Abstract
Objective:
To assess disparities in preventive dental service use in four major racial/ethnic groups and assess whether racial/ethnic and income-related disparities among children were reduced from 2016 to 2020.
Methods:
Data were from the 2016 and 2020 National Survey of Children’s Health (NSCH). The outcomes of interest were having dental sealants, fluoride treatment, and dental caries in the past 12 months. Racial/ethnic groups included non-Hispanic (NH) whites, blacks, Hispanics, Asians, and others. Family income level was categorized as below or above the 200% federal poverty level (low-income vs. high-income). Children ages 2-17 were included (N=161,539). All data were self-reported by parents/guardians. We estimated the trends of racial/ethnic disparities in having fluoride treatment, dental sealants, and dental caries from 2016-2020 and tested two 2-way interactions (i.e., year by race/ethnicity, year by income) and one 3-way interaction (year by income by race/ethnicity) to assess the change in disparities from 2016-2020. All analyses accounted for the survey design of NSCH.
Results:
Overall, no significant trends in receipt of fluoride treatment, dental sealants, or having dental caries were found from 2016-2020 among the racial/ethnic groups, except for a decreasing trend in dental sealants for Asian American children (p=0.03). In the adjusted analyses, overall, NH white children were more likely to have received preventive dental services than children from minority groups (all p <0.05); Asian American children (AOR=1.31, 95% CI: 1.13-1.53) were more likely to have dental caries than NH white children.
Conclusion:
Disparities in receipt of evidence-based preventive services by children persisted. Continuous efforts are needed to promote the use of preventive dental services among children of minority populations.
Introduction
Dental caries is the most common chronic disease of childhood.1,2 About 1 in 10 preschool children and 1 in 5 children ages 6 to 11 years in the U.S. have tooth decay that requires treatment.3,4 Pediatric dental caries cause pain, lead to severe infections and affect children’s normal growth and development.5,6 Given the serious consequences, caries prevention is paramount for good overall health.
Dental sealant placement and topical fluoride application are effective in preventing dental caries, and sealants can be cost-saving when delivered to children at high risk for tooth decay.7-10 In 2021, the United States Preventive Services Task Force (USPSTF) updated its 2014 statement, which recommends that primary care physicians apply fluoride varnish beginning with the eruption of the first tooth until the child is five years of age. Children should have fluoride varnish applied two to four times per year.11
Prior studies have found that preventive dental services may be underused by children from low-income families and racial/ethnic minorities.4 12-15 Childhood dental caries and untreated caries are more prevalent and severe among racial and ethnic minorities and lower-income households.3,4,13,16 Eliminating disparities and increasing the proportion of children from low-income families receiving a preventive visit is a national priority. Furthermore, beginning in 2014, the landmark legislation Affordable Care Act (ACA) required most insurers to cover ten essential health benefits, including pediatric dental services.17 However, racial disparities in oral health and use of preventive dental care have not been assessed recently. Moreover, prior studies on trends of children’s oral health disparities in the U.S. have primarily focused on three racial/ethnic groups: comparing non-Hispanic Black and Hispanic children with non-Hispanic white children. Asian American children were kept only in the overall data reporting and were not reported under a separate race/ethnicity category.3,4,18-20 An exception is a cross-sectional analysis12 by the Centers for Disease Control and Prevention (CDC) that estimated the prevalence of dental caries and dental sealants in Asian American children using the National Health and Nutrition Examination Survey (NHANES) 2011-2012. In the U.S., Asians are the fastest growing racial/ethnic group, with a population of more than 14 million as of 2010, which is projected to grow to nearly 36 million in 2060.21 The lack of reporting separate population-based data for Asian Americans masks their health needs and impedes efforts to set goals for improving health status and health behaviors that are necessary to achieve equity.
This study aimed to 1) provide an update on receipt of fluoride treatment, dental sealants, and having dental caries by children among four main racial and ethnic groups (non-Hispanic whites, non-Hispanic blacks, Hispanics, and Asian Americans), and assess whether racial/ethnic and income-related disparities in fluoride treatment, dental sealants, and having dental caries have narrowed from 2016-2020.
Methods
Data Source
Data were from the 2016-2020 National Survey of Children’s Health (NSCH), an annual nationally representative survey of children and youth ages 0 to 17 years across the 50 US states and the District of Columbia. NSCH is funded and directed by the Health Resources and Services Administration Maternal and Child Health Bureau.22 It provides rich data on multiple, intersecting aspects of children’s lives—including physical, mental, and oral health, access to quality health care, and the child’s family, neighborhood, school, and social context. Sampling weights were adjusted to account for nonresponse and reduce the magnitude of bias. Poststratification adjustment was conducted to ensure that sociodemographic subgroups were appropriately represented in the estimates.23 A revised version of the survey was conducted as a mail and web-based survey by the Census Bureau in 2016, 2017, 2018, 2019, and 2020. Survey respondents include parents or other caregivers familiar with the child’s health and healthcare needs. The total sample size included in this analysis was 161,539 children ages 2-17 years in the 2016-2020 NSCH. Due to missing values, the analytical sample was 159,688 children ages 2-17 years in assessing fluoride treatment, 160,276 children ages 2-17 years in assessing dental caries, and 123,442 children ages 6-17 years in assessing dental sealants. IRB review is exempted for this study because it used publicly available data.
Measures
Outcome variables.
Survey respondents (i.e., parents/caregivers) provided information on three outcomes of interest examined in this study. They were: 1) dental caries (Yes/No)—whether the child had decayed teeth or caries in the past 12 months; 2) fluoride treatment (Yes/No); and 3) sealants (Yes/No)—whether the child had these preventive dental services in the past 12 months.
Independent Variable.
The independent variable was racial/ethnic groups (non-Hispanic whites, non-Hispanic blacks, Hispanics, Asians, and others).
Covariates.
Time (survey years 2016, 2017, 2018, 2019, and 2020) was included as a covariate. Other covariates were selected based on data availability and existing literature:4,13,20,24 age (2-5, 6-8, 9-11, 12-15, and 16-17), sex, parents’ highest education (less than high school, high school, some college, and college and above), household income in relation to poverty level (<200% vs ≥200% federal poverty level [FPL]), insurance coverage (no-insurance, private, public, both public and private), and medical home (Yes/No).
Statistical analysis
We first calculated the weighted proportions of the three outcomes—children having fluoride treatment, dental sealants, and dental caries, by the four racial/ethnic groups. Then, we estimated the time trend by regressing these proportions of the outcome variables on the survey year, with the survey year (2016, 2017, 2018, 2019, and 2020) as the independent continuous variable. Third, we ran three different logistic regression models to assess whether racial/ethnic and income-related disparities in the three outcomes have changed from 2016 through 2020, by assessing two 2-way interaction terms—year by race/ethnicity, and year by income, and one 3-way interaction term—year by race/ethnicity by income. Interaction terms were removed from the final model if they were not significant. We checked the missing values in the independent variable and covariates. The variable with the most missing values was the insurance type variable, with about 1.5% missing. As such, we did not attempt to impute the missing values. Data analysis was conducted in Stata 16 (StataCorp). Sampling weights were incorporated into all the analyses to obtain national estimates. A significance level of p=0.05 was used in this analysis.
Results
The characteristics of children remained similar from 2016-2020. In each wave, about 24% children were ages 2-5 years, 18% ages 6-8 years, 19% ages 9-12 years, 26% ages 12-15 years, and 13% ages 16-17 years. About 50% were non-Hispanic white, 13% non-Hispanic black, 26% Hispanic, 5% Asian, and 6% categorized as other racial/ethnic groups (Table 1).
Table 1.
Characteristics of children: 2016-2020 NSCH (Weighted %)
| Variables | 2016 | 2017 | 2018 | 2019 | 2020 |
|---|---|---|---|---|---|
| Age group (in years) | |||||
| 2-5 | 24.43 | 24.34 | 24.25 | 24.33 | 24.34 |
| 6-8 | 18.95 | 18.72 | 18.28 | 18.02 | 17.95 |
| 9-11 | 18.85 | 19.11 | 19.45 | 19.39 | 19.17 |
| 12-15 | 25.20 | 25.13 | 25.29 | 25.67 | 26.08 |
| 16-17 | 12.58 | 12.69 | 12.73 | 12.58 | 12.46 |
| Sex | |||||
| Female | 48.96 | 48.85 | 48.89 | 48.86 | 48.92 |
| Male | 51.04 | 51.15 | 51.11 | 51.14 | 51.08 |
| Race/ethnicity | |||||
| Non-Hispanic white | 51.88 | 50.68 | 50.24 | 49.95 | 49.80 |
| Non-Hispanic black | 12.86 | 13.96 | 13.62 | 13.58 | 13.38 |
| Hispanics | 24.59 | 25.19 | 25.50 | 25.74 | 25.96 |
| Asian Americans | 4.61 | 4.41 | 4.63 | 4.65 | 4.64 |
| Other | 6.06 | 5.75 | 6.00 | 6.07 | 6.22 |
| Family income | |||||
| High | 56.34 | 57.12 | 58.40 | 59.88 | 60.33 |
| Low | 43.66 | 42.88 | 41.60 | 40.12 | 39.67 |
| Parents' highest education | |||||
| less than high school | 9.47 | 9.03 | 10.12 | 9.67 | 9.67 |
| High school | 19.73 | 20.23 | 19.39 | 19.14 | 19.68 |
| Some college | 22.57 | 22.23 | 21.91 | 21.94 | 20.47 |
| College or above | 48.23 | 48.51 | 48.58 | 49.24 | 50.19 |
| Insurance type | |||||
| No insurance coverage | 6.18 | 6.34 | 6.70 | 6.86 | 7.32 |
| Public insurance | 31.70 | 30.98 | 30.82 | 29.19 | 29.44 |
| Private | 57.71 | 57.63 | 58.49 | 59.14 | 58.22 |
| Both | 4.41 | 5.05 | 3.98 | 4.81 | 5.02 |
| Medical home | |||||
| Yes | 48.26 | 47.95 | 48.01 | 46.93 | 45.76 |
| No | 51.74 | 52.05 | 51.99 | 53.07 | 54.24 |
NSCH: National Survey of Children’s Health
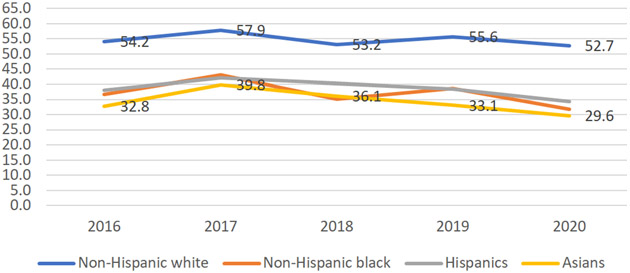
Figures 1-3 display the proportions of children of the four major racial/ethnic groups (i.e., non-Hispanic whites, non-Hispanic blacks, Hispanics, Asians) who had fluoride treatment, dental sealants, and dental caries from 2016-2020. As shown in Figure 1, the proportion of non-Hispanic white children who had fluoride treatment was significantly larger than that of other minority groups (p<0.05). In the study period 2016-2020, non-Hispanic white children had the highest proportions (from 54.2%, 57.9%, 53.2%, to 55.6%), whereas Asian American children had the lowest proportions (from 32.8%, 39.8%, 36.1%, 33.1%, to 29.6%), a gap of more than 20 percentage points on average. The proportions for Hispanics and Non-Hispanic black children were in the middle. The trend line for non-Hispanic white children was above that of other groups. In general, no significant trends in having fluoride treatment were observed for all four racial/ethnic groups from 2016-2020 (all trends p>0.05)
Fig 1.
Proportion of children having fluoride treatment, 2016-2020, by race/ethnicity
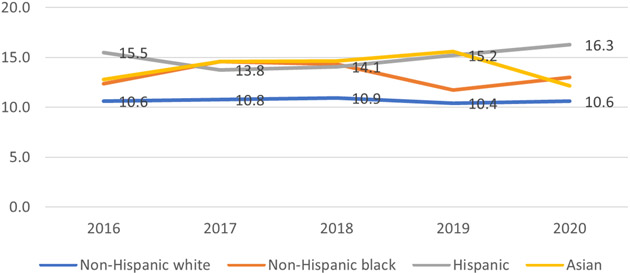
Fig 3.
Proportion of children having dental caries, 2016-2020, by race/ethnicity
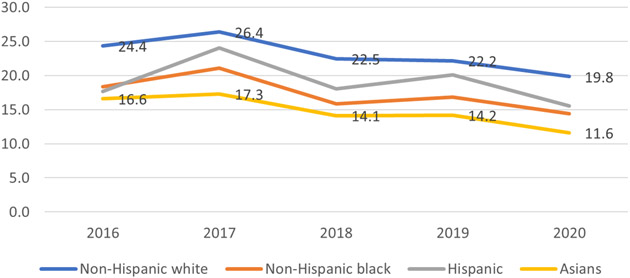
Figure 2 presents the trend for having dental sealants. The trend pattern is similar to Figure 1. The proportion of non-Hispanic white children with dental sealants was significantly larger than that of other minority groups (p<0.05) in all the years except 2017. A significant decreasing trend was shown for dental sealants in Asian children—the proportions having dental sealants decreased (from (16.6%, 17.3%, 14.1%, 14.2%, to 11.6%) (Trend p=0.03). No significant trends were shown for other racial/ethnic groups (all trends p >0.05).
Fig 2.
Proportion of children having dental sealants, 2016-2020, by race/ethnicity
In Figure 3, during the period 2016-2020, the proportions of non-Hispanic white children having dental caries (10.6%, 10.8%, 10.9%, 10.4%, to 10.6%) were significantly lower than that of Hispanics in the five survey years (all p<0.05), and significantly lower than that of Asian American children in two survey years 2018 and 2019 (all p<0.05). Overall, the trend lines of dental caries for Hispanic and Asian children were very close, and no significant trends were observed (all tend p>0.05). The trend lines for non-Hispanic white and black children were not significant (all trends p>0.05).
Logistic regression model results (Table 2)
Table 2.
Logistic regression model results of factors associated with having fluoride treatment, dental sealants, and dental caries among children: 2016-2020 NSCH
| Variables | Model I DV: Fluoride treatment |
Model II DV: Dental Sealants |
Model III DV: Dental caries |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| AOR | 95% CI | p | AOR | 95% CI | p | AOR | 95% CI | p | ||||
|
|
|
|
||||||||||
| Year (vs 2016) | <0.001 | <0.001 | 0.90 | |||||||||
| 2017 | 1.18 | 1.09 | 1.28 | 0.00 | 1.19 | 1.07 | 1.31 | 0.00 | 1.01 | 0.88 | 1.15 | 0.89 |
| 2018 | 0.98 | 0.91 | 1.05 | 0.53 | 0.94 | 0.86 | 1.03 | 0.18 | 1.01 | 0.91 | 1.13 | 0.81 |
| 2019 | 1.13 | 1.04 | 1.22 | 0.00 | 0.93 | 0.85 | 1.02 | 0.13 | 1.00 | 0.89 | 1.12 | 0.97 |
| 2020 | 0.97 | 0.90 | 1.03 | 0.32 | 0.78 | 0.71 | 0.84 | 0.00 | 1.05 | 0.94 | 1.17 | 0.36 |
| Age group (vs. 2-5 years) | <0.001 | <0.001 | <0.001 | |||||||||
| 6-8 | 2.51 | 2.32 | 2.71 | 0.00 | Ref. | 2.28 | 2.01 | 2.58 | 0.00 | |||
| 9-11 | 2.78 | 2.58 | 2.99 | 0.00 | 1.08 | 0.99 | 1.18 | 0.09 | 1.93 | 1.70 | 2.19 | 0.00 |
| 12-15 | 2.25 | 2.11 | 2.41 | 0.00 | 0.86 | 0.79 | 0.94 | 0.00 | 1.16 | 1.03 | 1.31 | 0.02 |
| 16-17 | 1.48 | 1.37 | 1.60 | 0.00 | 0.49 | 0.44 | 0.55 | 0.00 | 1.20 | 1.04 | 1.38 | 0.02 |
| Female | 1.01 | 0.97 | 1.06 | 0.57 | 1.10 | 1.03 | 1.17 | 0.00 | 0.94 | 0.87 | 1.02 | 0.14 |
| Race/ethnicity (vs. Non-Hispanic white) | <0.001 | <0.001 | <0.01 | |||||||||
| Non-Hispanic black | 0.60 | 0.56 | 0.65 | 0.00 | 0.78 | 0.70 | 0.87 | 0.00 | 0.91 | 0.80 | 1.03 | 0.13 |
| Hispanics | 0.76 | 0.70 | 0.81 | 0.00 | 0.99 | 0.89 | 1.09 | 0.82 | 1.03 | 0.93 | 1.14 | 0.59 |
| Asian Americans | 0.45 | 0.41 | 0.50 | 0.00 | 0.60 | 0.52 | 0.70 | 0.00 | 1.31 | 1.13 | 1.53 | 0.00 |
| Other | 0.95 | 0.88 | 1.03 | 0.23 | 1.10 | 0.99 | 1.23 | 0.08 | 1.08 | 0.95 | 1.22 | 0.26 |
| Low family Income | 0.96 | 0.87 | 1.06 | 0.43 | 0.89 | 0.82 | 0.97 | 0.01 | 1.12 | 1.01 | 1.24 | 0.03 |
| Parents' highest education (less than high school) | <0.001 | <0.001 | <0.001 | |||||||||
| High school | 1.57 | 1.35 | 1.82 | 0.00 | 1.57 | 1.26 | 1.97 | 0.00 | 0.93 | 0.78 | 1.11 | 0.41 |
| Some college | 1.95 | 1.69 | 2.26 | 0.00 | 1.84 | 1.48 | 2.29 | 0.00 | 0.94 | 0.79 | 1.11 | 0.45 |
| College or above | 2.53 | 2.18 | 2.93 | 0.00 | 2.01 | 1.61 | 2.50 | 0.00 | 0.74 | 0.62 | 0.88 | 0.00 |
| Insurance type (vs. no insurance coverage) | <0.001 | <0.001 | <0.001 | |||||||||
| Public insurance | 2.04 | 1.79 | 2.33 | 0.00 | 1.55 | 1.27 | 1.90 | 0.00 | 0.98 | 0.82 | 1.16 | 0.78 |
| Private | 2.32 | 2.04 | 2.63 | 0.00 | 1.39 | 1.15 | 1.69 | 0.00 | 0.61 | 0.51 | 0.73 | 0.00 |
| Both | 2.16 | 1.83 | 2.56 | 0.00 | 1.48 | 1.15 | 1.92 | 0.00 | 0.99 | 0.77 | 1.26 | 0.91 |
| Medical home | 1.46 | 1.39 | 1.53 | 0.00 | 1.20 | 1.13 | 1.28 | 0.00 | 0.80 | 0.74 | 0.87 | 0.00 |
| Interaction terms | ||||||||||||
| Year by race/ethnicity | NS | NS | NS | |||||||||
| Year by income | <0.001 | NS | NS | |||||||||
| 2017 by low income | 1.02 | 0.86 | 1.20 | 0.84 | ||||||||
| 2018 by low income | 1.01 | 0.87 | 1.17 | 0.92 | ||||||||
| 2019 by low income | 0.81 | 0.69 | 0.94 | 0.01 | ||||||||
| 2020 by low income | 0.78 | 0.68 | 0.90 | 0.00 | ||||||||
| Year by income by race | NS | NS | NS | |||||||||
DV=dependent variable. AOR=adjusted odds ratio. CI=confidence interval. Ref=reference group. NS=not significant
NSCH: National Survey of Children’s Health
Results of interaction terms: year by race/ethnicity, year by income level, and year by income level by race/ethnicity.
Overall, the year by race/ethnicity interaction was not significant in all the models (all p>0.05), suggesting that disparities associated with race/ethnicity did not change from 2016-2020. As for the interaction of year by income, a significant interaction was found only in the model for the fluoride treatment (p<0.001), suggesting that the disparities in fluoride treatment associated with family income level increased over time. That is, children from low-income families were less likely to have fluoride treatment from 2016-2020. The non-significant interactions of year by income in other models (i.e., fluoride treatment and dental caries models) suggest that disparities in having dental sealants and dental caries due to income level did not change over time from 2016-2020. Finally, the 3-way interaction term—year by income level by race/ethnicity—was not significant in all models, suggesting that the disparities among children from low-income families of the four racial and ethnic groups did not change over time (p>0.005).
Results of race/ethnicity, time, and other covariates
Overall, children from minority groups were less likely than non-Hispanic white children to have fluoride treatment and dental sealants (p<0.001). From 2016-2020, a decreasing trend was observed for having fluoride treatment and dental sealants (p<0.001). No significant trend was found for having dental caries.
In the fluoride treatment model, children older than six years were more likely to have received fluoride treatment than those aged 2-5 years (p<0.05). Children whose parents with more than a high school education (i.e., high school, some college, and college or above) were more likely than those whose parents with less than a high school education to have received fluoride treatment (all p <0.05). Children with insurance (public insurance, private insurance or both public and private insurance) were more likely than those without insurance coverage to have fluoride treatment (all p <0.05). Children with a medical home were more likely to have received fluoride treatment (AOR=1.45, 95% CI: 1.39-1.53).
In the dental sealants model, children ages 12-15 and 16-17 years were less likely than those ages 6-8 years to have received dental sealants (P<0.001). Children from low-income families were less likely than those from high-income families to have received dental sealants (AOR=0.89, 95% CI: 0.82-0.97). Children whose parents had more than a high school education were more likely than those whose parents had less than high school education to have received dental sealants (all p<0.001). Children with public insurance, private insurance or both public and private insurance were more likely than those without insurance coverage (all p<0.001). Children with a medical home were more likely than those without to have received dental sealants (AOR=1.20, 95% CI: 1.13-1.28).
Finally, in the dental caries model, children older than six years were more likely than those ages 2-5 years to have dental caries (p<0.05). Asian children (AOR=1.31, 95% CI: 1.13-1.53) were more likely than non-Hispanic white children to have dental caries. Children from low-income families (AOR=1.12, 95% CI: 1.01-1.24) were more likely than those from high-income families to have dental caries. Children with private insurance (AOR=0.61, 95% CI: 0.51-0.73) were less likely to have dental caries. Children with a medical home (AOR=0.80, 95% CI: 0.74-0.87) were less likely to have dental caries.
Discussion
Using the most recent NSCH data, this study provides an update on racial/ethnic disparities in receipt of fluoride treatment, dental sealants, and having dental caries among children in the U.S. For the fluoride treatment and dental sealants, a consistently lower proportion of minority children received these preventive dental services compared to non-Hispanic white children. Whereas for dental caries, a higher proportion of Hispanic children and Asian children had dental caries than non-Hispanic white children, although not statistically significant at p<0.05 level. Overall, no significant trends in receipt of fluoride treatment, dental sealants, and having dental caries by the four racial/ethnic groups were observed, except that a significant decreasing trend in having dental sealants was found for Asian American children. Overall, the study found that the disparities in receipt of these two preventive dental services and the prevalence of dental caries between non-Hispanic white and other minority groups persisted from 2016-2020.
Extending from prior studies on dental service and oral health disparities among children3,4,18 that mainly focused on three racial/ethnic groups—non-Hispanic white, non-Hispanic black, and Mexican American children, our study is the first to assess the trends of disparities in preventive dental services use and dental caries between non-Hispanic white children and Asian, non-Hispanic black, Hispanic children in the US. The study revealed that there was a gap of 20 percentage points in having fluoride treatment and a gap of 8 percentage points in having dental sealants between Asian and non-Hispanic white children. Moreover, although not statistically different, the proportions of Asian American children having these fluoride treatments and dental sealants services were consistently smaller—the trend lines for Asian children were below that of non-Hispanic black and Hispanic children. In addition, a significant decreasing trend was shown in having dental sealants by Asian American children from 2016-2020. These findings indicate substantial disparities between Asian and non-Hispanic white children and an under-utilization of these effective dental services. The findings also expand our understanding of disparities in preventive dental service utilization by Asian American children. This study provided up-to-date data on racial disparity trends that is necessary to inform policy changes for improving the oral health of vulnerable population subgroups.
The results showed that Asian American and non-Hispanic black and Hispanic children received fewer fluoride treatments and dental sealants. One potential factor contributing to the under-utilization of these preventive dental services may include parents’ lack of knowledge of the effectiveness of these dental preventive services, which would put these children at higher risk of dental caries. Prior research found that only 55% of parents of children below 18 years have knowledge of dental sealants, and the level of awareness of the purpose of dental sealants is even lower among low-income and racial- and ethnic-minority parents.25 Thus, increasing oral health knowledge among low-income and racial/ethnic minority parents could reduce disparities in the use of preventive dental services. Furthermore, the results also show that Asian American children were more likely than non-Hispanic white children to have dental caries. These findings implicate that fluoride treatment and dental sealants need to be further promoted among Asian American children, in conjunction with health education on oral hygiene and dietary behaviors. It should be noted that other risk factors for early childhood caries include going to bed with a bottle of juice, formula, or milk or consuming snacks multiple times a day.26,27
The study found decreasing trends in the receipt of fluoride treatment and dental sealants from 2016-2020, yet there were no changes in the prevalence of dental caries. A recent oral health surveillance report by CDC showed that both fluoride treatment and dental sealant treatment increased, and dental caries decreased from NHANES 1999–2004 to NHANES 2011–2016, with Mexican American children achieving the most significant progress compared to non-Hispanic black and non-Hispanic white children.3 For instance, from 1999-2004 to 2011-2016, the prevalence of untreated tooth decay in primary teeth in children ages 2-5 years decreased from 16.9% to 6.7% among non-Hispanic white children; from 24.3% to 14.8% among non-Hispanic black children; and from 30.8% to 15.1% among Mexican American children. And the prevalence of dental sealants among children ages 6-11 years increased, from 36.4% to 43.6% among non-Hispanic white children; from 21.1% to 31.7% among non-Hispanic black children; and from 24.2% to 44.4% among Mexican American children.3 Prior trend analyses also showed a steady reduction in dental caries in children.4,18 In this analysis, we assessed the changes from five surveys from 2016-2020. The short study period may account for the insignificant trends. The COVID-19 pandemic in 2020 affected dental service access, including preventive oral health care,28 which may explain the decreasing trends in the use of fluoride treatment and dental sealants as shown by the NSCH 2016-2020. Recent data from National Health Interview Survey showed that the percentage of children aged 1–17 years who had a dental examination or cleaning in the past 12 months decreased from 83.8% in 2019 to 80.9% in 2020.29 Nonetheless, the trends in dental service utilization need to be monitored in future surveys.
Results show that family income, parents’ education, and insurance coverage are enabling factors for preventive dental care for children, which corroborates prior findings.3,4,18 In addition, our study results show that having a medical home was a significant contributor to having both fluoride treatment and dental sealants and a protective factor for having dental caries, independent of income, education, and insurance coverage. As such, having a medical home for children can improve their oral health. A medical home can improve access to care for a child, meeting the well and sick needs, including referrals as needed, thus rendering patient-centered coordinated care.30 Pediatricians play an integral part in developing a medical home for the child by providing preventative dental care and establishing continued care through dental referrals.
We acknowledge several limitations. First, data were cross-sectional and reported by parents/guardians, which may be subject to recall bias. Parents may not recall or be aware of specific preventive services during visits. But the differences and trends between the racial/ethnic groups observed in this study are not likely to have been affected or confounded by recall bias. Second, details on the types of non-fluoride treatment the children received were unavailable in the database. Third, the NSCH asked whether the child had seen a dentist or other oral health care provider for any kind of dental or oral health care in the past 12 months. So we could not ascertain whether the preventive dental services (i.e., fluoride varnish applications) received were from a dentist or other primary care providers, such as pediatricians. Future studies are needed to identify the extent to which preventive dental services are provided by a dentist, other oral healthcare providers, or non-oral healthcare providers. Moreover, future national surveys need to oversample Asian Americans and include specific background data, such as country of birth.
Conclusion
This study provided an update on the trends of receipt of evidenced-based preventive dental services and dental caries in children. Disparities between non-Hispanic white and other minority children persisted from 2016-2020. The disparities in preventive dental services and dental caries between Asian American and non-Hispanic white children warrants more attention from policymakers and providers. Continuous efforts are needed to promote the value of preventive dental services among parents of low income and minority populations, especially parents of Asian American children. Additional programs are needed to improve access to preventive oral health services outside traditional dental offices, such as school-based programs for underserved minority children.31
Acknowledgments
Funding
This project was supported by grants from the Health Resources and Services Administration (Grant #: D88HP37544) and National Institute of Dental and Craniofacial Research (Grant #: R21 DE031368-01).
Contributor Information
Huabin Luo, Department of Public Health, Brody School of Medicine, East Carolina University, Greenville, NC 27834..
Mark E. Moss, Department of Foundational Sciences, School of Dental Medicine, East Carolina University, Greenville, NC 27834.
Wanda Wright, Department of Foundational Sciences, School of Dental Medicine, East Carolina University, Greenville, NC 27834.
Michael Webb, Department of Pediatric Dentistry and Orthodontics and Dentofacial Orthopedics, School of Dental Medicine, East Carolina University, Greenville, NC 27834.
Vanessa Pardi, Department of Foundational Sciences, School of Dental Medicine, East Carolina University, Greenville, NC 27834.
Suzanne Lazorick, Department of Public Health, Brody School of Medicine, East Carolina University, Greenville, NC 27834..
References
- 1.Colak H, Dülgergil CT, Dalli M, Hamidi MM. Early childhood caries update: A review of causes, diagnoses, and treatments. Journal of natural science, biology, and medicine. 2013;4(1):29–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.US Department of Health and Human Services. Oral Health in America: A Report of the Surgeon General. Rockville, MD: National Institute of Dental and Craniofacial Research, National Institutes of Health, US Dept of Health and Human Services; 2000. 2000. [Google Scholar]
- 3.Centers for Disease Control & Prevention. Oral Health Surveillance Report: Trends in Dental Caries and Sealants, Tooth Retention, and Edentulism, United States, 1999–2004 to 2011–2016. Atlanta, GA: CDC, US Dept of Health and Human Services; 2019. 2019. [Google Scholar]
- 4.Dye BA, Mitnik GL, Iafolla TJ, Vargas CM. Trends in dental caries in children and adolescents according to poverty status in the United States from 1999 through 2004 and from 2011 through 2014. Journal of the American Dental Association (1939). 2017;148(8):550–565.e557. [DOI] [PubMed] [Google Scholar]
- 5.Selwitz RH, Ismail AI, Pitts NB. Dental caries. Lancet (London, England). 2007;369(9555):51–59. [DOI] [PubMed] [Google Scholar]
- 6.Ayhan H, Suskan E, Yildirim S. The effect of nursing or rampant caries on height, body weight and head circumference. The Journal of clinical pediatric dentistry. 1996;20(3):209–212. [PubMed] [Google Scholar]
- 7.Ahovuo-Saloranta A, Forss H, Walsh T, et al. Sealants for preventing dental decay in the permanent teeth. The Cochrane database of systematic reviews. 2013(3):Cd001830. [DOI] [PubMed] [Google Scholar]
- 8.Marinho VC, Worthington HV, Walsh T, Chong LY. Fluoride gels for preventing dental caries in children and adolescents. The Cochrane database of systematic reviews. 2015;2015(6):Cd002280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Weintraub JA, Stearns SC, Rozier RG, Huang CC. Treatment outcomes and costs of dental sealants among children enrolled in Medicaid. American journal of public health. 2001;91(11):1877–1881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.National Academy of Medicine. Improving access to oral health care among underserved and vulnerable populations. Report Brief. Washington, DC: National Academy of Medicine, 2011. 2011. [Google Scholar]
- 11.Davidson KW, Barry MJ, Mangione CM, et al. Screening and Interventions to Prevent Dental Caries in Children Younger Than 5 Years: US Preventive Services Task Force Recommendation Statement. Jama. 2021;326(21):2172–2178. [DOI] [PubMed] [Google Scholar]
- 12.Dye BA, Thornton-Evans G, Li X, Iafolla TJ. Dental caries and sealant prevalence in children and adolescents in the United States, 2011-2012. NCHS Data Brief. 2015(191):1–8. [PubMed] [Google Scholar]
- 13.Slade GD, Sanders AE. Two decades of persisting income-disparities in dental caries among U.S. children and adolescents. Journal of public health dentistry. 2018;78(3):187–191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sathiyakumar T, Vasireddy D, Mondal S. Impact of Sociodemographic Factors on Dental Caries in Children and Availing Fluoride Treatment: A Study Based on National Survey of Children's Health (NSCH) Data 2016-2019. Cureus. 2021;13(9):e18395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Vasireddy D, Sathiyakumar T, Mondal S, Sur S. Socioeconomic Factors Associated With the Risk and Prevalence of Dental Caries and Dental Treatment Trends in Children: A Cross-Sectional Analysis of National Survey of Children's Health (NSCH) Data, 2016-2019. Cureus. 2021;13(11):e19184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rozier RG, White BA, Slade GD. Trends in Oral Diseases in the U.S. Population. Journal of dental education. 2017;81(8):eS97–eS109. [DOI] [PubMed] [Google Scholar]
- 17.Kranz AM, Dick AW. Changes in pediatric dental coverage and visits following the implementation of the affordable care act. Health services research. 2019;54(2):437–445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Capurro DA, Iafolla T, Kingman A, Chattopadhyay A, Garcia I. Trends in income-related inequality in untreated caries among children in the United States: findings from NHANES I, NHANES III, and NHANES 1999-2004. Community dentistry and oral epidemiology. 2015;43(6):500–510. [DOI] [PubMed] [Google Scholar]
- 19.Fisher-Owens SA, Isong IA, Soobader MJ, et al. An examination of racial/ethnic disparities in children's oral health in the United States. J Public Health Dent. 2013;73(2):166–174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lebrun-Harris LA, Canto MT, Vodicka P. Preventive oral health care use and oral health status among US children: 2016 National Survey of Children's Health. J Am Dent Assoc. 2019;150(4):246–258. [DOI] [PubMed] [Google Scholar]
- 21.Pew Research Center. Asian Americans Are the Fastest-Growing Racial or Ethnic Group in the U.S. Available at: https://www.pewresearch.org/fact-tank/2021/04/09/asian-americans-are-the-fastest-growing-racial-or-ethnic-group-in-the-u-s/. Accessed July 2022.
- 22.U.S. Department of Health and Human Services HRaSA, Maternal and Child Health Bureau. National Survey of Children’s Health,,. NSCH Survey Methodology. Available at: https://www.childhealthdata.org/learn-about-the-nsch/methods. Accessed July, 2022. [Google Scholar]
- 23.U.S. Department of Health and Human Services HRaSA, Maternal and Child Health Bureau. National Survey of Children’s Health,,. NSCH fast facts and frequently asked questions. Available at: https://www.childhealthdata.org/learn-about-the-nsch/FAQ. Accessed July 2022. [Google Scholar]
- 24.Lebrun-Harris LA, Canto MT, Vodicka P, Mann MY, Kinsman SB. Oral Health Among Children and Youth With Special Health Care Needs. Pediatrics. 2021;148(2). [DOI] [PubMed] [Google Scholar]
- 25.Junger ML, Griffin SO, Lesaja S, Espinoza L. Awareness Among US Adults of Dental Sealants for Caries Prevention. Preventing chronic disease. 2019;16:E29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Harris R, Nicoll AD, Adair PM, Pine CM. Risk factors for dental caries in young children: a systematic review of the literature. Community dental health. 2004;21(1 Suppl):71–85. [PubMed] [Google Scholar]
- 27.Kirthiga M, Murugan M, Saikia A, Kirubakaran R. Risk Factors for Early Childhood Caries: A Systematic Review and Meta-Analysis of Case Control and Cohort Studies. Pediatric dentistry. 2019;41(2):95–112. [PMC free article] [PubMed] [Google Scholar]
- 28.C.S. Mott Children’s Hospital. Pandemic-posed challenges to children’s oral health. Mott Poll Report 38(1). Available at: https://mottpoll.org/sites/default/files/documents/021521_DentalCare.pdf. Accessed July, 2022. [Google Scholar]
- 29.Adjaye-Gbewonyo D, Black LI. Dental Care Utilization Among Children Aged 1-17 Years: United States, 2019 and 2020. NCHS data brief. 2021(424):1–8. [PubMed] [Google Scholar]
- 30.American Academy of Pediatrics. Definition of the Medical Home: The medical home. Pediatrics. 1992;90(5):774. [PubMed] [Google Scholar]
- 31.Starr JR, Ruff RR, Palmisano J, Goodson JM, Bukhari OM, Niederman R. Longitudinal caries prevalence in a comprehensive, multicomponent, school-based prevention program. Journal of the American Dental Association (1939). 2021;152(3):224–233.e211. [DOI] [PubMed] [Google Scholar]