Novel Teaching Points.
-
•
The angiographic appearance of type 3 SCAD and atherosclerotic plaque can be similar.
-
•
Lack of angiographic healing after 2-4 weeks favours the diagnosis of atherosclerosis.
-
•
Intravascular imaging is a useful tool to differentiate SCAD from atherosclerotic plaque when the diagnosis is uncertain.
A 27-year-old woman presented with severe chest pain and was diagnosed with acute coronary syndrome. Coronary angiography demonstrated coronary artery tortuosity and severe coronary artery stenoses involving the ostial-proximal and mid-vessel locations in the left anterior descending artery. This case illustrates how intracoronary imaging defined the etiology of her presentation.
History of Presentation
A 27-year-old woman was admitted with non-ST elevation myocardial infarction (MI). She developed recurrent episodes of chest pain and was transferred for coronary angiography (electrocardiogram: Supplemental Fig. S1, laboratory investigations: Supplemental Table S1).
Past Medical History
The patient began experiencing exertional back pain 2 months prior to admission. She consulted a cardiologist who performed stress echocardiography. Although she remained asymptomatic during 13 minutes of treadmill exercise, anterior hypokinesis was present with stress. A coronary computed-tomographic angiogram was planned; however, the hospitalization superseded these plans.
The patient has anxiety, treated with escitalopram. Her only cardiac risk factor is premature coronary artery disease in her father and uncles.
Investigations
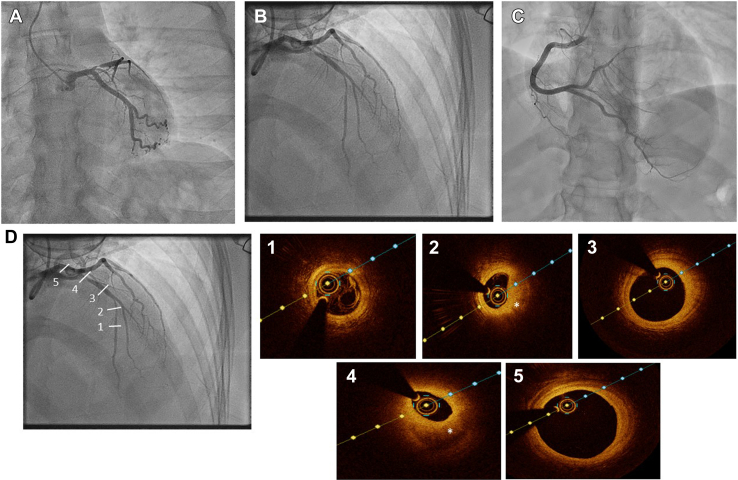
Echocardiography demonstrated preserved left ventricular systolic function with anterior hypokinesis. Coronary angiography (Fig. 1A-C; Videos 1-4
 , view videos online) demonstrated a 99% stenosis in the ostial-proximal left anterior descending artery (LAD), and a 60% long tubular stenosis in the mid-LAD. The rest of the coronary arteries were smooth, with mild tortuosity in the left circumflex and LAD arteries.
, view videos online) demonstrated a 99% stenosis in the ostial-proximal left anterior descending artery (LAD), and a 60% long tubular stenosis in the mid-LAD. The rest of the coronary arteries were smooth, with mild tortuosity in the left circumflex and LAD arteries.
Figure 1.
Initial coronary angiography. (A, B) Left coronary artery; (C) right coronary artery. (D) Optical coherence tomography of left anterior descending artery (LAD) at various levels: (1): Distal LAD: normal vessel architecture. (2) Mid-LAD lesion: high attenuation, homogeneous plaque with shadowy edges consistent with lipid-rich atherosclerotic plaque (asterisk). (3) Ectatic mid-LAD segment: lipid-rich plaque. (4) Ostial-proximal LAD severe stenosis caused by high attenuation, homogeneous plaque with shadowy edges consistent with lipid-rich plaque (asterisk). (5) Left main artery also demonstrates intimal thickening consistent with atherosclerosis.
Management
Based on the patient’s age and the presence of relatively smooth coronary arteries with some tortuosity, the diagnosis of spontaneous coronary artery dissection (SCAD)-related MI was initially favoured. However, the diagnosis of MI secondary to atherosclerosis could not be ruled out. The angiographic appearance was thought to be consistent with type 3 SCAD, which can be difficult to differentiate from atherosclerosis with angiography alone. Although initial intracoronary imaging was considered, the operator was concerned about undue coronary instrumentation in a patient with possible SCAD. Thus, the procedure was stopped, with a recommendation to consider relook angiography before discharge to confirm resolution of SCAD.
Aspirin and beta-blocker therapy were started. A head-to-pelvis computed-tomographic angiogram was performed without any signs of fibromuscular dysplasia. The patient was transferred to our centre because she lives nearby. During hospitalization, she experienced recurrent chest pain, with persistent T-wave inversions in several leads, but without further troponin elevation. Another angiogram was performed 2 weeks after initial admission (Videos 4 and 5
 , view videos online). The stenosis in the LAD was essentially unchanged. There was uncertainty as to whether sufficient time had passed to appreciate vessel healing, based on the reported literature.1 Despite administration of conscious sedation, the procedure was emotionally challenging for the patient, and the decision was made to end the procedure that day.
, view videos online). The stenosis in the LAD was essentially unchanged. There was uncertainty as to whether sufficient time had passed to appreciate vessel healing, based on the reported literature.1 Despite administration of conscious sedation, the procedure was emotionally challenging for the patient, and the decision was made to end the procedure that day.
After discussing this diagnostic dilemma (Supplemental Table S2), we reached a consensus that the angiographic findings were not typical for SCAD, as we expected that some evidence of vessel healing would be present by 2 weeks if the lesions were SCAD-related. Based on these findings, a diagnosis of atherosclerosis was favoured.
Follow-up
With an anesthesiologist providing deep conscious sedation, coronary angiography with intracoronary imaging was performed to reach a definite diagnosis (4 days after a second angiogram; Videos 6 and 7
 , view videos online). After predilatation of both LAD lesions with a 2-mm balloon, optical coherence tomography (OCT) examination of the LAD was performed. OCT revealed lipid-rich atherosclerotic plaque in the LAD, without evidence of intramural hematoma (Fig. 1D). Therefore, with the diagnosis of atherosclerosis confirmed, we proceeded to performing percutaneous coronary intervention (PCI) of the LAD.
, view videos online). After predilatation of both LAD lesions with a 2-mm balloon, optical coherence tomography (OCT) examination of the LAD was performed. OCT revealed lipid-rich atherosclerotic plaque in the LAD, without evidence of intramural hematoma (Fig. 1D). Therefore, with the diagnosis of atherosclerosis confirmed, we proceeded to performing percutaneous coronary intervention (PCI) of the LAD.
We performed OCT-guided PCI, implanting 2 drug-eluting stents in the LAD (a 2.5- × 24-mm Promus mid-LAD, and a 3.5- × 16-mm Promus ostial LAD; both Boston Scientific, Marlborough, MA). Post-interventional OCT identified some stent malapposition in the ectatic segment just proximal to the second diagonal branch (Supplemental Fig. S2), which required further postdilatation with larger noncompliant balloons. The final angiographic and OCT results were satisfactory (Videos 8-10
 , view videos online).
, view videos online).
Additional laboratory screening for vasculitis, collagen vascular diseases, and hypercoagulable state was negative. On a repeat extended lipid profile, the low-density lipoprotein level was 1.38 mmol/L while on statin therapy, and the lipoprotein (a) level was elevated at 234.9 nmol/L.
The patient was discharged 2 days after PCI on aspirin, ticagrelor, and rosuvastatin therapy.
Discussion
MI is uncommon among patients aged < 45 years and is very rare among patients aged < 30 years.2 Compared with older patients, those who are aged < 45 years are more likely to be male, current smokers, and obese, and to have a family history of premature coronary artery disease and higher low-density lipoprotein levels.2 SCAD is an etiology for acute coronary syndrome resulting from the formation of hematoma between the tunica media and the tunica adventitia layers of the vessel. This condition leads to luminal compression resulting in ischemia.3 SCAD is the cause of MI in nearly 35% of women aged < 50 years and should be considered in the differential diagnosis of all women presenting with MI.3
OCT is useful for differentiating SCAD from atherosclerosis. However, the performance of OCT for suspected SCAD carries some risks, including extension of dissection by the guidewire or imaging catheter, guide-catheter-related dissection, and hydraulic extension of dissection during contrast injection. Therefore, OCT should be used cautiously, and only when the diagnosis is uncertain.3
Our patient was very young, and she did not have cardiovascular risk factors except family history of premature coronary artery disease. Therefore, SCAD-related MI was favoured initially. OCT was not performed during the first 2 angiograms, to avoid potential complications. Most SCAD cases show some spontaneous healing within a few weeks.1 After the second angiogram (2 weeks after the initial presentation) did not show any healing of the LAD lesions, atherosclerosis-related MI became the favoured diagnosis. The elevated level of lipoprotein (a) also favoured atherosclerosis-related MI. OCT confirmed the diagnosis of atherosclerosis-related MI and was very helpful to precisely optimize the PCI in this patient.
Conclusions
SCAD and atherosclerosis can have similar angiographic appearances. Lack of improvement on follow-up angiograms favours an atherosclerosis-related MI. Intracoronary imaging is a useful tool to differentiate SCAD from atherosclerosis in cases of diagnostic uncertainty.
Acknowledgments
Ethics Statement
The research reported has adhered to relevant ethical guidelines.
Funding Sources
The authors have no funding sources to declare.
Disclosures
The authors have no conflicts of interest to disclose.
Footnotes
See page 347 for disclosure information.
To access the supplementary material accompanying this article, visit CJC Open at https://www.cjcopen.ca/ and at https://doi.org/10.1016/j.cjco.2023.03.011.
Supplementary Material
Coronary angiography via right radial artery. Left coronary artery (LCA) injection demonstrating ostial-proximal 99% LAD stenosis with Thrombolysis-in-myocardial-infarction (TIMI) grade 2 flow and otherwise smooth coronary arteries with mild distal tortuosity observed in the LAD and left circumflex arteries (left anterior oblique (LAO) 15°, Caudal 28°).
LCA injection demonstrating mid-LAD 60% stenosis and otherwise smooth coronary arteries with mild distal tortuosity observed in the LAD and left circumflex arteries. (LAO 18°, Cranial 27°)
Right coronary artery. (LAO 25°)
Re-look angiography via right radial artery. LCA injection demonstrating persistent ostial-proximal 99% LAD stenosis with TIMI grade 2 flow (RAO 18°, Caudal 18°).
LCA injection demonstrating mid-LAD 60-70% stenosis. (LAO 27°, Cranial 18°)
Second relook angiogram via right radial artery. LCA injection demonstrating persistent ostial-proximal 99% LAD stenosis with TIMI grade 2 flow (RAO 19°, Caudal 19°).
LCA injection demonstrating ostial-proximal 99% LAD stenosis and mid-LAD 60-70% stenosis. (RAO 10°, Cranial 39°)
Final angiographic view of LCA after PCI to LAD with implantation of 2 drug eluting stents (RAO 10°, Cranial 39°)
Post-PCI LCA (LAO 46°, Caudal 29°)
Post-PCI LCA (RAO 2°, Caudal 36°)
References
- 1.Hassan S., Prakash R., Starovoytov A., Saw J. Natural history of spontaneous coronary artery dissection with spontaneous angiographic healing. JACC Cardiovasc Interv. 2019;12:518–527. doi: 10.1016/j.jcin.2018.12.011. [DOI] [PubMed] [Google Scholar]
- 2.Jortveit J., Pripp A.H., Langørgen J., Halvorsen S. Incidence, risk factors and outcome of young patients with myocardial infarction. Heart. 2020;106:1420–1426. doi: 10.1136/heartjnl-2019-316067. [DOI] [PubMed] [Google Scholar]
- 3.Hayes S.N., Tweet M.S., Adlam D., et al. Spontaneous coronary artery dissection: JACC state-of-the-art review. J Am Coll Cardiol. 2020;76:961–984. doi: 10.1016/j.jacc.2020.05.084. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Coronary angiography via right radial artery. Left coronary artery (LCA) injection demonstrating ostial-proximal 99% LAD stenosis with Thrombolysis-in-myocardial-infarction (TIMI) grade 2 flow and otherwise smooth coronary arteries with mild distal tortuosity observed in the LAD and left circumflex arteries (left anterior oblique (LAO) 15°, Caudal 28°).
LCA injection demonstrating mid-LAD 60% stenosis and otherwise smooth coronary arteries with mild distal tortuosity observed in the LAD and left circumflex arteries. (LAO 18°, Cranial 27°)
Right coronary artery. (LAO 25°)
Re-look angiography via right radial artery. LCA injection demonstrating persistent ostial-proximal 99% LAD stenosis with TIMI grade 2 flow (RAO 18°, Caudal 18°).
LCA injection demonstrating mid-LAD 60-70% stenosis. (LAO 27°, Cranial 18°)
Second relook angiogram via right radial artery. LCA injection demonstrating persistent ostial-proximal 99% LAD stenosis with TIMI grade 2 flow (RAO 19°, Caudal 19°).
LCA injection demonstrating ostial-proximal 99% LAD stenosis and mid-LAD 60-70% stenosis. (RAO 10°, Cranial 39°)
Final angiographic view of LCA after PCI to LAD with implantation of 2 drug eluting stents (RAO 10°, Cranial 39°)
Post-PCI LCA (LAO 46°, Caudal 29°)
Post-PCI LCA (RAO 2°, Caudal 36°)