Abstract
Nonalcoholic fatty liver disease (NAFLD) is a prevalent condition among postmenopausal women that can lead to severe liver dysfunction and increased mortality. In recent years, research has focused on identifying potential lifestyle dietary interventions that may prevent or treat NAFLD in this population. Due to the complex and multifactorial nature of NAFLD in postmenopausal women, the disease can present as different subtypes, with varying levels of clinical presentation and variable treatment responses. By recognizing the significant heterogeneity of NAFLD in postmenopausal women, it may be possible to identify specific subsets of individuals who may benefit from targeted nutritional interventions. The purpose of this review was to examine the current evidence supporting the role of three specific nutritional factors—choline, soy isoflavones, and probiotics—as potential nutritional adjuvants in the prevention and treatment of NAFLD in postmenopausal women. There is promising evidence supporting the potential benefits of these nutritional factors for NAFLD prevention and treatment, particularly in postmenopausal women, and further research is warranted to confirm their effectiveness in alleviating hepatic steatosis in this population.
Keywords: nonalcoholic fatty liver disease, heterogeneity, women, menopause, estrogen, nutrition, choline, soy isoflavones, probiotics
1. Introduction
NAFLD is a chronic condition that develops due to an excessive accumulation of fat in the liver. It is a heterogeneous disorder that encompasses a range of liver diseases with varying degrees of severity, clinical characteristics, and outcomes. This spectrum includes isolated steatosis, which is defined as the accumulation of lipids in 5% or more of hepatocytes, as well as nonalcoholic steatohepatitis (NASH), which is characterized by liver inflammation and hepatocellular injury. In some individuals, NASH can progress to liver fibrosis, cirrhosis, and hepatocellular carcinoma [1]. Histological features of NAFLD also vary, including degrees of steatosis, inflammation, ballooning, and fibrosis. Predicting the disease trajectory in individual patients is a significant clinical challenge due to these variations.
The heterogeneity of NAFLD is multifactorial, stemming from a complex interplay of genetic and environmental factors, underlying pathophysiological mechanisms, and coexisting medical conditions, especially obesity, insulin resistance, and metabolic syndrome [2,3,4,5]. Indeed, the term “MAFLD” (metabolic dysfunction-associated fatty liver disease) has recently been proposed to more accurately capture its strong association with metabolic disorders such as obesity, insulin resistance, type 2 diabetes, dyslipidemia, and hypertension [6]. MAFLD encompasses a broader spectrum of liver diseases, including NAFLD, and comprises a wider range of affected individuals, including those with lean body mass and of a normal weight. Similar to NAFLD, MAFLD can progress from simple steatosis to severe liver disease, including hepatocellular carcinoma. Such heterogeneity has significant clinical implications that can affect the diagnosis, prognosis, and treatment of NAFLD [7]. For instance, some patients may rapidly progress to advanced stages of the disease, while others may remain stable or even improve over time [8]. Therefore, a personalized approach to NAFLD diagnosis and management is essential, one which considers the various subtypes and stages of the disease and individual risk factors and characteristics of each patient.
The prevalence of NAFLD is on the rise globally, with up to one-third of adults in Western countries affected, and even higher rates among individuals with obesity, type 2 diabetes, and metabolic syndrome [5]. Following menopause, women are at an increased risk of developing both NAFLD and advanced NASH fibrosis, with a prevalence that is comparable to, or even higher, than that in men of the same age, with rates between 15–62%, depending on geographical location, ethnicity, and method of diagnosis [9,10,11]. In addition, postmenopausal women have higher rates of advanced fibrosis compared to men (36.1% vs. 17.7%) [12]. While NAFLD is generally more prevalent in men, there has been a significant increase in its prevalence among women over the past decade, from 18.5% in 1988–1994 to 21.3% in 1999–2006 and to 24.9% in 2007–2014 [13]. Women are also experiencing a steeper annual rate increase [14] and higher mortality rate compared to men [15]. Notably, NASH has emerged as the leading reason for liver transplantation in women [16].
Because NAFLD is closely linked with obesity and insulin resistance [17], lifestyle modifications are the most effective approach to treating the condition. Specifically, reducing caloric intake, limiting consumption of simple sugars and saturated fats, and increasing physical activity levels to promote weight loss and improve metabolic parameters are recommended as the first-line therapy for NAFLD patients [18,19]. Controlling underlying metabolic conditions such as diabetes, hypertension, and hypercholesterolemia can further decrease the risk of NAFLD. Modest weight loss, representing only 5–10% of the total body weight, has been shown to reduce liver fat and improve liver function [20,21], even in individuals with a normal body weight [22,23].
While it may seem reasonable to expect that lifestyle modifications resulting in weight loss and improved metabolic parameters in postmenopausal women would lead to reductions in liver fat content, there are limited studies that investigate the role of diet in NAFLD. A recent randomized dietary intervention trial discovered that both paleolithic (high intake of vegetables, fruit, nuts, eggs, fish, and lean meat, while excluding refined sugar, salt, dairy products, and grains) and conventional low-fat diets (high intake of fruit, vegetables, whole grains, and fish, with low-fat meat and dairy products) resulted in a ~50% reduction of liver fat in healthy postmenopausal women with obesity [24]. In this study, it was observed that the reduction of liver fat in the low-fat diet group was linked to weight loss, while the paleolithic diet group exhibited improvements in liver fat due to a greater proportion of mono- and polyunsaturated fatty acids. These findings suggest that different dietary patterns may provide benefit to the liver through distinct mechanisms.
In a post hoc analysis of 4162 postmenopausal women from the UK Women’s Cohort Study, higher adherence to the Mediterranean diet, which is the recommended dietary pattern for all NAFLD patients [25], was associated with a smaller increase in waist circumference and a reduced risk of abdominal obesity in postmenopausal women with overweight [26]. A cross-sectional analysis of 2000 women revealed that greater adherence to the Mediterranean diet was linked with a reduced risk of metabolically unhealthy obesity in postmenopausal women; this association was not observed in premenopausal women [27]. However, a different study found that adherence to this diet had a favorable impact on hepatic steatosis in both postmenopausal and premenopausal women, albeit with a stronger effect observed in the latter [28].
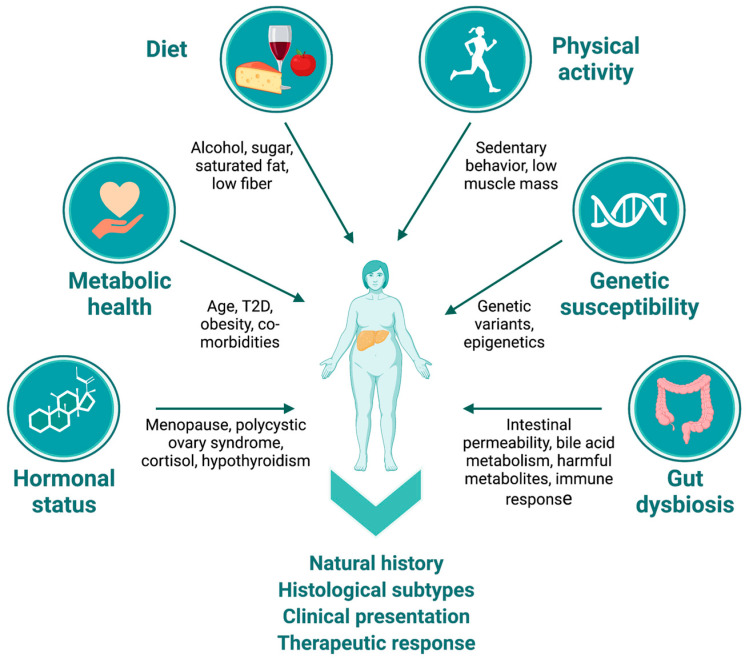
There are several factors that contribute to the complex heterogeneity underlying NAFLD that are particularly relevant in postmenopausal women. These include hormonal status, age, lifestyle factors, genetic factors, and gut dysbiosis (Figure 1). Hormones, especially sex hormones, have been shown to influence the development and progression of NAFLD, with the decline in estrogen levels after menopause contributing significantly to disease risk [29]. Increasing age is also an important factor that can affect the natural history of NAFLD in this population, as older individuals are more likely to have comorbidities that can exacerbate the disease [30,31]. Moreover, age-related changes in metabolism and hormone levels can also contribute to the progression of NAFLD [32]. Other hormonal imbalances, such as those observed in polycystic ovary syndrome (PCOS), are known to increase the risk of NAFLD [33]. Lifestyle factors such as diet, exercise, and alcohol consumption can interact dynamically with other factors to affect the development and natural history of NAFLD in all individuals, including postmenopausal women [34]. Metabolic health is a critical factor in the development and progression of NAFLD, with comorbidities such as insulin resistance, dyslipidemia, and metabolic syndrome increasing the risk of developing and progressing to NASH [35].
Figure 1.
NAFLD heterogeneity in postmenopausal women. Multiple etiological factors contribute to heterogeneity in natural history, histological subtypes, clinical presentation, and response to therapeutic interventions in postmenopausal women. Factors such as hormonal status, age, metabolic health and presence of comorbidities, quality of habitual diet, alcohol consumption patterns, levels of physical activity, genetic factors/ethnicity, and presence of gut dysbiosis through diverse mechanisms often interact dynamically to affect the clinical presentation of NAFLD in this population. (Figure created with BioRender.com, accessed on 31 May 2023).
NAFLD is a moderately heritable condition [36], and several common genetic variants have been consistently associated with risk of NAFLD across diverse populations [37]. Genetic factors can also influence the presentation of NAFLD in postmenopausal women. For instance, the rs738409 variant in the patatin-like phospholipase domain-containing protein 3 gene (PNPLA3) has been found to significantly modulate the relationship between dietary intake and fibrosis severity in a dose-dependent, genotype-specific manner. Specifically, carriers of the variant allele were more affected by dietary factors such as carbohydrate, n-3 polyunsaturated fatty acids, isoflavones, methionine, and choline [38]. Likewise, variants in the phosphatidylethanolamine N-methyltransferase gene (PEMT) can worsen the effects of insufficient choline intake on NAFLD risk in postmenopausal women [39]. Additionally, epigenetic modifications contribute to heterogeneity in the manifestation of NAFLD. For example, Sokolowska et al. [40] recently found that changes in the blood methylomes of NAFLD patients in response to a Mediterranean diet were correlated with improvements in hepatic steatosis and could stratify liver biopsies by fibrosis grade.
Gut dysbiosis, or alterations in the gut microbiota, is another factor known to contribute to the development and progression of NAFLD. Dysbiosis can lead to an increase in gut-derived endotoxins, triggering inflammation in the liver and contributing to the disease [41].
Due to the complex and multifactorial nature of NAFLD in postmenopausal women, the disease can present as different subtypes, with varying levels of clinical presentation, diverse pathological mechanisms, and treatment responses. By recognizing the significant heterogeneity of NAFLD in postmenopausal women, we might identify specific subsets of individuals who may benefit from targeted nutritional interventions. The objectives of this review were to explore the increased risk of NAFLD in postmenopausal women and examine the current evidence supporting the role of three specific nutritional factors—choline, soy isoflavones, and probiotics—as potential nutritional adjuvants in the prevention and treatment of NAFLD.
2. NAFLD in Postmenopausal Women
2.1. Why Does NAFLD Risk Increase after Menopause?
The prevalence of NAFLD increases significantly in women following menopause [30,42,43,44,45,46,47], with postmenopausal women having ~2–3 times higher rates of advanced fibrosis compared to premenopausal women [11,12]. Even in women without obesity, the risk of advanced fibrosis is substantially higher compared to premenopausal women, even after accounting for factors such as disease severity, body mass index (BMI), impaired glucose tolerance or diabetes, and hypertension [48]. Notably, in postmenopausal women, a larger waist circumference is associated with a higher risk of advanced fibrosis, while in men and premenopausal women, extremity, but not abdominal, size, is linked to advanced fibrosis [48]. Central adiposity, weight gain, and metabolic syndrome represent major risk factors for NAFLD in postmenopausal women [30,43]. In addition, the loss of muscle mass, i.e., sarcopenia, can have implications for NAFLD in postmenopausal women [49]. Sarcopenia is associated with metabolic abnormalities, including insulin resistance, dyslipidemia, and obesity, which are all risk factors for the development and progression of NAFLD [50,51].
The natural history of NAFLD in postmenopausal women remains unclear; however, menopause-associated changes in the hormonal milieu contribute to the development and progression of NAFLD. Estrogen is known to have a protective effect on the liver, corresponding to improved liver fat fraction, reduced inflammation and oxidative stress, and increased insulin sensitivity [10,52]. The decline in estrogen levels after menopause has been associated with an increase in visceral adiposity, insulin resistance, and inflammation, all of which are key risk factors for NAFLD [52,53,54]. An observational longitudinal study by Lovejoy et al. [55] demonstrated that while middle-aged women accrue subcutaneous adipose tissue with age, menopause is specifically associated with an increase in total body fat and visceral adipose tissue. Menopause onset was also observed to correspond with decreased energy expenditure and reduced fat oxidation [55]. Additionally, the metabolic changes that occur after menopause, such as an increase in total body fat, a shift towards central adiposity, and a decrease in lean body mass, exacerbate NAFLD risk in this population. Furthermore, postmenopausal women are more likely to have other risk factors for NAFLD, such as hypertension, dyslipidemia, and type 2 diabetes [56,57].
2.2. Strategies for Risk Reduction of NAFLD in Postmenopausal Women
Various strategies seek to reduce the risk of NAFLD in postmenopausal women by targeting underlying metabolic risk factors [58]. As noted, the major strategies to improve liver function and reduce liver fat accumulation, inflammation, and fibrosis are weight loss [4] and exercise [59,60]. However, lifestyle interventions may differ by sex. For instance, a study by Vilar-Gomez et al. [20] found that while weight loss improved NASH histology in both men and women, women had a lower probability of improvement or resolution of NASH compared to men, indicating that women may need to achieve greater weight loss to realize comparable hepatic benefit.
In addition to weight loss, menopause hormone therapy (MHT) may offer unique treatment targets for women with NAFLD due to their distinct hormonal profiles. Estrogen modulation, in particular, has been considered a potential treatment modality for NAFLD in women, supported by data demonstrating the benefits of estrogen on metabolic health and liver fibrosis. A randomized controlled trial (RCT) of MHT in women with type 2 diabetes and presumed NAFLD showed improvement in elevated liver enzymes among MHT users, suggesting potential protective effects of exogenous estrogen on hepatic inflammation [61]. In a large cross-sectional study involving 251 postmenopausal women, it was found that those taking MHT had a lower prevalence of NAFLD (14 out of 53; 26.4%) compared to those who were not taking MHT (79 out of 198; 39.9%) [62]. Additionally, levels of gamma-glutamyl transpeptidase (GGT), alanine transaminase (ALT), ferritin, and insulin resistance were higher in NAFLD patients who were not taking MHT, while women who were not taking MHT, regardless of their NAFLD status, had higher rates of overweight, obesity, and insulin resistance compared to those who used MHT.
A meta-analysis of over 100 randomized trials in postmenopausal women found that the use of estrogen supplementation, with or without progesterone, can increase lean body mass and reduce abdominal fat, improve insulin resistance, and decrease blood pressure [63]. These findings suggest that estrogen supplementation may reduce the metabolically unhealthy characteristics associated with menopause and support the role of estrogen deficiency in the accrual of excess weight in postmenopausal women. The meta-analysis also showed that MHT reduces abdominal obesity, insulin resistance, new-onset diabetes, lipids, blood pressure, adhesion molecules, and procoagulant factors in women without diabetes, also improving insulin resistance and fasting glucose in women with diabetes.
Pharmacological interventions, including insulin sensitizers such as metformin and thiazolidinediones, and lipid-lowering agents such as statins and fibrates, have also been studied for the treatment of NAFLD. These medications have shown promise in improving metabolic parameters and reducing liver fat accumulation, inflammation, and fibrosis. However, their efficacy and safety in treating NAFLD, particularly in postmenopausal women, are still being evaluated. Managing co-morbidities such as hypertension, dyslipidemia, and type 2 diabetes with pharmacological interventions is also important in reducing the risk of NAFLD [58]. Tight control of glycemia, blood pressure, and lipid levels with appropriate therapies can help improve metabolic parameters and decrease the risk of developing NAFLD.
Bariatric surgery is known to improve metabolic parameters and decrease the risk of NAFLD in individuals with severe obesity, which is largely attributed to the substantial weight loss, enhanced insulin sensitivity, and reduced inflammation following surgery [64].
In summary, strategies for reducing the risk of NAFLD in postmenopausal women include lifestyle modifications; use of MHT; pharmacological interventions, including management of co-morbidities; and bariatric surgery in women with obesity. These strategies should be individualized based on the specific metabolic risk factors present in each patient.
3. Nutritional Factors That May Benefit Postmenopausal Women with NAFLD
While there are no specific dietary factors associated with NAFLD that are unique to postmenopausal women, the effects of some of these factors could yield greater impact on hepatic fat accumulation under conditions of estrogen deficiency. Among these dietary factors, the best studied include a high fat diet, particularly one that is high in saturated and trans fats; excessive consumption of sugar and refined carbohydrates; inadequate consumption of fiber; and mild–moderate alcohol consumption, all of which can affect the development and progression of NAFLD [65].
There is also growing evidence that specific nutritional factors may help to prevent or treat NAFLD. For example, supplementation with vitamins C, D, and E may exert beneficial effects on liver health or related metabolic features, primarily through their antioxidant and anti-inflammatory properties [66,67,68,69]. Coffee consumption is inversely associated with a number of liver-related conditions, including slower progression of fibrosis, lower transaminase levels, and decreased liver-related mortality, and some of these positive effects may be due to caffeine [70,71]. Caffeine has also been shown to improve features of metabolic syndrome, including hepatic injury in high carbohydrate, high-fat-diet-fed rats [72]; increase energy expenditure [73]; and reduce total body, trunk, and visceral fat [74] or fat mass [75]. However, these vitamins and dietary factors are not specific for the treatment of NAFLD in postmenopausal women.
Emerging evidence suggests that three dietary factors, namely choline, soy isoflavones, and probiotics, may hold promise in providing potential benefits for specific subsets of postmenopausal women with NAFLD. The importance of these nutritional factors in women with estrogen deficiency and the role they play in improving liver health are discussed in the following sections.
3.1. Choline
Choline is an essential nutrient that plays a critical role in liver function and is a key component of phosphatidylcholine, a major phospholipid found in cell membranes [76]. Dietary choline deficiency, even for a short duration, causes significant liver dysfunction, including hepatic steatosis, in healthy men and women [39,77,78] and laboratory mice [79]. The Adequate Intake (AI) for choline is 550 mg/day for men and 425 mg/day for women [80,81,82]. However, dietary choline requirements vary among individuals, with some requiring much greater amounts of choline to avoid the development of metabolic dysfunction [77]. There is also evidence indicating that many individuals do not regularly meet the AI recommendations for choline [80,81,82].
Phosphatidylethanolamine N-methyltransferase (PEMT) catalyzes the conversion of phosphatidylethanolamine to phosphatidylcholine [83]. Formation of very low-density lipoprotein (VLDL), which conveys triacylglycerols from the liver to the circulation, requires phosphatidylcholine. Low levels of phosphatidylcholine result in insufficient VLDL production, leading to fat accumulation in hepatocytes [83,84,85]. In mice with reduced expression of the PEMT gene (Pemt−/−), hepatic steatosis, inflammation, and fibrosis swiftly developed in response to a high fat/high sucrose diet, and these effects were reversed using dietary choline supplementation [86,87,88,89,90]. We [91] and others [86] observed lower hepatic PEMT expression in NASH patients relative to NAFLD patients.
Common PEMT variants disrupt normal phosphatidylcholine synthesis and have been associated with a heightened predisposition to NAFLD [92,93], which can be further exacerbated by low dietary choline intake [39,94]. The rs7946 variant, which produces a Val-to-Met substitution at residue 175 of the human PEMT protein, has a higher frequency in NAFLD patients compared to those without NAFLD [92,95,96]. The Met isoform of PEMT also exhibits a specific activity that is 40% lower than the wild-type Val isoform [92]. Variant alleles in other common PEMT variants, rs1531100 and rs4646365, were associated with a higher risk of liver damage in postmenopausal women under low choline conditions [94].
The effects of choline deficiency on metabolic function may be worsened in postmenopausal women, in part because PEMT gene expression is regulated by estrogen [97,98]. As estrogen levels decline, the metabolism and utilization of choline shifts. An RCT to investigate the impact of choline depletion found that postmenopausal women were more susceptible than premenopausal women to developing fatty liver or muscle damage in response to the treatment. Specifically, 80% of postmenopausal women (12 out of 15) developed the conditions, whereas only 44% of premenopausal women (7 out of 16) did [77], suggesting that estrogen levels may mediate variation in choline requirements. A study examining the impact of choline intake on fibrosis severity in individuals with NAFLD from the NASH Clinical Research Network found that postmenopausal women with deficient choline intake experienced significantly worse fibrosis, even after controlling for other factors associated with NAFLD, such as age, race/ethnicity, obesity, elevated triglycerides, diabetes, alcohol use, and steroid use [99]. However, choline intake was not found to contribute to disease severity in children, men, or premenopausal women [99]. Conversely, studies have shown that women with a higher dietary choline intake have a lower risk of developing NAFLD. For instance, in one study, women who reported a higher dietary choline intake had a lower risk of abdominal ultrasound-diagnosed NAFLD [80]. This finding was further supported by another study conducted by Mazidi et al. [100], which found that postmenopausal participants from the National Health and Nutrition Examination Survey (NHANES) in the highest quartile of choline intake had a 26% lower risk of NAFLD compared to those in the lowest quartile.
Research suggests that the effects of estrogen deficiency on choline depletion can be reversed. A study conducted by Fischer et al. [39] found that postmenopausal women who were given exogenous estrogen had a significantly lower risk of developing liver dysfunction in response to a very-low-choline diet, compared to those who received a placebo. While the sample size was small (N = 22), the study suggests that hormone therapy during menopause may help prevent the development of hepatic steatosis in postmenopausal women who have a low dietary choline intake or are unable to produce endogenous choline efficiently due to genetic factors.
Additionally, we observed that postmenopausal women with NASH had significantly lower hepatic PEMT expression compared to those with normal liver histology [91]. Our study also found that PEMT expression decreased with increasing stage of fibrosis, indicating that postmenopausal women with low estrogen levels may be at a higher risk of disease progression due to reduced PEMT expression. This risk would likely be exacerbated by low dietary choline intake [39,77,94,99]. Overall, these findings suggest that MHT and increased choline intake may be potential strategies for reducing the risk of NAFLD in postmenopausal women.
3.2. Soy Isoflavones
Soy isoflavones are compounds found in legumes, with a chemical structure, albeit non-steroidal, similar to estrogen. Soybeans and soy products are the richest sources of isoflavones [101], including genistein, daidzein, and glycitein, which are conjugated to different sugars to form glycosides, malonylglucosides, and acetylglucosides [102]. However, the conjugated forms are not biologically active or bioavailable until they are hydrolyzed by intestinal glucosidases to release aglycons [103]. One such aglycon is S-equol, which is a metabolite of daidzein produced by certain intestinal bacteria. Equol has higher antioxidant activity than vitamins C or E; greater biological potency than its precursor, daidzein; and complete bioavailability [104]. Approximately 30% of Western adults and 60% of Asian adults can produce equol after consuming soy foods [105,106]. Individuals who can generate equol may derive the greatest benefit from soy isoflavone consumption [107].
Studies in animals suggest that soy isoflavones can protect against hepatic steatosis and fibrogenesis [108,109], with higher concentrations of soy isoflavones conferring greater protection [110]. Epidemiological studies have found an inverse association between soy food intake and newly diagnosed NAFLD [111]. Dietary intervention trials have further supported the beneficial impact of soy supplementation in NAFLD patients (Table 1) [112,113,114,115,116,117]. Although the human clinical trials conducted to date have varied by study design, treatment protocol, method of liver fat imaging, and outcomes, the results have been largely consistent, indicating a positive effect of soy protein on liver function in NAFLD patients.
Table 1.
Effects of soy product consumption on liver related outcomes in adults with NAFLD.
| Country | N | Intervention | Duration * (wk) | Key Liver Outcomes | Ref. |
|---|---|---|---|---|---|
| Iran | 45 | 30 g soy nut | 8 | Reduced ALT and AST levels | [116] |
| Iran | 70 | 240 mL soy milk | 8 | Reduced ALT, no change in fatty liver grade or AST, GGT, ALP levels | [112] |
| Germany | 22 | Soy meal replacement (83% soy protein isolate) | 24 | Reduced ALT and liver fat, but not different from the lifestyle modification control group | [118] |
* Duration is shown in weeks. Abbreviations: ALP: alkaline phosphatase; ALT: alanine transaminase; AST: aspartate transaminase; GGT: gamma-glutamyltransferase.
Concordant with the consumption of soy isoflavones, the production status of equol may also be an important factor to consider with respect to NAFLD in postmenopausal women. For instance, a study involving 38 NAFLD patients (13 men and 25 women) found that the differences in liver histology by equol production status varied depending on the patient’s sex [108]. Specifically, no differences were observed between male equol producers and nonproducers in terms of histological features. However, in postmenopausal women, the degree of fibrosis and hepatocyte ballooning was significantly higher in equol nonproducers compared to equol producers. Moreover, the percentage of postmenopausal nonproducers with a NAFLD activity score (NAS) ≥ 5 was significantly higher than that of producers, and equol production status was found to be the strongest contributor to the development of NASH in postmenopausal NAFLD patients.
Soy isoflavones may provide unique benefits for women who experience a decline in estrogen levels after menopause due to their estrogen-like effects on metabolism. Studies in postmenopausal women have reported ameliorative effects of soy isoflavones on bone health [119,120,121], menopausal symptoms [120,122,123,124,125], certain types of cancer [120,126,127,128], and obesity [120,129], although not all studies have observed benefits [130,131,132,133,134], and these discrepancies may be due, in part, to differences in the type, dose, or source of isoflavone used. Furthermore, higher levels of adiposity in both peri- and postmenopausal women have been associated with intestinal microflora that cannot metabolize daidzein [135,136]. While it is not yet clear whether the ability to produce equol affects the effectiveness of isoflavones on postmenopausal conditions [104], equol producers have been found to report fewer and less severe menopausal symptoms than non-producers [137]. In contrast, a recent study demonstrated that postmenopausal women consuming a low-fat vegan diet with daily intake of cooked soybeans (86 g) over a period of 12 weeks experienced an 88% reduction in moderate-to-severe hot flashes compared to a control group who did not make any dietary changes, and the degree of improvement in vasomotor symptoms was independent of equol producer status [138].
Currently, there are no studies that have specifically investigated the effects of soy isoflavones on hepatic fat content in postmenopausal women. However, Panneerselvam et al. [139] conducted an animal study using high-fat-diet-fed ovariectomized rats as an experimental model for human menopause. The results showed that when fed a high-fat diet, ovariectomized rats gained weight and developed hepatic steatosis and hypertriglyceridemia. Treatment with soy isoflavone extract improved these conditions. In addition, soy isoflavones reversed the hepatic overexpression of several lipogenic genes that were upregulated by ovariectomy and high-fat diet; and decreased circulating markers of liver injury, including aspartate transaminase, alanine transaminase, lactate dehydrogenase, total protein, and total bilirubin. Although this study was conducted in rats, the results suggest that soy isoflavones may have similarly beneficial effects on liver health and lipid metabolism in postmenopausal women.
The extent of isoflavone intake among postmenopausal women remains poorly characterized. According to the Framingham Heart Study, postmenopausal participants had a median isoflavone intake of 0.15 mg/day (with a range of 0.99–0.24 mg/day), and those in the highest quartile of isoflavone intake had significantly lower plasma triglyceride levels and a lower mean cardiovascular risk factor metabolic score compared to those in the lowest quartile [140]. This is in contrast to Asian countries, where typical soy isoflavone intake ranges from 25–50 mg/day, which is significantly higher than in the United States [141].
While there is some evidence to suggest that soy isoflavones may be beneficial for postmenopausal women, more research is needed to fully understand their effects and potential risks. Furthermore, inconsistent findings in human clinical trials highlight the need for more controlled mechanistic studies in vivo, due to the significant interpersonal variations in the human gut microbiome, which can lead to conflicting outcomes [142]. Soy isoflavone intake may therefore be particularly important for postmenopausal women who are equol producers and do not have gut dysbiosis.
3.3. Probiotics
Gut dysbiosis is a condition characterized by an imbalance in the relative abundance of certain bacterial species or groups, which is often accompanied by lower overall diversity of the gut microbiota [143,144]. This condition has been linked to the development and progression of NAFLD [144,145,146]. The imbalance in the gut microbiota can cause increased intestinal permeability, which enables bacterial products such as lipopolysaccharides (LPSs) to enter the circulation, triggering an immune response and leading to systemic inflammation and liver damage. In animal models, LPSs have been shown to promote the development of NAFLD, and high levels of LPSs have been found in the blood of NAFLD patients [147,148]. Moreover, gut dysbiosis can also affect bile acid metabolism, leading to changes in the composition of bile acids produced and excreted into the small intestine. Alterations in bile acid composition can affect lipid absorption and lead to the accumulation of lipids in the liver, thereby contributing to the development of NAFLD [149]. Additionally, dysbiosis can promote the growth of pro-inflammatory bacteria while reducing the abundance of anti-inflammatory bacteria, resulting in chronic low-grade systemic inflammation that may further contribute to NAFLD development [150].
Menopause has been linked to decreased alpha-diversity and changes in the abundance of different bacterial groups [143,151,152,153,154]. Peters et al. [143] conducted a large shotgun metagenomic sequencing study and discovered that postmenopausal women (N = 1027) had a gut microbiome diversity and overall composition that was similar to that found in men (N = 978) and lower than that in premenopausal women (N = 295). Menopause-related changes in the gut microbiome were also associated with an unfavorable cardiometabolic profile. Despite some heterogeneity, several studies of gut microbial composition in postmenopausal women have revealed a lower abundance of Firmicutes and Ruminococcus and a higher abundance of Butyricimonas, Dorea, Prevotella, Sutterella, and Bacteroides relative to premenopausal women [155]. However, the implications of these findings are not yet clear as the functions and health effects of these bacteria are not fully understood. Therefore, the health consequences of menopause-related gut microbiome alterations remain to be determined [155].
Several RCTs have investigated the impact of probiotic supplementation on liver-related outcomes in individuals with NAFLD. Despite variations in the types of treatments used, the duration of the interventions, and the outcomes measured across these studies, the findings suggest that probiotic supplementation has beneficial effects on liver health (Table 2). A meta-analysis of 21 RCTs, comprising 1252 participants, identified significant decreases in ALT levels and liver stiffness, and improvement in hepatic steatosis in response to probiotic/synbiotic use [156]. An independent meta-analysis of 18 studies demonstrated that the use of probiotics as adjuvant therapy for NAFLD patients improved liver function and reduced levels of liver transaminases, such as ALT, AST, and GGT, particularly when the duration of treatment was greater than 12 weeks [157]. This analysis also indicated positive effects on various cardiometabolic measures, including levels of triglycerides, total cholesterol, fasting blood glucose, insulin, insulin resistance, and BMI associated with probiotic supplementation. Based on this evidence, therapies aimed at targeting the gut microbiome could be a promising approach for the management of NAFLD.
Table 2.
Effects of probiotic supplementation on liver-related outcomes in adults with NAFLD.
| Country | N | Intervention | Duration * | Key Liver Outcomes | Ref. |
|---|---|---|---|---|---|
| Spain | 28 |
Lactobacillus bulgaricus and Streptococcus thermophilus |
12 | Reduced ALT, AST, and GGT levels | [158] |
| Iran | 72 | Probiotic-enriched yogurt | 8 | Reduced ALT and AST levels | [159] |
| Egypt | 30 | Lactobacillus acidophilus | 4 | Reduced ALT and AST levels, no change in AUS findings | [118] |
| Ukraine | 75 | Lactobacilli, Bifidobacteria, and Streptococcus thermophilus | 12 | Decreased ALT levels and liver stiffness | [160] |
| Ukraine | 58 | Multistrain probiotic | 8 | Decreased fatty liver index, reduced AST and GGT levels | [161] |
| Korea | 68 | Multistrain probiotic | 12 | Decreased intrahepatic fat | [162] |
| Iran | 89 | Multistrain probiotic | 12 | Decreased ALT, AST, GGT, and ALP levels | [163] |
| Iran | 53 | Bacillus coagulans plus inulin | 12 | Decreased levels ALT and GGT levels, improved steatosis | [164] |
| Malaysia | 33 | Multistrain probiotic | 24 | No significant changes in steatosis, inflammation, fibrosis, or ALT levels | [165] |
| United Kingdom | 35 | VSL#3 | 10 | No significant changes in transaminases, fibrosis risk score and ASQ | [166] |
* Duration is shown in weeks. Abbreviations: ALP: alkaline phosphatase; ALT: alanine transaminase; ASQ: acoustic structure quantification; AUS: abdominal ultrasound; AST: aspartate transaminase; GGT: gamma-glutamyltransferase.
To date, there have been no studies specifically examining the effects of probiotic supplementation on liver health in postmenopausal women. Nevertheless, a RCT in 81 postmenopausal women with obesity found that a 12-week course of multispecies probiotic supplements led to reduced levels of visceral and subcutaneous fat, lower waist circumference, and improved cardiometabolic markers, including uric acid, glucose, insulin, and HOMA-IR [167], all of which would be expected to yield hepatic benefit. However, 24 weeks of probiotic supplementation in individuals with biopsy-proven NASH (15 female/8 male; mean age 51.7 ± 11.4 years) did not result in any significant changes in liver function (ALT, AST, or GGT) or metabolic health (i.e., fasting glucose, HbA1c, insulin, triglycerides, cholesterol) [168]. Although menopause was not specifically considered in this study, the age range of the female participants is consistent with the average age of menopause in the United States [169]. The discrepancy between studies may be due to the experimental design and differences in both the study sample size and clinical endpoints. In general, the positive results of previous RCTs conducted in male and female participants of various ages [170] suggest that probiotic supplementation may also be a useful adjuvant therapy for postmenopausal NAFLD patients with gut dysbiosis.
Overall, menopause appears to be associated with lower gut microbiome diversity and a shift toward greater similarity to the male gut microbiome. However, further studies for identifying consistent and reproducible changes that occur in the taxa as a result of menopause are warranted, as are studies to better understand the contribution of the gut microbiota to menopause-related NAFLD risk and the impact of menopausal hormone therapy on the gut microbiome-NAFLD axis.
4. Conclusions
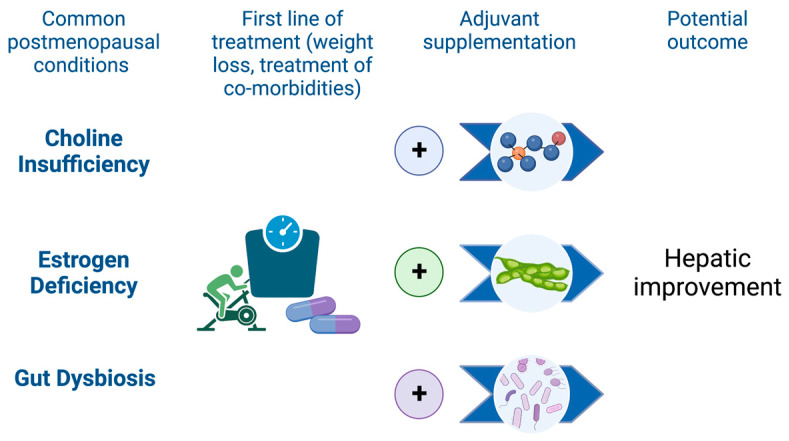
Following menopause, women experience a higher risk of NAFLD, as well as higher rates of advanced hepatic fibrosis and greater mortality [10]. Managing weight, increasing physical activity, and controlling comorbidities are essential strategies to reduce the burden of NAFLD in this population. In addition, specific subsets of postmenopausal women, such as those who experience chronic choline deficiency, estrogen deficiency, or gut dysbiosis, may benefit from targeted nutritional interventions that include consumption or supplementation with choline, soy isoflavones, or probiotics (Figure 2). There is promising evidence supporting the potential benefits of these nutritional factors for NAFLD prevention and treatment, and further research is warranted to confirm their effectiveness in alleviating hepatic steatosis in postmenopausal women. In the meantime, it remains crucial for women to follow a healthy diet that is rich in whole foods, low in processed foods, and balanced in nutrients to reduce the risk of NAFLD following the menopausal transition.
Figure 2.
Adjuvant nutritional strategies may enhance primary NAFLD management in postmenopausal women. Weight loss, lifestyle factors, and clinical management of comorbidities remain the cornerstones of therapy for NAFLD. Nutritional factors may further enhance the effectiveness of first-line therapy in specific subsets of postmenopausal patients. Increased choline intake, either through choline-rich foods or supplements, may help to resolve liver function in postmenopausal women who have a choline-depleted diet, genetic risk factors, or estrogen deficiency. Consumption of soy foods may provide hepatic benefit to postmenopausal women, especially those who can produce equol, through estrogen-like effects. In postmenopausal women with gut dysbiosis, supplementation with probiotics or consumption of fermented foods may correct microbial imbalance, leading to improvements in hepatic function. (Figure created with BioRender.com, accessed on 31 May 2023).
Acknowledgments
The author acknowledges the helpful comments provided by Glenn S. Gerhard and Richard M. Watanabe in the review of this manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The author declares no conflict of interest.
Funding Statement
This research was funded by grants from the National Institutes of Health (R01 DK127015-01A1 and R01 DK120890-01A1).
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Parthasarathy G., Revelo X., Malhi H. Pathogenesis of Nonalcoholic Steatohepatitis: An Overview. Hepatol. Commun. 2020;4:478–492. doi: 10.1002/hep4.1479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Marchesini G., Brizi M., Morselli-Labate A.M., Bianchi G., Bugianesi E., McCullough A.J., Forlani G., Melchionda N. Association of nonalcoholic fatty liver disease with insulin resistance. Am. J. Med. 1999;107:450–455. doi: 10.1016/S0002-9343(99)00271-5. [DOI] [PubMed] [Google Scholar]
- 3.Targher G., Corey K.E., Byrne C.D., Roden M. The complex link between NAFLD and type 2 diabetes mellitus—Mechanisms and treatments. Nat. Rev. Gastroenterol. Hepatol. 2021;18:599–612. doi: 10.1038/s41575-021-00448-y. [DOI] [PubMed] [Google Scholar]
- 4.Fabbrini E., Sullivan S., Klein S. Obesity and nonalcoholic fatty liver disease: Biochemical, metabolic, and clinical implications. Hepatology. 2010;51:679–689. doi: 10.1002/hep.23280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Younossi Z.M., Koenig A.B., Abdelatif D., Fazel Y., Henry L., Wymer M. Global epidemiology of nonalcoholic fatty liver disease-Meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology. 2016;64:73–84. doi: 10.1002/hep.28431. [DOI] [PubMed] [Google Scholar]
- 6.Eslam M., Newsome P.N., Sarin S.K., Anstee Q.M., Targher G., Romero-Gomez M., Zelber-Sagi S., Wai-Sun Wong V., Dufour J.F., Schattenberg J.M., et al. A new definition for metabolic dysfunction-associated fatty liver disease: An international expert consensus statement. J. Hepatol. 2020;73:202–209. doi: 10.1016/j.jhep.2020.03.039. [DOI] [PubMed] [Google Scholar]
- 7.Arrese M., Arab J.P., Barrera F., Kaufmann B., Valenti L., Feldstein A.E. Insights into Nonalcoholic Fatty-Liver Disease Heterogeneity. Semin. Liver Dis. 2021;41:421–434. doi: 10.1055/s-0041-1730927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Younossi Z.M., Loomba R., Rinella M.E., Bugianesi E., Marchesini G., Neuschwander-Tetri B.A., Serfaty L., Negro F., Caldwell S.H., Ratziu V., et al. Current and future therapeutic regimens for nonalcoholic fatty liver disease and nonalcoholic steatohepatitis. Hepatology. 2018;68:361–371. doi: 10.1002/hep.29724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Balakrishnan M., Patel P., Dunn-Valadez S., Dao C., Khan V., Ali H., El-Serag L., Hernaez R., Sisson A., Thrift A.P., et al. Women Have a Lower Risk of Nonalcoholic Fatty Liver Disease but a Higher Risk of Progression vs Men: A Systematic Review and Meta-analysis. Clin. Gastroenterol. Hepatol. 2021;19:61–71.e15. doi: 10.1016/j.cgh.2020.04.067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.DiStefano J.K. NAFLD and NASH in Postmenopausal Women: Implications for Diagnosis and Treatment. Endocrinology. 2020;161:bqaa134. doi: 10.1210/endocr/bqaa134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yang J.D., Abdelmalek M.F., Pang H., Guy C.D., Smith A.D., Diehl A.M., Suzuki A. Gender and menopause impact severity of fibrosis among patients with nonalcoholic steatohepatitis. Hepatology. 2014;59:1406–1414. doi: 10.1002/hep.26761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Suzuki A., Abdelmalek M.F., Unalp-Arida A., Yates K., Sanyal A., Guy C., Diehl A.M. Regional anthropometric measures and hepatic fibrosis in patients with nonalcoholic Fatty liver disease. Clin. Gastroenterol. Hepatol. 2010;8:1062–1069. doi: 10.1016/j.cgh.2010.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Arshad T., Golabi P., Paik J., Mishra A., Younossi Z.M. Prevalence of Nonalcoholic Fatty Liver Disease in the Female Population. Hepatol. Commun. 2019;3:74–83. doi: 10.1002/hep4.1285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Le M.H., Yeo Y.H., Zou B., Barnet S., Henry L., Cheung R., Nguyen M.H. Forecasted 2040 global prevalence of nonalcoholic fatty liver disease using hierarchical bayesian approach. Clin. Mol. Hepatol. 2022;28:841–850. doi: 10.3350/cmh.2022.0239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Paik J.M., Henry L., De Avila L., Younossi E., Racila A., Younossi Z.M. Mortality Related to Nonalcoholic Fatty Liver Disease Is Increasing in the United States. Hepatol. Commun. 2019;3:1459–1471. doi: 10.1002/hep4.1419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Noureddin M., Vipani A., Bresee C., Todo T., Kim I.K., Alkhouri N., Setiawan V.W., Tran T., Ayoub W.S., Lu S.C., et al. NASH Leading Cause of Liver Transplant in Women: Updated Analysis of Indications For Liver Transplant and Ethnic and Gender Variances. Am. J. Gastroenterol. 2018;113:1649–1659. doi: 10.1038/s41395-018-0088-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Younossi Z.M., Golabi P., Paik J.M., Henry A., Van Dongen C., Henry L. The global epidemiology of nonalcoholic fatty liver disease (NAFLD) and nonalcoholic steatohepatitis (NASH): A systematic review. Hepatology. 2023;77:1335–1347. doi: 10.1097/HEP.0000000000000004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rinella M.E., Neuschwander-Tetri B.A., Siddiqui M.S., Abdelmalek M.F., Caldwell S., Barb D., Kleiner D.E., Loomba R. AASLD Practice Guidance on the clinical assessment and management of nonalcoholic fatty liver disease. Hepatology. 2023;77:1797–1835. doi: 10.1097/HEP.0000000000000323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fernandez T., Vinuela M., Vidal C., Barrera F. Lifestyle changes in patients with non-alcoholic fatty liver disease: A systematic review and meta-analysis. PLoS ONE. 2022;17:e0263931. doi: 10.1371/journal.pone.0263931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Vilar-Gomez E., Martinez-Perez Y., Calzadilla-Bertot L., Torres-Gonzalez A., Gra-Oramas B., Gonzalez-Fabian L., Friedman S.L., Diago M., Romero-Gomez M. Weight Loss Through Lifestyle Modification Significantly Reduces Features of Nonalcoholic Steatohepatitis. Gastroenterology. 2015;149:367–378.e365; quiz e314–e365. doi: 10.1053/j.gastro.2015.04.005. [DOI] [PubMed] [Google Scholar]
- 21.Thoma C., Day C.P., Trenell M.I. Lifestyle interventions for the treatment of non-alcoholic fatty liver disease in adults: A systematic review. J. Hepatol. 2012;56:255–266. doi: 10.1016/j.jhep.2011.06.010. [DOI] [PubMed] [Google Scholar]
- 22.Hamurcu Varol P., Kaya E., Alphan E., Yilmaz Y. Role of intensive dietary and lifestyle interventions in the treatment of lean nonalcoholic fatty liver disease patients. Eur. J. Gastroenterol. Hepatol. 2020;32:1352–1357. doi: 10.1097/MEG.0000000000001656. [DOI] [PubMed] [Google Scholar]
- 23.Sinn D.H., Kang D., Cho S.J., Paik S.W., Guallar E., Cho J., Gwak G.Y. Weight change and resolution of fatty liver in normal weight individuals with nonalcoholic fatty liver disease. Eur. J. Gastroenterol. Hepatol. 2021;33:e529–e534. doi: 10.1097/MEG.0000000000002158. [DOI] [PubMed] [Google Scholar]
- 24.Otten J., Mellberg C., Ryberg M., Sandberg S., Kullberg J., Lindahl B., Larsson C., Hauksson J., Olsson T. Strong and persistent effect on liver fat with a Paleolithic diet during a two-year intervention. Int J. Obes. 2016;40:747–753. doi: 10.1038/ijo.2016.4. [DOI] [PubMed] [Google Scholar]
- 25.European Association for the Study of the Liver (EASL) European Association for the Study of Diabetes (EASD) European Association for the Study of Obesity (EASO) EASL-EASD-EASO Clinical Practice Guidelines for the management of non-alcoholic fatty liver disease. J. Hepatol. 2016;64:1388–1402. doi: 10.1016/j.jhep.2015.11.004. [DOI] [PubMed] [Google Scholar]
- 26.Best N., Flannery O. Association between adherence to the Mediterranean Diet and the Eatwell Guide and changes in weight and waist circumference in post-menopausal women in the UK Women’s Cohort Study. Post. Reprod. Health. 2023;29:25–32. doi: 10.1177/20533691231156643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Leone A., De Amicis R., Battezzati A., Bertoli S. Adherence to the Mediterranean Diet and Risk of Metabolically Unhealthy Obesity in Women: A Cross-Sectional Study. Front. Nutr. 2022;9:858206. doi: 10.3389/fnut.2022.858206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Leone A., Bertoli S., Bedogni G., Vignati L., Pellizzari M., Battezzati A. Association between Mediterranean Diet and Fatty Liver in Women with Overweight and Obesity. Nutrients. 2022;14:3771. doi: 10.3390/nu14183771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sarkar M., Cedars M.I. Untangling the Influence of Sex Hormones on Nonalcoholic Fatty Liver Disease in Women. Clin. Gastroenterol. Hepatol. 2022;20:1887–1888. doi: 10.1016/j.cgh.2021.09.006. [DOI] [PubMed] [Google Scholar]
- 30.Hamaguchi M., Kojima T., Ohbora A., Takeda N., Fukui M., Kato T. Aging is a risk factor of nonalcoholic fatty liver disease in premenopausal women. World J. Gastroenterol. 2012;18:237–243. doi: 10.3748/wjg.v18.i3.237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wang Z., Xu M., Hu Z., Shrestha U.K. Prevalence of nonalcoholic fatty liver disease and its metabolic risk factors in women of different ages and body mass index. Menopause. 2015;22:667–673. doi: 10.1097/GME.0000000000000352. [DOI] [PubMed] [Google Scholar]
- 32.Bertolotti M., Lonardo A., Mussi C., Baldelli E., Pellegrini E., Ballestri S., Romagnoli D., Loria P. Nonalcoholic fatty liver disease and aging: Epidemiology to management. World J. Gastroenterol. 2014;20:14185–14204. doi: 10.3748/wjg.v20.i39.14185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cerda C., Perez-Ayuso R.M., Riquelme A., Soza A., Villaseca P., Sir-Petermann T., Espinoza M., Pizarro M., Solis N., Miquel J.F., et al. Nonalcoholic fatty liver disease in women with polycystic ovary syndrome. J. Hepatol. 2007;47:412–417. doi: 10.1016/j.jhep.2007.04.012. [DOI] [PubMed] [Google Scholar]
- 34.Albhaisi S., Sanyal A.J. Gene-Environmental Interactions as Metabolic Drivers of Nonalcoholic Steatohepatitis. Front. Endocrinol. 2021;12:665987. doi: 10.3389/fendo.2021.665987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Rector R.S., Thyfault J.P., Wei Y., Ibdah J.A. Non-alcoholic fatty liver disease and the metabolic syndrome: An update. World J. Gastroenterol. 2008;14:185–192. doi: 10.3748/wjg.14.185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Eslam M., George J. Genetic contributions to NAFLD: Leveraging shared genetics to uncover systems biology. Nat. Rev. Gastroenterol. Hepatol. 2020;17:40–52. doi: 10.1038/s41575-019-0212-0. [DOI] [PubMed] [Google Scholar]
- 37.Carlsson B., Linden D., Brolen G., Liljeblad M., Bjursell M., Romeo S., Loomba R. Review article: The emerging role of genetics in precision medicine for patients with non-alcoholic steatohepatitis. Aliment. Pharmacol. Ther. 2020;51:1305–1320. doi: 10.1111/apt.15738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Vilar-Gomez E., Pirola C.J., Sookoian S., Wilson L.A., Belt P., Liang T., Liu W., Chalasani N. Impact of the Association Between PNPLA3 Genetic Variation and Dietary Intake on the Risk of Significant Fibrosis in Patients With NAFLD. Am. J. Gastroenterol. 2021;116:994–1006. doi: 10.14309/ajg.0000000000001072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Fischer L.M., da Costa K.A., Kwock L., Galanko J., Zeisel S.H. Dietary choline requirements of women: Effects of estrogen and genetic variation. Am. J. Clin. Nutr. 2010;92:1113–1119. doi: 10.3945/ajcn.2010.30064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sokolowska K.E., Maciejewska-Markiewicz D., Binkowski J., Palma J., Taryma-Lesniak O., Kozlowska-Petriczko K., Borowski K., Baskiewicz-Halasa M., Hawrylkowicz V., Zalecka P., et al. Identified in blood diet-related methylation changes stratify liver biopsies of NAFLD patients according to fibrosis grade. Clin. Epigenetics. 2022;14:157. doi: 10.1186/s13148-022-01377-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Albhaisi S.A.M., Bajaj J.S. The Influence of the Microbiome on NAFLD and NASH. Clin. Liver Dis. 2021;17:15–18. doi: 10.1002/cld.1010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Chen Y., Huang Q., Ai P., Liu H., Chen X., Xu X., Ding G., Li Y., Feng X., Wang X., et al. Association between Serum Uric Acid and Non-Alcoholic Fatty Liver Disease according to Different Menstrual Status Groups. Can. J. Gastroenterol. Hepatol. 2019;2019:2763093. doi: 10.1155/2019/2763093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Chung G.E., Yim J.Y., Kim D., Lim S.H., Yang J.I., Kim Y.S., Yang S.Y., Kwak M.S., Kim J.S., Cho S.H. The influence of metabolic factors for nonalcoholic Fatty liver disease in women. Biomed. Res. Int. 2015;2015:131528. doi: 10.1155/2015/131528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Gutierrez-Grobe Y., Ponciano-Rodriguez G., Ramos M.H., Uribe M., Mendez-Sanchez N. Prevalence of non alcoholic fatty liver disease in premenopausal, posmenopausal and polycystic ovary syndrome women. The role of estrogens. Ann. Hepatol. 2010;9:402–409. doi: 10.1016/S1665-2681(19)31616-3. [DOI] [PubMed] [Google Scholar]
- 45.Moon S.S. Relationship between serum uric acid level and nonalcoholic fatty liver disease in pre- and postmenopausal women. Ann. Nutr. Metab. 2013;62:158–163. doi: 10.1159/000346202. [DOI] [PubMed] [Google Scholar]
- 46.Ryu S., Suh B.S., Chang Y., Kwon M.J., Yun K.E., Jung H.S., Kim C.W., Kim B.K., Kim Y.J., Choi Y., et al. Menopausal stages and non-alcoholic fatty liver disease in middle-aged women. Eur. J. Obstet. Gynecol. Reprod. Biol. 2015;190:65–70. doi: 10.1016/j.ejogrb.2015.04.017. [DOI] [PubMed] [Google Scholar]
- 47.Zhou H., Zhang C., Ni J., Han X. Prevalence of cardiovascular risk factors in non-menopausal and postmenopausal inpatients with type 2 diabetes mellitus in China. BMC Endocr. Disord. 2019;19:98. doi: 10.1186/s12902-019-0427-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Yoneda M., Thomas E., Sumida Y., Eguchi Y., Schiff E.R. The influence of menopause on the development of hepatic fibrosis in nonobese women with nonalcoholic fatty liver disease. Hepatology. 2014;60:1792. doi: 10.1002/hep.27097. [DOI] [PubMed] [Google Scholar]
- 49.Maltais M.L., Desroches J., Dionne I.J. Changes in muscle mass and strength after menopause. J. Musculoskelet. Neuronal. Interact. 2009;9:186–197. [PubMed] [Google Scholar]
- 50.Zhai Y., Xiao Q. The Common Mechanisms of Sarcopenia and NAFLD. Biomed. Res. Int. 2017;2017:6297651. doi: 10.1155/2017/6297651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Kim J.A., Choi K.M. Sarcopenia and fatty liver disease. Hepatol. Int. 2019;13:674–687. doi: 10.1007/s12072-019-09996-7. [DOI] [PubMed] [Google Scholar]
- 52.Suzuki A., Abdelmalek M.F. Nonalcoholic fatty liver disease in women. Womens Health. 2009;5:191–203. doi: 10.2217/17455057.5.2.191. [DOI] [PubMed] [Google Scholar]
- 53.Lv Y., Wang F., Sheng Y., Xia F., Jin Y., Ding G., Wang X., Yu J. Estrogen supplementation deteriorates visceral adipose function in aged postmenopausal subjects via Gas5 targeting IGF2BP1. Exp. Gerontol. 2022;163:111796. doi: 10.1016/j.exger.2022.111796. [DOI] [PubMed] [Google Scholar]
- 54.Abildgaard J., Ploug T., Al-Saoudi E., Wagner T., Thomsen C., Ewertsen C., Bzorek M., Pedersen B.K., Pedersen A.T., Lindegaard B. Changes in abdominal subcutaneous adipose tissue phenotype following menopause is associated with increased visceral fat mass. Sci. Rep. 2021;11:14750. doi: 10.1038/s41598-021-94189-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Lovejoy J.C., Champagne C.M., de Jonge L., Xie H., Smith S.R. Increased visceral fat and decreased energy expenditure during the menopausal transition. Int. J. Obes. 2008;32:949–958. doi: 10.1038/ijo.2008.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Cerdas Perez S. Menopause and diabetes. Climacteric. 2023;26:1–6. doi: 10.1080/13697137.2023.2184252. [DOI] [PubMed] [Google Scholar]
- 57.Torosyan N., Visrodia P., Torbati T., Minissian M.B., Shufelt C.L. Dyslipidemia in midlife women: Approach and considerations during the menopausal transition. Maturitas. 2022;166:14–20. doi: 10.1016/j.maturitas.2022.08.001. [DOI] [PubMed] [Google Scholar]
- 58.Yuan L., Kardashian A., Sarkar M. NAFLD in women: Unique pathways, biomarkers and therapeutic opportunities. Curr. Hepatol. Rep. 2019;18:425–432. doi: 10.1007/s11901-019-00495-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Cigrovski Berkovic M., Bilic-Curcic I., Mrzljak A., Cigrovski V. NAFLD and Physical Exercise: Ready, Steady, Go! Front. Nutr. 2021;8:734859. doi: 10.3389/fnut.2021.734859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Molina-Molina E., Furtado G.E., Jones J.G., Portincasa P., Vieira-Pedrosa A., Teixeira A.M., Barros M.P., Bachi A.L.L., Sardao V.A. The advantages of physical exercise as a preventive strategy against NAFLD in postmenopausal women. Eur. J. Clin. Investig. 2022;52:e13731. doi: 10.1111/eci.13731. [DOI] [PubMed] [Google Scholar]
- 61.McKenzie J., Fisher B.M., Jaap A.J., Stanley A., Paterson K., Sattar N. Effects of HRT on liver enzyme levels in women with type 2 diabetes: A randomized placebo-controlled trial. Clin. Endocrinol. 2006;65:40–44. doi: 10.1111/j.1365-2265.2006.02543.x. [DOI] [PubMed] [Google Scholar]
- 62.Florentino G.S., Cotrim H.P., Vilar C.P., Florentino A.V., Guimaraes G.M., Barreto V.S. Nonalcoholic fatty liver disease in menopausal women. Arq. Gastroenterol. 2013;50:180–185. doi: 10.1590/S0004-28032013000200032. [DOI] [PubMed] [Google Scholar]
- 63.Salpeter S.R., Walsh J.M., Ormiston T.M., Greyber E., Buckley N.S., Salpeter E.E. Meta-analysis: Effect of hormone-replacement therapy on components of the metabolic syndrome in postmenopausal women. Diabetes Obes. Metab. 2006;8:538–554. doi: 10.1111/j.1463-1326.2005.00545.x. [DOI] [PubMed] [Google Scholar]
- 64.Fakhry T.K., Mhaskar R., Schwitalla T., Muradova E., Gonzalvo J.P., Murr M.M. Bariatric surgery improves nonalcoholic fatty liver disease: A contemporary systematic review and meta-analysis. Surg. Obes. Relat. Dis. 2019;15:502–511. doi: 10.1016/j.soard.2018.12.002. [DOI] [PubMed] [Google Scholar]
- 65.Riazi K., Raman M., Taylor L., Swain M.G., Shaheen A.A. Dietary Patterns and Components in Nonalcoholic Fatty Liver Disease (NAFLD): What Key Messages Can Health Care Providers Offer? Nutrients. 2019;11:2878. doi: 10.3390/nu11122878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Sindhughosa D.A., Wibawa I.D.N., Mariadi I.K., Somayana G. Additional treatment of vitamin D for improvement of insulin resistance in non-alcoholic fatty liver disease patients: A systematic review and meta-analysis. Sci. Rep. 2022;12:7716. doi: 10.1038/s41598-022-11950-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.He Z., Li X., Yang H., Wu P., Wang S., Cao D., Guo X., Xu Z., Gao J., Zhang W., et al. Effects of Oral Vitamin C Supplementation on Liver Health and Associated Parameters in Patients With Non-Alcoholic Fatty Liver Disease: A Randomized Clinical Trial. Front. Nutr. 2021;8:745609. doi: 10.3389/fnut.2021.745609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Pervez M.A., Khan D.A., Ijaz A., Khan S. Effects of Delta-tocotrienol Supplementation on Liver Enzymes, Inflammation, Oxidative stress and Hepatic Steatosis in Patients with Nonalcoholic Fatty Liver Disease. Turk. J. Gastroenterol. 2018;29:170–176. doi: 10.5152/tjg.2018.17297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Vadarlis A., Antza C., Bakaloudi D.R., Doundoulakis I., Kalopitas G., Samara M., Dardavessis T., Maris T., Chourdakis M. Systematic review with meta-analysis: The effect of vitamin E supplementation in adult patients with non-alcoholic fatty liver disease. J. Gastroenterol. Hepatol. 2021;36:311–319. doi: 10.1111/jgh.15221. [DOI] [PubMed] [Google Scholar]
- 70.Dranoff J.A. Coffee as chemoprotectant in fatty liver disease: Caffeine-dependent and caffeine-independent effects. Am. J. Physiol. Gastrointest. Liver Physiol. 2023;324:G419–G421. doi: 10.1152/ajpgi.00026.2023. [DOI] [PubMed] [Google Scholar]
- 71.Coelho M., Patarrao R.S., Sousa-Lima I., Ribeiro R.T., Meneses M.J., Andrade R., Mendes V.M., Manadas B., Raposo J.F., Macedo M.P., et al. Increased Intake of Both Caffeine and Non-Caffeine Coffee Components Is Associated with Reduced NAFLD Severity in Subjects with Type 2 Diabetes. Nutrients. 2022;15:4. doi: 10.3390/nu15010004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Panchal S.K., Wong W.Y., Kauter K., Ward L.C., Brown L. Caffeine attenuates metabolic syndrome in diet-induced obese rats. Nutrition. 2012;28:1055–1062. doi: 10.1016/j.nut.2012.02.013. [DOI] [PubMed] [Google Scholar]
- 73.Prather J.M., Florez C.M., Vargas A., Soto B., Harrison A., Willoughby D., Tinsley G., Taylor L. The effects of a thermogenic supplement on metabolic and hemodynamic variables and subjective mood states. J. Int. Soc. Sport. Nutr. 2023;20:2185538. doi: 10.1080/15502783.2023.2185538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Henn M., Babio N., Romaguera D., Vazquez-Ruiz Z., Konieczna J., Vioque J., Torres-Collado L., Razquin C., Buil-Cosiales P., Fito M., et al. Increase from low to moderate, but not high, caffeinated coffee consumption is associated with favorable changes in body fat. Clin. Nutr. 2023;42:477–485. doi: 10.1016/j.clnu.2023.02.004. [DOI] [PubMed] [Google Scholar]
- 75.Alperet D.J., Rebello S.A., Khoo E.Y., Tay Z., Seah S.S., Tai B.C., Tai E.S., Emady-Azar S., Chou C.J., Darimont C., et al. The effect of coffee consumption on insulin sensitivity and oTher. biological risk factors for type 2 diabetes: A randomized placebo-controlled trial. Am. J. Clin. Nutr. 2020;111:448–458. doi: 10.1093/ajcn/nqz306. [DOI] [PubMed] [Google Scholar]
- 76.Zeisel S.H., Da Costa K.A., Franklin P.D., Alexander E.A., Lamont J.T., Sheard N.F., Beiser A. Choline, an essential nutrient for humans. FASEB J. 1991;5:2093–2098. doi: 10.1096/fasebj.5.7.2010061. [DOI] [PubMed] [Google Scholar]
- 77.Fischer L.M., daCosta K.A., Kwock L., Stewart P.W., Lu T.S., Stabler S.P., Allen R.H., Zeisel S.H. Sex and menopausal status influence human dietary requirements for the nutrient choline. Am. J. Clin. Nutr. 2007;85:1275–1285. doi: 10.1093/ajcn/85.5.1275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Kohlmeier M., da Costa K.A., Fischer L.M., Zeisel S.H. Genetic variation of folate-mediated one-carbon transfer pathway predicts susceptibility to choline deficiency in humans. Proc. Natl. Acad. Sci. USA. 2005;102:16025–16030. doi: 10.1073/pnas.0504285102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Matsumoto M., Hada N., Sakamaki Y., Uno A., Shiga T., Tanaka C., Ito T., Katsume A., Sudoh M. An improved mouse model that rapidly develops fibrosis in non-alcoholic steatohepatitis. Int. J. Exp. Pathol. 2013;94:93–103. doi: 10.1111/iep.12008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Yu D., Shu X.O., Xiang Y.B., Li H., Yang G., Gao Y.T., Zheng W., Zhang X. Higher dietary choline intake is associated with lower risk of nonalcoholic fatty liver in normal-weight Chinese women. J. Nutr. 2014;144:2034–2040. doi: 10.3945/jn.114.197533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Wallace T.C., Blusztajn J.K., Caudill M.A., Klatt K.C., Natker E., Zeisel S.H., Zelman K.M. Choline: The UnderconsuMed. and Underappreciated Essential Nutrient. Nutr. Today. 2018;53:240–253. doi: 10.1097/NT.0000000000000302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Kim S., Fenech M.F., Kim P.J. Nutritionally recommended food for semi- to strict vegetarian diets based on large-scale nutrient composition data. Sci. Rep. 2018;8:4344. doi: 10.1038/s41598-018-22691-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Noga A.A., Zhao Y., Vance D.E. An unexpected requirement for phosphatidylethanolamine N-methyltransferase in the secretion of very low density lipoproteins. J. Biol. Chem. 2002;277:42358–42365. doi: 10.1074/jbc.M204542200. [DOI] [PubMed] [Google Scholar]
- 84.Yao Z.M., Vance D.E. The active synthesis of phosphatidylcholine is required for very low density lipoprotein secretion from rat hepatocytes. J. Biol. Chem. 1988;263:2998–3004. doi: 10.1016/S0021-9258(18)69166-5. [DOI] [PubMed] [Google Scholar]
- 85.Yao Z.M., Vance D.E. Reduction in VLDL, but not HDL, in plasma of rats deficient in choline. Biochem. Cell Biol. 1990;68:552–558. doi: 10.1139/o90-079. [DOI] [PubMed] [Google Scholar]
- 86.Nakatsuka A., Matsuyama M., Yamaguchi S., Katayama A., Eguchi J., Murakami K., Teshigawara S., Ogawa D., Wada N., Yasunaka T., et al. Insufficiency of phosphatidylethanolamine N-methyltransferase is risk for lean non-alcoholic steatohepatitis. Sci. Rep. 2016;6:21721. doi: 10.1038/srep21721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Zhu X., Song J., Mar M.H., Edwards L.J., Zeisel S.H. Phosphatidylethanolamine N-methyltransferase (PEMT) knockout mice have hepatic steatosis and abnormal hepatic choline metabolite concentrations despite ingesting a recommended dietary intake of choline. Biochem. J. 2003;370:987–993. doi: 10.1042/bj20021523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Waite K.A., Cabilio N.R., Vance D.E. Choline deficiency-induced liver damage is reversible in Pemt(-/-) mice. J. Nutr. 2002;132:68–71. doi: 10.1093/jn/132.1.68. [DOI] [PubMed] [Google Scholar]
- 89.Vance D.E. Physiological roles of phosphatidylethanolamine N-methyltransferase. Biochim. Biophys. Acta. 2013;1831:626–632. doi: 10.1016/j.bbalip.2012.07.017. [DOI] [PubMed] [Google Scholar]
- 90.Jacobs R.L., Zhao Y., Koonen D.P., Sletten T., Su B., Lingrell S., Cao G., Peake D.A., Kuo M.S., Proctor S.D., et al. Impaired de novo choline synthesis explains why phosphatidylethanolamine N-methyltransferase-deficient mice are protected from diet-induced obesity. J. Biol. Chem. 2010;285:22403–22413. doi: 10.1074/jbc.M110.108514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Piras I.S., Raju A., Don J., Schork N.J., Gerhard G.S., DiStefano J.K. Hepatic PEMT Expression Decreases with Increasing NAFLD Severity. Int. J. Mol. Sci. 2022;23:9296. doi: 10.3390/ijms23169296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Song J., da Costa K.A., Fischer L.M., Kohlmeier M., Kwock L., Wang S., Zeisel S.H. Polymorphism of the PEMT gene and susceptibility to nonalcoholic fatty liver disease (NAFLD) FASEB J. 2005;19:1266–1271. doi: 10.1096/fj.04-3580com. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Bale G., Vishnubhotla R.V., Mitnala S., Sharma M., Padaki R.N., Pawar S.C., Duvvur R.N. Whole-Exome Sequencing Identifies a Variant in Phosphatidylethanolamine N-Methyltransferase Gene to be Associated With Lean-Nonalcoholic Fatty Liver Disease. J. Clin. Exp. Hepatol. 2019;9:561–568. doi: 10.1016/j.jceh.2019.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.da Costa K.A., Corbin K.D., Niculescu M.D., Galanko J.A., Zeisel S.H. Identification of new genetic polymorphisms that alter the dietary requirement for choline and vary in their distribution across ethnic and racial groups. FASEB J. 2014;28:2970–2978. doi: 10.1096/fj.14-249557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Dong H., Wang J., Li C., Hirose A., Nozaki Y., Takahashi M., Ono M., Akisawa N., Iwasaki S., Saibara T., et al. The phosphatidylethanolamine N-methyltransferase gene V175M single nucleotide polymorphism confers the susceptibility to NASH in Japanese population. J. Hepatol. 2007;46:915–920. doi: 10.1016/j.jhep.2006.12.012. [DOI] [PubMed] [Google Scholar]
- 96.Zeisel S.H. People with fatty liver are more likely to have the PEMT rs7946 SNP, yet populations with the mutant allele do not have fatty liver. FASEB J. 2006;20:2181–2182. doi: 10.1096/fj.06-1005ufm. [DOI] [Google Scholar]
- 97.Resseguie M.E., da Costa K.A., Galanko J.A., Patel M., Davis I.J., Zeisel S.H. Aberrant estrogen regulation of PEMT results in choline deficiency-associated liver dysfunction. J. Biol. Chem. 2011;286:1649–1658. doi: 10.1074/jbc.M110.106922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Resseguie M., Song J., Niculescu M.D., da Costa K.A., Randall T.A., Zeisel S.H. Phosphatidylethanolamine N-methyltransferase (PEMT) gene expression is induced by estrogen in human and mouse primary hepatocytes. FASEB J. 2007;21:2622–2632. doi: 10.1096/fj.07-8227com. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Guerrerio A.L., Colvin R.M., Schwartz A.K., Molleston J.P., Murray K.F., Diehl A., Mohan P., Schwimmer J.B., Lavine J.E., Torbenson M.S., et al. Choline intake in a large cohort of patients with nonalcoholic fatty liver disease. Am. J. Clin. Nutr. 2012;95:892–900. doi: 10.3945/ajcn.111.020156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Mazidi M., Katsiki N., Mikhailidis D.P., Banach M. Adiposity May Moderate the Link Between Choline Intake and Non-alcoholic Fatty Liver Disease. J. Am. Coll Nutr. 2019;38:633–639. doi: 10.1080/07315724.2018.1507011. [DOI] [PubMed] [Google Scholar]
- 101.Setchell K.D., Cole S.J. Variations in isoflavone levels in soy foods and soy protein isolates and issues related to isoflavone databases and food labeling. J. Agric. Food Chem. 2003;51:4146–4155. doi: 10.1021/jf026199b. [DOI] [PubMed] [Google Scholar]
- 102.Xiao C.W., Hendry A. Hypolipidemic Effects of Soy Protein and Isoflavones in the Prevention of Non-Alcoholic Fatty Liver Disease- A Review. Plant Foods Hum. Nutr. 2022;77:319–328. doi: 10.1007/s11130-022-00984-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Setchell K.D., Brown N.M., Zimmer-Nechemias L., Brashear W.T., Wolfe B.E., Kirschner A.S., Heubi J.E. Evidence for lack of absorption of soy isoflavone glycosides in humans, supporting the crucial role of intestinal metabolism for bioavailability. Am. J. Clin. Nutr. 2002;76:447–453. doi: 10.1093/ajcn/76.2.447. [DOI] [PubMed] [Google Scholar]
- 104.Setchell K.D., Clerici C. Equol: History, chemistry, and formation. J. Nutr. 2010;140:1355S–1362S. doi: 10.3945/jn.109.119776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Setchell K.D.R. The history and basic science development of soy isoflavones. Menopause. 2017;24:1338–1350. doi: 10.1097/GME.0000000000001018. [DOI] [PubMed] [Google Scholar]
- 106.Arai Y., Uehara M., Sato Y., Kimira M., Eboshida A., Adlercreutz H., Watanabe S. Comparison of isoflavones among dietary intake, plasma concentration and urinary excretion for accurate estimation of phytoestrogen intake. J. Epidemiol. 2000;10:127–135. doi: 10.2188/jea.10.127. [DOI] [PubMed] [Google Scholar]
- 107.Mayo B., Vazquez L., Florez A.B. Equol: A Bacterial Metabolite from The Daidzein Isoflavone and Its PresuMed. Beneficial Health Effects. Nutrients. 2019;11:2231. doi: 10.3390/nu11092231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Akahane T., Kaya D., Noguchi R., Kaji K., Miyakawa H., Fujinaga Y., Tsuji Y., Takaya H., Sawada Y., Furukawa M., et al. Association between Equol Production Status and Nonalcoholic Steatohepatitis. Int. J. Mol. Sci. 2021;22:11904. doi: 10.3390/ijms222111904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Xin X., Chen C., Hu Y.Y., Feng Q. Protective effect of genistein on nonalcoholic fatty liver disease (NAFLD) Biomed. EPharmacother. 2019;117:109047. doi: 10.1016/j.biopha.2019.109047. [DOI] [PubMed] [Google Scholar]
- 110.Hakkak R., Spray B., Borsheim E., Korourian S. Diet Containing Soy Protein Concentrate With Low and High Isoflavones for 9 Weeks Protects Against Non-alcoholic Fatty Liver Steatosis Using Obese Zucker Rats. Front. Nutr. 2022;9:913571. doi: 10.3389/fnut.2022.913571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Zhang S., Kumari S., Gu Y., Wu X., Li X., Meng G., Zhang Q., Liu L., Wu H., Wang Y., et al. Soy Food Intake Is Inversely Associated with Newly Diagnosed Nonalcoholic Fatty Liver Disease in the TCLSIH Cohort Study. J. Nutr. 2020;150:3280–3287. doi: 10.1093/jn/nxaa297. [DOI] [PubMed] [Google Scholar]
- 112.Eslami O., Shidfar F., Maleki Z., Jazayeri S., Hosseini A.F., Agah S., Ardiyani F. Effect of Soy Milk on Metabolic Status of Patients with Nonalcoholic Fatty Liver Disease: A Randomized Clinical Trial. J. Am. Coll. Nutr. 2019;38:51–58. doi: 10.1080/07315724.2018.1479990. [DOI] [PubMed] [Google Scholar]
- 113.Deibert P., Lazaro A., Schaffner D., Berg A., Koenig D., Kreisel W., Baumstark M.W., Steinmann D., Buechert M., Lange T. Comprehensive lifestyle intervention vs soy protein-based meal regimen in non-alcoholic steatohepatitis. World J. Gastroenterol. 2019;25:1116–1131. doi: 10.3748/wjg.v25.i9.1116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Maleki Z., Jazayeri S., Eslami O., Shidfar F., Hosseini A.F., Agah S., Norouzi H. Effect of soy milk consumption on glycemic status, blood pressure, fibrinogen and malondialdehyde in patients with non-alcoholic fatty liver disease: A randomized controlled trial. Complement Ther. Med. 2019;44:44–50. doi: 10.1016/j.ctim.2019.02.020. [DOI] [PubMed] [Google Scholar]
- 115.Kani A.H., Alavian S.M., Esmaillzadeh A., Adibi P., Haghighatdoost F., Azadbakht L. Effects of a Low-Calorie, Low-Carbohydrate Soy Containing Diet on Systemic Inflammation Among Patients with Nonalcoholic Fatty Liver Disease: A Parallel Randomized Clinical Trial. Horm. Metab. Res. 2017;49:687–692. doi: 10.1055/s-0042-118707. [DOI] [PubMed] [Google Scholar]
- 116.Kani A.H., Alavian S.M., Esmaillzadeh A., Adibi P., Azadbakht L. Effects of a novel therapeutic diet on liver enzymes and coagulating factors in patients with non-alcoholic fatty liver disease: A parallel randomized trial. Nutrition. 2014;30:814–821. doi: 10.1016/j.nut.2013.11.008. [DOI] [PubMed] [Google Scholar]
- 117.Setchell K.D., Brown N.M., Lydeking-Olsen E. The clinical importance of the metabolite equol-a clue to the effectiveness of soy and its isoflavones. J. Nutr. 2002;132:3577–3584. doi: 10.1093/jn/132.12.3577. [DOI] [PubMed] [Google Scholar]
- 118.Abdel Monem S.M. Probiotic Therapy in Patients with Nonalcoholic Steatohepatitis in Zagazig University Hospitals. Euroasian J. Hepatogastroenterol. 2017;7:101–106. doi: 10.5005/jp-journals-10018-1226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Baranska A., Kanadys W., Bogdan M., Stepien E., Barczynski B., Klak A., Augustynowicz A., Szajnik M., Religioni U. The Role of Soy Isoflavones in the Prevention of Bone Loss in Postmenopausal Women: A Systematic Review with Meta-Analysis of Randomized Controlled Trials. J. Clin. Med. 2022;11:4676. doi: 10.3390/jcm11164676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Chen L.R., Chen K.H. Utilization of Isoflavones in Soybeans for Women with Menopausal Syndrome: An Overview. Int. J. Mol. Sci. 2021;22:3212. doi: 10.3390/ijms22063212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Kanadys W., Baranska A., Blaszczuk A., Polz-Dacewicz M., Drop B., Malm M., Kanecki K. Effects of Soy Isoflavones on Biochemical Markers of Bone Metabolism in Postmenopausal Women: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Int. J. Environ. Res. Public Health. 2021;18:5346. doi: 10.3390/ijerph18105346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Khapre S., Deshmukh U., Jain S. The Impact of Soy Isoflavone Supplementation on the Menopausal Symptoms in Perimenopausal and Postmenopausal Women. J. Midlife Health. 2022;13:175–184. doi: 10.4103/jmh.jmh_190_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Kim H.I., Kim M.K., Lee I., Yun J., Kim E.H., Seo S.K. Efficacy and Safety of a Standardized Soy and Hop Extract on Menopausal Symptoms: A 12-Week, Multicenter, Randomized, Double-Blind, Placebo-Controlled Clinical Trial. J. Altern Complement Med. 2021;27:959–967. doi: 10.1089/acm.2021.0027. [DOI] [PubMed] [Google Scholar]
- 124.Thangavel P., Puga-Olguin A., Rodriguez-Landa J.F., Zepeda R.C. Genistein as Potential Therapeutic Candidate for Menopausal Symptoms and OTher. Related Diseases. Molecules. 2019;24:3892. doi: 10.3390/molecules24213892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Taku K., Melby M.K., Kronenberg F., Kurzer M.S., Messina M. Extracted or synthesized soybean isoflavones reduce menopausal hot flash frequency and severity: Systematic review and meta-analysis of randomized controlled trials. Menopause. 2012;19:776–790. doi: 10.1097/gme.0b013e3182410159. [DOI] [PubMed] [Google Scholar]
- 126.Boutas I., Kontogeorgi A., Dimitrakakis C., Kalantaridou S.N. Soy Isoflavones and Breast Cancer Risk: A Meta-analysis. In Vivo. 2022;36:556–562. doi: 10.21873/invivo.12737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Liu J., Yuan F., Gao J., Shan B., Ren Y., Wang H., Gao Y. Oral isoflavone supplementation on endometrial thickness: A meta-analysis of randomized placebo-controlled trials. Oncotarget. 2016;7:17369–17379. doi: 10.18632/oncotarget.7959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Ollberding N.J., Lim U., Wilkens L.R., Setiawan V.W., Shvetsov Y.B., Henderson B.E., Kolonel L.N., Goodman M.T. Legume, soy, tofu, and isoflavone intake and endometrial cancer risk in postmenopausal women in the multiethnic cohort study. J. Natl. Cancer Inst. 2012;104:67–76. doi: 10.1093/jnci/djr475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Llaha F., Zamora-Ros R. The Effects of Polyphenol Supplementation in Addition to Calorie Restricted Diets and/or Physical Activity on Body Composition Parameters: A Systematic Review of Randomized Trials. Front. Nutr. 2020;7:84. doi: 10.3389/fnut.2020.00084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Finkeldey L., Schmitz E., Ellinger S. Effect of the Intake of Isoflavones on Risk Factors of Breast Cancer-A Systematic Review of Randomized Controlled Intervention Studies. Nutrients. 2021;13:2309. doi: 10.3390/nu13072309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Lacourt-Ventura M.Y., Vilanova-Cuevas B., Rivera-Rodriguez D., Rosario-Acevedo R., Miranda C., Maldonado-Martinez G., Maysonet J., Vargas D., Ruiz Y., Hunter-Mellado R., et al. Soy and Frequent Dairy Consumption with Subsequent Equol Production Reveals Decreased Gut Health in a Cohort of Healthy Puerto Rican Women. Int. J. Environ. Res. Public Health. 2021;18:8254. doi: 10.3390/ijerph18168254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Khankari N.K., Yang J.J., Sawada N., Wen W., Yamaji T., Gao J., Goto A., Li H.L., Iwasaki M., Yang G., et al. Soy Intake and Colorectal Cancer Risk: Results from a Pooled Analysis of Prospective Cohort Studies Conducted in China and Japan. J. Nutr. 2020;150:2442–2450. doi: 10.1093/jn/nxaa194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Lei Y.Y., Ho S.C., Cheng A., Kwok C., Cheung K.L., He Y.Q., Lee R., Yeo W. The association between soy isoflavone intake and menopausal symptoms after breast cancer diagnosis: A prospective longitudinal cohort study on Chinese breast cancer patients. Breast Cancer Res. Treat. 2020;181:167–180. doi: 10.1007/s10549-020-05616-3. [DOI] [PubMed] [Google Scholar]
- 134.Quaas A.M., Kono N., Mack W.J., Hodis H.N., Felix J.C., Paulson R.J., Shoupe D. Effect of isoflavone soy protein supplementation on endometrial thickness, hyperplasia, and endometrial cancer risk in postmenopausal women: A randomized controlled trial. Menopause. 2013;20:840–844. doi: 10.1097/GME.0b013e3182804353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Miller L.M., Lampe J.W., Newton K.M., Gundersen G., Fuller S., Reed S.D., Frankenfeld C.L. Being overweight or obese is associated with harboring a gut microbial community not capable of metabolizing the soy isoflavone daidzein to O-desmethylangolensin in peri- and post-menopausal women. Maturitas. 2017;99:37–42. doi: 10.1016/j.maturitas.2017.02.006. [DOI] [PubMed] [Google Scholar]
- 136.Frankenfeld C.L., Atkinson C., Wahala K., Lampe J.W. Obesity prevalence in relation to gut microbial environments capable of producing equol or O-desmethylangolensin from the isoflavone daidzein. Eur. J. Clin. Nutr. 2014;68:526–530. doi: 10.1038/ejcn.2014.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Newton K.M., Reed S.D., Uchiyama S., Qu C., Ueno T., Iwashita S., Gunderson G., Fuller S., Lampe J.W. A cross-sectional study of equol producer status and self-reported vasomotor symptoms. Menopause. 2015;22:489–495. doi: 10.1097/GME.0000000000000363. [DOI] [PubMed] [Google Scholar]
- 138.Barnard N.D., Kahleova H., Holtz D.N., Znayenko-Miller T., Sutton M., Holubkov R., Zhao X., Galandi S., Setchell K.D.R. A dietary intervention for vasomotor symptoms of menopause: A randomized, controlled trial. Menopause. 2023;30:80–87. doi: 10.1097/GME.0000000000002080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Panneerselvam S., Packirisamy R.M., Bobby Z., Elizabeth Jacob S., Sridhar M.G. Soy isoflavones (Glycine max) ameliorate hypertriglyceridemia and hepatic steatosis in high fat-fed ovariectomized Wistar rats (an experimental model of postmenopausal obesity) J. Nutr. Biochem. 2016;38:57–69. doi: 10.1016/j.jnutbio.2016.08.007. [DOI] [PubMed] [Google Scholar]
- 140.de Kleijn M.J., van der Schouw Y.T., Wilson P.W., Adlercreutz H., Mazur W., Grobbee D.E., Jacques P.F. Intake of dietary phytoestrogens is low in postmenopausal women in the United States: The FraminghAm. study(1-4) J. Nutr. 2001;131:1826–1832. doi: 10.1093/jn/131.6.1826. [DOI] [PubMed] [Google Scholar]
- 141.Messina M. Soy and Health Update: Evaluation of the Clinical and Epidemiologic Literature. Nutrients. 2016;8:754. doi: 10.3390/nu8120754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Leonard L.M., Choi M.S., Cross T.L. Maximizing the Estrogenic Potential of Soy Isoflavones through the Gut Microbiome: Implication for Cardiometabolic Health in Postmenopausal Women. Nutrients. 2022;14:553. doi: 10.3390/nu14030553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Peters B.A., Lin J., Qi Q., Usyk M., Isasi C.R., Mossavar-Rahmani Y., Derby C.A., Santoro N., Perreira K.M., Daviglus M.L., et al. Menopause Is Associated with an Altered Gut Microbiome and Estrobolome, with Implications for Adverse Cardiometabolic Risk in the Hispanic Community Health Study/Study of Latinos. mSystems. 2022;7:e0027322. doi: 10.1128/msystems.00273-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Schwimmer J.B., Johnson J.S., Angeles J.E., Behling C., Belt P.H., Borecki I., Bross C., Durelle J., Goyal N.P., Hamilton G., et al. Microbiome SignatuRes. Associated With Steatohepatitis and Moderate to Severe Fibrosis in Children With Nonalcoholic Fatty Liver Disease. Gastroenterology. 2019;157:1109–1122. doi: 10.1053/j.gastro.2019.06.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Boursier J., Mueller O., Barret M., Machado M., Fizanne L., Araujo-Perez F., Guy C.D., Seed P.C., Rawls J.F., David L.A., et al. The severity of nonalcoholic fatty liver disease is associated with gut dysbiosis and shift in the metabolic function of the gut microbiota. Hepatology. 2016;63:764–775. doi: 10.1002/hep.28356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Tsai M.C., Liu Y.Y., Lin C.C., Wang C.C., Wu Y.J., Yong C.C., Chen K.D., Chuah S.K., Yao C.C., Huang P.Y., et al. Gut Microbiota Dysbiosis in Patients with Biopsy-Proven Nonalcoholic Fatty Liver Disease: A Cross-Sectional Study in Taiwan. Nutrients. 2020;12:820. doi: 10.3390/nu12030820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Le Roy T., Llopis M., Lepage P., Bruneau A., Rabot S., Bevilacqua C., Martin P., Philippe C., Walker F., Bado A., et al. Intestinal microbiota determines development of non-alcoholic fatty liver disease in mice. Gut. 2013;62:1787–1794. doi: 10.1136/gutjnl-2012-303816. [DOI] [PubMed] [Google Scholar]
- 148.Jiang W., Wu N., Wang X., Chi Y., Zhang Y., Qiu X., Hu Y., Li J., Liu Y. Dysbiosis gut microbiota associated with inflammation and impaired mucosal immune function in intestine of humans with non-alcoholic fatty liver disease. Sci. Rep. 2015;5:8096. doi: 10.1038/srep08096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Mouzaki M., Wang A.Y., Bandsma R., Comelli E.M., Arendt B.M., Zhang L., Fung S., Fischer S.E., McGilvray I.G., Allard J.P. Bile Acids and Dysbiosis in Non-Alcoholic Fatty Liver Disease. PLoS ONE. 2016;11:e0151829. doi: 10.1371/journal.pone.0151829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Tilg H., Moschen A.R. Microbiota and diabetes: An evolving relationship. Gut. 2014;63:1513–1521. doi: 10.1136/gutjnl-2014-306928. [DOI] [PubMed] [Google Scholar]
- 151.Flores R., Shi J., Fuhrman B., Xu X., Veenstra T.D., Gail M.H., Gajer P., Ravel J., Goedert J.J. Fecal microbial determinants of fecal and systemic estrogens and estrogen metabolites: A cross-sectional study. J. Transl. Med. 2012;10:253. doi: 10.1186/1479-5876-10-253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Zhao H., Chen J., Li X., Sun Q., Qin P., Wang Q. Compositional and functional featuRes. of the female premenopausal and postmenopausal gut microbiota. FEBS Lett. 2019;593:2655–2664. doi: 10.1002/1873-3468.13527. [DOI] [PubMed] [Google Scholar]
- 153.Santos-Marcos J.A., Rangel-Zuniga O.A., Jimenez-Lucena R., Quintana-Navarro G.M., Garcia-Carpintero S., Malagon M.M., Landa B.B., Tena-Sempere M., Perez-Martinez P., Lopez-Miranda J., et al. Influence of gender and menopausal status on gut microbiota. Maturitas. 2018;116:43–53. doi: 10.1016/j.maturitas.2018.07.008. [DOI] [PubMed] [Google Scholar]
- 154.Mayneris-Perxachs J., Arnoriaga-Rodriguez M., Luque-Cordoba D., Priego-Capote F., Perez-Brocal V., Moya A., Burokas A., Maldonado R., Fernandez-Real J.M. Gut microbiota steroid sexual dimorphism and its impact on gonadal steroids: Influences of obesity and menopausal status. Microbiome. 2020;8:136. doi: 10.1186/s40168-020-00913-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Peters B.A., Santoro N., Kaplan R.C., Qi Q. Spotlight on the Gut Microbiome in Menopause: Current Insights. Int. J. Womens Health. 2022;14:1059–1072. doi: 10.2147/IJWH.S340491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Sharpton S.R., Maraj B., Harding-Theobald E., Vittinghoff E., Terrault N.A. Gut microbiome-targeted therapies in nonalcoholic fatty liver disease: A systematic review, meta-analysis, and meta-regression. Am. J. Clin. Nutr. 2019;110:139–149. doi: 10.1093/ajcn/nqz042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Wang Y., Wang Y., Sun J. The clinical effect of probiotics on patients with non-alcoholic fatty liver disease: A meta-analysis. Bioengineered. 2022;13:14960–14973. doi: 10.1080/21655979.2023.2185941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Aller R., De Luis D.A., Izaola O., Conde R., Gonzalez Sagrado M., Primo D., De La Fuente B., Gonzalez J. Effect of a probiotic on liver aminotransferases in nonalcoholic fatty liver disease patients: A double blind randomized clinical trial. Eur. Rev. Med. Pharmacol. Sci. 2011;15:1090–1095. [PubMed] [Google Scholar]
- 159.Nabavi S., Rafraf M., Somi M.H., Homayouni-Rad A., Asghari-Jafarabadi M. Effects of probiotic yogurt consumption on metabolic factors in individuals with nonalcoholic fatty liver disease. J. Dairy Sci. 2014;97:7386–7393. doi: 10.3168/jds.2014-8500. [DOI] [PubMed] [Google Scholar]
- 160.Manzhalii E., Virchenko O., Falalyeyeva T., Beregova T., Stremmel W. Treatment efficacy of a probiotic preparation for non-alcoholic steatohepatitis: A pilot trial. J. Dig. Dis. 2017;18:698–703. doi: 10.1111/1751-2980.12561. [DOI] [PubMed] [Google Scholar]
- 161.Kobyliak N., Abenavoli L., Mykhalchyshyn G., Kononenko L., Boccuto L., Kyriienko D., Dynnyk O. A Multi-strain Probiotic Reduces the Fatty Liver Index, Cytokines and Aminotransferase levels in NAFLD Patients: Evidence from a Randomized Clinical Trial. J. Gastrointestin. Liver Dis. 2018;27:41–49. doi: 10.15403/jgld.2014.1121.271.kby. [DOI] [PubMed] [Google Scholar]
- 162.Ahn S.B., Jun D.W., Kang B.K., Lim J.H., Lim S., Chung M.J. Randomized, Double-blind, Placebo-controlled Study of a Multispecies Probiotic Mixture in Nonalcoholic Fatty Liver Disease. Sci. Rep. 2019;9:5688. doi: 10.1038/s41598-019-42059-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Behrouz V., Aryaeian N., Zahedi M.J., Jazayeri S. Effects of probiotic and prebiotic supplementation on metabolic parameters, liver aminotransferases, and systemic inflammation in nonalcoholic fatty liver disease: A randomized clinical trial. J. Food Sci. 2020;85:3611–3617. doi: 10.1111/1750-3841.15367. [DOI] [PubMed] [Google Scholar]
- 164.Abhari K., Saadati S., Yari Z., Hosseini H., Hedayati M., Abhari S., Alavian S.M., Hekmatdoost A. The effects of Bacillus coagulans supplementation in patients with non-alcoholic fatty liver disease: A randomized, placebo-controlled, clinical trial. Clin. Nutr. ESPEN. 2020;39:53–60. doi: 10.1016/j.clnesp.2020.06.020. [DOI] [PubMed] [Google Scholar]
- 165.Mohamad Nor M.H., Ayob N., Mokhtar N.M., Raja Ali R.A., Tan G.C., Wong Z., Shafiee N.H., Wong Y.P., Mustangin M., Nawawi K.N.M. The Effect of Probiotics (MCP((R)) BCMC((R)) Strains) on Hepatic Steatosis, Small Intestinal Mucosal Immune Function, and Intestinal Barrier in Patients with Non-Alcoholic Fatty Liver Disease. Nutrients. 2021;13:3192. doi: 10.3390/nu13093192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Chong P.L., Laight D., Aspinall R.J., Higginson A., Cummings M.H. A randomised placebo controlled trial of VSL#3((R)) probiotic on biomarkers of cardiovascular risk and liver injury in non-alcoholic fatty liver disease. BMC Gastroenterol. 2021;21:144. doi: 10.1186/s12876-021-01660-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Szulinska M., Loniewski I., van Hemert S., Sobieska M., Bogdanski P. Dose-Dependent Effects of Multispecies Probiotic Supplementation on the Lipopolysaccharide (LPS) Level and Cardiometabolic Profile in Obese Postmenopausal Women: A 12-Week Randomized Clinical Trial. Nutrients. 2018;10:773. doi: 10.3390/nu10060773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Barcelos S.T.A., Silva-Sperb A.S., Moraes H.A., Longo L., de Moura B.C., Michalczuk M.T., Uribe-Cruz C., Cerski C.T.S., da Silveira T.R., Dall’Alba V., et al. Oral 24-week probiotics supplementation did not decrease cardiovascular risk markers in patients with biopsy proven NASH: A double-blind placebo-controlled randomized study. Ann. Hepatol. 2023;28:100769. doi: 10.1016/j.aohep.2022.100769. [DOI] [PubMed] [Google Scholar]
- 169.Grossman D.C., Curry S.J., Owens D.K., Barry M.J., Davidson K.W., Doubeni C.A., Epling J.W., Jr., Kemper A.R., Krist A.H., Kurth A.E., et al. Hormone Therapy for the Primary Prevention of Chronic Conditions in Postmenopausal Women: US Preventive Services Task Force Recommendation Statement. JAMA. 2017;318:2224–2233. doi: 10.1001/jama.2017.18261. [DOI] [PubMed] [Google Scholar]
- 170.Zhou X., Wang J., Zhou S., Liao J., Ye Z., Mao L. Efficacy of probiotics on nonalcoholic fatty liver disease: A meta-analysis. Medicine. 2023;102:e32734. doi: 10.1097/MD.0000000000032734. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.