Abstract
Introduction
Inguinoscrotal hernias are the commonest form of abdominal wall hernia, but for them to contain stomach is extremely rare. The management of these hernias can be very challenging owing to their acute nature of presentation and distortion of anatomy. Our aim was to systematically review the literature for all reported cases of inguinoscrotal hernias containing stomach. In turn we analysed patient demographics, site of hernia, presentation and treatment. Outcomes were reviewed where available.
Method
We conducted a systematic search of the PUBMED, Embase and Medline databases with a combination of keywords: Hernia AND (inguin* OR scrot*) AND (gastric OR gastro*). An author's own case has also been included.
Results
There were 20 case reports included in the review, plus the author’s own case. They ranged in publication date from 1942 to 2020. Mean age at presentation was 71 years (range 49 to 87). All cases were male. In total, 62% (n = 13) of cases presented with combined symptoms of abdominal pain and vomiting, 48% (n = 10) presented with gastric outlet obstruction (GOO) and 48% (n = 10) presented with gastric perforation. All successfully treated cases with gastric perforation required a midline laparotomy approach, whereas 56% (n = 5) of patients in the GOO group were successfully treated conservatively. There were three deaths reported in this review, all in the gastric perforation group.
Conclusion
Stomach as a content of inguinoscrotal hernias is extremely rare. These hernias predominantly present acutely in the form of GOO or gastric perforation. All patients with gastric perforation will require a midline laparotomy. Patients with GOO can be successfully managed either surgically or in selective cases with conservative management.
Keywords: Hernia, Inguinoscrotal, Inguinal, Stomach, Gastric
Introduction
Inguinal hernias are very common, with a lifetime risk of 27% for men and 3% for women.1 Inguinoscrotal hernias are also relatively common, and most of these will contain various combinations of omentum, small bowel and large bowel.2 However, it is very rare for these hernias to contain stomach, with limited cases reported in the literature.3
Inguinal hernias containing stomach are likely to present acutely either as gastric outlet obstruction (GOO) or with gastric perforation. The management of these patients is challenging as they often present acutely and in extremis. Moreover, surgery can be complicated by the gross distortion of abdominal anatomy.
There is no consensus on the management of inguinoscrotal hernias containing stomach, and currently there is limited information regarding this condition. We therefore undertook a systematic review of the literature pertaining to this type of hernia, which we hope can now act as a reference point for teams managing these cases.
Methods
Objective
Our aim was to systematically review the literature for all reported cases of inguinoscrotal hernias containing stomach. In turn we analysed patient demographics, site of hernia, presentation and treatment. Outcomes were reviewed where available.
Search strategy
We carried out an English language literature search using the PUBMED, Embase and Medline databases. This was carried out independently by two reviewers (Heylen and Lowcock). We also included a case of our own, reported in Appendix 1, under Heylen et al.
We searched using the keyword search: Hernia AND (inguin* OR scrot*) AND (gastric OR gastro*). We also conducted a reference check of the articles found for further reported cases.
As these cases are rare, there was no limitation to the time period for our search, which resulted in cases being included from 1942 to 2020.
Inclusion and exclusion criteria
We included case reports:
-
•
where stomach was a content of the inguinoscrotal hernia, either as the only content or with other viscera;
-
•
published in English;
-
•
from any time period;
-
•
for which full text was available digitally.
We excluded case reports:
-
•
published in non-English language;
-
•
where full text was not available digitally;
-
•
where the hernia contained only duodenum;
-
•
where the patient had undergone previous gastric surgery.
Data extraction
Two reviewers (Heylen and Ratnasingham) extracted all data independently using a data extraction sheet. For each case report included in the review, we collated information (where available) into a table regarding: year of publication, author, patient demographics, site of hernia, type of presentation, treatment received and outcome.
Risk of bias in individual case reports
The most significant potential bias was the requirement for authors to assess accurately the presence of stomach in the hernia. If the hernia was found to have only contained duodenum, it was excluded as per exclusion criteria. If the pylorus or more of the stomach was contained in the hernia, then it was included.
Reporting
The work was subsequently reported in line with PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) and AMSTAR (Assessing the methodological quality of systematic reviews) Guidelines.
Results
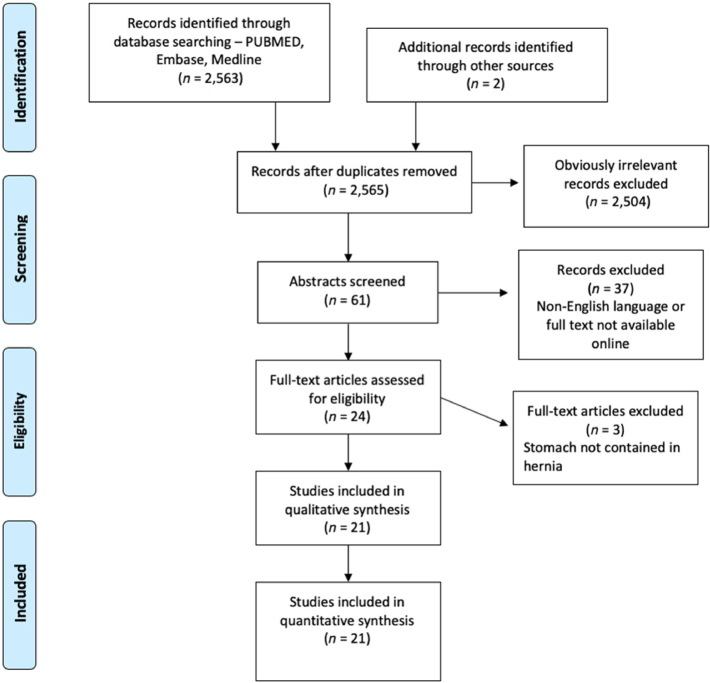
Our search strategy returned 2,565 records, 2,504 of which were excluded based on review of title and obvious inappropriateness. Of the remaining 61, a further 37 were excluded as they were non-English or the full text was not available digitally. Of the 24 full texts screened, 3 were excluded as the hernia did not contain stomach. Finally, this gave us 21 records that fulfilled our criteria, one of which was our own (Figure 1).
Figure 1 .
PRISMA flow chart
Phenotype
All cases were male with a mean age of 71 years. Laterality of the stomach was most commonly on the left side in 14 cases (67%), with 3 (14%) cases bilaterally, 3 cases on the right and 1 not stated (Table 1).
Table 1 .
Phenotype
| Male gender n (%) | 21 (100%) |
| Mean age (years) | 71 |
| Stomach in left groin n (%) | 14 (67%) |
| Stomach in right groin n (%) | 3 (14%) |
| Bilateral hernia present n (%) | 3 (14%) |
| Laterality not stated n (%) | 1 (5%) |
Presentation
In all but one case the patients presented acutely unwell. The most common presenting symptom was abdominal pain in combination with vomiting (13 (62%) cases). Presentation with abdominal pain or vomiting alone was less common, occurring in two and five cases, respectively (Table 2).
Table 2 .
Presentation
The commonest cause of these symptoms was GOO in ten cases (48%) and gastric perforation in ten cases (48%). Only one case was picked up incidentally and did not require surgery.
Management
In 19 out of the 21 cases, the reporters included their management strategy.
All patients with gastric perforation had operative management, of which eight out of the ten patients had a combination of midline laparotomy with an additional groin incision for hernia repair. One other patient was treated surgically with a midline laparotomy alone and one with laparoscopic repair.
In the GOO group, five patients were treated conservatively and four with operative management. Three out of the four cases of operative management involved repair via groin incision, and in the other case the patient underwent a combined groin incision and midline laparotomy (Table 3).
Table 3 .
Management
Discussion
Acute presentation of inguinoscrotal hernias with bowel obstruction is common. Indeed these hernias carry a 0.3% lifetime risk of strangulation.25 However, presentation with stomach in the hernia is extremely rare, and this is probably due to the stomach being a relatively fixed organ in the upper abdomen.
This review showed at least 19 (90%) of these hernias were chronic, with the remainder being unknown. This is expected as it takes a long time for the stomach to migrate to the groin. This downward descent is thought to be driven by the traction of the greater omentum and transverse colon as it is pulled into the giant hernia along with the bowel.22 At the time of presentation, in this review three cases (14%) had bilateral hernias, which is in keeping with the rate of bilateral inguinal hernias described elsewhere.26 Twenty cases (95%) had other viscera in the hernia sac: small and large bowel,4,5,7–24 bladder19 and pancreas.4
The large size and chronic nature of these hernias mean that patients in this series are likely to have ignored them up until the point at which they required emergency intervention owing to gastric perforation or outlet obstruction. This is reflected by the fact that 94% of these cases presented acutely.
The imaging modality used to diagnose the presence of stomach was computed tomography (CT) scan in 14 cases (67%). The remaining cases were diagnosed prior to the CT scan era with either barium swallow or clinical and operative findings. From this review, owing to the rarity of the cases, we cannot advocate imaging all patients presenting to outpatient clinics with large inguinoscrotal hernias. However, in patients presenting acutely with large inguinoscrotal hernias, cross-sectional imaging is useful in planning their management as discussed below.
The surgical approach used varied among cases. The main areas of difference between the cases, and in turn compared with the repair of conventional inguinoscrotal hernias, are as follows:
-
•
open vs laparoscopic approach;
-
•
method of hernia repair;
-
•
method of gastric repair;
-
•
conservative management;
-
•
singular vs staged procedures;
-
•
management of abdominal compartment syndrome risk.
Open vs laparoscopic approach
In the gastric perforation group, all patients underwent midline laparotomy with the exception of one who underwent a laparoscopic approach. Laparotomy allows for better washing of gastric contents from the abdominal cavity and careful inspection of the stomach prior to repair. In 8 (80%) of the cases, the surgeons then combined the midline laparotomy with a groin incision to repair the hernia. This approach is advantageous because it allows for toileting of the scrotum/sac and allows for repair of the hernia with a familiar approach.
Similarly, in the GOO group all patients underwent an open local repair of the hernia. However, additional laparotomy was only undertaken in one case. This reduced frequency of laparotomy is understandable as there are no gastric contents to wash and viscera to repair.
The almost exclusive use of open repair in these hernias concurs with the management of conventional inguinoscrotal hernias where large, randomised, prospective trials have shown superiority of open repair over laparoscopic repair with regards to recurrence.27
Method of hernia repair
The cases varied in their method of hernia repair with Bassini, Lichenstein and Wantz–Stoppa methods all used along with both testicle sparing and sacrificing. Recurrence or failure was reported in no cases. Mesh was used in three cases, including two with gastric perforation;12,16 none of these reported mesh infections.
Given the limited follow-up time, sparse reporting of complications and low patient numbers, it is impossible to infer any conclusions on superior method. Ultimately, hernia repair method should be driven by local guidelines, clinical competence and familiarity.
Method of gastric repair
Of the operatively managed patients, eight were found to have true gastric perforation. Of these, two cases utilised gastrectomy with anastomosis,11,14 while the others underwent suture repair.
Both gastrectomies were reported in the last decade, which aligns with the more recent consensus that large perforations should be treated with gastrectomy and anastomosis rather than primary suture repair. Indeed, the recent 2020 evidence-based guidance from the World Journal of Emergency Surgery suggests that perforations of <2cm should be managed with primary repair +/− omental patch, while those >2cm should be considered for resection dependent on anatomical location.28
Conservative management
It is important to note that five patients were successfully treated with conservative management, all from the GOO group. These patients made a full recovery up to discharge. This highlights that in selected patients without signs of perforation or systemic compromise, conservative management can be successfully employed. This is particularly important in an ageing, comorbid population. In addition, Davey et al demonstrated nasogastric tube decompression and conservative management can be used as a temporising measure in the acute setting, before a planned, lower risk elective repair.22
Singular vs staged procedures
A singular procedure was used in 11 (79%) operatively managed cases. A two-stage procedure was used in two cases. In these the gastric perforation was managed in the initial procedure and repair of the hernia done in a later procedure (either on index admission or at 3-month interval).4,5 In the final case a hybrid of these was used: the initial procedure involved a distal gastrectomy and repair of a left inguinal hernia, while a second procedure involved repair of the right inguinal hernia.11
Staged rather than single procedures may be more appropriate in cases of hernias with gastric perforation for two main reasons. Firstly is the idea of ‘damage control’ surgery. This concept is well documented in trauma surgery and has more recently been adopted into emergency general surgery. It involves a ‘rapid source control laparotomy’ in patients who are septic, unstable and comorbid and then return at a later date for the definitive procedure when the patient is more stable. Becher et al showed this may improve mortality in certain population groups.29 Hence, in unwell patients with gastric perforation from a giant inguinoscrotal hernia, repair of the perforation, subsequent stabilisation and then return at a later date for definitive hernia repair may improve mortality. Secondly, mesh repair has shown superiority over non-mesh repair in reducing risk of recurrence.30,31 However, as a prosthetic material, mesh should only be placed in a clean field; hence, a staged procedure allowing for the use of mesh in a clean field may improve the effectiveness of the final repair.
Management of abdominal compartment syndrome risk
Large inguinoscrotal hernias cause loss of domain, and on reduction of the hernia the risk of abdominal compartment syndrome is high. Three authors commented on their strategies to mitigate this. Techniques included: injection of Botox A into the abdominal wall muscles,11 delayed primary closure4 and colectomy to reduce visceral volume.16
Elsewhere in the literature, techniques such as progressive pneumoperitoneum have been described as effective and low risk but can only be utilised in the elective setting.32 Another technique of note is abdominal wall component separation. This helps reduce the tension in the abdominal wall and is widely used in large ventral hernia repair.33 It has subsequently been reported to help reduce abdominal compartment syndrome in the repair of giant inguinoscrotal hernias.34
Given the rarity of these presentations, it is impossible to draw conclusions as to best practice. However, it is imperative that surgeons are aware of the high risk of compartment syndrome and the management options.
Conclusion
This review has found that the presence of stomach in inguinoscrotal hernias is extremely rare. The presentation of these are usually in the acute setting either in the form of gastric perforation or GOO. If suitable for surgery, patients with suspected gastric perforation will require a midline laparotomy for toileting of abdominal cavity and repair of the perforation or gastrectomy. This should be combined with an additional groin incision for open repair of the hernia. Surgeons should be aware of the option of a staged procedure in the sickest patients with an initial rapid source control laparotomy and then return for planned repair of the hernia. Patients presenting with GOO can have definitive conservative management or at least in the initial period, with nasogastric tube decompression. If hernia repair is then indicated, it can be undertaken on an elective basis. In conclusion, these hernias are rare and there is no clear consensus on management, but appreciation and awareness of the issues discussed can help guide successful treatment.
References
- 1.Fitzgibbons RJ Jr, Forse RA. Groin hernias in adults. N Engl J Med 2014; 372: 756–763. 10.1056/NEJMcp1404068 [DOI] [PubMed] [Google Scholar]
- 2.Goyal S, Shrivastva M, Verma RK. ‘Uncommon contents of inguinal hernial sac’: a surgical dilemma. Indian J Surg 2015; 77: 305–309. 10.1007/s12262-013-0806-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Diaz Oller J, Medina Dominguez MT, Arcos Navarro Aet al. Stomach in inguinal-scrotal hernia. Rev Esp Enferm Dig 1997; 89: 325–328. [PubMed] [Google Scholar]
- 4.Fitz E, Chihara R, Stanton-Maxey KJ. Gastric perforation associated with bilateral inguinal hernias. J Am Coll Surg 2016; 222: e12–e13. 10.1016/j.jamcollsurg.2015.11.029 [DOI] [PubMed] [Google Scholar]
- 5.Sayad P, Tan AZ. A case report of a gastric perforation in a giant inguinoscrotal hernia: a two-step approach. Int J Surg Case Rep 2019; 55: 174–178. 10.1016/j.ijscr.2019.01.041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Birnbaum DJ, Grègoire E, Campan Pet al. A large inguinoscrotal hernia with stomach content. ANZ J Surg 2011; 81: 86–87. 10.1111/j.1445-2197.2010.05612.x [DOI] [PubMed] [Google Scholar]
- 7.Kerschaever I, Poelmans S, Vankeirsbilck J. Rare cause of gastric outlet obstruction: incarcerated pylorus within an inguinal hernia. Ann R Coll Surg Engl 2012; 94: e46–e48. 10.1308/003588412X13171221500907 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ship AG, Glick AH, Goldenson AB. Incarceration of the stomach in an inguinal hernia. report of a case. N Engl J Med 1960; 262: 78–80. 10.1056/NEJM196001142620207 [DOI] [PubMed] [Google Scholar]
- 9.Mehta T, Weissman S, Vash Aet al. Gastric inguinoscrotal hernia. ACG Case Reports J 2019; 6: e00187. 10.14309/crj.0000000000000187 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Abbas N, Kaimkhani S. Gastric outlet obstruction: an unusual hernia. Am J Surg Case Reports Sci Repos 2020; 2: 2. [Google Scholar]
- 11.Heylen J, Campioni-Norman D. Bilateral inguino-scrotal hernia with gastric contents and subsequent perforation; lessons in operative management. Int J Surg Case Rep 2020; 77: 853–856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Junge K, Otto J, Oral H. A rare cause of gastric outlet stenosis- scrotal hernia. Dtsch Arztebl Int 2019; 116: 507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Simmons H. Perforation of stomach in scrotal hernia. Br Med J 1949; 1: 808. 10.1136/bmj.1.4609.808-a [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dogar MA, Chaudhary A. Inguinal hernia containing stomach, transverse colon and small bowel. Pakistan J Med Heal Sci 2011; 5: 597–599. [Google Scholar]
- 15.Nugud AA, Nugud S. Long-Standing asymptomatic inguinoscrotal hernia. Sultan Qaboos Univ Med J 2017; 17: e250–e251. 10.18295/squmj.2016.17.02.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lajevardi SS, Gundara JS, Collins SAet al. Acute gastric rupture in a giant inguinoscrotal hernia. J Gastrointest Surg 2015; 19: 2283–2285. 10.1007/s11605-015-2916-y [DOI] [PubMed] [Google Scholar]
- 17.Fazekas B, Frecker P, Francis Let al. Aspiration pneumonia as a complication of a rare type of hernia. Int J Surg Case Rep 2014; 5: 1061–1063. 10.1016/j.ijscr.2014.10.070 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Creedon L, Peacock O, Singh Ret al. Gastric outlet obstruction secondary to incarcerated pylorus in an inguinal hernia. Ann R Coll Surg Engl 2014; 96: e26–e27. 10.1308/003588414X13946184901245 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ogul H, Gündoğdu H, Aslan Aet al. Bilateral inguinal hernia with uncommon content. Can J Gastroenterol 2013; 27: 14. 10.1155/2013/873702 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Naraynsingh V, Sieunarine K, Raju G. Recurrent gastric outlet obstruction due to an inguinal hernia. Postgrad Med J 1987; 63: 905–906. 10.1136/pgmj.63.744.905 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Padmanabhan AI, Lowenfels AB. Letter: An unusual hernia. JAMA 1976; 235: 2813. 10.1001/jama.1976.03260520013005 [DOI] [PubMed] [Google Scholar]
- 22.Davey WW, Strange SLet al. The stomach as a content of inguinal and femoral herniae. Br J Surg 1954; 41: 651–658. 10.1002/bjs.18004117023 [DOI] [PubMed] [Google Scholar]
- 23.Ferdinand E, Amir R, Manjunath Set al. Serendipity of giant proportions. Clin Gastroenterol Hepatol 2013; 11(10): A25–26. 10.1016/j.cgh.2013.01.009 [DOI] [PubMed] [Google Scholar]
- 24.Gue S. Spontaneous rupture of stomach. A rare complication of inguinal hernia. Br J Surg 1970; 57: 154–155. 10.1002/bjs.1800570218 [DOI] [PubMed] [Google Scholar]
- 25.Fitzgibbons RJ, Jonasson O, Gibbs Jet al. The development of a clinical trial to determine if watchful waiting is an acceptable alternative to routine herniorrhaphy for patients with minimal or no hernia symptoms. J Am Coll Surg 2003; 196: 737–742. 10.1016/S1072-7515(03)00003-6 [DOI] [PubMed] [Google Scholar]
- 26.Sayad P, Abdo Z, Cacchione Ret al. Incidence of incipient contralateral hernia during laparoscopic hernia repair. Surg Endosc 2000; 14: 543–545. 10.1007/s004640000101 [DOI] [PubMed] [Google Scholar]
- 27.Neumayer L, Giobbie-Hurder A, Jonasson Oet al. Open mesh versus laparoscopic mesh repair of inguinal hernia. N Engl J Med 2004; 350: 1819–1827. 10.1056/NEJMoa040093 [DOI] [PubMed] [Google Scholar]
- 28.Tarasconi A, Coccolini F, Biffl WLet al. Perforated and bleeding peptic ulcer: WSES guidelines. World J Emerg Surg 2020; 15: 1–24. 10.1186/s13017-019-0283-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Becher RD, Peitzman AB, Sperry JLet al. Damage control operations in non-trauma patients: defining criteria for the staged rapid source control laparotomy in emergency general surgery. World J Emerg Surg 2016; 11: 10. 10.1186/s13017-016-0067-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Vrijland WW, van den Tol MP, Luijendijk RWet al. Randomized clinical trial of non-mesh versus mesh repair of primary inguinal hernia. Br J Surg 2002; 89: 293–297. 10.1046/j.0007-1323.2001.02030.x [DOI] [PubMed] [Google Scholar]
- 31.Lockhart K, Dunn D, Teo Set al. Mesh versus non-mesh for inguinal and femoral hernia repair. Cochrane Database of Systematic Reviews 2018; 9: CD011517. 10.1002/14651858.CD011517.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Oprea V, Matei O, Gheorghescu Det al. Progressive preoperative pneumoperitoneum (PPP) as an adjunct for surgery of hernias with loss of domain. Chirurgia (Bucur) 2014; 109: 664–669. [PubMed] [Google Scholar]
- 33.Ramirez OM, Ruas E, Dellon AL. ‘Components separation’ method for closure of abdominal-wall defects. Plast Reconstr Surg 1990; 86: 519–526. 10.1097/00006534-199009000-00023 [DOI] [PubMed] [Google Scholar]
- 34.Staubitz JI, Gassmann P, Kauff DWet al. Surgical treatment strategies for giant inguinoscrotal hernia - A case report with review of the literature. BMC Surg 2017; 17: 135. 10.1186/s12893-017-0331-x [DOI] [PMC free article] [PubMed] [Google Scholar]