Abstract
Health systems responses to covid-19 can help to identify factors within and outside of the health system that affect its resilience to shocks, suggest Anna Sagan and colleagues
Health systems must constantly prepare for crises that threaten their operations. These include shocks that arise rapidly and are largely unforeseen, like pandemics or extreme weather events.1 Other types of shocks can arise more insidiously, such as the strains created by prolonged austerity or ageing populations. Yet as covid-19 showed, when a shock arrives, health systems are often unprepared.
The concept of resilience has often been invoked in discussions of health system preparedness and response to crises. However, with this increased interest comes confusion about what health system resilience actually is and how it can be applied and measured to decide if a health system is resilient.2 While it is difficult to agree a comprehensive measure of resilience, valuable insights can be gained by looking at how well health systems performed during covid-19 to help prepare for future shocks.2
What is health system resilience?
Put simply, something is resilient if it can, at least, recover rapidly after being exposed to a shock. However, in the case of a health system that can learn from experience we would hope that it does more than bounce back, especially if its original state could be improved. This learning is dynamic and often unpredictable, reflecting the multiplicity of actors and the complexity of power structures, processes, and feedback loops within the health system.3 Therefore a health system should not just react but also reflect and act, both during a shock and in its aftermath, to enhance its preparedness for any future shocks and ideally improve on how it was before. This points to a need to consider three phases in a health system response: absorption of a shock, adaptation to it, and transformation to strengthen the health system. Understood this way, resilience is a dynamic property of a health system that changes over time, sometimes rapidly, rather than being a constant state.
Challenges to measuring the resilience of health systems
Quantifying health system resilience to a shock is therefore challenging (box 1). To start with, deciding which indicators to measure resilience is not easy because there are different measures of success and what is considered important will vary over time.2 3 8 During the covid-19 pandemic the immediate priority was to interrupt transmission, and success was initially measured by numbers of covid-19 cases. Mortality during the pandemic was measured as case and infection fatality rates and excess mortality rates,9 each influenced by factors such as the extent of testing and diagnosis or, for excess mortality, the baseline chosen.10
Box 1. Challenges with quantifying a health system shock and its response.
Engineers test products to ensure that they can withstand shocks, but we cannot do the same with a health system. Modelling provides an alternative. However, although models can make good short term predictions, they face many challenges.4
Quantifying the scale and nature of both the shock and the predicted response in a health system is difficult. First, they may be difficult to measure—for example, because of the delay between infections occurring and data becoming available. In addition, infection may spread unnoticed within marginalised communities (which may be disproportionately affected because, for example, they live in precarious circumstances) making the size of an epidemic uncertain. Both the shock and the response are, using the word in its mathematical meaning, complex5 as they involve many diverse human responses.4
In a complex system, the spread of a shock and responses to it are influenced by where people and organisations start from (path dependency), reflecting factors such as morale, training, and reserve capacity; they are often non-linear and include feedback loops, with people adapting to the behaviour of those around them.6 Healthcare is especially constrained by how so many people and things must interact, especially when there are no easy substitutes. Scaling up hospital beds to cope with the surging numbers of people with covid-19, as was the aim of the Nightingale hospitals established in England, is relatively easy. Finding specialist staff is not. With so many factors at play, trying to model how health systems will respond to potential shocks is akin to informed guesswork. However, it does allow scenarios to be tested.7
Excess all-cause mortality has the benefit of also capturing deaths that are an indirect effect of the shock, such as those resulting from the decreased use of routine health services.11 12 However, more detailed and complex analysis is needed to disentangle the myriad factors that have contributed to excess mortality and, specifically, the functioning of the health system. This is inevitable given the blurred borders and complexity of health systems, and the importance of the socioeconomic context within which they are embedded. For example, indicators which focus on assessing health outcomes during covid-19, such as morbidity and mortality rates,13 14 15 16 17 miss some important factors, including morale of health workers and the effect on people who were socially isolated or dependent on essential services.11
Other indicators relevant to health system resilience relate to policy responses that lie beyond the health system, such as stringency of lockdowns, or other factors, such as the role of civil society in filling service gaps.18 Issues such as public trust and governance capacity must also be considered. For example, in the UK, public trust and confidence in the government’s ability to manage the pandemic was compromised at a critical time, which meant some people were less willing to follow rules and guidelines fundamental to controlling infection.19
Another challenge is knowing when to measure. Policies and outcomes change over time, and health systems often depend on decisions made beyond the health sector, the timing of which can be critical. When infections are increasing exponentially, for example, even a short delay in imposing restrictions on mixing will make an enormous difference in terms of the numbers of people infected and the subsequent effect on the health system.20 Some countries that initially responded rapidly and decisively to covid-19 had later surges of infections when they relaxed restrictions. This is exemplified by China, which having failed to achieve high vaccine uptake among its older population, saw high case numbers when it relaxed its successful control measures.21 22 These considerations apply equally to policies that contribute to societal resilience, such as social protection mechanisms that act over many years to reduce the number of people who might be more vulnerable to the effects of the pandemic and its countermeasures.23
Finally, given the complex environment within which health systems work, too narrow a focus on aspects of health system resilience, such as use of traditional measures of capacity (eg, workforce numbers, beds, and equipment), has been criticised for encouraging simplistic short term solutions to the detriment of other preparations such as prevention and control measures.24 Before the covid pandemic the US and UK were rated the top performing countries in pandemic preparedness based on traditional measures of health system capacity and technical measures of prevention (eg, biosafety) and detection (eg, laboratories). However, they had among the highest case and death rates, largely because of wider institutional weaknesses and poor political decision making.25 26
Operationalising a broader perspective of health system resilience requires understanding the challenges to comprehensively measuring it. Ideally, this would be a dynamic process, looking at various aspects of resilience, from patient care and frontline workers to political decision making, at different points in time.
Barely coping workforce reflects lack of system resilience
The pandemic was a stark reminder of the crucial importance of investment in a motivated, skilled, and engaged health workforce.27 Health workers in countries that acted rapidly to interrupt transmission, or which had previously invested in health system capacity, were relatively fortunate because they were better able to manage the shock.28 29 30 Others, whose governments had delayed acting and had underinvested over many years, struggled to respond, as did health systems where workers were already tired and demoralised.27 31 Yet, even in countries that were among the worst affected by rising numbers of cases, there were many examples of frontline health workers designing and implementing innovative responses in almost impossible circumstances. It is thus not surprising that in a 2022 systematic review of 68 studies measuring health system resilience across different health system shocks, workforce wellbeing was the second most commonly used indicator.32
Health system assessments of covid-19 responses often focused on the ability to ensure delivery of services both for patients with covid-19 and for those with other conditions by safeguarding and supporting the health workforce and, once vaccines became available, rolling them out at pace and scale, while reducing the accumulated backlogs of care. However, measures of the scale of disruption to care and subsequent recovery were fragmentary.33 34 One of the most detailed analyses, which included 31 services such as maternal and child health, HIV, and malaria, covered only 10 countries,35 and comparable data on important measures such as burnout in the health workforce are scarce. This is important because while a system may seem to be coping, it will be unsustainable if maintained by superhuman efforts of health workers. As with excess mortality, data on staff retention, sickness absence, or broader labour force participation can contribute useful insights because exhausted and sick health workers are a symptom of resilience being exhausted at the system level.36
What do we know about health system resilience during covid-19?
Even though it is the best studied global shock ever, it is difficult, and perhaps impossible, to unequivocally say which health systems were the most resilient to covid-19 as the answer will change over time. Resilience of the health system is also influenced by decisions taken outside of it, but a focus on service delivery provides a useful starting point by looking at the ways health systems were able to absorb, adapt, transform, and learn during the covid-19 pandemic.
Ability to absorb the shock
The ability of a health system to absorb a shock is largely a function of its preparedness. Health systems need the resources to respond and a plan to deploy them rapidly and appropriately (box 2). Unfortunately, few countries were well prepared.
Box 2. Response plans were inadequate.
A plan to guide the rapid and appropriate deployment of resources is critical to health system preparedness and response. Many countries did not have a pandemic preparedness and response plan in place, and even when one did exist, it had not been tested in realistic exercises.
Even when plans had been tested, such as Exercise Alice in the UK, which sought to identify challenges to managing a Middle East respiratory syndrome (MERS) outbreak in 2016, recommendations were not always followed up.37 38 Many countries used plans designed for pandemic influenza rather than coronaviruses.39 This had serious consequences, not least because of the delayed recognition of the importance of airborne spread.40
The resources needed—facilities, materials (eg, pharmaceuticals, medical equipment, protective equipment), and people—must not only be available in the right quantities but also in the right combination, with the right characteristics (skill mix, function, technological specifications), and in the right place. While there were many examples of staff working flexibly—for example, by redeploying and repurposing facilities24—the absence of a single health worker with specialist skills, such as an anaesthetist, can prevent an entire intensive care team from functioning.41 Unfortunately, data systems enumerate individual items and not their performance in combination.
The data we do have reveal stark differences in countries’ resource preparedness. Germany, with almost 34 intensive care beds per 100 000 population, was much better placed than England with 10.5 beds/100 000 and Ireland with 5/100 000 people.42 Low numbers of health workers in some countries compounded the challenges they faced. Within the European Economic Area the number of physicians differed by 60%, from fewer than 3 physicians/1000 population in Poland to 5/1000 people in Austria, while the variation in numbers of nurses was even greater, from fewer than 5/1000 population in Latvia and Bulgaria to 18/1000 in Norway.42 Having sufficient well motivated health workers is a core element of health system performance and resilience.
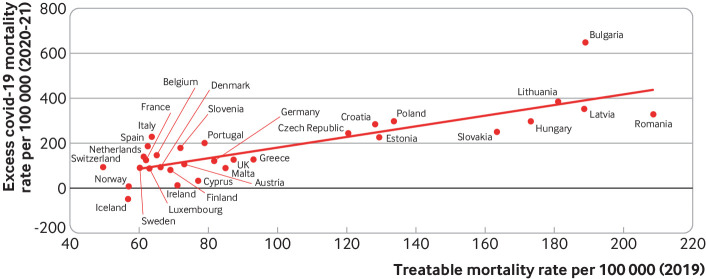
Treatable mortality, which captures deaths that can be avoided through timely and effective care, can shed additional light on the combined performance of individual health system elements before and during the pandemic. European countries that were achieving lower treatable mortality, indicating stronger health system performance before the pandemic, also had lower excess mortality rates during covid-19 (fig 1). Investment in strengthening health systems is thus not only essential to reduce barriers to accessing health services and achieve the goal of universal health coverage43 but may improve resilience to shocks.
Fig 1.
Association between excess covid-19 mortality16 and pre-pandemic treatable mortality (Eurostat database, 2019) in European Economic Area countries. A negative excess mortality rate means that the mortality rate observed during the pandemic was lower than the mortality rate that would have been expected if covid-19 did not happen (ie, an improvement)
Some of the resources needed can be stockpiled, repurposed, or scaled up rapidly, particularly non-specialist equipment such as beds. However, this will translate into meaningful healthcare capacity only if it is accompanied by a sufficient and capable workforce. In the short term, capacity can be partly boosted by mobilising and redeploying the existing workforce, although the risk of burnout is high. Medical students or retired health professionals can also be deployed, but this may require changes to regulatory systems and is not a panacea to acute shortages and chronic underinvestment in the workforce.24 There may, however, be potential to recruit staff for roles that require less training and supervision, as seen with volunteer vaccinators in the UK. The UK also recruited large numbers of contact tracers to work in private call centres, but at high cost and with questionable results.44
In addition, the appropriate design of health facilities is an overlooked aspect of preparedness. Countries in Asia benefited from having created physically separate pathways for infected and non-infected patients.45 This, coupled with attention to air quality, enabled them to maintain non-covid-19 services to a greater extent than in Europe.46 Other measures implemented in these countries in the aftermath of the severe acute respiratory syndrome (SARS) and Middle East respiratory syndrome (MERS epidemics, such as strengthening public health structures and response capacities, meant they were better able to respond to a new outbreak.
How health systems adapted
Adaptation involves reconfiguring the health system to respond to a threat. This is a reflective and proactive process, in contrast to the reactive aspects of absorption. It includes changes to the roles of health workers, adopting new technologies (such as lateral flow tests), and implementing new models of care. For example, many countries expanded the scope of work of nurses, pharmacists, and other health professionals.24 Countries where the roles of non-physicians had been most advanced before the pandemic—such as the UK, where nurses have long been able to prescribe within protocols—had an advantage.47 However, these changes brought substantial pressures, including high rates of burnout and moral injury (arising from health workers being unable to give lifesaving care because of inadequate resources).48
Advances in technology offer increasing possibilities for adaptation to a crisis. Teleconsultation greatly expanded in some countries, particularly in primary care.24 In Lithuania, for example, the number of remote primary care consultations was nearly 70 times higher in April 2020 than in April 2019.24 Although face-to-face consultations in primary care in England fell, online consultations more than compensated.49
Adaptation was also facilitated by earlier investment in data, research, and learning health systems. Having the right information and the capacity to learn was crucial to implementing adaptive actions. Initial capacity for surveillance and monitoring mattered, but many countries managed to put new systems in place.24 Yet, many gaps remain. For example, genomic sequencing, essential for tracking variants, is inadequate in many countries. Denmark and the UK were notable exceptions. Few countries collect data by ethnicity or migration status, essential to understand inequalities.49
Prior investment in research infrastructure made a difference. The UK’s Recovery trial, implemented at unprecedented speed and scale, provided crucial insights—for example on effectiveness of hydroxychloroquine and dexamethasone50—while the existence of learning networks, communities of practice that drove clinical and service innovation across England, was invaluable.51 Yet these UK successes were accompanied by some spectacular failures of governance, including possible corruption in public procurement of personal protective equipment, testing, and other services.52 53
Using pandemic response to transform the health system
Sometimes, weaknesses revealed in the absorption and adaptation phases highlight a need to transform the system to enhance its preparedness for future shocks.2 A shock can thus be an opportunity to tackle longstanding problems by accelerating (or resurrecting) existing reforms or introducing new ones. For example, the Irish government took advantage of its pandemic response to unlock stalled progress towards universal health coverage (the Sláintecare reform), having made all covid related care free of charge,54 while Finland finalised its largest ever social and healthcare reform (Sote), transferring responsibilities for health, social, and rescue services from over 300 municipalities to about 20 larger entities.55 Thailand made similar advances while recuperating from the 1997 Asian financial crisis when it introduced ambitious universal health coverage reforms.56
Transformation can also be spurred by the absorptive and adaptive responses to the shock. For example, some short term absorptive measures, such as postponing elective surgery, are not sustainable in the longer term and may necessitate more profound changes such as establishing virtual hospitals or introducing dual patient pathways, as Asian countries did after the SARS epidemic. Increased use of teleconsultations and some of the skill mix adjustments, such as allowing certain health professionals to prescribe medicines or vaccinate, are examples of adaptive measures that could be become permanent after the pandemic.57
These changes can be either reactive, focusing on fixing problems uncovered during the pandemic, or proactive, drawing lessons from the traumas of the past three years to ensure that we are better prepared for the next pandemic or other shock.1 For example, a project initiated by the European Commission at the end of 2021 is testing the resilience of European health systems to different shocks, from natural disasters to the cost-of-living crisis, as well as antimicrobial resistance, climate change, and further pandemics, to identify potential weaknesses.58 At the same time, the EU’s Recovery and Resilience Facility offers member states funding to invest in the health sector for post-pandemic recovery.59 But with the political focus shifting to other problems,60 61 the urgency of investing in health system transformations may wane, even in the EU.62
Assessing health system resilience is worth the challenge
A comprehensive measurement of resilience is a challenge, but efforts to assess it help us gain important insights into how health system resilience can be enhanced. In particular, looking at some of the actions health systems took to absorb, adapt, and transform in the midst of a crisis help us understand how various leverage points within and outside of the health system can enhance its preparedness and ability to maintain performance during a shock.
Efforts to assess the resilience of health systems are justified not only to increase preparedness for future shocks but also to achieve universal health coverage and related sustainable development goals. Health systems that performed better before the pandemic were better placed when it arose, but a coordinated response within and among countries will be needed to prepare better for the next pandemic or shock.
Key messages.
Health systems are often unprepared for shocks such as covid-19, but assessing resilience can help them prepare
Health system resilience to a shock is difficult to measure comprehensively
It can, however, be assessed by looking at what absorptive, adaptive, and transformative measures health systems adopted in response to a shock
Responses to covid-19 show how health system strengthening and factors outside the health system affect resilience
Contributors and sources: All contributors are engaged in research covering health systems, health systems resilience, and health systems responses to the covid-19 pandemic, and this article draws on their previous publications in these areas. AS, ST, and MM contributed equally to the conceptualisation, analysis, and implementing revisions. AS and MM led on the writing of the article and MM is the guarantor. EW supported the conceptualisation, analysis, and writing.
Competing interests: We have read and understood BMJ policy on declaration of interests and have no interests to declare.
Provenance and peer review: Commissioned; externally peer reviewed.
This article is part of a collection proposed by the Health Foundation, which also provided funding for the collection, including open access fees. The BMJ commissioned, peer reviewed, edited, and made the decision to publish these articles. Rachael Hinton and Paul Simpson were the lead editors for The BMJ.
References
- 1. McKee M. Drawing light from the pandemic: a new strategy for health and sustainable development. World Health Organization. Regional Office for Europe for the European Observatory on Health Systems and Policies, 2021. [Google Scholar]
- 2.Thomas S, Sagan A, Larkin J, et al. Strengthening health systems resilience: Key concepts and strategies. European Observatory on Health Systems and Policies, 2020. [PubMed] [Google Scholar]
- 3. Topp SM. Power and politics: the case for linking resilience to health system governance. BMJ Glob Health 2020;5:e002891. 10.1136/bmjgh-2020-002891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Pagel C, Yates CA. Role of mathematical modelling in future pandemic response policy. BMJ 2022;378:e070615. 10.1136/bmj-2022-070615. [DOI] [PubMed] [Google Scholar]
- 5. Nolte E, McKee M, Wait S. Describing and evaluating health systems. In: Bowling A, Ebrahim S, eds. Handbook of health research methods: investigation, measurement and analysis. Open University Press, 2005: 12-43. [Google Scholar]
- 6. Reicher S, Stott C. On order and disorder during the COVID-19 pandemic. Br J Soc Psychol 2020;59:694-702. 10.1111/bjso.12398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Rogers HL, Barros PP, Maeseneer J, et al. Resilience testing of health systems: how can it be done? Int J Environ Res Public Health 2021;18:4742. 10.3390/ijerph18094742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Saulnier DD, Blanchet K, Canila C, et al. A health systems resilience research agenda: moving from concept to practice. BMJ Glob Health 2021;6:e006779. 10.1136/bmjgh-2021-006779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Focacci CN, Lam PH, Bai Y. Choosing the right COVID-19 indicator: crude mortality, case fatality, and infection fatality rates influence policy preferences, behaviour, and understanding. Humanities and Social Sciences Communications 2022;9:19. 10.1057/s41599-021-01032-0. [DOI] [Google Scholar]
- 10. Shkolnikov VM, Klimkin I, McKee M, et al. What should be the baseline when calculating excess mortality? New approaches suggest that we have underestimated the impact of the COVID-19 pandemic and previous winter peaks. SSM Popul Health 2022;18:101118. 10.1016/j.ssmph.2022.101118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Douglas M, Katikireddi SV, Taulbut M, McKee M, McCartney G. Mitigating the wider health effects of covid-19 pandemic response. BMJ 2020;369:m1557. 10.1136/bmj.m1557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Mansfield KE, Mathur R, Tazare J, et al. Indirect acute effects of the COVID-19 pandemic on physical and mental health in the UK: a population-based study [published Online First: 20210218]. Lancet Digit Health 2021;3:e217-30. 10.1016/S2589-7500(21)00017-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Oh J, Lee H-Y, Khuong QL, et al. Mobility restrictions were associated with reductions in COVID-19 incidence early in the pandemic: evidence from a real-time evaluation in 34 countries. Sci Rep 2021;11:13717. 10.1038/s41598-021-92766-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Kontis V, Bennett JE, Parks RM, et al. Lessons learned and lessons missed: impact of the coronavirus disease 2019 (COVID-19) pandemic on all-cause mortality in 40 industrialised countries and US states prior to mass vaccination [version 2; peer review: 2 approved]. Wellcome Open Res 2022;6:279. 10.12688/wellcomeopenres.17253.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Schöley J, Aburto JM, Kashnitsky I, et al. Life expectancy changes since COVID-19. Nat Hum Behav 2022;6:1649-59. 10.1038/s41562-022-01450-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Wang H, Paulson KR, Pease SA, et al. COVID-19 Excess Mortality Collaborators . Estimating excess mortality due to the COVID-19 pandemic: a systematic analysis of COVID-19-related mortality, 2020-21. Lancet 2022;399:1513-36. 10.1016/S0140-6736(21)02796-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. COVID-19 Forecasting Team . Variation in the COVID-19 infection-fatality ratio by age, time, and geography during the pre-vaccine era: a systematic analysis. Lancet 2022;399:1469-88. 10.1016/S0140-6736(21)02867-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Blavatnik School of Government. Covid-19 government response tracker. 2023. https://www.bsg.ox.ac.uk/research/covid-19-government-response-tracker
- 19. Fancourt D, Steptoe A, Wright L. The Cummings effect: politics, trust, and behaviours during the COVID-19 pandemic. Lancet 2020;396:464-5. 10.1016/S0140-6736(20)31690-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Arnold KF, Gilthorpe MS, Alwan NA, et al. Estimating the effects of lockdown timing on COVID-19 cases and deaths in England: A counterfactual modelling study. PLoS One 2022;17:e0263432. 10.1371/journal.pone.0263432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Burki T. Moving away from zero COVID in China. Lancet Respir Med 2023;11:132. 10.1016/S2213-2600(22)00508-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Mallapaty S. China is relaxing its zero-COVID policy - here’s what scientists think. Nature 2022;612:383-4. 10.1038/d41586-022-04382-0. [DOI] [PubMed] [Google Scholar]
- 23. McNamara CL, McKee M, Stuckler D. Precarious employment and health in the context of COVID-19: a rapid scoping umbrella review. Eur J Public Health 2021;31(suppl_4):iv40-9. 10.1093/eurpub/ckab159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sagan A, Webb E, Azzopardi-Muscat N, et al. Health systems resilience during COVID-19: lessons for building back better. World Health Organization, Regional Office for Europe for the European Observatory on Health Systems and Policies, 2021. [PubMed] [Google Scholar]
- 25. Baum F, Freeman T, Musolino C, et al. Explaining covid-19 performance: what factors might predict national responses? BMJ 2021;372:n91. 10.1136/bmj.n91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Nuclear Threat Initiative (NTI) and the Johns Hopkins Center for Health Security. Global Health Security Index. 2021. https://www.ghsindex.org/about/
- 27. Fleming P, Caffrey L, Van Belle S, et al. How international health system austerity responses to the 2008 financial crisis impacted health system and workforce resilience – a realist review. Int J Health Policy Manage 2022. 10.34172/ijhpm.2022.7420 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Hanefeld J, Mayhew S, Legido-Quigley H, et al. Towards an understanding of resilience: responding to health systems shocks. Health Policy Plan 2018;33:355-67. 10.1093/heapol/czx183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Stuckler D, Reeves A, Loopstra R, Karanikolos M, McKee M. Austerity and health: the impact in the UK and Europe. Eur J Public Health 2017;27(suppl_4):18-21. 10.1093/eurpub/ckx167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Thomson S, García-Ramírez JA, Akkazieva B, Habicht T, Cylus J, Evetovits T. How resilient is health financing policy in Europe to economic shocks? Evidence from the first year of the COVID-19 pandemic and the 2008 global financial crisis. Health Policy 2022;126:7-15. 10.1016/j.healthpol.2021.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Baskin RG, Bartlett R. Healthcare worker resilience during the COVID-19 pandemic: An integrative review. J Nurs Manag 2021;29:2329-42. 10.1111/jonm.13395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Fleming P, O’Donoghue C, Almirall-Sanchez A, et al. Metrics and indicators used to assess health system resilience in response to shocks to health systems in high income countries-A systematic review. Health Policy 2022;126:1195-205. 10.1016/j.healthpol.2022.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.OECD, European Union. Dealing with backlogs: disruptions in non-COVID care during the pandemic. In: Health at a Glance: Europe 2022: State of Health in the EU Cycle. OECD, 2022. [Google Scholar]
- 34. van Ginneken E, Reed S, Siciliani L, et al. Addressing backlogs and managing waiting lists during and beyond the COVID-19 pandemic. World Health Organization. Regional Office for Europe, 2022. [PubMed] [Google Scholar]
- 35. Arsenault C, Gage A, Kim MK, et al. COVID-19 and resilience of healthcare systems in ten countries. Nat Med 2022;28:1314-24. 10.1038/s41591-022-01750-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. McKee M, Hiam L. Britain’s not working. BMJ 2022;378:o1883. 10.1136/bmj.o1883. [DOI] [PubMed] [Google Scholar]
- 37. Dyer C. Pandemic preparedness: UK government kept coronavirus modelling secret. BMJ 2021;373:n1501. 10.1136/bmj.n1501. [DOI] [PubMed] [Google Scholar]
- 38. McKee M. The UK government tested the response to a coronavirus-why are we only discovering this now? BMJ 2021;375:n2485. 10.1136/bmj.n2485. [DOI] [PubMed] [Google Scholar]
- 39. An BY, Tang S-Y. Lessons From covid-19 responses in east Asia: institutional infrastructure and enduring policy instruments. Am Rev Public Adm 2020;50:790-800. 10.1177/0275074020943707. [DOI] [Google Scholar]
- 40. Greenhalgh T, Ozbilgin M, Tomlinson D. How covid-19 spreads: narratives, counter narratives, and social dramas. BMJ 2022;378:e069940. 10.1136/bmj-2022-069940. [DOI] [Google Scholar]
- 41. van Klei WA, Hollmann MW, Sneyd JR. The value of anaesthesiologists in the COVID-19 pandemic: a model for our future practice? Br J Anaesth 2020;125:652-5. 10.1016/j.bja.2020.08.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.OECD, European Union. Chapter 7. Accessibility: affordability, availability and use of services. In: Health at a Glance: Europe 2020: State of Health in the EU Cycle. OECD, 2020. [Google Scholar]
- 43.Papanicolas I, Rajan D, Karanikolos M, et al. Health system performance assessment: a framework for policy analysis. World Health Organization, 2022. [PubMed] [Google Scholar]
- 44. Scally G, Jacobson B, Abbasi K. The UK’s public health response to covid-19. BMJ 2020;369:m1932. 10.1136/bmj.m1932. [DOI] [PubMed] [Google Scholar]
- 45. Cheng VCC, Wong SC, Chen JHK, et al. Escalating infection control response to the rapidly evolving epidemiology of the coronavirus disease 2019 (COVID-19) due to SARS-CoV-2 in Hong Kong. Infect Control Hosp Epidemiol 2020;41:493-8. 10.1017/ice.2020.58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Han E, Tan MMJ, Turk E, et al. Lessons learnt from easing COVID-19 restrictions: an analysis of countries and regions in Asia Pacific and Europe. Lancet 2020;396:1525-34. 10.1016/S0140-6736(20)32007-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Anderson M, O’Neill C, Macleod Clark J, et al. Securing a sustainable and fit-for-purpose UK health and care workforce. Lancet 2021;397:1992-2011. 10.1016/S0140-6736(21)00231-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Expert Panel on Effective Ways of Investing in Health . Supporting mental health of health workforce and other essential workers. European Commission, 2022. [Google Scholar]
- 49. Routen A, Akbari A, Banerjee A, et al. Strategies to record and use ethnicity information in routine health data. Nat Med 2022;28:1338-42. 10.1038/s41591-022-01842-y. [DOI] [PubMed] [Google Scholar]
- 50. Wise J, Coombes R. Covid-19: the inside story of the Recovery trial. BMJ 2020;370:m2670. 10.1136/bmj.m2670. [DOI] [PubMed] [Google Scholar]
- 51. Sidhu MS, Ford GA, Fulop NJ, Roberts CM. Learning networks in the pandemic: mobilising evidence for improvement. BMJ 2022;379:e070215. 10.1136/bmj-2022-070215. [DOI] [PubMed] [Google Scholar]
- 52. Iacobucci G. Covid-19: One in five government contracts had signs of possible corruption, report finds. BMJ 2021;373:n1072. 10.1136/bmj.n1072. [DOI] [PubMed] [Google Scholar]
- 53. McKee M. England’s PPE procurement failures must never happen again. BMJ 2020;370:m2858. 10.1136/bmj.m2858. [DOI] [PubMed] [Google Scholar]
- 54. Burke S, Parker S, Fleming P, Barry S, Thomas S. Building health system resilience through policy development in response to COVID-19 in Ireland: From shock to reform. Lancet Reg Health Eur 2021;9:100223. 10.1016/j.lanepe.2021.100223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.European Commission. Finland finalises its largest-ever social and healthcare reform. European Commission, 2022. https://ec.europa.eu/social/BlobServlet?docId=25947&langId=en
- 56. Sumriddetchkajorn K, Shimazaki K, Ono T, Kusaba T, Sato K, Kobayashi N. Universal health coverage and primary care, Thailand. Bull World Health Organ 2019;97:415-22. 10.2471/BLT.18.223693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. van Schalkwyk MC, Bourek A, Kringos DS, et al. European Commission Expert Panel on Effective ways of Investing in Health . The best person (or machine) for the job: Rethinking task shifting in healthcare. Health Policy 2020;124:1379-86. 10.1016/j.healthpol.2020.08.008. [DOI] [PubMed] [Google Scholar]
- 58. Tille F, Van Ginneken E, Winkelmann J, et al. Perspective: lessons from COVID-19 of countries in the European region in light of findings from the health system response monitor. Front Public Health 2023;10:1058729. 10.3389/fpubh.2022.1058729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Anderson M, Forman R, Mossialos E. Navigating the role of the EU Health Emergency Preparedness and Response Authority (HERA) in Europe and beyond. Lancet Regional Health . Europe 2021;9:100203. 10.1016/j.lanepe.2021.100203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Gilson L, Barasa E, Nxumalo N, et al. Everyday resilience in district health systems: emerging insights from the front lines in Kenya and South Africa. BMJ Glob Health 2017;2:e000224. 10.1136/bmjgh-2016-000224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Murphy A, Fuhr D, Roberts B, Jarvis CI, Tarasenko A, McKee M. The health needs of refugees from Ukraine. BMJ 2022;377:o864. 10.1136/bmj.o864. [DOI] [PubMed] [Google Scholar]
- 62.World Bank. From double shock to double recovery: health financing in the time of covid-19. 2022. https://www.worldbank.org/en/topic/health/publication/from-double-shock-to-double-recovery-health-financing-in-the-time-of-covid-19