Abstract
Due to modern medical advancements, greater proportions of the population will continue to age with longer life spans. Increased life span, however, does not always correlate with improved health span, and may result in an increase in aging-related diseases and disorders. These diseases are often attributed to cellular senescence, in which cells become disengaged from the cell cycle and inert to cell death. These cells are characterized by a proinflammatory secretome. The proinflammatory senescence-associated secretory phenotype, although part of a natural function intended to prevent further DNA damage, creates a microenvironment suited to tumor progression. This microenvironment is most evident in the gastrointestinal tract (GI), where a combination of bacterial infections, senescent cells, and inflammatory proteins can lead to oncogenesis. Thus, it is important to find potential senescence biomarkers as targets of novel therapies for GI diseases and disorders including cancers. However, finding therapeutic targets in the GI microenvironment to reduce the risk of GI tumor onset may also be of value. This review summarizes the effects of cellular senescence on GI aging, inflammation, and cancers, and aims to improve our understanding of these processes with a goal of enhancing future therapy.
Keywords: senescence, inflammation, cancer, aging, gastrointestinal tract
1. Introduction
According to the World Health Organization, 1.4 billion people globally will be older than 60 years in 2030 [1]. As a result, a considerable proportion of the population will be subject to aging-related health conditions, such as problems related to cellular senescence, a key driver of aging and aging-associated diseases, and also a higher risk of cancer. The incidence of gastrointestinal tract (GI) diseases, including cancers increases with age, partially due to the accumulation of senescent cells [2], and will no doubt increase further as the older population expands within the current decade. One therapeutic option in GI cancers may be to regulate cellular senescence, which is defined as a state of irreversible cell cycle arrest that typically occurs in response to DNA damage and the acquisition of a proinflammatory secretory phenotype. Although the aberrant accumulation of senescent cells is associated with aging-related diseases/disorders, this state can also be used to manage tumors. For instance, given the risk of toxicity from extreme drug dosages in chemotherapies, the combination of pro-senescence and senolytic therapy may reduce that risk while amplifying cancer destruction [3]. The detailed roles of cellular senescence in GI cancers are not clear, but evidence indicates that the senescent fibroblast microenvironment can increase the risk of colon cancers [4]. The unclear relationship between cellular senescence and GI cancers serves as a motivation to further develop research efforts on this topic to expand therapeutic options for the future aging population of the world.
Fragility in older persons often stems from multiple sources of disease, cascading effects caused by those sources, and accumulation of senescent cells. Older people are often at a higher risk for experiencing complications of several infectious diseases, such as COVID-19, intestinal bacterial overgrowth, and GI ulcers [5,6]. Many of these diseases can be attributed to senescence in some capacity; for example, COVID-19 overloads older persons with senescent cells, DNA damage accumulation, and inflammatory cytokines [7,8]. This could be detrimental in the long term, as it may lead to the development of other diseases and disorders if left untreated. Older persons are already affected by a greater morbidity from common GI disorders, such as esophageal reflux, dysphagia, chronic constipation, and gastroparesis (defined as delayed gastric emptying without mechanical blockage) [9,10]. Owing to the compounding effects of the high risk of infectious diseases, GI bleeding, and cancer progression, death is therefore more likely in the aging population. Thus, it is necessary to elucidate how the components and mechanisms of senescence interact to better understand how they contribute to disease development.
The innate immunity, which acts as the first line of defense against invading pathogens including Helicobacter pylori (a Gram-negative spiral-shaped bacterium in human stomachs), is also a key player in aging and aging-associated diseases. Age-associated innate immune dysfunction can also predispose the elderly to fragility and more severe disease. We also discuss the implications of age-associated changes in innate immunity to better understand the biological basis of the age-associated chronic inflammatory GI diseases and cancers.
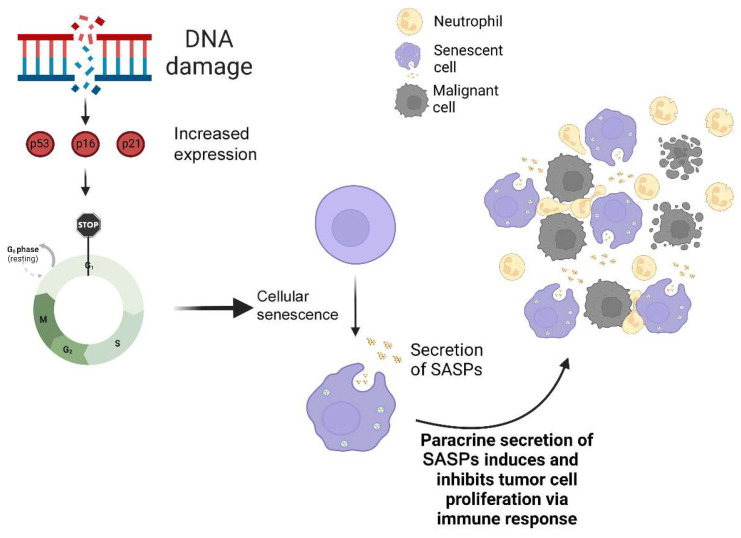
2. Cellular Senescence
Aging can be defined as the development of the human body from conception to death. Throughout this process, humans undergo an eventual decline of cellular function [11]. This decline is often associated with the accumulation of DNA damage and related cellular fates such as senescent cells, which results in the aging of the human body. Cellular senescence causes cells to undergo cell cycle arrest, at which point the cells are no longer able to grow and replicate but remain metabolically active so as to affect normal cells both locally and systemically [12]. It is an important defense mechanism against DNA damage, telomere destruction, and other stressors. Without senescence, DNA damage would rampantly increase tumor proliferation and progression [13]. The senescence pathway involves DNA damage, which activates tumor antigens such as the tumor suppressor p53 and cyclin-dependent kinase inhibitors p16 and p21, which then leads to cell cycle arrest and the increased generation of myriad cytokines, chemokines, and other inflammatory proteins from senescent cells (Figure 1). This protein expression pattern is termed the senescence-associated secretory phenotype (SASP). Telomere shortening or telomeric DNA damage can also lead to the activation of p16 and p21 [14], and stimuli such as cytokines or oncogene activity can also lead to cell cycle arrest and subsequent senescent phenotypic expression [15].
Figure 1.
Cellular senescence and cancer development. Cellular senescence is a stress response pathway that elicits an irreversible and permanent cell cycle arrest, and releases inflammatory cytokines termed senescence-associated secretory phenotype proteins (SASPs), which typically recruit immune cells, such as neutrophils, to respond to malignant tumor cells.
DNA damage is one of the main contributors to aging; it occurs naturally from metabolic processes such as the creation of oxidative byproducts by mitochondria [16]. Thus, DNA damage coincides with p53 expression, which is caused by mitochondrial apoptosis [17]; mitochondrial dysfunction, which increases p53 expression in senescent cells [18]; and p53 expression, which inhibits mitochondrial elongation in cell senescence [19]. Mitochondrial elongation is a mechanism that increases cell viability, which implies that p53 inherently increases the likelihood of cell apoptosis [20]. This is interesting, considering that senescence acts opposite to apoptosis, neither of which is directly correlated with the other. However, a recent study defined two downstream proteins of p53—PUMA, a key protein linked to p53-mediated apoptosis, and p21 (one of the genes linked to cellular senescence)as being significant contributors to lymphoma prevention [21]. p53 is involved in almost all DNA repair pathways. This implies that all three processes (cellular senescence, DNA repair, and apoptosis) work together through p53, which acts as a liaison.
Hypothetically, these three processes may be dependent on the needs of the cell, as senescence or apoptosis may be preferred in different situations. This is possible given how different organs vary in response to aging, such as the intestinal cells being more likely to undergo apoptosis and implies that different epigenomic alterations to the genome occur in different cell types [22]. Therefore, various senescence studies are needed, especially in GI research, as the many different cells throughout the GI most likely lead to a great variety in senescence-associated gene expression. p53 has been implied to exhibit an epigenetic effect on cells as shown by its positive relationship with α-ketoglutarate, an intermediate of the citric acid cycle and a key substrate for several epigenetic processes [23]. Additionally, a recent in vitro study showed no effect of α-ketoglutarate on p21 expression in senescent cells but did show an effect on SASP-related cytokine expression [24]. This suggests that p53 may have an epigenetic effect on its own downstream SASP expression.
As shown in Figure 1, several SASP proteins, such as interleukin (IL)-8, are involved in the recruitment of immune cells, such as neutrophils, to impede malignant cell growth [25,26]. The main functions of SASP proteins are to promote cell proliferation, tissue repair, and stem cell renewal; all of these suggest that the goal of SASP is to repair damage and prevent cancer development [27,28].
SASP protein overexpression is known to cause tumor progression by creating an inflammatory environment that leads to epithelial–mesenchymal transitions, which then increases cancer cell invasion [29]. SASP proteins such as IL-6 and IL-8 have also been shown to interact with chemokines and oncogenic proteins to promote cancer growth [30,31]. As a result, there is value in accounting for SASP when researching oncogenic development in older persons [32]. Given that mutations are more likely to occur through aging, a mutation in p53 may lead to the dysregulation of SASP and to subsequent cancer development, which was shown in a study in zebrafish in which a p53 mutation supported such a phenomenon [33]. Such mutations are common in human tumors. Most oncogenic development may stem not from SASP protein expression caused by natural senescent cell build up, but rather mutations in the regulation of senescence.
3. Senescence in GI Mucosa and Muscle
The susceptibility of GI cells to the senescence process varies depending on the specific cell type and region of GI; the potential contribution of senescent GI cells to age-related changes in GI health has not been fully investigated [10]. Although cellular senescence seems to be prevalent in GI mucosa [34,35], interstitial cells of Cajal (ICCs; pacemaker and neuromodulator cells of GI motor function) and their progenitor cells are reduced in number and function through cell cycle arrest due to reduced ERK signaling rather than the senescence pathway [34]. Cellular senescence is not only cell dependent or organ dependent, but also may be region dependent, as different regions of the colon have shown marked differences in p16 expression [36]. Additionally, no senescence markers specific to the GI have been found [37,38], so this merits investigation, and will be critical for improving our understanding of the roles of senescent cells in the GI. It would be rash to apply currently used senescence markers from other organs to the GI.
4. Immunosenescence
Immunosenescence is the natural decline in the immune system’s function, which drives accelerated aging. Specifically, as humans age, senescence occurs increasingly in certain subsets of immune cells, such as T cells. In mice that were genetically modified to have an accelerated senescence of the immune system, T cell numbers were found to have significantly reduced, which led to a compromised immune response [39]. Gut-associated lymphoid tissue (GALT) is the primary layer of defense against the infectious invasion of the GI. GALT includes lymphoid tissue in the esophagus, stomach, Peyer patches of the small intestine, large intestine, lymphoid follicles, and any lymphocytes in the epithelial layer or lamina propria of the GI [40]. As naïve T cells are often trafficked to the GALT [41], it makes sense that immunosenescence would greatly affect the immune responses arising in the GI.
Given that T cell counts decrease with age, the number of T cells in GALT could also decrease as a result. However, a previous study suggests the opposite: CD4+ T cells showed greater recruitment into the GALT of older mice compared with younger mice. Additionally, the recruitment was not correlated with an already-present immune response as (1) cytokines and chemokines were low in the GALT, (2) this T-cell recruitment was unique to GALT as the liver and lungs did not exhibit a similar response, and the (3) increased proliferation of existing CD4+ T cells in the GALT was not observed [42]. A study in human samples showed the opposite relationship between T-cell accumulation and aging in GALT, as CD4+ T cells decreased with age in the GALT [43]. This difference is interesting because it suggests different mechanisms of GALT immune cell recruitment in mice and in humans. However, the study did not compare the quantity of T cells in the rest of the body compared with the accumulation in the GALT/GI. Therefore, it is still possible that immunosenescence affects the rest of the body more than the GI. Indeed, aging impairs several signaling pathways in the innate immune system, which may result in the manifestation of certain inflammatory conditions and diseases, including diabetes and cancer.
5. Inflammatory Bowel Disease
Inflammatory bowel disease (IBD) describes a group of GI disorders that involves the major inflammation of the GI, with two major subsets: ulcerative colitis (UC) and Crohn’s disease. UC mostly involves inflammation and ulcer formation in the lining of the large intestine and rectum. Crohn’s disease involves chronic inflammation anywhere in the GI, including the esophagus and anus, but usually in the small intestine [44]. One study showed that the prevalence of IBD increased steadily over the past 10 years and was found to be higher in adults than children [45]. With the aging of the population, it becomes pertinent to understand any relationships between senescence/aging and IBD as this knowledge could help with therapies.
IBD is often marked by a dysregulated immune response involving T cells and B cells. One study showed UC-affected mucosa to have higher proportions of B cells than T cells [46], and another study showed naïve B cells to be significantly increased in patients with UC-inflamed colons [47]. Thus, it could be interpreted that increased B-cell proliferation in the large intestine is a biomarker for UC. A subset of B cells termed age-associated B cells (ABCs) are associated with not only aging but also autoimmune diseases, including Crohn’s disease and UC [48]. Several mouse models involving chemically induced colitis have shown excessive or dysregulated TLR signaling [49,50]. This coincides with how TLR signaling primes B cells for ABC transformation [51]. Thus, whereas immunosenescence decreases the immune response in the rest of the body, the increase in ABCs with aging may correlate with an increased risk of IBD.
Interestingly, TLR signaling was found to be significantly increased in benign polyps but was significantly decreased in polyps taken from patients who eventually had development of colorectal cancer (CRC) [52]. IBD is often associated with CRC due to the combination of chronic inflammation and ulcerative lesions that increases the risk of oncogenic progression [53,54]. In addition, high accumulations of senescent CD8+ T cells were found to be associated with greater oncogenic risk [55]. This implies that increased immunosenescence is either a product of or contributes to CRC. Interestingly, inhibition of chronic inflammation in the colon of mice not only increased their life span, but also reduced aging-related changes, especially oxidative DNA damage [56]. Another study showed a similar relationship between UC and cellular senescence: chronic inflammation created an environment that increased DNA damage and telomere shortening, and thereby led to eventual dysplasia and CRC development [57].
Further evidence in that IBD is connected to increased cellular senescence came from a study showing that UC increased macrophage counts (which in turn induced senescence), and Crohn’s disease also showed high levels of macrophages and senescence (yet macrophages were not found to be correlated with senescence) [58]. In the same study, macrophages increased senescence via nitric oxide production [58]. The presence of lesions in UC most likely led to the increase in senescence via macrophages, which produce inducible nitric oxide synthase [59]. Another study showed possible therapeutic avenues by manipulation of the telomere length [60]. Whereas telomere shortening was shown to be actively involved in UC development, telomere activators also reduced the expression of common senescence pathways such as p53, and also improved the crypt structure [60]. Recently, rare cases were reported of carcinoma formation in the GALT in the colons of patients with UC [61]. Although GALT is relatively scarce in the colon, these areas still carry a risk of oncogenic development, which requires further research [61].
6. Esophagitis
Esophagitis is an inflammation of the esophagus caused by eosinophilia, gastric reflux, or infection. A recent study showed a high prevalence of senescence and cancer-related somatic mutations, including p53 mutations, in the esophagus in older donor tissue [62]. This coincides with the results of a transcriptomic analysis of esophageal epithelium showing mitochondrial dysfunction in the esophagus of older mice [63]. Given the known relationship between p53 and mitochondria, the higher prevalence of p53 mutations may be connected to the dysfunction of mitochondria in older esophageal tissue. Reflux esophagitis has been shown to not only be caused by cytokine inflammation, but also a risk factor for Barrett’s esophagus metaplasia, a precursor to esophageal adenocarcinoma [64]. p53 mutations would most likely lead to increased senescence in the esophagus in older persons, and the added SASP would no doubt further increase cytokine inflammation in the esophagus. Thus, cellular senescence may contribute to a higher risk of esophagitis and eventual oncogenic development.
7. Helicobacter pylori, Senescence, and Gastric Cancer
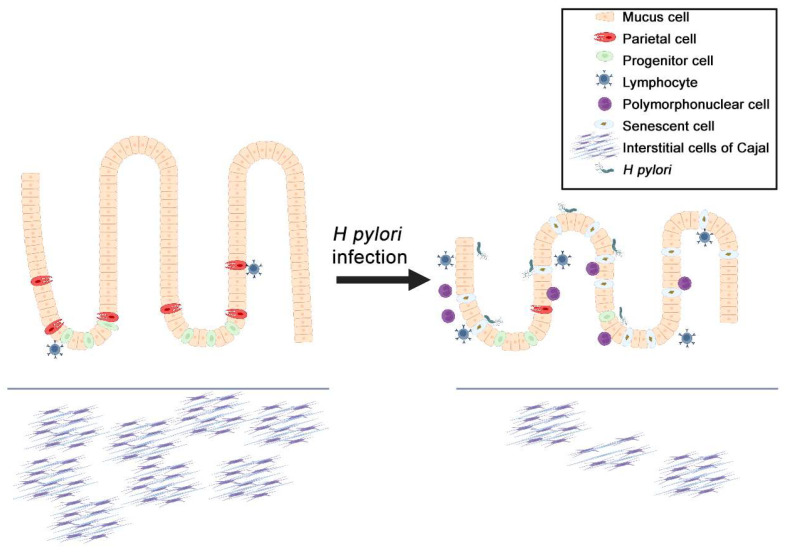
Helicobacter pylori is known to infect human stomachs, and H. pylori infection remains the major cause of gastric cancer, which involves multiple steps including gastritis, atrophic gastritis, intestinal metaplasia, dysplasia, and gastric cancer development [65,66]. The initial response of the innate immune system to H pylori involves gastric epithelial cells. The interaction between H pylori and gastric epithelial cells dysregulates signaling pathways leading to the generation of inflammatory and oncogenic processes. These processes include the accumulation of immune cells and DNA damage responses (Figure 2) [67]. As DNA damage directly correlates with the accumulation of senescent cells, H. pylori infection may therefore be a key trigger of cellular senescence in the GI.
Figure 2.
The effect of Helicobacter pylori infection and senescent cells on the mucosa of the stomach. H. pylori infection leads to oxidative stress on gastric mucosa and the creation of more senescent cells due to DNA damage. This, in turn, leads to the over-secretion of senescence-associated secretory phenotype (SASP) proteins, which creates a highly inflammatory microenvironment in the gastrointestinal tract. Although SASP is usually tumor suppressive due to an immune response, the combination of gastritis and inflammatory factors is tumor promotive, thereby increasing the chances of gastric oncogenesis.
H. pylori infection-induced atrophic gastritis has been linked to Wnt/β-catenin signaling activation [68,69,70]. Given that aberrant Wnt/β-catenin activation can induce the decrease in gastric ICC numbers with age, the presence of the bacteria may also damage the ICCs in the stomach (Figure 2). In fact, existing evidence shows that ICC numbers are reduced in the presence of H. pylori [71]. Given the evidence for correlation of Wnt signaling with the oncogenesis of gastrointestinal stromal tumor (GIST), a common human sarcoma of the GI muscle layer [72], the presence of H pylori could lead to higher risks of GIST development [73]. Injuries to the stomach, such as through gastritis, can cause metaplasia of chief cells, and gastric gland cells that release pepsinogen, as well as the loss of parietal cells that are responsible for secreting gastric acid to digest food. Although these changes are designed for wound healing, similar to senescent cells, their presence could be precancerous [74]. Additionally, the pro-inflammatory nature of H. pylori-related lesions and nitric oxide may work in tandem with the SASP of the senescent cells to create a highly oncogenic environment [75,76]. Inflammation and SASP increases immune cell recruitment (including polymorphonuclear cells, such as eosinophils and lymphocytes), which correlates with the increased metaplasia in the stomach and contributes to oncogenic progression [77,78]. Together, this suggests that senescence acts synergistically with the microenvironment of the GI to influence the onset of multiple aging-related GI disorders, especially cancer.
8. Cellular Senescence in GI Cancers and GIST
The relationship between cellular senescence and cancer is defined by contradiction. One study showed that senescent cells in advanced tumors reduce immune surveillance via SASP, yet cellular senescence was also shown to help tumor-suppressive mechanisms in hepatic carcinoma [79]. Given the senescent cells’ paradoxical roles in tumorigenesis, there is merit in using specific senescence biomarkers to mitigate tumor progression. For instance, the overexpression of tumor suppressors can induce senescence in tumor cells and prevent tumor cell proliferation [80]. The inactivation of genes such as PTEN and MYC can also cause cellular senescence. PTEN loss specifically causes p53 activation, which leads to senescent cell cycle arrest [81]. Thus, GIST may be assumed to have a similar relationship to senescence. However, there is no evidence that GIST can be treated with reinduction of senescence. Given that GIST is believed to develop from ICCs, which do not display senescent phenotypes, it is still possible that a different mechanism is critical for GIST development [34,82].
Instead of cellular senescence, cellular quiescence seems to be more relevant to drug-resistant GIST. Cellular quiescence is a reversible dormancy state of a cell that often leads to a permanent state of senescence [83]. Cellular quiescence is one reason total remission of GIST is infrequent; thus, quiescence proteins are considered as therapeutic targets. One possible example is combining imatinib mesylate, a tyrosine kinase inhibitor of the KIT receptor and the mainstay of treatment for GIST, with the quiescence therapeutic target, the DREAM complex [84], to induce complete cell death. Often, imatinib causes apoptosis in GIST but also results in quiescent cells. As a result, GIST recurrence is highly probable despite imatinib treatment [84]. However, the DREAM complex can be targeted to prevent quiescence via knockdown [85]. Notably, the protein that causes DREAM complex formation, DYRK1A, has an inverse relationship with both cyclin D1 and p21 [86]. The presence of quiescent cells often leads to imatinib-resistant GIST [87]. Furthermore, a recent study showed that imatinib-resistant GIST is highly affected by cyclin D1 targeting via proteasome inhibitors, which often leads to cell cycle arrest as well as the expression of p53 and p21 [88]. Additionally, increased p21 (as well as p53) expression has been associated with a poor prognosis of GIST [89], and p53 is a significant biomarker for GIST progression and proliferation [90,91]. Although these are senescence biomarkers, this is not a clear connection between senescence and GIST.
Evidence does exist, however, for manipulating senescent cells to prevent a tumor-progressive environment in the GI. A recent study showed that the synergism between cellular senescence and H. pylori is dependent on CXCR2 signaling [92]. H. pylori upregulates CXCR2, which exhibits a positive feedback on p53, and then increases cellular senescence. It is possible that CXCR2 can be pharmaceutically manipulated to decrease senescence caused by H. pylori and thus reduce the inflammatory cascade caused by the bacterial infection, subsequently reducing the likelihood of cancer progression [92,93].
Similarly, the CXCR4 signaling pathway is involved in tumor invasion and metastasis in CRC [94], the estimated third-leading cause of cancer death [95]. However, this pathway is most important for showcasing the relationship between the senescent tumor cells and immune cell impairment. Senescent tumor cells induce CXCR4 loss in T cells, which leads to impaired leukocyte migration and the inhibition of CD8+ T-cell infiltration [96]. This suggests that senescence is integral to CRC development due to the weakened immune system allowing further tumor cell invasion. Additional links between CRC and senescence include the presence of many senescent cells in the stroma of colorectal tumors and the relationship between the SASP and CRC growth [4,97]. Senescent fibroblasts in colonic stroma can enhance adenoma and CRC formation via a paracrine-mediated process that involves GDF15, a member of the TGFβ superfamily [4]. Escherichia coli can cause CRC via SASP protein secretion. This bacterial infection can upregulate miR-20a-5p in the colonic mucosa, which negatively regulates SENP1 (a negative regulator of p53) and leads to increased SASP protein expression and thus CRC growth [97]. These CRC studies show that CXCR4, GDF15, and miR-20a-5p are all potential biomarkers that could be targeted to reduce the oncogenic effect of senescent cells on the colon.
9. Senotherapeutics and Clinical Trials
Besides manipulating senescence, the destruction of senescent cells may provide optimal therapies. Senolytics are drugs that eliminate senescent cells through apoptosis, and senostatics are drugs that inhibit senescent cells’ function, and together are termed senotherapies [98]. Several clinical trials have already shown the effect of senotherapies on diseases. Senotherapies have been shown to decrease senescent cells in patients with diabetic kidney disease [99]. Circulating levels of α-Klotho, an antiaging protein that can alleviate aging processes, was restored through oral senolytics [100]. Another clinical trial showed senolytic drugs to mitigate the effects of diabetes in obese patients [101]. A study of premalignant pancreatic intraepithelial neoplasia lesions showed that senolytic therapies can reduce the progression of inflammatory lesions into cancer via senescent cell removal [102]. Given that this study showed a similar relationship between pancreatic lesions and senescence as in another study on H. pylori-induced atrophic gastritis [92], senolytics could therefore have a similar effect on precancerous gastritis.
Senotherapies could potentially be used to prevent the tumor-progressive microenvironment in an elderly GI. Unfortunately, senolytic clinical trials regarding the GI are currently scarce. However, a recent study showed that senotherapies can improve intestinal inflammation and overall health in older mice, and another study showed the antiaging potential of destroying senescent cells [103,104]. Thus, there is potential for more variation in senotherapy clinical trials involving the GI in the future.
Increasing evidence has shown that the gasotransmitter hydrogen sulfide (H2S) is integral to healthspan-extending interventions, and these effects of H2S might be related to a reduced cellular senescence in several tissues [105,106,107]. H2S plays this role via the post-translational modification of reactive cysteine residues by protein persulfidation (S-sulfhydration) [108]. The use of exogenous H2S might be an appealing application for aging and age-associated diseases but remains challenging due to the short half-life of H2S gas in vivo, and the risks of toxicity at high concentrations [109].
10. Conclusions
Overall, the evidence suggests that senescence is highly related to the onset of GI diseases and disorders, including cancers. Whether through the disruption of either tumor suppressor genes in the senescence pathway, or the combination of factors resulting from SASP and the GI microenvironment, targeting senescence can influence the development of tumors. As a result, further experimentation in GI cancers and cellular senescence is pertinent, as it would expand our information on the relationship between aging and tumor development. Knowledge of this relationship can then be used to create novel senotherapies that would help reduce the risk of GI oncogenesis in the aging population.
Acknowledgments
Alyssa B. Quiggle, ELS, Mayo Clinic, substantively edited the manuscript. The Scientific Publications staff at the Mayo Clinic provided proofreading and administrative and clerical support.
Abbreviations
| ABCs | Age-associated B cells |
| CRC | Colorectal cancer |
| GALT | Gut-associated lymphoid tissue |
| GI | Gastrointestinal tract |
| GIST | Gastrointestinal stromal tumor |
| H2S | Hydrogen sulfide |
| IBD | Inflammatory bowel disease |
| ICCs | Interstitial cells of Cajal |
| IL | Interleukin |
| SASP | Senescence-associated secretory phenotype |
| UC | Ulcerative colitis |
| Gene/Protein Expansions | |
| CXCR | C-X-C motif chemokine receptor |
| DREAM | Dimerization partner, RB-like, E2F and multi-vulval class B |
| DYRK1A | Dual specificity tyrosine-phosphorylation-regulated kinase 1A |
| ERK | Extracellular signal-regulated kinase |
| GDF15 | Growth differentiation factor 15 |
| KIT | KIT proto-oncogene, receptor tyrosine kinase |
| miR-20a-5p | MicroRNA-20a-5p |
| MYC | MYC proto-oncogene, bHLH transcription factor |
| PTEN | Phosphatase and tension homolog |
| PUMA | p53 upregulated modulator of apoptosis |
| SENP1 | SUMO specific peptidase 1 |
| TGFβ | Transforming growth factor β |
| TLR | Toll-like receptor |
| Wnt | Wingless/integrated |
Author Contributions
E.L.C.: conception and design, manuscript writing, N.T.: manuscript editing, A.C.: manuscript editing, Y.H.: conception and design, financial support, manuscript writing. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This work was supported in part by the National Institutes of Health Grants R01 DK121766 (Y.H.) and P30 DK084567 (Mayo Clinic Center for Cell Signaling in Gastroenterology); the Mayo Clinic Center for Biomedical Discovery Pilot Award (Y.H.); and the American Gastroenterology Association-Allergan Foundation Pilot Research Award in Gastroparesis (Y.H.). The funding agencies had no role in the study analysis or writing of the manuscript. Its contents are solely the responsibility of the authors.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.World Health Organization Ageing and Health. 2022. [(accessed on 12 April 2023)]. Available online: https://www.who.int/news-room/fact-sheets/detail/ageing-and-health.
- 2.Enzinger P.C., Mayer R.J. Gastrointestinal cancer in older patients. Semin. Oncol. 2004;31:206–219. doi: 10.1053/j.seminoncol.2003.12.031. [DOI] [PubMed] [Google Scholar]
- 3.Wang L., Lankhorst L., Bernards R. Exploiting senescence for the treatment of cancer. Nat. Rev. Cancer. 2022;22:340–355. doi: 10.1038/s41568-022-00450-9. [DOI] [PubMed] [Google Scholar]
- 4.Guo Y., Ayers J.L., Carter K.T., Wang T., Maden S.K., Edmond D., Newcomb P.P., Li C., Ulrich C., Yu M., et al. Senescence-associated tissue microenvironment promotes colon cancer formation through the secretory factor GDF15. Aging Cell. 2019;18:e13013. doi: 10.1111/acel.13013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pilott A., Fabrello R., Franceschi M., Scagnelli M., Soffiati F., Di Mario F., Fortunato A., Valerio G. Helicobacter pylori infection in asymptomatic elderly subjects living at home or in a nursing home: Effects on gastric function and nutritional status. Age Ageing. 1996;25:245–249. doi: 10.1093/ageing/25.3.245. [DOI] [PubMed] [Google Scholar]
- 6.Scapa E., Horowitz M., Waron M., Eshchar J. Duodenal ulcer in the elderly. J. Clin. Gastroenterol. 1989;11:502–506. doi: 10.1097/00004836-198910000-00004. [DOI] [PubMed] [Google Scholar]
- 7.Schmitt C.A., Tchkonia T., Niedernhofer L.J., Robbins P.D., Kirkland J.L., Lee S. COVID-19 and cellular senescence. Nat. Rev. Immunol. 2023;23:251–263. doi: 10.1038/s41577-022-00785-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lee S., Yu Y., Trimpert J., Benthani F., Mairhofer M., Richter-Pechanska P., Wyler E., Belenki D., Kaltenbrunner S., Pammer M., et al. Virus-induced senescence is a driver and therapeutic target in COVID-19. Nature. 2021;599:283–289. doi: 10.1038/s41586-021-03995-1. [DOI] [PubMed] [Google Scholar]
- 9.Camilleri M., Chedid V., Ford A.C., Haruma K., Horowitz M., Jones K.L., Low P.A., Park S.Y., Parkman H.P., Stanghellini V. Gastroparesis. Nat. Rev. Dis. Primers. 2018;4:41. doi: 10.1038/s41572-018-0038-z. [DOI] [PubMed] [Google Scholar]
- 10.Nguyen V.T.T., Taheri N., Chandra A., Hayashi Y. Aging of enteric neuromuscular systems in gastrointestinal tract. Neurogastroenterol. Motil. 2022;34:e14352. doi: 10.1111/nmo.14352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dodig S., Cepelak I., Pavic I. Hallmarks of senescence and aging. Biochem. Med. 2019;29:030501. doi: 10.11613/BM.2019.030501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Herranz N., Gil J. Mechanisms and functions of cellular senescence. J. Clin. Investig. 2018;128:1238–1246. doi: 10.1172/JCI95148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Basu A.K. DNA Damage, Mutagenesis and Cancer. Int. J. Mol. Sci. 2018;19:970. doi: 10.3390/ijms19040970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rossiello F., Jurk D., Passos J.F., d’Adda di Fagagna F. Telomere dysfunction in ageing and age-related diseases. Nat. Cell Biol. 2022;24:135–147. doi: 10.1038/s41556-022-00842-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Roger L., Tomas F., Gire V. Mechanisms and Regulation of Cellular Senescence. Int. J. Mol. Sci. 2021;22:13173. doi: 10.3390/ijms222313173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kowalska M., Piekut T., Prendecki M., Sodel A., Kozubski W., Dorszewska J. Mitochondrial and Nuclear DNA Oxidative Damage in Physiological and Pathological Aging. DNA Cell Biol. 2020;39:1410–1420. doi: 10.1089/dna.2019.5347. [DOI] [PubMed] [Google Scholar]
- 17.Carlsson M.J., Vollmer A.S., Demuth P., Heylmann D., Reich D., Quarz C., Rasenberger B., Nikolova T., Hofmann T.G., Christmann M., et al. p53 triggers mitochondrial apoptosis following DNA damage-dependent replication stress by the hepatotoxin methyleugenol. Cell Death Dis. 2022;13:1009. doi: 10.1038/s41419-022-05446-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wiley C.D., Velarde M.C., Lecot P., Liu S., Sarnoski E.A., Freund A., Shirakawa K., Lim H.W., Davis S.S., Ramanathan A., et al. Mitochondrial Dysfunction Induces Senescence with a Distinct Secretory Phenotype. Cell Metab. 2016;23:303–314. doi: 10.1016/j.cmet.2015.11.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kim Y.Y., Um J.H., Yoon J.H., Lee D.Y., Lee Y.J., Kim D.H., Park J.I., Yun J. p53 regulates mitochondrial dynamics by inhibiting Drp1 translocation into mitochondria during cellular senescence. FASEB J. 2020;34:2451–2464. doi: 10.1096/fj.201901747RR. [DOI] [PubMed] [Google Scholar]
- 20.Choi C.Y., Vo M.T., Nicholas J., Choi Y.B. Autophagy-competent mitochondrial translation elongation factor TUFM inhibits caspase-8-mediated apoptosis. Cell Death Differ. 2022;29:451–464. doi: 10.1038/s41418-021-00868-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Janic A., Valente L.J., Wakefield M.J., Di Stefano L., Milla L., Wilcox S., Yang H., Tai L., Vandenberg C.J., Kueh A.J., et al. DNA repair processes are critical mediators of p53-dependent tumor suppression. Nat. Med. 2018;24:947–953. doi: 10.1038/s41591-018-0043-5. [DOI] [PubMed] [Google Scholar]
- 22.Vougioukalaki M., Demmers J., Vermeij W.P., Baar M., Bruens S., Magaraki A., Kuijk E., Jager M., Merzouk S., Brandt R.M.C., et al. Different responses to DNA damage determine ageing differences between organs. Aging Cell. 2022;21:e13562. doi: 10.1111/acel.13562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Morris J.P., IV, Yashinskie J.J., Koche R., Chandwani R., Tian S., Chen C.C., Baslan T., Marinkovic Z.S., Sanchez-Rivera F.J., Leach S.D., et al. α-Ketoglutarate links p53 to cell fate during tumour suppression. Nature. 2019;573:595–599. doi: 10.1038/s41586-019-1577-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Asadi Shahmirzadi A., Edgar D., Liao C.Y., Hsu Y.M., Lucanic M., Asadi Shahmirzadi A., Wiley C.D., Gan G., Kim D.E., Kasler H.G., et al. Alpha-Ketoglutarate, an Endogenous Metabolite, Extends Lifespan and Compresses Morbidity in Aging Mice. Cell Metab. 2020;32:447–456.e6. doi: 10.1016/j.cmet.2020.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Martinez F.O., Sironi M., Vecchi A., Colotta F., Mantovani A., Locati M. IL-8 induces a specific transcriptional profile in human neutrophils: Synergism with LPS for IL-1 production. Eur. J. Immunol. 2004;34:2286–2292. doi: 10.1002/eji.200324481. [DOI] [PubMed] [Google Scholar]
- 26.Ponzetta A., Carriero R., Carnevale S., Barbagallo M., Molgora M., Perucchini C., Magrini E., Gianni F., Kunderfranco P., Polentarutti N., et al. Neutrophils Driving Unconventional T Cells Mediate Resistance against Murine Sarcomas and Selected Human Tumors. Cell. 2019;178:346–360.e24. doi: 10.1016/j.cell.2019.05.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Campisi J. Aging, cellular senescence, and cancer. Annu. Rev. Physiol. 2013;75:685–705. doi: 10.1146/annurev-physiol-030212-183653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Munoz-Espin D., Canamero M., Maraver A., Gomez-Lopez G., Contreras J., Murillo-Cuesta S., Rodriguez-Baeza A., Varela-Nieto I., Ruberte J., Collado M., et al. Programmed cell senescence during mammalian embryonic development. Cell. 2013;155:1104–1118. doi: 10.1016/j.cell.2013.10.019. [DOI] [PubMed] [Google Scholar]
- 29.Laberge R.M., Awad P., Campisi J., Desprez P.Y. Epithelial-mesenchymal transition induced by senescent fibroblasts. Cancer Microenviron. 2012;5:39–44. doi: 10.1007/s12307-011-0069-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zhai J., Shen J., Xie G., Wu J., He M., Gao L., Zhang Y., Yao X., Shen L. Cancer-associated fibroblasts-derived IL-8 mediates resistance to cisplatin in human gastric cancer. Cancer Lett. 2019;454:37–43. doi: 10.1016/j.canlet.2019.04.002. [DOI] [PubMed] [Google Scholar]
- 31.Qin X., Yan M., Wang X., Xu Q., Wang X., Zhu X., Shi J., Li Z., Zhang J., Chen W. Cancer-associated Fibroblast-derived IL-6 Promotes Head and Neck Cancer Progression via the Osteopontin-NF-kappa B Signaling Pathway. Theranostics. 2018;8:921–940. doi: 10.7150/thno.22182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Barajas-Gomez B.A., Rosas-Carrasco O., Morales-Rosales S.L., Pedraza Vazquez G., Gonzalez-Puertos V.Y., Juarez-Cedillo T., Garcia-Alvarez J.A., Lopez-Diazguerrero N.E., Damian-Matsumura P., Konigsberg M., et al. Relationship of inflammatory profile of elderly patients serum and senescence-associated secretory phenotype with human breast cancer cells proliferation: Role of IL6/IL8 ratio. Cytokine. 2017;91:13–29. doi: 10.1016/j.cyto.2016.12.001. [DOI] [PubMed] [Google Scholar]
- 33.Haraoka Y., Akieda Y., Nagai Y., Mogi C., Ishitani T. Zebrafish imaging reveals TP53 mutation switching oncogene-induced senescence from suppressor to driver in primary tumorigenesis. Nat. Commun. 2022;13:1417. doi: 10.1038/s41467-022-29061-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hayashi Y., Asuzu D.T., Bardsley M.R., Gajdos G.B., Kvasha S.M., Linden D.R., Nagy R.A., Saravanaperumal S.A., Syed S.A., Toyomasu Y., et al. Wnt-induced, TRP53-mediated Cell Cycle Arrest of Precursors Underlies Interstitial Cell of Cajal Depletion During Aging. Cell. Mol. Gastroenterol. Hepatol. 2021;11:117–145. doi: 10.1016/j.jcmgh.2020.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Liu H., Fergusson M.M., Castilho R.M., Liu J., Cao L., Chen J., Malide D., Rovira I.I., Schimel D., Kuo C.J., et al. Augmented Wnt signaling in a mammalian model of accelerated aging. Science. 2007;317:803–806. doi: 10.1126/science.1143578. [DOI] [PubMed] [Google Scholar]
- 36.Palmer A., Epton S., Crawley E., Straface M., Gammon L., Edgar M.M., Xu Y., Elahi S., Chin-Aleong J., Martin J.E., et al. Expression of p16 Within Myenteric Neurons of the Aged Colon: A Potential Marker of Declining Function. Front. Neurosci. 2021;15:747067. doi: 10.3389/fnins.2021.747067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.van Deursen J.M. The role of senescent cells in ageing. Nature. 2014;509:439–446. doi: 10.1038/nature13193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.SenNet Consortium NIH SenNet Consortium to map senescent cells throughout the human lifespan to understand physiological health. Nat. Aging. 2022;2:1090–1100. doi: 10.1038/s43587-022-00326-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Yousefzadeh M.J., Flores R.R., Zhu Y., Schmiechen Z.C., Brooks R.W., Trussoni C.E., Cui Y., Angelini L., Lee K.A., McGowan S.J., et al. An aged immune system drives senescence and ageing of solid organs. Nature. 2021;594:100–105. doi: 10.1038/s41586-021-03547-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Morbe U.M., Jorgensen P.B., Fenton T.M., von Burg N., Riis L.B., Spencer J., Agace W.W. Human gut-associated lymphoid tissues (GALT); diversity, structure, and function. Mucosal Immunol. 2021;14:793–802. doi: 10.1038/s41385-021-00389-4. [DOI] [PubMed] [Google Scholar]
- 41.Koboziev I., Karlsson F., Grisham M.B. Gut-associated lymphoid tissue, T cell trafficking, and chronic intestinal inflammation. Ann. N. Y. Acad. Sci. 2010;1207((Suppl. 1)):E86–E93. doi: 10.1111/j.1749-6632.2010.05711.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Martinet K.Z., Bloquet S., Bourgeois C. Ageing combines CD4 T cell lymphopenia in secondary lymphoid organs and T cell accumulation in gut associated lymphoid tissue. Immun. Ageing. 2014;11:8. doi: 10.1186/1742-4933-11-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Senda T., Dogra P., Granot T., Furuhashi K., Snyder M.E., Carpenter D.J., Szabo P.A., Thapa P., Miron M., Farber D.L. Microanatomical dissection of human intestinal T-cell immunity reveals site-specific changes in gut-associated lymphoid tissues over life. Mucosal Immunol. 2019;12:378–389. doi: 10.1038/s41385-018-0110-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Eisenstein M. Biology: A slow-motion epidemic. Nature. 2016;540:S98–S99. doi: 10.1038/540S98a. [DOI] [PubMed] [Google Scholar]
- 45.Ye Y., Manne S., Treem W.R., Bennett D. Prevalence of Inflammatory Bowel Disease in Pediatric and Adult Populations: Recent Estimates From Large National Databases in the United States, 2007–2016. Inflamm. Bowel Dis. 2020;26:619–625. doi: 10.1093/ibd/izz182. [DOI] [PubMed] [Google Scholar]
- 46.Mitsialis V., Wall S., Liu P., Ordovas-Montanes J., Parmet T., Vukovic M., Spencer D., Field M., McCourt C., Toothaker J., et al. Single-Cell Analyses of Colon and Blood Reveal Distinct Immune Cell Signatures of Ulcerative Colitis and Crohn’s Disease. Gastroenterology. 2020;159:591–608.e10. doi: 10.1053/j.gastro.2020.04.074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Uzzan M., Martin J.C., Mesin L., Livanos A.E., Castro-Dopico T., Huang R., Petralia F., Magri G., Kumar S., Zhao Q., et al. Ulcerative colitis is characterized by a plasmablast-skewed humoral response associated with disease activity. Nat. Med. 2022;28:766–779. doi: 10.1038/s41591-022-01680-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Cancro M.P. Age-Associated B Cells. Annu. Rev. Immunol. 2020;38:315–340. doi: 10.1146/annurev-immunol-092419-031130. [DOI] [PubMed] [Google Scholar]
- 49.Wang K.W., Zhan X., McAlpine W., Zhang Z., Choi J.H., Shi H., Misawa T., Yue T., Zhang D., Wang Y., et al. Enhanced susceptibility to chemically induced colitis caused by excessive endosomal TLR signaling in LRBA-deficient mice. Proc. Natl. Acad. Sci. USA. 2019;116:11380–11389. doi: 10.1073/pnas.1901407116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.McAlpine W., Sun L., Wang K.W., Liu A., Jain R., San Miguel M., Wang J., Zhang Z., Hayse B., McAlpine S.G., et al. Excessive endosomal TLR signaling causes inflammatory disease in mice with defective SMCR8-WDR41-C9ORF72 complex function. Proc. Natl. Acad. Sci. USA. 2018;115:E11523–E11531. doi: 10.1073/pnas.1814753115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Naradikian M.S., Myles A., Beiting D.P., Roberts K.J., Dawson L., Herati R.S., Bengsch B., Linderman S.L., Stelekati E., Spolski R., et al. Cutting Edge: IL-4, IL-21, and IFN-gamma Interact To Govern T-bet and CD11c Expression in TLR-Activated B Cells. J. Immunol. 2016;197:1023–1028. doi: 10.4049/jimmunol.1600522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Eiro N., Gonzalez L., Gonzalez L.O., Andicoechea A., Fernandez-Diaz M., Altadill A., Vizoso F.J. Study of the expression of toll-like receptors in different histological types of colorectal polyps and their relationship with colorectal cancer. J. Clin. Immunol. 2012;32:848–854. doi: 10.1007/s10875-012-9666-3. [DOI] [PubMed] [Google Scholar]
- 53.Yashiro M. Ulcerative colitis-associated colorectal cancer. World J. Gastroenterol. 2014;20:16389–16397. doi: 10.3748/wjg.v20.i44.16389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Shah S.C., Itzkowitz S.H. Colorectal Cancer in Inflammatory Bowel Disease: Mechanisms and Management. Gastroenterology. 2022;162:715–730.e3. doi: 10.1053/j.gastro.2021.10.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Giunco S., Petrara M.R., Bergamo F., Del Bianco P., Zanchetta M., Carmona F., Zagonel V., De Rossi A., Lonardi S. Immune senescence and immune activation in elderly colorectal cancer patients. Aging. 2019;11:3864–3875. doi: 10.18632/aging.102022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Matsumoto M., Kurihara S., Kibe R., Ashida H., Benno Y. Longevity in mice is promoted by probiotic-induced suppression of colonic senescence dependent on upregulation of gut bacterial polyamine production. PLoS ONE. 2011;6:e23652. doi: 10.1371/journal.pone.0023652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Risques R.A., Lai L.A., Himmetoglu C., Ebaee A., Li L., Feng Z., Bronner M.P., Al-Lahham B., Kowdley K.V., Lindor K.D., et al. Ulcerative colitis-associated colorectal cancer arises in a field of short telomeres, senescence, and inflammation. Cancer Res. 2011;71:1669–1679. doi: 10.1158/0008-5472.CAN-10-1966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Sohn J.J., Schetter A.J., Yfantis H.G., Ridnour L.A., Horikawa I., Khan M.A., Robles A.I., Hussain S.P., Goto A., Bowman E.D., et al. Macrophages, nitric oxide and microRNAs are associated with DNA damage response pathway and senescence in inflammatory bowel disease. PLoS ONE. 2012;7:e44156. doi: 10.1371/journal.pone.0044156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Smith K.J., Lassmann H. The role of nitric oxide in multiple sclerosis. Lancet Neurol. 2002;1:232–241. doi: 10.1016/S1474-4422(02)00102-3. [DOI] [PubMed] [Google Scholar]
- 60.Watanabe S., Hibiya S., Katsukura N., Kitagawa S., Sato A., Okamoto R., Watanabe M., Tsuchiya K. Importance of Telomere Shortening in the Pathogenesis of Ulcerative Colitis: A New Treatment From the Aspect of Telomeres in Intestinal Epithelial Cells. J. Crohn’s Colitis. 2022;16:109–121. doi: 10.1093/ecco-jcc/jjab115. [DOI] [PubMed] [Google Scholar]
- 61.Rubio C.A., Petris G.D.E., Puppa G. Gut-associated Lymphoid Tissue (GALT) Carcinoma in Ulcerative Colitis. Anticancer Res. 2018;38:919–921. doi: 10.21873/anticanres.12303. [DOI] [PubMed] [Google Scholar]
- 62.Martincorena I., Fowler J.C., Wabik A., Lawson A.R.J., Abascal F., Hall M.W.J., Cagan A., Murai K., Mahbubani K., Stratton M.R., et al. Somatic mutant clones colonize the human esophagus with age. Science. 2018;362:911–917. doi: 10.1126/science.aau3879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Kabir M.F., Karami A.L., Cruz-Acuna R., Klochkova A., Saxena R., Mu A., Murray M.G., Cruz J., Fuller A.D., Clevenger M.H., et al. Single cell transcriptomic analysis reveals cellular diversity of murine esophageal epithelium. Nat. Commun. 2022;13:2167. doi: 10.1038/s41467-022-29747-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Souza R.F. Reflux esophagitis and its role in the pathogenesis of Barrett’s metaplasia. J. Gastroenterol. 2017;52:767–776. doi: 10.1007/s00535-017-1342-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Pilotto A., Salles N. Helicobacter pylori infection in geriatrics. Helicobacter. 2002;7:56–62. doi: 10.1046/j.1523-5378.7.s1.9.x. [DOI] [PubMed] [Google Scholar]
- 66.Uemura N., Okamoto S., Yamamoto S., Matsumura N., Yamaguchi S., Yamakido M., Taniyama K., Sasaki N., Schlemper R.J. Helicobacter pylori infection and the development of gastric cancer. N. Engl. J. Med. 2001;345:784–789. doi: 10.1056/NEJMoa001999. [DOI] [PubMed] [Google Scholar]
- 67.Walecka-Kapica E., Knopik-Dabrowicz A., Klupinska G., Chojnacki J. The assessment of nitric oxide metabolites in gastric juice in Helicobacter pylori infected subjects in compliance with grade of inflammatory lesions in gastric mucosa. Pol. Merkur. Lekarski. 2008;24:95–100. [PubMed] [Google Scholar]
- 68.Neal J.T., Peterson T.S., Kent M.L., Guillemin K. H. pylori virulence factor CagA increases intestinal cell proliferation by Wnt pathway activation in a transgenic zebrafish model. Dis. Model. Mech. 2013;6:802–810. doi: 10.1242/dmm.011163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Song X., Xin N., Wang W., Zhao C. Wnt/beta-catenin, an oncogenic pathway targeted by H. pylori in gastric carcinogenesis. Oncotarget. 2015;6:35579–35588. doi: 10.18632/oncotarget.5758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Zuo W., Yang H., Li N., Ouyang Y., Xu X., Hong J. Helicobacter pylori infection activates Wnt/beta-catenin pathway to promote the occurrence of gastritis by upregulating ASCL1 and AQP5. Cell Death Discov. 2022;8:257. doi: 10.1038/s41420-022-01026-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Liu B., Dong J., Wang S., Yu H., Li Z., Sun P., Zhao L. Helicobacter pylori causes delayed gastric emptying by decreasing interstitial cells of Cajal. Exp. Ther. Med. 2021;22:663. doi: 10.3892/etm.2021.10095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Zeng S., Seifert A.M., Zhang J.Q., Cavnar M.J., Kim T.S., Balachandran V.P., Santamaria-Barria J.A., Cohen N.A., Beckman M.J., Medina B.D., et al. Wnt/beta-catenin Signaling Contributes to Tumor Malignancy and Is Targetable in Gastrointestinal Stromal Tumor. Mol. Cancer Ther. 2017;16:1954–1966. doi: 10.1158/1535-7163.MCT-17-0139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Kagihara J., Matsuda B., Young K.L., Li X., Lao X., Deshpande G.A., Omata F., Burnett T., Lynch C.F., Hernandez B.Y., et al. Novel association between Helicobacter pylori infection and gastrointestinal stromal tumors (GIST) in a multi-ethnic population. Gastrointest. Stromal Tumor. 2020;3:1. doi: 10.21037/gist-20-2. [DOI] [Google Scholar]
- 74.Goldenring J.R., Mills J.C. Cellular Plasticity, Reprogramming, and Regeneration: Metaplasia in the Stomach and Beyond. Gastroenterology. 2022;162:415–430. doi: 10.1053/j.gastro.2021.10.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Wang D., Cabalag C.S., Clemons N.J., DuBois R.N. Cyclooxygenases and Prostaglandins in Tumor Immunology and Microenvironment of Gastrointestinal Cancer. Gastroenterology. 2021;161:1813–1829. doi: 10.1053/j.gastro.2021.09.059. [DOI] [PubMed] [Google Scholar]
- 76.Guzik T.J., Korbut R., Adamek-Guzik T. Nitric oxide and superoxide in inflammation and immune regulation. J. Physiol. Pharmacol. 2003;54:469–487. [PubMed] [Google Scholar]
- 77.De Salvo C., Pastorelli L., Petersen C.P., Butto L.F., Buela K.A., Omenetti S., Locovei S.A., Ray S., Friedman H.R., Duijser J., et al. Interleukin 33 Triggers Early Eosinophil-Dependent Events Leading to Metaplasia in a Chronic Model of Gastritis-Prone Mice. Gastroenterology. 2021;160:302–316.e7. doi: 10.1053/j.gastro.2020.09.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Meyer A.R., Goldenring J.R. Injury, repair, inflammation and metaplasia in the stomach. J. Physiol. 2018;596:3861–3867. doi: 10.1113/JP275512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Eggert T., Wolter K., Ji J., Ma C., Yevsa T., Klotz S., Medina-Echeverz J., Longerich T., Forgues M., Reisinger F., et al. Distinct Functions of Senescence-Associated Immune Responses in Liver Tumor Surveillance and Tumor Progression. Cancer Cell. 2016;30:533–547. doi: 10.1016/j.ccell.2016.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Garbers C., Kuck F., Aparicio-Siegmund S., Konzak K., Kessenbrock M., Sommerfeld A., Haussinger D., Lang P.A., Brenner D., Mak T.W., et al. Cellular senescence or EGFR signaling induces Interleukin 6 (IL-6) receptor expression controlled by mammalian target of rapamycin (mTOR) Cell Cycle. 2013;12:3421–3432. doi: 10.4161/cc.26431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Chen Z., Trotman L.C., Shaffer D., Lin H.K., Dotan Z.A., Niki M., Koutcher J.A., Scher H.I., Ludwig T., Gerald W., et al. Crucial role of p53-dependent cellular senescence in suppression of Pten-deficient tumorigenesis. Nature. 2005;436:725–730. doi: 10.1038/nature03918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Akahoshi K., Oya M., Koga T., Shiratsuchi Y. Current clinical management of gastrointestinal stromal tumor. World J. Gastroenterol. 2018;24:2806–2817. doi: 10.3748/wjg.v24.i26.2806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Fujimaki K., Yao G. Cell dormancy plasticity: Quiescence deepens into senescence through a dimmer switch. Physiol. Genom. 2020;52:558–562. doi: 10.1152/physiolgenomics.00068.2020. [DOI] [PubMed] [Google Scholar]
- 84.DeCaprio J.A., Duensing A. The DREAM complex in antitumor activity of imatinib mesylate in gastrointestinal stromal tumors. Curr. Opin. Oncol. 2014;26:415–421. doi: 10.1097/CCO.0000000000000090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Boichuk S., Parry J.A., Makielski K.R., Litovchick L., Baron J.L., Zewe J.P., Wozniak A., Mehalek K.R., Korzeniewski N., Seneviratne D.S., et al. The DREAM complex mediates GIST cell quiescence and is a novel therapeutic target to enhance imatinib-induced apoptosis. Cancer Res. 2013;73:5120–5129. doi: 10.1158/0008-5472.CAN-13-0579. [DOI] [PubMed] [Google Scholar]
- 86.Chen J.Y., Lin J.R., Tsai F.C., Meyer T. Dosage of Dyrk1a shifts cells within a p21-cyclin D1 signaling map to control the decision to enter the cell cycle. Mol. Cell. 2013;52:87–100. doi: 10.1016/j.molcel.2013.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Hayashi Y., Nguyen V.T.T. A narrative review of imatinib-resistant gastrointestinal stromal tumors. Gastrointest. Stromal Tumor. 2021;4:6. doi: 10.21037/gist-21-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Chen T., Ni N., Yuan L., Xu L., Bahri N., Sun B., Wu Y., Ou W.B. Proteasome Inhibition Suppresses KIT-Independent Gastrointestinal Stromal Tumors Via Targeting Hippo/YAP/Cyclin D1 Signaling. Front. Pharmacol. 2021;12:686874. doi: 10.3389/fphar.2021.686874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Hu T.H., Tai M.H., Chuah S.K., Chen H.H., Lin J.W., Huang H.Y., Chou Y.P., Yi L.N., Kuo C.M., Changchien C.S. Elevated p21 expression is associated with poor prognosis of rectal stromal tumors after resection. J. Surg. Oncol. 2008;98:117–123. doi: 10.1002/jso.21094. [DOI] [PubMed] [Google Scholar]
- 90.Tsai M.C., Lin J.W., Lin S.E., Chen H.H., Lee C.M., Hu T.H. Prognostic analysis of rectal stromal tumors by reference of National Institutes of Health risk categories and immunohistochemical studies. Dis. Colon Rectum. 2008;51:1535–1543. doi: 10.1007/s10350-008-9370-9. [DOI] [PubMed] [Google Scholar]
- 91.Chou Y.P., Lin J.W., Wang C.C., Chiu Y.C., Huang C.C., Chuah S.K., Tai M.H., Yi L.N., Lee C.M., Changchien C.S., et al. The abnormalities in the p53/p21WAF1 pathway have a significant role in the pathogenesis and progression of gastrointestinal stromal tumors. Oncol. Rep. 2008;19:49–56. doi: 10.3892/or.19.1.49. [DOI] [PubMed] [Google Scholar]
- 92.Cai Q., Shi P., Yuan Y., Peng J., Ou X., Zhou W., Li J., Su T., Lin L., Cai S., et al. Inflammation-Associated Senescence Promotes Helicobacter pylori-Induced Atrophic Gastritis. Cell. Mol. Gastroenterol. Hepatol. 2021;11:857–880. doi: 10.1016/j.jcmgh.2020.10.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Deguchi R., Takagi A., Kawata H., Inoko H., Miwa T. Association between CagA+ Helicobacter pylori infection and p53, bax and transforming growth factor-beta-RII gene mutations in gastric cancer patients. Int. J. Cancer. 2001;91:481–485. doi: 10.1002/1097-0215(200002)9999:9999<::AID-IJC1088>3.0.CO;2-B. [DOI] [PubMed] [Google Scholar]
- 94.Khare T., Bissonnette M., Khare S. CXCL12-CXCR4/CXCR7 Axis in Colorectal Cancer: Therapeutic Target in Preclinical and Clinical Studies. Int. J. Mol. Sci. 2021;22:7371. doi: 10.3390/ijms22147371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Siegel R.L., Miller K.D., Fuchs H.E., Jemal A. Cancer Statistics, 2021. CA Cancer J. Clin. 2021;71:7–33. doi: 10.3322/caac.21654. [DOI] [PubMed] [Google Scholar]
- 96.Choi Y.W., Kim Y.H., Oh S.Y., Suh K.W., Kim Y.S., Lee G.Y., Yoon J.E., Park S.S., Lee Y.K., Park Y.J., et al. Senescent Tumor Cells Build a Cytokine Shield in Colorectal Cancer. Adv. Sci. 2021;8:2002497. doi: 10.1002/advs.202002497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Cougnoux A., Dalmasso G., Martinez R., Buc E., Delmas J., Gibold L., Sauvanet P., Darcha C., Dechelotte P., Bonnet M., et al. Bacterial genotoxin colibactin promotes colon tumour growth by inducing a senescence-associated secretory phenotype. Gut. 2014;63:1932–1942. doi: 10.1136/gutjnl-2013-305257. [DOI] [PubMed] [Google Scholar]
- 98.Short S., Fielder E., Miwa S., von Zglinicki T. Senolytics and senostatics as adjuvant tumour therapy. EBioMedicine. 2019;41:683–692. doi: 10.1016/j.ebiom.2019.01.056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Hickson L.J., Langhi Prata L.G.P., Bobart S.A., Evans T.K., Giorgadze N., Hashmi S.K., Herrmann S.M., Jensen M.D., Jia Q., Jordan K.L., et al. Senolytics decrease senescent cells in humans: Preliminary report from a clinical trial of Dasatinib plus Quercetin in individuals with diabetic kidney disease. EBioMedicine. 2019;47:446–456. doi: 10.1016/j.ebiom.2019.08.069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Zhu Y., Prata L., Gerdes E.O.W., Netto J.M.E., Pirtskhalava T., Giorgadze N., Tripathi U., Inman C.L., Johnson K.O., Xue A., et al. Orally-active, clinically-translatable senolytics restore alpha-Klotho in mice and humans. EBioMedicine. 2022;77:103912. doi: 10.1016/j.ebiom.2022.103912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Rouault C., Marcelin G., Adriouch S., Rose C., Genser L., Ambrosini M., Bichet J.C., Zhang Y., Marquet F., Aron-Wisnewsky J., et al. Senescence-associated beta-galactosidase in subcutaneous adipose tissue associates with altered glycaemic status and truncal fat in severe obesity. Diabetologia. 2021;64:240–254. doi: 10.1007/s00125-020-05307-0. [DOI] [PubMed] [Google Scholar]
- 102.Kolodkin-Gal D., Roitman L., Ovadya Y., Azazmeh N., Assouline B., Schlesinger Y., Kalifa R., Horwitz S., Khalatnik Y., Hochner-Ger A., et al. Senolytic elimination of Cox2-expressing senescent cells inhibits the growth of premalignant pancreatic lesions. Gut. 2022;71:345–355. doi: 10.1136/gutjnl-2020-321112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Wang T.W., Johmura Y., Suzuki N., Omori S., Migita T., Yamaguchi K., Hatakeyama S., Yamazaki S., Shimizu E., Imoto S., et al. Blocking PD-L1-PD-1 improves senescence surveillance and ageing phenotypes. Nature. 2022;611:358–364. doi: 10.1038/s41586-022-05388-4. [DOI] [PubMed] [Google Scholar]
- 104.Saccon T.D., Nagpal R., Yadav H., Cavalcante M.B., Nunes A.D.C., Schneider A., Gesing A., Hughes B., Yousefzadeh M., Tchkonia T., et al. Senolytic Combination of Dasatinib and Quercetin Alleviates Intestinal Senescence and Inflammation and Modulates the Gut Microbiome in Aged Mice. J. Gerontol. A Biol. Sci. Med. Sci. 2021;76:1895–1905. doi: 10.1093/gerona/glab002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Hine C., Harputlugil E., Zhang Y., Ruckenstuhl C., Lee B.C., Brace L., Longchamp A., Trevino-Villarreal J.H., Mejia P., Ozaki C.K., et al. Endogenous hydrogen sulfide production is essential for dietary restriction benefits. Cell. 2015;160:132–144. doi: 10.1016/j.cell.2014.11.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Latorre E., Torregrossa R., Wood M.E., Whiteman M., Harries L.W. Mitochondria-targeted hydrogen sulfide attenuates endothelial senescence by selective induction of splicing factors HNRNPD and SRSF2. Aging. 2018;10:1666–1681. doi: 10.18632/aging.101500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Yu H., Yu Q., Mi Y., Wang P., Jin S., Xiao L., Guo Q., Wu Y. Hydrogen Sulfide Inhibited Sympathetic Activation in D-Galactose-Induced Aging Rats by Upregulating Klotho and Inhibiting Inflammation in the Paraventricular Nucleus. Biomedicines. 2023;11:566. doi: 10.3390/biomedicines11020566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Zivanovic J., Kouroussis E., Kohl J.B., Adhikari B., Bursac B., Schott-Roux S., Petrovic D., Miljkovic J.L., Thomas-Lopez D., Jung Y., et al. Selective Persulfide Detection Reveals Evolutionarily Conserved Antiaging Effects of S-Sulfhydration. Cell Metab. 2019;30:1152–1170.e13. doi: 10.1016/j.cmet.2019.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Wilkie S.E., Borland G., Carter R.N., Morton N.M., Selman C. Hydrogen sulfide in ageing, longevity and disease. Biochem. J. 2021;478:3485–3504. doi: 10.1042/BCJ20210517. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.