Abstract
Background
Global health will increasingly be determined by cities. Currently over half of the world’s population, over 4 billion people, live in cities. This systematic scoping review has been conducted to understand what cities are doing to improve health and healthcare for their populations.
Methods
We conducted a systematic search to identify literature on city-wide initiatives to improve health. The study was conducted in accordance with PRISMA and the protocol was registered with PROSPERO (CRD42020166210).
Results
The search identified 42,137 original citations, yielding 1,614 papers across 227 cities meeting the inclusion criteria. The results show that the majority of initiatives were targeted at non-communicable diseases. City health departments are making an increasing contribution; however the role of mayors appears to be limited.
Conclusion
The collective body of evidence identified in this review, built up over the last 130 years, has hitherto been poorly documented and characterised. Cities are a meta-system with population health dictated by multiple interactions and multidirectional feedback loops. Improving health in cities requires multiple actions, by multiple actors, at every level. The authors use the term ‘The Vital 5’. They are the five most important health risk factors; tobacco use; harmful alcohol use; physical-inactivity, unhealthy diet and planetary health. These ‘Vital 5’ are most concentrated in deprived areas and show the greatest increase in low and middle income countries. Every city should develop a comprehensive strategy and action plan to address these ‘Vital 5’.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12889-023-15908-0.
Keywords: City, Urban, Health, Transformation, Systematic
Background
Global heath will increasingly be determined by cities. Currently over half (55 per cent) of the world’s population lives in cities and by 2050, 68 percent of the world’s population is projected to be urban [1]. This growth has occurred and will continue to occur over a relatively short period. The world’s cities are growing in both size and number in all regions [2] but there is particularly rapid growth in the number and size of cities across Asia, Africa and South America [3]. For example, between 1950 and 2005, the percentage of the population of China living in cities rose from 13 to 40% and it is predicted to rise to 60.3 percent by 2030 [2]. To put the scale of the urbanisation challenge and opportunity in context, since 2003, China poured more cement every two years than the US did in the entire 20th century [4]. Concrete manufacture accounts for at least 8% of global carbon emissions [5]. This will have a significant impact on environmental health which has both direct and indirect impact on population health.
Whilst cities contain some of the best health and healthcare, they also contain a disproportionate share of the worst [6]. There also remains significant variation in health and high levels of inequality [7]. Many urban health and environmental challenges are a consequence of how we organise and live in cities [8] which have resulted in cities that are making people sicker, fatter and more socially isolated [9–11]. Globally cities have been hardest hit by Covid-19 [12].
However, there are also reasons for optimism. Cities are the world's engines of economic growth, innovation, and social change [13]. City living is better for the environment [3] and city dwellers have had better health than their rural counterparts since at least the early to mid-20th century, in high income as well as low and middle income countries [6, 14] Climate change is the number one threat to population health [15–18] and it is cities that are leading the way in becoming carbon neutral [19]. Cities have been shown to succeed—where national governments have failed—in making significant improvements in areas affecting population health [20–26].
It is widely accepted we need to improve equitable health and care in cities. There is good financial imperative to do so; good health is not only a consequence of, but also a condition for sustained and sustainable economic development [27]. In this way, the health of a city creates a virtuous circle of improved health and improved economic prosperity. Not just for the city but for its nation [14]. There is a compelling case to improve health in city populations.
The aim of this global systematic scoping review is to provide an overview of the existing evidence of city initiatives to improve health. In addition, a summary of each of the 1614 papers which describe an initiative to improve health or healthcare is provided (Additional file 1) in a format that can be thematically searched. This will be a useful resource for academics and policy makers interested in improving urban health. The outputs of this systematic scoping review should be used to inform urban health policy for the next decade.
Methods
Aim and overview
A systematic search was conducted to identify literature on city-wide initiatives to improve health. This study was completed in accordance with the PRISMA extension for scoping reviews [28] The protocol was registered at PROSPERO (number CRD42020166210).
Search strategy and selection criteria
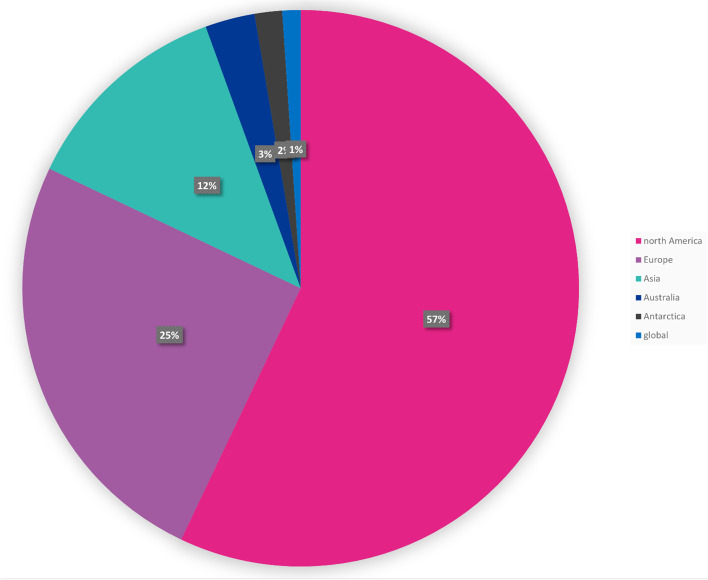
Ten databases were searched; Embase, Ovid Medline, Cochrane Database (CENTRAL), Scopus, Campbell Library, CINALH, Health Business Elite, Health Management Information Consortium (HMIC), PyschINFO and Prospero. Specific and pre-determined search terms were developed, tested and finalised for each database. These are available in Additional file 1. The inclusion criteria was: city-wide initiatives that aimed to improve health or healthcare. The definition of improvement, for the purposes of this research, was purposefully broad and included any initiative whose aim was to improve health outcomes or healthcare services. Citations that did not describe an improvement initiative or did describe an improvement initiative but only of a single organisation and not city-wide were excluded. City-wide improvement initiative of family planning services and malaria and dengue fever were excluded. Citations not in English language were also excluded. All databases were searched on the 10 – 12 February 2016, for entries from database inception to February 2016 (tranche 1). The search was updated on 16 March 2019, for entries from February 2016 to March 2019 (tranche 2). Extensive hand searching was also completed. The database results were uploaded to Endnote (version 9) (Fig. 1).
Fig. 1.
– PRISMA [29] study attrition flow chart
Publication selection
All types of study design were eligible for inclusion, including grey literature. Studies were not selected or screened based on methodological quality. The key factor was that the study needed to describe a city-wide initiative to improve health or healthcare. All initiatives were included irrespective of how ambitious they were. The primary outcome indicators that were sought and extracted were: improved health or reduced health inequalities; improved healthcare (safety, effectiveness, patient experience); failed initiative or negative or unintended consequences. The first tranche (31,251 original citations) were assessed independently by the lead author (SD) and HLP1 against the inclusion criteria. The level of inter-reviewer agreement on the articles was on average 96% (range 91%—98%). Where there was a disagreement, the two reviewers discussed and agreed on a final outcome. The second tranche was assessed by SD. Where it was uncertain whether the initiatives were city-wide, they were included.
Data analysis
Predetermined data fields were agreed prior to data extraction. The data fields were; date of publication; type of publication; initiative; how the initiative was implemented; city; city population; country; continent; quantitative outcome; author’s qualitative conclusion. A template (excel) was developed for data extraction and analysis. Where any of this data was not presented, it was coded as ‘not stated’. The only exception to this was with city population. Where this was not presented, the information was sought through world statistics organisation [30]. The latest available population data was used (irrespective of when the initiative took place). The lead author (SD) extracted the data and systematically coded and analysed the data. Studies that did not name a specific city were still included as long as that they indicated they were from a city. Inductive thematic analysis, in line with the guidelines of Braun and Clarke, [31] was carried out as it offered optimum flexibility and breadth. The included studies were not critically appraised for quality. However, the authors have highlighted throughout the text, major methodological issues, source of study heterogeneity and necessary contextual information for interpreting the results. This data was used by the authors to debate and agree the key findings and recommended policy actions.
Patient and public involvement
This research was done without patient or public involvement.
Results
The database searches yielded a total of 42,028 original citations after duplicates were removed through Endnote standard duplicate check. These electronic searches were augmented with an additional 109 citations found through expert recommendations or internet searches, giving a total of 42,137 original citations. These citations were assessed and resulted in 1614 citations meeting the inclusion criteria.
The full text of the 1614 citations was screened and all included in the inductive thematic coding. The overwhelming majority (90%, n = 1455) of papers were journal articles. The publication date ranged from 1892 to 2019.
Subject areas of health improvement
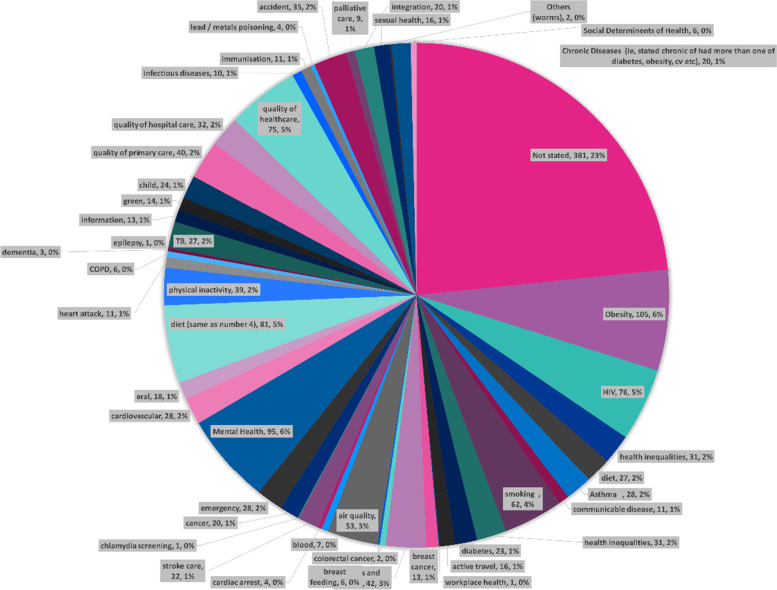
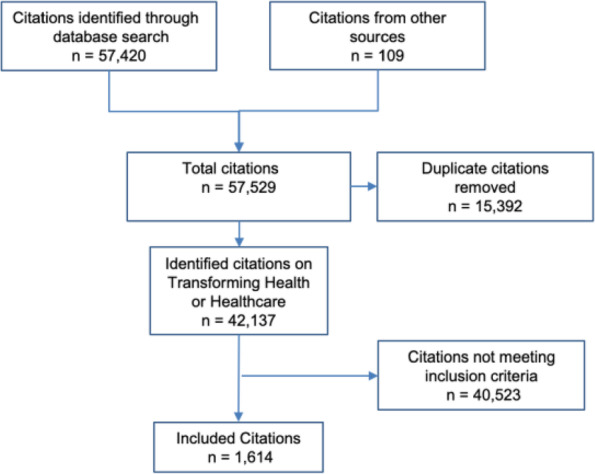
A total of 47 themes emerged as subject areas that cities were seeking to address. Just over two thirds (69% n = 1113) of the subject areas were related to improving health, with the remaining 31% (n = 501) related to improving health services. Across improving health and improving healthcare, 92% (n = 1483) were addressing non-communicable diseases (Fig. 2).
Fig. 2.
Subject area cities were seeking to address
Of those related to improving health, 1043 (94%) were focused on non-communicable diseases and 70 (6%) were focused on communicable diseases. In relation to non-communicable diseases, there were 39 different subject areas addressed. A significant proportion (n = 354 equivalent to 33%) did not state a specific area of health they were seeking to address. Where a specific area was stated, the highest was obesity (n = 104), followed by diet (n = 102), smoking (n = 61) and then air quality (n = 53). The non-communicable health subject areas are presented in Fig. 3 below. The communicable diseases [32] included; HIV (n = 44), TB (n = 12), Sexual Transmitted Disease (n = 1), Influenza, Small Pox, Typhoid and others (n = 10).
Fig. 3.
Non-communicable health subject areas that cities were seeking to address
This graph shows subject areas included in five or more citations. Those coded as general health or not stated have been removed.
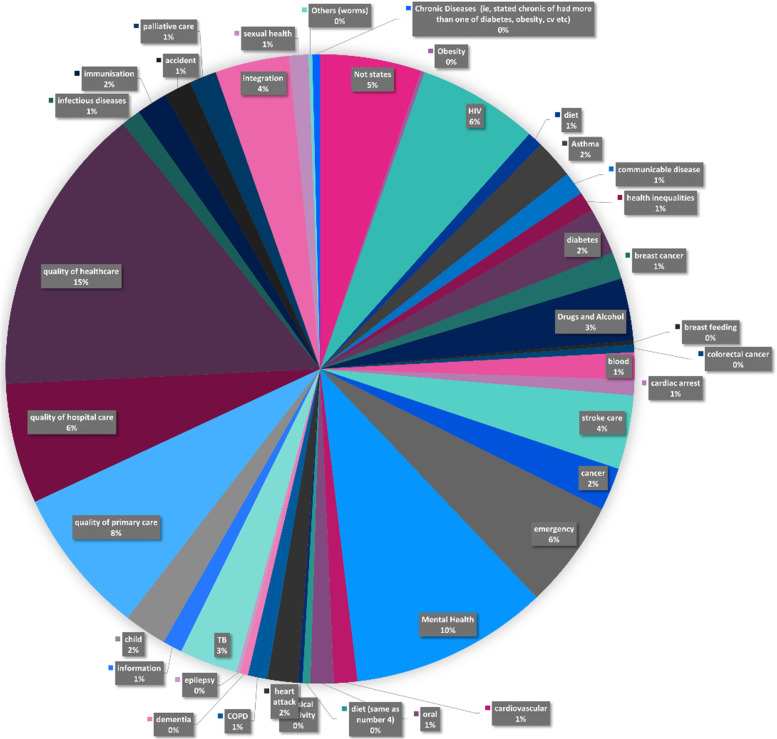
Those relating to improving health services (n = 501) were split across forty thematic areas as shown in Fig. 4 below.
Fig. 4.
Subject areas that were being addressed through improving healthcare
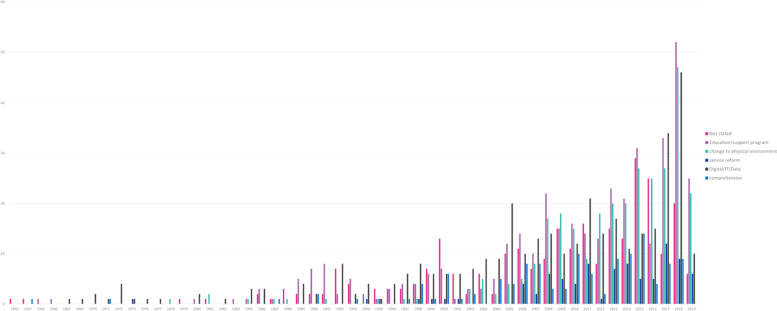
Type of initiative
There were 6 categories of initiative identified (Table 1). Education was the most frequently applied type of initiative with 26%, followed closely by service reform (23%) and change to physical environment (21%). A significant proportion (17%) either did not state the type of initiative or it was unclear. Less than a tenth (8%) described a comprehensive initiative and the smallest volume of initiatives were related to digital, data or IT (6%) (Fig. 5).
Table 1.
Type of initiative
| Category | Definition of category | # of papers | % |
|---|---|---|---|
| Education / support program | A programme to education or support the individual(s), either patient / population or workforce. For example, the education initiative to improve healthy lifestyles with a focus on school children [33] | 414 | 26% |
| Service reform | A change or addition to a health service, ie improved patient flow redesign or additional outpatient clinic. For example, the description of Shanghai’s service reforms [34] | 366 | 23% |
| Change to physical environment | A change to the physical environment to change the world in which the individual interacts. For example, Los Angeles banning fast-food restaurants [35] | 336 | 21% |
| Comprehensive | The initiative was described as, and believed to be, a comprehensive initiative (ie more than one single initiative) and / or it contained more than one of these 6 categories. For example, the urban health strategy in Detroit [36] | 124 | 8% |
| Digital / IT / Data | A digital or data initiative, or the use of IT more generally, to improve health or healthcare | 92 | 6% |
| Not stated / unclear | There was not an initiative or if there was it was not stated in the title or abstract. For example, Taipei’s multi-channel digital risk communications to prevent the spread of a communicable disease [37] | 282 | 17% |
Fig. 5.
Type of initiative per year
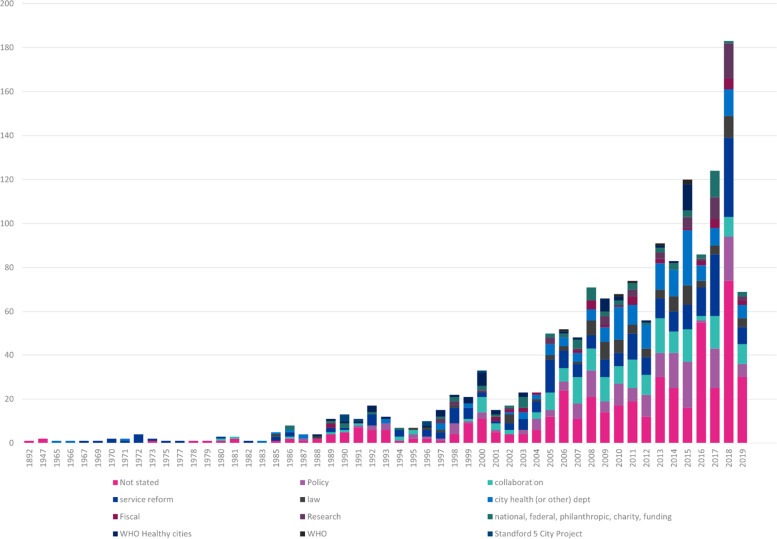
How the initiative was instigated
There were 12 categories which indicated how the initiative was instigated (Table 2). Eight were predetermined ahead of data extraction, four (national or philanthropic funded, research, WHO, Stanford 5 city project) were identified during extraction. Over a third (34%) did not state how the initiative was instigated. Policy (12%), collaboration (12%), service reform (11%) and law (11%) were the next highest methods of instigating an initiative. It is worth noting the contribution of City Health Departments (6%), WHO Healthy Cities (5%) and national or philanthropic (5%). Only 44 (3%) referenced a Mayor as having a significant role (Figure 6) (Table 2).
Table 2.
Number of papers in each category
| Categories of ‘how’ initiative was instigated | # of papers | % |
|---|---|---|
| Policy | 178 | 11% |
| Collaboration | 181 | 11% |
| Service Reform | 247 | 15% |
| Law | 91 | 6% |
| City Health (or other) Department | 163 | 10% |
| WHO Healthy Cities | 51 | 3% |
| National or Philanthropic | 68 | 4% |
| Fiscal / Financial levers | 38 | 2% |
| Research | 55 | 3% |
| WHO (but not Healthy Cities) | 6 | 0% |
| Stanford 5 City Project | 7 | 0% |
| Not stated | 529 | 33% |
Fig. 6.
How initiatives were instigated each year
Location
The city in which an initiative was carried out was recorded and coded, as was the country and continent of the city. In addition, the population of the city was recorded if it was stated and if it was not recorded it was sought. The 1614 citations represent initiatives from 227 cities. The majority of cities were just in one paper (n = 179 cites). New York City accounted for nearly one fifth (17% 279 of 1614) of the total papers, followed by Baltimore (51) and London (48). Collectively, these 3 cities (less than 1% of total number of cities) account for nearly a quarter (23%) of all the citations.
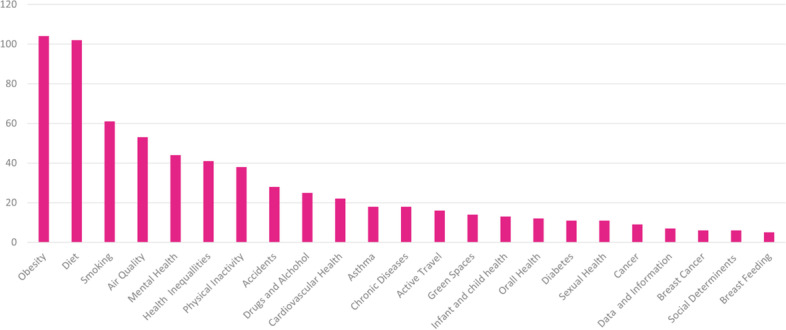
The 227 cities come from 80 countries across five continents. The USA accounts for the highest number of citations (n = 690), significantly more than the next highest (England with 135 citations). North America accounts for 57% of all the citations (Fig. 7).
Fig. 7.
Citations per continent
The populations of cities ranged from 1,465 (Stevenson, WA, USA) [38] to 23,019,196 (Shanghai, China) [34]. This highlights the vast variation in population size of cities and indicates the breadth of the interpretation and definition of a city.
Outcome of the initiatives
Outcome was extracted and coded into; 1) no outcome stated; 2) input or process measure; 3) positive outcome measure; or 4) negative outcome. Definition for 2) input or process measure is, for example, Feyerherm et al. [39] which reported on the number of organisations that participated and carried through some subsequent action (input measure). Or, for example, Sacks and Nonas [40] who reported on the outcome of number of adults reported as eating fruit and vegetables (process measure). Definition for 3) positive outcome measure is defined as a measure of health or a measure with a direct health benefit (eg reduced smoking, reduced obesity). For example; Duncan [41] who reported a 40% reduction in emergency department visits by high users (outcome related to healthcare). Or, Coady et al. [42] who reported a 27% decrease in smokers (direct health benefit). Or Weinstein [43] that reported on reduced infant mortality. Finally, an example of a negative outcome would be De Salazar [44] who reported the initiative to reduce prevalence of cardiovascular disease in Cali (Columbia) actually increased sedentary lifestyles.
More than half (57%) did not have an outcome recorded. Thirty four percent referenced an input or process measure. Eight percent reported an outcome measure and one percent reported a negative impact as a result of the initiative.
It is not possible to describe all the initiatives in detail in this manuscript. Therefore, an excel file is provided with all records and data extraction and analysis is available in Additional file 2. This Additional file can be used as a resource for policy makers and researchers to further interrogate and build on the data.
Discussion
There is growing interest in the actions that cities are taking to improve health and healthcare. This is in keeping with the increasing importance of cities in determining global population health. The earliest initiative was the House of Lords Select Committee Report on Metropolitan Hospitals, Provident and Other Public Dispensaries and Charitable Institutions for the Sick Poor, [45] published in 1892. Whilst the social context and healthcare delivery have developed significantly, the issues identified in this report, including the need for co-ordination between services and unacceptable inequalities, remain as relevant today. The collective body of evidence identified in this review, built up over the last 130 years, has hitherto been poorly documented and characterised. This may in part explain why longstanding issues remain pertinent today.
Education was the most frequently applied type of initiative (26%), with the trend increasing over time. It consistently features as one of the most reported initiatives in the last 15 years. With non-communicable diseases – often referred to as ‘life style choices’ [46, 47]—being such a high proportion (92%) of the subject areas that initiatives were seeking to address, it is perhaps not surprising that education features so strongly. Education initiatives tend to be straightforward to write up and evaluate [48], which lends them towards publication. They are also commonly associated with funding [49] that requires some kind of evaluation or report, which again lends towards publication. However, in our experience, trying to change individual behaviour without changing the system or environment within which people live does not work. The term ‘life style choices’is a misnomer. The reality is that we are strongly influenced by explicit and implicit prompts in our environment and those with the least resources have the least choice and are the most lectured.
Changes to the physical environment is linked with changing the environment within which we live. It was therefore disappointing that these types of initiatives accounted for only 21% (n = 336) of the total. It was also disappointing that only 21 of the 336 reported an outcome measure. These were addressing issues of obesity [50, 51] smoking [52–54] water borne infections [55–57], traffic related accidents and active travel [58–62]. These changes to physical environment were instigated by policy or legal changes in just under half (43%) of the initiatives. In considering the balance between education and system or environmental initiatives, more focus and effort should be on system and environment to ‘make the healthy choice the easy choice’.
Service reform (23% of the total citations) performed best on reporting an outcome measure (n = 34). These ranged from centralising heart attack and stroke services, [63, 64] injection drug user facilities for harm reduction, [65] decentralising and creating networks for care for diabetes [66] and dementia [67] to mass nicotine replacement therapy [32]. Service reform, which is defined as ‘a change or addition to a health service’, is akin to a change to the physical environment or system within which we live. It is also most directly linked to health services. Therefore, service reforms have a direct and clear link to any changes in outcomes. This is not to say the changes are easy or straightforward. Changing any provision of health service, particularly if controversial services or moving services further from a patient’s home, is likely to understandably attract public and political interest. Clinical leadership and genuine public and political engagement are key.
A relatively small number (n = 124) of initiatives described what was believed to be a comprehensive suite of initiatives. City health departments were most notable in leading these in a diverse range of cities including New York City (USA), [68] Geelong (Australia), [69] Barcelona (Spain), [70] Taipei (Tiawan) [71] to Nizwa (Oman) [72]. Coincidently, there were also 124 records that stated an outcome measure. It is striking that although a comprehensive approach only represented 8% of the total, they represent almost a quarter (23%) of the number with an outcome measure. There could be a number of reasons why outcome measures feature strongly when a comprehensive suite of initiatives is undertaken. A range of initiatives addressing the same subject area may be more likely to bring about a change in outcome compared to a single initiative.
City Health Departments are strongly associated with City Mayors. However, of the 1614 citations only 44 (3%) referenced a Mayor as having any kind of role. Considering Mayors are such features of cities, this was surprising. It was also notable, in general, that initiatives across all areas appeared quite piecemeal and carried out in insolation; a single initiative linked to a single health issue or risk factor without reference to a wider strategy, aim or other supporting initiatives. This could simply be a product of the way the papers were written. Indeed, there is a neat simplicity to this approach. However, the reality of the real world is that a single initiative is unlikely to making meaningful and lasting impact on long-standing issues. Cities are a meta-system with population health dictated by multiple interactions and multidirectional feedback loops. A change to one part of the system could both result in multiple unintended consequences or no impact on outcomes at all. Improving health in cities requires multiple actions, by multiple actors, at multiple levels. No single organisation, sector or initiative can solve the complex interlinked issues. The political and system leadership across a collaboration of partners by a Mayor will be crucial. The role and impact of Mayors in city residents’ health would warrant further investigation.
The initiative itself also affected how it was instigated (Table 3). It should be noted that “not stated” featured highly across all groups, ranging up to 54% in education and support and totalling 529 (33%) across all initiatives. Therefore, care should be taken with interpreting this result. The comprehensive initiatives were broadly split one fifth policy, collaboration and city health department, with 20%, 18%, 27%, respectively. Education initiatives were most associated with collaboration (15%), city health department (9%) and policy (6%). Changes made to the physical environment were strongly associated with policy (22%) and law (21%).Digital, IT and data was most commonly instigated by city health departments (21%) (Table 3).
Table 3.
Type of initiative and how it was instigated
| Type of Initiative | # of papers | % | How Intervention Instigated | How Instigated volume | How Instigated percentage | # with outcome measure | Percentage of the total of those with an outcome |
|---|---|---|---|---|---|---|---|
| Comprehensive | 124 | 8% | Policy | 25 | 20.2% | 3 | 2.4% |
| Collaboration | 22 | 17.7% | 1 | 0.8% | |||
| Service Reform | 0 | 0.0% | 0 | 0.0% | |||
| Law (4) | 1 | 0.8% | 1 | 0.8% | |||
| City Health Dept | 34 | 27.4% | 17 | 13.7% | |||
| Fiscal (6) | 0 | 0.0% | 0 | 0.0% | |||
| Research | 1 | 0.8% | 0 | 0.0% | |||
| National or philanthropc | 7 | 5.6% | 0 | 0.0% | |||
| WHO Healthy Cities (9) | 6 | 4.8% | 0 | 0.0% | |||
| WHO | 1 | 0.8% | 0 | 0.0% | |||
| Stanford (11) | 0 | 0.0% | 0 | 0.0% | |||
| Not stated | 27 | 21.8% | 7 | 5.6% | |||
| Education / support program | 414 | 26% | Policy | 26 | 6.3% | 2 | 1.6% |
| Collaboration | 63 | 15.2% | 4 | 3.2% | |||
| Service Reform | 9 | 2.2% | 0 | 0.0% | |||
| Law (4) | 8 | 1.9% | 0 | 0.0% | |||
| City Health Dept | 36 | 8.7% | 2 | 1.6% | |||
| Fiscal (6) | 3 | 0.7% | 4 | 3.2% | |||
| Research | 16 | 3.9% | 0 | 0.0% | |||
| National or philanthropc | 19 | 4.6% | 1 | 0.8% | |||
| WHO Healthy Cities (9) | 3 | 0.7% | 0 | 0.0% | |||
| WHO | 2 | 0.5% | 0 | 0.0% | |||
| Stanford (11) | 7 | 1.7% | 3 | 2.4% | |||
| Not stated | 222 | 53.6% | 14 | 11.3% | |||
| Change to physical environment | 336 | 21% | Policy | 75 | 22.3% | 1 | 0.8% |
| Collaboration | 17 | 5.1% | 1 | 0.8% | |||
| Service Reform | 4 | 1.2% | 1 | 0.8% | |||
| Law (4) | 69 | 20.5% | 4 | 3.2% | |||
| City Health Dept | 27 | 8.0% | 0 | 0.0% | |||
| Fiscal (6) | 16 | 4.8% | 1 | 0.8% | |||
| Research | 8 | 2.4% | 0 | 0.0% | |||
| National or philanthropc | 10 | 3.0% | 2 | 1.6% | |||
| WHO Healthy Cities (9) | 4 | 1.2% | 0 | 0.0% | |||
| WHO | 1 | 0.3% | 0 | 0.0% | |||
| Stanford (11) | 0 | 0.0% | 0 | 0.0% | |||
| Not stated | 105 | 31.3% | 11 | 8.9% | |||
| Service reform | 366 | 23% | Policy | 14 | 3.8% | 0 | 0.0% |
| Collaboration | 47 | 12.8% | 4 | 3.2% | |||
| Service Reform | 228 | 62.3% | 25 | 20.2% | |||
| Law (4) | 7 | 1.9% | 1 | 0.8% | |||
| City Health Dept | 31 | 8.5% | 3 | 2.4% | |||
| Fiscal (6) | 18 | 4.9% | 0 | 0.0% | |||
| Research | 2 | 0.5% | 0 | 0.0% | |||
| National or philanthropc | 19 | 5.2% | 1 | 0.8% | |||
| WHO Healthy Cities (9) | 0 | 0.0% | 0 | 0.0% | |||
| WHO | 0 | 0.0% | 0 | 0.0% | |||
| Stanford (11) | 0 | 0.0% | 0 | 0.0% | |||
| Not stated | 0 | 0.0% | 0 | 0.0% | |||
| Digital / IT / Data | 92 | 6% | Policy | 2 | 2.2% | 0 | 0.0% |
| Collaboration | 5 | 5.4% | 1 | 0.8% | |||
| Service Reform | 6 | 6.5% | 0 | 0.0% | |||
| Law (4) | 0 | 0.0% | 0 | 0.0% | |||
| City Health Dept | 19 | 20.7% | 1 | 0.8% | |||
| Fiscal (6) | 1 | 1.1% | 0 | 0.0% | |||
| Research | 7 | 7.6% | 0 | 0.0% | |||
| National or philanthropc | 4 | 4.3% | 0 | 0.0% | |||
| WHO Healthy Cities (9) | 3 | 3.3% | 0 | 0.0% | |||
| WHO | 0 | 0.0% | 0 | 0.0% | |||
| Stanford (11) | 0 | 0.0% | 0 | 0.0% | |||
| Not stated | 45 | 48.9% | 2 | 1.6% | |||
| Not stated / no intervention | 282 | 17% | Policy | 36 | 12.8% | 2 | 1.6% |
| Collaboration | 27 | 9.6% | 0 | 0.0% | |||
| Service Reform | 0 | 0.0% | 2 | 1.6% | |||
| Law (4) | 6 | 2.1% | 0.0% | ||||
| City Health Dept | 16 | 5.7% | 0 | 0.0% | |||
| Fiscal (6) | 0 | 0.0% | 0 | 0.0% | |||
| Research | 21 | 7.4% | 0 | 0.0% | |||
| National or philanthropc | 9 | 3.2% | 0 | 0.0% | |||
| WHO Healthy Cities (9) | 35 | 12.4% | 0 | 0.0% | |||
| WHO | 2 | 0.7% | 0 | 0.0% | |||
| Stanford (11) | 0 | 0.0% | 0 | 0.0% | |||
| Not stated | 130 | 46.1% | 2 | 1.6% |
Total citations with an outcome measure: 124
The majority of papers were from North America (57% of total, almost double the total of Europe) and in particular New York City which alone accounted for 17% (n = 279) of the total, more than the entire WHO Healthy City output found. It is not clear if this is because New York City is taking significant steps to improve health and healthcare or they are publishing a lot of their work, or both. This features in the bias and limitations identified in the section below. It also highlights the opportunity for further study through a survey of city health departments to get a more complete picture of the initiatives that cities are undertaking to improve population health.
The breadth of subject areas being addressed from a number of different perspectives and the interrelated nature of the subject areas is striking. For example, diet is known to impact on obesity, [73] and cancer [74], and cardiovascular [75] disease. Obesity is known to impact on cancer, [76] cardiovascular, [77] mental health [78] and mental health is known to impact on obesity [79]. Therefore, an initiative to improve diet could be an initiative to address obesity, cancer, cardiovascular disease, mental health or health generally.
The complexity of a range of subject areas being addressed could be simplified when the major causes of chronic diseases are well known. Indeed, the four main risk factors (tobacco use; harmful alcohol use; physical inactivity and unhealthy diet) account for at least 80% of all heart disease, stroke and type 2 diabetes and 40% of cancers [80]. The authors would add a fifth risk factor; planetary health. Planetary health is widely acknowledged to be a significant risk to human health [81–83] particularly impacting cities [84, 85]. The health risk factors are also directly linked to planetary health factors, for example diet [86] and evidence shows polices to promote sustainable food supply can improve personal and planetary health [87]. The authors would call these ‘The Vital 5’. They are the 5 most important health risk factors. These ‘Vital 5’ are most concentrated in deprived areas [88] and show the greatest increase is in low and middle income countries, even faster than has historically occurred in high income countries [89]. Therefore, action on these ‘Vital 5’ will be action on inequalities. Every city should develop a comprehensive strategy and action plan to address these ‘Vital 5’ of tobacco use; harmful alcohol use; physical inactivity, unhealthy diet and planetary health.
The 20th century was defined by breakthroughs in communicable diseases. Communicable diseases are certainly not eradicated; HIV [90–92] and TB [93–95] can still be seen to be particular issues in cities. The Covid-19 pandemic has also disproportionately impacted cities [12]. However, Covid-19 has also reminded us of the importance of these Vital 5. It is known that smoking, [96] alcohol, [97] poor diet, [98] physical inactivity [99] and air quality [100], all contribute to worse outcomes of Covid-19. They also contribute to other factors which have worse outcomes of Covid-19, such as high blood pressure [101] and obesity [102]. Crucially, it is also know that damaging the environment will make future pandemics more likely [103, 104]. If cities were to focus on these Vital 5 they would be improving immediate and long term population health.
This study has several limitations. The deliberate decision was taken to be as broad and inclusive as possible in the papers included. Mays et al. [105] and Strech and Tilburt [106] identify the tension between using only academically rigorous, but therefore less, research and the inclusion of other sources of data, which increase the volume, but that are more susceptible to bias and therefore risk contaminating results. Because of the volume of papers and restrictions on time only, the title and abstract were used in the data extraction. Formal quality assessment of the studies was not undertaken. Only studies in English language were included. A large volume of citations were from one city (New York City) which could introduce bias. Finally, given the heterogeneity of the study designs and data sources, meta-analysis was not undertaken. The authors acknowledge that despite a comprehensive and systematic approach they may have missed relevant documentation.
The authors believe non-communicable diseases will be the issue of the 21st century, accounting for over 40 million annual deaths globally (72% of total deaths) [107]. The Vital 5; tobacco use; harmful alcohol use; physical inactivity, unhealthy diet and planetary health impact on both non-communicable diseases and the likelihood of future communicable pandemics. The progress made in the treatment and prevention of HIV from death sentence 20 years ago to entirely treatable and preventable long-term condition, plus the rapid response to Covid-19 demonstrates what could be achieved to eliminate these ‘Vital 5’ with collective determination and resources. Cities have demonstrated they are well placed to take this action.
Conclusions
This global systematic scoping review provides an overview of the existing evidence of city initiatives to improve health and healthcare. Based on the findings, a summary of key findings and recommended policy actions is provided below. This, with the excel file with the 1614 records and associated extracted data (Additional file 2), will be a useful resource for academics and policy makers interested in improving urban health. The outputs of this systematic scoping review can be used to inform urban health policy for the next decade and shape future research. The role of Mayors and the real world understanding of the initiatives that city health departments are undertaking to improve population health warrants particular attention.
Key findings and recommended policy actions:
Key Finding: There is a large range of health issues and risk factors being addressed from a large number of perspectives. The overwhelming majority of the issues and initiative are addressing ‘non-communicable disease’ risk factors that are interrelated and overlapping.
Recommended Policy Action: The same level of ambition that was applied to HIV and Covid-19 should be applied to the ‘Vital 5’ risk factors; smoking, alcohol, physical inactivity, unhealthy diet and planetary health.
Key Finding: Education was the most commonly reported initiative.
Recommended Policy Action: The term ‘lifestyle choices’ is a misnomer. More focus and resource should be put on system and environmental changes to ‘make the healthy choice the easiest choice’
Key Finding: City health departments are making an increasing contribution in improving city population health.
Recommended Policy Action: Cities should collaborate and share learning in real world experience of initiatives to improve urban health.
Key Finding: The contribution of Mayors in improving health and healthcare appears to be limited
Recommended Policy Action: The role and impact of Mayors in city populations would warrant further study
Key Finding: New York City stands out with nearly one fifth (18%) of the total citations.
Recommended Policy Action: Further real world research to understand and get a comprehensive view on what cities are doing to improve population health would be of value.
Supplementary Information
Additional file 1. Database Search Strings.
Acknowledgements
We would like to thank the members of the Healthy London Partnership (HLP)* that helped on providing a second review of titles and abstracts. These were: Patrice Donnelly, Pascale Montiel, Emily Treder, Natalia Proctor, Sarah Bowker, Claire Ruiz, Lauren Walker, Dominic Jones, Suzi Griffiths, Steve Solasta, Jess Simpson, Raman Patria, David Groom, Emile Radyte, Amy Bowkett, Helen Daly, Jess Drummond, Gabriella Baker, Martina Dalton, Andrea Priest, Tanmay Kale, Lise Hansen and Katie Horrell.
Abbreviations
- Covid-19
Coronavirus disease 2019
- PRISMA
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- PROSPERO
International prospective register of systematic reviews
- HLP
Healthy London Partnership.
- HIV
Human immunodeficiency virus
- TB
Tuberculosis
- WHO
World Health Organisation
- IT
Information Technology
Authors’ contributions
Conception or design of the research: SD. Data collection: SD. Data analysis and interpretation: SD, HA, AD. Drafting the article: SD, HA. Critical revision of the article: SD, HA, AD. All authors read and approved final manuscript.
Authors’ information
SD is Director of Population Health and Equality at Kings Health Partners and South East London Integrated Care System. He has led transformation of health and healthcare across London for over 13 years. HA is Chief Scientific Advisor at the Institute of Global Health Innovation (Imperial College London) and has led and supervised multiple research projects. AD is the Co-director at the Institute of Global Health Innovation Imperial College London. He has led many city and national reviews of health and health care.
Funding
This manuscript received no specific funding. Infrastructure support for this research was provided by the NIHR Imperial Biomedical Research Centre (BRC).
Availability of data and materials
The data generated from this review is provided in the supplementary information files.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
AD is Chair and HA the Chief Scientific Officer of the Health Security Initiative at Flagship Pioneering UK Ltd. SD has no competing interests to declare.
Footnotes
See acknowledgements for full list.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.United Nations. 2018 Revision of World Urbanization Prospects 2018 [Available from: https://www.un.org/development/desa/publications/2018-revision-of-world-urbanization-prospects.html.
- 2.United Nations. Department of Economic and Social Affairs, Population Division (2018). The World’s Cities in 2018—Data Booklet (ST/ESA/ SER.A/417). 2018. p. 2. https://www.un.org/en/development/desa/population/publications/pdf/urbanization/the_worlds_cities_in_2018_data_booklet.pdf.
- 3.Satterthwaite D. Will most people live in cities? BMJ (Clinical Res Ed) 2000;321(7269):1143–1145. doi: 10.1136/bmj.321.7269.1143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hawkins A. The grey wall of China: inside the world's concrete superpower. The Guardian. 2019;2019:28. [Google Scholar]
- 5.Ellis LD, Badel AF, Chiang ML, Park RJY, Chiang YM. Toward electrochemical synthesis of cement—An electrolyzer-based process for decarbonating CaCO3 while producing useful gas streams. Proc Natl Acad Sci. 2020;117(23):12584–91. doi: 10.1073/pnas.1821673116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ezzati M, Webster CJ, Doyle YG, Rashid S, Owusu G, Leung GM. Cities for global health. BMJ. 2018;363:k3794. doi: 10.1136/bmj.k3794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Vlahov D, Fraudenberg N, Proietti F, Ompad D, Quinn A, Nandi V, Galea S. Urban as a determinant of health. J Urban Health. 2007;84(SUPPL.1):i16–i26. doi: 10.1007/s11524-007-9169-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dodman D. Blaming cities for climate change? An analysis of urban greenhouse gas emissions inventories. Environ Urban. 2009;21(1):185–201. doi: 10.1177/0956247809103016. [DOI] [Google Scholar]
- 9.Montgomery C. Happy City: Transforming Our Lives Through Urban Design. Kindle. New York: Penguin; 2013. [Google Scholar]
- 10.Sureda X, Villalbí JR, Espelt A, Franco M. Living under the influence: normalisation of alcohol consumption in our cities. Gac Sanit. 2017;31(1):66–68. doi: 10.1016/j.gaceta.2016.07.018. [DOI] [PubMed] [Google Scholar]
- 11.Kuddus MA, Tynan E, McBryde E. Urbanization: a problem for the rich and the poor? Public Health Rev. 2020;41(1):1. doi: 10.1186/s40985-019-0116-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.United Nations. Policy Brief: COVID-19 in an Urban World 2020 [Available from: https://www.un.org/sites/un2.un.org/files/sg_policy_brief_covid_urban_world_july_2020.pdf.
- 13.Colenbrander S. Cities as engines of economic growth The case for providing basic infrastructure and services in urban areas 2016 [Available from: https://pubs.iied.org/sites/default/files/pdfs/migrate/10801IIED.pdf.
- 14.Dye C. Health and urban living. Science. 2008;319(5864):766–769. doi: 10.1126/science.1150198. [DOI] [PubMed] [Google Scholar]
- 15.Lancet T. A commission on climate change. The Lancet. 2009;373(9676):1659. doi: 10.1016/S0140-6736(09)60922-3. [DOI] [PubMed] [Google Scholar]
- 16.Wight J, Middleton J. Climate change: the greatest public health threat of the century. BMJ. 2019;365:l2371. doi: 10.1136/bmj.l2371. [DOI] [PubMed] [Google Scholar]
- 17.Watts N, Adger WN, Agnolucci P, Blackstock J, Byass P, Cai W, et al. Health and climate change: policy responses to protect public health. The Lancet. 2015;386(10006):1861–1914. doi: 10.1016/S0140-6736(15)60854-6. [DOI] [PubMed] [Google Scholar]
- 18.Watts N, Amann M, Arnell N, Ayeb-Karlsson S, Belesova K, Boykoff M, et al. The 2019 report of the lancet countdown on health and climate change: ensuring that the health of a child born today is not defined by a changing climate. The Lancet. 1836;2019:394. doi: 10.1016/S0140-6736(19)32596-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Robertson D. Inside Copenhagen’s race to be the first carbon-neutral city. The Guardian. 2019. https://www.theguardian.com/cities/2019/oct/11/inside-copenhagens-race-to-be-the-first-carbon-neutral-city. Accessed 17 June 2021.
- 20.Naylor C, Buck D. The role of cities in improving population health: international insights: Kings Fund; 2018 [Available from: https://www.kingsfund.org.uk/sites/default/files/2018-06/Role_cities_population_health_Kings_Fund_June_2018_0.pdf.
- 21.Davies SC. Annual report of the chief medical officer 2019 [Available from: https://www.gov.uk/government/publications/chief-medical-officer-annual-report-2019-partnering-for-progress. [DOI] [PubMed]
- 22.Danielli S, Coffey T, Ashrafian H, Darzi A. Systematic review into city interventions to address obesity. EClinicalMedicine. 2021;32:100710. doi: 10.1016/j.eclinm.2020.100710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Diller P. Why do Cities innovate in public health? Implications of scale and structure 2014 [Available from: https://openscholarship.wustl.edu/cgi/viewcontent.cgi?referer=&httpsredir=1&article=6092&context=law_lawreview.
- 24.Barber B. If Mayors Ruled the World. Connecticut: Yale University Press; Reprint edition (September 30, 2014); 2014.
- 25.Hoornweg D, Pope K. Population predictions for the world’s largest cities in the 21st century. Environ Urban. 2016;29(1):195–216. doi: 10.1177/0956247816663557. [DOI] [Google Scholar]
- 26.Theis D, White M. Is obesity policy in England fit for purpose? Analysis of government strategies and policies, 1992–2020. Milbank Q. 2021;99(1):126–170. doi: 10.1111/1468-0009.12498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Frenk J. Health and the economy. Harvard Int Rev. 2014;35(4):62–64. [Google Scholar]
- 28.Tricco AC, Lillie E, Zarin W, O'Brien KK, Colquhoun H, Levac D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169(7):467–473. doi: 10.7326/M18-0850. [DOI] [PubMed] [Google Scholar]
- 29.Moher D, Liberati A, Tetzlaff J, Altman DG, Group P Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097-e. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.World Statistics Organisation. Population of Localities 2018 [Available from: https://world-statistics.org/index-pop.php.
- 31.Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101. doi: 10.1191/1478088706qp063oa. [DOI] [Google Scholar]
- 32.Miller N, Frieden ThomasR, Liu SzeYan, Matte ThomasD, Mastashari Farzad, Deitcher DeborahR, Cummings K, Chang Christina, Bauer Ursula, Bassett MaryT. Effectiveness of a large-scale distribution programme of free nicotine patches: A prospective evaluation. The Lancet. 2005;365(9474):1849–54. doi: 10.1016/S0140-6736(05)66615-9. [DOI] [PubMed] [Google Scholar]
- 33.Peñalvo JL, Sotos-Prieto M, Santos-Beneit G, Pocock S, Redondo J, Fuster V. The program SI! intervention for enhancing a healthy lifestyle in preschoolers: first results from a cluster randomized trial. BMC Public Health. 2013;13(1):1. doi: 10.1186/1471-2458-13-1208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Tsung-Mei C. Explaining Shanghai’s health care reforms, successes and challenges. Health Affairs. 2013;32(12):2199–205. doi: 10.1377/hlthaff.2013.1136. [DOI] [PubMed] [Google Scholar]
- 35.Sturm R, Cohen DA. Zoning For Health? The Year-Old Ban On New Fast-Food Restaurants In South LA. Health Affairs. 2009;28:w1088-NaN. doi: 10.1377/hlthaff.28.6.w1088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Whitelaw N, Warden G, Wenzler MR. Current efforts toward implementation of an urban health strategy: The Henry Ford Health System. J Urban Health. 1998;75(2):356–66. doi: 10.1007/BF02345103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Yen MY, Wu TSJ, Chiu AWH, Wong WW, Wang PE, Chan TC, King CC. Taipei's use of a multi-channel mass risk communication program to rapidly reverse an epidemic of highly communicable disease. PLoS ONE. 2009;4(11):e7962. doi: 10.1371/journal.pone.0007962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Tran AD. Addressing eating habits through food label education in Stevenson, WA. J Investig Med. 2010;58(1):204. [Google Scholar]
- 39.Feyerherm L, Tibbits M, Wang H, Schram S, Balluff M. Partners for a healthy city: implementing policies and environmental changes within organizations to promote health. Am J Public Health. 2014;104(7):1165–8. [DOI] [PMC free article] [PubMed]
- 40.Sacks RY, S. S.; Nonas, C. Increasing access to fruits and vegetables: perspectives from the New York City experience. American journal of public health. 2015;105(5):e29-e37. [DOI] [PMC free article] [PubMed]
- 41.Duncan BR. New healthcare model: Citywide care management. Otolaryngol - Head Neck Surg (United States) 2012;147:P125. [Google Scholar]
- 42.Coady MH, Chan CA, Auer K, Farley SM, Kilgore EA, Kansagra SM. Awareness and impact of New York City's graphic point-of-sale tobacco health warning signs. Tobacco Control. 2012. [DOI] [PubMed]
- 43.Weinstein I. Eighty years of public health in New York City. Bull N Y Acad Med. 1947;23(4):221–237. [PMC free article] [PubMed] [Google Scholar]
- 44.de Salazar L. Linking public health surveillance systems to program effectiveness evaluation. Colombia Medica. 2011;42(3):342–351. doi: 10.25100/cm.v42i3.881. [DOI] [Google Scholar]
- 45.House of Lords. Third report of the select committee of the house of lords on metropolitan hospitals. The Lancet. 1892;140(3592):49–52. https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(01)97445-8/fulltext. (Kings Fund library on 16 November 2022).
- 46.Kickbusch I, Allen L, Franz C. The commercial determinants of health. Lancet Glob Health. 2016;4(12):e895–e896. doi: 10.1016/S2214-109X(16)30217-0. [DOI] [PubMed] [Google Scholar]
- 47.Wainwright NWJ, Surtees PG, Welch AA, Luben RN, Khaw K-T, Bingham SA. Healthy lifestyle choices: could sense of coherence aid health promotion? J Epidemiol Community Health. 2007;61(10):871–876. doi: 10.1136/jech.2006.056275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Nana-Goar Pogosova NE, A.; Ausheva, A. Evaluation of the efficacy of cardiovascular prevention in the framework of the World Heart Day. European Journal of Preventive Cardiology. 2015 (1);S115.
- 49.Taing D, McKay K. Better Strength, Better Balance! Partnering to deliver a fall prevention program for older adults. Can J Public Health. 2017;108(3):e314-e319. 10.17269/CJPH.108.5901. [DOI] [PMC free article] [PubMed]
- 50.Economos CDH, R. R.; Must, A.; Goldberg, J. P.; Kuder, J.; Naumova, E. N.; Collins, J. J.; Nelson, M. E. Shape Up Somerville two-year results: A community-based environmental change intervention sustains weight reduction in children. Preventive medicine. 2013; 57(4):[322–7 pp.]. Available from: http://onlinelibrary.wiley.com/o/cochrane/clcentral/articles/426/CN-00910426/frame.html; http://ac.els-cdn.com/S009174351300193X/1-s2.0-S009174351300193X-main.pdf?_tid=b201df18-cfe8-11e5-9735-00000aab0f6c&acdnat=1455103583_2cfe0f0018bc97c80ed35598a603b6cf. [DOI] [PubMed]
- 51.Sekhobo J, Edmunds L, Dalenius K, Jernigan J, Davis C, Giddings M, et al. Neighborhood disparities in prevalence of childhood obesity among low-income children before and after implementation of New York City child care regulations. Prev Chronic Dis. 2014;11:E181. doi: 10.5888/pcd11.140152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Page RL, Slejko JF, Libby AM. A citywide smoking ban reduced maternal smoking and risk for preterm births: a colorado natural experiment. J Women’s Health. 2012;21(6):621–7. doi: 10.1089/jwh.2011.3305. [DOI] [PubMed] [Google Scholar]
- 53.Cesaroni G, Forastiere F, Agabiti N, Valente P, Zuccaro P, Perucci CA. Effect of the Italian smoking ban on population rates of acute coronary events. Circulation. 2008;117(9):1183–8. doi: 10.1161/CIRCULATIONAHA.107.729889. [DOI] [PubMed] [Google Scholar]
- 54.Bartecchi C, Alsever RN, Nevin-Woods C, Thomas WM, Estacio RO, Bartelson BB, Krantz MJ. Reduction in the incidence of acute myocardial infarction associated with a citywide smoking ordinance. Circulation. 2006;114(14):1490–6. doi: 10.1161/CIRCULATIONAHA.106.615245. [DOI] [PubMed] [Google Scholar]
- 55.Barreto ML, Genser B, Strina A, Teixeira MG, Assis AMO, Rego RF, Teles CA, Prado MS, Matos SM, Santos DN, dos Santos LA, Cairncross S. Effect of city wide sanitation programme on reduction in rate of childhood diarrhoea in northeast Brazil: assessment by two cohort studies. Lancet. 2007;370(9599):1622–8. doi: 10.1016/S0140-6736(07)61638-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Cutler D, Miller G. The role of public health improvements in health advances: the twentieth-century United States. Demography. 2005;42(1):1–22. doi: 10.1353/dem.2005.0002. [DOI] [PubMed] [Google Scholar]
- 57.Ogasawara K, Shirota S, Kobayashi G. Public health improvements and mortality in interwar Tokyo: a Bayesian disease mapping approach. Cliometrica. 2018;12(1):1–31. doi: 10.1007/s11698-016-0148-3. [DOI] [Google Scholar]
- 58.Huitema BE, Van Houten R, Manal H. Time-series intervention analysis of pedestrian countdown timer effects. Accident Analys Prev. 2014;72:23–31. doi: 10.1016/j.aap.2014.05.025. [DOI] [PubMed] [Google Scholar]
- 59.Muennig PA, Epstein M, Li G, DiMaggio C. The cost-effectiveness of New York City's safe routes to school program. Am J Public Health. 2014;104(7):1294–9. doi: 10.2105/AJPH.2014.301868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Rojas-Rueda D, de Nazelle Audrey, Tainio Marko, Nieuwenhuijsen MarkJ. The health risks and benefits of cycling in urban environments compared with car use: health impact assessment study. BMJ: Brit Med J. 2011;343(7819):1–8. doi: 10.1136/bmj.d4521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Tapia V, Carbajal L, Vásquez V, Espinoza R, Vásquez-Velásquez C, Steenland K, et al. Traffic regulation and environmental pollution by particulate material (2.5 and 10), sulfur dioxide, and nitrogen dioxide in Metropolitan Lima, Peru. Rev Peru Med Exp Salud Publica. 2018;35(2):190–7. doi: 10.17843/rpmesp.2018.352.3250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Nieuwenhuijsen MJ, Khreis H. Car free cities: pathway to healthy urban living. Environ Int. 2016;94:251–262. doi: 10.1016/j.envint.2016.05.032. [DOI] [PubMed] [Google Scholar]
- 63.Marcolino M, Brant LC, de Guimaraes C, de Araujo JG, Nascimento BR, Castro LR, Martins P, Lodi-Junqueira L, Ribeiro AL. The implementation of the myocardial infarction system of care in a large city in Brazil. Global Heart. 2014;9(1):193. doi: 10.1016/j.gheart.2014.03.1918. [DOI] [Google Scholar]
- 64.Hunter RM, Davie C, Rudd A, Thompson A, Walker H, Thomson N, Mountford J, Schwamm L, Deanfield J, Thompson K, Dewan B, Mistry M, Quoraishi S, Morris S. Impact on clinical and cost outcomes of a centralized approach to acute stroke care in London: a comparative effectiveness before and after model. PLoS ONE. 2013;8(8):e70420. doi: 10.1371/journal.pone.0070420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Jozaghi EA, Martin A. Should North America's first and only supervised injection facility (InSite) be expanded in British Columbia, Canada? Harm Reduct J. 2013;10:1. doi: 10.1186/1477-7517-10-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Rea RLJ, Gregory S, Prescott D, Gray T, Warren A, Hannah J, Langeland L, Dhindsa P, Tan G. First diabetes: A successful integrated healthcare partnership for diabetes patients in Derby. Diab Med. 2012;29:94. [Google Scholar]
- 67.Tanaka M. Medical care networks for dementia patients. Jap Med Assoc J. 2013;56(4):240–245. [Google Scholar]
- 68.Ong PLG, Demmer R. Evaluating the influence of bloomberg era policy on New York city cardiovascular disease mortality rates. Circulation Conference: American Heart Association's Epidemiology and Prevention/Lifestyle and Cardiometabolic Health. 2015;131(Suppl_1):(Supplement 1):AMP08.
- 69.Foulkes C. Lessons from healthy together geelong: Delivering systems change at scale across two levels of government. Obes Res Clin Pract. 2014;8:33. [Google Scholar]
- 70.Roset-Elias MA, Cardena-Franquet E, Puigdueta-Lucas I, Obea-Maso M. What a city council can do to improve the quality of life in the elderly? Ann Nutr Metab. 1846;2013:63. [Google Scholar]
- 71.Yu LH. Cancer prevention and therapy in Taipei city. Int J Urol. 2010;17:A17–A18. [Google Scholar]
- 72.Alanqoudi Z, Alhinai S. Nizwa healthy lifestyle project evaluation report 2010. 2010. https://www.emro.who.int/health-education/physical-activity-case-studies/the-nizwa-healthy-lifestyles-project-oman.html. Accessed 10 Apr 2021.
- 73.Cecchini M, Sassi F, Lauer JA, Lee YY, Guajardo-Barron V, Chisholm D. Tackling of unhealthy diets, physical inactivity, and obesity: health effects and cost-effectiveness. The Lancet. 2010;376(9754):1775–1784. doi: 10.1016/S0140-6736(10)61514-0. [DOI] [PubMed] [Google Scholar]
- 74.Key TJ, Bradbury KE, Perez-Cornago A, Sinha R, Tsilidis KK, Tsugane S. Diet, nutrition, and cancer risk: what do we know and what is the way forward? BMJ. 2020;368:m511. doi: 10.1136/bmj.m511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Afshin A, Sur PJ, Fay KA, Cornaby L, Ferrara G, Salama JS, et al. Health effects of dietary risks in 195 countries, 1990–2017: a systematic analysis for the global burden of disease study 2017. The Lancet. 2019;393(10184):1958–1972. doi: 10.1016/S0140-6736(19)30041-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Lancet T. The link between cancer and obesity. The Lancet. 2017;390(10104):1716. doi: 10.1016/S0140-6736(17)32659-4. [DOI] [PubMed] [Google Scholar]
- 77.Carbone S, Canada JM, Billingsley HE, Siddiqui MS, Elagizi A, Lavie CJ. Obesity paradox in cardiovascular disease: where do we stand? Vascular Health Risk Management. 2019;15:89–100. doi: 10.2147/VHRM.S168946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Sarwer DB, Polonsky HM. The Psychosocial Burden of obesity. Endocrinol Metab Clin North Am. 2016;45(3):677–688. doi: 10.1016/j.ecl.2016.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Kivimäki M, Lawlor DA, Singh-Manoux A, Batty GD, Ferrie JE, Shipley MJ, et al. Common mental disorder and obesity: insight from four repeat measures over 19 years: prospective Whitehall II cohort study. BMJ. 2009;339:b3765. doi: 10.1136/bmj.b3765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.World Health Organization . Preventing chronic diseases : a vital investment : WHO global report. Geneva: World Health Organization; 2005. [Google Scholar]
- 81.Sheffield PE, Herrera M, Kinnee EJ, Clougherty JE. Not so little differences: variation in hot weather risk to young children in New York City. Public Health. 2018;161:119–126. doi: 10.1016/j.puhe.2018.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Sewe MO, Bunker A, Ingole V, Egondi T, Åström DO, Hondula DM, et al. Estimated effect of temperature on years of life lost: A retrospective time-series study of low-, middle-, and high-income regions. Environ Health Perspect. 2018;126(1):017004. doi: 10.1289/EHP1745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Frumkin H, Haines A. Global environmental change and noncommunicable disease risks. Annu Rev Public Health. 2019;40(1):261–282. doi: 10.1146/annurev-publhealth-040218-043706. [DOI] [PubMed] [Google Scholar]
- 84.Rosenthal JK, Sclar ED, Kinney PL, Knowlton K, Crauderueff R, Brandt-Rauf PW. Links between the built environment, climate and population health: interdisciplinary environmental change research in New York City. Ann Acad Med Singap. 2007;36(10):834–846. doi: 10.47102/annals-acadmedsg.V36N10p834. [DOI] [PubMed] [Google Scholar]
- 85.Xiong X, Zhang L, Hao Y, Zhang P, Chang Y, Liu G. Urban dietary changes and linked carbon footprint in China: a case study of Beijing. J Environ Manage. 2020;255:109877. doi: 10.1016/j.jenvman.2019.109877. [DOI] [PubMed] [Google Scholar]
- 86.Swinburn BA, Kraak VI, Allender S, Atkins VJ, Baker PI, Bogard JR, et al. The global syndemic of obesity, undernutrition, and climate change: the lancet commission report. Lancet. 2019;393(10173):791–846. doi: 10.1016/S0140-6736(18)32822-8. [DOI] [PubMed] [Google Scholar]
- 87.Willett W, Rockström J, Loken B, Springmann M, Lang T, Vermeulen S, et al. Food in the anthropocene: the EAT–<em>Lancet</em> commission on healthy diets from sustainable food systems. The Lancet. 2019;393(10170):447–492. doi: 10.1016/S0140-6736(18)31788-4. [DOI] [PubMed] [Google Scholar]
- 88.Macdonald L, Olsen JR, Shortt NK, Ellaway A. Do ‘environmental bads’ such as alcohol, fast food, tobacco, and gambling outlets cluster and co-locate in more deprived areas in Glasgow City, Scotland? Health Place. 2018;51:224–231. doi: 10.1016/j.healthplace.2018.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Stuckler D, McKee M, Ebrahim S, Basu S. Manufacturing epidemics: the role of global producers in increased consumption of unhealthy commodities including processed foods, alcohol, and tobacco. PLoS Med. 2012;9(6):e1001235. doi: 10.1371/journal.pmed.1001235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Fisher HH, Hoyte T, Purcell DW, van Handel M, Williams W, Krueger A, Dietz P, Stratford D, Heitgerd J, Dunbar E, Wan C, Linley LA, Flores SA. Health department HIV prevention programs that support the national HIV/AIDS strategy: The enhanced comprehensive HIV prevention planning project, 2010–2013. Public Health Reports. 2016;131(1):185–94. doi: 10.1177/003335491613100126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Evans C, Suggs LS, Turner K, Occa A, Juma A, Blake H. Mobile phone messaging to promote uptake of HIV testing among migrant African communities in the UK. Health Educ J. 2018;78(1):24–37. doi: 10.1177/0017896918785928. [DOI] [Google Scholar]
- 92.Ard KL, Edelstein ZR, Bolduc P, Daskalakis D, Gandhi AD, Krakower DS, et al. Public health detailing for human immunodeficiency virus pre-exposure prophylaxis. Clin Infect Dis. 2019;68(5):860–864. doi: 10.1093/cid/ciy573. [DOI] [PubMed] [Google Scholar]
- 93.Lam CK, McGinnis Pilote K, Haque A, Burzynski J, Chuck C, Macaraig M. Using video technology to increase treatment completion for patients with latent tuberculosis infection on 3-month isoniazid and rifapentine: an implementation study. J Med Internet Res. 2018;20(11):e287. doi: 10.2196/jmir.9825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Qader G, Hamim A, Sayedi M, Rashidi M, Manzoor L, Seddiq MK, et al. Addressing tuberculosis control in fragile states: Urban DOTS experience in Kabul, Afghanistan, 2009–2015. PLoS ONE. 2017;12(5):e0178053. doi: 10.1371/journal.pone.0178053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Tabuchi T, Takatorige T, Hirayama Y, Nakata N, Harihara S, Shimouchi A, et al. Tuberculosis infection among homeless persons and caregivers in a high-tuberculosis-prevalence area in Japan: a cross-sectional study. BMC Infect Dis. 2011;11(1):22. doi: 10.1186/1471-2334-11-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Patanavanich R, Glantz SA. Smoking is associated with worse outcomes of COVID-19 particularly among younger adults: a systematic review and meta-analysis. BMC Public Health. 2021;21(1):1554. doi: 10.1186/s12889-021-11579-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Finlay I, Gilmore I. Covid-19 and alcohol—a dangerous cocktail. BMJ. 2020;369:m1987. doi: 10.1136/bmj.m1987. [DOI] [PubMed] [Google Scholar]
- 98.Butler MJ, Barrientos RM. The impact of nutrition on COVID-19 susceptibility and long-term consequences. Brain Behav Immun. 2020;87:53–54. doi: 10.1016/j.bbi.2020.04.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Sallis R, Young DR, Tartof SY, Sallis JF, Sall J, Li Q, et al. Physical inactivity is associated with a higher risk for severe COVID-19 outcomes: a study in 48 440 adult patients. Br J Sports Med. 2021;55(19):1099–1105. doi: 10.1136/bjsports-2021-104080. [DOI] [PubMed] [Google Scholar]
- 100.Travaglio M, Yu Y, Popovic R, Selley L, Leal NS, Martins LM. Links between air pollution and COVID-19 in England. Environ Pollut. 2021;268:115859. doi: 10.1016/j.envpol.2020.115859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Clark CE, McDonagh STJ, McManus RJ, Martin U. COVID-19 and hypertension: risks and management. A scientific statement on behalf of the British and Irish hypertension society. J Human Hyper. 2021;35(4):304–7. doi: 10.1038/s41371-020-00451-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Gao M, Piernas C, Astbury NM, Hippisley-Cox J, O'Rahilly S, Aveyard P, et al. Associations between body-mass index and COVID-19 severity in 6·9 million people in England: a prospective, community-based, cohort study. Lancet Diabetes Endocrinol. 2021;9(6):350–359. doi: 10.1016/S2213-8587(21)00089-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Gibb R, Redding DW, Chin KQ, Donnelly CA, Blackburn TM, Newbold T, et al. Zoonotic host diversity increases in human-dominated ecosystems. Nature. 2020;584(7821):398–402. doi: 10.1038/s41586-020-2562-8. [DOI] [PubMed] [Google Scholar]
- 104.Broom D. This is how we prevent future pandemics, say 22 leading scientists: World Economic Forum; 2020 [Available from: https://www.weforum.org/agenda/2020/11/covid-19-pandemics-nature-scientists/?utm_source=sfmc&utm_medium=email&utm_campaign=2737721_Agenda_weekly-4December2020&utm_term=&emailType=Newsletter.
- 105.Mays N, Pope C, Popay J. Systematically reviewing qualitative and quantitative evidence to inform management and policy-making in the health field. J Health Serv Res Policy. 2005;10(Suppl 1):6–20. doi: 10.1258/1355819054308576. [DOI] [PubMed] [Google Scholar]
- 106.Strech D, Tilburt J. Value judgments in the analysis and synthesis of evidence. J Clin Epidemiol. 2008;61(6):521–524. doi: 10.1016/j.jclinepi.2008.01.001. [DOI] [PubMed] [Google Scholar]
- 107.Healthier Societies for Healthy Populations Group Healthier societies for healthy populations. The Lancet. 2020;395(10239):1747–1749. doi: 10.1016/S0140-6736(20)31039-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1. Database Search Strings.
Data Availability Statement
The data generated from this review is provided in the supplementary information files.