Abstract
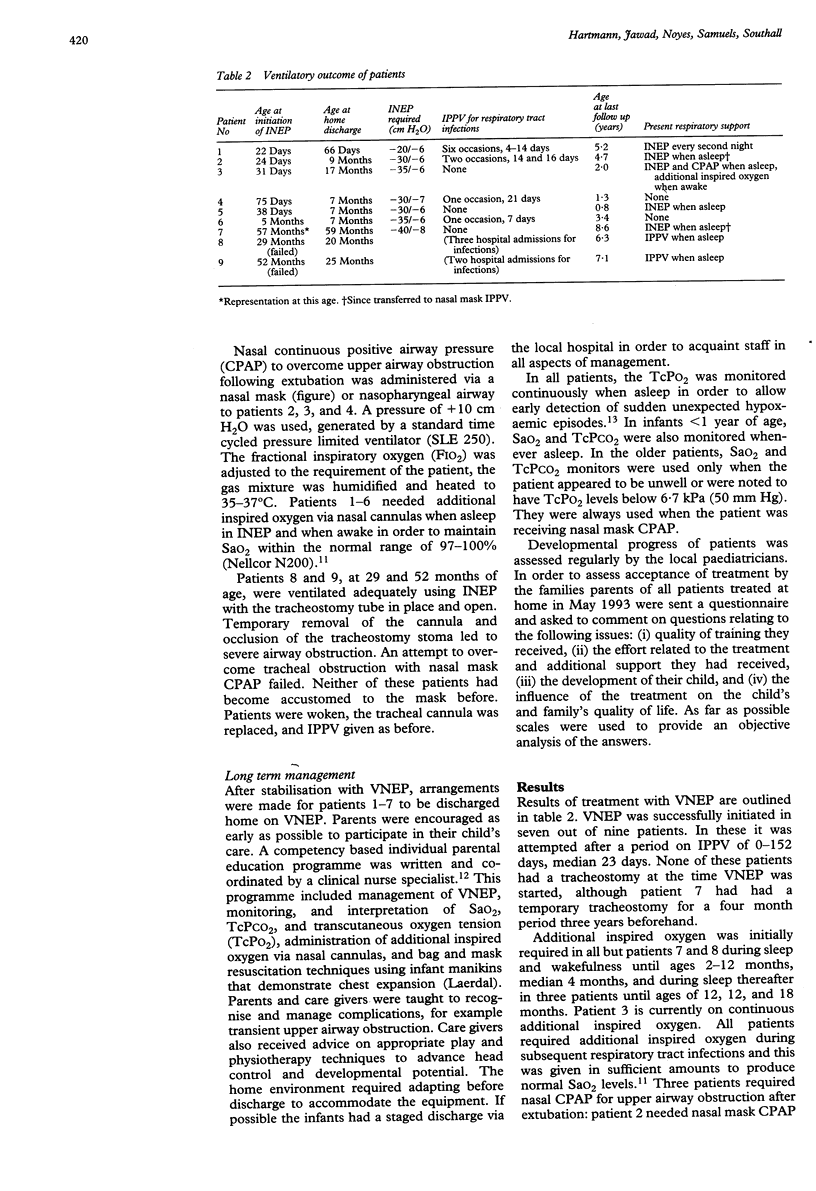
Nine patients with central hypoventilation syndrome (CHS) were treated with negative extrathoracic pressure ventilation (VNEP). Treatment with VNEP was started between 20 days and 57 months of age, which was two days to 47 months after diagnosis. The equipment to provide VNEP utilised a new system with a latex neck seal and Perspex chamber allowing easy access to the child. Seven patients are managed with VNEP at home by their parents. They did not have a tracheostomy when VNEP was started at ages of 22, 24, 31, 38, and 75 days, 5 and 57 months. They have continued to be successfully managed with VNEP and without tracheostomy. Short periods of intubation and positive pressure ventilation were required on 10 occasions (median duration 7 days, range 4 to 21 days) in four subjects during respiratory tract infections. Three patients required periods of continuous positive airway pressure (CPAP) via a nasal mask or a nasopharyngeal airway during sleep to overcome upper airway obstruction. In three patients the hypoventilation improved and two of these do not require regular ventilatory support at 1.3 and 3.4 years of age. Six of these seven patients are developing normally. In two patients with long term tracheostomies, VNEP could not be established at an age of 29 and 52 months because of tracheal obstruction after temporary removal of their tracheostomy cannula. VNEP is an effective, non-invasive, treatment in infants with CHS if initiated before tracheostomy. It may improve the children's quality of life during the daytime. If upper airway obstruction is a problem in the first year of life, it may be combined with nasal mask CPAP.
Full text
PDF
Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Aass A. S. Complications to tracheostomy and long-term intubation: a follow-up study. Acta Anaesthesiol Scand. 1975;19(2):127–133. doi: 10.1111/j.1399-6576.1975.tb05232.x. [DOI] [PubMed] [Google Scholar]
- Espinoza H., Palmer D. L., Kisch A. L., Ulrich J., Eberle B., Reed W. P. Clinical and immunologic response to bacteria isolated from tracheal secretions following tracheostomy. J Thorac Cardiovasc Surg. 1974 Sep;68(3):432–439. [PubMed] [Google Scholar]
- Freezer N. J., Beasley S. W., Robertson C. F. Tracheostomy. Arch Dis Child. 1990 Jan;65(1):123–126. doi: 10.1136/adc.65.1.123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gerson C. R., Tucker G. F., Jr Infant tracheotomy. Ann Otol Rhinol Laryngol. 1982 Jul-Aug;91(4 Pt 1):413–416. doi: 10.1177/000348948209100419. [DOI] [PubMed] [Google Scholar]
- Hunt C. E., Inwood R. J., Shannon D. C. Respiratory and nonrespiratory effects of doxapram in congenital central hypoventilation syndrome. Am Rev Respir Dis. 1979 Feb;119(2):263–269. doi: 10.1164/arrd.1979.119.2.263. [DOI] [PubMed] [Google Scholar]
- Hunt C. E., Matalon S. V., Thompson T. R., Demuth S., Loew J. M., Liu H. M., Mastri A., Burke B. Central hypoventilation syndrome: experience with bilateral phrenic nerve pacing in 3 neonates. Am Rev Respir Dis. 1978 Jul;118(1):23–28. doi: 10.1164/arrd.1978.118.1.23. [DOI] [PubMed] [Google Scholar]
- Ilbawi M. N., Idriss F. S., Hunt C. E., Brouillette R. T., DeLeon S. Y. Diaphragmatic pacing in infants: techniques and results. Ann Thorac Surg. 1985 Oct;40(4):323–329. doi: 10.1016/s0003-4975(10)60061-6. [DOI] [PubMed] [Google Scholar]
- MacRae D. L., Rae R. E., Heeneman H. Pediatric tracheotomy. J Otolaryngol. 1984 Oct;13(5):309–311. [PubMed] [Google Scholar]
- Marcus C. L., Bautista D. B., Amihyia A., Ward S. L., Keens T. G. Hypercapneic arousal responses in children with congenital central hypoventilation syndrome. Pediatrics. 1991 Nov;88(5):993–998. [PubMed] [Google Scholar]
- Marcus C. L., Jansen M. T., Poulsen M. K., Keens S. E., Nield T. A., Lipsker L. E., Keens T. G. Medical and psychosocial outcome of children with congenital central hypoventilation syndrome. J Pediatr. 1991 Dec;119(6):888–895. doi: 10.1016/s0022-3476(05)83038-0. [DOI] [PubMed] [Google Scholar]
- Nielson D. W., Black P. G. Mask ventilation in congenital central alveolar hypoventilation syndrome. Pediatr Pulmonol. 1990;9(1):44–45. doi: 10.1002/ppul.1950090110. [DOI] [PubMed] [Google Scholar]
- Noyes J. Respiratory failure in infants. 1990 Aug 29-Sep 4Nurs Stand. 4(49):28–30. doi: 10.7748/ns.4.49.28.s37. [DOI] [PubMed] [Google Scholar]
- Olson T. S., Woodson G. E., Heldt G. P. Upper airway function in Ondine's curse. Arch Otolaryngol Head Neck Surg. 1992 Mar;118(3):310–312. doi: 10.1001/archotol.1992.01880030098020. [DOI] [PubMed] [Google Scholar]
- Oren J., Kelly D. H., Shannon D. C. Long-term follow-up of children with congenital central hypoventilation syndrome. Pediatrics. 1987 Sep;80(3):375–380. [PubMed] [Google Scholar]
- Oren J., Newth C. J., Hunt C. E., Brouillette R. T., Bachand R. T., Shannon D. C. Ventilatory effects of almitrine bismesylate in congenital central hypoventilation syndrome. Am Rev Respir Dis. 1986 Nov;134(5):917–919. doi: 10.1164/arrd.1986.134.5.917. [DOI] [PubMed] [Google Scholar]
- Paton J. Y., Swaminathan S., Sargent C. W., Keens T. G. Hypoxic and hypercapnic ventilatory responses in awake children with congenital central hypoventilation syndrome. Am Rev Respir Dis. 1989 Aug;140(2):368–372. doi: 10.1164/ajrccm/140.2.368. [DOI] [PubMed] [Google Scholar]
- Poets C. F., Samuels M. P., Noyes J. P., Jones K. A., Southall D. P. Home monitoring of transcutaneous oxygen tension in the early detection of hypoxaemia in infants and young children. Arch Dis Child. 1991 Jun;66(6):676–682. doi: 10.1136/adc.66.6.676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Samuels M. P., Southall D. P. Negative extrathoracic pressure in treatment of respiratory failure in infants and young children. BMJ. 1989 Nov 18;299(6710):1253–1257. doi: 10.1136/bmj.299.6710.1253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stebbens V. A., Poets C. F., Alexander J. R., Arrowsmith W. A., Southall D. P. Oxygen saturation and breathing patterns in infancy. 1: Full term infants in the second month of life. Arch Dis Child. 1991 May;66(5):569–573. doi: 10.1136/adc.66.5.569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weese-Mayer D. E., Hunt C. E., Brouillette R. T., Silvestri J. M. Diaphragm pacing in infants and children. J Pediatr. 1992 Jan;120(1):1–8. doi: 10.1016/s0022-3476(05)80588-8. [DOI] [PubMed] [Google Scholar]