Abstract
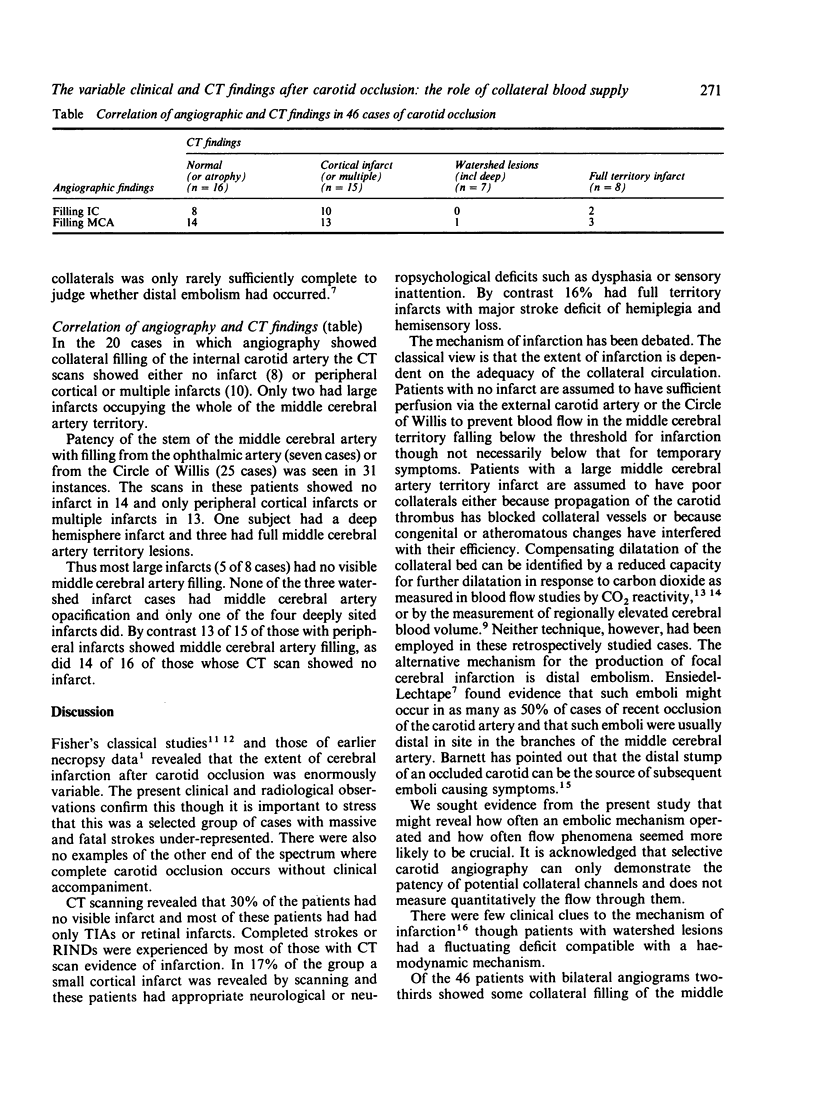
A retrospective review of 61 cases of angiographically confirmed occlusion of one or both carotid arteries was carried out to look at the evidence that the presence of collateral blood supply influenced the extent and type of cerebral infarction. Forty six patients had bilateral angiography from which it was possible to assess collateral filling of the internal carotid and middle cerebral arteries. As expected, patients with no CT scan evidence of infarction more frequently had transient ischaemic attacks or retinal infarcts than did those with visible cerebral infarcts. Patients with small cortical ischaemic lesions usually had appropriate neuropsychological or neurological deficits. Three patients with cortical watershed infarcts had a fluctuating deficit. Of the patients with bilateral angiograms 67% showed some filling via collaterals of the middle cerebral artery, and 43% of the internal carotid artery in the siphon. Those with collateral filling were mostly found to have normal CT scans or evidence of peripheral cortical lesions. By contrast most watershed and full territory infarcts were found in individuals whose angiograms showed no collateral filling. It is suggested that in many cases infarction occurs despite collateral flow and is due to distal embolism and that this may be relevant to the recently reported failure of the EC/IC bypass operation.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Barnett H. J., Peerless S. J., Kaufmann J. C. "Stump" on internal carotid artery--a source for further cerebral embolic ischemia. Stroke. 1978 Sep-Oct;9(5):448–456. doi: 10.1161/01.str.9.5.448. [DOI] [PubMed] [Google Scholar]
- Brown M. M., Wade J. P., Bishop C. C., Russell R. W. Reactivity of the cerebral circulation in patients with carotid occlusion. J Neurol Neurosurg Psychiatry. 1986 Aug;49(8):899–904. doi: 10.1136/jnnp.49.8.899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Castaigne P., Lhermitte F., Gautier J. C., Escourolle R., Derouesné C. Internal carotid artery occlusion. A study of 61 instances in 50 patients with post-mortem data. Brain. 1970;93(2):231–258. doi: 10.1093/brain/93.2.231. [DOI] [PubMed] [Google Scholar]
- FISHER M. Occlusion of the carotid arteries: further experiences. AMA Arch Neurol Psychiatry. 1954 Aug;72(2):187–204. doi: 10.1001/archneurpsyc.1954.02330020055006. [DOI] [PubMed] [Google Scholar]
- FISHER M. Occlusion of the internal carotid artery. AMA Arch Neurol Psychiatry. 1951 Mar;65(3):346–377. doi: 10.1001/archneurpsyc.1951.02320030083009. [DOI] [PubMed] [Google Scholar]
- Mitchinson M. J. The hypotensive stroke. Lancet. 1980 Feb 2;1(8162):244–246. doi: 10.1016/s0140-6736(80)90728-x. [DOI] [PubMed] [Google Scholar]
- Norrving B., Nilsson B., Risberg J. rCBF in patients with carotid occlusion. Resting and hypercapnic flow related to collateral pattern. Stroke. 1982 Mar-Apr;13(2):155–162. doi: 10.1161/01.str.13.2.155. [DOI] [PubMed] [Google Scholar]
- Powers W. J., Press G. A., Grubb R. L., Jr, Gado M., Raichle M. E. The effect of hemodynamically significant carotid artery disease on the hemodynamic status of the cerebral circulation. Ann Intern Med. 1987 Jan;106(1):27–34. doi: 10.7326/0003-4819-106-1-27. [DOI] [PubMed] [Google Scholar]
- Ringelstein E. B., Zeumer H., Angelou D. The pathogenesis of strokes from internal carotid artery occlusion. Diagnostic and therapeutical implications. Stroke. 1983 Nov-Dec;14(6):867–875. doi: 10.1161/01.str.14.6.867. [DOI] [PubMed] [Google Scholar]
- Rodda R. A. The arterial patterns associated with internal carotid disease and cerebral infarcts. Stroke. 1986 Jan-Feb;17(1):69–75. doi: 10.1161/01.str.17.1.69. [DOI] [PubMed] [Google Scholar]
- WIENER L. M., BERRY R. G., KUNDIN J. INTRACRANIAL CIRCULATION IN CAROTID OCCLUSION. Arch Neurol. 1964 Nov;11:554–561. doi: 10.1001/archneur.1964.00460230104011. [DOI] [PubMed] [Google Scholar]
- Zulch K. J., Gessaga E. Infarcts in the carotid system. Vasc Surg. 1972 May-Jun;6(3):114–119. doi: 10.1177/153857447200600302. [DOI] [PubMed] [Google Scholar]


