Abstract
Background
Extracorporeal shock wave therapy (ESWT) has been widely used for pain control in musculoskeletal disorders. Whether ESWT can relieve chronic low back pain (CLBP) and improve lumbar function is still unclear. Therefore, we conducted a meta-analysis of relevant studies to comprehensively analyse and determine the efficacy and safety of ESWT for chronic low back pain.
Methods
Four databases were systematically searched for randomized controlled trials (RCTs) on ESWT for CLBP. The quality of the included studies was evaluated according to Cochrane systematic review criteria, relevant data were extracted, and meta-analysis was performed using RevMan 5.4 software. The primary outcomes were pain intensity, disability status, and mental health. The data were expressed as standardized mean differences (SMD) or weighted mean difference (WMD) and 95% confidence intervals (CI). Heterogeneity was assessed using the I2 statistic. If I2 ≥ 50%, a random effects model was applied; otherwise, a fixed effects model was used.
Results
Twelve RCTs involving 632 patients were included in this meta-analysis. The ESWT group reported significantly more pain relief than the control group at 4 weeks (WMD = − 1.04; 95% CI = − 1.44 to − 0.65; P < 0.001) and 12 weeks (WMD = − 0.85; 95% CI = − 1.30 to − 0.41; P < 0.001). Regarding the dysfunction index, ESWT led to significant improvement in lumbar dysfunction compared with the control group at 4 weeks (WMD = − 4.22; 95% CI = − 7.55 to − 0.89; P < 0.001) and 12 weeks (WMD = − 4.51; 95% CI = − 8.58 to − 0.44; P = 0.03). For mental health, there was no significant difference between the ESWT group and the control group after 4 weeks of intervention (SMD = 1.17; 95% CI = − 0.10 to 2.45; P = 0.07).
Conclusion
This systematic review and meta-analysis found that ESWT provided better pain relief and improved lumbar dysfunction compared with the other interventions included, and no serious adverse effects were found. There was no significant effect of ESWT on the mental health of patients, but we hope to obtain more RCTs for further analysis in the future. Based on the pooled results, we suggest that ESWT is effective and safe for treating chronic low back pain.
Supplementary Information
The online version contains supplementary material available at 10.1186/s13018-023-03943-x.
Keywords: Chronic low back pain, Dysfunction, ESWT, Mental health, Meta-analysis
Introduction
CLBP refers to pain that lasts for at least 12 weeks and occurs in the area below the margin of the low ribs, above the transverse hip line and between the bilateral midaxillary line; this pain is usually accompanied by pain symptoms in one or both lower limbs [1]. The global prevalence rate of CLBP is 13.1~20.3%, and it has been increasing in the past decade, with the number of affected patients rising from 370 million in 1990 to 570 million in 2017 [2]. CLBP has become a global public health problem due to its high incidence, long course and easy recurrence, which seriously affects the quality of life of patients and even causes adverse psychological effects [3]. Pain and limitation of movement are its most basic symptoms. Pain alters the contraction pattern of the trunk muscles, resulting in spasm, increased tone and even atrophy of the low back muscles, thereby significantly reducing the ability of the muscles to engage and destabilize the spine and vertebral balance [4, 5]. In addition, prolonged poor posture in the low back can lead to fatigue of the low back muscles and oedema of the surrounding soft tissues, exudation of inflammatory cells, accumulation of metabolic products and degeneration of muscle fibres, resulting in local adhesions, chronic hypoxia of the muscles and pain; all of these symptoms can contribute to recurrent episodes of CLBP [6, 7].
At present, CLBP is mainly treated conservatively (e.g. physical exercise, physiotherapy, drugs and other nonsurgical therapy) with the purposes of relieving pain and restoring physical function [8–10]. However, as a self-exercise therapy, physical exercise has shortcomings such as lack of standard posture and poor adherence; physiotherapy has difficulty achieving a long-term analgesic effect, while drug treatment may be accompanied by nausea, constipation, fatigue and other side effects [11, 12]. Most guidelines advocate the use of non-steroidal anti-inflammatory drugs (NSAIDs) in CLBP, but their long-term efficacy is unknown and the effectiveness of NSAIDs may be overestimated [13, 14]. Recently, mesenchymal stem cells appear to have shown good results in relieving degenerative discogenic pain, but its scope of application is still limited and safety needs further confirmation [15]. In addition, despite the availability of various interventions, more than two-thirds of patients with low back pain relapse within 12 months of recovery [16]. Therefore, it is particularly important to seek other safe and effective treatment strategies.
As an emerging therapeutic method, ESWT is a series of single sound pulses characterized by a high pressure peak and short-term rapid pressure rises and has achieved significant results in the treatment of musculoskeletal system diseases such as osteonecrosis of the femoral head and myofascitis [17, 18]. However, the use of ESWT in the treatment of CLBP is still controversial, and some clinical guidelines do not recommend it as a routine choice [19]. In recent years, some RCTs have focused on the use of ESWT in the treatment of CLBP. Therefore, an updated meta-analysis is needed to synthesize the literature. The main purpose of this meta-analysis was to evaluate the efficacy and safety of ESWT in reducing pain, improving lumbar function, and promoting mental health in patients with CLBP compared with other treatment methods, such as physical exercise, physiotherapy, and drugs.
Methods
Design
This systematic review and meta-analysis was based on the Cochrane Handbook of Systematic Reviews on Interventions [20] and strictly followed the recommended reporting items for the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement guidelines [21]. The review protocol was registered in the PROSPERO database (registration number: CRD42023421589).
Search strategy
The PubMed, Embase, Web of Science, and Cochrane Library databases were systematically searched from the initial release of the relevant database until April 25, 2023, to identify studies related to the use of ESWT for CLBP. The following search terms were used in the initial literature search: (Extracorporeal Shock Wave Therapy or ESWT) and (Chronic Low Back Pain or low back pain). Two researchers (KL and LLC) independently reviewed the selected studies, and any disagreements were resolved through discussion with a third senior investigator (DJ). In addition, the reference lists of these articles were manually checked to identify other publications that might be relevant.
Inclusion criteria
The inclusion criteria were as follows: (1) Adult patients (aged ≥ 18 years): clinically diagnosed with CLBP of mechanical origin; (2) Experimental group: ESWT or ESWT combined with other intervention methods; (3) Control group: physical exercise, physiotherapy, medicine or other similar interventions; (4) Results: Visual analogue scale (VAS), Oswestry Disability Index (ODI), mental health and other functional parameters; (5) Study design: Randomized controlled trial (RCT).
Exclusion criteria
The exclusion criteria were as follows: (1) nonhuman research or animal experiments; (2) studies that included participants with post-spinal surgery, pregnancy, or other spinal conditions (fractures, tumours, spondylolisthesis, ankylosing spondylitis, severe osteoporosis, cauda equina syndrome); (3) articles such as abstracts, letters, editorials, expert opinions, comments, and case reports; (4) non-English studies; and (5) studies without suitable data for analysis.
Data extraction
The demographic characteristics extracted included first author, year of publication, study design, sample size of each study, mean age of patients, sex ratio, and follow-up. The main outcome measures of the treatment effect in this study included the VAS pain score, ODI dysfunction index and patients' mental health score. The main mental health scales include the 36-Item Short Form Health Survey (SF-36), Patient Health Questionnaire 9 (PHQ-9) and Beck Depression Index (BDI). If scores were recorded at different follow-up times, we chose the time points closest to 4 weeks and 12 weeks to predict efficacy. In addition, adverse events were recorded.
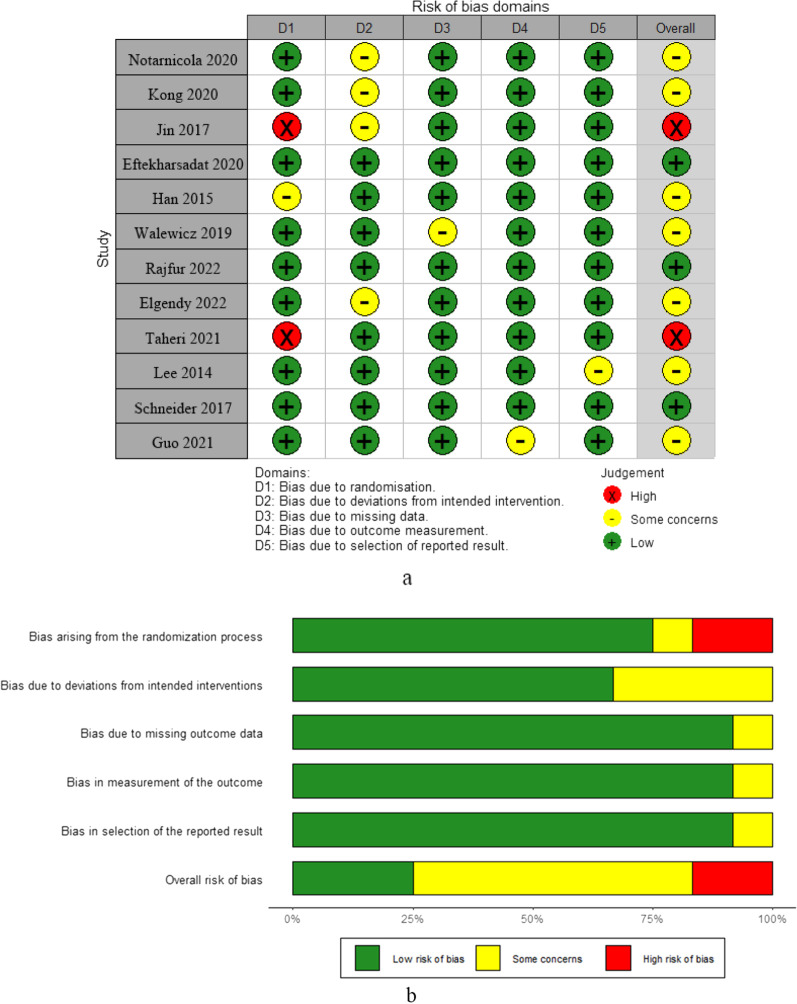
Bias assessment and quality classification
The quality of the included studies was assessed by the version 2 of the Risk of Bias tool of the Cochrane Library (RoB 2) [22]. Seven domains of bias, including selection bias, performance bias, detection bias, attribution bias, reporting bias, and other sources of bias, were evaluated. Judgements were presented as "high risk," "low risk," or "risk ambiguous," and the quality assessment numbers were generated by RevMan version 5.4. Two independent reviewers (QYZ and XQX) assessed the risk of bias, and a third senior investigator (DJ) resolved cases of disagreement between the former. The GRADE (Grading of Recommendations, Assessment, Development, and Evaluation) method was used to evaluate the overall quality of the evidence based on risk of bias, indirectness, inconsistency, publication bias, imprecision, and other factors. The GRADE method, depending on estimated effects, classifies the quality of evidence as high, moderate, low, or very low [23].
Statistical analyses
Meta-analysis was performed using RevMan5.4 software provided by the Cochrane Collaboration network, and forest maps were used to display the results. Since the measured data were continuous variables, the SMD or WMD and 95% CI were selected as the main effect parameters according to the differences in the measurement methods of the indicators. Heterogeneity was tested by the P value of Chi2 and I2. When statistical heterogeneity was significant (P < 0.10 or I2 > 50%), the random effects model was chosen. When statistical heterogeneity was not significant (P ≥ 0.10 or I2 ≤ 50%), the fixed effects model was adopted. Furthermore, the source of heterogeneity can be explored by sensitivity analysis and subgroup analysis. Subgroup analyses were performed according to follow-up time and intervention method. According to Egger et al. [24] and with more than ten included studies, we assessed the publication bias between the included studies by visual inspection of the funnel plot.
Results
Selection of studies
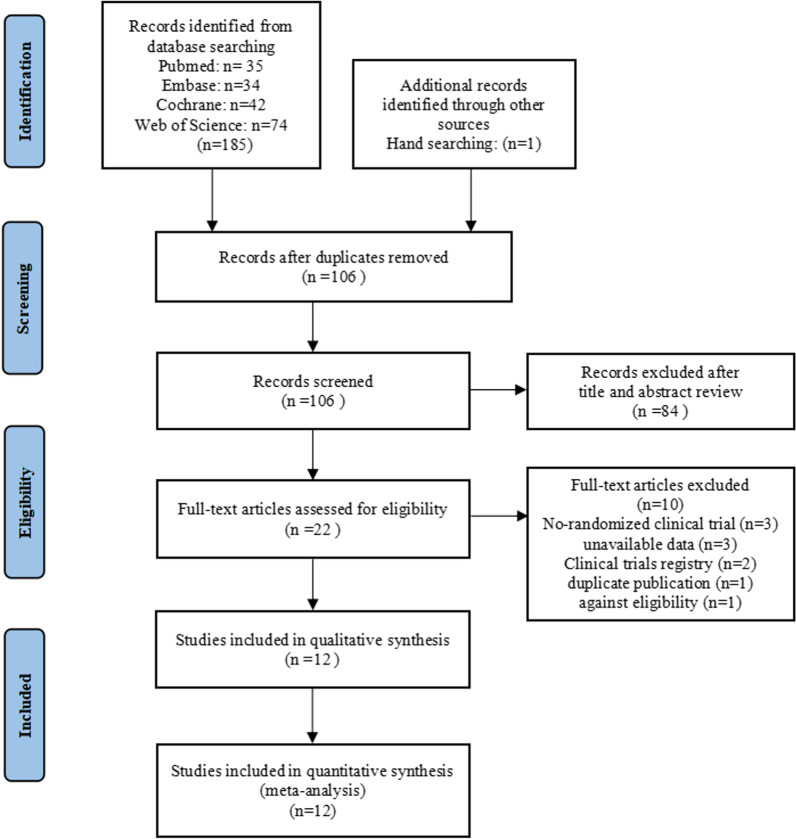
In the initial literature search, 186 papers were retrieved. We detected and removed 80 duplicate articles using Endnote X9 software. Additionally, 84 studies were excluded after reviewing the titles and abstracts. Then, after a full text review, we excluded ten articles that did not meet the inclusion criteria. Finally, 12 RCTs involving a total of 632 patients (318 in the ESWT group and 314 in the control group) were included in this study. The selection process is presented in the PRISMA flowchart (Fig. 1).
Fig. 1.
The selection process of this meta-analysis
Study characteristics and risk of bias
These studies are characterized in Table 1. All articles were published in English between 2014 and 2022. Sample sizes range from 28 to 200. All the experimental groups received ESWT treatment, while the control group received different conservative treatments, including exercise therapy [25–28], physiotherapy [29–31], drug injection [32, 33], oral medication [34, 35], and manual therapy [36]. The items for risk of bias included in each study are shown in Fig. 2. The quality level assessment of the relevant studies is shown in Additional file 1: Table S2.
Table 1.
Characteristics of the included RCTs
| References | Study design | Sample size | Gender (male) | Age (mean ± SD) | Intervention | Follow-up | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| ESWT | Control | ESWT | Control | ESWT | Control | |||||
| Notarnicola et al. [26] | RCT | 15 | 15 | – | – | 62.6 ± 11.8 | (range: 43.0–82.0) |
ESWT: Shockwaves of 2000 pulses in total were applied at 0.03 mj/mm2 and a frequency of 4 Hz/s, once per week for three sessions Control: Bridging exercise, adductor ball squeeze exercise, abdominal marching exercise and reverse curl-ups exercise (50 min), twice a week for 4 weeks |
12 weeks | |
| Kong et al. [31] | RCT | 100 | 100 | 60 | 60 | 44.45 ± 8.27 | 44.53 ± 8.19 |
ESWT: The impulse voltage is set as 7.0–9.0 kv, the impulse energy is 0.1–0.2 mj/mm2, and the times of shocks are set as 1200. ESWT was conducted usually for 1–2 courses, 5 times as 1 course Control: Laser therapeutic, once a week, with a total of 4 times |
1 year | |
| Jin et al. (2017) | RCT | 15 | 15 | 8 | 9 | 55.46 ± 15.09 | 53.13 ± 19.62 |
ESWT: With 2000 shock waves applied at each session at an intensity of 0.085–0.148 mj/mm2. We repeated this procedure a total of three times, at 3-day intervals Control: Trigger point injection |
4 weeks | |
| Eftekharsadat et al. [33] | RCT | 27 | 27 | 20 | 17 | 44.74 ± 9.34 | 45.04 ± 11.86 |
ESWT: Shockwaves of 1500 pulses with an energy flux density of 0.1 mj/mm2/min, energy level of 2–4, a frequency of 10–16 Hz, and pulse rate of 160/min in total, once a week for 5 weeks. Physical exercise: stretching exercises Control: Trigger point injection, muscle injection of 40 mg triamcinolone + 2 mL lidocaine 2%, one session. Physical exercise: stretching exercises |
4 weeks | |
| Han et al. [30] | RCT | 15 | 15 | 9 | 49.7 ± 8.3 | 46.0 ± 8.9 |
ESWT: Each patient assumed a prone position, and 1000 shock waves (7 times per sec) were applied at 2.5 Hz at low energy flux densities of 0.01–0.16 mj/mm2 using a 17 mm head. The treatment was conducted at the quadratus lumborum muscle and the sacroiliac joint, where the patients complained of pain Control: Bridging exercise, adductor ball squeeze exercise, abdominal marching exercise and reverse curl-ups exercise (50 min), twice a week for 4 weeks |
6 weeks | ||
| Walewicz et al. [25] | RCT | 20 | 20 | 6 | 5 | 51.1 ± 8.4 | 55.8 ± 9.3 |
ESWT: Shockwaves of 2000 pulses with the pressure of 2.5 bars (corresponding to an energy flux density of 0.1 mj/mm2), 5 Hz frequency, and treatment time of seven minutes; Physical exercise Control: Sham shockwaves therapy; Physical exercise |
12 weeks | |
| Rajfur et al. [27] | RCT | 19 | 18 | 10 | 10 | 43.0 ± 13.1 | 45.4 ± 14.0 |
ESWT: Shockwaves of 1000 pulses with an energy flux density of 0.15 mj/mm2/min, frequency 4 Hz, twice a week for 5 weeks. Physical exercise Control: Sham shockwaves therapy. Physical exercise |
12 weeks | |
| Elgendy et al. [28] | RCT | 15 | 15 | 10 | 10 | 32.73 ± 6.73 | 33.26 ± 5.48 |
ESWT: 2000 shocks, 0.10 mj/mm2 energy, 5 Hz frequency, using a 17 mm head were administered, twice a week for 6 weeks. Stretching exercises were performed for the hamstrings, iliopsoas, and back extensors Control: Stretching exercises were performed for the hamstrings, iliopsoas, and back extensors |
6 weeks | |
| Taheri et al. [34] | RCT | 17 | 15 | 6 | 9 | 42.5 ± 10.1 | 37.1 ± 11.8 |
ESWT: Shockwaves of 1500 pulses in total were applied at 0.15 mj/mm2 and a frequency of 4 Hz/s, once a week for 4 weeks. Oral medications; stretching exercises Control: Sham shockwaves therapy; Oral medications; stretching exercises |
12 weeks | |
| Lee et al. [29] | RCT | 13 | 15 | 9 | 53.92 ± 10.38 | 54.33 ± 13.16 |
ESWT: Shockwaves of 2000 pulses in total were applied at 0.10 mj/mm2 and a frequency of 5 Hz/s, twice a week for 6 weeks; Williams’ exercises and McKenzie’s exercise Control: Hot packs, and ultrasound and electrotherapy; Williams’ exercises and McKenzie’s exercise |
6 weeks | ||
| Schneider [36] | RCT | 15 | 15 | – | – | 43.2 (range: 23–65) |
ESWT: Impulse parameters: 15–42 Hz; Myofascial trigger therapy, twice a week for 3 weeks Control: Myofascial trigger therapy, twice a week for 3 weeks |
12 weeks | ||
| Guo et al. [35] | RCT | 47 | 44 | 22 | 25 | 34.9 ± 8.7 | 36.0 ± 11.2 |
ESWT: 4000 pulses, 15 Hz, once a week for 4 weeks Control: Medication: celecoxib and eperisone |
12 weeks | |
ESWT extracorporeal shock wave therapy, SD standard deviation
Fig. 2.
a Judgement plots for risk of bias items for each RCT. b Weighted summary plot of overall bias type in RCTs
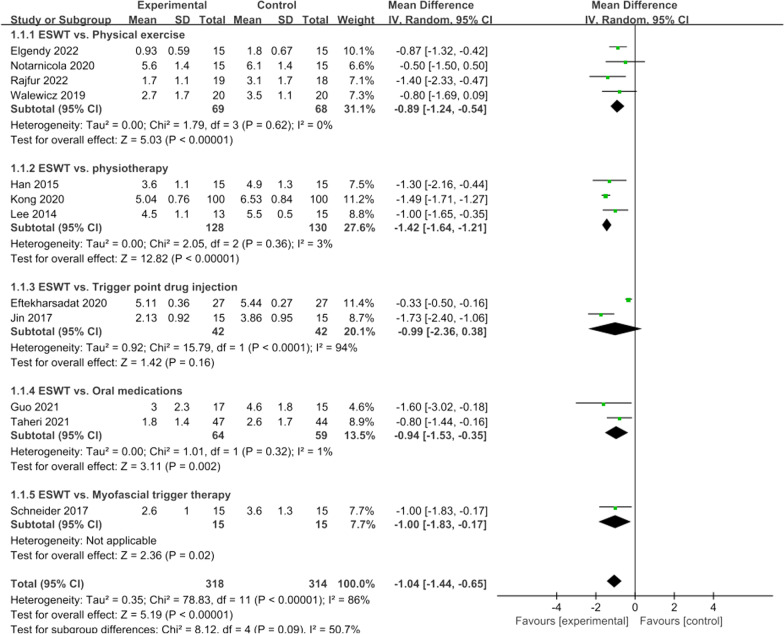
Pain score at 4 weeks
Twelve articles included in our study compared pain scores at 4 weeks between the ESWT group and the control group. There was significant heterogeneity (I2 = 86%, P < 0.001), so we conducted subgroup analysis according to the intervention methods of the control group using the random effects model. The results showed that the trigger drug injection group had high heterogeneity (I2 = 94%, P < 0.001), but there was no significant difference between this group and ESWT, so the overall results were still consistent. The present meta-analysis demonstrated that ESWT was associated with a significant reduction in pain score at 4 weeks (WMD = − 1.04; 95% CI = − 1.44 to − 0.65; P < 0.00001, Fig. 3).
Fig. 3.
Forest plot of pain score at 4 weeks
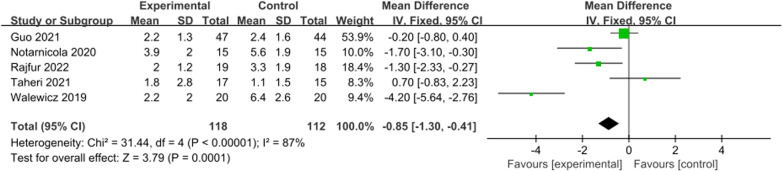
Pain score at 12 weeks
A total of five studies reported pain scores at 12 weeks. There was significant heterogeneity, and a random effects model was used (I2 = 87%, P < 0.001). This meta-analysis showed that the pain score of the ESWT group was significantly lower than that of the control group at 12 weeks (WMD = − 0.85; 95% CI = − 1.30 to − 0.41; P = 0.0001, Fig. 4).
Fig. 4.
Forest plot of pain score at 12 weeks
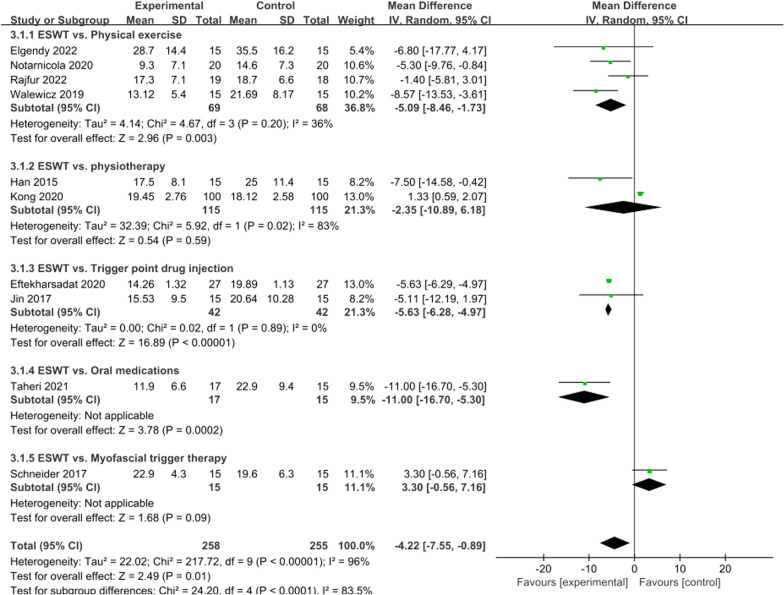
ODI score at 4 weeks
A total of ten articles compared ODI scores at 4 weeks between the ESWT and control groups. The difference was significant (I2 = 96%, P = 0.01). Subgroup analysis was conducted according to the intervention methods of the control group, and a random effects model was selected. The physiotherapy group was the main source of heterogeneity (I2 = 83%, P = 0.02), but there was no significant difference between the control group and the ESWT group, so the overall results were consistent and reliable. In the present meta-analysis, ESWT was associated with a significant increase in ODI scores at 4 weeks (WMD = − 4.22; 95% CI = − 7.55 to − 0.89; P = 0.01, Fig. 5).
Fig. 5.
Forest plot of ODI score at 4 weeks
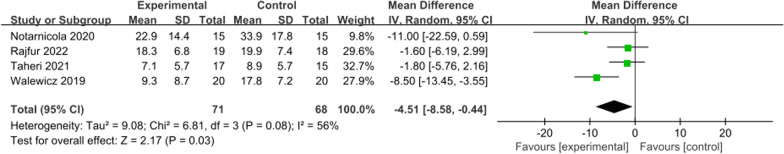
ODI score at 12 weeks
ODI scores at 12 weeks were obtained from four studies with significant heterogeneity (I2 = 56%, P = 0.08), and a random effects model was used. The combined results showed a significant difference between the groups (WMD = − 4.51; 95% CI = − 8.58 to − 0.44; P = 0.03, Fig. 6).
Fig. 6.
Forest plot of ODI score at 12 weeks
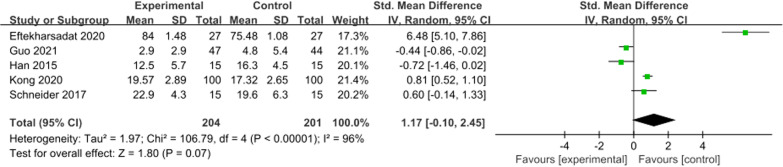
Mental health score at 4 weeks
A total of five studies reported mental health scores at 4 weeks, with significant heterogeneity (I2 = 96%, P < 0.001). The questionnaires used for mental health scores were inconsistent, so SMD was selected for meta-analysis. The results showed no specific significant difference in mental health score between the control group and ESWT group at 4 weeks (SMD = 1.17; 95% CI = − 0.10 to 2.45; P = 0.07, Fig. 7).
Fig. 7.
Forest plot of mental health score at 4 weeks
Adverse events
No serious adverse reactions were reported in any of the 12 studies; seven studies specifically reported that adverse reactions did not occur, and five studies did not record adverse reactions at all.
Qualitative analysis
The studies included in this meta-analysis involved both radial extracorporeal shockwave (r-ESWT) and focused extracorporeal shockwave (f-ESWT), so it is of interest to analyse which type of ESWT is more effective for CLBP. Based on the data available in this study, although it is not possible to directly quantify which device and type had a superiority in the treatment, we have obtained some valuable information from other relevant studies. A study of non-calcific rotator cuff tendinopathies showed that f-ESWT was significantly more effective than r-ESWT at long-term follow-up of more than 24 weeks [37]. Another study on knee osteoarthritis also showed the same results [38]. However, DeLuca et al. [39] reported that no significant difference was found between f-ESWT and r-ESWT in terms of efficacy in plantar fasciitis and that most patients could achieve functional gains with either form of shockwave. Which type of ESWT is more advantageous for CLBP still needs further verification.
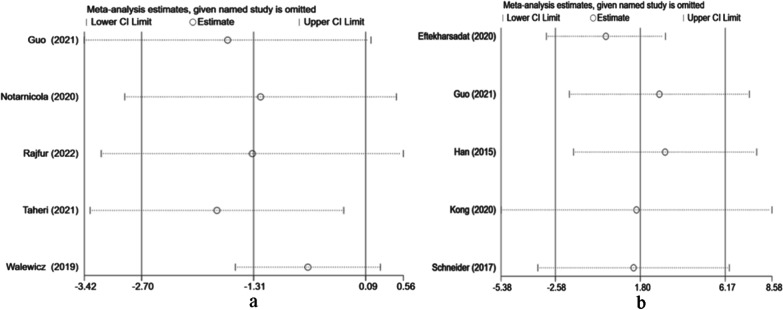
Sensitivity analysis
When comparing the effects of ESWT on pain at 12 weeks and mental health at 4 weeks, we performed a sensitivity analysis due to considerable heterogeneity. A single study was excluded each time to assess the impact of individual data on the overall outcome. The results showed that the merger effect was robust, and no significant deviation from the overall results was found in our study (Fig. 8).
Fig. 8.
a Results of sensitivity analysis for VAS after omitting each study one at a time. CI: confidence interval. b Results of sensitivity analysis for the mental health score after omitting each study one at a time. CI: confidence interval
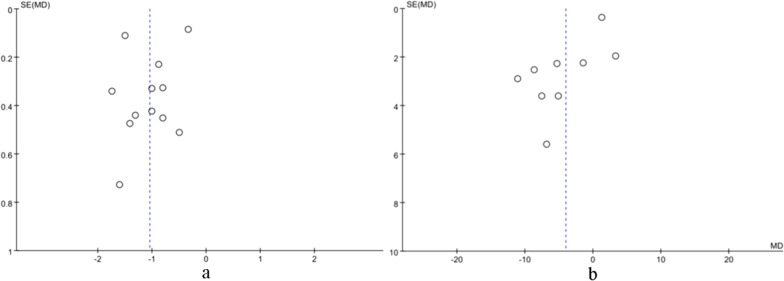
Publication bias
Stata 15.0 software was used to conduct funnel plot analysis of the included literature on ESWT for 4-week pain and ODI outcome indices. The funnel plot showed a basically symmetrical scatter point, indicating that there was no significant publication bias in the included literature, and the results of the meta-analysis were credible (Fig. 9).
Fig. 9.
Funnel plot for the comparison of ESWT vs. Control at week 4. (a) Left figure: pain outcome as measured on a VAS. (b) Right figure: ODI outcome
Discussion
The effectiveness of ESWT on the pain, function and mental health of patients with CLBP was systematically reviewed. The results of this meta-analysis showed that ESWT, either as stand-alone or adjuvant treatment for CLBP, significantly reduced VAS scores at week 4 and week 12 compared to the control group, with a “moderate” recommended level based on GRADE [23]. Furthermore, “low” quality evidence showed significant improvement in ODI scores at week 4 and week 12 for ESWT compared to other conservative treatments. However, with regard to mental health scores at week 4, we did not find significant differences between the two groups. In addition, no ESWT-related adverse events were found (not recorded or did not occur) in any of the 12 RCTs included in the study.
According to our information, there was only one previous meta-analysis about the application of ESWT in CLBP, but we found that this study had high heterogeneity in both pain and dysfunction index analyses, and no subgroup analysis or sensitivity analysis was conducted [40]. This previous study found a nonsignificant effect of ESWT on pain relief in CLBP at 3 months, but our meta-analysis still found better long-term efficacy at 12 weeks after the inclusion of more studies. In addition, we found that this previous meta-analysis included an unpublished master's thesis and a study of participants with postpartum low back pain. These studies may have affected the reliability of the results, excluding them from our study. Finally, we included 12 RCTs with a total of 632 patients and explored the sources of the associated heterogeneity. Moreover, studies have shown that the occurrence of CLBP is rarely caused by a single factor but by a variety of physical and psychological mechanisms [41]. Holmes et al. [42] believed that limitations or disabilities in patients' daily lives would lead to psychosocial problems, which would further damage their quality of life. Therefore, we conducted the first meta-analysis of mental health scores in CLBP patients.
CLBP is treated with a variety of clinical approaches, including conservative treatment and surgical treatment. In its initial clinical use, ESWT was used by German medical scientists to save patients from surgical pain treatment [43]. With the passage of time, ESWT technology has gradually matured, and its clinical application is also increasing. Many clinical trials have shown that ESWT treatment can significantly reduce pain and complications in patients with CLBP [25, 32]. ESWT mainly treats chronic low back pain through the direct mechanical action of shock waves and indirectly causes mechanical action through cavitation [44]. First, when shock waves enter the human body, different mechanical effects will be generated at the interface of different tissues due to different contact media, such as fat, tendon, ligament and bone tissue, and finally, different forces will be generated on cells [45]. In these forces, tensile stress can relax tissues. It promotes microcirculation, while compressive stress can change the elasticity of cells and increase their ability to absorb oxygen for therapeutic purposes [46, 47]. Second, ESWT causes a large number of tiny bubbles to be created in the tissue, which rapidly expand and burst under the action of the shock wave, producing a high-speed fluid microjet and a shock effect [48]. This cavitation effect is particularly effective in reopening occluded microvasculature and releasing soft tissue adhesions at the joint [49, 50]. The exact mechanism of the pain-relieving and functional properties of ESWT is not fully understood, and several studies have attempted to elucidate the mechanisms of shock waves from basic science and clinical studies. Studies have shown that the energy released by ESWT is able to stimulate pain receptors located in skin, muscle, connective tissue, bone and joints and activate unmyelinated C and A delta fibres to initiate the "gated" pain control system and block nerve transmission, resulting in analgesic effects [51, 52]. In addition, ESWT has been shown to significantly downregulate the levels of IL-1, TNF-α and MMPs in degenerated joint tissues, thereby reducing the local inflammatory response [53, 54]. Additionally, ESWT also promotes the secretion of pain-reducing chemicals (e.g. endorphins), inhibits the release of pain factors such as substance P and calcitonin gene-related peptides, reduces peripheral nerve sensitivity and increases pain threshold levels [55, 56].
It is well known that adverse reactions are a major concern when evaluating the efficacy of ESWT. Therefore, the higher the risk of adverse reactions, the lower the clinical value of ESWT. In our study, no serious adverse reactions were reported in any of the 12 studies. Therefore, based on the current meta-analysis, ESWT did not increase the risk of local reactions. However, considering the small sample size included in the study, the safety of ESWT needs to be further discussed.
Limitations
Some limitations of this study should be noted. First, there are differences in aetiology, pain duration, and related parameters used by ESWT in each study, which may lead to heterogeneity in the combination of results and limited evidence. Second, there are inevitably heterogeneous factors among the included patients, such as age, gender, and racial differences. Next, different biases, including selection bias, language bias, data provision bias and publication bias, may reduce the accuracy of the results. Last but not least, the pain, function and mental health scores included in this meta-analysis were all obtained through questionnaires, and the outcome indicators may be subjective. If there are enough articles with objective observation indicators in the future, relevant studies can be improved. Therefore, more RCTs need to be included in the future to further investigate the efficacy and safety of ESWT.
Conclusion
ESWT is effective in reducing pain and dysfunction in CLBP patients without increasing the risk of adverse reactions, but it should be performed with caution. However, no significant effect was found on the improvement in mental health. More RCTs are needed to verify the findings in the current study.
Supplementary Information
Additional file 1: Quality of evidence assessment by GRADE of the included studies.
Acknowledgements
Not applicable.
Abbreviations
- ESWT
Extracorporeal shock wave therapy
- RCT
Randomized controlled trials
- CLBP
Chronic low back pain
- VAS
Visual analogue scale
- ODI
Oswestry Disability Index
- WMD
Weighted mean difference
- SMD
Standardized mean difference
- SD
Standard deviation
Author contributions
JD, KL, and QYZ conceived and designed the study. KL, LLC, and HRZ searched and selected relevant studies. QYZ, XQX extracted and interpreted data. KL, JD, and ZNY analysed the data. KL and QYZ wrote the paper. JD and XQX revised the manuscript. All authors read and approved the final manuscript.
Funding
This work was partially supported by the Young Scholars Program of Shandong Provincial Hospital, the Young Taishan Scholars Program of Shandong Province (Grant number tsqn201909183), the Academic Promotion Program of Shandong First Medical University (Grant number 2020RC008), and the Natural Science Foundation of Shandong Province (Grant numbers ZR2020QH072 and ZR2020MH098).
Availability of data and materials
The datasets used and analysed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Kun Liu and Qingyu Zhang contributed equally to this article.
References
- 1.Clark S, Horton R. Low back pain: a major global challenge. Lancet. 2018;391(10137):2302. doi: 10.1016/S0140-6736(18)30725-6. [DOI] [PubMed] [Google Scholar]
- 2.Wu A, March L, Zheng X, Huang J, Wang X, Zhao J, Blyth FM, Smith E, Buchbinder R, Hoy D. Global low back pain prevalence and years lived with disability from 1990 to 2017: estimates from the Global Burden of Disease Study 2017. Ann Transl Med. 2020;8(6):299. doi: 10.21037/atm.2020.02.175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Katz JN. Lumbar disc disorders and low-back pain: socioeconomic factors and consequences. J Bone Joint Surg Am. 2006;88(Suppl 2):21–24. doi: 10.2106/JBJS.E.01273. [DOI] [PubMed] [Google Scholar]
- 4.Goubert D, De Pauw R, Meeus M, Willems T, Cagnie B, Schouppe S, Van Oosterwijck J, Dhondt E, Danneels L. Lumbar muscle structure and function in chronic versus recurrent low back pain: a cross-sectional study. Spine J. 2017;17(9):1285–1296. doi: 10.1016/j.spinee.2017.04.025. [DOI] [PubMed] [Google Scholar]
- 5.Russo M, Deckers K, Eldabe S, Kiesel K, Gilligan C, Vieceli J, Crosby P. Muscle control and non-specific chronic low back pain. Neuromodulation. 2018;21(1):1–9. doi: 10.1111/ner.12738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Goubert D, Oosterwijck JV, Meeus M, Danneels L. Structural changes of lumbar muscles in non-specific low back pain: a systematic review. Pain Phys. 2016;19(7):E985–E1000. [PubMed] [Google Scholar]
- 7.Purushotham S, Stephenson RS, Sanderson A, Abichandani D, Greig C, Gardner A, Falla D. Microscopic changes in the spinal extensor musculature in people with chronic spinal pain: a systematic review. Spine J. 2022;22(7):1205–1221. doi: 10.1016/j.spinee.2022.01.023. [DOI] [PubMed] [Google Scholar]
- 8.Qaseem A, Wilt TJ, Mclean RM, Forciea MA, Denberg TD, Barry MJ, Boyd C, Chow RD, Fitterman N, Harris RP, et al. Noninvasive treatments for acute, subacute, and chronic low back pain: a clinical practice guideline from the American College of Physicians. Ann Intern Med. 2017;166(7):514–530. doi: 10.7326/M16-2367. [DOI] [PubMed] [Google Scholar]
- 9.George SZ, Fritz JM, Silfies SP, Schneider MJ, Beneciuk JM, Lentz TA, Gilliam JR, Hendren S, Norman KS. Interventions for the management of acute and chronic low back pain: revision 2021. J Orthop Sport Phys. 2021;51(11):G1–G60. doi: 10.2519/jospt.2021.0304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Baroncini A, Maffulli N, Eschweiler J, Molsberger F, Klimuch A, Migliorini F. Acupuncture in chronic aspecific low back pain: a Bayesian network meta-analysis. J Orthop Surg Res. 2022;17(1):319. doi: 10.1186/s13018-022-03212-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Deyo RA, Von Korff M, Duhrkoop D. Opioids for low back pain. BMJ Br Med J. 2015;350:g6380. doi: 10.1136/bmj.g6380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Migliorini F, Maffulli N, Eschweiler J, Betsch M, Catalano G, Driessen A, Tingart M, Baroncini A. The pharmacological management of chronic lower back pain. Expert Opin Pharmacother. 2021;22(1):109–119. doi: 10.1080/14656566.2020.1817384. [DOI] [PubMed] [Google Scholar]
- 13.Migliorini F, Maffulli N. Choosing the appropriate pharmacotherapy for nonspecific chronic low back pain. J Orthop Surg Res. 2022;17(1):556. doi: 10.1186/s13018-022-03426-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Migliorini F, Maffulli N, Eschweiler J, Tingart M, Baroncini A. Non-steroidal anti-inflammatory drugs and gabapentinoids for chronic lumbar pain: a Bayesian network meta-analysis of randomized controlled trials. Br Med Bull. 2021;138(1):85–95. doi: 10.1093/bmb/ldab003. [DOI] [PubMed] [Google Scholar]
- 15.Miranda L, Quaranta M, Oliva F, Maffulli N. Stem cells and discogenic back pain. Br Med Bull. 2023;146(1):73–87. doi: 10.1093/bmb/ldad008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Da ST, Mills K, Brown BT, Pocovi N, de Campos T, Maher C, Hancock MJ. Recurrence of low back pain is common: a prospective inception cohort study. J Physiother. 2019;65(3):159–165. doi: 10.1016/j.jphys.2019.04.010. [DOI] [PubMed] [Google Scholar]
- 17.Wang CJ. Extracorporeal shockwave therapy in musculoskeletal disorders. J Orthop Surg Res. 2012;7:11. doi: 10.1186/1749-799X-7-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ioppolo F, Rompe JD, Furia JP, Cacchio A. Clinical application of shock wave therapy (SWT) in musculoskeletal disorders. Eur J Phys Rehab Med. 2014;50(2):217–230. [PubMed] [Google Scholar]
- 19.Kreiner DS, Matz P, Bono CM, Cho CH, Easa JE, Ghiselli G, Ghogawala Z, Reitman CA, Resnick DK, Watters WR, et al. Guideline summary review: an evidence-based clinical guideline for the diagnosis and treatment of low back pain. Spine J. 2020;20(7):998–1024. doi: 10.1016/j.spinee.2020.04.006. [DOI] [PubMed] [Google Scholar]
- 20.Shamseer L, Moher D, Clarke M, Ghersi D, Liberati A, Petticrew M, Shekelle P, Stewart LA. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ Br Med J. 2015;350:g7647. doi: 10.1136/bmj.g7647. [DOI] [PubMed] [Google Scholar]
- 21.Furlan AD, Malmivaara A, Chou R, Maher CG, Deyo RA, Schoene M, Bronfort G, van Tulder MW. 2015 updated method guideline for systematic reviews in the Cochrane Back and Neck Group. Spine. 2015;40(21):1660–1673. doi: 10.1097/BRS.0000000000001061. [DOI] [PubMed] [Google Scholar]
- 22.Sterne JAC, Savovic J, Page MJ, Elbers RG, Blencowe NS, Boutron I, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:l4898. doi: 10.1136/bmj.l4898. [DOI] [PubMed] [Google Scholar]
- 23.Guyatt G, Oxman AD, Akl EA, Kunz R, Vist G, Brozek J, Norris S, Falck-Ytter Y, Glasziou P, DeBeer H, Jaeschke R, Rind D, Meerpohl J, Dahm P, Schünemann HJ. GRADE guidelines: 1. Introduction-GRADE evidence profiles and summary of findings tables. J Clin Epidemiol. 2011;64(4):383–394. doi: 10.1016/j.jclinepi.2010.04.026. [DOI] [PubMed] [Google Scholar]
- 24.Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Walewicz K, Taradaj J, Rajfur K, Ptaszkowski K, Kuszewski MT, Sopel M, Dymarek R. The effectiveness of radial extracorporeal shock wave therapy in patients with chronic low back pain: a prospective, randomized, single-blinded pilot study. Clin Interv Aging. 2019;14:1859–1869. doi: 10.2147/CIA.S224001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Notarnicola A, Maccagnano G, Moretti L, Salvemini M, Bianchi FP, Covelli I, Tafuri S, Moretti B. Conservative treatment of sacroiliac joint pain with extracorporeal shockwave therapy. J Biol Reg Homeos Ag. 2020;34(2):697–703. doi: 10.23812/19-378-L-68. [DOI] [PubMed] [Google Scholar]
- 27.Rajfur K, Rajfur J, Matusz T, Walewicz K, Dymarek R, Ptaszkowski K, Taradaj J. Efficacy of focused extracorporeal shock wave therapy in chronic low back pain: a prospective randomized 3-month follow-up study. Med Sci Monitor. 2022;28:e936614. doi: 10.12659/MSM.936614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Elgendy MH, Mohamed M, Hussein HM. A single-blind randomized controlled trial investigating changes in electrical muscle activity, pain, and function after shockwave therapy in chronic non-specific low back pain: pilot study. Ortop Traumatol Rehabil. 2022;24(2):87–94. doi: 10.5604/01.3001.0015.8266. [DOI] [PubMed] [Google Scholar]
- 29.Lee S, Lee D, Park J. Effects of extracorporeal shockwave therapy on patients with chronic low back pain and their dynamic balance ability. J Phys Ther Sci. 2014;26(1):7–10. doi: 10.1589/jpts.26.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Han H, Lee D, Lee S, Jeon C, Kim T. The effects of extracorporeal shock wave therapy on pain, disability, and depression of chronic low back pain patients. J Phys Ther Sci. 2015;27(2):397–399. doi: 10.1589/jpts.27.397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kong L, Tian X, Yao X. Effects of extracorporeal shock wave therapy on chronic low back pain and quality of life. Minerva Surg. 2022;29(4):883. doi: 10.23736/S2724-5691.22.09537-5. [DOI] [PubMed] [Google Scholar]
- 32.Kong L, Tian X, Yao X. Effects of extracorporeal shock wave therapy on chronic low back pain and quality of life. Minerva Surg. 2023;78(3):305–306. doi: 10.23736/S2724-5691.22.09537-5. [DOI] [PubMed] [Google Scholar]
- 33.Eftekharsadat B, Fasaie N, Golalizadeh D, Babaei-Ghazani A, Jahanjou F, Eslampoor Y, Dolatkhah N. Comparison of efficacy of corticosteroid injection versus extracorporeal shock wave therapy on inferior trigger points in the quadratus lumborum muscle: a randomized clinical trial. BMC Musculoskel Dis. 2020;21(1):695. doi: 10.1186/s12891-020-03714-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Taheri P, Khosrawi S, Ramezani M. Extracorporeal shock wave therapy combined with oral medication and exercise for chronic low back pain: a randomized controlled trial. Arch Phys Med Rehab. 2021;102(7):1294–1299. doi: 10.1016/j.apmr.2020.12.008. [DOI] [PubMed] [Google Scholar]
- 35.Guo X, Li L, Yan Z, Li Y, Peng Z, Yang Y, Zhang Y, Schmitz C, Feng Z. Efficacy and safety of treating chronic nonspecific low back pain with radial extracorporeal shock wave therapy (rESWT), rESWT combined with celecoxib and eperisone (C + E) or C + E alone: a prospective, randomized trial. J Orthop Surg Res. 2021;16(1):705. doi: 10.1186/s13018-021-02848-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Schneider R. Effectiveness of myofascial trigger point therapy in chronic back pain patients is considerably increased when combined with a new, integrated, low-frequency shock wave vibrotherapy (Cellconnect Impulse): a two-armed, measurement repeated, randomized, controlled pragmatic trial. J Back Musculoskelet. 2018;31(1):57–64. doi: 10.3233/BMR-169662. [DOI] [PubMed] [Google Scholar]
- 37.Li C, Li Z, Shi L, Wang P, Gao F, Sun W. Effectiveness of focused shockwave therapy versus radial shockwave therapy for noncalcific rotator cuff tendinopathies: a randomized clinical trial. Biomed Res Int. 2021;9(2021):6687094. doi: 10.1155/2021/6687094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ko NY, Chang CN, Cheng CH, Yu HK, Hu GC. Comparative effectiveness of focused extracorporeal versus radial extracorporeal shockwave therapy for knee osteoarthritis-randomized controlled study. Int J Environ Res Public Health. 2022;19(15):9001. doi: 10.3390/ijerph19159001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.DeLuca S, Robinson DM, Yun PH, Rosenberg C, Tan CO, Tenforde AS. Similar functional gains using radial versus combined shockwave therapy in management of plantar fasciitis. J Foot Ankle Surg. 2021;60(6):1098–1102. doi: 10.1053/j.jfas.2021.04.013. [DOI] [PubMed] [Google Scholar]
- 40.Yue L, Sun MS, Chen H, Mu GZ, Sun HL. Extracorporeal shockwave therapy for treating chronic low back pain: a systematic review and meta-analysis of randomized controlled trials. Biomed Res Int. 2021;2021:5937250. doi: 10.1155/2021/5937250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.La Touche R, Perez-Fernandez M, Barrera-Marchessi I, Lopez-De-Uralde-Villanueva I, Villafane JH, Prieto-Aldana M, Suso-Marti L, Paris-Alemany A. Psychological and physical factors related to disability in chronic low back pain. J Back Musculoskelet. 2019;32(4):603–611. doi: 10.3233/BMR-181269. [DOI] [PubMed] [Google Scholar]
- 42.Holmes S. Research. Pursuit of happiness Nurs Mirror. 1985;161(13):43–45. [PubMed] [Google Scholar]
- 43.Bierkens AF, Hendrikx AJ, De La Rosette JJ, Stultiens GN, Beerlage HP, Arends AJ, Debruyne FM. Treatment of mid- and lower ureteric calculi: extracorporeal shock-wave lithotripsy vs laser ureteroscopy. A comparison of costs, morbidity and effectiveness. Br J Urol. 1998;81(1):31–35. doi: 10.1046/j.1464-410x.1998.00510.x. [DOI] [PubMed] [Google Scholar]
- 44.Simplicio CL, Purita J, Murrell W, Santos GS, Dos SR, Lana J. Extracorporeal shock wave therapy mechanisms in musculoskeletal regenerative medicine. J Clin Orthop Trauma. 2020;11(Suppl 3):S309–S318. doi: 10.1016/j.jcot.2020.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Schroeder AN, Tenforde AS, Jelsing EJ. Extracorporeal shockwave therapy in the management of sports medicine injuries. Curr Sport Med Rep. 2021;20(6):298–305. doi: 10.1249/JSR.0000000000000851. [DOI] [PubMed] [Google Scholar]
- 46.Romeo P, Lavanga V, Pagani D, Sansone V. Extracorporeal shock wave therapy in musculoskeletal disorders: a review. Med Prin Pract. 2014;23(1):7–13. doi: 10.1159/000355472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Alvarez L. Extracorporeal shockwave therapy for musculoskeletal pathologies. Vet Clin N Am-Small. 2022;52(4):1033–1042. doi: 10.1016/j.cvsm.2022.03.007. [DOI] [PubMed] [Google Scholar]
- 48.Gerdesmeyer L, Wagenpfeil S, Haake M, Maier M, Loew M, Wortler K, Lampe R, Seil R, Handle G, Gassel S, et al. Extracorporeal shock wave therapy for the treatment of chronic calcifying tendonitis of the rotator cuff: a randomized controlled trial. JAMA J Am Med Assoc. 2003;290(19):2573–2580. doi: 10.1001/jama.290.19.2573. [DOI] [PubMed] [Google Scholar]
- 49.Giordano L, Murrell WD, Maffulli N. Prolotherapy for chronic low back pain: a review of literature. Br Med Bull. 2021;138(1):96–111. doi: 10.1093/bmb/ldab004. [DOI] [PubMed] [Google Scholar]
- 50.Asheghan M, Hashemi SE, Hollisaz MT, Roumizade P, Hosseini SM, Ghanjal A. Dextrose prolotherapy versus radial extracorporeal shock wave therapy in the treatment of chronic plantar fasciitis: A randomized, controlled clinical trial. Foot Ankle Surg. 2021;27(6):643–649. doi: 10.1016/j.fas.2020.08.008. [DOI] [PubMed] [Google Scholar]
- 51.Ludwig J, Lauber S, Lauber HJ, Dreisilker U, Raedel R, Hotzinger H. High-energy shock wave treatment of femoral head necrosis in adults. Clin Orthop Relat R. 2001;387:119–126. doi: 10.1097/00003086-200106000-00016. [DOI] [PubMed] [Google Scholar]
- 52.Luh JJ, Huang WT, Lin KH, Huang YY, Kuo PL, Chen WS. Effects of extracorporeal shock wave-mediated transdermal local anesthetic drug delivery on rat caudal nerves. Ultrasound Med Biol. 2018;44(1):214–222. doi: 10.1016/j.ultrasmedbio.2017.09.010. [DOI] [PubMed] [Google Scholar]
- 53.Peng BG. Pathophysiology, diagnosis, and treatment of discogenic low back pain. World J Orthop. 2013;4(2):42–52. doi: 10.5312/wjo.v4.i2.42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Liu H, Li H, Jin X, Yu S, Xi L, Zhao Z, Tian W. Effect of extracorporeal shock wave on the expression of IL-1β, TNF-α and MMP-13 in the joint fluid of patients with early to mid-stage osteoarthritis of the knee. Orthopedic Journal of China. 2016;24(19):1807–1810. [Google Scholar]
- 55.Hausdorf J, Lemmens MA, Kaplan S, Marangoz C, Milz S, Odaci E, Korr H, Schmitz C, Maier M. Extracorporeal shockwave application to the distal femur of rabbits diminishes the number of neurons immunoreactive for substance P in dorsal root ganglia L5. Brain Res. 2008;1207:96–101. doi: 10.1016/j.brainres.2008.02.013. [DOI] [PubMed] [Google Scholar]
- 56.Wang CJ, Sun YC, Wong T, Hsu SL, Chou WY, Chang HW. Extracorporeal shockwave therapy shows time-dependent chondroprotective effects in osteoarthritis of the knee in rats. J Surg Res. 2012;178(1):196–205. doi: 10.1016/j.jss.2012.01.010. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Quality of evidence assessment by GRADE of the included studies.
Data Availability Statement
The datasets used and analysed during the current study are available from the corresponding author on reasonable request.