Abstract
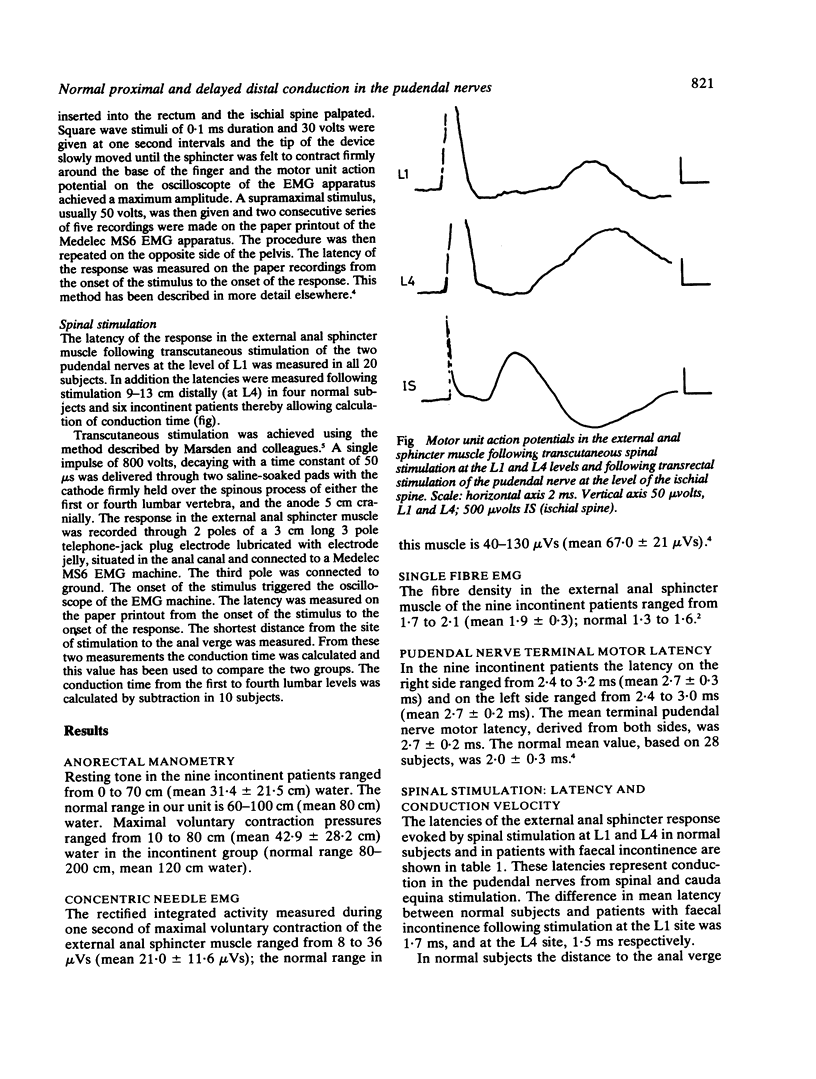
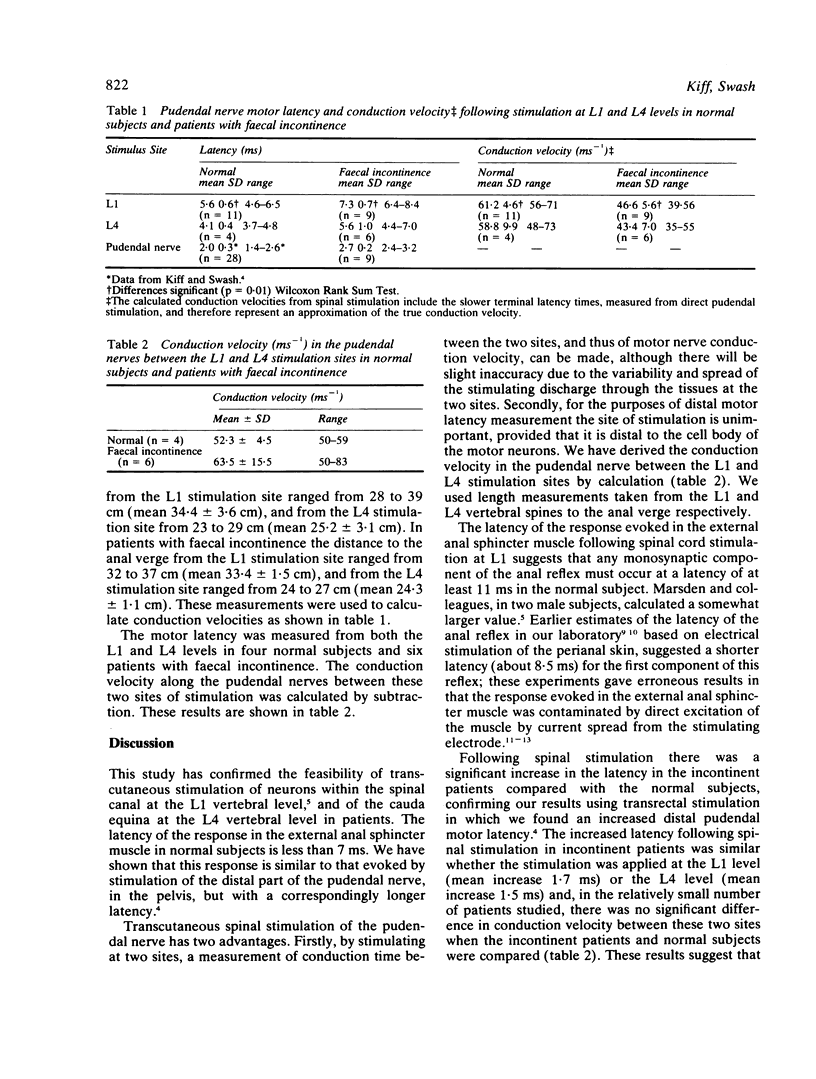
The latency of the response in the external anal sphincter muscle following transcutaneous stimulation of the cauda equina at the L1 vertebral level was measured in nine women with neurogenic faecal incontinence (mean 7.3 SD 0.7 ms) and 11 normal subjects (mean 5.6 SD 0.6 ms) (p = 0.01). There was no difference in conduction velocity between the L1 and L4 vertebral levels thus supporting the suggestion that conduction delay in faecal incontinence occurs distally.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Brindley G. S. Electroejaculation: its technique, neurological implications and uses. J Neurol Neurosurg Psychiatry. 1981 Jan;44(1):9–18. doi: 10.1136/jnnp.44.1.9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henry M. M., Parks A. G., Swash M. The anal reflex in idiopathic faecal incontinence: an electrophysiological study. Br J Surg. 1980 Nov;67(11):781–783. doi: 10.1002/bjs.1800671105. [DOI] [PubMed] [Google Scholar]
- Henry M. M., Swash M. Assessment of pelvic-floor disorders and incontinence by electrophysiological recording of the anal reflex. Lancet. 1978 Jun 17;1(8077):1290–1291. doi: 10.1016/s0140-6736(78)91271-0. [DOI] [PubMed] [Google Scholar]
- Neill M. E., Parks A. G., Swash M. Physiological studies of the anal sphincter musculature in faecal incontinence and rectal prolapse. Br J Surg. 1981 Aug;68(8):531–536. doi: 10.1002/bjs.1800680804. [DOI] [PubMed] [Google Scholar]
- Neill M. E., Swash M. Increased motor unit fibre density in the external anal sphincter muscle in ano-rectal incontinence: a single fibre EMG study. J Neurol Neurosurg Psychiatry. 1980 Apr;43(4):343–347. doi: 10.1136/jnnp.43.4.343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parks A. G., Swash M., Urich H. Sphincter denervation in anorectal incontinence and rectal prolapse. Gut. 1977 Aug;18(8):656–665. doi: 10.1136/gut.18.8.656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pedersen E., Harving H., Klemar B., Tørring J. Human anal reflexes. J Neurol Neurosurg Psychiatry. 1978 Sep;41(9):813–818. doi: 10.1136/jnnp.41.9.813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pedersen E., Klemar B., Schrøder H. D., Tørring J. Anal sphincter responses after perianal electrical stimulation. J Neurol Neurosurg Psychiatry. 1982 Sep;45(9):770–773. doi: 10.1136/jnnp.45.9.770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swash M. Early and late components in the human anal reflex. J Neurol Neurosurg Psychiatry. 1982 Sep;45(9):767–769. doi: 10.1136/jnnp.45.9.767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vodusek D. B., Janko M., Lokar J. Direct and reflex responses in perineal muscles on electrical stimulation. J Neurol Neurosurg Psychiatry. 1983 Jan;46(1):67–71. doi: 10.1136/jnnp.46.1.67. [DOI] [PMC free article] [PubMed] [Google Scholar]


