Abstract
BACKGROUND:
Hospital readmission is a significant contributor to increasing health care use related to caring for older trauma patients. This study was undertaken with the following aims: determine the proportion of older adult trauma patients who experience unplanned readmission, as well as risk factors for these readmissions and identify the most common readmission diagnoses among these patients.
STUDY DESIGN:
We conducted a retrospective cohort study of trauma patients age 55 years and older who survived their hospitalization at a statewide trauma center between 2009 and 2010. Linking 3 statewide databases, nonelective readmission rates were calculated for 30 days, 6 months, and 1 year after index discharge. Competing risk regression was used to determine risk factors for readmission and account for the competing risk of dying without first being readmitted. Subhazard ratios (SHR) are reported, indicating the relative risk of readmission by 30 days, 6 months, and 1 year.
RESULTS:
The cumulative readmission rates for the 14,536 participants were 7.9%, 18.9%, and 25.2% at 30 days, 6 months, and 1 year, respectively. In multivariable models, the strongest risk factors for readmission at 1 year (based on magnitude of SHR) were severe head injury (adjusted SHR = 1.47; 95% CI, 1.24–1.73) and disposition to a skilled nursing facility (SHR = 1.54; 95% CI, 1.39–1.71). The diagnoses most commonly associated with readmission were atrial fibrillation, anemia, and congestive heart failure.
CONCLUSIONS:
In this statewide study, unplanned readmissions after older adult trauma occurred frequently up to 1 year after discharge, particularly for patients who sustained severe head trauma and who could not be discharged home independently. Examining common readmission diagnoses might inform the development of interventions to prevent unplanned readmissions.
The US population is aging, with the elderly increasing both in absolute number and as a proportion of the total population. Elderly patients are over-represented in the trauma population. In Washington State, the annual number of patients aged 65 and older in the state trauma registry has increased from 4,266 in 2000 to 11,226 in 2012, corresponding to an increase in the percentage of the population that sustains trauma from 30% to 42% (Washington State Department of Health, unpublished data). In contrast, in 2013, persons aged 65 and older made up only 13.6% of the overall state population.1
Advanced age often predicts inferior outcomes after trauma, both in morbidity and mortality.2–4 Factors that might contribute to poor outcomes include comorbidities,5,6 increased severity of injury,7,8 and lack of physiologic reserve.9 Although the age cutoff commonly used to define a geriatric patient is 65 years, worse outcomes after trauma have been documented in patients starting at age 55 years.3,7
Older adult trauma places a burden on the health care system that is increasingly relevant as government and private funders recognize and attempt to curtail the increasing costs of medical care. Hospital readmission is a substantial contributor to this financial strain,10,11 and it has also been posited as a measure of quality of care.12,13 As a result of these concerns, in 2012, the Affordable Care Act instituted the Hospital Readmissions Reduction Program, allowing the Centers for Medicare and Medicaid Services to reduce payments to hospitals for perceived excess readmissions.14
Factors that contribute to readmission have been studied extensively in certain medical populations13,15; however surgical patients (including trauma patients) have not received the same level of attention.16–18 In light of the increasing demand placed on the health care system by older adult trauma, and to inform further policy discussion, we undertook this study with the following aims: determine the proportion of older patients who require unplanned readmission after hospitalization for trauma, as well as risk factors for these readmissions, and identify the most common readmission diagnoses among older patients requiring readmission after trauma.
METHODS
Setting, participants, and data sources
This retrospective cohort study included all trauma patients aged 55 years and older who were residents of Washington State and whose admission was captured by the Washington State Trauma Registry between January 2009 and December 2010. The Trauma Registry is an inclusive registry containing data from 81 designated trauma centers (Level I to V). Submission to the registry is required for all patients who have a traumatic diagnosis (ICD-9 diagnosis codes 800–904, 910–959, 994.1, 994.7, or 994.8) and one or more of the following: a full or modified trauma team activation; death on arrival to the facility; death within the facility; transfer out to another facility by Emergency Medical Services; transfer in from another facility by Emergency Medical Services; flown directly from the scene to the facility; all pediatric patients (aged 0 to 14 years); and all adult patients (aged 15+ years) with a facility length of stay >48 hours. Patients with isolated hip or femoral neck fractures and patients with isolated burns were excluded from this study. Only patients who survived their index trauma admission and were at risk for readmission were included. The registry provided patient and injury characteristics, as well as features of the index trauma admission. The earlier literature is not consistent with respect to the strata used for age when examining older adult injury,9,17,19 therefore, the current study used the following strata: 55 to 64, 65 to 74, 75 to 84, and 85+ years. Trauma center level was stratified as I/II vs III/IV/V, in keeping with earlier work within Washington State.2
To determine readmissions that occurred after trauma, the Trauma Registry was linked to the Comprehensive Hospital Abstract Reporting System (CHARS), a statewide database that contains hospital discharge information. The CHARS database includes all acute care hospitalizations in the state, allowing capture of readmissions to hospitals other than the index facility. As this study sought to examine both short- and long-term readmissions, CHARS data were included through December 2011. Only the first nonelective readmission after index trauma hospitalization was included (identified by categorization in CHARS) to maintain a focus on unexpected rehospitalizations. Cumulative readmission rates were then calculated for 30 days, 6 months, and 1 year after discharge from the index hospitalization. The Comprehensive Hospital Abstract Reporting System also provided ICD-9 diagnosis codes for the readmissions of interest. The 20 most common diagnostic codes for readmissions during each time interval were examined and the 10 most common are reported here.
To ensure that readmission rates were not biased by deaths that occurred after the index trauma hospitalization, the Trauma Registry and CHARS datasets were further linked to the Washington State Death Registry. Due to the use of competing risk analysis (see Statistical Analysis), we were interested in deaths that occurred out of hospital, without the patient first having been readmitted. We did not include deaths that occurred during a readmission, or deaths that occurred out of hospital after a readmission. Therefore, at each time point, we calculated the cumulative number of readmissions, the cumulative number of deaths that occurred without having been readmitted to hospital, and the cumulative number of people who survived without having been readmitted to hospital. The primary outcomes of the study included the cumulative percentage of patients with unplanned readmission by each of the study time points, as well as the risk factors for unplanned readmission. Secondary outcomes included risk factors for death without readmission. In addition, the most common diagnoses responsible for unplanned readmissions in this population were examined.
Statistical analyses
The study population was described with respect to patient, injury, and index hospitalization characteristics. To further characterize the factors associated with an increased risk of readmission, a multivariable competing risk regression model was used. Competing risk analysis is a type of survival analysis that statistically accounts for the presence of competing events that preclude the future outcomes of interest.20
We suspected that out-of-hospital deaths after trauma would be relatively frequent in this population, so we used competing risk regressions with time-specific readmissions as the outcomes of interest, and death without earlier hospitalization as the competing event. To further account for the suspected frequency of out-of-hospital deaths in this population, we created a reverse model in which deaths without earlier readmission were the outcomes of interest, and readmission was the competing event. This reverse model can be used to further understand the factors associated with readmission. For example, patient groups who appear to be at a low risk of readmission might appear this way because they have a high risk of dying and, therefore, are not alive to be at risk of readmission.21
Both multivariable competing risk models incorporated the following variables, all determined at the time of the index hospitalization: age, sex, insurance type, Charlson Comorbidity Index, mechanism of injury, Injury Severity Score (ISS), maximum head Abbreviated Injury Scale (AIS) score, trauma center level, ICU admission, modified Functional Independence Measure (FIM) score at index discharge, and discharge disposition location. The modified FIM is a measure of functional outcomes that is a shortened version of the original FIM. It has a range of 3 to 12, where 3 indicates complete functional dependence and 12 indicates independence.22,23 Approximately 11% of values for the modified FIM were missing and were therefore imputed before regression using the method of chained equations with a total of 5 imputations.24,25 Competing risk regression reports subhazard ratios (SHR), which in this study indicate the relative risk of readmission between groups at any moment in the specified time period. An SHR of 1 indicates that there is no difference in risk of readmission between groups. All statistical analyses were performed using Stata version 12.0 (Stata Corp). Statistical significance for an SHR was defined as the 95% CI of the SHR, excluding 1.0. The study was performed with approval from the Washington State IRB.
RESULTS
In 2009–2010, there were 31,071 adult patients captured by the Trauma Registry, of which 15,914 (51.2%) were aged 55 years and older. The 14,536 patients who survived their index trauma hospitalization were the population of interest in this study (Fig. 1). Characteristics of the patients, injuries, and index hospitalizations are shown in Table 1.
Figure 1.
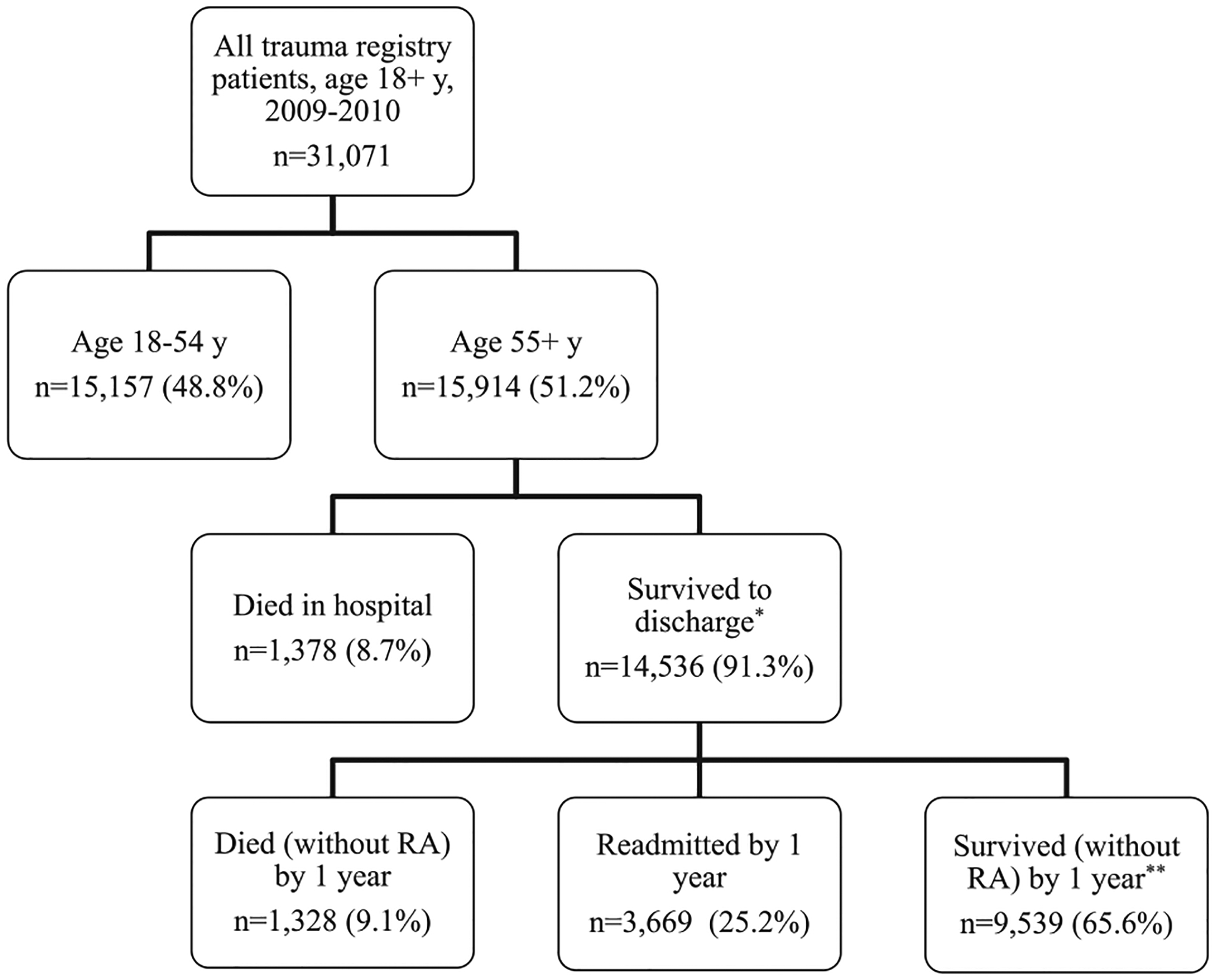
Flowchart of patient selection and outcomes. Each row totals 100%. *The group “Survived to Discharge” is the cohort examined in the current study. **“Survived without Readmission” is presumptive, based on not being readmitted and not dying during the year. RA, readmission.
Table 1.
Characteristics of Study Population by Outcomes at the End of the Study Period (1 Year Post-Discharge)
| By outcomes at end of study period* | ||||||||
|---|---|---|---|---|---|---|---|---|
| Overall* (n = 14,536) | Readmitted (n = 3,669) | Died without readmission (n = 1,328) | Survived without readmission (n = 9,539) | |||||
| n | % | n | % | n | % | n | % | |
| Age group, y† | ||||||||
| 55–64 | 3,821 | 26.3 | 757 | 20.6 | 84 | 6.3 | 2,980 | 31.2 |
| 65–74 | 2,946 | 20.3 | 736 | 20.1 | 145 | 10.9 | 2,065 | 21.7 |
| 75–84 | 3,787 | 26.0 | 1,051 | 28.6 | 340 | 25.6 | 2,396 | 25.1 |
| 85+ | 3,981 | 27.4 | 1,125 | 30.7 | 759 | 57.2 | 2,097 | 22.0 |
| Sex† | ||||||||
| Female | 8,416 | 57.9 | 2,166 | 59.0 | 754 | 56.8 | 5,496 | 57.6 |
| Male | 6,118 | 42.1 | 1,503 | 41.0 | 574 | 43.2 | 4,041 | 42.4 |
| Charlson Comorbidity Index | ||||||||
| 0 | 14,038 | 96.6 | 3,501 | 95.4 | 1,241 | 93.4 | 9,296 | 97.4 |
| 1+ | 498 | 3.4 | 168 | 4.6 | 87 | 6.6 | 243 | 2.6 |
| Injury mechanism† | ||||||||
| Blunt‡ | 2,800 | 19.3 | 529 | 14.4 | 74 | 5.6 | 2,197 | 23.0 |
| Penetrating | 231 | 1.6 | 26 | 0.7 | 7 | 0.5 | 198 | 2.1 |
| Falls | 11,253 | 77.4 | 3,045 | 83.0 | 1,238 | 93.2 | 6,970 | 73.2 |
| Other | 241 | 1.7 | 68 | 1.8 | 9 | 0.7 | 164 | 1.7 |
| ISS | ||||||||
| 0–8 | 4,929 | 33.9 | 1,517 | 41.3 | 319 | 24.0 | 3,093 | 32.4 |
| 9–15 | 6,711 | 46.2 | 1,353 | 36.9 | 740 | 55.7 | 4,618 | 48.4 |
| 16–24 | 1,900 | 13.1 | 529 | 14.4 | 166 | 12.5 | 1,205 | 12.6 |
| ≥25 | 967 | 6.6 | 257 | 7.0 | 101 | 7.6 | 609 | 6.4 |
| Missing | 29 | 0.2 | 13 | 0.4 | 2 | 0.2 | 14 | 0.1 |
| Maximum head AIS | ||||||||
| ≤3 | 12,767 | 87.8 | 3,106 | 84.7 | 1,120 | 84.3 | 8,541 | 89.5 |
| >3 | 1,769 | 12.2 | 563 | 15.3 | 208 | 15.7 | 998 | 10.5 |
| Trauma center level | ||||||||
| I/II | 5,696 | 39.2 | 1,509 | 41.1 | 381 | 28.7 | 3,806 | 39.9 |
| III/IV/V | 8,753 | 60.2 | 2,129 | 58.0 | 942 | 70.9 | 5,682 | 59.6 |
| Missing | 87 | 0.6 | 31 | 0.9 | 5 | 0.4 | 51 | 0.5 |
| ICU admission† | ||||||||
| No | 11,235 | 77.3 | 2,763 | 75.3 | 1,035 | 77.9 | 7,437 | 78.0 |
| Yes | 3,292 | 22.6 | 905 | 24.7 | 293 | 22.1 | 2,094 | 22.0 |
| FIM score at index discharge | ||||||||
| 11–12 | 7,023 | 48.3 | 1,658 | 45.2 | 304 | 22.9 | 5,061 | 53.1 |
| 8–10 | 4,818 | 33.1 | 1,354 | 36.9 | 453 | 34.1 | 3,011 | 31.6 |
| 3–7 | 1,105 | 7.6 | 274 | 7.5 | 312 | 23.5 | 519 | 5.4 |
| Missing | 1,590 | 10.9 | 383 | 10.4 | 259 | 19.5 | 948 | 9.9 |
| Discharge disposition | ||||||||
| Home, independent | 4,787 | 32.9 | 961 | 26.2 | 125 | 9.4 | 3,701 | 38.8 |
| Home, with assist | 1,150 | 7.9 | 313 | 8.5 | 87 | 6.6 | 750 | 7.9 |
| Rehabilitation | 810 | 5.6 | 226 | 6.2 | 28 | 2.1 | 556 | 5.8 |
| SNF | 6,703 | 46.1 | 1,997 | 54.4 | 858 | 64.6 | 3,848 | 40.3 |
| Other§ | 1,086 | 7.5 | 172 | 4.7 | 230 | 17.3 | 684 | 7.2 |
Percentages might not sum to 100 due to rounding.
Variables were missing <0.1% of values.
Blunt injuries excluding falls.
Includes patients discharged to hospice care.
AIS, Abbreviated Injury Scale score; FIM, modified Functional Independence Measure; ISS, Injury Severity Score; SNF, skilled nursing facility.
At 30 days from index hospitalization discharge, 1,145 patients had already had an unplanned readmission (7.9%), with 2,718 (18.7%) being readmitted by 6 months and 3,669 (25.2%) being readmitted by 1 year (Fig. 2).
Figure 2.
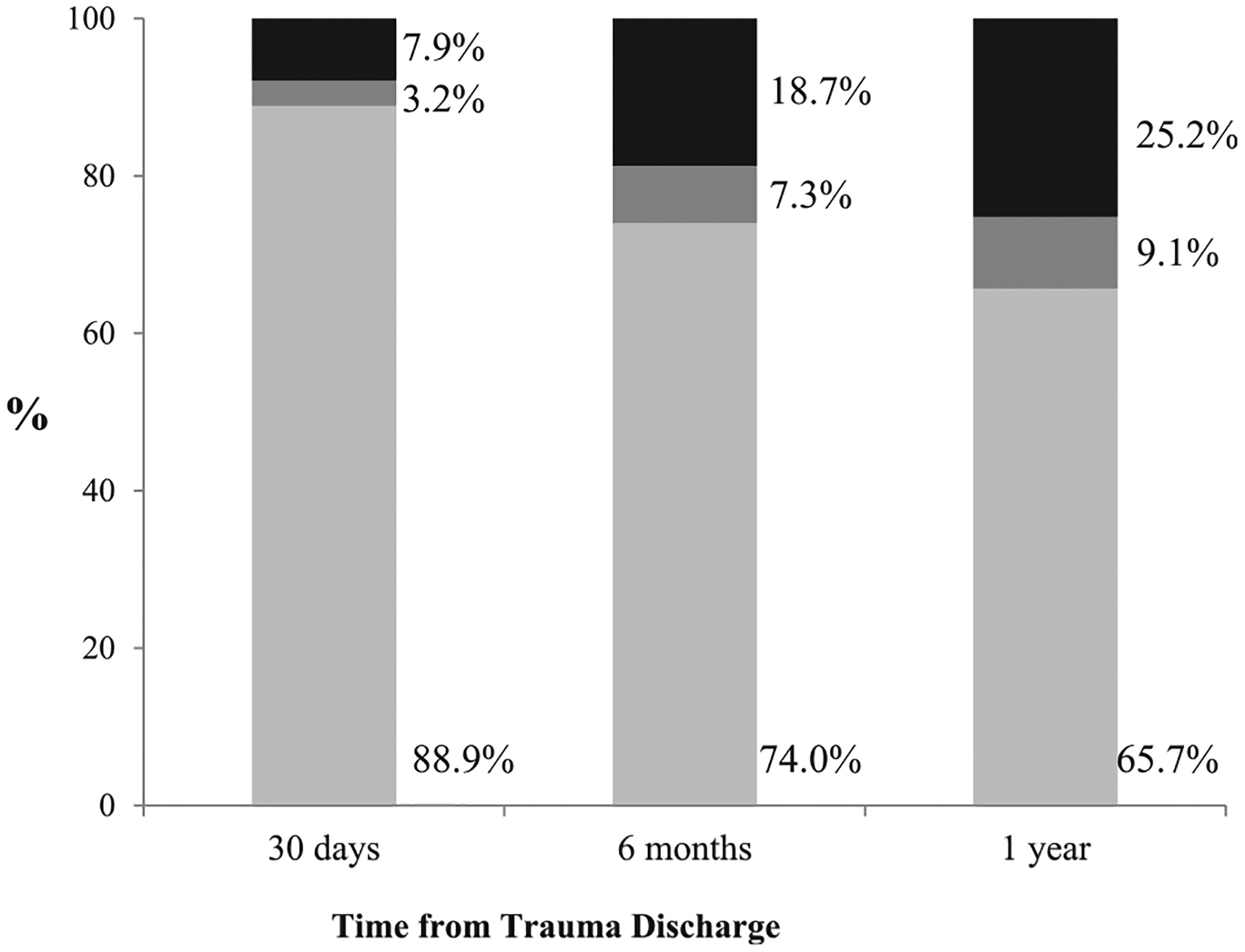
Cumulative patient outcomes at 30 days, 6 months, and 1 year from trauma discharge. Each column totals the whole study population (N = 14,536). Black bar, readmitted; dark gray bar, died without readmission; light gray bar, survived without readmission (presumptive, based on not being readmitted and not dying during the year).
The multivariable competing risk regression model identified several factors that placed patients at significantly increased risk for readmission by each of the 3 study time points (Table 2). For mechanism of injury, falls were a risk factor for readmission (30 day SHR = 1.21; 95% CI, 1.01–1.45; 6-month SHR = 1.30; 95% CI, 1.15–1.48; 1-year SHR = 1.29; 95% CI, 1.16–1.43). Severe head injury (indicated by a maximum head AIS >3) was strongly predictive of readmission at all end points (30-day SHR = 1.34; 95% CI, 1.04–1.73; 6-month SHR = 1.41; 95% CI, 1.18–1.70; 1-year SHR = 1.47; 95% CI, 1.24–1.73). Likewise, admission to the ICU was a risk factor for rehospitalization, although the magnitude of this risk decreased with time (30-day SHR = 1.32; 95% CI, 1.11–1.58; 6-month SHR = 1.25; 95% CI, 1.11–1.40; 1-year SHR = 1.16; 95% CI, 1.05–1.28). Patients who had their index admission to a Level III/IV/V trauma center were less likely to be readmitted than those who were at Level I or II centers (30-day SHR = 0.78; 95% CI, 0.68–0.89; 6-month SHR = 0.81; 95% CI, 0.74–0.88; 1-year SHR = 0.79; 95% CI, 0.73–0.85).
Table 2.
Multivariable Competing Risk Analysis of Time to Readmission and Time to Death without Readmission
| 30 Days | 6 Months | 1 Year | ||||
|---|---|---|---|---|---|---|
| Readmission, adjusted* SHR (95% CI) | Death without readmission, adjusted* SHR (95% CI) | Readmission, adjusted* SHR (95% CI) | Death without readmission, adjusted* SHR (95% CI) | Readmission, adjusted* SHR (95% CI) | Death without readmission, adjusted* SHR (95% CI) | |
| Age group, y | ||||||
| 55–64 | Reference | Reference | Reference | Reference | Reference | Reference |
| 65–74 | 1.01 (0.82–1.23) | 1.01 (0.62–1.67) | 1.03 (0.90–1.17) | 1.81 (1.30–2.54) | 1.05 (0.94–1.18) | 1.87 (1.40–3.72) |
| 75–84 | 0.95 (0.77–1.17) | 2.02 (1.30–3.13) | 1.00 (0.88–1.15) | 2.74 (1.99–3.77) | 1.06 (0.95–1.20) | 2.82 (2.13–3.72) |
| 85+ | 0.90 (0.73–1.12)) | 4.09 (2.66–6.28) | 1.04 (0.91–1.20) | 5.51 (4.03–7.54) | 1.10 (0.97–1.24) | 5.63 (4.28–7.40) |
| Sex | ||||||
| Female | Reference | Reference | Reference | Reference | Reference | Reference |
| Male | 1.16 (1.02–1.31) | 1.69 (1.38–2.06) | 1.07 (0.98–1.16) | 1.54 (1.35–1.76) | 1.06 (0.98–1.13) | 1.51 (1.34–1.70) |
| Insurance type | ||||||
| Commercial | Reference | Reference | Reference | Reference | Reference | Reference |
| Government† | 0.68 (0.52–0.90) | 0.89 (0.51–1.57) | 0.92 (0.77–1.09) | 1.12 (0.79–1.58) | 1.05 (0.91–1.21) | 1.10 (0.81–1.49) |
| Medicare | 1.11 (0.94–1.32) | 0.98 (0.74–1.30) | 1.21 (1.08–1.35) | 1.08 (0.89–1.30) | 1.23 (1.11–1.35) | 1.01 (0.86–1.18) |
| None | 0.85 (0.57–1.24) | 0.81 (0.38–1.74) | 0.99 (0.77–1.27) | 0.90 (0.52–1.55) | 0.97 (0.78–1.21) | 0.78 (0.47–1.29) |
| CCI | ||||||
| 0 | Reference | Reference | Reference | Reference | Reference | Reference |
| 1+ | 1.05 (0.76–1.45) | 1.42 (0.99–2.04) | 1.37 (1.15–1.64) | 1.32 (1.03–1.71) | 1.36 (1.16–1.58) | 1.37 (1.10–1.71) |
| Injury mechanism | ||||||
| Blunt‡ | Reference | Reference | Reference | Reference | Reference | Reference |
| Penetrating | 0.56 (0.28–1.13) | 0.68 (0.08–5.61) | 0.68 (0.44–1.05) | 1.30 (0.48–3.50) | 0.57 (0.38–0.86) | 1.35 (0.60–3.03) |
| Fall | 1.21 (1.01–1.45) | 3.83 (2.31–6.35) | 1.30 (1.15–1.48) | 2.57 (1.91–3.44) | 1.29 (1.16–1.43) | 2.24 (1.74–2.86) |
| Other | 1.32 (0.84–2.07) | 2.72 (0.63–11.77) | 1.29 (0.94–1.77) | 2.17 (0.93–5.07) | 1.39 (1.07–1.80) | 1.96 (0.94–4.12) |
| ISS category | ||||||
| 0–8 | Reference | Reference | Reference | Reference | Reference | Reference |
| 9–15 | 0.64 (0.56–0.73) | 1.15 (0.91–1.46) | 0.58 (0.53–0.63) | 1.44 (1.24–1.69) | 0.57 (0.53–0.61) | 1.49 (1.30–1.71) |
| 16–24 | 0.84 (0.65–1.09) | 1.61 (1.00–2.60) | 0.70 (0.58–0.84) | 1.43 (1.03–2.00) | 0.67 (0.57–0.78) | 1.28 (0.94–1.74) |
| 25+ | 0.82 (0.60–1.13) | 1.84 (1.03–3.28) | 0.62 (0.49–0.78) | 1.61 (1.06–2.43) | 0.57 (0.46–0.70) | 1.48 (1.00–2.17) |
| Maximum head AIS | ||||||
| ≤3 | Reference | Reference | Reference | Reference | Reference | Reference |
| >3 | 1.34 (1.04–1.73) | 1.05 (0.67–1.64) | 1.41 (1.18–1.70) | 1.09 (0.79–1.52) | 1.47 (1.24–1.73) | 1.22 (0.90–1.67) |
| Trauma center level | ||||||
| I/II | Reference | Reference | Reference | Reference | Reference | Reference |
| III/IV/V | 0.78 (0.68–0.89) | 0.86 (0.67–1.09) | 0.81 (0.74–0.88) | 1.02 (0.87–1.20) | 0.79 (0.73–0.85) | 1.02 (0.88–1.18) |
| ICU admission | ||||||
| No | Reference | Reference | Reference | Reference | Reference | Reference |
| Yes | 1.32 (1.11–1.58) | 0.90 (0.67–1.21) | 1.25 (1.11–1.40) | 1.13 (0.93–1.38) | 1.16 (1.05–1.28) | 1.03 (0.86–1.23) |
| FIM score at discharge | ||||||
| 11–12 | Reference | Reference | Reference | Reference | Reference | Reference |
| 8–10 | 1.14 (0.98–1.32) | 2.05 (1.43–2.93) | 1.01 (0.92–1.11) | 1.43 (1.15–1.77) | 1.01 (0.93–1.10) | 1.34 (1.11–1.61) |
| 3–7 | 1.03 (0.81–1.30) | 7.38 (5.21–10.47) | 0.86 (0.73–1.01) | 3.68 (2.95–4.59) | 0.87 (0.75–0.99) | 3.23 (2.65–3.94) |
| Discharge disposition | ||||||
| Home | Reference | Reference | Reference | Reference | Reference | Reference |
| Home with assist | 1.34 (1.05–1.70) | 2.78 (1.72–4.51) | 1.30 (1.10–1.52) | 2.10 (1.51–2.90) | 1.32 (1.15–1.51) | 1.82 (1.37–2.41) |
| Rehabilitation | 1.15 (0.87–1.52) | 0.32 (0.12–0.84) | 1.42 (1.18–1.70) | 0.68 (0.42–1.10) | 1.35 (1.15–1.58) | 0.60 (0.39–0.92) |
| SNF | 1.44 (1.20–1.73) | 1.52 (0.97–2.38) | 1.59 (1.41–1.79) | 2.00 (1.51–2.63) | 1.54 (1.39–1.71) | 1.87 (1.48–2.37) |
| Other§ | 0.68 (0.49–0.95) | 6.26 (3.98–9.86) | 0.84 (0.69–1.03) | 4.89 (3.66–6.54) | 0.78 (0.65–0.93) | 4.19 (3.27–5.39) |
Statistical significance in indicated by 95% CIs that exclude 1.00.
Adjusted for age, sex, insurance type, Charlson Comorbidity Index, mechanism of injury, ISS, maximum head AIS score, trauma center Level (I/II vs III/IV/V), ICU admission, modified FIM score at index discharge, and discharge disposition location.
Government insurance excluding Medicare.
Blunt injuries excluding falls.
Includes patients discharged to hospice care.
AIS, Abbreviated Injury Scale score; CCI, Charlson Comorbidity Index; FIM, modified Functional Independence Measure; ISS, Injury Severity Score; SHR, subhazard ratio; SNF, skilled nursing facility.
Compared with being discharged home independently after the index trauma admission, patients who were discharged home with assistance or to skilled nursing facilities (SNFs) were more likely to be readmitted in the follow-up period, particularly those discharged to SNFs (30-day SHR = 1.44; 95% CI, 1.20–1.73; 6-month SHR = 1.59; 95% CI, 1.41–1.79; 1-year SHR = 1.54; 95% CI, 1.39–1.71). Other variables examined either did not significantly increase or decrease the risk of readmission, or did so variably by time end point.
With respect to the multivariable analysis of death without first having been readmitted (readmission being the competing event), the risk factors at all 3 time end points were older age, male sex, falls as mechanism of injury, functional impairment (modified FIM scores of ≤10), and disposition to home with assistance or to rehabilitation (Table 2).
The ICD-9 diagnosis codes that were recorded for the readmissions in this study were compiled (up to 20 per readmission), and the 3 codes that were noted most commonly were the same for all readmission end points; atrial fibrillation, anemia (“post-hemorrhagic” or “other/unspecified”), and congestive heart failure (“acute on chronic” or “unspecified”) (Table 3). These diagnoses accounted for a mean of 14%, 14%, and 12% of readmission diagnoses, respectively.
Table 3.
Most Common ICD-9 Diagnoses for Readmissions by 30 Days, 6 Months, and 1 Year
| 30 Days (n = 2,283)* | 6 Months (n = 5,380)* | 1 Year (n = 7,130)* | ||||||
|---|---|---|---|---|---|---|---|---|
| Diagnosis | n | % | Diagnosis | n | % | Diagnosis | n | % |
| Atrial fibrillation | 304 | 13.3 | Atrial fibrillation | 746 | 13.9 | Atrial fibrillation | 1,017 | 14.3 |
| Anemia (post-hemorrhagic and other) | 300 | 13.1 | Anemia (post-hemorrhagic and other) | 742 | 13.8 | Anemia (post-hemorrhagic and other) | 974 | 13.7 |
| Congestive heart failure (unspecified and acute-on-chronic) | 260 | 11.4 | Congestive heart failure (unspecified and acute-on-chronic) | 635 | 11.8 | Congestive heart failure (unspecified and acute-on-chronic) | 834 | 11.7 |
| Dehydration | 258 | 11.3 | Dehydration | 627 | 11.6 | Dehydration | 824 | 11.6 |
| Urinary tract infection | 247 | 10.8 | Urinary tract infection | 604 | 11.2 | Urinary tract infection | 793 | 11.1 |
| Acute renal failure | 192 | 8.4 | Acute renal failure | 462 | 8.6 | Acute renal failure | 610 | 8.6 |
| Pneumonia | 141 | 6.2 | Pneumonia | 329 | 6.1 | Pneumonia | 453 | 6.4 |
| Acute respiratory failure (acute and acute-on-chronic) | 117 | 5.1 | Acute respiratory failure (acute and acute-on-chronic) | 274 | 5.1 | Acute respiratory failure (acute and acute-on-chronic) | 353 | 5.0 |
| Aspiration pneumonia | 84 | 3.7 | Aspiration pneumonia | 164 | 3.0 | Aspiration pneumonia | 211 | 3.0 |
| Traumatic subdural hemorrhage (after injury, with and without concussion) | 56 | 2.4 | COPD exacerbation | 137 | 2.6 | COPD exacerbation | 202 | 2.8 |
Denotes the sum of the 20 most common diagnoses at each time end point. The numbers and percentages shown here are in relation to that sum, and therefore reflect the relative frequency of each diagnosis. Only 10 most common diagnoses are shown for brevity.
DISCUSSION
Older adult patients have a high likelihood of rehospitalization after trauma, and that risk is maintained even a year after the index admission. This study used competing risk regression and demonstrated that the patients with the highest risk of readmission in the year after injury were those who had falls, those who had a severe head injury, those admitted to the ICU on their index admission, and those who could not be discharged home independently.
Previous studies have found that 30-day readmission rates after trauma range from 4.3% to 13.7%.17,18,26 However, only Spector and colleagues17 focused on older adults, finding a 30-day readmission rate that was considerably higher than in the current study (13.7% vs 7.9%).17 This difference might be accounted for by the fact that their study cohort was older (65 years and older) and therefore perhaps more prone to rehospitalization. In addition, the most common reason for readmission in that study was surgery of the extremities, which, in the current study would likely have been excluded by virtue of being elective. Finally, the current study included index trauma admissions only from hospitals with a statewide trauma center designation, and the study by Spector and colleagues included all acute care hospitals. However, the Washington State Trauma System is unique in that the majority of acute care facilities in the state (81 of 93) have a trauma center designation and were therefore included in this analysis.
Discharge to an SNF was the strongest independent predictor of readmission in this study, in terms of magnitude of SHR, which is important, considering that 46% of the patients were discharged to an SNF. Earlier studies have shown that discharge to an SNF conveys an increased risk of both hospital readmission and post-hospital death in all-age trauma patients,2 as well as older trauma patients.27A possible explanation might be the differences between patients discharged to SNF rather than home independently, particularly from a functional standpoint, although the current study was not designed to answer this question.
Despite being developed to predict poor outcomes in terms of in-hospital mortality,28 patients with higher Injury Severity Scores (ISS) were actually less likely to be readmitted compared with those with mild injury (ISS = 0 to 8). Other studies have similarly found that ISS has been an inconsistent predictor of longer-term outcomes after trauma.2,29 On the other hand, the apparent “protective” effect of increasing ISS can relate to the use of a competing risk model in a population where the proportion of patients experiencing the competing event is high.20,21 This is understood by examining the reverse competing risk model of death without readmission. Patients with higher ISS scores were at increased risk of out-of-hospital death, possibly nullifying any elevated risk of readmission from a statistical standpoint.21
In a similar fashion, our multivariable model showed that patients who were considered to be functionally severely dependent at index discharge (modified FIM scores of 3 to 7) were significantly less likely to be readmitted than those who were completely independent (modified FIM scores of 11 to 12). However, there was a high risk of mortality among patients with severe functional impairment, which can be interpreted by postulating that they were not at increased risk of being readmitted because they had such a high risk of dying first.
Although the use of the CHARS database did not allow differentiation of the primary diagnosis for each readmission from all other diagnoses, it is interesting to note that the most common diagnoses were largely medical rather than surgical in nature. Similarly, Jencks and colleagues13 found that >70% of 30-day readmissions in a mixed surgical population were due to medical diagnoses.
Recognizing this need for specialized care of older adults who sustain injury, several interventions have shown benefit in improving in-hospital outcomes of injured elderly patients. These include co-management by surgeons and geriatricians,30 as well as creation of formal geriatric trauma consultation services.31,32 This need for focused care has also led to the creation of geriatric trauma centers, with requirements for specialized personnel (including full-time geriatrician coverage), practice standards for conditions common in older populations, and close ties with post–acute care facilities.33 The ability of these efforts to decrease unplanned readmissions has not been examined in older adult trauma patients; however, in light of the most common readmission diagnoses in the current study, it is possible that similar interventions would have an impact.
Additionally, given that many trauma hospitals discharge patients to a focused number of SNFs, improving care transitions (eg, by communicating detailed care plans to providers at the SNF) and participating in the creation of standardized levels of care quality in the facilities to which they discharge can represent specific opportunities whereby hospitals can reduce readmissions.
Due to current health care–related financial constraints, there is a growing focus on value-based health care, the premise of which is to optimize health care quality and outcomes and minimize costs. By withholding payments to hospitals for excess readmissions, the Centers for Medicare and Medicaid Services is hoping to encourage improvements in patient outcomes and decrease costs. The use of these financial penalties for hospitals with excess readmissions is predicated on two assumptions: the first is that readmission is a marker of quality of care, and the second is that hospitals have the capacity to prevent a proportion of readmissions. Unfortunately, the association between quality of care during an index admission and subsequent readmission is inconsistent.12,16,34,35 Similarly, the evidence for the preventability of readmissions is also variable,36 which might partially be due to the subjectivity that is inherent in determining preventability.37
A strength of this study is the use of competing risk analysis, particularly given the frequency with which death without an earlier readmission occurred. Many studies that analyze readmissions using survival analysis techniques censor patients who die without first having being readmitted. However, in study populations where death is relatively common, it is more appropriately treated as a competing event (one that precludes future outcomes of interest). Studies have shown that in some cases in which standard survival analysis is used and competing events are not treated appropriately from a statistical standpoint, the risk of the outcomes of interest can be considerably overestimated.21 Competing risk analysis was chosen in this study to decrease the likelihood of overestimating the relative risk of readmission between groups, based on the covariates of interest.
Additionally, earlier studies have shown that readmissions commonly occur at hospitals other than the index facility,26 and the use of statewide data allowed us to capture more of these readmissions. The detail of the CHARS database also permitted exclusion of elective readmissions, therefore, targeting unplanned rehospitalizations.
The study does have a number of limitations, the first of which is its retrospective nature. This investigation captured patients who had their index trauma admission at one of the state’s 81 designated trauma centers; however, injured patients admitted to the 12 other acute care facilities in the state were not included. In addition, retrospective studies such as this can be limited in their documentation of patient comorbidities, likely an important contributor to readmission risk. This is demonstrated by the fact that the vast majority of our older adult patients had a Charlson Comorbidity Index score of 0, indicating no comorbidities. Additionally, the readmissions that were captured in this study did not include visits to the emergency department, admissions under observation status, or readmissions in other states, thereby underestimating the health care use burden. However, study inclusion of only Washington State residents likely minimized the latter. Finally, the CHARS database does not highlight the primary admitting diagnosis, with obvious implications for assessing the preventability of readmissions in this study.
CONCLUSIONS
Despite the ongoing debate surrounding the quality of care implications and preventability of excess hospital readmissions, they remain a focus for health care payers. In this study, unplanned readmissions after trauma in older adults caused high health care use even up to 1 year after discharge, particularly for those patients who had falls, who sustained severe head trauma, who were admitted to the ICU, and who could not be discharged home independently. The reasons for readmission were likely multifactorial, but the commonality of medical comorbidities as the diagnoses of admission suggests that targeting high-risk populations with optimization of these conditions (with the assistance of geriatric specialists, for example), as well as ensuring adequate communication of care plans with post-discharge providers, might have the potential to reduce preventable readmissions.
Abbreviations and Acronyms
- AIS
Abbreviated Injury Scale
- CHARS
Comprehensive Hospital Abstract Reporting System
- FIM
Functional Independence Measure
- ISS
Injury Severity Score
- SHR
subhazard ratio
- SNF
skilled nursing facility
Footnotes
Author Contributions
Study conception and design: Fawcett, Flynn-O’Brien, Shorter, Rivara, Arbabi
Acquisition of data: Shorter
Analysis and interpretation of data: Fawcett, Flynn-O’Brien, Shorter, Davidson, Bulger, Rivara, Arbabi
Drafting of manuscript: Fawcett, Rivara, Arbabi
Critical revision: Flynn-O’Brien, Shorter, Davidson, Bulger, Rivara, Arbabi
CME questions for this article available at http://jacscme.facs.org
Disclosure Information: Authors have nothing to disclose. Timothy J Eberlein, Editor-in-Chief, has nothing to disclose.
Presented at the American College of Surgeons Committee on Trauma Annual Meeting, Philadelphia PA, March 2014.
REFERENCES
- 1.US Census Bureau. State & county quickfacts. Washington, DC. Available from: www.quickfacts.census.gov/qfd/states/53000.html. Accessed June 2, 2014. [Google Scholar]
- 2.Davidson GH, Hamlat CA, Rivara FP, et al. Long-term survival of adult trauma patients. JAMA 2011;305:1001–1007. [DOI] [PubMed] [Google Scholar]
- 3.MacKenzie EJ, Rivara FP, Jurkovich GJ, et al. A national evaluation of the effect of trauma-center care on mortality. N Engl J Med 2006;354:366–378. [DOI] [PubMed] [Google Scholar]
- 4.Thompson HJ, McCormick WC, Kagan SH. Traumatic brain injury in older adults: epidemiology, outcomes, and future implications. J Am Geriatr Soc 2006;54:1590–1595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Taylor MD, Tracy JK, Meyer W, et al. Trauma in the elderly: intensive care unit resource use and outcome. J Trauma 2002; 53:407–414. [DOI] [PubMed] [Google Scholar]
- 6.Grossman MD, Miller D, Scaff DW, Arcona S. When is an elder old? Effect of preexisting conditions on mortality in geriatric trauma. J Trauma 2002;52:242–246. [DOI] [PubMed] [Google Scholar]
- 7.Kuhne CA, Ruchholtz S, Kaiser GM, Nast-Kolb D Working Group on Multiple Trauma of the German Society of Trauma. Mortality in severely injured elderly trauma patients—when does age become a risk factor? World J Surg 2005;29: 1476–1482. [DOI] [PubMed] [Google Scholar]
- 8.Keller JM, Sciadini MF, Sinclair E, O’Toole RV. Geriatric trauma: demographics, injuries, and mortality. J Orthop Trauma 2012;26:e161–e165. [DOI] [PubMed] [Google Scholar]
- 9.Bennett KM, Scarborough JE, Vaslef S. Outcomes and health care resource utilization in super-elderly trauma patients. J Surg Res 2010;163:127–131. [DOI] [PubMed] [Google Scholar]
- 10.Bosco JA III, Karkenny AJ, Hutzler LH, et al. Cost burden of 30-day readmissions following Medicare total hip and knee arthroplasty. J Arthroplast 2014;29[5]:903–905. [DOI] [PubMed] [Google Scholar]
- 11.Keller DS, Swendseid B, Khorgami Z, et al. Predicting the unpredictable: comparing readmitted versus non-readmitted colorectal surgery patients. Am J Surg 2014;207:346–351; discussion 350–351. [DOI] [PubMed] [Google Scholar]
- 12.Ashton CM, Del Junco DJ, Souchek J, et al. The association between the quality of inpatient care and early readmission: a meta-analysis of the evidence. Med Care 1997;35:1044–1059. [DOI] [PubMed] [Google Scholar]
- 13.Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med 2009;360:1418–1428. [DOI] [PubMed] [Google Scholar]
- 14.Readmissions-Reduction-Program. Centers for Medicare and Medicaid Services. [cited 2014 Apr 14]. Available at: http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/Readmissions-Reduction-Program.html. Accessed June 2, 2014.
- 15.Franchi C, Nobili A, Mari D, et al. Risk factors for hospital readmission of elderly patients. Eur J Intern Med 2013;24:45–51. [DOI] [PubMed] [Google Scholar]
- 16.Tsai TC, Joynt KE, Orav EJ, et al. Variation in surgical-readmission rates and quality of hospital care. N Engl J Med 2013;369:1134–1142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Spector WD, Mutter R, Owens P, Limcangco R. Thirty-day, all-cause readmissions for elderly patients who have an injury-related inpatient stay. Med Care 2012;50:863–869. [DOI] [PubMed] [Google Scholar]
- 18.Morris DS, Rohrbach J, Sundaram LMT, et al. Early hospital readmission in the trauma population: are the risk factors different? Injury 2014;45:56–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bonne S, Schuerer DJE. Trauma in the older adult: epidemiology and evolving geriatric trauma principles. Clin Geriatr Med 2013;29:137–150. [DOI] [PubMed] [Google Scholar]
- 20.Lau B, Cole SR, Gange SJ. Competing risk regression models for epidemiologic data. Am J Epidemiol 2009;170: 244e256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Grams ME, Coresh J, Segev DL, et al. Vascular disease, ESRD, and death: interpreting competing risk analyses. Clin J Am Soc Nephrol 2012;7:1606–1614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Williamson OD, Gabbe BJ, Sutherland AM, et al. Comparing the responsiveness of functional outcome assessment measures for trauma registries. J Trauma 2011;71:63–68. [DOI] [PubMed] [Google Scholar]
- 23.Susman M, DiRusso SM, Sullivan T, et al. Traumatic brain injury in the elderly: increased mortality and worse functional outcome at discharge despite lower injury severity. J Trauma 2002;53:219–223, discussion 223–224. [DOI] [PubMed] [Google Scholar]
- 24.van Buuren S, Boshuizen HC, Knook DL. Multiple imputation of missing blood pressure covariates in survival analysis. Stat Med 1999;18:681–694. [DOI] [PubMed] [Google Scholar]
- 25.Royston P. Multiple imputation of missing values: update of ice. Stata J 2005;5:527–536. [Google Scholar]
- 26.Moore L, Stelfox HT, Turgeon AF, et al. Rates, patterns, and determinants of unplanned readmission after traumatic injury: a multicenter cohort study. Ann Surg 2014;259:374–380. [DOI] [PubMed] [Google Scholar]
- 27.Ayoung-Chee P, McIntyre L, Ebel BE, et al. Long-term outcomes of ground-level falls in the elderly. J Trauma Acute Care Surg 2014;76:498–503. [DOI] [PubMed] [Google Scholar]
- 28.Linn S. The Injury Severity Score—importance and uses. Ann Epidemiol 1995;5:440–446. [DOI] [PubMed] [Google Scholar]
- 29.Claridge JA, Leukhardt WH, Golob JF, et al. Moving beyond traditional measurement of mortality after injury: evaluation of risks for late death. J Am Coll Surg 2010;210:788–794, 794–796. [DOI] [PubMed] [Google Scholar]
- 30.Rocca Della GJ, Moylan KC, Crist BD, et al. Comanagement of geriatric patients with hip fractures: a retrospective, controlled, cohort study. Geriatr Orthop Surg Rehabil 2013; 4:10–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Fallon WF, Rader E, Zyzanski S, et al. Geriatric outcomes are improved by a geriatric trauma consultation service. J Trauma 2006;61:1040–1046. [DOI] [PubMed] [Google Scholar]
- 32.Lenartowicz M, Parkovnick M, McFarlan A, et al. An evaluation of a proactive geriatric trauma consultation service. Ann Surg 2012;256:1098–1101. [DOI] [PubMed] [Google Scholar]
- 33.Pape H-C, Friess T, Liener U, et al. Development of geriatric trauma centers—an effort by the German Society for Trauma and Orthopaedics. Injury 2014;45:1513–1515. [DOI] [PubMed] [Google Scholar]
- 34.Joynt KE, Orav EJ, Jha AK. Thirty-day readmission rates for Medicare beneficiaries by race and site of care. JAMA 2011; 305:675–681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Joynt KE, Jha AK. Characteristics of hospitals receiving penalties under the Hospital Readmissions Reduction Program. JAMA 2013;309:342–343. [DOI] [PubMed] [Google Scholar]
- 36.van Walraven C, Bennett C, Jennings A, et al. Proportion of hospital readmissions deemed avoidable: a systematic review. Can Med Assoc J 2011;183:E391–E402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hechenbleikner EM, Makary MA, Samarov DV, et al. Hospital readmission by method of data collection. J Am Coll Surg 2013;216:1150–1158. [DOI] [PubMed] [Google Scholar]


