Abstract
Klebsiella pneumoniae sequence type (ST) 17 is a global problem clone that causes multidrug-resistant (MDR) hospital infections worldwide. In 2008–2009, an outbreak of MDR ST17 occurred at a neonatal intensive care unit (NICU) in Stavanger, Norway. Fifty-seven children were colonized. We observed intestinal persistence of ST17 in all of the children for up to two years after hospital discharge. Here, we investigated the within–host evolution of ST17 in 45 of those children during long-term colonization and compared the outbreak with 254 global strains. Ninety-two outbreak-related isolates were whole-genome sequenced. They had capsule locus KL25, O locus O5 and carried yersiniabactin. During within–host colonization ST17 remained stable with few single nucleotide polymorphisms, no acquisition of antimicrobial resistance (AMR) or virulence determinants, and persistent carriage of a bla CTX-M-15-encoding IncFII(K) IncFIB(K) plasmid (pKp2177_1). The global collection included ST17 from 1993 to 2020 from 34 countries, that were from human infection (41.3%), colonization (39.3%) and respiratory specimens (7.3%), from animals (9.3%), and from the environment (2.7%). We estimate that ST17 emerged mid-to-late 19th century (1859, 95 % HPD 1763–1939) and diversified through recombinations of the K and O loci to form several sublineages, with various AMR genes, virulence loci and plasmids. There was limited evidence of persistence of AMR genes in any of these lineages. A globally disseminated sublineage with KL25/O5 accounted for 52.7 % of the genomes. It included a monophyletic subclade that emerged in the mid-1980s, which comprised the Stavanger NICU outbreak and 10 genomes from three other countries, which all carried pKp2177_1. The plasmid was also observed in a KL155/OL101 subclade from the 2000s. Three clonal expansions of ST17 were identified; all were healthcare-associated and carried either yersiniabactin and/or pKp2177_1. To conclude, ST17 is globally disseminated and associated with opportunistic hospital-acquired infections. It contributes to the burden of global MDR infections, but many diverse lineages persist without acquired AMR. We hypothesize that non-human sources and human colonization may play a crucial role for severe infections in vulnerable patients, such as preterm neonates.
Keywords: Klebsiella pneumoniae, ST17, in vivo evolution, infection, colonization, global dynamics
Data Summary
The genome sequences generated in this study have been deposited at the European Nucleotide Archive under BioProject PRJEB36392. The BioSample accession numbers and associated metadata for the genomes are available in Table S1 (available in the online version of this article). The completed annotated genome assembly of Kp2177 is available in GenBank under accession numbers CP075591 (chromosome), CP075592 (pKp2177_1), CP075593 (pKp2177_2) and CP075594 (pKp2177_3). The global dataset of 300 ST17 genomes is available for interactive viewing in Microreact at https://microreact.org/project/kpst17.
Impact Statement.
Klebsiella pneumoniae is an opportunistic pathogen that frequently causes hospital-associated multidrug-resistant (MDR) infections. Infections with K. pneumoniae strains that are resistant to third-generation cephalosporins and/or carbapenems are considered to be a major public health threat, as there are limited treatment options available. Some MDR K. pneumoniae clones, including ST307 and ST258, are global problem clones because they disproportionately contribute to the burden of MDR infections and are common causes of such infections and/or outbreaks in hospitals around the world. Here we describe another such clone, ST17, which caused an MDR outbreak in our neonatal intensive care unit, affecting 57 children. We found that this clone underwent minor within–host evolution during two years of long-term gastrointestinal colonization after hospital discharge. We then investigated the evolutionary history of ST17 globally, as it had not previously been studied. When we compared ST17 isolates from around the world with the isolates from our hospital, we discovered that whilst ST17 with antimicrobial resistance has contributed to outbreaks in other neonatal care units, it also frequently causes infections or colonizes humans and non-human sources without any antimicrobial resistance.
Introduction
The Gram-negative bacteria Klebsiella pneumoniae are a common cause of infections in both healthcare and community settings [1, 2]. Notably, they are a major pathogen responsible for bacterial outbreaks in neonatal intensive care units (NICUs) [3–5]. Several sequence types (STs) of K. pneumoniae are associated with multidrug resistance [6]. Some clones carry genes encoding extended-spectrum beta-lactamases (ESBLs) or carbapenemases and co-linked resistance determinants, resulting in severely limited treatment options [5]. Some multidrug-resistant (MDR) clones remain localized, e.g. within a healthcare or community setting, whilst others have spread across continents and become global problem clones [5]. One such clone is K. pneumoniae ST17, which has been detected in several countries, often with an MDR phenotype causing difficult-to-treat hospital infections [5, 7–9]. ST17 has also been found colonizing healthy humans in the community setting [10–12], in animals [13, 14] and in the environment [15–17].
From November 2008 to April 2009 an outbreak caused by ESBL-producing (bla CTX-M-15) ST17 occurred in a NICU at Stavanger University Hospital, Norway [8]. The outbreak was first discovered when ESBL-producing K. pneumoniae was recovered from three neonates: one clinical sample from conjunctiva and two routine screening samples. Subsequent screening revealed that 92 % (22/24) of the patients in the ward were colonized with ESBL-producing K. pneumoniae . The index isolate of the outbreak (Kp2177) was isolated from breast milk from one of the mothers. During the outbreak, a total of 57 children were colonized with ST17. Only one of them developed a bloodstream infection (BSI), which was successfully treated with meropenem.
A follow-up study revealed intestinal persistence of the ST17 strain in all 57 children after hospital discharge, all carrying a bla CTX-M-15-encoding IncFII(K) IncFIB(K) plasmid (pKp2177_1), for up to two years (median 12 months) [18, 19]. Risk factors for prolonged carriage were identified as having received antibiotics (ampicillin and gentamicin intravenously) during hospitalization or being delivered by caesarean section [19]. Phenotypic testing of plasmid stability revealed that there were little to no fitness costs associated with carrying the pKp2177_1 plasmid [18].
Here, we first characterized the genomic diversity and in vivo evolution of ST17 within and between 45 NICU patients in Stavanger to study the evolution of this strain during long-term gut colonization. As the bla CTX-M-15 ST17 strain persisted for up to two years in these children, we wanted to examine how the in vivo evolution compared to the evolutionary dynamics of ST17 on a global scale. Whilst ST17 has been observed in several countries and settings, specific analyses to determine its global dynamics have not been reported previously. We therefore carried out a literature and genome search to assess the global presence of ST17, followed by core genome evolutionary analyses of 300 ST17 strains from around the world that were isolated from human infections and colonization, animals, plants and water.
Methods
Collection and sequencing of the Stavanger NICU outbreak isolates
During the outbreak in the Stavanger NICU, 57 children were colonized. They were examined for intestinal persistence over a two-year period [19], and for 45 of the children, we had two ST17 isolates available for genomic comparison in this study. For each child, one sample was isolated during the NICU stay (between January and March 2009) and another after hospital discharge (between June 2009 and November 2010). The duration of colonization between the two isolates from each child ranged 3–21 months (median 11). All of the colonizing isolates were from faecal swabs, except one nasal swab isolate. We performed whole-genome sequencing using Illumina MiSeq (n=46) or HiSeq (n=46) technology to produce 300 or 150 bp paired-end short-read sequences of in total 92 isolates: the 45 NICU and 45 follow-up isolates, the BSI isolate and the index (breast milk) isolate Kp2177. BioSample accessions are given in Table S1 (available in the online version of this article). To generate a reference genome for the outbreak, Kp2177 was also long-read sequenced with the Oxford Nanopore Technologies platform, and hybrid assembly was performed to resolve the complete genome sequence (deposited in GenBank under accessions CP075591–94; details in Methods S1).
Global dataset of ST17 genomes
A literature search querying PubMed for titles or abstracts containing the word ‘ST17’ with and without ‘Klebsiella pneumoniae’ resulted in 36 peer-reviewed articles that contributed novel data on K. pneumoniae ST17 (as of November 2021), but only 29 ST17 isolates were whole-genome sequenced and available for download. We therefore also included ST17 genomes from other sources: a recent study analysed 13 156 publicly available K. pneumoniae genomes and identified their STs [20]. Those that were confirmed ST17 and had <500 assembled contigs, known year of collection and sample source (n=149) were included in our global dataset. Additionally, we included 64 ST17 genomes from the recent SpARK study [17] and 41 ST17 genomes from Norwegian surveillance studies that were not linked to the Stavanger NICU outbreak [11, 21–23]. For analyses of global dynamics, we also included 46 of the Stavanger NICU outbreak genomes, resulting in a global dataset of 300 genomes (BioSample accessions are given in Table S2).
Genome assembly and genotyping
All short-read Illumina sequences were filtered with TrimGalore v0.6.6 (https://github.com/FelixKrueger/TrimGalore) to exclude low-quality reads and adapter contamination before de novo assembly was performed with Unicycler v0.4.8 [24], using SPAdes v3.13.0 [25] and Pilon v1.23 [26], with default settings. Detection of antimicrobial resistance (AMR) and virulence genes was based on analysis of genome assemblies using Kleborate v2.2.0 [20], which uses a manually curated version of CARD v3.1.13 for acquired AMR determinants. We also used SRST2 v0.2.0 [27] to query the unassembled short-reads directly, using the same database. If a gene was missing in the Kleborate analysis of assemblies but found with SRST2 analysis of reads, we considered it present in the genome. Capsule (K) and lipopolysaccharide (LPS) O-antigen serotype predictions were performed with Kaptive v2.0.0; as low-confidence calls are most likely due to assembly quality, we reported the best matching K and O loci regardless of confidence call, except for those called KL107 with low confidence, which were designated unknown [28]. Plasmid replicons were detected using Abricate v1.0.1 (https://github.com/tseemann/abricate) with the PlasmidFinder database v2021-01-13 (https://bitbucket.org/genomicepidemiology/plasmidfinder_db).
Between– and within–host comparison of the Stavanger NICU outbreak genomes
To identify single nucleotide polymorphisms (SNPs) between and within the outbreak genomes, core genome alignments were produced with RedDog v1beta.11 (https://github.com/katholt/RedDog) by aligning the raw reads of the 92 outbreak genomes against Kp2177. Within–host SNPs were defined as SNPs between the NICU and follow-up genome of a child, from the overall core genome alignment. Bowtie2 v2.3.5.1 [29] was used for sequence alignment and SAMTools v1.9 [30] was used to identify SNPs. Further details are given in Methods S1. RAxML v8.2.12 [31] was used to infer a core genome maximum likelihood (ML) phylogeny from the chromosomal alignment of 113 SNPs. To estimate a substitution rate (SNPs/year) for the outbreak, we divided the number of SNPs against Kp2177 from each genome by the difference in isolation time.
To identify genes that had been gained or lost between the NICU and follow-up genomes, we characterized their pangenome with Panaroo v1.2.7 [32], using annotations from Prokka v1.14.6 [33] as input. As all the genomes belonged to the same outbreak strain and we wanted to identify any changes in gene content, we ran Panaroo using the sensitive mode with the protein family identity set to 90 %. To identify whether gene gain/loss events were independent or if genes were gained/lost together in larger events (such as recombinations or movement of mobile genetic elements like plasmids), we counted any genes that were co-located on the same contig within 1000 bp of each other and showed the same presence/absence pattern as being gained/lost together in one event.
Phylogenetic inference and molecular dating of the global ST17 collection
We performed ML and Bayesian phylogenetic analyses of 300 genomes to compare the Stavanger NICU outbreak (n=44 follow-up faecal, 1 blood, 1 breast milk) with ST17 from other geographical locations and collection years (n=254), and to estimate the evolutionary rate of the clone. We generated a core chromosomal SNP alignment of the genomes against Kp2177 with RedDog as described in Methods S1. Gubbins v3.1.6 [34] was used to identify and filter recombinant SNPs from the alignment, which was then passed to RaxML v8.2.12 [31] to infer an ML phylogeny. We investigated the relationship between the root-to-tip distance in the ML tree and the years of isolation using linear regression in TempEST v1.5.3 [35]. To estimate the evolutionary rate and dated phylogeny, we performed Bayesian phylodynamic analysis with beast2 v2.6.5 [36] on a subset of 145 of the 300 genomes, which were selected to capture the diversity across the clades in the full ML tree as detailed in Methods S1. The temporal signal of the clone was confirmed by performing date-randomization tests (Fig. S1).
Statistical analyses
All statistical analyses were performed with R version 4.0.2 (2020-06-22) [37]. Paired data were analysed with two-tailed Wilcoxon paired signed rank tests. Comparisons of groups were analysed with Wilcoxon signed rank tests and binomial data were compared with chi square tests. P-values <0.05 were considered statistically significant.
Results
The Stavanger NICU outbreak
The index isolate (Kp2177) of the Stavanger NICU outbreak, which was isolated from breast milk, belonged to ST17, had capsule locus KL25 and O locus O5, and consisted of a 5.38 Mbp chromosome and three plasmids [pKp2177_1, 182 kbp, IncFII(K) and IncFIB(K); pKp2177_2, 83 kbp, IncR and IncFIA(H1); and pKp2177_3, 3 kbp, no plasmid replicon marker detected]. A total of 5303 genes were annotated in the genome. pKp2177_1 harboured the ESBL gene bla CTX-M-15, the beta-lactamase gene bla TEM1-D and the aminoglycoside resistance gene aac(3)-IIa. pKp2177_2 carried strAB, dfrA14, sul2 and catA2, encoding resistance towards streptomycin, trimethoprim, sulphonamides and chloramphenicol, respectively. Of known virulence factors, yersiniabactin (ybt 16) was chromosomally encoded on an ICEKp12 mobile genetic element. No other siderophores or hypermucoviscosity-encoding genes were present.
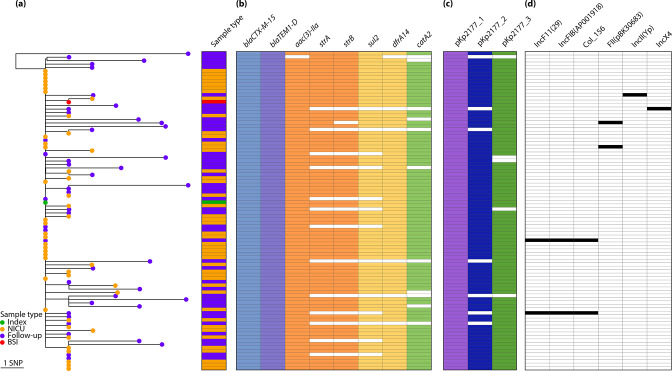
All of the colonizing NICU (n=45) and subsequent follow-up isolates (n=45) belonged to the same ST17 strain, with KL25/O5 and ≤8 SNPs compared to the index Kp2177 isolate. The three Kp2177 plasmids were conserved in all 45 NICU genomes, with high sequence coverage (98.3 –100 %, Table S1). The AMR and virulence genes in Kp2177 were also present in all of the NICU genomes, except for one that did not harbour catA2 (however the follow-up genome for this child did). There was more variation in the follow-up genomes, which were collected up to 21 months (median 11) after initial colonization (Fig. 1). The bla CTX-M-15-encoding plasmid pKp2177_1 was persistent in all of the strains with minimal variation (≤1 SNP and 68.8–100% sequence coverage, median 100%). The pKp2177_2 and pKp2177_3 plasmids varied in coverage and AMR gene content and were missing in 16% (n=7) and 11 % (n=5) of the 45 follow-up genomes. In six of the follow-up genomes we detected plasmid replicon markers that were not present in Kp2177 or in the NICU genomes. However, none of the 90 colonizing genomes encoded additional AMR or virulence determinants not present in Kp2177. Some children were given antibiotics during their NICU stay or after hospital discharge (Table S3). No significant difference in the number of AMR genes was observed between the children that had received antibiotics (n=34) and those that did not (n=11) (P=0.92).
Fig. 1.
Phylogeny of 92 Klebsiella pneumoniae ST17 outbreak isolates and their gene content. (a) Midpoint-rooted maximum likelihood phylogeny of the 45 NICU (orange tip) and 45 follow-up (purple) isolates from colonization and the BSI isolate (red) against the outbreak index isolate Kp2177 (green). (b) Presence (colour) or absence (white) of AMR genes as listed in the columns (blocks are coloured by drug class). (c) Presence (colour) or absence of the Kp2177 plasmids and (d) of acquired plasmid replicon markers.
Only one child developed a systemic infection (KN_0144A) [8]. The BSI genome also belonged to the Kp2177 strain and was highly similar (1 SNP, wza-G178A), with no acquisition of genes that were unique to this genome. The follow-up genome for this patient (KN_0144A-L), which was isolated from gut colonization 14 months after the BSI occurred, had the most SNPs of any in the outbreak (n=10). None of them were present in other outbreak genomes (Fig. 1a and Table S4), nor in the global ST17 dataset (see below).
Diversity and evolution within and between hosts
To assess the diversity and in vivo evolution of the outbreak strain over a 21 month period, we performed a core genome phylogenetic analysis using Kp2177 as the reference genome. In total, 120 unique SNPs were identified, 113 of which were in positions in the chromosome, 3 in pKp2177_1 and 4 in pKp2177_2 (full list of SNPs and their consequences are given in Table S4). The 45 NICU genomes differed from Kp2177 by 0–3 SNPs (median 1). In contrast, the 45 follow-up genomes differed from the index by 0–8 SNPs (median 2) and showed significantly more evolutionary divergence from Kp2177 (P<0.0001). Based on the chromosomal alignment and the time between Kp2177 and the isolate collection dates, we calculated a substitution rate for the outbreak of 2.60 SNPs/year (95 % CI 1.96–3.24), or 4.84×10−7 SNPs/year/site (95 % CI 3.64x10−7–6.02×10−7).
We observed few genome changes within hosts during up to 21 months of colonization. Within–host SNPs were detected in 84.4 % (38/45) of the NICU and follow-up pairs (Table S3). The number of SNPs in each child ranged from 0 to 10 (median 2), of which up to 6 were nonsynonymous SNPs (nsSNPs) and the rest synonymous or intergenic. Most of the SNPs (91.7%, n=110/120) occurred only once, in one genome each. However, in eight genes, >1 SNP was observed, in different genomes (Table S4). Notably, two genes had several SNPs: barA and uvrY, that make up the BarA–UvrY two-component system (TCS) [38]. In uvrY, there were two SNPs leading to different amino acid changes in the same codon (G76W, G76R). In barA, four nsSNPs were present, two resulting in premature stop codons (Q260*, R305H, V311G and Q466*). These six mutations were variably present in nine genomes from children that were colonized >6 months (median 1.2 years). Of these mutations, only uvrY-G76R was also present in the global ST17 dataset (see below), in one genome (KP_NORM_URN_2013_95870), but an additional 12 nsSNPs in these two genes were present across the global phylogeny in 19 genomes.
Among the 91 colonizing genomes there were 5742 unique genes. Of those, 76.5 % (n=4393) were core, i.e. present in all of the genomes. The accessory genes were either very common (60.3 % of the 1349 accessory genes were present in >90 % of the genomes) or rare (32.2 % were present in <5 % of genomes). Overall, there was a significant within–host increase in the number of genes in the follow-up (median 5279; range 5081–5428) compared to the NICU genomes (median 5253; 5175–5306) (P=0.005, Fig. S2). Within each child, between 5 and 166 (median 42) gene gain or loss events occurred during the colonization period. In five of the 45 children, more than 150 genes had been gained in multiple events; none of the genes encoded known AMR or virulence determinants or plasmid replicon markers. There were also two children in which over 150 chromosomal genes had been lost in multiple events (Table S3).
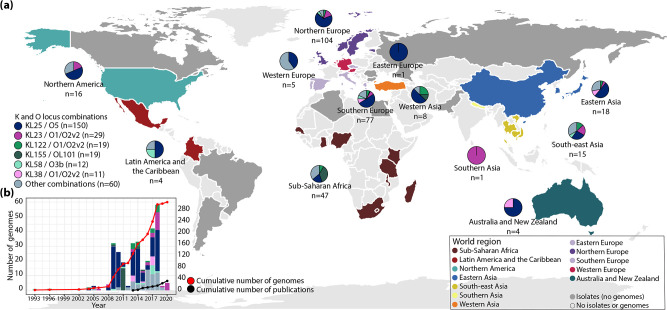
ST17 is globally disseminated and highly diverse
To understand the ST17 variation in the Norwegian children in the context of the global diversity of this strain, we included 300 ST17 genomes for comparative and phylogenetic analyses. The genomes were globally distributed, including isolates from 34 countries in 12 United Nations defined geographical regions over a 28 year period (1993–2020) (Fig. 2 and Table S2). The majority were from humans (88%, n=264/300): infection [n=124, most from blood (n=79) or urine (n=43)], colonization [n=118, most from faeces (n=109, the Stavanger NICU outbreak accounted for 44 of these)] and respiratory sites with unknown infection status (n=22). The genomes from non-human sources (12%, n=36/300) came from animals (n=26, from dogs, broilers, a chicken, cows, a fly, pigs and turkeys), marine bivalves (n=2), different sources of water (n=7) and a sugar cane (n=1). The animal genomes were sampled from intestinal isolates, except one from a chicken meat isolate.
Fig. 2.
Geographical distribution of Klebsiella pneumoniae ST17 genomes, their K and O loci, and reports of ST17. (a) World map highlighting countries of collection for ST17 genomes that were available for download (coloured by region as in Fig. 3) and countries with isolates reported but not included in the global dataset (coloured dark grey). The pie charts show the distribution of K and O loci per region (n, number of genomes), highlighting loci with ≥10 genomes. (b) Number of ST17 genomes by collection year (bars, coloured by KL/OL) and cumulative number (red line, secondary axis), and cumulative number of reports of ST17 in PubMed abstracts or titles (black line, secondary axis) as of November 2021.
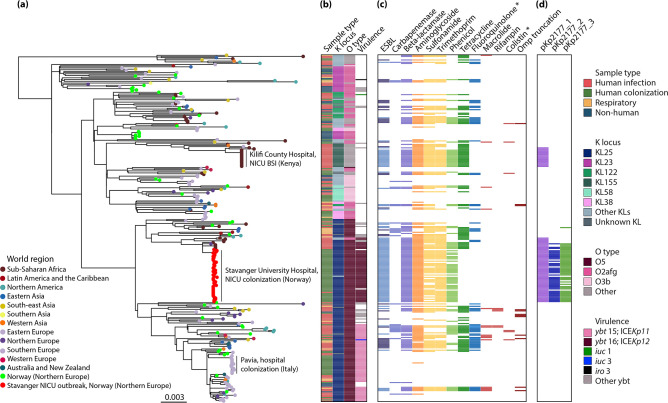
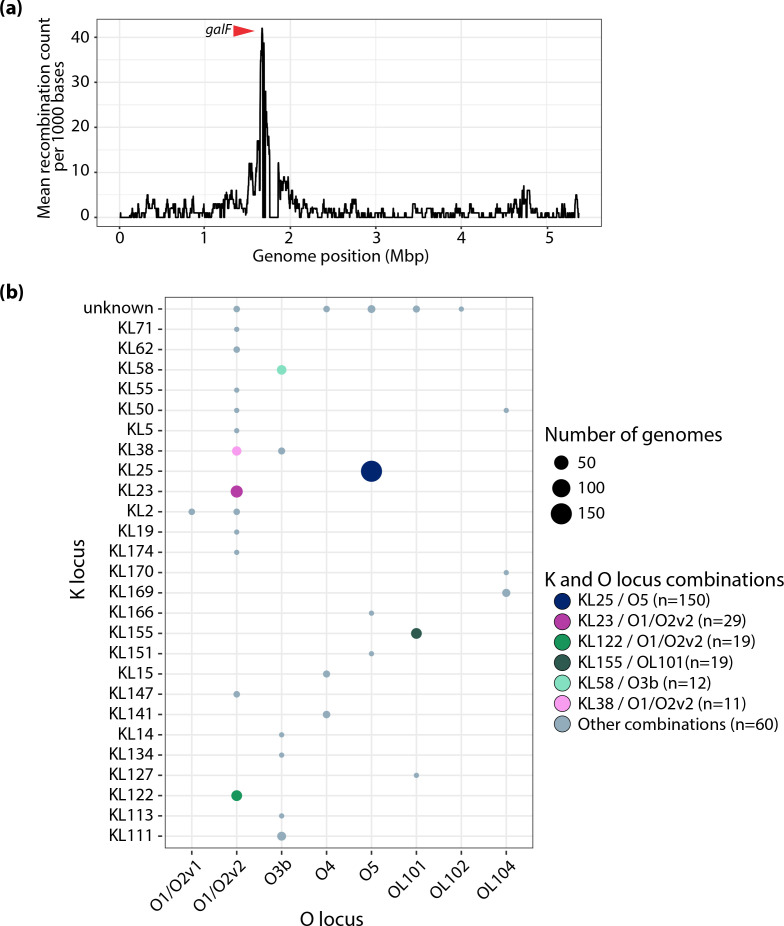
An ML phylogeny of the 300 genomes was created (Fig. 3, also available for interactive viewing at https://microreact.org/project/kpst17). Due to the size and diversity of the dataset, 145 representative sequences were selected to estimate the evolutionary rate of ST17 using Bayesian modelling in beast2 (Fig. S3) (see details in Methods S1). The Bayesian analysis of 11 345 SNPs in 145 genomes indicated that ST17 emerged in 1859 (95 % HPD 1763–1939) with an estimated evolutionary rate of 4.04×10−7 substitutions/site/year (95 % HPD 2.30×10−7–5.79×10−7), equivalent to 2.17 SNPs per year. Since its emergence, the clone has undergone several recombination events (the ratio of nucleotide substitutions introduced by recombination vs point mutation was estimated as r/m=3.27), which were centred in a hotspot surrounding the K and O loci (Fig. 4a). These recombinations have led to a diversification of ST17 strains by creating distinct sublineages with different combinations of K and O loci. In total, there were 8 O and 27 K loci (including unknown KLs), and 34 combinations of these, among the 300 ST17 genomes (Fig. 4b). Over half (52.7%, n=158/300) of the genomes belonged to a clade that had KL25/O5 (except for two genomes with KL2/O2v1, one KL166/O5 and five unknown KL25/O5) that emerged in 1943 (95 % HPD 1905–1972). This clade was found in 19 countries across 11 world regions (all except Southern Asia), and in all sample types. The genomes in the remaining sublineages of ST17 were found in 29 countries (all world regions except Eastern Europe) and had a much larger variety of K and O loci (32 combinations), with KL23/O1/O2v2 (n=29), KL155/OL101 (n=19) and KL122/O1/O2v2 (n=19) being the most prevalent (Fig. 2). KL23/O1/O2v2 and KL122/O1/O2v2 were intermingled with genomes carrying other combinations of K/O loci, whilst KL155/OL101 formed a monophyletic clade.
Fig. 3.
Global phylogeny of 300 Klebsiella pneumoniae ST17 genomes. (a) Maximum likelihood tree with tips coloured by region of collection. Additionally, the Stavanger NICU outbreak genomes are coloured red and other genomes from Norway green. The three clonal expansions that were observed in ST17 are labelled. (b) Sample type and loci as indicated in the column names. The most prevalent loci are indicated in the inset legend. (c) Presence (colour) or absence (white) of genes encoding resistance to the listed antimicrobial resistance drug classes (blocks are coloured by drug class). Lighter colour in the ESBL column indicates bla CTX-M-15. (d) Presence (colour) or absence (white) of the Kp2177 plasmids. Several plasmid replicon markers were present across ST17; these are shown in Fig. S4. More details about the metadata and genotypes are available for interactive viewing at https://microreact.org/project/kpst17. *, acquired genes and mutations.
Fig. 4.
Recombinations and K/O loci diversity. (a) Recombination counts per base calculated over non-overlapping windows of 1000 base pairs. There is a peak in the recombination count, which surrounds the K and O loci. The red arrow indicates the gene galF, which is the 5’-most K locus gene. (b) Combinations of K and O loci found among the 300 genomes. Bubbles indicate the number of genomes and are coloured by the K/O combinations as in Figs 2 and 3.
The dominant KL25/O5 clade was also distinct from the rest of the tree by high prevalence of yersiniabactin: 84.2 % (133/158) of the genomes in this clade carried a yersiniabactin locus, compared to 7.0 % (10/142) of the genomes in the rest of the tree. The majority of the yersiniabactin loci were ybt 15, located on ICEKp11, (n=63, complete or truncated) and ybt 16, on ICEKp12, (n=52, complete or truncated), which formed distinct subclades in the KL25/O5 sublineage (see Fig. 3). Other yersiniabactin loci (n=10) were sporadically present across the tree, in 28 genomes, including in these subclades. There were few hypervirulence-associated genes, but aerobactin (iuc 1 and 3) or salmochelin (iro 3) with incomplete hypermucoviscosity rmp genes were present in three genomes.
Several different AMR determinants (n=81) and plasmid replicon markers (n=44) were detected in the ST17 genomes (Table S2 and Fig. S4). In the overall collection, the number of AMR genes ranged from 0 to 19 (median 3), with 42.7 % (128/300) of genomes having no AMR genes present at all and 48.3 % (145/300) being MDR (carried resistance genes to ≥1 antimicrobial agent in >3 antimicrobial classes). We observed no differences in the number of AMR determinants or MDR genomes between the samples from humans (infection, respiratory and colonization). However, significantly fewer AMR genes were detected in the non-human isolate genomes (non-human: median 0, range 0–11 vs human: median 4.5, range 0–19, P<0.0001). Of the AMR encoding genomes, 127 carried ESBL genes: bla CTX-M-15 (n=92), bla CTX-M-14 (n=20), bla CTX-M-27 (n=1), bla CTX-M-63 (n=1), bla SHV-12 (n=13), bla SHV-2 (n=3), bla SHV-5 (n=2), bla SHV-7 (n=1) and bla SHV-24 (n=1); and 25 carried carbapenemase-encoding genes: bla KPC-2 (n=10), bla NDM-1 (n=6), bla KPC-3 (n=4), bla OXA-48 (n=3), bla NDM-7 (n=1), bla OXA-181 (n=1) and bla VIM-1 (n=1). The AMR genes were found across many sublineages, but there was limited evidence of AMR persistence within subclades.
Clonal expansions of ST17 were hospital-associated and carried yersiniabactin or a bla CTX-M-15-encoding plasmid
Only three clonal expansions (≥15 genomes) were observed across the global dataset, and all were hospital-associated (see Fig. 3). One of these included the Stavanger NICU outbreak, which formed a monophyletic clade. Its closest neighbours were a cluster of four identical NICU blood isolates from Kilifi, Kenya (2009; 47 SNPs from Kp2177), five blood isolates from Nigeria (2009; 40 SNPs, 2015–2016; 143–831 SNPs) and one from the UK (2011; 38 SNPs) (Fig. S5). The most recent common ancestor (MRCA) for this cluster was in 1984 (95 % HPD 1967–1998). These genomes carried the bla CTX-M-15-encoding pKp2177_1 plasmid that was persistent in the Stavanger NICU outbreak (≤1 SNP and 100 % sequence coverage), and were highly similar, except for four genomes from Nigeria; two that had KL2/O2v1 instead of KL25/O5, and two that carried ybt 13 (on ICEKp2) rather than ybt 16 (on ICEKp12).
The bla CTX-M-15 pKp2177_1 plasmid was present (≤2 SNPs and ≥95 % sequence coverage, median 100%) in one other clonal expansion of ST17, in a cluster of 17 genomes, which all had KL155/OL101, of which only one genome encoded yersiniabactin (ybt 9 on ICEKp3) (see Fig. 3). These were invasive isolates from Kilifi, Kenya in 2011 (n=15, 1 SNP between them), Nigeria in 2015 (n=1, 89 SNPs from the ones from Kenya) and Ghana (n=1, 90 SNPs) in 2015, with an MRCA in 2000 (95 % HPD 1990–2007).
The last of the three clonal expansions consisted of 16 isolates from gut colonization in a hospital in Pavia, Italy during 2018 [17] (see Fig. 3). These had KL25/O5 and carried ybt 15 (on ICEKp11) but no AMR genes [except one with aac(6′)-Ib-Suzhou]. In 2017–2018, 48 other ST17s were isolated from different sources in Pavia, Italy. These were not related to the clonal expansion in the local hospital, but were found across the entire global phylogeny, carrying a range of KL/OLs, and with varying presence of yersiniabactin and AMR genes. The same was the case for the Norwegian ST17 genomes that were not part of the Stavanger NICU outbreak (n=43).
To see if the pKp2177_1 plasmid had spread in Norway between STs, we screened 3212 non-ST17 K. pneumoniae genomes for the presence of the bla CTX-M-15 pKp2177_1 plasmid (see Methods S1). These covered 1076 STs from multiple human and non-human sources in Norway between 2001 and 2020. We found only one genome that carried this plasmid, with 100 % sequence coverage; a clinical ST307 urine isolate from 2013, previously described in [39].
Discussion
In this study we investigated the global dynamics of K. pneumoniae ST17 and the in vivo evolution within and between children that were colonized following an outbreak in an NICU in Stavanger, Norway in 2008–2009. During up to 21 months of colonization, few changes (0–10 SNPs) occurred in the core genome, and the majority were present in only one genome each. However, there was one SNP that was shared among several follow-up genomes and it was also found in one genome in the global dataset. This was in the gene uvrY (G76R). UvrY is a response regulator that is part of a TCS with BarA, a sensor kinase, that has been described in uropathogenic Escherichia coli [38]. Across the outbreak and global ST17, several independent nsSNPs were seen in these two genes. Pernestig et al. [38] found that mutations in either of those genes can affect survival in long-term competition cultures; when using media with gluconeogenic carbon sources, E. coli with knockout mutations in barA or uvrY had a clear growth advantage over the wild-type, whereas when using media with carbon sources feeding into the glycolysis, the wild-type had the growth advantage. Other studies found that homologues of these genes in other bacteria led to decreased virulence in infection models [40, 41]. It is possible that the mutations in these genes in ST17, if rendering the genes non-functional, gave an advantage to long-term colonization in the gut, which is a source of gluconeogenic carbon.
The Stavanger NICU outbreak strain persistently carried a bla CTX-M-15-encoding IncFII(K) IncFIB(K) plasmid (pKp2177_1) for up to two years, but the presence of other plasmids varied. Whilst some genes were gained during the follow-up period, no additional known virulence- or antibiotic resistance-encoding determinants were acquired. This could be a result of the children acquiring a more diverse microbiome once they left the hospital, enabling horizontal gene transfer to or from the ST17 strains. The outbreak and the global ST17 had overlapping evolutionary rates, but unlike the relatively stable genomes within the Stavanger NICU outbreak, ST17 exists globally with many sublineages, harbouring various AMR determinants and plasmid replicons, frequently carrying yersiniabactin and in a few cases also the hypervirulence-associated aerobactin and salmochelin loci.
The first detected ST17 was isolated from a pig brain in the UK in 1993 [14], and the earliest ESBL-producing isolate was a bla CTX-M-15-carrying clinical isolate from Canada in 2002 [42]. However, the Bayesian phylogeny analysis suggested that ST17 emerged much earlier than this, in the mid-to-late 19th century. ST17 is older, and has a slower evolutionary rate (4.04×10−7 substitutions/site/year), compared to other global problem MDR lineages that have been estimated, such as ST307 (1.18×10−6 substitutions/site/year, MRCA 1994), ST258 (1.03×10−6, 1995) and ST147-KL64 (1.03×10−6, 1994) [39, 43, 44]. Since its emergence, recombination has driven diversification of the K and O biosynthesis loci in ST17, which has led to the formation of several sublineages. This is similar to what has been seen in other MDR clones, including ST258 and ST147 [45].
The MDR clones ST258, ST307 and ST147 frequently encode ESBL or carbapenemase genes [5]. Unlike these, ST17 was not strongly associated with any specific AMR genes. In fact, less than half of the ST17 genomes carried resistance to third-generation cephalosporins and/or carbapenems. On the other hand, 48.3 % (145/300) of the ST17 genomes were MDR, carrying various AMR genes, including carbapenemases in 25 genomes and ESBL in 127, of which 92 carried bla CTX-M-15. MDR strains were found in many sublineages, but there was limited evidence of persistence of any AMR genes within these, nor within specific countries or collection years, with the possible exception of the bla CTX-M-15-encoding pKp2177_1 plasmid, which was present in two clonal expansions.
One of the sublineages, KL25/O5, which emerged in the mid-1940s, contained over half of the ST17 genomes and was globally disseminated. The Stavanger NICU outbreak was located on this sublineage, in a cluster with 10 genomes from Nigeria, Kenya and the UK. They all carried the bla CTX-M-15-harbouring pKp2177_1 plasmid, with an estimated MRCA in 1984. The plasmid was also seen in another sublineage, KL155/OL101, with 17 genomes from Kenya, Ghana and Nigeria (MRCA 2000). The isolates from the two sublineages in Kenya were from 2009 and 2011 and both were from the same NICU in Kilifi County Hospital [46]. In that hospital, ST17 with/without ESBL phenotypes were observed in blood culture isolates almost every year since it first emerged [46], indicating undetected transmission of this strain in the hospital or region, and that the pKp2177_1 plasmid is circulating between ST17 strains. Given the MRCAs of these pKp2177_1 plasmid-encoding clusters and the larger diversity of the pKp2177_1-encoding genomes in Nigeria, it is probable that the plasmid was acquired by an ancestor in Nigeria in the mid-1980s, where it subsequently diversified and transmitted to the other countries, and that the plasmid later transferred into or between these two ST17 subclades, either in Nigeria or Kenya.
In a previous study, phenotypic tests of the pKp2177_1 plasmid were performed. Only minor fitness costs were associated with carriage of pKp2177_1 in the Stavanger NICU outbreak, and the cost did not change during the colonization period, indicating that the plasmid was well adapted to its bacterial host [18]. This may explain why the plasmid continued to persist in vivo outside of the hospital environment, without antibiotic selection pressure, having initially contributed to the host strain’s ability to establish colonization under antibiotic selection. Further, we observed no evidence of plasmid transfer to E. coli in vitro [18] or to other bacterial hosts in vivo during the two years of colonization [19], possibly due to the lack of the transfer region gene trbE, which was observed in all genomes that carried pKp2177_1 (the gene was incomplete with only 65 % sequence coverage and 88 % identity). Additionally, only one of 3212 non-ST17 genomes from Norway carried pKp2177_1, further supporting that pKp2177_1 is well adapted to ST17.
We included two large collections of ST17 from Norway (n=89) and Pavia, Italy (n=64) [17]. The genomes were spread across the ST17 sublineages and were found in several host species and sample types. This shows that the diversified descendants of the ancestral ST17 co-circulate both within and between ecological niches, even in highly localized geographic regions. Further, it suggests that there have been multiple independent importations of ST17 to these locations, and that the same patterns would be observed for other countries given larger sample sizes, which was also the case for ST307 [39]. The NICU outbreaks in the collection indicate that this highly flexible and widely disseminated clone can rapidly colonize neonates in hospital settings. This may be associated with the presence of the bla CTX-M-15 pKp2177_1 plasmid and/or yersiniabactin, although more data would be needed to confirm this: the 2009 NICU outbreaks in Stavanger, Norway and Kilifi, Kenya carried the pKp2177_1 plasmid and ybt 16 on ICEKp12; the 2011 NICU outbreak in Kilifi carried the plasmid but no yersiniabactin locus; and in Pavia, Italy, the genomes did not carry the plasmid, but had ybt 15 on ICEKp11. In addition to these large hospital transmissions, some small local clusters (≤7 genomes) occurred. These were mainly reported from studies investigating the movement of strains in close communities, e.g. circulation of ST17 between animals [22] or between animals and people in the community [13], where the same strain was present in animals and humans, indicating that animals may be reservoirs for ST17.
It has been estimated that around half of healthcare-associated infections caused by K. pneumoniae arise from opportunistic colonizing strains infecting immunocompromised and vulnerable patients, such as neonates [1, 47, 48]. Consistent with this, the ST17 NICU outbreak in Stavanger mainly caused intestinal colonization and only one systemic infection occurred, after colonization. In Kilifi, Kenya, only invasive infections with ST17 were reported, however colonization was not screened for and it is likely that it existed without being detected. The ability of ST17 to cause infection may be related to opportunity, such as host factors and environment, rather than its own intrinsic properties. ST17 isolates have predominantly been reported in studies aiming to characterize Gram-negative bacteria or K. pneumoniae isolated from given populations (often ESBL- or carbapenemase-producing), as minor STs (i.e. incidental findings), and not because they were causing disease outbreaks (Table S5). For example, a study of AMR Gram-negative bacteria in low- and middle-income countries found that K. pneumoniae was the main cause of neonatal sepsis [49]. In that study, ST17 accounted for 3.1 % (8/258) of the K. pneumoniae isolates. Some outbreak reports do exist, and notably they mainly concern NICU outbreaks, e.g. in Norway [8], Kenya [46] and PR China [7, 9]. Taken together, this indicates that ST17 strains typically colonize a host before opportunistically causing infections, rather than causing clonal expansions of infectious outbreaks within wards, although there are exceptions in highly vulnerable host populations such as those found in NICUs.
Löhr et al. [18] identified AMR, heavy metal and thermoresistance determinants on the pKp2177_1 plasmid and hypothesized that they may in part explain why the strain persisted and spread in the NICU environment. Another reason may be related to the host itself: during long-term colonization, the ST17 strain stably maintained the pKp2177_1 plasmid and colonized the children for a median duration of 12 months. In comparison, the same strain only colonized 11 out of 53 parents (who were living in the same household as the colonized children), with a median colonization duration of 2.5 months [19]. Löhr et al. [19] identified two risk factors that were associated with the children having prolonged carriage of the strain: (i) being delivered by caesarean section and (ii) receiving antibiotics (ampicillin and gentamicin intravenously) during hospitalization. These factors may have delayed the establishment of a healthy gut microbiota, resulting in reduced colonization resistance and thus longer persistence of the strain in these children compared to the adults. With long colonization periods in vulnerable neonates, ST17 may have more opportunity to spread and cause outbreaks in NICUs than in other settings.
In conclusion, ST17 is a globally disseminated generalist clone that frequently colonizes both humans and non-human sources, and opportunistically causes infections, often in neonates. During within–host colonization for up to 21 months, ST17 in the Stavanger NICU outbreak remained comparatively stable, with few SNPs and no acquisition of AMR or virulence determinants. Globally, ST17 is highly diverse and harbours a range of AMR genes, virulence loci and plasmids. It contributes to the global burden of MDR infections but is also frequently found without AMR. The ESBL-encoding pKp2177_1 plasmid or yersiniabactin may offer some advantage in clonal expansions of ST17 strains in hospitals, but more data would be needed to assess this. Given the movement of the pKp2177_1 plasmid, the presence of similar ST17 strains in animals and humans, and the deep-branching global phylogeny, we hypothesize that non-human sources and human colonization play a crucial role for severe infections in vulnerable patients, such as in preterm neonates.
Supplementary Data
Funding information
This study was supported by the Western Norway Regional Health Authority (grant number F-12508 to MAKH) and the KLEB-GAP project (project number TMS2019TMT03) funded by the Trond Mohn Foundation. The funding bodies had no involvement in the study design, collection, management, analysis or interpretation of data.
Acknowledgements
We wish to thank Olav Natås and Knut Øymar for their support during the NICU outbreak and follow-up study, and Umaer Naseer for his contribution and expertise related to previous experimental plasmid studies. We thank Edward Feil for providing then-unpublished genomes from the SpARK One Health consortium project, and others who have made genomes and metadata from their studies publicly available in online repositories. We also wish to thank Benjamin Silvester, Zoe Dyson, Kelly Wyres, Margaret Lam and Ryan Wick for valuable discussions. This work was presented at the 13th International Meeting on Microbial Epidemiological Markers (IMMEM XIII) in Bath, UK in September 2022.
Author contribution
M.A.K.H., J.H., K.E.H., A.S. and I.H.L. conceptualized the study. S.I.R. collected samples and data from the Stavanger NICU outbreak. E.B. and R.B. performed whole-genome sequencing. H.K. contributed bacterial genomes from animals. M.A.K.H. performed the genomic analyses. M.A.K.H. wrote the first draft of the manuscript. All authors contributed to data interpretation, reviewed and edited the manuscript, and have read and agreed to the published version of the manuscript.
Conflicts of interest
The authors declare that there are no conflicts of interest.
Footnotes
Abbreviations: AMR, antimicrobial resistance; BSI, bloodstream infection; CI, confidence interval; ESBL, extended-spectrum beta-lactamase; HPD, highest posterior density; MDR, multidrug-resistant; ML, maximum likelihood; MRCA, most recent common ancestor; NICU, neonatal intensive care unit; nsSNP, nonsynonymous single nucleotide polymorphism; SNP, single nucleotide polymorphism; ST, sequence type; TCS, two-component system.
All supporting data, code and protocols have been provided within the article or through supplementary data files. Five supplementary figures and five supplementary tables are available with the online version of this article.
References
- 1.Martin RM, Bachman MA. Colonization, infection, and the accessory genome of Klebsiella pneumoniae . Front Cell Infect Microbiol. 2018;8:4. doi: 10.3389/fcimb.2018.00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Diancourt L, Passet V, Verhoef J, Grimont PAD, Brisse S. Multilocus sequence typing of Klebsiella pneumoniae nosocomial isolates. J Clin Microbiol. 2005;43:4178–4182. doi: 10.1128/JCM.43.8.4178-4182.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sonda T, Kumburu H, van Zwetselaar M, Alifrangis M, Mmbaga BT, et al. Molecular epidemiology of virulence and antimicrobial resistance determinants in Klebsiella pneumoniae from hospitalised patients in Kilimanjaro, Tanzania. Eur J Clin Microbiol Infect Dis. 2018;37:1901–1914. doi: 10.1007/s10096-018-3324-5. [DOI] [PubMed] [Google Scholar]
- 4.Holt KE, Wertheim H, Zadoks RN, Baker S, Whitehouse CA, et al. Genomic analysis of diversity, population structure, virulence, and antimicrobial resistance in Klebsiella pneumoniae, an urgent threat to public health. Proc Natl Acad Sci. 2015;112:E3574–81. doi: 10.1073/pnas.1501049112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wyres KL, Lam MMC, Holt KE. Population genomics of Klebsiella pneumoniae . Nat Rev Microbiol. 2020;18:344–359. doi: 10.1038/s41579-019-0315-1. [DOI] [PubMed] [Google Scholar]
- 6.Magiorakos A-P, Srinivasan A, Carey RB, Carmeli Y, Falagas ME, et al. Multidrug-resistant, extensively drug-resistant and pandrug-resistant bacteria: an international expert proposal for interim standard definitions for acquired resistance. Clin Microbiol Infect. 2012;18:268–281. doi: 10.1111/j.1469-0691.2011.03570.x. [DOI] [PubMed] [Google Scholar]
- 7.Jin Y, Shao C, Li J, Fan H, Bai Y, et al. Outbreak of multidrug resistant NDM-1-producing Klebsiella pneumoniae from a neonatal unit in Shandong Province, China. PLoS One. 2015;10:e0119571. doi: 10.1371/journal.pone.0119571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rettedal S, Löhr IH, Natås O, Giske CG, Sundsfjord A, et al. First outbreak of extended-spectrum β-lactamase-producing Klebsiella pneumoniae in a Norwegian neonatal intensive care unit; associated with contaminated breast milk and resolved by strict cohorting. APMIS. 2012;120:612–621. doi: 10.1111/j.1600-0463.2012.02879.x. [DOI] [PubMed] [Google Scholar]
- 9.Zhang X, Li X, Wang M, Yue H, Li P, et al. Outbreak of NDM-1-producing Klebsiella pneumoniae causing neonatal infection in a teaching hospital in mainland China. Antimicrob Agents Chemother. 2015;59:4349–4351. doi: 10.1128/AAC.03868-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Büdel T, Kuenzli E, Clément M, Bernasconi OJ, Fehr J, et al. Polyclonal gut colonization with extended-spectrum cephalosporin- and/or colistin-resistant Enterobacteriaceae: a normal status for hotel employees on the island of Zanzibar, Tanzania. J Antimicrob Chemother. 2019;74:2880–2890. doi: 10.1093/jac/dkz296. [DOI] [PubMed] [Google Scholar]
- 11.Raffelsberger N, Hetland MAK, Svendsen K, Småbrekke L, Löhr IH, et al. Gastrointestinal carriage of Klebsiella pneumoniae in a general adult population: a cross-sectional study of risk factors and bacterial genomic diversity. Gut Microbes. 2021;13:1939599. doi: 10.1080/19490976.2021.1939599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Huynh B-T, Passet V, Rakotondrasoa A, Diallo T, Kerleguer A, et al. Klebsiella pneumoniae carriage in low-income countries: antimicrobial resistance, genomic diversity and risk factors. Gut Microbes. 2020;11:1287–1299. doi: 10.1080/19490976.2020.1748257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Büdel T, Kuenzli E, Campos-Madueno EI, Mohammed AH, Hassan NK, et al. On the island of Zanzibar people in the community are frequently colonized with the same MDR Enterobacterales found in poultry and retailed chicken meat. J Antimicrob Chemother. 2020;75:2432–2441. doi: 10.1093/jac/dkaa198. [DOI] [PubMed] [Google Scholar]
- 14.Bidewell CA, Williamson SM, Rogers J, Tang Y, Ellis RJ, et al. Emergence of Klebsiella pneumoniae subspecies pneumoniae as a cause of septicaemia in pigs in England. PLoS One. 2018;13:e0191958. doi: 10.1371/journal.pone.0191958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Reyna-Flores F, Barrios-Camacho H, Dantán-González E, Ramírez-Trujillo JA, Lozano Aguirre Beltrán LF, et al. Draft genome sequences of endophytic isolates of Klebsiella variicola and Klebsiella pneumoniae obtained from the same sugarcane plant. Genome Announc. 2018;6:e00147-18. doi: 10.1128/genomeA.00147-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Alouache S, Estepa V, Messai Y, Ruiz E, Torres C, et al. Characterization of ESBLs and associated quinolone resistance in Escherichia coli and Klebsiella pneumoniae isolates from an urban wastewater treatment plant in Algeria. Microb Drug Resist. 2014;20:30–38. doi: 10.1089/mdr.2012.0264. [DOI] [PubMed] [Google Scholar]
- 17.Thorpe HA, Booton R, Kallonen T, Gibbon MJ, Couto N, et al. A large-scale genomic snapshot of Klebsiella spp. isolates in Northern Italy reveals limited transmission between clinical and non-clinical settings. Nat Microbiol. 2022;7:2054–2067. doi: 10.1038/s41564-022-01263-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Löhr IH, Hülter N, Bernhoff E, Johnsen PJ, Sundsfjord A, et al. Persistence of a pKPN3-like CTX-M-15-encoding IncFIIK plasmid in a Klebsiella pneumonia ST17 host during two years of intestinal colonization. PLoS One. 2015;10:e0116516. doi: 10.1371/journal.pone.0116516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Löhr IH, Rettedal S, Natås OB, Naseer U, Oymar K, et al. Long-term faecal carriage in infants and intra-household transmission of CTX-M-15-producing Klebsiella pneumoniae following a nosocomial outbreak. J Antimicrob Chemother. 2013;68:1043–1048. doi: 10.1093/jac/dks502. [DOI] [PubMed] [Google Scholar]
- 20.Lam MMC, Wick RR, Watts SC, Cerdeira LT, Wyres KL, et al. A genomic surveillance framework and genotyping tool for Klebsiella pneumoniae and its related species complex. Nat Commun. 2021;12:4188. doi: 10.1038/s41467-021-24448-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fostervold A, Hetland MAK, Bakksjø R, Bernhoff E, Holt KE, et al. A nationwide genomic study of clinical Klebsiella pneumoniae in Norway 2001-15: introduction and spread of ESBLs facilitated by clonal groups CG15 and CG307. J Antimicrob Chemother. 2022;77:665–674. doi: 10.1093/jac/dkab463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Franklin-Alming FV, Kaspersen H, Hetland MAK, Bakksjø R-J, Nesse LL, et al. Exploring Klebsiella pneumoniae in healthy poultry reveals high genetic diversity, good biofilm-forming abilities and higher prevalence in Turkeys than Broilers. Front Microbiol. 2021;12:725414. doi: 10.3389/fmicb.2021.725414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Håkonsholm F, Hetland MAK, Svanevik CS, Lunestad BT, Löhr IH, et al. Insights into the genetic diversity, antibiotic resistance and pathogenic potential of Klebsiella pneumoniae from the Norwegian marine environment using whole-genome analysis. Int J Hyg Environ Health. 2022;242:113967. doi: 10.1016/j.ijheh.2022.113967. [DOI] [PubMed] [Google Scholar]
- 24.Wick RR, Judd LM, Gorrie CL, Holt KE. Unicycler: resolving bacterial genome assemblies from short and long sequencing reads. PLoS Comput Biol. 2017;13:e1005595. doi: 10.1371/journal.pcbi.1005595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bankevich A, Nurk S, Antipov D, Gurevich AA, Dvorkin M, et al. SPAdes: a new genome assembly algorithm and its applications to single-cell sequencing. J Comput Biol. 2012;19:455–477. doi: 10.1089/cmb.2012.0021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Walker BJ, Abeel T, Shea T, Priest M, Abouelliel A, et al. Pilon: an integrated tool for comprehensive microbial variant detection and genome assembly improvement. PLoS One. 2014;9:e112963. doi: 10.1371/journal.pone.0112963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Inouye M, Dashnow H, Raven L-A, Schultz MB, Pope BJ, et al. SRST2: rapid genomic surveillance for public health and hospital microbiology labs. Genome Med. 2014;6:90. doi: 10.1186/s13073-014-0090-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lam MMC, Wick RR, Judd LM, Holt KE, Wyres KL. Kaptive 2.0: updated capsule and lipopolysaccharide locus typing for the Klebsiella pneumoniae species complex. Microb Genom. 2022;8:000800. doi: 10.1099/mgen.0.000800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Langmead B, Salzberg SL. Fast gapped-read alignment with Bowtie 2. Nat Methods. 2012;9:357–359. doi: 10.1038/nmeth.1923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Li H, Handsaker B, Wysoker A, Fennell T, Ruan J, et al. The sequence alignment/map format and SAMtools. Bioinformatics. 2009;25:2078–2079. doi: 10.1093/bioinformatics/btp352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Stamatakis A. RAxML version 8: a tool for phylogenetic analysis and post-analysis of large phylogenies. Bioinformatics. 2014;30:1312–1313. doi: 10.1093/bioinformatics/btu033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tonkin-Hill G, MacAlasdair N, Ruis C, Weimann A, Horesh G, et al. Producing polished prokaryotic pangenomes with the Panaroo pipeline. Genome Biol. 2020;21:180. doi: 10.1186/s13059-020-02090-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Seemann T. Prokka: rapid prokaryotic genome annotation. Bioinformatics. 2014;30:2068–2069. doi: 10.1093/bioinformatics/btu153. [DOI] [PubMed] [Google Scholar]
- 34.Croucher NJ, Page AJ, Connor TR, Delaney AJ, Keane JA, et al. Rapid phylogenetic analysis of large samples of recombinant bacterial whole genome sequences using Gubbins. Nucleic Acids Res. 2015;43:e15. doi: 10.1093/nar/gku1196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Rambaut A, Lam TT, Max Carvalho L, Pybus OG. Exploring the temporal structure of heterochronous sequences using TempEst (formerly Path-O-Gen) Virus Evol. 2016;2:vew007. doi: 10.1093/ve/vew007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bouckaert R, Vaughan TG, Barido-Sottani J, Duchêne S, Fourment M, et al. BEAST 2.5: an advanced software platform for Bayesian evolutionary analysis. PLoS Comput Biol. 2019;15:e1006650. doi: 10.1371/journal.pcbi.1006650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.R Core Team Vienna, Austria: R Foundation for Statistical Computing; 2022. R: a language and environment for statistical computing.www.R-project.org/ [Google Scholar]
- 38.Pernestig A-K, Georgellis D, Romeo T, Suzuki K, Tomenius H, et al. The Escherichia coli BarA-UvrY two-component system is needed for efficient switching between glycolytic and gluconeogenic carbon sources. J Bacteriol. 2003;185:843–853. doi: 10.1128/JB.185.3.843-853.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wyres KL, Hawkey J, Hetland MAK, Fostervold A, Wick RR, et al. Emergence and rapid global dissemination of CTX-M-15-associated Klebsiella pneumoniae strain ST307. J Antimicrob Chemother. 2019;74:577–581. doi: 10.1093/jac/dky492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wong SM, Carroll PA, Rahme LG, Ausubel FM, Calderwood SB. Modulation of expression of the ToxR regulon in Vibrio cholerae by a member of the two-component family of response regulators. Infect Immun. 1998;66:5854–5861. doi: 10.1128/IAI.66.12.5854-5861.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ahmer BM, van Reeuwijk J, Watson PR, Wallis TS, Heffron F. Salmonella SirA is a global regulator of genes mediating enteropathogenesis. Mol Microbiol. 1999;31:971–982. doi: 10.1046/j.1365-2958.1999.01244.x. [DOI] [PubMed] [Google Scholar]
- 42.Peirano G, Sang JHK, Pitondo-Silva A, Laupland KB, Pitout JDD. Molecular epidemiology of extended-spectrum-β-lactamase-producing Klebsiella pneumoniae over a 10 year period in calgary, Canada. J Antimicrob Chemother. 2012;67:1114–1120. doi: 10.1093/jac/dks026. [DOI] [PubMed] [Google Scholar]
- 43.Bowers JR, Kitchel B, Driebe EM, MacCannell DR, Roe C, et al. Genomic analysis of the emergence and rapid global dissemination of the clonal group 258 Klebsiella pneumoniae pandemic. PLoS One. 2015;10:e0133727. doi: 10.1371/journal.pone.0133727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Rodrigues C, Desai S, Passet V, Gajjar D, Brisse S. Genomic evolution of the globally disseminated multidrug-resistant Klebsiella pneumoniae clonal group 147. Microb Genom. 2022;8:000737. doi: 10.1099/mgen.0.000737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Wyres KL, Wick RR, Judd LM, Froumine R, Tokolyi A, et al. Distinct evolutionary dynamics of horizontal gene transfer in drug resistant and virulent clones of Klebsiella pneumoniae . PLoS Genet. 2019;15:e1008114. doi: 10.1371/journal.pgen.1008114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Henson SP, Boinett CJ, Ellington MJ, Kagia N, Mwarumba S, et al. Molecular epidemiology of Klebsiella pneumoniae invasive infections over a decade at Kilifi County Hospital in Kenya. Int J Med Microbiol. 2017;307:422–429. doi: 10.1016/j.ijmm.2017.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Gorrie CL, Mirceta M, Wick RR, Edwards DJ, Thomson NR, et al. Gastrointestinal carriage is a major reservoir of Klebsiella pneumoniae infection in intensive care patients. Clin Infect Dis. 2017;65:208–215. doi: 10.1093/cid/cix270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Thuy DB, Campbell J, Thuy CT, Hoang NVM, Voong Vinh P, et al. Colonization with Staphylococcus aureus and Klebsiella pneumoniae causes infections in a Vietnamese intensive care unit. Microb Genom. 2021;7:000514. doi: 10.1099/mgen.0.000514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Sands K, Carvalho MJ, Portal E, Thomson K, Dyer C, et al. Characterization of antimicrobial-resistant gram-negative bacteria that cause neonatal sepsis in seven low- and middle-income countries. Nat Microbiol. 2021;6:512–523. doi: 10.1038/s41564-021-00870-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.