Abstract
Hepatic insulin resistance is recognized as a driver of type 2 diabetes and fatty liver disease but specific therapies are lacking. Here we explore the potential of human induced pluripotent stem cells (iPSCs) for modeling hepatic insulin resistance in vitro, with a focus on resolving the controversy about the impact of inflammation in the absence of steatosis. For this, we establish the complex insulin signaling cascade and the multiple inter-dependent functions constituting hepatic glucose metabolism in iPSC-derived hepatocytes (iPSC-Heps). Co-culture of these insulin-sensitive iPSC-Heps with isogenic iPSC-derived pro-inflammatory macrophages induces glucose output by preventing insulin from inhibiting gluconeogenesis and glycogenolysis and activating glycolysis. Screening identifies TNFα and IL1β as the mediators of insulin resistance in iPSC-Heps. Neutralizing these cytokines together restores insulin sensitivity in iPSC-Heps more effectively than individual inhibition, reflecting specific effects on insulin signaling and glucose metabolism mediated by NF-κB or JNK. These results show that inflammation is sufficient to induce hepatic insulin resistance and establish a human iPSC-based in vitro model to mechanistically dissect and therapeutically target this metabolic disease driver.
Subject terms: Induced pluripotent stem cells, Metabolic syndrome, Type 2 diabetes
Hepatic insulin resistance is an established driver of type 2 diabetes but is difficult to model in vitro. Here researchers use co-culture of hepatocytes and macrophages derived from the same human iPSC line to show how inflammation disrupts insulin-mediated regulation of hepatic glucose metabolism and identify targets for therapy of hepatic insulin resistance.
Introduction
The potential of human induced pluripotent stem cell (iPSC)-derived hepatocytes (iPSC-Heps) for in vitro disease modeling rests on their ability to replicate complex functions provided by the human liver in vivo. One such function that is of high clinical relevance is hepatic glucose metabolism and its regulation by insulin. Some aspects of the insulin signaling cascade have been shown to be active in iPSC-Heps1,2, but whether these cells allow for the faithful study of disease mechanisms affecting insulin-mediated regulation of glucose metabolism remains to be determined. In fact, it is currently unknown whether insulin and the counterregulatory hormone glucagon exert physiological control over glucose metabolism in iPSC-Heps. Studies are needed that show that the fast-acting and complex hepatic insulin signaling cascade—revolving around the interaction of the insulin receptor (INSR) with insulin receptor substrate (IRS) 1 and 2 and subsequent activation of the central metabolic regulator protein kinase B (AKT) through phosphoinositide 3-kinase and 3-phosphoinositide-dependent kinase 13,4—regulates gluconeogenesis, glycolysis, glycogen metabolism and thereby glucose output in iPSC-Heps.
iPSC-Heps equipped with fully developed hormone-regulated glucose metabolism would facilitate studies of hepatic insulin resistance, which is common in obesity and critical for manifestation and progression of type 2 diabetes and fatty liver disease5–7. Lipid accumulation is thought to be the main cause of hepatic insulin resistance4. However, earlier studies in mice showed that inflammation induced by activated macrophages can also impair insulin sensitivity of hepatocytes, leading to disrupted downstream signaling and increased hepatic glucose output8,9. Activated macrophages can cause hepatic insulin resistance by secreting pro-inflammatory cytokines10,11. In vivo evidence points to interleukin 6 (IL6) as a mediator of the effects activated macrophages have on hepatic glucose metabolism, but comprehensive studies are lacking12. Moreover, findings about the contribution of inflammation to hepatic insulin resistance have been contradictory, with some studies showing it acts as an adjuvant to steatosis, whereas others argue it is sufficient by itself 8,9,11,12.
Disruption of hepatic insulin signaling by IL6 has also been shown in vitro using liver cell lines and primary mouse hepatocytes13. Similar effects have been reported for tumor necrosis factor α (TNFα) and interleukin 1β (IL1β) in liver cell lines and primary rat hepatocytes10,14,15. Moreover, TNFα has been shown in co-cultures of primary rat cells to mediate the disruption of insulin signaling in hepatocytes by activated macrophages8. A limitation of these in vitro studies is insufficient analysis of insulin-regulated functions constituting hepatic glucose metabolism, particularly of glucose output, which is at the core of type 2 diabetes and fatty liver disease16. In fact, glucose production is reportedly low and not responsive to insulin in liver cell lines17. Primary human hepatocytes (PHHs) exhibit insulin-regulated glucose production in vitro as long as differentiation is stabilized by co-culture with stromal cells18. Such co-cultures showed that hyperglycemia causes steatosis-associated hepatic insulin resistance19. Similarly, spheroid culture maintains insulin sensitivity of PHHs, with signs of insulin resistance developing after long-term metabolic challenge with high-level fatty acids, insulin and glucose20. The role of inflammation has not been investigated in these PHH-based models.
Human iPSCs address many limitations of primary cells, including expandability and ability to generate multiple cell types from the same iPSC line, thereby eliminating immunological and genetic biases in co-culture models. iPSC-Heps have been successfully used for human liver disease modeling in vitro; however, incomplete differentiation of iPSC-Heps generated with current protocols requires in-depth characterization to ascertain adequate function21.
To develop an iPSC-based model of hepatic insulin resistance and resolve the controversy about the impact of inflammation, we modified differentiation of iPSC-Heps to achieve physiologically relevant insulin sensitivity and co-cultured the cells with pro-inflammatory (classically activated; M1) or undifferentiated/non-activated (M0) macrophages derived from the same iPSC line (iPSC-Macs). In addition to defining the effects of inflammation on hepatic insulin signaling and glucose metabolism, we identified the causative cytokines and devised a strategy to restore insulin sensitivity in iPSC-Heps. We ascertained the authenticity of our findings by confirmation in PHHs co-cultured with primary human macrophages (PHMs). These findings establish the potential of our human iPSC-based model for further mechanistic studies and development of new therapies for hepatic insulin resistance.
Results
iPSC-Heps exhibit physiological regulation of glucose metabolism
Current protocols for iPSC-Hep generation include insulin and glucocorticoids to enhance differentiation and survival22–24. We reasoned that continuous stimulation with these hormones may render iPSC-Heps insensitive to hormone boluses25,26. Therefore, we amended our protocol to include a 24-h starvation period without insulin, glucocorticoids or growth factors after the 22-day differentiation process (Supplementary Fig. 1a). We ascertained normal viability (Supplementary Fig. 1b) and differentiation (Supplementary Fig. 1c–e) of iPSC-Heps generated with the amended protocol, including mitochondrial activity (Supplementary Fig. 1f, g).
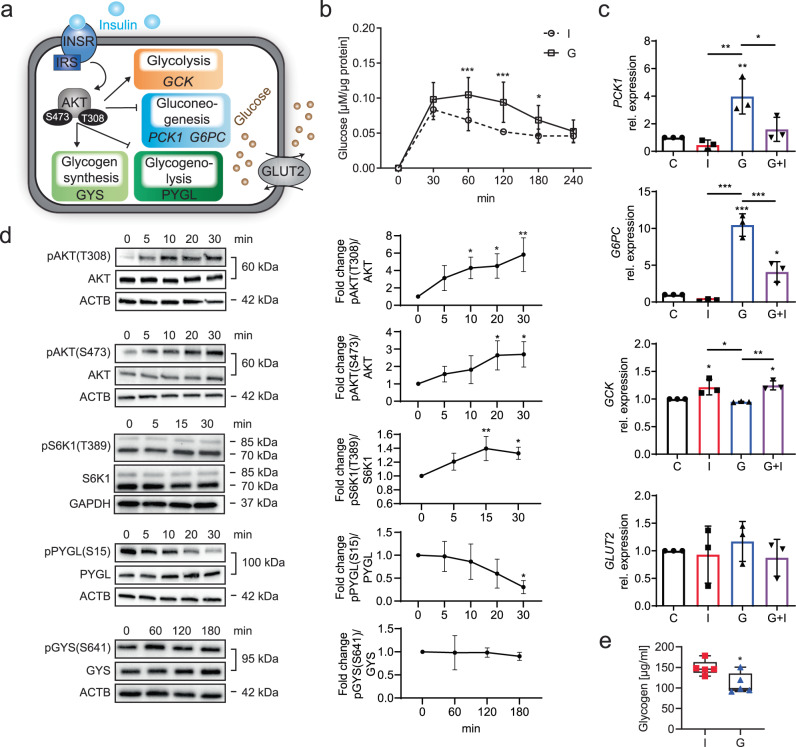
To determine the insulin sensitivity of our iPSC-Heps, we analyzed glucose production and other functions constituting hepatic glucose metabolism and key aspects of insulin signaling (Fig. 1a). Initially, we observed that an insulin bolus applied after the starvation period was effective in reducing hepatic glucose production but only moderately and briefly (Supplementary Fig. 2a). In contrast, treatment with the physiological insulin antagonist glucagon caused a marked increase in hepatic glucose production for 3 h (Fig. 1b). Increased hepatic glucose production was associated with increased gluconeogenesis, as evidenced by analysis of PCK1 and G6PC gene expression, which was induced by glucagon and reduced by subsequent insulin stimulation (Fig. 1c). GCK gene expression indicated that glycolysis was not affected by glucagon but induced by insulin (Fig. 1c). Expression of the three major genes of the INSR complex, INSR, IRS1 and IRS2, was reduced by both insulin and glucagon, with maximum reduction after serial stimulation with both hormones, indicating an insulin-dependent negative feedback loop27,28 (Supplementary Fig. 2b). We excluded that these differences in hepatic glucose production were caused by changes in gene expression of GLUT2, the major bi-directional hepatic glucose transporter29 (Fig. 1c). Prompted by these findings, we added a 1-h glucagon-stimulation period after the 24-h starvation period to our protocol (Supplementary Fig. 1a).
Fig. 1. Insulin and glucagon effects on glucose metabolism in iPSC-Heps.
a Overview of insulin signaling and functions constituting glucose metabolism in hepatocytes. b Time course of analysis of glucose release into glucose-free media by iPSC-Heps after insulin (I) and glucagon (G). Data are mean ± SD; n = 6, two-way ANOVA (two-stage step-up method of Benjamini, Krieger and Yekutieli), *P < 0.05 and ***P < 0.001 vs. I at indicated timepoints. c Gene expression analysis in iPSC-Heps after 4 h of no hormones (C, control), insulin (I), glucagon (G) or 2 h of glucagon followed by 2 h of insulin (G+I). Data are mean ± SD; n = 3, one-way ANOVA (Tukey’s test), *P < 0.05, **P < 0.01 and ***P < 0.001 vs. C or between indicated conditions. d Time course of western blot analysis of AKT, S6K1, PYGL and GYS phosphorylation in iPSC-Heps after insulin. Data are mean ± SD; n = 3, one-way ANOVA (Dunnett’s test), *P < 0.05 and **P < 0.01 vs. time point 0 min. e Quantification of glycogen in iPSC-Heps after 3 h of insulin or glucagon. Data are mean ± SD; n = 5, unpaired two-tailed Student’s t test, *P < 0.05. Source data are provided as a Source Data file.
Next, we investigated whether the speed and complexity of insulin-mediated regulation of hepatic glucose production found in primary hepatocytes is replicated by iPSC-Heps30. For this, we generated a time course of phosphorylation-mediated activation of INSR and AKT. After insulin bolus, autophosphorylation of INSR and phosphorylation of AKT at T308 and S473 were initiated within 5 min, with AKT phosphorylation increasing for 30 min, indicating involvement of both INSR signaling and mTORC2 signaling, the latter being partially insulin independent4,31,32; we also confirmed that insulin causes phosphorylation of p70 S6 kinase (S6K1) at T389, which acts downstream of mTORC1 and is essential for hepatic glucose homeostasis33 (Supplementary Fig. 2c, Fig. 1d). In addition, we investigated whether glycogen metabolism is regulated by insulin through glycogen phosphorylase L (PYGL)-mediated glycogenolysis and glycogen synthase (GYS)-mediated glycogen synthesis34. We found that PYGL is rapidly and progressively dephosphorylated at S15 and thus deactivated after insulin bolus, leading to inhibition of glycogenolysis within 30 min (Fig. 1d). We did not find initiation of glycogen synthesis by activating dephosphorylation of GYS at S641 within 3 h of insulin stimulation (Fig. 1d), although its negative regulator glycogen synthase kinase-3β (GSK3B) appeared to be inactivated by phosphorylation at S935 (Supplementary Fig. 2d), probably because glycogen levels were high in iPSC-Heps at baseline (Supplementary Fig. 2e). Nevertheless, the net result of insulin’s effects on iPSC-Heps was glycogen accumulation as evidenced by comparison to cells treated with glucagon (Fig. 1e). These results establish that the functions constituting glucose metabolism are fully developed in iPSC-Heps and subject to regulation by insulin and glucagon.
M1 iPSC-Macs cause inflammation and insulin resistance in iPSC-Heps
Previous studies used iPSCs to model fatty liver disease, including macrophage-mediated inflammation, but they focused on lipid metabolism and fibrosis36,37. To investigate how macrophage-mediated inflammation affects glucose metabolism in iPSC-Heps, we co-cultured them with M1 or M0 iPSC-Macs generated from the same healthy-donor iPSC line (WTC38) using our recently published differentiation protocol39 (Supplementary Fig. 1a). Because macrophages are thought to disrupt glucose metabolism by secreting pro-inflammatory cytokines40, we established indirect 24-h co-culture of iPSC-Heps with M1 or M0 iPSC-Macs in a cell-impermeable transwell system (Fig. 2a). Before co-culture we confirmed that iPSC-Macs are viable and express principal markers of the hematopoietic and monocytic lineages as well as activation-specific markers (Supplementary Fig. 3a, b).
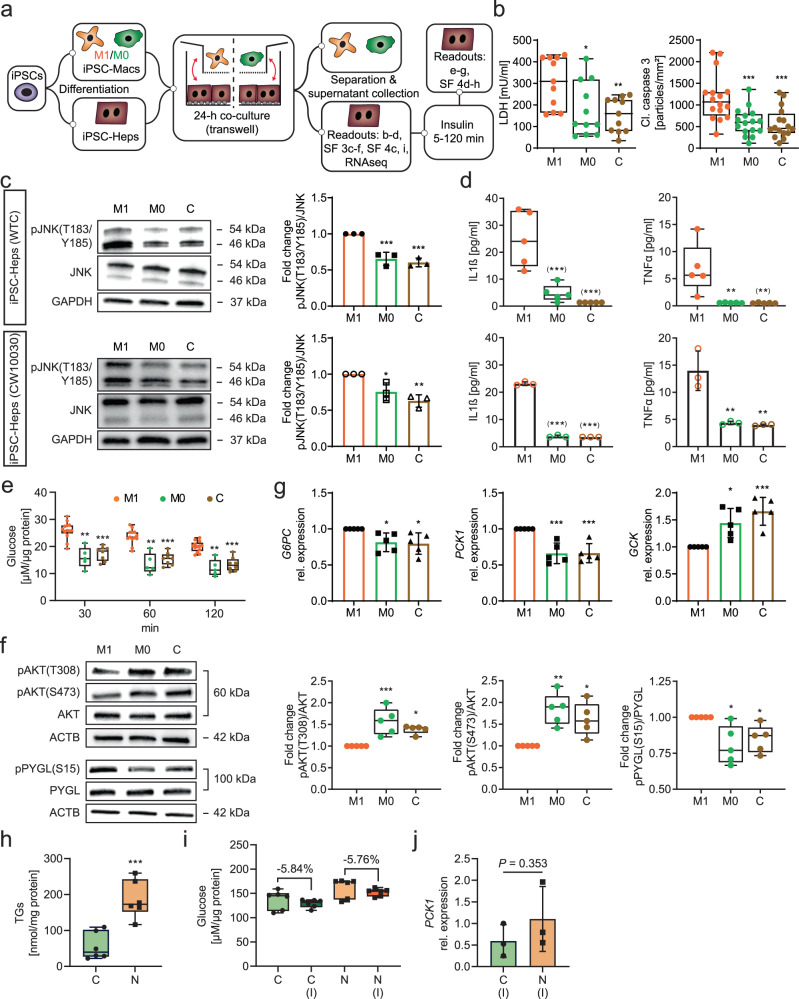
Fig. 2. Inflammation and glucose metabolism changes in iPSC-Heps co-cultured with M1 or M0 iPSC-Macs or accumulating lipid.
a Overview of experimental approach. SF, Supplementary Fig. b Quantification of LDH in media (n = 11) and of immunofluorescence of cleaved caspase 3 particles in iPSC-Heps (n = 4, 3 random regions/n). Data are mean ± SD; one-way ANOVA (Dunnett’s test), *P < 0.05, **P < 0.01 and ***P < 0.001 vs. M1. c, d Western blot analysis of JNK phosphorylation in iPSC-Heps (n = 3) (c) and pro-inflammatory cytokine release into media (WTC: n = 5, CW10030: n = 3) (d) after 24-h co-culture of iPSC-Heps with M1 or M0 iPSC-Macs or in iPSC-Hep mono-culture (C, control) comparing cells generated from the WTC and CW10030 iPSC lines. Data are mean ± SD; one-way ANOVA (Dunnett’s test), *P < 0.05, **P < 0.01 and ***P < 0.001 vs. M1. Asterisks in parentheses indicate values set to the detection limit of the assay. e–g Time course of analysis of glucose release into 1 mM glucose-containing media after insulin (M1: n = 13, M0: n = 5, C: n = 8) (e), western blot analysis of AKT and PYGL phosphorylation in iPSC-Heps 30 min after insulin (n = 5) (f) and gene expression analysis in iPSC-Heps 1 h after insulin (n = 5) (g) after 24-h co-culture of iPSC-Heps with M1 or M0 iPSC-Macs or in iPSC-Hep mono-culture (C, control). Data are mean ± SD; two-way (e) or one-way (f, g) ANOVA (Dunnett’s test), *P < 0.05, **P < 0.01 and ***P < 0.001 vs. M1. h–j Quantification of triglycerides (TGs) in iPSC-Heps (n = 6) (h), quantification of glucose release into 1 mM glucose-containing media after 2 h without or with insulin (I) (n = 6) (i) and gene expression analysis in iPSC-Heps 1 h after insulin (n = 3) (j) comparing iPSC-Heps from 3 healthy (C, control) and 3 NASH (N) patients. Data are mean ± SD; unpaired two-tailed Student’s t test, ***P < 0.001. Source data are provided as a Source Data file.
First, we assessed manifestation of inflammation of iPSC-Heps, which showed that co-culture with M1 iPSC-Macs, but not with M0 iPSC-Macs or mono-culture, causes damage and death, as evidenced by measurement of lactate dehydrogenase (LDH) in the media and cleaved caspase 3 immunofluorescence (Fig. 2b, Supplementary Fig. 3c). Analysis of CASP1, CASP4 and CASP5 gene expression pointed to pyroptosis as a mechanism involved in iPSC-Hep death, which accords with previous findings in mice41 (Supplementary Fig. 3d). Moreover, we found activation of the NF-κB and JNK signaling pathways, which are known to play prominent roles in inflammation-induced hepatocyte damage and hepatic insulin resistance42. Specifically, in addition to increased expression of the marker genes NFKB2 and TNF, we found increased phosphorylation of JNK at T183/Y185 in iPSC-Heps co-cultured with M1 iPSC-Macs; we confirmed these results in another healthy-donor iPSC line (CW1003043) (Fig. 2c, Supplementary Fig. 3e). In accord, pro-inflammatory cytokines such as IL1β, TNFα, IL6 and interferon γ (IFNγ) were much more abundant in media from co-cultures of iPSC-Heps with M1 than with M0 iPSC-Macs or from iPSC-Hep mono-cultures, despite a mitigating effect of iPSC-Heps on cytokine and chemokine release by M1 iPSC-Macs (Fig. 2d, Supplementary Fig. 3f).
Next, we asked whether insulin sensitivity and functions constituting glucose metabolism are affected in iPSC-Heps by iPSC-Mac co-culture. Indeed, after insulin bolus we found higher glucose levels in media from co-cultures of iPSC-Heps with M1 than with M0 iPSC-Macs or from iPSC-Hep mono-cultures (Fig. 2e). In contrast to M1 iPSC-Mac co-culture, 24-h treatment with any one of the pro-inflammatory cytokines IL1β, TNFα, IL6 or IFNγ—at a dose reportedly causing damage and impaired insulin signaling in primary hepatocytes13–15,44—failed to increase LDH or post-insulin glucose levels in media from iPSC-Hep mono-cultures (Supplementary Fig. 4a, b). Thus, iPSC-Heps mimic in vitro the resilience characteristic for primary hepatocytes in vivo45–47, which excludes that M1 iPSC-Mac-induced insulin resistance of iPSC-Heps is a mere byproduct of damage or death. Moreover, these results highlight that the complexity of the interaction of M1 iPSC-Macs and iPSC-Heps cannot be faithfully replicated with single cytokines.
To determine how M1 iPSC-Macs disrupt insulin-mediated regulation of hepatic glucose production, we compared co-cultures of M1 or M0 iPSC-Macs with iPSC-Heps and iPSC-Hep mono-cultures using the readouts described in Fig. 1a. At baseline, we found no effect of iPSC-Mac co-culture on glycogen levels in iPSC-Heps (Supplementary Fig. 4c). After insulin bolus, we found increased IRS1 and IRS2 gene expression in iPSC-Heps co-cultured with M1 iPSC-Macs, indicating that the negative feedback loop observed in iPSC-Hep mono-cultures was disrupted; GLUT2 gene expression was not altered (Supplementary Figs. 4d, 2b). Moreover, inhibitory phosphorylation of IRS1 at S307 was increased in these cells, which has a negative effect on insulin signaling3 (Supplementary Fig. 4e). In accord, insulin-induced activation of AKT by phosphorylation at T308 and S473 was impaired (Fig. 2f), resulting in reduced activation of S6K1 by phosphorylation at T389 (Supplementary Fig. 4f). At the functional level, we found failure to downregulate G6PC and PCK1 and upregulate GCK gene expression in response to insulin, leading to increased gluconeogenesis and decreased glycolysis (Fig. 2g). In addition, glycogenolysis continued to be active despite insulin bolus, as evidenced by lack of dephosphorylation of PYGL at S15 (Fig. 2f). The effect of insulin on the phosphorylation of GYS at S641 in iPSC-Heps was similar among all culture conditions, excluding a substantial contribution of impaired glycogen synthesis to increased hepatic glucose production caused by M1 iPSC-Macs (Supplementary Fig. 4g). Gene expression of the lipogenic transcription factor SREBP-1c was decreased in iPSC-Heps co-cultured with M1 iPSC-Macs (Supplementary Fig. 4h), which further illustrates impaired AKT activation and excludes de novo lipogenesis as the cause of insulin resistance48,49. In accord, triglyceride staining showed no lipid accumulation in iPSC-Heps co-cultured with M1 iPSC-Macs (Supplementary Fig. 4i).
Prompted by the rapid onset of M1 iPSC-Mac-induced insulin resistance, we investigated whether lipid accumulation is similarly disruptive in iPSC-Heps using gluconeogenesis and glycolysis as readouts. We found that treatment with the fatty acids oleate and palmitate for 6 days caused steatosis but had no effect on insulin-mediated regulation of glucose production and PCK1 and GCK gene expression in iPSC-Heps in mono-culture (Supplementary Fig. 4j–l). We confirmed these results in iPSC-Heps genetically predisposed to lipid accumulation50. For this, we used iPSC lines from three donors homozygous for the PNPLA3 I148M variant who have biopsy-confirmed nonalcoholic steatohepatitis (NASH)43. Comparison to iPSC-Heps generated from three healthy-donor iPSC lines43 showed increased triglycerides in the NASH iPSC-Heps but normal insulin sensitivity as evidenced by unaltered glucose output and PCK1 and SREBP1c gene expression after insulin bolus (Fig. 2h–j, Supplementary Fig. 4m). In addition, gene expression of JUN, a transcription factor activated by JNK under lipotoxic conditions51, was unaltered (Supplementary Fig. 4n). These results show that M1 iPSC-Macs, but not steatosis, rapidly cause insulin resistance in iPSC-Heps by secreting one or more soluble factors—probably pro-inflammatory cytokines—that activate NF-κB and JNK signaling and thereby inhibit IRS-mediated activation of AKT52,53.
TNFα, IL1β and IFNγ mediate M1 iPSC-Mac-induced inflammation of iPSC-Heps
To identify the M1 iPSC-Mac-derived soluble factors responsible for causing inflammation and insulin resistance in iPSC-Heps, we investigated whether specific pathways were activated by RNA sequencing (RNAseq). Bioinformatic analysis revealed high similarity between iPSC-Hep mono-cultures and co-cultures with M0 iPSC-Macs, prompting us to focus on the 2937 genes significantly differentially expressed between iPSC-Heps co-cultured with M1 or M0 iPSC-Macs (Fig. 3a–c, Supplementary Data 1).
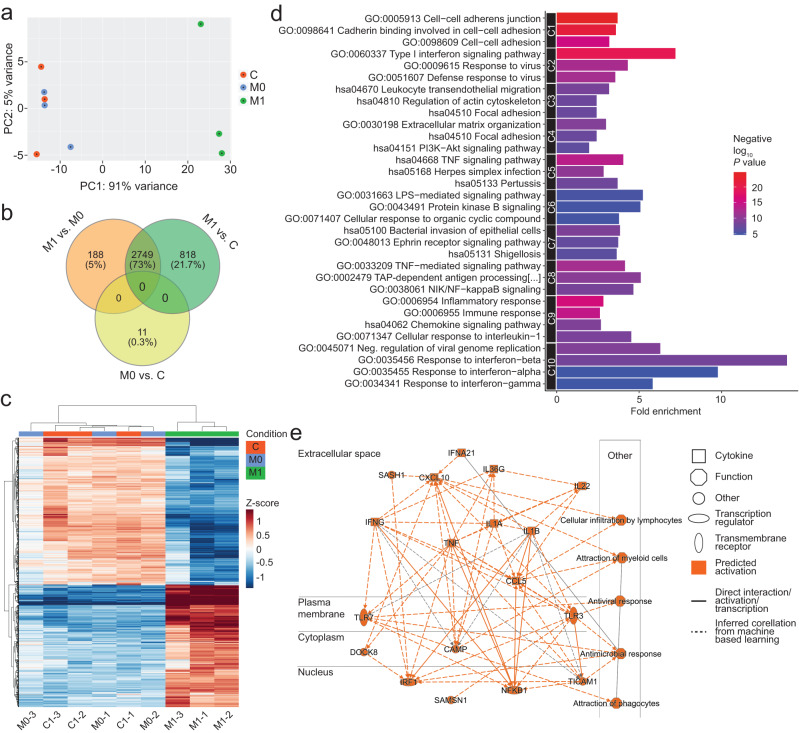
Fig. 3. RNAseq analysis of iPSC-Heps co-cultured with M1 or M0 iPSC-Macs.
a Principal component analysis of gene expression profile of iPSC-Heps after 24-h co-culture with M1 or M0 iPSC-Macs or in iPSC-Hep mono-culture (C, control). n = 3. b Venn diagram of significantly differentially expressed genes comparing the indicated conditions. n = 3, FDR-adjusted P value (P < 0.05) by Wald test. c Heatmap of the top 1000 differentially expressed genes in iPSC-Heps under the indicated conditions in three independent experiments. The Z-score represents the gene-wise deviation from the mean of the log-transformed and variance-stabilized read counts. n = 3. d Top 10 upregulated pathway clusters enriched (Cluster Enrichment Score > 1.3) in the genes differentially expressed between iPSC Heps co-cultured with M1 or M0 iPSC-Macs identified using DAVID. Vertical axis represents enrichment fold values and horizontal axis shows the names of GO-BP, GO-MF and GO-CC terms and KEGG pathways. Node color indicates the enrichment significance, red represents higher significance. n = 3, FDR-adjusted P value (P < 0.05) by Wald test. e Molecular activity predictor pathway analysis generated using IPA representing the regulatory effects with top consistency scores showing TNFα, IL1β and IFNγ as the pro-inflammatory cytokines most active on iPSC-Heps co-cultured with M1 iPSC-Macs. n = 3, FDR-adjusted P value (P < 0.05) by Wald test.
Functional annotation using Database for Annotation, Visualization and Integrated Discovery (DAVID) showed that many gene clusters related to inflammation were upregulated in iPSC-Heps co-cultured with M1 iPSC-Macs, with NF-κB, TNF, IL1 and IFN signaling being most significantly induced (Fig. 3d). In addition, CXCL2, CXCL9, CX3CL1 and CCL20, genes involved in chemotaxis and immune cell recruitment, were also upregulated (Supplementary Fig. 5a). In contrast, metabolic and synthetic functions were downregulated in iPSC-Heps co-cultured with M1 iPSC-Macs (Supplementary Fig. 5b).
To further substantiate these results, we investigated whether the observed gene expression changes could be linked to extracellular regulators using Ingenuity Pathway Analysis (IPA). This analysis confirmed TNFα, IL1β and IFNγ as the pro-inflammatory cytokines with the most profound effects on iPSC-Heps co-cultured with M1 iPSC-Macs (Fig. 3e). Moreover, IPA suggested that IL1β exerts its pro-inflammatory effects by activating the NFKB1 and IRF1 genes (Fig. 3e). These results show the prominent role of TNFα, IL1β and IFNγ in M1 iPSC-Mac-induced inflammation of iPSC-Heps.
Neutralizing M1 iPSC-Mac-derived TNFα and IL1β restores insulin sensitivity in iPSC-Heps
TNFα and IL1β have been independently pursued as therapeutic targets in clinical trials for type 2 diabetes and systemic insulin resistance54–56. To determine the contribution of these pro-inflammatory cytokines to M1 iPSC-Mac-induced insulin resistance in iPSC-Heps, we inhibited them individually or in combination in co-cultures of iPSC-Heps with M1 iPSC-Macs using neutralizing antibodies.
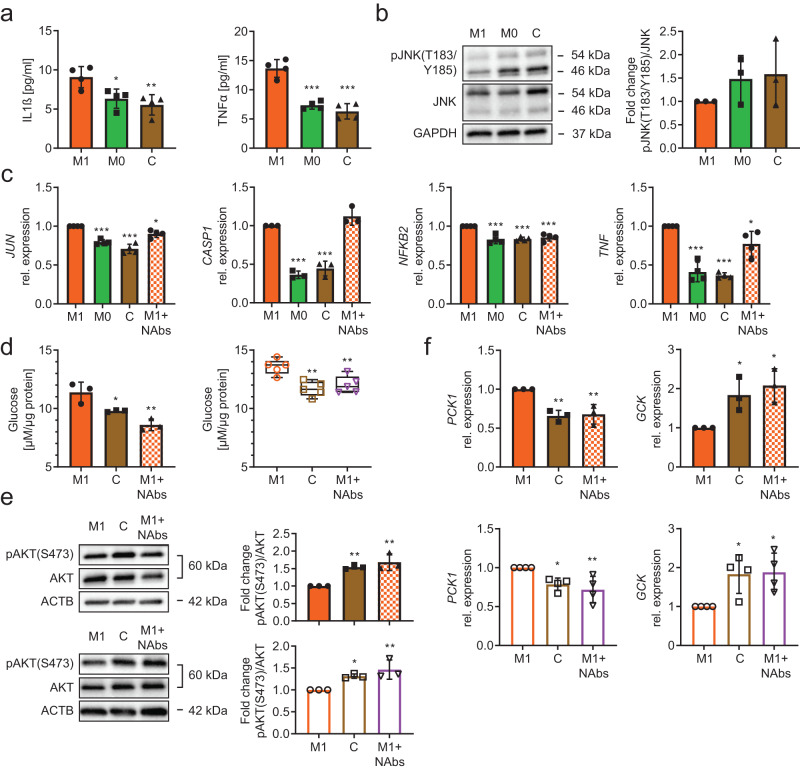
Media LDH levels and CASP1 gene expression indicated iPSC-Heps were not protected from damage or death by TNFα and/or IL1β neutralization (Fig. 4a, Supplementary Fig. 6a). However, NF-κB and JNK signaling was mitigated by neutralization of TNFα alone or in combination with IL1β, as evidenced by reduction of NFKB2 or TNF gene expression, respectively (Fig. 4b, Supplementary Fig. 6a). Neutralization of IL1β alone or in combination with TNFα was effective in reducing activating phosphorylation of JNK at T183/Y185 (Fig. 4c). Interestingly, TNFα neutralization also impacted M1 iPSC-Macs, not their principal polarization but susceptibility to recruitment as evidenced by analysis of CD86 and CCR2 cell surface levels57 (Supplementary Fig. 6b).
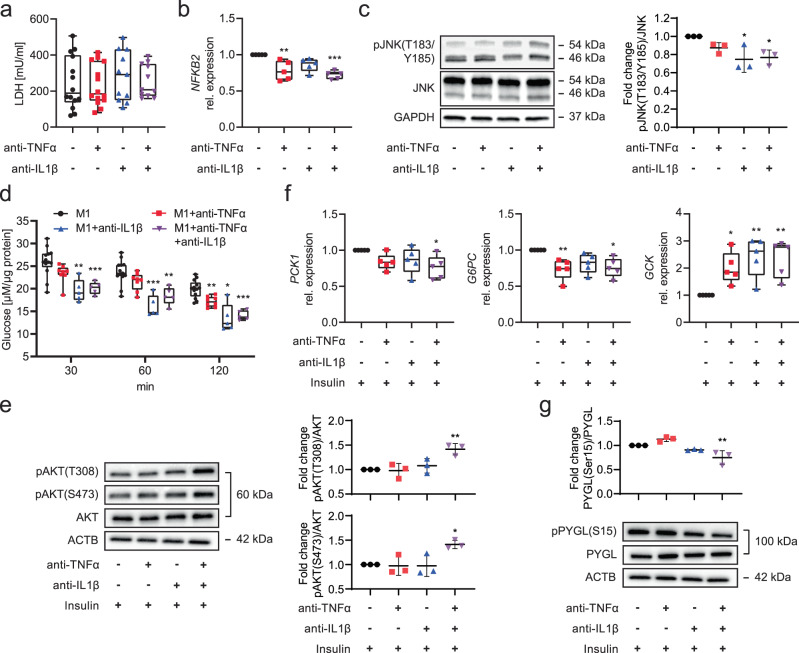
Fig. 4. Effect of TNFα and/or IL1β neutralization on inflammation and glucose metabolism changes in iPSC-Heps co-cultured with M1 iPSC-Macs.
a–c Quantification of LDH in media (M1 and M1+anti-TNFα: n = 14, M1+anti-IL1β and M1+anti-TNFα+anti-IL1β: n = 11) (a), gene expression analysis in iPSC-Heps (n = 5) (b) and western blot analysis of JNK phosphorylation in iPSC-Heps (n = 3) (c) after 24-h co-culture of iPSC-Heps with M1 iPSC-Macs and indicated antibody treatments. Data are mean ± SD; one-way ANOVA (Dunnett’s test), *P < 0.05, **P < 0.01 and ***P < 0.001 vs. no-antibody condition. d–g Time course of analysis of glucose release into 1 mM glucose-containing media after insulin (M1: n = 13, M1+anti-TNFα: n = 8, M1+anti-IL1β and M1+anti-TNFα+anti-IL1β: n = 5) (d), western blot analysis of AKT phosphorylation in iPSC-Heps 30 min after insulin (n = 3) (e), gene expression analysis in iPSC-Heps 1 h after insulin (n = 5) (f) and western blot analysis of PYGL phosphorylation in iPSC-Heps 30 min after insulin (n = 3) (g) after 24-h co-culture of iPSC-Heps with M1 iPSC-Macs and indicated antibody treatments. Data are mean ± SD; two-way (d) and one-way (e–g) ANOVA (Dunnett’s test), *P < 0.05, **P < 0.01 and ***P < 0.001 vs. no-antibody condition. Source data are provided as a Source Data file.
Next, we investigated the effect of TNFα and/or IL1β neutralization on insulin sensitivity and functions constituting glucose metabolism in iPSC-Heps co-cultured with M1 iPSC-Macs. We found that media glucose levels were reduced by IL1β neutralization, alone or in combination with TNFα, at 30 min and for 2 h after insulin bolus; in contrast, neutralization of TNFα alone showed an effect only after 2 h (Fig. 4d). At the signaling level, TNFα and/or IL1β neutralization only partially restored the insulin-dependent negative feedback loop regulating the INSR complex, as evidenced by suppression of gene expression of IRS2, but not IRS1, and unaltered phosphorylation of IRS1 at S307 (Supplementary Fig. 6c, d). However, neutralization of both TNFα and IL1β restored activating phosphorylation of AKT at T308 and S473 (Fig. 4e). At the functional level, we found that neutralization of TNFα alone or in combination with IL1β promoted insulin-induced reduction of gene expression of G6PC but not PCK1, which required neutralization of both TNFα and IL1β; GCK gene expression was increased after neutralization of TNFα and/or IL1β (Fig. 4f). Neutralization of both TNFα and IL1β caused deactivating dephosphorylation of PYGL at S15 (Fig. 4g). These results show that M1 iPSC-Macs disrupt insulin-mediated regulation of gluconeogenesis, glycolysis and glycogenolysis in iPSC-Heps by secreting TNFα and IL1β and that both must be neutralized to restore insulin sensitivity to near normal.
TNFα and IL1β neutralization reverses inflammation-induced insulin resistance in PHHs
Finally, we determined whether our iPSC-based model accurately reflects primary cells. We found a similar pattern of increased IL1β and TNFα media levels in 24-h co-cultures of PHHs with M1 PHMs, with more contribution from PHHs than observed for iPSC-Heps (Figs. 5a, 2d). Because we could not detect differences in phosphorylation of JNK at T183/Y185 between PHHs co-cultured with M1 or M0 PHMs, or PHH mono-cultures, at this time point (Fig. 5b), we generated a time course, which showed that this modification of JNK already occurred in PHHs after 2 h of co-culture with M1 PHMs (Supplementary Fig. 7a). While JNK phosphorylation subsequently declined, gene expression of the effector of JNK-mediated inflammation JUN remained increased in PHHs after 24 h of co-culture with M1 PHMs (Fig. 5c). Combined antibody-mediated neutralization of IL1β and TNFα was effective in reversing increased gene expression of JUN, NFKB2 and TNF but not CASP1 at this time point (Fig. 5c), exactly as in our iPSC-based model (Fig. 4b, Supplementary Fig. 6a).
Fig. 5. Effect of TNFα and/or IL1β neutralization on inflammation and glucose metabolism changes in PHHs co-cultured with M1 PHMs.
a, b Pro-inflammatory cytokine release into media (n = 4) (a) and western blot analysis of JNK phosphorylation (n = 3) (b) in PHHs after 24-h co-culture with M1 or M0 PHMs or in PHH mono-culture (C, control). Data are mean ± SD; one-way ANOVA (Dunnett’s test), *P < 0.05, **P < 0.01 and ***P < 0.001 vs. M1. c Gene expression analysis of PHHs after 24-h co-culture with M1 or M0 PHMs, in PHH mono-culture (C, control) or after 24-h co-culture with M1 PHMs including TNFα and IL1β neutralizing antibodies (M1+NAbs). Data are mean ± SD; JUN, NFKB2, TNF: n = 4, CASP1: n = 3, one-way ANOVA (Dunnett’s test), *P < 0.05 and ***P < 0.001 vs. M1. d–f Analysis of glucose release into 1 mM glucose-containing media 2 h after insulin (primary cells: n = 3, CW10030 iPSC-derived cells: n = 5) (d), western blot analysis of AKT phosphorylation 30 min after insulin (n = 3) (e) and gene expression analysis 1 h after insulin (primary cells: n = 3, CW10030 iPSC-derived cells: n = 4) (f) in hepatocytes after 24-h co-culture with M1 macrophages or in hepatocyte mono-culture (C, control) or after 24-h co-culture with M1 macrophages including TNFα and IL1β neutralizing antibodies (M1+NAbs). Primary cells, filled bars/symbols; CW10030 iPSC-derived cells, open bars/symbols. Data are mean ± SD; one-way ANOVA (Dunnett’s test), *P < 0.05 and **P < 0.01 vs. M1. Source data are provided as a Source Data file.
We also investigated inflammation-induced insulin resistance in co-cultures of PHHs and PHMs. We performed these experiments side by side with iPSC-Heps and iPSC-Macs generated from the CW10030 line to facilitate direct comparison and validate our results obtained with the WTC iPSC line. For both primary cells and iPSC derivatives, after insulin bolus we found higher media glucose levels, impaired activation of AKT by phosphorylation at S473 and failure to downregulate PCK1 and upregulate GCK gene expression in co-cultures of hepatocytes with M1 macrophages, indicating insulin resistance in hepatocytes, which could be reversed by neutralization of IL1β and TNFα (Fig. 5d–f). We also confirmed in primary cells our finding made in iPSC derivatives that M1 macrophages induce gene expression of G6PC in hepatocytes, including IL1β and TNFα acting as mediators (Supplementary Fig. 7b). Primary-cell co-cultures differed from co-cultures of derivatives of both iPSC lines in that insulin dephosphorylated PYGL at S15 in PHHs normally whereas phosphorylation of GSK3B at S9 was impaired in PHHs by IL1β and TNFα released by M1 PHMs (Supplementary Fig. 7c, d), resulting in decreased glycogenolysis and increased glycogen synthesis, probably as a result of much lower glycogen levels in PHHs than in iPSC-Heps (Supplementary Fig. 2e).
Discussion
Here we developed an iPSC-based model of hepatic insulin resistance, a common clinical condition that drives type 2 diabetes and fatty liver disease in obesity. For this, we generated iPSC-Heps with hormone-regulated glucose metabolism and, to define the impact of inflammation, established co-culture with isogenic M1 or M0 iPSC-Macs. We ascertained the authenticity of our iPSC-based model by comparison to co-cultures of PHHs with PHMs.
Specifically, our iPSC-Heps replicate the physiological hepatic glucose production identified in clinical studies58, including rapid response to insulin and glucagon boluses. Our iPSC-Heps also replicate the mechanistic underpinnings, that is, the complex hepatic insulin signaling cascade regulating gluconeogenesis, glycolysis and glycogen metabolism, which could thus far only be studied in animal models and primary hepatocytes17,59. In addition, as reported for hepatocytes in patients with fatty liver disease60, we found that our iPSC-Heps undergo inflammation-induced damage and death (possibly pyroptosis) when exposed to M1 iPSC-Macs. Moreover, our iPSC-Heps respond to M1 iPSC-Mac co-culture by downregulating metabolic and synthetic functions, which supports clinical data suggesting hepatocyte dedifferentiation as a driver of fatty liver disease61,62.
Taking advantage of the responsiveness of our iPSC-Heps to co-culture with M1 iPSC-Macs, we investigated whether macrophage-mediated inflammation is sufficient to induce hepatic insulin resistance. Indeed, we found increased glucose output by iPSC-Heps co-cultured with M1 iPSC-Macs in the absence of steatosis. Moreover, we found that iPSC-Heps remain insulin sensitive in two models of steatosis: exogeneous fatty acid challenge and genetic predisposition caused by the PNPLA3 I148M variant50. The latter finding is consistent with the clinical observation that PNPLA3 I148M-associated steatosis is not linked to hepatic insulin resistance50,63. These findings highlight the rapid and profound effect of macrophage-mediated inflammation on insulin signaling and glucose metabolism in hepatocytes and question whether lipid accumulation alone causes insulin resistance4. In accord, reports that steatosis-induced hepatic insulin resistance coincides with lipotoxicity and ER stress suggest involvement of some of the same inflammatory signaling pathways as induced by macrophages, particularly JNK52,64,65.
At the mechanistic level, we found that multiple dysfunctions—increased gluconeogenesis and glycogenolysis and decreased glycolysis—contribute to M1 iPSC-Mac-induced insulin resistance in iPSC-Heps, which accords with original observations in patients with hepatic insulin resistance in the setting of type 2 diabetes66–68 but is at odds with findings in animal models that the acute action of insulin in hepatocytes is limited to glycogen metabolism34,69. In fact, we found that insulin has a strong effect on glycogenolysis but none on glycogen synthesis in iPSC-Hep mono-cultures. However, this finding is probably due to high glycogen levels in iPSC-Heps leading to suppression of glycogen synthesis because insulin’s effects in co-cultures of M1 PHMs with PHHs with low glycogen levels were reversed70, which warrants further studies of the regulation of the enzymes involved in glycogen homeostasis, including the effects of allosteric regulation71.
The authentic interplay between our iPSC-Heps and M1 iPSC-Macs allowed us to identify TNFα and IL1β as the cytokines causing inflammation and insulin resistance in iPSC-Heps. Neutralization of these cytokines revealed specificity in how they cause inflammation, with TNFα acting through NF-κB and IL1β through JNK, both pathways implicated in hepatic insulin resistance52,53. These cytokines also differed in effect on insulin-regulated glucose production by iPSC-Heps, with TNFα acting slower and weaker than IL1β. These findings suggest that decreased glycolysis plays a major role in inflammation-induced insulin resistance in iPSC-Heps because glycolysis has been shown in mice to be more affected by IL1β than TNFα72.
In accord with different mechanisms of action, neutralization of both TNFα and IL1β showed an additive effect on insulin resistance in iPSC-Heps, which we confirmed in PHHs co-cultured with PHMs. Together, these findings provide an explanation for mixed outcomes of clinical trials in which either of these cytokines was inhibited to restore systemic insulin sensitivity in patients with type 2 diabetes56.
Our finding that single TNFα or IL1β boluses failed to increase glucose output by iPSC-Heps shows that faithful modeling of macrophage-induced inflammation of hepatocytes requires sustained secretion and interaction of multiple cytokines as provided by iPSC-Mac co-culture. By using iPSC-Heps and iPSC-Macs generated from the same iPSC line our model facilitates bias-free validation of genetic risk factors and screens for new therapeutic targets. Along these lines, our model could readily be expanded to include gene editing and other iPSC-derived cell types to study the effects of hepatic insulin resistance on metabolic disease progression in and outside the liver.
In summary, our results establish the efficacy of iPSC-Hep and iPSC-Mac co-culture as an authentic and tunable model of inflammation-induced hepatic insulin resistance that facilitates in-depth mechanistic studies and development of new therapies.
Methods
Experimental model and iPSC culture
The human male healthy-donor iPSC line GM25256 (WTC38) was used for most experiments. In addition, the healthy-donor iPSC lines CW10001, CW10030 and CW10037 and the NASH-patient iPSC lines CW10152, CW10201 and CW10208 from the CIRM iPSC Repository available at Fujifilm Cellular Dynamics were used43. Undifferentiated iPSCs were cultured in mTeSR1 (StemCell Technologies) in six-well plates coated with Cultrex Reduced Growth Factor Basement Membrane Extract (RGF-BME; R&D Systems) at 1:30 dilution in Knockout DMEM (Gibco) at 37 °C in 5% CO2 and 5% O2.
Differentiation of iPSC-Heps
Differentiation was performed at 37 °C in 5% CO2 and 5% O2 unless stated otherwise. iPSCs were differentiated into iPSC-Heps using a refined version of a previously published protocol73. At 70 to 80% confluency, colonies of iPSCs were detached using Accutase (StemCell Technologies) and 100,000 cells/cm² diluted in mTeSR1 including 10 μM Y-27632 (Thermo Fisher Scientific) were seeded in RGF-BME-coated six-well plates. After 24 h, medium was changed to endoderm-induction medium (EIM), consisting of RPMI 1640 (Life Technologies) containing 2% Gem21 without insulin (GeminiBio), 1% Glutamax (Gibco), 1% non-essential amino acids solution (NEAA; Gibco), 0.5 mM sodium butyrate (Sigma-Aldrich) and 100 ng/ml activin A (StemCell Technologies), for 7 days in 20% O2. The following compounds were added to EIM during the first 3 days: 3 μM CHIR (StemCell Technologies) on day 1, 20 ng/ml basic fibroblast growth factor (FGFb; Peprotech) and 10 ng/ml bone morphogenetic protein 4 (BMP4; Peprotech) on days 1 and 2, 50 nM PI103 (Thermo Fisher Scientific) on days 1 to 3, knockout serum replacement (KSR; Life Technologies) at 2% on day 1, 1% on day 2 and 0.2% on day 3.
On days 8 to 17, cells were cultured in hepatic induction medium (HIM), consisting of IMDM (Thermo Fisher Scientific) containing 1% Glutamax, 1% NEAA, 100 nM dexamethasone (Sigma-Aldrich), 100 nM insulin (GeminiBio) and 0.5 mM 1-thioglycerol (Sigma-Aldrich). The following compounds were added to HIM between days 8 and 17: 10 ng/ml FGFb and 20 ng/ml BMP4 between days 8 and 17, 20 ng/ml hepatocyte growth factor (HGF; Peprotech) between days 12 and 17. On day 10, cells were detached using 0.25% trypsin-EDTA (Gibco) and split 1:2 into RGF-BME-coated 12 or 24-well plates.
On days 18 to 22, cells were cultured in Hepatocyte Culture Medium BulletKit (HCM; Lonza) without epidermal growth factor, including 20 ng/ml oncostatin M (Peprotech) and 20 ng/ml HGF in 20% O2. After day 22 (end of differentiation), iPSC-Heps were used within 7 days for experiments. Medium was changed daily during differentiation and maintenance.
PHH culture
Cryopreserved, plateable PHHs (Lot: BMO) were purchased from BioIVT; the cells were reported to be metabolically active and isolated from a 45-year-old Caucasian male with BMI of 22.6 and no history of excessive alcohol consumption or smoking. PHHs were plated at a density of 250,000 viable cells/cm² in collagen I-coated 24-well plates (Corning) in INVITROGRO CP medium (BioIVT). After attachment, media was changed to HCM including 20 ng/ml HGF at 37 °C in 5% CO2 and 5% O2. After 24 h, PHHs were used for co-culture experiments and analyzed the same way as iPSC-Heps.
Differentiation of iPSC-Macs
M1 and M0 iPSC-Macs were generated using a recently published protocol (M0 there referred to as M2)39. iPSC-Macs were seeded and polarized in ThinCert transwell inserts with 0.4 μm pore size (Greiner BioOne) 24 h before co-culture with iPSC-Heps.
Isolation and differentiation of PHMs
Human peripheral blood mononuclear cells (PBMCs) from three healthy male donors were isolated by Biocoll (Sigma-Aldrich) density gradient centrifugation. PBMCs were washed and seeded in six-well plates at a density of 1 × 106 cells/cm2 in Monocyte Attachment Medium (PromoCell). After attachment, monocytes were washed three times with PBS to remove non-adherent cells and differentiated into macrophages in ImmunoCult Macrophage Medium (StemCell Technologies) including 100 ng/ml MCSF for 7 days at 37 °C in 5% CO2 and 5% O2 with media exchange every 2 days. Purity of adherent monocytes was verified 24 h after isolation by flow cytometry analysis of CD14. After 7 days, PHMs were detached using Accutase, seeded and polarized in ThinCert transwell inserts with 0.4 μm pore size 24 h before co-culture with PHHs, as done for iPSC-Macs.
Co-culture of iPSC-Heps/PHHs with iPSC-Macs/PHMs and cytokine neutralization
iPSC-Heps were cultured in 24-well plates without iPSC-Macs or with isogenic M1 or M0 iPSC-Macs at a ratio of 6:1 in a 50:50 mixture of HCM without insulin and hydrocortisone and RPMI including 10% fetal bovine serum (Gibco), 1% penicillin/streptomycin (Gibco) and 100 ng/ml MCSF (Peprotech). PHHs and PHMs were co-cultured the same way. For cytokine neutralization, antibodies against TNFα (Infliximab; Selleckchem) or IL1β (Human IL-1 beta/IL-1F2 Antibody; R&D Systems) were added to co-culture medium at 5 μg/ml or 0.2 μg/ml, respectively. The transwell inserts containing iPSC-Macs/PHMs were removed after 24 h of co-culture for subsequent analysis of media and cells and for hormonal stimulation of iPSC-Heps/PHHs.
Hormonal stimulation of iPSC-Heps
iPSC-Heps were cultured without dexamethasone and insulin for 24 h at 37 °C in 5% CO2 and 20% O2. After washing twice with PBS, medium was changed to DMEM (Gibco) containing 2 mM sodium pyruvate (Gibco), 10 mM sodium lactate (Sigma-Aldrich) and 5.55 mM glucose (Gibco) unless stated otherwise in the figure legends. In addition, 100 nM glucagon (EMD Millipore) was added 1 h (except Fig. 1b, c and Supplementary Fig. 2a, b) before stimulation with 100 nM insulin. Hormonal stimulation of PHHs was done the same way.
Oxygen consumption measurements
Mitochondrial respiration in the presence of electron transport chain inhibitors and uncouplers (oligomycin, 1.5 μM; carbonyl cyanide-p-trifluoromethoxyphenylhydrazone, 2 μM; rotenone, 0.5 μM; antimycin A, 0.5 μM) was measured in adherent iPSCs and iPSC-Heps using a Seahorse XFe24 Analyzer (Agilent) and the Mito Stress Test Kit (Agilent) according to the manufacturer’s instructions. Oxygen consumption rates were normalized in each well by the number of cells assessed by nucleus counting after Hoechst 33342 (Sigma-Aldrich) staining using CellProfiler image analysis software.
Fatty acid treatment of iPSC-Heps
iPSC-Heps were cultured without dexamethasone and insulin and treated every 48 h with 100 μM oleate (Sigma-Aldrich) and 100 μM palmitate (Sigma-Aldrich) for 6 days.
Cytokine stimulation of iPSC-Heps
Fully differentiated iPSC-Heps were stimulated with either IL1β (10 ng/ml; Peprotech), TNFα (20 ng/ml; Peprotech), IL6 (20 ng/ml; Peprotech) or IFNγ (20 ng/ml; Peprotech) for 24 h in HCM without insulin and hydrocortisone before analysis.
RNA isolation
RNA was isolated using PureLink RNA Mini Kit (Invitrogen) according to the manufacturer’s instructions.
qRT-PCR
cDNA was synthesized from purified RNA using qScript cDNA SuperMix (QuantaBio) according to the manufacturer’s instructions. qRT-PCR was performed using SYBR Green PCR Master Mix (Applied Biosystems) in a ViiA 7 Real-Time PCR system (Applied Biosystems) using Quantstudio Real-Time PCR software (Applied Biosystems) for analysis. Oligonucleotide primers for each target gene were designed using the Primer3Plus website and synthesized by Integrated DNA Technologies. Relative mRNA expression was determined by the ΔΔ-Ct method normalized to RPLP0. Primers for qRT-PCR are listed in Supplementary Table 1.
Immunofluorescence and triglyceride staining
Cells were washed twice with PBS and fixed with 4% paraformaldehyde (Thermo Fisher Scientific) in PBS for 10 min at room temperature. Afterwards, cells were washed three times and blocked/permeabilized in PBS containing 0.1% saponin (Sigma-Aldrich) and 3% normal donkey serum (NDS; Thermo Fisher Scientific) for 1 h at room temperature. Primary antibody incubation was performed at 4 °C overnight in PBS containing 0.1% saponin and 0.3% NDS. Afterwards, cells were washed three times with PBS containing 0.1% saponin and incubated for 1 h in PBS containing 0.1% saponin and 0.3% NDS with the respective secondary antibody. For triglyceride staining, permeabilized cells were incubated for 1 h with 2.5 μM BODIPY 493/503 (Cayman Chemicals) in PBS containing 0.1% saponin. Nuclei were stained with DAPI (Thermo Fisher Scientific). Cells were mounted in Fluoromount-G (Southern Biotech) before analysis. Images were acquired using an IX-71 microscope (Olympus). 4 random regions were analyzed per sample for quantification. Primary and secondary antibodies are listed in Supplementary Table 2.
Mitochondria and viability staining
For mitochondria staining, iPSCs and iPSC-Heps were washed once with PBS and incubated in PBS containing Hoechst 33342 (341/486 nm) and MitoTracker Red FM (mitochondrial potential-dependent; Thermo Fisher Scientific) at 500 nM for 20 min at 37 °C and 5% CO2 in the dark. Staining solution was then removed, cells were washed three times with PBS and immediately imaged using a BioTek Cytation cell imaging reader (BioTek). For viability staining, iPSC-Heps were washed once with PBS and incubated in PBS containing 1 μM Calcein-AM (Biolegend) and 1 μg/ml propidium iodide (Sigma-Aldrich) for 15 min. Staining solution was then removed, cells were washed twice with PBS and images were acquired using an Olympus IX-71 microscope.
Triglyceride measurements
Triglycerides were measured using the Triglyceride Assay Kit (Biovision) according to the manufacturer’s instructions. Briefly, iPSC-Heps were homogenized in 200 μl 5% NP-40 after which samples were slowly heated twice to 100 °C for 3 min followed by cooling to room temperature. Subsequently, samples were centrifuged at 16,000 × g, supernatants were mixed with lipase for 20 min and then glycerol content was measured using a Synergy HT microplate reader (BioTek). Results were normalized to the total cellular protein content. Triglycerides were also measured using the Triglyceride-Glo assay (Promega) according to the manufacturer’s instructions and analyzed using a Synergy HT microplate reader.
Flow cytometry analysis
Freshly thawed PHHs, PHMs detached using Accutase, fully differentiated iPSC-Heps detached using 0.25% trypsin-EDTA and M1/M0 iPSC-Macs detached using Accutase were incubated with the respective antibodies in PBS including 0.1% BSA and 2 mM EDTA for 20 min at 4 °C and washed once before flow cytometry analysis. Antibodies are listed in Supplementary Table 2. Viable cells were distinguished using SYTOX Green/Blue Dead Cell Stain (Invitrogen). Unstained cells were used as control. Cells were analyzed using a LSRFortessa flow cytometer (BD Biosciences) and FloJo software (v10.6.1; BD Biosciences). A representative gating strategy example is shown in Supplementary Fig. 8.
Cytokine analysis
Cytokine concentrations were measured in co-culture supernatants using LEGENDplex Human Inflammation Panel 1 (Biolegend) according to the manufacturer’s instructions, analyzed using a LSRFortessa flow cytometer and quantified using LEGENDplex software (Biolegend). In addition, samples were sent to Eve Technologies for analysis with the Human Cytokine/Chemokine 48-Plex Discovery Assay (HD48); fluorescence intensity was used to generate cytokine heatmaps.
Protein quantification and western blotting
All procedures were performed on ice or at 4 °C unless stated otherwise. Cells were lysed for 10 min in 1x RIPA buffer (Cell Signaling) including Halt Proteinase and Phosphatase Inhibitor Cocktail (Thermo Fisher Scientific). Lysates were centrifuged at 16,000 × g for 20 min. Protein concentration was measured using Pierce BCA Protein Assay Kit (Thermo Fisher Scientific) kit according to the manufacturer’s instructions. 4-15% pre-cast gels (Bio-Rad) were loaded with equal protein amounts for each individual experiment and run at 100 V for 75 min at room temperature. Protein was transferred to a nitrocellulose membrane (Bio-Rad) in transfer buffer at 100 V for 60 min. Membranes were blocked for 1 h at room temperature in TBS buffer containing 0.1% Tween 20 (TBST; Thermo Fisher Scientific) and 5% milk. Membranes were washed once in TBST and incubated in primary antibody solution (TBST containing 5% bovine serum albumin) overnight. Membranes were washed thrice in TBST and incubated for 1 h at room temperature in secondary antibody solution (TBST containing 5% bovine serum albumin). Chemiluminescence assays were performed using Pierce ECL Western Blotting Substrate (Thermo Fisher Scientific) and detected with a ChemiDoc XRS+ system (Bio-Rad). Image analyses and band density quantification were performed using Image Lab software (Bio-Rad) and FIJI open-source software. Quantification of relative protein phosphorylation changes was done separately for each biological replicate/individual blot. Primary and secondary antibodies are listed in Supplementary Table 2.
Glucose measurement
Glucose in media was measured using Amplex Red Glucose/Glucoseoxidase Kit (Invitrogen) according to the manufacturer’s instructions. Glucose concentration was normalized to total cellular protein.
LDH measurement
LDH in media was measured using LDH Cytotoxicity Assay (ScienCell) according to the manufacturer’s instructions.
Glycogen staining and measurement
Glycogen staining was performed using Epredia’s Perodic Acid Schiff Kit (Thermo Fisher Scientific) according to the manufacturer’s instructions. Intracellular glycogen was quantified using the Glycogen-Glo assay (Promega) according to the manufacturer’s instructions.
RNA sequencing and bioinformatic analysis
mRNA library preparation with polyA enrichment and sequencing was performed by Novogene. Sequencing reads were aligned to the human reference genome GRCh38.96 and reads per gene matrix were counted with the latest Ensemble annotation build using STAR_2.7.2b74. Read counts per gene were used as input to DESeq2 v1.30.175 to determine differential gene expression between conditions using the Wald test while correcting for possible covariates. Genes passing a multiple test correcting P < 0.05 (FDR method) were considered significant. Data were analyzed by Gene Ontology analysis76 and Kyoto Enrichment of Genes and Genomes pathway analysis77 in DAVID and Ingenuity Pathway Analysis (IPA; QIAGEN). Venn diagram was generated using Venny v2.1.0 (open source); R software v4.0.2 (open source) was used for RNAseq data analysis. R software information and packages are listed in Supplementary Table 3.
Statistics and reproducibility
Data were analyzed using Prism software (GraphPad) (except RNAseq data), including statistical analysis using one-way ANOVA (Dunnett’s and Tukey’s multiple comparison tests) and two-way ANOVA (Dunnett’s multiple comparison test and two-stage step-up method of Benjamini, Krieger and Yekutieli). Due to the relatively small sample size normality testing was not feasible and all data were assumed to have a normal distribution. Group comparisons are indicated in the figure legends and P values < 0.05 were considered statistically significant and indicated as *P < 0.05, **P < 0.01 and ***P < 0.001. In whisker/box plots all data points are included, whiskers extend from minima to maxima, boxes extend from 25th to 75th percentile and lines in boxes represent median. n values refer to biologically independent replicates of analyzed cells or media. All experiments were repeated independently with similar results at least three times, except for Supplementary Fig. 1e (flow cytometry analysis of freshly thawed PHHs). P values of statistically significant results are provided in Supplementary Table 4.
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Supplementary information
Description of Additional Supplementary Files
Acknowledgements
The authors thank Tania Moody and Walter Eckalbar for help with RNAseq data analysis, Jae-Jun Kim for help with flow cytometry, Beltrán Borges and Simon N. Chu for donating and drawing blood, Suneil Koliwad for discussion and Simone Kurial and Pamela Derish for manuscript editing. This study was funded by NIH UG3/UH3 DK120004 to H.W. and E.C.H., NIH P30 DK026743 (UCSF Liver Center) to H.W. and J.J.M., a grant from the UCSF Academic Senate to J.J.M., a grant from the Weston Havens Foundation to J.J.M. and D.L.G., the Robert L. Kroc Chair III in Rheumatic and Connective Tissue Disease to E.C.H., an individual fellowship from the German Research Foundation (GR 5417/1-1) to M.G., an individual fellowship from NIH T32 DK060414 to E.H.A. and an individual fellowship from the Sao Paulo Research Foundation (2022/08157-5) to K.A.T.-S.
Source data
Author contributions
M.G. conceived the study, performed experiments, analyzed the data, generated the figures, performed the statistical analyses and wrote the manuscript. K.M., E.H.A., A.P., D.L.G. and K.A.T.-S. performed experiments. C.P. analyzed the RNAseq data. E.C.H. and J.J.M. supervised experiments and edited the manuscript. H.W. conceived the study, supervised experiments and wrote the manuscript.
Peer review
Peer review information
Nature Communications thanks Salman Khetani, Hanyang Liu and the other, anonymous reviewer(s) for their contribution to the peer review of this work. A peer review file is available.
Data availability
Primer sequences, antibody sources, software information and P values are provided in Supplementary Tables 1–4. Raw RNAseq data were deposited in the NCBI Gene Expression Omnibus database repository under accession number GSE228765. Processed RNAseq data are provided in Supplementary Data 1. Source data are provided with this paper.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
The online version contains supplementary material available at 10.1038/s41467-023-39311-w.
References
- 1.Holmgren G, et al. Characterization of human induced pluripotent stem cell-derived hepatocytes with mature features and potential for modeling metabolic diseases. Int. J. Mol. Sci. 2020;21:469. doi: 10.3390/ijms21020469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rashid ST, et al. Modeling inherited metabolic disorders of the liver using human induced pluripotent stem cells. J. Clin. Investig. 2010;120:3127–3136. doi: 10.1172/JCI43122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Copps KD, White MF. Regulation of insulin sensitivity by serine/threonine phosphorylation of insulin receptor substrate proteins IRS1 and IRS2. Diabetologia. 2012;55:2565–2582. doi: 10.1007/s00125-012-2644-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Petersen MC, Shulman GI. Mechanisms of insulin action and insulin resistance. Physiol. Rev. 2018;98:2133–2223. doi: 10.1152/physrev.00063.2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bazotte RB, Silva LG, Schiavon FPM. Insulin resistance in the liver: deficiency or excess of insulin? Cell Cycle. 2014;13:2494–2500. doi: 10.4161/15384101.2014.947750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Giri B, et al. Chronic hyperglycemia mediated physiological alteration and metabolic distortion leads to organ dysfunction, infection, cancer progression and other pathophysiological consequences: an update on glucose toxicity. Biomed. Pharmacother. 2018;107:306–328. doi: 10.1016/j.biopha.2018.07.157. [DOI] [PubMed] [Google Scholar]
- 7.Sarwar R, Pierce N, Koppe S. Obesity and nonalcoholic fatty liver disease: current perspectives. Diabetes Metab. Syndr. Obes. 2018;11:533–542. doi: 10.2147/DMSO.S146339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Huang W, et al. Depletion of liver Kupffer cells prevents the development of diet-induced hepatic steatosis and insulin resistance. Diabetes. 2010;59:347–357. doi: 10.2337/db09-0016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lanthier N, et al. Kupffer cell activation is a causal factor for hepatic insulin resistance. Am. J. Physiol. Gastrointest. Liver Physiol. 2010;298:G107–16. doi: 10.1152/ajpgi.00391.2009. [DOI] [PubMed] [Google Scholar]
- 10.Kim DH, et al. FoxO6-mediated IL-1β induces hepatic insulin resistance and age-related inflammation via the TF/PAR2 pathway in aging and diabetic mice. Redox Biol. 2019;24:101184. doi: 10.1016/j.redox.2019.101184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tencerova M, et al. Activated Kupffer cells inhibit insulin sensitivity in obese mice. FASEB J. 2015;29:2959–2969. doi: 10.1096/fj.15-270496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Klover PJ, Zimmers TA, Koniaris LG, Mooney RA. Chronic exposure to interleukin-6 causes hepatic insulin resistance in mice. Diabetes. 2003;52:2784–2789. doi: 10.2337/diabetes.52.11.2784. [DOI] [PubMed] [Google Scholar]
- 13.Senn JJ, Klover PJ, Nowak IA, Mooney RA. Interleukin-6 induces cellular insulin resistance in hepatocytes. Diabetes. 2002;51:3391–3399. doi: 10.2337/diabetes.51.12.3391. [DOI] [PubMed] [Google Scholar]
- 14.Hirosumi J, et al. A central role for JNK in obesity and insulin resistance. Nature. 2002;420:333–336. doi: 10.1038/nature01137. [DOI] [PubMed] [Google Scholar]
- 15.Nov O, et al. Interleukin-1beta may mediate insulin resistance in liver-derived cells in response to adipocyte inflammation. Endocrinology. 2010;151:4247–4256. doi: 10.1210/en.2010-0340. [DOI] [PubMed] [Google Scholar]
- 16.Sanyal AJ. Past, present and future perspectives in nonalcoholic fatty liver disease. Nat. Rev. Gastroenterol. Hepatol. 2019;16:377–386. doi: 10.1038/s41575-019-0144-8. [DOI] [PubMed] [Google Scholar]
- 17.Molinaro A, Becattini B, Solinas G. Insulin signaling and glucose metabolism in different hepatoma cell lines deviate from hepatocyte physiology toward a convergent aberrant phenotype. Sci. Rep. 2020;10:12031. doi: 10.1038/s41598-020-68721-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Davidson MD, Lehrer M, Khetani SR. Hormone and drug-mediated modulation of glucose metabolism in a microscale model of the human liver. Tissue Eng. Part C. Methods. 2015;21:716–725. doi: 10.1089/ten.tec.2014.0512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Davidson MD, Ballinger KR, Khetani SR. Long-term exposure to abnormal glucose levels alters drug metabolism pathways and insulin sensitivity in primary human hepatocytes. Sci. Rep. 2016;6:28178. doi: 10.1038/srep28178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kozyra M, et al. Human hepatic 3D spheroids as a model for steatosis and insulin resistance. Sci. Rep. 2018;8:14297. doi: 10.1038/s41598-018-32722-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Blaszkiewicz J, Duncan SA. Advancements in disease modeling and drug discovery using iPSC-derived hepatocyte-like cells. Genes. 2022;13:573. doi: 10.3390/genes13040573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ang LT, et al. A roadmap for human liver differentiation from pluripotent stem cells. Cell Rep. 2018;22:2190–2205. doi: 10.1016/j.celrep.2018.01.087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gao X, et al. Hepatocyte-like cells derived from human induced pluripotent stem cells using small molecules: implications of a transcriptomic study. Stem Cell Res. Ther. 2020;11:393. doi: 10.1186/s13287-020-01914-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mallanna SK, Duncan SA. Differentiation of hepatocytes from pluripotent stem cells. Curr. Protoc. Stem Cell Biol. 2013;26:1G.4.1–1G.4.13. doi: 10.1002/9780470151808.sc01g04s26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ferris HA, Kahn CR. New mechanisms of glucocorticoid-induced insulin resistance: make no bones about it. J. Clin. Investig. 2012;122:3854–3857. doi: 10.1172/JCI66180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rozance PJ, et al. Effects of chronic hyperinsulinemia on metabolic pathways and insulin signaling in the fetal liver. Am. J. Physiol. Endocrinol. Metab. 2020;319:E721–E733. doi: 10.1152/ajpendo.00323.2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Fritsche L, et al. Insulin-induced serine phosphorylation of IRS-2 via ERK1/2 and mTOR: studies on the function of Ser675 and Ser907. Am. J. Physiol. Endocrinol. Metab. 2011;300:E824–36. doi: 10.1152/ajpendo.00409.2010. [DOI] [PubMed] [Google Scholar]
- 28.Payankaulam S, Raicu A-M, Arnosti DN. Transcriptional regulation of INSR, the insulin receptor gene. Genes. 2019;10:984. doi: 10.3390/genes10120984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Karim S, Adams DH, Lalor PF. Hepatic expression and cellular distribution of the glucose transporter family. World J. Gastroenterol. 2012;18:6771–6781. doi: 10.3748/wjg.v18.i46.6771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Molinaro A, et al. Insulin-driven PI3K-AKT signaling in the hepatocyte is mediated by redundant PI3Kα and PI3Kβ activities and is promoted by RAS. Cell Metab. 2019;29:1400–1409.e5. doi: 10.1016/j.cmet.2019.03.010. [DOI] [PubMed] [Google Scholar]
- 31.Dong XC, et al. Inactivation of hepatic Foxo1 by insulin signaling is required for adaptive nutrient homeostasis and endocrine growth regulation. Cell Metab. 2008;8:65–76. doi: 10.1016/j.cmet.2008.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sarbassov DD, Guertin DA, Ali SM, Sabatini DM. Phosphorylation and regulation of Akt/PKB by the rictor-mTOR complex. Science. 2005;307:1098–1101. doi: 10.1126/science.1106148. [DOI] [PubMed] [Google Scholar]
- 33.Um SH, D’Alessio D, Thomas G. Nutrient overload, insulin resistance, and ribosomal protein S6 kinase 1, S6K1. Cell Metab. 2006;3:393–402. doi: 10.1016/j.cmet.2006.05.003. [DOI] [PubMed] [Google Scholar]
- 34.Petersen MC, Vatner DF, Shulman GI. Regulation of hepatic glucose metabolism in health and disease. Nat. Rev. Endocrinol. 2017;13:572–587. doi: 10.1038/nrendo.2017.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Beurel E, Grieco SF, Jope RS. Glycogen synthase kinase-3 (GSK3): regulation, actions, and diseases. Pharm. Ther. 2015;148:114–131. doi: 10.1016/j.pharmthera.2014.11.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Collin de l’Hortet A, et al. Generation of human fatty livers using custom-engineered induced pluripotent stem cells with modifiable SIRT1 metabolism. Cell Metab. 2019;30:385–401.e9. doi: 10.1016/j.cmet.2019.06.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ouchi R, et al. Modeling steatohepatitis in humans with pluripotent stem cell-derived organoids. Cell Metab. 2019;30:374–384.e6. doi: 10.1016/j.cmet.2019.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kreitzer FR, et al. A robust method to derive functional neural crest cells from human pluripotent stem cells. Am. J. Stem Cells. 2013;2:119–131. [PMC free article] [PubMed] [Google Scholar]
- 39.Matsuo K, et al. ACVR1R206H extends inflammatory responses in human induced pluripotent stem cell-derived macrophages. Bone. 2021;153:116129. doi: 10.1016/j.bone.2021.116129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kazankov K, et al. The role of macrophages in nonalcoholic fatty liver disease and nonalcoholic steatohepatitis. Nat. Rev. Gastroenterol. Hepatol. 2019;16:145–159. doi: 10.1038/s41575-018-0082-x. [DOI] [PubMed] [Google Scholar]
- 41.Tsuchiya K, et al. Caspase-1 initiates apoptosis in the absence of gasdermin D. Nat. Commun. 2019;10:2091. doi: 10.1038/s41467-019-09753-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Chen Z, Yu R, Xiong Y, Du F, Zhu S. A vicious circle between insulin resistance and inflammation in nonalcoholic fatty liver disease. Lipids Health Dis. 2017;16:203. doi: 10.1186/s12944-017-0572-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Duwaerts CC, et al. Induced pluripotent stem cell-derived hepatocytes from patients with nonalcoholic fatty liver disease display a disease-specific gene expression profile. Gastroenterology. 2021;160:2591–2594.e6. doi: 10.1053/j.gastro.2021.02.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kano A, Watanabe Y, Takeda N, Aizawa S, Akaike T. Analysis of IFN-gamma-induced cell cycle arrest and cell death in hepatocytes. J. Biochem. 1997;121:677–683. doi: 10.1093/oxfordjournals.jbchem.a021639. [DOI] [PubMed] [Google Scholar]
- 45.Filliol A, et al. RIPK1 protects from TNF-α-mediated liver damage during hepatitis. Cell Death Dis. 2016;7:e2462. doi: 10.1038/cddis.2016.362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Jin X, et al. Paradoxical effects of short- and long-term interleukin-6 exposure on liver injury and repair. Hepatology. 2006;43:474–484. doi: 10.1002/hep.21087. [DOI] [PubMed] [Google Scholar]
- 47.Knight B, Lim R, Yeoh GC, Olynyk JK. Interferon-gamma exacerbates liver damage, the hepatic progenitor cell response and fibrosis in a mouse model of chronic liver injury. J. Hepatol. 2007;47:826–833. doi: 10.1016/j.jhep.2007.06.022. [DOI] [PubMed] [Google Scholar]
- 48.Horton JD, Goldstein JL, Brown MS. SREBPs: activators of the complete program of cholesterol and fatty acid synthesis in the liver. J. Clin. Investig. 2002;109:1125–1131. doi: 10.1172/JCI0215593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Yecies JL, et al. Akt stimulates hepatic SREBP1c and lipogenesis through parallel mTORC1-dependent and independent pathways. Cell Metab. 2011;14:21–32. doi: 10.1016/j.cmet.2011.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Liu Z, et al. Causal relationships between NAFLD, T2D and obesity have implications for disease subphenotyping. J. Hepatol. 2020;73:263–276. doi: 10.1016/j.jhep.2020.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Yung JHM, Giacca A. Role of c-Jun N-terminal kinase (JNK) in obesity and type 2 diabetes. Cells. 2020;9:706. doi: 10.3390/cells9030706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Chen L, Chen R, Wang H, Liang F. Mechanisms linking inflammation to insulin resistance. Int. J. Endocrinol. 2015;2015:508409. doi: 10.1155/2015/508409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Samuel VT, Shulman GI. Mechanisms for insulin resistance: common threads and missing links. Cell. 2012;148:852–871. doi: 10.1016/j.cell.2012.02.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Larsen CM, et al. Interleukin-1-receptor antagonist in type 2 diabetes mellitus. N. Engl. J. Med. 2007;356:1517–1526. doi: 10.1056/NEJMoa065213. [DOI] [PubMed] [Google Scholar]
- 55.Straczkowski M, et al. Changes in tumor necrosis factor-alpha system and insulin sensitivity during an exercise training program in obese women with normal and impaired glucose tolerance. Eur. J. Endocrinol. 2001;145:273–280. doi: 10.1530/eje.0.1450273. [DOI] [PubMed] [Google Scholar]
- 56.Velikova TV, Kabakchieva PP, Assyov YS, Georgiev TА. Targeting inflammatory cytokines to improve type 2 diabetes control. Biomed. Res. Int. 2021;2021:7297419. doi: 10.1155/2021/7297419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.She S, et al. Functional roles of chemokine receptor CCR2 and its ligands in liver disease. Front. Immunol. 2022;13:812431. doi: 10.3389/fimmu.2022.812431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Aronoff SL, Berkowitz K, Shreiner B, Want L. Glucose metabolism and regulation: beyond insulin and glucagon. Diabetes Spectr. 2004;17:183–190. doi: 10.2337/diaspect.17.3.183. [DOI] [Google Scholar]
- 59.Titchenell PM, Chu Q, Monks BR, Birnbaum MJ. Hepatic insulin signalling is dispensable for suppression of glucose output by insulin in vivo. Nat. Commun. 2015;6:7078. doi: 10.1038/ncomms8078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Gaul S, et al. Hepatocyte pyroptosis and release of inflammasome particles induce stellate cell activation and liver fibrosis. J. Hepatol. 2021;74:156–167. doi: 10.1016/j.jhep.2020.07.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Pantano L, et al. Molecular characterization and cell type composition deconvolution of fibrosis in NAFLD. Sci. Rep. 2021;11:18045. doi: 10.1038/s41598-021-96966-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Suppli MP, et al. Hepatic transcriptome signatures in patients with varying degrees of nonalcoholic fatty liver disease compared with healthy normal-weight individuals. Am. J. Physiol. Gastrointest. Liver Physiol. 2019;316:G462–G472. doi: 10.1152/ajpgi.00358.2018. [DOI] [PubMed] [Google Scholar]
- 63.Franko A, et al. Dissociation of fatty liver and insulin resistance in I148M PNPLA3 carriers: differences in diacylglycerol (DAG) FA18:1 lipid species as a possible explanation. Nutrients. 2018;10:1314. doi: 10.3390/nu10091314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Mota M, Banini BA, Cazanave SC, Sanyal AJ. Molecular mechanisms of lipotoxicity and glucotoxicity in nonalcoholic fatty liver disease. Metabolism. 2016;65:1049–1061. doi: 10.1016/j.metabol.2016.02.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Ozcan U, et al. Endoplasmic reticulum stress links obesity, insulin action, and type 2 diabetes. Science. 2004;306:457–461. doi: 10.1126/science.1103160. [DOI] [PubMed] [Google Scholar]
- 66.Basu R, Chandramouli V, Dicke B, Landau B, Rizza R. Obesity and type 2 diabetes impair insulin-induced suppression of glycogenolysis as well as gluconeogenesis. Diabetes. 2005;54:1942–1948. doi: 10.2337/diabetes.54.7.1942. [DOI] [PubMed] [Google Scholar]
- 67.Krssak M, et al. Alterations in postprandial hepatic glycogen metabolism in type 2 diabetes. Diabetes. 2004;53:3048–3056. doi: 10.2337/diabetes.53.12.3048. [DOI] [PubMed] [Google Scholar]
- 68.Magnusson I, Rothman DL, Katz LD, Shulman RG, Shulman GI. Increased rate of gluconeogenesis in type II diabetes mellitus. A 13C nuclear magnetic resonance study. J. Clin. Investig. 1992;90:1323–1327. doi: 10.1172/JCI115997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Perry RJ, et al. Hepatic acetyl CoA links adipose tissue inflammation to hepatic insulin resistance and type 2 diabetes. Cell. 2015;160:745–758. doi: 10.1016/j.cell.2015.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Winnick JJ, et al. Hepatic glycogen supercompensation activates AMP-activated protein kinase, impairs insulin signaling, and reduces glycogen deposition in the liver. Diabetes. 2011;60:398–407. doi: 10.2337/db10-0592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Nozaki Y, et al. Metabolic control analysis of hepatic glycogen synthesis in vivo. Proc. Natl Acad. Sci. USA. 2020;117:8166–8176. doi: 10.1073/pnas.1921694117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Ott LW, et al. Tumor Necrosis Factor-alpha- and interleukin-1-induced cellular responses: coupling proteomic and genomic information. J. Proteome Res. 2007;6:2176–2185. doi: 10.1021/pr060665l. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Si-Tayeb K, et al. Highly efficient generation of human hepatocyte-like cells from induced pluripotent stem cells. Hepatology. 2010;51:297–305. doi: 10.1002/hep.23354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Dobin A, et al. STAR: ultrafast universal RNA-seq aligner. Bioinformatics. 2013;29:15–21. doi: 10.1093/bioinformatics/bts635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Love MI, Huber W, Anders S. Moderated estimation of fold change and dispersion for RNA-seq data with DESeq2. Genome Biol. 2014;15:550. doi: 10.1186/s13059-014-0550-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Ashburner M, et al. Gene ontology: tool for the unification of biology. The Gene Ontology Consortium. Nat. Genet. 2000;25:25–29. doi: 10.1038/75556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Kanehisa M, Goto S. KEGG: Kyoto Encyclopedia of Genes and Genomes. Nucleic Acids Res. 2000;28:27–30. doi: 10.1093/nar/28.1.27. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Description of Additional Supplementary Files
Data Availability Statement
Primer sequences, antibody sources, software information and P values are provided in Supplementary Tables 1–4. Raw RNAseq data were deposited in the NCBI Gene Expression Omnibus database repository under accession number GSE228765. Processed RNAseq data are provided in Supplementary Data 1. Source data are provided with this paper.