN的下降密切关联[11],与本研究结果一致。一项基于我国39名健康大学生的研究发现,地铁车厢内TVOC短期暴露仅与男性LF降低密切关联,而与女性的SDNN、LF及HF无关联[9]。同时,一项基于加拿大42名自行车手的交叉试验研究发现,骑行过程中的TVOC短期暴露与SDNN、rMSSD、pNN50、LF及HF均无关联[12]。
造成上述结果差异的因素可能包括研究暴露环境的不同、研究设计的差别以及人群间的异质性等[11-12]。本研究基于定组研究设计,使用实时监测设备对研究对象的室内环境暴露与HRV指标进行连续重复测量,在一定程度上可降低测量误差及个体变异性等信息偏倚。此外,既往研究发现,噪声与PM2.5是HRV重要的环境影响因素[16, 26], 而本研究在控制相关因素对TVOC与HRV关联的混杂后,仍观察到TVOC与HRV的负面关联,因此相关结果具有一定的稳健性。
本研究未观察到TVOC短期暴露与HF和rMSSD的关联。HF、rMSSD及pNN50主要反映副交感神经的活动状况。本研究发现,在睡眠状态下,主要受副交感神经影响的HF、rMSSD及pNN50指标与TVOC水平的关联变化不如预期结果,但仍观察到HF的变化趋势。
本研究存在如下局限性:(1)研究未对TVOC的具体成分进行测量,未来研究尚需进一步探索对人群健康影响较为严重的挥发性有机物;(2)研究未考虑日间及更早时间TVOC暴露的潜在影响。
综上,本研究结果揭示了一组年轻女性的TVOC暴露与夜间HRV之间的关联,提示即使低浓度的短期TVOC暴露仍可能会对年轻女性个体的心脏自主神经功能产生影响,研究结果可为室内环境污染对人群健康的影响及防控提供科学依据。
Funding Statement
国家重点研发计划(2022YFC3702704、2017YFC0702700)和国家自然科学基金(82073506)
Supported by the National Key Research and Development Program of China (2022YFC3702704, 2017YFC0702700) and the National Natural Science Foundation of China (82073506)
Contributor Information
邓 芙蓉 (Fu-rong DENG), Email: lotus321321@126.com.
郭 新彪 (Xin-biao GUO), Email: guoxb@bjmu.edu.cn.
References
- 1.Hulin M, Simoni M, Viegi G, et al. Respiratory health and indoor air pollutants based on quantitative exposure assessments. Eur Respir J. 2012;40(4):1033–1045. doi: 10.1183/09031936.00159011. [DOI] [PubMed] [Google Scholar]
- 2.Li B, Ho SSH, Li X, et al. A comprehensive review on anthropogenic volatile organic compounds (VOCs) emission estimates in China: Comparison and outlook. Environ Int. 2021;156:106710. doi: 10.1016/j.envint.2021.106710. [DOI] [PubMed] [Google Scholar]
- 3.梁 小明, 陈 来国, 沈 国锋, et al. 中国生活源挥发性有机物排放清单. 环境科学. 2021;42(11):5162–5168. doi: 10.13227/j.hjkx.202102007. [DOI] [PubMed] [Google Scholar]
- 4.Fang SC, Wu YL, Tsai PS. Heart rate variability and risk of all-cause death and cardiovascular events in patients with cardiovascular disease: A meta-analysis of cohort studies. Biol Res Nurs. 2020;22(1):45–56. doi: 10.1177/1099800419877442. [DOI] [PubMed] [Google Scholar]
- 5.Heart rate variability: Standards of measurement, physiological interpretation and clinical use. Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology [J]. Circulation, 1996, 93(5): 1043-1065.
- 6.Hsu HC, Lee HF, Lin MH. Exploring the association between sleep quality and heart rate variability among female nurses. Int J Environ Res Public Health. 2021;18(11):5551. doi: 10.3390/ijerph18115551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Voss A, Schroeder R, Heitmann A, et al. Short-term heart rate variability: Influence of gender and age in healthy subjects. PLoS One. 2015;10(3):e0118308. doi: 10.1371/journal.pone.0118308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ma CM, Lin LY, Chen HW, et al. Volatile organic compounds exposure and cardiovascular effects in hair salons. Occup Med (Lond) 2010;60(8):624–630. doi: 10.1093/occmed/kqq128. [DOI] [PubMed] [Google Scholar]
- 9.刘 雅倩, 张 文楼, 刘 琪, et al. 地铁车厢内挥发性有机物污染水平及对健康人群心电指标的影响. 首都公共卫生. 2020;14(1):13–15. doi: 10.16760/j.cnki.sdggws.2020.01.005. [DOI] [Google Scholar]
- 10.Mizukoshi A, Kumagai K, Yamamoto N, et al. A novel methodo-logy to evaluate health impacts caused by VOC exposures using real-time VOC and Holter monitors. Int J Environ Res Public Health. 2010;7(12):4127–4138. doi: 10.3390/ijerph7124127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lin LY, Chuang HC, Liu IJ, et al. Reducing indoor air pollution by air conditioning is associated with improvements in cardiovascular health among the general population. Sci Total Environ. 2013;(463/464):176–181. doi: 10.1016/j.scitotenv.2013.05.093. [DOI] [PubMed] [Google Scholar]
- 12.Weichenthal S, Kulka R, Dubeau A, et al. Traffic-related air pollution and acute changes in heart rate variability and respiratory function in urban cyclists. Environ Health Perspect. 2011;119(10):1373–1378. doi: 10.1289/ehp.1003321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.刘 越, 黄 婧, 郭 新彪, et al. 定组研究在我国空气污染流行病学研究中的应用. 环境与健康杂志. 2013;30(10):932–935. doi: 10.16241/j.cnki.1001-5914.2013.10.013. [DOI] [Google Scholar]
- 14.Koch S, Zelembaba A, Tran R, et al. Vascular effects of physical activity are not modified by short-term inhaled diesel exhaust: Results of a controlled human exposure study. Environ Res. 2020;183:109270. doi: 10.1016/j.envres.2020.109270. [DOI] [PubMed] [Google Scholar]
- 15.Joseph G, Marott JL, Torp-Pedersen C, et al. Dose-response association between level of physical activity and mortality in normal, elevated, and high blood pressure. Hypertension. 2019;74(6):1307–1315. doi: 10.1161/HYPERTENSIONAHA.119.13786. [DOI] [PubMed] [Google Scholar]
- 16.Wang W, Zhang W, Li L, et al. Associations between personal noise exposure and heart rate variability were modified by obesity and PM2.5: The study among obese and normal-weight adults (SONA) Environ Res. 2022;214(Pt 2):113888. doi: 10.1016/j.envres.2022.113888. [DOI] [PubMed] [Google Scholar]
- 17.Penttinen P, Timonen KL, Tiittanen P, et al. Number concentration and size of particles in urban air: Effects on spirometric lung function in adult asthmatic subjects. Environ Health Perspect. 2001;109(4):319–323. doi: 10.1289/ehp.01109319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Liu C, Chen R, Sera F, et al. Ambient particulate air pollution and daily mortality in 652 cities. N Engl J Med. 2019;381(8):705–715. doi: 10.1056/NEJMoa1817364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pei J, Yin Y, Liu J, et al. An eight-city study of volatile organic compounds in Chinese residences: Compounds, concentrations, and characteristics. Sci Total Environ. 2020;698:134137. doi: 10.1016/j.scitotenv.2019.134137. [DOI] [PubMed] [Google Scholar]
- 20.乔 俊, 许 琳, 张 桂枝, et al. 大同市室内空气质量及检测行业现状调查分析. 广州化工. 2017;45(17):129–131. [Google Scholar]
- 21.王 永姣, 束 亮亮, 姜 耀鹏. 上海市居民住宅室内空气质量调查. 建筑科技. 2020;4(4):93–98. [Google Scholar]
- 22.Ma Y, Hou F, Yang AC, et al. Symbolic dynamics of electroencephalography is associated with the sleep depth and overall sleep quality in healthy adults. Physica A: Statistical Mechanics and its Applications. 2019;513:22–31. doi: 10.1016/j.physa.2018.08.043. [DOI] [Google Scholar]
- 23.de Zambotti M, Trinder J, Silvani A, et al. Dynamic coupling between the central and autonomic nervous systems during sleep: A review. Neurosci Biobehav Rev. 2018;90:84–103. doi: 10.1016/j.neubiorev.2018.03.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Castro-Diehl C, Diez Roux AV, Redline S, et al. Sleep duration and quality in relation to autonomic nervous system measures: The multi-ethnic study of atherosclerosis (MESA) Sleep. 2016;39(11):1927–1940. doi: 10.5665/sleep.6218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jackowska M, Dockray S, Endrighi R, et al. Sleep problems and heart rate variability over the working day. J Sleep Res. 2012;21(4):434–440. doi: 10.1111/j.1365-2869.2012.00996.x. [DOI] [PubMed] [Google Scholar]
- 26.Huang C, Tang M, Li H, et al. Particulate matter air pollution and reduced heart rate variability: How the associations vary by particle size in Shanghai, China. Ecotoxicol Environ Saf. 2021;208:111726. doi: 10.1016/j.ecoenv.2020.111726. [DOI] [PubMed] [Google Scholar]