Abstract
Aims
To assess the correlation between calf circumference and cardiac metabolic risk factors such as hypertension, abnormal blood glucose and dyslipidaemia among middle-aged and elderly women.
Methods
The cross-sectional study population consisted of 476 female participants aged 40–80 years, including 304 perimenopausal and 172 postmenopausal women. Calf circumference, body mass index (BMI), blood pressure, blood glucose and blood lipids were measured. Logistic regression analysis was used to evaluate the study aims.
Results
Calf circumference was lower in postmenopausal than perimenopausal women, and postmenopausal women had the highest rates of hypertension, abnormal blood glucose and abnormal blood lipids. Pearson correlation coefficients showed that calf circumference was positively correlated with triglycerides (TGs), BMI, fasting plasma glucose (FPG),2-h plasma glucose, glycated haemoglobin (HbA1C), systolic blood pressure and diastolic blood pressure; and negatively correlated with high-density lipoprotein cholesterol (HDL-C) and total cholesterol (TC). The group with the lowest quantile of calf circumference had higher rates of hypertension (odds ratio (OR)2.14,95% confidence interval (CI)1.67–2.74),dysglycaemia (OR1.40,95%CI1.03–1.90) and dyslipidaemia (OR2.14,95%CI 1.86–2.46).
Conclusion
In perimenopausal women, measurements of calf circumference can be used to predict the presence of cardiac metabolic risk factors, which can be detected by observing blood pressure, blood glucose, and blood lipids.
Keywords: Middle-aged, Female, Calf circumference, Cardiac metabolic risk
1. Introduction
Cardiovascular disease is the leading cause of death in adults. Hyperlipidaemia, hypertension, hyperglycaemia and obesity are important risk factors for cardiovascular diseases [1]. In the past 20 years, the number of patients with dyslipidaemia, hypertension and diabetes in China has increased 1.5–5 fold [2]. Before age 50, the number of men with these risk factors is higher than the number of women with these factors, but after age 50. the number of women with these risk factors is significantly higher than the number of men [3]. Calf circumference (CC) refers to the circumference of the widest part of the gastrocnemius muscle and is a proxy for light weight and peripheral subcutaneous fat [4]. A French study [5] found that women with a CC less than 33 cm were at high risk for carotid plaques, which is a known risk factor for stroke. At present, CC is used to assess muscle mass and nutrition in China and around the world [6,7], but its correlation with cardiac metabolic risk factors is rarely reported. Hypertension, diabetes, smoking, dyslipidaemia, and obesity are risk factors for cardiovascular disease in women [8]. The Heart Disease and Stroke Statistics (report from the American Heart Association) shows that prevention of cardiovascular risk factors and early diagnosis and treatment of high-risk populations may effectively reduce cardiovascular diseases mortalitys [9]. The “Healthy China 2030” initiative proposes that, by 2020, the probability of premature mortality from major chronic diseases in China should decrease by 10% compared to that in 2015, and by 2030, it should decrease by 30% [10]. Therefore, blood lipids, blood glucose, and blood pressure should be carefully monitored in menopausal women. This study explored the relationship between CC and cardiovascular metabolic risk factors in middle-aged and elderly women and provided a basis for the prediction of cardiovascular events and health management in postmenopausal women.
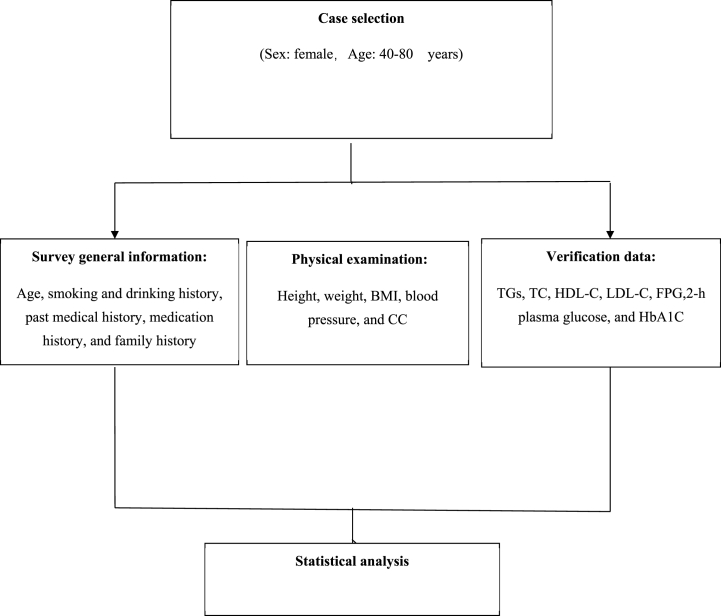
2. Materials and methods (Fig. 1)
Fig. 1.
Research flow.
2.1. Study subjects
Convenience sampling was used to select women who underwent a physical examination in our hospital from July to November 2019. After excluding ineligible women and women with incomplete data, 476 women were selected. The inclusion criteria were as follows: (1) voluntary participation with a signed informed consent form; (2) age from 40 to 80 years old; and (3) the ability to communicate normally. The exclusion criteria were as follows: (1) poor compliance; (2) current hormone replacement therapy (HRT); or (3) varicose veins and oedema of the lower extremities and an inability to walk.
2.2. Methods
2.2.1. General information questionnaire
The questionnaire developed by the National Centre for Cardiovascular Diseases was used, and a face-to-face survey was conducted by properly trained investigators. The questionnaire gathered information such as age, smoking and drinking history, past medical history (hypertension, diabetes, and coronary heart disease), medication history (antihypertensive drugs, lipid-lowering drugs, and hypoglycaemic drugs), and family history.
2.2.1.1. Physical examination
The physical examination included height, weight, body mass index (BMI), blood pressure, and CC measurements performed by special investigators. The morning after fasting (fasting ≥10 h), body weight was measuredment after urination. When measuring the CC, participants were asked to remove their shoes and stand upright, with their left leg placed for measurement and their feet at a natural distance. The measuring tape was wrapped around the widest part of the calf, typically 10 cm below the knee. The measuring tape was kept level and snug around the calf, without compressing the skin. To an accuracy of 0.1 cm, this was recorded as the CC. The accuracy for height was 0.1 cm and that for weight was 0.1 kg. The BMI was calculated as weight/height2 (kg/m2). Blood pressure was measured using a calibrated Omron electronic blood pressure monitor (Colin BP–203RVIIIC, Kyoto, Japan). After resting for ≥15 min, blood pressure was measured twice on each subject's nondominant arm, with an interval of 2 min between measurements, and the average blood pressure was recorded.
2.2.1.2. Laboratory indicators and diagnostic criteria for cardiovascular risk factors
Laboratory indicators included triglycerides (TGs), high-density lipoprotein cholesterol (HDL-C), low-density lipoprotein cholesterol (LDL-C), total cholesterol (TC), fasting blood glucose (FBG), 2-h plasma glucose, and glycated haemoglobin (HbA1C). Fasting venous blood samples (fasting ≥10 h) were collected in the morning and analyzed using an automated biochemical analyser.
2.2.1.3. Cardiac metabolic risk indicators and diagnostic criteria
The diagnostic criteria for dyslipidaemia were based on the 2007 Chinese Guidelines for the Management of Dyslipidaemia in Adults issued by the Joint Committee on the formulation of Chinese guidelines for the management of dyslipidaemia in adults [11]: and included the use of lipid-lowering drugs, TGs level≥ 2.26 mmol/L, TC > 6.22 mmol/L, LDL-C ≥ 4.14 mmol/L, or HDL-C<1.04 mmol/L. The criteria for hypertension included the prior or current use of antihypertensive drugs, a history of hypertension or a systolic blood pressure (SBP) ≥ 140 mmHg (1 mmHg = 0.133 kPa) and/or a diastolic blood pressure (DBP) ≥ 90 mmHg measured during the physical examination [12]. According to the WHO criteria, impaired fasting glycaemia (IFG) was defined as the prior or current use of anti-hypoglycaemic drugs, a history of diabetes or a fasting blood glucose level> 6.1 mmol/L. Impaired glucose tolerance (IGT) was diagnosed based on a fasting plasma glucose (FPG) level< 7.0 mmol/L (126 mg/dL) and a 2- h glucose level of 7.8–11.1 mmol/L (140–200 mg/dL). Impaired fasting glucose was diagnosed based on a FPG level between 6.1 and 6.9 mmol/L (110–125 mg/dL) and (if measured) a 2 h-plasma glucose level <7.8 mmol/L (<140 mg/dL). An HbA1C level 6.0–6.4% corresponded to prediabetes. Smoking was defined as smoking once a day or at least seven cigarettes a week. Drinking was defined as consuming alcohol at least once a week for more than 6 months.
2.3. Statistical methods
Normally distributed measurement data are presented as the mean ± standard deviation, and independent two samples t-tests were used for comparisons between the 2 groups. Count data are presented as the frequency and composition ratio, and the chi-square test was used for comparisons between groups. The subjects were divided into 4 groups according to CC quartile (i.e., Q1 (CC ≥ 35.7 cm), Q2 (34 ≤ CC < 35.7 cm), Q3 (31.9 ≤ CC < 34 cm), and Q4 (CC < 31.9 cm). The odds ratios (ORs) and 95% confidence intervals (CIs) for predicting cardiovascular risk factors using the CC were determined by multivariate logistic regression analyses after controlling for other potential confounders. The covariates adjusted for bias included age, smoking, drinking, and BMI. Statistical analyses were carried out using SPSS for Windows 24.0 (SPSS Inc. Chicago, IL, USA). A P value less than 0.05 was considered statistically significant.
To ensure the reliability and validity of measurements, centralized training programs and regular quality control were implemented for the special investigators. Additionally, a reproducibility study was performed. The mean absolute difference and correlation coefficient between repeated examinations of CC were, 0.06 mm and 0.69, respectively.
3. Results
3.1. Comparison of general characteristics between perimenopausal and menopausal women
Middle-aged and elderly women were divided into perimenopausal [13] (40–60 years old) and menopausal (61–80 years old) groups according to age for comparison. No difference in BMI was noted between the two groups, but differences in CC, dyslipidaemia, dysglycaemia, and hypertension were identified (Table 1).
Table 1.
Comparison of general characteristics between perimenopausal and menopausal women (N = 476, cases, %).
| Indicator | Perimenopausal (n = 304) | Menopausal (n = 172) | P value |
|---|---|---|---|
| BMI (x ± s, kg/m2) | 23.29 ± 3.08 | 23.11 ± 3.42 | 0.548a |
| CC | 34.42 ± 2.5 | 32.65 ± 2.80 | 0.000a |
| Dyslipidaemia | 188 (29.0%) | 136 (79.1%) | 0.000b |
| Dysglycaemia | 52 (17.1%) | 100 (58.1%) | 0.000b |
| Hypertension | 42 (13.8%) | 60 (34.9%) | 0.000b |
Data are represented as the mean ± standard deviation (S.D.) or proportion (%). A) t-test. B) chi-square test.
3.2. Analysis of relationship s between CC and cardiac metabolic indices
Pearson correlation coefficients were used to analyse the relationships between CC and cardiac metabolic indices. CC was positively correlated with TGs, BMI, FPG, 2-h plasma glucose, HbA1C, SBP and DBP; CC was negatively correlated with HDL-C and TC; and CC was not correlated with LDL-C (Table 2).
Table 2.
Correlation analysis between CC and cardiac metabolic indices in middle-aged and elderly women.
| lindex | CC |
P |
|---|---|---|
| r | ||
| BMI (kg/m2) | 0.603 | <0.001** |
| TC (mmol/L)a | −0.148 | <0.001** |
| TGs (mmol/L)a | 0.176 | <0.001** |
| LDL-C (mmol/L)a | −0.308 | 0.410 |
| HDL-C (mmol/L)a | −0.348 | <0.001** |
| FPG (mmol/L)b | 0.261 | <0.001** |
| 2-h plasma glucose (mmol/L)b | 0.119 | <0.001** |
| HbA1C (%)b | 0.216 | <0.001** |
| SBP, mmHgc | 0.237 | 0.003** |
| DBP, mmHgc | 0.149 | <0.001** |
Notes:*a: Except for dyslipidaemia patients; b: Except for diabetic patients; c: Except for hypertension patients.
* Differences are indicated by**P < 0.05.
3.3. Correlations between CC and cardiovascular risk factors
Logistic regression analysis was performed using factors that influence hypertension, dyslipidaemia, and dysglycaemia as dependent variables, and sex, age, BMI, and CC were used as independent variables. A multi-factor logistic regression model analysis was performed based on the CC quartiles. The risks of hypertension, dysglycaemia and dyslipidaemia in the group with the lowest CC quartile were 2.14, 1.40 and 2.14 times higher than those in the highest CC quartile group (P < 0.01) (Table 3).
Table 3.
Association analysis between CC quartile and cardiac metabolic factors in middle-aged and elderly women (OR (95% CI)).
| Indicator | CC |
||||
|---|---|---|---|---|---|
| Quartile 4* OR (95% CI) | Quartile 3 OR (95% CI) | Quartile 2 OR (95% CI) | Quartile 1 OR (95% CI) | P for Trend | |
| n | 128 | 124 | 104 | 120 | |
| Hypertension | |||||
| Model 1 | 1.00 | 0.36 (0.19–0.66) | 0.45 (0.25–0.84) | 0.52 (0.29–0.94) | 0.000 |
| Model 2 | 1.00 | 0.76 (0.39–1.47) | 0.97 (0.61–1.54) | 2.14 (1.67–2.74) | 0.000 |
| Dysglycaemia | |||||
| Model 1 | 1.00 | 0.30 (0.15–0.67) | 0.70 (0.77–1.15) | 0.89 (0.69–1.30) | 0.000 |
| Model 2 | 1.00 | 0.46 (0.26–0.81) | 0.78 (0.68–0.89) | 1.40 (1.03–1.90) | 0.032 |
| Dyslipidaemia | |||||
| Model 1 | 1.00 | 0.85 (0.51–1.32) | 0.77 (0.45–1.42) | 1.06 (0.64–1.76) | 0.145 |
| Model 2 | 1.00 | 0.76 (0.67–0.86) | 0.97 (0.84–1.12) | 2.14 (1.86–2.46) | 0.000 |
Note: * Highest CC quartile.
Model 1 (uncorrected variables); Model 2 adjusted for age, BMI, TC, and HDL-C (blood pressure was not corrected in the analysis of hypertension, and TC and HDL-C were not corrected in the analysis of dyslipidaemia).
4. Discussion
This study explored the correlation between CC and cardiovascular metabolic risk factors including hypertension, abnormal blood glucose and dyslipidaemia in middle-aged and elderly women aged 40–80 years old. The results showed differences in CC and the prevalence of hypertension, dysglycaemia and dyslipidemia between perimenopausal and postmenopausal women; CC was positively correlated with TGs, BMI, FPG, 2-h plasma glucose, HbA1C, SBP and DBP values; CC was negatively correlated with HDL-C and TC values; and CC was not correlated with LDL-C. After mixed factors, such as age, smoking, drinking and BMI, were corrected for by quantile logistic regression analysis, the presence of cardiac metabolic risk factors was found to increase with decreasing CC (trend P < 0.05). The risk levels of hypertension, dysglycaemia and dyslipidaemia in the corrected Q1 (lowest quartile) were 2.14, 1.40 and 2.14 times higher than those in Q4 (highest quartile). Another study [14] showed that a reduction in CC was an independent risk factor for dyslipidaemia in middle-aged and elderly people.
Sakinah et al. [15] showed that CC decreased with increasing age and decreasing physical activity, which is consistent with the results of this study. CC is an anthropometric parameter closely related to the body's muscle mass. It is currently known to be related to the nutritional status of elderly individuals. CC can reflect a change in fat-free weight and is a sensitive indicator of muscle mass and peripheral subcutaneous fat in middle-aged and elderly people. Bai et al. [6] showed a linear correlation between CC and adipose tissue and that a high CC might reflect a large amount of subcutaneous fat and fat infiltration into muscles. Kawakami et al. [7] used CC as a surrogate marker for the muscle mass of Japanese males and females and hypothesized that subcutaneous fat in the calves may enhance and store free fatty acids (FFAs), thus promoting blood circulation to avoid the formation of carotid plaques. The incidence of carotid plaques increases in individuals with a low CC [16], and carotid plaques are known risk factors for stroke. Some animal studies have shown that the loss of IGF-1 sensitization in skeletal muscle leads to the development of insulin resistance (IR) [17]. According to previous studies, IR is associated with muscle strengthand muscle mass in middle-aged and elderly people. A low CC has been positively correlated with carotid atherosclerosis and IR in diabetic patients [18], and IR increases the concentration of FFAs and TGs in the blood, resulting in elevated blood lipids. IR increases blood free fatty acids and triglyceride levels, leading to dyslipidaemia and dysglycaemia.
Another study showed [19] no correlations between CC and resting SBP or DBP, pulse pressure or mean pressure in healthy elderly women, but CC was negatively correlated with the resting 1-min pulse rate. A low CC may be related to a high resting heart rate and low capillary density. Heart rate acceleration is secondary to reduced stroke output and exercise intolerance. Low capillary density is related to muscle blood flow [20], high resting heart rate and mean blood pressure. The CC can be used as a screening test for the resting pulse rate, which can be used to prevent cardiovascular events in elderly women [21]. Another cross-sectional study showed that a low CC may indicate a low risk of cardiovascular disease [22]. Therefore, the above negative factors related to low CC may increase the risk of cardiovascular events. The awareness of the interaction between CC and cardiovascular events. The inverse relationship between carotid plaque and increased calf circumference may also reflect the protective effect of calf circumference.
Another study [23] showed that a low CC was associated with a high prevalence of metabolic syndrome (MetS). The use of MetS combined with CC has an increased predictive ability for cardiovascular mortality. This is the first time the idea of incorporating CC and MetS components in different ways to predict the risk of death has been proposed. After considering other factors, a correlation was found between a decreased CC and hypertension. A possible reason for this correlation is that a low CC is associated with a high resting heart rate and low capillary density [24]. A high resting heart rate can increase the risk of cardiovascular events and cause persistent hypertension. Muscular blood flow is positively correlated with capillary density [25]. In the human calf, the soleus is the muscle that performs pumping. Hernelati et al. [26] reported that the amount of slow twitch muscle fibres was negatively correlated with the presence of hypertension [27]. A low proportion of slow twitch muscle fibres can lead to high vascular resistance. In addition, capillary density is associated with SBP and endothelial function [28]. However, a high proportion of fast twitch muscle fibres can result in a high resting mean blood pressure due to muscular sympathetic nervous activity [29]. The amount of fast twitch muscle fibres may affect resting systolic or diastolic pressure, pulse pressure, and mean blood pressure [21]. Another cross-sectional study showed that a large CC might indicate a reduced risk of cardiovascular disease [30]. The inverse relationship between carotid plaque and an increased CC might also reflect the protective effect of CC and thigh circumference. The above negative factors associated with a low CC may contribute to an increased risk of cardiovascular events. Therefore, the CC can provide valuable information on susceptibility to adverse cardiovascular events.
In summary, CC may be a useful screening measure for cardiovascular disease risk factors in middle-aged and elderly women. If an individual's CC is less than 34 cm, her blood glucose, blood pressure, and blood lipids should be monitored regularly to reduce her risk of developing cardiovascular diseases. Risk reduction measures may include adopting a healthy diet and exercise routine, quitting smoking, and managing other risk factors such as high blood pressure and cholesterol. Monitoring simple measures such as CC may help identify potential waming signs early.
While larger CC may be protective against cardiovascular diseases, further research is needed to determine the optimal calf size and the mechanisms that underlie this relationship. It is important to note that CC is one factor among many that contribute to cardiovascular disease risk and should not be used as a sole measure of risk.
This study had some possible limitations. It was a cross-sectional study with no causal control. The sample size, location, and subjects of this study limit the generalizability of the conclusions. The study did not assess whether a reduction in CC reflected a loss of muscle or fat, which requires further investigation via ultrasound, computed tomography, and magnetic resonance imaging. Therefore, the data should be interpreted with caution before extrapolating the results to the general population. Despite the limitations, the results are extremely relevant, indicating the practical applicability of a low-cost and easily applicable method to predict cardiovascular disease risk in middle-aged and elderly women.
Ethics approval and informed consent
This study was approved by the Medical Ethics Committee of Wenzhou Central Hospital (2019-03-009), and the subjects signed an informed consent form.
Consent for publication
Not applicable.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author contribution statement
Lele Bian: Conceived and designed the experiments; Wrote the paper.
Ai-Chun Lan: Conceived and designed the experiments; Analyzed and interpreted the data.
Yong-ke Zheng: Contributed reagents, materials, analysis tools or data.
Hai-Yan Xue: Conceived and designed the experiments.
Qiao Ye: Performed the experiments; Analyzed and interpreted the data; Contributed reagents, materials, analysis tools or data.
Data availability statement
Data included in article/supplementary material/referenced in article.
Authors’ information
Lele Bian (1987-), Female, Master, Associate Clinical Professor, Geriatrics, Wenzhou Central Hospital, Wenzhou, Zhejiang 325,000, China. E-mail: bll0177@163.com. Research interest: Geriatrics.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper
Acknowledgements
This study was supported by Wenzhou Science and Technology Project (Y20190621). Ai-Chun Lan,Wenzhou Central Hospital. Jin-Ying Bao,Lucheng District People's Hospital, Wenzhou. Ying-Ying Zhang, Wenzhou Central Hospital. Yi-Dong Wang, Wenzhou Central Hospital. Qiao Ye, Wenzhou Central Hospital. Jing Pan,Wenzhou Central Hospital. Yan Cheng, Wenzhou Central Hospital. Su-Ni Wei, Wenzhou Central Hospital. China.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.heliyon.2023.e17456.
Abbreviations
- CC
calf circumference
- HRT
hormone replacement therapy
- BMI
body mass index
- TGs
triglycerides
- TC
total cholesterol
- HDL-C
high-density lipoprotein cholesterol
- LDL-C
low-density lipoprotein cholesterol
- SBP
systolic blood pressure
- DBP
diastolic blood pressure
- IFG
impaired fasting glycaemia
- FBG
fasting blood glucose
- HbA1C
glycated haemoglobin
- FFAs
free fatty acids
- MetS
metabolic syndrome
- IGT
impaired glucose tolerance
- S.D.
standard deviation
- ORs
odds ratios
- CIs
confidence intervals
- FPG
fasting plasma glucose
- IR
insulin resistance
Appendix A. Supplementary data
The following are the Supplementary data to this article.
References
- 1.Benjamin E.J., Virani S.S., Callaway C.W., et al. Heart dease and sroke ttistics–2018 udate: a eport from the American heart association[J] Circulation. 2018;137(12):e467–e492. doi: 10.1161/CIR.0000000000000558. [DOI] [PubMed] [Google Scholar]
- 2.Wang L., Gao P., Zhang M., et al. Prevalence and ethnic pattern of diabetes and prediabetes in China in 2013. JAMA. 2017;317(24):2515–2523. doi: 10.1001/jama.2017.7596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wang B., Zhang J., Tang M., et al. Relationship between the prevalence of dyslipidaemia and its influencing factors in a northern Chinese population. Mol Cardiol China. 2013;13(3):520–522. [Google Scholar]
- 4.Takagi D., Morikami A., Kamo T., et al. The association of calf circumference with resting pulse rate in community-dwelling healthy elderly women -pilot study- J. Phys. Ther. Sci. 2013 Jun;25(6):705–707. doi: 10.1589/jpts.25.705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Stephanie Debette M.D., Nathalie Leone M.D., Courbon Dominique, PhD, etal Calf circumference is inversely associated with carotid. Plaques.Stroke. 2008;39:2958–2965. doi: 10.1161/STROKEAHA.108.520106.9. [DOI] [PubMed] [Google Scholar]
- 6.Bai H., Sun J., Chen M., Xie H., Xu D., Chen Y. Relationship between calf circumference and skeletal muscle mass,strength and function in the elderly. Chin J Clin Nutr. 2018;26(5):284–287. doi: 10.3760/cma.j.issn.1674-635X.2018.05.005. [DOI] [Google Scholar]
- 7.Kawakami R., Murakami H., Sanada K., et al. Calf circumference as a surrogate marker of muscle mass for diagnosing sarcopenia in Japanese men and women[J] Geriatr. Gerontol. Int. 2014;15(8):969–976. doi: 10.1111/ggi.12377. [DOI] [PubMed] [Google Scholar]
- 8.Yan X., Wang C. Management and evaluation of cardiovascular diseases in perimenopausal women. Matern Child Health Care China. 2013;28(5):798–801. [Google Scholar]
- 9.Ma L., Wu Y., Chen W. Key points in 2018 report on cardiovascular diseases in China. Chin J Hypertens. 2019;27(8):712–716. doi: 10.16439/j.cnki.1673-7245.2019.08.006. [DOI] [Google Scholar]
- 10.Xinhua News Agency . 2016. Outline for the “healthy China 2030” initiative [EB/OL] Available from:: htttp://hongdou.Gxnews.Com. Cn/viewthread-17022251. Html. Accessed December 19, 2016. [Google Scholar]
- 11.Zhao S. Essential points in and explanations of 2016 Chinese guideline for the management of dyslipidaemia in adults. Chin. J. Cardiol. 2016;44(10):827–829. doi: 10.3760/cma.j.issn.0253-3758.2016.10.003. [DOI] [PubMed] [Google Scholar]
- 12.Liu L.S. Chinese guidelines for the management of hypertension. Chin. J. Cardiol. 2011;39(7):579–615. doi: 10.3760/cma.j.issn.0253-3758.2011.07.002. [DOI] [PubMed] [Google Scholar]
- 13.North American Menopause Society Estrogen and progestogen use in postmenopausal women: 2010 position statement of the North American menopause society. Menopause. 2010;17(2):242–255. doi: 10.1097/gme.0b013e3181d0f6b9. [DOI] [PubMed] [Google Scholar]
- 14.Lan A., Bao J., Zheng Y., et al. The effects of neck circumference and calf circumference on blood lipids, blood pressure and blood glucose in 960 middle-aged and elderly people. J. Nurs. 2021;28(3):53–57. [Google Scholar]
- 15.Sakinah H., Siti N.A., Suzana A. Determination of calf circumference cut-off values for Malaysian elderly and its predictive value in assessing risk of malnutrition. Malaysian Journal of Nutrition. 2016;3:375–387. [Google Scholar]
- 16.Park J.S., Cho M.H., Ahn C.W., et al. The association of insulin resistance and carotid atherosclerosis with thigh and calf circumference in patients with type 2 diabetes[J] Cardiovasc. Diabetol. 2012;11(1):62. doi: 10.1186/1475-2840-11-62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sun Yu-Shan, Kao Tung-Wei. Yaw-wen Chang,etal.Calf circumference as a novel tool for risk of disability of the elderly population. Sci. Rep. 2017;7(1):1647–1649. doi: 10.1038/s41598-017-16347-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Grundy S.M., Cleeman J.I., Daniels S.R., etal Diagnosis and management of the metabolic syndrome: an American heart association/national heart, lung, and blood institute scientific statement. Circulation. 2005;112:2735–2752. doi: 10.1161/circulationaha.105.169404. [DOI] [PubMed] [Google Scholar]
- 19.Hedman A., Andersson P.E., Reneland R., etal Insulin-mediated changes in leg blood flow are coupled to capillary density in skeletal muscle in healthy 70-year-old men. Metab. Clin. Exp. 2001;50:1078–1082. doi: 10.1053/meta.2001.25604. [DOI] [PubMed] [Google Scholar]
- 20.Takagi D., Morikami A., Kamo T., et al. The association of calf circumference with resting pulse rate in community-dwelling healthy elderly women -pilot study- J. Phys. Ther. Sci. 2013;25(6):705–707. doi: 10.1589/jpts.25.705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Takagi Daisuke. The association of calf circumference with resting pulse rate in community-dwelling healthy elderly women—pilot study. Phys.Ther.Sci. 2013;25:705–707. doi: 10.1589/jpts.25.705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Loenneke J.P., Loprinzi P.D. Obesity is associated with insulinre rsistance but not skeletal muscle dysfunction or all-cause mortality. Age. 2016;38(1):2. doi: 10.1007/s11357-015-9865-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wu C.J., Kao T.W., Chang Y.W., etal Does the additional component of calf-circumference refine metabolic syndrome in correlating with cardiovascula r risk?[J] J. Clin. Endocrinol. Metab. 2018;103(3):1151–1160. doi: 10.1210/jc.2017-02320. [DOI] [PubMed] [Google Scholar]
- 24.Hedman A., Andersson P.E., Reneland R., Lithell H.O. Insulin-mediated changes in leg blood flow are coupled to capillary density in skeletal muscle in healthy 70-year-old men. Metabolism. 2001;50(9):1078–1082. doi: 10.1053/meta.2001.25604. [DOI] [PubMed] [Google Scholar]
- 25.Takagi D., Morikami A., Kamo T., et al. The association of calf circumference with resting pulse rate in community-dwelling healthy elderly women -pilot study. J. Phys. Ther. Sci. 2013;25(6):705–707. doi: 10.1589/jpts.25.705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hernelahti M., Tikkanen H.O., Karjalainen J., et al. Muscle fiber-type distri-bution as a predictor of blood pressure: a 19-year follow-up study. Hypertension. 2005;45:1019–1023. doi: 10.1161/01.HYP.0000165023.09921.34. [DOI] [PubMed] [Google Scholar]
- 27.Juhlin-Dannfelt A., Frisk-Holmberg M., Karlsson J., et al. Central and pe-ripheral circulation in relation to muscle—fibre composition in normo— and hypertensive man. Clin. Sci. 1979;56:335–340. doi: 10.1042/cs0560335. ([Medline]) [DOI] [PubMed] [Google Scholar]
- 28.Cheng C., Daskalakis C., Falkner B. Association of capillary density and function measures with blood pressure, fasting plasma glucose, and insulin sensitivity. J. Clin. Hypertens. 2010;12:125–135. doi: 10.1111/j.1751-7176.2009.00231.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Saito M. NAP Limited; 2007. Human Cardiovascular Regulation during Exercise and Adaptation; pp. 71–74. [Google Scholar]
- 30.Loenneke J.P., Loprinzi P.D. Obesity is associated with insulinre rsistance but not skeletal muscle dysfunction or all-cause mortality. Age. 2016;38(1):2. doi: 10.1007/s11357-015-9865-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data included in article/supplementary material/referenced in article.