Abstract
Objective
The aim of the current meta-analysis was to evaluate the accuracy of using BMI based on self-reported height and weight (BMIsr) to estimate the prevalence of overweight and obesity among children and adolescents.
Design
A systematic literature search was conducted to select studies that compared the prevalence rates of overweight and obesity based on BMIsr and BMIm (BMI based on measured height and weight). A random-effect model was assumed to estimate summary prevalence rates and prevalence ratio (PR).
Results
Thirty-seven studies were included. The aggregated prevalence of overweight and obesity based on BMIsr (0·190, 95 % CI 0·163, 0·221) was significantly lower than that based on BMIm (0·233, 95 % CI 0·203, 0·265). The pooled mean PR was 0·823 (95 % CI 0·775, 0·875). Moderator analyses showed that the underestimation was related to gender, age, weight status screened (overweight v. obesity) and weight status screening tool.
Conclusions
BMIsr may produce less biased results under some conditions than others. Future researchers using BMIsr may consider these findings and avoid the conditions that could lead to more severe underestimation of the prevalence of overweight and obesity among children and adolescents.
Keywords: Self-reported BMI, Children and adolescents, Overweight and obesity, Prevalence, Meta-analysis
Globally, overweight and obesity among children and adolescents rose by 47·1 % between 1980 and 2013 in both developed and developing countries( 1 ). Because of the serious health problems (CHD, high blood pressure, stroke, type 2 diabetes, metabolic syndrome, etc.) associated with overweight and obesity( 2 , 3 ) and the negative impact on quality of life( 4 – 9 ), overweight and obesity has become a major public health issue for children and adolescents.
To assess overweight and obesity, BMI (BMI=[weight (kg)]/[height (m)]2) is used as the most common proxy measure of weight status for both clinical and epidemiological studies( 10 ). For children and adolescents, BMI has been recommended as an appropriate single indicator for assessing overweight and obesity( 11 , 12 ).
Although direct measurement of height and weight is the ‘gold standard’ to obtain BMI, in large-scale epidemiological surveys, such as the Youth Risk and Behavior Surveillance Study (YRBSS)( 13 ) and the National Health Interview Surveys (NHIS)( 14 ), the prevalence of overweight and obesity is often estimated using BMI derived from self-reported height and weight (BMIsr) for practical and financial reasons, instead of BMI based on measured height and weight (BMIm).
It should be noted that the purpose of using BMIsr is either for assessing a person’s weight status at the individual level or for monitoring the prevalence of weight status at the population level( 15 ). Specifically, for screening individuals with overweight and obesity at the individual level, researchers care about the diagnostic accuracy (e.g. sensitivity and specificity)( 16 ) of using BMIsr. For example, the sensitivity of using BMIsr is the probability of correctly identifying an individual as being overweight/obese when indeed that is the case( 17 ). However, at the population level, researchers care about the difference between the prevalence rate derived from BMIsr and the prevalence rate derived from BMIm.
In the previous research literature there are several studies( 18 – 20 ) that have different recommendations for using BMIsr at the individual and population levels, respectively. For instance, Fonseca et al.( 18 ) suggested that BMIsr was not accurate at the individual level for assessing weight status, but it might be a simple and valid tool for estimating the prevalence of overweight and obesity at the population level. Thus, the results and implications of using BMIsr could vary depending on the level (individual v. population) at which BMIsr is used.
Currently, a meta-analysis about the accuracy of using BMIsr at the individual level has been conducted( 17 ). The study used a special meta-analytic method, diagnostic meta-analysis( 21 ), which is specially designed for synthesizing effect sizes of diagnostic test accuracy, and showed that for screening children and adolescents with overweight and obesity, the use of BMIsr presented a pooled sensitivity and specificity of 0·76 and 0·96, respectively( 17 ). However, because the results and implications of using BMIsr can be different depending on its application at individual or population level( 18 – 20 ), and the analysis methods are also quite different for analyses intended for these two different levels( 17 , 22 , 23 ), there is a strong need to conduct a meta-analysis at the population level for understanding the suitability of using BMIsr for monitoring the prevalence of overweight and obesity among children and adolescents.
To date, there have been dozens of studies examining the accuracy of using BMIsr to estimate the prevalence of overweight and obesity for children and adolescents. Many studies have reported that, when compared with the estimated prevalence based on BMIm, children and adolescents tend to over-report height and under-report weight, resulting in a lower BMI that leads to underestimation of the prevalence of overweight and obesity( 24 – 34 ). In contrast, some other studies exist reporting either no difference( 18 , 35 – 38 ) or a higher prevalence from BMIsr-based estimation( 39 ). As a result, the suitability of using BMIsr to estimate the prevalence remains controversial. Some studies have suggested that BMIsr should be used with caution( 28 , 37 , 40 , 41 ) and a correction should be applied to the self-reported data( 27 , 29 , 31 , 34 , 39 , 41 – 45 ), or not to use BMIsr at all( 32 , 33 , 46 , 47 ). On the other hand, there are also studies supporting the validity of BMIsr use in epidemiological studies for children and adolescents( 18 , 24 , 35 , 36 , 38 ).
Considering the inconsistency among the existing literature on the accuracy of BMIsr for such use and the inevitable use of BMIsr in future studies, especially in large-scale surveys, we decided to conduct a meta-analysis of the existing literature on this issue. Such a systematic synthesis would not only allow researchers to have a better understanding about the degree of discrepancy, or lack thereof, between BMIsr-based and BMIm-based prevalence rates of overweight and obesity among children and adolescents, but would also allow researchers to understand the roles of some potential moderators (e.g. gender( 24 , 27 , 44 , 48 ) and age( 24 , 46 , 49 , 50 )).
Therefore, by doing a systematic quantitative review of the research literature at the population level, the aims of the current meta-analysis were to estimate the overall discrepancy between BMIsr-based prevalence and BMIm-based prevalence of overweight and obesity for children and adolescents, and to determine whether, and to what extent, some potential factors (e.g. sample and/or study characteristics such as gender and age) could have affected the difference between the estimated prevalence rates based on BMIsr and BMIm, respectively.
Methods
It should be noted that because the current meta-analysis was conducted based on the literature search results of the previous diagnostic meta-analysis for the accuracy of using BMIsr at an individual level( 17 ), there are some overlaps (e.g. studies included) between the current meta-analysis and the previous one. On the other hand, these two meta-analysis studies differ substantially in multiple aspects, including research aims, methods, results and related implications for future studies, as discussed above.
Literature search
Following the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines( 51 ), the search was conducted in three databases, namely PubMed, Web of Science and EBSCOhost (all sub-databases used). The search covered the research literature up to September 2016. The keywords used were: (self-reported OR self-report) AND (height and weight OR BMI OR BMI) AND (children OR adolescents OR kids OR youngsters OR youth OR pediatric). Moreover, in a follow-up search, from September to October 2016, we also used Google Scholar and find additional relevant articles that were not contained in the databases searched above. In addition, when one article was found to meet the selection criteria, the references cited in the selected article were also checked for potential articles.
Selection criteria
To be included in the current meta-analysis, a study had meet the following criteria: (i) be published as a peer-reviewed journal article; (ii) be published in English; (iii) age of the participants was no more than 21 years, to be consistent with the Stages of Adolescent Development( 52 ); (iv) be an observational study (longitudinal or cross-sectional design); and (v) report prevalence rates of overweight and/or obesity using both BMIsr and BMIm, or there was sufficient information in the study to allow the calculation of the rates from BMIsr and BMIm.
Assessment of quality
The first two authors independently assessed the quality of the selected articles. Because the meta-analysis concerned the comparison of the prevalence rates based on two methods (BMIsr and BMIm), we chose the Revised Tool for the Quality Assessment of Diagnostic Accuracy (QUADAS-2)( 53 ) to assess the quality of the selected studies. The QUADAS-2 identifies four key domains, namely ‘selection of patients’, ‘index test’, ‘reference standard’ and ‘flow and timing’. Specifically, in the current meta-analysis, ‘selection of patients’ assesses the sample representativeness based on the sample selection in a study; ‘index test’ and ‘reference standard’ are BMIsr and BMIm, respectively, because we assessed the accuracy of BMIsr by using BMIm as the reference in the current meta-analysis; and ‘flow and timing’ concerns the time interval between the index test (i.e. BMIsr) and the reference standard (i.e. BMIm). These four domains were combined to assess the quality of the studies included. After obtaining the independent ratings of quality, some minor disagreements were resolved through discussion between the two evaluators.
Extraction of data
The first two authors independently extracted the data, and a very limited number of coding discrepancies between the two coders were later resolved through discussion within the research team. The information coded in our current meta-analysis was: (i) the last name of the first author; (ii) publication year; (iii) country; (iv) sampling methods; (v) sample size; (vi) age; (vii) gender; (viii) weight status measured (overweight, obesity, mixed); (ix) weight status screening tool (WHO, Centers for Disease Control and Prevention (CDC), International Obesity Task Force (IOTF), other); (x) the prevalence rate of overweight and/or obesity based on BMIsr; and (xi) the prevalence rate of overweight and/or obesity based on BMIm.
Data synthesis and statistical analysis
From each study, the prevalence rate of overweight and obesity based on BMIsr and that based on BMIm (P sr and P m, respectively) were obtained, and the prevalence ratio (PR; PR=P sr/P m) between the two prevalence rates from each study was derived. As used in this context, the PR provides information about the relative possibility of being classified into the overweight and obesity category based on BMIsr relative to the ‘gold standard’ of BMIm. More specifically, PR>1, PR=1 and PR<1 indicate overestimation, equal estimation and underestimation of overweight and obesity cases, respectively, by the BMIsr method.
In the overall analyses, the pooled estimates of P sr, P m and PR with the 95 % CI were obtained by using a random-effects model, which is generally more appropriate than a fixed-effects model because it assumes that the true effect size varies among studies included( 54 ). The heterogeneity across studies was assessed by the Q statistic and the I 2 statistic, which represents the percentage of variation across studies that is due to heterogeneity rather than chance( 55 ). I 2 values of 25 %, 50 % and 75 % indicate low, moderate and high heterogeneity, respectively( 55 ). Publication bias was assessed by Begg’s and Egger’s tests, with a non-significant P value indicating insufficient evidence of publication bias( 56 , 57 ).
To explore the factors that might have affected the difference between the prevalence rates derived from the two approaches (BMIsr and BMIm), moderator analyses were conducted based on PR for three categorical variables (i.e. gender, weight status category, weight status screening tool) and one continuous variable (i.e. age) by assuming a mixed-effects model. In addition, a mixed-effects model uses a random-effects model within subgroups and a fixed-effect model across subgroups, and it is generally advocated for subgroup analyses( 54 ). To measure the effect of each moderator variable, R 2 was used as the proportion of variance accounted for by the moderator variable( 58 ). All statistical analyses were performed by using Comprehensive Meta-analysis version 3.0 (Biostat, Englewood, NJ, USA), a statistical analysis software specially designed for conducting meta-analysis.
Results
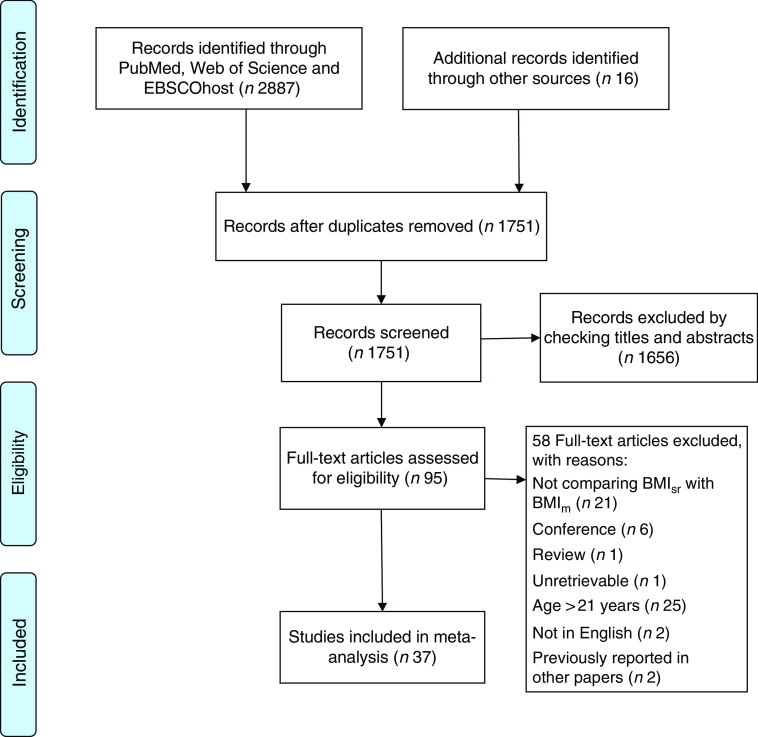
The process of selecting the usable studies for the meta-analysis is described diagrammatically in Fig. 1. We identified 2903 articles in total. After removal of duplicates, 1751 were left for screening of titles and abstracts, from which ninety-five articles were retrieved for full-text screening. Finally, thirty-seven studies were found to have met all the selection criteria( 18 , 24 – 41 , 43 – 49 , 59 – 69 ).
Fig. 1.
Flowchart showing selection of studies for inclusion in the current meta-analysis (BMIsr, BMI derived from self-reported height and weight; BMIm, BMI derived from measured height and weight)
Descriptive characteristics of the studies
The main characteristics of the thirty-seven studies included in the meta-analyses are summarized in the online supplementary material, Supplemental Table 1. Studies were carried out from 1992 to 2016. A total of 59 735 children and adolescents were included in these thirty-seven studies, with an average of 49·10 % (range 22·20–61·65 %) male and a mean age of 13·8 years (range 6–21 years). Nineteen studies differentiated the prevalence rates of overweight and obesity by gender (male and female); eighteen studies did not provide information about gender-specific prevalence rates and these were assumed to have included both female and male participants. Twenty-four studies differentiated the prevalence rates by weight status category (i.e. overweight v. obesity) and twelve studies were coded as ‘mixed’ for not providing information about overweight-only and obesity-only prevalence rates. All studies provided information on the weight status screening tool used, with ten studies using CDC, fourteen using IOTF, three using WHO, seven using national-specific standard (e.g. the Korean child and adolescent growth charts( 24 )) and three using other references (e.g. the National Health and Nutrition Examination Survey( 70 )). In addition, it should be noted that the different weight status screening tools (e.g. CDC, IOTF, WHO, national-specific standard) have different BMI cut-off values to screen overweight and obesity among children and adolescents( 71 ).
Table 1.
Summary results of moderator analyses for the prevalence ratio estimates
| 95 % CI | |||||
|---|---|---|---|---|---|
| k | PR | Lower limit | Upper limit | ANOVA/meta-regression results | |
| Gender | |||||
| Female | 19 | 0·791 | 0·726 | 0·861 | Q B(2)=19·975, P<0·01; R 2=0·091 |
| Male | 19 | 0·862 | 0·794 | 0·936 | |
| Mixed | 18 | 0·828 | 0·754 | 0·909 | |
| Weight status category | |||||
| Overweight | 24 | 0·855 | 0·787 | 0·929 | Q B(2)=39·006, P<0·01; R 2=0·145 |
| Obese | 24 | 0·799 | 0·706 | 0·904 | |
| Mixed | 12 | 0·805 | 0·730 | 0·888 | |
| Weight status screening tools | |||||
| CDC | 10 | 0·831 | 0·741 | 0·932 | Q B(2)=25·076, P<0·01; R 2=0·117 |
| IOTF | 14 | 0·760 | 0·683 | 0·845 | |
| WHO | 3 | 1·006 | 0·547 | 1·849 | |
| National-specific standard | 7 | 0·886 | 0·822 | 0·956 | |
| Age | |||||
| B PR | 36 | −0·051 | −0·096 | −0·005 | Q regression=4·727, P<0·05; R 2=0·125 |
k, number of studies; PR, prevalence ratio; CDC, Centers for Disease and Control; IOTF, International Obesity Task Force; B PR, meta-regression coefficient; Q B, between-group heterogeneity statistic to test the effect of the moderator variable on the prevalence rates; R 2, proportion of variance accounted for by the moderator variable; Q regression, heterogeneity accounted for by the regression model.
Overall analyses
The forest plots comparing the prevalence rates of overweight and obesity based on BMIsr and BMIm for each of the selected studies are presented in Fig. 2. The pooled P sr and P m were 0·190 (95 % CI 0·163, 0·221; P<0.01) and 0·233 (95 % CI 0·203, 0·265; P<0.01), respectively, with each estimate outside the 95 % CI of the other, suggesting that the pooled P sr was significantly lower than the pooled P m. The pooled mean PR was 0·823 (95 % CI 0·775, 0·875; P<0.01), with a significant Q statistic (Q (36)=218·74, P<0.01) and a relatively large I 2 (83·54 %). The findings from the overall analyses indicated two things. First, the BMIsr method generally underestimated the prevalence rate of overweight and obesity among children and adolescents when compared against the ‘gold standard’ of BMIm, with the risk of being identified as overweight and obese based on BMIsr being about 18 % lower than that based on BMIm. Second, the heterogeneity test for the findings of the individual studies indicated a considerable amount of heterogeneity across the studies, which points to the need for conducting moderator analyses( 72 ). Thus, to understand what factors may have contributed to the inconsistencies of the findings across the studies, moderator analyses were carried out as reported in the following section.
Fig. 2.
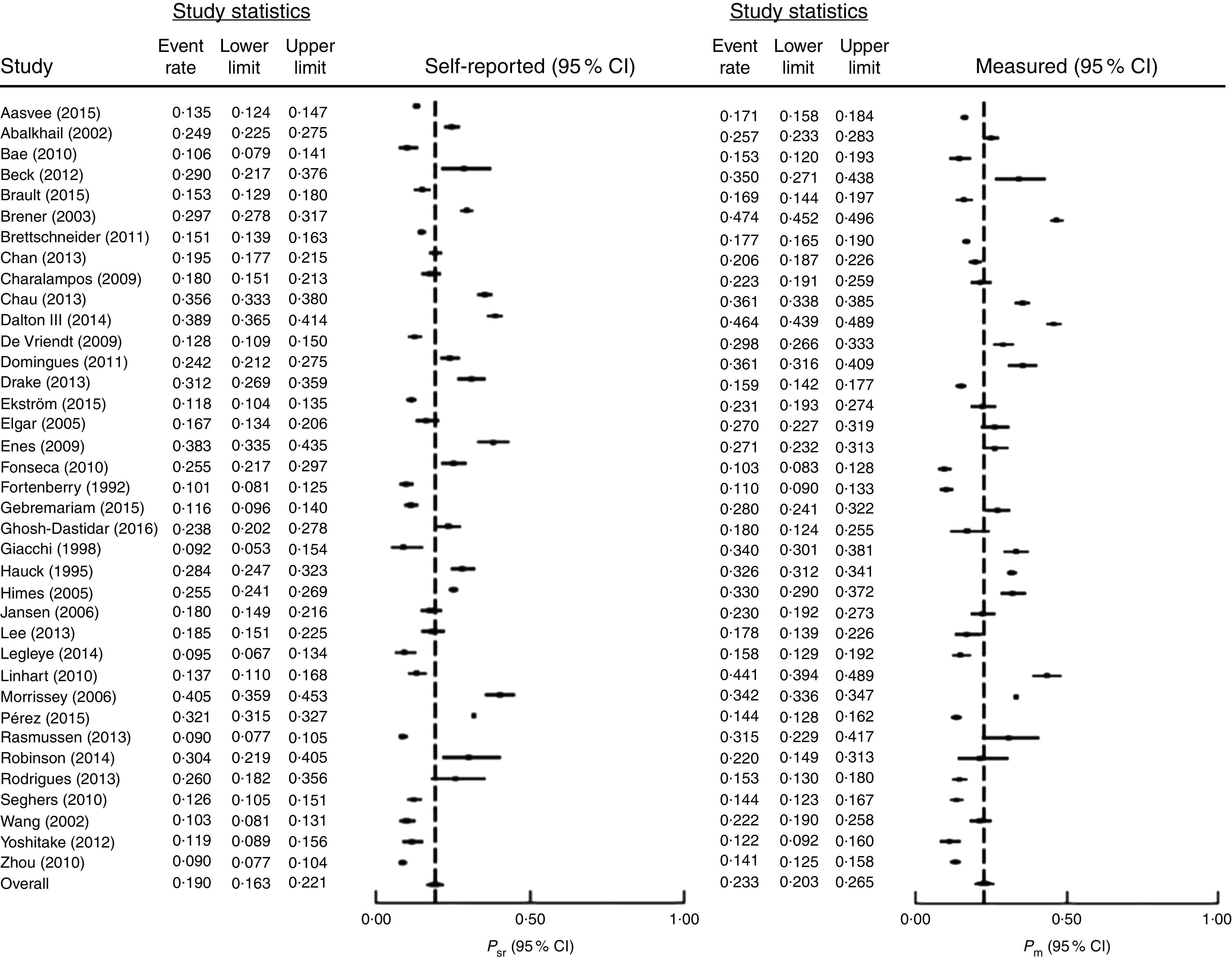
Forest plots for the prevalence rates of overweight and obesity in children and adolescents based on BMIsr (left) and BMIm (right). The study-specific prevalence rate and 95 % CI are represented by the black square and horizontal line, respectively; the centre of the diamond represents the pooled prevalence rate and its width represents the pooled 95 % CI (BMIsr, BMI derived from self-reported height and weight; BMIm, BMI derived from measured height and weight; P sr, prevalence rate based on BMIsr; P m, prevalence rate based on BMIm)
Moderator analyses
According to the results presented in Table 1, 9·1 % of the between-study heterogeneity could be explained by gender, with the PR higher for males (PR=0·862, 95 % CI 0·794, 0·936; P<0.01) than for females (PR=0·791, 95 % CI 0·726, 0·861; P<0.01). The moderator variable of weight status category could account for 14·5 % of the heterogeneity, with the PR for overweight (PR=0·855, 95 % CI 0·787, 0·929) being significantly higher than that for obesity (PR=0·799, 95 % CI 0·706, 0·904; P<0.01). Regarding weight status screening tools, 11·7 % of the between-study variance could be accounted for. The differences among the four groups of screening references (i.e. CDC, IOTF, WHO and national-specific standard) were statistically significant, with the PR for WHO being the highest (PR=1·006, 95 % CI 0·547, 1·849; P<0.01), followed by national-specific standard (PR=0·886, 95 % CI 0·822, 0·956; P<0.01), CDC (PR=0·831, 95 % CI 0·741, 0·932; P<0.01) and IOTF (PR=0·760, 95 % CI 0·683, 0·845; P<0.01). For the moderator variable of age, a significant regression slope (B PR=−0·051; P<0.05) and 12·5 % of variance explained were found in the meta-regression analysis, which indicated that PR decreased significantly in value with the increase of age.
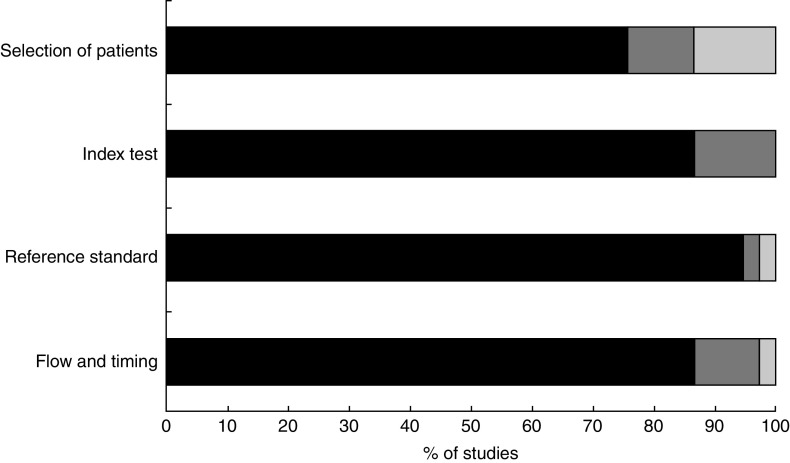
Methodological quality and publication bias
The methodological quality of the thirty-seven included studies is summarized in Fig. 3. Based on our quality assessment procedures described above, a majority of the studies showed a low risk of bias across the four domains; only four studies were considered as having high risk of bias due to ‘selection of patients’, one study having high risk due to ‘reference standard’, one study having high risk due to ‘flow and timing’, and no study having high risk of bias due to ‘index test’. Thus, the selected thirty-seven studies overall showed good methodological quality.
Fig. 3.
Quality assessment ( , low;
, low;  , unclear;
, unclear;  , high) in the four main domains of QUADAS-2 for studies (n 37) included in the current meta-analysis (QUADAS-2, Revised Tool for the Quality Assessment of Diagnostic Accuracy(
53
))
, high) in the four main domains of QUADAS-2 for studies (n 37) included in the current meta-analysis (QUADAS-2, Revised Tool for the Quality Assessment of Diagnostic Accuracy(
53
))
According to the result of Begg’s and Egger’s tests, only Egger’s test (P=0.03), and not Begg’s test (P=0.979), showed any evidence of publication bias. By using Duval and Tweedie’s trim-and-fill method( 73 ), four additional PR were imputed to achieve no publication bias, and the adjusted estimate of PR (0·794; 95 % CI 0·774, 0·847) was close to the original estimate of PR (0·823; 95 % CI 0·774, 0·875). Thus, the publication bias was not likely to be a threat to the validity of the estimated mean PR.
Discussion
The current meta-analysis reveals that, for children and adolescents, the estimated prevalence rate of overweight and obesity based on BMIsr (19·0 %) was significantly lower than the prevalence rate estimate based on BMIm (23·3 %). In terms of the relative risk for overweight and obesity, the BMIsr method underestimated the risk of children and adolescents being classified into the category of overweight and obesity by about 18 % (PR=0·823). This finding indicates that, relative to the ‘gold standard’ of BMIm, the use of BMIsr would lead to under-identification of cases of overweight and/or obesity among children and adolescents. This result is not a surprise, as most previous studies reported underestimation of the prevalence of overweight and obesity based on self-reported data when compared with the result based on the measured data( 24 – 34 ). However, in consideration of the relatively high heterogeneity among the thirty-seven selected studies (I 2=83·54), this overall finding should be interpreted with caution, because it was not adjusted for other factors (e.g. gender, age, weight status category, weight status screening tool).
It is notable that a significant effect of gender was found, with the PR for female participants being significantly lower than for male participants (0·791 v. 0·862), which reveals that, when BMIsr was used for estimating the prevalence of overweight and obesity, the underestimation bias was more severe for females than for males. Put differently, it was more accurate to use BMIsr to monitor the prevalence of overweight and obesity for males than for females. This finding is consistent with some previous studies reporting that females show a stronger tendency of over-reporting height and under-reporting weight than males, which would lead to a greater underestimation bias of the prevalence of overweight and obesity( 24 , 27 ). With respect to weight status category, we found that the PR for overweight was significantly higher than for obesity (0·855 v. 0·799). This finding indicates that use of the BMIsr method would lead to a greater underestimation of the prevalence for obesity condition than for overweight condition. This is consistent with the findings from a number of studies reporting that BMIsr tends to be underestimated to a greater degree by heavier children and adolescents( 25 , 28 , 30 , 40 , 46 , 47 , 49 , 60 , 65 , 68 ), so it would be less accurate to use BMIsr for evaluating obesity than for overweight.
As for the effect of weight status screening tools, the results show that the highest PR was from the studies using WHO (1·006), followed by those using national-specific standard (0·886) and CDC (0·831), while those studies using IOTF showed the lowest PR (0·760). As there is no previous literature concerning the comparison of these references by using both BMIsr and BMIm, the finding of the current meta-analysis indicates that when BMIsr would be used to monitor the prevalence of overweight and obesity, the WHO reference might have the least underestimation of the prevalence, followed by national-specific standard, CDC and IOTF in that order.
Regarding the effect of age, previous studies have reported inconsistent findings. Some studies reported that BMIsr was less reliable for estimating overweight and obesity in older children compared with younger children( 37 , 41 , 49 ). However, other studies reported no age difference( 38 ), or even that the prevalence estimate based on BMIsr tended to be more accurate for older children( 24 , 46 ). The result of our meta-analysis (i.e. regression slope for age: B PR=−0·051; P<0·05) revealed a significant negative relationship between age and PR. As the overall PR (i.e. 0·823) represents an underestimation of the prevalence of overweight and obesity based on BMIsr, this finding (i.e. negative relationship between age and PR) indicates that PR would decrease in value with the increase of age, suggesting that the underestimation of the prevalence rate of overweight and obesity by BMIsr would be more severe for older children.
Limitations
There are two likely limitations of the current meta-analysis. The first is related to the moderator variable of weight status screening tools. Because of the small number of studies (k=3) for the condition of WHO reference, the high PR (i.e. 1·006) for the WHO reference condition should be considered tentative, and caution is warranted in the interpretation of this finding. The second limitation concerns some potential moderator variables reported in previous studies, but not included in our moderator analyses (e.g. race( 33 , 44 )), mainly because too few studies contained the relevant information to allow us to conduct moderator analysis for these variables. However, these potential moderators should be examined in the future when sufficient studies have the relevant information about these moderator variables.
Conclusion
Overall, the prevalence of overweight and obesity estimated by BMIsr was significantly lower than the prevalence based on BMIm. The degree of underestimation of BMIsr, however, could vary depending on gender, age, weight status category and weight status screening tool. More specifically, more severe underestimation is associated with female (in contrast to male), older age (in contrast to younger age), obesity (in contrast to overweight condition), CDC and IOTF (in contrast to WHO and national-specific standards). We believe that such a meta-analysis at the population level will provide very useful information for future epidemiological studies when researchers consider the use of BMIsr to estimate the prevalence of overweight and obesity for children and adolescents.
Acknowledgements
Financial support: This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors. Conflict of interest: The authors have nothing to disclose. Authorship: J.H. designed the research; J.H., Z.C. and X.F. conducted the research; J.H. and Z.C. analysed the data; J.H., Z.C. and X.F. wrote the paper. All authors read and approved the final manuscript. Ethics of human subject participation: Not applicable.
Supplementary material
For supplementary material accompanying this paper visit https://doi.org/10.1017/S1368980018000368.
click here to view supplementary material
References
- 1. Ng M, Fleming T, Robinson M et al. (2014) Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 384, 766–781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. National Heart, Lung, and Blood Institute (2010) What are the Health Risks of Overweight and Obesity. Washington, DC: US Department of Health and Human Services, National Institutes of Health. [Google Scholar]
- 3. Must A, Jacques PF, Dallal GE et al. (1992) Long-term morbidity and mortality of overweight adolescents: a follow-up of the Harvard Growth Study of 1922 to 1935. N Engl J Med 327, 1350–1355. [DOI] [PubMed] [Google Scholar]
- 4. Buttitta M, Iliescu C, Rousseau A et al. (2014) Quality of life in overweight and obese children and adolescents: a literature review. Qual Life Res 23, 1117–1139. [DOI] [PubMed] [Google Scholar]
- 5. Pellicer-Chenoll M, Garcia-Massó X, Morales J et al. (2015) Physical activity, physical fitness and academic achievement in adolescents: a self-organizing maps approach. Health Educ Res 30, 436–448. [DOI] [PubMed] [Google Scholar]
- 6. Schwimmer JB, Burwinkle TM & Varni JW (2003) Health-related quality of life of severely obese children and adolescents. JAMA 289, 1813–1819. [DOI] [PubMed] [Google Scholar]
- 7. Williams J, Wake M, Hesketh K et al. (2005) Health-related quality of life of overweight and obese children. JAMA 293, 70–76. [DOI] [PubMed] [Google Scholar]
- 8. Tsiros MD, Olds T, Buckley JD et al. (2009) Health-related quality of life in obese children and adolescents. Int J Obes (Lond) 33, 387–400. [DOI] [PubMed] [Google Scholar]
- 9. He J, Zhu H, Luo X et al. (2015) Chinese version of impact of weight on quality of life for kids: psychometric properties in a large school-based sample. J Public Health 38, e187–e193. [DOI] [PubMed] [Google Scholar]
- 10. Himes JH (2009) Challenges of accurately measuring and using BMI and other indicators of obesity in children. Pediatrics 124, Suppl. 1, S3–S22. [DOI] [PubMed] [Google Scholar]
- 11. Krebs NF, Himes JH, Jacobson D et al. (2007) Assessment of child and adolescent overweight and obesity. Pediatrics 120, Suppl. 4, S193–S228. [DOI] [PubMed] [Google Scholar]
- 12. Cole TJ, Bellizzi MC, Flegal KM et al. (2000) Establishing a standard definition for child overweight and obesity worldwide: international survey. BMJ 320, 1240–1243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Centers for Disease Control and Prevention (2016) Youth Risk Behavior Surveillance System (YRBSS). http://www.cdc.gov/healthyyouth/data/yrbs/ (accessed October 2016).
- 14. Centers for Disease Control and Prevention (2016) The National Health Interview Survey (NHIS). http://www.cdc.gov/nchs/nhis/ (accessed October 2016).
- 15. He J (2017) The suitability of using body mass index based on self-report height and weight for screening childhood obesity: individual level and population level. Obes Diagn Treat 1, 5.1. [Google Scholar]
- 16. Šimundić A-M (2008) Measures of diagnostic accuracy: basic definitions. Med Biol Sci 22, 61–65. [PMC free article] [PubMed] [Google Scholar]
- 17. He J, Cai Z & Fan X (2017) Accuracy of using self-reported data to screen children and adolescents for overweight and obesity status: a diagnostic meta-analysis. Obes Res Clin Pract 11, 257–267. [DOI] [PubMed] [Google Scholar]
- 18. Fonseca H, Silva A, Matos M et al. (2010) Validity of BMI based on self‐reported weight and height in adolescents. Acta Paediatr 99, 83–88. [DOI] [PubMed] [Google Scholar]
- 19. Kee C, Teh C, Tee E et al. (2017) Validity of self-reported weight and height: a cross-sectional study among Malaysian adolescents. BMC Med Res Methodol 17, 85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Yoong SL, Carey ML, D’Este C et al. (2013) Agreement between self-reported and measured weight and height collected in general practice patients: a prospective study. BMC Med Res Methodol 13, 38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Leeflang M (2014) Systematic reviews and meta‐analyses of diagnostic test accuracy. Clin Microbiol Infect 20, 105–113. [DOI] [PubMed] [Google Scholar]
- 22. Shaffi A (2011) Measures derived from a 2 × 2 table for an accuracy of a diagnostic test. J Biomet Biostat 2, 128. [Google Scholar]
- 23. He J, Cai Z & Fan X (2017) Prevalence of binge and loss of control eating among children and adolescents with overweight and obesity: an exploratory meta‐analysis. Int J Eat Disord 50, 91–103. [DOI] [PubMed] [Google Scholar]
- 24. Aasvee K, Rasmussen M, Kelly C et al. (2015) Validity of self-reported height and weight for estimating prevalence of overweight among Estonian adolescents: the Health Behaviour in School-aged Children study. BMC Res Notes 8, 606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Bae J, Joung H, Kim J-Y et al. (2010) Validity of self-reported height, weight, and body mass index of the Korea Youth Risk Behavior Web-based Survey questionnaire. J Prev Med Public Health 43, 396–402. [DOI] [PubMed] [Google Scholar]
- 26. Brener ND, McManus T, Galuska DA et al. (2003) Reliability and validity of self-reported height and weight among high school students. J Adolesc Health 32, 281–287. [DOI] [PubMed] [Google Scholar]
- 27. Brettschneider A-K, Rosario AS & Ellert U (2011) Validity and predictors of BMI derived from self-reported height and weight among 11 to 17 year-old German adolescents from the KiGGS study. BMC Res Notes 4, 414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Charalampos H, Michael T, Antonia S et al. (2012) Validity of self-reported height, weight and body mass index among Cypriot adolescents: accuracy in assessing overweight status and weight overestimation as predictor of disordered eating behaviour. Mediterr J Soc Sci 3, 209–217. [Google Scholar]
- 29. Drake KM, Longacre MR, Dalton MA et al. (2013) Two-method measurement for adolescent obesity epidemiology: reducing the bias in self-report of height and weight. J Adolesc Health 53, 322–327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Elgar FJ, Roberts C, Tudor-Smith C et al. (2005) Validity of self-reported height and weight and predictors of bias in adolescents. J Adolesc Health 37, 371–375. [DOI] [PubMed] [Google Scholar]
- 31. Giacchi M, Mattei R & Rossi S (1998) Correction of the self-reported BMI in a teenage population. Int J Obes Relat Metab Disord 22, 673–677. [DOI] [PubMed] [Google Scholar]
- 32. Hauck FR, White L, Cao G et al. (1995) Inaccuracy of self-reported weights and heights among American Indian adolescents. Ann Epidemiol 5, 386–392. [DOI] [PubMed] [Google Scholar]
- 33. Himes JH, Hannan P, Wall M et al. (2005) Factors associated with errors in self-reports of stature, weight, and body mass index in Minnesota adolescents. Ann Epidemiol 15, 272–278. [DOI] [PubMed] [Google Scholar]
- 34. Jansen W, Van de Looij-Jansen P, Ferreira I et al. (2006) Differences in measured and self-reported height and weight in Dutch adolescents. Ann Nutr Metab 50, 339–346. [DOI] [PubMed] [Google Scholar]
- 35. Chan NP, Choi KC, Nelson EAS et al. (2013) Self-reported body weight and height: an assessment tool for identifying children with overweight/obesity status and cardiometabolic risk factors clustering. Matern Child Health J 17, 282–291. [DOI] [PubMed] [Google Scholar]
- 36. Domingues AP, Silva AM, de Matos MMNG et al. (2013) Accuracy of self-reported measures of height and weight in children and adolescents. Rev Psicolog Crianca Adolesc 2, 41–51. [Google Scholar]
- 37. Yoshitake N, Okuda M, Sasaki S et al. (2012) Validity of self‐reported body mass index of Japanese children and adolescents. Pediatr Int 54, 397–401. [DOI] [PubMed] [Google Scholar]
- 38. Rodrigues PRM, Gonçalves-Silva RMV & Pereira RA (2013) Validity of self-reported weight and stature in adolescents from Cuiabá, Central-Western Brazil. Rev Nutr 26, 283–290. [Google Scholar]
- 39. Enes CC, Fernandez PMF, Voci SM et al. (2009) Validity and reliability of self-reported weight and height measures for the diagnoses of adolescent’s nutritional status. Rev Bras Epidemiol 12, 627–635. [Google Scholar]
- 40. Seghers J & Claessens AL (2010) Bias in self-reported height and weight in preadolescents. J Pediatr 157, 911–916. [DOI] [PubMed] [Google Scholar]
- 41. Zhou X, Dibley MJ, Cheng Y et al. (2010) Validity of self-reported weight, height and resultant body mass index in Chinese adolescents and factors associated with errors in self-reports. BMC Public Health 10, 190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Brettschneider A-K, Schaffrath Rosario A, Wiegand S et al. (2015) Development and validation of correction formulas for self-reported height and weight to estimate BMI in adolescents. Results from the KiGGS study. Obes Facts 8, 30–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Legleye S, Beck F, Spilka S et al. (2014) Correction of body-mass index using body-shape perception and socioeconomic status in adolescent self-report surveys. PLoS One 9, e96768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Pérez A, Gabriel KP, Nehme EK et al. (2015) Measuring the bias, precision, accuracy, and validity of self-reported height and weight in assessing overweight and obesity status among adolescents using a surveillance system. Int J Behav Nutr Phys Act 12, 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Ghosh-Dastidar MB, Haas AC, Nicosia N et al. (2016) Accuracy of BMI correction using multiple reports in children. BMC Obes 3, 37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Beck J (2012) Accuracy of self-reported height and weight in children aged 6 to 11 years. Prev Chronic Dis 9, e119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Ekström S, Kull I, Nilsson S et al. (2015) Web-based self-reported height, weight, and body mass index among Swedish adolescents: a validation study. J Med Internet Res 17, e73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. De Vriendt T, Huybrechts I, Ottevaere C et al. (2009) Validity of self-reported weight and height of adolescents, its impact on classification into BMI-categories and the association with weighing behaviour. Int J Environ Res Public Health 6, 2696–2711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Wang Z, Patterson CM & Hills AP (2002) A comparison of self‐reported and measured height, weight and BMI in Australian adolescents. Aust N Z J Public Health 26, 473–478. [DOI] [PubMed] [Google Scholar]
- 50. Tienboon P, Wahlqvist ML & Rutishauser IH (1992) Self-reported weight and height in adolescents and their parents. J Adolesc Health 13, 528–532. [DOI] [PubMed] [Google Scholar]
- 51. Moher D, Liberati A, Tetzlaff J et al. (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med 151, 264–269. [DOI] [PubMed] [Google Scholar]
- 52. Spano S (2004) Stages of Adolescent Development. Ithaca, NY: Cornell University, University of Rochester, and the New York State Center for School Safety. [Google Scholar]
- 53. Whiting PF, Rutjes AW, Westwood ME et al. (2011) QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med 155, 529–536. [DOI] [PubMed] [Google Scholar]
- 54. Borenstein M, Hedges LV, Higgins JP et al. (2009) Introduction to Meta-Analysis. Chichester: Wiley. [Google Scholar]
- 55. Higgins JP, Thompson SG, Deeks JJ et al. (2003) Measuring inconsistency in meta-analyses. BMJ 327, 557–560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Egger M, Smith GD, Schneider M et al. (1997) Bias in meta-analysis detected by a simple, graphical test. BMJ 315, 629–634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Dear KB & Begg CB (1992) An approach for assessing publication bias prior to performing a meta-analysis. Stat Sci 7, 237–245. [Google Scholar]
- 58. Cooper H, Hedges LV & Valentine JC (2009) The Handbook of Research Synthesis and Meta-Analysis. New York: Russell Sage Foundation. [Google Scholar]
- 59. Abalkhail BA, Shawky S & Soliman NK (2002) Validity of self-reported weight and height among Saudi school children and adolescents. Saudi Med J 23, 831–837. [PubMed] [Google Scholar]
- 60. Brault M-C, Turcotte O, Aimé A et al. (2015) Body mass index accuracy in preadolescents: can we trust self-report or should we seek parent report? J Pediatr 167, 366–371. [DOI] [PubMed] [Google Scholar]
- 61. Chau N, Chau K, Mayet A et al. (2013) Self-reporting and measurement of body mass index in adolescents: refusals and validity, and the possible role of socioeconomic and health-related factors. BMC Public Health 13, 815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Dalton WT III, Wang L, Southerland JL et al. (2014) Self-reported versus actual weight and height data contribute to different weight misperception classifications. South Med J 107, 348–355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Lee B, Chung S-J, Lee S-K et al. (2013) Validation of self-reported height and weight in fifth-grade Korean children. Nutr Res Pract 7, 326–329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Morrissey SL, Whetstone LM, Cummings DM et al. (2006) Comparison of self‐reported and measured height and weight in eighth-grade students. J Sch Health 76, 512–515. [DOI] [PubMed] [Google Scholar]
- 65. Robinson L, Suminski R, Perez G et al. (2014) Accuracy of self-reported height and weight in low-income, rural African American children. J Child Adolesc Behav 2, 144. [Google Scholar]
- 66. Rasmussen M, Holstein BE, Melkevik O et al. (2013) Validity of self-reported height and weight among adolescents: the importance of reporting capability. BMC Med Res Methodol 13, 85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Linhart Y, Romano-Zelekha O & Shohat T (2010) Validity of self-reported weight and height among 13-14 year old schoolchildren in Israel. Isr Med Assoc J 12, 603–605. [PubMed] [Google Scholar]
- 68. Fortenberry JD (1992) Reliability of adolescents’ reports of height and weight. J Adolesc Health 13, 114–117. [DOI] [PubMed] [Google Scholar]
- 69. Gebremariam MK, Andersen LF, Bjelland M et al. (2015) Are weight-related attitudes and behaviours associated with the accuracy of BMI derived from self-reported weight and height among 13-year-olds? Scand J Public Health 43, 130–137. [DOI] [PubMed] [Google Scholar]
- 70. Must A, Dallal GE & Dietz WH (1991) Reference data for obesity: 85th and 95th percentiles of BMI (wt/ht2) and triceps skinfold thickness. Am J Clin Nutr 53, 839–846. [DOI] [PubMed] [Google Scholar]
- 71. Rolland-Cachera MF (2011) Childhood obesity: current definitions and recommendations for their use. Pediatr Obes 6, 325–331. [DOI] [PubMed] [Google Scholar]
- 72. Lipsey MW & Wilson DB (2001) Practical Meta-Analysis. Thousand Oaks, CA: SAGE Publications, Inc. [Google Scholar]
- 73. Duval S & Tweedie R (2000) Trim and fill: a simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics 56, 455–463. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
For supplementary material accompanying this paper visit https://doi.org/10.1017/S1368980018000368.
click here to view supplementary material