Abstract
Multiple dietary patterns have been associated with different diseases; however, their comparability to improve overall health is yet to be determined. In 205,852 healthcare professionals from three US cohorts followed for up to 32 years, we prospectively assessed two mechanism-based diets and six diets based on dietary recommendations in relation to major chronic disease, defined as a composite outcome of incident major cardiovascular disease, type 2 diabetes, and cancer. We demonstrated that adherence to a healthy diet was generally associated with a lower risk of major chronic disease (hazard ratio [HR] comparing the 90th to 10th percentile of dietary pattern scores: 0.58–0.80). Participants with low insulinemic (HR 0.58, 95% confidence interval [CI] 0.57, 0.60), low inflammatory (HR 0.61, 95% CI 0.60, 0.63), or diabetes risk-reducing diet (HR 0.70, 95% CI 0.69, 0.72) had the largest risk reduction for incident major cardiovascular disease, type 2 diabetes, and cancer in composite and individually. Similar findings were observed across sex, and diverse ethnic groups. Our results suggest that dietary patterns that are associated with markers of hyperinsulinemia and inflammation and diabetes development may inform on future dietary guidelines for chronic disease prevention.
Introduction
Chronic diseases account for more than half of all premature deaths and more than 90% of yearly healthcare spending in the United States1,2. With 11 million deaths and 255 million disability-adjusted life-years globally attributable to poor nutrition, following a healthy diet can be a potentially cost-effective strategy for lowering the risk of chronic diseases3,4. Much existing diet-related research, however, focuses on specific foods, and hence may not provide clear knowledge about the ideal diet for overall health. Dietary patterns, characterizing a variety of foods, nutrients, and beverages, may serve as useful tools to represent the overall effects of diet on the risk of health outcomes.
Dietary patterns that emphasize high-quality foods, adherence to dietary recommendations, and a focus on plant-based foods have been demonstrated to reduce the risk of cardiovascular disease (CVD), type 2 diabetes, cancer, and all-cause mortality5. Based on this evidence, the 2015-2020 Dietary Guidelines for Americans propose Healthy U.S.-Style, Mediterranean-style, vegetarian diets, and Dietary Approaches to Stop Hypertension as examples of healthy diets6. Despite this, only a few studies have explicitly examined these diets in the same context for their potential health impact.
The purpose of this study is to compare the relative effectiveness of dietary patterns in improving general health by focusing on risk reduction of chronic diseases that contribute substantially to mortality in the United States, including CVD, cancer, and diabetes. Using data from three US cohorts (Health Professionals Follow-up Study [HPFS], Nurses’ Health Study [NHS], and NHS II) with up to 32 years of follow-up, we compared several dietary patterns that were promoted in the Dietary Guidelines for Americans and previously created for predicting major chronic diseases or important biological pathways for their associations with major chronic diseases (Fig.1).
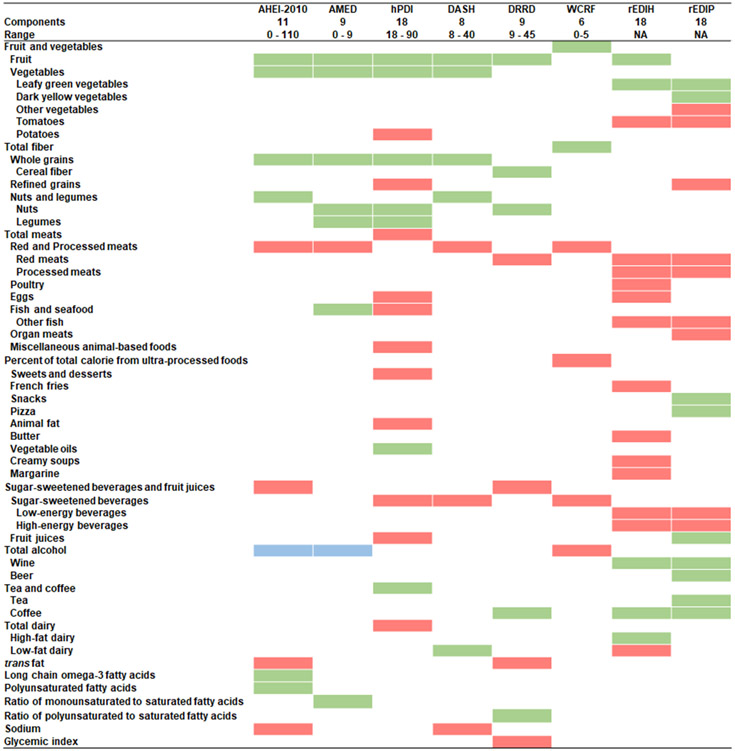
Fig.1.
Detailed components of dietary patterns. Higher points or positive weights were assigned to higher intakes of components in green. Lower points or negative weights were assigned to higher intakes of components in red. Higher points were assigned to moderate intakes of components in blue. AHEI-2010, Alternative Healthy Eating Index-2010; AMED, Alternate Mediterranean Diet score; DASH, Dietary Approaches to Stop Hypertension score; DRRD, Diabetes Risk Reduction Diet; hPDI, Healthful plant-based diet index; rEDIH, reversed Empirical dietary index for hyperinsulinemia; rEDIP, reversed Empirical dietary inflammation pattern; WCRF/AICR, World Cancer Research Fund/American Institute for Cancer Research (WCRF/AICR) dietary score.
Results
Population characteristics.
We evaluated the associations of eight dietary patterns with major chronic diseases in composite and individually. Fig.1 shows the components of dietary patterns, and Supplementary Table 1 shows the outcome definition. The present study included 162,667 women from the NHS and NHSII, and 43,185 men from the HPFS (Extended Data Fig.1). During a median follow-up of 26 years, we observed 44,975 major chronic disease events, 12,962 major CVD, 18,615 diabetes, and 17,909 total cancers in the three cohorts.
Table 1 shows the age-standardized characteristics of the study population. Individuals in the highest quintile of dietary pattern scores were more likely to be older, exercise more, have lower body mass index (BMI), take multivitamins, use postmenopausal hormones (women), and were less likely to be current smokers. Individuals with the highest adherence to the reversed empirical dietary index for hyperinsulinemia (rEDIH) and reversed empirical dietary inflammatory pattern (rEDIP) drank more alcohol while those with the highest adherence to the World Cancer Research Fund/American Institute for Cancer Research (WCRF/AICR) dietary score drank less. Participants with higher scores of healthful Plant-based Diet Index (hPDI), Diabetes Risk Reduction Diet (DRRD), rEDIH, and rEDIP consumed more coffee, whereas those with higher WCRF/AICR consumed less.
Table 1.
Age-standardized characteristics of study population in the lowest and highest quintiles of energy-adjusted dietary patterns during the follow-up in the pooled data
| Quintile | Q1 | Q5 | Q1 | Q5 | Q1 | Q5 | Q1 | Q5 |
|---|---|---|---|---|---|---|---|---|
| Pattern | AHEI-2010 | AMED | hPDI | DASH | ||||
| Median scorea | 39.0 | 65.0 | 2.3 | 6.4 | 47.2 | 62.5 | 17.9 | 29.1 |
| Ageb, year | 52.2 (11.6) | 58.3 (11.1) | 53.7 (11.4) | 56.2 (11.7) | 53.7 (11.6) | 56.4 (11.7) | 53.4 (11.1) | 56.5 (12.0) |
| Family history of cancer, % | 35.9 | 43.1 | 39.3 | 39.2 | 39.7 | 39.1 | 38.8 | 39.3 |
| Family history of diabetes, % | 24.0 | 28.7 | 26.6 | 25.8 | 26.3 | 26.8 | 26.2 | 25.8 |
| Family history of CVD, % | 40.6 | 44.0 | 42.0 | 43.0 | 41.7 | 43.5 | 42.0 | 42.5 |
| Physical activity, METS-h/week | 15.2 (17.1) | 30.0 (27.0) | 15.9 (17.6) | 28.1 (25.6) | 16.6 (17.8) | 28.0 (26.8) | 15.4 (17.1) | 29.2 (27.0) |
| Height, cm | 167.3 (8.7) | 166.9 (8.3) | 167.2 (8.7) | 167.0 (8.3) | 167.3 (8.6) | 166.9 (8.4) | 167.0 (8.7) | 167.2 (8.3) |
| Body mass index, kg/m2 | 25.6 (4.8) | 24.4 (4.0) | 25.7 (4.9) | 24.4 (3.9) | 25.6 (4.8) | 24.6 (4.1) | 25.7 (4.9) | 24.4 (4.0) |
| Alcohol consumption, g/day | 5.9 (12.6) | 6.8 (7.3) | 5.8 (11.7) | 6.7 (7.7) | 5.2 (8.8) | 6.7 (10.1) | 6.7 (11.4) | 5.3 (7.9) |
| Current smoking, % | 24.3 | 13.4 | 24.5 | 14.2 | 20.6 | 16.0 | 28.0 | 11.8 |
| Regular aspirin usec, % | 26.5 | 23.2 | 25.2 | 24.9 | 25.2 | 24.7 | 25.6 | 23.8 |
| Regular NSAIDs used, % | 22.8 | 26.1 | 25.8 | 23.4 | 25.0 | 24.2 | 25.9 | 22.6 |
| Multivitamin use, % | 42.5 | 57.2 | 43.6 | 56.0 | 45.0 | 54.9 | 40.8 | 58.0 |
| Postmenopausal hormone use, % | 12.6 | 15.5 | 12.3 | 15.8 | 12.3 | 15.7 | 12.3 | 15.5 |
| Coffee, cup/d | 1.8 (1.6) | 1.9 (1.4) | 1.9 (1.6) | 1.8 (1.4) | 1.5 (1.4) | 2.2 (1.5) | 1.9 (1.6) | 1.8 (1.4) |
| Total energy intake, kcal/d | 1836 (485) | 1836 (497) | 1824 (515) | 1832 (445) | 1841 (462) | 1834 (508) | 1839 (516) | 1845 (451) |
| Pattern | DRRD | WCRF/AICR | rEDIH | rEDIP | ||||
| Median scorea | 20.6 | 33.4 | 1.5 | 3.2 | -0.7 | -0.2 | -0.3 | 0.4 |
| Ageb, year | 53.6 (11.5) | 56.4 (11.7) | 52.9 (11.3) | 56.9 (11.9) | 52.4 (11.1) | 57.6 (11.5) | 53.9 (11.8) | 55.6 (11.2) |
| Family history of cancer, % | 39.1 | 39.6 | 37.9 | 39.8 | 36.7 | 42.4 | 38.1 | 40.7 |
| Family history of diabetes, % | 26.3 | 26.3 | 24.0 | 27.5 | 26.6 | 26.0 | 28.0 | 24.7 |
| Family history of CVD, % | 41.7 | 43.6 | 41.7 | 42.7 | 41.6 | 42.9 | 42.5 | 42.6 |
| Physical activity, METS-h/week | 15.9 (17.5) | 28.5 (26.6) | 16.6 (17.7) | 27.7 (26.9) | 17.4 (19.0) | 28.0 (26.6) | 18.8 (20.6) | 24.8 (24.2) |
| Height, cm | 167.0 (8.7) | 167.1 (8.3) | 167.3 (8.6) | 166.9 (8.4) | 167.4 (8.8) | 167.1 (8.2) | 166.9 (8.7) | 167.4 (8.4) |
| Body mass index, kg/m2 | 25.7 (4.9) | 24.5 (3.9) | 25.0 (4.4) | 25.0 (4.4) | 26.7 (5.2) | 23.7 (3.5) | 26.5 (5.2) | 24.2 (3.8) |
| Alcohol consumption, g/day | 5.0 (9.3) | 6.6 (9.4) | 9.3 (11.7) | 3.4 (6.6) | 4.5 (8.7) | 10.0 (12.0) | 3.2 (7.0) | 12.1 (13.5) |
| Current smoking, % | 21.2 | 15.0 | 26.0 | 12.4 | 21.3 | 17.2 | 17.6 | 22.5 |
| Regular aspirin usec, % | 24.8 | 25.2 | 26.5 | 23.2 | 26.6 | 23.9 | 25.6 | 26.1 |
| Regular NSAIDs used, % | 24.9 | 24.3 | 24.9 | 23.1 | 25.2 | 25.5 | 25.2 | 26.2 |
| Multivitamin use, % | 43.2 | 56.5 | 44.2 | 55.9 | 43.5 | 55.6 | 45.5 | 53.1 |
| Postmenopausal hormone use, % | 12.5 | 15.9 | 13.0 | 15.1 | 13.2 | 14.5 | 13.4 | 14.6 |
| Coffee, cup/d | 1.2 (1.3) | 2.3 (1.5) | 2.0 (1.5) | 1.7 (1.5) | 1.3 (1.4) | 2.5 (1.6) | 1.0 (1.1) | 2.9 (1.6) |
| Total energy intake, kcal/d | 1825 (499) | 1827 (484) | 1806 (466) | 1801 (499) | 1915 (534) | 1923 (487) | 1893 (531) | 1889 (496) |
AHEI-2010, Alternative Healthy Eating Index-2010; AMED, Alternate Mediterranean Diet score; CVD, cardiovascular disease; DASH, Dietary Approaches to Stop Hypertension score; DRRD, Diabetes Risk Reduction Diet; METS, metabolic equivalent for task score; NSAIDs, nonsteroidal anti-inflammatory drugs; hPDI, Healthful plant-based diet index; rEDIH, reversed Empirical dietary index for hyperinsulinemia; rEDIP, reversed Empirical dietary inflammation pattern; WCRF/AICR, World Cancer Research Fund/American Institute for Cancer Research (WCRF/AICR) dietary score.
Values are means (standard deviations) for continuous variables and percentages for categorical variables if not specified otherwise.
Energy-adjusted scores are shown.
All variables are standardized to the age distribution of the study population, except for age.
Regular users are defined as participants who take at least 2 tablets of aspirin (325 mg/tablet) per week in the NHS and at least 2 times per week in the HPFS and NHSII.
Regular users are defined as participants who take at least 2 times per week.
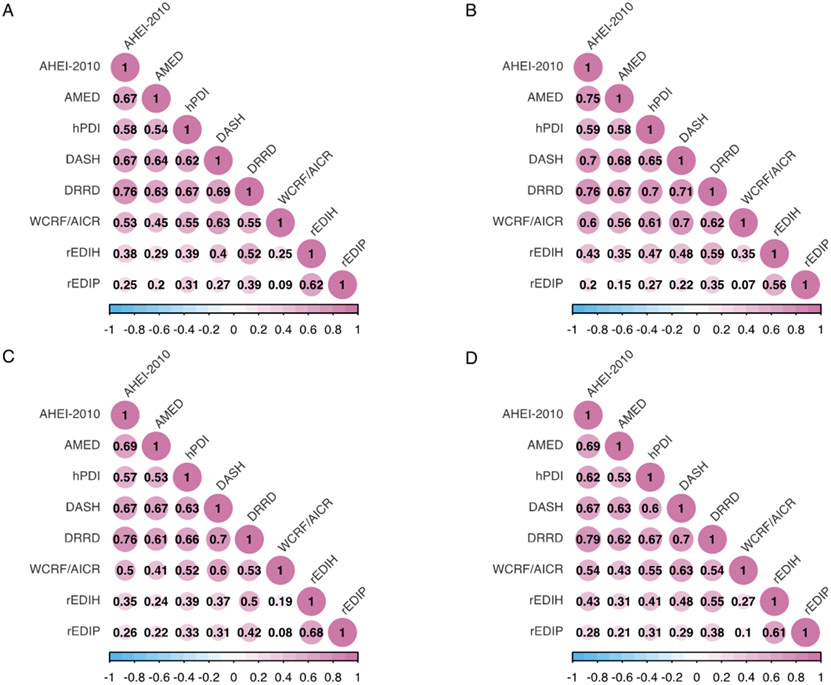
Correlations between dietary patterns were comparable across cohorts (Extended Data Fig.2). The Alternative Healthy Eating Index-2010 (AHEI-2010), Alternate Mediterranean Diet (AMED), Dietary Approaches to Stop Hypertension (DASH), hPDI, DRRD, and WCRF/AICR dietary score were strongly correlated with each other, with Spearman correlation coefficients ranging from 0.45 to 0.76 in the pooled data. The rEDIH and rEDIP had relatively lower correlations with other dietary patterns.
Because the point estimates in the pooled data and random-effects meta-analysis based on three cohorts are nearly identical (Supplementary Table 2), we presented the associations obtained in the pooled data for all analyses. Although the point estimates for the associations between patterns and outcomes varied by cohort, the general direction and magnitude ranking for the associations were similar.
Dietary patterns and major chronic diseases.
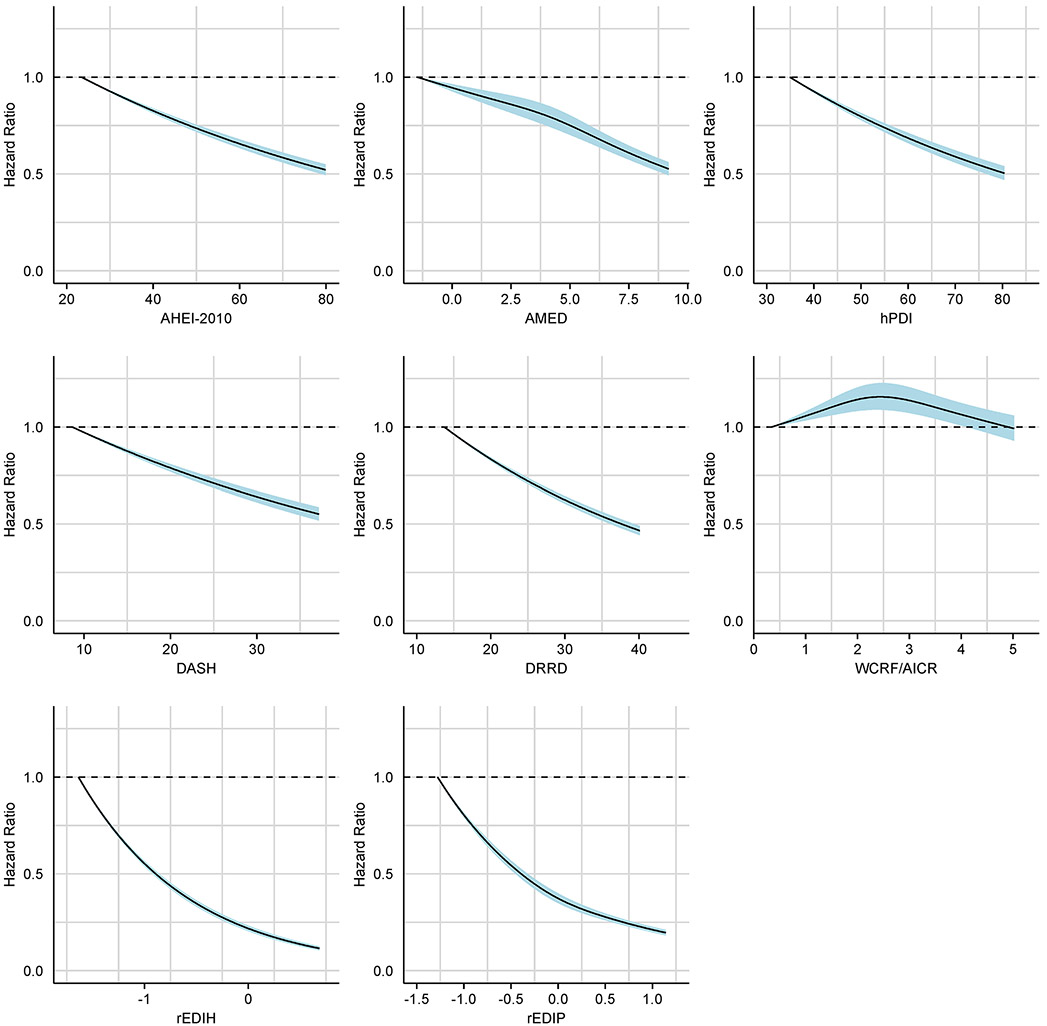
Table 2 shows the hazard ratios (HR) for major chronic disease (the composite of major cardiovascular disease, type 2 diabetes, and total cancer) comparing the 90th (high adherence) to 10th (low adherence) percentile scores for each dietary pattern. The multivariable-adjusted associations were strongest for the rEDIH (HR 0.58, 95% confidence interval [CI] 0.57, 0.60), rEDIP (HR 0.61, 95% CI 0.60, 0.63), and DRRD (HR 0.70, 95% CI 0.69, 0.72). Inverse associations with major chronic disease were also observed for AHEI-2010, AMED, hPDI, and DASH, with HRs between 0.76 and 0.80. In contrast, the WCRF/AICR dietary score was not associated with major chronic disease. Although the spline analysis demonstrated statistically significant nonlinearity for the AMED, WCRF/AICR dietary score, and rEDIP, the curves were largely monotonic for the rEDIP and AMED (Extended Data Fig.3) and the relationship between the WCRF/AICR dietary score and major chronic disease also appeared monotonic after the alcohol component was removed from the score (data not shown). Similar findings were observed when using pattern scores in quintiles as the exposure (Supplementary Table 3).
Table 2.
Associations of cumulative average dietary patterns (comparing the 90th to 10th percentile) with major chronic disease and its major components in the pooled data
| Outcome | Major Chronic Disease | Major Cardiovascular Disease | Type 2 Diabetes | Total Cancer | |
|---|---|---|---|---|---|
| Cases | 44,975 | 12,962 | 18,615 | 17,909 | |
| Person-year | 4,852,894 | 5,148,378 | 4,630,725 | 5,138,951 | |
| Pattern | Model | HR (95% CI) | HR (95% CI) | HR (95% CI) | HR (95% CI) |
| AHEI-2010 | Age | 0.64 (0.62, 0.66) | 0.63 (0.60, 0.66) | 0.49 (0.47, 0.51) | 0.81 (0.78, 0.84) |
| MVa | 0.76 (0.74, 0.78) | 0.77 (0.73, 0.81) | 0.62 (0.59, 0.64) | 0.94 (0.90, 0.98) | |
| MV + nSESb | 0.78 (0.76, 0.80) | 0.79 (0.75, 0.83) | 0.66 (0.63, 0.69) | 0.93 (0.89, 0.97) | |
| MV + BMIc | 0.83 (0.80, 0.85) | 0.79 (0.75, 0.83) | 0.73 (0.70, 0.77) | 0.95 (0.91, 0.99) | |
| AMED | Age | 0.65 (0.64, 0.67) | 0.64 (0.61, 0.67) | 0.56 (0.53, 0.58) | 0.78 (0.75, 0.81) |
| MVa | 0.79 (0.77, 0.81) | 0.80 (0.76, 0.84) | 0.71 (0.68, 0.74) | 0.92 (0.89, 0.96) | |
| MV + nSESb | 0.81 (0.78, 0.83) | 0.82 (0.78, 0.86) | 0.74 (0.71, 0.77) | 0.92 (0.88, 0.96) | |
| MV + BMIc | 0.86 (0.84, 0.88) | 0.83 (0.79, 0.87) | 0.85 (0.82, 0.89) | 0.94 (0.90, 0.98) | |
| hPDI | Age | 0.70 (0.69, 0.72) | 0.72 (0.69, 0.76) | 0.57 (0.55, 0.59) | 0.86 (0.83, 0.90) |
| MVa | 0.80 (0.78, 0.82) | 0.84 (0.80, 0.88) | 0.70 (0.67, 0.72) | 0.94 (0.90, 0.98) | |
| MV + nSESb | 0.80 (0.78, 0.83) | 0.84 (0.80, 0.88) | 0.71 (0.68, 0.73) | 0.94 (0.90, 0.98) | |
| MV + BMIc | 0.84 (0.82, 0.87) | 0.85 (0.81, 0.90) | 0.78 (0.75, 0.81) | 0.95 (0.91, 0.99) | |
| DASH | Age | 0.63 (0.61, 0.64) | 0.62 (0.59, 0.65) | 0.52 (0.50, 0.54) | 0.76 (0.73, 0.79) |
| MVa | 0.78 (0.76, 0.80) | 0.81 (0.77, 0.85) | 0.66 (0.64, 0.69) | 0.94 (0.91, 0.99) | |
| MV + nSESb | 0.79 (0.77, 0.81) | 0.83 (0.79, 0.87) | 0.69 (0.66, 0.72) | 0.94 (0.90, 0.98) | |
| MV + BMIc | 0.83 (0.81, 0.86) | 0.83 (0.79, 0.87) | 0.77 (0.74, 0.81) | 0.96 (0.92, 1.00) | |
| DRRD | Age | 0.61 (0.59, 0.62) | 0.62 (0.59, 0.65) | 0.44 (0.43, 0.46) | 0.83 (0.80, 0.87) |
| MVa | 0.70 (0.69, 0.72) | 0.73 (0.69, 0.76) | 0.56 (0.54, 0.58) | 0.92 (0.88, 0.96) | |
| MV + nSESb | 0.72 (0.70, 0.73) | 0.74 (0.71, 0.78) | 0.58 (0.56, 0.60) | 0.92 (0.88, 0.96) | |
| MV + BMIc | 0.76 (0.74, 0.78) | 0.75 (0.71, 0.79) | 0.66 (0.63, 0.69) | 0.94 (0.90, 0.98) | |
| WCRF/AICR | Age | 0.84 (0.82, 0.86) | 0.80 (0.77, 0.84) | 0.86 (0.83, 0.90) | 0.85 (0.81, 0.88) |
| MVa | 1.00 (0.98, 1.03) | 1.00 (0.96, 1.05) | 1.05 (1.01, 1.10) | 1.01 (0.97, 1.05) | |
| MV + nSESb | 1.01 (0.98, 1.04) | 1.01 (0.96, 1.06) | 1.07 (1.02, 1.11) | 1.01 (0.97, 1.05) | |
| MV + BMIc | 0.96 (0.94, 0.99) | 0.99 (0.94, 1.03) | 0.95 (0.91, 0.99) | 1.00 (0.96, 1.04) | |
| rEDIH | Age | 0.53 (0.52, 0.54) | 0.61 (0.59, 0.64) | 0.30 (0.29, 0.31) | 0.85 (0.82, 0.88) |
| MVa | 0.58 (0.57, 0.60) | 0.68 (0.65, 0.71) | 0.35 (0.34, 0.36) | 0.90 (0.87, 0.94) | |
| MV + nSESb | 0.59 (0.58, 0.61) | 0.70 (0.66, 0.73) | 0.36 (0.35, 0.37) | 0.90 (0.86, 0.93) | |
| MV + BMIc | 0.75 (0.73, 0.77) | 0.76 (0.72, 0.79) | 0.57 (0.54, 0.59) | 0.95 (0.91, 0.99) | |
| rEDIP | Age | 0.59 (0.57, 0.60) | 0.67 (0.64, 0.70) | 0.33 (0.32, 0.34) | 0.93 (0.90, 0.97) |
| MVa | 0.61 (0.60, 0.63) | 0.69 (0.66, 0.72) | 0.38 (0.36, 0.39) | 0.90 (0.87, 0.94) | |
| MV + nSESb | 0.62 (0.60, 0.63) | 0.70 (0.67, 0.73) | 0.38 (0.37, 0.40) | 0.90 (0.87, 0.94) | |
| MV + BMIc | 0.75 (0.73, 0.77) | 0.75 (0.72, 0.79) | 0.57 (0.55, 0.59) | 0.94 (0.91, 0.98) | |
AHEI-2010, Alternative Healthy Eating Index-2010; AMED, Alternate Mediterranean Diet score; BMI, body mass index; CI, Confidence interval; DASH, Dietary Approaches to Stop Hypertension score; DRRD, Diabetes Risk Reduction Diet; hPDI, Healthful plant-based diet index; HR, Hazard ratio; MV, multivariable; nSES, neighborhood socioeconomic status; rEDIH, reversed Empirical dietary index for hyperinsulinemia; rEDIP, reversed Empirical dietary inflammation pattern; WCRF/AICR, World Cancer Research Fund/American Institute for Cancer Research (WCRF/AICR) dietary score.
Analyses were stratified by age (in month), calendar year, and cohort. MV model: adjusted for physical activity (<3.0, 3.0-8.9, 9.0-17.9, 18.0-26.9, 27.0-41.9, or ≥42 MET-h/week), cigarette smoking status (never, former quitting ≥10 y, former quitting <10 y, current), cigarette smoking pack-years (0, 1-4, 5-14, 15-24, or ≥25 pack-years), multivitamin use (yes or no), regular aspirin use (yes or no), regular non-steroidal anti-inflammatory drugs use (yes or no), postmenopausal hormone use (premenopausal, never, former, or current use) for women, and total energy intake (quintiles). Alcohol consumption (<5.0, 5.0-14.9, or ≥15.0 g/d) was adjusted for DASH, hPDI, and DRRD. For major chronic disease, the model was additionally adjusted for family history of diabetes (yes or no), family history of cancer (yes or no), and family history of cardiovascular disease (yes or no). For type 2 diabetes, the model was additionally adjusted for family history of diabetes (yes or no). For major cardiovascular disease, the model was additionally adjusted for family history of cardiovascular disease (yes or no). For total cancer, the model was additionally adjusted for family history of cancer (yes or no) and height (continuous).
Adjusted for nSES (continuous).
Adjusted for BMI (continuous).
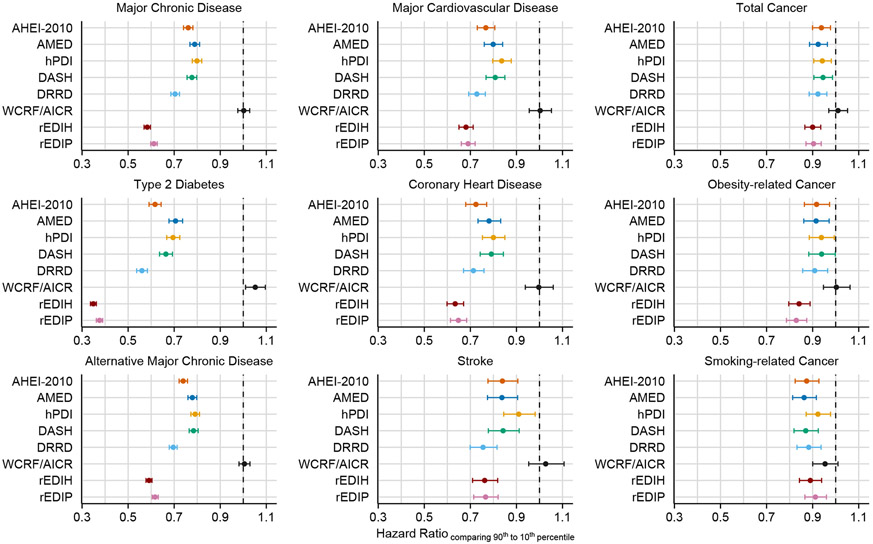
We next investigated the associations between dietary pattern scores and each individual component of major chronic disease as presented in Fig.2, Table 2, and Extended Data Table 1. In general, the strongest relationships among the various outcomes (cardiovascular diseases, cancer, and type 2 diabetes) were those between dietary patterns and type 2 diabetes. Among the dietary patterns, rEDIH, rEDIP, and DRRD score had the strongest associations with type 2 diabetes (HR: 0.35–0.56). These three pattern scores were also among the top three patterns that were strongly associated with CVD-related outcomes, including major CVD, coronary heart disease, and stroke (HR: 0.63–0.77). The estimates for AHEI-2010 were comparable with DRRD score for coronary heart disease. The estimates for cancer-related outcomes were closer to null compared with type 2 diabetes or cardiovascular diseases, for all dietary patterns. Participants with higher rEDIH, rEDIP, or DRRD scores had a decreased risk of total cancer, obesity-related cancer, and smoking-related cancer (HR: 0.83–0.92). For total cancer and smoking-related cancer, participants with higher AHEI-2010, AMED, and DASH presented comparable or lower risk than those with higher rEDIH, rEDIP, or DRRD. The WCRF/AICR dietary score was not associated with secondary outcomes except for a positive association with type 2 diabetes (HR 1.05; 95% CI: 1.01–1.10). As in the primary analysis, dietary patterns were similarly associated with an alternatively defined major chronic disease, which includes non-traumatic death in addition to major chronic disease incidence.
Fig.2.
Multivariable-adjusted associations of cumulative average dietary patterns (comparing the 90th to 10th percentile) with major chronic disease and secondary outcomes in the pooled data of three cohorts (n = 205,852 participants). The Analyses details and corresponding estimates are provided in Table 2 and Extended Data Table 1. The hazard ratios are indicated by the circles and the 95% confidence intervals are reflected by the error bars. AHEI-2010, Alternative Healthy Eating Index-2010; AMED, Alternate Mediterranean Diet score; DASH, Dietary Approaches to Stop Hypertension score; DRRD, Diabetes Risk Reduction Diet; hPDI, Healthful plant-based diet index; rEDIH, reversed Empirical dietary index for hyperinsulinemia; rEDIP, reversed Empirical dietary inflammation pattern; WCRF/AICR, World Cancer Research Fund/American Institute for Cancer Research (WCRF/AICR) dietary score.
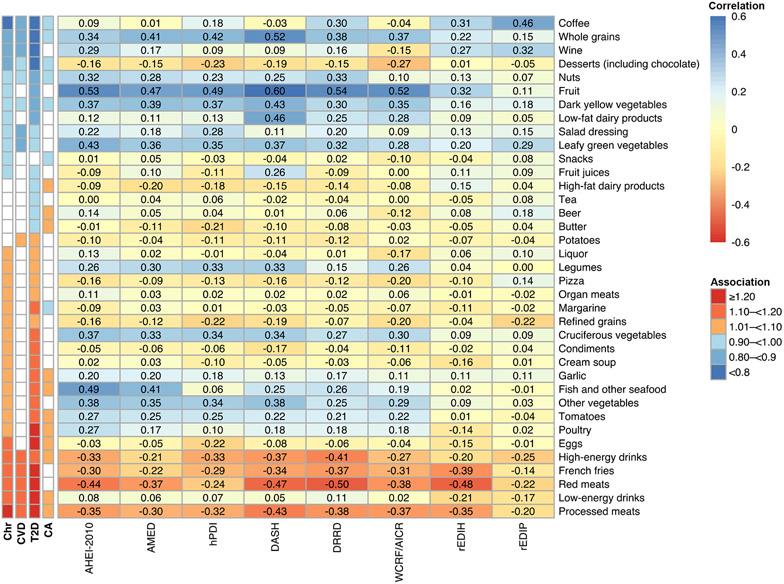
Fig.3 shows the associations between individual food groups with dietary patterns and major chronic diseases. The estimates for food groups were largely similar across major chronic diseases, although the associations were slightly stronger for type 2 diabetes. Coffee, whole grains, wine, desserts were inversely associated with major chronic disease, whereas processed meats, low-energy drinks, red meats, French fries, high-energy drinks, and eggs were positively associated with major chronic disease. Compared with other patterns, the rEDIH, rEDIP, and DRRD appeared to be more or at least similarly correlated with food groups that were associated with major chronic diseases (particularly type 2 diabetes), such as coffee, wine, processed meats, red meats, French fries, and sugar-sweetened beverages. The rEDIH and rEDIP had relatively lower correlations with fruit and vegetables compared to other dietary patterns except for leafy green vegetables.
Fig.3.
Baseline Spearman correlations between energy-adjusted cumulative average dietary patterns and food groups in the pooled data of three cohorts (n = 205,852 participants). Spearman correlation coefficients are shown and highlighted in color. Food groups are ordered based on the hazard ratios of their associations with major chronic disease (Chr). The associations of food groups (comparing the 90th to 10th percentile) with major chronic disease (Chr), major cardiovascular disease (CVD), type 2 diabetes (T2D), or total cancer (CA) are indicated on the left of the figure. We reported unadjusted P values based on two-sided statistical tests. Significant associations (P<0.05) are highlighted in color according to the magnitude of hazard ratios. AHEI-2010, Alternative Healthy Eating Index-2010; AMED, Alternate Mediterranean Diet score; DASH, Dietary Approaches to Stop Hypertension score; DRRD, Diabetes Risk Reduction Diet; hPDI, Healthful plant-based diet index; rEDIH, reversed Empirical dietary index for hyperinsulinemia; rEDIP, reversed Empirical dietary inflammation pattern; WCRF/AICR, World Cancer Research Fund/American Institute for Cancer Research (WCRF/AICR) dietary score.
Subgroup and latency analyses.
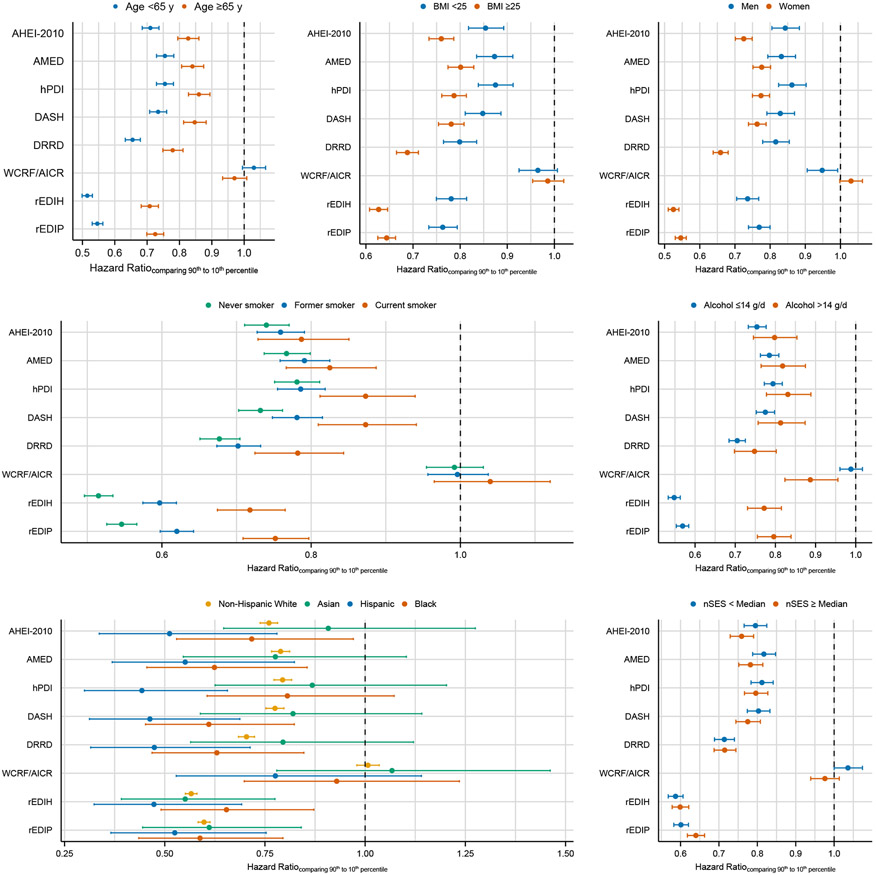
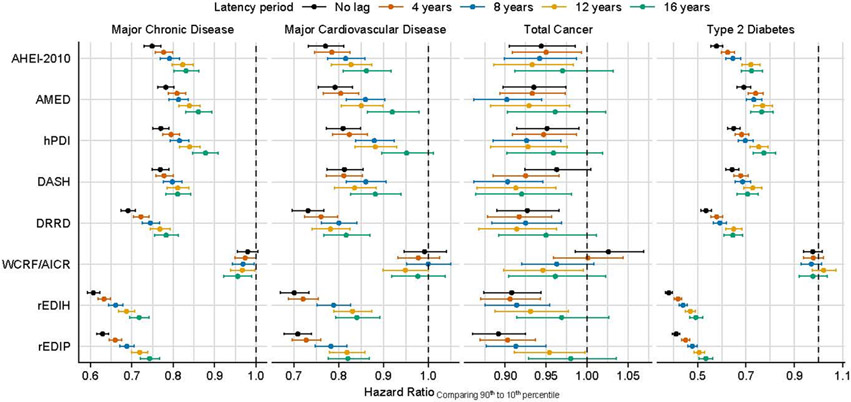
The associations between patterns and major chronic disease persisted in subgroups defined by age, BMI, sex, smoking status, alcohol intake, neighborhood socioeconomic status (nSES), and race/ethnicity(Fig.4, Extended Data Table 2). The inverse associations between dietary patterns and major chronic disease were generally stronger in participants who were younger, overweight or have obesity, women, and Hispanic. Although WCRF/AICR exhibited an inverse association with major chronic disease in participants who drank more alcohol, the rEDIH and rEDIP showed stronger associations in participants who never smoked or drank less. Comparable associations with major chronic disease were observed in subgroups defined by nSES. With longer latency periods, the associations between dietary patterns and major chronic disease were slightly attenuated (Extended Data Fig.4, Extended Data Table 3). A similar trend was observed for major cardiovascular disease and type 2 diabetes, but not for total cancer.
Fig.4.
Multivariable-adjusted associations between cumulative average dietary patterns (comparing the 90th to 10th percentile) and major chronic disease in subgroups. Analyses details and corresponding estimates are provided in Extended Data Table 2. The hazard ratios are indicated by the circles and the 95% confidence intervals are reflected by the error bars. AHEI-2010, Alternative Healthy Eating Index-2010; AMED, Alternate Mediterranean Diet score; BMI, body mass index; DASH, Dietary Approaches to Stop Hypertension score; DRRD, Diabetes Risk Reduction Diet; hPDI, Healthful plant-based diet index; nSES, neighborhood socioeconomic status; rEDIH, reversed Empirical dietary index for hyperinsulinemia; rEDIP, reversed Empirical dietary inflammation pattern; WCRF/AICR, World Cancer Research Fund/American Institute for Cancer Research (WCRF/AICR) dietary score.
Sensitivity analyses.
After removing the alcohol component from the dietary pattern scores, the associations for AHEI-2010, AMED, rEDIH, and rEDIP were attenuated only slightly but remained largely similar (Methods, Extended Data Table 4). In contrast to the main results, the WCRF/AICR dietary score without the alcohol component was inversely associated with major chronic disease, major CVD, and Type 2 diabetes (HR: 0.77–0.88). After removing the coffee component, the associations of DRRD, rEDIH, and rEDIP with major chronic disease attenuated but remained strong (Extended Data Table 5). The HRs for the association of dietary patterns with major chronic disease and its components barely changed after adjusting for the nSES score (HR change: 0.00–0.04) (Table 2, Extended Data Table 1). After adjusting for BMI, we observed an attenuated association with major chronic disease, especially for rEDIH and rEDIP, yet the rEDIH, rEDIP, and DRRD remained to show the strongest associations (Table 2, Extended Data Table 1). Additional sensitivity analyses showed that our findings remained unchanged (Supplementary Table 4). Compared with the same participants who were never in the highest quintiles of any pattern, the rEDIH, rEDIP, and DRRD remained the top three dietary patterns that were strongly associated with the risk of major chronic disease (Extended Data Table 6). The composite outcome in the pooled data did not meet the proportional hazards assumption, which can be related to effect modification by age (P value <0.05 for all patterns except WCRF/AICR). Thus, the results estimated in the pooled data should be interpreted as the average associations during the follow-up.
Discussion
The current understanding of dietary patterns on general health is based mostly on the synthesis of the literature for individual diseases rather than more composite outcomes of chronic diseases. Furthermore, the relationships between patterns and major chronic diseases have rarely been compared in the same study utilizing the same data collection and statistical analysis approach. In this study, we compared two mechanism-based dietary patterns with six dietary patterns reflecting general or disease-specific dietary guidelines in 205,852 participants over the course of more than two decades. In general, adherence to a healthy diet was associated with a decreased risk of major chronic diseases. Participants who reported high adherence to low insulinemic, low inflammatory, and diabetes risk-reducing dietary patterns displayed a decreased risk for major chronic diseases when examined as individual or composite outcome.
The rEDIH and rEDIP represent dietary patterns empirically constructed based on foods that are either positively or inversely associated with biomarkers of two important and related biological pathways for chronic disease—hyperinsulinemia and chronic inflammation7,8. Assuming causal associations, the dietary patterns can be interpreted as individuals with high adherence to the rEDIH and rEDIP tending to have lower markers of insulin and inflammation, though these biomarkers could have other determinants. Therefore, strong associations were observed between these two patterns with chronic disease risk, which can be largely shaped by their connections to pathophysiologic underpinnings of insulin resistance and type 2 diabetes. As shown in other studies, participants with low rEDIH or rEDIP scores had a higher risk of developing type 2 diabetes9,10. Despite this, associations were observed between rEDIH or rEDIP and other elements of chronic diseases, which may be mediated by the same mechanistic pathways. In line with our findings, prior investigations in the NHS and HPFS showed an inverse association between rEDIP and CVD, as well as rEDIH and total mortality11. Additionally, when compared to other patterns, the rEDIH and rEDIP showed greater associations with both composite and specific chronic diseases. Previous studies showed that these two diets are predictive of a diverse range of biomarkers for atherosclerosis, hyperlipidemia, hyperinsulinemia, and systemic inflammation12,13, supporting the hypothesis that rEDIH and rEDIP address fundamental biological pathways that are shared by multiple chronic diseases. The weighting of foods by a measured biological response may also account for differential measurement errors among specific foods.
Although not as strong as that for rEDIH or rEDIP, we observed an inverse association between DRRD and major chronic disease. Consisting of dietary components with sufficient evidence for type 2 diabetes, the DRRD has been shown to be associated with risk of type 2 diabetes across diverse racial and ethnic populations14. Participants with higher adherence to DRRD were associated with a lower risk of death from all causes, cardiovascular disease, and cancer in a US-based study15, which is compatible with our findings, indicating that the preventive role of DRRD may extend beyond type 2 diabetes to cardiovascular disease, cancer, and death. One possible explanation might be that a diet targeting type 2 diabetes captures dietary insulinemic potential that is etiologically crucial for developing a wide spectrum of chronic diseases.
While their relationships with specific outcomes vary somewhat, the AHEI-2010, AMED, DASH, and hPDI all showed an inverse association with major chronic disease. This aligns with numerous studies supporting the protective associations of AHEI-2010, AMED, and DASH with cardiovascular disease, type 2 diabetes, and cancer16-18. Because we accounted for smoking intensity and quit time, the inverse relationships of AHEI-2010, AMED, and DASH with smoking-related cancer may not be entirely explained by residual confounding by smoking. Although dietary evidence for smoking-related cancer is sparse, a meta-analysis found that the inverse association between the Mediterranean diet and lung cancer was greater in former smokers19, suggesting potential effect modification by smoking status. Previous research suggested that individuals who have increased their adherence to healthy plant-based diets had decreased risks of type 2 diabetes, overall cardiovascular disease, and overall mortality20-22. We found that, in agreement with findings from a meta-analysis on plant-based diets20, the inverse relationship between hPDI and cardiovascular disease was more pronounced for coronary heart disease than for stroke. One possibility is that the hPDI may have distinct relationships with ischemic and hemorrhagic stroke.
Despite moderate correlations with other dietary patterns, the WCRF/AICR dietary score includes the fewest items. The WCRF/AICR dietary score was not specifically customized to prevent diseases other than cancer may account for the null association with major chronic disease. However, we found an unexpected positive association for type 2 diabetes, and generally null associations for cancer-related outcomes. Because the 2018 WCRF/AICR recommendations included behavioral components beyond nutritional guidance23, this score based solely on dietary recommendations may not represent the optimal diet for cancer prevention. Prior studies showed that the inverse associations between the WCRF/AICR lifestyle score and cancer incidence and all-cause mortality, as well as the improvement of biomarker profile, were predominantly driven by physical activity and body weight components, as opposed to the dietary components24-26.
Due in part to the heterogeneity of cancer, the associations between dietary patterns and cancer-related outcomes were not as strong as those for other outcomes. Total cancer is a diverse constellation of unique diseases with a variety of causes, such as cigarette smoking, obesity, physical inactivity, and infections27. Even within one type of cancer, there are multiple subtypes. Some cancers, such as colorectal cancer, are diet-related while others are not27. A ten percent reduction from dietary patterns alone (ignoring the potential effect of diet on weight control) would be considered relatively large based on current understanding. Although more directly related to cardiometabolic diseases, the rEDIH, rEDIP, and DRRD displayed that a portion of cancers can be prevented by diet. Additionally, following these three diets may be equally or even more beneficial for cancer prevention compared to other healthy diets, including the one that is specially designed for cancer.
The individual food components and scoring methods of dietary patterns may partially explain the differential associations between dietary patterns and chronic disease. The WCRF/AICR score considers alcohol drinking as harmful due to strong evidence supporting its carcinogenic effect27, which might obscure the potential benefits of moderate drinking for reducing coronary heart disease, ischemic stroke, type 2 diabetes, and all-cause mortality28-30. The AHEI-2010 and AMED discourage low or heavy drinking while supporting moderate drinking. On the other hand, alcoholic beverages are given positive weights in the rEDIP and rEDIH because drinking alcohol is associated with lower levels of insulinemia and inflammation. Given the complex effects of alcohol on health, recommendations on alcohol intake should be personalized based on each person’s risk profile. Nonetheless, the associations of these four scores with risk of subsequent chronic diseases only changed modestly when the alcohol component was eliminated, suggesting that health improvement may still be achieved without alcohol intake. Coffee drinking, which is considered in the DRRD, rEDIH and rEDIP, has been associated with a lower risk of cardiometabolic disease31. The lower level of coffee intake among participants who scored high for WCRF/AICR might also contribute to the slightly positive association between WCRF/AICR and type 2 diabetes. Dietary guidelines emphasizing foods contributing to caloric intake would not account for dietary factors such as coffee consumption.
Our results also highlight that dietary patterns could reflect the overall effects of diet beyond the sum of individual foods. From a reductionist perspective, specific dietary components, such as coffee or moderate alcohol intake, may contribute to the benefits of maintaining a healthy diet. The relatively weak correlations of rEDIH and rEDIP with some frequently recommended foods, such as cruciferous vegetables and legumes, suggest that the metabolic effects of diet may be cumulative and not dominated by a few components. The unexpected protective association of dessert intake with chronic diseases may be explained by its inverse correlations with foods that appeared unfavorable for metabolic diseases (such as poultry, tomatoes, and eggs). The flavonoids in the chocolate may also contribute to the inverse associations between dessert and chronic diseases32,33. Given the varying degrees of health benefits associated with dietary patterns, future research on the subtle difference between patterns may be important for maximizing the effectiveness of dietary interventions.
After adjusting for BMI, the relationships with chronic disease for rEDIH and rEDIP were attenuated most because these two scores had the strongest association with BMI, possibly because of the residual confounding (BMI) or mediation effect (long-term weight gain)34. Our results remained consistent across several sensitivity tests. The stronger associations found in the subgroup analysis imply that dietary modification may be more advantageous for women, younger people, and people with higher BMI. The associations with rEDIH, rEDIP and DRRD were particularly strong for those with high BMI. This result would be expected as the influence of diet related to insulin resistance and inflammation is likely to be greater in individuals at risk for insulin resistance resulting from a high BMI. Yet, even in those with normal BMI, these scores still had the strongest inverse association with chronic disease. The strong associations between dietary patterns and major chronic disease in both ever- and never-smokers underscore the potential of dietary modification.
The goal of dietary guidelines for adults is to provide advice on food and beverage choices to meet nutritional needs and to help prevent diet-related chronic diseases. The pathophysiologic processes underlying major chronic diseases include, among others, lipids, blood pressure, glycemia, insulinemia, and inflammation. From an overall health perspective, the most important dietary components will likely be those that substantially affect the pathophysiologic processes that affect sizable numbers of multiple chronic diseases. Our findings for rEDIH and rEDIP may reflect that hyperinsulinemia and inflammation are strongly influenced by diet, have overlapping factors, and are quantitatively important for multiple diseases. The considerably stronger associations for rEDIH and rEDIP than other recommended dietary patterns may indicate that when recommendations are formulated, greater emphasis may need to be given to specific dietary components that influence inflammation and insulinemia, especially in the context of rising trends in obesity.
The strengths of this study include large sample size, long follow-up period, repeated assessments of dietary intake using validated instruments, detailed collection of lifestyle and medical data allowing for adjustment for potential confounders, and comprehensive comparisons of multiple dietary patterns with major chronic diseases within the same analytical framework.
Study limitations should be acknowledged. The composite outcome of major chronic disease did not include cognitive outcomes and other functional impairments. We included incident cases for diseases that are leading causes of death in the US and are well ascertained in the cohorts. To capture other chronic conditions severe enough to increase mortality, non-traumatic death was included in the alternative definition of major chronic disease. However, the possibility for reverse causation could increase after including mortality endpoints. We attempted to address this by conducting latency analyses and observed consistent strong associations for both individual and composite outcomes. With longer latency between diet and outcome assessment, the analysis may be conservative in not accounting for recent diet, but largely exclude the effect of reverse causation. Our study also implies that diet has more immediate effects on cardiometabolic diseases, but a longer latency period is required for cancer. The Four dietary patterns—AMED, DASH, hPDI, and DRRD—were determined based on the distribution of the research population using either the median or quintiles as the cut-off, which may not represent populations with more diverse racial and ethnic compositions. Yet, we found comparable associations across different ethnic groups, supporting the generalizability of the diet and disease associations.
In conclusion, we found that maintaining a healthy diet was generally associated with a lower risk of developing major chronic diseases. Among the eight dietary patterns examined in this study, those reflecting low insulinemic, low inflammatory, and diabetes risk reduction diet may confer the largest risk reduction for various chronic diseases. The rEDIH and rEDIP were developed empirically based on associations between specific foods and biomarkers of insulinemia and inflammation, which may contribute to their strong predictive capacity. Future research is needed to explore more specific biological mechanisms underlying the relationship between diet and overall health.
Methods
Study population.
This study leveraged data collected in three prospective cohorts: the Nurses’ Health Study (NHS), the NHSII, and the Health Professionals Follow-up Study (HPFS). The NHS was established in 1976 and enrolled 121,700 female nurses ages 30 to 55 at baseline. As a younger cohort, the NHSII enrolled 116,429 female nurses ages 25 to 42 in 1989. The HPFS enrolled 51,529 male health professionals ages 40 to 75 in 1986. Questionnaires were sent to participants in these cohorts to collect and update their lifestyle and medical history every two years. Participants provided data on their dietary intake during the preceding year using validated semi-quantitative food frequency questionnaires (FFQ) every four years. The follow-up rates were around 90% in all three cohorts. In this study, we used 1984 for the NHS, 1991 for the NHSII, and 1986 for the HPFS as the baseline when detailed dietary data were first assessed using an expanded FFQ with more than 100 items.
We excluded participants who were missing data on dietary pattern scores, those with implausible energy intake, those with a baseline history of CVD, diabetes, or cancer (except non-melanoma skin cancer and non-fatal prostate cancer), and those with extreme body mass index (<15 or > 50 kg/m2). To reduce potential reverse causation, participants were censored when they were 80 years old. The institutional review boards of the Brigham and Women's Hospital, Harvard T.H. Chan School of Public Health, and participating registries have approved the study protocol.
Ethics.
This is an observational study. The study protocol was approved by the institutional review boards (IRBs) of the Brigham and Women’s Hospital, Harvard T.H. Chan School of Public Health, and participating registries (IRB Protocol number: 2001P001945/BWH and 10372). The IRBs allowed participants’ completion of questionnaires to be considered as implied consent for participation in these studies of health professionals. Written informed consent was required for biomarker collection and for medical record acquisition. The study was performed in accordance with the Declaration of Helsinki.
Dietary assessment.
Participants were asked to specify their food consumption frequency of specified portion sizes in the FFQ. The nutrient intake was computed as the sum of the nutrient content of each contributing food multiplied by its consumption frequency. Several studies have evaluated the validity and reliability of self-reported food and nutrient measures. Comparing the estimates from FFQ with those from multiple one-week diet records, the average correlation coefficient for food was 0.66 in the NHS and 0.63 in the HPFS, and for nutrients was 0.53 in the NHS and 0.66 in the HPFS35-39. The correlation coefficient for dietary patterns ranges from 0.50 to 0.80 in the NHS and the HPFS40.
Details of each dietary pattern can be found in Fig.1. As a measure of healthy US-style eating, the Alternative Healthy Eating Index-2010 (AHEI-2010) assigns zero to ten points to each of the 11 dietary components based on the portion size41. The Alternate Mediterranean Diet (AMED) depicts a Mediterranean-style diet and assigns zero or one point to each of the nine components based on whether the intakes are higher than population median42. Representing a vegetarian diet, the healthful Plant-based Diet Index (hPDI) includes 18 food groups, and each group receives one to five points based on its consumption quintile43. The Dietary Approaches to Stop Hypertension (DASH) score contains eight components, each of which receives one to five points according to its consumption quintile44. The Diabetes Risk Reduction Diet (DRRD) score similarly assigns one to five points to each of the nine components associated with type 2 diabetes45. Based on five dietary recommendations for cancer prevention, the World Cancer Research Fund/American Institute for Cancer Research (WCRF/AICR) dietary score assigns zero to one point to each depending on adherence level23. To reflect the long-term dietary hyperinsulinemia potential, the empirical dietary index for hyperinsulinemia (EDIH) was derived to predict fasting plasma C-peptide8. The empirical dietary inflammatory pattern (EDIP) was developed to simultaneously predict plasma interleukin-6, C-reactive protein, and tumor necrosis factor α receptor 27.
Covariates assessment.
We extracted information from biennial questionnaires for race, family history of diabetes, family history of cancer, family history of CVD, physical activity, BMI, height, cigarette smoking (status, pack-years, and time since quitting), multivitamin use, regular aspirin use, regular non-steroidal anti-inflammatory drugs use, and postmenopausal hormone use for women. Data on census tract-level variables were obtained by linking the United States Census to participants’ geocoded addresses. A summary score for neighborhood socioeconomic status was calculated based on nine census tract variables including median family income, median home value, percent over 25 with college or higher degree, percent of families receiving interest dividends or rent income, percent occupied housing units, percent white, percent black, percent foreign-born, percent over 16 unemployed46.
Outcome definition.
The primary outcome was major chronic disease, defined as the first occurrence of incident major CVD, type 2 diabetes, or total cancer (excluding non-melanoma skin cancer and non-fatal prostate cancer). Secondary outcomes were the components of major chronic disease: major CVD (coronary heart disease and stroke), type 2 diabetes, and total cancer (obesity-related cancer47 and smoking-related cancer27). To test the influence of conditions not included in the primary outcome, we examined alternative major chronic disease, defined as the first occurrence of incident major CVD, type 2 diabetes, total cancer, or non-traumatic death from all other causes. The diseases and corresponding ICD-8 codes are provided in Supplementary Table 1.
Participants who reported a new diagnosis of CVD or cancer were asked for permission to obtain their medical records and pathological reports48. Deaths were identified through the next-of-kin or postal office when questionnaires were mailed and through searches of the National Death Index. Death ascertainment using National Death Index was reported to have a high sensitivity (98%) and specificity (100%)49,50. Permission was obtained from the next-of-kin or other contact person to review the medical records. Physicians who were blinded to the exposure information reviewed the medical records to confirm the diagnosis or determine the cause of death. Fatal coronary heart disease and fatal stroke were confirmed by death certificate and additional pathological evidence from either autopsy reports or medical records. Nonfatal myocardial infarction was confirmed according to the World Health Organization criteria and nonfatal stroke was confirmed according to the National Survey of Stroke criteria51,52. Type 2 diabetes was confirmed according to the National Diabetes Data Group criteria (before 1988) or the American Diabetes Association criteria (after 1988) using a supplementary questionnaire53,54. The confirmation rate based on medical records was estimated to range from 97% to 98%55,56.
Statistical analysis.
Person-time of follow-up accumulated from baseline until the occurrence of the outcome, death, age 80, or the end of follow-up (Jan 2016 for the HPFS, June 2016 for the NHS, and June 2017 for NHSII), whichever came first. The length of follow-up differed because separate analyses were conducted for each outcome. The main analysis used cumulative averages of dietary pattern scores as the exposure to capture long-term intake. To limit the potential influence of outliers, pattern scores were winsorized at the 0.5 and 99.5 percentiles57. We used the residual method to compute energy-adjusted scores by fitting each pattern score against the total energy intake58. Non-missing values from the preceding data cycle were used to fill in missing dietary variables and covariates. To facilitate comparison across pattern scores, we reversed the EDIH and EDIP scores so that the highest levels for both scores are regarded as the healthiest, similarly to the other scores.
We assessed the relationship of energy-adjusted pattern scores to each other using the Spearman correlation coefficients. Time-dependent Cox proportional hazards regression models with age as the time scale were fitted to estimate the associations of patterns with the risk of major chronic diseases and secondary outcomes. Each pattern score was modeled as a continuous variable standardized by its increment from the 10th to 90th percentile. The potential non-linear relationship between dietary pattern scores and outcome was examined by restricted cubic splines59. We also examined the associations for patterns in quintiles. The proportional hazards assumption was tested by adding an interaction term between each major dietary pattern and the time scale age.
Analyses were performed in each cohort as well as the pooled data of three cohorts. All the analyses were stratified by age in months and calendar year of the questionnaire. In the pooled data, the model was additionally stratified by cohort. The estimates from pooled data were compared with the random-effects meta-analyses based on three cohorts. Multivariable models were adjusted for family history of diabetes, family history of cancer, family history of CVD, physical activity, cigarette smoking (status, pack-years, and time since quitting), multivitamin use, regular aspirin use, regular non-steroidal anti-inflammatory drugs use, postmenopausal hormone use for women, and total energy intake. The model was also adjusted for alcohol intake for dietary patterns that did not include alcohol, such as DASH, hPDI, and DRRD. We did not adjust for BMI in the main analysis but did so in a sensitivity analysis because adiposity is a potential mediator for the diet and chronic disease relationship.
Further, we explored which foods might explain the associations. The definition of food groups has been described previously38. The relationships between pattern scores and food groups were evaluated using the Spearman correlation coefficients. The associations of food groups with major chronic diseases were examined using the Cox proportional hazards regression models. Each food group was modeled as a continuous variable standardized by its increment from the 10th to 90th percentile. The models were adjusted for the same set of covariates used in the main analysis.
We conducted subgroup analyses by age, BMI, sex, smoking status, alcohol, nSES, and race/ethnicity. Potential interaction was assessed by the Wald test (binary variable) or likelihood ratio test (categorical variable). To better understand possible latency, we investigated dietary pattern scores with different latency periods (0-4, 4-8, 8-12, or 12-16 years) 60. For example, in a 4-8 year latency analysis, the pattern score constructed based on the 1990 FFQ was used as the exposure for the follow-up period between 1994 and 1998.
Finally, we conducted several sensitivity analyses. We adjusted for the nSES score to evaluate potential residual confounding. For the rEDIH, rEDIP, AHEI-2010, AMED, and WCRF/AICR dietary score, we evaluated if removing alcohol from the pattern scores influenced the associations. Given that coffee consumption was inversely associated with cardiometabolic disease31, we also examined the associations of DRRD, rEDIH, and rEDIP with major chronic disease after removing coffee from the pattern scores. Because diabetes was identified based on questionnaires, we examined the associations for diabetes with additional censoring at the last questionnaire response. Participants were similarly censored in a sensitivity analysis for major chronic disease. Participants may change their dietary habits after a diagnosis with an intermediate endpoint, such as hypertension, hypercholesterolemia, angina, transient ischemic attack, or coronary artery bypass graft surgery. In a sensitivity analysis, we stopped updating the dietary information at the diagnosis of these intermediate endpoints. Using the same reference group, we compared individuals who were in the highest quintile (the healthiest level) of each dietary pattern with those who were never in the highest quintiles of any pattern.
Statistical analyses were performed using SAS 9.4 (SAS Institute, Cary, NC). We reported unadjusted P values based on two-sided statistical tests. We did not adjust for multiple testing because we aimed to compare the patterns, some of which have been examined individually previously.
Extended Data
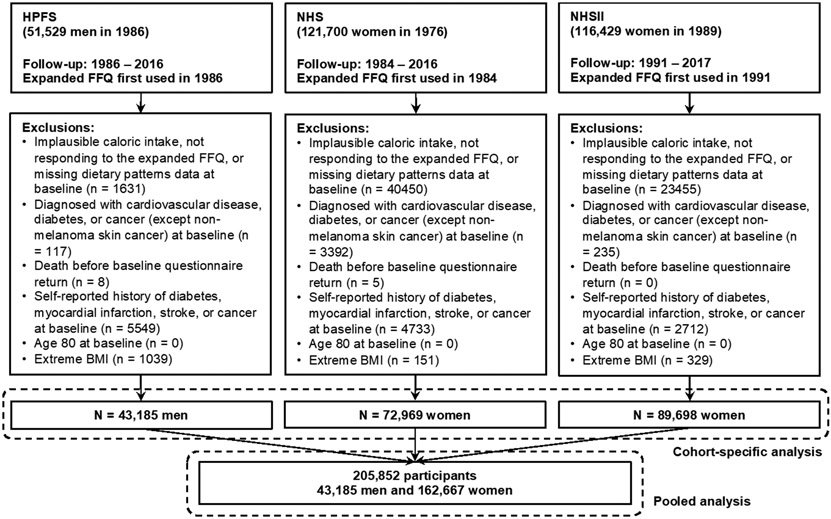
Extended Data Fig.1. Flowchart of participants included in the main analysis.
BMI, body mass index; FFQ, food frequency questionnaires; Nurses’ Health Study (NHS); Health Professionals Follow-up Study (HPFS).
Extended Data Fig.2. Baseline Spearman correlations between energy-adjusted cumulative average dietary patterns in (A) all cohorts, (B) the Health Professionals Follow-up Study, (C) the Nurses’ Health Study, and (D) Nurses’ Health Study II.
P values based on the two-sided tests were <0.0001 for all correlations (not adjusted for multiple comparisons). AHEI-2010, Alternative Healthy Eating Index-2010; AMED, Alternate Mediterranean Diet score; DASH, Dietary Approaches to Stop Hypertension score; DRRD, Diabetes Risk Reduction Diet; hPDI, Healthful plant-based diet index; rEDIH, reversed Empirical dietary index for hyperinsulinemia; rEDIP, reversed Empirical dietary inflammation pattern; WCRF/AICR, World Cancer Research Fund/American Institute for Cancer Research (WCRF/AICR) dietary score.
Extended Data Fig.3. Multivariable-adjusted spline analysis of dietary pattern scores with risk of major chronic disease.
P values for nonlinearity based on the two-sided tests were statistically significant for AMED (P = 0.03), WCRF/AICR (P = 0.007), and rEDIP (P = 0.008) (not adjusted for multiple comparisons). The hazard ratios (black line) and the 95% confidence intervals (grey bands) are shown. The models were adjusted for the same list of covariates as in Table 2. AHEI-2010, Alternative Healthy Eating Index-2010; AMED, Alternate Mediterranean Diet score; DASH, Dietary Approaches to Stop Hypertension score; DRRD, Diabetes Risk Reduction Diet; hPDI, Healthful plant-based diet index; HR, Hazard ratio; rEDIH, reversed Empirical dietary index for hyperinsulinemia; rEDIP, reversed Empirical dietary inflammation pattern; WCRF/AICR, World Cancer Research Fund/American Institute for Cancer Research (WCRF/AICR) dietary score.
Extended Data Fig.4. Multivariable-adjusted associations between cumulative average dietary patterns (comparing the 90th to 10th percentile) and major chronic disease and major components in the pooled data of three cohorts (n = 205,852 participants) with different lags.
Analyses details and corresponding estimates are provided in Extended Data Table 3. The hazard ratios are indicated by the circles and the 95% confidence intervals are reflected by the error bars. AHEI-2010, Alternative Healthy Eating Index-2010; AMED, Alternate Mediterranean Diet score; DASH, Dietary Approaches to Stop Hypertension score; DRRD, Diabetes Risk Reduction Diet; hPDI, Healthful plant-based diet index; rEDIH, reversed Empirical dietary index for hyperinsulinemia; rEDIP, reversed Empirical dietary inflammation pattern; WCRF/AICR, World Cancer Research Fund/American Institute for Cancer Research (WCRF/AICR) dietary score.
Extended Data Table 1.
Associations between cumulative average dietary patterns (comparing the 90th to 10th percentile) and secondary outcomes in the pooled data
| Outcome | Coronary Heart Disease |
Stroke | Obesity-related Cancer |
Smoking-related Cancer |
Alternative Major Chronic Disease |
|
|---|---|---|---|---|---|---|
| Cases | 8,083 | 5,398 | 8,660 | 9,118 | 53,524 | |
| Person-year | 5,185,291 | 5,203,823 | 5,189,782 | 5,204,833 | 4,852,894 | |
| Pattern | Model | HR (95% CI) | HR (95% CI) | HR (95% CI) | HR (95% CI) | HR (95% CI) |
| AHEI-2010 | Age | 0.57 (0.54, 0.61) | 0.72 (0.67, 0.77) | 0.83 (0.78, 0.88) | 0.68 (0.64, 0.72) | 0.60 (0.59, 0.62) |
| MVa | 0.72 (0.68, 0.77) | 0.84 (0.78, 0.91) | 0.92 (0.86, 0.97) | 0.87 (0.82, 0.93) | 0.74 (0.72, 0.76) | |
| MV + nSESb | 0.75 (0.70, 0.80) | 0.86 (0.79, 0.93) | 0.92 (0.87, 0.98) | 0.87 (0.82, 0.93) | 0.76 (0.74, 0.78) | |
| MV + BMIc | 0.75 (0.71, 0.80) | 0.86 (0.79, 0.93) | 0.94 (0.89, 1.00) | 0.88 (0.83, 0.94) | 0.79 (0.77, 0.81) | |
| AMED | Age | 0.60 (0.57, 0.64) | 0.71 (0.66, 0.76) | 0.81 (0.77, 0.86) | 0.64 (0.61, 0.68) | 0.62 (0.61, 0.63) |
| MVa | 0.78 (0.73, 0.83) | 0.84 (0.77, 0.91) | 0.91 (0.86, 0.97) | 0.86 (0.81, 0.92) | 0.78 (0.76, 0.80) | |
| MV + nSESb | 0.80 (0.75, 0.85) | 0.85 (0.79, 0.92) | 0.92 (0.86, 0.97) | 0.86 (0.81, 0.92) | 0.79 (0.77, 0.81) | |
| MV + BMIc | 0.81 (0.76, 0.87) | 0.86 (0.79, 0.93) | 0.94 (0.89, 1.00) | 0.87 (0.82, 0.92) | 0.84 (0.82, 0.86) | |
| hPDI | Age | 0.67 (0.63, 0.71) | 0.81 (0.76, 0.87) | 0.87 (0.83, 0.92) | 0.79 (0.75, 0.84) | 0.68 (0.67, 0.70) |
| MVa | 0.80 (0.75, 0.85) | 0.91 (0.84, 0.98) | 0.94 (0.89, 0.99) | 0.92 (0.87, 0.98) | 0.79 (0.77, 0.81) | |
| MV + nSESb | 0.80 (0.76, 0.86) | 0.92 (0.85, 0.99) | 0.94 (0.89, 0.99) | 0.92 (0.87, 0.98) | 0.80 (0.78, 0.82) | |
| MV + BMIc | 0.82 (0.77, 0.87) | 0.92 (0.86, 1.00) | 0.96 (0.90, 1.01) | 0.93 (0.88, 0.98) | 0.83 (0.81, 0.85) | |
| DASH | Age | 0.59 (0.55, 0.62) | 0.69 (0.64, 0.74) | 0.81 (0.76, 0.86) | 0.60 (0.57, 0.64) | 0.60 (0.59, 0.62) |
| MVa | 0.79 (0.74, 0.84) | 0.84 (0.78, 0.91) | 0.94 (0.88, 1.00) | 0.87 (0.82, 0.92) | 0.78 (0.77, 0.80) | |
| MV + nSESb | 0.81 (0.76, 0.87) | 0.86 (0.79, 0.93) | 0.94 (0.89, 1.00) | 0.87 (0.82, 0.92) | 0.80 (0.78, 0.82) | |
| MV + BMIc | 0.81 (0.76, 0.87) | 0.86 (0.79, 0.93) | 0.96 (0.90, 1.02) | 0.87 (0.82, 0.93) | 0.83 (0.81, 0.85) | |
| DRRD | Age | 0.58 (0.55, 0.62) | 0.67 (0.62, 0.72) | 0.84 (0.79, 0.89) | 0.73 (0.69, 0.77) | 0.58 (0.57, 0.60) |
| MVa | 0.71 (0.67, 0.76) | 0.76 (0.70, 0.82) | 0.91 (0.86, 0.97) | 0.88 (0.83, 0.94) | 0.70 (0.68, 0.71) | |
| MV + nSESb | 0.73 (0.69, 0.78) | 0.77 (0.71, 0.83) | 0.91 (0.86, 0.97) | 0.88 (0.83, 0.94) | 0.71 (0.69, 0.72) | |
| MV + BMIc | 0.74 (0.69, 0.79) | 0.77 (0.71, 0.83) | 0.94 (0.88, 0.99) | 0.89 (0.84, 0.94) | 0.74 (0.72, 0.76) | |
| WCRF/AICR | Age | 0.77 (0.73, 0.82) | 0.87 (0.81, 0.93) | 0.89 (0.85, 0.94) | 0.71 (0.67, 0.75) | 0.81 (0.79, 0.83) |
| MVa | 1.00 (0.94, 1.06) | 1.03 (0.95, 1.11) | 1.00 (0.95, 1.06) | 0.95 (0.90, 1.01) | 1.00 (0.98, 1.03) | |
| MV + nSESb | 1.01 (0.95, 1.07) | 1.03 (0.96, 1.11) | 1.00 (0.95, 1.06) | 0.95 (0.90, 1.01) | 1.01 (0.99, 1.04) | |
| MV + BMIc | 0.98 (0.92, 1.04) | 1.01 (0.94, 1.09) | 0.98 (0.93, 1.04) | 0.95 (0.89, 1.00) | 0.97 (0.95, 1.00) | |
| rEDIH | Age | 0.56 (0.53, 0.59) | 0.71 (0.66, 0.76) | 0.81 (0.76, 0.85) | 0.80 (0.76, 0.85) | 0.53 (0.51, 0.54) |
| MVa | 0.63 (0.60, 0.67) | 0.76 (0.71, 0.82) | 0.84 (0.80, 0.89) | 0.89 (0.84, 0.94) | 0.59 (0.58, 0.60) | |
| MV + nSESb | 0.65 (0.61, 0.69) | 0.77 (0.72, 0.83) | 0.84 (0.80, 0.89) | 0.89 (0.84, 0.94) | 0.60 (0.59, 0.61) | |
| MV + BMIc | 0.71 (0.67, 0.76) | 0.82 (0.77, 0.89) | 0.93 (0.88, 0.99) | 0.92 (0.87, 0.97) | 0.73 (0.71, 0.75) | |
| rEDIP | Age | 0.63 (0.59, 0.66) | 0.75 (0.70, 0.81) | 0.83 (0.79, 0.88) | 0.95 (0.90, 1.00) | 0.59 (0.58, 0.60) |
| MVa | 0.65 (0.61, 0.68) | 0.77 (0.71, 0.82) | 0.83 (0.79, 0.87) | 0.91 (0.87, 0.96) | 0.62 (0.60, 0.63) | |
| MV + nSESb | 0.66 (0.62, 0.69) | 0.77 (0.72, 0.83) | 0.83 (0.79, 0.88) | 0.91 (0.87, 0.96) | 0.62 (0.61, 0.64) | |
| MV + BMIc | 0.71 (0.67, 0.75) | 0.82 (0.76, 0.88) | 0.90 (0.86, 0.96) | 0.94 (0.89, 0.99) | 0.73 (0.72, 0.75) | |
AHEI-2010, Alternative Healthy Eating Index-2010; AMED, Alternate Mediterranean Diet score; BMI, body mass index; CI, Confidence interval; DASH, Dietary Approaches to Stop Hypertension score; DRRD, Diabetes Risk Reduction Diet; hPDI, Healthful plant-based diet index; HR, Hazard ratio; MV, multivariable; nSES, neighborhood socioeconomic status; rEDIH, reversed Empirical dietary index for hyperinsulinemia; rEDIP, reversed Empirical dietary inflammation pattern; WCRF/AICR, World Cancer Research Fund/American Institute for Cancer Research (WCRF/AICR) dietary score.
Analyses were stratified by age (in month), calendar year, and cohort. MV model: adjusted for physical activity (<3.0, 3.0-8.9, 9.0-17.9, 18.0-26.9, 27.0-41.9, or ≥42 MET-h/week), cigarette smoking status (never, former quitting ≥10 y, former quitting <10 y, current), cigarette smoking pack-years (0, 1-4, 5-14, 15-24, or ≥25 pack-years), multivitamin use (yes or no), regular aspirin use (yes or no), regular non-steroidal anti-inflammatory drugs use (yes or no), postmenopausal hormone use (premenopausal, never, former, or current use) for women, and total energy intake (quintiles). Alcohol consumption (<5.0, 5.0-14.9, or ≥15.0 g/d) was adjusted for DASH, hPDI, and DRRD. For alternative major chronic disease, the model was additionally adjusted for family history of diabetes (yes or no), family history of cancer (yes or no), family history of cardiovascular disease (yes or no). For coronary heart disease and stroke, the model was additionally adjusted for family history of cardiovascular disease (yes or no). For obesity-related or smoking-related cancer, the model was additionally adjusted for family history of cancer (yes or no) and height (continuous).
Additionally adjusted for nSES (continuous).
Additionally adjusted for BMI (continuous).
Extended Data Table 2.
Multivariable-adjusted associations of the cumulative average dietary patterns (comparing the 90th to 10th percentile) with major chronic disease in subgroups
| Agea, year | BMIb, kg/m2 | Sexc | ||||
|---|---|---|---|---|---|---|
| <65 | ≥65 | <25 | ≥25 | Men | Women | |
| Case | 24,246 | 20,729 | 16,250 | 28,725 | 14427 | 30,548 |
| Person-year | 3,719,096 | 1,133,799 | 2,785,883 | 2,067,011 | 879,987 | 3,972,907 |
| AHEI-2010 | 0.71 (0.68, 0.74) | 0.83 (0.79, 0.86) | 0.85 (0.82, 0.89) | 0.76 (0.73, 0.79) | 0.84 (0.81, 0.88) | 0.72 (0.70, 0.75) |
| AMED | 0.76 (0.73, 0.78) | 0.84 (0.81, 0.87) | 0.87 (0.83, 0.91) | 0.80 (0.77, 0.83) | 0.83 (0.79, 0.87) | 0.78 (0.75, 0.80) |
| hPDI | 0.75 (0.73, 0.78) | 0.86 (0.83, 0.89) | 0.87 (0.84, 0.91) | 0.79 (0.76, 0.81) | 0.86 (0.82, 0.90) | 0.77 (0.75, 0.80) |
| DASH | 0.73 (0.71, 0.76) | 0.85 (0.81, 0.88) | 0.85 (0.81, 0.89) | 0.78 (0.75, 0.81) | 0.83 (0.79, 0.87) | 0.76 (0.74, 0.79) |
| DRRD | 0.66 (0.63, 0.68) | 0.78 (0.75, 0.81) | 0.80 (0.76, 0.84) | 0.69 (0.66, 0.71) | 0.82 (0.78, 0.85) | 0.66 (0.64, 0.68) |
| WCRF/AICR | 1.03 (0.99, 1.07) | 0.97 (0.93, 1.01) | 0.96 (0.93, 1.01) | 0.99 (0.95, 1.02) | 0.95 (0.91, 0.99) | 1.03 (1.00, 1.06) |
| rEDIH | 0.51 (0.50, 0.53) | 0.71 (0.68, 0.73) | 0.78 (0.75, 0.81) | 0.63 (0.61, 0.65) | 0.74 (0.70, 0.77) | 0.53 (0.51, 0.54) |
| rEDIP | 0.55 (0.53, 0.56) | 0.72 (0.70, 0.75) | 0.76 (0.73, 0.79) | 0.64 (0.63, 0.66) | 0.77 (0.74, 0.80) | 0.55 (0.53, 0.56) |
| Smoking Statusd | Alcohole, g/day | nSESf | ||||
| Never | Former | Current | ≤14 | >14 | < Median | |
| Case | 19,941 | 18,719 | 6,315 | 37,456 | 7,519 | 24,693 |
| Person-year | 2,689,238 | 1,671,370 | 492,287 | 4,228,443 | 624,451 | 2,424,086 |
| AHEI-2010 | 0.74 (0.71, 0.77) | 0.76 (0.73, 0.79) | 0.79 (0.73, 0.85) | 0.75 (0.73, 0.78) | 0.80 (0.75, 0.85) | 0.79 (0.77, 0.82) |
| AMED | 0.77 (0.74, 0.80) | 0.79 (0.76, 0.82) | 0.82 (0.77, 0.89) | 0.79 (0.76, 0.81) | 0.82 (0.76, 0.87) | 0.82 (0.79, 0.85) |
| hPDI | 0.78 (0.75, 0.81) | 0.79 (0.75, 0.82) | 0.87 (0.81, 0.94) | 0.79 (0.77, 0.82) | 0.83 (0.78, 0.89) | 0.81 (0.78, 0.84) |
| DASH | 0.73 (0.70, 0.76) | 0.78 (0.75, 0.82) | 0.87 (0.81, 0.94) | 0.77 (0.75, 0.80) | 0.81 (0.76, 0.87) | 0.80 (0.77, 0.83) |
| DRRD | 0.68 (0.65, 0.70) | 0.70 (0.67, 0.73) | 0.78 (0.72, 0.84) | 0.70 (0.68, 0.73) | 0.75 (0.70, 0.80) | 0.71 (0.69, 0.74) |
| WCRF/AICR | 0.99 (0.95, 1.03) | 1.00 (0.96, 1.04) | 1.04 (0.96, 1.12) | 0.99 (0.96, 1.02) | 0.89 (0.82, 0.96) | 1.04 (1.00, 1.07) |
| rEDIH | 0.51 (0.50, 0.53) | 0.60 (0.57, 0.62) | 0.72 (0.67, 0.77) | 0.55 (0.53, 0.56) | 0.77 (0.73, 0.81) | 0.59 (0.57, 0.61) |
| rEDIP | 0.55 (0.53, 0.57) | 0.62 (0.60, 0.64) | 0.75 (0.71, 0.80) | 0.57 (0.55, 0.58) | 0.80 (0.76, 0.84) | 0.60 (0.58, 0.62) |
| nSESg | Race/Ethnicityg | |||||
| ≥ Median | Non-Hispanic White |
Asian | Hispanic | Black | Unknown | |
| Case | 20,282 | 39,433 | 554 | 354 | 686 | 3,948 |
| Person-year | 2,428,808 | 4,501,212 | 62,284 | 47,875 | 58,149 | 183,374 |
| AHEI-2010 | 0.76 (0.73, 0.79) | 0.76 (0.74, 0.78) | 0.91 (0.65, 1.28) | 0.51 (0.34, 0.78) | 0.72 (0.53, 0.97) | 0.85 (0.78, 0.94) |
| AMED | 0.78 (0.75, 0.81) | 0.79 (0.77, 0.81) | 0.78 (0.55, 1.10) | 0.55 (0.37, 0.82) | 0.62 (0.46, 0.86) | 0.88 (0.80, 0.96) |
| hPDI | 0.80 (0.77, 0.83) | 0.79 (0.77, 0.82) | 0.87 (0.63, 1.20) | 0.44 (0.30, 0.66) | 0.81 (0.61, 1.07) | 0.96 (0.88, 1.05) |
| DASH | 0.78 (0.74, 0.81) | 0.77 (0.75, 0.80) | 0.82 (0.59, 1.14) | 0.46 (0.31, 0.69) | 0.61 (0.45, 0.82) | 0.92 (0.84, 1.00) |
| DRRD | 0.72 (0.69, 0.74) | 0.70 (0.68, 0.72) | 0.80 (0.56, 1.12) | 0.47 (0.32, 0.71) | 0.63 (0.47, 0.85) | 0.84 (0.76, 0.92) |
| WCRF/AICR | 0.98 (0.94, 1.01) | 1.01 (0.98, 1.04) | 1.07 (0.78, 1.46) | 0.78 (0.53, 1.14) | 0.93 (0.70, 1.24) | 0.97 (0.89, 1.06) |
| rEDIH | 0.60 (0.58, 0.62) | 0.57 (0.55, 0.58) | 0.55 (0.39, 0.77) | 0.47 (0.32, 0.69) | 0.65 (0.49, 0.87) | 0.87 (0.80, 0.94) |
| rEDIP | 0.64 (0.62, 0.66) | 0.60 (0.58, 0.61) | 0.61 (0.44, 0.84) | 0.52 (0.37, 0.75) | 0.59 (0.44, 0.79) | 0.86 (0.79, 0.92) |
AHEI-2010, Alternative Healthy Eating Index-2010; AMED, Alternate Mediterranean Diet score; BMI, body mass index; DASH, Dietary Approaches to Stop Hypertension score; DRRD, Diabetes Risk Reduction Diet; hPDI, Healthful plant-based diet index; MV, multivariable; nSES, neighborhood socioeconomic status; rEDIH, reversed Empirical dietary index for hyperinsulinemia; rEDIP, reversed Empirical dietary inflammation pattern; WCRF/AICR, World Cancer Research Fund/American Institute for Cancer Research (WCRF/AICR) dietary score. Analyses were stratified by age (in month), calendar year, and cohort.
Models were adjusted for family history of diabetes (yes or no), family history of cancer (yes or no), family history of cardiovascular disease (yes or no), physical activity (<3.0, 3.0-8.9, 9.0-17.9, 18.0-26.9, 27.0-41.9, or ≥42 MET-h/week), cigarette smoking status (never, former quitting ≥10 y, former quitting <10 y, current), cigarette smoking pack-years (0, 1-4, 5-14, 15-24, or ≥25 pack-years), multivitamin use (yes or no), regular aspirin use (yes or no), regular non-steroidal anti-inflammatory drugs use (yes or no), postmenopausal hormone use (premenopausal, never, former, or current use) for women, and total energy intake (quintiles). For DASH, hPDI, and DRRD, alcohol consumption (<5.0, 5.0-14.9, or ≥15.0 g/d) was additionally adjusted for. We reported unadjusted P values based on two-sided statistical tests.
P values for the Wald test of interaction term (Pattern x Age) were <0.0001 for all pattern scores except WCRF/AICR (P = 0.21).
P values for the Wald test of interaction term (Pattern x BMI) were <0.0001 for all pattern scores except AMED (P = 0.80), hPDI (P = 0.006), DASH (P = 0.46), and WCRF/AICR (P = 0.54).
P values for the Wald test of interaction term (Pattern x Sex) were <0.0001 for all pattern scores except WCRF/AICR (P = 0.30).
P values for the Likelihood ratio test of interaction terms (Pattern x Smoking status) were <0.0001 for all pattern scores.
P values for the Wald test of interaction term (Pattern x Alcohol) were <0.05 for DRRD (P = 0.007), WCRF/AICR (P = 0.04), rEDIH (P <0.0001), and rEDIP (P <0.0001.
P values for the Wald test of interaction term (Pattern x nSES) were <0.05 for AMED (P = 0.0009), DASH (P = 0.02), DRRD (P = 0.04), WCRF/AICR (P = 0.004), and rEDIP (P = 0.02).
P values for the Likelihood ratio test of interaction terms (Pattern x Race/Ethnicity) were <0.0001 for all pattern scores except WCRF/AICR (P = 0.03).
Extended Data Table 3.
Association between cumulative average dietary patterns (comparing the 90th to 10th percentile) and major chronic disease and major components in the pooled data with different latency periods
| Latency period | No lag | 4 years | 8 years | 12 years | 16 years | |
|---|---|---|---|---|---|---|
| Outcome | Pattern | HR (95% CI) | HR (95% CI) | HR (95% CI) | HR (95% CI) | HR (95% CI) |
| Major Chronic Disease | Cases | 44,975 | 42,698 | 38,080 | 31,232 | 22,585 |
| Person-year | 4,852,894 | 4,135,546 | 3,399,860 | 2,652,663 | 1,925,289 | |
| AHEI-2010 | 0.75 (0.73, 0.77) | 0.78 (0.76, 0.80) | 0.79 (0.77, 0.81) | 0.82 (0.80, 0.85) | 0.83 (0.80, 0.86) | |
| AMED | 0.78 (0.76, 0.80) | 0.81 (0.79, 0.83) | 0.81 (0.79, 0.84) | 0.84 (0.81, 0.87) | 0.86 (0.83, 0.89) | |
| hPDI | 0.77 (0.75, 0.79) | 0.79 (0.77, 0.82) | 0.81 (0.79, 0.84) | 0.84 (0.81, 0.87) | 0.88 (0.85, 0.91) | |
| DASH | 0.77 (0.75, 0.79) | 0.78 (0.76, 0.80) | 0.80 (0.78, 0.82) | 0.81 (0.79, 0.84) | 0.81 (0.78, 0.84) | |
| DRRD | 0.69 (0.67, 0.71) | 0.72 (0.70, 0.74) | 0.75 (0.72, 0.77) | 0.77 (0.74, 0.79) | 0.78 (0.75, 0.81) | |
| WCRF/AICR | 0.98 (0.96, 1.01) | 0.97 (0.95, 1.00) | 0.97 (0.94, 1.00) | 0.97 (0.94, 1.00) | 0.96 (0.92, 0.99) | |
| rEDIH | 0.61 (0.59, 0.62) | 0.63 (0.62, 0.65) | 0.66 (0.64, 0.68) | 0.69 (0.67, 0.71) | 0.72 (0.69, 0.74) | |
| rEDIP | 0.63 (0.61, 0.64) | 0.66 (0.64, 0.68) | 0.69 (0.67, 0.71) | 0.72 (0.70, 0.74) | 0.74 (0.72, 0.77) | |
| Major Cardiovascular Disease | Cases | 12,962 | 12,844 | 11,960 | 10,114 | 7,694 |
| Person-year | 5,148,378 | 4,402,319 | 3,616,470 | 2,805,738 | 2,012,374 | |
| AHEI-2010 | 0.77 (0.73, 0.81) | 0.79 (0.75, 0.83) | 0.82 (0.78, 0.86) | 0.83 (0.78, 0.87) | 0.86 (0.81, 0.92) | |
| AMED | 0.79 (0.75, 0.83) | 0.80 (0.77, 0.84) | 0.86 (0.82, 0.90) | 0.85 (0.81, 0.90) | 0.92 (0.86, 0.98) | |
| hPDI | 0.81 (0.77, 0.85) | 0.82 (0.79, 0.86) | 0.88 (0.84, 0.92) | 0.88 (0.84, 0.93) | 0.95 (0.90, 1.01) | |
| DASH | 0.81 (0.77, 0.85) | 0.81 (0.77, 0.85) | 0.86 (0.82, 0.91) | 0.84 (0.79, 0.88) | 0.88 (0.83, 0.94) | |
| DRRD | 0.73 (0.70, 0.77) | 0.76 (0.72, 0.80) | 0.80 (0.76, 0.84) | 0.78 (0.74, 0.83) | 0.82 (0.77, 0.87) | |
| WCRF/AICR | 0.99 (0.95, 1.04) | 0.98 (0.93, 1.03) | 1.00 (0.95, 1.05) | 0.95 (0.90, 1.00) | 0.98 (0.92, 1.04) | |
| rEDIH | 0.70 (0.67, 0.73) | 0.72 (0.69, 0.75) | 0.79 (0.75, 0.83) | 0.83 (0.79, 0.87) | 0.84 (0.79, 0.89) | |
| rEDIP | 0.71 (0.68, 0.74) | 0.73 (0.70, 0.76) | 0.78 (0.75, 0.82) | 0.82 (0.78, 0.86) | 0.82 (0.78, 0.87) | |
| Type 2 Diabetes | Cases | 18,615 | 16,588 | 15,056 | 11,951 | 8,077 |
| Person-year | 4,630,725 | 3,726,657 | 3,124,205 | 2,365,983 | 1,646,645 | |
| AHEI-2010 | 0.58 (0.55, 0.60) | 0.62 (0.60, 0.65) | 0.65 (0.62, 0.68) | 0.72 (0.68, 0.76) | 0.72 (0.68, 0.77) | |
| AMED | 0.69 (0.66, 0.72) | 0.74 (0.71, 0.77) | 0.73 (0.70, 0.77) | 0.77 (0.73, 0.81) | 0.77 (0.72, 0.81) | |
| hPDI | 0.65 (0.62, 0.67) | 0.68 (0.65, 0.71) | 0.70 (0.67, 0.73) | 0.75 (0.72, 0.79) | 0.77 (0.73, 0.82) | |
| DASH | 0.64 (0.62, 0.67) | 0.68 (0.65, 0.71) | 0.69 (0.66, 0.72) | 0.73 (0.69, 0.77) | 0.71 (0.66, 0.75) | |
| DRRD | 0.54 (0.51, 0.56) | 0.58 (0.56, 0.60) | 0.59 (0.57, 0.62) | 0.65 (0.62, 0.68) | 0.65 (0.61, 0.69) | |
| WCRF/AICR | 0.98 (0.94, 1.02) | 0.98 (0.94, 1.02) | 0.97 (0.93, 1.01) | 1.02 (0.97, 1.07) | 0.98 (0.92, 1.04) | |
| rEDIH | 0.38 (0.37, 0.39) | 0.42 (0.40, 0.43) | 0.44 (0.42, 0.46) | 0.47 (0.45, 0.49) | 0.49 (0.47, 0.52) | |
| rEDIP | 0.41 (0.40, 0.43) | 0.45 (0.43, 0.47) | 0.48 (0.46, 0.50) | 0.51 (0.49, 0.53) | 0.53 (0.51, 0.56) | |
| Total Cancer | Cases | 17,909 | 16,595 | 14,176 | 11,127 | 7,682 |
| Person-year | 5,138,951 | 4,397,783 | 3,616,916 | 2,808,237 | 2,015,999 | |
| AHEI-2010 | 0.94 (0.90, 0.99) | 0.95 (0.91, 0.99) | 0.94 (0.90, 0.99) | 0.93 (0.89, 0.98) | 0.97 (0.91, 1.03) | |
| AMED | 0.93 (0.90, 0.97) | 0.93 (0.89, 0.97) | 0.90 (0.86, 0.94) | 0.93 (0.88, 0.98) | 0.96 (0.90, 1.02) | |
| hPDI | 0.95 (0.91, 0.99) | 0.95 (0.91, 0.99) | 0.93 (0.89, 0.97) | 0.93 (0.88, 0.98) | 0.96 (0.90, 1.02) | |
| DASH | 0.96 (0.92, 1.00) | 0.92 (0.89, 0.97) | 0.90 (0.86, 0.95) | 0.91 (0.87, 0.96) | 0.92 (0.86, 0.98) | |
| DRRD | 0.93 (0.89, 0.97) | 0.92 (0.88, 0.96) | 0.93 (0.88, 0.97) | 0.91 (0.87, 0.96) | 0.95 (0.89, 1.01) | |
| WCRF/AICR | 1.03 (0.99, 1.07) | 1.00 (0.96, 1.04) | 0.96 (0.92, 1.01) | 0.95 (0.90, 1.00) | 0.96 (0.90, 1.02) | |
| rEDIH | 0.91 (0.87, 0.94) | 0.91 (0.87, 0.94) | 0.91 (0.88, 0.95) | 0.93 (0.89, 0.98) | 0.97 (0.91, 1.03) | |
| rEDIP | 0.89 (0.86, 0.92) | 0.90 (0.87, 0.94) | 0.91 (0.88, 0.95) | 0.95 (0.91, 1.00) | 0.98 (0.93, 1.04) | |
AHEI-2010, Alternative Healthy Eating Index-2010; AMED, Alternate Mediterranean Diet score; CI, Confidence interval; DASH, Dietary Approaches to Stop Hypertension score; DRRD, Diabetes Risk Reduction Diet; hPDI, Healthful plant-based diet index; HR, Hazard ratio; MV, multivariable; rEDIH, reversed Empirical dietary index for hyperinsulinemia; rEDIP, reversed Empirical dietary inflammation pattern; WCRF/AICR, World Cancer Research Fund/American Institute for Cancer Research (WCRF/AICR) dietary score.
Analyses were stratified by age (in month), calendar year, and cohort. MV model: adjusted for physical activity (<3.0, 3.0-8.9, 9.0-17.9, 18.0-26.9, 27.0-41.9, or ≥42 MET-h/week), cigarette smoking status (never, former quitting ≥10 y, former quitting <10 y, current), cigarette smoking pack-years (0, 1-4, 5-14, 15-24, or ≥25 pack-years), multivitamin use (yes or no), regular aspirin use (yes or no), regular non-steroidal anti-inflammatory drugs use (yes or no), postmenopausal hormone use (premenopausal, never, former, or current use) for women, and total energy intake (quintiles). For DASH, hPDI, and DRRD, alcohol consumption (<5.0, 5.0-14.9, or ≥15.0 g/d) was additionally adjusted for. For major chronic disease, the model was additionally adjusted for family history of diabetes (yes or no), family history of cancer (yes or no), and family history of cardiovascular disease (yes or no). For type 2 diabetes, the model was additionally adjusted for family history of diabetes (yes or no). For major cardiovascular disease, the model was additionally adjusted for family history of cardiovascular disease (yes or no). For total cancer, the model was additionally adjusted for family history of cancer (yes or no) and height (continuous).
Extended Data Table 4.
Association between cumulative average dietary patterns without alcohol component (comparing the 90th to 10th percentile) and outcomes in the pooled data
| Outcome | Major Chronic Disease | Major Cardiovascular Disease |
Type 2 Diabetes | Total Cancer | |
|---|---|---|---|---|---|
| Cases | 44,975 | 12,962 | 18,615 | 17,909 | |
| Person-year | 4,852,894 | 5,148,378 | 4,630,725 | 5,138,951 | |
| AHEI-2010 | Age | 0.69 (0.67, 0.71) | 0.66 (0.63, 0.69) | 0.57 (0.55, 0.59) | 0.82 (0.79, 0.86) |
| MV | 0.83 (0.81, 0.85) | 0.82 (0.78, 0.86) | 0.74 (0.71, 0.77) | 0.97 (0.93, 1.01) | |
| AMED | Age | 0.68 (0.67, 0.70) | 0.66 (0.63, 0.69) | 0.62 (0.60, 0.65) | 0.78 (0.75, 0.81) |
| MV | 0.84 (0.82, 0.86) | 0.83 (0.79, 0.87) | 0.81 (0.77, 0.84) | 0.94 (0.90, 0.98) | |
| WCRF/AICR | Age | 0.72 (0.70, 0.73) | 0.72 (0.68, 0.75) | 0.57 (0.55, 0.59) | 0.89 (0.85, 0.92) |
| MV | 0.86 (0.84, 0.89) | 0.88 (0.84, 0.92) | 0.77 (0.73, 0.80) | 1.00 (0.96, 1.05) | |
| rEDIH | Age | 0.55 (0.54, 0.56) | 0.64 (0.61, 0.67) | 0.33 (0.32, 0.35) | 0.83 (0.80, 0.86) |
| MV | 0.62 (0.60, 0.63) | 0.72 (0.68, 0.75) | 0.41 (0.39, 0.42) | 0.89 (0.85, 0.92) | |
| rEDIP | Age | 0.61 (0.60, 0.63) | 0.69 (0.66, 0.72) | 0.39 (0.38, 0.41) | 0.87 (0.84, 0.90) |
| MV | 0.66 (0.64, 0.67) | 0.73 (0.70, 0.76) | 0.47 (0.45, 0.48) | 0.87 (0.84, 0.90) | |
AHEI-2010, Alternative Healthy Eating Index-2010; AMED, Alternate Mediterranean Diet score; CI, Confidence interval; CVD, cardiovascular disease; HR, Hazard ratio; MV, multivariable; rEDIH, reversed Empirical dietary index for hyperinsulinemia; rEDIP, reversed Empirical dietary inflammation pattern; WCRF/AICR, World Cancer Research Fund/American Institute for Cancer Research (WCRF/AICR) dietary score.
Analyses were stratified by age (in month), calendar year, and cohort. MV model: adjusted for physical activity (<3.0, 3.0-8.9, 9.0-17.9, 18.0-26.9, 27.0-41.9, or ≥42 MET-h/week), cigarette smoking status (never, former quitting ≥10 y, former quitting <10 y, current), cigarette smoking pack-years (0, 1-4, 5-14, 15-24, or ≥25 pack-years), multivitamin use (yes or no), regular aspirin use (yes or no), regular non-steroidal anti-inflammatory drugs use (yes or no), postmenopausal hormone use (premenopausal, never, former, or current use) for women, and total energy intake (quintiles). Alcohol consumption (<5.0, 5.0-14.9, or ≥15.0 g/d) was adjusted for DASH, hPDI, and DRRD. For major chronic disease, the model was additionally adjusted for family history of diabetes (yes or no), family history of cancer (yes or no), and family history of cardiovascular disease (yes or no). For type 2 diabetes, the model was additionally adjusted for family history of diabetes (yes or no). For major cardiovascular disease, the model was additionally adjusted for family history of cardiovascular disease (yes or no). For total cancer, the model was additionally adjusted for family history of cancer (yes or no) and height (continuous).
Extended Data Table 5.
Association between cumulative average dietary patterns without coffee component (comparing the 90th to 10th percentile) and outcomes in the pooled data
| Outcome | Major Chronic Disease | Major Cardiovascular Disease |
Type 2 Diabetes | Total Cancer | |
|---|---|---|---|---|---|
| Cases | 44,975 | 12,962 | 18,615 | 17,909 | |
| Person-year | 4,852,894 | 5,148,378 | 4,630,725 | 5,138,951 | |
| DRRD | Age | 0.62 (0.60, 0.63) | 0.61 (0.58, 0.64) | 0.49 (0.47, 0.51) | 0.79 (0.76, 0.82) |
| MV | 0.74 (0.72, 0.76) | 0.76 (0.72, 0.80) | 0.62 (0.60, 0.65) | 0.93 (0.89, 0.97) | |
| rEDIH | Age | 0.53 (0.52, 0.54) | 0.60 (0.58, 0.63) | 0.31 (0.30, 0.32) | 0.81 (0.78, 0.84) |
| MV | 0.61 (0.59, 0.62) | 0.71 (0.67, 0.74) | 0.38 (0.36, 0.39) | 0.91 (0.87, 0.94) | |
| rEDIP | Age | 0.58 (0.57, 0.59) | 0.64 (0.62, 0.67) | 0.36 (0.34, 0.37) | 0.85 (0.82, 0.88) |
| MV | 0.66 (0.64, 0.67) | 0.73 (0.70, 0.76) | 0.42 (0.41, 0.44) | 0.92 (0.88, 0.95) | |
CI, Confidence interval; CVD, cardiovascular disease; DRRD, Diabetes Risk Reduction Diet; HR, Hazard ratio; MV, multivariable; rEDIH, reversed Empirical dietary index for hyperinsulinemia; rEDIP, reversed Empirical dietary inflammation pattern.
Analyses were stratified by age (in month), calendar year, and cohort. MV model: adjusted for physical activity (<3.0, 3.0-8.9, 9.0-17.9, 18.0-26.9, 27.0-41.9, or ≥42 MET-h/week), cigarette smoking status (never, former quitting ≥10 y, former quitting <10 y, current), cigarette smoking pack-years (0, 1-4, 5-14, 15-24, or ≥25 pack-years), multivitamin use (yes or no), regular aspirin use (yes or no), regular non-steroidal anti-inflammatory drugs use (yes or no), postmenopausal hormone use (premenopausal, never, former, or current use) for women, and total energy intake (quintiles). Alcohol consumption (<5.0, 5.0-14.9, or ≥15.0 g/d) was adjusted for DASH, hPDI, and DRRD. For major chronic disease, the model was additionally adjusted for family history of diabetes (yes or no), family history of cancer (yes or no), and family history of cardiovascular disease (yes or no). For type 2 diabetes, the model was additionally adjusted for family history of diabetes (yes or no). For major cardiovascular disease, the model was additionally adjusted for family history of cardiovascular disease (yes or no). For total cancer, the model was additionally adjusted for family history of cancer (yes or no) and height (continuous).
Extended Data Table 6.
Associations between cumulative average dietary patterns and risk of major chronic disease using the same reference group
| Pattern | Model | Reference group | Highest Quintile |
|---|---|---|---|
| AHEI-2010 | Cases | 23,708 | 7,660 |
| Person-year | 2,292,086 | 967,242 | |
| Age | 1 | 0.66 (0.64, 0.68) | |
| MV | 1 | 0.75 (0.73, 0.77) | |
| AMED | Cases | 23,708 | 7,625 |
| Person-year | 2,292,086 | 972,409 | |
| Age | 1 | 0.67 (0.65, 0.68) | |
| MV | 1 | 0.77 (0.75, 0.79) | |
| hPDI | Cases | 23,708 | 8,063 |
| Person-year | 2,292,086 | 972,078 | |
| Age | 1 | 0.69 (0.67, 0.71) | |
| MV | 1 | 0.78 (0.76, 0.80) | |
| DASH | Cases | 23,708 | 7,857 |
| Person-year | 2,292,086 | 972,141 | |
| Age | 1 | 0.66 (0.65, 0.68) | |
| MV | 1 | 0.78 (0.76, 0.80) | |
| DRRD | Cases | 23,708 | 7,463 |
| Person-year | 2,292,086 | 972,819 | |
| Age | 1 | 0.64 (0.63, 0.66) | |
| MV | 1 | 0.74 (0.72, 0.76) | |
| WCRF/AICR | Cases | 23,708 | 8,841 |
| Person-year | 2,292,086 | 970,161 | |
| Age | 1 | 0.75 (0.73, 0.77) | |
| MV | 1 | 0.86 (0.84, 0.88) | |
| rEDIH | Cases | 23,708 | 7,164 |
| Person-year | 2,292,086 | 969,987 | |
| Age | 1 | 0.62 (0.60, 0.63) | |
| MV | 1 | 0.67 (0.65, 0.69) | |
| rEDIP | Cases | 23,708 | 6,690 |
| Person-year | 2,292,086 | 971,184 | |
| Age | 1 | 0.64 (0.62, 0.66) | |
| MV | 1 | 0.67 (0.65, 0.69) |
AHEI-2010, Alternative Healthy Eating Index-2010; AMED, Alternate Mediterranean Diet score; CI, Confidence interval; DASH, Dietary Approaches to Stop Hypertension score; DRRD, Diabetes Risk Reduction Diet; hPDI, Healthful plant-based diet index; HR, Hazard ratio; MV, multivariable; rEDIH, reversed Empirical dietary index for hyperinsulinemia; rEDIP, reversed Empirical dietary inflammation pattern; WCRF/AICR, World Cancer Research Fund/American Institute for Cancer Research (WCRF/AICR) dietary score.
Participants who were in the highest quintile of each dietary pattern were compared with those who were never in the highest quintile of any pattern. Analyses were stratified by age (in month), calendar year, and cohort. MV model: adjusted for family history of diabetes (yes or no), family history of cancer (yes or no), family history of cardiovascular disease (yes or no), physical activity (<3.0, 3.0-8.9, 9.0-17.9, 18.0-26.9, 27.0-41.9, or ≥42 MET-h/week), cigarette smoking status (never, former quitting ≥10 y, former quitting <10 y, current), cigarette smoking pack-years (0, 1-4, 5-14, 15-24, or ≥25 pack-years), multivitamin use (yes or no), regular aspirin use (yes or no), regular non-steroidal anti-inflammatory drugs use (yes or no), postmenopausal hormone use (premenopausal, never, former, or current use) for women, and total energy intake (quintiles). For DASH, hPDI, and DRRD, alcohol consumption (<5.0, 5.0-14.9, or ≥15.0 g/d) was additionally adjusted for.
Supplementary Material
Acknowledgements
The authors would like to acknowledge the contribution to this study from central cancer registries supported through the Centers for Disease Control and Prevention’s National Program of Cancer Registries (NPCR) and/or the National Cancer Institute’s Surveillance, Epidemiology, and End Results (SEER) Program. Central registries may also be supported by state agencies, universities, and cancer centers. Participating central cancer registries include the following: Alabama, Alaska, Arizona, Arkansas, California, Delaware, Colorado, Connecticut, Florida, Georgia, Hawaii, Idaho, Indiana, Iowa, Kentucky, Louisiana, Maine, Maryland, Massachusetts, Michigan, Mississippi, Montana, Nebraska, Nevada, New Hampshire, New Jersey, New Mexico, New York, North Carolina, North Dakota, Ohio, Oklahoma, Oregon, Pennsylvania, Puerto Rico, Rhode Island, Seattle SEER Registry, South Carolina, Tennessee, Texas, Utah, Virginia, West Virginia, Wyoming.
This work was supported by grants from the National Institutes of Health (UM1 CA186107 [A.H.E.], P01 CA087969 [A.H.E., E.L.G.], R01 HL034594, R01 HL088521, U01 CA176726 [W.C.W., A.H.E.], U01 HL145386, U01 CA167552 [W.C.W.], R01 HL035464 [E.B.R.], U01 CA261961 [M.S.], K99 CA207736 [F.K.T.]). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Competing Interests
The authors have declared that no conflict of interest exists.
Data availability Statement
Because of participant confidentiality and privacy concerns, data are available upon written request. According to standard controlled access procedure, applications to use the Nurses’ Health Studies and Health Professionals Follow-up Study resources will be reviewed by our External Collaborators Committee for scientific aims, evaluation of the fit of the data for the proposed methodology, and verification that the proposed use meets the guidelines of the Ethics and Governance Framework and the consent that was provided by the participants. Investigators wishing to use the Nurses’ Health Studies and Health Professionals Follow-up Study data are asked to submit a brief description of the proposed project. Further information including the procedures to obtain and access data from the Nurses’ Health Studies and Health Professionals Follow-up Study is described at https://www.nurseshealthstudy.org/researchers (contact: nhsaccess@channing.harvard.edu) and https://sites.sph.harvard.edu/hpfs/for-collaborators/.
Code Availability Statement
The analysis programs are publicly available through https://github.com/pwangepi/DPs-and-chronic-disease.
References
- 1.Buttorff C, Ruder T & Bauman M Multiple Chronic Conditions in the United States. (RAND Corporation, Santa Monica, CA, 2017). [Google Scholar]
- 2.Murphy SL, Kochanek KD, Xu J & Arias E Mortality in the United States, 2020. NCHS Data Brief, 1–8 (2021). [PubMed] [Google Scholar]
- 3.Rao M, Afshin A, Singh G & Mozaffarian D Do healthier foods and diet patterns cost more than less healthy options? A systematic review and meta-analysis. BMJ Open 3, e004277 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.GBD 2017 Diet Collaborators. Health effects of dietary risks in 195 countries, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2019. May 11;393(10184):1958–1972. doi: 10.1016/S0140-6736(19)30041-8. Epub 2019 Apr 4. Erratum in: Lancet. 2021 Jun 26;397(10293):2466. PMID: 30954305; PMCID: PMC6899507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dietary Guidelines Advisory Committee. Scientific Report of the 2020 Dietary Guidelines Advisory Committee: Advisory Report to the Secretary of Agriculture and the Secretary of Health and Human Services. (U.S. Department of Agriculture, Agricultural Research Service, Washington, D.C., 2020). [Google Scholar]
- 6.U.S. Department of Agriculture and U.S. Department of Health and Human Services. Dietary Guidelines for Americans, 2020–2025. (2020). [Google Scholar]
- 7.Tabung FK, et al. Development and Validation of an Empirical Dietary Inflammatory Index. J Nutr 146, 1560–1570 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tabung FK, et al. Development and validation of empirical indices to assess the insulinaemic potential of diet and lifestyle. Br J Nutr 116, 1787–1798 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jin Q, et al. Insulinemic and Inflammatory Dietary Patterns Show Enhanced Predictive Potential for Type 2 Diabetes Risk in Postmenopausal Women. Diabetes Care 44, 707–714 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lee DH, et al. Dietary Inflammatory and Insulinemic Potential and Risk of Type 2 Diabetes: Results From Three Prospective U.S. Cohort Studies. Diabetes Care 43, 2675–2683 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wan Y, et al. Dietary Insulinemic Potential and Risk of Total and Cause-Specific Mortality in the Nurses' Health Study and the Health Professionals Follow-up Study. Diabetes Care 45, 451–459 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Li J, et al. Dietary Inflammatory Potential and Risk of Cardiovascular Disease Among Men and Women in the U.S. J Am Coll Cardiol 76, 2181–2193 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shi N, et al. Proinflammatory and Hyperinsulinemic Dietary Patterns Are Associated With Specific Profiles of Biomarkers Predictive of Chronic Inflammation, Glucose-Insulin Dysregulation, and Dyslipidemia in Postmenopausal Women. Front Nutr 8, 690428 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rhee JJ, Mattei J, Hughes MD, Hu FB & Willett WC Dietary diabetes risk reduction score, race and ethnicity, and risk of type 2 diabetes in women. Diabetes Care 38, 596–603 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wang CR, et al. Type 2 Diabetes-Prevention Diet and All-Cause and Cause-Specific Mortality: A Prospective Study. Am J Epidemiol 191, 472–486 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Morze J, Danielewicz A, Hoffmann G & Schwingshackl L Diet Quality as Assessed by the Healthy Eating Index, Alternate Healthy Eating Index, Dietary Approaches to Stop Hypertension Score, and Health Outcomes: A Second Update of a Systematic Review and Meta-Analysis of Cohort Studies. J Acad Nutr Diet 120, 1998–2031 e1915 (2020). [DOI] [PubMed] [Google Scholar]
- 17.Sofi F, Cesari F, Abbate R, Gensini GF & Casini A Adherence to Mediterranean diet and health status: meta-analysis. BMJ 337, a1344 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bloomfield HE, et al. Effects on Health Outcomes of a Mediterranean Diet With No Restriction on Fat Intake: A Systematic Review and Meta-analysis. Ann Intern Med 165, 491–500 (2016). [DOI] [PubMed] [Google Scholar]
- 19.Bahrami A, et al. Adherence to the Mediterranean diet and the risk of lung cancer: a systematic review and dose-response meta-analysis of observational studies. Nutr Rev 80, 1118–1128 (2022). [DOI] [PubMed] [Google Scholar]
- 20.Gan ZH, Cheong HC, Tu YK & Kuo PH Association between Plant-Based Dietary Patterns and Risk of Cardiovascular Disease: A Systematic Review and Meta-Analysis of Prospective Cohort Studies. Nutrients 13(2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Baden MY, et al. Changes in Plant-Based Diet Quality and Total and Cause-Specific Mortality. Circulation 140, 979–991 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chen Z, et al. Changes in Plant-Based Diet Indices and Subsequent Risk of Type 2 Diabetes in Women and Men: Three U.S. Prospective Cohorts. Diabetes Care 44, 663–671 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Shams-White MM, et al. Operationalizing the 2018 World Cancer Research Fund/American Institute for Cancer Research (WCRF/AICR) Cancer Prevention Recommendations: A Standardized Scoring System. Nutrients 11(2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kaluza J, Harris HR, Hakansson N & Wolk A Adherence to the WCRF/AICR 2018 recommendations for cancer prevention and risk of cancer: prospective cohort studies of men and women. Br J Cancer 122, 1562–1570 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Shams-White MM, Brockton NT, Mitrou P, Kahle LL & Reedy J The 2018 World Cancer Research Fund/American Institute for Cancer Research (WCRF/AICR) Score and All-Cause, Cancer, and Cardiovascular Disease Mortality Risk: A Longitudinal Analysis in the NIH-AARP Diet and Health Study. Curr Dev Nutr 6, nzac096 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tabung FK, et al. Associations between adherence to the World Cancer Research Fund/American Institute for Cancer Research cancer prevention recommendations and biomarkers of inflammation, hormonal, and insulin response. Int J Cancer 140, 764–776 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.IARC Working Group on the Evaluation of Carcinogenic Risks to Humans. A review of human carcinogens. Part E: Personal habits and indoor combustions. IARC monographs on the evaluation of carcinogenic risks to humans 100(Pt E), 373–472 (2012). [PMC free article] [PubMed] [Google Scholar]
- 28.Lichtenstein AH, et al. 2021 Dietary Guidance to Improve Cardiovascular Health: A Scientific Statement From the American Heart Association. Circulation 144, e472–e487 (2021). [DOI] [PubMed] [Google Scholar]
- 29.Knott C, Bell S & Britton A Alcohol Consumption and the Risk of Type 2 Diabetes: A Systematic Review and Dose-Response Meta-analysis of More Than 1.9 Million Individuals From 38 Observational Studies. Diabetes Care 38, 1804–1812 (2015). [DOI] [PubMed] [Google Scholar]
- 30.Xi B, et al. Relationship of Alcohol Consumption to All-Cause, Cardiovascular, and Cancer-Related Mortality in U.S. Adults. J Am Coll Cardiol 70, 913–922 (2017). [DOI] [PubMed] [Google Scholar]
- 31.Grosso G, Godos J, Galvano F & Giovannucci EL Coffee, Caffeine, and Health Outcomes: An Umbrella Review. Annu Rev Nutr 37, 131–156 (2017). [DOI] [PubMed] [Google Scholar]
- 32.Zhao B, et al. Relationship between chocolate consumption and overall and cause-specific mortality, systematic review and updated meta-analysis. Eur J Epidemiol 37, 321–333 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hooper L, et al. Effects of chocolate, cocoa, and flavan-3-ols on cardiovascular health: a systematic review and meta-analysis of randomized trials. Am J Clin Nutr 95, 740–751 (2012). [DOI] [PubMed] [Google Scholar]
- 34.Tabung FK, Satija A, Fung TT, Clinton SK & Giovannucci EL Long-Term Change in both Dietary Insulinemic and Inflammatory Potential Is Associated with Weight Gain in Adult Women and Men. J Nutr 149, 804–815 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
Methods only references
- 35.Salvini S, et al. Food-based validation of a dietary questionnaire: the effects of week-to-week variation in food consumption. Int J Epidemiol 18, 858–867 (1989). [DOI] [PubMed] [Google Scholar]
- 36.Yuan C, et al. Validity of a Dietary Questionnaire Assessed by Comparison With Multiple Weighed Dietary Records or 24-Hour Recalls. Am J Epidemiol 185, 570–584 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Feskanich D, et al. Reproducibility and validity of food intake measurements from a semiquantitative food frequency questionnaire. J Am Diet Assoc 93, 790–796 (1993). [DOI] [PubMed] [Google Scholar]
- 38.Hu FB, et al. Reproducibility and validity of dietary patterns assessed with a food-frequency questionnaire. Am J Clin Nutr 69, 243–249 (1999). [DOI] [PubMed] [Google Scholar]
- 39.Al-Shaar L, et al. Reproducibility and Validity of a Semiquantitative Food Frequency Questionnaire in Men Assessed by Multiple Methods. Am J Epidemiol 190, 1122–1132 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Yue Y, et al. Reproducibility and validity of diet quality scores derived from food-frequency questionnaires. Am J Clin Nutr 115, 843–853 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Chiuve SE, et al. Alternative dietary indices both strongly predict risk of chronic disease. J Nutr 142, 1009–1018 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Fung TT, et al. Diet quality is associated with the risk of estrogen receptor-negative breast cancer in postmenopausal women. J Nutr 136, 466–472 (2006). [DOI] [PubMed] [Google Scholar]
- 43.Satija A, et al. Plant-Based Dietary Patterns and Incidence of Type 2 Diabetes in US Men and Women: Results from Three Prospective Cohort Studies. PLoS Med 13, e1002039 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Fung TT, et al. Adherence to a DASH-style diet and risk of coronary heart disease and stroke in women. Arch Intern Med 168, 713–720 (2008). [DOI] [PubMed] [Google Scholar]
- 45.Wang T, et al. Diabetes Risk Reduction Diet and Survival after Breast Cancer Diagnosis. Cancer Res 81, 4155–4162 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Iyer HS, et al. Impact of neighborhood socioeconomic status, income segregation, and greenness on blood biomarkers of inflammation. Environ Int 162, 107164 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Lauby-Secretan B, et al. Body Fatness and Cancer--Viewpoint of the IARC Working Group. N Engl J Med 375, 794–798 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Colditz GA, et al. Validation of questionnaire information on risk factors and disease outcomes in a prospective cohort study of women. Am J Epidemiol 123, 894–900 (1986). [DOI] [PubMed] [Google Scholar]
- 49.Stampfer MJ, et al. Test of the National Death Index. Am J Epidemiol 119, 837–839 (1984). [DOI] [PubMed] [Google Scholar]
- 50.Rich-Edwards JW, Corsano KA & Stampfer MJ Test of the National Death Index and Equifax Nationwide Death Search. Am J Epidemiol 140, 1016–1019 (1994). [DOI] [PubMed] [Google Scholar]
- 51.Walker AE, Robins M & Weinfeld FD The National Survey of Stroke. Clinical findings. Stroke 12, I13–44 (1981). [PubMed] [Google Scholar]
- 52.Mendis S, et al. World Health Organization definition of myocardial infarction: 2008-09 revision. Int J Epidemiol 40, 139–146 (2011). [DOI] [PubMed] [Google Scholar]
- 53.American Diabetes, A. Standards of medical care in diabetes--2010. Diabetes Care 33 Suppl 1, S11–61 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Classification and diagnosis of diabetes mellitus and other categories of glucose intolerance. National Diabetes Data Group. Diabetes 28, 1039–1057 (1979). [DOI] [PubMed] [Google Scholar]
- 55.Manson JE, et al. Physical activity and incidence of non-insulin-dependent diabetes mellitus in women. Lancet 338, 774–778 (1991). [DOI] [PubMed] [Google Scholar]
- 56.Hu FB, et al. Physical activity and television watching in relation to risk for type 2 diabetes mellitus in men. Arch Intern Med 161, 1542–1548 (2001). [DOI] [PubMed] [Google Scholar]
- 57.Mozaffarian D, Hao T, Rimm EB, Willett WC & Hu FB Changes in diet and lifestyle and long-term weight gain in women and men. N Engl J Med 364, 2392–2404 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Willett W & Stampfer MJ Total energy intake: implications for epidemiologic analyses. Am J Epidemiol 124, 17–27 (1986). [DOI] [PubMed] [Google Scholar]
- 59.Durrleman S & Simon R Flexible regression models with cubic splines. Stat Med 8, 551–561 (1989). [DOI] [PubMed] [Google Scholar]
- 60.Lee JE, et al. Folate intake and risk of colorectal cancer and adenoma: modification by time. Am J Clin Nutr 93, 817–825 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Because of participant confidentiality and privacy concerns, data are available upon written request. According to standard controlled access procedure, applications to use the Nurses’ Health Studies and Health Professionals Follow-up Study resources will be reviewed by our External Collaborators Committee for scientific aims, evaluation of the fit of the data for the proposed methodology, and verification that the proposed use meets the guidelines of the Ethics and Governance Framework and the consent that was provided by the participants. Investigators wishing to use the Nurses’ Health Studies and Health Professionals Follow-up Study data are asked to submit a brief description of the proposed project. Further information including the procedures to obtain and access data from the Nurses’ Health Studies and Health Professionals Follow-up Study is described at https://www.nurseshealthstudy.org/researchers (contact: nhsaccess@channing.harvard.edu) and https://sites.sph.harvard.edu/hpfs/for-collaborators/.
The analysis programs are publicly available through https://github.com/pwangepi/DPs-and-chronic-disease.