Abstract
Background
Previously improving UK mortality trends stalled around 2012, with evidence implicating economic policy as the cause. This paper examines whether trends in psychological distress across three population surveys show similar trends.
Methods
We report the percentages reporting psychological distress (4+ in the 12-item General Health Questionnaire) from Understanding Society (Great Britain, 1991–2019), Scottish Health Survey (SHeS, 1995–2019) and Health Survey for England (HSE, 2003–2018) for the population overall, and stratified by sex, age and area deprivation. Summary inequality indices were calculated and segmented regressions fitted to identify breakpoints after 2010.
Results
Psychological distress was higher in Understanding Society than in SHeS or HSE. There was slight improvement between 1992 and 2015 in Understanding Society (with prevalence declining from 20.6% to 18.6%) with some fluctuations. After 2015 there is some evidence of a worsening in psychological distress across surveys. Prevalence worsened notably among those aged 16–34 years after 2010 (all three surveys), and aged 35–64 years in Understanding Society and SHeS after 2015. In contrast, the prevalence declined in those aged 65+ years in Understanding Society after around 2008, with less clear trends in the other surveys. The prevalence was around twice as high in the most deprived compared with the least deprived areas, and higher in women, with trends by deprivation and sex similar to the populations overall.
Conclusion
Psychological distress worsened among working-age adults after around 2015 across British population surveys, mirroring the mortality trends. This indicates a widespread mental health crisis that predates the COVID-19 pandemic.
Keywords: mental health, epidemiology, health inequalities
WHAT IS ALREADY KNOWN ON THIS TOPIC
Improving trends in mortality rates, and healthy life expectancy, stalled after around 2012 in the UK and many high-income countries. However, it is not known whether trends in psychological distress show similar trends.
WHAT THIS STUDY ADDS
We found that overall trends in population psychological distress worsened in Great Britain, England and Scotland after 2015, but these were caused entirely by a worsening in those aged under 65 years.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY
It is clear that Great Britain has experienced a multifaceted health crisis even prior to the COVID-19 pandemic. The COVID-19 pandemic and recent inflation are likely to have compounded this, necessitating an urgent and comprehensive public policy response.
Introduction
From the mid-20th century onwards, average life expectancy in the UK increased steadily.1 However, these average trends stalled after around 2012 across all UK nations,2 3 and mortality rates increased for those living in the most deprived areas.4 5 There is evidence that healthy life expectancy, a measure that combines self-rated health with mortality, has also been declining in Scotland over a similar time period.6 However, it is less clear whether trends in mental health and well-being have changed in tandem with mortality trends.
Unlike all-cause mortality,7 it is known that mental health is likely to worsen during periods of recession.8 However, mortality trends and mental health trends may be impacted more by the economic policy responses to recession rather than recessions themselves.7 9 Indeed, the austerity policies imposed by a range of countries following the ‘Great Recession’ (ca 2008–2010) have been demonstrated as the likely explanation for the stalled mortality trends.9
Routine surveillance data from the Scottish Health Survey (SHeS) and Health Survey for England (HSE) are available to examine annual trends across the UK using the 12-item General Health Questionnaire (GHQ-12), a long-standing screening tool for identifying non-psychotic and minor psychiatric disorders in the general population. The Understanding Society panel data set also provides a means to monitor mental health trends. Although there have been analyses of particular population subgroups,10–15 there have not yet been any comprehensive analyses of trends in psychological distress for the population overall, sex, age and deprivation strata, nor has there been any comparison across concurrent survey data sets for these populations.
This paper explores whether trends in mental health changed in parallel to the overall life expectancy trends using population-representative data from the Understanding Society from 1991 to 2019, HSE from 2003 to 2018 and SHeS from 1995 to 2019, using the prevalence of psychological distress based on the GHQ as the outcome of interest.
Methods
Data sources
We obtained 3-year rolling average age-standardised mortality rates (ASMRs), standardised to the 2013 European Standard Population, for England and Scotland by sex for all ages between 1990–1992 and 2017–2019 from the Office for National Statistics to allow a comparison between mortality and mental health trends.
GHQ-12 is a 12-question validated survey measure used to estimate the prevalence of psychological distress in populations.16 GHQ-12 prevalence represents the share of the population with a score of 4+, on a scale between 0 and 12, with higher values indicating greater psychological distress. The GHQ questionnaire is presented in online supplemental file 1.
jech-2022-219660supp001.pdf (52.4KB, pdf)
We analyse data for people aged 16+ years from:
Understanding Society from 1991 to 2019 (called the British Household Panel Survey (BHPS) from 1991 to 2008, and the UK Household Longitudinal Survey until 2019). Overall, we have 648 859 individual year-level observations coming from 106 417 individuals, with an average of 22 374 observations per year. The data are weighted to represent Great Britain (GB).
HSE from 2003 to 2018 (with gaps for some years). The completed sample of adults in each year is around 8000 individuals. The data are weighted to represent England.
SHeS from 1995 to 2019 (with gaps for some years). The completed sample of adults in each year is around 5000 individuals. The data are weighted to represent Scotland.
Analytical approach
Simple descriptive figures for the total weighted populations, and then stratified by sex, age and area deprivation fifth, were produced. The summary inequality indices, the Slope Index of Inequality (SII) and Relative Index of Inequality (RII) were produced assuming that each deprivation fifth represented exactly 20% of the population. Using the approach detailed by Pamuk,17 we then produced linear regressions for each year across the deprivation categories to calculate the SII, and divided that by the population mean to calculate the RII. Finally, we fitted segmented regression models to the data trends in each survey, age group and deprivation fifth, limiting the number of breakpoints to 1, and to the period after 2010. The last step was executed in Stata V.17.0 with its nl command, where we specified a two-piece regression function with one intercept, one breakpoint, two slopes before and after the breakpoint, and these four parameters were estimated using non-linear least squares method such that the estimated segmented regression equation fits the data best in a least squares sense.
Results
Overall population trends
Figure 1 shows trends in ASMRs for England and Scotland, and trends in the percentage of the total adult populations of GB, Scotland and England scoring 4+ on the GHQ-12, between 1990–1992 and 2017–2019 for ASMR, and between 1991 and 2019 for GHQ-12. The previously noted stalling in mortality trends is evident for males and females in Scotland and England from around 2012 to 2014. For GHQ-12, the time series for GB from the Understanding Society data set is the longest and displays a gradual improvement (ie, a decline in the percentage reporting psychological distress), although with substantial year-on-year variation, between 1992 and 2015. However, after 2015 the percentage of people reporting psychological distress steadily increases to 2019. The SHeS shows a similar trend, but with substantially lower percentages until 2018. Here, the percentage is relatively stable until around 2016, with a subsequent increase peaking in 2018. The HSE figures are similar to those from SHeS, and lower than Understanding Society. Here, there is some evidence of an increasing trend over time, but with peaks in 2009 and 2016. The trends are very similar when the data are stratified by sex, with similar increases across the surveys after 2015. However, the percentage of the population reporting psychological distress is consistently higher for women than men (online supplemental figures S2.1 and S2.2).
Figure 1.
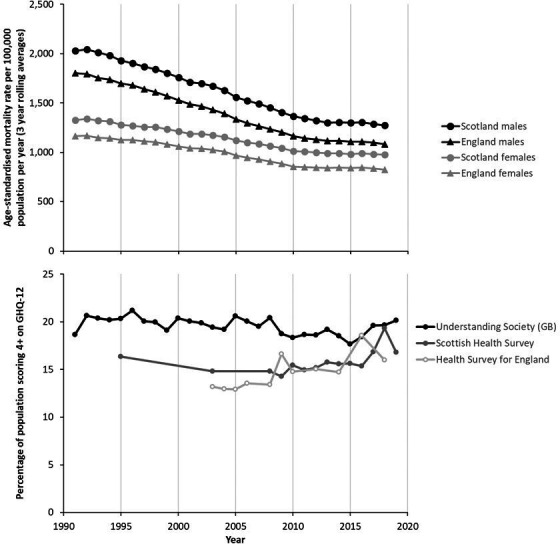
Trends in age-standardised mortality rates (ASMRs) for England and Scotland, and trends in psychological distress in Great Britain (GB), Scotland and England, 1991–2019. GHQ-12, 12-item General Health Questionnaire (Sources: Understanding Society, Scottish Health Survey, Health Survey for England).
jech-2022-219660supp002.pdf (4.4MB, pdf)
Age-stratified trends
When the trends are stratified by age, there is a marked divergence which is obscured in the average population data (figure 2), although the smaller sample sizes mean that the trends have more year-on-year variation than for the total population. The increase in psychological distress after 2015 is only seen among people aged 16–34 and 35–64 years. For those aged 65+ years, there is a decline in psychological distress after 2008 in Understanding Society, but with less stable trends in SHeS and HSE (indeed, HSE shows a marked peak in 2009 for this age group). It is also notable that the increase in psychological distress is evident earlier for those aged 16–34 years compared with those aged 35–64 years, starting around 2010. The marked difference in trends by age suggests that the causes of the worsening trends are likely to be related to factors impacting substantially on working-age adults rather than older adults.
Figure 2.
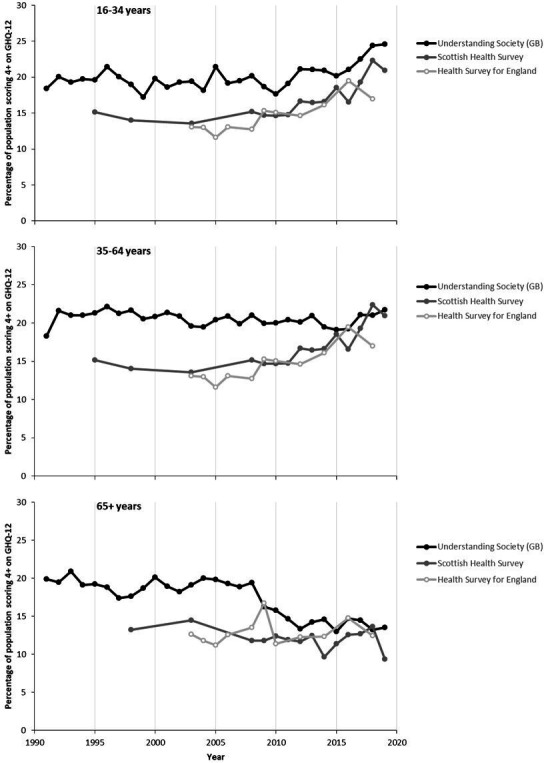
Trends in psychological distress in Great Britain (GB), Scotland and England, stratified by age, 1991–2019. GHQ-12, 12-item General Health Questionnaire (Sources: Understanding Society, Scottish Health Survey, Health Survey for England).
Deprivation-stratified trends
When the data are stratified by area deprivation, the inequalities in psychological distress are exposed (figure 3). The trends in the summary measures of absolute inequality (SII) and relative inequality (RII) across the populations are provided in online supplemental figures S2.3–S2.5. Across GB, Scotland and England, and for the entire time series, there are large inequalities in the prevalence of psychological distress, with a stepwise gradient across the ranked population. The trends for the SII and RII are very similar across all data sets as there is no strong secular trend in the population means (which would create a divergence between the absolute and relative measures). In the SHeS and HSE, the percentage of the population reporting psychological distress in the most deprived areas is around double that of the least deprived areas. The stepwise gradient across the population becomes clearer in the Understanding Society data set only after 2009, and is associated with a notable increase in inequalities (online supplemental figure S2.3) that looks likely to be associated with the changes in the panel make-up at that time. Prior to 2009, there are some marked year-on-year fluctuations in inequalities in the Understanding Society data set and evidence of reduced inequalities after 2013. Within the SHeS and HSE data sets the trends in inequalities after 2010 are very unstable with marked fluctuations between years on both the SII and RII reflecting a lack of parallel trends across deprivation fifths. It is notable that the rise in the percentage reporting psychological distress in Scotland is much more marked in the most deprived 40% of areas.
Figure 3.
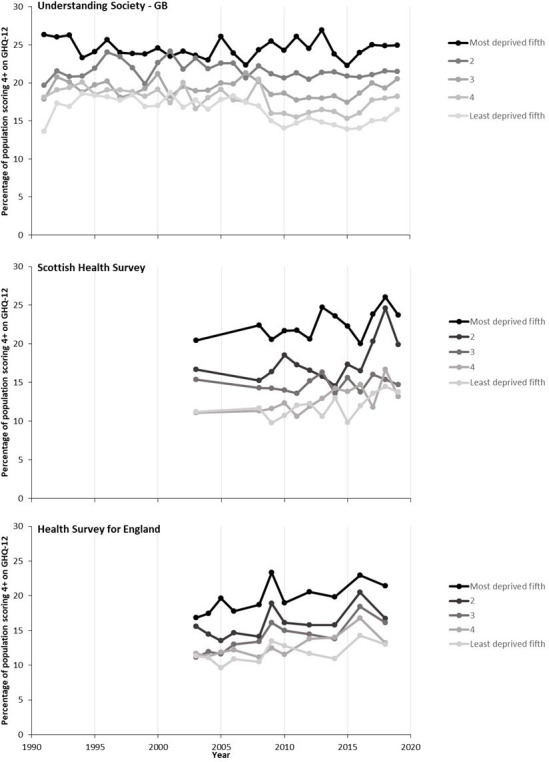
Trends in psychological distress in Great Britain (GB), Scotland and England, stratified by area deprivation, 1991–2019. GHQ-12, 12-item General Health Questionnaire (Sources: Understanding Society, Scottish Health Survey, Health Survey for England).
Intersectional stratifications
When the data are stratified concurrently across combinations of age, sex and deprivation, the numbers in each group are much smaller, and as a result the trends become less stable and clear. Online supplemental figures S2.6 and S2.7 show the trends stratified by deprivation and sex, and indicate clearer and wider inequalities by deprivation for men than women. The deprivation inequalities are widest among those aged 35–64 years compared with younger or older adults (online supplemental figures S2.8–S2.10).
Breakpoints in the trends
When formal segmented regression analyses are fitted to the data to identify the breakpoints in the trends, there is a change from improving trends to a marked worsening in the trends for Scotland (SHeS) after 2011 and across GB after 2016 (Understanding Society) that are obvious. The trend for England worsens throughout the time series with only a minor change in trend (towards a less rapid worsening between 2016 and 2018) (online supplemental figure S2.11). The changes in trends and their timing are similar when the data are stratified by sex (online supplemental figure S2.12). However, when the data are stratified by age the differences noted in the descriptive analyses are obvious. For people aged 16–34 and 35–64 years psychological distress worsens in the latest time period and, except for the HSE data for 35–64 year-olds, is getting worse more quickly. The change in trends for 16–34 year-olds occurs earlier (ca 2010, across surveys) than for people aged 35–64 years, and especially in Understanding Society. In contrast, with the exception of SHeS, there is a more rapid improvement in those aged 65+ years in the most recent period (online supplemental figure S2.13). Finally, when the data are stratified by deprivation fifth there is some variance in the timing of the changes in trends (online supplemental figure S2.14).
Discussion
Main results
The percentage of the overall population scoring 4+ on the GHQ-12 over time is higher in Understanding Society (for GB) than in the SHeS (for Scotland) or HSE (for England). The long time series for GB improved between 1991 and around 2015, although with some fluctuations. After 2015 there is some evidence of a deterioration in mental health across surveys, but the data for Scotland and England have substantial year-on-year variation. However, there are much clearer trends when the data are stratified by age, with consistent increases in psychological distress across surveys for those aged 16–34 years after 2010, and increases for those aged 35–64 years in Understanding Society and SHeS after 2015. In contrast, psychological distress declines in those aged 65+ years in Understanding Society after around 2008, and shows no clear pattern in the other surveys. This difference in trend by age strongly suggests that the causes of the worsening trends are to be found in the conditions facing workers, people on working-age benefits and people with young children. Throughout the time series there are substantial inequalities in psychological distress with around double the prevalence in the most deprived areas compared with the least deprived areas, and a higher prevalence among females compared with males.
Strengths and limitations
Although life expectancy is a critical measure of the health of populations, it is also a very narrow one. Taken with the existing work on mortality and healthy life expectancy,2–6 9 18 this paper provides a more holistic picture of health and health inequality trends and the extent to which the stalling of life expectancy is reflected in other measures. The data used here are among the best available for understanding the experience of mental health. They are drawn from government-funded surveys which aim to be representative of the population, and use validated and comparable measures of the prevalence of psychological distress.16 By triangulating data across three surveys there is greater certainty in the trends, and the difficulties associated with the periodic changes in sampling are reduced. Using survey data avoids the problems associated with changes in clinical practice, or the acceptability of treatments, as would be the case if prescribing for mental health conditions was used as an outcome. Similarly, the outcome is not impacted by health service capacity or focused on only the most severe mental health outcomes as would be the case with admission to hospital or suicide mortality. By stratifying the data we identified divergent trends, particularly by age, which were otherwise obscured.
We limited the Understanding Society data set to GB to avoid the step change associated with the inclusion of Northern Ireland part way through the time series. However, there was a change in the sample for Understanding Society after 2009 which may have created a risk of a step change. The original sample of BHPS (1991–2009), the predecessor survey of Understanding Society, was not included in Understanding Society until its second wave (2010–2012).19 As a result, 98% of the observations in 2009 were from a new sample. Although the data used here are the best available for GB, Scotland and England, they are subject to limitations. In particular, non-response bias is a growing problem for the SHeS and HSE (and made the data in 2020 and 2021 virtually unusable), and is likely to have created an ever-increasing healthy responder bias.20 It would be expected that this would bias the sample and the trends towards improving health outcomes over time, and so the increased prevalence of psychological distress might be a substantial underestimate of the extent of the problematic trend. The sampling strategy of SHeS and HSE (as repeat cross-sectional surveys) is different from Understanding Society (panel survey) and the latter would be expected to have attrition which is also likely to bias towards healthy respondents. It is unclear whether falling response rates or attrition were likely to have created larger biases. Some of the secular trends may also have been due to changes in the age structure of the populations over time, particularly given the different trends observed when the data were age stratified.
How this fits with the existing literature
The stalling in life expectancy trends after around 2012 across the UK, and many other high-income countries, has been clearly described.2 9 18 This has been due to changes in mortality trends across almost all age groups and causes of death.21 22 More recently, a deterioration in healthy life expectancy has also been described, with contributions from both self-rated health and mortality.6 Psychological distress arguably has a non-linear relationship with age, being worst in middle age. Despite this, within the Understanding Society data set, the temporal trends have been found to dominate the impacts of cohort or age effects.23 We find here that there are markedly divergent trends by age group across surveys, with much clearer increases in prevalence for younger adults than older adults. This fits with the broader literature on the causes of the contemporaneous stalled life expectancy trends as being due to factors that have primarily impacted on working-age populations, such as cuts and increased conditionality of working-age social security benefits, and rising employment precarity.9 As noted previously, recessions may narrow socioeconomic and gender inequalities in mental health, but austerity exacerbates them.24
The worsening in psychological distress among working-age adults in GB described in our study is consistent with other analyses using these data sets, and with data from primary care records. In Scotland, there was an increase in reporting of symptoms of anxiety and depression, and the reporting of suicide attempts and having ever self-harmed, between 2012–2013 and 2018–2019.25 There does not seem to have been any trend analyses published by the HSE team based on GHQ-12 for all adults after 2010.26 Other researchers have used the HSE and found that, between 1991 and 2010, mental health (measured with GHQ-12) in English working-age adults (25–64 years) slightly improved on average, especially between 1997 and 2003 for women,10 but with persistently worse mental health for women and for people with lower incomes, less education and in lower socioeconomic positions.11 Similarly, among studies focused on children and young people in GB, there was evidence of increased prevalence of long-standing mental health conditions between 1995 and 2014, and in psychological distress between 2011 and 2014,12 and between 2009/2010 and 2018/2019, particularly for those aged 16–18 years and of white ethnicity.13 The increase in psychological distress among young adults (aged 16–34 years) in the BHPS/Understanding Society has been reported previously.14 Finally, there is also evidence of a rise in anxiety and depression diagnoses and symptoms among people aged 18–24 years, and especially women, from UK primary care records between 2014 and 2018.15 27
Relevant to explaining these trends, a systematic review of observational studies showed that policies which reduced the eligibility and generosity of social security led to a worsening in mental health and increased inequalities, while increased eligibility and generosity improved mental health.28 For example, the change to Universal Credit in the UK, which reduced eligibility and the real value of social security, led to a 7% increase in psychological distress after adjusting for confounders.29 Indeed, there is evidence that tightening of the sanctions on unemployment benefits in 2012, which increased the length of time for which people were in receipt of no benefit, led to increases in anxiety and depression.30 There is also now high-quality systematic review evidence that changes in income, and especially movement into or out of poverty, have a profound impact on mental health and well-being.31 In Scotland, antidepressant use increased over the period 2009–2015, and especially in those areas impacted most by unemployment and reductions in the real value of social security benefits.32 More recently, a wide range of mental health measures are evidenced to have worsened during the COVID-19 pandemic for some groups,33 34 with mixed results for the short-term impacts of the pandemic from studies with less robust sampling methods.35
Implications
The stalling of life expectancy trends and mortality inequalities are among the biggest public health challenges we face,36 with very substantial impacts on the years of life lost.37 The stalled life expectancy trends are likely to be largely due to the austerity policies introduced from 2010 onwards,9 38 and the associated cuts to local government funding and social security.9 There is now a substantial body of evidence that the increased conditionality and reduced real terms value of social security benefits have had marked deleterious impacts on mental health, and this is likely to be a substantial contributor to the overall population mental health trends exposed here. Governments should act to protect population health and reduce health inequalities by addressing the economic causes of these trends as well as the wider range of social determinants of health, the recommendations for which have been published in detail elsewhere.9 39 40
Conclusion
The prevalence of psychological distress increased after 2010 in young adults and after 2015 in working-age adults across GB. Inequalities in psychological distress are substantial by area deprivation, with around double the prevalence in the most deprived areas compared with the least deprived areas. Psychological distress is higher in females than in males. The trends in psychological distress are similar to those for overall population life expectancy and healthy life expectancy, indicating a population health challenge that predates the COVID-19 pandemic and which demands a radical and coherent governmental response.
Footnotes
Twitter: @thierrygagn, @gerrymccartney1
Contributors: The idea for the manuscript was developed by GM and EP. AZ, DW and TG obtained and cleaned the relevant data. AZ and GM undertook the data analysis. GM drafted the manuscript with critical contributions from all authors. All authors approved the final draft. GM is the guarantor.
Funding: AZ, AC, EP and GM are salaried by the University of Glasgow; TG by University College London; and DW by the Glasgow Centre for Population Health.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
All data relevant to the study are included in the article or uploaded as supplementary information.
Ethics statements
Patient consent for publication
Not applicable.
References
- 1. McCartney G, Walsh D, Whyte B, et al. Has Scotland always been the ‘sick man’ of Europe? An observational study from 1855 to 2006. Eur J Public Health 2012;22:756–60. 10.1093/eurpub/ckr136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Fenton L, Minton J, Ramsay J, et al. Recent adverse mortality trends in Scotland: comparison with other high-income countries. BMJ Open 2019;9:e029936. 10.1136/bmjopen-2019-029936 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Minton J, Fletcher E, Ramsay J, et al. How bad are life expectancy trends across the UK, and what would it take to get back to previous trends? J Epidemiol Community Health 2020;74:741–6. 10.1136/jech-2020-213870 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Walsh D, McCartney G, Minton J, et al. Changing mortality trends in countries and cities of the UK: a population-based trend analysis. BMJ Open 2020;10:e038135. 10.1136/bmjopen-2020-038135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Fenton L, Wyper GM, McCartney G, et al. Socioeconomic inequality in recent adverse all-cause mortality trends in Scotland. J Epidemiol Community Health 2019;73:971–4. 10.1136/jech-2019-212300 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Walsh D, Wyper GMA, McCartney G. Trends in healthy life expectancy in the age of austerity. J Epidemiol Community Health 2022;76:743–5. 10.1136/jech-2022-219011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. McCartney G, Hearty W, Arnot J, et al. Impact of political economy on population health: a systematic review of reviews. Am J Public Health 2019;109:e1–12. 10.2105/AJPH.2019.305001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Frasquilho D, Matos MG, Salonna F, et al. Mental health outcomes in times of economic recession: a systematic literature review. BMC Public Health 2015;16:115. 10.1186/s12889-016-2720-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. McCartney G, Walsh D, Fenton L, et al. Resetting the course for population health. Glasgow: Glasgow Centre for Population Health and the University of Glasgow, 2022. [Google Scholar]
- 10. Katikireddi SV, Niedzwiedz CL, Popham F. Trends in population mental health before and after the 2008 recession: a repeat cross-sectional analysis of the 1991-2010 health surveys of England. BMJ Open 2012;2:e001790. 10.1136/bmjopen-2012-001790 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Jokela M, Batty GD, Vahtera J, et al. Socioeconomic inequalities in common mental disorders and psychotherapy treatment in the UK between 1991 and 2009. Br J Psychiatry 2013;202:115–20. 10.1192/bjp.bp.111.098863 [DOI] [PubMed] [Google Scholar]
- 12. Pitchforth J, Fahy K, Ford T, et al. Mental health and well-being trends among children and young people in the UK, 1995-2014: analysis of repeated cross-sectional National health surveys. Psychol Med 2019;49:1275–85. 10.1017/S0033291718001757 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Gagné T, Nandi A, Schoon I. Time trend analysis of social inequalities in psychological distress among young adults before and during the pandemic: evidence from the UK household longitudinal study COVID-19 waves. J Epidemiol Community Health 2022;76:421–7. 10.1136/jech-2021-217266 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Gagné T, Schoon I, McMunn A, et al. Mental distress among young adults in Great Britain: long-term trends and early changes during the COVID-19 pandemic. Soc Psychiatry Psychiatr Epidemiol 2022;57:1261–72. 10.1007/s00127-021-02194-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Slee A, Nazareth I, Freemantle N, et al. Trends in generalised anxiety disorders and symptoms in primary care: UK population-based cohort study. Br J Psychiatry 2021;218:158–64. 10.1192/bjp.2020.159 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Goldberg DP, Gater R, Sartorius N, et al. The validity of two versions of the GHQ in the who study of mental illness in general health care. Psychol Med 1997;27:191–7. 10.1017/s0033291796004242 [DOI] [PubMed] [Google Scholar]
- 17. Pamuk ER. Social class inequality in mortality from 1921 to 1972 in England and Wales. Population Studies 1985;39:17–31. 10.1080/0032472031000141256 [DOI] [PubMed] [Google Scholar]
- 18. Ho JY, Hendi AS. Recent trends in life expectancy across high income countries: retrospective observational study. BMJ 2018;362:k2562. 10.1136/bmj.k2562 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Lynn P. Sample design for understanding society. Understanding society working paper series, 2009-01. Institute for Social and Economic Research, University of Essex, 2009. [Google Scholar]
- 20. Gorman E, Leyland AH, McCartney G, et al. Adjustment for survey non-representativeness using record-linkage: refined estimates of alcohol consumption by deprivation in Scotland. Addiction 2017;112:1270–80. 10.1111/add.13797 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Public Health England . A review of recent trends in mortality in England. London: Public Health England, 2018. [Google Scholar]
- 22. Ramsay J, Minton J, Fischbacher C, et al. How have changes in death by cause and age group contributed to the recent stalling of life expectancy gains in Scotland? Comparative decomposition analysis of mortality data, 2000-2002 to 2015-2017. BMJ Open 2020;10:e036529. 10.1136/bmjopen-2019-036529 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Prior L, Jones K, Manley D. Ageing and cohort trajectories in mental ill-health: an exploration using multilevel models. PLOS ONE 2020;15:e0235594. 10.1371/journal.pone.0235594 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Thomson RM, Niedzwiedz CL, Katikireddi SV. Trends in gender and socioeconomic inequalities in mental health following the great recession and subsequent austerity policies: a repeat cross-sectional analysis of the health surveys for England. BMJ Open 2018;8:e022924. 10.1136/bmjopen-2018-022924 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Scottish Government . Scottish health survey 2019 - volume 1: main report. Edinburgh: Scottish Government, 2020. Available: https://www.gov.scot/publications/scottish-health-survey-2019-volume-1-main-report/pages/5/ [Google Scholar]
- 26. Office for National Statistics . Health Survey for England 2018. London: Office for National Statistics, 2019. [Google Scholar]
- 27. Cybulski L, Ashcroft DM, Carr MJ, et al. Temporal trends in annual incidence rates for psychiatric disorders and self-harm among children and adolescents in the UK, 2003-2018. BMC Psychiatry 2021;21:229. 10.1186/s12888-021-03235-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Simpson J, Albani V, Bell Z, et al. Effects of social security policy reforms on mental health and inequalities: a systematic review of observational studies in high-income countries. Soc Sci Med 2021;272:113717. 10.1016/j.socscimed.2021.113717 [DOI] [PubMed] [Google Scholar]
- 29. Wickham S, Bentley L, Rose T, et al. Effects on mental health of a UK welfare reform, universal credit: a longitudinal controlled study. The Lancet Public Health 2020;5:e157–64. 10.1016/S2468-2667(20)30026-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Williams E. Punitive welfare reform and claimant mental health: the impact of benefit sanctions on anxiety and depression. Soc Policy Adm 2021;55:157–72. 10.1111/spol.12628 [DOI] [Google Scholar]
- 31. Thomson RM, Igelström E, Purba AK, et al. How do income changes impact on mental health and wellbeing for working-age adults? A systematic review and meta-analysis. Lancet Public Health 2022;7:e515–28. 10.1016/S2468-2667(22)00058-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Cherrie M, Curtis S, Baranyi G, et al. A data linkage study of the effects of the great recession and austerity on antidepressant prescription usage. Eur J Public Health 2021;31:297–303. 10.1093/eurpub/ckaa253 [DOI] [PubMed] [Google Scholar]
- 33. Niedzwiedz CL, Green MJ, Benzeval M, et al. Mental health and health behaviours before and during the initial phase of the COVID-19 lockdown: longitudinal analyses of the UK household longitudinal study. J Epidemiol Community Health 2021;75:224–31. 10.1136/jech-2020-215060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Pierce M, Hope H, Ford T, et al. Mental health before and during the COVID-19 pandemic: a longitudinal probability sample survey of the UK population. Lancet Psychiatry 2020;7:883–92. 10.1016/S2215-0366(20)30308-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. O’Connor RC, Wetherall K, Cleare S, et al. Mental health and well-being during the COVID-19 pandemic: longitudinal analyses of adults in the UK COVID-19 mental health & wellbeing study. Br J Psychiatry 2021;218:326–33. 10.1192/bjp.2020.212 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. McCartney G, Douglas M, Taulbut M, et al. Tackling population health challenges as we build back from the pandemic. BMJ 2021;375:e066232. 10.1136/bmj-2021-066232 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. McCartney G, Leyland A, Walsh D, et al. Scaling COVID-19 against inequalities: should the policy response consistently match the mortality challenge? J Epidemiol Community Health 2021;75:315–20. 10.1136/jech-2020-214373 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. McCartney G, McMaster R, Popham F, et al. Is austerity a cause of slower improvements in mortality in high-income countries? A panel analysis. Soc Sci Med 2022;313:115397. 10.1016/j.socscimed.2022.115397 [DOI] [PubMed] [Google Scholar]
- 39. Sayer A, McCartney G. Economic relationships and health inequalities: improving public health recommendations. Public Health 2021;199:103–6. 10.1016/j.puhe.2021.08.017 [DOI] [PubMed] [Google Scholar]
- 40. Walsh D, Lowther M, McCartney G, et al. Can Scotland achieve its AIM of narrowing health inequalities in a post-pandemic world? Public Health Pract (Oxf) 2020;1:100042. 10.1016/j.puhip.2020.100042 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
jech-2022-219660supp001.pdf (52.4KB, pdf)
jech-2022-219660supp002.pdf (4.4MB, pdf)
Data Availability Statement
All data relevant to the study are included in the article or uploaded as supplementary information.


