Abstract
Background
Similar to a modified star excursion balance test, the Y-balance test is recommended for use in clinical settings to evaluate dynamic balance, particularly in athletes with chronic ankle instability. However, due to the testing errors, there are certain restrictions. As a result, the modification of the centre of mass tracking system was developed in order to aid in the detection of the ability to control the dynamic balance. Therefore, the purpose of this study was to correlate the usage of an accelerometer for the shifting of the centre of mass during a dynamic balance test with a Y-balance test reach distance score.
Methodology
Forty professional football athletes with CAI participated in this study by performing the Y-balance test three times while wearing an accelerometer. The jerk, RMS sway amplitude, mean velocity from the time domain, and the normalised reach distance scores of the Y-balance test in the anterior, posteromedial, and posterolateral directions were all collected.
Results
There was a strong positive correlation of jerk and RMS sway amplitude with the normalised reach distance scores in the posteromedial direction (r = 0.706 and 0.777, respectively), a moderate positive correlation of jerk and RMS sway amplitude with the normalised reach distance scores in the posterolateral direction (r = 0.609 and 0.606, respectively), a moderate positive correlation of jerk and RMS sway amplitude with the composite reach distance scores (r = 0.531 and 0.573, respectively) and significant differences in the posteromedial, posterolateral and overall directions (p-value < 0.001).
Conclusion
These findings indicate that the area of the centre of mass shifting as represented by the accelerometer can disclose the body’s ability to control the centre of mass over the base of support when the body is moving. Furthermore, in this study, the RMS sway variable in the posteromedial direction appears to be the most prominent.
Keywords: Body kinematics, Y-balance test, Balance measurement, Postural control, Ankle instability
1. Introduction
Ankle sprains are the most commonly reported injury in athletes, contributing to 15% of all reported injuries [1]. Injuries have been documented in a variety of sports that involve running, cutting, jumping, and landing [2]. Men’s football has the highest incidence rates (injury rate: 1.34/1000 AEs). Furthermore, the injury rate increases during practice and competition (9.6/1000 AEs and 35.9/1000 AEs, respectively) [3]. Acute ankle sprains often have a significant recurrence rate, which is linked to the development of chronic ankle instability (CAI) [4], defined as impaired somatosensory feedback and an impaired proprioceptive sense of the ankle joint caused by a loss of function of the mechanoreceptor at the ligament after a frequent injury [5] leading to a feeling like “giving way”. In addition, this occurrence results in a loss of balance control while standing, particularly when standing on the CAI affected leg. Poor balance performance has been shown to be related to neuromuscular dysfunction [6], return-to-play status, and the risk of recurrent ankle sprain [7].
Balance refers to an individual’s ability to maintain their centre of mass (CoM) or line of gravity within their base of support (BoS). It is also described as the capacity to sustain equilibrium, which is defined as any condition in which all acting forces cancel each other out, resulting in a stable, balanced system. Balance is a sensory integration of the somatosensory or proprioceptive, visual, and vestibular systems. In normal circumstances, somatosensory information has the most significant influence, contributing to around 70% of all received feedback on a firm surface [8]. Balance is classified into static and dynamic balance, with static balance being the ability to maintain the body in a stable posture or keep the CoM above the BoS when resting [9]. The ability to move the vertical projection of the CoM around the supporting BoS or to keep the CoM over the BoS in motion is defined as dynamic balance [9]. Sufficient body muscle power, adequate postural sensibility, normal function of the visual and vestibular systems, and appropriate coordination of the cerebellum and basal ganglia are necessary for good balance.
Dynamic balance is a crucial specific skill for most sports, which is related to the ability to sprint and change directions on the field. Football is one of the field sports that most frequently requires dynamic balance control during the gameplay, particularly dynamic unilateral movements when kicking the ball [10]. Various measurements using several methods have been employed, including both lab-based and clinical, and one of the acknowledged methods with good validity and reliability is the ground reaction force of a force plate (GRF) [11]. Many methods have been developed to measure the orientation of the CoM, some of which are based on the kinematics of the entire human body and are known as segmental methods [12], which examine the data from fourteen sets of markers spanning all of the body segments in order to determine the body’s CoM by a 3-D motion capture system. This provides a firm estimate of CoM displacement in specific sports activities and is significantly accurate when applied with GRF [13]. Furthermore, a previous study on CoM that used a 3-D motion capture system while performing a dynamic balance test described it as being able to demonstrate the effects of real-time processing on balance control [14]. However, the evaluation tool’s features and cost-effectiveness are not ideal for all users.
The accelerometer is a technological device used to detect the changes of sensor position in time and angular motion, in which a biomedical measurement is used to assess balance control [15] in the vertical and horizontal planes, the study of CoM was reported as a point that replaces the entire body [16]. The use of CoM to evaluate balance is described as posturography, which is typically quantified by characterising the displacements of an accelerometer placed on the lower back (L5 spinous process) [17]. Furthermore, accelerometer-based balance control assessment has been studied in both healthy and diseased populations [18,19]. Previous research has demonstrated that accelerometers can objectively detect deviations in the dynamic CoM, which are represented as the root mean square (RMS) of the accelerations contributing to each independent axis, the jerkiness of the COM, and the velocity [20], and have good reliability and validity with regard to detecting the changes of balance with GRF [21], particularly in the time domain of the jerk, RMS sway, and mean velocity. These parameters describe the jerkiness of the CoM, the movement speed along the distance of the CoM replacement in the anteromedial and mediolateral directions, and the average velocity of the CoM movement. Furthermore, the accelerometer has been investigated as a valuable tool that can be used within clinical settings for various applications such as static balance, side jump landing [21] and performance evaluation [20]. However, few application studies have been conducted to examine its use with dynamic balance testing.
The star excursion balance test (SEBT), modified star excursion balance test (mSEBT), and Y-balance test (YBT) are clinical field-based dynamic balance tests that are reliable and valid for detecting balance deficits in musculoskeletal injuries, particularly ankle instability [22,23]. The clinical test requires the tester to stand on one leg and stretch other leg as far as possible in the designated directions. Furthermore, kinematic information has been reported in trunk and lower body regions while performing a leg reach [24,25], which is defined as a helping strategy to control balance. However, this field test has some limitations. Several errors must be checked during the assessment, causing it difficult to focus on both the scoring record and the fault detection. As mentioned, overcompensation during leg reaching was shown in excessive pushing effort or body shift in excess of generally required to maintain dynamic balance, which refers to excessive sway or arm extension.
Given the comprehensive implementation of field tests with higher precision for dynamic balance tests, kinematic data as shifts in CoM could be applied to examine and analyse the ability to control the CoM in motion with field dynamic balance data. As a result, the aim of this study was to investigate the CoM evaluation by use of an accelerometer and its relationship with the normalised reach distance score in YBT performance, which is hypothesised to have a good positive correlation.
2. Materials and methods
A cross-sectional study design was used in this study. The research was carried out between December 2019 and October 2020. The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Institutional Review Board of Rangsit University (RSUERB2019-004, approved in February 2019), and each participant provided written informed consent prior to participation.
2.1. Study participants
The sample size was calculated using the G-power program (version 3.1.9.7) with the following parameters: Correlations: Bivariate normal model, correlation ρ H1 = 0.4 and ρ H0 = 0, Significant level (α) = 0.05, Power = 80%. The data of forty participants were calculated. They are full-time practicing and competing male athletes having an age range of 18–28 years with a history of ankle sprain at least once within five years and a Cumberland Ankle Instability Tool (CAIT) questionnaire score below 24 out of 30, which indicates a functional ankle instability [26]. Moreover, they reported no history of ankle surgery, history of lower limb injuries within one week, pain that influenced the single leg squat of the testing side, or vestibular impairment.
2.2. Experiment protocol
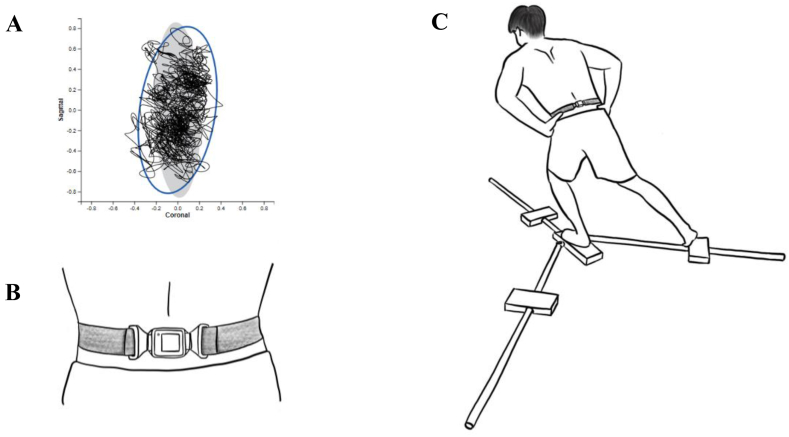
The measurement of CoM interprets the changes in bodily alignment as a body sways. The movement of the CoM was measured using a portable wireless sensor (Accelerometer, Opal) attached at the fifth spinous process of the lumbar vertebrae (L5) (Fig. 1B). The sensor was connected to the primary data receiver (APDM Inc., USA) and indicated the linear acceleration and angular velocity in the anteroposterior and mediolateral directions, which shown in a graph (Fig. 1A). The accelerometry parameters were analysed by Mobility Lab (APDM Inc., USA) and reported as jerkiness (jerk), sway area, RMS sway (direction), mean velocity in the time domain. There was moderate to good reliability in terms of static balance, with an ICC of 0.87 in jerk and a range of 0.60–0.89 in other time-domain parameters, as well as a validity with a gold standard protocol [27] and a high correlation with the berg balance scale and the timed up and go test in clinical applications [28].
Fig. 1.
Protocol and setting: (A) Sway diagram, (B) Portable wireless sensor “Opal” attachment at the fifth spinous process of the lumbar vertebrae (L5), and (C) Performance in the posterolateral of the Y-balance test with accelerometer.
Before the test, individuals were allowed to perform a leg reach three times in each direction after being equipped with an accelerometer. During the testing, individuals did a leg reach as far as possible in three different directions three times (Fig. 1C). The instructions were to perform a single-leg stand on the CAI leg in the centre of the Y-balance kit platform (FMS Y-Balance), which was modified from the eight directions of the star excursion balance test to three directions with high sensitivity and reliability in the anterior, posterolateral, and posteromedial directions (ICC 0.88, 0.90, and 0.88, respectively) [29]. The participants put both hands on the hips, then used their other leg to push the indicator as far as possible with the big toe and return to the initial two-foot standing position [30] The participants were permitted to bend the knee and hip of the CAI leg. However, the task would be failed and repeated if the individuals could not return to the initial position or an excessive movement occurred [31]. The accelerometer sensor recorded jerk, RMS sway, and mean velocity data, and the reach distance shown in the equipment bar was averaged for each movement. The formula for the normalised reach distance is the longest distance in each direction divided by the individual subject’s leg length and multiplied by 100. Composite reach distance is calculated by combining the longest distance in three directions, dividing it by three times the individual subject’s leg length, and multiplying it by 100 [32].
2.3. Data analyses
The algorithms for signal analysis were derived from Mobility Lab (APDM Inc., USA). The Shapiro-Wilk test was used to determine the normality of the data. The correlation between the accelerometry sway variables and normalised reach distance scores in all directions and composite reach distance scores of YBT were analysed by the Pearson correlation coefficient based on the interpretation of weak to very strong correlations [33]. Statistical analysis was performed using SPSS for Windows version 22 (IBM Corporation, Armonk, NY, USA), with statistical significance set a priori at p < 0.05.
3. Results
There were no major side effects reported by participants during the research, and all of them completed the process. Table 1 shows the characteristics of the forty male football players who experienced ankle injuries that led to CAI.
Table 1.
Demographic and clinical characteristics.
| Variables | Mean ± SD (n = 40) |
|---|---|
| Age (years) | 20.28 ± 2.45 |
| BMI (kg/m2) CAI side (left:right) Experience as football player (years) |
22.20 ± 1.73 22:18 9.53 ± 3.51 |
| History of ankle sprain (times per year) | 2.90 ± 1.61 |
| CAIT (points) | 17.15 ± 3.53 |
Note: Values are shown as mean ± SD; BMI (Body mass index); CAIT (Cumberland Ankle Instability Tool).
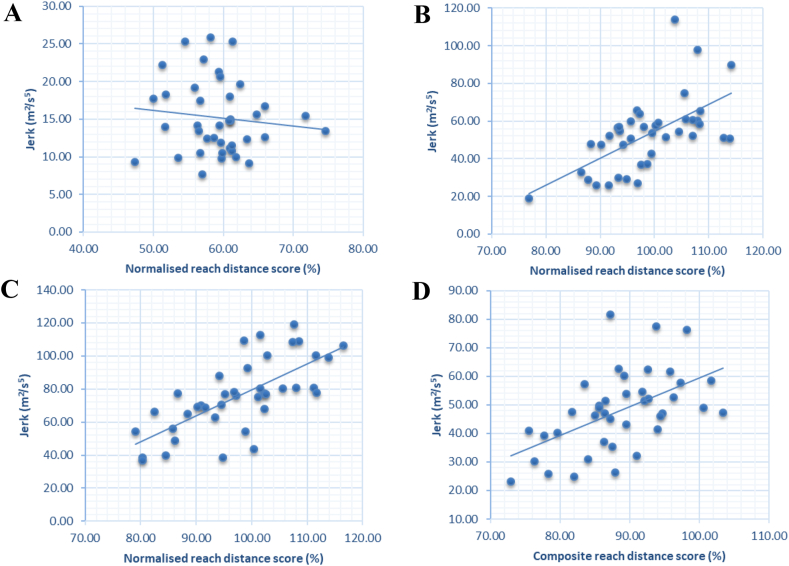
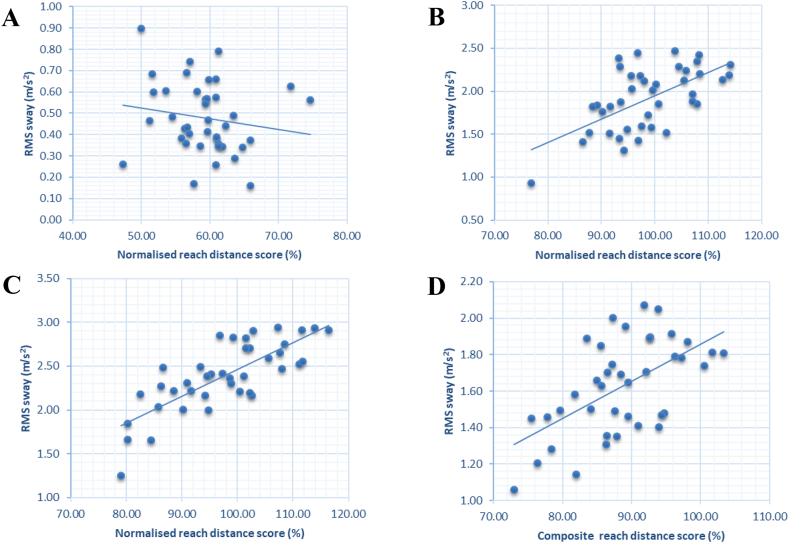
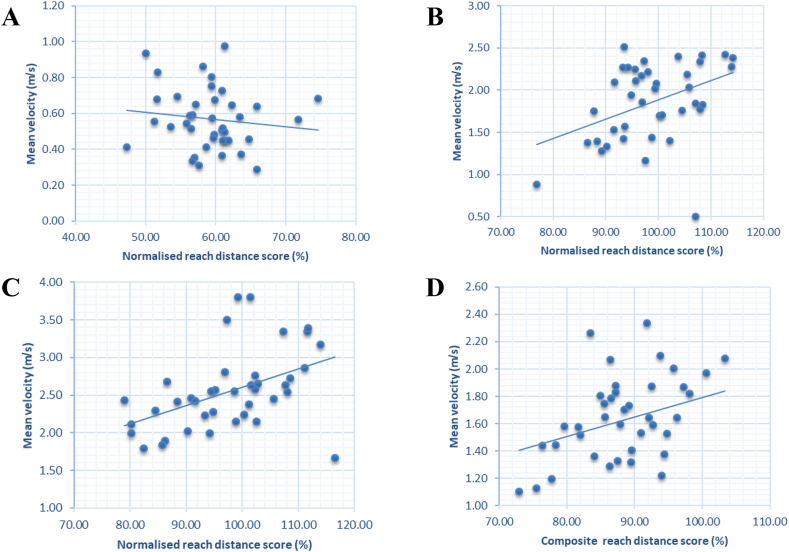
The correlations of the normalised reach distance scores with the accelerometry sway measurements was shown in Table 2, Figs. 2A–D, 3A–D and 4A–D. The jerk and the RMS sway of posteromedial direction were found to be strong correlation (r value = 0.706 and 0.777, respectively). In contrast, for the mean velocity, a moderate correlation (r value = 0.459) was found, and the posterolateral direction showed a moderate correlation of all variables (r value = 0.609, 0.606, and 0.405, respectively). The composite reach distance of the overall directions showed a moderate correlation of jerk and RMS sway (r value = 0.531 and 0.573, respectively), with a significant difference of 0.05. However, all variables in the anterior direction had no significant differences, with a weak negative correlation.
Table 2.
Correlation of accelerometry sway parameters and normalised reach distance scores of YBT in individual directions and overall directions.
| Normalised reach distance scores |
|||||
|---|---|---|---|---|---|
| Anterior | Posterolateral | Posteromedial | Composite | ||
| Jerk | Anterior | −0.114 | |||
| Posterolateral | 0.609∗∗ | ||||
| Posteromedial | 0.706∗∗ | ||||
| Average | 0.531∗∗ | ||||
| RMS sway | Anterior | −0.127 | |||
| Posterolateral | 0.606∗∗ | ||||
| Posteromedial | 0.777∗∗ | ||||
| Average | 0.573∗∗ | ||||
| Mean velocity | Anterior | −0.160 | |||
| Posterolateral | 0.405∗ | ||||
| Posteromedial | 0.459∗ | ||||
| Average | 0.314∗ | ||||
Note: Values are shown as r value; 0.10–0.39 = weak correlation, 0.40–0.69 = moderate correlation, 0.70–0.89 = strong correlation and 0.90–1.00 = very strong correlation.
significant difference (p-value <0.05);
significant difference (p-value <0.001).
Fig. 2.
Scatter plot for correlation of jerkiness and normalised reach distance scores of the (A) anterior, (B) posterolateral, and (C) posteromedial directions and (D) the composite reach distance scores.
Fig. 3.
Scatter plot for correlation of RMS sway and normalised reach distance scores of the (A) anterior, (B) posterolateral, and (C) posteromedial directions and (D) the composite reach distance scores.
Fig. 4.
Scatter plot for correlation of mean velocity and normalised reach distance scores of the (A) anterior, (B) posterolateral, and (C) posteromedial directions and (D) the composite reach distance scores.
4. Discussion
The major purpose of this study was to correlate the use of an accelerometer during dynamic balance tests with reaching scores on a YBT. The change in the body’s CoM characterized by jerk, RMS sway, and mean velocity in the time domain are the most accurate variables in static balance studies [27] and also reliable in dynamic balance assessments [21]. A significant positive correlation was shown with the normalised reach distance scores in the posteromedial and posterolateral directions as well as the composite reach distance scores.
The accelerometer can wirelessly transmit body sway related to gravity as well as trunk postural adjustments in anticipation of leg reach, known as anticipatory postural adjustments. This represents the feedforward balance control of stability while moving the body. As a result, the accelerometry-based assessment provides a sensitive tool for measuring balance [17,34]. The present study applies the innovation of the CoM detecting evaluation in the CAI population, which confirms that the changing of CoM supports the balance control during leg reaching in YBT performance. Similarly, previous research has identified the CoM as the stable primary reference for posture and movement coordination during whole-body reaching, as well as for the central regulation of posture and voluntary movement [35]. The findings of this study indicate a strong positive and significant correlation in the posteromedial and posterolateral directions. This study discovered that RMS sway is the most significantly associated variable to clinical field test scores, which is the change of CoM in both axes, hence it directly describes body sway. According to Hertel’s previous study, the posterolateral and posteromedial directions are the most sensitive and reliable for use in detection of the dynamic balance change in people with CAI by conducting the star excursion balance test (SEBT), which is the original test that the YBT was developed from Ref. [23], and complement the findings in our investigation.
The single-leg squat and contralateral leg reach are required based to the clinical testing protocol. Due to the balance control strategies research, while performing a dynamic balance test by YBT, kinematic changes are revealed in the joints of the lower extremities: hips, knees [36] and ankles [24]. Ankle strategy is the first mechanism used in balance control that corrects changes in balance by activating muscles around the ankle joint. Typically, the tibialis anterior, peroneus, and gastrocnemius are engaged. However, the YBT tests showed a higher tibialis anterior activation for postural control in the posterolateral and posteromedial directions than in the other directions [37]. Furthermore, the instability of the CAI ankle influences balance control, resulting in decreased control of weight-bearing ankle inversion, particularly in a single-leg stance [38]. The eccentric ankle evertor muscle weakening may reduce joint dynamic stability and contribute significantly to functional joint instability [39]. Additionally, the greater angular velocity peaks during single-leg weight bearing indicates an increase in ankle inversion movement amplitudes and durations [38]. The hip and knee strategy will be the second mechanism to aid with balance control after the ankle adjustment. Hip and knee flexion is critical in defining the quality of single-leg squats, which are essential in testing [40]. As a result, the change in ROM in hip and knee flexion correlates with the reach distance. Moreover, the muscles surrounding the hips and knees will be activated during the control balance. The gluteus medius controls the pelvic level and the hip abduction/adduction angle, the gluteus maximus maintains the posture, and the quadriceps and hamstring muscles control the knee angle [41]. Finally, there is a large amount of trunk flexion and little contralateral trunk bending in the posterolateral direction reach, and a great deal of trunk flexion and a minimal amount of ipsilateral trunk bending in the posteromedial direction reach [24] for the last compensates control to maintain the CoM in the same BoS. Likewise, trunk and pelvic rotation have been reported to aid in maintaining a proximal stable posture and compensating for distal instability [42]. As previous noted, the axial strategies are used to minimise the displacement of CoM in motion and movement [43]. As mentioned before, the CAI has a direct effect on peripheral balance control strategies and results in excessive trunk movement, which supports our finding of a correlation between CoM displacement and leg reaching distance scores.
However, the anterior direction was shown to have a weak negative correlation because of the lower muscular activity of the ankle joint, where the tibialis anterior does not exhibit as much activity as the other two directions because different muscle groups control the hip strategies with them. Additionally, the quadriceps are most active in the anterior reach, whereas the hamstring is more active in the posteromedial and posterolateral reach [37]. The most essential explanation is that the anterior leg reach rarely interferes with the torso movement, which was found to be just a minor extension [24]. As a result, anterior displacement of the CoM during the dynamic balance test does not correlate with the YBT normalised reach distance scores.
This study has been deficient in terms of the information other than reach directions for the highest sensitivity to detect the proximal body alteration, as well as a comparison with a healthy ankle population to determine CAI’s effect on trunk compensation. Moreover, the non-CAI and CAI dynamic balance control in individual participants' legs must be evaluated in order to determine the intrinsic factors in each person. Further research might investigate the absence of information on reach direction and the factors influencing CoM changes in healthy ankles and CAI populations. Finally, it will be necessary to develop a method for assessing dynamic balance using the YBT in CoM evaluation by the accelerometer, which can regulate the errors of the testing for clear evaluation of dynamic balance.
5. Conclusion
The frequent shifts of the CoM of the accelerometry parameters show dynamic balance control while moving, with RMS sway representing the best correlation with the clinical test. According to the results of this study, the dynamic stability outcomes from the accelerometer approach can be applied in combination with the original examination and trends in order to be used as a clinical test for dynamic balance, particularly in the CAI population. Furthermore, it provides the benefit of reduction of the errors of conventional testing by focusing on the failed task movement rather than the foot placement scores.
Author contributions
Phuaklikhit C. designed the model and conceptual framework, as well as carried out the experiments and analysed the data.Junsri T. assisted with dynamic balance measurements and contributed to the interpretation of the results. Maikaew U. aided as accelerometer controller during data collection and interpretation with Phuaklikhit C. The manuscript was drafted collaboratively by all participants. Finally, Phuaklikhit C. revised and approved the submitted version.
Data availability statement
The data that support the findings of this investigation are available from the corresponding author upon reasonable request.
Additional information
No additional information is available for this paper.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper
Acknowledgements
This research was supported by a grant from the Research Institute, Rangsit University (grant no. 52/2561, 2018). The authors would like to thank the Faculty of Physical Therapy and Sports Medicine for providing a location and materials for data collection.
References
- 1.Roos K.G., Kerr Z.Y., Mauntel T.C., Djoko A., Dompier T.P., Wikstrom E.A. The epidemiology of lateral ligament complex ankle sprains in National Collegiate Athletic Association Sports. Am. J. Sports Med. 2016;45(1):201–209. doi: 10.1177/0363546516660980. [DOI] [PubMed] [Google Scholar]
- 2.Doherty C., Delahunt E., Caulfield B., Hertel J., Ryan J., Bleakley C. The incidence and prevalence of ankle sprain injury: a systematic review and meta-analysis of prospective epidemiological studies. Sports Med. 2014;44(1):123–140. doi: 10.1007/s40279-013-0102-5. [DOI] [PubMed] [Google Scholar]
- 3.Hootman J.M., Dick R., Agel J. Epidemiology of collegiate injuries for 15 sports: summary and recommendations for injury prevention initiatives. J. Athl. Train. 2007;42(2):311–319. [PMC free article] [PubMed] [Google Scholar]
- 4.Attenborough A.S., Hiller C.E., Smith R.M., Stuelcken M., Greene A., Sinclair P.J. Chronic ankle instability in sporting populations. Sports Med. 2014;44(11):1545–1556. doi: 10.1007/s40279-014-0218-2. [DOI] [PubMed] [Google Scholar]
- 5.Xue X., Ma T., Li Q., Song Y., Hua Y. Chronic ankle instability is associated with proprioception deficits: a systematic review and meta-analysis. J. Sport Health Sci. 2021;10(2):182–191. doi: 10.1016/j.jshs.2020.09.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Olmsted L.C., Carcia C.R., Hertel J., Shultz S.J. Efficacy of the star excursion balance tests in detecting reach deficits in subjects with chronic ankle instability. J. Athl. Train. 2002;37(4):501. [PMC free article] [PubMed] [Google Scholar]
- 7.Gribble P.A., Terada M., Beard M.Q., Kosik K.B., Lepley A.S., McCann R.S., et al. Prediction of lateral ankle sprains in football players based on clinical tests and body mass index. Am. J. Sports Med. 2016;44(2):460–467. doi: 10.1177/0363546515614585. [DOI] [PubMed] [Google Scholar]
- 8.Peterka R.J. Sensorimotor integration in human postural control. J. Neurophysiol. 2002;88(3):1097–1118. doi: 10.1152/jn.2002.88.3.1097. [DOI] [PubMed] [Google Scholar]
- 9.O’Sullivan S.B., Schmitz T.J., Fulk G.D. sixth ed. F.A. Davis Co.; Philadelphia: 2014. Physical Rehabilitation. [Google Scholar]
- 10.Hrysomallis C. Balance ability and athletic performance. Sports Med. (Auckland, NZ) 2011;41(3):221–232. doi: 10.2165/11538560-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 11.Ross S.E., Guskiewicz K.M., Yu B. Single-leg jump-landing stabilization times in subjects with functionally unstable ankles. J. Athl. Train. 2005;40(4):298–304. [PMC free article] [PubMed] [Google Scholar]
- 12.Saini M., Kerrigan D., Annaswamy T., Duff-Raffaele M. The vertical displacement of the center of mass during walking: a comparison of four measurement methods. J. Biomech. Eng. 1998;120:133–139. doi: 10.1115/1.2834293. [DOI] [PubMed] [Google Scholar]
- 13.Mapelli A., Zago M., Fusini L., Galante D., Colombo A., Sforza C. Validation of a protocol for the estimation of three-dimensional body center of mass kinematics in sport. Gait Posture. 2014;39(1):460–465. doi: 10.1016/j.gaitpost.2013.08.025. [DOI] [PubMed] [Google Scholar]
- 14.Andreo P., Khalaf K., Heale L., Jelinek H.F., Donnan L. Effects of kinesiology tape on non-linear center of mass dispersion during the Y balance test. Front. Physiol. 2018;9:1527. doi: 10.3389/fphys.2018.01527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bonato P. Advances in wearable technology and applications in physical medicine and rehabilitation. J. NeuroEng. Rehabil. 2005;2(1):2. doi: 10.1186/1743-0003-2-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Erdmann W. Center of mass of the human body helps in analysis of balance and movement. MOJ Appl. Bionics Biomech. 2018;2:144–148. [Google Scholar]
- 17.Mancini M., Horak F.B. The relevance of clinical balance assessment tools to differentiate balance deficits. Eur. J. Phys. Rehabil. Med. 2010;46(2):239–248. [PMC free article] [PubMed] [Google Scholar]
- 18.Fujimoto M., Chou L.-S. Dynamic balance control during sit-to-stand movement: an examination with the center of mass acceleration. J. Biomech. 2012;45(3):543–548. doi: 10.1016/j.jbiomech.2011.11.037. [DOI] [PubMed] [Google Scholar]
- 19.Kizilova N., Jarmalienė E., Šešok A., Daunoravičienė K., Griskevicius J. Evaluation of human postural balance in quiet standing by direct measurement of human body center of mass acceleration. J. Vibroeng. 2009;11:556–561. [Google Scholar]
- 20.Schütte K.H., Maas E.A., Exadaktylos V., Berckmans D., Venter R.E., Vanwanseele B. Wireless tri-axial trunk accelerometry detects deviations in dynamic center of mass motion due to running-induced fatigue. PLoS One. 2015;10(10) doi: 10.1371/journal.pone.0141957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Heebner N.R., Akins J.S., Lephart S.M., Sell T.C. Reliability and validity of an accelerometry based measure of static and dynamic postural stability in healthy and active individuals. Gait Posture. 2015;41(2):535–539. doi: 10.1016/j.gaitpost.2014.12.009. [DOI] [PubMed] [Google Scholar]
- 22.Plisky P.J., Gorman P.P., Butler R.J., Kiesel K.B., Underwood F.B., Elkins B. The reliability of an instrumented device for measuring components of the star excursion balance test. N. Am. J. Sports Phys. Ther. 2009;4(2):92–99. [PMC free article] [PubMed] [Google Scholar]
- 23.Hertel J., Braham R.A., Hale S.A., Olmsted-Kramer L.C. Simplifying the star excursion balance test: analyses of subjects with and without chronic ankle instability. J. Orthop. Sports Phys. Ther. 2006;36(3):131–137. doi: 10.2519/jospt.2006.36.3.131. [DOI] [PubMed] [Google Scholar]
- 24.Kang M.H., Kim G.M., Kwon O.Y., Weon J.H., Oh J.S., An D.H. Relationship between the kinematics of the trunk and lower extremity and performance on the Y-balance test. PM & R. 2015;7(11):1152–1158. doi: 10.1016/j.pmrj.2015.05.004. [DOI] [PubMed] [Google Scholar]
- 25.Eltoukhy M., Kuenze C., Oh J., Wooten S., Signorile J. Kinect-based assessment of lower limb kinematics and dynamic postural control during the star excursion balance test. Gait Posture. 2017;58:421–427. doi: 10.1016/j.gaitpost.2017.09.010. [DOI] [PubMed] [Google Scholar]
- 26.Hiller C.E., Refshauge K.M., Bundy A.C., Herbert R.D., Kilbreath S.L. The Cumberland ankle instability tool: a report of validity and reliability testing. Arch. Phys. Med. Rehabil. 2006;87(9):1235–1241. doi: 10.1016/j.apmr.2006.05.022. [DOI] [PubMed] [Google Scholar]
- 27.Mancini M., Salarian A., Carlson-Kuhta P., Zampieri C., King L., Chiari L., et al. ISway: a sensitive, valid and reliable measure of postural control. J. NeuroEng. Rehabil. 2012;9:59. doi: 10.1186/1743-0003-9-59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.O’Sullivan M., Blake C., Cunningham C., Boyle G., Finucane C. Correlation of accelerometry with clinical balance tests in older fallers and non-fallers. Age Ageing. 2009;38(3):308–313. doi: 10.1093/ageing/afp009. [DOI] [PubMed] [Google Scholar]
- 29.Powden C.J., Dodds T.K., Gabriel E.H. The reliability of the star excursion balance test and lower quarter y-balance test in healthy adults: a systematic review. Int. J. Sports Phys. Ther. 2019;14(5):683–694. [PMC free article] [PubMed] [Google Scholar]
- 30.Gribble P.A., Hertel J., Plisky P. Using the Star Excursion Balance Test to assess dynamic postural-control deficits and outcomes in lower extremity injury: a literature and systematic review. J. Athl. Train. 2012;47(3):339–357. doi: 10.4085/1062-6050-47.3.08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Plisky P.J., Rauh M.J., Kaminski T.W., Underwood F.B. Star Excursion Balance Test as a predictor of lower extremity injury in high school basketball players. J. Orthop. Sports Phys. Ther. 2006;36(12):911–919. doi: 10.2519/jospt.2006.2244. [DOI] [PubMed] [Google Scholar]
- 32.Bulow A., Anderson J.E., Leiter J.R., MacDonald P.B., Peeler J. The modified star excursion balance and y-balance test results differ when assessing physically active healthy adolescent females. Int. J. Sports Phys. Ther. 2019;14(2):192–203. [PMC free article] [PubMed] [Google Scholar]
- 33.Schober P., Boer C., Schwarte L.A. Correlation coefficients: appropriate use and interpretation. Anesth. Analg. 2018;126(5):1763–1768. doi: 10.1213/ANE.0000000000002864. [DOI] [PubMed] [Google Scholar]
- 34.Massion J. Movement, posture and equilibrium: interaction and coordination. Prog. Neurobiol. 1992;38(1):35–56. doi: 10.1016/0301-0082(92)90034-c. [DOI] [PubMed] [Google Scholar]
- 35.Stapley P.J., Pozzo T., Cheron G., Grishin A. Does the coordination between posture and movement during human whole-body reaching ensure center of mass stabilization? Exp. Brain Res. 1999;129(1):134–146. doi: 10.1007/s002210050944. [DOI] [PubMed] [Google Scholar]
- 36.Robinson R., Gribble P. Kinematic predictors of performance on the star excursion balance test. J. Sport Rehabil. 2008;17(4):347–357. doi: 10.1123/jsr.17.4.347. [DOI] [PubMed] [Google Scholar]
- 37.Earl J.E., Hertel J. Lower-extremity muscle activation during the star excursion balance tests. J. Sport Rehabil. 2001;10(2):93–104. [Google Scholar]
- 38.Terrier R., Rose-Dulcina K., Toschi B., Forestier N. Impaired control of weight bearing ankle inversion in subjects with chronic ankle instability. Clin. BioMech. 2014;29(4):439–443. doi: 10.1016/j.clinbiomech.2014.01.005. [DOI] [PubMed] [Google Scholar]
- 39.Fox J., Docherty C.L., Schrader J., Applegate T. Eccentric plantar-flexor torque deficits in participants with functional ankle instability. J. Athl. Train. 2008;43(1):51–54. doi: 10.4085/1062-6050-43.1.51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Horan S.A., Watson S.L., Carty C.P., Sartori M., Weeks B.K. Lower-limb kinematics of single-leg squat performance in young adults. Physiother. Can. 2014;66(3):228–233. doi: 10.3138/ptc.2013-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Zeller B.L., McCrory J.L., Ben Kibler W., Uhl T.L. Differences in kinematics and electromyographic activity between men and women during the single-legged squat. Am. J. Sports Med. 2003;31(3):449–456. doi: 10.1177/03635465030310032101. [DOI] [PubMed] [Google Scholar]
- 42.de la Motte S., Arnold B.L., Ross S.E. Trunk-rotation differences at maximal reach of the star excursion balance test in participants with chronic ankle instability. J. Athl. Train. 2015;50(4):358–365. doi: 10.4085/1062-6050-49.3.74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Alexandrov A., Frolov A., Massion J. Axial synergies during human upper trunk bending. Exp. Brain Res. 1998;118(2):210–220. doi: 10.1007/s002210050274. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this investigation are available from the corresponding author upon reasonable request.