Abstract
The Nipah virus is a zoonotic infection that can potentially be transmitted from person to person as well as through ingesting contaminated food. It has a high fatality rate, and no treatment or cure at present. Several nations in South Asia have reported Nipah virus outbreaks occurred during a particular season of the year. Since it was first found in Bangladesh in 2001, there have been a total of 335 people infected with it, and 237 of those people have passed away as a result of their infection. With increased public awareness, community engagement, and preventative measures, this potentially fatal virus has been suppressed. Yet, following a pandemic and a considerable increase in the health burden, the transmission rate continuously increased over a few years, indicating that there is a growing possibility to become a global public health concern. Without effective vaccines and reliable treatment options, its capacity for human‐to‐human transmission and potential to spread throughout the area could result in a disastrous public health emergency worldwide.
Keywords: henipavirus, henipavirus infections, Nipah virus, Nipah virus infection, paramyxovirus, viral encephalitis
1. BACKGROUND
The recent outbreak of deadly Nipah virus (NiV) infection has raised concern and fear among the general population, who are still fighting the COVID‐19. 1 According to the World Health Organization (WHO), NiV infection is a zoonotic infection that typically transmits from animal to human. But it may also get transmitted through food contaminated with the virus. Even human transmission of this deadly virus is possible. According to WHO, the mortality rate of infected population by the NiV is extremely high. 2 Fruit bats of the Pteropus genus are a natural reservoir host of the NiV. 3 But there have been several reported cases of human‐to‐human transmission. 4 This deadly virus has been found in urine and respiratory secretions of infected individuals. 5 Besides, the NiV is an RNA virus that is prone to mutation. 6 This virus may mutate suddenly and increase its power of transmission and fatality. Similar to COVID‐19, the NiV is a potential virus that may cause a pandemic on a global scale. 7 There are no established treatments against the NiV infection. The care for infected patients primarily consists of symptomatic treatments and supportive. 8 Its high mortality rate is a matter of concern. Moreover, the absence of efficacious treatment measures makes this virus a significant threat to the global public health. 9 The outbreak in Bangladesh may be a wake‐up call to the rest of the world. Hence, scientists, the government, and epidemiologists should be aware and take precautionary steps as quickly as possible.
2. HISTORY OF NIPAH VIRUS INFECTION
From 1998 to 1999, NiV infection among humans was first identified. 10 At that time, the pig was associated with the NiV outbreak. Malaysia launched a pig culling operation to curb the epidemic. This outbreak killed 105 people in Malaysia. 11 By this time, the outbreak had spread to Singapore. The country used to import pigs from Malaysia. The virus entered Singapore through the pig slaughterhouse. It could only kill one person due to the prompt action of the government of Singapore. The Singaporean authorities prohibited the export of pigs from Malaysia to prevent a possible epidemic. 12 In early 2001, an encephalitis outbreak due to the NiV was recorded in Siliguri, India. It killed 45 infected individuals. The series of events suggest the association between the outbreaks. 13 Another outbreak in the Nadia district in India killed five people with a 100% mortality rate. 14 In 2018, the NiV outbreak in Kerala caused 21 deaths. 15 In 2014, the NiV was found in people with neurological diseases like encephalitis, meningitis, and so forth, in the Philippines. Several horses died during that period as well. Therefore, the horse was thought to act as an intermediate host in this outbreak. 16 At first, researchers identified the virus causing the outbreak as the Japanese encephalitis virus. Scientists later identified the virus and its reservoir host as bats. 3 The epidemics in Malaysia and Singapore happened because of pigs, as the pigs may have been the intermediate hosts. The pigs may have consumed bat‐contaminated fruits.
3. EPIDEMIOLOGY OF NIPAH VIRUS INFECTION
Although the NiV is zoonotic disease but it can be transmitted through contaminated food and date palm sap (DPS). NiV is found in the secretions of bats. In addition, it can be transmitted through body secretions such as saliva and respiratory droplets of an infected individual. A survey in Goalondo suggests that people who climb trees are more susceptible to infection. 17 , 18 According to the WHO, the fatality rate due to NiV infection ranges between 40% and 75%. 2 Institute of Epidemiology, Disease Control and Research (IEEDCR), Bangladesh estimated that the local death rate due to NiV infection is approximately 73%. Notwithstanding the fact that the fatality rate is contingent on the clinical and epidemiological knowledge of the outbreak region, it is sufficient to cause global alarm. NiV infection causes a severe inflammation in the brain called encephalitis. The high mortality rate of NiV infection associated with encephalitis is a common feature. 19 There are currently no specific treatments for this viral infection. The majority of treatments for those infected with the NiV are symptomatic and supportive. Anticonvulsants are used for seizure prevention. Treatment is given against secondary infections. Those suffering from respiratory distress are administered ventilation and intensive care unit treatments. Ribavirin was administered as a broad‐spectrum antiviral during the outbreak in Malaysia, which lowered mortality somewhat. 20 In Singapore, Acyclovir was utilized. But, its effectiveness against the infection is inexplicable. In India, anti‐G and anti‐F monoclonal antibodies were utilized in emergency situations. 21
4. RECENT NIPAH VIRUS OUTBREAK IN BANGLADESH
We have seen several outbreaks of NiV infection in India and some other South Asian countries. Bangladesh is three‐sided bordered by India. Therefore, the country recorded its very first outbreak of NiV infection in 2001 along with India. NiV infection outbreaks are seasonal in Bangladesh. People suffered from encephalitis in the Meherpur district of Bangladesh. But the virus was not identified there. A similar event was seen in parts of the Naogaon district that killed eight people. Concerns were raised regarding the similarities between the events and their causative agent. After that, samples were sent to CDC. CDC reported that the disease was caused by the NiV. 22 After 2001, NiV outbreaks were reported annually in India and Bangladesh. 23 Since 2001, seasonal outbreaks of NiV infection between December and May, consistent with the DPS harvesting season in the country from November to March. Reported cases ranged from 0 to 67 from 2001 to 2016. The country observed a reduced number of reported cases from 2016 due to the mass awareness campaign against the consumption of raw DPS.
However, between January 4, 2013, to February 13, 2023, 11 cases (10 laboratories confirmed and one probable) of NiV infection cases and eight associated deaths were reported from seven districts of two divisions in Bangladesh. It is the highest number of reported NiV cases and deaths after 2015 when the country recorded 15 NiV cases and 11 associated deaths (WHO). Dhaka division reported six NiV cases and four associated deaths (6/4) from the districts of Narsingdi (1/1), Rajbari (4/3), and Shariatpur (1/0). Rajshahi Division reported five cases and four related deaths (5/4) from the districts of Naogaon (2/1), Natore (1/1), Pabna (1/1), and Rajshahi (1/1). The average case fatality rate is 73% which is very alarming. Among the 11 cases, 4 were females, and 7 were males. The median age of the case was 16 years ranging from 15 to 50. Ten NiV cases had a raw DPS drinking history out of 11. The median incubation period was 14 days ranging from 3 to 15. After the onset of symptoms, all 11 cases were hospitalized. 24 Year wise number of reported NiV cases and deaths in Bangladesh from 2001 to 2013 are presented in Figure 1. 24 , 25 A geographical distribution‐comparison of so far and this year's outbreak in Bangladesh is shown in Figure 2. 24 , 25
Figure 1.
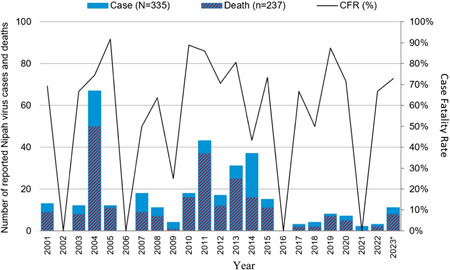
Number of reported Nipah virus cases and deaths from 2001 to 2023, Bangladesh. This figure has been adopted from the original work “Nipah virus disease–Bangladesh. Geneva: World Health Organization (WHO); 2023. Licence: CC BY‐NC‐SA 3.0 IGO.” This adoptation was not created by WHO. WHO is not responsible for the content or accuracy of this adoptation. The original edition shall be the binding and authentic edition. Source: Bangladesh Ministry of Health and Family Welfare. *As of 16 February, 2013.
Figure 2.
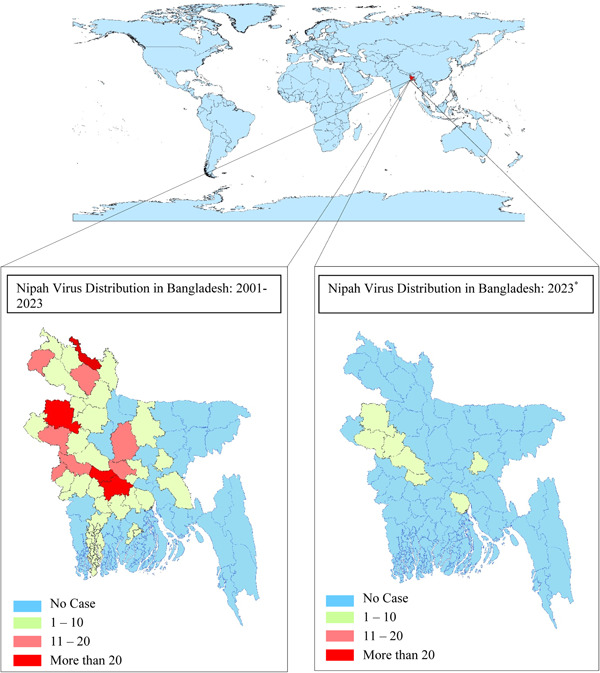
Comparison of Nipah virus distribution in Bangladesh. Source: Bangladesh Ministry of Health and Family Welfare. *As of February 16, 2023.
5. A POTENTIAL THREAT TO GLOBAL PUBLIC HEALTH
Current circumstances indicate that the NiV has the potential to cause global public health emergency. We have previously observed that the viral outbreak in Bangladesh extended to India. 13 Hence, the virus can circumvent regional borders and spread to adjacent nations. The proven instances of human‐to‐human transmission are a grave warning to the entire globe. 18 It can spread through saliva and respiratory droplets. Hence, there will inevitably be a case of secondary transmission. Past outbreaks indicate that domestic animals are responsible for the virus's propagation. Thus, domestic animals were slaughtered to combat the epidemic. Further outbreaks may result in the death of the cattle, and people may be forced to kill the animals as well. This will exacerbate the persistent global food shortage and developing agricultural issues. Infectious disease has a significant negative impact on society's socioeconomic balance as well. 26 The NiV is a related RNA virus to the coronavirus. Mutations of the RNA virus are a regular occurrence. Similar to the coronavirus, the NiV can undergo rapid mutations that increase its virulence, transmission, mortality, and morbidity. 27 Globally, infectious diseases have a negative impact on people's mental health. For example, the COVID‐19 pandemic has significantly affected the mental equilibrium of people of all ages. 28 Infected individuals with the NiV also exhibit depressive symptoms and other mental disorders. So, it can be hypothesized that the NiV is capable of causing a pandemic with catastrophic results.
6. RISK COMMUNICATION AND PREVENTATIVE MEASURES
As there are no effective treatments against the NiV infection, preventive measures should be strictly followed. Reports suggest that the raw DPS contaminated by a bat is responsible for the NiV infection in Bangladesh. Therefore, people should not be allowed to drink raw date palm juice. Besides, fruits partially eaten by bats should not be consumed as well. Seminars and workshops should be arranged for rural people not accustomed to following health care measures. Pigs and horses were responsible for the outbreaks in Malaysia and the Philippines, respectively. 11 , 16 So, the infected animals should be identified as quickly as possible and should be isolated. The infected animals might be killed by the government if needed. Supportive treatments like mechanical ventilation must be ensured throughout the country, specifically in the areas prone to outbreaks. Adequate supportive care will reduce the mortality rate as well. 2 Bats are the natural reservoir host of the NiV. So, areas inhabited by bats should be appropriately monitored. Human‐to‐human transmission is possible, so anyone who comes into direct contact with an infected person or eats contaminated fruit or raw DPS and develops symptoms like fever, headache, myalgia, vomiting, neurological issues, encephalitis, and respiratory distress should be isolated immediately to prevent secondary transmission. They should be kept inside a ward dedicated to NiV infection. They can only be discharged from there after getting a negative RT‐PCR result. As the incubation period is not fully elucidated, the discharged patients are also advised to get isolated for 21 days from the day of infection detection. 29 Unfortunately, no currently established therapeutics or vaccines are available against this virus. So, we have to emphasize prevention rather than treatment. The Old people is typically thought to be the most reluctant to alter their lifelong health behaviors. 30 Seminars targeting the old people should be arranged to raise awareness against this deadly virus. Healthcare professionals should wear PPE while providing health services. Early detection is the key to preventing any outbreaks caused by infectious diseases. Hence, the suspected person should be tested quickly. The government needs to ensure diagnostic facilities in the affected areas. BSL‐4 must be maintained in the lab to prevent further infection while handling. Antiviral drugs may be prescribed for infected people. WHO has identified NiV infection as a priority disease for research. Other concerned authorities should also come forward to raise awareness among the general population regarding this new enemy. Currently, there are no vaccines or therapeutics available against the NiV. Scientists must take prompt action to develop an effective vaccine against the NiV, as they have already developed corona vaccines very quickly. 31 Besides, effective antiviral drugs must be discovered and formulated to treat this disease. Affected people show signs of depression and other symptoms of neurological disorders in the long run. These need to be correctly addressed and effectively treated. People of all classes have been severely affected by COVID‐19. 32 The newer variants of COVID‐19 are always a headache to the world. 33 , 34 Among the existing pandemic, the world and its inhabitants are not ready for another pandemic.
7. COMMUNITY INVOLVEMENT IN EFFECTIVE RESPONSE
Moreover, the mental health of people worldwide has been affected by quarantine and isolation. This emerging virus may also cause people to follow the similar preventive measures, which will be very hard for the general population to deal with. Hence, healthcare professionals, government, and respective authorities should take necessary steps to prevent the outbreak and raise awareness among the general population. Authorities concerned with the public health should always keep monitoring the emergence of infectious diseases to take prompt action. 35 Lessons learnt from COVID‐19 pandemic may help to direct health policies to combat this new emerging infectious disease. 36 Furthermore, the concerned health authorities should create comprehensive preventive and therapeutic strategies to counteract the recent rise of this viral infection. They should develop evidence‐based treatment and management guidelines. 37 Researchers should also conduct studies to develop vaccines and therapeutics. Considering the recent outbreaks of COVID‐19 and monkeypox, the researchers and respective authorities should be aware of the NiV outbreak. More research should be conducted to elaborate on the nature, symptoms, and treatments of NiV infection.
8. CONCLUSION
The latest outbreak of NiV in Bangladesh, which resulted in an extremely high case fatality rate, will create pressure on public health systems already struggling to cope with the COVID‐19. Due to the high mortality rate associated with this virus, it has the potential to cause death and is even more dangerous than coronavirus disease. In addition, it can be transmitted from human to human makes it a possible risk for another pandemic. Therefore, the respective authorities should take the necessary actions to stop the current spread of the virus.
AUTHOR CONTRIBUTIONS
Nazmunnahar: Conceptualization; data curation; writing—original draft. Iftekhar Ahmed: Conceptualization; data curation; writing—original draft. A. S. M. Roknuzzaman: Conceptualization; supervision; writing—review and editing. Md. Rabiul Islam: Conceptualization; supervision; writing—review and editing.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflict of interest.
TRANSPARENCY STATEMENT
The lead author Md. Rabiul Islam affirms that this manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
Nazmunnahar, Ahmed I, Roknuzzaman ASM, Islam MR. Recent Nipah virus outbreak in Bangladesh could be a threat for global public health: a brief report. Health Sci Rep. 2023;6:e1423. 10.1002/hsr2.1423
DATA AVAILABILITY STATEMENT
Data available on request from the authors.
REFERENCES
- 1. The Daily Star . Five die of NiV this year. The Daily Star. January 29, 2023. Accessed March 1, 2023. http://www.thedailystar.net/health/disease/news/five-die-Nipah-virus-year-3233881
- 2. World Health Organization . NiV. May 30, 2018. Accessed February 27, 2023. https://www.who.int/news-room/fact-sheets/detail/nipah-virus
- 3. Clayton BA, Wang LF, Marsh GA. Henipaviruses: an updated review focusing on the pteropid reservoir and features of transmission. Zoonoses Public Health. 2013;60(1):69‐83. 10.1111/j.1863-2378.2012.01501.x [DOI] [PubMed] [Google Scholar]
- 4. Luby SP, Gurley ES, Hossain MJ. Transmission of human infection with nipah virus. Clin Infect Dis. 2009;49(11):1743‐1748. 10.1086/647951 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Chua KB, Lam SK, Goh KJ, et al. The presence of Nipah virus in respiratory secretions and urine of patients during an outbreak of Nipah virus encephalitis in Malaysia. J Infect. 2001;42(1):40‐43. 10.1053/jinf.2000.0782 [DOI] [PubMed] [Google Scholar]
- 6. Carrasco‐Hernandez R, Jácome R, López Vidal Y, Ponce de León S. Are RNA viruses candidate agents for the next global pandemic? A review. ILAR J. 2017;58(3):343‐358. 10.1093/ilar/ilx026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Devnath P, Masud HMAA. Nipah virus: a potential pandemic agent in the context of the current severe acute respiratory syndrome coronavirus 2 pandemic. New Microbes New Infect. 2021;41:100873. 10.1016/j.nmni.2021.100873 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Ang BSP, Lim TCC, Wang L. Nipah virus infection. J Clin Microbiol. 2018;56(6):e01875‐17. 10.1128/JCM.01875-17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. World Health Organization . Nipah virus. 2018. Accessed June 22, 2023. https://www.who.int/news-room/fact-sheets/detail/nipah-virus
- 10. Chua KB. Nipah virus outbreak in Malaysia. J Clin Virol. 2003;26(3):265‐275. 10.1016/s1386-6532(02)00268-8 [DOI] [PubMed] [Google Scholar]
- 11. Lam SK, Chua KB. Nipah virus encephalitis outbreak in Malaysia. Clin Infect Dis. 2002;34(suppl 2):S48‐S51. 10.1086/338818 [DOI] [PubMed] [Google Scholar]
- 12. Paton NI, Leo YS, Zaki SR, et al. Outbreak of Nipah‐virus infection among abattoir workers in Singapore. Lancet. 1999;354(9186):1253‐1256. 10.1016/S0140-6736(99)04379-2 [DOI] [PubMed] [Google Scholar]
- 13. Chadha MS, Comer JA, Lowe L, et al. Nipah virus‐associated encephalitis outbreak, Siliguri, India. Emerg Infect Dis. 2006;12(2):235‐240. 10.3201/eid1202.051247 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Kulkarni DD, Tosh C, Venkatesh G, Senthil Kumar D. Nipah virus infection: current scenario. Indian J Virol. 2013;24(3):398‐408. 10.1007/s13337-013-0171-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Arunkumar G, Chandni R, Mourya DT, et al. Outbreak investigation of Nipah virus disease in Kerala, India, 2018. J Infect Dis. 2019;219(12):1867‐1878. 10.1093/infdis/jiy612 [DOI] [PubMed] [Google Scholar]
- 16. Ching PKG, de los Reyes VC, Sucaldito MN, et al. Outbreak of henipavirus infection, Philippines, 2014. Emerg Infect Dis. 2015;21(2):328‐331. 10.3201/eid2102.141433 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Montgomery JM, Hossain MJ, Gurley E, et al. Risk factors for Nipah virus encephalitis in Bangladesh. Emerg Infect Dis. 2008;14(10):1526‐1532. 10.3201/eid1410.060507 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Gurley ES, Montgomery JM, Hossain MJ, et al. Person‐to‐person transmission of Nipah virus in a Bangladeshi community. Emerg Infect Dis. 2007;13(7):1031‐1037. 10.3201/eid1307.061128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Alam AM. Nipah virus, an emerging zoonotic disease causing fatal encephalitis. Clin Med. 2022;22(4):348‐352. 10.7861/clinmed.2022-0166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Chong HT, Kamarulzaman A, Tan CT, et al. Treatment of acute Nipah encephalitis with ribavirin. Ann Neurol. 2001;49(6):810‐813. 10.1002/ana.1062 [DOI] [PubMed] [Google Scholar]
- 21. Aditi ShariffM, Shariff M. Nipah virus infection: a review. Epidemiol Infect. 2019;147:e95. 10.1017/S0950268819000086 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Hsu VP, Hossain MJ, Parashar UD, et al. Nipah virus encephalitis reemergence, Bangladesh. Emerg Infect Dis. 2004;10(12):2082‐2087. 10.3201/eid1012.040701 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Islam MS, Sazzad HMS, Satter SM, et al. Nipah virus transmission from bats to humans associated with drinking traditional liquor made from date palm sap, Bangladesh, 2011–2014. Emerg Infect Dis. 2016;22(4):664‐670. 10.3201/eid2204.151747 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. World Health Organization . Nipah virus infection – Bangladesh. 2023. Accessed March 2, 2023. https://www.who.int/emergencies/disease-outbreak-news/item/2023-DON442
- 25. Ministry of Health & Family Welfare . Government of the People's Republic of Bangladesh. Accessed March 2, 2023. http://www.mohfw.gov.bd/
- 26. Nicola M, Alsafi Z, Sohrabi C, et al. The socio‐economic implications of the coronavirus pandemic (COVID‐19): a review. Int J Surg. 2020;78:185‐193. 10.1016/j.ijsu.2020.04.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. El‐Shabasy RM, Nayel MA, Taher MM, Abdelmonem R, Shoueir KR, Kenawy ER. Three waves changes, new variant strains, and vaccination effect against COVID‐19 pandemic. Int J Biiol Macromol. 2022;204:161‐168. 10.1016/j.ijbiomac.2022.01.118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Das R, Hasan MR, Daria S, Islam MR. Impact of COVID‐19 pandemic on mental health among general Bangladeshi population: a cross‐sectional study. BMJ Open. 2021;11(4):e045727. 10.1136/bmjopen-2020-045727 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Ministry of Health & Family Welfare‐Government of India . NiV guidelines. National Centre for Disease Control (NCDC). February 27, 2023. Accessed February 28, 2023. https://ncdc.mohfw.gov.in/index4.php?lang=1&level=0&linkid=113&lid=228
- 30. Agha M, Agha R. The rising prevalence of obesity: part B‐public health policy solutions. Int J Surg Oncol. 2017;2(7):e19. 10.1097/IJ9.0000000000000019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Li M, Wang H, Tian L, et al. COVID‐19 vaccine development: milestones, lessons and prospects. Signal Transduct Target Ther. 2022;7(1):146. 10.1038/s41392-022-00996-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Sohrabi C, Mathew G, Franchi T, et al. Impact of the coronavirus (COVID‐19) pandemic on scientific research and implications for clinical academic training ‐ A review. Int J Surg. 2021;86:57‐63. 10.1016/j.ijsu.2020.12.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Akif A, Bhuiyan MA, Islam MR. SARS‐COV‐2 omicron subvariant BF.7 is again triggering the Covid fear: what we need to know and what we should do? J Med Virol. 2023;95:e28551. 10.1002/jmv.28551 [DOI] [PubMed] [Google Scholar]
- 34. Nazmunnahar B, Ahmed I, Islam MR. Risk evaluation and mitigation strategies for newly detected SARS‐CoV‐2 Omicron BF.7 subvariant: a brief report. Health Sci Rep. 2023;6:e1127. 10.1002/hsr2.1127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Sohrabi C, Alsafi Z, O'Neill N, et al. World Health Organization declares global emergency: a review of the 2019 novel coronavirus (COVID‐19). Int J Surg. 2020;76:71‐76. 10.1016/j.ijsu.2020.02.034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Nicola M, Sohrabi C, Mathew G, et al. Health policy and leadership models during the COVID‐19 pandemic: a review. Int J Surg. 2020;81:122‐129. 10.1016/j.ijsu.2020.07.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Nicola M, O'Neill N, Sohrabi C, Khan M, Agha M, Agha R. Evidence based management guideline for the COVID‐19 pandemic ‐ review article. Int J Surg. 2020;77:206‐216. 10.1016/j.ijsu.2020.04.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data available on request from the authors.


