Abstract
This study examines whether Medicare Advantage (MA) enrollees with more chronic conditions were more likely to disenroll when MA enrollment grew rapidly from 2009 to 2019.
Medicare Advantage (MA) is becoming the dominant source of Medicare coverage. MA plans are paid capitated rates and have historically selectively enrolled healthier individuals. In response, Medicare has repeatedly recalibrated the risk-adjustment model. However, concerns still exist that MA plans may have access barriers (eg, restrictive clinician or hospital networks and utilization management) for enrollees with demanding health needs.1 We examined whether MA enrollees with more chronic conditions are more likely to disenroll over a recent 10-year period when MA enrollment grew rapidly.
Methods
This repeated cross-sectional study used 2009-2019 data (except unreleased 2014 data) from the Medicare Current Beneficiary Survey,2 a nationally representative, in-person panel survey of Medicare beneficiaries, with response rates of 65.2% for initial interviews and 78.3% for follow-up interviews (eMethods in Supplement 1). We identified community-dwelling beneficiaries 65 years or older with at least 2 consecutive years of data. Switching was identified as enrollment in MA at the end of a year and Medicare fee-for-service (FFS) enrollment the following year or vice versa.
We counted the number of chronic conditions reported by enrollees and categorized it as 0 to 1, 2 to 3, 4 to 5, and 6 or more following Centers for Medicare & Medicaid Services methodology.3 We estimated logistic regressions adjusted for demographic characteristics and Medicare-Medicaid dual eligibility to calculate adjusted annual switching rates for MA to FFS and FFS to MA, by number of chronic conditions (see eMethods in Supplement 1 for details). We also conducted stratified analyses by dual eligibility. All analyses accounted for the survey design and nonresponse rates, and adjusted Wald statistics were used for statistical significance (2-sided P < .05).
The Ohio State University Institutional Review Board approved this study and exempted informed consent for using secondary data. Data were analyzed using Stata/MP version 14.2 (StataCorp).
Results
The study sample included 15 403 MA enrollees and 28 627 FFS enrollees (unweighted) (55.8% female; mean age, 74.8 years; mean 3.9 chronic conditions; weighted). The overall adjusted mean rates of switching from MA to FFS were not significantly associated (P = .09) with the number of chronic conditions: 4.0% (95% CI, 2.9%-5.2%) among those with 0 to 1 condition (n = 1753), 3.4% (95% CI, 2.8%-3.9%) for 2 to 3 conditions (n = 5128), 2.8% (95% CI, 2.3%-3.2%) for 4 to 5 conditions (n = 5021), and 4.0% (95% CI, 3.0%-4.9%) for 6 or more conditions (n = 3501). Mean MA disenrollment rates decreased between 2010-2011 (6.4% [95% CI, 5.3%-7.4%]) and 2012-2013 (2.9% [95% CI, 2.1%-3.6%]), but remained stable after 2013 for all condition groups. The trends in adjusted switching rates over time did not significantly differ by number of conditions (P = .92) (Figure 1A).
Figure 1. Adjusted Rates of Switching Between Medicare Advantage (MA) and Medicare Fee-for-Service (FFS), 2010-2019.
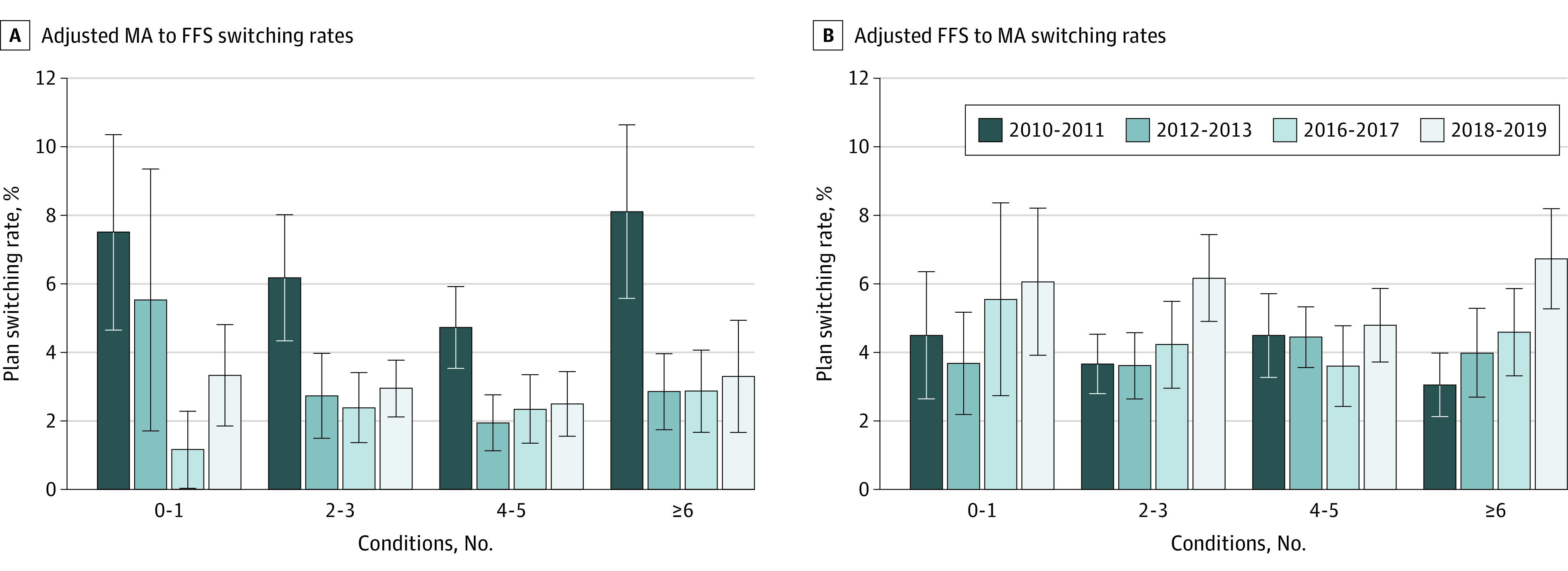
Medicare Current Beneficiary Survey data for 2014 are unavailable because they were never released by the Centers for Medicare & Medicaid Services. Therefore, Medicare enrollment switching could not be identified for 2014 or 2015. Error bars represent 95% CIs for adjusted switching rates, calculated from logistic regression models using interactions between year and number of chronic conditions.
The mean rates of switching from FFS to MA were stable between 2010-2011 (3.9% [95% CI, 3.3%-4.5%]) and 2016-2017 (4.3% [95% CI, 3.5%-5.1%]), then increased to 5.8% (95% CI, 5.0%-6.6%) in 2018-2019, with no differences by condition group (P = .16) (Figure 1B). Switching rates were not significantly associated (P = .50) with the number of chronic conditions.
Dual-eligible enrollees (n = 2446) had higher mean MA disenrollment rates than non–dual-eligible enrollees (n = 12 957) (5.3% vs 3.0%, P < .001). MA disenrollment rates were not different across condition groups for dual-eligible (P = .63; Figure 2A) or non–dual-eligible (P = .87; Figure 2B) enrollees.
Figure 2. Adjusted Rates of Switching From Medicare Advantage (MA) to Medicare Fee-for-Service (FFS) by Medicaid Dual Eligibility, 2010-2019.
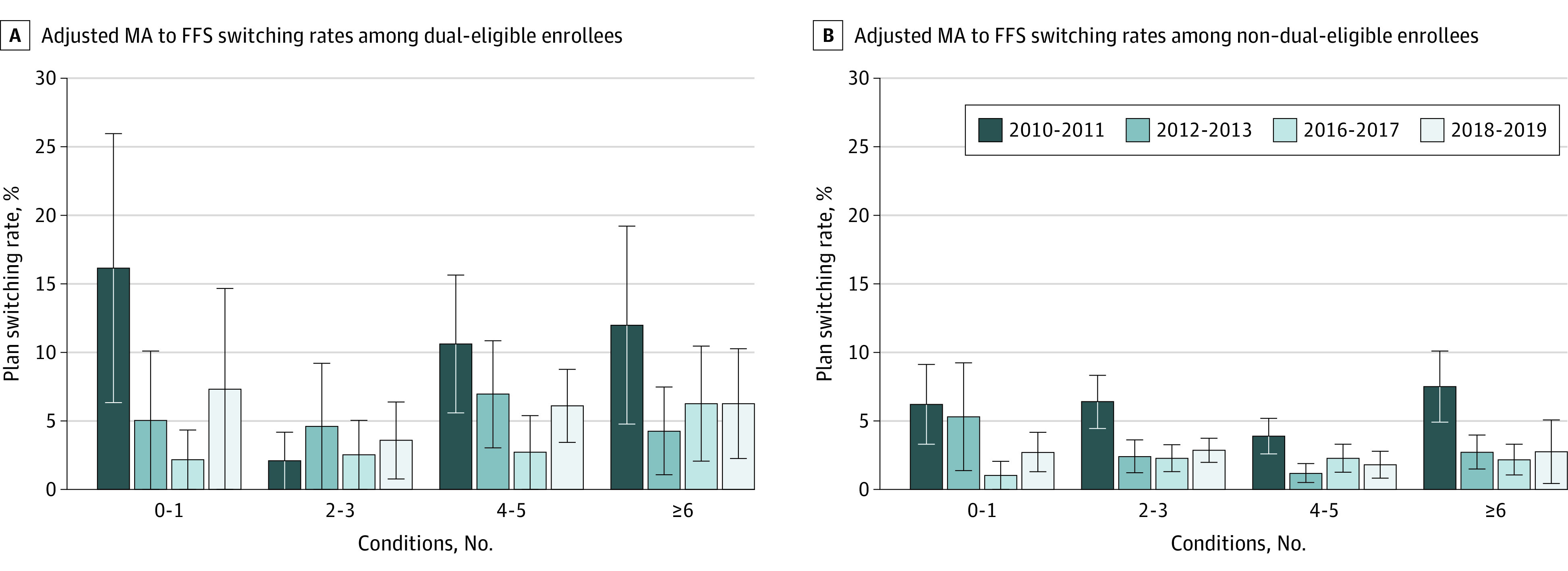
Medicare Current Beneficiary Survey data for 2014 are unavailable because they were never released by the Centers for Medicare & Medicaid Services. Therefore, Medicare enrollment switching could not be identified for 2014 or 2015. Error bars represent 95% CIs for adjusted switching rates, calculated from logistic regression models using interactions between year and number of chronic conditions.
Discussion
Although MA disenrollment rates decreased over time, having multiple chronic conditions was not associated with switching between MA and FFS between 2010 and 2019. Prior research found higher MA disenrollment rates among enrollees with a specific condition or new functional disability than those without, using data from before 2015.4,5,6 Several reasons may explain the study findings. First, the current risk-adjusted payments may have mitigated MA plans’ incentives to avoid high-risk enrollees. Second, MA plans may make efforts to retain sicker people from whom they can generate larger revenue from risk-adjusted payments. Third, MA plans have lower out-of-pocket costs with supplemental benefits to manage chronic conditions that are particularly helpful for those with multiple conditions.
Study limitations include being ungeneralizable to beneficiaries younger than 65 years, potential measurement errors for self-reported conditions, and being unable to account for multiple switches.
While these findings do not support the concern about disproportionate MA disenrollment among sick enrollees, future research should monitor the portion of enrollees that disenroll from MA and whether MA plans meet the needs of enrollees, especially those who are dual-eligible.
Section Editors: Jody W. Zylke, MD, Deputy Editor; Kristin Walter, MD, Senior Editor.
eMethods
eReferences
Data Sharing Statement
References
- 1.Meyers DJ, Belanger E, Joyce N, McHugh J, Rahman M, Mor V. Analysis of drivers of disenrollment and plan switching among Medicare Advantage beneficiaries. JAMA Intern Med. 2019;179(4):524-532. doi: 10.1001/jamainternmed.2018.7639 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Centers for Medicare & Medicaid Services . Medicare current beneficiary survey. Accessed January 10, 2023. https://www.cms.gov/Research-Statistics-Data-and-Systems/Research/MCBS
- 3.Centers for Medicare & Medicaid Services . Multiple chronic conditions. December 1, 2021. Accessed April 25, 2023. https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/Chronic-Conditions/MCC_Main
- 4.Meyers DJ, Rahman M, Rivera-Hernandez M, Trivedi AN, Mor V. Plan switching among Medicare Advantage beneficiaries with Alzheimer’s disease and other dementias. Alzheimers Dement (N Y). 2021;7(1):e12150. doi: 10.1002/trc2.12150 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Park S, Fishman P, White L, Larson EB, Coe NB. Disease-specific plan switching between Traditional Medicare and Medicare Advantage. Perm J. 2020;24:19.059. doi: 10.7812/TPP/19.059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ankuda CK, Ornstein KA, Covinsky KE, Bollens-Lund E, Meier DE, Kelley AS. Switching between Medicare Advantage and Traditional Medicare before and after the onset of functional disability. Health Aff (Millwood). 2020;39(5):809-818. doi: 10.1377/hlthaff.2019.01070 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eMethods
eReferences
Data Sharing Statement


