Abstract
Cancer stem cells (CSCs) are considered to be responsible for tumor recurrence and metastasis. Therefore, clarification of the mechanisms involved in CSC stemness maintenance and cell fate determination would provide a new strategy for cancer therapy. Unregulated cellular energetics has been accepted as one of the hallmarks of cancer cells, but recent studies have revealed that mitochondrial metabolism can also actively determine CSC fate by affecting nuclear stemness gene expression. Herein, from the perspective of mito-nuclear communication, we review recent progress on the influence of mitochondria on CSC potential from four aspects: metabolism, dynamics, mitochondrial homeostasis, and reactive oxygen species (ROS).
Video Abstract
Supplementary Information
The online version contains supplementary material available at 10.1186/s12964-023-01160-x.
Keywords: Cancer stem cells (CSCs), Mitochondria, Cell fate determination, Mito-nuclear communication
Introduction
Cancer stem cells (CSCs) are a subpopulation of cancer cells with the potential for self-renewal and multidifferentiation and thus drive carcinogenesis, chemoresistance, recurrence and metastasis [1–6]. CSCs are also known as cancer stem cell-like cells [7], tumorigenic cells [8], tumor stem-like cells (TSCs) [9], and cancer- or tumor-initiating cells (CICs or TICs) [10, 11]. In 1997, CSCs were successfully isolated from the blood of leukemia patients for the first time [12]. Subsequently, CSCs were further identified in solid tumors, such as colon cancer [13], breast cancer [14], skin squamous cell cancer [15] and glioblastoma (GBM) [16]. However, CSCs are as heterogeneous as cancer cells, include metastatic cancer stem cell (MeCSC) or chemoresistant cancer stem cell (CRCSC) subsets, and have a quiescent or proliferative status and epithelial or mesenchymal status [17]. In response to various stimuli, the subsets or status of CSCs can be altered accordingly; therefore, CSCs are also plastic [18]. Moreover, upon attack by chemo/radiotherapy [19–22], hypoxia [23] and detachment [24], cancer cells can acquire stemness potential. Thus, plasticity is an important feature of CSCs and the key point to understanding CSC stemness maintenance and fate determination.
Mitochondrial energy metabolism is essential to CSCs in various intracellular activities, especially for nuclear stemness gene expression. Under different functional statuses or environmental conditions, plastic CSCs might adopt different metabolic patterns accordingly. Thus, the acquisition of CSC potential is accompanied by a reprogramming of cellular metabolism [25, 26]. Furthermore, cellular metabolism has been reported to determine CSC fate by epigenetically modifying nuclear stemness genes via metabolites. Therefore, mitochondrial energy metabolism is not merely a phenotype of CSCs but also a determinant of CSC fate. In this review, we focus on the regulation of CSC plasticity from the view of mitochondrial signals, that is, the regulation of mitochondrial metabolism, dynamics, mitochondrial homeostasis, and reactive oxygen species (ROS) on CSC potentials and the involvement of mito-nuclear communication.
Cancer stem cell plasticity and fate determination
The CSC theory holds that cancer cells are heterogeneous, and rare CSCs are the major driver of tumor initiation, metastasis and therapeutic resistance and thus the target for eradicating tumors [27–30]. More recently, the plastic CSC model has become widely accepted, and plasticity has become the main challenge of CSC targeted therapy [31]. Effective therapy must focus on the key regulatory factors that both maintain and induce the stemness of CSCs.
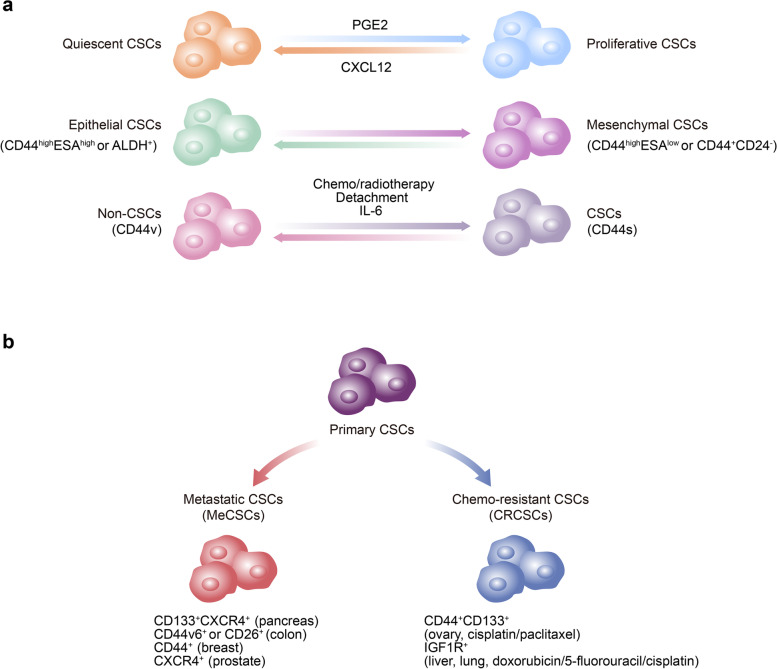
Cancer stem cell plasticity
Cell plasticity is defined as the ability of cells to quickly adapt to the changing microenvironment by dynamically switching between different cellular statuses or phenotypes in a reversible manner, which hijacks the program of dedifferentiation or transdifferentiation in cells [32–34]. The plasticity of CSCs, however, is exhibited as the dynamic and reversible transitions between quiescent and proliferative CSCs, epithelial and mesenchymal CSCs, CSCs and non-CSCs, or the evolution from primary CSCs to MeCSCs or CRCSCs, which respond to the adverse tumor microenvironment (Fig. 1). Higher CSC plasticity is likely to facilitate tumor progression and is associated with poor patient clinical outcomes.
Fig. 1.
Phenotypic plasticity of cancer stem cells. The plasticity of CSCs is exhibited as the dynamic and reversible transitions between quiescent and proliferative CSCs, epithelial and mesenchymal CSCs and CSCs and non-CSCs (A) or the evolution from primary CSCs to MeCSCs or CRCSCs (B). CSCs Cancer stem cells, MeCSCs Metastatic cancer stem cells, CRCSCs Chemoresistant cancer stem cells
Due to changing microenvironment signals, CSCs are not always in a quiescent status but can be activated and enter a proliferative status and then initiate tumor growth and recurrence [35]. In bladder cancer, for example, combined treatment with gemcitabine and cisplatin (GC) induces the production of a high level of prostaglandin E2 (PGE2), which further forces CSCs to exit from a quiescent status and enter a proliferative status and then causes tumor progression [36]. In addition, Prx1+ mesenchymal progenitor-derived CXCL12 maintains leukemic stem cells (LSCs) in a quiescent and tyrosine kinase inhibitor (TKI)-resistant status, whereas CXCL12 deletion forces LSCs to enter a proliferative (cycling) status and makes them subsequently sensitive to TKI [37] (Fig. 1A).
Another important manifestation of CSC plasticity is the transition between epithelial-like phenotypes and mesenchymal-like phenotypes, that is, epithelial-to-mesenchymal transition (EMT). In squamous cell carcinoma, two different CSC subsets are found: CD44highESAhigh CSCs (non-EMT subset), which have an epithelial phenotype and proliferate rapidly; and CD44highESAlow CSCs (EMT subset), which have a mesenchymal phenotype and migrate extensively [38]. When migrating to a secondary site, EMT CSCs recover into a proliferative mesenchymal-to-epithelial transition (MET) phenotype and then form metastatic tumors. Similarly, CD24-CD44+ breast cancer stem cells (BCSCs) located at the tumor invasive frontier display a quiescent mesenchymal phenotype, while aldehyde dehydrogenase-positive (ALDH+) BCSCs distributed more centrally show a proliferative epithelial phenotype. Moreover, BCSCs switch between a mesenchymal phenotype and an epithelial phenotype [39] (Fig. 1A).
Moreover, CSCs and non-CSCs can interconvert and achieve a dynamic balance [40, 41]. It has been reported that bulk breast cancer cells can convert into BCSCs under certain conditions, such as chemo/radiotherapy [42], detachment [24], and IL-6 induction [43]. During this process, breast cancer cells are switched between non-CSCs and CSCs by selective splicing of CD44 into CD44v or CD44s, and cancer cells with high levels of CD44v lose CSC stemness, while those with high levels of CD44s gain CSC stemness [44] (Fig. 1A).
In addition, CSCs exhibit phenotypic evolution during the process of tumor progression. During the early stage of tumorigenesis, primary CSCs are present in tumor cells with gene mutations. As a tumor develops into an advanced stage, MeCSCs with the potential to disseminate from the primary site, survive in the circulation, and seed and expand in the new microenvironment evolve (Fig. 1B). These MeCSCs can be organ specific [45]. When patients receive targeted therapy and/or chemotherapy, primary CSCs survive long-term administration of drugs; that is, CRCSCs or drug-resistant CSCs are developed [17] (Fig. 1B). It has been reported that MeCSCs share similar stemness potentials and epigenetic regulation mechanisms with primary CSCs. The first MeCSCs were identified as CD133+CXCR4+ subpopulations in CD133+ pancreatic CSCs with the potential to metastasize to the liver [46]. MeCSC subpopulations such as CD44v6 CSCs or CD26+ CSCs in colorectal cancer [47, 48], CD44+ CSCs in breast cancer [49], and CXCR4+ CSCs in prostate cancer [50] have also been found. Regarding CRCSCs, the CD44+CD133+ subpopulation with the potential for drug resistance was identified in CSC-like SKOV3 ovarian tumorspheres treated with cisplatin and/or paclitaxel [51]. In addition, IGF1R+ chemoresistant TSCs are found in lymphoma hepatocellular carcinoma (HCC) or Lewis lung cancer cells treated with doxorubicin, 5-fluorouracil or cisplatin [9] (Fig. 1B).
The plasticity of phenotype and status indicates that the developmental fate of cells can be changed; for example, it can be shifted toward a more undifferentiated status via dedifferentiation or to other lineages via transdifferentiation. Plasticity enables CSCs to better survive in adverse environments by easily switching their status and quickly altering phenotypes in response to various internal or external signals [52].
Cancer stem cell fate determination
Although the alteration of plastic cellular phenotype or status is triggered by environmental cues, the decision of CSC fate is actually determined by the expression of nuclear stemness genes, which are regulated by specific transcription factors (TFs) [53]. In glioblastoma stem cells (GSCs), for example, the expression levels of key stemness-related TFs (POU3F2, SOX2, SALL2, and OLIG2) are significantly higher than those in more differentiated tumor cells. These four TFs can dedifferentiate and reprogram GBM cells into GSCs in in vitro cultured cells and in vivo animal models [54]. In contrast, dual-specificity tyrosine phosphorylation-regulated kinase 1A (DYRK1A) promotes the differentiation of GSCs and inhibits the acquisition of stemness potential by decreasing the expression of SOX2 [55].
With the gain or loss of stemness potential, the expression of stemness-related TFs is increased or decreased and is regulated at the posttranscriptional or translational level via epigenetic modifications. Growing evidence reveals that nonmutational and reversible epigenetic events, such as histone and chromatin modifications or DNA methylation, significantly contribute to CSC plasticity and carcinogenesis. For instance, SIRT1-mediated deacetylation of β-catenin maintains its stability, and the resulting nuclear accumulation of β-catenin increases the transcriptional level of NANOG and promotes the stemness potential of liver CSCs [56]. In another study, the zinc finger and homeobox 2 (ZHX2) protein was reported to eliminate liver CSC features by transcriptionally repressing KDM2A and inhibiting KDM2A-mediated demethylation of histone H3 lysine 36 in the promoter regions of stemness-related TFs (NANOG, SOX4, OCT4) [57].
Many factors inside and outside the cells, such as growth factors, inflammatory mediators, intracellular pH, mitochondrial metabolites and ROS, can influence the activity of stemness-related TFs at the level of epigenetic modification and then alter cell fates [58, 59]. Recently, an increasing number of studies have suggested that mitochondria play important roles not only in maintaining CSC stemness but also in determining CSC fate [60–66]. Therefore, we summarize CSC fate determination from a new view of mito-nuclear communication.
Mito-nuclear communication and CSC fate determination
Mitochondria have their own genetic material (mtDNA) and corresponding gene transcription and protein translation systems. However, the majority (>99%) of proteins in mitochondria are not encoded by the mitochondrial genome but by the nuclear genome [67]. To harmonize nuclear-encoded protein synthesis with appropriate mitochondrial biogenesis or energy metabolism, the crosstalk between mitochondria and nucleus, in other words, mito-nuclear communication, has evolved. Proper communication between mitochondria and the nucleus allows mutual benefits and ensures the overall fitness of cells.
Ordinarily, mitochondria are under tight control by the nucleus through anterograde regulation signaling (from nucleus to mitochondria) according to cellular energy needs [68]. However, more recent studies have demonstrated that mitochondria can also generate retrograde signals to the nucleus via mito-to-nuclear communication mediated by small molecules, metabolites, peptides, mtDNA and ions through physical contact or signal transmission [69–71]. This concept expands the previous understanding that mitochondria are not merely semiautonomous organelles. Moreover, mitochondria can actively influence the expression of nuclear stemness genes, reprogram cell metabolism and phenotype, and thus determine CSC fate [68, 72, 73].
First, mitochondrial energy metabolism-derived metabolites or ROS are reported to play important roles in CSC fate determination through metabolic and epigenetic modification of stemness genes. In addition, mitochondrial dynamics or the balance between biogenesis and mitophagy could exert an influence on CSCs. In the following section, we discuss the influences of mitochondrial retrograde signaling on CSC fate determination in four aspects: energy metabolism, dynamics, mitochondrial homeostasis, and ROS.
Mitochondrial energy metabolism
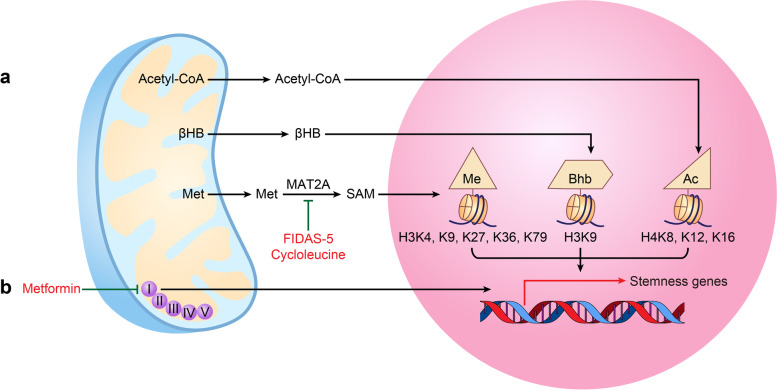
Mitochondrial energy metabolism has profound impacts on the fate of CSCs [74–76] (Fig. 2). Recently, mitochondrial metabolites, which are generally involved in energy support, were reported to act as signaling molecules and to play critical roles in controlling gene expression [77]. In detail, mitochondrial metabolites, such as acetyl-coenzyme A (acetyl-CoA), β-hydroxybutyric acid (βHB), S-adenosylmethionine (SAM), NAD+, succinate, α-ketoglutarate (α-KG), ATP, and FAD, act as cofactors of epigenetic modifying enzymes and drive the acquisition of stemness potential by affecting stemness gene expression [72, 78]. For example, by enhancing the acetylation levels of histone H4K8ac, H4K12ac, and H4K16ac, acetyl-CoA activates the protein expression of stemness-related TFs (c-MYC, OCT4, KLF4, SOX2), which further increases the tumorsphere formation of CSCs in triple-negative breast cancer [79] (Fig. 2A). Furthermore, in hepatocellular carcinoma, accumulated βHB upregulates the expression levels of CD44, CD133, SOX9 and EpCAM by increasing the β-hydroxybutyrylation level of histone H3K9bhb and then significantly improves the proportions of CSCs for in vivo tumor formation and increases the abilities of colony formation and tumorsphere formation [80] (Fig. 2A). However, in acute myeloid leukemia (AML), low SAM levels decrease global DNA methylation, causing increased expression of differentiated myeloid genes (CD11b, CD14) but decreased expression of stemness genes, thereby enhancing differentiation but inhibiting self-renewal in LSCs [81].
Fig. 2.
Mitochondrial energy metabolism and cancer stem cell stemness. A Acetyl-CoA promotes the expression of stemness-related transcription factors by enhancing the acetylation levels of histone H4K8ac, H4K12ac, and H4K16ac. βHB upregulates the expression levels of CSC marker genes by increasing the β-hydroxybutyrylation level of histone H3K9bhb. B Metformin suppresses mitochondrial complex I of oxidative phosphorylation and downregulates the expression of CSC-related genes. Inhibitors of the key methionine cycle enzymes MAT2A, cycloleucine and FIDAS-5 reduce CSC stemness by decreasing SAM levels and the expression of the methylation marks H3K4me3 alone or H3K9me3, H3K27me3, H3K36me2, H3K36me3 and H3K79me3. acetyl-CoA acetyl-coenzyme A, βHB β-hydroxybutyric acid, CSC Cancer stem cell, TFs Transcription factors, MAT2A Methionine adenosyltransferase 2A, SAM S-adenosylmethionine
Mitochondrial dynamics
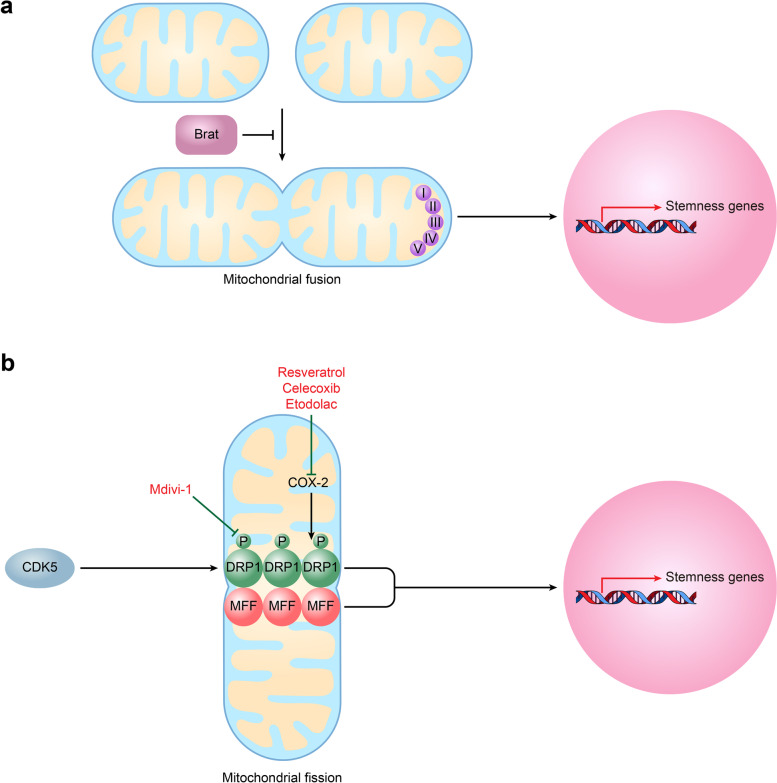
Mitochondrial dynamics, which involve vigorous changes in mitochondrial morphology between fission and fusion, are essential events that maintain the distribution, function and vitality of mitochondria [82–85]. Mitochondrial fission is the process by which a single mitochondrion divides into two short, round, balloon-shaped or fragmented daughter mitochondria and is mainly regulated by dynamin-related protein 1 (DRP1), DRP1 receptor mitochondrial fission factor (MFF), and fission factor 1 (FIS1) [86, 87]. Mitochondrial fusion is a phenomenon in which two closely contacted mitochondria are coordinately fused in the outer and inner membranes, forming an elongated, large, and interconnected mitochondrial network. The process of mitochondrial fusion is mainly regulated by the outer membrane fusion proteins mitofusins 1 and 2 (MFN1, MFN2) and the inner membrane fusion protein optic atrophy 1 (OPA1) [88]. To meet the cellular energy requirements in response to environmental changes, mitochondria dynamically switch between tubular and fragmented forms by balancing the process of fission and fusion.
Both fusion and fission can enhance CSC stemness and maintain self-renewal, depending on the tissue type of the tumor. Bonnay et al found that mitochondrial fusion helps to sustain CSC fates or phenotypes in neuroblastoma [89]. In detail, mitochondrial fusion induced by brat knockdown increased oxidative phosphorylation (OXPHOS) and NAD+ levels and then drove the immortalization and tumorigenicity of TICs [89] (Fig. 3A). However, some other studies have indicated that mitochondrial fission promotes the potential and self-renewal of CSCs [90]. In liver cancer, the complex formed by T-box transcription factor 19 (TBX19) and PRMT1 induces MFF expression by increasing histone H4R3me2a/H3K9ac levels; then, MFF promotes mitochondrial fission, increases the expression level of OCT4, enhances the formation of tumorspheres and enriches the side populations (SPs) [91] (Fig. 3B). In glioblastomas, cycle-dependent kinase 5 (CDK5) phosphorylates DRP1 at Ser616 and increases mitochondrial cleavage, which then induces the expression of stemness genes (OLIG2, OCT4, NANOG, NESTIN, POU3F2, CD133, SSEA1) [92] (Fig. 3B). Contrary to popular views, recent studies have shown evidence that mitochondrial fission inhibits the stemness of CSCs. For example, the activation of mitochondrial fission by overexpressing MFF impairs BCSC propagation through methods such as reducing the capacity for tumorsphere formation and the enzyme activity of the stem cell marker ALDH [93].
Fig. 3.
Mitochondrial dynamics and cancer stem cell stemness. A Mitochondrial fusion induced by brat knockdown increased OXPHOS and NAD+ levels and then drove the immortalization and tumorigenicity of tumor-initiating cells (TICs). B CDK5 phosphorylates DRP1 and increases mitochondrial cleavage, which then induces the expression of stemness genes. Similarly, MFF promotes mitochondrial fission and then increases OCT4 expression levels. Mdivi-1 reduces the expression of stemness genes by inhibiting DRP1; selective COX-2 inhibitors resveratrol, celecoxib, and etodolac reduce the expression level of stemness genes by inhibiting DRP1 indirectly. OXPHOS Oxidative phosphorylation, TICs Tumor-initiating cells, CDK5 Cycle-dependent kinase 5, MFF Mitochondrial fission factor
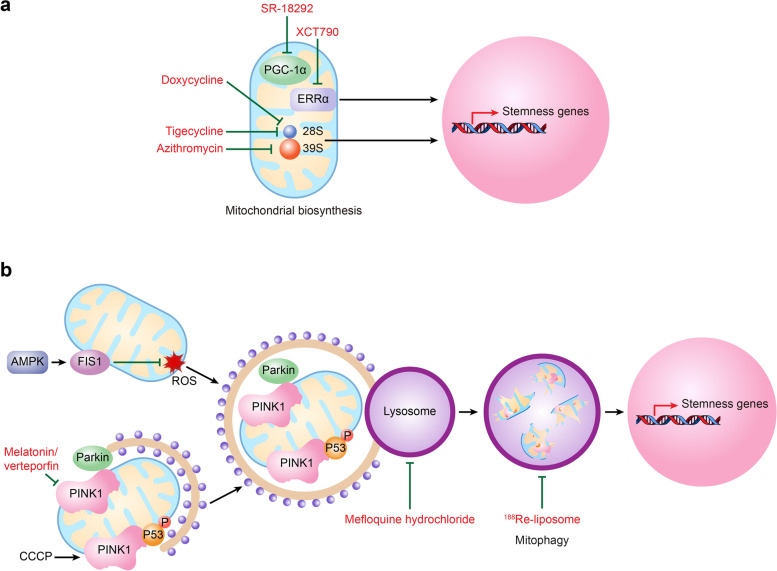
Mitochondrial homeostasis
Mitochondrial biogenesis and mitophagy are two balanced processes in cells that control the quantity and quality of mitochondria [94]. Mitochondrial biogenesis is the process of replenishing new healthy mitochondria, while mitophagy is the activity by which cells spontaneously phagocytose or selectively degrade dysfunctional or redundant aging mitochondria under conditions of stress such as hypoxia or nutritional deficiency [95–98]. Mitochondrial biogenesis and mitophagy are both key events in regulating the stemness of CSCs.
Promoting mitochondrial biogenesis by PGC-1α [99] or its cofactor estrogen-related receptor α (ERRα) [100] increases tumorsphere formation in pancreatic cancer and breast cancer, respectively (Fig. 4A). In contrast, PGC-1α knockdown in glioblastoma cells leads to the attenuation of the neoplastic phenotype and loss of stem-like features, which was reflected by reduced expression of the stemness gene SOX2 but prolonged survival of nude mice [101].
Fig. 4.
Mitochondrial homeostasis and cancer stem cell stemness. A PGC-1α or its cofactor ERRα increases mitochondrial biogenesis, which further promotes the maintenance of the CSC phenotype. Azithromycin, doxycycline, and tigecycline block mitochondrial biogenesis by targeting mitochondrial ribosomes 39S and 28S and then inhibit CSC self-renewal capability. In addition, the selective PGC-1α inhibitor SR-18292 or ERRα inverse agonist XCT790 downregulates the expression of stemness genes and reduces the ratio of CSCs. B AMPK-FIS1 signaling promotes mitophagy, thereby enhancing CSC self-renewal by inhibiting ROS production. CCCP increases CSC ratios by recruiting PINK1 and enhancing mitophagy-mediated removal of phosphorylated p53 and then increases NANOG expression. In contrast, the combination of melatonin and verteporfin reduces CSC stemness by inhibiting the expression of PINK1/Parkin, while mefloquine hydrochloride reduces the ratio of colon CSCs by inhibiting mitophagy and lysosomal activity. In addition, 188Re-liposomes reduced the protein levels of mitophagy markers, which further decreased the function of CSCs. CSC Cancer stem cell, AMPK Adenosine 5'-monophosphate-activated protein, FIS1 Fission factor 1, CCCP Carbonyl cyanide chlorophenylhydrazone, PINK1 PTEN-induced kinase 1
Regarding mitophagy, an increase in mitophagy by the depression of oxidative stress or an attenuation of mitophagy by parkin interference can lead to the generation or loss of CD44highCD24-/low esophageal CSCs [102]. For example, adenosine 5'-monophosphate-activated protein (AMPK)-FIS1 signaling-mediated mitophagy leads to the elimination of damaged mitochondria, thereby inhibiting intracellular ROS production and promoting the self-renewal and survival of LSCs [103] (Fig. 4B). At the molecular level, mitophagy promotes the formation of CSCs by altering the subcellular location of phosphorylated p53 between mitochondria and the nucleus. In detail, when mitophagy is enhanced by carbonyl cyanide chlorophenylhydrazone (CCCP), PTEN-induced kinase 1 (PINK1) recruits and phosphorylates p53 at serine-392 and entraps p53 on mitochondria; subsequently, p53 is removed by mitophagy, and thus, the expression of NANOG and the ratio of the CD133+ liver CSC population are increased (Fig. 4B). Conversely, when mitophagy is inhibited by a mitochondrial fission inhibitor (Mdivi-1), PINK1-phosphorylated p53 is rapidly translocated to the nucleus, which results in the suppressed expression of NANOG and a reduction in the CD133+ CSC ratio [104].
Mitochondrial ROS
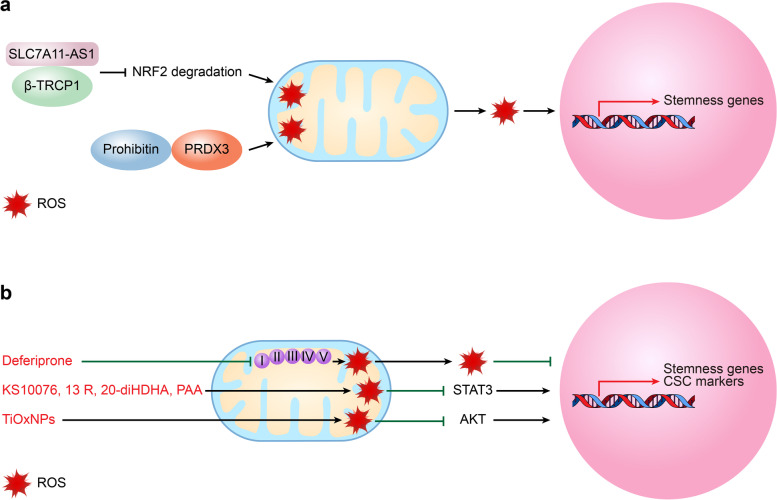
ROS, the main byproducts of oxidative metabolism, include superoxide radical anions, hydroxyl radicals, hydrogen peroxide, and lipid hydrogen peroxide [105, 106]. The roles of ROS in regulating CSC self-renewal and survival occur in a context- and tissue-dependent manner. Generally, ROS are reported to maintain CSC properties and to induce CSC proliferation and tumorigenicity. In colorectal cancer (CRC), RAC1 activation upon Apc loss triggers the production of high levels of ROS in the intestines of vil-Cre-ERT2 Apcfl/fl Rac1fl/fl mice; then, ROS further increase the expression of stemness genes (LGR5, OLFM4, RGMB), confer LGR5 CSC phenotypes, and thus initiate CRC [107]. Conversely, as ROS levels decrease following a sublethal dose of H2O2, ESA+CD44+CD24- BCSCs lose the ability to form tumorspheres and colonies [108]. However, many studies have found that increasing intracellular ROS levels can induce CSC death and that a low level of ROS is required for the maintenance of cancer stemness [109]. In pancreatic cancer, lncRNA SLC7A11-AS1 promoted stemness potential by scavenging ROS, which functioned by interacting with β-TRCP1 and then blocking nuclear factor erythroid-2-related factor 2 (NRF2) degradation [110] (Fig. 5A). In GSCs, high levels of prohibitin promote GSC self-renewal by stabilizing PRDX3 and maintaining low levels of mitochondrial ROS [111] (Fig. 5A).
Fig. 5.
Mitochondrial ROS signaling and cancer stem cell stemness. A SLC7A11-AS1/β-TRCP1 or prohibitin promote CSC stemness potential by blocking NRF2 degradation and thus scavenging ROS or by interacting with PRDX3 and maintaining low mitochondrial ROS levels. B By blocking the role of iron in electron transport, deferiprone induces mitochondrial ROS and disrupts CSC stemness. KS10076, 13 R, 20-diHDHA, and PAA induce the production of ROS, degrade STAT3 or decrease the expression levels of CSC self-renewal genes, while TiOxNPs reduce CSC marker expression levels by inducing ROS levels and inactivating AKT signaling. CSC Cancer stem cell, 13 R 20-diHDHA, 13R 20-dihydroxydocosahexaenoic acid, PAA Phenylacetaldehyde, TiOxNPs Titanium peroxide nanoparticles
Blocking mito-nuclear communication as an emerging strategy for anti-CSC therapy
Despite significant improvements in anticancer drug development, CSC-derived chemoresistance and recurrence are still major challenges for cancer treatments. As CSCs and non-CSCs have different metabolic characteristics and mitochondrial metabolism governs CSC fates, blocking mito-nuclear communication would be an effective and innovative strategy. In the following section, we summarize the recent progress in gene interventions and therapeutic agents targeting mito-nuclear communication for CSC eradication (Tables 1 and 2).
Table 1.
Genetic inhibition for blocking mito-nuclear communication in CSCs
| Patterns of mito-nuclear communication | Names of genes | Mechanisms of action | CSC types and tissue origins |
|---|---|---|---|
| Mitochondrial fission | DRP1 | Reduces the capability of tumorsphere and tumor formation, especially the self-renewal of CSCs | CD133+CD15+ BTICs [92] |
| MFF or BRD4 | Reduces the capability of tumorsphere and tumor formation, especially the self-renewal of CSCs | Prostate CSCs [112] | |
| FIS1 | Reduces the expression levels of stemness genes and inhibits tumorsphere and tumor formation, especially the self-renewal of CSCs | sphere enriched Lung CSCs [113] | |
| Mitophagy | PINK1 and TBC1D15 | Decreases the levels of self-renewal markers | LSCs [103] |
| ATG14 | Decreases the expression levels of self-renewal and stemness markers and the number of tumorspheres | CSCs in oral squamous cell carcinoma [114] | |
| BNIP3L | Decreases the expression levels of stemness markers and the percentage of SP+ subpopulations | LCSCs [115] |
Table 2.
Therapeutic agents for blocking mito-nuclear communication in CSCs
| Patterns of mito-nuclear communication | Key mitochondrial behaviors and targets | Therapeutic agents | Mechanisms of action | CSC types and tissues origin |
|---|---|---|---|---|
| Mitochondrial energy metabolism | Oxidative phosphorylation, mitochondrial complex I | Metformin, mitochondrial complex I inhibitor | Downregulates the expression of CSC-related genes, decreases the ratios of CD44highALDHhigh cells as well as the sizes and numbers of tumorspheres, reduces the volume of tumors | sphere enriched CSCs in cholangiocarcinoma [116]; HNSCC CSCs [117] |
| Methionine cycle, SAM levels | FIDAS-5, MAT2A inhibitor | Inhibits the expression of methylation marks of H3K4me3 etc., reduces the mass and volume of xenograft tumors, diminishes the size of NOD.Cg-Prkdcscid Il2rgtm1Wjl/SzJ mouse lung lesions, decreases the ratio of CD166+ CSCs | sphere enriched and CD166+ Lung CSCs [118] | |
| Cycloleucine, MAT2A inhibitor | Suppresses the demethylation of H3K4me3 and inhibits the protein expression of the stemness transcription factor SOX9; the combination of cycloleucine and methionine depletion more effectively reduces mammospheres in vitro and the burden of primary and lung metastases in vivo | sphere enriched BCSCs [119] | ||
| Mitochondrial dynamics | Mitochondrial fission | Mdivi-1, DRP1 inhibitor | Reduces the percentages of SP+ and CD44+ CSC subpopulations, inhibits the expression of stemness genes, suppresses the formation capacity of tumorspheres in vitro and tumors in vivo, and decreases the ability of self-renewal | LCSCs [91]; NPC CSCs [120]; Ovarian CSCs and Colorectal CSCs [121]; Pancreatic CSCs [86]; CD133+CD15+BTICs [92]; EpCAM+CD133+ LCSCs [91] |
| Resveratrol, etodolac, celecoxib; selective COX-2 inhibitor | Reduces the expression levels of the stemness genes, the ratio of SP+ subpopulations, and the capacity for tumorsphere formation | NPC CSCs [120]; Bladder CSCs [122]; Glioblastoma CSCs [123]; | ||
| MFF | OTX015, BRD4 inhibitor | Suppresses tumorigenicity and self-renewal ability | Prostate CSCs [112] | |
| Furamidine, PRMT1 inhibitor | Blocks TBX19-induced mitochondrial fission, and decreases the capacity of tumorsphere formation and tumorigenesis | LCSCs [91] | ||
| Mitochondrial homeostasis | Mitochondrial mitophagy |
Combination of melatonin and verteporfin, PINK1/parkin signa lling pathway inhibitor |
Reduces the capacity of tumorsphere formation and the numbers of CD44+CD24− and CD133+ CSCs | HNSCC CSCs [124] |
| Mefloquine hydrochloride, lysosomes RAB5/7 inhibitor | Decreases the ratio of CD44v9+/CD133+ colon CSCs | CD44v9+/CD133+ Colon CSCs [125] | ||
| 188Re-liposome, nanomedicine, lysosomal proteins inhibitor | Reduces the protein levels of (Lamp-1 and cathepsin-B) and autophagy/mitophagy (LC3B, Atg16 L and Becline-1) markers, decreases tumor growth in xenograft mouse models, lowers CA-125 levels, and prolongs ovarian cancer patients’ survival in a clinical phase I trial | Ovarian CSCs [126, 127] | ||
| Mitochondrial biosynthesis | Azithromycin, doxycycline; Tigecycline, mitochondrial ribosome inhibitor | Targets the 39 s and 28 s mitochondrial ribosomes and inhibits tumorsphere formation, tumorigenicity and self-renewal ability | CSCs in breast, ovarian, lung, prostate, pancreatic cancer, melanoma, DCIS and GBM [128]; LSCs [129] | |
| SR-18292, selective PGC-1α inhibitor | Reduces tumorsphere formation, shrinks tumor size, and downregulates the expression of genes involved in stemness maintenance and self-renewal | sphere enriched CSCs in cholangiocarcinoma [116] | ||
| XCT790, ERRα-PGC1 signaling pathway inhibitor | Inhibits the formation of mammospheres and decreases the proportion, survival and propagation of CD44+CD24− BCSCs | BCSCs [100] | ||
| Mitochondrial ROS | Electron transport | Deferiprone, iron chelator | Decreases the proportions of tumorspheres and ALDH+ CSCs | BCSCs [130] |
| ROS-STAT3 signaling pathway | KS10076, metal chelator | Reduces the capacity for tumor formation, decreases the expression levels of CSC self-renewal genes, and decreases the ratios of subpopulations of ALDH+ or CD44highCD24low CSCs | Colon CSCs [131] | |
| 13 R, 20-diHDHA, dihydroxy-DHA derivative | Reduces the capacity for tumorsphere formation, decreases the expression levels of CSC self-renewal genes, and decreases the ratios of subpopulations of ALDH+ or CD44highCD24low BCSCs | sphere enriched BCSCs [132] | ||
| PAA, flower flavor | Reduces the capacity for tumorsphere formation and tumor formation, decreases the expression levels of CSC self-renewal genes, and decreases the ratios of subpopulations of ALDH+ or CD44+CD24− CSCs | sphere enriched BCSCs [133] | ||
| ROS-AKT signaling pathway | TiOxNPs, titanium peroxide nanoparticles | Sensitizes radioresistant CSCs to ionizing radiation, decreases tumorsphere number and CSC marker expression levels, reduces the pancreatic CSC self-renewal ability, decreases tumor growth rate and necrosis area, and improves of mouse survival rate | sphere enriched Pancreatic CSCs [134] |
Targeting mitochondrial energy metabolism
The well-known means of disrupting the maintenance of CSC features by interfering with mitochondrial energy metabolism is the inhibition of mitochondrial complex I of oxidative phosphorylation. One such example is the effective drug metformin, which downregulates the expression of CSC-related genes, decreases the ratios of CD44highALDHhigh cells as well as the sizes and numbers of tumorspheres, and thus reduces the volume of tumors in cholangiocarcinoma and head and neck squamous cell cancer (HNSCC) [116, 117] (Fig. 2B).
In addition, mitochondrial-derived metabolites are popular choices for targeting CSCs by interfering with mitochondrial energy metabolism. For example, SAM is the universal donor for DNA and histone methylation and has been linked to CSC self-renewal; therefore, decreasing SAM levels by blocking the methionine cycle key enzyme adenosyltransferase 2A (MAT2A) is considered an ideal strategy for eradicating CSCs. In lung cancer, it was reported that the MAT2A inhibitor FIDAS-5 strongly decreases the intracellular level of SAM and significantly inhibits the expression of methylation marks such as H3K4me3, H3K9me3, H3K27me3, H3K36me2, H3K36me3 and H3K79me3 in CSCs, thereby greatly lowering the tumorigenic potential of CSCs, which includes reducing the mass and volume of xenograft tumors and diminishing the size of NOD. Cg-Prkdcscid Il2rgtm1Wjl/SzJ mouse lung lesions and decreased the ratio of CD166+ CSCs [118] (Fig. 2B). Another MAT2A inhibitor, cycloleucine, has been found to enhance the suppressive effect of methionine depletion on BCSCs by inhibiting the protein expression of the stemness transcription factor SOX9 by suppressing the demethylation of H3K4me3 (Fig. 2B). In addition, the combination of MAT2A inhibition and methionine depletion could more effectively reduce mammospheres in vitro and the burden of primary and lung metastases in vivo [119].
Targeting mitochondrial dynamics
Some studies have found that inhibiting mitochondrial fission-related proteins may be another potential therapeutic strategy for targeting the stemness potential of CSCs. For example, knockdown of mitochondrial fission-related genes, such as DRP1, MFF, BRD4 or FIS1, reduces the expression levels of stemness genes and the capability of forming tumorspheres and tumors, especially the self-renewal of CSCs in brain, prostate and lung cancers [92, 112, 113] (Table 1).
For pharmacological intervention, Mdivi-1 is the most common and generally recognized DRP1-selective inhibitor that has been reported to reduce the percentage of SP+ or CD44+ CSC subpopulations, the expression of stemness genes, and the formation capacity of tumorspheres in vitro and in tumors in vivo in the context of nasopharyngeal carcinoma (NPC), liver cancer, ovarian cancer, etc. [86, 91, 120, 121] (Fig. 3B). Moreover, Mdivi-1 directly suppresses the function of CSCs that are isolated by stem cell markers. In detail, Mdivi-1 inhibits the self-renewal and tumor initiation capacities of CD133+CD15+ brain tumor-initiating cells (BTICs) [92] and decreases the levels of stemness genes in EpCAM+CD133+ liver cancer stem cells (LCSCs) [91]. As COX-2 maintains the CSC phenotype by activating DRP1, selective COX-2 inhibitors, such as resveratrol, celecoxib, and etodolac, are reported to reduce the expression levels of stemness genes, the ratio of SP+ subpopulations, and the tumorsphere formation capacity in NPC, bladder cancer, and glioblastoma [120, 122, 123] (Fig. 3B). In addition, BRD4 or PRMT1 can act as a transcription regulator or an epigenetic activator for MFF, respectively; therefore, targeting BRD4 or PRMT1 can be an attractive therapeutic option for eradicating CSCs by blocking mitochondrial fission. Therefore, the BRD4 inhibitor OTX015 suppresses tumorigenicity and self-renewal ability in prostate CSCs, and the PRMT1 inhibitor furamidine blocks TBX19-induced mitochondrial fission and decreases the capacity for tumorsphere formation and tumorigenesis in LCSCs [91].
Targeting mitophagy or mitochondrial biosynthesis.
Because mitophagy actively promotes the production of CSCs, targeting mitophagy-related genes could counteract CSCs. In AML, oral squamous cell cancer, and liver cancer, the knockdown of mitophagy-related regulator genes, such as PINK1, TBC1D15, ATG14, and BNIP3, decreases the levels of self-renewal and stemness, the number of tumorspheres, and the percentage of SP+ subpopulations [103, 114, 115] (Table 1).
Unfortunately, there are few reports on targeting CSCs by mitophagy-specific inhibitors but indirect mitophagy inhibition. For example, the combination of the circadian rhythm-regulating molecule melatonin and the YAP/TAZ inhibitor verteporfin was shown to decrease the expression of PINK1/parkin and then to reduce the capacity for tumorsphere formation and the numbers of CD44+CD24- and CD133+ CSCs in HNSCC [124] (Fig. 4B). However, some reports have revealed that targeting mitophagy-associated lysosomes could interfere with CSC function. As RAB5/7 (the regulators of early and late lysosome biogenesis) and LAMP1/2 (lysosomal/late endosomal marker and lysosomal receptor, respectively) were able to facilitate PINK1/parkin-dependent mitophagy, targeting RAB5/7 or LAMP1/2 could be a potential strategy for eradicating CSCs (Fig. 4B). Mefloquine hydrochloride, a novel RAB5/7 inhibitor, was reported to disrupt CD44v9+CD133+ colon CSCs by inhibiting lysosomal activity and mitophagy and thus could be a promising colorectal CSC-targeting drug [125] (Fig. 4B). In addition, the nanomedicine 188Re-liposome was shown to effectively suppress the expression of stemness markers and reduce the protein levels of lysosome (Lamp-1 and cathepsin-B) and autophagy/mitophagy (LC3B, Atg16L and Beclin-1) markers, which then resulted in decreased tumor growth in xenograft mouse models, lowered CA-125 levels and prolonged ovarian cancer patient survival in a clinical phase I trial [126, 127] (Fig. 4B).
In contrast to inhibitors of mitophagy, many antibiotics that inhibit mitochondrial biogenesis have become a prospective means of depleting CSCs. Azithromycin, doxycycline, and tigecycline, which target the 39S and 28S mitochondrial ribosomes, were shown to inhibit tumorsphere formation, tumorigenicity and self-renewal ability in breast cancer, AML, etc. [128, 129] (Fig. 4A). More specifically, drugs targeting PGC-1α and related genes are another attractive therapeutic choice for CSC elimination. SR-18292, a selective PGC-1α inhibitor, reduces tumorsphere formation, shrinks tumor size, and downregulates the expression of genes involved in stemness maintenance and self-renewal in cholangiocarcinoma [116] (Fig. 4A). XCT790, an ERRα inverse agonist, inhibits the formation of mammospheres in a concentration-dependent manner and decreases the percentage, survival and propagation of CD44+CD24- BCSCs [100] (Fig. 4A).
Induction of mitochondrial ROS production
CSCs maintain mitochondrial ROS at a low level; thus, inducing mitochondrial ROS is considered a novel option for anti-CSC-based therapy. Due to the critical roles of iron in electron transport and ROS generation, an iron chelator is considered a candidate for eradicating CSCs. FDA-approved deferiprone is such an example that dose-dependently decreases the tumorsphere numbers of CSCs and ALDH+ BCSCs by inducing mitochondrial ROS and is now being recommended for phase II clinical trials [130] (Fig. 5B). By inducing ROS-mediated STAT3 degradation or downregulation, the metal chelator KS10076, a novel dihydroxy-DHA derivative 13R, 20-dihydroxydocosahexaenoic acid (13 R, 20-diHDHA), and flower flavor phenylacetaldehyde (PAA) were reported to be potential agents for targeting CSCs by reducing the size of the tumorsphere and tumor formation, decreasing the expression of CSC self-renewal genes, and decreasing the ratios of subpopulations of ALDH+ or CD44highCD24low (CD44+CD24−) CSCs in colon and breast cancers [131–133] (Fig. 5B). In addition, by producing intolerable levels of ROS and inactivating AKT signaling, titanium peroxide nanoparticles (TiOxNPs) sensitize radioresistant CSCs to ionizing radiation through the decline of tumorsphere number and CSC marker expression and the reduction of pancreatic CSC self-renewal ability, which then leads to decreases in tumor growth rate and necrosis area while improving mouse survival rate [134] (Fig. 5B).
Conclusions and perspectives
Mitochondria have emerged as a regulatory hub of energy and signaling that can alter the fate of CSCs through the mito-nuclear communication process described above. Therefore, targeting mito-nuclear communication would eradicate CSCs and provide therapeutic benefits for cancer patients. To date, although a few studies that focus on blocking mito-nuclear communication have made great breakthroughs in inhibiting CSC potential, there are some challenges that still need to be overcome in the future.
First, the functional activities of the mitochondria are essential to both normal cells and CSCs. Thus, normal cells may be impaired by therapeutic agents that target mitochondria, which results in some side effects. However, the sensitivity of normal cells and CSCs to drugs may be different. More importantly, real-time monitoring of drug concentrations and metabolite levels would help to improve the specificity of targeting CSC agents and to reduce their toxicity to normal cells.
Second, during the process of tumorigenesis, the metabolic requirements of cancer cells change continuously. As these changes are caused by the input and changes in microenvironment signals, we need to target microenvironment signaling and CSCs together. Normal cells and CSCs may have different responses to changes in microenvironment signaling; thus, it is possible to eradicate CSCs while avoiding damaging normal cells.
Acknowledgements
We thank American Journal Experts for their professional editing and proofreading (W8ZY69GC).
Abbreviations
- CSCs
Cancer stem cells
- ROS
Reactive oxygen species
- TSCs
Tumor stem-like cells
- CICs
Cancer initiating cells
- TICs
Tumor-initiating cells
- MeCSC
Metastatic cancer stem cell
- CRCSC
Chemo-resistant cancer stem cell
- GBM
Glioblastoma
- GC
Gemcitabine and cisplatin
- PGE2
Prostaglandin E2
- BCSCs
Breast cancer stem cells
- EMT
Epithelial-to-mesenchymal transition
- MET
Mesenchymal-to-epithelial transition
- ALDH+
Aldehyde dehydrogenase positive
- HCC
Hepatocellular carcinoma
- TFs
Transcription factors
- GSCs
Glioblasoma stem cells
- ZHX2
Zinc-finger and homeoboxe 2
- mtDNA
Mitochondrial DNA
- acetyl-CoA
Acetyl-coenzyme A
- βHB
β-Hydroxybutyric acid
- SAM
S-adenosylmethionine
- α-KG
α-Ketoglutarate
- AML
Acute myeloid leukemia
- LSC
Leukemia stem cell
- TKI
Tyrosine kinase inhibitor
- DRP1
Dynamin-related protein 1
- MFF
Mitochondrial fission factor
- FIS1
Fission factor 1
- MFN1
Mitofusin 1
- MFN2
Mitofusin 2
- OPA1
Optic atrophy 1
- OXPHOS
Oxidative phosphorylation
- TBX19
T-box transcription factor 19
- SP
Side population
- CDK5
Cyclin-dependent kinase 5
- ERRα
Estrogen-Related Receptor α
- CCCP
Carbonyl cyanide m-chlorophenylhydrazone
- PINK1
PTEN-induced kinase 1
- Mdivi-1
Mitochondrial fission inhibitor
- AMPK
Adenosine 5'-monophos-phate-activated protein kinase
- CRC
Colorectal cancer
- NRF2
Nuclear factor erythroid-2-related factor 2
- NPC
Nasopharyngeal carcinoma
- BTICs
Brain tumor-initiating cells
- LCSCs
Liver cancer stem cells
- 13 R
20-DiHDHA: 13R: 20-dihydroxydocosahexaenoic acid
- MAT2A
Methionine adenosyltransferase 2A
- STAT3
Signal transducer and activator of transcription 3
- HNSCC
Head and neck squamous cell carcinoma
Authors’ contributions
Conceptualization, L.L. and Y.S.; writing-original draft preparation, M.F.; writing-review and editing, J.Z. and L.L.; supervision, L.L.; funding acquisition, L.L. and Y.S. All authors read and approved the final manuscript.
Funding
This work was supported by the National Natural Science Foundation of China (NSFC) [grant No. 31571469 & 81872349]; Key Project Program of the State Key Laboratory of Cancer Biology, Fourth Military Medical University [grant No. CBSKL2022ZZ09]; General Project of Natural Science Basic Research Program of Shaanxi [grant No. 2022JQ-874]; Science and Technology Innovation Team of Tumor Development and Antitumor Drug Development of Yan'an, and the Special Support Plan 'Regional Development Talents' Project of Shaanxi.
Availability of data and materials
Not applicable.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
All authors have given their consent for publication.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Mengchen Fan and Ying Shi contributed equally to this paper.
Contributor Information
Mengchen Fan, Email: fmc9966@163.com.
Ying Shi, Email: yingshi0703@163.com.
Jumei Zhao, Email: jmz2003.stu@163.com.
Ling Li, Email: liling25@fmmu.edu.cn.
References
- 1.Wang SY, Hu QC, Wu T, Xia J, Tao XA, Cheng B. Abnormal lipid synthesis as a therapeutic target for cancer stem cells. World j stem cells. 2022;14(2):146–162. doi: 10.4252/wjsc.v14.i2.146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Swati K, Agrawal K, Raj S, Kumar R, Prakash A, Kumar D. Molecular mechanism(s) of regulations of cancer stem cell in brain cancer propagation. Med Res Rev. 2023;43(3):441–463. doi: 10.1002/med.21930. [DOI] [PubMed] [Google Scholar]
- 3.Zhou HM, Zhang JG, Zhang X, Li Q. Targeting cancer stem cells for reversing therapy resistance: mechanism, signaling, and prospective agents. Signal Transduct Target Ther. 2021;6(1):62. doi: 10.1038/s41392-020-00430-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Paul S, Sinha S, Kundu CN. Targeting cancer stem cells in the tumor microenvironment: An emerging role of PARP inhibitors. Pharmacol Res. 2022;184:106425. doi: 10.1016/j.phrs.2022.106425. [DOI] [PubMed] [Google Scholar]
- 5.Shrestha S, Banstola A, Jeong JH, Seo JH, Yook S. Targeting Cancer Stem Cells: Therapeutic and di-agnostic strategies by the virtue of nanoparticles. J control release. 2022;348:518–536. doi: 10.1016/j.jconrel.2022.06.013. [DOI] [PubMed] [Google Scholar]
- 6.Sher G, Masoodi T, Patil K, et al. Dysregulated FOXM1 signaling in the regulation of cancer stem cells. Semin Cancer Biol. 2022;86:107–121. doi: 10.1016/j.semcancer.2022.07.009. [DOI] [PubMed] [Google Scholar]
- 7.Yang F, Cui P, Lu Y, Zhang X. Requirement of the transcription factor YB-1 for maintaining the stemness of cancer stem cells and reverting differentiated cancer cells into cancer stem cells. Stem Cell Res Ther. 2019;10(1):233. doi: 10.1186/s13287-019-1360-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Luo M, Wicha MS. Targeting Cancer Stem Cell Redox Metabolism to Enhance Therapy Responses. Semin Radiat Oncol. 2019;29(1):42–54. doi: 10.1016/j.semradonc.2018.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cao Z, Scandura JM, Inghirami GG, Shido K, Ding BS, Rafii S. Molecular Checkpoint Decisions Made by Subverted Vascular Niche Transform Indolent Tumor Cells into Chemoresistant Cancer Stem Cells. Cancer Cell. 2017;31(1):110–126. doi: 10.1016/j.ccell.2016.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Qian Y, Zhang L, Cai M, et al. The prostate cancer risk variant rs55958994 regulates multiple gene ex-pression through extreme long-range chromatin interaction to control tumor progression. Sci Adv. 2019;5(7):eaaw6710. doi: 10.1126/sciadv.aaw6710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wang C, Shao L, Pan C, et al. Elevated level of mitochondrial reactive oxygen species via fatty acid β-oxidation in cancer stem cells promotes cancer metastasis by inducing epithelial-mesenchymal transi-tion. Stem Cell Res Ther. 2019;10(1):175. doi: 10.1186/s13287-019-1265-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bonnet D, Dick JE. Human acute myeloid leukemia is organized as a hierarchy that originates from a primitive hematopoietic cell. Nat Med. 1997;3(7):730–737. doi: 10.1038/nm0797-730. [DOI] [PubMed] [Google Scholar]
- 13.Vaiopoulos AG, Kostakis ID, Koutsilieris M, Papavassiliou AG. Colorectal cancer stem cells. Stem cells. 2012;30(3):363–371. doi: 10.1002/stem.1031. [DOI] [PubMed] [Google Scholar]
- 14.Al-Hajj M, Wicha MS, Benito-Hernandez A, Morrison SJ, Clarke MF. Prospective identification of tumorigenic breast cancer cells. Proc Natl Acad Sci USA. 2003;100(7):3983–3988. doi: 10.1073/pnas.0530291100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Han J, Fujisawa T, Husain SR, Puri RK. Identification and characterization of cancer stem cells in human head and neck squamous cell carcinoma. BMC Cancer. 2014;14:173. doi: 10.1186/1471-2407-14-173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Singh SK, Clarke ID, Terasaki M, et al. Identification of a cancer stem cell in human brain tumors. Cancer Res. 2003;63(18):5821–5828. [PubMed] [Google Scholar]
- 17.Baccelli I, Trumpp A. The evolving concept of cancer and metastasis stem cells. J Cell Biol. 2012;198(3):281–293. doi: 10.1083/jcb.201202014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Thankamony AP, Saxena K, Murali R, Jolly MK, Nair R. Cancer Stem Cell Plasticity - A Deadly Deal. Front Mol Biosci. 2020;7:79. doi: 10.3389/fmolb.2020.00079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Yang Q, Zhao S, Shi Z, et al. Chemotherapy-elicited exosomal miR-378a-3p and miR-378d promote breast cancer stemness and chemoresistance via the activation of EZH2/STAT3 signaling. J Exp Clin Cancer Res. 2021;40(1):120. doi: 10.1186/s13046-021-01901-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Shen M, Dong C, Ruan X, et al. Chemotherapy-Induced Extracellular Vesicle miRNAs Promote Breast Cancer Stemness by Targeting ONECUT2. Cancer Res. 2019;79(14):3608–3621. doi: 10.1158/0008-5472.CAN-18-4055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Liu L, Yang L, Yan W, et al. Chemotherapy Induces Breast Cancer Stemness in Association with Dysregulated Monocytosis. Clin cancer res. 2018;24(10):2370–2382. doi: 10.1158/1078-0432.CCR-17-2545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Arnold KM, Opdenaker LM, Flynn NJ, Appeah DK, Sims-Mourtada J. Radiation induces an inflam-matory response that results in STAT3-dependent changes in cellular plasticity and radioresistance of breast cancer stem-like cells. Int J Radiat Biol. 2020;96(4):434–447. doi: 10.1080/09553002.2020.1705423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chen S, Zhang J, Chen J, et al. RER1 enhances carcinogenesis and stemness of pancreatic cancer under hypoxic environment. J Exp Clin Cancer Res. 2019;38(1):15. doi: 10.1186/s13046-018-0986-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Meng Y, Fan XY, Yang LJ, et al. Detachment Activated CyPA/CD147 Induces Cancer Stem Cell Po-tential in Non-stem Breast Cancer Cells. Front Cell Dev Biol. 2020;8:543856. doi: 10.3389/fcell.2020.543856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mello T, Simeone I, Galli A. Mito-Nuclear Communication in Hepatocellular Carcinoma Metabolic Rewiring. Cells. 2019;8(5):417. doi: 10.3390/cells8050417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Li H, Feng Z, He ML. Lipid metabolism alteration contributes to and maintains the properties of cancer stem cells. Theranostics. 2020;10(16):7053–7069. doi: 10.7150/thno.41388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Qi W, Liang W, Jiang H, Miuyee WM. The function of miRNA in hepatic cancer stem cell. Biomed Res Int. 2013;2013:358902. doi: 10.1155/2013/358902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Naz F, Shi M, Sajid S, Yang Z, Yu C. Cancer stem cells: a major culprit of intra-tumor heterogeneity. Am J Cancer Res. 2021;11(12):5782–5811. [PMC free article] [PubMed] [Google Scholar]
- 29.Kapoor-Narula U, Lenka N. Cancer stem cells and tumor heterogeneity: Deciphering the role in tumor progression and metastasis. Cytokine. 2022;157:155968. doi: 10.1016/j.cyto.2022.155968. [DOI] [PubMed] [Google Scholar]
- 30.Zeng X, Liu C, Yao J, et al. Breast cancer stem cells, heterogeneity, targeting therapies and therapeutic implications. Pharmacol Res. 2021;163:105320. doi: 10.1016/j.phrs.2020.105320. [DOI] [PubMed] [Google Scholar]
- 31.Olivares-Urbano MA, Griñán-Lisón C, Marchal JA, Núñez MI. CSC Radioresistance: A Therapeutic Challenge to Improve Radiotherapy Effectiveness in Cancer. Cells. 2020;9(7):1651. doi: 10.3390/cells9071651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sarnella A, D'Avino G, Hill BS, et al. A Novel Inhibitor of Carbonic Anhydrases Prevents Hypox-ia-Induced TNBC Cell Plasticity. Int J Mol Sci. 2020;21(21):8405. doi: 10.3390/ijms21218405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ma SKY, Chan ASF, Rubab A, Chan WCW, Chan D. Extracellular Matrix and Cellular Plasticity in Musculoskeletal Development. Front Cell Dev Biol. 2020;8:781. doi: 10.3389/fcell.2020.00781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Paul R, Dorsey JF, Fan Y. Cell plasticity, senescence, and quiescence in cancer stem cells: Biological and therapeutic implications. Pharmacol Ther. 2021;231:107985. doi: 10.1016/j.pharmthera.2021.107985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Batlle E, Clevers H. Cancer stem cells revisited. Nat Med. 2017;23(10):1124–1134. doi: 10.1038/nm.4409. [DOI] [PubMed] [Google Scholar]
- 36.Kurtova AV, Xiao J, Mo Q, et al. Blocking PGE2-induced tumour repopulation abrogates bladder cancer chemoresistance. Nature. 2015;517(7533):209–213. doi: 10.1038/nature14034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Agarwal P, Isringhausen S, Li H, et al. Mesenchymal Niche-Specific Expression of Cxcl12 Controls Quiescence of Treatment-Resistant Leukemia Stem Cells. Cell Stem Cell. 2019;24(5):769–84.e766. doi: 10.1016/j.stem.2019.02.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Biddle A, Liang X, Gammon L, et al. Cancer stem cells in squamous cell carcinoma switch between two distinct phenotypes that are preferentially migratory or proliferative. Cancer Res. 2011;71(15):5317–5326. doi: 10.1158/0008-5472.CAN-11-1059. [DOI] [PubMed] [Google Scholar]
- 39.Liu S, Cong Y, Wang D, et al. Breast cancer stem cells transition between epithelial and mesenchymal states reflective of their normal counterparts. Stem cell reports. 2014;2(1):78–91. doi: 10.1016/j.stemcr.2013.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ibragimova M, Tsyganov M, Litviakov N. Tumour stem cells in breast cancer. Int J Mol Sci. 2022;23(9):5058. [DOI] [PMC free article] [PubMed]
- 41.Das PK, Pillai S, Rakib MA, et al. Plasticity of Cancer Stem Cell: Origin and Role in Disease Progression and Therapy Resistance. Stem cell rev rep. 2020;16(2):397–412. doi: 10.1007/s12015-019-09942-y. [DOI] [PubMed] [Google Scholar]
- 42.Chen X, Liao R, Li D, Sun J. Induced cancer stem cells generated by radiochemotherapy and their therapeutic implications. Oncotarget. 2017;8(10):17301–17312. doi: 10.18632/oncotarget.14230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Iliopoulos D, Hirsch HA, Wang G, Struhl K. Inducible formation of breast cancer stem cells and their dynamic equilibrium with non-stem cancer cells via IL6 secretion. Proc Natl Acad Sci USA. 2011;108(4):1397–1402. doi: 10.1073/pnas.1018898108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Zhang H, Brown RL, Wei Y, et al. CD44 splice isoform switching determines breast cancer stem cell state. Genes Dev. 2019;33(3–4):166–179. doi: 10.1101/gad.319889.118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ganesh K, Massagué J. Targeting metastatic cancer. Nat Med. 2021;27(1):34–44. doi: 10.1038/s41591-020-01195-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Hermann PC, Huber SL, Herrler T, et al. Distinct populations of cancer stem cells determine tumor growth and metastatic activity in human pancreatic cancer. Cell Stem Cell. 2007;1(3):313–323. doi: 10.1016/j.stem.2007.06.002. [DOI] [PubMed] [Google Scholar]
- 47.Todaro M, Gaggianesi M, Catalano V, et al. CD44v6 is a marker of constitutive and reprogrammed cancer stem cells driving colon cancer metastasis. Cell Stem Cell. 2014;14(3):342–356. doi: 10.1016/j.stem.2014.01.009. [DOI] [PubMed] [Google Scholar]
- 48.Pang R, Law WL, Chu AC, et al. A subpopulation of CD26+ cancer stem cells with metastatic capacity in human colorectal cancer. Cell Stem Cell. 2010;6(6):603–615. doi: 10.1016/j.stem.2010.04.001. [DOI] [PubMed] [Google Scholar]
- 49.Liu H, Patel MR, Prescher JA, et al. Cancer stem cells from human breast tumors are involved in spon-taneous metastases in orthotopic mouse models. Proc Natl Acad Sci USA. 2010;107(42):18115–18120. doi: 10.1073/pnas.1006732107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Dubrovska A, Elliott J, Salamone RJ, et al. CXCR4 expression in prostate cancer progenitor cells. PLoS ONE. 2012;7(2):e31226. doi: 10.1371/journal.pone.0031226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Liu CL, Chen YJ, Fan MH, Liao YJ, Mao TL. Characteristics of CD133-Sustained Chemoresistant Cancer Stem-Like Cells in Human Ovarian Carcinoma. Int J Mol Sci. 2020;21(18):6467. doi: 10.3390/ijms21186467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Zheng X, Yu C, Xu M. Linking Tumor Microenvironment to Plasticity of Cancer Stem Cells: Mecha-nisms and Application in Cancer Therapy. Front Oncol. 2021;11:678333. doi: 10.3389/fonc.2021.678333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Wainwright EN, Scaffidi P. Epigenetics and Cancer Stem Cells: Unleashing, Hijacking, and Restricting Cellular Plasticity. Trends in cancer. 2017;3(5):372–386. doi: 10.1016/j.trecan.2017.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Suvà ML, Rheinbay E, Gillespie SM, et al. Reconstructing and reprogramming the tumor-propagating potential of glioblastoma stem-like cells. Cell. 2014;157(3):580–594. doi: 10.1016/j.cell.2014.02.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Chen B, McCuaig-Walton D, Tan S, et al. DYRK1A Negatively Regulates CDK5-SOX2 Pathway and Self-Renewal of Glioblastoma Stem Cells. Int J Mol Sci. 2021;22(8):4011. doi: 10.3390/ijms22084011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Chen X, Huan H, Liu C, et al. Deacetylation of β-catenin by SIRT1 regulates self-renewal and onco-genesis of liver cancer stem cells. Cancer Lett. 2019;463:1–10. doi: 10.1016/j.canlet.2019.07.021. [DOI] [PubMed] [Google Scholar]
- 57.Lin Q, Wu Z, Yue X, et al. ZHX2 restricts hepatocellular carcinoma by suppressing stem cell-like traits through KDM2A-mediated H3K36 demethylation. EBioMedicine. 2020;53:102676. doi: 10.1016/j.ebiom.2020.102676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Tatapudy S, Aloisio F, Barber D, Nystul T. Cell fate decisions: emerging roles for metabolic signals and cell morphology. EMBO Rep. 2017;18(12):2105–2118. doi: 10.15252/embr.201744816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Stadhouders R, Filion GJ, Graf T. Transcription factors and 3D genome conformation in cell-fate deci-sions. Nature. 2019;569(7756):345–354. doi: 10.1038/s41586-019-1182-7. [DOI] [PubMed] [Google Scholar]
- 60.Genovese I, Vezzani B, Danese A, et al. Mitochondria as the decision makers for cancer cell fate: from signaling pathways to therapeutic strategies. Cell Calcium. 2020;92:102308. doi: 10.1016/j.ceca.2020.102308. [DOI] [PubMed] [Google Scholar]
- 61.Filippi MD, Ghaffari S. Mitochondria in the maintenance of hematopoietic stem cells: new perspectives and opportunities. Blood. 2019;133(18):1943–1952. doi: 10.1182/blood-2018-10-808873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Chiu HY, Tay EXY, Ong DST, Taneja R. Mitochondrial Dysfunction at the Center of Cancer Therapy. Antioxid Redox Signal. 2020;32(5):309–330. doi: 10.1089/ars.2019.7898. [DOI] [PubMed] [Google Scholar]
- 63.Bahat A, Gross A. Mitochondrial plasticity in cell fate regulation. J Biol Chem. 2019;294(38):13852–13863. doi: 10.1074/jbc.REV118.000828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Mohareer K, Medikonda J, Vadankula GR, Banerjee S. Mycobacterial Control of Host Mitochondria: Bioenergetic and Metabolic Changes Shaping Cell Fate and Infection Outcome. Front Cell Infect Microbiol. 2020;10:457. doi: 10.3389/fcimb.2020.00457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Skoda J, Borankova K, Jansson PJ, Huang ML, Veselska R, Richardson DR. Pharmacological targeting of mitochondria in cancer stem cells: An ancient organelle at the crossroad of novel anti-cancer therapies. Pharmacol Res. 2019;139:298–313. doi: 10.1016/j.phrs.2018.11.020. [DOI] [PubMed] [Google Scholar]
- 66.Vasconcelos ESJ, Simão D, Terrasso AP, et al. Unveiling dynamic metabolic signatures in human in-duced pluripotent and neural stem cells. PLoS Comput Biol. 2020;16(4):e1007780. doi: 10.1371/journal.pcbi.1007780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Walker BR, Moraes CT. Nuclear-mitochondrial interactions. Biomolecules. 2022;12(3):427. [DOI] [PMC free article] [PubMed]
- 68.Ludikhuize MC, Meerlo M, Gallego MP, et al. Mitochondria Define Intestinal Stem Cell Differentiation Downstream of a FOXO/Notch Axis. Cell Metab. 2020;32(5):889–900.e887. doi: 10.1016/j.cmet.2020.10.005. [DOI] [PubMed] [Google Scholar]
- 69.English J, Son JM, Cardamone MD, Lee C, Perissi V. Decoding the rosetta stone of mitonuclear com-munication. Pharmacol Res. 2020;161:105161. doi: 10.1016/j.phrs.2020.105161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Mottis A, Herzig S, Auwerx J. Mitocellular communication: Shaping health and disease. Science. 2019;366(6467):827–832. doi: 10.1126/science.aax3768. [DOI] [PubMed] [Google Scholar]
- 71.Quiros PM, Mottis A, Auwerx J. Mitonuclear communication in homeostasis and stress. Nat Rev Mol Cell Biol. 2016;17(4):213–226. doi: 10.1038/nrm.2016.23. [DOI] [PubMed] [Google Scholar]
- 72.Chakrabarty RP, Chandel NS. Mitochondria as Signaling Organelles Control Mammalian Stem Cell Fate. Cell Stem Cell. 2021;28(3):394–408. doi: 10.1016/j.stem.2021.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Egan G, Khan DH, Lee JB, Mirali S, Zhang L, Schimmer AD. Mitochondrial and Metabolic Pathways Regulate Nuclear Gene Expression to Control Differentiation, Stem Cell Function, and Immune Re-sponse in Leukemia. Cancer Discov. 2021;11(5):1052–1066. doi: 10.1158/2159-8290.CD-20-1227. [DOI] [PubMed] [Google Scholar]
- 74.Zhang Q, Li W. Correlation between amino acid metabolism and self-renewal of cancer stem cells: Perspectives in cancer therapy. World j stem cells. 2022;14(4):267–286. doi: 10.4252/wjsc.v14.i4.267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Menendez JA. Metabolic control of cancer cell stemness: Lessons from iPS cells. Cell cycle. 2015;14(24):3801–3811. doi: 10.1080/15384101.2015.1022697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Chen F. Linking metabolism to epigenetics in stem cells and cancer stem cells. Semin Cancer Biol. 2019;57:iii–v. doi: 10.1016/j.semcancer.2019.05.005. [DOI] [PubMed] [Google Scholar]
- 77.Martínez-Reyes I, Chandel NS. Mitochondrial TCA cycle metabolites control physiology and disease. Nat Commun. 2020;11(1):102. doi: 10.1038/s41467-019-13668-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Sun L, Zhang H, Gao P. Metabolic reprogramming and epigenetic modifications on the path to cancer. Protein Cell. 2022;13(12):877–919. doi: 10.1007/s13238-021-00846-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Yang D, Peng M, Hou Y, et al. Oxidized ATM promotes breast cancer stem cell enrichment through energy metabolism reprogram-mediated acetyl-CoA accumulation. Cell Death Dis. 2020;11(7):508. doi: 10.1038/s41419-020-2714-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Zhang H, Chang Z, Qin LN, et al. MTA2 triggered R-loop trans-regulates BDH1-mediated β-hydroxybutyrylation and potentiates propagation of hepatocellular carcinoma stem cells. Signal Transduct Target Ther. 2021;6(1):135. doi: 10.1038/s41392-021-00464-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Singh RP, Jeyaraju DV, Voisin V, et al. Disrupting Mitochondrial Copper Distribution Inhibits Leukemic Stem Cell Self-Renewal. Cell Stem Cell. 2020;26(6):926–37.e910. doi: 10.1016/j.stem.2020.04.010. [DOI] [PubMed] [Google Scholar]
- 82.Miwa S, Kashyap S, Chini E, von Zglinicki T. Mitochondrial dysfunction in cell senescence and aging. J Clin Investig. 2022;132(13):e158447. doi: 10.1172/JCI158447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Du F, Yu Q, Yan S, et al. PINK1 signalling rescues amyloid pathology and mitochondrial dysfunction in Alzheimer's disease. Brain. 2017;140(12):3233–3251. doi: 10.1093/brain/awx258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Sessions DT, Kashatus DF. Mitochondrial dynamics in cancer stem cells. Cell mol life sci. 2021;78(8):3803–3816. doi: 10.1007/s00018-021-03773-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Lee JH, Mourkioti F. Fission impossible: Mitochondrial dynamics direct muscle stem cell fates. Cell Stem Cell. 2022;29(9):1287–1289. doi: 10.1016/j.stem.2022.08.010. [DOI] [PubMed] [Google Scholar]
- 86.Courtois S, de Luxán-Delgado B, Penin-Peyta L, et al. Inhibition of Mitochondrial Dynamics Preferen-tially Targets Pancreatic Cancer Cells with Enhanced Tumorigenic and Invasive Potential. Cancers. 2021;13(4):698. doi: 10.3390/cancers13040698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.van der Bliek AM, Shen Q, Kawajiri S. Mechanisms of mitochondrial fission and fusion. Cold Spring Harb Perspect Biol. 2013;5(6):a011072. [DOI] [PMC free article] [PubMed]
- 88.Wang S, Tan J, Miao Y, Zhang Q. Mitochondrial Dynamics, Mitophagy, and Mitochondria-Endoplasmic Reticulum Contact Sites Crosstalk Under Hypoxia. Front Cell Dev Biol. 2022;10:848214. doi: 10.3389/fcell.2022.848214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Bonnay F, Veloso A, Steinmann V, et al. Oxidative Metabolism Drives Immortalization of Neural Stem Cells during Tumorigenesis. Cell. 2020;182(6):1490–1507 e1419. doi: 10.1016/j.cell.2020.07.039. [DOI] [PubMed] [Google Scholar]
- 90.Chen H, Chan DC. Mitochondrial Dynamics in Regulating the Unique Phenotypes of Cancer and Stem Cells. Cell Metab. 2017;26(1):39–48. doi: 10.1016/j.cmet.2017.05.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Tang M, Yang M, Wu G, et al. Epigenetic Induction of Mitochondrial Fission Is Required for Mainte-nance of Liver Cancer-Initiating Cells. Cancer Res. 2021;81(14):3835–3848. doi: 10.1158/0008-5472.CAN-21-0436. [DOI] [PubMed] [Google Scholar]
- 92.Xie Q, Wu Q, Horbinski CM, et al. Mitochondrial control by DRP1 in brain tumor initiating cells. Nat Neurosci. 2015;18(4):501–510. doi: 10.1038/nn.3960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Sánchez-Alvarez R, De Francesco EM, Fiorillo M, Sotgia F, Lisanti MP. Mitochondrial Fission Factor (MFF) Inhibits Mitochondrial Metabolism and Reduces Breast Cancer Stem Cell (CSC) Activity. Front oncol. 2020;10:1776. doi: 10.3389/fonc.2020.01776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Liu L, Li Y, Wang J, et al. Mitophagy receptor FUNDC1 is regulated by PGC-1α/NRF1 to fine tune mitochondrial homeostasis. EMBO Rep. 2021;22(3):e50629. doi: 10.15252/embr.202050629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Roberts FL, Markby GR. New Insights into Molecular Mechanisms Mediating Adaptation to Exercise; A Review Focusing on Mitochondrial Biogenesis, Mitochondrial Function, Mitophagy and Autophagy. Cells. 2021;10(10):2639. doi: 10.3390/cells10102639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Praharaj PP, Panigrahi DP, Bhol CS, et al. Mitochondrial rewiring through mitophagy and mitochondrial biogenesis in cancer stem cells: A potential target for anti-CSC cancer therapy. Cancer Lett. 2021;498:217–228. doi: 10.1016/j.canlet.2020.10.036. [DOI] [PubMed] [Google Scholar]
- 97.Poole LP, Macleod KF. Mitophagy in tumorigenesis and metastasis. Cell mol life sci. 2021;78(8):3817–3851. doi: 10.1007/s00018-021-03774-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Ma K, Chen G, Li W, Kepp O, Zhu Y, Chen Q. Mitophagy, Mitochondrial Homeostasis, and Cell Fate. Front Cell Dev Biol. 2020;8:467. doi: 10.3389/fcell.2020.00467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Sancho P, Burgos-Ramos E, Tavera A, et al. MYC/PGC-1α Balance Determines the Metabolic Phenotype and Plasticity of Pancreatic Cancer Stem Cells. Cell Metab. 2015;22(4):590–605. doi: 10.1016/j.cmet.2015.08.015. [DOI] [PubMed] [Google Scholar]
- 100.De Luca A, Fiorillo M, Peiris-Pagès M, et al. Mitochondrial biogenesis is required for the anchor-age-independent survival and propagation of stem-like cancer cells. Oncotarget. 2015;6(17):14777–14795. doi: 10.18632/oncotarget.4401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Bruns I, Sauer B, Burger MC, et al. Disruption of peroxisome proliferator-activated receptor γ coactivator (PGC)-1α reverts key features of the neoplastic phenotype of glioma cells. J Biol Chem. 2019;294(9):3037–3050. doi: 10.1074/jbc.RA118.006993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Whelan KA, Chandramouleeswaran PM, Tanaka K, et al. Autophagy supports generation of cells with high CD44 expression via modulation of oxidative stress and Parkin-mediated mitochondrial clearance. Oncogene. 2017;36(34):4843–4858. doi: 10.1038/onc.2017.102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Pei S, Minhajuddin M, Adane B, et al. AMPK/FIS1-Mediated Mitophagy Is Required for Self-Renewal of Human AML Stem Cells. Cell Stem Cell. 2018;23(1):86–100.e106. doi: 10.1016/j.stem.2018.05.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Liu K, Lee J, Kim JY, et al. Mitophagy Controls the Activities of Tumor Suppressor p53 to Regulate Hepatic Cancer Stem Cells. Mol Cell. 2017;68(2):281–92.e285. doi: 10.1016/j.molcel.2017.09.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Jovanović M, Podolski-Renić A, Krasavin M, Pešić M. The Role of the Thioredoxin Detoxification System in Cancer Progression and Resistance. Front Mol Biosci. 2022;9:883297. doi: 10.3389/fmolb.2022.883297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Glasauer A, Chandel NSROS. Curr Biol. 2013;23(3):R100–R102. doi: 10.1016/j.cub.2012.12.011. [DOI] [PubMed] [Google Scholar]
- 107.Myant KB, Cammareri P, McGhee EJ, et al. ROS production and NF-κB activation triggered by RAC1 facilitate WNT-driven intestinal stem cell proliferation and colorectal cancer initiation. Cell Stem Cell. 2013;12(6):761–773. doi: 10.1016/j.stem.2013.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Zhong G, Qin S, Townsend D, Schulte BA, Tew KD, Wang GY. Oxidative stress induces senescence in breast cancer stem cells. Biochem Biophys Res Commun. 2019;514(4):1204–1209. doi: 10.1016/j.bbrc.2019.05.098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Culp-Hill R, D'Alessandro A, Pietras EM. Extinguishing the Embers: Targeting AML Metabolism. Trends Mol Med. 2021;27(4):332–344. doi: 10.1016/j.molmed.2020.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Yang Q, Li K, Huang X, et al. lncRNA SLC7A11-AS1 Promotes Chemoresistance by Blocking SCF(β-TRCP)-Mediated Degradation of NRF2 in Pancreatic Cancer. Mol Ther Nucleic Acids. 2020;19:974–985. doi: 10.1016/j.omtn.2019.11.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Huang H, Zhang S, Li Y, et al. Suppression of mitochondrial ROS by prohibitin drives glioblastoma progression and therapeutic resistance. Nat Commun. 2021;12(1):3720. doi: 10.1038/s41467-021-24108-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Civenni G, Bosotti R, Timpanaro A, et al. Epigenetic Control of Mitochondrial Fission Enables Self-Renewal of Stem-like Tumor Cells in Human Prostate Cancer. Cell Metab. 2019;30(2):303–18.e306. doi: 10.1016/j.cmet.2019.05.004. [DOI] [PubMed] [Google Scholar]
- 113.Liu D, Sun Z, Ye T, et al. The mitochondrial fission factor FIS1 promotes stemness of human lung cancer stem cells via mitophagy. FEBS Open Bio. 2021;11(7):1997–2007. doi: 10.1002/2211-5463.13207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Naik PP, Mukhopadhyay S, Panda PK, et al. Autophagy regulates cisplatin-induced stemness and chemoresistance via the upregulation of CD44, ABCB1 and ADAM17 in oral squamous cell carcinoma. Cell Prolif. 2018;51(1):e12411. doi: 10.1111/cpr.12411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Chen YY, Wang WH, Che L, et al. BNIP3L-Dependent Mitophagy Promotes HBx-Induced Cancer Stemness of Hepatocellular Carcinoma Cells via Glycolysis Metabolism Reprogramming. Cancers. 2020;12(3):655. doi: 10.3390/cancers12030655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Raggi C, Taddei ML, Sacco E, et al. Mitochondrial oxidative metabolism contributes to a cancer stem cell phenotype in cholangiocarcinoma. J Hepatol. 2021;74(6):1373–1385. doi: 10.1016/j.jhep.2020.12.031. [DOI] [PubMed] [Google Scholar]
- 117.Wu X, Yeerna H, Goto Y, et al. Metformin Inhibits Progression of Head and Neck Squamous Cell Car-cinoma by Acting Directly on Carcinoma-Initiating Cells. Cancer Res. 2019;79(17):4360–4370. doi: 10.1158/0008-5472.CAN-18-3525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Wang Z, Yip LY, Lee JHJ, et al. Methionine is a metabolic dependency of tumor-initiating cells. Nat Med. 2019;25(5):825–837. doi: 10.1038/s41591-019-0423-5. [DOI] [PubMed] [Google Scholar]
- 119.Strekalova E, Malin D, Weisenhorn EMM, et al. S-adenosylmethionine biosynthesis is a targetable metabolic vulnerability of cancer stem cells. Breast Cancer Res Treat. 2019;175(1):39–50. doi: 10.1007/s10549-019-05146-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Zhou TJ, Zhang SL, He CY, et al. Downregulation of mitochondrial cyclooxygenase-2 inhibits the stemness of nasopharyngeal carcinoma by decreasing the activity of dynamin-related protein 1. Theranostics. 2017;7(5):1389–1406. doi: 10.7150/thno.17647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Prasad P, Ghosh S, Roy SS. Glutamine deficiency promotes stemness and chemoresistance in tumor cells through DRP1-induced mitochondrial fragmentation. Cell mol life sci. 2021;78(10):4821–4845. doi: 10.1007/s00018-021-03818-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Ooki A, Del Carmen Rodriguez Pena M, Marchionni L, et al. YAP1 and COX2 Coordinately Regulate Urothelial Cancer Stem-like Cells. Cancer Res. 2018;78(1):168–81. doi: 10.1158/0008-5472.CAN-17-0836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Wu M, Guan J, Li C, et al. Aberrantly activated Cox-2 and Wnt signaling interact to maintain cancer stem cells in glioblastoma. Oncotarget. 2017;8(47):82217–82230. doi: 10.18632/oncotarget.19283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Shin YY, Seo Y, Oh SJ, et al. Melatonin and verteporfin synergistically suppress the growth and stemness of head and neck squamous cell carcinoma through the regulation of mitochondrial dynamics. J Pineal Res. 2022;72(1):e12779. doi: 10.1111/jpi.12779. [DOI] [PubMed] [Google Scholar]
- 125.Takeda M, Koseki J, Takahashi H, et al. Disruption of Endolysosomal RAB5/7 Efficiently Eliminates Colorectal Cancer Stem Cells. Cancer Res. 2019;79(7):1426–1437. doi: 10.1158/0008-5472.CAN-18-2192. [DOI] [PubMed] [Google Scholar]
- 126.Chang CM, Lan KL, Huang WS, et al. (188)Re-Liposome Can Induce Mitochondrial Autophagy and Reverse Drug Resistance for Ovarian Cancer: From Bench Evidence to Preliminary Clinical Proof-of-Concept. Int J Mol Sci. 2017;18(5):903. doi: 10.3390/ijms18050903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Shen YA, Lan KL, Chang CH, et al. Intraperitoneal (188)Re-Liposome delivery switches ovarian cancer metabolism from glycolysis to oxidative phosphorylation and effectively controls ovarian tumour growth in mice. Radiother oncol. 2016;119(2):282–290. doi: 10.1016/j.radonc.2016.02.007. [DOI] [PubMed] [Google Scholar]
- 128.Lamb R, Ozsvari B, Lisanti CL, et al. Antibiotics that target mitochondria effectively eradicate cancer stem cells, across multiple tumor types: treating cancer like an infectious disease. Oncotarget. 2015;6(7):4569–4584. doi: 10.18632/oncotarget.3174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Skrtić M, Sriskanthadevan S, Jhas B, et al. Inhibition of mitochondrial translation as a therapeutic strategy for human acute myeloid leukemia. Cancer Cell. 2011;20(5):674–688. doi: 10.1016/j.ccr.2011.10.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Fiorillo M, Tóth F, Brindisi M, Sotgia F, Lisanti MP. Deferiprone (DFP) Targets Cancer Stem Cell (CSC) Propagation by Inhibiting Mitochondrial Metabolism and Inducing ROS Production. Cells. 2020;9(6):1529. doi: 10.3390/cells9061529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Kim J, Park A, Hwang J, et al. KS10076, a chelator for redox-active metal ions, induces ROS-mediated STAT3 degradation in autophagic cell death and eliminates ALDH1(+) stem cells. Cell Rep. 2022;40(3):111077. doi: 10.1016/j.celrep.2022.111077. [DOI] [PubMed] [Google Scholar]
- 132.Wang L, Choi HS, Lee B, Choi JH, Jang YS, Seo JW. 13R,20-Dihydroxydocosahexaenoic Acid, a Novel Dihydroxy- DHA Derivative, Inhibits Breast Cancer Stemness through Regulation of the Stat3/IL-6 Signaling Pathway by Inducing ROS Production. Antioxidants. 2021;10(3):457. doi: 10.3390/antiox10030457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Choi HS, Kim SL, Kim JH, Ko YC, Lee DS. Plant Volatile, Phenylacetaldehyde Targets Breast Cancer Stem Cell by Induction of ROS and Regulation of Stat3 Signal. Antioxidants. 2020;9(11):1119. doi: 10.3390/antiox9111119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Salah M, Akasaka H, Shimizu Y, et al. Reactive oxygen species-inducing titanium peroxide nanoparticles as promising radiosensitizers for eliminating pancreatic cancer stem cells. J Exp Clin Cancer Res. 2022;41(1):146. doi: 10.1186/s13046-022-02358-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.