Abstract
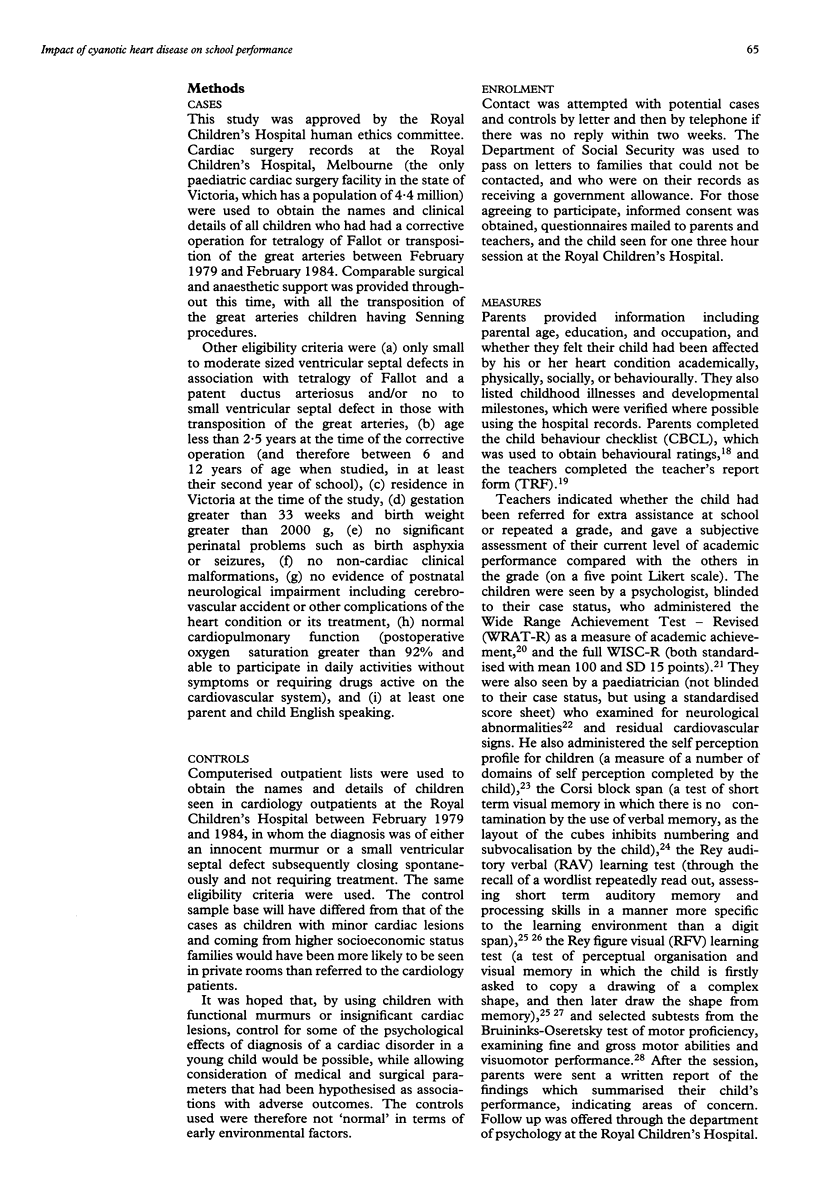
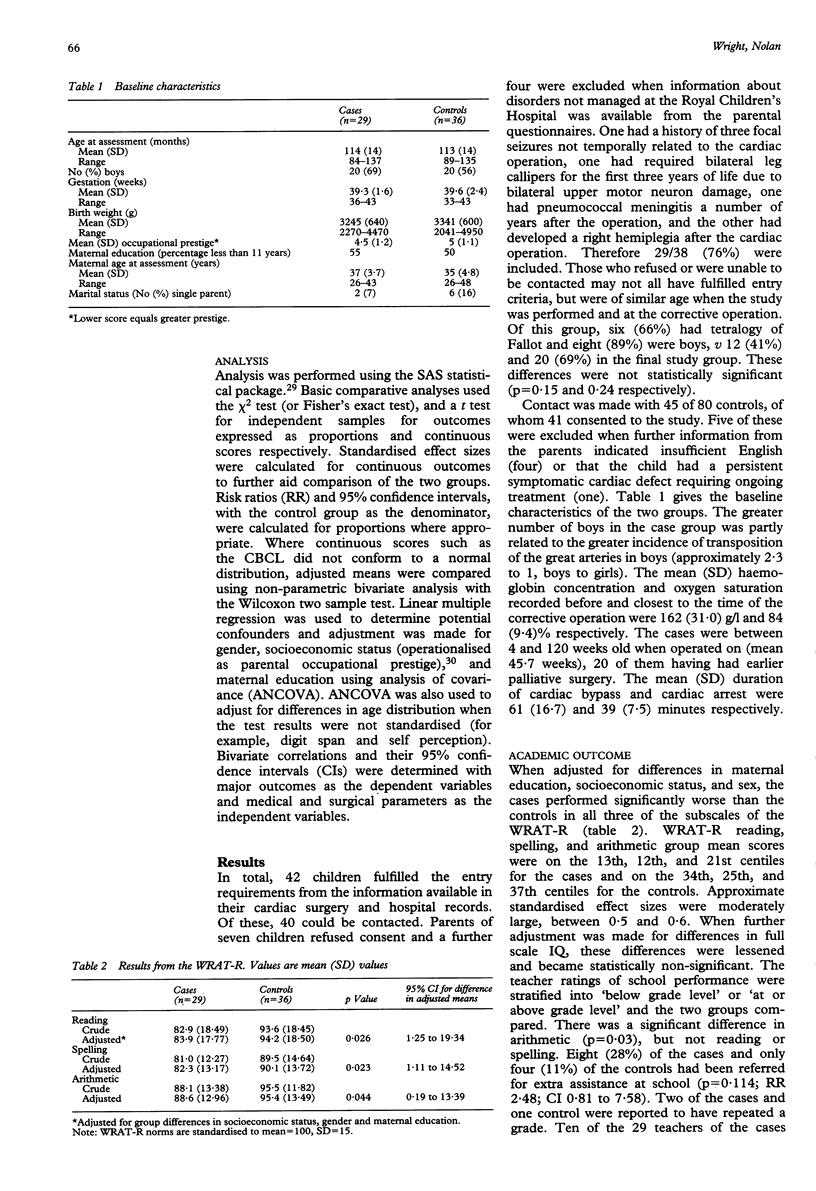
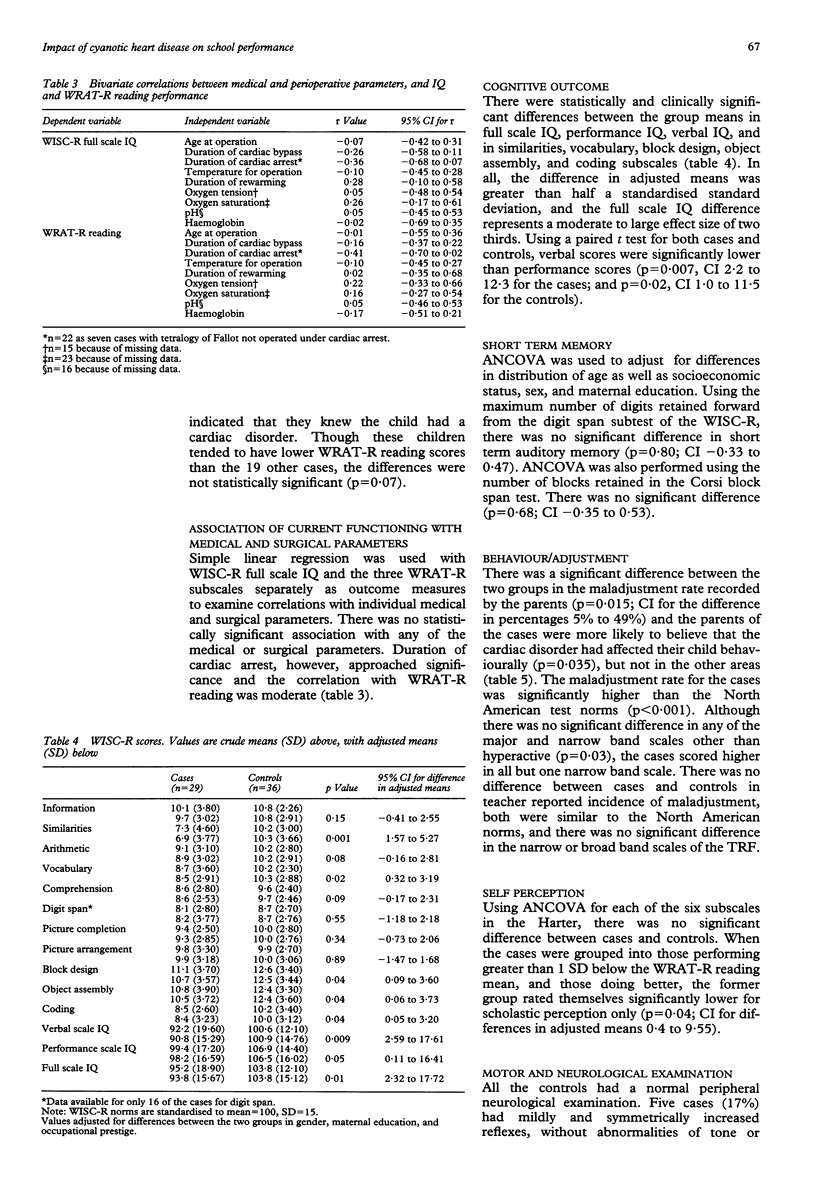
Surgical correction greatly decreases the mortality and cardiac morbidity of cyanotic congenital heart disease, but children remain at risk of long term difficulties in other areas. A historical cohort study was conducted to determine the relation between heart disease and school performance in 29 children aged 7 to 12 years old with simple transposition of the great arteries or tetralogy of Fallot. All children had surgical correction of their lesion before 2.5 years of age. Those at greater risk of school difficulties because of recognised complications of their heart disease or for reasons other than directly attributable to the heart disease were excluded. Comparison was made with 36 children who had presented with cardiac murmurs at a similar age, but who did not require treatment. Children with cyanotic disease showed significantly poorer performance in all academic areas assessed by the Wide Range Achievement Test-Revised; the difference in group mean score (adjusted for differences in maternal education, sex, and parental occupational prestige) for reading was 10.3 points (confidence interval (CI) 1.25 to 19.34), for spelling 7.8 (CI 1.11 to 14.52), and for arithmetic 6.8 (CI 0.19 to 13.39). The differences in adjusted group means for the Wechsler Intelligence Scale for Children-Revised full scale, performance and verbal IQs were significant, particularly the later at 10.1 points (CI 2.59 to 17.61). Teacher reports indicated significant differences in arithmetic when outcome was dichotomised to 'below grade' or 'not below grade'. There were no significant associations between outcome measures and the medical or perioperative parameters, however, including those related to hypoxia. It is concluded that the increased incidence of academic problems and the nature of the cognitive difficulties in children with uncomplicated corrective cardiac surgery for cyanotic heart disease are not fully explained by chronic hypoxia, or by other factors related to the cardiac surgery.
Full text
PDF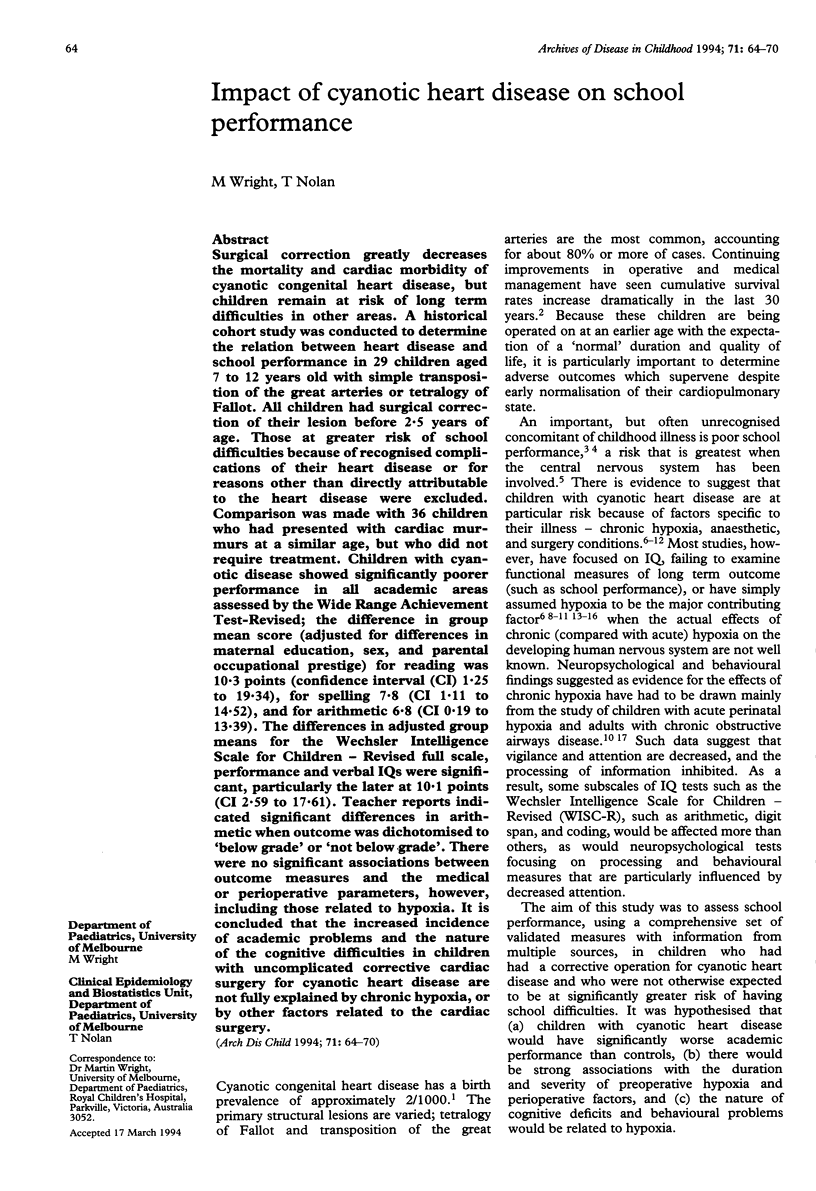
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Aisenberg R. B., Rosenthal A., Nadas A. S., Wolff P. H. Developmental delay in infants with congenital heart disease. Correlation with hypoxemia and congestive heart failure. Pediatr Cardiol. 1982;3(2):133–137. doi: 10.1007/BF02312960. [DOI] [PubMed] [Google Scholar]
- Aisenberg R. B., Rosenthal A., Wolff P. H., Nadas A. S. Hypoxemia and critical flicker frequency in congenital heart disease. Am J Dis Child. 1974 Sep;128(3):335–338. doi: 10.1001/archpedi.1974.02110280065008. [DOI] [PubMed] [Google Scholar]
- Bellinger D. C., Wernovsky G., Rappaport L. A., Mayer J. E., Jr, Castaneda A. R., Farrell D. M., Wessel D. L., Lang P., Hickey P. R., Jonas R. A. Cognitive development of children following early repair of transposition of the great arteries using deep hypothermic circulatory arrest. Pediatrics. 1991 May;87(5):701–707. [PubMed] [Google Scholar]
- DeMaso D. R., Beardslee W. R., Silbert A. R., Fyler D. C. Psychological functioning in children with cyanotic heart defects. J Dev Behav Pediatr. 1990 Dec;11(6):289–294. [PubMed] [Google Scholar]
- Dickinson D. F., Sambrooks J. E. Intellectual performance in children after circulatory arrest with profound hypothermia in infancy. Arch Dis Child. 1979 Jan;54(1):1–6. doi: 10.1136/adc.54.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feldt R. H., Ewert J. C., Stickler G. B., Weidman W. H. Children with congenital heart disease. Motor development and intelligence. Am J Dis Child. 1969 Mar;117(3):281–287. doi: 10.1001/archpedi.1969.02100030283005. [DOI] [PubMed] [Google Scholar]
- Fowler M. G., Johnson M. P., Atkinson S. S. School achievement and absence in children with chronic health conditions. J Pediatr. 1985 Apr;106(4):683–687. doi: 10.1016/s0022-3476(85)80103-7. [DOI] [PubMed] [Google Scholar]
- GREEN M., SOLNIT A. J. REACTIONS TO THE THREATENED LOSS OF A CHILD: A VULNERABLE CHILD SYNDROME. PEDIATRIC MANAGEMENT OF THE DYING CHILD, PART III. Pediatrics. 1964 Jul;34:58–66. [PubMed] [Google Scholar]
- Gonzalez-Pardo L., Miles M., Taylor M., Mattioli L. Congenital heart disease: developmental and neurological evaluation in preschool children. J Kans Med Soc. 1981 Mar;82(3):115-8, 136. [PubMed] [Google Scholar]
- Gortmaker S. L., Walker D. K., Weitzman M., Sobol A. M. Chronic conditions, socioeconomic risks, and behavioral problems in children and adolescents. Pediatrics. 1990 Mar;85(3):267–276. [PubMed] [Google Scholar]
- Hesz N., Clark E. B. Cognitive development in transposition of the great vessels. Arch Dis Child. 1988 Feb;63(2):198–200. doi: 10.1136/adc.63.2.198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kramer H. H., Awiszus D., Sterzel U., van Halteren A., Classen R. Development of personality and intelligence in children with congenital heart disease. J Child Psychol Psychiatry. 1989 Mar;30(2):299–308. doi: 10.1111/j.1469-7610.1989.tb00242.x. [DOI] [PubMed] [Google Scholar]
- Linde L. M., Rasof B., Dunn O. J. Longitudinal studies of intellectual and behavioral development in children with congenital heart disease. Acta Paediatr Scand. 1970 Mar;59(2):169–176. doi: 10.1111/j.1651-2227.1970.tb08984.x. [DOI] [PubMed] [Google Scholar]
- Linde L. M., Rasof B., Dunn O. J. Mental development in congenital heart disease. J Pediatr. 1967 Aug;71(2):198–203. doi: 10.1016/s0022-3476(67)80072-6. [DOI] [PubMed] [Google Scholar]
- Linde L. M., Rasof B., Dunn O. J., Rabb E. Attitudinal factors in congenital heart disease. Pediatrics. 1966 Jul;38(1):92–101. [PubMed] [Google Scholar]
- Mendoza J. C., Wilkerson S. A., Reese A. H. Follow-up of patients who underwent arterial switch repair for transposition of the great arteries. Am J Dis Child. 1991 Jan;145(1):40–43. doi: 10.1001/archpedi.1991.02160010042013. [DOI] [PubMed] [Google Scholar]
- Messmer B. J., Schallberger U., Gattiker R., Senning A. Psychomotor and intellectual development after deep hypothermia and circulatory arrest in early infancy. J Thorac Cardiovasc Surg. 1976 Oct;72(4):495–502. [PubMed] [Google Scholar]
- Milner B., Taylor L. Right-hemisphere superiority in tactile pattern-recognition after cerebral commissurotomy: evidence for nonverbal memory. Neuropsychologia. 1972 Apr;10(1):1–15. doi: 10.1016/0028-3932(72)90038-3. [DOI] [PubMed] [Google Scholar]
- Morris C. D., Menashe V. D. 25-year mortality after surgical repair of congenital heart defect in childhood. A population-based cohort study. JAMA. 1991 Dec 25;266(24):3447–3452. [PubMed] [Google Scholar]
- Myers-Vando R., Steward M. S., Folkins C. H., Hines P. The effects of congenital heart disease on cognitive development, illness causality concepts, and vulnerability. Am J Orthopsychiatry. 1979 Oct;49(4):617–625. doi: 10.1111/j.1939-0025.1979.tb02647.x. [DOI] [PubMed] [Google Scholar]
- Newburger J. W., Silbert A. R., Buckley L. P., Fyler D. C. Cognitive function and age at repair of transposition of the great arteries in children. N Engl J Med. 1984 Jun 7;310(23):1495–1499. doi: 10.1056/NEJM198406073102303. [DOI] [PubMed] [Google Scholar]
- Norwood W. I., Dobell A. R., Freed M. D., Kirklin J. W., Blackstone E. H. Intermediate results of the arterial switch repair. A 20-institution study. J Thorac Cardiovasc Surg. 1988 Dec;96(6):854–863. [PubMed] [Google Scholar]
- O'Dougherty M., Nuechterlein K. H., Drew B. Hyperactive and hypoxic children: signal detection, sustained attention, and behavior. J Abnorm Psychol. 1984 May;93(2):178–191. doi: 10.1037//0021-843x.93.2.178. [DOI] [PubMed] [Google Scholar]
- O'Dougherty M., Wright F. S., Garmezy N., Loewenson R. B., Torres F. Later competence and adaptation in infants who survive severe heart defects. Child Dev. 1983 Oct;54(5):1129–1142. [PubMed] [Google Scholar]
- O'Dougherty M., Wright F. S., Loewenson R. B., Torres F. Cerebral dysfunction after chronic hypoxia in children. Neurology. 1985 Jan;35(1):42–46. doi: 10.1212/wnl.35.1.42. [DOI] [PubMed] [Google Scholar]
- Robertson C. M., Finer N. N., Grace M. G. School performance of survivors of neonatal encephalopathy associated with birth asphyxia at term. J Pediatr. 1989 May;114(5):753–760. doi: 10.1016/s0022-3476(89)80132-5. [DOI] [PubMed] [Google Scholar]
- SIMONSON E., WINCHELL P. Effect of high carbon dioxide and of low oxygen concentration on fusion frequency of flicker. J Appl Physiol. 1951 May;3(11):637–641. doi: 10.1152/jappl.1951.3.11.637. [DOI] [PubMed] [Google Scholar]
- Shampaine E. L., Nadelman L., Rosenthal A., Behrendt D., Sloan H. Longitudinal psychological assessment in tetralogy of Fallot. Pediatr Cardiol. 1989 Summer;10(3):135–140. doi: 10.1007/BF02081676. [DOI] [PubMed] [Google Scholar]
- Silbert A., Wolff P. H., Mayer B., Rosenthal A., Nadas A. S. Cyanotic heart disease and psychological development. Pediatrics. 1969 Feb;43(2):192–200. [PubMed] [Google Scholar]
- Wells F. C., Coghill S., Caplan H. L., Lincoln C. Duration of circulatory arrest does influence the psychological development of children after cardiac operation in early life. J Thorac Cardiovasc Surg. 1983 Dec;86(6):823–831. [PubMed] [Google Scholar]


